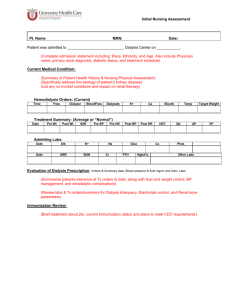
PROJECT STAFF
advertisement

PROJECT STAFF Paul Shekelle, MD, PhD Task Order Director Erin G. Stone, MD Principle Investigator Steven Kania, MD Investigator Scott Weingarten, MD, MPH Investigator Margie Snape, MLS Research Librarian Michael Hirt, MD screening/abstraction Tommy Tomizawa, MD Gregory Dorn, MD Luca De Simone, MD Article Acknowledgements: We would like to thank Gunter Rieg, M.D. for his help in translation of the German studies, and Irma Porras, Vanessa Walker and Shannon Rhodes for secretarial assistance. CONTENTS EXECUTIVE SUMMARY . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 1 INTRODUCTION . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9 METHODS ................................................................................................... 1 1 CLINICAL QUESTIONS ...................................................................................................................... 11 LITERATURE REVIEW....................................................................................................................... 14 Inclusion and Exclusion Criteria ..........................................................................................................................................................1 5 Article Selection and Abstraction ........................................................................................................................................................1 5 Critical Appraisal Method for Prognostic Articles .........................................................................................................................1 6 Critical Appraisal Method for Diagnostic Articles .........................................................................................................................1 7 Critical Appraisal Method for Treatment Articles ............................................................................................................................1 8 Evidence Synthesis...................................................................................................................................................................................1 9 RESULTS .................................................................................................... 2 0 DISTRIBUTION OF EVIDENCE.............................................................................................................. 20 FIGURE 1. ARTICLE SELECTION PROCESS ............................................................................................. 21 Question 1: Which measure of nutritional status best predicts patient morbidity/ mortality in chronic dialysis patients?...............................................................................................................................................................2 2 Question 2: Which measure is the best diagnostic test for protein/ calorie nutritional status in chronic dialysis patients?...............................................................................................................................................................2 2 Question 3: What is the effect of acid/ base status on nutritional measures in chronic dialysis patients? .....................2 3 Question 4: Which levels of intake of protein and calories in chronic dialysis patients produce the lowest morbidity/ mortality (also optimal changes in nutritional parameters and best nitrogen balance)?...............................................................................................................................................................................2 6 Question 5: Which levels of intake of protein and calories in predialysis patients produce the lowest morbidity at the initiation of dialysis?........................................................................................................................2 7 Question 6: How does resting energy expenditure in dialysis patients compare with resting energy expenditure in patients not on dialysis?.....................................................................................................................2 8 Question 7: Which nutritional interventions produce the lowest morbidity/ morality or the most optimum changes in nutritional status in dialysis patients?..................................................................................................2 8 Question 8: Is interdialytic weight gain a good measure for dietary compliance or a good prognostic indicator in dialysis patients? .......................................................................................................................................2 9 Questions 9-12: Carnitine Supplementation.....................................................................................................................................2 9 Pediatrics Question 1: Which measure of nutritional status best predicts patient morbidity/ mortality (and growth rate in children) in chronic dialysis patients?............................................................................................3 3 Pediatrics Question 2: Which measure is the best diagnostic test for protein/ calorie nutritional status in chronic dialysis patients? ...............................................................................................................................................3 4 Pediatrics Question 3: What is the effect of acid/ base status on nutritional measures in chronic dialysis patients? ...............................................................................................................................................................................3 4 Pediatrics Question 4 and Question 5: Which levels of intake of protein and calories in chronic dialysis produce the lowest morbidity/ mortality? Which levels of intake of protein and calories in predialysis patients produce the lowest morbidity at the initiation of dialysis? ...........................................3 4 Pediatrics Question 6: How does resting energy expenditure in dialysis patients compare with resting energy expenditure in patients not on dialysis?.......................................................................................................3 5 Pediatrics Question 7: Which nutritional interventions produce the lowest morbidity/ mortality (and best growth rate in children) or the most optimum changes in nutritional status in dialysis patients? ...............................................................................................................................................................................3 5 Pediatrics Question 8: Is interdialytic weight gain a good measure for dietary compliance or a good prognostic indicator in dialysis patients? .................................................................................................................3 6 Pediatrics Question 13: Does growth hormone therapy improve morbidity/ mortality in pediatric chronic dialysis patients?...............................................................................................................................................................3 6 Pediatric Question 14: Does vitamin or mineral supplementation improve morbidity/ mortality in pediatric dialysis patients? (Calcium, magnesium, and vitamin D were not examined.) ..................................................3 7 SUMMARY .................................................................................................. 3 8 IN-TEXT REFERENCES . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 4 2 APPENDIXES . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 4 5 APPENDIX A: GLOSSARY................................................................................................................... 46 APPENDIX B: TECHNICAL EXPERTS - NKF DOQI NUTRITION IN DIALYSIS WORKGROUP ............................. 56 APPENDIX C: SEARCH STRATEGIES..................................................................................................... 58 Strategies for Questions 1-8 ...................................................................................................................................................................5 8 Search strategy for Questions 9-12.......................................................................................................................................................6 1 Search strategy for Question 13 , 14 and IGF (Pediatric Question 1) ........................................................................................6 2 i APPENDIX D: BIBLIOGRAPHY OF ACCEPTED ARTICLES ............................................................................ 63 References for Questions 1-12 - Adults...............................................................................................................................................6 3 References for Pediatric Sections...........................................................................................................................................................8 5 APPENDIX E: ABSTRACTION FORMS .................................................................................................... 93 NKF Prognostic Article Abstract Form ..............................................................................................................................................9 3 NKF Diagnostic Article Abstract Form ..............................................................................................................................................9 5 NKF Treatment Article Abstract Form .................................................................................................................................................9 7 APPENDIX F: TREATMENT ARTICLE QUALITY SCORE ALGORITHM...........................................................100 APPENDIX G: EVIDENCE TABLES.......................................................................................................102 ii EXECUTIVE SUMMARY INTRODUCTION Chronic dialysis is a common and expensive therapy for end stage renal disease. The number of patients prescribed this therapy is increasing with time. Using a variety of measures, a number of articles studying patients in both the US and other countries have reported the prevalence of malnutrition in this population to range from 25% to 73%. Malnutrition increases morbidity, mortality, and cost, and produces growth retardation in children. It is therefore important to determine methods to adequately assess the nutritional status of dialysis patients, to prevent malnutrition from occurring in these patients, and to adequately treat malnutrition once it is discovered. This evidence report addresses nutritional prognostic, diagnostic, and treatment issues in dialysis patients. M ETHODS We performed a systematic review to assemble and critically appraise relevant studies answering the clinical questions of interest. The technical experts for this Evidence Report are the members of the National Kidney Foundation (NKF) Dialysis Outcomes Quality Initiative (DOQI) Workgroups. With their input we formulated the following key clinical questions: Question 1. Which measure of nutritional status best predicts patient morbidity/ mortality (and growth rate in children) in chronic dialysis patients? Question 2. Which measure is the best diagnostic test for protein/ calorie nutritional status in chronic dialysis patients? 1 Question 3. What is the effect of acid/ base status on nutritional measures in chronic dialysis patients? Question 4. Which levels of intake of protein and calories in chronic dialysis produce the lowest morbidity/ mortality? Question 5. Which levels of intake of protein and calories in predialysis patients produce the lowest morbidity at the initiation of dialysis? Question 6. How does resting energy expenditure in dialysis patients compare with resting energy expenditure in patients not on dialysis? Question 7. Which nutritional interventions produce the lowest morbidity/ mortality (and best growth in children) or the most optimum changes in nutritional status in dialysis patients? Question 8. Is interdialytic weight gain a good measure for dietary compliance or a good prognostic indicator in dialysis patients? Question 9. Which measure of L-carnitine nutritional status best predicts patient morbidity/ mortality in chronic adult dialysis patients? Question 10. What are the best measures of L-carnitine nutritional status in chronic adult dialysis patients? Question 11. Does L-carnitine supplementation in chronic adult dialysis patients improve morbidity/ mortality? 2 Question 12. What are the toxic/ adverse effects of L-carnitine in adult chronic dialysis patients? Question 13. Does growth hormone therapy improve morbidity/ mortality in pediatric chronic dialysis patients? Question 14. Does vitamin or mineral supplementation improve morbidity/ mortality in pediatric dialysis patients? (Calcium, magnesium, and vitamin D were not examined.) A structured database search of two computerized bibliographic databases (MEDLINE, EMBASE) was performed in collaboration with a librarian experienced in searching computerized bibliographic databases and performing “evidence-based” systematic reviews. We also hand-search the Journal of Renal Nutrition since it was not indexed in these bibliographic databases. Additionally, referrals from the technical experts were reviewed. For Questions 9-12 an extensive carnitine bibliography was provided by Sigma Tau, Rome, Italy. Articles addressing the clinical questions were included in the selection steps detailed below. Animal studies, letters, editorials, reviews, case reports, and abstracts of meeting proceedings were excluded. After loading articles from MEDLINE, EMBASE, technical expert referrals, and the Sigma Tau bibliography into an electronic database, one reviewer performed an initial title review and selection. Two independent reviewers then selected articles based on article abstracts. Selection disagreements were resolved by consensus. English language articles selected at the abstract stage were then reviewed and selected by two independent reviewers. Information was abstracted from the articles by one abstracter and verified by a second. Articles that were rejected at this stage were coded using the following codes: 3 R1: Editorial, letter, review, case report, article published as abstracts R2: Article doesn’t answer clinical question of interest R3: Article doesn’t have study design of interest R4: Pediatric Article (rejected from the adult questions only) R5: Not human R6: Adult article (rejected from the pediatric questions only) English titles, and English abstracts when available, of selected foreign language articles were sent to all technical experts for review. A foreign language article was abstracted by someone fluent with that particular language if any technical expert indicated an article would potentially contribute to the evidence in a particular area. Because of the volume of accepted articles, further selections were made based on article study design. For prognostic articles, only those with prospective cohort or historical prospective cohort designs were included for further analysis. For diagnostic articles, only those where the authors compared a test with what they considered to be a gold standard for nutritional status were included for further analysis. For treatment articles, only those with a prospective design with concurrent controls were included for further analysis. (These restrictions did not apply to the carnitine sections or to the pediatric sections.) After article abstraction, evidence tables were produced from a subset of abstracted data elements and presented to the technical experts (also called workgroups) during meetings in Los Angeles in August 1998 and January 1999. The technical experts accepted or rejected articles based on the study methods, and adequacy in addressing the clinical questions. 4 R ESULTS The initial literature search identified 19,272 MEDLINE and 4,943 EMBASE titles. In addition, the technical experts referred 134 articles for review, and the Sigma Tau bibliography contained 138 references not found by other means. This review yielded 24,487 titles. Of these, 22,362 titles were rejected, leaving 2,125 titles. Abstracts of these articles were reviewed and 1,021 were rejected, thus leaving 1,104 articles. One hundred and seventy of these were foreign language articles whose titles and abstracts were sent to the technical experts. Of these, 102 were not selected for further evaluation, 2 were selected but could not be translated, and 66 were further evaluated. Of the 934 English language articles, 29 were unobtainable, leaving 971 English and foreign language articles to be abstracted Of these, 640 were rejected (R1-R6) and the remaining 331 were sent to the technical experts along with evidence tables for these articles created from the abstraction forms. The technical experts rejected 81 articles either because the article did not adequately address a clinical question of interest or because the article was of poor study design, thus leaving 250 accepted articles. Question 1: Which measure of nutritional status best predicts patientmorbidity/ mortality in chronic dialysis patients? We identified 46 studies which assessed the value of nutritional measures as predictors of morbidity/ mortality in patients on chronic dialysis. Many articles studied albumin and anthropometrics as prognostic factors, with other factors being less well studied. There is consistent evidence that serum albumin is related to mortality in dialysis patients. Other prognostic factors have been studied less frequently and/ or have had less consistent results. 5 Question 2: Which measure is the best diagnostic test for protein/ calorie nutritional status in chronic dialysis patients? Our literature search identified 29 studies pertaining to diagnostic tests for protein/ calorie nutritional status. A consistent gold standard for the diagnosis of nutritional status in dialysis patients was absent. Given this limitation, some support was found for the validity of serum albumin, pre-albumin, creatinine, protein catabolic rate (PCR), protein equivalent of total nitrogen appearance (PNA), the subjective global nutritional assessment (SGA), anthropometric measurements, the dual x-ray photon absorptiometry (DEXA), and transferrin. Question 3: What is the effect of acid/ base status on nutritional measures in chronic dialysis patients? Nine studies dealing with acid/ base status and nutrition in general supported the hypothesis that correcting acidosis improved nutritional status. Question 4: Which levels of intake of protein and calories in chronic dialysis patients produce the lowest morbidity/ mortality (also optimal changes in nutritional parameters and best nitrogen balance) The 16 articles identified contained primarily nitrogen balance articles and in general indicate that a dietary protein intake of 1.2g per kilogram per day is necessary to avoid nitrogen imbalance. Question 5: Which levels of intake of protein and calories in predialysis patients produce the lowest morbidity at the initiation of dialysis? Two meta-analyses assessing the effect of a low protein diet on predialysis patients both reached the conclusion that such diets have a significant mortality benefit. 6 Question 6: How does resting energy expenditure in dialysis patients compare with resting energy expenditure in patients not on dialysis? The gold standard for the five articles selected was indirect calorimetry and the majority of evidence indicates there is little difference in resting energy expenditure between dialysis patients and patients not on dialysis. Question 7: Which nutritional interventions produce the lowest morbidity/ morality or the most optimum changes in nutritional status in dialysis patients? These 18 articles contained studies of both enteral and parenteral supplementation as well as counseling. Results were inconsistent and no conclusion could be drawn. Question 8: Is interdialytic weight gain a good measure for dietary compliance or a good prognostic indicator in dialysis patients? The 12 identified articles did not support a clinically important correlation between interdialytic weight gain and dietary compliance or patient outcomes. Questions 9-12: Carnitine Supplementation We identified 33 studies where serum triglycerides were the outcome, five studies where cardiac function and arrhythmia were the outcome, six studies where symptoms of malaise asthenia, muscle cramps, weakness and fatigue were the outcome, five studies where exercise capacity and muscle strength were the outcome, and 10 studies where anemia was the outcome. This evidence on potential beneficial effects of carnitine is moderately extensive but of uneven quality. Sufficient evidence to prove a benefit for carnitine was not found for any outcome. The outcome with the best evidence of benefit was anemia. Several clinical trials reported statistically significant improvements in hematocrit or decreases in erythropoietin requirements. However, in none of these studies was the effect on anemia the primary outcome, so these results must be viewed with caution as results of secondary 7 outcomes usually are known to overestimate efficacy. There is no evidence that administration of carnitine in standard doses is associated with side effects. Pediatrics Questions 1-14: The evidence specific to pediatric patients was very sparce, with the exception of growth hormone. One placebo-controlled double blind cross over trial of growth hormone in prepubertal children with chromic renal failure provided strong evidence that growth hormone treatment could greatly improve height velocity in such children. Other studies reported that the improvement in linear growth in patients treated with dialysis is not as great as that observed in patients with stable chronic renal failure and that the gain in height across subsequent years is diminished. C ONCLUSION A large number of studies have been published in the medical literature on nutrition in dialysis patients. Through the series of selection steps detailed above, approximately 1 in 20 of the 24,487 articles obtained from various sources was selected for data abstraction. Of these, approximately 3% were unavailable, and two thirds were further rejected once the article was read and evaluated. Of the remaining one third (331 articles), the technical experts rejected approximately 1 in 4, leaving 250 accepted articles. Of these 250 accepted articles, pediatric nephrology patients were the subjects in approximately one fourth, with adult patients being the subjects in the remaining three fourths. There is sufficient evidence of validity for some diagnostic, prognostic, and treatment procedures. This report will provide the evidence for the development of clinical practice guidelines by the Nation Kidney Foundation Dialysis Outcomes Quality Initiative. 8 INTRODUCTION Of the nearly 200,000 patients in the US with end stage renal disease (ESRD) in 1990, 70% were receiving either hemodialysis or peritoneal dialysis as renal replacement therapy (1). The estimated cost of care for all patients with ESRD in 1990 was US$7.26 billion. It is estimated that nearly 300,000 patients in the US will have ESRD in the year 2000, with an attendant rise in the costs of care. The number and cost of patients with ESRD worldwide are even greater. The prevalence of malnutrition in dialysis patients has been studied in various countries using various methods. Anthropometric measures and albumin were significantly below normal in 37% to 70% of hemodialysis patients in Thailand (2). Eighty-two percent of continuous ambulatory peritoneal dialysis (CAPD) patients in Mexico were found to be malnourished (3). Using subjective global assessment, serum chemistries, and anthropometric measures, 51% of elderly Italian dialysis patients were found to be malnourished (4). In Pakistan, 34% to 70% of hemodialysis patients were found to be malnourished when assessed by albumin levels and various anthropometric measures (5). Malnutrition in Spanish hemodialysis patients was found to range from 40% to 73% (6; 7), and was found to be 54% in Denmark (8). A number of studies in the US have found the prevalence of malnutrition to range from 25% to 70% using a variety of assessment tools including anthropometric measures, blood tests, and composite and global assessments (9-12). One US study, however, found many patients to have anthropometric measurements not dissimilar to those in the general population (13). 9 A number of causes have been proposed for malnutrition in dialysis patients. These include the catabolic state of dialysis, the loss of nutrients during the dialysis procedure, the predialysis protein-restricted diet frequently prescribed, abnormal metabolism of nutrients, and dialysisinduced anorexia (14). Malnutrition increases morbidity, mortality, and cost, and produces growth retardation in children. Thus, it in incumbent on the nephrology community to determine methods to adequately assess the nutritional status of dialysis patients, to prevent malnutrition from occurring in these patients, and to adequately treat malnutrition once it is discovered. To these ends, the National Kidney Foundation has commissioned a systematic review of nutrition in chronic renal failure, the details of which are contained in this report. 10 METHODS We performed a systematic review that “involves the application of scientific strategies, in ways that limit bias, to the assembly, critical appraisal, and synthesis of all relevant studies that address a specific clinical question.” (15; 16) A glossary of terms related to systematic reviews is listed in Appendix A. C LINICAL Q U E S T I O N S With the guidance of the technical experts of the National Kidney Foundation (NKF) Dialysis Outcomes Quality Initiative (DOQI) Workgroup (Appendix B) we formulated the following clinical questions: Question 1. Which measure of nutritional status best predicts patient morbidity/ mortality (and growth rate in children) in chronic dialysis patients? The technical experts chose to review only the following measures: • Pre-albumin • Subjective Global Assessment • Albumin • Dietary history • Anthropometric measures (height, weight, • Cholesterol skinfold thickness, body mass index • Transferrin (BMI), percent of normal body weight, • PCR/PNA percent of ideal body weight, post-dialysis • Prognostic nutrition index body weight) • Acute phase protein (C-reactive protein) • Bio-electric impedence • Alpha-1 glycoprotein • Urea nitrogen appearance • DEXA • Pre-dialysis creatinine • IGF in pediatric patients • More than 1 of the above measures 11 Question 2. Which measure is the best diagnostic test for protein/ calorie nutritional status in chronic dialysis patients? The technical experts chose to review only the following measures: • Pre-albumin • Subjective Global Assessment • Albumin • Dietary history • Anthropometric measures (height, weight, • Cholesterol skinfold thickness, body mass index • Transferrin (BMI), percent of normal body weight, • PCR/PNA percent of ideal body weight, post-dialysis • Prognostic nutrition index body weight) • Acute phase protein (C-reactive protein) • Bio-electric impedence • Alpha-1 glycoprotein • Urea nitrogen appearance • DEXA • Pre-dialysis creatinine • IGF in pediatric patients • More than 1 of the above measures Question 3. What is the effect of acid/ base status on nutritional measures in chronic dialysis patients? Question 4. Which levels of intake of protein and calories in chronic dialysis produce the lowest morbidity/mortality? The technical experts chose to also review the following: • The most optimum changes in nutritional status using measures from question #1 above? • Best nitrogen balance • Best growth in children Question 5. Which levels of intake of protein and calories in predialysis patients produce the lowest morbidity at the initiation of dialysis? (Though this question was addressed by both adult and pediatric groups, the pediatric group chose to use these articles to inform Question 4, while the adult group chose to write a separate guideline for this section.) 12 Question 6. How does resting energy expenditure in dialysis patients compare with resting energy expenditure in patients not on dialysis? Question 7. Which nutritional interventions produce the lowest morbidity/mortality (and best growth in children) or the most optimum changes in nutritional status in dialysis patients? The technical experts chose to review the following measures from Question 1 above. • Intradialytic supplementation • Intra-PD supplementation • Tube feeding • Oral supplements • Nutrition counseling • Acid/base correction • Intravenous supplementation Question 8. Is interdialytic weight gain a good measure for dietary compliance or a good prognostic indicator in dialysis patients? Question 9. Which measure of carnitine nutritional status best predicts patient morbidity/ mortality in chronic adult dialysis patients? The technical experts chose to review only the following measures: • Plasma carnitine levels • Plasma acylcarnitine levels • Muscle carnitine levels Question 10. What are the best measures of carnitine nutritional status in chronic adult dialysis patients? (Question 11 was addressed first, with Question 10 being addressed if carnitine supplementation at any carnitine/acylcarnitine level was felt to change outcomes.) The technical experts chose to review only the following measures: • Plasma carnitine levels • Plasma acylcarnitine levels 13 • Muscle carnitine levels Question 11. Does carnitine supplementation in chronic adult dialysis patients improve morbidity/ mortality? The technical experts chose to also review the following:: • Hypertriglyceridemia • Exercise tolerance • Anemia • Left ventricular dysfunction • Intradialytic dysrythmias • Quality of life Question 12. What are the toxic/ adverse effects of L-carnitine in adult chronic dialysis patients? Question 13. Does growth hormone therapy improve morbidity/ mortality in pediatric chronic dialysis patients? Question 14. Does vitamin or mineral supplementation improve morbidity/ mortality in pediatric chronic dialysis patients? (calcium, magnesium, and vitamin D were not examined.) L ITERATURE R E V I E W A structured database search of 2 computerized bibliographic databases (MEDLINE, EMBASE) was performed with the following specifications: • Language: English and non-English articles • Dates: 1966 through 1997 • Subjects: Human. • Article types: letters, editorials, reviews, case reports, and abstracts of meeting proceedings were excluded. The search was performed in collaboration with a librarian experienced in searching computerized bibliographic databases and performing “evidence-based” systematic reviews. The MEDLINE search strategies are detailed in Appendix C. The EMBASE strategies were similar. 14 We also hand-search the Journal of Renal Nutrition since it was not indexed in the bibliographic databases listed above. Additionally, referrals from technical experts were reviewed. For Questions 9-12, an extensive carnitine bibliography was provided by Sigma Tau, Rome, Italy. Inclusion and Exclusion Criteria Articles meeting the specifications listed above, and addressing at least 1 of the clinical questions detailed above were included. All others were excluded. Article Selection and Abstraction After loading articles from MEDLINE, EMBASE, technical expert referrals and the Sigma Tau bibliography into an electronic database, one reviewer performed an initial title review of these articles, applying the above inclusion and exclusion criteria. Abstracts were requested for all articles accepted at the title screening phase. Two independent reviewers then screened the abstracts and applied the above inclusion and exclusion criteria. Selection disagreements were resolved by consensus. English language articles accepted at the abstract screening phase were obtained and divided into the appropriate sections (see above) based on the clinical question the article addressed. These articles were then reviewed by two independent reviewers. Information was abstracted from the articles (see below) by one abstracter and verified by a second. Disagreements were resolved by consensus. Articles rejected at the abstraction stage were coded using the following: R1: Editorial, letter, review, case report, article published as abstracts R2: Article doesn’t answer clinical question of interest R3: Article doesn’t have study design of interest R4: Pediatric Article (rejected from the adult questions only) R5: Not human R6: Adult article (rejected from the pediatric questions only) 15 Article publication language was not limited to English in order to increase precision and reduce systematic errors (17), and because of the potential publication bias for positive studies in the English literature (18). After discussing the process of foreign language article selection with the technical experts, we decided to send the English titles, and English abstracts when available, to all technical experts for review. A foreign language article was abstracted by someone fluent with that particular language if any technical expert indicated that an article would possibly contribute to the evidence in a particular area. Because of the volume of accepted articles, selections were further made based on article study design. For prognostic articles, only those with prospective cohort or historical prospective cohort designs were included for further analysis. For diagnostic articles, only those where the authors compared a test with what they considered to be a gold standard for nutritional status were included for further analysis. For treatment articles, only those with a prospective design with concurrent controls were included for further analysis. (These restrictions did not apply to the carnitine sections or to the pediatric sections.) After article abstraction (see below), evidence tables were produced from a subset of abstracted data elements and presented to the technical experts during meetings in Los Angeles in August, 1998 (adult technical experts), January, 1999 (pediatric technical experts), and during a series of subsequent conference calls. The technical experts accepted or rejected articles based on the study methods and adequacy in addressing the clinical questions. The article selection process is detailed in Appendix D. The final selected articles are listed in Appendix E. Critical Appraisal Method for Prognostic Articles For each prognostic article (Questions 1, 3, 4, 5, and 8), we abstracted data to answer the following questions (19): 16 • What was the type of study? • What were the three most frequently occurring co-morbid conditions? • Was there a representative and well-defined sample of patients at a similar point in the course of disease? • What was the follow-up time period? • Were the outcome criteria objective and application of them unbiased? • Was adjustment made for important known prognostic factors? • What were the results? In addition, we abstracted a number of data elements that addressed study population and dialysis characteristics that might have affected the study results: • Number of patients at start of study • Years on dialysis • Age of patients • Type of dialysis • Dialysate • Membrane and whether it was reused • Dialysis schedule • For HD, type of vascular access • Economic status • Race • Residual renal function A copy of the article abstraction form is in Appendix F. Critical Appraisal Method for Diagnostic Articles For each diagnostic article (Questions 2 and 6), we abstracted data to answer the following questions (20; 21): • What was the type of study? • What were the three most frequently occurring co-morbid conditions? 17 • Was there an independent blind comparison with a reference (gold) standard? • Did results of the test being studied influence the decision to perform the reference standard? • Was the spectrum of patients in the study similar to the spectrum seen in dialysis centers? • Was the test methodology described well enough to be reproducible? • What were the results? In addition, we abstracted a number of data elements that addressed study population and dialysis characteristics that might have affected the study results. These were the same as for the prognosis sections listed above. A copy of the article abstraction form is in Appendix F Critical Appraisal Method for Treatment Articles For each treatment article (Questions 7, 13, and 14), we abstracted data to answer the following questions (22; 23): • What was the type of study? • What were the three most frequently occurring co-morbid conditions? • What were the Jadad quality scores?: • Randomization score ? • Double blind score ? • All patients accounted for score ? • Were all patients analyzed in the treatment group to which assigned? • Were the treatment groups similar at baseline? • Were the treatment groups treated equally except for the studied intervention? • What were the results? 18 In addition, we abstracted a number of data elements that addressed study population and dialysis characteristics that might have affected the study results. These are the same as for the prognosis sections listed above. The Jadad quality scores have been empirically shown to distinguish the effect size between reports of clinical trials. It assesses clinical trials in three domains: randomization, blinding, and withdrawals and dropouts. Scores range from 0-5 with higher scores indicating better quality. (24-28). The algorithm for the Jadad quality scores is shown in Appendix G. A copy of the article abstraction form is in Appendix F. Evidence Synthesis Due to sparseness of data and clinical heterogeneity among studies, we did not perform metaanalysis. Therefore, our synthesis of the evidence is qualitative. 19 RESULTS D ISTRIBUTION OF EVIDENCE The initial literature search identified 19,272 MEDLINE and 4,943 EMBASE titles. In addition, the technical experts referred 134 articles for review, and the Sigma Tau bibliography contained 138 references not found by other means. This review yielded 24,487 titles. Of these, 22,362 titles were rejected as not meeting the inclusion criteria, leaving 2,125 titles. Of these 1,021 were rejected at abstract screening as not meeting the inclusion criteria, thus leaving 1,104 articles. One hundred and seventy of these were foreign language articles whose titles and abstracts were sent to the technical experts. Of these, 102 were not selected for further evaluation, 2 were selected but could not be translated, and 66 were further evaluated. Of the 934 English language articles, 29 were unobtainable, leaving 971 English and foreign language articles to be abstracted. Of these, 640 were rejected (R1-R6) and the remaining 331 were sent to the technical experts along with evidence tables for these articles created from the abstraction forms. The technical experts rejected 81 articles thus leaving 250 accepted articles entering into this evidence report (figure 1). These articles are divided by questions and listed in Appendix E. Evidence tables for each question are detailed in Appendix H. 20 F IGURE 1. ARTICLE S ELECTION P R O C E S S Medline 19,272 Embase 4,943 Sigma Tau 138 Technical Expert referrals 134 Titles reviewed 24,487 Rejected at title stage 22,362 Selected titles, abstracts reviewed 2,125 Foreign language sent to technical experts 170 Rejected by technical experts 102 Unable to translate 2 Abstracte d 66 Rejected at abstract stage 1,021 Selected abstracts, articles ordered 1,104 Articles unavailable 29 Articles reviewed and abstracted 971 Rejected (R1-R6) 640 Rejected by technical experts 81 Selected articles reviewed by technical experts 331 Articles Accepted 250 21 Question 1: Which measure of nutritional status best predicts patient morbidity/ mortality in chronic dialysis patients? Our literature search identified 46 studies which assessed the value of nutritional measures as predictors of morbidity/mortality in patients on chronic dialysis. The great majority of these studies were prospective in nature and several had follow-up of five years or more of duration. They were evenly distributed between studies of patients on hemodialysis and peritoneal dialysis (18 studies of hemodialysis, 15 studies peritoneal dialysis, 12 studies of both). The best studied nutritional measure by far was serum albumin, which was reported in 35 studies. Most of these studies reported a statistically significant association between lower serum albumin and higher mortality, and this was true for patients on hemodialysis and peritoneal dialysis. Other nutritional prognostic factors were studied less frequently and had less consistent results. Details of studies are provided in Evidence Table 1. Question 2: Which measure is the best diagnostic test for protein/ calorie nutritional status in chronic dialysis patients? For this study question, we identified 29 studies of which 12 were prospective cohorts, 15 were cross-sectional assessments of diagnostic tests and nutritional status, and two had study designs that were unclear. Both hemodialysis and peritoneal dialysis patients were studied. A great variety of possible diagnostic tests were assessed and the reference standard for nutritional status also varied between studies. The results were not consistent across studies. However, some support was found for the validity of serum albumin, pre-albumin, creatinine, protein catabolic rate (PCR), protein equivalent of total nitrogen appearance (PNA), the subjective global nutritional assessment (SGA), anthropometric measurements, the dual x-ray photon absorptiometry (DEXA), and transferrin. 22 Full details of the individual studies are presented in Evidence Table 2. Question 3: What is the effect of acid/ base status on nutritional measures in chronic dialysis patients? Our literature search identified nine studies providing evidence relevant to this study question. Five of these studies were randomized clinical trials, two were prospective cohort studies, one was a clinical trial and one was a cross sectional analysis. In a prospective, randomized, double-blind, controlled trial, Otte and colleagues (1990) assessed the effects of a bicarbonate-based hemodialysis fluid compared with an acetatebased one in 16 patients on chronic hemodialysis. The study was cross-over in design so that each patient served as their own control. The period of time on each dialysate was 12 weeks. Blood chemistries were measured at the start and every 4 weeks throughout the study and the anthropometrics were measured at the start, at 12 weeks and at the end of the study. Dietary assessments by a dietician were performed periodically and adverse events were registered by the nursing staff during each dialysis. Other than a slight metabolic acidosis that was more pronounced in patients on acetate dialysis, no differences were found between groups in any of the outcomes measured. In a controlled trial (Graham, 1997), six patients on chronic hemodialysis were randomly assigned in a cross-over trial to standard dialysis or dialysis with 40 mmol of bicarbonate. Oral sodium bicarbonate was given in addition as needed to correct acidosis. Treatment resulted in an increase in the subject’s mean bicarbonate concentration from 18.5 mmol per liter to 24.8 mmol per liter and a subsequent increase in pH from 7.36 to 7.40. While no significant differences in anthroprometrics and body mass index were noted, radioactive leucine infusion tests demonstrated that leucine appearance from body protein decreased significantly with 23 correction of acidosis. The authors interpreted their results as indicating that correction of acidosis in hemodialysis is beneficial in terms of protein turn-over. In Stein and colleagues (1997), 200 consecutive patients who were newly placed on continuous ambulatory peritoneal dialysis were randomized in a single blinded fashion to receive a high or a low alkali-dialysis for one year. Other measures were taken to correct acidosis in the high alkali group. By one year of follow-up, persons randomized to the high-alkali group had a greater increase in body weight and mid-arm circumference than those in the low-alkali group; however, there was no difference in tricep skin fold thickness, serum albumin or dietary protein intake. The high-alkali group had fewer hospital admissions and spent less days in the hospital per year than the low-alkali group. A randomized clinical trial involved 46 patients who were stable on hemodialysis (Williams, 1997). The study was single blind double crossover trial with six months during each period. The study reported a significant improvement in triceps skin-fold thickness for patients in the high bicarbonate dialysate compared to those in the low bicarbonate dialysate. There were no statistically significant differences in other measures of nutrition including serum albumin concentration, mid-arm muscle circumference, and the normalized protein catabolic rate. In the randomized clinical trial by Brady and colleauge (1998), 36 patients who had been stable for at least three months on hemodialysis were divided into two groups, one of whom was dialyzed against a standard bicarbonate bath and the second group was dialyzed against a high-alkali bicarbonate bath. The subjects randomized to the high-alkali bicarbonate bath in addition received oral sodium bicarbonate as necessary. After 16 weeks of treatment, there were no statistically significant differences between groups in the nutritional parameters measured, which were serum albumin and the total lymphocyte count. 24 In a clinical trial (Harris, 1995) tested the effects of standard dialysate, a high bicarbonate dialysate, and “modeled” bicarbonate dialysate for 4 weeks each in 9 stable adult patients on hemodialysis. Modeled bicarbonate dialysate is a procedure where lower bicarbonate concentrations are used early in dialysis to reduce intracellular shifting of phosphate and higher bicarbonate is used during the last hour of dialysis to correct the acidosis, and has been postulated to more safely improve phosphate removal. The trial was a double blind crossover trial of the three treatments with a washout period between treatments. Oral bicarbonate therapy was given to both the high bicarbonate dialysate and the modeled bicarbonate dialysate groups in order to maintain plasma bicarbonate concentrations at 24-26 mmol per liter. The authors reported no difference among groups in any of the outcome measures including measures of phosphate clearance, plasma concentration of the urea, total calcium, blood pressure and symptoms. The two cohort studies (Dumler, 1996 and Kang, 1997), involve 79 and 106 peritoneal dialysis patients, respectively, and had follow-up periods of 21 months and two years. No effect of mild acidosis was found on measures of nutritional status in either study. In a cross-sectional analysis by Movilli and colleagues (1998), 81 patients on chronic hemodialysis had a variety of blood chemistry and nutritional measures assessed along with bicarbonate. The authors report a modest correlation between serum albumin level and serum bicarbonate levels and an inverse correlation between the normalized protein catabolic rate and increasing serum bicarbonate. In summary, most (but not all) studies support an association between correction of acidosis and better nutritional status. Further details can be found in Evidence Table 3. 25 Question 4: Which levels of intake of protein and calories in chronic dialysis patients produce the lowest morbidity/ mortality (also optimal changes in nutritional parameters and best nitrogen balance)? Our literature search identified 16 articles describing 15 studies that were all prospective cohorts. Both peritoneal dialysis and hemodialysis patients were studied. Most of the studies were small with only six studies having more than 20 patients. The length of follow-up was anywhere from a few days to several years. In general the studies showed that increasing dietary protein intake was associated with improvement in nutritional status measures, such as serum albumin, pre-albumin, cholesterol, and measures of nitrogen balance. Two studies (Kopple, 1969A & B; Archiaedo, 1990) also reported patient outcomes. In the study of Kopple and colleagues (1969), no difference was found between patients with a lower dietary protein intake and those with a higher dietary protein intake in terms of infection and cardiovascular accidents. Both serum albumin and body weight increased in the patients prescribed a high dietary protein intake. Uremic symptoms were more common in the patients with a higher dietary protein index. In Archiaedo and colleagues (1990), 136 patients were followed prospectively for one year. Patients were divided at baseline into five groups based on historical data, one of which was “inadequate protein intake.” Patients on an inadequate diet of less than 0.8 grams of protein per kilogram per day had a greater number of hospital days per year than patients receiving an adequate diet. In general the studies show that a dietary protein intake of 1.2 grams per kilogram per day is necessary to avoid nitrogen imbalance. The details of all studies are presented in Evidence Table 4. 26 Question 5: Which levels of intake of protein and calories in predialysis patients produce the lowest morbidity at the initiation of dialysis? Our literature search identified two meta-analyses dealing with low protein diet and patient outcomes, and additional studies including randomized clinical trials, prospective cohorts, and nitrogen balance studies. The first meta-analysis (Fouque, 1992), assessed six randomized clinical trials covering 890 patients with mild-to-severe renal failure who were followed for at least one year. The difference in protein intake between groups in a trial needed to be at least 0.2 grams of protein per kilogram per day in order to be included. The results of this data synthesis were that patients randomized to the low protein diet had an odds ratio of renal death of 0.54 relative to control with a 95% confidence interval of 0.37 to 0.79. The second meta-analysis (Pedrini, 1996), assessed the effect of low protein diets on patients with chronic renal disease stratified by whether the renal disease was diabetic or non-diabetic in etiology. In both strata, five randomized clinical trials were identified, comprising 1413 patients with non-diabetic renal disease and 108 patients with diabetic nephropathy. For patients with non-diabetic renal disease, the relative risk of renal failure or death was reported in the pooled analysis as 0.67 with a 95% confidence interval of 0.5 to 0.89. For patients with diabetic nephropathy, a low protein diet significantly slowed the increase in the urinary albumin level or the decline in the glomerular filtration rate with a relative risk of 0.56 and a 95% confidence interval of 0.40 to 0.77. Therefore, the results of both meta-analyses are consistent with the hypothesis that a low protein diet has a significant benefit in decreasing death for patients with both diabetic and nondiabetic renal disease. The results of the individual prospective cohorts and other studies were in general agreement with the meta-analysis. 27 The details of all studies presented in Evidence Table 5. Question 6: How does resting energy expenditure in dialysis patients compare with resting energy expenditure in patients not on dialysis? Our literature search identified five studies that assessed the energy expenditure of patients using indirect calorimetry. Studies ranged in size from eight to 25 patients. Four studies addressed patients on hemodialysis and one addressed patients on continuous ambulatory peritoneal dialysis. Three studies (Olevitch,1994; Schmeweiss, 1990; Montian,1986), reported no difference in energy expenditure either between patients on hemodialysis and control patients or between patients with chronic renal failure during periods of hemodialysis and the inter-dialytic period. One study (Ikizler, 1996), did report a difference in energy expenditure both between chronic hemodialysis patients and normal patients and in patients with chronic renal failure on hemodialysis compared to the period of time between dialysis. The one study of patients on peritoneal dialysis (Harty, 1995), reported no significant difference in resting energy parameters between patients on peritoneal dialysis and non-uremic control patients. In summary, the majority of evidence indicates there is little difference in resting energy expenditure between dialysis patients and patients not on dialysis. Full details of all articles are presented in Evidence Table 6. Question 7: Which nutritional interventions produce the lowest morbidity/ morality or the most optimum changes in nutritional status in dialysis patients? Our literature search identified 18 studies relevant to this question. Nine of these were randomized clinical trials and nine were controlled clinical trials or cohort studies. Of the nine 28 randomized clinical trials, only four had a Jadad score greater than or equal to three, a threshold which has previously been used to characterize good quality studies. The clinical trials studied small numbers of patients, generally between ten and thirty. A variety of oral supplements or changes in the dialysate were assessed. Most of the studies reported mixed results with some nutritional parameters improving and others showing no difference between groups. A clear conclusion from these studies cannot be drawn. The details of identified studies are reported in Evidence Table 7. Question 8: Is interdialytic weight gain a good measure for dietary compliance or a good prognostic indicator in dialysis patients? Our literature search identified 12 studies relevant to this study question. These were prospective or retrospective cohort studies, most of which had methodologic flaws. The results of the studies were mixed. Most studies reported no correlation or only a weak correlation between interdialytic weight gain and dietary compliance on patient outcome. The details of all studies are reported in Evidence Table 8. Questions 9-12: Carnitine Supplementation Question 9: Which measure of carnitine nutritional status best predicts patient morbidity/ mortality in chronic adult dialysis patients? Question 10: What are the best measures of carnitine nutritional status in chronic adult dialysis patients? Question 11: Does carnitine supplementation in chronic adult dialysis patients improve morbidity/ mortality? Question 12: What are the toxic/ adverse effects of L-carnitine in adult chronic dialysis patients? 29 Carnitine is known to be an essential co-factor in fatty acid and energy metabolism. It has also been shown that patients on maintenance dialysis usually have low serum free L-Carnitine concentrations and that skeletal muscle carnitine is sometimes decreased. Therefore there have been several studies investigating the effect that replacement of L-Carnitine has on a variety of patient outcomes, including serum triglycerides, cardiac functions and arrhythmia, malaise asthenia, muscle cramps, weakness and fatigue, exercise capacity, and anemia. Studies will be summarized within each of these outcomes. Elevated Serum Triglycerides Our literature search identified 33 studies relevant to the question of the effect of L-Carnitine administration on elevated serum triglycerides. Ten of these were randomized clinical trials of which eight had a Jadad score greater than or equal to three, a threshold that has been proposed as defining “good” quality. Of these, five studied intravenous administration or oral administration and one gave LCarnitine in the dialysite. Seven of these studies did not report any statistically significant affect of L-Carnitine administration on triglycerides while one did report statistical significance. Of the two other randomized clinical trials with Jadad scores less than three, one gave L-Carnitine orally and one gave it intravenously. Both studies reported a positive effect on triglycerides of L-Carnitine administration. The remaining non-randomized studies reported mixed results. Details of all studies are reported in Evidence Table 9. In summary, data from randomized clinical trials generally do not support a beneficial effect of L-Carnitine administration on elevated serum triglycerides in patients on maintenance dialysis although this conclusion was not reached by all studies. 30 Cardiac Function and Arrhythmia Our literature search identified five studies relevant to the question of the effect of L-Carnitine administration on cardiac function and arrhythmia. Three of these were randomized clinical trials of which 2 had a Jadad score greater than or equal to 3. Almost all of the studies measured the cardiac outcomes differently, including dialysis-associated arrhythmia, heart volume, ejection fraction, blood pressure and pulse rate, and measures of cardiac size. Of the 2 best quality randomized clinical trials, neither reported a significant change in cardiac outcomes. Details of all studies are summarized in Evidence Table 10. In summary, there is no evidence that L-Carnitine supplementation improves cardiac outcomes in patients on maintenance dialysis. Malaise Asthenia, Muscle Cramps, Weakness and Fatigue Our literature search identified six studies that provided evidence assessing the effect of LCarnitine administration on any of the symptoms malaise asthenia, muscle cramps, weakness and fatigue occurring, either interdialytically or in the post dialysis period. Four of these were randomized studies of which all scored greater than or equal to three on Jadad scale. Two studies reported significant effects of carnitine supplementation and two studies did not. Details of all studies are reported in Evidence Table 11. In summary, there is mixed evidence regarding the effect of L-Carnitine supplementation on improvement in symptoms of malaise asthenia, muscle cramps, weakness and fatigue in the interdialytic and post dialectic symptoms. 31 Exercise Capacity Our literature search identified five studies providing relevant to the question of L-Carnitine supplementation on exercise capacity or muscle strength. Of these, three were randomized clinical trials; all had a Jadad score greater than or equal to three. One study (Ahmad, 1990) reported an improvement in some measures of exercise capacity but not others. Another study (Albertazzi, 1980) reported a significant improvement in subjective muscle strength. The last study (Fagher, 1985) reported no significant difference between treatment and placebo arms and maximum strength or dynamic endurance. Details of all studies are summarized in Evidence Table 12. In summary, there is mixed evidence on the effect of L-Carnitine supplementation on improvement in exercise capacity on patients on maintenance dialysis. Anemia It has been proposed that Carnitine deficiency may reduce erythrocyte half-life by adversely influencing the integrity of the erythrocyte membrane. Our literature search identified ten studies providing information relevant to the question of whether L-Carnitine supplementation improves anemia or decreases erythropoietin requirements in patients on maintenance dialysis. Of these, five studies were randomized and four of these had a Jadad score greater than or equal to three. Of these four studies, three reported an improvement in hemoglobin or hematocrit and one did not. The details of all studies are summarized in Evidence Table 13. 32 In summary, there is evidence from several small randomized trials that L-Carnitine supplementation may improve anemia in patients on maintenance dialysis. In several of these studies, the effect of L-Carnitine supplementation on anemia was not a primary outcome of interest, but rather a secondary analysis and therefore these findings require confirmation in a randomized clinical trial where treatment of anemia is the primary outcome of interest. As our literature search did not identify convincing evidence of a benefit of carnitine supplementation, the technical experts decided there was no need to search for evidence regarding measurement and prognosis (Questions 9 and 10). Regarding possible side effects of carnitine, most studies made no mention of side effects. Four studies specifically stated no side effects occurred, one study stated there was “some euphoria” with carnitine administration, and one study reported one patient had nausea. In sum, there is no evidence that carnitine in standard doses is associated with serious side effects. Pediatrics Question 1: Which measure of nutritional status best predicts patient morbidity/ mortality (and growth rate in children) in chronic dialysis patients? Our literature search identified one study possibly relevant to this question. In this study (Chan, 1978) 19 pediatric patients between the ages of five and seventeen were followed prospectively for up to 59 months. All patients were on chronic hemodialysis. The patients were noted to be consuming far fewer calories and protein per day than recommended and growth was in general one to four standard deviations below the mean for age. In addition to this article there were three articles that dealt with insulin-like growth factor 1 (IGF-1). Two of these were prospective cohorts and one was a cross-sectional study. The cross-sectional study (Besbas, 1998), reported an association between lower IGF-1 levels and patients with malnutrition as defined by tricep skin fold thickness. However, neither of the 33 prospective cohort studies (Jasper, 1991; Hodson, 1992) identified a significant correlation between IGF -1 levels and growth rates or nutritional parameters. In summary, there is evidence that IGF -1 is not correlated with growth retardation in children with chronic renal failure. Details of the articles are listed in Evidence Table 14. Pediatrics Question 2: Which measure is the best diagnostic test for protein/ calorie nutritional status in chronic dialysis patients? Our literature search identified three studies relevant to this question. One study was a retrospective cohort study, and the other two were cross sectional studies. Patients on hemodialysis and on peritoneal dialysis were included. One study correlated skin fold thickness and bioelectrical impedance and reported a high correlation between these two (Stefanidis, 1996). A second study assessed the correlations between dual energy x-ray absorptiometry, lean body mass, and urinary excretion of creatinine and reported high correlations between all three (Cochat, 1996). A third study assessed the relation between insulin-like growth factor 1 (IGF-1) and protein energy malnutrition as defined by anthropometric measures in seventeen children with chronic renal failure on maintenance hemodialysis. Transferrin and serum albumin were not correlated with anthropometric measures while IGF-1 was significantly correlated (Besbas, 1998). Full details of studies are presented in Evidence Table 15. Pediatrics Question 3: What is the effect of acid/ base status on nutritional measures in chronic dialysis patients? We identified no studies pertaining to pediatrics and relevant to this question. Pediatrics Question 4 and Question 5: Which levels of intake of protein and calories in chronic dialysis produce the lowest morbidity/ mortality? Which 34 levels of intake of protein and calories in predialysis patients produce the lowest morbidity at the initiation of dialysis? Our literature search identified 24 studies relevant to these two questions. Sixteen of these were prospective cohort studies. Two were retrospective cohort studies and three were cross sectional studies. In addition there were three randomized trials of a low protein diet. Most studies assessed either dietary energy intake or dietary protein intake on growth or nutritional measures such as serum albumin, transferrin and cholesterol. Children on both hemodialysis and peritoneal dialysis were studied. Follow-up times ranged from one year to as much as ten years. Results were mixed and there was not a consistent correlation across studies between protein and energy intake and the outcomes measured. All three RCTs (Wingen, 1992; Kist, 1993; Uauy, 1994) of low protein diet concluded that the low protein diet was of minimal or no value. Full details of included studies are in Evidence Table 16. Pediatrics Question 6: How does resting energy expenditure in dialysis patients compare with resting energy expenditure in patients not on dialysis? We identified no studies pertaining to pediatrics and relevant to this question. Pediatrics Question 7: Which nutritional interventions produce the lowest morbidity/ mortality (and best growth rate in children) or the most optimum changes in nutritional status in dialysis patients? We identified 11 studies relevant to this question. Of these, one was a small randomized controlled trial that included seven patients on continuous ambulatory peritoneal dialysis and which assessed the effect of added amino acids in the dialysate on measures of plasma, glucose and amino-acids. The study reported that the amino-acid dialysate was less effective than traditional glucose-containing dialysates by the standard measures of filtration. However, the amino-acid dialysate had some significant metabolic advantages in the short-term. The 35 observational studies assessed a variety of protein and calorie supplements including aminoacid dialysates, nasal gastric tube feedings and oral supplements on a variety of outcomes including height, weight, serum albumin, hospital admissions, catheter infections and peritonitis. Results were mixed and findings were not consistent across studies. Full details of these studies can be found in Evidence Table 17. Pediatrics Question 8: Is interdialytic weight gain a good measure for dietary compliance or a good prognostic indicator in dialysis patients? We identified no studies pertaining to pediatrics and relevant to this question. Pediatrics Question 13: Does growth hormone therapy improve morbidity/ mortality in pediatric chronic dialysis patients? Our literature search identified 14 studies relevant to this study question. One of these studies (Hokken-Koelega, 1991) was a placebo-controlled double blind cross over trial of growth hormone treatment in pre-pubertal children with chronic renal failure. In this study, 16 children with chronic renal failure and severe growth retardation were given biosynthetic growth hormone at a dose of four international units per meter squared per day. Height velocity increased in every patient during the time in every patient during the time on growth hormone. Compared to placebo, the height velocity increase while on growth hormone was 0.9 centimeters greater per six months. This study proved that growth hormone treatment could greatly improve height velocity in children with chronic renal failure and growth retardation. The other studies identified in our literature search were observational and assessed either the effects of growth hormone on different types of patients or the effect of different levels of growth hormone. The general conclusion from these studies is that the improvement in linear growth in patients treated with dialysis is not as great as that observed in patients with stable chronic renal failure and that the gain in height across subsequent years is diminished. 36 The details of all studies can be found in Evidence Table 18. Pediatric Question 14: Does vitamin or mineral supplementation improve morbidity/ mortality in pediatric dialysis patients? (Calcium, magnesium, and vitamin D were not examined.) Our literature search identified three studies relevant to this question. Two studies (Kriley, 1991; Warady, 1994) were cross-sectional examinations of dietary intake and determinations of vitamin stores or concentrations. Both of these studies reported that the levels of many vitamins were normal or greater than normal in both children and infants receiving peritoneal dialysis and also on a vitamin supplementation regimen. The third study (Zlotkin, 1987) assessed the affect of zinc absorption from glucose and amino acid dialysis solutions in children on peritoneal dialysis. This study reported that there is a significant net absorption of zinc from glucose containing dialysis solutions and concluded that peritoneal dialysis does not contribute to zinc depletion. The details of all studies can be found in Evidence Table 19. 37 SUMMARY A large number of studies have been published in the medical literature on nutrition in dialysis patients. Through the series of selection steps detailed above, approximately 1 in 20 of the 24,487 titles obtained from various sources was selected for data abstraction. Of these, approximately 3% were unavailable, and two thirds were further rejected once the article was read and evaluated in greater detail. Of the remaining 331 articles, the technical experts rejected approximately 1 in 4, leaving 250 accepted articles. Of these 250 accepted articles, pediatric nephrology patients were the subjects in approximately one fourth, with adult patients being the subjects in the remaining three fourths. Of the questions pertaining to adults, Question 9 (which measure of carnitine nutritional status best predicts patient morbidity/mortality in chronic adult dialysis patients?) and Question 10 (what are the best measures of carnitine nutritional status in chronic adult dialysis patients?) were not addressed because there was insufficient evidence to conclude (for Question 11) that carnitine supplementation in chronic adult dialysis patients improves morbidity or mortality. Of the questions pertaining to pediatric patients, Question 3 (what is the effect of acid/base status on nutritional measures?), Question 6 (how does resting energy expenditure in dialysis patients compare with resting energy expenditure in patients not on dialysis?), and Question 8 (is interdialytic weight gain a good measure for dietary compliance or a good prognostic indicator in dialysis patients?) contained no accepted articles. 38 Question 1: Which measure of nutritional status best predicts patientmorbidity/ mortality in chronic dialysis patients? We identified 46 studies which assessed the value of nutritional measures as predictors of morbidity/ mortality in patients on chronic dialysis. Many articles studied albumin and anthropometrics as prognostic factors, with other factors being less well studied. There is consistent evidence that serum albumin is related to mortality in dialysis patients. Other prognostic factors have been studied less frequently and/ or have had less consistent results. Question 2: Which measure is the best diagnostic test for protein/ calorie nutritional status in chronic dialysis patients? Our literature search identified 29 studies pertaining to diagnostic tests for protein/ calorie nutritional status. A consistent gold standard for the diagnosis of nutritional status in dialysis patients was absent. Given this limitation, some support was found for the validity of serum albumin, pre-albumin, creatinine, protein catabolic rate (PCR), protein equivalent of total nitrogen appearance (PNA), the subjective global nutritional assessment (SGA), anthropometric measurements, the dual x-ray photon absorptiometry (DEXA), and transferrin. Question 3: What is the effect of acid/ base status on nutritional measures in chronic dialysis patients? Nine studies dealing with acid/ base status and nutrition in general supported the hypothesis that correcting acidosis improved nutritional status. Question 4: Which levels of intake of protein and calories in chronic dialysis patients produce the lowest morbidity/ mortality (also optimal changes in nutritional parameters and best nitrogen balance) The 16 articles identified contained primarily nitrogen balance articles and in general indicate that a dietary protein intake of 1.2g per kilogram per day is necessary to avoid nitrogen imbalance. 39 Question 5: Which levels of intake of protein and calories in predialysis patients produce the lowest morbidity at the initiation of dialysis? Two meta-analyses assessing the effect of a low protein diet on predialysis patients both reached the conclusion that such diets have a significant mortality benefit. Question 6: How does resting energy expenditure in dialysis patients compare with resting energy expenditure in patients not on dialysis? The gold standard for the five articles selected was indirect calorimetry and the majority of evidence indicates there is little difference in resting energy expenditure between dialysis patients and patients not on dialysis. Question 7: Which nutritional interventions produce the lowest morbidity/ morality or the most optimum changes in nutritional status in dialysis patients? These 18 articles contained studies of both enteral and parenteral supplementation as well as counseling. Results were inconsistent and no conclusion could be drawn. Question 8: Is interdialytic weight gain a good measure for dietary compliance or a good prognostic indicator in dialysis patients? The 12 identified articles did not support a clinically important correlation between interdialytic weight gain and dietary compliance or patient outcomes. Questions 9-12: Carnitine Supplementation We identified 33 studies where serum triglycerides were the outcome, five studies where cardiac function and arrhythmia were the outcome, six studies where symptoms of malaise asthenia, muscle cramps, weakness and fatigue were the outcome, five studies where exercise capacity and muscle strength were the outcome, and 10 studies where anemia was the outcome. This evidence on potential beneficial effects of carnitine is moderately extensive but of uneven quality. Sufficient evidence to prove a benefit for carnitine was not found for any outcome. The outcome with the best evidence of benefit was anemia. Several clinical trials reported statistically significant improvements in hematocrit or decreases in 40 erythropoietin requirements. However, in none of these studies was the effect on anemia the primary outcome, so these results must be viewed with caution as results of secondary outcomes usually are known to overestimate efficacy. There is no evidence that administration of carnitine in standard doses is associated with any serious side effects. Pediatrics Questions 1-14: The evidence specific to pediatric patients was very sparce, with the exception of growth hormone. One placebo-controlled double blind cross over trial of growth hormone in prepubertal children with chromic renal failure provided strong evidence that growth hormone treatment could greatly improve height velocity in such children. Other studies reported that the improvement in linear growth in patients treated with dialysis is not as great as that observed in patients with stable chronic renal failure and that the gain in height across subsequent years is diminished. 41 IN-TEXT REFERENCES 1. Morbidity and mortality of dialysis. NIH Consensus Statement Online. 11(22), 1-33. 1993. 11-1-1993. 2. Komindr S, Thirawitayakom J, Taechangam S, Puchaiwatananon O, Songchisomboon S, Domrongkitchaiporn S. Nutritional status in chronic hemodialysis patients. Biomedical & Environmental Sciences. 1996;9:256-62. 3. Espinosa A, Cueto-Manzano AM, Velazquez-Alva C, et al. Prevalence of malnutrition in Mexican CAPD diabetic and nondiabetic patients. Advances in Peritoneal Dialysis. 1996;12:302-6. 4. Cianciaruso B, Brunori G, Traverso G, et al. Nutritional status in the elderly patient with uraemia. Nephrology, Dialysis, Transplantation. 1995;10 Suppl 6:65-8. 5. Kumar H, Safdar N, Naqvi SA. Nutritional assessment of patients on maintenance haemodialysis. Journal of the Pakistan Medical Association. 1994;44:277-9. 6. Sanz A, Uson J, Alvarez R, Sancho MA, Jimenez A, Celaya S. The prevalence of malnutrition in hemodialysis. Nutricion Hospitalaria. 1992;7:173-7. 7. Gomez P, Martinez JA, Purroy A, Larralde J. The body composition of patients undergoing maintenance hemodialysis on an outpatient regimen. Nutricion Hospitalaria. 1989;4:48-50. 8. Marckmann P. Nutritional status of patients on hemodialysis and peritoneal dialysis. Clinical Nephrology. 1988;29:75-8. 9. Schoenfeld PY, Henry RR, Laird NM, Roxe DM. Assessment of nutritional status of the National Cooperative Dialysis Study population. Kidney International Supplement. 1983;S80-S88. 10. Thunberg BJ, Swamy AP, Cestero RV. Cross-sectional and longitudinal nutritional measurements in maintenance hemodialysis patients. American Journal of Clinical Nutrition. 1981;34:2005-12. 11. Wolfson M, Strong CJ, Minturn D, Gray DK, Kopple JD. Nutritional status and lymphocyte function in maintenance hemodialysis patients. American Journal of Clinical Nutrition. 1984;39:547-55. 12. Young GA, Kopple JD, Lindholm B, et al. Nutritional assessment of continuous ambulatory peritoneal dialysis patients: an international study. American Journal of Kidney Diseases. 1991;17:462-71. 42 13. Nelson EE, Hong CD, Pesce AL, Peterson DW, Singh S, Pollak VE. Anthropometric norms for the dialysis population. American Journal of Kidney Diseases. 1990;16:32-7. 14. Wolfson M. Causes, manifestations, and assessment of malnutrition in chronic renal failure. In: Kopple JD, Massry SG, eds. Nutritional management of renal disease. Baltimore, MD: Williams and Wilkins; 1997:245-56. 15. Cook DJ, Mulrow CD, Haynes RB. Systematic reviews: synthesis of best evidence for clinical decisions. Ann Intern.Med. 1997;126:376-80. 16. Jadad AR, McQuay HJ. Searching the literature. Be systematic in your searching [letter]. BMJ. 1993;307:66. 17. Moher D, Fortin P, Jadad AR, et al. Completeness of reporting of trials published in languages other than English: implications for conduct and reporting of systematic reviews. Lancet. 1996;347:363-6. 18. Egger M, Zellweger-Zahner T, Schneider M, Junker C, Lengeler C, Antes G. Language bias in randomised controlled trials published in English and German. Lancet. 1997;350:326-9. 19. Laupacis A, Wells G, Richardson WS, Tugwell P. Users' guides to the medical literature. V. How to use an article about prognosis. Evidence-Based Medicine Working Group. JAMA. 1994;272:234-7. 20. Jaeschke R, Guyatt G, Sackett DL. Users' guides to the medical literature. III. How to use an article about a diagnostic test. A. Are the results of the study valid? EvidenceBased Medicine Working Group. JAMA. 1994;271:389-91. 21. Jaeschke R, Guyatt GH, Sackett DL. Users' guides to the medical literature. III. How to use an article about a diagnostic test. B. What are the results and will they help me in caring for my patients? The Evidence-Based Medicine Working Group. JAMA. 1994;271:703-7. 22. Guyatt GH, Sackett DL, Cook DJ. Users' guides to the medical literature. II. How to use an article about therapy or prevention. A. Are the results of the study valid? EvidenceBased Medicine Working Group. JAMA. 1993;270:2598-601. 23. Guyatt GH, Sackett DL, Cook DJ. Users' guides to the medical literature. II. How to use an article about therapy or prevention. B. What were the results and will they help me in caring for my patients? Evidence-Based Medicine Working Group. JAMA. 1994;271:59-63. 24. Khan KS, Daya S, Jadad A. The importance of quality of primary studies in producing unbiased systematic reviews. Arch Intern.Med. 1996;156:661-6. 43 25. Jadad AR, Rennie D. The randomized controlled trial gets a middle-aged checkup. JAMA. 1998;279:319-20. 26. Jadad AR, Moore RA, Carroll D, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17:1-12. 27. Schulz KF, Chalmers I, Hayes RJ, Altman DG. Empirical evidence of bias. Dimensions of methodological quality associated with estimates of treatment effects in controlled trials. JAMA. 1995;273:408-12. 28. Moher D, Jadad AR, Nichol G, Penman M, Tugwell P, Walsh S. Assessing the quality of randomized controlled trials: an annotated bibliography of scales and checklists. Control Clin Trials. 1995;16:62-73. 44 A PPENDIX A: G L O S S A R Y * (Uncontrolled) before and after study A prospective study where a cohort is determined to be the control group before an intervention, and the same cohort is determined to be the treatment group after the intervention. Outcomes are measured during both the control period and the treatment period and then compared. There is not a separate group acting as concurrent controls. Blinding (synonym: masking) Keeping secret group assignment (e.g. to treatment or control) from the study participants or investigators. Blinding is used to protect against the possibility that knowledge of assignment may affect patient response to treatment, provider behaviours (performance bias) or outcome assessment (detection bias). Blinding is not always practical (e.g. when comparing surgery to drug treatment). The importance of blinding depends on how objective the outcome measure is; blinding is more important for less objective outcome measures such as pain or quality of life. See also single blind, double blind and triple blind. Case series An uncontrolled observational study involving an intervention and outcome for more than one person. Case study (synonyms: anecdote, case history, single case report) An uncontrolled observational study involving an intervention and outcome for a single person. * Taken primarily from The Cochrane Collaboration Handbook, Version 3.0.2 (September 1997) 46 A PPENDIX A: GLOSSARY (CONTINUED) Case-control study (synonyms: case referent study, retrospective study) A study that starts with identification of people with the disease or outcome of interest (cases) and a suitable control group without the disease or outcome. The relationship of an attribute (intervention, exposure or risk factor) to the outcome of interest is examined by comparing the frequency or level of the attribute in the cases and controls. For example, to determine whether thalidomide caused birth defects a group of children with birth defects (cases) could be compared to a group of children without birth defects (controls). The groups would then be compared with respect to the proportion exposed to thalidomide through their mothers taking the tablets. Casecontrol studies are sometimes described as being retrospective as they are always performed looking back in time. Clinical trial (synonyms: therapeutic trial, intervention study) A trial that tests out a drug or other intervention to assess its effectiveness and safety. This general term encompasses randomised controlled trials and controlled clinical trials. Cohort study (synonyms: follow-up, incidence, longitudinal, prospective study) An observational study in which a defined group of people (the cohort) is followed over time and outcomes are compared in subsets of the cohort who were exposed or not exposed, or exposed at different levels, to an intervention or other factor of interest. Cohorts can be assembled in the present and followed into the future (a "concurrent cohort study"), or identified from past records and followed forward from that time up to the present (a "historical cohort study"). Because random allocation is not used, matching or statistical adjustment must be used to ensure that the comparison groups are as similar as possible. 47 A PPENDIX A: GLOSSARY (CONTINUED) Control 1. In clinical trials comparing two or more interventions, a control is a person in the comparison group that receives a placebo, no intervention, usual care or another form of care. 2. In case-control studies a control is a person in the comparison group without the disease or outcome of interest. 3. In statistics control means to adjust for or take into account extraneous influences or observations. 4. Control can also mean programs aimed at reducing or eliminating the disease when applied to communicable (infectious) diseases. Controlled clinical trial Refers to a study that compares one or more intervention groups to one or more comparison (control) groups. Whilst not all controlled studies are randomised, all randomised trials are controlled. Cross-sectional study (synonym: prevalence study) A study that examines the relationship between diseases (or other health related characteristics) and other variables of interest as they exist in a defined population at one particular time. The temporal sequence of cause and effect cannot necessarily be determined in a cross-sectional study. Cross-over trial A type of clinical trial comparing two or more interventions in which the participants, upon completion of the course of one treatment are switched to another. For example, for a 48 A PPENDIX A: GLOSSARY (CONTINUED) comparison of treatments A and B, half the participants are randomly allocated to receive them in the order A, B and half to receive them in the order B, A. A problem with this design is that the effects of the first treatment may carry over into the period when the second is given. Double blind (synonym: double masked) Neither the participants in a trial nor the investigators (outcome assessors) are aware of which intervention the participants are given. The purpose of blinding the participants (recipients and providers of care) is to prevent performance bias. The purpose of blinding the investigators (outcome assessors, who might also be the care providers) is to protect against detection bias. See also blinding, single blind, triple blind, concealment of allocation. EMBASE (Excerpta Medica database) A European-based electronic database of pharmacological and biomedical literature covering 3,500 journals from 110 countries. Years of coverage - 1974 to present. Gold standard The method, procedure or measurement that is widely accepted as being the best available against which new interventions should be compared. It is particularly important in studies of the accuracy of diagnostic tests. For example, handsearching is sometimes used as the gold standard for identifying trials against which electronic searches of databases such as MEDLINE are compared. 49 A PPENDIX A: GLOSSARY (CONTINUED) Historical control Person or group for whom data were collected earlier than for the group being studied. Because of changes over time in risks, prognosis, healthcare, etc. there is a large risk of bias (in studies that use historical controls) due to systematic differences between the comparison groups. Intention-to-treat An intention-to-treat analysis is one in which all the participants in a trial are analyzed according to the intervention to which they were allocated, whether they received it or not. Intention-totreat analyzes are favoured in assessments of effectiveness as they mirror the non-compliance and treatment changes that are likely to occur when the intervention is used in practice, and because of the risk of attrition bias when participants are excluded from the analysis. MEDLINE (MEDlars onLINE) An electronic database produced by the United States National Library of Medicine. It indexes millions of articles in selected (about 3,700) journals. It is available through most medical libraries, and can be accessed on CD-ROM, the Internet and by other means. Years of coverage 1966 to present. Methodological quality (synonyms: validity, internal validity) The extent to which the design and conduct of a trial are likely to have prevented systematic errors (bias). Variation in quality can explain variation in the results of trials included in a systematic review. More rigorously designed (better 'quality') trials are more likely to yield results that are closer to the 'truth'. See also external validity, validity. 50 A PPENDIX A: GLOSSARY (CONTINUED) Observational study (synonym: non-experimental study) A study in which nature is allowed to take its course. Changes or differences in one characteristic (e.g. whether or not people received the intervention of interest) are studied in relation to changes or differences in other(s) (e.g. whether or not they died), without the intervention of the investigator. There is a greater risk of selection bias than in experimental studies (randomised controlled trials). Odds ratio (OR) The ratio of the odds of an event in the experimental (intervention) group to the odds of an event in the control group. Odds are the ratio of the number of people in a group with an event to the number without an event. Thus, if a group of 100 people had an event rate of 0.20, 20 people had the event and 80 did not, and the odds would be 20/80 or 0.25. An odds ratio of one indicates no difference between comparison groups. For undesirable outcomes an OR that is less than one indicates that the intervention was effective in reducing the risk of that outcome. When the event rate is small, odds ratios are very similar to relative risks. Per protocol analysis Analysis performed where only patients remaining in the study at study conclusion are analyzed. Placebo An inactive substance or procedure administered to a patient, usually to compare its effects with those of a real drug or other intervention, but sometimes for the psychological benefit to the patient through a belief that s/he is receiving treatment. Placebos are used in clinical trials to 51 A PPENDIX A: GLOSSARY (CONTINUED) blind people to their treatment allocation. Placebos should be indistinguishable from the active intervention to ensure adequate blinding. Prospective study In evaluations of the effects of healthcare interventions, a study in which people are divided into groups that are exposed or not exposed to the intervention(s) of interest before the outcomes have occurred. Randomised controlled trials are always prospective studies and case control studies never are. Concurrent cohort studies are prospective studies, whereas historical cohort studies are not (see cohort study), although in epidemiology a prospective study is sometimes used as a synonym for cohort study. See retrospective study. P-value The probability (ranging from zero to one) that the observed results in a study, or results more extreme, could have occurred by chance. In a meta-analysis the P-value for the overall effect assesses the overall statistical significance of the difference between the treatment and control groups, whilst the P-value for the heterogeneity statistic assesses the statistical significance of differences between the effects observed in each study. Quality score A value assigned to represent the validity of a study either for a specific criterion, such as allocation concealment, or overall. Quality scores can be use letters (A, B, C) or numbers. An advantage of using letters is that the order of best to worst may be more obvious than for numbers. 52 A PPENDIX A: GLOSSARY (CONTINUED) Quasi-random allocation A method of allocating participants to different forms of care that is not truly random; for example, allocation by date of birth, day of the week, medical record number, month of the year, or the order in which participants are included in the study (e.g. alternation). Random allocation A method that uses the play of chance to assign participants to comparison groups in a trial, e.g. by using a random numbers table or a computer-generated random sequence. Random allocation implies that each individual or unit being entered into a trial has the same chance of receiving each of the possible interventions. It also implies that the probability that an individual will receive a particular intervention is independent of the probability that any other individual will receive the same intervention. See also concealment of allocation, quasi-random allocation, randomization. Randomization Method used to generate a random allocation sequence, such as using tables of random numbers or computer-generated random sequences. The method of randomization should be distinguished from concealment of allocation because of the risk of selection bias despite the use of randomization, if there is not adequate allocation concealment. For instance, a list of random numbers may be used to randomize participants, but if the list is open to the individuals responsible for recruiting and allocating participants, those individuals can influence the allocation process, either knowingly or unknowingly. 53 A PPENDIX A: GLOSSARY (CONTINUED) Randomized control trial (RCT) (synonym: randomized clinical trial) An experiment in which investigators randomly allocate eligible people into (e.g. treatment and control) groups to receive or not to receive one or more interventions that are being compared. The results are assessed by comparing outcomes in the treatment and control groups. NOTE: when using randomized controlled trial as a search term (publication type) in MEDLINE, the US spelling (randomized) must be used. Relative Risk (RR) (synonym: risk ratio) The ratio of risk in the intervention group to the risk in the control group. The risk (proportion, probability or rate) is the ratio of people with an event in a group to the total in the group. A relative risk of one indicates no difference between comparison groups. A relative risk of one indicates no difference between comparison groups. For undesirable outcomes a RR that is less than one indicates that the intervention was effective in reducing the risk of that outcome. Retrospective study A study in which the outcomes have occurred to the participants before the study commenced. Case control studies are always retrospective, cohort studies sometimes are, randomized controlled trials never are. See prospective study. Statistical significance An estimate of the probability of an association (effect) as large or larger than what is observed in a study occurring by chance, usually expressed as a P-value. For example, a P-value of 0.049 for a risk difference of 10% means that there is less than a one in 20 (0.05) chance of an association that is as large or larger having occurred by chance and it could be said that the results are 54 A PPENDIX A: GLOSSARY (CONTINUED) "statistically significant" at P = 0.05). The cut-off for statistical significance is usually taken at 0.05, but sometimes at 0.01 or 0.10. These cut-offs are arbitrary and have no specific importance. Although it is often done, it is inappropriate to interpret the results of a study differently according to whether the P-value is, say, 0.055 or 0.045 (which are quite similar values, not diametrically opposed ones). Washout period The stage in a cross-over trial when treatment is withdrawn before the second treatment is given. Washout periods are usually necessary because of the possibility that the intervention administered first can affect the outcome variable for some time after treatment ceases. A run-in period before a trial starts is sometimes called a washout period if treatments that participants were using before entering the trial are discontinued. 55 A PPENDIX B: TECHNICAL E XPERTS - NKF DOQI N UTRITION W ORKGROUP IN D IALYSIS ADULT T ECHNICAL EXPERTS Joel D. Kopple, M.D. Professor of Medicine and Public Health University of California, Los Angeles Schools of Medicine and Public Health Chief, Division of Nephrology and Hypertension Harbor-UCLA Medical Center Torrance, California Charles Foulks, M.D., F.A.C.P. Professor of Medicine Director Division of Nephrology and Hypertension Texas A&M University Center for the Health Sciences Scott & White Clinic Temple, TX Suhail Ahmad, M.B.,B.S. Associate Professor, Medicine Medical Director, Dialysis & Apheresis Lab. University of Washington, Medical Director, Scribner Kidney Center, Seattle Denis Fouque, MD,PhD Professor of Nephrology Director, Cochrane Renal Group Hospital Edouard Herriot University Claude Bernard Lyon1 France Bradley J. Maroni, M.D. Associate Medical Director AMGEN, Inc. Thousand Oaks, CA Jerrilynn Burrowes, MS, RD, CS Research Coordinator Division of Nephrology & Hypertension. Beth Israel Medical Center New York Linda W. Moore, RD Sr.Manager, Scientific Publications SangStat Medical Corporation Germantown, TN 38138 Glenn M. Chertow, MD, MPH, CNSP Director of Clinical Services Divisions of Nephrology Moffitt-Long Hospitals and UCSF-Mt. Zion Medical Center Assistant Professor of Medicine in Residence University of California, San Francisco Marsha Wolfson, M.D. Medical Director, Renal Division Baxter Healthcare Corporation McGaw Park, IL David Cochram, M.S., R.D. Clinical Research Scientist Medical and Scientific Affairs Ross Products Division Abbott Laboratories Columbus, OH 56 APPENDIX B: TECHNICAL EXPERTS - NKF DOQI NUTRITION IN DIALYSIS W ORKGROUP (CONTINUED) PEDIATRIC T ECHNICAL EXPERTS Bruce Morgenstern, M.D. Associate Professor of Pediatrics Mayo Medical School Consultant in Pediatric Nephrology Mayo Clinic Rochester, MN Isidro B. Salusky, M.D. Professor of Pediatrics Director, Pediatric Dialysis Program Director, General Clinical Research Center UCLA School of Medicine James Chan, M.D. Professor of Pediatrics Chair, Division of Pediatric Nephrology Vice Chair, Department of Pediatrics Medical College of Virginia Richmond Pauline Nelson, R.D. Pediatric Renal Dietitian Department of Nutrition UCLA Medical Center Los Angeles Bradley A. Warady M.D. Professor of Pediatrics University of Missouri - Kansas City School of Medicine Chief, Section of Pediatric Nephrology Director, Dialysis and Transplantation The Childrens Mercy Hospital Richard Fine, M.D. Professor and Chairman Department of Pediatrics SUNY at Stonybrook School of Medicine Craig B. Langman, M.D. Professor of Pediatrics Northwestern University School of Medicine Head, Nephrology and Mineral Metabolism Children's Memorial Medical Center Chicago 57 A PPENDIX C: SEARCH S T R A T E G I E S Strategies for Questions 1-8 #1965-April, 1998 1) hemodialysis/ 2) hemodiafiltration/ 3) hemodialysis, home/ 4) hemofiltration/ 5) hemodiafiltration/ 6) peritoneal dialysis/ 7) peritoneal dialysis, continuous ambulatory/ 8) 1 or 2 or 3 or 4 or 5 or 6 or 7 9) kidney, artificial/ 10) dialysis/ 11) 9 or 10 12) kidney failure, chronic/ 13) 8 or 11 14) renal replacement therapy/ 15) 8 or 11 or 12 or 14 16) 8 or 12 or 14 17) nutrition assessment/ 18) nutrition surveys/ 19) diet surveys/ 20) 17 or 18 or 19 21) nutrition/ 22) diet/ 23) energy intake/ 24) nutritional requirements/ 25) nutritional status/ 26) 21 or 22 or 23 or 24 or 25 27) nutrition disorders/ 28) protein deficiency/ 29) protein-energy malnutrition/ 30) 27 or 28 or 29 31) caloric intake/ 32) exp dietary proteins/ 33) nutrition$.tw. 34) protein$.tw. 35) calori$.tw. 36) dh.fs. 37) exp diet therapy/ 58 39) 40) 41) 42) 43) 44) 45) 46) 47) 48) 49) 50) 51) 52) 53) 54) 55) 56) 57) 58) 59) 60) 61) 62) 63) 64) 65) 66) 67) 68) 69) 70) 71) 72) 73) 74) 75) skinfold thickness/ anthropometry/ body mass index/ body height/ body surface area/ body weight/ creatinine/ cholesterol/ exp proteins/ kidney function tests/ blood urea nitrogen/ diet records/ subjective global assessment.tw. acute phase protein.tw. prognos$.tw. prognosis/ npna.tw. npcr.tw. pcr.tw. pna.tw. protein catabolic rate.tw. (protein adj4 nitrogen appearance).tw. body water/ electric impedance/ or/39-62 predialysis.tw. energy expenditure.tw. resting energy.tw. exp energy metabolism/ nitrogen/ nitrogen.tw. reference values/ reference standards/ dh.fs. intradialytic.tw. diet therapy/ diet, protein-restricted/ APPENDIX C: SEARCH STRATEGIES (CONTINUED) 38) 20 or 26 or 30 or 31 or 32 or 33 or 34 or 35 or 36 or 37 59 76) nutritional support/ APPENDIX C: SEARCH STRATEGIES (CONTINUED) Strategies for Questions 1-8 (continued) 77) enteral nutrition/ 78) parenteral nutrition/ 79) parenteral nutrition, home/ 80) parenteral nutrition, home total/ 81) parenteral nutrition, total/ 82) parenteral nutrition, home total/ 83) (nutrition$ adj4 counsel$).ti,ab,sh. 84) (oral adj4 supplement$).tw. 85) tube feeding/ 86) food, formulated/ 87) or/64-86 88) health education/ 89) patient education/ 90) patient education.tw. 91) counsel$.tw. 92) or/88-91 93) 38 or 63 or 87 94) 16 and 93 95) 8 and 92 96) 94 or 95 97) 96 not letter.pt. 98) 97 not editorial.pt. 99) 98 not news.pt. 100) 99 not case report/ 101) 100 not animal/ 102) limit 100 to human 103) 101 or 102 60 APPENDIX C: SEARCH STRATEGIES (CONTINUED) Search strategy for Questions 9-12 1) 2) 3) 4) 5) 6) 7) 8) 9) 10) 11) 12) 13) 14) 15) 16) 17) 18) 19) 20) 21) 22) 23) 24) 25) 26) 27) 28) 29) 30) 31) hemodialysis/ hemodiafiltration/ hemodialysis, home/ hemofiltration/ hemodiafiltration/ peritoneal dialysis/ peritoneal dialysis, continuous ambulatory/ 1 or 2 or 3 or 4 or 5 or 6 or 7 kidney, artificial/ dialysis/ 9 or 10 kidney failure, chronic/ 8 or 11 8 or 11 or 12 carnitine/ acetylcarnitine/ palmitoylcarnitine/ 15 or 16 or 17 541-15-1.rn. 1935-18-8.rn. 14992-62-2.rn. l-carnitine.tw. carnitine.tw. bicarnesine.tw. vitamin bt.tw. vitamin b t.tw. or/18-26 8 and 27 14 and 27 29 not letter.pt. 30 not news.pt. 61 APPENDIX C: SEARCH STRATEGIES (CONTINUED) Search strategy for Question 13 , 14 and IGF (Pediatric Question 1) 1) 2) 3) 4) 5) 6) 7) 8) 9) 10) 11) 12) 13) 14) 15) 16) 17) 18) 19) 20) 21) 22) 23) 24) 25) 26) 27) 28) 29) 30) 31) 32) 33) 34) renal replacement therapy/ hemodialysis/ hemodiafiltration/ hemodialysis, home/ hemofiltration/ hemodiafiltration/ peritoneal dialysis/ peritoneal dialysis, continuous ambulatory/ 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 limit 9 to (newborn infant <birth to 1 month> or infant <1 to 23 months> or preschool child <2 to 5 years> or child <6 to 12 years> or adolescence <13 to 18 years>) 10 not letter.pt. 11 not review.pt. 12 not editorial.pt. 13 not case report/ insulin-like growth factor i/ somatomedins/ 14 and 15 14 and 16 14 and igf.tw. 14 and insulin like growth.tw. or/17-20 exp minerals/ 14 and 22 vitamins/ ascorbic acid/ bioflavonoids/ vitamin a/ vitamin b complex/ vitamin e/ vitamin k/ vitamin u/ 24 or 25 or 26 or 27 or 28 or 29 or 30 or 31 14 and 32 23 or 33 62 A PPENDIX D: B IBLIOGRAPHY OF A CCEPTED ARTICLES * References for Questions 1-12 - Adults Question 1 - adults 1. Acchiardo SR, Moore LW, Latour PA. Malnutrition as the main factor in morbidity and mortality of hemodialysis patients. Kidney International - Supplement. 1983;16:S199S203. Reference ID: 12089 2. Avram MM, Goldwasser P, Erroa M, Fein PA. Predictors of survival in continuous ambulatory peritoneal dialysis patients: the importance of prealbumin and other nutritional and metabolic markers. American Journal of Kidney Diseases. 1994;23:91-8. Reference ID: 3778 3. Avram MM, Mittman N, Bonomini L, Chattopadhyay J, Fein P. Markers for survival in dialysis: A seven-year prospective study. American Journal of Kidney Diseases. 1995;26:209-19. Reference ID: 2672 4. Avram MM, Fein PA, Bonomini L, et al. Predictors of survival in continuous ambulatory peritoneal dialysis patients: a five-year prospective study. Peritoneal Dialysis International. 1996;16 Suppl 1:S190-S194. Reference ID: 1975 5. Barrett BJ, Parfrey PS, Morgan J, et al. Prediction of early death in end-stage renal disease patients starting dialysis. American Journal of Kidney Diseases. 1997;29:214-22. Reference ID: 789 6. Bilbrey GL, Cohen TL. Identification and treatment of protein calorie malnutrition in chronic hemodialysis patients. Dialysis Transplant. 1989;18:669-77+700. Reference ID: 4907 7. Blake PG, Sombolos K, Abraham G, et al. Lack of correlation between urea kinetic indices and clinical outcomes in CAPD patients [published erratum appears in Kidney Int 1991 Aug;40(2):388]. Kidney International. 1991;39:700-6. Reference ID: 6826 8. Blake PG, Flowerdew G, Blake RM, Oreopoulos DG. Serum albumin in patients on continuous ambulatory peritoneal dialysis--predictors and correlations with outcomes. Journal of the American Society of Nephrology. 1993;3:1501-7. Reference ID: 4841 * Reference ID numbers correspond with those listed in the evidence tables. 63 APPENDIX D: BIBLIOGRAPHY OF ACCEPTED ARTICLES (CONTINUED) 9. Canaud B, Garred LJ, Argiles A, Flavier JL, Bouloux C, Mion C. Creatinine kinetic modelling: a simple and reliable tool for the assessment of protein nutritional status in haemodialysis patients. Nephrology, Dialysis, Transplantation. 1995;10:1405-10. Reference ID: 2921 10. Chertow, G. M., Jacobs, D. O., Lazarus, J. M., Lew, N. L., and Lowrie, E. G. Phase angle predicts survival in hemodialysis patients. Journal of Renal Nutrition 7(4), 204-207. 1997. (GENERIC) Reference ID: 18834 11. Churchill DN, Taylor DW, Cook RJ, et al. Canadian hemodialysis morbidity study. Am.J.Kidney Dis. 1992;19:214-34. Reference ID: 4884 12. Churchill DN, Taylor DW, Keshaviah PR, et al. Adequacy of dialysis and nutrition in continuous peritoneal dialysis: Association with clinical outcomes. Journal of the American Society of Nephrology. 1996;7:198-207. Reference ID: 5129 13. Churchill DN, Thorpe KE, Vonesh EF, Keshaviah PR. Lower probability of patient survival and continuous peritoneal dialysis in the United States compared with Canada. Journal of the American Society of Nephrology. 1997;8:965-71. Reference ID: 5076 14. Davies SJ, Phillips L, Russell GI. Peritoneal solute transport predicts survival on CAPD independently of residual renal function. Nephrology Dialysis Transplantation. 1998;13:962-8. Reference ID: 5038 15. De Lima J, Sesso R, Abensur H, et al. Predictors of mortality in long-term haemodialysis patients with a low prevalence of comorbid conditions. Nephrology, Dialysis, Transplantation. 1995;10:1708-13. Reference ID: 2455 16. Degoulet P, Legrain M, Reach I, et al. Mortality risk factors in patients treated by chronic hemodialysis. Report of the Diaphane collaborative study. Nephron. 1982;31:103-10. Reference ID: 12751 17. Fenton SS, Johnston N, Delmore T, et al. Nutritional assessment of continuous ambulatory peritoneal dialysis patients. ASAIO Transactions. 1987;33:650-3. Reference ID: 9955 64 APPENDIX D: BIBLIOGRAPHY OF ACCEPTED ARTICLES (CONTINUED) 18. Fine A, Cox D. Modest reduction of serum albumin in continuous ambulatory peritoneal dialysis patients is common and of no apparent clinical consequence [see comments]. American Journal of Kidney Diseases. 1992;20:50-4. Reference ID: 5722 19. Foley RN, Parfrey PS, Harnett JD, Kent GM, Murray DC, Barre PE. Hypoalbuminemia, cardiac morbidity, and mortality in end-stage renal disease. Journal of the American Society of Nephrology. 1996;7:728-36. Reference ID: 1576 20. Fried L, Bernardini J, Piraino B. Neither size nor weight predicts survival in peritoneal dialysis patients. Peritoneal Dialysis International. 1996;16:357-61. Reference ID: 1203 21. Goldwasser P, Michel MA, Collier J, et al. Prealbumin and lipoprotein(a) in hemodialysis: relationships with patient and vascular access survival. American Journal of Kidney Diseases. 1993;22:215-25. Reference ID: 4753 22. Goldwasser P, Mittman N, Antignani A, et al. Predictors of mortality in hemodialysis patients. Journal of the American Society of Nephrology. 1993;3:1613-22. Reference ID: 4686 23. Himmelfarb J, Holbrook D, McMonagle E, Robinson R, Nye L, Spratt D. Kt/V, nutritional parameters, serum cortisol, and insulin growth factor-1 levels and patient outcome in hemodialysis. American Journal of Kidney Diseases. 1994;24:473-9. Reference ID: 3628 24. Husebye DG, Westlie L, Styrvoky TJ, Kjellstrand CM. Psychological, social, and somatic prognostic indicators in old patients undergoing long-term dialysis. Archives of Internal Medicine. 1987;147:1921-4. Reference ID: 9917 25. Ifudu O, Paul HR, Homel P, Friedman EA. Predictive value of functional status for mortality in patients on maintenance hemodialysis. American Journal of Nephrology. 1998;18:109-16. Reference ID: 5037 26. Iseki K, Uehara H, Nishime K, et al. Impact of the initial levels of laboratory variables on survival in chronic dialysis patients. American Journal of Kidney Diseases. 1996;28:541-8. Reference ID: 1523 65 APPENDIX D: BIBLIOGRAPHY OF ACCEPTED ARTICLES (CONTINUED) 27. Iseki K, Miyasato F, Tokuyama K, et al. Low diastolic blood pressure, hypoalbuminemia, and risk of death in a cohort of chronic hemodialysis patients. Kidney International. 1997;51:1212-7. Reference ID: 863 28. Jassal SV, Douglas JF, Stout RW. Prognostic markers in older patients starting renal replacement therapy. Nephrology, Dialysis, Transplantation. 1996;11:1052-7. Reference ID: 1657 29. Lowrie EG, Huang WH, Lew NL. Death risk predictors among peritoneal dialysis and hemodialysis patients: A preliminary comparison. American Journal of Kidney Diseases. 1995;26:220-8. Reference ID: 5157 30. Maggiore Q, Nigrelli S, Ciccarelli C, Grimaldi C, Rossi GA, Michelassi C. Nutritional and prognostic correlates of bioimpedance indexes in hemodialysis patients. Kidney International. 1996;50:2103-8. Reference ID: 1277 31. Maiorca R, Brunori G, Zubani R, et al. Predictive value of dialysis adequacy and nutritional indices for mortality and morbidity in CAPD and HD patients. A longitudinal study. Nephrology, Dialysis, Transplantation. 1995;10:2295-305. Reference ID: 2371 32. Marcen R, Teruel JL, de lA, Gamez C. The impact of malnutrition in morbidity and mortality in stable haemodialysis patients. Spanish Cooperative Study of Nutrition in Hemodialysis [see comments]. Nephrology, Dialysis, Transplantation. 1997;12:2324-31. Reference ID: 173 33. Movilli E, Mombelloni S, Gaggiotti M, Maiorca R. Effect of age on protein catabolic rate, morbidity, and mortality in uraemic patients with adequate dialysis. Nephrol.Dial.Transplant. 1993;8:735-9. Reference ID: 4867 34. Movilli E, Filippini M, Brunori G, et al. Influence of protein catabolic rate on nutritional status, morbidity and mortality in elderly uraemic patients on chronic haemodialysis: a prospective 3-year follow-up study. Nephrology, Dialysis, Transplantation. 1995;10:5148. Reference ID: 2946 35. Oksa H, Pasternack A, Pasanen M. Serum urea-creatinine ratio as a prognostic index in hemodialysis patients. Clinical Nephrology. 1987;27:125-30. Reference ID: 9936 66 APPENDIX D: BIBLIOGRAPHY OF ACCEPTED ARTICLES (CONTINUED) 36. Owen WF, Jr., Lew NL, Liu Y, Lowrie EG, Lazarus JM. The urea reduction ratio and serum albumin concentration as predictors of mortality in patients undergoing hemodialysis. New Engl.J.Med. 1993;329:1001-6. Reference ID: 4857 37. Piccoli GB, Quarello F, Salomone M, et al. Are serum albumin and cholesterol reliable outcome markers in elderly dialysis patients?. Nephrology, Dialysis, Transplantation. 1995;10 Suppl 6:72-7. Reference ID: 2911 38. Piraino B, Bernardini J, Centa PK, Johnston JR, Sorkin MI. The effect of body weight on CAPD related infections and catheter loss. Peritoneal Dialysis International. 1991;11:64-8. Reference ID: 6916 39. Pollock CA, Ibels LS, Allen BJ, et al. Total body nitrogen as a prognostic marker in maintenance dialysis. Journal of the American Society of Nephrology. 1995;6:82-8. Reference ID: 2690 40. Soucie JM, McClellan WM. Early death in dialysis patients: risk factors and impact on incidence and mortality rates. Journal of the American Society of Nephrology. 1996;7:2169-75. Reference ID: 1075 41. Spiegel DM, Breyer JA. Serum albumin: a predictor of long-term outcome in peritoneal dialysis patients. American Journal of Kidney Diseases. 1994;23:283-5. Reference ID: 3835 42. Sreedhara R, Avram MM, Blanco M, Batish R, Mittman N. Prealbumin is the best nutritional predictor of survival in hemodialysis and peritoneal dialysis. American Journal of Kidney Diseases. 1996;28:937-42. Reference ID: 1240 43. Struijk DG, Krediet RT, Koomen GC, Boeschoten EW, Arisz L. The effect of serum albumin at the start of continuous ambulatory peritoneal dialysis treatment on patient survival [see comments]. Peritoneal Dialysis International. 1994;14:121-6. Reference ID: 4052 44. Teehan BP, Schleifer CR, Brown JM, Sigler MH, Raimondo J. Urea kinetic analysis and clinical outcome on CAPD. A five year longitudinal study. Advances in Peritoneal Dialysis. 1990;6:181-5. Reference ID: 7051 Question 2 - adults 67 APPENDIX D: BIBLIOGRAPHY OF ACCEPTED ARTICLES (CONTINUED) 1. Bilbrey GL, Cohen TL. Identification and treatment of protein calorie malnutrition in chronic hemodialysis patients. Dialysis Transplant. 1989;18:669-77+700. Reference ID: 4907 2. Borovnicar DJ, Wong KC, Kerr PG, et al. Total body protein status assessed by different estimates of fat-free mass in adult peritoneal dialysis patients. European Journal of Clinical Nutrition. 1996;50:607-16. Reference ID: 1031 3. Chauveau P, Naret C, Puget J, Zins B, Poignet JL. Adequacy of haemodialysis and nutrition in maintenance haemodialysis patients: clinical evaluation of a new on-line urea monitor. Nephrology, Dialysis, Transplantation. 1996;11:1568-73. Reference ID: 1335 4. Chertow GM, Lowrie EG, Wilmore DW, et al. Nutritional assessment with bioelectrical impedance analysis in maintenance hemodialysis patients. Journal of the American Society of Nephrology. 1995;6:75-81. Reference ID: 2689 5. Chertow GM, Lazarus JM, Lew NL, Ma L, Lowrie EG. Bioimpedance norms for the hemodialysis population. Kidney International. 1997;52:1617-21. Reference ID: 313 6. Cueto-Manzano AM, Espinosa A, Hernandez A, Correa-Rotter R. Peritoneal transport kinetics correlate with serum albumin but not with the overall nutritional status in CAPD patients. American Journal of Kidney Diseases. 1997;30:229-36. Reference ID: 815 7. De Fijter M, De FW, Oe PL, ter WM, Donker AJ. Assessment of total body water and lean body mass from anthropometry, Watson formula, creatinine kinetics, and body electrical impedance compared with antipyrine kinetics in peritoneal dialysis patients. Nephrology, Dialysis, Transplantation. 1997;12:151-6. Reference ID: 248 8. Formica C, Atkinson MG, Nyulasi I, McKay J, Heale W, Seeman E. Body composition following hemodialysis: Studies using dual-energy X-ray absorptiometry and bioelectrical impedance analysis. Osteoporosis Int. 1993;3:192-7. Reference ID: 4869 9. Han DS, Lee SW, Kang SW, et al. Factors affecting low values of serum albumin in CAPD patients. Advances in Peritoneal Dialysis. 1996;12:288-92. Reference ID: 1373 68 APPENDIX D: BIBLIOGRAPHY OF ACCEPTED ARTICLES (CONTINUED) 10. Harrison JE, McNeill KG, Strauss AL. A nitrogen index - total body protein normalized for body size - for diagnosis of protein status in health and disease. Nutr.Res. 1984;4:209-24. Reference ID: 4959 11. Harty JC, Boulton H, Curwell J, et al. The normalized protein catabolic rate is a flawed marker of nutrition in CAPD patients. Kidney International. 1994;45:103-9. Reference ID: 3810 12. Jacob V, Marchant PR, Wild G, Brown CB, Moorhead PJ, el NM. Nutritional profile of continuous ambulatory peritoneal dialysis patients. Nephron. 1995;71:16-22. Reference ID: 2966 13. Johansson AC, Attman PO, Haraldsson B. Creatinine generation rate and lean body mass: a critical analysis in peritoneal dialysis patients. Kidney International. 1997;51:855-9. Reference ID: 635 14. Jones CH, Newstead CG, Will EJ, Smye SW, Davison AM. Assessment of nutritional status in CAPD patients: serum albumin is not a useful measure. Nephrology, Dialysis, Transplantation. 1997;12:1406-13. Reference ID: 733 15. Kawaguchi Y, Sugino N, Arai J, et al. Nutritional assessment of patients on continuous ambulatory peritoneal dialysis. Nippon Jinzo Gakkai Shi.Japanese Journal of Nephrology. 1993;35:843-51. Reference ID: 4315 16. Kuhlmann MK, Winkelspecht B, Hammers A, Kohler H. [Malnutrition in hemodialysis patients. Self-assessment, medical evaluation and "verifiable" parameters]. [German]. Medizinische Klinik. 1997;92:13-7. Reference ID: 242 17. Lorenzo V, de BE, Rufino M, et al. Caloric rather than protein deficiency predominates in stable chronic haemodialysis patients. Nephrology, Dialysis, Transplantation. 1995;10:1885-9. Reference ID: 2193 18. Madore F, Wuest M, Ethier JH. Nutritional evaluation of hemodialysis patients using an impedance index. Clinical Nephrology. 1994;41:377-82. Reference ID: 3278 19. Oe B, De Fijter CWH, Oe PL, Stevens P, De Vries PMJ. Four-site skinfold anthropometry (FSA) versus body impedance analysis (BIA) in assessing nutritional status of patients on maintenance hemodialysis: Which method is to be preferred in routine patient care. Clinical Nephrology. 1998;49:180-5. Reference ID: 5043 69 APPENDIX D: BIBLIOGRAPHY OF ACCEPTED ARTICLES (CONTINUED) 20. Oksa H, Ahonen K, Pasternack A, Marnela KM. Malnutrition in hemodialysis patients. Scandinavian Journal of Urology & Nephrology. 1991;25:157-61. Reference ID: 6603 21. Panzetta G, Tessitore N, Faccini G, Maschio G. The protein catabolic rate as a measure of protein intake in dialysis patients: usefulness and limits. Nephrology, Dialysis, Transplantation. 1990;5 Suppl 1:125-7. Reference ID: 7096 22. Pollock CA, Allen BJ, Warden RA, et al. Total-body nitrogen by neutron activation in maintenance dialysis [published erratum appears in Am J Kidney Dis 1993 Feb;21(2):237]. Reference ID: 6975 23. Rayner HC, Stroud DB, Salamon KM, et al. Anthropometry underestimates body protein depletion in haemodialysis patients. Nephron. 1991;59:33-40. Reference ID: 6582 24. Schmidt R, Dumler F, Cruz C, Lubkowski T, Kilates C. Improved nutritional follow-up of peritoneal dialysis patients with bioelectrical impedance. Advances in Peritoneal Dialysis. 1992;8:157-9. Reference ID: 5421 25. Sombolos K, Berkelhammer C, Baker J. Nutritional assessment and skeletal muscle function in patients on continuous ambulatory peritoneal dialysis. Peritoneal Dial.Bull. 1986;6:53-8. Reference ID: 4938 26. Stall SH, Ginsberg NS, DeVita MV, et al. Comparison of five body-composition methods in peritoneal dialysis patients. American Journal of Clinical Nutrition. 1996;64:125-30. Reference ID: 5109 27. Stenver DI, Gotfredsen A, Hilsted J, Nielsen B. Body composition in hemodialysis patients measured by dual-energy X-ray absorptiometry. American Journal of Nephrology. 1995;15:105-10. Reference ID: 5164 28. Woodrow G, Oldroyd B, Smith MA, Turney JH. Measurement of body composition in chronic renal failure: comparison of skinfold anthropometry and bioelectrical impedance with dual energy X-ray absorptiometry. European Journal of Clinical Nutrition. 1996;50:295-301. Reference ID: 1566 29. Young GA, Kopple JD, Lindholm B, et al. Nutritional assessment of continuous ambulatory peritoneal dialysis patients: an international study. American Journal of Kidney Diseases. 1991;17:462-71. Reference ID: 6439 70 APPENDIX D: BIBLIOGRAPHY OF ACCEPTED ARTICLES (CONTINUED) Question 3 - adults 1. Brady JP, Hasbargen JA. Correction of metabolic acidosis and its effect on albumin in chronic hemodialysis patients. American Journal of Kidney Diseases. 1998;31:35-40. Reference ID: 6 2. Dumler F, Galan M. Impact of acidosis on nutritional status in chronic peritoneal dialysis patients. Advances in Peritoneal Dialysis. 1996;12:307-10. Reference ID: 1369 3. Graham KA, Reaich D, Channon SM, Downie S, Goodship THJ. Correction of acidosis in hemodialysis decreases whole-body protein degradation. Journal of the American Society of Nephrology. 1997;8:632-7. Reference ID: 5061 4. Harris DC, Yuill E, Chesher DW. Correcting acidosis in hemodialysis: effect on phosphate clearance and calcification risk. Journal of the American Society of Nephrology. 1995;6:1607-12. Reference ID: 2358 5. Kang SW, Lee SW, Lee IH, et al. Impact of metabolic acidosis on serum albumin and other nutritional parameters in long-term CAPD patients. Advances in Peritoneal Dialysis. 1997;13:249-52. Reference ID: 395 6. Movilli E, Bossini N, Viola BF, et al. Evidence for an independent role of metabolic acidosis on nutritional status in haemodialysis patients. Nephrology Dialysis Transplantation. 1998;13:674-8. Reference ID: 5046 7. Otte KE, Lillevang ST, Rasmussen AG, Christensen HK, Pedersen FB. Acetate or bicarbonate for haemodialysis: a randomised, double-blind controlled trial. Nephrology, Dialysis, Transplantation. 1990;5:931-6. Reference ID: 7553 8. Stein A, Moorhouse J, Iles-Smith H, et al. Role of an improvement in acid-base status and nutrition in CAPD patients. Kidney International. 1997;52:1089-95. Reference ID: 101 9. Williams AJ, Dittmer ID, McArley A, Clarke J. High bicarbonate dialysate in haemodialysis patients: effects on acidosis and nutritional status. Nephrology, Dialysis, Transplantation. 1997;12:2633-7. Reference ID: 327 Question 4 - adults 71 APPENDIX D: BIBLIOGRAPHY OF ACCEPTED ARTICLES (CONTINUED) 1. Acchiardo SR, Moore LW, Burk L. Morbidity and mortality in hemodialysis patients. ASAIO Transactions. 1990;36:M148-M151 Reference ID: 7291 2. Bajardi P, Cravero R, Valenti M, et al. [Protein metabolism and nutritional status in hemodialysis]. Minerva Urologica e Nefrologica. 1991;43:153-8. Reference ID: 5993 3. Bergstrom J, Furst P, Alvestrand A, Lindholm B. Protein and energy intake, nitrogen balance and nitrogen losses in patients treated with continuous ambulatory peritoneal dialysis. Kidney International. 1993;44:1048-57. Reference ID: 4072 4. Blumenkrantz MJ, Kopple JD, Moran JK, Grodstein GP, Coburn JW. Nitrogen and urea metabolism during continuous ambulatory peritoneal dialysis. Kidney International. 1981;20:78-82. Reference ID: 13048 5. Blumenkrantz MJ, Kopple JD, Moran JK, Coburn JW. Metabolic balance studies and dietary protein requirements in patients undergoing continuous ambulatory peritoneal dialysis. Kidney International. 1982;21:849-61. Reference ID: 12547 6. Davies SJ, Russell L, Bryan J, Phillips L, Russell GI. Comorbidity, urea kinetics, and appetite in continuous ambulatory peritoneal dialysis patients: their interrelationship and prediction of survival. American Journal of Kidney Diseases. 1995;26:353-61. Reference ID: 2389 7. Davies SJ, Russell L, Bryan J, Phillips L, Russell GI. Impact of peritoneal absorption of glucose on appetite, protein catabolism and survival in CAPD patients. Clinical Nephrology. 1996;45:194-8. Reference ID: 1610 8. Fenton SS, Johnston N, Delmore T, et al. Nutritional assessment of continuous ambulatory peritoneal dialysis patients. ASAIO Transactions. 1987;33:650-3. Reference ID: 9955 9. Giordano C, De SG, Pluvio M, et al. Protein requirement of patients on CAPD: a study on nitrogen balance. International Journal of Artificial Organs. 1980;3:11-4. Reference ID: 13558 10. Guarnieri G, Faccini L, Lipartiti T, et al. Simple methods for nutritional assessment in hemodialyzed patients. American Journal of Clinical Nutrition. 1980;33:1598-607. Reference ID: 13518 72 APPENDIX D: BIBLIOGRAPHY OF ACCEPTED ARTICLES (CONTINUED) 11. Ikizler TA, Greene JH, Yenicesu M, Schulman G, Wingard RL, Hakim RM. Nitrogen balance in hospitalized chronic hemodialysis patients. Kidney International - Supplement. 1996;57:S53-S56 Reference ID: 1281 12. Kopple JD, Shinaberger JH, Coburn JW, Sorensen MK, Rubini ME. Evaluating modified protein diets for uremia. Journal of the American Dietetic Association. 1969A;54:481-5. Reference ID: 18223 13. Kopple JD, Shinaberger JH, Coburn JW, Sorensen MK, Rubini ME. Optimal dietary protein treatment during chronic hemodialysis. Transactions - American Society for Artificial Internal Organs. 1969B;15:302-8. Reference ID: 18335 14. Lindner A, Tenckhoff H. Nitrogen balance in patients on maintenance peritoneal dialysis. Transactions - American Society for Artificial Internal Organs. 1970;16:255-9. Reference ID: 18071 15. Schilling H, Wu G, Pettit J. Nutritional status of patients on long-term CAPD. Peritoneal Dial.Bull. 1985;5:12-8. Reference ID: 4949 16. Slomowitz LA, Monteon FJ, Grosvenor M, Laidlaw SA, Kopple JD. Effect of energy intake on nutritional status in maintenance hemodialysis patients. Kidney International. 1989;35:704-11. Reference ID: 8089 17. Wardle EN, Kerr DN, Ellis HA. Serum proteins as indicators of poor dietary intake in patients with chronic renal failure. Clinical Nephrology. 1975;3:114-8. Reference ID: 16003 18. Young GA, Young JB, Young SM, et al. Nutrition and delayed hypersensitivity during continuous ambulatory peritoneal dialysis in relation to peritonitis. Nephron. 1986;43:17786. Reference ID: 10663 Question 5 - adults 1. Bernard S, Fouque D, Laville M, Zech P. Effects of low-protein diet supplemented with ketoacids on plasma lipids in adult chronic renal failure. Mineral & Electrolyte Metabolism. 1996;22:143-6. Reference ID: 1880 73 APPENDIX D: BIBLIOGRAPHY OF ACCEPTED ARTICLES (CONTINUED) 2. Fouque D, Laville M, Boissel JP, Chifflet R, Labeeuw M, Zech PY. Controlled low protein diets in chronic renal insufficiency: meta-analysis [see comments]. BMJ. 1992;304:216-20. Reference ID: 5287 3. Ikizler TA, Greene JH, Wingard RL, Parker RA, Hakim RM. Spontaneous dietary protein intake during progression of chronic renal failure. Journal of the American Society of Nephrology. 1995;6:1386-91. Reference ID: 2250 4. Kopple JD, Monteon FJ, Shaib JK. Effect of energy intake on nitrogen metabolism in nondialyzed patients with chronic renal failure. Kidney International. 1986;29:734-42. Reference ID: 10167 5. Kopple JD, Berg R, Houser H, Steinman TI, Teschan P. Nutritional status of patients with different levels of chronic renal insufficiency. Modification of Diet in Renal Disease (MDRD) Study Group. Kidney International - Supplement. 1989;27:S184-S194 Reference ID: 7977 6. Maroni BJ, Tom K, Masud T, Chapman T, Young VR. How is lean body mass conserved with the very-low protein diet regimen?. Mineral & Electrolyte Metabolism. 1996;22:54-7. Reference ID: 1883 7. Masud T, Young VR, Chapman T, Maroni BJ. Adaptive responses to very low protein diets: the first comparison of ketoacids to essential amino acids. Kidney International. 1994;45:1182-92. Reference ID: 4229 8. Park JS, Jung HH, Yang WS, et al. Protein intake and the nutritional status in patients with pre-dialysis chronic renal failure on unrestricted diet. Korean Journal of Internal Medicine. 1997;12:115-21. Reference ID: 215 9. Pedrini MT, Levey AS, Lau J, Chalmers TC, Wang PH. The effect of dietary protein restriction on the progression of diabetic and nondiabetic renal diseases: a meta-analysis [see comments]. Ann.Intern.Med. 1996;124:627-32. Reference ID: 5288 10. Pollock CA, Ibels LS, Zhu FY, et al. Protein intake in renal disease. Journal of the American Society of Nephrology. 1997;8:777-83. Reference ID: 564 11. Tom K, Young VR, Chapman T, Masud T, Akpele L, Maroni BJ. Long-term adaptive responses to dietary protein restriction in chronic renal failure. American Journal of Physiology. 1995;268:E668-E677 Reference ID: 3097 74 APPENDIX D: BIBLIOGRAPHY OF ACCEPTED ARTICLES (CONTINUED) 12. Walser M. Does prolonged protein restriction preceding dialysis lead to protein malnutrition at the onset of dialysis?. Kidney International. 1993;44:1139-44. Reference ID: 3940 Question 6 - adults 1. Harty J, Conway L, Keegan M, et al. Energy metabolism during CAPD: a controlled study. Advances in Peritoneal Dialysis. 1995;11:229-33. Reference ID: 2414 2. Ikizler TA, Wingard RL, Sun M, Harvell J, Parker RA, Hakim RM. Increased energy expenditure in hemodialysis patients. Journal of the American Society of Nephrology. 1996;7:2646-53. Reference ID: 1271 3. Monteon FJ, Laidlaw SA, Shaib JK, Kopple JD. Energy expenditure in patients with chronic renal failure. Kidney International. 1986;30:741-7. Reference ID: 10433 4. Olevitch LR, Bowers BM, DeOreo PB. Measurement of resting energy expenditure via indirect calorimetry among adult hemodialysis patients. Journal of Renal Nutrition. 1994;4:192 Reference ID: 2 5. Schneeweiss B, Graninger W, Stockenhuber F, et al. Energy metabolism in acute and chronic renal failure [see comments]. American Journal of Clinical Nutrition. 1990;52:596-601. Reference ID: 7625 Question 7 - adults 1. Allman MA, Stewart PM, Tiller DJ, Horvath JS, Duggin GG, Truswell AS. Energy supplementation and the nutritional status of hemodialysis patients. American Journal of Clinical Nutrition. 1990;51:558-62. Reference ID: 7825 2. Bannister DK, Acchiardo SR, Moore LW, Kraus AJ. Nutritional effects of peritonitis in continuous ambulatory peritoneal dialysis (CAPD) patients. Journal of the American Dietetic Association. 1987;87:53-6. Reference ID: 9993 3. Beutler KT, Park GK, Wilkowski MJ. Effect of oral supplementation on nutrition indicators in hemodialysis patients. Journal of Renal Nutrition. 1997;7:77 Reference ID: 12 75 APPENDIX D: BIBLIOGRAPHY OF ACCEPTED ARTICLES (CONTINUED) 4. Cano N, Labastie-Coeyrehourq J, Lacombe P, et al. Perdialytic parenteral nutrition with lipids and amino acids in malnourished hemodialysis patients. American Journal of Clinical Nutrition. 1990;52:726-30. Reference ID: 7159 5. Capelli JP, Kushner H, Camiscioli TC, Chen SM, Torres MA. Effect of intradialytic parenteral nutrition on mortality rates in end-stage renal disease care [see comments]. American Journal of Kidney Diseases. 1994;23:808-16. Reference ID: 3712 6. Chertow GM, Ling J, Lew NL, Lazarus JM, Lowrie EG. The association of intradialytic parenteral nutrition administration with survival in hemodialysis patients. American Journal of Kidney Diseases. 1994;24:912-20. Reference ID: 3345 7. Hecking E, Kohler H, Zobel R, et al. Is parenteral or oral administration of essential amino acids beneficial in patients on chronic haemodialysis?. Proceedings of the European Dialysis & Transplant Association. 1977;14:577-80. Reference ID: 15171 8. Hecking E, Kohler H, Zobel R, et al. Treatment with essential amino acids in patients on chronic hemodialysis: a double blind cross-over study. American Journal of Clinical Nutrition. 1978;31:1821-6. Reference ID: 14429 9. Kluthe R, Luttgen FM, Capetianu T, Heinze V, Katz N, Sudhoff A. Protein requirements in maintenance hemodialysis. American Journal of Clinical Nutrition. 1978;31:1812-20. Reference ID: 14431 10. Maurer O, Saxenhofer H, Jaeger P, Casez JP, Descoeudres C, Horber FF. Six-month overnight administration of intraperitoneal amino acids does not improve lean mass. Clinical Nephrology. 1996;45:303-9. Reference ID: 1560 11. Misra M, Ashworth J, Reaveley DA, Muller B, Brown EA. Nutritional effects of amino acid dialysate (Nutrineal) in CAPD patients. Advances in Peritoneal Dialysis. 1996;12:311-4. Reference ID: 1368 12. Neuhauser M, Ulm A, Leber HW, Schutterle G. Influence of essential amino acids and keto acids on protein metabolism and the anaemia of patients on chronic intermittent haemodialysis. Proceedings of the European Dialysis & Transplant Association. 1977;14:557-62. Reference ID: 15176 76 APPENDIX D: BIBLIOGRAPHY OF ACCEPTED ARTICLES (CONTINUED) 13. Rubin J. Nutritional support during peritoneal dialysis-related peritonitis. American Journal of Kidney Diseases. 1990;15:551-5. Reference ID: 6964 14. Stewart J, Schvaneveldt NB, Christensen NK, Lauritzen GC, Stein DM. The effect of computerized dietary analysis nutrition education on nutrition knowledge, nutrition status, dietary compliance, and quality of life of hemodialysis patients. Journal of Renal Nutrition. 1993;3:177 Reference ID: 10 15. Tietze IN, Pedersen EB. Effect of fish protein supplementation on aminoacid profile and nutritional status in haemodialysis patients. Nephrology, Dialysis, Transplantation. 1991;6:948-54. Reference ID: 6546 16. Toigo G, Situlin R, Tamaro G, et al. Effect of intravenous supplementation of a new essential amino acid formulation in hemodialysis patients. Kidney International Supplement. 1989;27:S278-S281 Reference ID: 7976 17. Ulm A, Neuhauser M, Leber HW. Influence of essential amino acids and keto acids on protein metabolism and anemia of patients on intermittent hemodialysis. American Journal of Clinical Nutrition. 1978;31:1827-30. Reference ID: 14418 18. Wiser NA, Shane JM, McGuigan AT, Memken JA, Olsson PJ. The effects of a group nutrition education program on nutrition knowledge, nutrition status, and quality of life in hemodialysis patients. Journal of Renal Nutrition. 1997;7:187-93. Reference ID: 1 Question 8 - adults 1. Blackburn SL. Dietary compliance of chronic hemodialysis patients. Journal of the American Dietetic Association. 1977;70:31-7. Reference ID: 15003 2. De Lima J, Sesso R, Abensur H, et al. Predictors of mortality in long-term haemodialysis patients with a low prevalence of comorbid conditions. Nephrology, Dialysis, Transplantation. 1995;10:1708-13. Reference ID: 2455 77 APPENDIX D: BIBLIOGRAPHY OF ACCEPTED ARTICLES (CONTINUED) 3. Ifudu O, Dulin AL, Friedman EA. Interdialytic weight gain correlates with glycosylated hemoglobin in diabetic hemodialysis patients. American Journal of Kidney Diseases. 1994;23:686-91. Reference ID: 3643 4. Manley M, Sweeney J. Assessment of compliance in hemodialysis adaptation. Journal of Psychosomatic Research. 1986;30:153-61. Reference ID: 10639 5. Procci WR. Dietary abuse in maintenance hemodialysis patients. Psychosomatics. 1978;19:16-24. Reference ID: 14799 6. Ruggiero L, Brantley PJ, Bruce BK, McKnight GT, Cocke TB. The role of dietary compliance in survival of hemodialysis patients. Dialysis Transplant. 1992;21:14-7. Reference ID: 4885 7. Safdar N, Baakza H, Kumar H, Naqvi SA. Non-compliance to diet and fluid restrictions in haemodialysis patients. JPMA - Journal of the Pakistan Medical Association. 1995;45:293-5. Reference ID: 2254 8. Schmicker R, Baumbach A. Dietary compliance in hemodialysis patients. Contributions to Nephrology. 1990;81:115-23. Reference ID: 7471 9. Sensky T, Leger C, Gilmour S. Psychosocial and cognitive factors associated with adherence to dietary and fluid restriction regimens by people on chronic haemodialysis. Psychotherapy & Psychosomatics. 1996;65:36-42. Reference ID: 1996 10. Sherman RA, Cody RP, Rogers ME, Solanchick JC. Interdialytic weight gain and nutritional parameters in chronic hemodialysis patients. American Journal of Kidney Diseases. 1995;25:579-83. Reference ID: 2406 11. Teraoka S, Toma H, Nihei H, et al. Current status of renal replacement therapy in Japan. American Journal of Kidney Diseases. 95 A.D.;25:151-64. Reference ID: 18837 12. Yanitski AE. Compliance of the hemodialysis patient. AANNT Journal. 1983;10:11-6. Reference ID: 12140 Question 9 – adults 78 APPENDIX D: BIBLIOGRAPHY OF ACCEPTED ARTICLES (CONTINUED) None selected Question 10 – adults None selected Questions 11, 12 – adults 1. Ahmad S, Robertson HT, Golper TA, et al. Multicenter trial of L-carnitine in maintenance hemodialysis patients. II. Clinical and biochemical effects. Kidney International. 1990;38:912-8. Reference ID: 51 2. Albertazzi A, Spisni C, Del Rosso G, Palmieri PF, Rossini PM. Electromyographic changes induced by oral carnitine treatment in dialysis patients. Proceedings of the Clinical Dialysis & Transplant Forum. 1980;10:1-6. Reference ID: 154 3. Albertazzi A, Capelli P, Di Paola B, Pola P, Tondi P, Vaccario O. Endocrine-metabolic effects of l-carnitine in patients on regular dialysis treatment. Proceedings of the European Dialysis & Transplant Association. 1983;19:302-7. Reference ID: 130 4. Bellinghieri G, Savica V, Mallamace A, et al. Correlation between increased serum and tissue L-carnitine levels and improved muscle symptoms in hemodialyzed patients. American Journal of Clinical Nutrition. 1983;38:523-31. Reference ID: 118 5. Bellinghieri G, Savica V, Barbera CM, et al. L-carnitine and platelet aggregation in uremic patients subjected to hemodialysis. Nephron. 1990;55:28-32. Reference ID: 55 6. Caruso U, Cravotto E, Tisone G. Long-term treatment with L-carnitine in uremic patients undergoing chronic hemodialysis: Effects on the lipid pattern. Current Therapeutic Research, Clinical & Experimental. 1983;33:1098-104. Reference ID: 435 7. Caruso U, Leone L, Cravotto E, Nava D. Effects of L-carnitine on anemia in aged hemodialysis patients treated with recombinant human erythropoietin: a pilot study. Dialysis & Transplantation. 1998;27:498-506. Reference ID: 671 79 APPENDIX D: BIBLIOGRAPHY OF ACCEPTED ARTICLES (CONTINUED) 8. Casciani CU, Caruso U, Cravotto E, et al. L-carnitine in haemodialysed patients. Changes in lipid pattern. Arzneimittel-Forschung. 1982;32:293-7. Reference ID: 139 9. Casciani CU, Caruso U, Cravotto E. Beneficial effects of L-carnitine in post dialysis syndrome. Current Therapeutic Research, Clinical & Experimental. 1982;32:116-27. Reference ID: 439 10. Dionisio P, Bergia R, Caramello E, et al. [Effects of long-term treatment with L-carnitine on dyslipemia in hemodialysis patients]. [Italian]. Minerva Medica. 1985;76:229-34. Reference ID: 108 11. Donatelli M, Terrizzi C, Zummo G, Russo V, Bucalo ML, Scarpinato A. Effects of Lcarnitine on chronic anemia and erythrocyte adenosine triphosphate concentration in hemodialyzed patients. Curr Ther Res. 1987;41:620-4. Reference ID: 467 12. Fagher B, Cederblad G, Monti M, Olsson L, Rasmussen B, Thysell H. Carnitine and left ventricular function in haemodialysis patients. Scandinavian Journal of Clinical & Laboratory Investigation. 1985;45:193-8. Reference ID: 106 13. Fagher B, Cederblad G, Eriksson M, et al. L-carnitine and haemodialysis: double blind study on muscle function and metabolism and peripheral nerve function. Scandinavian Journal of Clinical & Laboratory Investigation. 1985;45:169-78. Reference ID: 110 14. Fujita Y, Shinzato T, Takai I, Kobayakawa H, Ozawa Y, Maeda K. Efficacy of L-carnitine administration for long-term dialysis patients with continuous hypotension. [Japanese]. Japanese Journal of Artificial Organs. 1988;17:132-5. Reference ID: 478 15. Galeone F, Giacomelli A, Rossi A, Giuntoli F, Micheli C, Saba P. L-carnitine activity on serum lipid patterns in chronic uraemia. A study of patients on dialysis. Clin Trials J. 1987;24:417-24. Reference ID: 484 16. Golper TA, Wolfson M, Ahmad S, et al. Multicenter trial of L-carnitine in maintenance hemodialysis patients. I. Carnitine concentrations and lipid effects. Kidney International. 1990;38:904-11. Reference ID: 50 80 APPENDIX D: BIBLIOGRAPHY OF ACCEPTED ARTICLES (CONTINUED) 17. Guarnieri G, Toigo G, Crapesi L, et al. Metabolic effects of supplementation of L-carnitine in the dialysate of patients treated with acetate hemodialysis. Kidney International Supplement. 1989;36, Suppl 27:S247-S255 Reference ID: 59 18. Guarnieri G, Fonda M, Situlin R, Vasile A, Toigo G, Cattin L. Effects of L-carnitine supplementation in the dialysate on serum lipoprotein composition of hemodialysis patients. Contributions to Nephrology. 1992;98:36-43. Reference ID: 41 19. Guarnieri GF, Ranieri F, Toigo G, et al. Lipid-lowering effect of carnitine in chronically uremic patients treated with maintenance hemodialysis. American Journal of Clinical Nutrition. 1980;33:1489-92. Reference ID: 152 20. Huissoon AP, Meehan S, Brian KJ. Carnitine replacement and maintenance by addition of L-carnitine to dialysis fluid. Journal of Nephrology. 1993;6:103-7. Reference ID: 511 21. Labonia WD, Morelli OJ, Gimenez MI, Freuler PV, Morelli OH. Effects of L-carnitine on sodium transport in erythrocytes from dialyzed uremic patients. Kidney International. 1987;32:754-9. Reference ID: 88 22. Labonia WD. L-carnitine effects on anemia in hemodialyzed patients treated with erythropoietin. American Journal of Kidney Diseases. 1995;26:757-64. Reference ID: 18 23. Lundholm K, Persson H, Wennberg A. Whole body fat oxidation before and after carnitine supplementation in uremic patients on chronic haemodialysis. Clinical Physiology. 1988;8:417-26. Reference ID: 78 24. Maeda K, Shinzato T, Kobayakawa H. Effects of L-carnitine administration on short-chain fatty acid (acetic acid) and long-chain fatty acid metabolism during hemodialysis. Nephron. 1989;51:355-61. Reference ID: 69 25. Mayer G, Graf H, Legenstein E, Linhart L, Auer B, Lohninger A. L-carnitine substitution in patients on chronic hemodialysis. Nephron. 1989;52:295-9. Reference ID: 70 81 APPENDIX D: BIBLIOGRAPHY OF ACCEPTED ARTICLES (CONTINUED) 26. Mioli V, Tarchini R, Boggi R. Use of D,L- and L-carnitine in uraemic patients on intermittent haemodialysis. International Journal of Clinical Pharmacology Research. 1982;2:143-8. Reference ID: 555 27. Nilsson-Ehle P, Cederblad G, Fagher B, Monti M, Thysell H. Plasma lipoproteins, liver function and glucose metabolism in haemodialysis patients: lack of effect of L-carnitine supplementation. Scandinavian Journal of Clinical & Laboratory Investigation. 1985;45:179-84. Reference ID: 109 28. Rogerson ME, Rylance PB, Wilson R, et al. Carnitine and weakness in haemodialysis patients. Nephrology, Dialysis, Transplantation. 1989;4:366-71. Reference ID: 68 29. Siami G, Clinton ME, Mrak R, Griffis J, Stone W. Evaluation of the effect of intravenous L-carnitine therapy on function, structure and fatty acid metabolism of skeletal muscle in patients receiving chronic hemodialysis. Nephron. 1991;57:306-13. Reference ID: 47 30. Sohn HJ, Choi GB, Yoon KI. [L-Carnitine in maintenance hemodialysis clinical, lipid and biochemical effects]. Kor J Nephrol. 1992;11:260-9. Reference ID: 603 31. Spagnoli LG, Palmieri G, Mauriello A, et al. Morphometric evidence of the trophic effect of L-carnitine on human skeletal muscle. Nephron. 1990;55:16-23. Reference ID: 56 32. Srivastava DK, Kumar S, Misra AP. Reversal of haemodialysis induced hypertriacylglycerolemia by L-carnitine. Indian Journal of Clinical Biochemistry. 1992;7:19-21. Reference ID: 296 33. Thompson CH, Irish AB, Kemp GJ, Taylor DJ, Radda GK. The effect of propionyl Lcarnitine on skeletal muscle metabolism in renal failure. Clinical Nephrology. 1997;47:3728. Reference ID: 3 34. Trivelli G, Vitali P, Girmenia S, Castelli F. Treatment of serum lipid abnormalities in hemodialysed patients with carnitine [Trattamento della dislipidemia dell'emodializzato con l-carnitina]. Clin.Eur. 1983;22:405-15. Reference ID: 612 82 APPENDIX D: BIBLIOGRAPHY OF ACCEPTED ARTICLES (CONTINUED) 35. Trovato GM, Ginardi V, Di Marco V, Dell'Aira AE, Corsi M. Long term L-carnitine treatment of chronic anaemia of patients with end stage renal failure. Curr Ther Res. 1982;31:1042-9. Reference ID: 614 36. Vacha GM, Giorcelli G, Siliprandi N, Corsi M. Favorable effects of L-carnitine treatment on hypertriglyceridemia in hemodialysis patients: decisive role of low levels of high-density lipoprotein-cholesterol. American Journal of Clinical Nutrition. 1983;38:532-40. Reference ID: 119 37. Vacha GM, Giorcelli G, D'Iddio S, et al. L-carnitine addition to dialysis fluid. A therapeutic alternative for hemodialysis patients. Nephron. 1989;51:237-42. Reference ID: 71 38. van Es A, Henny FC, Kooistra MP, Lobatto S, Scholte HR. Amelioration of cardiac function by L-carnitine administration in patients on haemodialysis. Contributions to Nephrology. 1992;98:28-35. Reference ID: 42 39. Wanner C, Forstner-Wanner S, Schaeffer G, Schollmeyer P, Horl WH. Serum free carnitine, carnitine esters and lipids in patients on peritoneal dialysis and hemodialysis. American Journal of Nephrology. 1986;6:206-11. Reference ID: 102 40. Wanner C, Wieland H, Wackerle B, Boeckle H, Schollmeyer P, Horl WH. Ketogenic and antiketogenic effects of L-carnitine in hemodialysis patients. Kidney International Supplement. 1989;27:S264-S268 Reference ID: 61 41. Wanner C, Wieland H, Nauck M, Schaeffer G, Schollmeyer P, Horl WH. Effective hypolipidaemic therapy with beclobrate in haemodialysis patients: Interference with Lcarnitine. Nephrol.Dial.Transplant. 1990;5:588-93. Reference ID: 243 42. Weschler A, Aviram M, Levin M, Better OS, Brook JG. High dose of L-carnitine increases platelet aggregation and plasma triglyceride levels in uremic patients on hemodialysis. Nephron. 1984;38:120-4. Reference ID: 116 43. Yderstraede KB, Pedersen FB, Dragsholt C, Trostmann A, Laier E, Larsen HF. The effect of L-carnitine on lipid metabolism in patients on chronic haemodialysis. Nephrology, Dialysis, Transplantation. 1987;1:238-41. Reference ID: 94 83 APPENDIX D: BIBLIOGRAPHY OF ACCEPTED ARTICLES (CONTINUED) 44. Zilleruelo G, Novak M, Hsia SL, et al. Effect of dialysate composition on the lipid response to L-carnitine supplementation. Kidney International - Supplement. 1989;27:S259-S263 Reference ID: 62 84 APPENDIX D: BIBLIOGRAPHY OF ACCEPTED ARTICLES (CONTINUED) References for Pediatric Sections Question 1 - pediatrics A-Peds 1. Chan JC. Late complications of long-term hemodialysis in children: clinical aspects and some measurable variables concerning parathyroid hormone, divalent ions, acid-base metabolism, anemia, nutrition, growth and survival data. Journal of Urology. 1978;120:578-85. Reference ID: 14484 IGF-Peds 1. Besbas N, Ozdemir S, Saatci U, et al. Nutritional assessment of children on haemodialysis: value of IGF-I, TNF-alpha and IL-1beta. Nephrol Dial Transplant. 1998;13:1484-8. Reference ID: 7719 (also in B section) 2. Hodson EM, Brown AS, Roy LP, Rosenberg AR. Insulin-like growth factor-1, growth hormone-dependent insulin-like growth factor-binding protein and growth in children with chronic renal failure. Pediatr Nephrol. 1992;6:433-8. Reference ID: 23 3. Jasper HG, Ferraris JR. Insulin-like growth factor I (IGF-I) and growth in children undergoing hemodialysis or after successful renal transplantation. Medicina (B Aires). 1991;51:127-32. Reference ID: 30 Question 2 - pediatrics 1. Besbas N, Ozdemir S, Saatci U, et al. Nutritional assessment of children on haemodialysis: value of IGF-I, TNF-alpha and IL-1beta. Nephrol Dial Transplant. 1998;13:1484-8. Reference ID: 7719 (also in IGF section) 2. Cochat P, Braillon P, Feber J, et al. Body composition in children with renal disease: use of dual energy X-ray absorptiometry. Pediatric Nephrology. 1996;10:264-8. Reference ID: 1666 3. Stefanidis C, Siapera D, Papadopoulou A, Michelis K. Body composition of children on CAPD. Peritoneal Dialysis International. 1996;16 Suppl 1:S561-S566 Reference ID: 1944 * Reference ID numbers correspond with those listed in the evidence tables. 85 APPENDIX D: BIBLIOGRAPHY OF ACCEPTED ARTICLES (CONTINUED) Question 3 – pediatrics None selected Question 4 - pediatrics 1. Fischbach M, Terzic J, Lahlou A, et al. Nutritional effects of KT/V in children on peritoneal dialysis: are there benefits from larger dialysis doses? Advances in Peritoneal Dialysis. 1995;11:306-8. Reference ID: 28 2. Kleinknecht C, Broyer M, Gagnadoux MF, et al. Growth in children treated with long-term dialysis. A study of 76 patients. Adv Nephrol Necker Hosp. 1980;9:133-63:133-63. Reference ID: 132 3. Canepa A, Divino FC, Forsberg AM, et al. Children on continuous ambulatorial peritoneal dialysis: muscle and plasma proteins, amino acids and nutritional status. Clinical Nephrology. 1996;46:125-31. Reference ID: 1311 4. Salusky IB, Fine RN, Nelson P. Nutritional status of children undergoing continuous ambulatory peritoneal dialysis. Am.J.Clin.Nutr. 1983;38:599-611. Reference ID: 4965 5. Kohaut EC. Growth in children treated with continuous ambulatory peritoneal dialysis. Int.J.Pediatr.Nephrol. 1983;4:93-8. Reference ID: 4966 6. Chan JCM. Late complications of long-term hemodialysis in children: Clinical aspects and some measurable variables concerning parathyroid hormone, divalent ions, acid-base metabolism, anemia, nutrition, growth and survival data. J.Urol. 1978;120:578-85. Reference ID: 4997 7. Zadik Z, Frishberg Y, Drukker A, et al. Excessive dietary protein and suboptimal caloric intake have a negative effect on the growth of children with chronic renal disease before and during growth hormone therapy. Metabolism: Clinical and Experimental. 1998;47:264-8. Reference ID: 5041 8. Honda M, Kamiyama Y, Kawamura K, et al. Growth, development and nutritional status in Japanese children under 2 years on continuous ambulatory peritoneal dialysis. Pediatric Nephrology. 1995;9:543-8. Reference ID: 5143 86 APPENDIX D: BIBLIOGRAPHY OF ACCEPTED ARTICLES (CONTINUED) 9. Querfeld U, Salusky IB, Nelson P, Foley J, Fine RN. Hyperlipidemia in pediatric patients undergoing peritoneal dialysis. Pediatric Nephrology. 1988;2:447-52. Reference ID: 8807 10. Macdonald A. The practical problems of nutritional support for children on continuous ambulatory peritoneal dialysis. Human Nutrition - Applied Nutrition. 1986;40:253-61. Reference ID: 10271 11. Broyer M, Niaudet P, Champion G, Jean G, Chopin N, Czernichow P. Nutritional and metabolic studies in children on continuous ambulatory peritoneal dialysis. Kidney International - Supplement. 1983;15:S106-S110 Reference ID: 11953 12. Broyer M, Kleinknecht C, Loirat C, Marti-Henneberg C, Roy MP. Growth in children treated with long-term hemodialysis. Journal of Pediatrics. 1974;84:642-9. Reference ID: 16260 Question 5 - pediatrics 1. Claris-Appiani A, Ardissino GL, Dacco V, Funari C, Terzi F. Catch-up growth in children with chronic renal failure treated with long-term enteral nutrition. Jpen: Journal of Parenteral & Enteral Nutrition. 1995;19:175-8. Reference ID: 2282 2. Uauy RD, Hogg RJ, Brewer ED, Reisch JS, Cunningham C, Holliday MA. Dietary protein and growth in infants with chronic renal insufficiency: a report from the Southwest Pediatric Nephrology Study Group and the University of California, San Francisco. Pediatric Nephrology. 1994;8:45-50. Reference ID: 3871 3. Ratsch IM, Catassi C, Verrina E, et al. Energy and nutrient intake of patients with mild-tomoderate chronic renal failure compared with healthy children: an Italian multicentre study. European Journal of Pediatrics. 1992;151:701-5. Reference ID: 5007 4. Zadik Z, Frishberg Y, Drukker A, et al. Excessive dietary protein and suboptimal caloric intake have a negative effect on the growth of children with chronic renal disease before and during growth hormone therapy. Metabolism: Clinical and Experimental. 1998;47:264-8. Reference ID: 5041 87 APPENDIX D: BIBLIOGRAPHY OF ACCEPTED ARTICLES (CONTINUED) 5. Wingen AM, Fabian-Bach C, Mehls O. Multicentre randomized study on the effect of a low-protein diet on the progression of renal failure in childhood: one-year results. European Study Group for Nutritional Treatment of Chronic Renal Failure in Childhood. Mineral & Electrolyte Metabolism. 1992;18:303-8. Reference ID: 5510 6. Abitbol CL, Warady BA, Massie MD, et al. Linear growth and anthropometric and nutritional measurements in children with mild to moderate renal insufficiency: a report of the Growth Failure in Children with Renal Diseases Study. Journal of Pediatrics. 1990;116:S46-S54 Reference ID: 7784 7. Rizzoni G, Basso T, Setari M. Growth in children with chronic renal failure on conservative treatment. Kidney International. 1984;26:52-8. Reference ID: 11503 8. Betts PR, Magrath G. Growth pattern and dietary intake of children with chronic renal insufficiency. British Medical Journal. 1974;2:189-93. Reference ID: 16464 9. Ruley EJ, Bock GH, Kerzner B, Abbott AW, Majd M, Chatoor I. Feeding disorders and gastroesophageal reflux in infants with chronic renal failure. Pediatr Nephrol. 1989;3:424-9. Reference ID: 16465 10. Kist-van Holthe tEJ, Nauta J, Hop WC, et al. Protein restriction in chronic renal failure. Arch.Dis Child. 1993;68:371-5. Reference ID: 16466 11. Arnold WC, Danford D, Holliday MA. Effects of caloric supplementation on growth in children with uremia. Kidney Int. 1983;24:205-9. Reference ID: 16467 12. Betts PR, Magrath G, White RH. Role of dietary energy supplementation in growth of children with chronic renal insufficiency. Br.Med J. 1977;1:416-8. Reference ID: 16468 Question 6 – pediatrics None Selected Question 7 - pediatrics 88 APPENDIX D: BIBLIOGRAPHY OF ACCEPTED ARTICLES (CONTINUED) 1. Balfe JW, Secker DJ, Coulter PE, Balfe JA, Geary DF. Tube feeding in children on chronic peritoneal dialysis. Adv Perit.Dial. 1990;6:257-61:257-61. Reference ID: 17651 2. Brewer ED. Growth of small children managed with chronic peritoneal dialysis and nasogastric tube feedings: 203-month experience in 14 patients. Advances in Peritoneal Dialysis. 1990;6:269-72. Reference ID: 7039 3. Canepa A, Perfumo F, Carrea A, et al. Long-term effect of amino-acid dialysis solution in children on continuous ambulatory peritoneal dialysis. Pediatric Nephrology. 1991;5:2159. Reference ID: 6682 4. Coleman JE, Watson AR. Micronutrient supplementation in children on continuous cycling peritoneal dialysis (CCPD). Advances in Peritoneal Dialysis. 1992;8:396-401. Reference ID: 5068 5. Coleman JE, Watson AR, Rance CH, Moore E. Gastrostomy buttons for nutritional support on chronic dialysis. Nephrol Dial Transplant. 1998;13:2041-6. Reference ID: 17648 6. Dabbagh S, Fassinger N, Clement K, Fleischmann LE. The effect of aggressive nutrition on infection rates in patients maintained on peritoneal dialysis. Advances in Peritoneal Dialysis. 1991;7:161-4. Reference ID: 6044 7. Dello SL, Principato F, Sinibaldi D, et al. Feeding dysfunction in infants with severe chronic renal failure after long-term nasogastric tube feeding. Pediatr Nephrol. 1997;11:84-6. Reference ID: 17650 8. Hanning RM, Balfe JW, Zlotkin SH. Effectiveness and nutritional consequences of amino acid-based vs glucose-based dialysis solutions in infants and children receiving CAPD. American Journal of Clinical Nutrition. 1987;46:22-30. Reference ID: 9639 9. Kaiser BA, Polinsky MS, Stover J, Morgenstern BZ, Baluarte HJ. Growth of children following the initiation of dialysis: a comparison of three dialysis modalities. Pediatric Nephrology. 1994;8:733-8. Reference ID: 4 10. Warady BA, Weis L, Johnson L. Nasogastric tube feeding in infants on peritoneal dialysis. Perit.Dial Int. 1996;16 Suppl 1:S521-5:S521-S525 Reference ID: 17649 89 APPENDIX D: BIBLIOGRAPHY OF ACCEPTED ARTICLES (CONTINUED) 11. Zachwieja J, Duran M, Joles JA, et al. Amino acid and carnitine supplementation in haemodialysed children. Pediatric Nephrology. 1994;8:739-43. Reference ID: 3385 Question 8 – pediatrics None Selected Question 13 – pediatrics 1. Berard E, Crosnier H, Six-Beneton A, Chevallier T, Cochat P, Broyer M. Recombinant human growth hormone treatment of children on hemodialysis. French Society of Pediatric Nephrology. Pediatr Nephrol. 1998;12:304-10. Reference ID: 18823 2. Fine RN, Koch VH, Boechat MI, et al. Recombinant human growth hormone (rhGH) treatment of children undergoing peritoneal dialysis. Peritoneal Dialysis International. 1990;10:209-14. Reference ID: 7590 3. Greco M, Cappa M, Perruzza I, Rizzoni G. Can provocative growth hormone testing predict the response to recombinant human growth hormone (rhGH) treatment?. British Journal of Clinical Practice.Supplement. 1996;85:38-40. Reference ID: 977 4. Hokken-Koelega AC, Stijnen T, de MS, et al. Placebo-controlled, double-blind, cross-over trial of growth hormone treatment in prepubertal children with chronic renal failure. Lancet. 1991;338:585-90. Reference ID: 5933 5. Laron Z, Wang XL, Klinger B, et al. Growth hormone treatment increases circulating lipoprotein(a) in children with chronic renal failure. J Pediatr Endocrinol.Metab. 1996;9:533-7. Reference ID: 10 6. Lippe B, Yadin O, Fine RN, Moulton L, Nelson PA. Use of recombinant human growth hormone in children with chronic renal insufficiency: an update. Hormone Research. 1993;40:102-8. Reference ID: 4470 90 APPENDIX D: BIBLIOGRAPHY OF ACCEPTED ARTICLES (CONTINUED) 7. Schaefer F, Wuhl E, Haffner D, Mehls O. Stimulation of growth by recombinant human growth hormone in children undergoing peritoneal or hemodialysis treatment. German Study Group for Growth Hormone Treatment in Chronic Renal Failure. Advances in Peritoneal Dialysis. 1994;10:321-6. Reference ID: 3451 8. Schwartz ID, Warady BA, Buchanan CL, et al. "Low-dose" growth hormone therapy during peritoneal dialysis or following renal transplantation. Pediatric Nephrology. 1995;9:320-4. Reference ID: 2634 9. Tonshoff B, Mehis O, Heinrich U, Blum WF, Ranke MB, Schauer A. Growth-stimulating effects of recombinant human growth hormone in children with end-stage renal disease. Journal of Pediatrics. 1990;116:561-6. Reference ID: 7841 10. Tonshoff B, Dietz M, Haffner D, Tonshoff C, Stover B, Mehls O. Effects of two years of growth hormone treatment in short children with renal disease. The German Study Group for Growth Hormone Treatment in Chronic Renal Failure. Acta Paediatrica Scandinavica Supplement. 1991;379:33-41. Reference ID: 6449 11. Vaisman N, Zadik Z, Duchan R, Voet H, Lotan D, Drukker A. Changes in body composition of children with chronic renal failure during growth hormone treatment. Pediatric Nephrology. 1994;8:201-4. Reference ID: 3946 12. Wuhl E, Haffner D, Tonshoff B, Mehls O. Predictors of growth response to rhGH in short children before and after renal transplantation. German Study Group for Growth Hormone Treatment in Chronic Renal Failure. Kidney International - Supplement. 1993;43:S76-S82 Reference ID: 4182 13. Wuhl E, Haffner D, Nissel R, Schaefer F, Mehls O. Short dialyzed children respond less to growth hormone than patients prior to dialysis. German Study Group for Growth Hormone Treatment in Chronic Renal Failure. Pediatric Nephrology. 1996;10:294-8. Reference ID: 1671 14. Zadik Z, Frishberg Y, Drukker A, et al. Excessive dietary protein and suboptimal caloric intake have a negative effect on the growth of children with chronic renal disease before and during growth hormone therapy. Metabolism. 1998;47:264-8. Reference ID: 18821 Question 14 – pediatrics 91 APPENDIX D: BIBLIOGRAPHY OF ACCEPTED ARTICLES (CONTINUED) 1. Kriley M, Warady BA. Vitamin status of pediatric patients receiving long-term peritoneal dialysis. Am J Clin Nutr. 1991;53:1476-9. Reference ID: 47 2. Warady BA, Kriley M, Alon U, Hellerstein S. Vitamin status of infants receiving long-term peritoneal dialysis. Pediatr Nephrol. 1994;8:354-6. Reference ID: 27 3. Zlotkin SH, Rundle MA, Hanning RM, Buchanan BE, Balfe JW. Zinc absorption from glucose and amino acid dialysis solutions in children on continuous ambulatory peritoneal dialysis (CAPD). J Am Coll.Nutr. 1987;6:345-50. Reference ID: 176 92 A PPENDIX E: ABSTRACTION F O R M S NKF Prognostic Article Abstract Form Date: ___________________ Reference ID Number: _________ First author’s last name: ________________________ Reviewer: MH SK SW ES TT GD Publication year: 19_____ Type of study: Case control / Prospective cohort / Retrospective cohort / Unsure -If not a prospective cohort and not a carnitine or pediatric acticle, StopStudy population and dialysis characteristics: Number of patients at start of study: ___________________ Years on dialysis: ________________ Age of patients: __________________ Type of dialysis: HD __________, CAPD ______________ Dialysate: _____________________ Membrane: ____________________, Reused? Y/N Dialysis schedule: __________ exchanges/day for CAPD, sessions/wk @ _________ hrs/session for HD _____________ For HD, vascular access: ____Temporary, _____Permanent Economic status: ________________________________________________ Race: _________________________________________________________ Residual renal function: ___________________________________________ 93 APPENDIX E: ABSTRACTION FORMS (CONTINUED) Top 3 co-morbid conditions: ________________________________________ _______________________________________________________________ Representative and well-defined sample of patients at a similar point in the course of disease? Y / N Follow-up time period: ____________________________________________ Outcome criteria objective and application of them unbiased? Y/N Adjustment for important known prognostic factors (see above)? Y/N Reported results (point estimate and confidence interval or p-value): Outcome: #1 #2 #3 ________ _________ ________ Prog factor 1: _____________________ ________ _________ ________ CI or p-value ________ _________ ________ Prog factor 2: _____________________ ________ _________ ________ CI or p-value ________ _________ ________ Prog factor 3: _____________________ ________ _________ ________ CI or p-value ________ _________ ________ Prog factor 4: _____________________ ________ _________ ________ CI or p-value _________ ________ ________ Comments: _______________________________________________________________ _______________________________________________________________ 94 APPENDIX E: ABSTRACTION FORMS (CONTINUED) NKF Diagnostic Article Abstract Form Date:__________________ Reference ID Number: _________ First author’s last name: ________________________ Reviewer: MH SK SW ES TT GD MP Publication year: 19_____ Type of study: Prospective / Retrospective / Unsure Study population and dialysis characteristics: Number of patients at start of study: ___________________ Years on dialysis: ________________ Age of patients: __________________ Type of dialysis: HD __________, CAPD ______________ Dialysate: _____________________ Membrane: ____________________, Reused? Y/N Dialysis schedule: __________ exchanges/day for CAPD, sessions/wk @ _________ hrs/session for HD _____________ Dose of dialysis (Kt/V): ____________________________________ For HD, vascular access: ____Temporary, _____Permanent Economic status: ________________________________________________ Race: _________________________________________________________ Residual renal function: ___________________________________________ 95 APPENDIX E: ABSTRACTION FORMS (CONTINUED) Top 3 co-morbid conditions: ________________________________________ Independent blind comparison with a reference (gold) standard? Y/N (If Yes, list reference standard: _______________________________________) --If No and not carnitine or pediatric article, Stop-- Did results of test influence decision to perform the reference standard? Y / N Spectrum of patients in study similar to spectrum seen in dialysis centers? Y / N Test methodology described well enough to be reproducible? Y/N Results (test characteristics): Test Sens Spec LR+ LR- No 1:___________________________ ____ ____ ____ ____ No 2:___________________________ ____ ____ ____ ____ No 3:___________________________ ____ ____ ____ ____ No 4:___________________________ ____ ____ ____ ____ No 5:___________________________ ____ ____ ____ ____ No 6:___________________________ ____ ____ ____ ____ Comments: _______________________________________________________________ _______________________________________________________________ 96 APPENDIX E: ABSTRACTION FORMS (CONTINUED) NKF Treatment Article Abstract Form Date: _______________________ Reference ID Number: _________ First author’s last name: ________________________ Reviewer: MH SK SW ES Publication year: 19_____ Type of study: Case control / RCT / Non-randomized clinical trial / Cross-over / Unsure -If not a clinical trial and not a carnitine or pediatric article, StopStudy population and dialysis characteristics: Number of patients at start of study: ___________________ Years on dialysis: ________________ Age of patients: __________________ Type of dialysis: HD __________, CAPD ______________ Dialysate: _____________________ Membrane: ____________________, Reused? Y/N Dialysis schedule: __________ exchanges/day for CAPD, sessions/wk @ _________ hrs/session for HD _____________ For HD, vascular access: ____Temporary, _____Permanent Economic status: ________________________________________________ Race: _________________________________________________________ Residual renal function: ___________________________________________ 97 APPENDIX E: ABSTRACTION FORMS (CONTINUED) Top 3 co-morbid conditions: ________________________________________ Jadad and Schulz score (see scoring guidelines): • Randomization score (0,1 or 2) _______ • Double blind score (0,1 or 2) _______ • All patients accounted for score (0 or 1) _______ Analyzed in treatment group to which assigned? Treatment groups similar at baseline? Y/N Y/N Treatment groups treated equally except for studied intervention? Y/N Treatments and sample size (Intention to treat and Per Protocol): Treatment/Control ITT PP Rx1=___________________________ _____ _____ Rx2=___________________________ _____ _____ Rx3=___________________________ _____ _____ Rx4=___________________________ _____ _____ Reported results (point estimate and confidence interval): Outcome/result: Rx1 Rx2 Rx3 Rx4 No. 1-ITT________________________ _____ _____ _____ _____ No. 1-PP________________________ _____ _____ _____ _____ No. 2-ITT________________________ _____ _____ _____ _____ No. 2-PP________________________ _____ _____ _____ _____ No. 3-ITT________________________ _____ _____ _____ _____ No. 3-PP________________________ _____ _____ _____ _____ 98 APPENDIX E: ABSTRACTION FORMS (CONTINUED) No. 4-ITT________________________ _____ _____ _____ _____ No. 4-PP________________________ _____ _____ _____ _____ No. 5-ITT________________________ _____ _____ _____ _____ No. 5-PP________________________ _____ _____ _____ _____ No. 6-ITT________________________ _____ _____ _____ _____ No. 6-PP________________________ _____ _____ _____ _____ No 1: ___________________ _____ _____ _____ _____ No 2: ___________________ _____ _____ _____ _____ No 3: ___________________ _____ _____ _____ _____ No 4: ___________________ _____ _____ _____ _____ Adverse effects: Comments: _______________________________________________________________ _______________________________________________________________ 99 A PPENDIX F: TREATMENT A RTICLE Q UALITY S CORE A L G O R I T H M 1. Was the study described as randomized? 2. Was the study described as double-blind? 3. Was there a description of withdrawals and drop-outs? Give a score of 1 point for each ‘Yes’ or 0 points for each ‘No’ Give 1 additional point each Deduct 1 point each If randomization/blinding appropriate If randomization/ blinding inappropriate Scoring Range: 0-5 Poor Quality < 3 Jadad et al. Controlled Clinical Trials 1996;17:1-12 100 APPENDIX F: TREATMENT ARTICLE QUALITY SCORE ALGORITHM (CONTINUED) GUIDELINES FOR ASSESSMENT: JADAD QUALITY SCALE 1. Randomization A method to generate the sequence of randomization will be regarded as appropriate if it allowed each study participant to have the same chance of receiving each intervention and the investigators could not predict which treatment was next. Methods of allocation using date of birth, date of admission, hospital numbers, or alternation should not be regarded as appropriate. 2. Double blinding A study must be regarded as double blind if the word “double blind” is used. The method will be regarded as appropriate if it is stated that neither the person doing the assessment nor the study participant could identify the intervention being assessed, or if in the absence of such a statement for use of active placebos, identical placebos, or dummies is mentioned. 3. Withdrawals and Dropouts Participants who were included in the study but did not complete the observation period or who were not included in the analysis must be described. The number and the reasons for withdrawals in each group must be stated. If there were no withdrawals, it should be stated in the article. If there is no statements or withdrawals, this item must be given no points. 101 A PPENDIX G: EVIDENCE T A B L E S abbreviation # ↑ ↓ ∆ µmol/l AA AC ADV AMC asymp. BA BIA-PA bicarb. BMI BSA BUN Bwt CAPD cf Cr CRF CPD d DEI DEXA DF dial. DPI EAA ESRD f/b FFM 4CM GH GT Gluc gm meaning number / count increased decreased change micro moles per liter Amino Acid (also see EAA, NEAA) Arm Circumference Antipyrine Distribution Volume Arm Muscle Circumference asymptomatic "Before and After" study (no concurrent controls) Bioimpedance Analysis-Phase Angle bicarbonate Body Mass Index Body Surface Area Blood Urea Nitrogen Body Weight Continuous Ambulatory Peritoneal Dialysis compared with Creatinine Chronic Renal Failure Chronic Peritoneal Dialysis days Dietary Energy Intake dual energy X-ray absorptiometry Discriminant Function dialysis Dietary Protein Intake Essential Amino Acid (also see AA, NEAA) End Stage Renal Disease followed by Fat Free Mass - Four Compartment Model Growth Hormone Gastrostomy Tube Glucose gram 102 A PPENDIX G: EVIDENCE TABLES (CONTINUED ) abbreviation HD HgB hr HPNI HV IBW IDPN IDWN IPD ITT IU IV IVNAA K (or K+) kg MAC MAMC min ml mo N N/A NEAA NGT nPCR nl NR NRCT NS NSD OR O/E pt(s) P PCR PCRn PD PDPN Phos meaning Hemodialysis Hemoglobin hour(s) Hemodialysis Prognostic Nutrition Index Height Velocity Ideal Body Weight Intradialytic Parenteral Nutrition Intradialytic Weight Gain Intermittent Peritoneal Dialysis Intention to treat analysis International Units intravenous in vivo neutron activation analysis Potassium kilogram Mid-arm circumference Mid-arm muscle circumference minutes milliliters month(s) sample size (or "No" depending on context) not applicable Non-essential Amino Acid (also see AA, EAA) Nasogastric Tube normalized Protein Catabolic Rate (see also PCR) normal Not Reported Non Randomized Clinical Trial not statistically significant no significant difference/change Odds Ratio Observed/Exepected patient(s) P-value (statistical significance) Protein Catabolic Rate (see also nPCR) see nPCR Peritoneal Dialysis Per Dialytic Parenteral Nutrition Phosphorus 103 A PPENDIX G: EVIDENCE TABLES (CONTINUED ) abbreviation PO PP qd q wk r RCT RDA RR Rx SDS SFT SGA SSF Stand Dev symp. sx TBK TBPr Technique Failure TSF TSFT TST URR vs w/ w/o wks Wt WI Y Z Score meaning by mouth Per-protocol analysis per day per week Regression Coefficient Randomized Controlled Clinical Trial Recommended Daily Allowance Relative Risk Treatment / Intervention Standard Deviation Score Skin Fold Thickness Subjective Global Assessment Subscapular skinfold Standard Deviation symptomatic symptoms Total Body Potassium Total Body Protein CAPD failed; required hemodialysis Triceps skinfold thickness (also see TST) see TSF, TST Triceps skinfold thickness (also see TSF) Urea Reduction Rate versus with without week(s) Weight Weight Index Yes Standard Deviation Score NB: data in italics not reported in study but inferred by abstractor 104