Using Genetics to Save Lives: a new paradigm for breast and services
advertisement
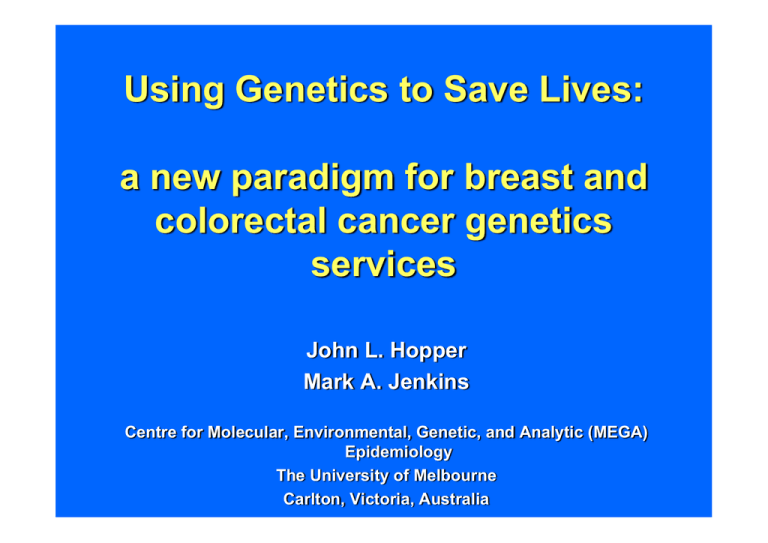
Using Genetics to Save Lives: a new paradigm for breast and colorectal cancer genetics services John L. Hopper Mark A. Jenkins Centre for Molecular, Environmental, Genetic, and Analytic (MEGA) Epidemiology The University of Melbourne Carlton, Victoria, Australia from tumour-type to genotype Australian Breast Cancer Family Study Population-based sampling - 1,600 Cases (Vic & NSW Cancer Registries) - 1,000 Controls (Government Electoral Rolls) Cases - unselected for family history - over-sampled for early onset (50% < age 40) Epidemiological data (by questionnaire) Genetic and molecular (blood, tissue) Funded by NHMRC, VicHealth, and since 1995, by NIH as part of Cancer Family Registries (see e.g. John, Hopper, et al., Br Cancer Res 2004) Australasian Colorectal Cancer Family Study Population-based sampling - 1,000 Cases (Vic Cancer Registries) - 800 Controls (Spouses and Government Electoral Rolls) Clinic-based families - selected for family history - 500 from across Australia & New Zealand Epidemiological data (by questionnaire) Genetic and molecular (blood, tissue) Funded by NHMRC, VicHealth, and since 1997, by NIH as part of Cancer Family Registries (see e.g. Newcombe et al., ) Summary of this talk • People vary greatly in disease risk • We know some genes for breast & bowel cancer • But why would you want to know? • How high are the risks? • What can you do about your risk? • How to best find carriers? • New paradigm - tumours tell the story • Change? Are all (wo)men really created equal? For most common diseases, people vary greatly in the familial component of their risk How do we know this? • The unaffected relatives of people with the disease are at increased risk of the disease A feature of most common diseases Increase risk typically on average about 2-fold Increased risk is associated with: • Closer relationship to affected(s) • Having more affected relatives • Younger age at diagnosis of affected relative(s) • Relatives with bilateral or multiple related diseases e.g. breast & ovarian cancer • Ethnicity e.g. Ashkenazi Jews & breast cancer Lifetime Risk Individual Risk 30 20 10 Population Risk 1 Q1 Median Q3 Familial Causes Breast cancer Most women Average = 11% Women with a strong family history/earlyonset disease Colorectal cancer 18 16 Relative Frequency 14 Unaffected people (population) (average risk = 5%) 12 10 Unaffected people with strong and/or early onset family history 8 6 4 2 0 0 8.05 0% 5% 0.2 20% 0.4 40% 0.6 60% 0.8 80% Lifetim e Risk 1001 % People in the highest 25% risk group are 20 times more likely to get CRC than the lowest 25% risk group 90% of the population are below the median risk Genetic risk • Very wide spectrum • Most at very low risk • Some at very high risk • What influences, or influenced, those at one end of the spectrum may differ from what influences the average! Known Breast Cancer Genes TP53 PTEN Relative Risk 10 BRCA1 Don’t exist! BRCA2 High-risk 2 BRIP1 PALB2 ATM CHEK2 Rare moderate risk Common low risk 1.5 FGFR2 TNRC9 5q 1.1 Too hard to find! 0.1% 1% 2q MAP3K1 8q LSP1 10% Minor allele frequency 30% CASP8 Known Colorectal Cancer Genes 100 MUTYH (biallelic) High-risk APC Don’t exist! Relative Risk MSH2 30 MSH6 MLH1 PSH2 Rare moderate risk 2 MUTHY (monoallelic) Common low risk MLH1 93 1.5 1.1 Too hard to find! 0.1% 1% 11q23 8q23 19q13 10% Minor allele frequency 16q22 30% 20p12 14q22 18q21 Contribution of known genes to explaining familial aggregation of breast cancer BRCA1 BRCA2 TP53 PTEN ATM CHEK2,BRIP1,PALB2 CASP8 8 WGA SNPs Other familial risk factors (genes, environment) Contribution of known genes to explaining familial aggregation of colorectal cancer MLH1 MSH2 PMS2 MSH6 MUTHY 8+ WGA SNPs Other familial risk factors (genes, environment) 䇾… quite contrary to the opinion I started with …䇿 • BRCA1 discovered in 1995 • We carried out extensive 䇾manual䇿 sequencing for ~90 early-onset cases: – half with a family history – half with no family history • Found 3 carriers: 1 with family history and 2 with no family history! • Family history was not related to the mutation!! BRCA2 2bp del 6503 (TT) 64 57 75 6 58 0 Breast(55) (+) 44 + 41 + 12 60 67 59 76 6 78 Breast(38) Bowel(58) Breast(62) ?Bowel(67) + 54 52 _ _ 50 + 41 38 _ Breast(38) + 12 12 10 8 3172 That was the 䇾outlier䇿 It does not represent a 䇾typical BRCA1/2 family䇿! BRCA1 1bp del 1876 (C) 81 70 75 88 ?Breast(42) 47 65 61 57 Prostate(65) 63 74 Breast(48) _ 38 40 73 53 69 ?Breast(53) 41 42 60 ?Larynx(60) 37 64 50 61 58 ?Lung(50) 34 Breast(38) + 3159 BRCA1 2bp del 3888 / BRCA2 1bp del 6174 (T) 53 86 50 _56 _ / 33 90 _61 /+ 31 69 3 64 29 Breast(33) +/+ 3104 Breast cancer diagnosed < age 40 • ~10% have mutation in BRCA1 or BRCA2 • 60% of carriers have no family history (first- & second degree) Majority of Hereditary Breast Cancer is Sporadic Hereditary: strong family history High-risk genes Familial: Sporadic: no family history No genes modest family history Low risk genes Hereditary: strong family history High-risk genes Familial: Sporadic: no family history No genes modest family history Low risk genes >2 affected 2 affected 1 affected Familial Sporadic 0 affected Breast Ca < 40 1 in 2 1 in 8 1 in 16 1 in 20 Hereditary <1% 5% 35% 60% Family history is NOT a good predictor of BRCA1 and BRCA2 mutations! Family history does better for MMR genes (at least when applied to early-onset colorectal cancers) but still not all that good Amsterdam II 1 in 5 10% 2 affected 1 in 10 15% 1 affected 1 in 15 50% 0 affected 1 in 100 25% Familial Sporadic CRC all ages Hereditary Amsterdam II 1 in 1.5 50% 2 affected 1 in 8 33% 1 affected 1 in 8 11% 0 affected 1 in 50 Familial Sporadic CRC < 45 Hereditary 6% Why would you want to know your genetic risk status? • Your disease risk is high • You can do something about it • Benefits outweigh the negatives How high are the risks? Clinic-based, population-based, and population estimates of penetrance from families • Penetrance: age-specific cumulative risk • Average, over the … mutations specific to sampled population & weighted by their observed frequency • Based on risks to carrier relatives • Therefore, influenced by the genetic and environmental background of the families Hopper et al., CEBP 1999 Average Cumulative risk of cancer Males Females 70 70 60 60 CRC for MLH1 or MSH2 BC for BRCA1 50 Cumulativerisk% CumulativeRisk% 50 40 30 20 30 CRC for MLH1 or MSH2 20 CRC for MSH6 CRC for PMS2 10 BC for BRCA2 40 0 CRC for MSH6 CRC for PMS2 10 0 30 40 50 60 70 Age(years) 30 40 50 60 70 Age(years) CRC for population BC for population CRC for population What can you do about your risk? … otherwise why would you want to know? Breast cancer • Mastectomy – 90% reduction in risk • Oophorectomy – 50% reduction • Chemoprevention, e.g. Tamoxifen – 50% reduction • Smoking - ? • OC use - ? • HRT use - ? Colorectal cancer • Annual colonoscopy & polypectomy > 65% reduction in risk • Weight reduction - ? 30% reduction (overweight to normal weight) • Smoking – 60% increased risk • OC and HRT use - ? • Exercise, aspirin, alcohol - ? How to best find carriers? • Family history is not all that good, especially for breast cancer, except if very strong • Affecteds are good place to start, especially if you can analyse their tumours • Age at onset is important LAMBDA Log Odds of Carrying an Ancestral Mutation in BRCA1 or BRCA2 for a Defined Personal and Family History in an Ashkenazi Jewish Woman • Studied Ashkenazi Jewish women from Australia & UK • Worked out what aspects of personal and family history best predicted carriers • Simplified the output to make a tool clinicians and women could use – without a computer • Validated using large North American studies Apicella et al., 2002, 2007; Lindor et al., 2006 LAMBDA score Age at diagnosis / Age if unaffected <40 Affected Self Breast Bilateral Ovarian First-degree Breast Ovarian Second-degree Breast Ovarian Not affected 40-49 50-59 3 1 3 2 1 3 1 1 3 1.5 1.5 1.0 1.5 0.5 1.5 0.5 1.0 0 1.0 0 1.0 -0.5 -1.0 -1.5 Sum scores Table Probability >2 affected 2 affected Familial Sporadic 1 affected 0 affected 1 in 2 1 in 8 1 in 16 1 in 20 Hereditary <1% 5% 35% 60% New paradigm for cancer genetic screening … tumours have tell-tale signs of their causes Amsterdam II 1 in 1.5 50% 2 affected 1 in 8 33% 1 affected 1 in 8 11% 0 affected 1 in 50 Familial Sporadic CRC < 45 Hereditary 6% Amsterdam II 1 in 1.5 50% 2 affected 1 in 8 33% 1 affected 1 in 8 11% 0 affected 1 in 50 Familial Sporadic CRC < 45 Hereditary 6% Victorian Colorectal Cancer Family Study • Population-based sample of 131 incident cases of primary adenocarcinoma of colon or rectum • Identified through Victorian Cancer Registry • < 45 years at diagnosis (1993-97) • • • Recruit first- & second-degree adult relatives Epidemiology and family history q䇻aires Blood and tumour samples sought Mismatch repair loss (e.g. MLH1) and carcinogenesis MLH1 MLH1 Germline or Somatic mutation Normal mismatch repair No mismatch MLH1 MLH1 If mismatch affects a gene in cancer pathway Somatic mutation Tumour with microsatellite instability (MSI) – a.k.a MSI-High and lacking MLH1 protein expression (immunohistochemistry) Immunohistochemistry measures mismatch repair deficiency phenotype Protein present in tumour Protein absent in tumour Family History Alone MSH2 MLH1 Amsterdam II PMS2 MSH6 MSI Testing Alone hMLH 1 hMSH2 hMSH6 MSI High MSI Low IHC Testing Alone MLH1 &/or PSM2 MSH2 MLH2 MLH1 MSH6 MSH6 only MSH2 Family History Alone hMLH1 hMSH2 Amsterdam II hMSH6 Family History Alone hMSH2 hMLH1 Amsterdam II hMSH6 MSI Testing Alone hMLH 1 hMSH2 hMSH6 MSI High MSI Low What if diagnosis after age 45? Figure 1b. Probability of carrier given MSI+ 1.00 0.90 0.80 0.88 0.76 0.75 Probability 0.70 0.78 0.60 0.50 0.40 0.40 0.30 0.20 0.10 0.09 0.00 0-34 35-39 40-44 45-49 Age at diagnosis group MSI+ = MSI at BAT26 50-54 55-59 Hampel et al. 2008 Supplementary data Figure 1b. Probability of carrier given MSI+ 1.00 0.90 0.80 Probability 0.70 0.67 0.60 0.50 0.44 0.40 0.30 0.28 0.20 0.10 0.07 0.04 0.00 0-40 40-49 50-59 60-69 70-79 Age at diagnosis group MSI+ = MSI-H or MSI-L 0.00 80+ Molecular screening of all tumours < 50, followed by genetic testing, will identify most carriers • ~80% of MSI-H cases will be carriers • Constitutes ~75% of all Lynch cases <60 • Extending to 50-59: triples molecular testing • Few carriers diagnosed after age 60 Early Onset Case Informed Consent Tumour Clinical management IHC MSI Future Cases Genetic counselling Mutation testing Cascade testing Carriers Non carriers Clinical surveillance Population surveillance Early Onset Case Informed Consent Tumour Clinical management IHC MSI Future Cases Genetic counselling Mutation testing Cascade testing Carriers Non carriers Clinical surveillance Population surveillance Could even increase efficiency even more using additional pathology features Pathologists Jass JR (McGill), Hayashi S (McGill), O’Shea A-M (Toronto), Burgart LJ (Mayo), Smyrk TC (Mayo), Shimizu D (Hawaii), Waring PM (PeterMac), Ruszkiewicz AR (Adelaide), Pollett AF (Ontario), Redston M (Harvard), Molecular biologists Thibodeau SN (Mayo), Barker MA (QIMR), Casey G (Clevlenad Clinic), Walsh MD (QIMR) Young JP (QIMR), Epidemiologists/statisticians Jenkins MA (UoM) Dowty JG (UoM), Baron JA (Dartmouth), Giles GG (Victorian Cancer Registry), Newcomb P (Fred Hutchinson) Principal investigators Lindor NM (Mayo), Haile RW (Uni Southern California), LeMarchand L (Uni Hawaii), Gallinger S (Mt.Sinai, Toronto), Potter JD (Fred Hutchnson), Hopper JL (UoM_ Population-based recruitment – Colon Cancer Family Registry (NIH) Seattle Ontario Mayo Hawaii Melbourne Pathology review Pathology review Pathology review Pathology review Pathology review MSI testing MSI testing MSI testing MSI testing MSI testing Colorectal tumors diagnosed before age 60 n = 1,098 colorectal tumors Association with microsatellite instability FEATURE Odds ratio* (95% CI) p-value Tumor infil. lymphocytes 9.1 (5.9 – 14.1) <0.001 Right sided 4.7 (3.1 – 7.3) <0.001 Mucinous histology 2.8 (1.7 – 4.8) <0.001 Poorly differentiated 1.9 (1.2 – 3.1) 0.005 Crohn-like lymph. reaction 1.9 (1.2 – 2.9) 0.004 Age at diagnosis <50 yrs 1.9 (1.3 – 2.9) 0002 Any one feature 21.6 (5.3 – 87.9) <0.001 *Adjusted for all other features Percentage of tumours 3 cases = no instability in mononucleotide markers and no loss of mismatch repair proteins Percentage of tumours Test for loss of mismatch repair function Diagnosis under 50 yrs MSI-H MSI-L/MSS Diagnosis 50-59 yrs MsPath score Features of BRCA1 tumours mitotic index greater than 50/10HPF nuclear pleomorphism low tubule formation syncytial growth pattern pushing margin circumscribed lymphocytic infiltrate (moderate or intense) growth pattern (primary or secondary) trabecular necrosis ER IHC PR IHC Atypicalmedullarycarcinomaina womanwithagermlineBRCA1 mutation H&E,x2 Circumscribed,bosselated appearanceobservedatlowpower. Apredominantpushingmargin H&E,x25 Thetumorhasasyncytialgrowth pattern,highmitoticrate,high nucleargrade,andanareaof necrosis. H&E,x100 Armesetal.,1999 Atypicalmedullarycarcinomaina womanwithagermlineBRCA1 mutation H&Ex10 Apredominantlypushingmargin Highgradenuclearpleomorphism, asyncytialgrowthpattern H&Ex25 Highmitoticrateathighpower (H&E,x100 Alsoknowntohighhighfrequencyof p53somaticmutations. Armesetal.,1999 Diagnosed <40 years (ABCFS) 140 number of tumours 120 100 80 27/29 carriers 60 27/107 tumours were carriers 40 20 0 0 1 2 3 4 SCORE score BRCA1 germline mutation carrier 5 6 7 5+ Criteria 8 9 Diagnosed <40 years (ABCFS) Strong family history number of tumours 20 15 8/8 carriers 10 8/18 tumours were carriers 5 0 0 1 2 3 4 score BRCA1 germline mutation carrier 5 6 7 8 9 Family History Alone BRCA1 BRCA2 Familial Breast-Ovary Syndrome Pathology “5+” Criteria Alone BRCA1 BRCA2 ? Predictors of BRCA1 carriers Mitotic index > 50 mitoses per HPF: OR = 10 (95% CI 3-38; p<0.001) Trabecular growth pattern: OR = 14 (3-78; p<0.001) Each first degree relative with breast cancer diagnosed before the age of 60 years: OR = 2.9 (1.4-6.7; p=0.007) Area under the Receiver Operator Characteristic (ROC) curve: 0.91 (95% CI: 0.63-0.98) 3-variable model for BRCA1 carriers Early Onset Case Informed Consent Tumour Clinical management Pathology Future Cases Genetic counselling Mutation testing Cascade testing Carriers Non carriers Clinical surveillance Population surveillance Change How to achieve it? Colorectal cancer The Cancer Council Victoria (TCCV) has endorsed IHC for all cases diagnosed before the age of 50 yrs Happening in other states, e.g. South Sydney, Perth (using MSI BAT26 only) One specialised pathology service could handle all of Australia䇻s work load 1,000 case < 50 per year in Australia IHC/MSI would target <150 for genetic testing ~100 carrier families identified, therefore ~ 400 carriers identified (case + 3 rels) per year Could be done retrospectively as well Breast cancer 䇾Rapid䇿 testing beginning to happen in ad hoc manner BOADICEA soon to include ER and PR Developing local version that includes the 2 pathology features above Not to replace current practice of seeing 䇾worried well䇿, but make breast cancer services more cost-effective by shifting emphasis to early-onset cases We have the evidence to do things better Mutation carriers better identified by studying tumours of early-onset cases Even independently of family history Implementation will depend on local issues (ethics, resources, skills, cost-benefit, turf) May not apply (as well) to later onset cases Should become standard practice for Victorian cancer family genetics services Acknowledgements Epidemiology and Statistical Analyses Margaret McCredie, Graham Giles, Mark Jenkins, Roger Milne, Gillian Dite, Carmel Apicella, James Dowty, Graham Byrnes, Maggie Angelakos, and many others Genetic Analyses Melissa Southey, Andrea Tesoriero, Letitia Smith, Fleur Hammet, Fabrice Odefrey, Caroline Chatfield, Leeanne Mead,and many others Co-ordination and Interviewing Judi Maskiell and many, many others Study participants and their relatives Funding National Health & Medical Research Council, Vic Health, VBCRC, NBCF, NSW Cancer Council, National Institutes of Health (USA)