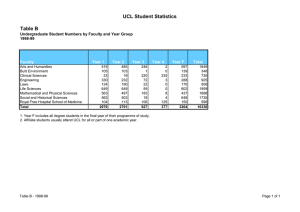
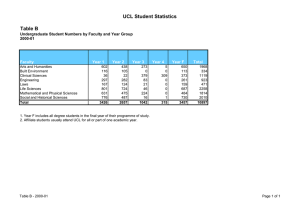
Population Health 4 UCL SChooL of Life and MediCaL SCienCeS
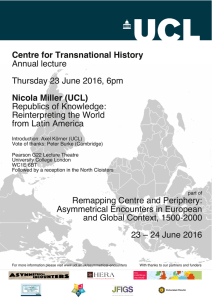
advertisement

Population Health UCL School of Life and Medical Sciences Creating knowledge, achieving impact 4 PREFACE UCL’s School of Life and Medical Sciences encompasses arguably the greatest concentration of biomedical science and population health expertise in Europe. Our performance in the UK’s last Research Assessment Exercise was outstanding, and for most key measures the School comfortably tops UK league tables. In part because of UCL’s size and organisational complexity, the scale of its achievements is not always apparent. This publication, one of four, seeks to address this. Our recent reorganisation, with the creation of four new Faculties, has been designed to create a more coherent structure, of which the Faculty of Population Health Sciences headed by the Dean, Professor Graham Hart, is a clear example. But the School’s restructuring has also placed great emphasis on cross-Faculty interactions and interdisciplinary research – and indeed on interactions with departments outside the School across UCL. Such interdisciplinary endeavour is promoted through the establishment of ‘Domains’, inclusive strategically led fluid networks. Nowhere is this more important than in the field of population health given its myriad determinants – including, for example, economic status, the built environment and cultural differences in health beliefs, as well as more obvious genetic and environmental factors. Professor Anne Johnson chairs UCL’s Population Health Domain, working closely with the Faculty as well as colleagues in other disciplines. UCL is acutely aware that scientific advance of real relevance to society is not only aided by an interdisciplinary approach but also through collaborative strategic alliances with other research-intensive institutions with complementary strengths. Our founding partner status in the new Francis Crick Institute engages us in what will be the European powerhouse of biomedical research expertise. In the population health field our growing collaboration with our Bloomsbury neighbours, the London School of Hygiene and Tropical Medicine, is fuelling exciting developments in the fields of genetic epidemiology and pathogen research and we are both proud to be members of the new NIHR School for Public Health Research. The breadth and quality of our research creates almost unique opportunities. Whatever an individual’s interests, there is likely to be a worldleading expert with complementary interests nearby. Thanks to our size, we have been able to establish support services and platform technologies to accelerate research. Our highly productive links to the health service, through UCL Partners, provides access to unmatched clinical expertise and large patient groups. The School’s academic environment is one in which intellectual curiosity can prosper, while a high priority is also given to the practical application of knowledge to improve health and quality of life. This can take many forms, including commercialisation of new products as well as developing and informing health and social policy, and engaging with important stakeholders, including the public. In keeping with UCL’s traditions, there is a radical element to our work, with national and global inequalities a key concern. This publication, one of four (see right), showcases some of the outstanding research in population health being carried out within the School and with collaborators across UCL, in London, nationally and internationally. It is impossible to be comprehensive, but the stories give a flavour of the breadth, quality and impact of the School’s research. Looking forward, our aims are to enhance and expand our research to ensure we remain a global leader, and to see more people benefit from the groundbreaking research being carried out across the School. Sir John Tooke Vice-Provost (Health) and Head of the UCL School of Life and Medical Sciences. 1 Basic Life Sciences: ‘Discovery’ research, from molecules to ecosystems. 2 Translation and Experimental Medicine: Driving translation to benefit patients’ health and well-being. 3 Neuroscience and Mental Health: The science of the brain and nervous system, from synapse to social interactions. 4 Population Health: Protecting and improving the health of populations, UK and globally. CONTENTS Overview: The health of the people 2 The aim of UCL’s Population Health research is to keep people healthier for longer and to reduce health inequalities. Section 1: Women and children first 4 How cohort- and community-based studies help to safeguard the health of women and infants. Feature: Let’s talk about sex: The National Survey of Sexual Attitudes and Lifestyles 12 Section 2: Young people and transition to adulthood 14 A succession of birth cohorts has shed light on the health, development and welfare of generations of UK children. 20 Section 3: The middle years How adult life is shaped by past experience, and influences our ‘third age’. Feature: The heart of the civil service: The Whitehall studies 30 Section 4: How to age successfully 32 Population studies have highlighted key factors contributing to a healthy old age. Feature: Sixty-five years young: The 1946 Birth Cohort 38 Section 5: Global health research 40 Tackling public health threats outside the UK, from maternal health to climate change. UCL institutes, support services, partners, funding and sponsors. 46 POPULATION HEALTH UCL School of Life and Medical Sciences 1 The health of the people The aim of UCL’s Population Health research is to keep people healthier for longer and to reduce health inequalities. Jeremy Bentham, an influential figure in UCL’s history, is perhaps best known for his utilitarian ethics – promoting “the greatest good for the greatest number of people”. While that may not exactly translate to UCL’s current Population Health research, it does capture a flavour of the domain’s aims. Modern science has proven remarkably successful at developing interventions that, unlike most remedies from previous eras, actually work. More are needed, of course, but their success has transformed the health landscape of the UK, generating new priorities: how do we prevent people becoming ill? How do we deal with chronic conditions? How can we deliver healthcare most effectively? Moreover, health is not simply ‘absence of disease’ but encompasses quality of life and mental well-being, not just for their own sake but also because they can protect from physical and mental ill-health. 2 If a goal is a Bentham-esque “the greatest health for the greatest number of people”, where should attention be focused? On the one hand, almost every aspect of modern life has some impact on our health – what we eat, what exercise we take, what germs we encounter, how we are treated by others, whether we smoke, what happens at work (if we have a job). How these factors affect our health is complex, subtle and difficult to disentangle. Exposure to a virus might render us sick within a few days; an extra burger every week might take decades to have an effect. Moreover, influences accumulate over a lifetime. Our education, how we were parented, even our birthweight can influence how healthy we are years and decades later. On the other hand, when our health does fail, we rely on the NHS to put it right. Our first port of call is usually our GP and primary care; we may then be referred on to ...birth cohorts have focused attention on the long-lasting effects of early-life events, highlighting childhood as a crucial phase to intervene not just for the immediate benefit of children but to alter the trajectory of entire lives. specialist secondary care. Collectively, these systems account for a substantial proportion of national expenditure, and play a big part in maintaining the nation’s health. A research agenda The Population Health research agenda therefore spans work within healthcare systems (principally primary care) and within society. The common questions are: how do we keep people healthier for longer? And how do we ensure that health gains are shared equitably? Large cohorts (healthy populations as well as patients) are a major focus: UCL researchers lead healthrelated studies on several major cohorts, including the UK’s national birth POPULATION HEALTH UCL School of Life and Medical Sciences cohorts (1946, 1958 and 2000). Some £28 million has recently been announced for a major new birth cohort, led by Professor Carol Dezateux. UCL has also played a major role in the groundbreaking ‘Whitehall’ cohorts. In Whitehall I, Professor Sir Michael Marmot identified a strong ‘socioeconomic gradient’ – people’s health was dependent on their position within a social hierarchy. These findings helped to establish the field of healthcare inequalities, in which Professor Marmot remains a world-recognised authority. Birth cohorts – and comparisons between them – have also emphasised the ‘life course’ perspective on disease. Health is dependent on past experience as well as current circumstances. In particular, birth cohorts have focused attention on the long-lasting effects of early-life events, highlighting childhood as a crucial phase to intervene not just for the immediate benefit of children but to alter the trajectory of entire lives. Cohorts have traditionally focused on environmental influences, but are increasingly integrating genetic approaches. Genes influence biology and health throughout life. Moreover, there is extensive crosstalk between genes and environment – it is increasingly meaningless to talk about the effects of nature and nurture as the two are so intertwined. Technological advances have paved the way for large-scale genetic studies, ushering in a new era of ‘genomic epidemiology’. Disease-specific cohorts are also important, particularly in HIV research. UCL researchers have been involved in some of the world’s largest and longestrunning HIV patient cohorts, providing key information on treatment and drug resistance. Study of health behaviours is becoming an increasingly important area. Considerable work is undertaken to document behaviours relevant to health, for example Health Surveys for England and the National Survey of Sexual Attitudes and Lifestyles (Natsal). Other projects have attempted to modify behaviours – not always, it has to be said, with a great deal of success. There is thus a need to gain a better understanding of why people behave as they do and what kinds of interventions lead to behaviour change at individual and population levels. Primary care UCL has major programmes of research in primary care, particularly around mental health and ageing, with several nationally important trials being coordinated in the ‘Priment’ Clinical Trials Unit. A large programme of applied health research is examining issues around healthcare organisation and delivery. UCL researchers also contribute to the development of health policy, as advisers to the Department of Health, through work on advisory committees and drafting guidelines for bodies such as the National Institute for Health and Clinical Excellence (NICE). ‘Data mining’ of electronic patient records is a further important focus. With the NHS, the UK is in the enviable position of having centrally coordinated data collection, offering enormous opportunities for analysis of routinely captured data to guide practice. UCL researchers have helped to develop data standards to facilitate effective use of health records, and many studies have analysed health record data in centralised repositories. An ‘e-health’ initiative aims to harness the enormous potential of the web and new technologies to deliver interventions to large numbers of people. PARTNERS FOR HEALTH By working closely with institutions delivering healthcare, UCL aims to ensure that its research benefits local populations. UCL has forged close links with some of London’s leading clinical centres. It has established UCL Partners with UCL Hospitals NHS Foundation Trust, the Royal Free Hampstead NHS Trust, Moorfield’s Eye Hospital NHS Foundation Trust and Great Ormond Street Hospital for Children NHS Trust. In 2009, UCL Partners was designated one of the UK’s first five Academic Health Science Centres. Its 11 priority areas reflect both UCL research strengths and local health priorities. UCL Partners aims to improve the health of communities in London and beyond served by its NHS members. Translation is further supported by the presence of three NIHR Biomedical Research Centres within UCL Partners – at UCLH, Moorfields and Great Ormond Street. New £165m five-year funding was awarded in 2011 by the NIHR, including support for a new Biomedical Research Unit specialising in dementia. UCL Partners is also a member of the North East London, North Central London and Essex (NECLES) Health Innovation and Education Cluster, with North-East London Health and Anglia Ruskin University and its health-service partners. Collectively, NECLES covers 5.8 million people (10 per cent of the UK population) and accounts for 10 per cent of NHS expenditure. A key aim of NECLES, and of a cross-cutting public health programme at UCL Partners, is to identify ways in which healthcare inequalities can be tackled. Ultimately, impact on people is likely to come through translation of promising laboratory science, improved delivery of healthcare, and initiatives in public health – all validated by rigorous research. Indeed, a major challenge is to integrate public services that protect and improve health, whether they fall within public health, primary care, secondary care or even social care – creating a ‘national health system’ that takes a citizen’s-eye view of health and wellbeing from cradle to grave. The wider context and globalisation, all with enormous potential to impact on health, have led to productive partnerships with a wide range of disciplines, from philosophy to urban planning. The scope of population health studies is broad. With an increasing appreciation of the wide range of factors affecting health – and their economic and sociopolitical context – research increasingly draws upon expertise in other areas of UCL. The momentous changes in the ‘anthropocene’ era – climate change, ecosystem destruction, urbanisation This naturally promotes a focus on global health issues. UCL has established an Institute for Global Health with its Grand Challenge Programme and helped to raise awareness of the health effects of climate change, particularly through the UCL–Lancet Commission, set up to focus attention on the potentially catastrophic impact of global climate change on health. UCL researchers also carry out important research overseas, particularly in Asia and Africa, where Professor Anthony Costello and colleagues have pioneered a participatory approach to the development of community interventions to improve neonatal health. UCL therefore aims to have an impact at local, national and international levels. A common theme is the insidious impact of social inequalities. Identifying these inequalities and how they come about – and trying to do something about them – is a core principle. Jeremy Bentham would surely have approved. POPULATION HEALTH UCL School of Life and Medical Sciences 3 SECTION 1 Women and children first The health of women and infants is rightly a high priority. Cohort- and community-based studies have done much to safeguard the health of both mothers and their babies. A major challenge now is to develop services that are organised around women’s needs and recognise the importance of life-course influences. 4 POPULATION HEALTH School of Life and Medical Sciences Childbirth was once the leading cause of death for women. Thanks to better healthcare and important social changes, death in childbirth is now extremely rare and neonatal mortality also greatly reduced (at least in developed countries). Recent years have seen greater survival of premature babies. The gestational age at which premature babies can survive has been progressively pushed back, through the use of steroids to promote lung development and surfactants to improve breathing after birth, as well as advances in paediatric intensive care. This might seem like an unqualified success, but saving the lives of extremely pre-term infants does have consequences. These have been documented in a unique long-term study, EPICure, which since 1995 has followed the progress of a cohort of babies born before 25 weeks (see page 7). Many of these infants had disabilities, and others have gone on to suffer problems with physical health (such as respiratory conditions) and mental development during childhood. Run in A lack of oxygen at birth – birth asphyxia – is one of the most common problems at birth, potentially leading to oxygen starvation and damage to the brain and, in the most severe cases, death. partnership with Nottingham and Warwick, EPICure is continuing to follow its cohort as they approach adolescence and adulthood. Its findings have been highly influential in policy debates about extreme prematurity. mild cooling – now the recommended treatment in the UK (see page 8 ). Interestingly, the noble gas xenon – coincidentally, discovered at UCL in the 19th century – may offer additional protection. Lung function is one of the most critical aspects of birth, as a newborn begins to acquire oxygen from the air around it. A lack of oxygen at birth – birth asphyxia – is one of the most common problems at birth, potentially leading to oxygen starvation and damage to the brain and, in the most severe cases, death. Cooling could have even more impact in developing countries, where birth asphyxia is very common. Dr Nikki Robertson and colleagues have explored the potential application of the procedure in resourcepoor settings, using locally available materials (such as widely used water bottles to hold cooled water). However, considerable thought needs to be given to implementation in countries with less welldeveloped healthcare infrastructures, especially when the potential for harm is great if techniques are misapplied. Currently work is underway to assess the feasibility of undertaking a trial. Research at UCL has had significant impact in this area. Advances in infant brain imaging, used to monitor energy expenditure, revealed a gap between oxygen starvation and subsequent death of nerve cells. Researchers have sought ways to intervene in this window to prevent damage, one of the most successful being POPULATION HEALTH UCL School of Life and Medical Sciences 5 The UCL Centre for Prenatal Genetic Diagnosis (PGD) was one of the first centres in the world to offer PGD, and continues to combine research with clinical service, advancing understanding of early human development as well as improving clinical practice. Much research in this area is undertaken at UCL Elizabeth Garrett Anderson Institute for Women’s Health, which enjoys a close relationship with University College London Hospital. In spring 2011 Professor Peter Brocklehurst moved from the University of Oxford to take over as Director, having previously collaborated extensively with researchers at the Institute. Professor Brocklehurst is one of the UK’s leading figures in perinatal research and is leading a number of trials of perinatal care. The Institute’s research covers four main themes: gynaecological cancer, maternal and fetal medicine, neonatology and reproductive health. Research on gynaecological 6 cancers, led by former Institute Director Professor Ian Jacobs and Professor Usha Menon, has been particularly notable. An important focus has been early detection of ovarian cancer, including large clinical trials assessing the value of different screening approaches (the UKCTOCS and FOCSS trials; see page 7). A key theme in maternal and fetal medicine is prenatal screening and prenatal genetic diagnosis (PGD). Professor Lyn Chitty, for example, is leading a five-year multicentre study exploring the potential of analysing fetal DNA in the maternal bloodstream to diagnose Down syndrome. The UCL Centre for PGD was one of the first centres in the world to offer PGD, and continues to combine research with clinical service, advancing understanding of early human development as well as improving clinical practice. An important recent move has been the appointment of Professor Kypros Nicolaides, who now holds a joint appointment at UCL and King’s College London. A world-leading figure in fetal medicine, Professor Nicolaides’ research interests include early screening for fetal abnormalities and pregnancy complications. In collaboration with medical staff at Great Ormond Street Hospital, UCL researchers have also carried out innovative studies on postmortem magnetic resonance imaging of fetuses. There are understandable sensitivities about fetal post-mortems, particularly among some ethnic minority communities. Clinical trials comparing conventional and non-invasive approaches POPULATION HEALTH UCL School of Life and Medical Sciences suggest that high-resolution MRI could offer a noninvasive alternative way of characterising tissue damage. Population-based reproductive health research covers a range of areas, including an evaluation by Professor Judith Stephenson and colleagues of England’s National Teenage Pregnancy Strategy (see page 11). In terms of interventions, a large randomised controlled trial of peer-led sex education, RIPPLE, involved long-term (seven-year) follow up in 27 schools in England. The peer-led approach was popular with school students, and may have reduced the number of live births, but abortion rates were the same as in groups receiving teacher-led sex education1. 1 Stephenson J et al. The long-term effects of a peer-led sex education programme (RIPPLE): a cluster randomised trial in schools in England. PLoS Med. 2008;5(11):e224. Screening under the microscope Too much too young? The EPICure study has identified a host of long-term issues associated with extreme pre-term birth. Over the past decades great strides have been made in the survival of extremely pre-term infants. While a young life saved might seem an incontrovertible good thing, it soon became apparent that prematurity had significant consequences. The EPICure study was set up to assess this impact systematically, and has documented a wide-range of issues associated with extreme prematurity as children develop. Begun in 1995, the EPICure study, led by Professor Neil Marlow with colleagues in Nottingham, Queen Mary College, Sheffield and Warwick, is an ambitious and influential study of all births before 25 weeks and 6 days gestation. The 314 survivors have been followed ever since, with major assessments at age six and age 11. The study’s findings have shed important light on the challenges faced by these children and their families, and done much to shape policy in the difficult area of extremely pre-term birth. At 30 months, 24 per cent of survivors were categorised as having severe difficulties. By age six, a comparison with peers revealed significant deficits, particularly in cognitive performance – almost twice as many, 41 per cent, showed general cognitive deficits. Assessments at 11 years of age have shown increased risk for behavioural and emotional disorders, with extremely preterm children being more than three times more likely to have a psychiatric disorder than classmates (23 per cent). Around one in eight attended special schools and more than half of those in mainstream education had special educational needs. The children also showed physical problems, with 78 per cent showing abnormalities in lung function. The EPICure study has also begun to assess both the economic and personal impact of extreme prematurity, using quality of life questionnaires. Planning is underway to survey the participants again at age 19. In 2006, a follow-up study, EPICure2, was launched. This has documented a significant increase in the number of babies born extremely pre-term, but survival is improving and infants are now less likely to be seriously affected. This unique study is thus continuing to provide objective data on a particularly difficult area of health policy. Marlow N et al. Neurologic and developmental disability at six years of age after extremely preterm birth. N Engl J Med. 2005;352(1):9–19. Lum S et al. Nature and severity of lung function abnormalities in extremely pre-term children at 11 years of age. Eur Respir J. 2011;37(5):1199–207. Johnson S et al. Psychiatric disorders in extremely preterm children: longitudinal finding at age 11 years in the EPICure study. J Am Acad Child Adolesc Psychiatry. 2010;49(5):453–63.e1. Johnson S et al. Academic attainment and special educational needs in extremely preterm children at 11 years of age: the EPICure study. Arch Dis Child Fetal Neonatal Ed. 2009;94(4):F283–9. Petrou S et al. Economic costs and preference-based health-related quality of life outcomes associated with childhood psychiatric disorders. Br J Psychiatry. 2010;197:395–404. Large trials will reveal whether screening for ovarian cancer can save lives? Ovarian cancer is the most common gynaecological cancer and the fifth leading cause of death from cancer in women. As it is often detected late, survival rates are poor. There is therefore great interest in screening to detect cancer at earlier stages, when survival rates are much higher. Professor Usha Menon, Professor Ian Jacobs and colleagues are running large-scale trials to assess whether two screening techniques – a blood test and ultrasound – are suitable for widespread implementation. The first trial, UKCTOCS, is a randomised controlled trial comparing a blood test for CA-125 (a well-known marker for ovarian cancer) interpreted using a novel algorithm, transvaginal ultrasound and a control arm where screening is not used. The primary aim is to see whether screening will prevent deaths from ovarian cancer. The trial is also addressing psychological impacts, possible drawbacks (complications in women undergoing surgery after false positive results) and the financial cost of screening, and whether strategies based on a blood test or ultrasound would be more feasible for population screening. Involving some 202,000 women, the trial is the largest of its kind in the world. In the preliminary results from 100,000 women in the screen arms of the trial, ovarian cancer was identified in 87 women and missed by screening in 13 women. These results are encouraging and suggest that either of the two approaches could potentially be used in population screening programmes. However, a definitive answer will depend on the results of continued annual screening and long-term follow-up. This is due to be completed in 2014, when it will be clear whether screening has sufficient benefits on mortality to be worth implementing. A second trial, UKFOCCS, is targeting a specific population, those with either a family history of ovarian cancer or mutations in the breast cancer genes BRCA1 or BRCA2, which also increase the risk of ovarian cancer. The trial is assessing the value of fourmonthly blood tests and an annual ultrasound for this high-risk group. Around 5000 women are participating, and the study is due to complete by 2013. Professor Menon and colleagues are also leading the UK’s contribution to an international collaboration, the Ovarian Cancer Association Collaboration, searching for genetic risk factors for ovarian cancer. These studies should provide tools to stratify populations and provide an individualised risk assessment for women based on their genetic make-up. Menon U et al. Sensitivity and specificity of multimodal and ultrasound screening for ovarian cancer, and stage distribution of detected cancers: results of the prevalence screen of the UK Collaborative Trial of Ovarian Cancer Screening (UKCTOCS). Lancet Oncol. 2009;10(4):327–40. Menon U et al. Recruitment to multicentre trials – lessons from UKCTOCS: descriptive study. BMJ. 2008;337:a2079. Goode EL et al. A genome-wide association study identifies susceptibility loci for ovarian cancer at 2q31 and 8q24. Nature Genet. 2010;42(10): 874–9. POPULATION HEALTH UCL School of Life and Medical Sciences 7 A family affair Healing by degrees Pregnancy and childbirth can have a significant impact on the mental health of mothers and fathers. Cooling of babies suffering asphyxia at birth saves lives – and adding xenon to the mix might help even more survive. Childbirth is supposed to be a time of great joy, but the reality can be quite different. The stress of dealing with the needs of a fragile new life and the accompanying upheaval, lack of sleep and economic impact can be difficult to deal with, especially when combined with pre-existing mental health problems. Professor Irwin Nazareth and Dr Irene Petersen’s work on a population cohort including new mothers and their partners is shedding light on important issues, including parental depression and antidepressant use in pregnancy. The Health Improvement Network primary care database is one of the largest of its kind in the UK, containing information on more than 9 million patients (3.4 million active patients), equivalent to 40 million patient years of data. Using the database to pinpoint new mothers, Professor Nazareth’s team further identified a male in the same household, ultimately collecting data on 87,000 mother–father–child triads. By the time their child was 12 years old, 39 per cent of mothers and 21 per cent of fathers had experienced an episode of depression, but the risk of depression was highest during the first year after birth. The risk of postnatal depression in women is well-known, but these data confirm that depression in fathers is far from rare. The database has also provided insight into the treatment of pregnant women with depression. Although antidepressant use increased fourfold between 1992 and 2006, pregnant women were more likely to stop taking their medication, particularly during the first six weeks of pregnancy. Only 10 per cent of women treated before pregnancy still received antidepressants at the start of the third trimester, while 35 per cent of non-pregnant women were still being treated after a similar time period. The difference is likely to reflect concerns about the effects of antidepressants on an unborn child, but such risks have to be weighed against those associated with untreated depression. Mild cooling, ‘therapeutic hypothermia’, is now the recommended treatment in the UK for babies suffering birth asphyxia. Its origins lie in observations on infant brains made at UCL 30 years ago, as well as results gained on a unique animal model still being used by Dr Nikki Robertson and colleagues to optimise treatments. And a discovery made at UCL more than 100 years ago may yet hold the key to further advances. Although used by doctors for hundreds of years, cold treatments fell out of favour after the war. Neonatal use of cooling grew out of studies conducted at UCL in the early 1980s by Osmund Reynolds and colleagues, who discovered that there was a marked delay between oxygen deprivation in infants and the ensuing neural damage. Since then, researchers have sought ‘neuroprotective’ agents for use in this therapeutic window – cooling being one. Babies with birth asphyxia are now cooled by 3°C for three days. Reynolds established a model system – the piglet – in which to study this phenomenon and test possible neuroprotective approaches. As well as similarities in size and physiology, the same biomarkers of neural damage can be followed in both piglets and humans, providing a valuable ‘bridge’ from experimental studies to clinical application. Work on the piglet model helped to establish that mild cooling reduces the levels of death and disability caused by birth asphyxiation. It also helped refine treatments, identifying the optimal degree of cooling – too much cooling and damage starts to increase again – and the timing and duration of intervention. Cooling was initially thought to have a generic slowing effect on metabolism, but its effects are more subtle, influencing specific physiological pathways and programmed cell death (apoptosis). It may therefore be possible to enhance hypothermia’s actions by intervening in these pathways. By a curious quirk of fate, one possible agent is the noble gas xenon, isolated at UCL by William Ramsay in 1898. Experimental studies with xenon have been highly promising and a clinical trial at UCLH has just begun. Furthermore, in collaboration with the Institute of Neurology, Dr Robertson has identified another potential neuroprotectant – melatonin. Melatonin is a naturally occurring hormone, which influences circadian rhythms but also has anti-ageing and anti-oxidant effects. It too has an inhibitory effect on apoptosis and offers enhanced protection with cooling in the piglet model, and may yet join the unusual array of interventions for neonatal asphyxia. Petersen I, Gilbert RE, Evans SJ, Man SL, Nazareth I. Pregnancy as a major determinant for discontinuation of antidepressants: an analysis of data from The Health Improvement Network. J Clin Psychiatry. 2011;72(7):979–85. Davé S, Petersen I, Sherr L, Nazareth I. Incidence of maternal and paternal depression in primary care: a cohort study using a primary care database. Arch Pediatr Adolesc Med. 2010;164(11):1038-44. Iwata O et al. “Therapeutic time window” duration decreases with increasing severity of cerebral hypoxia-ischaemia under normothermia and delayed hypothermia in newborn piglets. Brain Res. 2007;1154:173–80. O’Brien FE et al. Delayed whole-body cooling to 33 or 35 degrees C and the development of impaired energy generation consequential to transient cerebral hypoxia-ischemia in the newborn piglet. Pediatrics. 2006;117(5):1549–59. Kelen D, Robertson NJ. Experimental treatments for hypoxic ischaemic encephalopathy. Early Hum Dev. 2010;86(6):369–77. Faulkner S et al. Xenon augmented hypothermia reduces early lactate/Nacetylaspartate and cell death in perinatal asphyxia. Ann Neurol. 2011;70(1):133–50. 8 POPULATION HEALTH UCL School of Life and Medical Sciences It should therefore be possible to arrange services that are sex-specific and life-stage-specific, so women can receive advice, support and services across a range of areas that are relevant to them at the current stage in their lives. A key aim going forward is to enhance service delivery, by developing a more integrated approach to women’s health based on women’s needs and wishes rather than the boundaries of traditional medical disciplines. Working with partners including the influential ‘Mumsnet’ website, Professor Stephenson’s team is applying this principle to antenatal care. To support this work, an online ‘longitudinal care record’ is being developed to capture information about women’s interactions with different parts of the health system through their pregnancies. Greater integration is also the aim of a project aiming to bring together services linked to sexual health and minor gynaecological problems, which has been well-received in initial stages. A more general theme is to consider women’s health within a life-course perspective. Women’s health follows a well-structured path, with reproductive landmarks at particular life stages (with due regard for the fact that many women will not have children). It should therefore be possible to arrange services that are sex-specific and life-stagespecific, so women can receive advice, support and services across a range of areas that are relevant to them at the current stage in their lives. This idea also draws on the life-course perspective emphasised by cohort studies, which have demonstrated how health issues important at one stage in life might have their roots much earlier (even in previous generations). It also reflects other key themes, such as prevention and patient-oriented service provision, as well as the hugely important social inequalities agenda, through which inequalities are perpetuated from generation to generation. Highly influential work has also been carried out at the Institute on intersex syndromes. For many years, feminising surgery was carried out on children with ambiguous genitalia. A review highlighting the detrimental adult outcomes of this practice, published by Dr Sarah Creighton in the Lancet, led to a complete re-evaluation of the role of feminising surgery in childhood2. As influenza virus poses a particular threat to pregnant women, they were a priority group for vaccination during the 2009 H1N1 pandemic. A prospective cohort study, carried out with the vaccine manufacturers, showed no deviation from routinely seen outcome measures, providing reassurance that the pandemic flu vaccine was safe for use in this important group3. Screening and detection Primary care The reproductive health of women and health of infants is also studied in other areas of UCL. Analysis of health records can be an important way of gathering information about pregnancy, childbirth and infant care. Linking health records to household arrangements, for example, has provided insight about antidepressant and antibiotic use by mothers and a surprisingly high incidence of paternal depression (see page 8). Primary care researchers at UCL, led by Professor Irwin Nazareth, were selected to explore the safety of H1N1 swine flu vaccination in pregnant women. Research at the UCL Institute of Child Health naturally also impinges on maternal and infant health. Several population-based studies have addressed early detection of potentially hazardous infections or inherited conditions. In a study comparing countries across Europe, Professor Ruth Gilbert and colleagues found that identifying the singlecelled parasite Toxoplasma in pregnant women, and treating infections with antibiotics, could reduce serious neurological effects or death in infected offspring by about three-quarters4. However, there was no evidence that prenatal 2 Creighton SM, Minto CL, Steele SJ. Objective cosmetic and anatomical outcomes at adolescence of feminising surgery for ambiguous genitalia done in childhood. Lancet. 2001;358(9276): 124–5. 3 Tavares F et al. Pregnancy and safety outcomes in women vaccinated with an AS03-adjuvanted split virion H1N1 (2009) pandemic influenza vaccine during pregnancy: A prospective cohort study. Vaccine. 2011;29(37):6358–65. 4 Cortina-Borja M et al. Prenatal treatment for serious neurological sequelae of congenital toxoplasmosis: an observational prospective cohort study. PLoS Med. 2010;7(10). pii: e1000351. POPULATION HEALTH UCL School of Life and Medical Sciences 9 treatment significantly reduced the risk of fetal infection. Toxoplasma infection can lead to neurological damage and to eye disease in infected fetuses. However, infections are relatively rare and a randomised controlled trial and economic analysis would be needed before a screening policy could be considered in the UK or other low-prevalence countries. The study also found that a less potent antibiotic, spiramycin, was as good as the more commonly used, and more toxic, pyrimethamine-sulfonamide. A pilot study led by Professor Carol Dezateux has led to the introduction of a blood test for a rare metabolic condition – medium chain acyl CoA dehydrogenase deficiency (MCADD) – for all newborn babies across England. MCADD affects the body’s ability to break down fat for energy, and can be fatal unless treated. 10 The pilot study, at six centres, tested 1.5 million babies over four years. Around 200 tested positive and about 150 were confirmed as having MCADD through further tests. As well as confirming that MCADD detection was technically feasible, the pilot also showed that the relatively small number of cases could be identified without causing anxiety to the families of the vast majority of unaffected children. The test is also practicable, as it can be applied to routinely taken blood spots. In other work, Professor Bobby Gaspar and colleagues have identified significant benefits associated with detection of severe combined immunodeficiency at birth5. By comparing patients and their younger siblings who were diagnosed at birth, the UCL team found that the latter suffered fewer infections and had dramatically better survival both before and after bone marrow transplant. These findings, and other evidence, form a strong case for newborn screening of all infants for severe combined immunodeficiency. Observational studies are also being used to explore issues related to pregnancy and childbirth. Dr Claire Townsend and colleagues have looked at the impact of antiretroviral drugs on HIVinfected pregnant women. The drugs have dramatically cut the incidence of motherto-child transmission of the virus, and do not appear to cause fetal abnormalities, but may be associated with an increased risk of premature delivery 6. Other trials are examining interventions to achieve healthier pregnancies. Dr Nick Greene and colleagues, for example, are testing whether a simple nutritional supplement, inositol, can reduce the POPULATION HEALTH UCL School of Life and Medical Sciences incidence of neural tube defects. The trial builds on work in mice showing that inositol can prevent neural tube defects that do not respond to folate, the supplement usually given to prevent such defects. Dietary supplements are also a research interest of Dr Elina Hypönnen. She has drawn attention to the conflicting policy advice currently surrounding the use of vitamin D supplements in women of child-bearing age (see page 11). 5 Brown L et al. Neonatal diagnosis of severe combined immunodeficiency leads to significantly improved survival outcome: the case for newborn screening. Blood. 2011;117(11):3243–6. 6 Townsend CL, Tookey PA, Newell ML, Cortina-Borja M. Antiretroviral therapy in pregnancy: balancing the risk of preterm delivery with prevention of mother-tochild HIV transmission. Antivir Ther. 2010;15(5):775–83. Townsend CL, Willey BA, Cortina-Borja M, Peckham CS, Tookey PA. Antiretroviral therapy and congenital abnormalities in infants born to HIV-infected women in the UK and Ireland, 1990-2007. AIDS. 2009;23(4):519–24. A well-conceived plan? D for deficiency An evaluation of the UK’s teenage pregnancy strategy suggests it may have had some impact, but may not have been tackling all the right risk factors. Is vitamin D deficiency widespread in the UK? Wilkinson P et al. Teenage conceptions, abortions, and births in England, 1994-2003, and the national teenage pregnancy strategy. Lancet. 2006;368(9550):1879–86. For more than 150 years sunshine and cod liver oil have been known to prevent rickets in children. The discovery of vitamin D provided a mechanistic explanation for their effects. But with rickets beginning to reappear in the UK, and vitamin D implicated in a far wider range of physiological processes, Dr Elina Hyppönen suggests that vitamin D deficiency is again a public health issue. The wider impact of vitamin D was amply demonstrated in a study of more than 12,000 pregnant women in north Finland, who were enrolled in a birth cohort in 1966. Many (but not all) of the infants received vitamin D supplements, most at very high doses, providing a ‘natural experiment’ in which to study the effects of supplementation on later health. With colleagues in Finland, Dr Hyppönen found a strong inverse relationship between vitamin D intake and type 1 diabetes, suggesting that it may be protecting against development of this autoimmune disease. The population findings tallied with a growing awareness that vitamin D had a potent effect on immune responses. Vitamin D also has an important role in pregnancy, severe deficiency causing potentially life-threatening neonatal complications. But evidence is growing that less serious deficiency may have implications for the health of mother and child. Because of the UK’s climate, and reduced exposure to sunlight because of skin cancer concerns, vitamin D synthesis in the skin is limited. Work on the 1958 British Birth Cohort (see page 26), for example, found alarmingly high levels of deficiency, particularly in winter and spring. Unfortunately, Dr Hyppönen points out, the UK has a contradictory policy framework that is sending confusing messages about the need for vitamin D. Official Department of Health advice to healthy pregnant and breastfeeding mothers is to ensure they are getting adequate vitamin D; however, these recommendations are not systematically endorsed by NICE. The UK is also unique among 31 European countries in not having any recommendation for dietary vitamin D intake for the general adult population. While attempting to clarify this policy confusion, Dr Hyppönen has also turned to genetics to unpick the physiology of vitamin D. Her work as part of the SUNLIGHT consortium has identified four genes influencing vitamin D status (and susceptibility to type 1 diabetes). Currently Dr Hyppönen leads a large international collaboration aiming to establish the wider effects of vitamin D deficiency using genes as proxy markers for low vitamin D levels. Allen E et al. Does the UK government’s teenage pregnancy strategy deal with the correct risk factors? Findings from a secondary analysis of data from a randomised trial of sex education and their implications for policy. J Epidemiol Community Health. 2007;61(1):20–7. Hyppönen E, Läärä E, Reunanen A, Järvelin MR, Virtanen SM. Intake of vitamin D and risk of type 1 diabetes: a birth-cohort study. Lancet. 2001;358(9292):1500–3. The UK has traditionally topped the table for teenage pregnancy rates in west European countries. In 1999, in what was widely seen as a significant shift from morally led to evidence-driven policy development, the UK Government introduced a national teenage pregnancy strategy with very ambitious targets – to halve teenage pregnancies by 2010. A mid-term evaluation by Professor Judith Stephenson and colleagues found some progress being made toward this target and provided a more refined view of key risk factors. The 1999 strategy was notable in focusing on the risk factors associated with teenage pregnancy – such as socioeconomic disadvantage, being the child of a teenage parent, not being in education or work, alcohol misuse, and low levels of sexual health. However, the evidence it drew upon was limited and relatively old. The evaluation therefore looked both at how successful it had been and whether its priority areas were still appropriate. The conception data revealed that teenage pregnancies did decline from 1999 onwards, by about 2 per cent a year or 11 per cent total up to 2004. Although encouraging, the decline would not enable the 50 per cent target to be reached. One notable finding was that the biggest effects were seen in socioeconomically deprived areas – the opposite of what is usually seen in population interventions – suggesting that targeting such areas was effective. As for the key risk factors, the analysis confirmed many of the previously identified factors, particularly socioeconomic status, low educational attainment and expectations. Several factors appeared to be protective, including easy communication with parents and guardians and obtaining information about sex at school. However, sexual knowledge per se did not seem to be a significant risk factor – although myths can still arise, the basics of sex and pregnancy are now much more widely known by teenagers. Hence it may be that development of open communication and emotional literacy in sex education may be the route to further reductions in teenage pregnancies. Hyppönen E, Power C. Hypovitaminosis D in British adults at age 45 y: nationwide cohort study of dietary and lifestyle predictors. Am J Clin Nutr. 2007;85(3):860–8. Hyppönen E, Boucher BJ. Avoidance of vitamin D deficiency in pregnancy in the United Kingdom: the case for a unified approach in National policy. Br J Nutr. 2010;104(3):309–14. Wang TJ et al. Common genetic determinants of vitamin D insufficiency: a genome-wide association study. Lancet. 2010;376(9736):180–8. POPULATION HEALTH UCL School of Life and Medical Sciences 11 The first National Survey of Sexual Attitudes and Lifestyles, Natsal, was a groundbreaking project documenting the sexual behaviours of the British population. Now in its third incarnation, Natsal provides a fascinating insight into this most private of areas but, more importantly, also generates invaluable evidence shaping health and social policy. Let’s talk about sex In 1981, a frightening new health threat appeared: HIV and AIDS. First noted in an obscure report of an unusual immunodeficiency affecting the San Francisco gay community, AIDS rapidly mushroomed into a global crisis. In an age before antiretroviral drugs, HIV infection was a death sentence, and there was a strong public health imperative to prevent its spread. But as well as limited knowledge about the virus itself, the UK’s public health authorities had almost no evidence on which to base public health campaigns. Almost nothing was known about behaviours relevant to sexual health, and attitudes that might affect them. Although some data did exist, they were drawn largely from sexual health clinics, and their relevance to general populations was debatable. This glaring gap was an important stimulus for a uniquely ambitious project: a large, nationally representative survey of sexual attitudes and lifestyles. Its aim would be to gather information to inform public health measures – for HIV/ AIDS and other sexually transmitted infections – and other areas of importance to health or social policy, such 12 “I remember saying one day, ‘we really ought to do a general population-based study on sexual behaviour with a proper random sample’. I remember a senior colleague… looking at me with an expression that suggested I’d cracked.” Anne Johnson as age at first intercourse and first pregnancy. The plans for Natsal were hatched by Professor Anne Johnson at UCL, in collaboration with colleagues now at the London School of Hygiene and Tropical Medicine and the National Centre for Social Research. They were almost scuppered when the Conservative Government – at the personal behest of Prime Minister Margaret Thatcher – vetoed the study, arguing that it was too intrusive, even though the science had been favourably reviewed by Research Councils. Fortunately, the Wellcome Trust stepped in with funding enabling the first survey, Natsal I, to go ahead in 1990. Attitudes had relaxed sufficiently a decade later for the MRC to be able to fund a follow up, Natsal II, completed in 2001. A third survey, funded by the MRC and the Wellcome Trust, is due to report in 2013. Natsal I provided a valuable snapshot to inform the response to the HIV epidemic. Natsal II was important not only in providing an updated data set but also in giving insight into behavioural trends. And the period between 1990 and 2000 was one of considerable social change. Following the HIV scare in the 1980s, sexual risk behaviours had reduced and STI rates declined rapidly. Between 1990 and 2000, however, those trends began to reverse. Both men and women reported more sexual partners (consistent with the steep rise in sexually transmitted infections from 1995 onwards). And although condom use had increased, Natsal II identified major changes in a range of risky behaviours, including increased numbers of heterosexual partners, homosexual encounters, concurrent partnerships, paying for sex and heterosexual anal sex. Natsal II also revealed a continuing drop in the age POPULATION HEALTH UCL School of Life and Medical Sciences Ethnic variation Sexual behaviour varies in different ethnic populations. By sampling across different ethnic groups in Britain, Natsal has been able to shed light on sexual behaviours and attitudes within particular populations. Indeed, reported behaviours differed markedly between groups. In terms of numbers of sexual partners, for example, black Caribbean and black African men reported higher numbers of lifetime sexual partners (median nine), as did white and black Caribbean women (median five and four, respectively). Indian and Pakistani men and women typically reported fewer partners (as well as later age of first intercourse). These figures were mirrored in the incidence of STIs. Although individual risk behaviours are the biggest determinant of the likelihood of sexual health problems, population norms will also have an influence – people cannot entirely avoid what is happening around them. The results provide important insight into the sexual health issues of ethnically defined subpopulations. They should provide the backdrop against which culturally sensitive interventions can be developed. Fenton KA et al. Ethnic variations in sexual behaviour in Great Britain and risk of sexually transmitted infections: a probability survey. Lancet. 2005;365(9466):1246–55. of first intercourse – 30 per cent of men and 26 per cent of women aged 16–19 reported having sex before the age of 16. However, the trend for women to have sex at younger ages appeared to be stabilising by mid-decade. Early intercourse was associated with poorer later life sexual health, and was linked to early onset of menstruation, disrupted family life and, in particular, poor educational achievement – emphasising the important links between social and health policy. Natsal II also offered testing for Chlamydia to half the population of sexually active 18–44-year-olds. Surprisingly, Chlamydia was as prevalent in men than women, even though national screening initiatives had previously targeted women. Natsal data have been a treasure trove for researchers exploring important sexual health issues, and form the widely used benchmark against which other studies compare their findings. Natsal III is an even bigger exercise, recruiting 15,000 men and women aged 16–74 – the first time people aged 60–74 have been included. It will cover similar ground to its predecessors, to enable comparisons to be made, while incorporating methodological advances, some new areas and biological measures (STIs and sex hormone levels). A combination of data from all three studies will provide extraordinary power to examine not just representatives of different age groups over time, but also the experience of successive birth cohorts, as data will be available on people born between the 1930s and the 1990s. Johnson AM et al. Sexual behaviour in Britain: partnerships, practices, and HIV risk behaviours. Lancet. 2001;358(9296):1835–42. Wellings K et al. Sexual behaviour in Britain: early heterosexual experience. Lancet. 2001;358(9296):1843–50. Fenton KA et al. Sexual behaviour in Britain: reported sexually transmitted infections and prevalent genital Chlamydia trachomatis infection. Lancet. 2001;358(9296):1851–4. Asking for help Natsal revealed that sexual function problems were surprisingly common, but relatively few people seek specialist help. One area touched upon in the Natsal survey was the extent of sexual function problems in the population at large. Defined quite broadly – having at least one sexual problem lasting at least one month – sexual function problems were remarkably common, reported by 35 per cent of men and 54 per cent of women. For men, the most common problems were lack of interest in sex, premature ejaculation and anxiety; for women, inability to achieve orgasm and painful intercourse. Persistent sexual problems – of at least six months’ duration – were less common but by no means rare, affecting 6.2 per cent of men and 15.6 per cent of women. Notably, just 11 per cent of men and 21 per cent of women who reported sexual function problems had actually sought help for their problem. Even among the smaller number with persistent problems, the numbers were only 21 per cent and 32 per cent. The nature of ‘sexual dysfunction’, and the role of medical interventions, remains a controversial area. Nevertheless, Natsal provided valuable evidence on what has been a ‘hidden’ issue. Mercer CH et al. Sexual function problems and help seeking behaviour in Britain: national probability sample survey. BMJ. 2003;327(7412):426–7. POPULATION HEALTH UCL School of Life and Medical Sciences 13 SECTION 2 Young people and transition to adulthood A succession of birth cohorts has shed light on the health, development and welfare of generations of UK children. Much has changed for the better, but new issues have emerged – not least high levels of obesity – and inequality remains a powerful force affecting young people and the adults they become. 14 POPULATION HEALTH UCL School of Life and Medical Sciences Improved nutrition and living conditions, education and the control of infectious disease, most recently by vaccination, have had a profound impact on young people’s health. Comparisons across UK birth cohorts – those of 1946, 1958, 1970 and 2000 – have shown how childhood has changed, in terms of health and physical, social and educational development. Indeed, while there is no cause to be complacent, a major focus of research in young people is the longer-term consequences of childhood experiences. A life-course perspective on health – a particularly valuable aspect of long-term cohort studies, particularly ‘cradle-to-grave’ studies such as the 1946 Birth Cohort (see page 38) – can reveal how early influences affect later-life illness. It is increasingly apparent that experiences at school age (and even earlier) can have a profound effect on later-life physical and mental well-being. ...experiences at school age (and even earlier) can have a profound effect on later-life physical and mental well-being. In this context, the rise in childhood obesity documented in the Millennium Birth Cohort is of some concern (see page 16). By the age of three, nearly one in four UK children were classified as overweight or obese, and in some populations the proportion was even higher. An analysis of trends suggests that those overweight early in life – as young as three years old – tend to be the same children who are overweight at later ages. As well as the immediate impacts of obesity on quality of life (and interactions with peers), excess weight gain in early years is storing up a host of problems for later life. Obesity will be a major focus of the latest UK birth cohort, to be launched in 2012. The £28 million initiative, funded by the UK’s Medical Research Council (MRC) and Economic and Social Research Council, is being led by Professor Carol Dezateux, Director of the MRC Centre of Epidemiology for Child Health at UCL, who chairs the Child Health Group of the Millennium Cohort Study. The 2012 Birth Cohort will address important questions affecting children’s health and well-being, from the key factors enabling children to overcome social disadvantage at birth to links between eating and physical activity behaviours in very early life and growth and weight gain in later childhood. It will also focus on temperament and social and emotional communication styles, as well as the effects of exposure to a range of environmental pollutants during early infancy. POPULATION HEALTH UCL School of Life and Medical Sciences 15 Weighty matters Special cases Unhealthy weight gain starts remarkably early in life, work on the Millennium Birth Cohort suggests. Treatment of HIV in the young requires special consideration. The UK’s ‘obesity epidemic’ raises fears of a surge in chronic later life diseases such as type 2 diabetes. Alarmingly, excess weight gain is already apparent in young people, triggering a range of public health promotions to promote healthier lifestyles, such as the ‘Change4Life’ campaign. The work of Professors Carol Dezateux, Catherine Law, Tim Cole and their colleagues Lucy Griffiths and Summer Hawkins on the Millennium Birth Cohort has revealed worrying levels of obesity at early ages and shed important light on its origins. Data from the Millennium Birth Cohort has revealed the full scale of unhealthy weight gain in infancy and childhood. By age three, almost one in four children (23 per cent) were classified as overweight or obese. A variety of factors were associated with excess weight – mothers smoking during pregnancy, parents being overweight, mothers being overweight before pregnancy and maternal working. Black children were at particular risk, while breastfeeding and Indian ethnicity were associated with protection from excess weight. Obesity levels were similar at age five. Indeed, the trajectory of weight gain seems to have been set early in life, with 63 per cent of overweight children and 88 per cent of obese children showing rapid weight gain between the ages of three and five. As well as high BMI at age three, key influences were very similar to those seen before, plus exposure to second-hand smoke. The numbers stress how early childhood obesity arises, and the likelihood that those overweight at an early age are likely to stay overweight. They also highlight significant modifiable parental influences – particularly smoking and weight. Some 28 per cent of mothers were overweight or obese before pregnancy and 34 per cent smoked during pregnancy. More positively, breastfeeding helped prevent excess weight gain before age three. The long-term risks of being overweight are well-established, but the Millennium Birth Cohort has also highlighted its immediate psychosocial impacts. At age five, obese boys were at higher risk of conduct problems, hyperactivity and attention difficulties, and peer relationship problems; girls were at risk only for the last of these. Thus obese children – and boys in particular – are at risk of emotional and behavioural problems at a very young age. Hawkins SS et al. An ecological systems approach to examining risk factors for early childhood overweight: findings from the UK Millennium Cohort Study. J Epidemiol Community Health. 2009;63(2):147–55. Griffiths LJ et al. Risk factors for rapid weight gain in preschool children: findings from a UK-wide prospective study. Int J Obes (Lond). 2010;34(4):624–32. Griffiths LJ, Smeeth L, Hawkins SS, Cole TJ, Dezateux C. Effects of infant feeding practice on weight gain from birth to 3 years. Arch Dis Child. 2009;94(8):577–82. Griffiths LJ, Dezateux C, Hill A. Is obesity associated with emotional and behavioural problems in children? Findings from the Millennium Cohort Study. Int J Pediatr Obes. 2011;6(2-2):e423–32. 16 Although HIV is predominantly a sexually transmitted infection, it can also be acquired by infants in the womb or by breastfeeding. Professor Diana Gibb and colleagues at the MRC Clinical Trials Unit have contributed to a series of influential international collaborations that have shaped WHO treatment guidelines for paediatric HIV worldwide. Although antiretrovirals have proven spectacularly successful in combating HIV, they are not a cure and treatment will be lifelong. They have both short-term and long-term side-effects, and their use raises the risk of drug resistance. Young people’s immune systems are also more dynamic than those of adults, so potentially more able to generate new immune cells. Deciding when to start treatment therefore calls for careful weighing up of pros and cons. For infants, recent evidence has been unequivocal – infants should be started on antiretrovirals as rapidly as possible. Key data have come from the CHER trial, a collaboration between the MRC Clinical Trials Unit and groups in South Africa, which showed a fourfold reduction in death rates when infants were tested and treated immediately, rather than waiting for clinical symptoms to develop or for CD4 cell numbers to fall significantly. Although this trial was carried out in South Africa, results have also changed European and US guidelines; a meta-analysis of data from European infants confirmed a similar benefit in European settings. For children above the age of one, data from multiple studies suggest that treatment should begin when certain clinical signs appear or when CD4 cell numbers fall below threshold levels. A series of clinical trials and cohort studies run by the MRC Clinical Trials Unit in collaboration with the French ANRS trials unit under the PENTA (Paediatric European Network for Treatment of AIDS) umbrella has contributed much to inform the best management strategies for HIV-infected children, including practical issues such as which antiretrovirals to start and switch to, what doses to use and when to change drugs when first-line treatment starts to fail. Concerns about drug resistance were highlighted in a recent metaanalysis of children’s cohorts, which demonstrated higher levels of resistance five years after starting treatment than in adults. Violari A et al. Early antiretroviral therapy and mortality among HIV-infected infants. N Engl J Med. 2008;359:2233–44. Goetghebuer T et al. Effect of early antiretroviral therapy on the risk of AIDS/ death in HIV-infected infants. AIDS. 2009;23:597–604. Dunn D et al. HIV Paediatric Prognostic Markers Collaborative Study Group. Short-term risk of disease progression in HIV-1-infected children receiving no antiretroviral therapy or zidovudine monotherapy: a meta-analysis. Lancet. 2003;362(9396):1605–11. PENPACT-1 (PENTA 9/PACTG 390) Study Team et al. First-line antiretroviral therapy with a protease inhibitor versus non-nucleoside reverse transcriptase inhibitor and switch at higher versus low viral load in HIV-infected children: an open-label, randomised phase 2/3 trial. Lancet Infect Dis. 2011;11(4):273–83. Pursuing Later Treatment Options II (PLATO II) project team for the Collaboration of Observational HIV Epidemiological Research Europe (COHERE) et al. Risk of triple-class virological failure in children with HIV: a retrospective cohort study. Lancet. 2011;377(9777):1580–7. POPULATION HEALTH UCL School of Life and Medical Sciences As well as documenting trends in nutrition, exercise and weight gain, the cohort has also shed light on issues such as uptake of the MMR vaccine and the interplay between work, parenting and child development. The pioneering 1946 Birth Cohort was established because of concerns about the impact of poverty and poor living conditions on childbirth, and has generated much information about the impact of social inequalities on health and social development. Despite the 65-year gap, these issues remain equally pertinent today. Though health inequalities are now widely recognised, they remain stubbornly large. Early years are crucial in establishing the trajectory for later life, and will be a particular focus of the new cohort. There will also be an opportunity to explore how biological, social and other environmental factors interact during this critical period to shape current and future health and well-being. Work on the new cohort is likely to feed into health and social policy, mirroring the impact of the Millennium Birth Cohort. As well as documenting trends in nutrition, exercise and weight gain, the cohort has also shed light on issues such as uptake of the MMR vaccine and the interplay between work, parenting and child development. Indeed, one of the strengths of the cohorts is their holistic approach, drawing out links between social, educational and health domains. Insight into obesity in children has also come from other work on cohorts being studied at UCL. Professor Jane Wardle has carried out multiple studies investigating children’s food choices. These include the PEACHES (Physical Exercise and Appetite in Children) study, a longitudinal investigation of behaviours affecting obesity risk in 7–8-yearold children, TEMPEST, an EU-funded study of the role of self-regulatory skills in adolescents, and the GEMINI Twin Birth Cohort, 2402 families with twins in England and Wales born between March and December 2007. Professor Wardle is particularly interested in the links between genetic factors implicated in weight gain and eating behaviours. The studies recognise that childhood weight depends on the interplay between many factors – including genetics, parenting practice and the home environment. Her group has also run several interventions aimed at improving young people’s diets. These include the POPPETS ‘Healthy Habits’ (POSH) intervention, which uses the habit-formation framework to modify parental behaviour in order to improve children’s diets, as well as a family-based intervention for childhood obesity, run in partnership with Great Ormond Street Hospital. This work is carried out through the Weight Concern charity established by Professor Wardle. Her group has also tested the impact of reward on children’s eating habits7. Other UCL researchers are also examining the experience and care of overweight children, but with a greater focus on implications for the NHS. Professor Russell Viner has been awarded major funding from the National Institute for Health Research (NIHR) for five linked studies where significant gaps in knowledge have been identified. These include pilot studies of an electronic tool to guide referrals, a trial of the Healthy Eating and Lifestyle Programme (HELP), an evaluation of the use of anti-obesity drugs in young people, and an assessment of bariatric surgery in adolescents. The health and well-being of children living with HIV needs special attention. Pan-European cohort studies, organised by the MRC Clinical Trials Unit, have provided information about key issues such as which drugs to use and when to start antiretroviral treatment (see page 16). As the first children infected with HIV reach adolescence and enter adulthood, further work will be needed to support them through a difficult period in life and to help them manage what is in effect a chronic condition. 7 Cooke LJ et al. Eating for pleasure or profit: the effect of incentives on children’s enjoyment of vegetables. Psychol Sci. 2011;22(2):190–6. POPULATION HEALTH UCL School of Life and Medical Sciences 17 A programme of research on public attitudes to the human papilloma virus vaccine, led by Professor Wardle, helped to shape its national rollout. Vaccination Vaccines have been an essential component of public health, and UCL research has provided significant input into important areas of vaccine policy. A programme of research on public attitudes to the human papilloma virus vaccine, led by Professor Wardle, helped to shape its national rollout. The Millennium Birth Cohort provided an opportunity to examine take up of MMR and use of single antigen vaccines8. Uptake was high (89 per cent) but below that required for effective herd immunity. Use of single antigen vaccines was associated with wealthier, more educated families – a rare example of a ‘reverse socioeconomic gradient’. Worryingly, almost half of children given single vaccines did not receive all three jabs. Sexual behaviours One of the potentially most important influences on health from adolescence onwards is sexual behaviour. Here, the National Survey 18 of Sexual Attitudes and Lifestyles (Natsal), led by Professor Anne Johnson (see page 12), has provided valuable insight into behaviours likely to affect the spread of sexually transmitted infections (STIs), including HIV. The world’s first representative population surveys of sexual attitudes and lifestyles, Natsal revealed significant increases in risk-taking behaviour and in STIs in young adults between its surveys in 1990 and 2000. Natsal 2000 data revealed a marked shift in the age at which people were first having sex – 30 per cent of men and 26 per cent of women reported having sex before the age of 16. The third and most extensive survey, Natsal III, due to report in 2013, will reveal whether these trends are continuing. Natsal provided information on attitudes and behaviours within different ethnic communities, and other UCL research has generated important findings about risk behaviours of migrant groups. Dr Fiona Burns and colleagues have shown that more African men than previously suspected had acquired HIV in the UK. More recently, her work has shed important light on the risk behaviours of East European migrants (see page 19). Mental health UCL’s Priment Clinical Trials Unit is coordinating several studies relevant to children and young adults. These include the HELP trial of obesity management in children and several studies linked to care of people with schizophrenia (including the innovative MATISSE trial of art therapy). Other projects are examining the care of people with schizophrenia or other long-term mental conditions. In the REACT project, for example, Dr Helen Killaspy and colleagues found that, in the UK setting, assertive community care was no better than care provided by community mental health teams9 (work that led to an Association of European Psychiatrists’ research prize in 2007). Dr Killaspy has also led an EC-funded programme developing a toolkit for assessment of long-term care facilities. UCL researchers are also involved in major intervention projects aimed at the mental POPULATION HEALTH UCL School of Life and Medical Sciences health and well-being of young people. Professor Peter Fonagy is leading the START (Systemic Therapy For At Risk Teens) trial, a large multicentre study spread across 10 sites in the UK investigating an intervention for young people and their families who are experiencing difficulties at home, at school and possibly with the police. He is also involved in the IMPACT study, a randomised controlled trial of two psychotherapies in adolescents with moderate to severe depression. His group is also evaluating the Targeted Mental Health in Schools (TaMHS) initiative, a three-year programme providing mental health support in schools for children aged five to 13 at risk of, or already experiencing, mental health problems. 8 Pearce A et al. Factors associated with uptake of measles, mumps, and rubella vaccine (MMR) and use of single antigen vaccines in a contemporary UK cohort: prospective cohort study. BMJ. 2008;336(7647):754–7. 9 Killaspy H et al. Randomised evaluation of assertive community treatment: 3-year outcomes. Br J Psychiatry. 2009;195(1):81–2. Supporting modern families Risky behaviours? An increase in the numbers of working mothers may impact on children’s health? The first major survey of Central and East European migrants to London has revealed concerning risk-taking behaviours. A notable social trend of recent decades has been the increasing numbers of women in paid work, a trend that is unlikely to be reversed. Yet, as research by Professor Catherine Law and colleagues on the Millennium Birth Cohort indicates, these changes may also have knock-on effects, both good and bad, on children’s health. One significant area of inquiry has been children’s diet and activity habits. After adjustment for other influences on children’s health behaviours (such as mother’s level of education), at age five, children of employed mothers were more likely to consume sweetened drinks between meals and less likely to snack on fruit or vegetables. They were also more likely to spend two hours or more in front of the TV or computer and more likely to be driven to school than children whose mothers did not go out to work. Consistent with these changes, maternal employment after birth was associated with early childhood overweight, independent of other factors such as social circumstances. Strikingly, though, this was true only for children from high-income households. Hence it may be lack of time rather than money that underlies this greater risk of obesity. The increase in women working has depended on a growth in childcare, either formal or informal (such as family members). Not surprisingly, early return to employment after birth and use of day care is also associated with lower rates of breastfeeding. Interestingly, while formal childcare had no independent link with early childhood overweight, informal childcare did – but only among the better off. It may therefore make sense to target health promotion at grandparents, a frequent source of informal childcare. Use of both formal and informal childcare also had a negative effect on breastfeeding, an area where the UK has a poor record. In informal care, all groups of mothers were affected, but in formal childcare the effect was seen only in better off families. Collectively the results reveal that women’s greater participation in the workplace has the potential to affect their children’s health. They highlight areas in which social policies can be focused to help modern families, in their many forms, provide a healthy environment for their children. Hawkins SS, Cole TJ, Law C. Maternal employment and early childhood overweight: findings from the UK Millennium Cohort Study. Int J Obes (Lond). 2008;32(1):30–8. Hawkins SS et al. Examining the relationship between maternal employment and health behaviours in 5-year-old British children. J Epidemiol Community Health. 2009;63(12):999–1004. Pearce A et al. Is childcare associated with the risk of overweight and obesity in the early years? Findings from the UK Millennium Cohort Study. Int J Obes (Lond). 2010;34(7):1160–8. Pearce A et al. Childcare use and inequalities in breastfeeding: findings from the UK Millennium Cohort Study. Arch Dis Child. 2010 Jun 7. The accession of ten Central and East European countries into the EU since 2004 has led to extensive migration to the UK. Improving the health of migrants should benefit the UK and their home countries, so it is important to get a good picture of their health-related behaviours and needs. The SALLEE (Sexual Attitudes and Lifestyles of London’s Eastern Europeans) project, run by Dr Fiona Burns and colleagues, including researchers at UCL’s School of Slavonic and East European Studies, has provided the first detailed information about these behaviours, and identified several of public health concern. Capturing a population sample broadly representative of Central and East European migrants proved a major challenge. Various sampling strategies were adopted, including community sampling in two London boroughs, Newham and Hammersmith, surveying attendees at sexual and reproductive health clinics, and via the internet, including two gay dating websites. In all the team recruited 3638 migrants, including 691 men who have sex with men and 299 clinic attendees. Results were compared with UK population data. Of particular note, heterosexual migrants reported high rates of behaviours associated with increased risk of HIV infection or sexually transmitted infection (STI), such as having multiple partners, injecting drug use, or paying for sex – something a third of males reported. STI rates in these Central and Eastern European migrants were lower than those seen in London populations, but the behaviours reported after arrival may place them at increased risk of STIs in the UK. Similarly, the gay men reported high-risk behaviours. Nearly a quarter reported unprotected anal intercourse with a casual partner in the past year and 20 per cent had been paid for sex at some time in their lives. The UK has Western Europe’s highest rate of HIV infection, and it again appears that migrants are adopting the risky behaviours prevalent locally – possibly a reaction to the limited opportunities available back home, where homosexuality is generally still stigmatised. Economic migrants are typically adventurous, willing to take the risk of moving countries to better themselves. These results suggest that risk-taking might also extend to their lifestyles. With many UK and European nationals making the most of economic opportunities throughout the EU, the results not only provide important food for thought for UK public health authorities but also emphasise the need for healthcare and disease surveillance systems to transcend national boundaries. Burns FM et al. Sexual and HIV risk behaviour in Central and Eastern European migrants in London. Sex Transm Infect. 2011;87(4):318–24. Evans AR et al. Factors associated with genitourinary medicine clinic attendance and sexually transmitted infection diagnosis among central and east European migrants in London. Sex Transm Infect. 2011;87(4):331–6. Evans AR et al. Central and East European migrant men who have sex with men: an exploration of sexual risk in the UK. Sex Transm Infect. 2011;87(4):325–30. POPULATION HEALTH UCL School of Life and Medical Sciences 19 SECTION 3 The middle years Our middle years are often when our lifestyle catches up with us. The first signs begin to appear of the common conditions that are responsible for the bulk of deaths in the UK. Health priorities therefore span not just immediate treatments but ways to preserve good health in later life. 20 POPULATION HEALTH UCL School of Life and Medical Sciences The middle years are a period when we are accumulating experiences that will shape our future health. Whether we are careful with our diet and exercise will influence our risk of heart disease; whether we can maintain a healthy weight will affect our risk of type 2 diabetes; our sunbathing behaviours will impact on our risk of skin cancer; if we smoke, we are increasing our chances of suffering a wide range of conditions. Thus as well as endeavouring to stay healthy in the present, the middle years are also about taking positive action to remain healthy in the future – the kind of ‘delayed gratification’ at which humans are notoriously bad. Consistent with this idea is a growing emphasis on identifying the early signs of disease, to promote prevention and early treatment. Cohort studies are particularly well-suited to identifying temporal associations. The cohorts The cohorts studied by UCL researchers have provided important information about life-course influences on adult-onset diseases, particularly the ‘lifestyle’-associated conditions affecting the heart, circulatory system and metabolism. studied by UCL researchers have provided a wealth of important information about life-course influences on adult-onset diseases, particularly the ‘lifestyle’associated conditions affecting the heart, circulatory system and metabolism. Among the most notable has been the Whitehall study. Set up in 1967 by Professor Geoffrey Rose, Whitehall I followed the lives of 18,000 civil servants. Not only did it provide valuable information about the key lifestyle factors associated with cardiovascular and respiratory disease, guiding public health policy and practice, it revealed a remarkable socioeconomic gradient in health: contrary to expectations, stress and heart disease afflicted those at the bottom of the hierarchy more than those at the top. Moreover, the effect was not just a difference between those at the very top and those at the bottom. It was a genuine gradient, with men at every level faring better than those below them and worse than those above them. The socioeconomic gradient has become akin to a fundamental, albeit unwritten law of epidemiology. It has been seen repeatedly, in a multitude of situations, across numerous countries, affecting a vast range of conditions. Partly it arises because lifestyle behaviours are themselves socially patterned – the less well-off tend to have poorer diet, smoke more and exercise less. But these do not fully account for the gradient. Many other factors contribute to the gradient, and these POPULATION HEALTH UCL School of Life and Medical Sciences 21 Gut feelings A throw of the dice Why is there such a strong socioeconomic gradient in bowel screening? Principles established by Gregor Mendel are helping researchers make sense of markers associated with disease. Despite concerted efforts to make bowel cancer screening available to all regardless of their circumstances, take-up shows a marked socioeconomic gradient, with people from poorer areas significantly less likely to participate. Part of the reason, suggests a team led by Professor Jane Wardle and Dr Christian von Wagner, lies in the way participants weigh up the short-term and long-term implications of bowel screening. The bowel cancer screening programme is open to everyone aged 60–69. They are sent a do-it-yourself kit for collecting and returning a stool sample. The test is free and sent directly to recipients’ homes, so there are no obvious practical or economic barriers to participation. Yet Professor Wardle’s team discovered a marked gradient in responses. In the most affluent areas, 61 per cent of people responded; in the least affluent areas, just 35 per cent. Given the significant benefits of participating – mortality can be reduced by up to 27 per cent through regular screening – this disparity is troubling. The findings imply attitudinal differences to screening – or disease prevention more generally – among different socioeconomic groups. To explore this issue, the UCL team examined attitudes to screening in people who had indicated they might participate in a separate bowel screening trial (of flexible sigmoidoscopy). Take up again showed a strong socioeconomic bias – 63 per cent in the most affluent areas, 38 per cent in the least affluent. The goal was to assess, in a quantifiable way, if any attitudes correlated with socioeconomic status were associated with the ultimate decision to attend screening. In particular, the team examined a concept known as ‘future orientation’ – broadly speaking, having relatively shorter-term or longer-term perspectives. They found that a tendency to focus on the short term – known to be associated with lower socioeconomic status – was a significant factor influencing the decision to attend. Those who did not attend tended to overweigh the short-term obstacles and underappreciate the long-term benefits. Although not the full story, the results begin to shed light on the basis of an important health-related behaviour. In practical terms, they also suggest ways in which the socioeconomic imbalance could be addressed, for example by emphasising the short-term benefits of participating in screening, such as peace of mind. For complex diseases, it is useful to have simple biochemical markers that faithfully track disease severity and progression. They can be useful tools in diagnosis and risk prediction and, potentially, valuable therapeutic leads. But markers are typically identified by association, so must be viewed with caution: they may be the result rather than the cause of disease, or a byproduct of more fundamental disease processes. The distinction is extremely important: there is no point developing therapies to lower levels of a marker if it is not directly related to a disease. To tackle this issue, Dr Aroon Hingorani is using a technique inspired by the ‘father of genetics’, Gregor Mendel. ‘Mendelian randomisation’ is based on Mendel’s second law, which states that units of heredity (genes as we now know them) are distributed at random to gametes and hence to the next population. Crucially, once the die has been cast, the distribution of genes cannot change, so will not be affected by other risk factors (as biochemical markers may be). Hence, if a marker is directly contributing to a disease, then a gene raising levels of that marker should put people at greater risk of disease. Professor Hingorani and colleagues have used this approach to examine the role of C-reactive protein (CRP) in coronary heart disease. CRP is a circulating marker of inflammation and its levels correlate with risk of heart disease. Since atherosclerosis has a strong inflammatory element to it, it was a reasonable assumption that CRP was contributing directly to atherosclerosis and heart disease. To test this idea, Professor Hingorani examined the association between genetic variants in the CRP gene, circulating CRP levels and measures of atherosclerosis or the incidence of heart disease in different cohorts. Certain variants reliably increase CRP levels so should put individuals carrying those variants at greater risk of pathology or disease. In reality, they do not. Once the influence of other risk factors is stripped away, having a CRP-raising allele has no impact on heart disease risk. A very large international meta-analysis has reinforced these findings. Thus CRP is almost certainly not driving disease. More generally, the results highlight the power of genetics and Mendelian randomisation to delve deeper into the meaning of associations. von Wagner C et al. Inequalities in participation in an organized national colorectal cancer screening programme: results from the first 2.6 million invitations in England. Int J Epidemiol. 2011;40(3):712–8. Wensley F et al. Association between C reactive protein and coronary heart disease: mendelian randomisation analysis based on individual participant data. BMJ. 2011;342:d548. doi: 10.1136/bmj.d548. Kivimäki M et al. Does high C-reactive protein concentration increase atherosclerosis? The Whitehall II Study. PLoS One. 2008;3(8):e3013. von Wagner C, Good A, Whitaker KL, Wardle J. Psychosocial determinants of socioeconomic inequalities in cancer screening participation: a conceptual framework. Epidemiol Rev. 2011;33(1):135–47. Whitaker KL et al. Socioeconomic inequalities in colorectal cancer screening uptake: does time perspective play a role? Health Psychol. (in press). 22 POPULATION HEALTH UCL School of Life and Medical Sciences ...our health and well-being depends not just on our genes, or what we eat, or what infections we are exposed to, but also on what jobs our parents did, their parenting style, what kind of education we had, and how we are treated at work. are often out of our control – how we are treated at work, for example, and how we were brought up (as well as our genetic inheritance). There is also the fascinating question of why certain health behaviours are socially patterned. Professor Jane Wardle and colleagues, for example, have examined why there is a social gradient in uptake of bowel cancer screening, despite exhaustive efforts to avoid inequality in access (see page 22). At least part of the answer can be put down to different psychological attitudes to screening in socioeconomically disadvantaged groups. Launched in 1985, Whitehall II, the follow up to Whitehall I, has confirmed the socioeconomic gradient and extended its predecessor’s findings into other areas, such as mental health and well-being. It has begun to explore some of the biological mediators that turn social phenomena into physiological effects. The British Regional Heart Survey approached similar questions to Whitehall I from a different angle. It was originally established in the 1970s to investigate regional differences in heart disease, which at one point were thought to be linked to geographical variation in hard water supply. The hard water hypothesis did not hold water – hard water was not protective against hardened arteries. In fact, geographic differences are largely accounted for by regional variation in conventional risk factors: heart disease is more common where people smoke more, have a poor diet and take less exercise. The 1946 and 1958 birth cohorts have also generated a wealth of information on lifestyle factors and adult life. As birth cohorts, they have been able to cast light on the impact of early life events. Data from the 1946 cohort, for example, were among the first to suggest that low birth weight for gestational age was a risk factor for later-life metabolic conditions. This fed into the influential ‘Barker hypothesis’, which linked poor maternal nutrition to the ‘programming’ of fetal metabolism, preparing a newborn for a life of hardship. Unfortunately, this may leave them poorly adapted to a life of plenty. The multidisciplinary nature of the birth cohorts has provided unrivalled opportunities to explore links between health and social, economic, domestic and other circumstances. Indeed they have done much to emphasise the interconnectedness of these domains – our health and well-being depends not just on our genes, or what we eat, or what infections we are exposed to, but also on what jobs our parents did, their parenting style, what kind of education we had, and how we are treated at work. Indeed, much of the recent Marmot Review’s policy framework for tackling health inequalities is explicitly social in nature (see page 30). While cohorts have traditionally focused principally on environmental influences on health, they are increasingly being integrated with genetic-based approaches. Advances in high-throughput genetic analysis are offering a wealth of opportunities to apply genetic techniques at a population-based level. Most common diseases are affected by genes, but not in a simple deterministic way. A great many genetic variants influence common diseases, but each is likely to have only a small effect. New genetic tools are being used to identify these variants in collections of patients, but their impact can also be explored in large, well-phenotyped population cohorts. POPULATION HEALTH UCL School of Life and Medical Sciences 23 There is now a growing trend to use population cohorts to search for genetic variants affecting disease-relevant phenotypic and physiological traits, taking advantage of cohorts’ excellent phenotypic data. In addition, cohorts provide a way to examine the impact of disease-associated variants in ‘normal’ populations. One further advantage is that cohorts can add a life-course perspective, shedding light on when a genetic variant has its effect. The emerging discipline of ‘genomic epidemiology’ is thus likely to be of profound importance. One other application is ‘mendelian randomisation’, which can be used to test whether an association – say between a biomarker and a disease – is really indicative of a causal role in disease or a byproduct of some more fundamental link. For individuals, the implications are less clear. Although genetic profiling has the potential to be used for risk prediction, it is doubtful that it can yet provide sufficiently useful information to guide healthcare or personal health beyond traditional 24 guidance (eat more fruit, don’t smoke). One potential use may be to refine treatments – being explored in the FOCCS ovarian cancer trial and for familial hypercholesterolaemia (see companion volume on Translation and Experimental Medicine). More generally, large-scale genetic studies identify leads for follow up in laboratory studies, shedding light on mechanisms of disease. Professor Andrew Phillips and colleagues have been working with some of the world’s largest and longest-running cohorts of people with HIV. As well as generating important findings on treatment, monitoring of these cohorts has revealed the emergence of resistance to antiretroviral drugs. This information again feeds into laboratory studies, with investigations by Professor Deenan Pillay and colleagues of the molecular mechanisms of drug resistance. Population data can also be used to support mathematical modelling of transmission. Such studies can be used to explore the potential of variation in therapy, in ‘virtual trials’ Flu Watch has targeted several thousand households directly, collecting nasal swabs from participants to ensure accurate diagnosis. that would be impossible to conduct in real-life situations. Flu is an ongoing public health concern, exacerbated by the recent H1N1 swine flu pandemic. Understanding the transmission of flu is challenging: the flu strains in circulation change every year, and reporting through general practice may give an incomplete picture of flu in the community, as only a proportion of people seek treatment. In response to the threat from H1N1 swine flu, Dr Andrew Hayward was funded by the MRC and the Wellcome Trust to extend the ‘Flu Watch’ project, a unique nationwide collaboration characterising flu strains circulating in the community. Flu Watch has targeted several thousand households directly, collecting nasal swabs from participants to ensure accurate diagnosis. The study revealed a high incidence of mild or asymptomatic H1N1 infections. Strikingly, even though visits to GPs surged during the summer pandemic, the POPULATION HEALTH UCL School of Life and Medical Sciences Flu Watch data showed no corresponding jump in infections – the effect probably reflected a change in people’s health-seeking behaviours in the face of intense media coverage. The study has tracked the changing nature of circulating flu strains, with pandemic H1N1 having largely ousted seasonal H1N1 and a previously dominant H3N2 strain. The results have provided a much clearer picture of the reality of the H1N1 pandemic and seasonal flu. Flu Watch results are also shedding light on the impact of disease-control initiatives, and of antiviral drug and vaccine use, while analysis of blood samples should reveal which aspects of the immune response are associated with protective immunity. The results will help to shape the response to future flu epidemics, and are also helping researchers more accurately model flu outbreaks and plan interventions. Heart breaking The magic number Influenza infections may be responsible for large numbers of heart attacks. When is the right time to begin antiretroviral therapies? Despite accumulating evidence that influenza virus can affect the heart and circulatory system, there has been no definitive demonstration that influenza infections are a cause of clinical heart problems. A systematic review carried out by UCL MRC clinical fellow Dr Charlotte Warren-Gash, Dr Andrew Hayward and Professor Liam Smeeth of the London School of Hygiene and Tropical Medicine has clearly shown a connection between the virus and the incidence of heart attacks, and some evidence that vaccination might be protective. The group looked at 42 publications describing 39 studies, the earliest dating back to 1932. All reports at a population level found an increase in the numbers of deaths due to heart disease or numbers of heart attacks when influenza virus was circulating. Moreover, the virus appears to have a significant effect – 35–50 per cent of excess deaths due to influenza could be attributed to cardiovascular causes. A range of observational studies in different settings likewise reported links between acute respiratory infections – influenza in particular – and heart attacks, and a less strong link to deaths associated with cardiovascular conditions. The picture was more mixed for vaccination. Four out of eight observational studies found vaccination to be beneficial. Of two small randomised controlled trials, one found evidence for significant benefits while the other was inconclusive. Larger studies would be needed to provide a conclusive answer, but the evidence collectively suggest that improving vaccine coverage in at-risk populations – in 2008/09 vaccine coverage in chronic disease groups was less than 50 per cent – would help to reduce the number of cardiovascular events triggered by influenza infections. Warren-Gash C, Smeeth L, Hayward AC. Influenza as a trigger for acute myocardial infarction or death from cardiovascular disease: a systematic review. Lancet Infect Dis. 2009;9(10):601-10. The development of antiretroviral drugs raised hopes that HIV could be eliminated from patients. Such hopes were dashed when it was discovered that HIV could persist at low levels in reservoirs in the body. Patients will therefore have to take antiretrovirals for long periods, probably the rest of their lives. To protect them from the short-term and long-term adverse effects of antiretroviral drugs, treatment has typically been initiated only when levels of the immune cells infected by HIV – CD4 cells – fall below a particular threshold. The work of Professor Andrew Phillips and colleagues has done much to influence what this threshold should be. Professor Phillips has worked with some of the world’s longest running cohorts of people living with HIV, recruited from HIV clinics around the UK in the 1980s. Antiretroviral drugs were a life-saver for these individuals, but had serious side-effects. Combined with fears about the development of resistance, this led to the belief that they should be used sparingly. If patients still had reasonable CD4 cell numbers, it was argued, the benefits of giving them such powerful drugs might not outweigh the risks. In one early strategy, treatment was initiated at a CD4 count of 250 CD4 cells per cubic millilitre but halted when numbers rose above 350. However, the international SMART (Strategies for the Management of Antiretroviral Therapy) study found that such ‘episodic’ treatment increase the risk not only of AIDS disease but also of several non-AIDS diseases and of death. Although drug use still has to be weighed against side-effects, the development of improved drugs tilted the balance firmly towards earlier treatment, and 350 is now the widely used threshold. However, it is still empirically defined – no clinical trial has ever directly tested its validity. Indeed, untreated HIV-infected individuals with sturdy CD4 cell counts had a modest but significantly higher death rate than the general population, and lower CD4 levels were associated with higher mortality even above the 350 threshold. As the longevity of successfully treated people with HIV now approaches that of the general population (at least in the developed world), such discrepancies are troubling. Hence the magic number of 350 may yet be revised upwards. Indeed, with collaborators in Denmark, Professor Phillips is involved in a trial of HIV patients with CD4 counts above 500, comparing immediate start with initiation at 350. This should reveal whether early therapy is beneficial to patients, and it may also have population benefits by reducing transmission. El-Sadr WM et al. CD4+ count-guided interruption of antiretroviral treatment. New Engl J Med. 2006;355(22):2283–96. Sterne JA et al. Timing of initiation of antiretroviral therapy in AIDS-free HIV1-infected patients: a collaborative analysis of 18 HIV cohort studies. Lancet. 2009; 373(9672):1352–63. Lodwick RK et al. Death rates in HIV-positive antiretroviral-naive patients with CD4 count greater than 350 cells per microL in Europe and North America: a pooled cohort observational study. Lancet. 2010;376(9738):340–5. POPULATION HEALTH UCL School of Life and Medical Sciences 25 A long legacy QuIRC of fate The roots of adult obesity may lie in early life experience – and even in the womb. A newly developed toolkit provides an internationally validated tool for assessing facilities for people with long-term mental health problems. Adult obesity is a risk factor for many conditions and a growing public health concern. Adult behaviours are seen as central to obesity, and are the target of numerous interventions, yet early-life factors are also an important influence on adult weight. Working with the 1958 British Birth Cohort, Professor Chris Power and colleagues documented early signs of the ‘obesity epidemic’ and have identified some of the early-life factors contributing to it. A comparison between the 1958 and 1946 cohorts provided graphic evidence of the roots of the epidemic. Despite being born just 12 years later, the 1958 cohort grew more rapidly and ended up taller. Although no bigger at birth, they were on average 1 cm taller in childhood, grew more rapidly, ending up 3–4 cm taller in adolescence. BMI trajectories diverged markedly from early adulthood – by midadulthood the 1958 cohort had 6–7 cm larger waists and double the levels of obesity. Greater prosperity and the ready availability of food were clearly important factors in these changes. But work on the 1958 cohort points to much earlier influences on adult obesity. One striking observation has been the link between early-life adversity and adult obesity. Even mild forms of adversity – strict upbringing, physical punishment, verbal abuse, lack of parental interest – were significant risk factors for poor glucose control in adulthood (a proxy for diabetes risk). This increased risk was mediated entirely through adult obesity. Several adversities increased the risk of obesity by 20–50 per cent. Obesity risk can be increased by even earlier events. Maternal smoking substantially increased the risk of mid-life obesity, equating to an average increase in waist size of 2 cm. Studies of the 1958 cohort were among the first to show that low birthweight, linked to maternal smoking or other factors, increased the risk of adult health problems such as type 2 diabetes. Interestingly, work on the 1958 cohort suggests that this effect is mediated through an association with adult obesity – risks are not increased for lowbirthweight individuals who are not overweight as adults. Recently, the 1958 cohort has begun contributing to genetic research. Thanks to its large size and excellent phenotypic data, the cohort was used as a control group by the Wellcome Trust Case Control Consortium and is now involved with international consortia studying genetic influences on physiological variables. Li L, Hardy R, Kuh D, Lo Conte R, Power C. Child-to-adult BMI and height trajectories: a comparison of two British birth cohorts. Am J Epidemiol. 2008;168:1008–15. Despite widespread moves towards ‘deinstitutionalisation’, or care within the community, people with severe mental health problems are often treated in long-term facilities. To help improve standards, the ten-country, EC-funded ‘DEMoBinc’ project, led by Dr Helen Killaspy, has developed an internationally validated tool for assessing the quality of these institutions. People with long-term mental health problems are among the most socially excluded. Their conditions are associated with impairments of thinking and motivation that disrupt their ability to function. They may also have other problems that slow their recovery, such as substance misuse and challenging behaviours. For many years, the answer was simply to confine them to asylums. Deinstitutionalisation is gradually being introduced. However, even in deinstitutionalised countries, longer-term facilities are still used for the most difficult-to-treat patients, and across Europe, most people with severe problems are treated in institutions. Although many offer high standards of care, there is undoubtedly often room for improvement. To develop a framework for assessing quality of care, the project undertook a systematic literature review, consulted with international experts, and reviewed care standards in ten European countries. A draft toolkit was rigorously piloted in over 200 units across the ten countries and tested for reliability, which confirmed that the toolkit was robust, practical to use and wellreceived by facility managers. Toolkit ratings were also validated against patients’ experiences of care. The final version comprises 145 questions assessing seven domains of care. A web-based version of QuIRC is available in ten languages at www.quirc.eu. It has already been incorporated into the UK’s peer-accreditation process for mental health rehabilitation units (coordinated by the Royal College of Psychiatrists’ Centre for Quality Improvement), and Dr Killaspy is leading a five-year NIHR-funded programme (‘REAL’, Rehabilitation Effectiveness for Activities for Life) which is collating comprehensive national data on units in England. A similar exercise is underway in Portugal, and there are plans for national projects in many other countries. QuIRC is an accessible and useful tool that can be used for quality assessment and benchmarking for long-term mental health facilities across Europe. Given the potential vulnerability of those that use these facilities, it is a much-needed resource that provides a powerful lever to drive up standards of care. Thomas C, Hyppönen E, Power C. Obesity and type 2 diabetes risk in mid adult life: The role of childhood adversity. Pediatrics. 2008;121:e1240–9. Killaspy H et al. The development of the Quality Indicator for Rehabilitative Care (QuIRC): a measure of best practice for facilities for people with longer term mental health problems. BMC Psychiatr. 2011;11:35. Thomas C, Hyppönen E, Power C. Prenatal exposures and glucose metabolism in adulthood: are effects mediated through birthweight and adiposity? Diabetes Care. 2007;30:918–24. Turton P et al. Promoting recovery in long-term institutional mental health care: an international Delphi study. Psychiatr Serv. 2010;61(3):293–9. Power C, Atherton K, Thomas C. Maternal smoking in pregnancy, adult adiposity and other risk factors for cardiovascular disease. Atherosclerosis. 2010;211:643–8. 26 POPULATION HEALTH UCL School of Life and Medical Sciences Taylor TL et al. A systematic review of the international published literature relating to quality of institutional care for people with longer term mental health problems. BMC Psychiatr. 2009;9:55. Health service research While cohorts provide a strong public health focus, UCL also has extensive programmes in health services and implementation research. These encompass both clinical trials, primarily focused on primary care interventions, and studies of healthcare delivery within the NHS. Much of this work draws on close links with associated NHS bodies, particularly ‘UCL Partners’ (see page 3). Research has a strong focus on mental health and treatment in general practice. Development of evidencebased tools for prediction of depression and anxiety has been one important element. The Priment Clinical Trials Unit is hosting several studies examining depression or other mental health issues, particularly schizophrenia. Trials are examining management of chronic depression by practice nurses (PROCEED), prevention of depression in primary care (PREDICTPREV), and rehabilitation for people Health data analysis with chronic mental health conditions (REAL). Professor Rosalind Raine, Director of the Centre for Applied Health Research, leads a programme of studies providing information directly relevant to healthcare delivery. This work is particularly focused on healthcare inequalities, in a range of healthcare settings and for a wide range of conditions (see page 34), and health economics, drawing on the expertise of Steve Morris, Professor of Health Economics. Current areas of interest include the relationship between use of healthcare and health inequalities (a five-year programme funded by the Department of Health) and clinical decision-making by groups of clinicians (including NICE Guideline Development Groups) and its impact on social inequalities. Evaluations are also undertaken of public health and healthcare interventions, including the Department of Health Heatwave Plan and community mental health interventions. A further important theme – and one of particular importance in the UK – has been the analysis of routinely collected health data. As well as providing a source of data on how healthcare is actually delivered to patients, such studies are invaluable for retrospectively analysing potential influences on health or outcomes. They also provide a mechanism for studying rare events where it would be impractical to organise large trials. A number of studies have analysed data held in the Health Information Network database and the General Practice Research Database. Findings have illuminated a number of areas, from risk of suicide and cardiovascular death in severe mental illness to patterns of antibiotic prescribing. A further important source of information can be routinely collected population data, such as the UK’s Adult Psychiatric Morbidity Survey. Analyses have revealed worryingly high levels of suicidal thinking (one in six of the population had had death wishes or considered suicide) 10 and of mental distress in non-heterosexual populations (roughly double levels seen in the heterosexual population) 11, and illustrated the long-term adverse impact of sexual abuse12. More positively, studies have also revealed that the UK population is, for the most part, in a good mood – 40 per cent very happy and 52 per cent fairly happy13. 10 Bebbington PE et al. Suicidal ideation, self-harm and attempted suicide: results from the British psychiatric morbidity survey 2000. Eur Psychiatry. 2010;25(7):427–31. 11 Chakraborty A, McManus S, Brugha TS, Bebbington P, King M. Mental health of the non-heterosexual population of England. Br J Psychiatry. 2011;198(2):143–8. 12 Bebbington P et al. Childhood sexual abuse and psychosis: data from a cross-sectional national psychiatric survey in England. Br J Psychiatry. 2011;199:29–37. 13 Cooper C et al. Happiness across age groups: results from the 2007 National Psychiatric Morbidity Survey. Int J Geriatr Psychiatry. 2011;26(6):608–14. POPULATION HEALTH UCL School of Life and Medical Sciences 27 The benefits of bilirubin Can the web cut problem drinking? Bilirubin, a blood breakdown product, might be protective against a range of respiratory conditions. A ‘psychologically enhanced’ online intervention reduced problem drinking – but so did its comparator. Routinely collected data held in health records are a valuable repository of information for exploring the origins of ill-health, or factors that might be protective. With evidence emerging that bilirubin might have beneficial health effects, Dr Laura Horsfall and colleagues examined the health records of more than half a million patients to look for associations between blood bilirubin levels and a range of respiratory ailments. Their analysis revealed that relatively high levels of bilirubin, within the normal range, were associated with less respiratory illness. The study looked at data on 504,206 adults without bilirubin-linked disease whose health records were part of the General Practice Research Database. Blood bilirubin levels were compared with the incidence of lung cancer, chronic obstructive pulmonary disease (COPD) and all-cause death. In all three cases, relatively high levels of blood bilirubin (though still within the range considered normal) were associated with health benefits. Each 0.1 mg/dl increase in bilirubin levels was associated with an 8 per cent decrease in the incidence of lung cancer for men and an 11 per cent decrease for women, and a 6 per cent decrease in COPD and a 3 per cent decrease mortality for men and women. A study such as this cannot identify the mechanisms by which bilirubin has a protective effect, though there is some evidence that it has anti-oxidant properties and may be protecting cells from damaging oxidant molecules. In the long term, suppressing the activity of the liver enzyme that eliminates bilirubin could be a considered as a therapeutic strategy to protect against respiratory disease. The study also highlights the advantage of research based on large numbers of health records. The UK is one of the few countries where this kind of study could have been carried out. Regular excessive drinking is extremely common and has considerable health and social impact. So the demonstration by Dr Elizabeth Murray and colleagues that an innovative web-based intervention, Down Your Drink, halved alcohol consumption might be considered good news. However, its comparator – a simple text-based website – was equally effective, leaving open the question of what is actually responsible for the drop in alcohol consumption. The Down Your Drink website was the brainchild of Dr Stuart Linke, an Islington-based clinician. Swamped with people seeking help for problem drinking, he developed a web-based resource that he could direct patients to, with support from the charity Alcohol Concern. An initial analysis found that users of the site cut their alcohol intake, but in the absence of a control group it was impossible to conclude that this was due to their use of the site. Despite no further promotion or development, the site continued to attract a steady stream of traffic, encouraging Dr Linke and Dr Murray to develop an enhanced version. The new site was founded on validated psychologically based approaches to alcohol reduction and was redesigned following extensive dialogue with users. To evaluate the new resource, the team used a simple text-based website as comparator. The site was again accessible via the Alcohol Concern website, with users randomly directed to one or other resource. The trial recruited nearly 8000 participants. Down Your Drink again achieved very positive results, reducing alcohol consumption by about a half. Strikingly, though, people using the simple website cut their drinking by a similar amount. The findings are thus difficult to interpret. Participants using the control site may have sought additional material elsewhere, helping them to achieve better results. It is also possible that the assessments used in the trial prompted all participants to cut down intake. In the meantime, some health authorities have been impressed enough to implement a version of the resource. However, implementation is raising a further issue, as it is proving difficult to persuade healthcare workers to refer individuals – partly because the numbers identified as having problematic drinking habits are staggeringly high; the perception is that something so common cannot be a problem. The fact that deaths from liver cirrhosis have increased tenfold in some age groups over the past 30 years suggests that it is. Horsfall LJ et al. Serum bilirubin and risk of respiratory disease and death. JAMA. 2011;305(7):691–7. Wallace P et al. On-line randomized controlled trial of an internet based psychologically enhanced intervention for people with hazardous alcohol consumption. PLoS One. 2011;6(3):e14740. Linke S, McCambridge J, Khadjesari Z, Wallace P, Murray E. Development of a psychologically enhanced interactive online intervention for hazardous drinking. Alcohol Alcohol. 2008;43(6):669–74. 28 POPULATION HEALTH UCL School of Life and Medical Sciences New technology also holds promise as a way of engaging members of the public in their own healthcare. Despite much enthusiasm, however, the area remains one of great potential rather than concrete progress. Specialist expertise in electronic health records is held in the UCL Centre for Health Informatics and Multiprofessional Education (CHIME). CHIME has played an important role in UK and European collaborations establishing data standards for clinical information and ensuring data privacy. In practical terms, its work with the community cardiology services of the Whittington Hospital NHS Trust has led to web-based applications supporting a range of clinical functions at the Whittington and at neighbouring hospital, primary care and pharmacy sites. CHIME is also engaged in research into computer tools to support clinical decision making, for example through the development of computerassisted diagnosis tools and analysis of the processes by which clinical guidelines are developed. New technology also holds promise as a way of engaging members of the public in their own healthcare. Despite much enthusiasm, however, the area remains one of great potential rather than concrete progress. UCL’s e-Health Unit, led by Dr Elizabeth Murray, is engaged in a range of projects covering sexual health promotion (‘Sexunzipped’), selfmanagement for type 2 diabetes and alcohol use (‘Down your Drink’), and is also exploring the impact of new technologies and information gathering on doctor–patient relationships. Part of the enthusiasm for online projects reflects their potential to provide an in-depth, individualised experience on a very large scale, with very low incremental costs. In one area, alcohol use, a systematic review by Dr Murray and colleagues suggests online interventions can work, and the Down Your Drink site has gathered encouraging data (see page 28). Success is more likely if interventions are rooted in a strong theoretical framework, to ensure that evidencebased approaches are adopted and that learning can be applied to future developments. It is also vital to get users involved in development from the very beginning. The field is new and rapidly evolving, and exactly how online approaches (or other new technologies) will ultimately affect formal healthcare or public health is hard to predict. The type 2 diabetes project aims to integrate web-based approaches into clinical care, while other interventions may be better targeted directly at the public. By reaching large numbers of people, even a small change could have substantial benefits at a population level, at very low cost. Predicting depression A simple screening tool might be sufficient to identify patients at risk of depression. Major depression is common and disabling. As with many conditions, prevention is better than cure. But while well-validated tools have been developed for common conditions such as cardiovascular disease, GPs have had no equivalent ways to identify reliably those at risk of depression. To remedy this situation, Professor Michael King and colleagues have developed and tested a simple screening tool for assessing risk of depression, PredictD, and adapted the tool for use with anxiety disorders. A healthcare screening tool needs to be sensitive, specific and practicable for everyday use. Many factors are known to increase the risk of depression but individually are of little value in guiding clinical decision-making. To develop a practical healthcare tool, Professor King and colleagues gathered data on 39 known risk factors for depression in more than 5000 non-depressed attendees at general practices in six European countries. By identifying those who experienced depression at six months or 12 months, the team was able to develop a highly specific and sensitive risk algorithm. Furthermore, the algorithm performed well when tested with an entirely independent sample of patients in Chile. The algorithm contains just nine factors, four of which are potentially open to change (physical health score, current mental health score, unsupported difficulties at work and experience of discrimination). And although the remaining five risk factors (age, sex, educational level, past experience and family history of depression) cannot be changed directly, they help to identify highrisk people who can be supported through active listening or given advice about lifestyle. Although more work needs to be done to assess its practical utility, PredictD has the potential to be used as a simple screening tool in general practice to identify patients at risk of depression. Moreover, its international development suggests it could have widespread applicability. The work has also led to a follow-up project to develop a similar tool for generalised anxiety and panic syndromes, using a similar methodology and starting with 38 known risk factors. In fact, the anxiety algorithm, PredictA, shares several constituents with PredictD, suggesting the two conditions may share at least some underlying mechanisms. King M et al. An international risk prediction algorithm for the onset of generalized anxiety and panic syndromes in general practice attendees: predictA. Psychol Med. 2011; 41(8):1625–39. King M et al. Development and validation of an international risk prediction algorithm for episodes of major depression in general practice attendees: the PredictD study. Arch Gen Psychiatr. 2008;65(12):1368-76. POPULATION HEALTH UCL School of Life and Medical Sciences 29 The original ‘Whitehall’ cohort study overturned the conventional view of work, stress and health – it was the lower orders who suffered most, not the ‘stressed executive’. Its follow-up, Whitehall II, is shedding more light on the links between socioeconomic status and health. The heart of the civil service While studying for a PhD at the University of California Berkeley in the 1970s, Michael Marmot examined the incidence of heart disease in Japanese men who had migrated to Hawaii and California. He discovered that the health advantage enjoyed by Japanese men was dissipated by migration – and the greater their cultural assimilation, the more their health was affected. The results graphically illustrated the influence of environment on heart disease. But they also raised interesting questions about how living circumstances could affect people’s health. Returning to the UK, Professor Marmot became involved in the ‘Whitehall’ study – a pioneering study examining the roots of chronic conditions in a cohort of 18,000 civil servants. He was keen to examine the influence of social and cultural factors, but the only even vaguely relevant indicator was employment grade (the UK civil service being highly hierarchical). Remarkably, analysis of heart disease data by grade revealed a very clear gradient: the further down the employment ladder 30 someone sat, the worse their health was likely to be. This flatly contradicted received wisdom. The most senior mandarins, with the supposedly most stressful jobs, should have been the ones most prone to heart disease. Not only was the reverse true – it was those at the base of the pyramid that fared worse – but there was also a clear gradient of effect: ill-health increased at every step from top to bottom. So was stress not significant after all? No: stress does not come with power, but with lack of power. The most stressful circumstances are experienced by those further down the hierarchy, who have increasingly less control over their lives and fewer opportunities to influence what goes on around them. The marked socioeconomic gradient apparent in the Whitehall study has since been seen in multiple cohorts all over the world. Almost anywhere anyone has looked, the lower someone’s socioeconomic status, the worse their health is likely to be. The first Whitehall study is thus a landmark in one of the most important health, social and political issues of the day – health inequalities. In the UK, health inequalities are dramatic. Life expectancy differs by seven years between rich and poor neighbourhoods (disabilityfree life expectancy differs by an astounding 17 years). On essentially every measure of health and well-being, a gradient exists between rich and poor (see Box). Professor Marmot has been instrumental in establishing other important cohorts, including the English Longitudinal Study of Ageing (see page 34) and population cohorts in four East European countries. He also leads a Whitehall follow up, Whitehall II. Launched in 1985, Whitehall II is tracking 10,000 civil POPULATION HEALTH UCL School of Life and Medical Sciences servants (this time including women). As well as covering some of the same territory as Whitehall I, it is also examining a wider range of psychological and psychosocial factors, diet and links between social circumstances, behaviour, biology and disease. Whitehall I (and many other studies) revealed that much of the socioeconomic gradient could be linked to socially patterned health behaviours – such as smoking or exercising too little. One challenge is to understand why these behaviours show social patterning (and ideally to do something about them). On the other hand, Whitehall data also imply that health behaviours cannot fully account for the socioeconomic gradient, suggesting an important role for other factors (particularly other ‘life-course influences’, such as neonatal and childhood experiences and even prenatal exposures). A fuller understanding of all these influences can suggest when and how to tackle health inequalities. Perhaps most significantly, they suggest that inequalities need to be tackled at an early age. At a time when medical science is increasingly searching at the smallest possible level for the causes of disease, the Whitehall studies are a reminder that ‘people interactions’, as well as molecular interactions, are fundamental to healthy lives. “In this study of civil servants, a man’s grade of employment was a stronger predictor of his subsequent risk of CHD death than any of the other major coronary risk factors.” An ideologue with evidence Professor Sir Michael Marmot has spent decades collecting information on the detrimental impact of inequalities on health, and trying to persuade those in power to tackle them. One of Michael Marmot’s first roles at the Whitehall study was as a delivery boy. With an MD and freshly minted Berkeley PhD to his name, his task was to deliver a copy of the first Whitehall paper to the Lancet. The paper described the now classic risk factors such as smoking and lack of exercise associated with chronic diseases in British civil servants. Professor Marmot’s discovery of the socioeconomic gradient in these effects had a profound impact. The pervasiveness and scale of the gradient has been demonstrated repeatedly. Rather than just documenting health inequalities, though, he has been actively involved in trying to eradicate them – the difficult territory where science meets politics. In the late 1970s, Sir Douglas Black produced the first national report on health inequalities. Commissioned by a Labour Government, by the time it was published a new Conservative government had come to power and promptly suppressed it. The issue was revisited in the 1990s by the Chief Medical Officer of the time, Sir Donald Acheson, who invited Professor Marmot to contribute. This led to a commission from the World Health Organization to investigate the social determinants of health. The resulting report, Closing the Gap in a Generation, led the recent Labour government to ask Professor Marmot to develop recommendations for tackling health inequalities in the UK. Despite a change of government, Fair Society, Healthy Lives (‘the Marmot Review’), published in 2010, has not suffered the ignominious fate of the Black Report. The Marmot Review collates a wealth of information on health inequalities, and makes no bones about the need to tackle social inequality in order to achieve health benefits. It is, he argues, simply a matter of social justice. This position has not escaped comment – one critic described Closing the Gap as ‘ideology with evidence’. It is a criticism he is happy to embrace. The WHO continues to pursue the social determinants agenda, with a world conference hosted by the government of Brazil taking place in October 2011. In Europe, work is underway on a Regional European Health Policy that will examine social determinants of health. Professor Marmot continues to press home the key messages of the Marmot Review – that the health gradient affects people significantly at all levels, at enormous social and individual cost, and the policy tools exist to do something about it. Academic outputs also continue to accumulate, delivered these days by email rather than overqualified messenger boy. Marmot M et al. Employment grade and coronary heart disease in British Civil Servants. J Epidemiol Community Health 1978;32:244–9. POPULATION HEALTH UCL School of Life and Medical Sciences 31 SECTION 4 How to age successfully The key to a healthy old age is to live healthier in early life and to adopt a positive frame of mind to ageing. It also helps to be wealthy… 32 POPULATION HEALTH UCL School of Life and Medical Sciences With longevity continuing to increase at a remarkable rate – currently around three months for every year lived – health and well-being in old age become ever more important. Globally, there were around 600 million people aged 60plus in 2000 and numbers are projected to rise to 1.2 billion by 2025 and 2 billion by 2050. Ageing is also of profound importance to healthcare systems: more than half of an individual’s lifetime healthcare costs typically accumulate after the age of 65. A longer-living population can be considered a great achievement. However, adding extra years to lifespan is only one part of the equation – quality of life in those years needs to be considered too. The concept of ‘successful ageing’ has become increasingly popular. Although not rigorously defined, the term captures a sense of later life free from chronic diseases and with the freedom to function effectively, both physically and mentally. The term has been attributed to US academic R J Havighurst in the 1960s, who likened it to ‘adding life to years’ rather than just ‘years to life’. The concept of ‘successful ageing’ has become popular. Although not rigorously defined, the term captures a sense of later life free from chronic diseases and with the freedom to function effectively, both physically and mentally. ‘Ageing’ is in some senses a counter-intuitive idea as it does not equate simply with number of years lived. Differences in lifestyle can mean that two people who have lived the same number of years are at quite different stages of ageing. Similarly, biological markers of ageing – accumulated damage to cells – do not correspond directly to years lived. Hence, just as some 80-year-olds seem as sprightly as 60-year-olds, biological markers of ageing may be equally divergent from chronological age. Ageing is accompanied by a characteristic set of changes, affecting both physical and mental function. Older people typically experience a decline in physical strength and loss of muscle mass as well as some loss of cognitive powers. Many conditions also show an association with age, including cancers, chronic conditions and, notably, dementia and neurodegenerative disorders. Longitudinal studies have enormous power to shed light on ageing at a population level. In particular, they can provide a life-course perspective that examines the consequences of past life experiences on the timing and nature of ageing. Indeed, the take-home message could be that successful ageing begins at birth – or even before. One crucial factor is, inevitably, socioeconomic status. Findings from the Whitehall II study (see page 30) indicate that the impact of socioeconomic status actually increases in old age14. Physical health worsened more rapidly for workers on lower grades, such that the average physical age of a 70-yearold in a high grade was equivalent to that of a 62-year-old in a low grade. Although mental health improved at both ends of the socioeconomic gradient, those at the top gained more, again increasing health inequalities. Since most of the civil servants had retired at the time of analysis, the results suggest that occupational status has long-lasting impacts, and raise concerns about a possible growth in inequalities in old age. 14 Chandola T, Ferrie J, Sacker A, Marmot M. Social inequalities in self reported health in early old age: followup of prospective cohort study. BMJ. 2007;334(7601):990. POPULATION HEALTH UCL School of Life and Medical Sciences 33 An ageing raw deal? Much ado about ageing Older patients may be being treated less favourably, according to a large-scale analysis of GPs’ behaviour. A comparison between ageing in the UK and the USA ignited a firestorm of controversy in the USA, while scarcely raising a ripple in the UK. Since 2010 it has been against the law in the UK to discriminate against people on the basis of their age. Even so, the research of Professor Rosalind Raine and colleagues suggests that older people are not receiving the same level of care as younger citizens. GPs hold positions of considerable influence within the UK National Health Service, not least by deciding who should be referred for specialist treatment. In theory factors such as age (or sex or socioeconomic circumstances) should have little or no influence on these decisions. Yet an analysis of GP consultations on more than 125,000 patients – 5500 with post-menopausal bleeding, 23,000 with hip pain and 100,000 with dyspepsia – revealed significant age-related inequalities in referral across all three conditions. This study made use of the Health Improvement Network database, as did a further study examining drug prescribing behaviour for stroke patients. Despite explicit guidance, just 25.6 per cent of men and 20.8 per cent of women received lipid-lowering drugs for secondary prevention – and there was a clear age gradient in the numbers receiving drugs. The odds of 80–89-yearolds receiving drugs was almost half that of 50–59-year-olds. This is particularly shocking as drug use halved mortality – mortality after one year was 5.7 per cent in patients receiving drugs and 11.1 per cent in those not prescribed them. Similar trends were seen in an analysis of hospital data, and treatment for three common cancers (colorectal, breast and lung cancer) in half a million patients. Despite a national plan to reduce inequalities in cancer care, age-related inequalities existed for all three cancer types. Older people were more likely to be admitted as emergencies rather than as planned admissions, and less likely to have their preferred treatments. Planned admissions are generally associated with better outcomes, so the disparities could underlie age-related differences in survival. Equity of access is a fundamental principle of the NHS. Yet for age – as well as sex and socioeconomic status – that principle may not be being met in practice. McBride D, Hardoon S, Walters K, Gilmour S, Raine R. Explaining variation in referral from primary to secondary care: cohort study. BMJ. 2010;341:c6267. Raine R et al. Social variations in access to hospital care for patients with colorectal, breast, and lung cancer between 1999 and 2006: retrospective analysis of hospital episode statistics. BMJ. 2010;340:b5479. Despite having just 5 per cent of the world’s population, the USA accounts for more than half of all money spent on healthcare globally. So when a study published by Professor Sir Michael Marmot and colleagues found that seniors in the UK generally enjoyed better health than those in the USA, the impact was profound. The work compared participants aged 55–64 in the US Health and Retirement Survey and UK English Longitudinal Study of Ageing. One factor common to both countries was the socioeconomic gradient – in both the USA and the UK, the lower someone’s socioeconomic status, the worse their health was likely to be. Adjusting for purchasing power, the USA was spending almost twice as much on its healthcare as the UK. Yet on seven key measures of health – diabetes, hypertension, heart disease, myocardial infarction, stroke, lung disease and cancer – UK seniors were doing better than their US peers. Moreover, the findings were not due to national biases in reporting: several biological markers of disease showed similar patterns. The US and UK health systems are quite different, with the UK’s NHS providing free healthcare at the point of delivery and the US relying on health insurance. Yet access to healthcare was not the cause of the disparity: the vast majority of the US cohort had health insurance. The story was front-page news in the USA, and Professor Marmot was still fielding media calls weeks later. A New York Times editorial, headlined ‘Our sick society’, noted that “…Americans are so much sicker that the richest third of Americans is in worse health than the poorest third of the English.” Oddly, the UK media showed little interest – a classic example of bad news being a stronger story than good news. Stung by the findings, the US National Institute on Aging asked the National Research Council to examine the USA’s relatively poor standing in life expectancy. Other studies have followed up the ELSA analysis, identifying a similar pattern across other age groups – leading one commentator to note that, “exporting the poorest English to America might improve the average health status of both countries!” Curiously, conventional risk factors account for only a proportion of the US–UK differences. There may be a deeper structural explanation: the social support systems characteristic of the UK may be having a hidden benefit, lifting health levels across the board. Banks J, Marmot M, Oldfield Z, Smith JP. Disease and disadvantage in the United States and in England. J Am Med Assoc. 2006;295(17):2037–45. 34 POPULATION HEALTH UCL School of Life and Medical Sciences Whitehall II has also generated evidence on earlier influences on ageing. A recent analysis suggested that a rather sobering 13 per cent of men and 15 per cent of women could be said to be ageing successfully15. As well as midlife socioeconomic status, successful ageing was also predicted by ‘healthy lifestyle’ factors – not smoking, diet and exercise. Notably, though, it was also affected by education (for men) and height (particularly for women), which probably reflects childhood factors such as nutrition. Interesting sex differences were seen, with moderate alcohol consumption being important for women and work support for men. Other cohorts are also generating important information on ageing, not least the English Longitudinal Study of Ageing (ELSA), led by Professor Sir Michael Marmot and Professor Andrew Steptoe in collaboration with researchers from the Institute of Fiscal Studies and the National Centre for Social Research. Modelled on the US Health and Retirement Study, it is intended to provide an integrated view of the health, economic and social aspects of ageing, and to provide a source of evidence to inform UK health and social policy. It samples around 7000 people over the age of 50 every two years. ELSA has also shown that the socioeconomic gradient is felt as keenly in later life as at earlier stages. Between the first two waves of the survey, participants aged 50–59 from the poorest fifth of the population were more than 10 times more likely to die than their peers from the richest fifth16. For most measures relevant to health and quality of life, greater wealth is associated with higher scores. ELSA is part of a wider European programme, SHARE, the Survey of Health, Ageing and Retirement in Europe. First begun in 11 countries, it now covers 45,000 individuals aged 50plus across 13 countries. Important European data are also being collected through the HAPIEE (Health, Alcohol and Psychosocial Factors in East Europe) study, organised by Professor Marmot and Dr Martin Bobak, which is following four cohorts in Russia, Poland, the Czech Republic and Lithuania. The health of East Europeans typically lagged that of West Europeans in the Communist era, but this effect was exacerbated by the fall of Communism. Life expectancy plummeted: between 1990 and 1994, male life expectancy in Russia fell by six years to 57. However, life expectancy has varied in complex ways across East Europe. The HAPIEE study is exploring the theory that alcohol consumption, diet and nutrition, and economic circumstances have been responsible for reducing life expectancy. Although recent evidence suggests more positive trends, data analysed to date suggest that unhealthy lifestyles are having a significant impact on health17. Although originally established to examine factors affecting childbirth, the 1946 Birth Cohort, now the responsibility of Professor Diana Kuh at the MRC Unit for Lifelong Health and Ageing, has refocused on health and well-being at the end of life. The world’s longestrunning birth cohort, it will provide a unique glimpse of life-course influences, from cradle to grave, on an ageing population. The 1946 Birth Cohort is part of a suite of cohorts examining ageing, known as HALCyon (Healthy Ageing Across the Life Course), which collectively cover some 30,000 participants. As with the Whitehall cohorts, the 1946 Birth Cohort has documented a wide range of influences across the life course that influence later-life health and well-being. For example, several factors have been found to affect physical capability in later life, which is in turn predictive of mortality. Interestingly, perceptions of when old age begins may be a good indicator of future longevity. In the Whitehall II cohort, those who thought old age began at relatively early ages were likely to die sooner than those who thought it began at later ages. Attitudes were influenced by current health, as well as by socioeconomic status, the extent of social networks and perceived life control. Similarly, in ELSA surveys, those who think of themselves as younger than their actual age have better health than those who think of themselves as older. Health inequalities could be exacerbated if older people receive less favourable treatment by the NHS. Indeed, Professor Rosalind Raine and colleagues have found evidence that older people do not always receive the same levels of care as younger people, in primary and secondary care (see page 34). In trials, Professor Michael King and colleagues have shown that cognitive behavioural therapy is an effective treatment for elderly people with depression, even though they are rarely offered it18. Interventions relevant to older people are among the studies being carried out at the Priment Clinical Trials Unit. These include ProAge65, which aims to boost exercise in people aged 65 15 Britton A, Shipley M, Singh-Manoux A, Marmot MG. Successful aging: the contribution of early-life and midlife risk factors. J Am Geriatr Soc. 2008;56(6):1098–105. 16 Banks J, Breeze E, Lessof C, Nazroo J. eds. Retirement, health and relationships in the older population in England: the English Longitudinal Study of Ageing 2004 (wave 2). 2006. London: Institute for Fiscal Studies. 17 Boylan S et al. Dietary habits in three Central and Eastern European countries: the HAPIEE study. BMC Public Health. 2009;9:439. 18 Serfaty MA et al. Clinical effectiveness of individual cognitive behavioral therapy for depressed older people in primary care: a randomized controlled trial. Arch Gen Psychiatry. 2009 (12):1332–40. POPULATION HEALTH UCL School of Life and Medical Sciences 35 and over, and randomised trials of cognitive stimulation for dementia and of support for carers of people with dementia (all funded through the NIHR). A study funded by the Food Standards Agency, led by Dr Alan Dangour of the London School of Hygiene and Tropical Medicine, is examining whether vitamin B12 supplements improve cognitive function in older people. In addition, the HOPE trial is evaluating a home-based intervention for frail older people. UCL also contributes to other important research infrastructure. It acts as the north London hub of the Mental Health Research Network and is the coordinating centre for the north London hub of DeNDRoN (Dementias and Neurodegenerative Diseases Research Network). Dementia Perhaps the most profound challenge to successful ageing, for individuals, families and health services, will come from dementia. There are currently around 600,000 people in the UK with dementia, a number likely to rise to 840,000 by 2026 and 1.2 million by 2050. Globally it accounts for more years lived with disability than stroke, heart disease and cancer combined, and the annual healthcare cost to 36 the UK is projected to rise to a staggering £50 billion by mid-century. UCL researchers are at the forefront of dementia health research. Professor Steve Iliffe, the UK’s only Professor of Primary Care for Older People, has made numerous contributions to healthcare guidelines, and helped to establish the UK Department of Health’s National Dementia Strategy in 2008 (see page 37). Dr Elizabeth Sampson (supported by Marie Curie Cancer Care) has raised awareness of the need for palliative care for people with dementia, as well as characterising numerous issues with hospital care of elderly patients with dementia (see page 37). As well as affecting patients, dementia can have a substantial impact on carers. Professor Gill Livingston, Dr Claudia Cooper and colleagues have drawn attention to the problems they face before a diagnosis is given, when few support mechanisms are available. She has also documented concerning levels of abusive behaviour by carers towards patients, one-third of whom reported ‘significant’ levels of abuse19. Even more worryingly, follow up a year later found an increase in abusive behaviour, associated with symptoms of anxiety and depression in carers20. Conversely, more than a third of carers had experienced abuse from the person with dementia they were looking after 21. Dementia is also an important theme of UCL’s Deafness, Cognition and Language research centre, led by Professor Bencie Woll. The centre is leading a project, funded by the Alzheimer’s Society, which aims to improve early diagnosis and management of dementia among Deaf people who use British Sign Language. Almost nothing is currently known about how dementia affects Deaf people, or how it could be diagnosed. Researchers are studying normal ageing with the help of several hundred Deaf people who meet each year for a holiday organised by the English Deaf Darby and Joan Club. The team is also exploring the experiences of Deaf people with dementia and their carers, to identify their priorities for care and how to improve early identification and support services. A significant programme of work at UCL is exploring ways to use brain imaging to provide earlier detection of neurodegenerative disorders (see companion volume, Neuroscience and Mental Health). POPULATION HEALTH UCL School of Life and Medical Sciences Over the longer term, ways to promote more successful ageing may come from a better understanding of the basic biological processes involved in ageing. UCL hosts one of the world’s leading research centres in ageing, led by Professor Dame Linda Partridge – who, among many honours, was awarded the title ‘Living Legend’ by Help the Aged in 2006. Working mainly with model organisms, Professor Partridge’s Institute of Healthy Ageing is gathering key insight into the genes and physiological processes that affect ageing, work that may suggest strategies to promote healthier ageing in people (see companion volume, on Basic Life Sciences). 19 Cooper C et al. Abuse of people with dementia by family carers: representative cross sectional survey. BMJ. 2009;338:b155. 20 Cooper C, Blanchard M, Selwood A, Walker Z, Livingston G. Family carers’ distress and abusive behaviour: longitudinal study. Br J Psychiatry. 2010;196(6):480–5. 21 Cooper C, Selwood A, Blanchard M, Livingston G. Abusive behaviour experienced by family carers from people with dementia: the CARD (caring for relatives with dementia) study. J Neurol Neurosurg Psychiatry. 2010;81(6):592–6. Dying with dementia Diagnosing dementia Acute hospital wards are not geared up for patients with dementia, and patients would rather not be there either. Can a GP education programme improve the early diagnosis of dementia? Dementia currently affects some 700,000 people in the UK and numbers are projected to surpass 1 million before mid-century. Increasingly, people at the end of their lives will be suffering from dementia, with multiple medical and social care needs. Supported by Marie Curie Cancer Care, Dr Elizabeth Sampson has highlighted the major problems associated with hospital admission for this group of patients, as well as possible solutions based on coordinated palliative care pathways. The study of more than 600 acute hospital admissions of patients aged over 70 revealed not only a significant prevalence of dementia – 42.4 per cent overall, rising to 75.0 per cent in those over 90 – but also alarmingly high numbers of undiagnosed cases, half of the total. Patients with dementia fared significantly worse than those without – those with most severe cognitive impairment were three times more likely to die during admission. Patients with dementia were also much more likely to suffer a healthcare-related ‘adverse event’, possibly because medical staff were not aware of walking difficulties or other deficits (several patients with short-term memory problems were instructed to use call bells). The results suggest that admission to hospital is not prolonging life for meaningful periods. Ironically, the evidence also suggests that most patients would prefer to die at home. Working with the London Borough of Haringey, and Barnet, Enfield and Haringey Mental Health Trust, Dr Sampson’s team has also undertaken a more detailed examination of the experience of individuals and agencies involved in a small number of terminal cases. This work identified examples of good practice, as well as highlighting problem areas and reasons why patients are admitted to hospital. Coordination between different agencies is a challenge, and emergency services were often involved because staff in nursing homes or other carers were concerned about the medico-legal consequences of not seeking emergency help. The study has enabled Haringey to develop a care pathway for patients with dementia nearing the end of their lives. Dr Sampson’s work has highlighted the growing issue of palliative care for people with dementia. It has fed into the UK’s national strategy for dementia and informed policy development at the Alzheimer’s Society. More generally, it has raised awareness of the value of ‘advanced care plans’, in which patients can lay out their wishes and guide the actions of carers and healthcare and social support teams as they enter their final days. Dementia is a devastating condition for patients and for their carers. The scale of the problem is vast – globally, it is responsible for 11.2 per cent of years lived with disability (more than heart disease and cancer combined). In the UK, annual costs of £17bn are projected to rise to £50bn by 2040. Dementia is not one of primary care’s strengths, and Professor Steve Iliffe and colleagues are testing whether an educational package can improve one important area – early diagnosis. It is clear that dementia is not being spotted early, for several reasons. Patients and families may see symptoms of dementia as typical signs of ageing, or be put off by the enduring stigma attached to a diagnosis of dementia. Similarly, doctors may be influenced by the risk of stigmatisation, and may not think a diagnosis of dementia is in the patient’s best interests. Moreover, dementia is difficult to assess, and the typical GP may make only one or two diagnoses a year. Nevertheless, the benefits of early diagnosis are generally thought to outweigh these drawbacks. When appropriate, drug use can be begun earlier, and both families and support agencies can take steps to prepare for a patient’s inevitable decline. Even so, an analysis of data in the Health Improvement Network primary care database found strikingly high mortality rates, much higher than in community samples, implying late diagnosis at time of crisis. To improve early diagnosis, Professor Iliffe’s team tested three approaches – a CD-ROM, practice-based workshops and decision-based software – in a randomised controlled trial in 36 practices. Both the workshops and the software significantly improved detection rates – but had little impact on what GPs then did. Following up this encouraging start, the team is now conducting a second trial, EVIDEM-ED, in 20 practices and with 200 patients to see if a combination of workshops and electronic information can go one step further and alter the clinical management of patients with dementia. Professor Iliffe was instrumental in developing the early diagnosis guidelines for the UK’s National Dementia Strategy, launched in 2009. If the EVIDEM-ED trial is successful it may point to a way to tackle at least one important aspect of dementia care. Sampson EL, Blanchard MR, Jones L, Tookman A, King M. Dementia in the acute hospital: prospective cohort study of prevalence and mortality. Br J Psychiatr. 2009;195(1):61–6. Rait G et al. Survival of people with clinical diagnosis of dementia in primary care: cohort study. BMJ. 2010;341:c3584. Watkin L, Blanchard MR, Tookman A, Sampson EL. Prospective cohort study of adverse events in older people admitted to the acute general hospital: risk factors and the impact of dementia. Int J Geriatr Psychiatr. 2011. doi: 10.1002/ gps.2693. Downs M et al. Effectiveness of educational interventions in improving detection and management of dementia in primary care: cluster randomised controlled study. BMJ. 2006;332(7543):692-6. Iliffe S et al. Evidence-based interventions in dementia: A pragmatic cluster-randomised trial of an educational intervention to promote earlier recognition and response to dementia in primary care (EVIDEM-ED). Trials. 2010;11:13. POPULATION HEALTH UCL School of Life and Medical Sciences 37 A pioneering study of childbirth has become an equally pioneering study of ageing. Sixty-five years young Babies born in the first week of March 1946 were particularly special. They were enrolled in a groundbreaking study exploring the factors contributing to healthy birth. Remarkably, 65 years later, many of these infants are still contributing to science, as part of the world’s longest running birth cohort. In between they have contributed to a host of influential studies shaping multiple areas of health and social policy. In 1946 there was considerable concern about the UK’s declining birth rate, and the potential impact of poverty and poor living conditions. James Douglas, a doctor noted for his work on air raid casualties, was asked to organise a nationwide study to examine these factors. At their routine eight-week follow-up, health workers across the country were asked to interview all mothers who had given birth during the first week of March. Remarkably, for a country still recovering from the traumas of the Second World War, by June 1946 nearly 14,000 mothers had been interviewed – more than 90 38 per cent of eligible families. The results were reported a year later and a book on the survey, Maternity in Great Britain, was published in 1948. The results painted a dramatic picture of the realities of childbirth for socially disadvantaged women. Neonatal mortality was 19 per 1000 births for the wealthiest families but 30 per 1000 for the poorest. Less well-off mothers had lower birthweight babies. With no NHS backup, the poorest mothers could not afford to have a doctor present at birth, and as few midwives could administer gas and air, just 20 per cent of mothers received any kind of pain relief during birth. The shock of this last finding triggered the first policy impact – a parliamentary bill that changed the rules on the administration of pain relief. Maternity in Great Britain was so successful that funding was rapidly agreed for a follow up study – 5362 infants becoming part of the National Survey of Health and Development. Although its future has occasionally been in doubt, the study has continued ever since, evolving to shed light on different questions at different life stages, with the Medical Research Council (MRC) providing funding since 1962. The study proved highly influential. Its findings changed the way children were looked after in hospital and how they were taught in primary schooling. The insight it shed on the UK education system’s failure of bright children from less well off families had a particular profound impact. In mid-life, work on the cohort shifted focus, with an increasing emphasis on health. Indeed, the longevity of the cohort has contributed considerable insights into ‘life course’ influences on health. Much of our health is dependent on the accumulated impact of past experiences – many of them carefully recorded in the cohort records. This information has provided an opportunity to see how participants’ health in later life has been influenced by their experiences in childhood and earlier adult life. Even what happens before birth has turned out to be significant, with the study providing some of the first evidence that low POPULATION HEALTH UCL School of Life and Medical Sciences birthweight had an impact on the risk of higher blood pressure in adult life, as well as many other aspects of adult function and chronic disease risk in later life such as diabetes. By contrast, babies of higher birthweight are at higher risk of breast cancer. Sadly, born out of concerns about the impact of poverty, the cohort continues to provide evidence of the damaging impact of inequality on health as well as social opportunities, providing much material for the 2010 Marmot Review (see page 30). Current research on the cohort is providing an insight into ageing – and tying in early-life events to later life decline. Most participants are still going strong, but as they collectively pass their 65th birthdays the effects of passing years begin to tell. The cohort is now the responsibility of the MRC Unit for Lifelong Health and Ageing, led by Professor Diana Kuh, and forms part of a multi-cohort collaboration, HALCyon (Healthy Ageing across the Life Course), also led by Professor Kuh. The nine HALCyon cohorts collectively include some Choose your parents well… The secret to long life, so the joke goes, is to choose your parents well. As we age, physical strength becomes a highly significant factor in health and longevity. Loss of physical capabilities dramatically reduces quality of life and increases the risk of death, for example through falls. Work by the MRC Unit for Lifelong Health and Ageing has shown that lower levels of physical capability (in terms of muscle strength and physical performance) is associated with a greater risk of death, and has revealed how factors throughout life – and even before birth – affect physical capabilities in mid- and later life. Physical capabilities can be measured relatively easily, by assessing grip strength, walking speed, the time taken to rise from a chair and ability to balance while standing. One striking finding has been the importance of socioeconomic status to these measures, in childhood as well as adulthood. A father’s occupation and a mother’s education level both affect later-life physical performance. A metaanalysis carried out under HALCyon confirmed this observation. Work on the 1946 Birth Cohort was also the first to demonstrate that childhood growth and development influenced mid-life physical strength. Other contributing factors include cognitive abilities (associated with better balance), the timing of developmental milestones, and physical activity. For men, being married and having children were associated with higher levels of physical capability. As well as confirming the long-term impact of socioeconomic disadvantage on health, the studies also suggest that protection against frailty in old age could be achieved by promoting physical fitness decades early. Cooper R et al. Objectively measured physical capability levels and mortality: systematic review and meta-analysis. BMJ. 2010;341:c4467. doi: 10.1136/bmj. c4467. Kuh D et al. Developmental origins of midlife physical performance: evidence from a British birth cohort. Am J Epidemiol. 2006;164(2):110–21. Strand BH, Cooper R, Hardy R, Kuh D, Guralnik J. Lifelong socioeconomic position and physical performance in midlife: results from the British 1946 birth cohort. Eur J Epidemiol. 2011;26(6):475–83. Birnie K et al. Childhood socioeconomic position and objectively measured physical capability levels in adulthood: a systematic review and meta-analysis. PLoS One. 2011;6(1):e15564. Guralnik JM et al. Reduced midlife physical functioning among never married and childless men: evidence from the 1946 British birth cohort study. Aging Clin Exp Res. 2009;21(2):174–81. 30,000 participants born between 1918 and 1958. Much of the success of 1946 Birth Cohort studies has been down to the excellent phenotypic data gathered over such a long period. This has recently enabled studies to contribute to large-scale studies searching for genetic influences on health. This adds insight into genetic as well as environmental influences. But they also add a unique life course dimension, revealing not just which genetic variants might be influential but when they might be influential. A further exciting emerging opportunity is the study of ‘epigenetic’ effects – control of gene activity by chemical modification of DNA. Indeed, epigenetic changes may be one route by which environmental factors have a long-term influence on cells and tissues. Cohort studies may thus be the ideal approach for studying how this interplay between genes, epigenetics and the environment shapes physiology and health over decades of life. Kuh D et al. Cohort profile: updating the cohort profile for the MRC National Survey of Health and Development: a new clinic-based data collection for ageing research. Int J Epidemiol. 2011;40(1):e1–9. Pearson H. Study of a lifetime. Nature. 2011:471;20–4. POPULATION HEALTH UCL School of Life and Medical Sciences 39 SECTION 5 Global health research The greatest public health needs lie outside the UK, particularly in the developing world. Despite some encouraging progress, profound global changes – particularly linked to climate change – threaten to make a bad situation much worse. 40 POPULATION HEALTH UCL School of Life and Medical Sciences Resource-poor countries have traditionally been blighted by infectious diseases, some restricted to tropical areas and others more globally distributed but having a disproportionate impact on less-developed countries. Infectious diseases such as HIV/AIDS, tuberculosis and malaria (and countless others) remain key challenges. But developing countries also face a second wave of health threats, linked to major demographic shifts and changing lifestyles. Noncommunicable diseases are becoming of ever greater importance, particularly in urban areas – now home to more than half the world’s population. Other causes of illness and death should not be overlooked. Road traffic accidents and injury (including violent injury) are major problems. Mental health problems – predicted by the WHO to be the greatest burden of disease by 2020 – are generally not well recognised or treated. Furthermore, developing countries also find themselves at the mercy of global forces over which they have precious little control. Climate change threatens many populations – from those in low-lying coastal areas facing greater saltwater ingression and An important feature of these trials has been their participative nature. Rather than plan interventions in advance, researchers work with communities to identify key health issues and ways they might be addressed. flooding to agricultural communities dealing with a greater likelihood of extreme weather and drought. Global trade, economics and politics can all exert influences that ultimately affect people’s lives. Few developing countries have adequate health infrastructure. One solution is to mobilise communities, creating networks of health support workers at a local level. Professor Anthony Costello and colleagues have pioneered such an approach to tackle neonatal mortality in Asia (see page 43). Randomised clinical trials have demonstrated significant benefits, with interventions that are realistic and potentially scalable. The trial in India was awarded ‘Trial of the Year’ by the Society for Clinical Trials, which described the work as an “extraordinary randomised clinical trial, conducted with high quality in a very difficult setting, and achieving dramatic results of great public health importance”. An important feature of these trials has been their participative nature. Rather than plan interventions in advance, researchers work with communities to identify key health issues and ways they might be addressed. Priorities are thereby established by the communities themselves, generating a greater sense of ownership and increasing the chances that benefits will be maintained after the trial. Further trials are currently underway in Nepal, Bangladesh and Malawi. As well as playing a major part in these trials, Wellcome Trust Senior Research Fellow Dr David Osrin is leading a programme of research on the health of slum dwellers in Mumbai. He has a particular interest in maternal health and nutrition, and works closely with local community groups and organisations. UCL also has major research interests in Africa. One of the most significant has been Professor MarieLouise Newell’s involvement in the Wellcome Trust’s Africa Centre for Health and Population Studies in KwaZulu-Natal, South Africa, which Professor Newell has led on secondment from UCL since 2005. Research POPULATION HEALTH UCL School of Life and Medical Sciences 41 Zumla has also highlighted the alarming rise of TB in the UK – particularly in London, where the numbers of cases rose by nearly 50 per cent in 1999–2009. at the Africa Centre has revealed much about the dynamics of HIV infection in a poor rural community and the impact of antiviral rollout programmes. The Africa Centre has one of the largest demographic surveillance systems in Africa, covering 90,000 people. The area has been badly affected by HIV: one in four of the local population has the virus, including half of all women aged 25–29; 22 per cent of children have lost at least one parent to AIDS. The Centre works extremely closely with the local community, playing an important role in healthcare delivery as well as research, and ultimately aims to have a significant impact on the spread of HIV locally – though its research is also of broader international significance. Professor Newell and colleagues have carried out influential work on motherto-child transmission of HIV, including the Mamanengane trial (‘Mamanengane’ is Zulu for ‘mother and child’), which showed that exclusive breastfeeding was feasible for both infected and uninfected women, and resulted in markedly lower transmission of HIV to offspring compared to breastfeeding combined 42 with solid food22. The study contributed to new WHO guidelines on infant feeding. The Centre also contributed to the landmark multicentre Kesho Bora trial, which showed that antiretrovirals effectively prevented transmission of HIV during pregnancy and breastfeeding. The Centre has also been actively involved in the rollout of antiretrovirals. It has generated vital evidence that rollout in poor rural areas does deliver substantial health improvements, in adults and children. The Centre is also beginning the ‘Treatment as Prevention’ trial, to see if antiretroviral use can reduce HIV transmission as well as help patients. Africa has also been the main focus of Professor Alimuddin Zumla, one of the world’s leading experts on TB. Professor Zumla is involved in a wide range of initiatives centred on practical methods of HIV diagnosis and new drug treatments. He has also been a tireless advocate of the need to tackle TB – responsible for nearly two million deaths every year. The disease is not just a problem in Africa: it is a major issue in the restructuring economies of East Europe, and Professor Professor Zumla led a Lancet TB Series, a set of definitive reviews of key issues around TB. The series is linked to the Lancet TB Observatory, a global initiative addressing the most important issues in TB control and treatment. He has done much to develop research in his home country, helping to found the University of Zambia– University College London Medical School (UNZAUCLMS) Research and Training Project, a regional centre of excellence linked to six south African countries and six in Europe. Long-term collaborator Dr Peter Mwaba, recipient of the Royal Society of Tropical Medicine and Hygiene’s prestigious Chalmers Medal in 2005, has gone on to become Zambia’s Permanent Secretary in the Ministry of Health. TB is also a focus for Dr Tim McHugh, who is part of a nationwide consortium of academic groups, the UK tuberculosis drug development consortium (TBD-UK). Supported by the MRC, TBD-UK aims to provide a focus for increased activity on TB drug development and facilitate early stages of drug development within the academic environment. TBDUK has identified several promising chemicals with anti-TB activity. Dr McHugh’s team is also playing an important role in the Pan-African Consortium for the Evaluation of Antituberculosis Antibiotics (PanACEA), a European– African initiative organising clinical trials of new drug treatments designed to shorten and simplify TB treatment. The UCLsponsored REMoxTB trial, POPULATION HEALTH UCL School of Life and Medical Sciences one of the largest ever undertaken in TB treatment, is assessing whether use of moxifloxicin can reduce treatment length from six to four months. PanACEA also incorporates two other trials led from Germany and The Netherlands, to which the UCL team is also contributing. Capacity building is an important aspect of the REMoxTB trial. The REMoxTB laboratory team has ensured that laboratories in host countries are brought up to international standards for clinical trials. The UCL team has also developed a manual of microbiological techniques – essential for work in TB – and trained staff in their use at participating sites, an important transfer of knowledge and skills. As well as generating important findings on TB treatment, the work should also leave the Africa centres well-placed to conduct further clinical trials in the future. The REMoxTB trial also involves the MRC Clinical Trials Unit, which is embedded within UCL. The Unit has organised a series of ground-breaking clinical trials of HIV treatments in Africa, led by Professor Diana Gibb (see page 43). The DART trial of antiretrovirals in Uganda and Zimbabwe, for example, has shown that it is not necessary to use hightech equipment to monitor people on therapy, vitally important in resource-poor countries. Moreover, the trial infrastructure provided a platform on which other studies could be added – creating a suite of DART projects. As well as HIV drug therapies, other trials have tested vaginal microbicidal 22 Coovadia H, Rollins N, Bland R et al. Mother-to-child transmission of HIV-1 infection during exclusive breastfeeding: the first six months of life. Lancet. 2007;369:1607–16. DART sharpens practice Two out of three Results from the DART trial suggest that laboratory analysis is not essential to successful HIV treatment – paving the way for wider roll-out of antiretroviral therapies. Two large trials have shown that community-based interventions can significantly reduce neonatal mortality in poor rural areas. The past decade has seen a much-needed influx of antiretroviral drugs into Africa, even if many in need still have little access to them. As well as availability of affordable drugs, getting antiretrovirals to patients is difficult in countries with negligible healthcare infrastructures. Moreover, in developed countries antiretroviral use is typically guided by CD4 cell numbers, which requires specialist equipment and regular blood testing to check for drug side-effects. Yet the DART trial found that, in typical African settings, laboratory testing for safety provided no benefits and measuring CD4 counts offered only minimal benefits at significant additional cost – which, in budget-limited times, could be better spent on improving access to antiretrovirals. The DART (Development of Antiretroviral Therapy) trial compared treatment based on either laboratory testing of CD4 counts or clinical assessment in more than 3000 HIV-infected adults commencing antiretroviral therapy in Uganda and Zimbabwe. Coordinated by the MRC Clinical Trials Unit, DART was the largest trial of antiretrovirals ever carried out in Africa. Survival in both arms of the trial was remarkably good – in the laboratory tests arm, 90 per cent of patients were still alive after five years, as were 87 per cent of patients managed clinically. The difference between the two groups only appeared in later years, and probably reflected switching of patients onto second-line drugs in the laboratory tests arm, after drops in CD4 cell numbers provided warning signs of first-line treatment failure. However, given the economic and practical difficulties involved in laboratory testing, this small difference could be greatly outweighed by the potential benefits of treating more patients. Health economic analyses suggest that, for the same investment needed to achieve laboratory testing, the numbers of patients treated could be increased by about a third. Professor Anthony Costello and colleagues have pioneered an inclusive, participatory approach to the development of interventions to improve neonatal health. Large-scale trials in Nepal and India have been highly successful, reducing neonatal mortality by up to 45 per cent. The failure of a trial in Bangladesh was therefore disappointing, but may have identified some of the factors critical to the success of this approach. Nearly 4 million neonatal deaths occur each year, 98 per cent of them in the developing world. Reducing this number is essential if Millennium Development Goal 4, reducing child mortality by two-thirds, is to be met. However, the challenge is daunting. In rural areas, health service infrastructures are limited and mothers have little access to trained antenatal healthcare. Interventions have to recognise these constraints and consider issues such as sustainability – will changes be maintained after the trial – and scalability: could an intervention be applied to larger populations. Professor Costello’s group has developed a distinctive bottom-up and participatory approach. Rather than descend on populations with ready-planned interventions, his team works with community groups to identify key health issues and potential solutions. The effectiveness of these interventions is then tested in randomised trials. Using this approach, the UCL team has worked with women’s groups to develop low-cost interventions which achieved excellent results in Nepal – reducing neonatal mortality by 30 per cent. A similar strategy was even more successful in two regions of India, cutting neonatal deaths by 45 per cent in a high-mortality area. These dramatic success stories are tempered by the results from a study in Bangladesh, which failed to achieve any improvement in mortality rates. The failure may, however, highlight important factors necessary for successful interventions. In Bangladesh, the women’s groups covered larger populations, and group coordinators had more groups to coordinate. Local factors, such as adverse weather conditions, may also have affected the effectiveness of the delivery of the intervention. Collectively the studies suggest that women’s group could play an important role in neonatal healthcare in the developing world. However, particular care needs to be given to how interventions are developed and implemented to ensure they are successful. Mugyenyi P et al. Routine versus clinically driven laboratory monitoring of HIV antiretroviral therapy in Africa (DART): a randomised non-inferiority trial. Lancet. 2010;375(9709):123–31. Manandhar DS et al. Effect of a participatory intervention with women’s groups on birth outcomes in Nepal: cluster-randomised controlled trial. Lancet. 2004;364:970–9. Tripathy P et al. Effect of a participatory intervention with women’s groups on birth outcomes and maternal depression in Jharkhand and Orissa, India: a cluster-randomised controlled trial. Lancet. 2010;375(9721):1182–92. Azad K et al. Effect of scaling up women’s groups on birth outcomes in three rural districts in Bangladesh: a cluster-randomised controlled trial. Lancet. 2010;375(9721):1193–202. POPULATION HEALTH UCL School of Life and Medical Sciences 43 Climate change threatens to have a disproportionate effect on the world’s poorest (and, ironically, those who have contributed least to it). gels and a prototype HIV vaccine. Ongoing trials include ARROW, comparing first-line treatments for children with HIV, and EARNEST, which aims to identify the best second-line options in resource-poor settings. Is a bolus the best? A clinical trial in Africa has raised serious questions about a routinely used treatment for severe shock in children. The symptoms of severe shock are all too common in African children, typically associated with malaria or bacterial infection. In the developed world, infants in shock are rapidly given rehydrating fluids in a single intravenous shot or ‘bolus’. Smallscale (but uncontrolled) trials in Africa had suggested that a similar approach might also be beneficial in low-resource setting. But a large, multicentre, randomised controlled trial organised by Professor Kath Maitland at the Wellcome Trust– KEMRI Research Programme, Kilifi, Kenya, and Professor Diana Gibb and colleagues from the MRC Clinical Trials Unit was stopped early when it became clear that the fluid bolus was actually increasing mortality compared with giving fluids slowly – raising major questions about the procedure in rich as well as poor countries. The study, carried out in six hospitals in Kenya, Tanzania and Uganda, compared two different types of bolus infusion – saline and albumin solution – with no infusion. Otherwise, children received WHO-recommended standards of emergency care. Recruitment was based on symptoms – the underlying causes of severe shock are rarely known on admission to hospital – though children with malnutrition or gastroenteritis were excluded. The study was halted after around 3000 infants had been treated, when it became clear that an extra three to four deaths occurred within 48 hours for every 100 children given a bolus. Of note, the clinical systems used in the trial actually resulted in better survival rates overall. Survival rates of between 80–85 per cent are typical in African children with shock, whereas in this study 89.4 per cent of those given boluses survived the first 48 hours in hospital. Children given fluids more slowly did even better, however, with 92.7 per cent surviving. The results are disappointing but imply that rapid fluid resuscitation for shock is not advisable in resource-poor settings. The reasons are unclear, underlining the current limited understanding of shock. Furthermore, the findings raise questions about fluid management in the developed world, where fluid resuscitation is believed to have contributed to a major reduction in paediatric deaths from septic shock but has never been formally assessed in a randomised controlled trial. Maitland K et al. Mortality after fluid bolus in African children with severe infection. New Engl J Med. 2011;364(26):2483–95. 44 Other studies have focused on prevention. In Zimbabwe, Dr Frances Cowan and colleagues have carried out one of the world’s largest trials of a behavioural intervention. The trial failed to achieve any lasting impact on HIV transmission, illustrating just how hard it can be to alter behaviour. The Africa Centre has noted a similar phenomenon, with HIV transmission rates remaining stubbornly high. Diversity Beyond infectious disease, UCL researchers are exploring a diverse range of international health issues. Professor Therese Hesketh, for example, is one of the UK’s leading experts on healthcare in China. She has been leading a major project, funded by the UK Department for International Development, which aims to address inequalities in access to medicines in rural areas of China with a total population of around 15 million people. Professor Hesketh’s previous work has identified high levels of stress in China’s highly pressured primary schools23. She has also drawn attention to the excess numbers of boys and sex-selective abortion in China24. In 2005, there were 32 million more boys than girls under 20. POPULATION HEALTH UCL School of Life and Medical Sciences Professor Nora Groce, an anthropologist formerly at Yale University, is leading a programme of work on disability and social inclusion in the developing world. An adviser to the WHO, UNICEF and UNFPA, Professor Groce was guest editor of a special issue of the Lancet dedicated to disability. Epidemiologist Dr David Batty is carrying out a wide range of analyses of data from the UK, Europe and further afield. He has examined associations between adult obesity and cancer mortality in more than 400,000 participants from Asia, Australia and New Zealand. Although data are scarce in Asia, overweight and obese individuals in populations across the Asia-Pacific region have a significantly increased risk of mortality from several types of common cancers. Dr Batty is also studying risk factors for suicide in more than one million adults in South Korea, which has one of the world’s highest suicide rates. Although child mortality remains desperately high in many countries, some progress has been made. But there is also evidence that premature death of older children and young adults is not receiving the attention it deserves. Using WHO figures, Professor Russell Viner and colleagues in Australia and Switzerland found that, of 2.6 million deaths in young people aged 10–24 years in 2004, 97 per cent were in the developing world25. Deaths rate were particularly high in older age groups and although causes varied by sex, age and region, maternal conditions, traffic accidents and violence were all having an impact on the same scale as the classic infectious diseases. The global environment The future health of many communities is intimately bound up with global ‘big issues’ – climate change, international trade, migration and urbanisation, and population growth. Reflecting these profoundly important issues, UCL’s global health research is increasingly multidisciplinary. In 2009, the UCL–Lancet Commission on Managing the Health Effects of Climate Change described climate change as ‘the biggest global health threat of the 21st century’. The commission, which drew on UCL expertise in 19 different units, including law, anthropology, politics, economics and engineering as well as public health and international development, drew attention to the current health impact of climate change, as well as its potential future catastrophic effects26. Climate change threatens to have a disproportionate effect on the world’s poorest (and, ironically, those who have contributed least to it). The commission recommended framing climate change in terms of its health impact, to galvanise decision-makers and promote action across a number of domains to limit carbon consumption and to encourage adaptation. The Commission called for a ‘collation of global expertise’ and a new multidisciplinary and multisectoral public health movement to coordinate thinking and action across governments, international agencies, NGOs, and academic institutions. In related work, Yvonne Rydin, Professor of Planning, Environment and Policy, is leading an initiative on ‘Healthy Cities’, which is assessing how changing the built environment might affect the health of residents. This ranges from examining community-led sanitation projects in Mumbai to how social housing might affect mental health in London. Links between urban development, climate change and sustainable cities are an important theme. Economic perspectives are provided by such luminaries as Professor Costas Meghir and Professor Orazio Attanasio. With economist Dr Noemi Pace, Professor Costello has highlighted how speculative investment in food commodity derivatives can disrupt the supply of food to meet human needs27. UCL organises a wide range of events linked to global health. In May 2011, with funding from the Leverhulme Trust, it hosted a symposium on ‘Population Footprints: Challenging debates on popular, gender and development’. The event brought together groups that might not normally interact, including researchers, policy makers and advocates from a broad range of fields. Almost 300 delegates took part, representing 33 countries, and a satellite meeting, with 100 delegates, was held in Kenya. The initiative also included a public event, and follow-up public engagement activities. 23 Hesketh T et al. Stress and psychosomatic symptoms in Chinese school children: cross-sectional survey. Arch Dis Child. 2010;95(2):136–40. 24 Zhu WX, Lu L, Hesketh T. China’s excess males, sex selective abortion, and one child policy: analysis of data from 2005 national intercensus survey. BMJ. 2009;338:b1211. 25 Viner RM et al. 50-year mortality trends in children and young people: a study of 50 low-income, middle-income, and high-income countries. Lancet. 2011;377(9772):1162–74. 26 Costello A et al. Managing the health effects of climate change: Lancet and University College London Institute for Global Health Commission. Lancet. 2009;373(9676):1693–733. 27 Pace N, Seal A, Costello A. Food commodity derivatives: a new cause of malnutrition? Lancet. 2008;371(9625):1648–50. POPULATION HEALTH UCL School of Life and Medical Sciences 45 Population Health research at UCL Component institutes Most of the population health research at UCL is carried out by groups within the UCL Faculty of Population Health Sciences, which comprises: • UCL Institute of Epidemiology and Health Care • UCL Institute of Child Health • UCL Institute for Women’s Health The broader Population Health Domain at UCL encompasses researchers across the whole of the UCL School of Life and Medical Sciences, as well as individuals with relevant interests outside the School. Domain Chair: Professor Anne Johnson www.ucl.ac.uk/slms/domains/population-health • UCL Institute of Cardiovascular Science Dean: Professor Graham Hart www.ucl.ac.uk/populationhealth-sciences/ UCL in London Partners Researchers in the UCL School of Life and Medical Sciences occupy a range of buildings on UCL’s central Bloomsbury Campus, at the nearby Royal Free Hospital and Whittington Hospital/Archway Campus sites, and other central London locations. UCL School of Life and Medical Sciences works closely with a range of local, national and international partners. Of particular significance are its close links to local NHS bodies, collectively forming UCL Partners, one of just five UK Academic Health Science Centres. These links underpin UCL’s NIHR Biomedical Research Centres at UCLH, the UCL Institute of Child Health (with Great Ormond Street Hospital) and the UCL Institute of Ophthalmology (with Moorfields Eye Hospital). 1 UCL Main Campus 2 UCL Hospital 3 Great Ormond Street Hospital and UCL Institute of Child Health 4 Moorfields Eye Hospital and UCL Institute of Ophthalmology 5 Royal Free Hospital and UCL School of Medicine 6 Whittington Hospital and Archway Campus With the MRC, Wellcome Trust and Cancer Research UK, UCL is also a founding partner of the Francis Crick Institute, led by Professor Sir Paul Nurse, which is due to open in 2015. UCL also establishes wider partnerships in the UK, for example with Imperial College to set up the London Centre for Nanotechnology, and with Imperial, King’s College London, the MRC and GlaxoSmithKline on the ‘Imanova’ clinical imaging initiative. The agreement was forged under the umbrella of the Global Medical Excellence Cluster (GMEC), a public–private partnership bringing together world-leading academic, health and industrial partners in South-East England. 6 5 2 1 4 3 46 The School has also developed ties with nearby academic centres, including the London School of Hygiene and Tropical Medicine and Birkbeck College. As well as many joint research initiatives, the institutions also liaise at a strategic level. London As well as numerous international research collaborations, UCL has developed a strategic alliance with Yale University, the Yale–UCL Collaborative, to promote cross-fertilisation and joint ventures across education, research and application. POPULATION HEALTH UCL School of Life and Medical Sciences Support: Resource centres and platforms Research income The scale of UCL’s research enables it to provide a range of technical infrastructure platforms to support research. These include outstanding facilities and technical expertise in molecular and cellular imaging, as well as pre-clinical and clinical imaging, and several sites specialising in high-throughput sequencing and genome analysis. ‘Live’ grants as at 1 September 2011 Other core platform technologies cover small-chemical libraries, proteomics, biological services and transgenics, and informatics. UCL researchers are also involved in numerous biobanking initiatives and cohort studies, providing access to extensive collections of materials and data. UCL also provides capital infrastructure funding to enable labs to develop their equipment base. For clinical research, a Research Support Centre provides access to essential support for work on people and patients, including liaison with the UCLH/UCL NIHR Biomedical Research Centre, UCL Clinical Trials Unit and UCLH/UCL Clinical Research Facility. The Translational Research Office works to promote the translation of research into therapies, techniques and products with therapeutic value. www.ucl.ac.uk/platforms/ www.ucl.ac.uk/slms/research_support_centre NIHR and other UK Government £177.1m MRC £194.6m Other UK Research Councils UK charities £83.3m £500.4m £53.6m Commercial (UK and international) EU£78.4m £62.6m Other international, inc. NIH Other£14.7m Total£1164.7m Figures refer to research within the UCL School of Life and Medical Sciences. NIHR: National Institute for Health Research; MRC: Medical Research Council; NIH: National Institutes of Health. UCL Grand Challenges UCL is committed to developing wise and timely counsel to address significant intellectual, cultural, scientific, economic, environmental and health problems. The UCL Grand Challenges – of Global Health, Sustainable Cities, Intercultural Interaction and Human Wellbeing – facilitate collective, collaborative working practices in order to gain fresh perspectives and address aspects of the world’s key problems in their full complexity. We are also intent on making the resulting conclusions compelling to policy makers and practitioners. POPULATION HEALTH UCL School of Life and Medical Sciences 47 Sponsors of research We are grateful to all the individuals and organisations who support research in the UCL School of Life and Medical Sciences. Abbott France, Abbott Laboratories, Ablynx NV, Academy of Medical Sciences, Action Medical Research, Action on Hearing Loss, Adam Dealy Foundation, Against Breast Cancer, Age UK (Formerly Research Into Ageing), Agennix AG, Aims 2 Cure, Alcohol Education and Research Council, Alder Hey Children’s NHS Foundation Trust, Alexion Pharmaceuticals, Allergan Inc., Alpha-1 Foundation, Alzheimer’s Society, Alzheimer’s Research UK, Amyotrophic Lateral Sclerosis Association, Anatomical Society of Great Britain & Ireland, Anna Freud Centre, Anthony Nolan Bone Marrow Trust, Apatech Ltd, Apitope Technology (Bristol) Ltd, Aqix Ltd, Argonne National Laboratory, Ark Therapeutics Ltd, Arthritis Research UK, Arts and Humanities Research Council, Assisted Conception Unit, Association for International Cancer Research, Association Francaise Contre les Myopathies, Association Monegasque Contre Les Myopathies, Association of Coloproctology of Great Britain and Ireland, Asthma UK, Astra Zeneca (UK) Ltd, Ataxia UK, Autonomic Disorders Association – Sara Matheson Trust, AVI BioPharma Inc., AXA Research Fund, Bachmann-Strauss Dystonia and Parkinson Foundation, Baily Thomas Charitable Trust, Baily Thomas Charitable Trust, Barts and The London Charity, Batten Disease Family Association, Baxter Healthcare Corp., Bayer – AG, Bayer SAS, Big Lottery Fund, Bill & Melinda Gates Foundation, Biochemical Society, Biocompatibles Ltd, Biogen, Biogen Idec Inc., Biomarin Pharmaceutical Inc., Biorex R&D, Biotechnology and Biological Sciences Research Council, Birkbeck College, Biss Davies Charitable Trust, Boehringer Ingleheim, Bone Cancer Research Trust, Brain Research Trust, Breast Cancer Campaign, Bristol Myers Squibb, British Academy, British Council for Prevention of Blindness, British Heart Foundation, British HIV Association, British Lung Foundation, British Medical Association, British Neurological Research Trust, British Orthodontic Society, British Pharmacological Society, British Psychological Society, British Retinitis Pigmentosa Society, British Skin Foundation, British Society for Haematology, British Tinnitus Association, British Urological Foundation, BUPA Foundation Medical Research Charity, Burdett Trust for Nursing, Burroughs Wellcome Fund, Cambridge University Hospital NHS Foundation Trust, Camden and Islington Health Authority, Canadian Institutes of Health Research, Cancer Fund, Cancer Research Institute USA, Cancer Research UK, Carbon Trust Ltd, Carl Zeiss Surgical GMBH, Celera Corp., Cell Medica Ltd, Centocor Inc., Central and East London CLRN, Central Research Fund, Cephalon Inc., Charles Wolfson Charitable Trust, Chemel AB, Child Growth Foundation, Child Health Research Appeal Trust, Children Living with Inherited Metabolic Diseases (CLIMB), Children With Cancer UK, Children’s Brain Diseases, Children’s Cancer and Leukaemia Group, Children’s Liver Disease Foundation, Children’s Research Fund, Children’s Trust, Chordoma Foundation, Chronic Fatigue Syndrome Research Foundation, Chronic Granulomatous Disease Trust, Chugai Pharma Europe Ltd, Cincinnati Children’s Hospital Medical Center, Circulation Foundation, CLEFT – Bridging The Gap, Clement Wheeler Bennett Trust, CMT UK, Cobra Bio-Manufacturing PLC, Cochlear Research and Development Ltd, Coda Therapeutics Inc., Cogent (Holdings) Ltd, Colgate-Palmolive Europe, College of Optometrists, Colt Foundation, Creating Resources for Empowerment and Action Inc., Cure Parkinson’s Trust, Cure PSP – Society for Progressive Supranuclear Palsy, Cyberonics Inc., Cystic Fibrosis Research Trust, Cystinosis Foundation Ireland, Cystinosis Research Network Inc., David and Elaine Potter Charitable Foundation, Davis Schottlander & Davis Ltd, Deafness Research (Formerly Defeating Deafness), Defense Advanced Research Projects Agency, Department for Children, Schools and Families, Department for Education and Skills, Department for International Development, Department of Health, Department of Health and Human Services, Department of Trade and Industry, Dermatitis and Allied Diseases Research Trust, Deutsche Forschungsgemeinschaft, Diabetes Research and Wellness Foundation, Diabetes UK, Diagenode SA, Doctors Laboratory, Dowager Countess Eleanor Peel Trust, Duchenne Parent Project, Dystonia Medical Research Foundation, Dystrophic Epidermolysis Bullosa Research Association, East Midlands Specialised Commissioning Group, Economic and Social Research Council, Edinburgh University, Edmond J Safra Philanthropic Foundation, Effort – Eastman Foundation, Efic, Eisai (London) Research Laboratories Ltd, El.En. S.p.A, Elan Pharmaceuticals Ltd, Eli Lilly and Co. Ltd, Emergency Nutrition Network, Engineering and Physical Sciences Research Council, Epic Database Research Company Ltd, Epilepsy Action, 48 Epilepsy Research UK, Eular – European League Against Rheumatism, Eurocoating S.P.A, European and Developing Countries Clinical Trials, European Association for the Study of Liver, European Commission, European Huntington’s Disease Network, European Organisation For Research and Treatment of Cancer, European Orthodontic Society, European Parliament, European Respiratory Society, European Society for Immunodeficiencies, Eve Appeal, Experimental Psychology Society, F Hoffmann La Roche Ltd, Fidelity Foundation, Fight For Sight, Fondation de France, Food Standards Agency, Foundation for Fighting Blindness, Foundation for Liver Research, Foundation for the Study of Infant Deaths, Foundation Leducq, Frances and Augustus Newman Foundation, Frost Charitable Trust, Fundacao Bial, Gatsby Charitable Foundation, Gen-Probe Life Sciences Ltd, Genentech Inc., General Charitable Trust of ICH, General Medical Council, Genethon, Genex Biosystems Ltd, Genzyme Corp., Gilead Sciences Inc., GlaxoSmithKline, Glaxosmithkline (China) R&D Co. Ltd, Global Alliance for TB Drug Development, Government Communications Planning Directorate, Great Britain Sasakawa Foundation, Great Ormond Street Hospital Charity, Great Ormond Street Hospital Special Trustees, Grifols UK Ltd, Grovelands Priory Hospital, Grunenthal GMBH, Guarantors of Brain, Guide Dogs for the Blind Association, Gynaecological Cancer Research Fund, H J Heinz Co. Ltd, Harbour Foundation, Health and Safety Executive, Health Foundation, Health Protection Agency, Healthcare Commission, Healthcare Quality Improvement Partnership, Heart Research UK, Helpage International – Africa Regional Development, Henry Smith Charity, Hestia Foundation, High Q Foundation, Histiocytosis Research Trust, Hospital For Sick Children, Human Early Learning Partnership, Human Frontier Science Program, Human Genome Sciences Inc., Huntington’s Disease Association, Ichthyosis Support Group, Illumina Cambridge Ltd, Imperial College Consultants Ltd, Imperial College of Science, Technology and Medicine, Inhibox Ltd, Institut de Recherche Servier, Institut Straumann AG, Instrumentarium Science Foundation, Intensive Care Society, International Association for the Study of Pain, International Balzan Foundation, International Child Development Programme, International Glaucoma Association, International Primary Care Respiratory Group, International Serious Adverse Events Consortium, International Spinal Research Trust, Ipsen Fund, Ipsen Ltd, Iqur Ltd, ISTA Pharmaceuticals, ITI Foundation, Jabbs Foundation, James S McDonnell Foundation, James Tudor Foundation, Janssen Pharmaceutica NV, Janssen-Cilag Ltd, Japan Society for the Promotion of Science, Jean Corsan Foundation, Jerini Ophthalmic Inc., John Templeton Foundation, John Wyeth & Brother Ltd, Johns Hopkins University, Johnson & Johnson Consumer Services EAME Ltd, Juvenile Diabetes Foundation, Katherine Dormandy Trust, Kay Kendall Leukaemia Fund, Kidney Research UK, Kids Company, Kids Kidney Research, King’s Fund, King’s College London, Legal and General Assurance Society Ltd, Leonard Cheshire Disability, Leukaemia and Lymphoma Research, Leverhulme Trust, Lincy Foundation, Linkoping University, Linnean Society of London, Lister Institute of Preventive Medicine, Liver Group, London Borough of Camden, London Deanery, London School of Hygiene and Tropical Medicine, Lowe Syndrome Trust, Lowy Medical Research Institute, Ludwig Institute for Cancer Research, Lund University, Lupus UK, Lymphoma Research Trust, Macmillan Cancer Relief (UK Office), Macular Disease Society, Marc Fisher Trust, Marie Curie Cancer Care, Mars Symbioscience, Mary Kinross Charitable Trust, Mason Medical Research Foundation, Matt’s Trust Fund for Cancer, Maurice Hatter Foundation, Max Planck Institute for Molecular Genetics, Max Planck Institute of Biology and Ageing, Medac GmBH, Medical Research Council, Medical Research Council of Canada, Medical Research Foundation, Melford Charitable Trust, Mend Central Ltd, Meningitis Research Foundation, Meningitis Trust, Merck Ltd, Merck Serono, Mermaid, Michael and Morven Heller Charitable Foundation, Michael J Fox Foundation for Parkinson’s Research, Middlesex Hospital Special Trustees, MIND, Mologic Ltd, Monument Trust, Moorehead Trust, Moorfields Eye Hospital (LORS), Moorfields Eye Hospital Development Fund, Moorfields Eye Hospital Special Trustees, Moorfields Hospital NHS Foundation Trust, Motor Neurone Disease Association, Moulton Charitable Trust, Mr and Mrs Fitzpatrick, MRCP(UK), MSS Research Foundation, Multiple Sclerosis International Federation, Multiple Sclerosis Society of Great Britain and Ireland, Mundipharma Research Ltd, Muscular Dystrophy Association, Muscular Dystrophy Campaign, Myasthenia Gravis Association, Myeloma UK, National Association for Colitis and Crohn’s Disease, National Brain Appeal, National Cancer Institute, National Centre for Social Research, National Centre for the POPULATION HEALTH UCL School of Life and Medical Sciences Replacement, Refinement and Reduction of Animals in Research, National Contest for Life, National Eye Institute, National Geographic, National Health and Medical Research Council, National Institute for Health and Clinical Excellence, National Institute for Health Research, National Institute of Academic Anaesthesia, National Institute of Mental Health, National Institutes of Health, National Kidney Research Fund, National Multiple Sclerosis Society, National Osteoporosis Society, National Screening Committee, Natural Environment Research Council, NCL Stiftung, Netherlands Organisation for Scientific Research, Neuroblastoma Society, New England Research Institutes Inc., Newlife Foundation For Disabled Children, NHS Blood and Transplant, NHS Executive, NHS Patient Safety Research Programme, Nicholls Foundation, Nicox SA, NIHR School of Primary Care Research, Nippon Telegraph and Telephone Corporation, No Surrender Charitable Trust, Nobel Biocare AB, North Essex Mental Health Partnership NHS Trust, Northern California Institute for Research and Education, Novartis Pharma AG, Novartis Pharmaceuticals Corp., Novartis Pharmaceuticals UK Ltd, Novo Nordisk Pharmaceuticals Ltd, Nuffield Foundation, Ocean Park Conservation Foundation, Ocera Therapeutics Inc., Octapharma, Office for National Statistics, Options Consultancy Services Ltd, Organisation for the Understanding of Cluster Headache, Organon Laboratories Ltd, Orphan Europe (UK) Ltd, Ovarian Cancer Action, Overweight and Heart Diseases Research Trust, Oxalosis and Hyperoxaluria Foundation, Oxford Optronix Ltd, Oxigene Inc., Ozics OY, Paediatric Rheumatology Discretionary Fund, Palaeontological Association, Pancreatic Cancer UK, Parkinson’s Disease Society, Path Vaccine Solutions, Pathogen Solutions UK Ltd, Pathological Society of Great Britain and Ireland, Paul Hamlyn Foundation, PCI Biotech, Pelican Cancer Foundation, Peptide Protein Research Ltd, Pervasis Therapeutics Inc., Peter Samuel Fund, Petplan Charitable Trust, Pfizer Ltd, Philips Medical Systems NL BV, Philips Oral Healthcare Inc., Physiological Society, Planer Plc, Polycystic Kidney Disease Charity, Primary Immunodeficiency Association, Procter and Gamble Technical Centre Ltd, Progressive Supranuclear Palsy (PSP Europe) Association, Prostate Action, Prostate Cancer Research Centre, PTC Therapeutics Inc., Qatar National Research Fund, Race Equality Foundation, Rank Bequest, Raymond and Beverly Sackler Foundation, Raynaud’s and Scleroderma Association, Repregen Ltd, Research in Motion Ltd (Canada), Research into Childhood Cancer, Rheumatology Discretionary Fund, Rho Inc., RMS Innovations UK Ltd, Roche Bioscience, Roche Products Ltd, Rockefeller Foundation, Roddick Foundation, Ronald McDonald House Charities UK, Rosetrees Trust, Roslin Cells Ltd, Royal Academy of Engineering, Royal Centre for Defence Medicine, Royal College of Anaesthetists, Royal College of General Practitioners, Royal College of Ophthalmologists, Royal College of Paediatrics, Royal College of Physicians, Royal College of Radiologists, Royal College of Surgeons of England, Royal Free Cancer Research Trust, Royal Free Hampstead NHS Trust, Royal Free Hospital Special Trustees, Royal National Institute for the Blind, Royal Society, Samantha Dickson, Sanofi Pasteur, Sanofi-Aventis, Santhera Pharmaceuticals Ltd, Sarah Cannon Research UK Ltd, Sarcoma Alliance for Research Through Collaboration, Save The Children, Science and Technology Facilities Council, Scope International AG, Selcia Ltd, Sheffield Teaching Hospitals NHS Foundation Trust, Shire Human Genetic Therapies AB, Siemens plc, Sir Halley Stewart Trust, Sir Jules Thorn Charitable Trust, Skeletal Cancer Action Trust Plc, SMA Trust, Smith & Nephew Plc, Society for Endocrinology, Society for Pediatric Radiology, Sport Aiding Medical Research For Kids (SPARKS), St George’s Hospital Medical School, St Peter’s Research Trust, Stanford University, Stanley Medical Research Institute, Stanley Thomas Johnson Foundation, Stanmore Implants Worldwide Ltd, Stroke Association, Sue Harris Bone Marrow Trust, Summit plc, Supreme Biotechnologies Ltd, Susan G Komen Breast Cancer Foundation, Swiss National Science Foundation, Syngenta, Sysmex Ltd, Takeda Cambridge Ltd, Takeda Europe Research and Development Centre Ltd, Takeda Pharmaceutical Co. Ltd, Tana Trust, Target Ovarian Cancer, Tavistock and Portman NHS Trust, Tavistock Trust for Aphasia, Technology and Medicine, Technology Strategy Board, Teenage Cancer Trust, Thomas Pocklington Trust, Thrombosis Research Institute, Tissue Regenix Group Plc, Tourette Syndrome Association Inc., Toyota Motor Europe, Tuberous Sclerosis Association of Great Britain, UBS AG, UCB Pharma SV, UCB S.A, UCLH/UCL Comprehensive Biomedical Research Centre, UK Clinical Research Collaboration, UK Human Tissue Bank, UK Stem Cell Foundation, Unilever UK Central Resources Ltd, United Kingdom Continence Society, United Therapeutics Corporation, University College London Hospitals, University College London Hospitals Charities, University Medical Center Hamburg–Eppendorf, University of Alabama at Birmingham, University of California, University of Coimbra, University of Iowa, University of Kansas Medical Center, University of Kwazulu-Natal, University of London, University of Oulu, University of Oxford, University of Rochester, University of Southampton, University of Sussex, University of Washington, University of Western Australia, Varian Ltd, Ventana Medical Systems Inc., Veterinary Laboratories Agency, Vitaflo International Ltd, Vital Therapies Inc., Vitol Charity Fund, Wayne State University, Weight Concern, Weizmann UK, Wellbeing of Women, Wellchild, Wellcome Trust, Welton Foundation, Wockhardt UK Ltd, Wolfson Foundation, World Cancer Research Fund, World Health Organization, World Vision International, Wyeth Laboratories and Wyeth Pharmaceuticals Inc. CREDITS Commissioned photography: David Bishop (pages 7, 19, 22, 25, 26, 34, 37). Other images from UCL/UCLH collections except cover: iStockphoto/ CEFutcher; page 2: iStockphoto/Paha_L; page 4: iStockphoto/Brosa; page 5: iStockphoto/Mishatc; page 6: iStockphoto/Reynardt; pages 7, 8: iStockphoto/Rubberball; page 8: iStockphoto/nano; page 9: CNRI/Science Photo Library; page 10: iStockphoto/RapidEye; page 11: Ian Jones; pages 12–13: iStockphoto/stuartbur; page 13: iStockphoto/sonicken; page 13: iStockphoto/RapidEye; page 14: iStockphoto/sjlocke; page 15: Mary Evans Picture Library/Roger Mayne; page 16: Krista Kennell/ZUMA/Corbis; page 17: iStockphoto/Juanmonino; page 18: Jean-Yves Sgro/Visuals Unlimited/Corbis; page 18: iStockphoto/Kuzma; page 19: iStockphoto/Blend_Images; page 20: iStockphoto/Photo_Concepts; page 21: iStockphoto/skynesher; page 22: iStockphoto/AndreasKermann; page 23: iStockphoto/mimal; page 24: Paul Griggs, Wellcome Images; page 24: Anna Tanczos, Wellcome Images; page 26: PBNJ Productions/Corbis; page 27: Wellcome Images; page 27: Justine Desmond, Wellcome Images; page 28: Ed Kashi/Corbis; page 28: iStockphoto/ sjlocke; page 29: iStockphoto/surpasspro; pages 30–31: Peter Macdiarmid/ Getty Images; page 32: iStockphoto/Yuri_Arcurs; page 33: Punchstock; page 34: iStockphoto/Falcon76; page 35: iStockphoto/DavorLovincic; page 36: istockphoto/monkeybusinessimages; page 36: Najlah Feanny/Corbis; page 37: iStockphoto/AlexRaths; page 38: iStockphoto/filizturkseven; page 40: iStockphoto/guenterguni; page 41: Frederic Soltan/Corbis; page 42: Africa Centre for Health and Population Studies; page 43: Clive Chilvers, Wellcome Images; pages 43, 45: iStockphoto/hadynyah; page 44: John Stanmeyer/VII/ Corbis; page 45: Nyani Quarmyne/Aurora Photos/Corbis. Text: Ian Jones, Jinja Publishing Ltd Design: Jag Matharu, Thin Air Productions Ltd © UCL. Text may not be reproduced without permission. The UCL ‘dome’ logo and the letters ‘UCL’ are the registered trademarks of UCL and may not be used without permission. TAP1345/16-12-11/V8 POPULATION HEALTH UCL School of Life and Medical Sciences 49 About UCL Founded in 1826, UCL was the first English university established after Oxford and Cambridge, the first to admit students regardless of race, class, religion or gender, and the first to provide systematic teaching of law, architecture and medicine. UCL is among the world’s top universities, as reflected by performance in a range of international rankings and tables. Alumni include Marie Stopes, Jonathan Dimbleby, Lord Woolf, Alexander Graham Bell, and members of the band Coldplay. UCL currently has over 13,000 undergraduate and 9,000 postgraduate students. Its annual income is over £700 million. www.ucl.ac.uk UCL Gower Street London WC1E 6BT Tel: +44 (0)20 7679 2000