Keeping up with CKD Davy Ip Sir Seewoosagur Ramgoolam National Hospital
advertisement

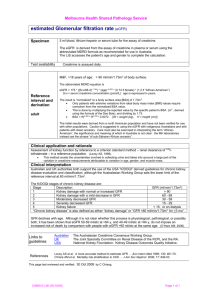
Sir Seewoosagur Ramgoolam National Hospital Keeping up with CKD Davy Ip Keeping up with CKD Davy Ip Why eGFR? Why CKD? Proteinuria and haematuria CKD guidelines CKD caveats Reports that say that something hasn't happened are always interesting to me, because as we know, there are known knowns; there are things we know we know. We also know there are known unknowns; that is to say we know there are some things we do not know. But there are also unknown unknowns - the ones we don't know we don't know Why eGFR? Why use eGFR ? To estimate renal function Functions of the kidney Homeotasis Fluid, electrolytes and acid base balance Excretion of metabolites Organic acids Phosphates Urea / creatinine etc Hormone production Renin / angiotensin Vit D metabolites Erythropoietin GFR is usually accepted as the best overall index of kidney function in health and disease. GFR cannot be measured directly CAPILLARY WALL BLOOD GLOMERULAR BASEMENT MEMBRANE URINE URINARY EPITHELIUM Glomerular filtration Capillary Net glomerular filtration pressure wall = URINE BLOOD Hydrostatic pressure – oncotic pressure – capsular pressure GLOMERULAR BASEMENT MEMBRANE Urinary epithelium Glomerular filtration rate The renal clearance of any substance is the volume of plasma that can be completely cleared by the kidney in unit time or urine concn. x urine flow rate plasma concentration Glomerular function rate Sum of all nephron filtration rates a measurement of excretory kidney function Normal GFR varies according to age, sex, and body size; In young adults it is approximately 120-130 ml/min/1.73 m2 and declines with age. Reduction implies a problem The Gold Standard The ideal marker. If a substance in stable concentration in the plasma is physiologically inert, freely filtered at the glomerulus, and neither secreted, reabsorbed, synthesized, nor metabolized by the kidney, the amount of that substance filtered at the glomerulus is equal to the amount excreted in the urine. Inulin satisfies all the properties of an ideal marker and is the gold standard for the measurement of GFR. Inulin clearance = GFR = UV/P Urea The majority of nitrogen from the breakdown of dietary or body proteins is excreted as urea in the urine. Nitrogenous waste goes to the liver as NH4+. The liver removes the toxic NH4+ and produces urea. Urea case 1 A 68 year old man presents to the hospital feeling unwell. He is very tired and feels ‘fluish’. He has been diagnosed with lymphoma a month ago after presenting with marked widespread lymphadenopathy. He has a course of chemotherapy and is still taking prednisolone 30mg daily. His GP has prescribed oxytetracycline for an acneiform rash. He complains that his stools seem to be much darker and loose.His U+Es are as follows: Na+ 138 K+ 4.7 Urea 26 Creatinine 110 Explain these figures. Urea case 2 A 31 year old woman presents to the hospital feeling unwell and with abdominal distension. She is known to have an alcohol problem, she admits to have drunk heavily on and off since her teenage years. On examination, though her face and limbs look emaciated, she has a distended abdomen. Her blood results are as follows. Na+ 138 K+ 4.7 Urea 2.6 Creatinine 70 Explain these figures. Far from ideal: urea PRODUCTION ELIMINATION Dietary protein GI bleed Renal disease Increased catabolism Surgery Infection Trauma Cancer/ tumour lysis syndrome Drugs Corticosteroids Tetracyclines Deceased metabolism Old age Protein Amino Acids pool Pre-renal failure causes a disproportionately high urea due to the need to conserve water compared to intrinsic and post-renal kidney failure GFR increased in pregnancy Liver Blood Urea Liver failure Urine Urea Creatinine Derived mainly from muscle metabolism, proportional to muscle mass, and is virtually all excreted by the kidneys. Usually produced at a more steady rate for a given individual compared to urea. Easy to measure. Creatinine Creatinine - Problems Serum creatinine (umol/L) 1000 900 800 700 600 500 400 300 200 100 0 0 10 20 30 40 50 60 70 80 90 100 110 120 GFR (Inulin clearance, ml/min/1.73m2) Not a sensitive marker for changes in GFR when renal function is or is normal. Indeed, people may lose 50% of normal GFR and have a borderline high GFR. Use of creatinine as an index of GFR rests on 3 major faulty assumptions: (1) creatinine is an ideal filtration marker whose clearance approximates GFR Tubular secretion Proportionately more important in advanced CKD Blocked by commonly used medications Extra-renal creatinine excretion Minimal in people with normal renal function but increased in patients with CKD Use of creatinine as an index of GFR rests on 3 major faulty assumptions: (2) creatinine production is constant among individuals and over time Factors affecting muscle mass Age Female Sex Afro-Caribbean race Muscular Malnutrition/ muscle wasting/ amputation Obesity Diet and drugs Vegetarian diet vs Meat diet Trimethoprim, cimetidine reduce tubular secretion of creatinine Effect of Muscle Mass on Serum Creatinine Normal Muscle Mass Normal Muscle Mass Increased Muscle Mass Reduced Muscle Mass Creatinine Input Plasma Pool Content Output Kidney Normal Kidneys Diseased Kidneys Normal Kidneys Diseased Kidneys 32yr old 55yr old 70kg 26yr old 26yr old 55yr old 84yr old 48kg 70kg 96kg 99kg 70kg These people all have a creatinine of 136 micromol/l and urea of 5 mmol/l. Please order in terms of GFR! 32yr old 26yr old 26yr old 55yr old 55yr old 70kg 84yr old 48kg 70kg 96kg 99kg 70kg 32yr old 26yr old 26yr old 55yr old 55yr old 70kg 84yr old 48kg 70kg 96kg 99kg 70kg 26yr old 96kg 32yr old 84yr old 48kg 55yr old 70kg 55yr old 70kg 70kg 26yr old 99kg 26yr old 96kg 32yr old 84yr old 48kg 55yr old 70kg 26yr old 55yr old 70kg 70kg 99kg Beware of serum creatinine interpretation 84yr old 48kg 55yr old 70kg 32yr old 26yr old 70kg 99kg 26yr old 55yr old 70kg 96kg Beware of serum creatinine interpretation Audrey Audley CCl 80-120ml/min CCl 80-120ml/min Creatinine 67-45 mol/l Creatinine 190-126mol/l Use of creatinine as an index of GFR rests on 3 major faulty assumptions: (2) creatinine production is constant among individuals and over time Factors affecting muscle mass Age Female Sex Afro-Caribbean race Muscular Malnutrition/ muscle wasting/ amputation Obesity Diet and drugs Vegetarian diet vs Meat diet Trimethoprim, cimetidine reduce tubular secretion of creatinine Use of creatinine as an index of GFR rests on 3 major faulty assumptions: (3) measurement of creatinine is accurate and reproducible across clinical laboratories. It was not so until the last few years because of different assays for creatinine used, some of them interfered with b drugs eg cephalosporins Creatinine - Problems Summary Not linear relationship with renal function Poorly sensitive in early CKD and near normal renal function Overestimation of renal function in advanced CKD Affected by muscle mass – age /sex/ race – abnormal body habitus Laboratory assays give differing results Improving on creatinine Serum creatinine (umol/L) 1000 900 800 700 600 500 400 300 200 100 0 0 10 20 30 40 50 60 70 80 90 100 110 120 GFR (Inulin clearance, ml/min/1.73m2) Alternative markers 125I-iothalamate 99mTc-DTPA Iohexol 51Cr-EDTA Serum cystatin C Creatinine clearance The previously commonly used estimate of GFR. Patient has to do a 24 hour urine collection and a blood test within hours of finishing the collection. Creatinine clearance Problems: Poor patient compliance, unreliable A small amount of creatinine is secreted by the tubules leading to overestimation of GFR, particularly at low GFR Prediction equations to estimate GFR Cockcroft-Gault equation CrCl in ml/min = [(140 - age) x weight (kg)]/SCr x 72 (x0.85 if female) Cockcroft DW, Gault MH: Prediction of creatinine clearance from serum creatinine. Nephron 16:31-41, 1976 MDRD equation GFR in ml/min/1.73m2 = 186 x (serum creatinine in µmol/L x 0.011312)-1.154 x (Age)-0.203 x (1.212 if Black) x (0.742 if female) Levey AS, Greene T, Kusek JW, Beck GJ: A simplified equation to predict glomerular filtration rate from serum creatinine. J Am Soc Nephrol 11:A0828, 2000 MDRD equation On average, GFR estimated from the MDRD Study equation is more accurate than measured creatinine clearance or creatinine clearance estimated from the Cockcroft-Gault equation in patients with reduced GFR Levey, A, Bosch, J, Lewis, JB, Greene, T, Rogers, N, Roth, D. A more accurate method to estimate glomerular filtration rate from serum creatinine: A new prediction equation. Ann Intern Med. 1999. 130: p. 461-470 MDRD equation Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D: A more accurate method to estimate glomerular filtration rate from serum creatinine: A new prediction equation. Modification of Diet in Renal Disease Study Group. Ann Intern Med 130:461-470, 1999 MDRD equation Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D: A more accurate method to estimate glomerular filtration rate from serum creatinine: A new prediction equation. Modification of Diet in Renal Disease Study Group. Ann Intern Med 130:461-470, 1999 MDRD equation - limitations Use of the MDRD Study equation, or any other equation, without re-calibration of serum creatinine assay to the assay used in the laboratory in which the equation was developed can introduce a systematic error into GFR estimates. This error is greater at low serum creatinine values. MDRD equation - limitations Validated in Caucasians with with chronic kidney disease (mean GFR 40ml/min/1.73 m2) including diabetic kidney disease, kidney transplant recipients, and African Americans with non-diabetic kidney disease. Not validated in children (age <18 years), pregnant women, the elderly (age >70 years), racial or ethnic subgroups other than Caucasians and African Americans, in individuals with normal kidney function who are at increased risk for CKD, or in normal individuals. MDRD equation - limitations Furthermore any of the limitations with the use of serum creatinine as related to nutritional status, unusual body habitus medication usage are not accounted for in the MDRD Study equation. Not applicable to situations with rapidly changing serum creatinine e.g ARF MDRD equation - BSA Correction for body surface area GFR varies with body size, usually expressed as BSA, which can be estimated from height and weight. Body surface area of 1.73 m2 is the normal mean value for young adults. Adjustment for body surface area is needed for meaningful comparing a patient’s estimated GFR to normal values, or to the levels defining the stages of CKD. However, drug dosing should not used eGFR corrected for 1.73 m2 MDRD equation: changes to come? CKD-EPI A new equation with the same input parameters as the MDRD equation Proposed to reduce the underestimation of GFR with people with near normal renal function The issue of ethnicity correction Black-American vs Black African South Asian vs East Asian Chinese vs Japanese Assume creatinine 136, urea 5, 1.73m2 Estimated creatinine clearance 21 46 50 68 76102 56 56 56 56 68 99 MDRD equation 34 37 MDRD equation with BSA 34 37 59 factored in 50 48 59 Assume creatinine 136, urea 5, 1.73m2 Cockcroft-Gault 21 46 50 68 76102 56 56 56 56 68 99 MDRD equation 34 37 MDRD equation with BSA 34 37 59 factored in 50 48 59 DO NOT USE eGFR TO CALCULATE DRUG DOSES! MDRD equation 34 37 56 56 56 59 Assume creatinine 136, urea 5 84yr old 48kg 55yr old 70kg 32yr old 26yr old 70kg 99kg 26yr old 55yr old 70kg 96kg Assume creatinine 136, urea 5 Estimated creatinine clearance 21 84yr old 48kg 46 55yr old 70kg 54 68 102 32yr old 26yr old 70kg 99kg 99 26yr old 55yr old 70kg 96kg Assume creatinine 136, urea 5 Estimated creatinine clearance 21 46 54 68 102 99 50 56 59 59 MDRD equation 34 84yr old 48kg 37 55yr old 70kg 32yr old 26yr old 70kg 99kg 26yr old 55yr old 70kg 96kg Assume creatinine 136, urea 5 Estimated creatinine clearance 21 46 54 68 102 99 50 56 59 59 MDRD equation 34 84yr old 48kg 37 55yr old 70kg 32yr old 26yr old 70kg 99kg 26yr old 55yr old 70kg 96kg Role of 24-hour urine collections • • • • • • • • • Extremes of age and body size Severe malnutrition or obesity Disease of skeletal muscle Paraplegia or quadriplegia Vegetarian diet Rapidly changing kidney function Prior to dosing drugs with significant toxicity that are excreted by the kidneys Pregnancy Creatinine - Problems C-G Not linear relationship with renal function Poorly sensitive near normal renal function Overestimation of renal function in advanced CKD Affected by muscle mass – age /sex/ race Affected by muscle mass – abnormal body habitus Laboratory assays give differing results Poor collection Correction for BSA, not ‘real’ Large margin of error at near normal renal function MDRD Measurement of renal function Inulin/ Iohexol/ Iothalamate Accurate Isotopes- radioactive MDRD eGFR Cockcroft-Gault creatinine clearance 24hr urine collection creatinine clearance Serum creatinine Serum urea Urine volume/appearance Inaccurate Proteinuria and haematuria “Acceptable” proteinuria Does normal urine contain protein? < 150 mg/24 hours or PCR< 15mg/mmol Orthostatic proteinuria Low grade proteinuria of PCR<100 in children and young adults. Diagnosis made when absent in early morning specimen. Mechanism unclear but good prognosis Transient/ haemodynamic proteinuria Fever/ Exercise/ Heart failure/ Hyperadrenergic state Benign prognosis More confounding factors Biological variation (day-to-day CV 45%) Haematuria/menstrual contamination Uncontrolled hypertension Urinary tract infection Pathological proteinuria Fixed or persistent Glomerular diseases Increased glomerulus permeability to protein Tubulointerstitial diseases Decreased tubular reabsorption of protein Overflow Causes – paraproteinaemia (myeloma, primary amyloid) Increased low molecular weight protein production Detecting and Quantifying Proteinuria Reagent strip tests 24 hour urine Spot urine tests Urine protein electrophoresis Urinary protein or albumin/creatinine ratios (PCR/ACR) Dipstick proteinuria 150mg/l 300mg/l Pitfalls of urine dipstick Semiquantitive More sensitive to albumin than other proteins Does not often detect urinary light chains (Bence-Jones protein) Does not detect microalbuminuria False positive with alkaline urine (as in UTI) and some drugs False negative with very acid urine and some drugs Affected by urine concentration Assuming 1-1.5l uniform urine output Normal LOW ACR PCR 24hrP 24hrA mg/mmol mg/24hr 3 Microalbuminuria if diabetic Proteinuria as defined by CKD guidelines Severe proteinuria Nephrotic range DIPSTICK -ve Trace + 30 15 150 30 50 500 70 100 1000 300 3000 ++ DIPSTICK +ve +++ HIGH 300 Total Protein Versus Albumin Nephrology literature based on total protein, DM literature defined by albuminuria Proteinuria is predominantly albumin but 150 mg/L TP contains 30 mg/L albumin 300 mg/L TP contains 150 mg/L albumin 1000 mg/L TP contains 700 mg/L albumin UK CKD recommend albumin in diabetes and total protein or albumin in non-diabetic setting, on basis of cost Total protein costs £0.10 Albumin costs £0.50 Microalbuminuria Sensitive immunoassays can detect increased albumin in urine before clinical (dipstick) proteinuria is detectable It is common in diabetes mellitus and predicts progression to ESRD and vascular complications Early detection enables intervention to slow progression Microalbuminuria and diabetic nephropathy (DN) Pre DN Early DN Overt DN ESRF GFR 100 ml/min GFR Albuminuria 0 5 MICROALBUMINURIA RANGE 15 25 years Approach to Patient with Proteinuria before Sept 2008 • If dipstick negative for proteinuria and patient has diabetes then send urine for ACR as per diabetes guidelines • If dipstick positive for proteinuria send urine for PCR in non-diabetics Approach to Patient with Proteinuria after Sept 2008 To detect and identify proteinuria, use urine ACR in preference, as it has greater sensitivity than PCR for low levels of proteinuria. For quantification and monitoring of proteinuria, PCR can be used as an alternative. ACR is the recommended method for people with diabetes. Early identification and management of chronic kidney disease in adults in primary and secondary care http://www.nice.org.uk/CG73 Haematuria When testing for the presence of haematuria, use reagent strips rather than urine microscopy. Evaluate further if there is a result of 1+ or more. Do not use urine microscopy to confirm a positive result. When there is the need to differentiate persistent invisible haematuria in the absence of proteinuria from transient haematuria, regard two out of three positive reagent strip tests as confirmation of persistent invisible haematuria. Haematuria Confounding factors Can be renal or lower urinary tract in origin Menstrual bleeding Urine dipstick – false positive for myoglobinuria and haemoglobinuria Haematuria Referral and follow-up Persistent invisible haematuria, with or without proteinuria, should prompt investigation for urinary tract malignancy in appropriate age groups. Persistent invisible haematuria in the absence of proteinuria should be followed up annually with repeat testing for haematuria, proteinuria/albuminuria (see recommendations above), GFR and blood pressure monitoring as long as the haematuria persists. Testing kidney function: summary Request and look at eGFR as well as serum creatinine and urea. Correct for ethnicity: multiply eGFR by 1.21 for African-Caribbean or African ethnicity. Where a highly accurate measure of GFR is required – for example, during monitoring of chemotherapy – use a gold standard measure. Interpret eGFR with caution for people with extremes of muscle mass. Make an allowance for biological and analytical variability of serum creatinine (± 5%) when interpreting changes in eGFR. When to test for CKD Blood test for eGFR and creatinine Urine for dipstick for ACR Early morning No meat in the last 12 hours No recent heavy exercise No recent trauma Send blood and urine samples early enough to allow analysis within 12 hours of sampling Renal Ultrasound Offer a renal ultrasound to all people with CKD who: •have progressive CKD (eGFR decline more than 5 ml/min/1.73 m2 within 1 year, or more than 10 ml/min/1.73 m2 within 5 years) •have visible or persistent invisible haematuria •have symptoms of urinary tract obstruction •have a family history of polycystic kidney disease and are aged over 20 •have stage 4 or 5 CKD •are considered by a nephrologist to require a renal biopsy. Advise people with a family history of inherited kidney disease about the implications of an abnormal result before a renal ultrasound scan is arranged for them. Progressive CKD Define progression as a decline in eGFR of > 5 ml/min/1.73 m2 within 1 year, or > 10 ml/min/1.73 m2 within 5 years. – Take at least 3 eGFRs over at least 90 days. – For a new finding of reduced eGFR, repeat test within 2 weeks to exclude acute kidney injury (acute renal failure). Consider whether the progression continuing at the observed rate would mean renal replacement therapy within the person’s lifetime. Chronic use of NSAIDs may be associated with progression; exercise caution and monitor GFR. Why CKD? Incidence Rate for RRT in the UK: 1980-2004 Mortality in HD Patients Annual Mortality (%) 100 10 Dialysis Male 1 Dialysis Female Healthy Male 0.1 Healthy Female 0.01 25-34 35-44 45-54 55-64 65-74 75-84 >85 Age (years) Foley AJKD 1998 The Nephrologist CMO highlights CKD PAGES 12 AND 32 Walsgrave’s transplant success PAGES 13 AND 38 The future of haemodialysis PAGES 16 AND 42 A SURVEY OF SALT AFTER PAGE 56 Patients with CKD are more likely to die than require dialysis STAGE GFR RRT Death 2 60-89 1.1% 19.5% 3 30-59 1.3% 24.3% 4 15-29 19.9% 45.7% Keith, AIM 2004 Progression of kidney disease Normal kidney Renal scarring Endstage kidney The Cardiovascular Continuum Tissue Injury Vascular Disease Endothelial Dysfunction Risk Factors Adapted from Dzau,1991 Pathological Remodeling Target Organ Dysfunction End-stage Organ Failure Death Mortality in CKD: USA • Health care system, • 35% of local population, • at least one serum creatinine • > 1,2Mio adults • > 20y of age • Excluded at entry: ESRF, renal transplant • MDRD: eGFR Go A S et al. NEJM 2004 Cardiovascular Events From Any Cause (per 100 person-year) Of Cardiovascular Events (per 100 person-year) Any Cause Estimated GFR (ml/min/1.73m2) 1,120,295 Ambulatory Adults Estimated GFR (ml/min/1.73m2) of Hospitalization (per 100 person-year) Age-Standardized Rate Hospitalization Estimated GFR (ml/min/1.73m2) Complications of CKD KIDNEY DAMAGE Hypertension more frequent than amongst patients without CKD Mild elevation of PTH Hypertension common Altered lipid metabolism ↓ spontaneous protein intake ↓ PO4 excretion ↓ Ca absorption Marked PTH rise Renal anaemia LVH STAGE 1 STAGE 2 STAGE 3 STAGE 4 STAGE 5 Kidney Damage with Normal or ↑ Kidney Function Kidney Damage with Mild ↓ Kidney Function Moderate ↓ Kidney Function Severe ↓ Kidney Function Kidney failure Persistent microalbuminuria Persistent proteinuria Persistent haematuria Structural abnormalities of the kidneys Biopsy-proven chronic glom’nephritis GFR mL/min/1.73 m2 Hypertension frequent 90 60 30 As Stage 3 but more pronounced & Metabolic acidosis Hyperkalaemia ↓ libido As stage 4(with greater severity) & Salt and water retention causing apparent heart failure Anorexia Vomiting Pruritus 15 0 Classification of CKD <2008 Other evidence of kidney damage Persistent diabetic microalbuminuria ACR >3* Persistent proteinuria ACR>30 Persistent haematuria after exclusion of other causes Structural abnormalities of the kidneys shown by radiology Biopsy proven glomerulonephritis National Kidney Federation, K/DOQI guidelines for CKD AJKD 2002 Classification of CKD >2008 The CKD guidelines What are they? CKD Issued April 2006 Chronic Kidney Disease Guidelines for adults Department of Nephrology Early recognition of CKD offers the chance to reduce progression and associated cardiovascular complications. This document gives guidance on screening, classification and management of CKD in primary care as well as advice on how and when to refer to the nephrologist. CKD challenges 7 Stage 5 GFR 15-29 16 Stage 4 GFR 30-59 98 Stage 3 GFR <15 GFR 60-89 ? Stage 2 879 GFR >90 CKD: ? Stage 1 a typical GP practice of 1000 GFR and age GFR and age GFR and age 140 Mean Cov Mean-1sd Mean-2sd eGFR (ml/min/1.73 m2) 120 100 80 60 Stage 3a 40 Stage 3b Stage 4 20 Stage 5 0 20-34 35-44 45-54 55-64 65-74 Age bands 75-84 85+ CKD and age 70 • Age 40-49 years 60 • Age 60-69 years – 5200 pmp • Age ≥ 80 years % Known – 1000 pmp 50 40 30 20 10 0 – 60,000 pmp < 50 50-59 60-69 70-79 > 80 Age Pitfalls in young patients with CKD Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D: A more accurate method to estimate glomerular filtration rate from serum creatinine: A new prediction equation. Modification of Diet in Renal Disease Study Group. Ann Intern Med 130:461-470, 1999 Pitfalls in young patients with CKD Serum creatinine (umol/L) 1000 900 800 700 600 500 400 300 200 100 0 0 10 20 30 40 50 60 70 80 90 100 110 120 GFR (Inulin clearance, ml/min/1.73m2) Not a sensitive marker for changes in GFR when renal function is or is normal. Indeed, people may lose 50% of normal GFR and have a borderline high GFR. Pitfalls in young patients with CKD 30 25 20 RR of Mortality 15 (Hazard Ratio) 10 5 <15 15-29 30-44 Renal Function 45-59 (ml/min/1.73m2) 0 20-44 45-54 55-64 Age bands (years) 65-74 >60 75-84 85+ CKD A leopard with changing spots?