Two-week Clinical Experience The Collaborative Model Purpose of PTS 651: practice time
advertisement

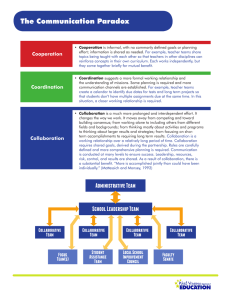
Two-week Clinical Experience The Collaborative Model Purpose of PTS 651: Provide practice time for basic skill acquisition in a collaborative setting Collaborative Learning Principles: Principles of collaborative learning (Johnson & Johnson, 1991) ◦ Students actively seek out knowledge, guided by the Clinical Instructor ◦ Takes place within a cooperative context - no competition among students! ◦ Students take responsibility for their own and each other’s learning Evidence: Research on collaborative learning indicates that students: (Baldry, 2003; Johnson, Johnson & Smith,1998; Johnson & Johnson, 1990) ◦ achieve at a higher level ◦ apply reasoning strategies more frequently ◦ are more motivated ◦ exhibit more confidence Successful in medical, nursing, and occupational therapy, as well as physical therapy education Team Building Behaviors: Collaborative learning requires that students: ◦ ◦ ◦ ◦ work in teams communicate with each other effectively become adept at giving feedback become adept at receiving feedback (Cohn et. al, 2001) Team Building Behavior Students are expected to provide each other with feedback regarding effective teamwork behaviors ◦ self assessment form ◦ peer assessment form Early Clinical Learning Assumptions: Practice needs to occur with real patients, but not in “real time”, because students need to “process” what they are learning. Learning requires observation and feedback. Students can learn from observing and providing feedback to each other with guidance from the Clinical Instructor. And… Not all learning needs to be supervised. Some learning units may be completed during non-patient care time. However, all practice sessions involving patients are to be supervised by a PT. Structure: Only students in good academic standing are eligible to enroll in clinical education experiences Groups of 2-4 students per Clinical Instructor Practice skills previously acquired in the classroom Student Responsibilities: Maintain confidentiality and adhere to facility’s policies & procedures Complete 10 learning units (see syllabus) Practice self/peer assessment (see assessment tool) and seek feedback from CI Demonstrate beginning level of clinical professional behaviors and work on developing level skills And… Interact effectively with peers, CI and coworkers to maximize learning (see team building behaviors) Acknowledge that CI is primary care provider who delegates to the student Structure time and demonstrate initiative in independent learning with peer(s) Identify & access resources needed for learning units Clinical Instructor Responsibilities: Serve as a resource for students Assume responsibility for patient/client care Identify appropriate clients suitable for students’ skill practice Be familiar with the learning units Provide clear and concise feedback Contact UW-La Crosse faculty immediately should issues arise UW-L Faculty Responsibilities: Ensure student competency prior to clinical placement Serve as a liaison between clinical facility, student and university Be available for questions or guidance Learning Units: Each student must complete 10 out of 15 learning units: ◦ Units 1-4 are required ◦ Units 5-15: any 6 units are to be selected by the CI Assessment forms are completed by student and peer ◦ CI only “signs off” that skills were completed Unit 1: Medical Chart Review Required unit CI may create a collaborative activity Example of skill practice: ◦ Each student reviews the same chart, making note of what they think is important information. Both students discuss their findings and “fill in” each other’s “gaps.” Together, both students present their combined findings to the CI, who provides feedback or encourages further exploration with guiding questions. Unit 2: Medical History Required unit CI may create a collaborative activity Example of skill practice: ◦ Students collaborate to develop a list of questions for collecting a subjective history from a patient. Then one student interviews the patient, while the other student considers peer’s effectiveness, SPT & patient non-verbal messages, or additional questions that would have been helpful. Together, both students discuss and seek feedback from CI. Unit 3: Documentation Required unit CI may create a collaborative activity Example of skill practice: ◦ Following observation of an intervention by the CI, both students write their own SOAP note on loose paper – trying to catch all the pertinent information. Next, students collaborate to develop a “better” note. Finally, CI offers feedback regarding strengths and areas needing improvement in their SOAP note. (Need not become part of chart.) Unit 4: Physiological Status Required unit CI may create a collaborative activity Examples of skill practice: ◦ Students take BP and HR measures of staff in therapy department. ◦ Students identify medications in patient charts that indicate or influence BP or HR issues. ◦ While observing interventions by CI, students make note of the patient’s physiological responses such as color, perspiration, respiration, etc. Unit 5: ROM Measurement Optional skill per CI choice CI may create a collaborative activity Example of skill practice: ◦ Students work together to measure ROM needed for functional mobility, such as: climbing stairs, opening doors, getting dishes out of cupboard, getting out of chairs, getting into cars, etc. Unit 6: Strength Measurement Optional skill per CI choice CI may create a collaborative activity Example of skill practice: ◦ Students perform MMT as delegated by CI, providing each other with feedback regarding technique and communication. Unit 7: Posture Assessment Optional skill per CI choice CI may create a collaborative activity Examples of skill practice: ◦ Students observe patients in the waiting room, making note of postural problems/concerns. ◦ Students observe neighbors shoveling snow, making note of postural concerns. Unit 8: Gait Assessment Optional skill per CI choice CI may create a collaborative activity Examples of skill practice: ◦ Students observe hospital staff in the hallways, noting gait deviations. ◦ Students observe orthopedic patients entering the clinic and, without knowing the involved limbs/joint(s), try to make predictions regarding impairment(s). Unit 9: Neuro Examination Optional skill per CI choice CI may create a collaborative activity Examples of test & measures: Cognition Coordination Tone Cranial Nerves Balance Sensation Proprioception Unit 10: Heat & Cold Optional skill per CI choice CI may create a collaborative activity Examples of skill practice: ◦ Students administer heat or cold modalities as delegated by CI, providing feedback for technique, skin inspection, and patient nonverbal communication. Unit 11: Electrical Stimulation Optional skill per CI choice CI may create a collaborative activity Examples of skill practice: ◦ Students administer electrical stimulation as delegated by CI, providing feedback for technique, skin inspection, and patient nonverbal communication. Unit 12: Other Providers Optional skill per CI choice CI may create a collaborative activity Examples of skill practice: ◦ Students shadow OT, SLP, Neuro-Psychology, Respiratory Therapy, etc. ◦ Students select a patient who receives multiple services, then identify which impairments/functional limitations each discipline addresses. Unit 13: Cost of Care Optional skill per CI choice CI may create a collaborative activity Examples of skill practice: ◦ Students interview social worker regarding funding sources for care and equipment. ◦ Students interview billing specialist regarding billing process, reimbursement barriers, productivity standards, etc. ◦ After observing intervention by CI, students determine total charges for that visit, including patient co-pay. Unit 14: Patient Report Optional skill per CI choice CI may create a collaborative activity Examples of skill practice: ◦ Students develop early clinical decision making skills by using data from patient examination to consider possible diagnosis, prognosis and plan of care. Unit 15: Optional Unit Clinical instructor may develop a collaborative activity based on: ◦ Learning opportunities unique to this site; or ◦ Need for an alternative plan due to inclement weather Absences: Absences are allowed in the following situations only: Inclement weather If CI concurs with student that travel would be dangerous, the CI may create a learning unit for students to do from home/campus Illness UW-L faculty must be notified of any absences We truly appreciate your willingness to support our students in their early clinical education. Please call or email the should any questions or concerns arise. Angela Binsfeld abinsfeld@uwlax.edu 608-785-8472