Reduced-Form Behavioral Public Finance Josh Schwartzstein 1 / 37
advertisement

Reduced-Form Behavioral Public Finance
Josh Schwartzstein
Based on joint work with Sendhil Mullainathan, Kate Baicker, and Bill Congdon
1 / 37
Background
Growing recognition that behavioral tendancies matter for thinking about
a variety of policy problems
I
commodity taxation – e.g., sin taxes
(e.g., Gruber and Koszegi 2001, O’Donoghue and Rabin
2006, Chetty et al. 2009)
I
savings – e.g., new levers like defaults available to policy-maker
(e.g.,
Madrian and Shea 2001, Carroll et al. 2009, Beshears et al. 2008)
I
I
I
health insurance design – no longer clear incentives/insurance
trade-off (e.g., Baicker, Mullainathan, and Schwartzstein 2013)
unemployment insurance (e.g., DellaVigna and Paserman 2005, Spinnewijn 2014)
energy efficiency – may want to subsidize energy-efficient behaviors by
more than suggested by externalities alone (e.g., Allcott, Mullainathan and Taubinsky
2011)
2 / 37
Background
To make progress, the literature has largely proceeded by drawing out the
implications of particular biases in these settings
I
I
commodity taxation – present-bias (e.g., Gruber and Koszegi 2001, O’Donoghue and Rabin
2006), inattention (e.g., Chetty et al. 2009, Goldin 2014)
savings – present-bias (e.g., Carroll et al. 2009), inattention, anchoring (Bernheim et al.
2011)
I
health insurance design – present-bias
(e.g., Newhouse 2006),
false beliefs
(e.g.,
Pauly and Blavin 2008)
I
unemployment insurance – present-bias (e.g., DellaVigna and Paserman 2005),
overoptimism (e.g., Spinnewijn 2014), reference-dependent preferences (e.g.,
DellaVigna et al. 2014 )
I
energy efficiency – inattention (e.g., Allcott, Mullainathan and Taubinsky 2011; Allcott and
Taubinsky 2014), present-bias (e.g., Heutel 2011)
3 / 37
Observation
This literature can feel a bit scattered
I
Biases vary from paper to paper
I
It is difficult to easily assess which results extend and which depend
on the specific psychologies considered
Compare with traditional public finance: provides a much more integrated
treatment for how different policy levers affect total welfare
Goal: develop a reduced-form framework that highlights lessons that are
robust across specific psychologies and contexts
4 / 37
Roadmap
1. Illustrate features of framework through a specific example on health
insurance design
I
Based on Baicker, Mullainathan, and Schwartzstein (2014, first draft
2010)
2. Give a flavor for broader framework and implications
I
Based on Mullainathan, Schwartzstein and Congdon (2012)
5 / 37
Keep in Mind
Some things to keep in mind
I
I
The reduced-form approach is a complement, not a substitute for
drawing out the implications of specific behavioral assumptions
The focus will be on normative issues, but not so much on how to
identify welfare
I
I
I
Others have focused on the identification question, e.g., Bernheim and
Rangel (2009), Hojman and Green (2008), Rubinstein and Salant
(2011)
The focus will primarily be on analyzing the impact of standard price
levers rather than nudges
Reduced-form approaches have a long tradition in public finance
I
E.g., in the spirit of the “sufficient statistics literature” (e.g., Chetty
2009)
6 / 37
Health Insurance
Problem of health insurance design: trade-off between financial protection
and moral hazard
Example:
I
Josh gets a headache of severity s
I
Treatment provides benefit b(s) and costs c
I
It is socially efficient for Josh to get treated only if headache is
sufficiently severe: b(s) > c
The problem of health insurance
I
I
I
Insurance means Josh only pays p < c
Josh seeks treatment if b(s) > p
7 / 37
Standard Model
Standard model: The concern is overutilization due to moral hazard
8 / 37
Example: Type-II Diabetes
Diabetes:
I
Can have many serious complications (e.g., blindness, lost limbs,
coma)
I
Broad consensus of how to treat
I
Adherence to treatment recommendations has been shown to reduce
the probability of adverse events
But many do not adhere
I
I
Recent study: almost half of diabetic patients did not consistently fill
prescriptions, doubling their risk of hospitalization (Sokol et al. 2005)
9 / 37
Examples of Underuse of High Value Care
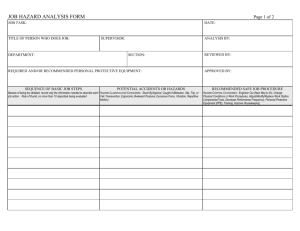
Table 1a: Examples of Underuse of High Value Care
Estimates of return to care
Usage rates of
clinically relevant
population
Statins
Reduce all cause mortality (Relative Risk .90),
cardiovascular disease mortality (RR .8), fatal
myocardial infarction (RR.82), non-fatal MI (RR.74),
and strokes (RR .86)
Adherence < 70%
Beta-blockers
Reduce mortality by 25% post heart attack
Adherence < 70%
Anti-asthmatics
Reduced Hospital Admissions (OR .58). Improvement Adherence < 50%
in airflow obstruction (OR .43)
Anti-diabetics
Decrease of cardiovascular mortality (OR .74); risk
of hospitalization halved
Adherence < 65%
Immunosuppresants
Reduction in the risk of organ rejection seven-fold
Adherence < 66-75%
Recommended Preventive
Care
Care of known efficacy including immunizations,
disease management, follow-up care post surgery
Pre-natal care
Inadequate prenatal care increases infant mortality
(RR 2.13)
<55% care delivered
(36% diabetics receiving
semi-annual blood tests,
40% colorectal cancer
45.8 % received
adequate or better care
10 / 37
What’s Going On?
Mis-measurement?
I
Perhaps unobserved side effects drive underuse
I
Given clinical evidence, hard to argue for many of these examples
Heterogeneity?
I
I
Perhaps there is a lot of heterogeneity and people properly self sort
Evidence tends to be inconsistent with this hypothesis
I
e.g., studies examining heterogeneous demand responses to co-pay
changes by clinical status (Goldman et al. 2006)
Dynamic moral hazard?
I
Perhaps people underuse preventive care because they are insured in
the future
I
We focus on underuse where benefits seem to outweigh costs to the
consumer ; i.e., uninsurable costs of non-adherence are large
11 / 37
What’s Going On?
Present-bias?
I
In deciding whether to get recommended preventive care, a
present-biased agent underweighs the delayed benefits (Newhouse
2006)
I
Should get treated if
b(s) = v (s) − k(s) > p,
v (s) represents delayed benefits and k(s) represents immediate costs
I
Gets treated if
βv (s) − k(s) > p ⇐⇒ b(s) − (1 − β)v (s) > p
β≤1
12 / 37
What’s Going On?
Inattention or symptom salience?
I
An inattentive agent underweighs the benefits of filling an
antidiabetic prescription since diabetes is “silent” much of the time
(Rubin 2005, Osterberg and Blaschke 2005)
I
Should get treated if
b(s) = b(v + n + o) > p
where v represents salient symptoms, n opaque or non-painful
symptoms, and o other symptoms
I
Instead gets treated if
b(αv + βn + o) > p ⇐⇒
b(s) + [b(αv + βn + o) − b(v + n + o)] > p
α ≥ 1, β ≤ 1
13 / 37
What’s Going On?
False beliefs?
I
Once symptoms have abated, an agent with false beliefs may believe
that continuing a TB drug regimin is no longer necessary (Pauly and
Blavin 2008)
I
Should get treated if
b(s) > p
I
Instead gets treated if
b̂(s) > p ⇐⇒ b(s) + (b̂(s) − b(s)) > p
14 / 37
Resolution
Observation: Agents with present-bias, inattention, and false beliefs all
make choices according to whether
b(s) + ε(s) > p
In these cases, there is a clear wedge between “decision” and “hedonic”
utility (Kahneman et al. 1997), given by ε(s)
I
Not true for all “behavioral factors”, e.g., anxiety (Koszegi 2003)
Call misbehavior resulting from ε 6= 0 behavioral hazard
I
suboptimal choices resulting from mistakes or behavioral biases
I
in contrast to privately optimal but socially suboptimal choices
resulting from misaligned incentives
15 / 37
Simple Insight
Simple Insight: We can generally draw out the implications of “behavioral
hazard” for welfare calculations and optimal co-pay formulas
I
We don’t need to separately consider present-bias, symptom salience,
and false beliefs to see how BH changes central insights of the
“standard” model
I
The feature of a behavioral bias that matters most is how it affects
who is marginal with respect to the copay
I
But, as we saw above, we can re-write ε in terms of primitives of
specific behavioral models
16 / 37
Further Details on the Basic Setup
Setup:
I
Individual has wealth y
I
Insurance costs premium P
I
When healthy, the individual has utility U(y − P)
I
With probability q, she falls sick with varying degrees of severity
s ∼ F (s)
I
Absent treatment, the sick individual receives utility U(y − P − s)
Treatment costs society c and the patient co-pay p; its benefit b(s)
depends on severity: b 0 (s) ∈ [0, 1]
I
I
I
To simplify certain statements, will assume in the talk that b(s) = s
With treatment, the sick individual receives utility
U(y − P − s + b(s) − p)
17 / 37
Choice to Receive Treatment
Without behavioral hazard: Choose to get treated if b(s) > p
With behavioral hazard: Choose to get treated if b(s) + ε(s) > p
I
Shouldn’t think of ε(s) as fixed, but as systematically varying across
diseases and treatments
I
I
I
drugs treating chronic conditions: ε < 0
antibiotics for children’s ear infections or treatment of back pain: ε > 0
To simplify formulas today, ignore heterogeneity in behavioral hazard
across people
I
I
Does not matter for what I’ll discuss
Paper considers more general case
With BH misutilization is not solely a consequence of health insurance
18 / 37
Re-Thinking The Welfare Impact of Co-pay Changes
What are some implications of BH for optimal co-pays?
Planner’s problem:
Demand
Pr(b(s)+ε(s)>p)
max W = E [U] subject to P =
p
z }| {
M(p)
·(c − p)
Raising the co-pay has two effects:
1. It reduces insurance value
- doesn’t matter whether there is behavioral hazard
2. It affects utilization
- interpretation of demand response depends on whether there is
behavioral hazard
19 / 37
Welfare Effects of Changing the Co-pay: No BH
Without BH: Differentiate W and normalize:
Demand Response
Sufficient Statistic
E [U 0 (C )|m=1]−E [U 0 (C )]
E [U 0 (C )]
z
}|
{
dW dW
/
= −M 0 (p)(c − p) −
|
dp dy
| {z }
Welfare Impact
z }| {
I · M(p)
{z
·M(p)
Insurance Value
}
FOC for optimal co-pay
c − pS
=
pS
I
η
|{z}
Demand Elasticity
I
More elastic demand implies higher co-pay
I
Insurance optimally partial: p S ∈ (0, c) if η > 0, I > 0
20 / 37
Optimal Copay: Behavioral Hazard
Taking BH into Account: Differentiate W and normalize:
Demand Response
Not Sufficient Statistic
z
}|
{
dW dW
/
≈ −M 0 (p)(c − p + ε) −I · M(p)
{z
}
|
dp dy
| {z }
Sign Could Become (-)
Welfare Impact
FOC
c − pB
I
ε
≈ − B
η p
pB
I
More elastic demand does not necessarily mean higher co-pay
I
E.g., the fact that elasticities for beta blockers and cold remedies are
similar does not necessarily imply similar co-pays
21 / 37
Re-thinking Optimal Co-pays (Continued)
I
c − pB
ε
≈ − B
B
η p
p
I
Optimal co-pays create incentives for more efficient treatment
decisions, not just insurance value: when I = 0, p B = c + ε(s(p B ))
I
I
I
optimal co-pays price “internalities”
health insurance can actually lead to more efficient utilization
It can be optimal to fully cover effective treatments, even if they are
ineffective for some insurees: can optimally have p B ≤ 0 even when
M 0 (0) < 0
22 / 37
Implication
Modal evidence for moral hazard has been the demand response
This can be very misleading
I
Being marginal does not necessarily imply indifference
Implications can even be the wrong sign!
More than an abstract concern
23 / 37
Example
Example: Choudhry et al. (NEJM, 2011)
I
I
Study impact of eliminating copays for recent heart attack victims
Randomly assigned patients discharged after heart attacks to a
control group with usual coverage
I
I
copayments in $12 to $20 range
Or a treatment group with no co-payments
I
For statins, beta blockers and ACE inhibitors
24 / 37
/,))*.'%"($G"*
3"2&.$E'0*$2#"("0."*
!"#$%&&&*
;7,$)*.'%"($G"*
A=5JbAT!7*
!"4$P-)'.M"(7*
!_\[]!
!^\^]!
14$E07*
![\8]!
A))*:*.)$77"7*
!_\^]!
+a9\99`*<'(*$))*.'6B$(&7'07*
*!:`]*
!:8]!
!37%!
!^`]!
Implication
Modal evidence for moral hazard has been the demand response
This can be very misleading
I
Being marginal does not necessarily imply indifference
Implications can even be the wrong sign!
More than an abstract concern
How can we tell?
25 / 37
Understanding the Marginal Internality
Use health responses
I
I
Define H(p) = E [m(p; s)b(s) − s] to equal the aggregate level of
health
Standard model: H 0 (p) = M 0 (p)p
I
I
Can infer the health response directly from the demand response and
the co-pay
With behavioral hazard:
−
I
H 0 (p)
ε
=
−1
p
pM 0 (p)
Can infer the degree of behavioral hazard from the return to the last
private dollar spent on treatment
I
Can only equate H 0 (p) = M 0 (p) · p when we are confident there is no
marginal behavioral hazard
26 / 37
Understanding the Marginal Internality
Use health responses
I
I
Define H(p) = E [m(p; s)b(s) − s] to equal the aggregate level of
health
Standard model: H 0 (p) = M 0 (p)p
I
I
Can infer the health response directly from the demand response and
the co-pay
With behavioral hazard:
−
I
ε
H 0 (p)
=
−1
p
pM 0 (p)
Can infer the degree of behavioral hazard from the return to the last
private dollar spent on treatment
I
Can only equate H 0 (p) = M 0 (p) · p when we are confident there is no
marginal behavioral hazard
26 / 37
Re-Thinking Optimal Co-pays
Re-Thinking Optimal Co-pays
I
Optimal co-pays also depend on marginal health value, unlike in
standard model
!
0 B H (p )
I
c − pB
≈ +
−1
η
pB
p B |M 0 (p B )|
I
Helps rationalize VBID (Chernew et al. 2007): lower cost-sharing for
treatments with greater health benefits
I
Fixing the demand response, co-pays should be lower when this
response translates into relatively worse health
27 / 37
3$e'(*%$7.,)$(*"%"047*f/$4$)*'(*0'0<$4$)*3Jg*,074$-)"*$0G&0$g*=I/g*74('M"h*
!"#$%&&&*
T$4"*B"(*`99*
B"(7'0*K"$(7*
/,))*
.'%"($G"*
;7,$)*
.'%"($G"*
``\9*
`8\d*
NO-6)#4*K8=6M8#
"`^]*
$-))#4*K8=6M8#
;6<6=.#=6>*#?@3A#B"CD#:EFG#?:EHIJ:E@@C#
'JK6)-8D#:E:L#
P*E#6+#%(OQ#
;7,$)*.'%"($G"*
/,))*.'%"($G"*
:9`9*
8d^_*
8:[`*
88i_*
`[_8*
`_j8*
`9ii*
`9`:*
[[8*
[8_*
:ji*
:^9*
`:`*
`:_*
The Pitfalls of Ignoring Behavioral Hazard
The pitfalls of ignoring behavioral hazard
Taking behavioral hazard into account can dramatically influence the
inferences we draw from data
Let’s compare the optimal co-pay under behavioral hazard, p B , to the
co-pay a “neo-classical” analyst who ignores behavioral hazard would think
is optimal
I.e., ignoring corners and multiplicity the neo-classical analyst believes p N
is optimal, where p N solves:
−M 0 (p) · (c − p) − I (p) · M(p) = 0
28 / 37
Numerical Example
Consider a numerical example, where we make the following assumptions:
I
Quadratic utility: U(C ) = αC − βC 2
I
Uniformly distributed disease severity: s ∼ U[0, s̄]
I
Specific values for income, etc.:
y = 2500, α = 7000, β = 1, q = .1, s̄ = 200
I
Coinsurance rates perfectly coincide with co-pay levels: cost c = 100
I
Consider the deviation between p B and p N as a function of ε(s) ≡ ε̃:
ε̃ ∈ {−99, −50, 0, 50, 99}
29 / 37
Numerical Illustration
ε̃ = −99
ε̃ = −50
ε̃ = 0
ε̃ = 50
ε̃ = 99
Neo-classical Co-Pay (p N )
99.90
95.25
90.92
87.13
0
Optimal Co-pay (p B )
-2.85
42.78
90.92
141.08
192.86
1. p B < p N if ε̃ < 0; p B > p N if ε̃ > 0
2. p B increasing in ε̃
3. p N instead decreasing in ε̃
4. Deviation between p B and p N can thus be huge
30 / 37
Important Point
Illustrates: When behavioral hazard is really positive or really negative,
situations where the neo-classical analyst believes co-pays should be low
are precisely instances where co-pays should be high and vice-versa!
Intuition: First take case of really positive behavioral hazard.
1. Neo-classical optimal co-pay: Almost everybody gets treated when
p=c
⇒ looks like there is approximately no benefit to controlling moral
hazard
⇒ low co-pay
2. Optimal co-pay: Many people who demand treatment at p = c are
inefficiently doing so
⇒ big benefit to raising the co-pay above cost
⇒ very high co-pay (provided people are not extremely risk averse)
31 / 37
Intuition Continued
Now take the case of really negative behavioral hazard.
1. Neo-classical optimal co-pay: Almost nobody gets treated at p = c
⇒ looks like huge benefit to controlling moral hazard
⇒ high co-pay
I
(appears optimal so long as people are not extremely risk averse)
2. Optimal co-pay: Even at a co-pay of zero, people at the margin of
getting treated have a benefit above cost
⇒ no benefit to controlling behavior by raising the co-pay above zero,
but there (may be) an insurance value cost
⇒ the co-pay should be at most zero.
32 / 37
Using Choudhry Data
If we assume moral hazard (don’t look at health outcomes)
I
Full coverage ⇒ $106 increase in spending (per patient)
I
Average patient share 25% ⇒ extra care consumed has monetized
health value of at most $.25 on the dollar, or $26.50 overall
I
Marginal (social) dollar has -$.75 net return
I
Eliminating copayments bad policy (abstracting from insurance value)
Taking behavioral hazard into account
I
Take a small part of the health impact: mortality reduction
I
.3 percentage point reduction ⇒ $3000 value using common value of
statistical life ($1 million of death averted)
I
Marginal (social) dollar has $27 net return
I
Eliminating copayments very good policy
33 / 37
Using Choudhry Data
If we assume moral hazard (don’t look at health outcomes)
I
Full coverage ⇒ $106 increase in spending (per patient)
I
Average patient share 25% ⇒ extra care consumed has monetized
health value of at most $.25 on the dollar, or $26.50 overall
I
Marginal (social) dollar has -$.75 net return
I
Eliminating copayments bad policy (abstracting from insurance value)
Taking behavioral hazard into account
I
Take a small part of the health impact: mortality reduction
I
.3 percentage point reduction ⇒ $3000 value using common value of
statistical life ($1 million of death averted)
I
Marginal (social) dollar has $27 net return
I
Eliminating copayments very good policy
33 / 37
Summarizing a Few Points
I
With behavioral hazard, health insurance can provide more than just
financial protection: it can lead to more efficient health delivery
I
I
Demand responses no longer form a sufficient statistic for setting
co-pays
I
I
Optimal insurance may be full or nothing
We derive a formula for the optimal-copay level that can be empirically
implemented based on demand and health responses
Situations where the neo-classical analyst believes co-pays should be
low can be precisely instances where co-pays should be high and
vice-versa
34 / 37
Mullainathan, Schwartzstein and Congdon (2012)
Broader insight: Significant progress can be made without relying on
specific psychological assumptions about why behavior may deviate from
the optimum
I
What matters for much of the analysis is the wedge between the
marginal private benefit and demand curves
Mullainathan, Schwartzstein and Congdon (2012) review how this plays
out in other policy problems, e.g.,
I
Taxing to finance a public good
I
Taxing to correct an externality
I
Taxing to provide social insurance
We also consider nudges
35 / 37
Welfare Impact of Policy Change
The analysis proceeds much like it did with health insurance because the
welfare impact of a marginal increase in the tax to finance a transfer can
typically be broken into the same two terms:
Impact of Changing Behavior + Impact of Transferring Resources
I
Commodity taxation - distorts behavior; benefits stem from increasing
revenue
I
Taxing to correct an externality - changing behavior is beneficial; need
not have other benefits
Again, behavioral hazard matters because it changes who is marginal
Impact of Changing Behavior = M 0 (t)[t + ME + |{z}
MI ]
=−ε
36 / 37
More Broadly
I
Behavioral public finance often seems messy
I
I
I
Many different biases
Lessons seem context specific
However, there are some common features across biases and policy
contexts
I
I
There is a wedge between marginal private value and demand
Nudges influence demand (next talk)
I
By building a framework based on these features, the goal is to
highlight broader lessons
I
Behavioral public finance is not as messy as it seems
37 / 37