Trust Board Committee: Wednesday 12 November 2014 TB2014.120 Title
advertisement

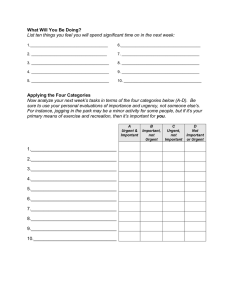
Trust Board Committee: Wednesday 12 November 2014 TB2014.120 Title Winter Preparedness Status This is an annual report to the Trust Board. History An outline paper was submitted to Trust Management Executive on 11th September 2014 and this paper was submitted to Trust Board Seminar on 24th September 2014 and Finance & Performance Committee in October 2014. Board Lead(s) Mr Paul Brennan, Director of Clinical Services Key purpose Strategy TB2014.120 Winter Preparedness Assurance Policy Performance Page 1 of 9 Oxford University Hospitals TB2014.120 Executive Summary 1. The paper sets out the Trust plans for delivering safe care over the coming winter and the actions to manage the forecast activity profile for the October 2014 to March 2015 period. The paper also outlines the additional elective activity to be undertaken during late Q2/Q3 to reflect the capacity implications. 2. Details are provided on the specific service developments being implemented during October and November 2014 and funded as part of the national £400m System Resilience Allocation announced by NHS England. Information on the recent external validation review is also included. 3. Recommendation The Trust Board is asked to note the report. TB2014.120 Winter Preparedness Page 2 of 9 Oxford University Hospitals TB2014.120 Winter Plan 1. Background 1.1. This paper sets out the key actions being implemented by the Trust in preparation for winter. In addition, the paper includes the activity assumptions that underpin the plan and identifies the initiatives the Trust is implementing as part of the System Resilience Programme funded by the national non-recurrent resources. 1.2. The Trust is also seeking to treat additional elective patients as part of the national RTT programme and the key assumptions are set out in this paper given the implications this additional activity will have on staff and physical capacity. 2. Activity Assumptions 2.1. Emergency and elective spells and ED attendances continue to run at levels above the position in 2013/14 but in line with the Trust’s activity forecast. At Month 6 actual activity and forecasts are shown in the table below. Table 1: Activity April to September 2014 and Year End Forecasts Activity Type Month 6 Actual Year End Forecast at April 2014 Month 6 Based Forecast Emergency Spells 44,751 92,376 91,802 Elective Spells 56,848 115,890 113,696 101,599 208,266 205,498 70,304 140,036 141,902 Total Spells ED Attendances 2.2. As can be seen from Table 1 the forecast based on Month 6 actual activity is closely aligned to the start year forecast activity and it is anticipated the 1.5% variance in spells is likely to close as the additional RTT activity is undertaken. 2.3. ED attendances as at Quarter 2 are 70,304 indicating activity for the year will be approximately 140,600 which is in line with the start year forecast. 2.4. The Trust is undertaking additional elective activity during 2014 initially to improve performance against the 18 week standards and subsequently as part of the national initiative to reduce both the size of the waiting list and the number of patients waiting over 18 weeks. This additional activity is and will impact on overall capacity in the run up to winter and during the initial winter period (October and November 2014). The graphs below identify activity and breach levels for admitted and non-admitted clock stops for the periods April to September 2013 and 2014. TB2014.120 Winter Preparedness Page 3 of 9 Oxford University Hospitals TB2014.120 Graph 1: Admitted Clock Stops Graph 2: Non-Admitted Clock Stops 2.5. During the period September to November 2014 inclusive the Trust is expecting to treat an additional 1,296 patients compared to the same period in 2013. 2.6. Admitted clock stops for the first six months of 2014 were 26,253 compared to 23,435 for the same period in 2013 representing an increase of 12%. 2.7. Non-admitted clock stops for the first six months of 2014 were 58,576 compared to 51,866 for the same period in 2013 representing an increase of 12.9%. TB2014.120 Winter Preparedness Page 4 of 9 Oxford University Hospitals 3. TB2014.120 Winter Plan Initiatives 3.1. The Trust is currently implementing a series of initiatives designed to increase capacity, improve flow and enhance seven day working in preparation for winter. The main service developments are set out below: Capacity Increases 1. Capacity Project Adams/Bedford (4 beds) Workforce Profile 4.5wte Nurses Performance Indicators Bed occupancy reduced to 95% OCE/NOC (10 beds) 10.75wte Nurses 5.38wte Clincal Support Workers Bed occupancy reduced to 95% F Ward HGH (3 beds) 4.5wte Nurses Bed occupancy reduced to 95% City/Comm JR (20 beds) 21wte Nurses 10wte Clinical Support Workers 3wte Admin/Ward Clerk Bed occupancy reduced to 95% Churchill (5 day to 7 day beds 8 beds) 5wte Nurses Bed occupancy reduced to 95% Workforce Profile 8wte Clinical Support Workers Performance Indicators 4 hour A&E standard to 95% 4 hour A&E standard to 95% Improve Flow – ED 2. Emergency Department Project Additional Healthcare Assistants Extend ED Consultant Rota to increase presence during afternoon/evening shift Paediatric CDU 4wte Consultants 2wte Consultants 1.5wte Physio and OT 4 hour A&E standard to 95% GPs in ED 84 hours GP equates to 2.3wte ED dedicated portering 12wte Porters 4 hour A&E standard to 95% 4 hour A&E standard to 95% Improve Flow and Seven Day Working 3. Extended Working and Flow Project Workforce Profile Performance Indicators SSIP GP referral unit Pharmacy on AGM Wards 7wte Nurses 1wte Consultant 3 wte Clinical Support Workers 2wte Admin Support Staff 4wte Pharmacy Technicians 4 hour A&E standard to 95% 60 discharges per day Discharge Lounge Additional Transport 3.6wte Nurses 4wte Clinical Support Workers 1wte Facility Staff Contract for service 4 hour A&E standard to 95% 60 discharges per day TB2014.120 Winter Preparedness Page 5 of 9 Oxford University Hospitals TB2014.120 3. Extended Working and Flow Extended Pharmacy 15wte Care Workers 2wte Nurses 0.5wte Consultant 8wte Pharmacists (using long line agency staff) 60 discharges per day 7 Day Endoscopy 11PAs Consultant 1.5wte Nurses 0.1wte Admin Note £7,000 non-pay cost 60 discharges per day and bed occupancy reduced to 95% Increase in urgent bookable list Echocardiology 2PAs Consultant 1wte Scrub Nurse 0.5wte ODO 0.5wte Recovery Nurses 1wte Cardiology Technician 60 discharges per day 60 discharges per day SHDS Expansion 4. 60 discharges per day External Validation 4.1 The Trust plans and current arrangements for managing front line urgent care services were subject to external review by the national Emergency Care Intensive Support Team on 15th September 2014 as part of a system-wide review which continued on 16th and 17th September 2014. The review team visited ED, SEU, four medical wards, the Operations Team and the Discharge Team. The initial feedback was positive though the following observations were made: 4.1.1 One of the four wards visited did not have estimated date of discharge for all patients 4.1.2 Weekend discharges were disproportionately low 4.1.3 Expressed reservations as to whether the twice daily medical ward rounds were regularly occurring. 4.2 Very positive comments were made about our new approach to managing surgical emergencies and the reverse triage model introduced in ED alongside positive comments on staff commitment and resolve to improve performance. The draft report, for comment on factual accuracy, has been received and following comments by the Trust we are awaiting publication of the final report. 5. 4 Hour Action Plan 5.1 The Trust has developed an internal four hour action plan which is reviewed monthly by the Trust Urgent Care Programme Group. The plan covers a wide range of actions as well as incorporating the winter plan initiatives described in section 3 above. A copy of the plan is attached at Appendix 1. 6. Recommendations The Trust Board is asked to receive the report and note the actions that are being put in place to ensure that the Trust is able to accommodate the increase in activity that is anticipated over the winter months. TB2014.120 Winter Preparedness Page 6 of 9 Oxford University Hospitals TB2014.120 Paul Brennan, Director of Clinical Services September 2014 TB2014.120 Winter Preparedness Page 7 of 9 Oxford University Hospitals Appendix 1 ED Action Plan 2014/5 Version 6 Updated 27.08.14 Number Category Improvement Description 1 Staffing Revised MDT model in EAU concentrated on rapid assessment, investigation, decisionmaking and flow 2 Staffing Medical leadership 3 Staffing Senior physician support to level 1 4 Report/Workstream Development and implementation of new MDT assessment Reports to AMR Directorate Urgent and treatment model in EAU to facilitate the rapid assessment, Care/Pressures Group. ordering of diagnostic tests and decision-making for patients referred directly by GP's to EAU enabling more timely decisions about discharge, follow-up on an ambulatory basis and admission. This model will also support more rapid investigation of patients referred from ED to EAU. 1. Task and Finish Group chaired by Dr Sudhir Singh, Clinical Lead for AGM meets fortnightly to manage the process of change associated with development and implementation of this model 2. Project plan covering implementation phase and review in place 3. Action cards describing the roles for medical and nursing staff in rapid assessment are complete 4. Flow charts mapping the pathway are in the process of being completed and will be displayed in the "Goldfish bowl" in EAU 5. Revised arrangements for deployment of medical staff to ensure there is always a doctor available to EAU to receive the 'take' are in place 6. Communications plan describing the new model has been developed and rolled out. 7. An identified constraint to optimal deployment of the rapid nurse assessment model is the current level of nursing vacancies in EAU and retention of existing staff. One element of this constraint is being managed via the appointment of a PDN. An attempt is also being in the short term to employ phlebotomists. Timescale (1) In place (2) Complete (3) Completed (4) Completed 05.09.14 (5) In place (6) Completed (7) On-going with review 26.09.14 Staffing Continuation of drive to recruit to middle-grade vacancies by AMR Directorate Performance Review Continuation of drive to participation in further Trust-wide led overseas recruitment fill middle grade medical initiatives posts and ensure Re-invigorate the pro-active scrutiny of middle-grade medical optimal deployment staff deployment to ensure best value for money and optimise input to rota gaps Programme for the appointment, development and rettention of ANP's underway. 1. Participate in the forthcoming overseas recruitment drive. 2. Revise and document the process for pro-active review of middle-grade deployment. 3. Programme in place with appointment to posts made. (1) In progress (2) Complete (3)In place James Price / Larry Fitton supported by Alex Monahan and Chris Shields 3. Andrea Dale 5 Staffing EAAs to continue to play a proactive role with referring GPs, Continue to develop the supporting flow and fully utilising capacity to review referred role of the Emergency patients on the following day Assessment Advisers AMR Directorate Performance Review 1.EAAs to continue to play a proactive role with referring GPs, seeking alternatives to attendance at EAU wherever possible 2. Fully exercise clinical assessment skills in the same way as ED senior nurses making referrals direct to specialties without the requirement to be first reviewed by a medic 3. Support medical teams to use next day appointments on DDU. 4. DOS completed. 5. Review of EAA Model following the resignation of one of the two postholders. Preferred emerging model looks to further intergrate the role of the EAAs into the EAU senior nurse establishment supported by a PDN. (6) Review of model to be complete by 30.09.14 (6) Louise Rawlinson/Lily O'Connor 6 Flow Plan at 2 hours for all patients in ED Flow Compliance with internal standards All patients to be assessed and have a defined clinical management plan within a maximum of 2 hours. Urgent Care Programme Group Internal monitoring of performance with escalation to ‘floor consultant’ when not being met. Remains under active review Louise Rawlinson Larry Fitton Continue to work on compliance with internal standards for ED Urgent Care Programme Group 'referred to' specialties to ensure timeliness within the 4 hour window ED to exercise their admitting/transfer rights to SEU and SSIP as follows Remains under 1. Following initial clinical assessment in ED, time critical diagnostics will continue to be ordered by ED. For those requiring a surgical opinion where active review by investigation is assessed by ED to be less time critical patients will be immediately transferred to SEU and SSIP. the UCPG 2. Patients should be managed on an ambulatory basis wherever possible 3. There will be onward direct referral of patients triaged by a senior ED nurse without the requirement to be seen by an ED medic, where appropriate. 4. Patients requiring a surgical opinion in ED will be transferred to the ward for assessment if a request for assessment on ED is not responded to within 30 minutes. The above actions will be supported by: 1. Diagnostic availability to SEU will be enhanced to that of ED and EAU 2. Patients will transfer with clinical and demographic information collected at the point of assessment together with details of drugs administered e.g. pain relief and clear instructions in relation to frequency of observations. Improvements to responsiveness are evident. Louise Rawlinson Larry Fitton 8 Flow Expected referrals and transfers Expediting the flow of expected patients and transfers from the Urgent Care Programme Group Horton ED 1. Transfers from the Horton ED for specialty opinion to be direct to the appropriate ward and not held in ED 2. Increased senior and junior medical staff presence on the medical wards to facilitate earlier decision making and discharge where appropriate. 3. Use of additional assessment bed in EAU to assist with privacy and dignity as well as to aid patient flow 4. SHDS participating in daily (7 day) post take ward rounds to assist in identifying support needs at home for patients 5. SHDS providing home discharge support to patients from southern Northamptonshire (in pilot phase) 6. Review of and increase in the number of patients being treated in the Rowan Day Unit – expansion of types of patients that can be cared for on a day case basis. 7. Development of a cross site medical staffing hub to aid recruitment of staff and management of staffing resources across JR ED + medicine and Horton ED + Medicine (1) Completed (2) Update 30.09.14 (3) Completed (4) Partially implemented (5) Implemented (6) Implemented (7) In progress James Price, Sudhir Singh, Siobhan Hurley and Caroline Mills 9 Flow General Surgical support Increasing JR dedicated Consultant Surgeons to four Urgent Care Programme Group (1) One to commence in post in June with two further appointments made on 6.6.14. New appointees to commence in October. Elective component of these posts will cover the urgent bookable lists and a rota will be introduced on a rolling 4 week basis to cover: • Surgical Emergency Unit • Urgent Bookable List – note need to move from two to four scheduled lists per week • Front door • Cover (2) Draft plan to move from 5 to 7 day consultant physician cover on the emergency surgery wards. (1)Partial completion (2) In Development (1) Paul Brennan (2) Sudhir Singh 10 Flow Paediatrics Improving flow to Paediatrics Urgent Care Programme Group 1. Paediatric CDU to continue to pro-actively “pull” patients from ED at all times of the day and night. 2. Requests for Paediatric opinions at the Horton will be consistently responded to within 30 minutes by consultants given 24/7 resident presence. 3.The Children’s & Women’s Divisional Nurse and General Manager to be informed of any failure to respond. 4. Winter pressure bid to recruit 1.5 WTE Paediatric ED Consultant (1), (2), (3) Completed (4) VCFs approved Paul Brennan TB2014.120 Winter Preparedness RAG Rating (1) Sudhir Singh (2) Caroline Mills (3) Sudhir Singh and Louise Rawlinson (4) Caroline Mills (5) Sudhir Singh (6) Caroline Mills (7) Louise Rawlinson/Lily O'Connor (1) Larry Fitton (2) James Price (3) Louise Rawlinson Senior decision maker on level 1 for 6 hours a day. Monday to Urgent Care Programme Group Friday 1pm to 7pm, Saturday and Sunday 2pm to 8pm. 1. ED Consultant job descriptions have been drawn up for an additional four posts and are currently with the CEM for approval. This will allow for a third Consultant to be on duty during the latter half of the day between 1pm to 10pm, mapped to activity pressures and thereby minimising the build up of queues into the night. 2. Interviews scheduled for mid October 3.Senior Nurse Coordinator to provide more support to ST4/5s overnight to facilitate decision-making. Responsible Lead (1) Completed (2) In progress, due for completion 21.10.14 (3) Completed and kept under active 1. Current model of physician deployment will be kept under active review in the context of the changes to managing more patients on an ambulatory Partially basis in EAU. This has been supplemented by a level 1 SHO. 75% of Consultant shifts are covered currently, working towards a 95% coverage during completed and will the winter period. be monitored 7 ED Additional ED Consultant presence to enhance the capacity for Urgent Care Programme Group timely management of patients attending ED. Action being taken James Price Page 8 of 9 Oxford University Hospitals TB2014.120 (1) (2) Complete Paul Brennan 11 Flow Bed management and escalation triggers Escalation triggers to continue to be proactively acted on to influence bed management decisions Urgent Care Programme Group 1. Internal mechanisms for escalation in place 2. External (system wide) mechanism in use for escalation 12 Flow Increase discharges with the support of SHDS Role and function of SHDS extended to include therapy and nursing staff to support a larger number of dependent patients and promote their rehabilitation at home Urgent Care Programme Group 1.Nursing staff have been recruited to work alongside care workers with phone based consultant medical advice available to enable broader spectrum (1) Completed of patients to be managed at home. The expanded service will initially focus on increasing patients discharged following an acute admission. (2) In progress 2. SHDS currently working in an intergraed way with ORS to promote discharge by pulling patients from the wards. 3. A senior physiotherapist has been working alongside an SHDS assessor at the front door promoting the use of Ambulatory pathways and expediting discharge. (1) Liz Hobbs (2) Liz Hobbs (3) Liz Hobbs 13 Flow Portering Ensuring access to and availability of porters for the transfer of patients for investigation and to ward areas is not a constraint. Urgent Care Programme Group 1. ED Team have reviewed options regarding the portering service with a view to setting up a dedicated portering team for ED and EAU. The preferred (1) Completed solution is to have a minimum of two porters available to ED/EAU 24/7 without the requirement to use the current telephone booking system. (2) Underway 2. To be funded from winter pressure funding. Trust to go at risk with regard to recruitment. Siobhan Hurley / Louise Rawlinson 14 Use of Transfer Lounge The Transfer Lounge will proactively take patients from all specialties in the John Radcliffe. Investment in both trained and untrained staff being made via winter pressure funding. Urgent Care Programme Group (1-4) Completed 1. All Matrons in all specialties have a responsibility to actively support the flow of patients by identifying patients to move to the Transfer Lounge but kept under before 10.30am. active review 2. Matrons to support ward staff to obtain early decisions on discharge from all hospital medical teams. 3. Operations Team to support ED and EAU Coordinator by working more closely with the wards to ensure beds are made available much more quickly than currently. Further support for this ‘hands-on’ role to be provided by the Directorate Operational Service Managers and Matrons with escalation to the Divisional General Managers and Divisional Nurses when constraints are not being actively and assertively managed. 4. Discharge by time of day to the Transfer Lounge will be reviewed weekly to monitor performance. 5. Breach analysis to be undertaken for any patients discharged direct from the ward (rather than via the discharge lounge). Lily O'Connor 15 Flow Patient transport Ensuring access to PTS does not continue to be a constraint to both timely discharge and management on an ambulatory basis Urgent Care Programme Group 1. Difficulties with booking and accessing PTS are now being reported on Datix 2. Log of transportation issues to be kept in ED/EAU, particularly regarding access to 2 man/stretcher crews Sara Randall 16 Alternatives to ED ENT Referral Unit Expand the hours of operation for the SSIP GP referral Unit. Urgent Care Programme Group 1. Activity through the designated cubicles on SSIP is currently reported to be low due to limited hours of operation. A bid to extend coverage has been (1) 1.10.14 made as part of winter planning and recruitment is underway. (2) 31.03.15 2. There is a requirement to formally evaluate the impact of this on the four hour standard performance. 17 Clinical pathway Dementia Emergency Department will develop a pathway for Dementia patients, similar to the already effective Stroke pathway. Urgent Care Programme Group and Trust Dementia Strategy Group 1. Initial focus will be on ambulatory management, expediting a return to home as quickly as possible. The In-reach medicine team will be asked to make early assessment of patients with dementia in ED to enable some patients to be sent home quickly. 2. To be managed within a maximum of 2 hours and where in-patient admission is required patients will be fast-tracked, by rapid assessment, to a definitive ward (proposed 7C and 7D) with a largely pre-determined set of test results. 3. The pathway will identify those patients that need to be managed in ED but require special input with guidance on how best to accommodate these patients to reduce any risks to provide staff with more awareness on care of vulnerable patients and / how to communicate with the family 4. The location of the ward (7C and 7D proposed) or other required area will be assessed and agreed with receiving departments within the Division. Some modifications to the ward environment may also need to be considered as part of this process. 5. Pathway developed with the Trust Dementia lead and the Trust Safeguarding Adults lead, to ensure staff awareness and good practice is included in any relevant material 6. Staff awareness sessions for the introduction of the pathway. 7. Monitoring of pathway introduction / appropriate use of the pathway 8. Post implementation review of the pathway. 9. Internal ED Training for 12 "Dementia Champions" to cascade learning/support to ED workforce, which includes simulation training, role play, and environmental factors consideration. Emergency Psychiatric Service In addition the Director of Clinical Services is to review Oxford Health EDPS provision as the introduction of the dementia pathway will ensure that senior nurses flag dementia patients early and that they are seen by the Trust internal Psychiatry Team in ED or on admission. Note this is a gap as agreed role split between EDPS and internal team excludes internal team from ED but EPDS focus is self-harm. Progress Kathleen Simcock underway and regular monthly updates provided via CQC Action Plan 18 Physical works Provision of additional ambulatory space in EAU Works to increase the number of assessment/ambulatory spaces in EAU by 14. Work to add 5 additional spaces was completed December 2013 the programme of works for a further increase of nine will commence in October 2014. AMR Directorate Urgent Care/Pressures Group. Progress reports taken to Trust Urgent Care Programme Group chaired by Paul Brennan Enabling works (internal and external) 26th August – 3rd October Delivery, fit out & commissioning of Portacabin 7th September – 3rd October Phase 1 6th October – 5th January Commissioning of Phase 1 5th January – 9th January Removal of portacabin & make good 12th January – 30th January Time scales as per phasing Louise Bishop/Louise Rawlinson/ Siobhan Hurley 19 Physical works Environmental improvement actions identified by the CQC Privacy and dignity issues Urgent Care Programme Group 1.All issues identified by the CQC inspection related to privacy and dignity have been completed. 2. Expansion of Resuscitation. There is potential to expand into x-ray and the admissions office. A specification to increase resuscitation bays from 4 to 6/7 spaces has been developed. Discussed with Director of Clinical Services 04/07/2014 - Feasibility study underway. (1) Completed (2) Underway Siobhan Hurley / Louise Rawlinson 20 Activity Levels Monitoring attendances at the two EDs Urgent Care Programme Group Q1 ED attendances out turned at 35,300 compared to 32,483 for the same period last year, double previous year on year rise. Trajectory of growth still predicted. On-going Paul Brennan 21 Performance Daily performance review Urgent Care Programme Group 1. Daily bed state and performance reports circulated in the Trust at regular intervals throughout the day. Actions to be taken agreed at the Safe Staffing and Capacity meeting. 2. Daily reports showing attendance, admissions and discharges circulated each day. On-going Paul Brennan 22 Winter system resilience bids Reference has been made throughout the action plan to elements of capacity which will be funded through winter pressure funding. In the interests of getting staff into post the Trust has commenced recruitment to these posts "at risk" pending confirmation of available funding. Urgent Care Programme Group and System Resilience Group 1. Additional beds will be opened on each of the four Trust sites for a limited period to accommodate winter pressures. 2. Investment will be made in additional consultant posts in ED. 3. Staffing in the Transfer Lounge, SHDS, Pharmacy and HCA's in ED will be increased. 4. Investment will also be made in urgent bookable theatre operating capacity, endoscopy and echo cardiography to promote flow on the urgent care pathway. 5. Short term enhancement to PTS will be made. TB2014.120 Winter Preparedness In progress Neil Cowan Paul Brennan Page 9 of 9