Physician Views on the Use of Comparative Effectiveness Data: A Comparative Effectiveness Data: A National Surveyy
advertisement

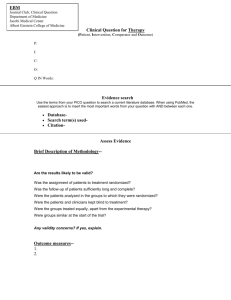
Physician Views on the Use of Comparative Effectiveness Data: A Comparative Effectiveness Data: A National Surveyy Salomeh Keyhani MD MPH Salomeh Keyhani MD MPH James J. Peters VAMC Mount Sinai School of Medicine Acknowledgements Co‐Investigators: Alex Federman, MD MPH Alex Federman, MD MPH Mark Woodward, PhD This project was supported by a grant from This project was supported by a grant from the Robert Wood Johnson Foundation. Background • Comparative effectiveness research (CER) has been promoted as a vehicle to improve the p p quality and efficiency of practice. • The inclusion of funding for CER in the stimulus bill of 2009 triggered a national debate over the appropriate role of evidence debate over the appropriate role of evidence in health care. Background • Rationing Rationing of medical care of medical care • Intrusion of the government in the doctor‐ patient relationship i l i hi • Loss of physician autonomy p y y • Cookbook medicine The Patient Protection and Affordable Care Act • Omission Omission of any mechanism to oblige of any mechanism to oblige physicians to apply CER data in their clinical practice. practice • CER may not be used: as mandates, guidelines or recommendations for payment coverage or or recommendations for payment, coverage or treatment decisions. Objectives • To To examine physician examine physician’ss views on the use of views on the use of data generated from CER. • To examine the characteristics of physicians p y who demonstrated a more negative view towards the development and use of CER towards the development and use of CER. Methods Design Methods‐Design • A national, mailed survey of a random sample l off physicians h i i b between t JJune 25th and October, 31st 2009. Methods Sample Methods‐Sample • Physician contact information was obtained from the AMA Physician M t fil Master file, which contains data on all U.S. Physicians. hi h t i d t ll U S Ph i i • This was a sub study of larger survey on coverage expansions • A random sample 1500 physicians from each of four specialty groups were surveyed (total, n=6000). Groups: • Primary care • Non‐surgical specialists N i l i li t • Surgical specialists • Other specialists (e.g., radiologists, anesthesiologists, and pathologists). • 50% random selection of physicians included in a larger study of physicians’ views about health insurance expansion. Methods Survey Development Methods‐Survey Development • We empanelled 7 nationally recognized physician p y g p y leaders and health policy and survey research experts. • We drafted survey questions and asked the expert panel to rank these items in terms of importance. • We refined the content and survey questions through yq g cognitive interviews with 16 physicians representing 7 states, 10 specialties, and 4 types of practice settings ( l (solo, group, free‐standing clinic, and hospital‐based f di li i dh i l b d clinic). Methods Survey Development Methods‐Survey Development S Survey Questions: Q ti 1) National guidelines should be developed to guide physician National guidelines should be developed to guide physician practice. 2) If national guidelines are established, comparative effectiveness data should be used in their development. 3) CER data will be used to restrict my freedom to choose treatments for my patients. 4) The availability of CER data would improve the quality of care provided to patients. Methods Analysis Methods‐Analysis Excluded physicians in training and physicians from U.S. territories. Compared the characteristics of respondents and non‐respondents using d h h f d d d data available in the AMA master file. Reported the percentage of physicians that agree with each statement. Examined differences in agreement with the four items by physician characteristics using chi‐square statistics. Grouped outcome variables as agree vs. disagree or uncertain Methods Analysis Methods‐Analysis • Examined physician characteristics associated with a more negative view of CER. ti i f CER • Considered Considered physicians as having a more negative view of physicians as having a more negative view of CER: If they agreed that CER would restrict freedom to choose treatment choices for their patients. Disagreed that it would improve quality of care. Disagreed that it would improve quality of care • Multivariable logistic regression analysis to examine physician characteristics associated with a more negative h h d h view of CER. Results: Responders vs. Non Responders • 2 2416 eligible physicians received the survey with 6 li ibl h i i i d h ih CER questions. • Response rate 50.9%. p • Survey Survey respondents were slightly older than non‐ respondents were slightly older than non‐ respondents (52.0 vs. 50.2 years, p<0.001) • No significant differences by gender, geographic l ti location, specialty category, or type of practice. i lt t t f ti National Guidelines Should be Developed to Guide Physician Practice to Guide Physician Practice 60.0% 56.5% 50.0% 40.0% 31 2% 31.2% 30.0% Agree Unsure Disagree 20.0% 12.1% 10.0% 0 0% 0.0% If National Guidelines are Established, Comparative Effectiveness Data Should be Used in their Effectiveness Data Should be Used in their Development 90.0% 80 0% 80.0% 77.8% 70.0% 60 0% 60.0% Agree 50.0% Uncertain 40 0% 40.0% Disagree 30.0% 20 0% 20.0% 10.0% 0 0% 0.0% 11.9% 10.2% Comparative Effectiveness data Will be Used to Restrict My Freedom to Choose Treatments My Freedom to Choose Treatments for My Patients 70.0% 65.7% 60.0% 50.0% 40 0% 40.0% Agree Uncertain 30.0% 20.0% 10 0% 10.0% 0.0% Disagree g 18.2% 15.9% The Availability of Comparative Effectiveness D t Data would Improve the Quality of Care ld I th Q lit f C Provided to Patients 60.0% 55.2% 50.0% 40 0% 40.0% 30.0% 20.0% 10 0% 10.0% 0.0% Agree 28.0% Uncertain 16.6% Disagree Results‐Agreement by Physician Characteristics Physician Characteristics Guidelines Should be Should be Developed If Guidelines Developed Developed, CER data Should be Used CER will Restrict My Restrict My Freedom CER will Improve the Improve the Quality of Care Yes 50.3% 82.6% 71.6% 50.1% No 64.2% 74.0% 58.3% 61.9% Practice owner Hours of Patient Care >=20 53.9% 76.3% 67.7% 52.7% <20 69.2% 84.9% 56.1% 67.9% West 59.7% 83.3% 61.7% 60.1% Northeast 63.1 80.7% 64.4% 57.8% South 48.8% 70.7% 69.9% 48.7% Midwest 58.0% 79.8% 65.1% 57.4% Census Region Results: A Negative View of CER Results: A Negative View of CER 35.5% did not believe that CER would improve quality and also believed that it would restrict li d l b li d h i ld i a physician’s freedom to choose treatments for their patient. Results‐Physician Characteristics Associated with a More Negative View of Associated with a More Negative View of CER (N=1203) Unadjusted Odds (95% CI) Adjusted Odds (95% CI) 1.80 (1.39‐2.35) 1.59 (1.16‐2.19) Practice owner yes No reference reference Hours of Patient Care Hours of Patient Care >=20 2.16 (1.48‐3.17) 1.96 (1.27‐3.02 <20 hours reference reference West 0.84 (0.57‐1.24) 0.82 (0.54‐1.24) Northeast 1.05 (0.70‐1.58) South 1.01 (0.68‐1.49) 1.54 (1.09‐2.18) Midwest reference reference Census Region 1.52 (1.06‐2.17) Adjusted for physician specialty, training (MD or DO), age, practice type, urban or rural location, and source of income Limitations • Modest response rate Modest response rate. • Other than age there were no statistically significant differences between non‐ p p respondents and respondents. • The extent to which physician respondents understood the purpose and potential use of CER is unclear but questions on CER were prefaced with the following information: information “Comparative effectiveness research compares existing therapies or diagnostics used for the same condition (e.g., a beta‐blocker used for the same condition (e.g., a beta blocker vs. a diuretic to prevent heart vs. a diuretic to prevent heart attack in patients with hypertension). Congress is considering the creation of national clinical guidelines using CER data.” • The Patient Protection and Affordable Care Act h d ff d bl d does not mandate the d h development of guidelines or the use of CER in guidelines. Conclusions • A majority of physicians support the use of CER data and believe it will improve the p quality of health care despite acknowledging that information derived from CER could be that information derived from CER could be used to restrict treatment choices. • A A sizable minority have negative views sizable minority have negative views regarding the use of CER data. Implications • Language adapted into barring the use of CER in guidelines or in coverage decisions demonstrates fears regarding the implications of y p this research for industry as well as patients. • Policymakers need to lay the foundation for the eventual use of CER data CER data. • Physicians’ support will play an important role in ensuring that comparative effectiveness research can live up to its promise of ti ff ti h li t it i f improving the quality of care and reducing costs. • Need to understand why a third of physicians hold an unfavorable view of CER.