Introduction to the Lower Extremity Wound Pathway Current challenges for nurses 3/21/2016
advertisement

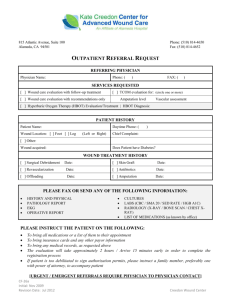
3/21/2016 Introduction to the Lower Extremity Wound Pathway Carolyn Morin, Enterostomal Therapy Nurse, Saskatoon Health Region Michelle Heidel, Skin & Wound Consultant, Prairie North Regional Health Authority Current challenges for nurses • Incomplete info/orders from primary care • Lack of standardized wound care protocols, product formulary • Capacity for wound care not always available in the homecare team • Sometimes difficult to access wound resource nurse/ physicians/ specialists for advice • Wound care takes many homecare hours Pathway proposes • Wound care referral form for family physicians and nurse practitioners • Standardized wound care protocols & product formulary (no orders required) T2 • Capacity‐building for homecare team • Forms to record & share information with wound resource nurse/ physician/ specialist • Tools to support better wound measurement and tracking, faster healing 1 Slide 3 T2 delete collect, replace with record Tessa, 3/1/2016 3/21/2016 How does the Pathway work? T3 Step 1: primary care referral Primary Care Referral Form 2 Slide 4 T3 Are we still proposing "tertiary clinic"? May want to change to "Tertiary care" Tessa, 3/1/2016 3/21/2016 Primary Care Triage • Contact on‐call vascular surgeon and fax this form for URGENT REFERRALS (red flags) • FAX REFERRAL to nearest Regional Wound Care Team for initiation of treatment according to wound pathway protocols • FAX REFERRAL to BOTH Regional wound team AND specialist office for all DIABETIC FOOT ULCERS. Regional wound team will initiate care; specialist assessment/consult takes place within three weeks Step 2: limb/wound assessment Standardized assessment form • • • • Should be completed ASAP after admission Assessment flow through Assists to identify probable etiology Please refer to printable copy 3 3/21/2016 Clinical Signs and Symptoms of Wound Infection in Diabetic Foot Ulcers (DFU) In this immunocompromised population, infection needs to be recognized and treated early. Infection is a serious complication within the foot; the various compartments, tendon sheaths and neurovascular bundles favor the spread of infection¹ and can be rapidly limb threatening. If any of these signs/symptoms are present contact the wound clinician nurse, family physician/NP. The presence of infection is defined by 2 or more classic findings of inflammation or purulence ² Increased pain ³ ⁴ > 2 cm of redness ² ⁴ Local inflammatory response (warmth, swelling) ² ⁴ Increased amount Wound breakdown ³ Foul odor ² ³ of exudate ² ³ Friable granulation tissue ³ Probe to bone ² ³ ⁴ Clinical Signs and Symptoms of Wound Infection in Venous Ulcers Increased Bacterial Bioburden Localized Infection Systemic Infection Non‐healing (minimal change in wound measurements after 3 weeks of care) Peri wound induration (firm edema) greater than/equal to 2cm Pale pink, non‐pebbly tissue Friable(bleeds easily) or hypergranulation (raised, deep/bright red, friable) tissue Peri wound erythema (redness) greater than/equal to 2cm Increased peri wound warmth Increased wound size and / or the development of sinus tracts and / or satellite wounds next to the original wound Rigor / chills Purulent exudate (thickened, greenish or yellow/white fluid) Change in behaviour or cognition (especially in elderly clients) Unexplained high blood sugar (in clients who are diabetic) New areas of necrotic slough (yellow/grey/cream colored tissue) Increased amount of exudate Change in characteristics of exudate from watery and serous to purulent (thickened, greenish or yellow/white fluid) Odour after wound cleansing If 3 or more signs/symptoms present add a topical antimicrobial to the wound dressing and contact the wound clinician nurse Onset of wound pain or increasing pain Increased dysreflexia(abnormal response to physiologic stimuli) or spasticity in clients with spinal cord injury If 3 or more signs/symptoms present swab the wound for C&S, add a topical antimicrobial to the wound dressing and contact the wound clinician nurse and physician/surgeon General malaise (predominantly in clients who are elderly, immunocompromised & children) Fever (may be muted in clients who are elderly or immunocompromised) Septic shock potentially leading to multi organ failure Wound probes to bone If any of these signs/symptoms are present contact the physician/ surgeon for review of the patient immediately or activate EMS Interpretation of ABI/TBI in Determining Compression ABPI Value Interpretation/Clinical Significance >1.3 Abnormally high range, renders ABPI test ‐ TBI indicated, contact wound clinician Compression Therapy* Incompressible arteries 1.0 – 1.3 Normal High compression 0.8 ‐ .99 Borderline to mild obstruction/peripheral arterial disease High compression 0.71 – 0.79 Mild to moderate obstruction/ peripheral arterial disease Modified compression <0.7 Contact wound clinician or /physician/NP. Contra‐indicated unless ordered by specialist Compression Therapy TBI Value Interpretation/Clinical Significance > 0.7 Normal .41‐0.69 Mild to moderate peripheral arterial disease Modified compression < 0.4 Severe ischemia –contact wound clinician or /physician/NP Contra‐indicated High compression 4 3/21/2016 Communication to referring provider Step 3: initiate treatment according to protocol Standardized treatment protocols • Based on wound etiology • Evidence based standardized care • If wound fails to follow wound‐healing trajectory or if concerns with protocols, contact wound resource nurse. • Wound team may vary by region – identify local wound resources and coordinate care • Please refer to printable copies 5 3/21/2016 Diabetic Foot Ulcer Venous Leg Ulcer Non‐healable wound 6 3/21/2016 Suggested formulary Sealant/barrier: Cavilon No Sting, Skin Prep Alginate: Biatain Hydrofibre: Aquacel Absorbent cover dressing: Mesorb, Mextra, Mepilex foam • Compression: Coban 2/Coban 2 lite • Antimicrobial dressing if indicated: Acticoat Flex 3, Iodosorb, Silvercel Ag (alginate), Aquacel Ag (hydrofibre) • • • • Step 4: monitor wound progress NISS Wound Record • electronic version or app may be available to calculate % change in wound area • Wounds that do not decrease in size by 50% within 4 weeks are not on track 7 3/21/2016 What happens in specialty care? Who is part of the multidisciplinary team? • • • • • • Patient & family Primary care provider Community nurse Wound resource nurse Podiatrist Diabetes educator • • • • • • Physiotherapist Occupational therapist Nutritionist Social worker Orthotist Vascular specialist What nurses need to know: • Takes a team approach to heal a wound • Access wound resource nurses with any concerns • If vascular surgeon is directing local wound care treatment, they will review regularly and follow up • Investigate possibility of telehealth 8 3/21/2016 Capacity‐building & resources • NURS 1684 “Care of the Patient with Lower Extremity Wounds” SK Polytechnic • Nurses still need certification as per regional policy • Pathway web pages (search sask wound pathway) for documents & links In summary: The purpose of the pathway is to improve patient outcomes through early optimal wound management: • Better healing times • Reduced hospitalization and amputation In summary: Improvements for providers include: • Standardized tools and protocols • Better communication and teamwork • Improved patient outcomes = reduced provider hours/products 9 3/21/2016 The LEW Pathway is still in development. Objectives for this year are: • Support wound care capacity‐building for nurses and primary care • Introduce and build familiarity with standardized wound care forms & protocols • Work on electronic versions of tools and forms • Improve access to vascular specialist and other wound services Questions and Suggestions Lower Extremity Wound Pathway Contact: Lori Latta, Project Manager 306‐787‐7159, lori.latta@gov.sk.ca 10