V i ti i M di id M
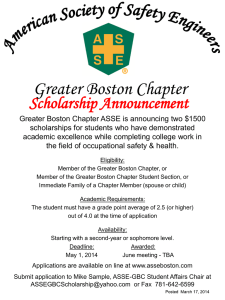
advertisement

Variation V i ti in i Medicaid M di id Managed M d Care C Emergency g y Department p Discharge g among Members with Asthma Sally Turbyville, MA, MS Robert Saunders, PhD June 2010 Academy Health ARM, Boston 28 June 2010 1 Today’s Objectives • Research Question • Study Design – Measure Descriptions – Design • Principal p Findings g • Limitations • Implications Going Forward Academy Health ARM, Boston 28 June 2010 2 Research Question • Is there a relationship between – quality lit off care and d resource use… – for treatment of patients with asthma… – in Medicaid HMOs • Quality: Percent of patients with “persistent asthma” that receive a “ “preferred f d asthma th therapy th medication” di ti ” • Resource use: Risk adjusted j rate of ambulatory ED use per 1000 member years (i.e., (i e discharged to community) Academy Health ARM, Boston 28 June 2010 3 Why This Study? • ED use is an important driver of cost of care and often an inappropriate setting, setting especially for children (IOM, 2006a,b). • Asthma is a condition that can be managed effectively without ED use • Asthma is a prevalent and costly condition diti for f Medicaid M di id and d society i t – $1.8b/yr y direct treatment ((Gergen, g 2001)) – 7.2m days of lost productivity, $1.2b/yr (http://www.ncqacalculator.com/) Academy Health ARM, Boston 28 June 2010 4 NCQA’s Experience: Quality • An established quality measure –A Ages 5-56 5 56 (5-9, (5 9 10 10-17, 17 18 18-56) 56) – In 2008, the average commercial plan provided appropriate asthma treatment 92% of the time (NCQA, 2009) – We expect higher quality implies less ED use (patient’s asthma is managed (p g and does not progress to emergent level) Academy Health ARM, Boston 28 June 2010 5 NCQA’s Experience: RRU • NCQA’s Relative Resource Use (RRU) measures compare a plan’s observed utilization rate to their expected utilization for select chronic diseases (indexed O/E) – Indirect standardization – Risk adjusted by age, gender, presence of select comorbid conditions – For ED, we collect ED visits because of inconsistent billing practices (other services we convert to dollars using standard prices) Academy Health ARM, Boston 28 June 2010 6 Health Plans Can Impact Costs Health Plan Functions Disease Management Wellness Programs Benefit Design Network Design Reimbursement Policy Provider Contracting Results Utilization Unit Price/Discount RRU Focus Premium Admin. costs, Strategic considerations, etc Academy Health ARM, Boston 28 June 2010 7 Population Studied • 74 Medicaid HMO plans (out of 163) – Submitted S b itt d both b th quality lit and d RRU HEDIS • Excludes plans with < 30 asthma cases (n=28) • Excludes plans that elect not to report RRU – Members with asthma continuously enrolled in same plan for at least 22 months across 2008 and 2007 • A very select group of members but… • Can’t blame discontinuity y for p performance – 60% of cases under age 18 Academy Health ARM, Boston 28 June 2010 8 Box Plot, Asthma Quality & ED RRU (n=74) ED Index O/E Quality Index 0 .5 1 1.5 2 HEDIS 2009, Medicaid HMO data Academy Health ARM, Boston 28 June 2010 9 .05 Density y .1 .15 .2 Histogram, Asthma Quality (n=74) 0 = 89.1 80 85 90 95 Asthma Quality (%) HEDIS 2009, Medicaid HMO data Academy Health ARM, Boston 28 June 2010 10 .5 nsity Den 1 1 1.5 Histogram, ED RRU (n=74) 0 = 1.00 0.00 0.50 1.00 1.50 2.00 ED RRU Index O/E HEDIS 2009, Medicaid HMO data Academy Health ARM, Boston 28 June 2010 11 Principal Findings • Despite similar, high levels of quality, there is substantial variation in ED utilization among plans • Plans with higher quality were associated with lower ED use among these members (-0.3322, p<0.004). – similar pattern for commercial plans Academy Health ARM, Boston 28 June 2010 12 Asthma Quality & ED RRU (n=74) 1.30 High Quality, Low Use High Quality, High Use 1.20 Quality 1.10 1.00 = -0.3322 0.90 p < 0.004 0.80 Low Quality, Low Use Low Quality, High Use 0.70 0.20 0.40 0.60 0.80 1.00 1.20 1.40 1.60 1.80 2.00 Relative Resource Use HEDIS 2009, Medicaid HMO data Academy Health ARM, Boston 28 June 2010 13 Limitations • Cross-sectional data, so causality is weak • Voluntary reporting of RRU • Measures are restricted to members continuously enrolled in Medicaid for 2yr • Measures M are restricted t i t d to t ambulatory b l t ED visits (i.e., not admitted to inpatient) – Complex sorting/selection process Academy Health ARM, Boston 28 June 2010 14 Going Forward • 4th year of collecting plan-level data in commercial Medicare and Medicaid commercial, • This y year NCQA will p publicly y report p its RRU measures for commercial plans – Expect to report Medicaid and Medicare in future years – With public reporting reporting, we expect plans will address their own excess utilization – Working ki tto improve i our RA methodology th d l (address more comorbid conditions) Academy Health ARM, Boston 28 June 2010 15 Going Forward • Plans can “slice-and-dice” their own data – Plans have received and will continue to receive from NCQA O/E ratios for reporting cohorts (i.e., (i e risk adjustors) • Are there members who require case management due to complex comorbidities? • Are there other interventions for the sub-population? – They still have the underlying data, data too • There may be limits to plan actions – Are these ED visits “money makers” for p Hospital p market p power issues? hospitals? Academy Health ARM, Boston 28 June 2010 16 References • Gergen PJ. (2001). Understanding the economic burden of asthma. J Allergy gy Clin Immunol,, 107:S445-8. • IOM. (2006a). Emergency care for children: Growing pains. Washington, DC: National Academy of Sciences. • IOM. (2006b). Hospital-based emergency care: At the breaking point. Washington, DC: National Academy of Sciences. • NCQA. (2009). State of health care quality 2008. W hi t Washington, DC: DC N National ti lC Committee itt for f Quality Q lit Assurance. Academy Health ARM, Boston 28 June 2010 17 Contact • Robert Saunders, PhD Research Scientist, Scientist NCQA saunders@ncqa.org 202-955-3500 Academy Health ARM, Boston 28 June 2010 18