Are There Racial/Ethnic Disparities in Mortality Rates and Surgical Health Administration?
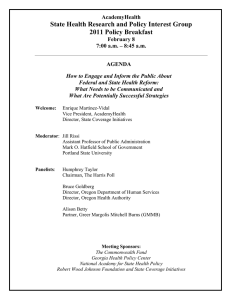
advertisement

Are There Racial/Ethnic Disparities in Mortality Rates and Surgical Procedure Use in the Veterans Health Administration? Stephanie Shimada, PhD Amy K. Rosen, PhD Priscilla Chew, MPH Ann M. Borzecki, MD MPH VA HSR&D QUERI SDP05-006 AcademyHealth ARM, June 2009 Rationale Racial disparities in quality continue to be a significant problem. The AHRQ Inpatient Quality Indicators (IQIs) are a measure of inpatient quality of care based on administrative data. – The National Healthcare Disparities Report has shown disparities in some IQIs outside the VA. Stephanie Shimada, AcademyHealth ARM June 2009 What are the Inpatient Quality Indicators (IQIs)? Volume Indicators e.g., Pancreatic resection volume Mortality Indicators for Inpatient Procedures e.g., Abdominal aortic aneurysm rate Mortality Indicators for Inpatient Conditions e.g., Congestive heart failure mortality rate Utilization Indicators e.g., Cesarean delivery rate Stephanie Shimada, AcademyHealth ARM June 2009 How are IQIs defined? IQIs are generated by applying AHRQ software to administrative discharge data to determine which hospitalizations are in the denominator or numerator for a given IQI. – Denominator=All discharges at risk – Numerator=All discharges in denominator with ICD-9CM codes indicating the event occurred. – IQI Mortality or Utilization Rate=Numerator/Denominator Stephanie Shimada, AcademyHealth ARM June 2009 Research Question Do IQI mortality rates and utilization rates vary by racial/ethnic group in VA? – Previous research has found fewer racial disparities in other measures of quality in VA. Stephanie Shimada, AcademyHealth ARM June 2009 Methods Data Sources: – VA Medical SAS Inpatient Data Files (Patient Treatment Files) for Fiscal Years 2004-2007 (October 1, 2003-September 30, 2007) Sample: Veterans receiving inpatient care at one of 123 VA acute-care hospitals between FY2004 and FY2007 – N= 2,272,894 hospitalizations – N= 1,024,406 unique individuals Stephanie Shimada, AcademyHealth ARM June 2009 Analyses Combined and created racial/ethnic groups using inpatient data sources. – Racial groups : White, African-American, Latino, Asian/Pacific Islander, American Indian, Unknown Applied AHRQ IQI software (v 3.1a) to VA discharge data to obtain IQI indicators and obtain risk-adjusted IQI rates and IQI composites by race. Logistic Regression controlling for age, sex, and the 29 comorbidities in the AHRQ Comorbidities Software, and adjusting for clustering at the VISN (hospital region) level. Stephanie Shimada, AcademyHealth ARM June 2009 Number of Deaths by Procedure White Black Unknown Latino Asian PI American Indian 600 # Deaths 500 400 300 200 100 0 om ct re rte da En id ot t ar C en A em TC lac P ep R y m ip H oto ni ra C n G ir t io B A pa ec C s n e R R e t io c AA ic se A ea t e cr al R an P age ph so E y IQI Stephanie Shimada, AcademyHealth ARM June 2009 Number of In-Hospital Deaths # Deaths White Black Unknown Latino Asian PI American Indian 5000 4500 4000 3500 3000 2500 2000 1500 1000 500 0 ia on um ne re P tu ac e Fr ag rh or ip H r fe ns tra em ke tr o F IH G S H C I o In M M A A IQIs Stephanie Shimada, AcademyHealth ARM June 2009 Risk-Adjusted Mortality Rates per 100 Discharges for CHF CHF Mortality Rates (IQI16) 7 6 5 4.4 4 3.7 3 2 1 0 All VA White Black Latino Asian PI Stephanie Shimada, AcademyHealth ARM June 2009 American Indian Unknown Risk-Adjusted Mortality Rates per 100 Discharges for Pneumonia Pneumonia Mortality (IQI20) 9 8 7 6.4 6 6.9 6.7 5 4.5 4 3 2 1 0 All VA White Black Latino Asian PI Stephanie Shimada, AcademyHealth ARM June 2009 American Indian Unknown Risk-Adjusted Rates per 100 Cholecystectomies Laparascopic Cholecystectomy (IQI23) 90 80 79.6 70 65.1 60 64.2 58.3 50 40 30 20 10 0 All VA White Black Latino Asian PI Stephanie Shimada, AcademyHealth ARM June 2009 American Indian Unknown Risk-Adjusted Rate of Incidental Appendectomy per 100 Abdominal Surgeries Incidental Appendectomy in the Elderly (IQI24) 6 5 4 3 2 1.4 1 0.8 0.8 0 All VA White Black Latino Asian PI Stephanie Shimada, AcademyHealth ARM June 2009 American Indian Unknow n Risk-Adjusted Rate of Bilateral Catheterization per 100 Cardiac Catheterizations Bilateral Cardiac Catheterization (IQI25) 14 12 10 9.7 8 7.6 8.2 6 5.9 4 2 0 All VA White Black Latino Asian PI American Unknown Indian Stephanie Shimada, AcademyHealth ARM June 2009 Mortality for Selected Procedures IQI Composite 1 2.5 2 1.6 1.5 1.3 1.3 1 1.2 1.0 1.0 0.5 0 White Black Latino Asian / Pacific Islander Stephanie Shimada, AcademyHealth ARM June 2009 American Indian Unknown Mortality for Selected Conditions IQI Composite 2 1.4 1.2 1 0.8 1.0 0.9 0.9 1.0 1.0 American Indian Unknown 0.8 0.6 0.4 0.2 0 White Black Latino Asian / Pacific Islander Stephanie Shimada, AcademyHealth ARM June 2009 Results: In-Hospital Mortality Rates IQI Name (IQI Number) Odds Ratios African-American vs. White AMI Mortality Rate (15) AMI Mortality Rate, w/o transfer (32) CHF Mortality Rate (16) Acute Stroke Mortality Rate (17) GI Hemorrhage Mortality Rate (18) Hip Fracture Mortality Rate (19) Other Minority vs. White 1.06 1.01 ***0.72 1.01 0.97 *0.78 0.87 0.82 0.90 1.02 0.86 0.86 *1.15 **0.68 Pneumonia Mortality Rate (20) Stephanie Shimada, AcademyHealth ARM June 2009 Results: Utilization Rates IQI Name (IQI Number) Odds Ratios AfricanAmerican vs. White Laparascopic Cholecystectomy Rate (23) Incidental Appendectomy in the Elderly Rate (24) Bilateral Cardiac Catheterization Rate (25) Stephanie Shimada, AcademyHealth ARM June 2009 0.93 **0.58 1.18 Other Minority vs. White 1.36 0.53 1.16 Conclusions We found few racial disparities in IQI rates. – There were no significant racial differences in risk-adjusted IQI rates for 12 of 18 IQIs. – Differences found showed that minorities were at higher risk for some IQIs but at lower risk for others. – No significant differences in mortality composites. Stephanie Shimada, AcademyHealth ARM June 2009 Implications There was large variation in laparascopic cholecystectomy utilization. Underuse of this procedure amongst American Indian vets should be addressed. VA should address all differences found through research and target with QI interventions as needed. Stephanie Shimada, AcademyHealth ARM June 2009 Thank You Stephanie Shimada, PhD stephanie.shimada@va.gov shimada@bu.edu Results – Patient Race All discharge records (N=2,272,894) Frequency Percent 1,433,546 63.1% 434,941 19.14% Latino 32,605 1.59% Asian/Pacific Islander 19,519 0.86% American Indian 12,386 0.54% Unknown 336,297 14.8% White AfricanAmerican Stephanie Shimada, AcademyHealth ARM June 2009