Binyrehormoner ) Binyrebarkhormoner
advertisement
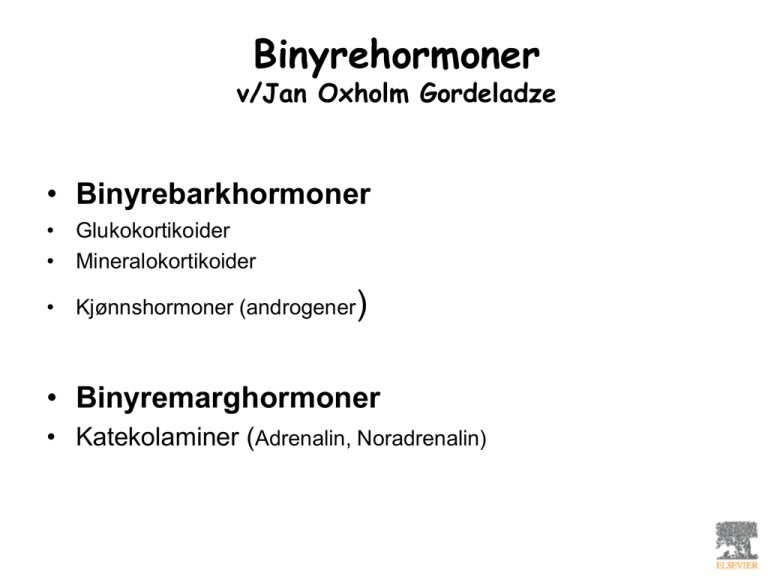
Binyrehormoner v/Jan Oxholm Gordeladze • Binyrebarkhormoner • Glukokortikoider • Mineralokortikoider • Kjønnshormoner (androgener) • Binyremarghormoner • Katekolaminer (Adrenalin, Noradrenalin) Downloaded from: StudentConsult (on 30 January 2011 02:17 PM) © 2005 Elsevier Binyrebarkhormoner Glukokortikoider • Binyrebark og –marg: separate celler i felles kjertel på/ved siden av øvre nyrepoler (adrenal, suprarenal glands) • Separate deler av barken: ytre lag er zona glomerulosa, midtre lag er zona fasciculata, indre lag er zona reticularis • Produserer steroidhormoner (kortisol, aldosteron, kjønnshormoner) • Innerst ligger binyremargen, produserer katekolaminer (adrenalin) Cerebral regulering • Overordnete stressutløsere • Emosjoner, kognitive responser • Homeostatiske stressutløsere • Blodtap, sirkulatorisk sjokk etc. Hypotalamus-hypofyse-binyreaksen (HPA – hypothalamic-pituitary-adrenal axis) • ”Feedback” og ”feed-forward” regulering av ACTH frisetting • ”Stress” definert som stimuli som øker ACTH frisetning Downloaded from: StudentConsult (on 30 January 2011 02:17 PM) © 2005 Elsevier Hypofyserespons • • • • • POMC-genet (pro-opiomelanocortin) ACTH (adrenocorticotropin) Beta-endorfin Lipotropin MSH (melanocyttstimulerende hormon) Downloaded from: StudentConsult (on 30 January 2011 02:17 PM) © 2005 Elsevier Downloaded from: StudentConsult (on 30 January 2011 02:17 PM) © 2005 Elsevier Downloaded from: StudentConsult (on 30 January 2011 02:17 PM) © 2005 Elsevier Glukokortikoider • Naturlige (kortisol, kortikosteron) • Syntetiske (prednison, dexamethason) Metabolic effects of Cortisol • Anti-insulin action • Protein catabolism • Increased gluconeogenesis and glycogenesis • No effects on CNS and heart Cushings’ syndrome • • • • • Excess Cortisol Protein catabolsim, buffalo hump Moon face Bleeding Kyphosis Cushing's syndrome. This is caused by excessive exposure to glucocorticoids, and may be caused by disease (e.g. an adrenocorticotrophic hormone-secreting tumour) or by prolonged administration of glucocorticoid drugs (iatrogenic Cushing's). Italicised effects are particularly common. Less frequent effects, related to dose and duration of therapy, are shown in parentheses. Antiinflammatory Pharmacologic Effects • Strong antiinflammatory effect via multiple pathways • Resistance to ”stress” Glucocorticoids and the Immune System • Immune System: • Increase in intravascular leukocyte concentration • Decrease in migration of inflammatory cells to sites of injury • Suppression of immune system (thymolysis; suppression of cytokines, prostanoids, kinins, serotonin, histamine, collagenase , and plasminogen activator) Activation of the hypothalamic– pituitary–adrenal axis and the sympathetic nervous system (SNS) leads to the release of cortisol and adrenaline from the adrenal cortex and medulla, respectively. These hormones inhibit the release of tumour necrosis factor (TNF) by monocytes. Interleukin-6 (IL-6) produced by contracting skeletal muscle also downregulates the production of TNF by monocytes and may stimulate further cortisol release. Acute elevations in IL-6 stimulate the release of IL-1 receptor antagonist (IL-1RA) from monocytes and macrophages, thus increasing the circulating concentrations of this anti-inflammatory cytokine. Exercise training mobilizes regulatory T (TReg) cells (which are a major source of the anti-inflammatory cytokine IL10) and decreases the ratio of inflammatory (CD14lowCD16+) monocytes to classical (CD14hiCD16−) monocytes. Following exercise, CD14hiCD16− monocytes express less Toll-like receptor 4 (TLR4), and thereby induce a reduced inflammatory response marked by lower levels of pro-inflammatory cytokines and reduced adipose tissue infiltration. Exercise also increases plasma concentrations of key inflammatory immune cell chemokines; repeated elevations of such chemokines may lead to a downregulation of their cellular receptors, resulting in reduced tissue infiltration. A reduction in adipose tissue mass and adipocyte size, along with reduced macrophage infiltration and a switch from an M1 to an M2 macrophage phenotype, may contribute to a reduction in the release of proinflammatory cytokines (such as IL-6 and TNF) and an increase in the release of anti-inflammatory cytokines (such as adiponectin and IL-10) from adipose tissue. The effect of a healthy diet and physical exercise on inflammatory processes A healthy diet and physical activity maintain the anti-inflammatory phenotype of adipose tissue, which is marked by small adipocyte size and the presence of anti-inflammatory immune cells, such as M2-type macrophages and CD4+ regulatory T (TReg) cells. A positive energy balance and physical inactivity lead to an accumulation of visceral fat and adipose tissue infiltration by pro-inflammatory macrophages and T cells. The pro-inflammatory M1 macrophage phenotype predominates and inflamed adipose tissue releases pro-inflammatory adipokines, such as tumour necrosis factor (TNF), which causes a state of persistent low-grade systemic inflammation. This may promote the development of insulin resistance, tumour growth, neurodegeneration and atherosclerosis. Atherosclerosis is exacerbated by the deleterious changes in the blood lipid profile that are associated with a lack of physical activity. LDL, low-density lipoprotein; IL-6, interleukin-6;TLR, Toll-like receptor. Aldosteron RAA = Renin, Angiotensin, Aldosteron (forklaring av figuren på neste slide) Control of aldosterone secretion • Three pathways (in three different colours) stimulate the glomerulosa cells of the adrenal cortex to secrete aldosterone. ACE, angiotensin-converting enzyme; ACTH, adrenocorticotropin hormone; AVP, arginine vasopressin; CRH, corticotropinreleasing hormone. I følge semesterboka: læringsmål • Addison’s syndrom • Pheochromocytoma Multiple choice 1-7: Which of the following statements is/are false 1) Higher centra (via physical emotional and biochemical stimuli) may affect the secretion of CRH (corticotropin releasing hormone), while diurnal «variation» of signals from the hypothalamus does not. 2) Cortisol negatively modulates CRH- and ACTH-secretion from the hypothalamus and the pituitary, respectively. 3) The secretion of ACTH is a Ca2+-mediated process stimulated by the cAMP-PKA axis, while the synthesis and secretion of cortisol from the adrenals are mediated activation of a tyrosin kinase (acting via rasproteins), which may lead to cortisol producing tumours, also affecting the secretion of adrenalin and sex hormones. 4) The POMC-gene also codes for MSH, which is responsible for the pigmentation of the skin seen in the elderly, when cortisol levels are diminished. 5) Cortisol blood levels are high in the morning and low in the evening. 6) Cortisol affects the health of multiple organs: bone and muscle mass (negatively), cartilage mass (positively), immune cells (negatively), maintains cardiac output and glomerular filtration. 7) ACTH also affects the secretion of aldosterone, while not as effective as the renin-angiotensin system and plasma K+-levels.