Why Didn’t That Hip Get Fixed? operative Treatment for Hip Fracture
advertisement
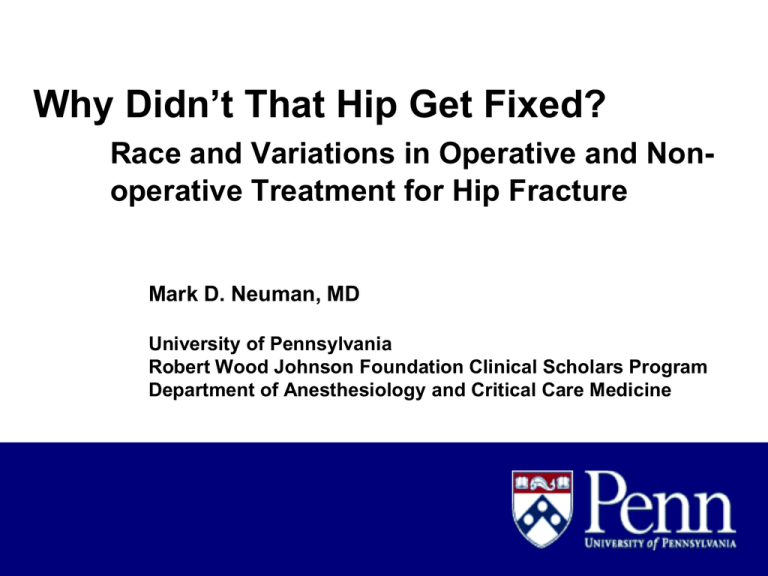
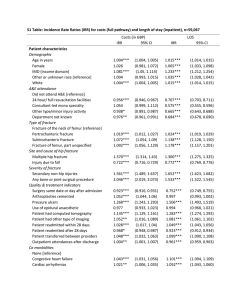
Why Didn’t That Hip Get Fixed? Race and Variations in Operative and Nonoperative Treatment for Hip Fracture Mark D. Neuman, MD University of Pennsylvania Robert Wood Johnson Foundation Clinical Scholars Program Department of Anesthesiology and Critical Care Medicine Background • Hip fracture is a disease of older adults • Most fractures occur due to a combination of osteoporosis and low-velocity trauma (i.e. falls) • 340,000 events in US each year • 20-30% 1 year mortality; 40% do not return to pre-fracture level of walking • Higher mortality & worsened mobility among non-white patients at 6 months Background • Hospital admission indicated for all patients with hip fracture • Operative repair is the standard of care • Non-operative repair only if moribund, refusing surgery, or no chance of functional recovery Parker, M. et al. BMJ 2006;333:27-30 Aims 1. Estimate the frequency of operative and nonoperative management for hip fracture in a population-based sample 2. Assess associations between patient race, income, and comorbidities and the odds of non-operative management Data sources • Inpatient Medicare claims • Obesity and Surgical Outcomes (OBSOS) Study • New York, Illinois, Texas 2002-2006 • 3,975,666 patients; 12,103,966 admissions • Hip fracture defined by ICD-9-CM diagnosis codes • 3-Month look-back to exclude re-admissions Methods • Operative care defined by presence of 104 ICD-9-CM procedure codes within 1 month • 60 Patient-level variables • Univariate analyses: chi-square, t-test • Predictive models for operative or nonoperative care: multivariable logistic regression • Survival analyses: Kaplan-Meier, MantelHanszel analyses Hip fracture care in NY, TX, and IL: 2002-2006 Number Percent Operative management* 155,178 93.8% Non-operative management 10,283 6.2% Total 165,861 100% *Operative care defined as presence of any of 104 ICD-9-CM procedure codes for surgery on proximal femur or hip joint within one month of admission Selected patient variables: operative vs non-operative* Variable Operative Non-operative Age: 85 and over (%) 43.6 49.7 Median # of comorbidities 4.3 4.6 CHF (%) 29.0 39.6 COPD (%) 26.0 29.0 Renal failure (%) 10.2 18.2 Alzheimer’s disease (%) 32.8 38.2 Race: white (%) 92.0 88.3 Race: black (%) 3.7 7.3 * P<0.0001 For all comparisons (χ2) Predictors of non-operative management (selected)* Parameter Odds Ratio 95% CI P Age 85 and over (vs. 65-74) 1.36 1.28, 1.46 <0.0001 CHF 1.46 1.40, 1.53 <0.0001 COPD 1.13 1.08, 1.18 <0.0001 Renal failure 1.66 1.56, 1.76 <0.0001 Alzheimer’s disease 1.17 1.12, 1.22 <0.0001 Race: black (vs. white) 1.80 1.65, 1.96 <0.0001 Income: below 25th percentile (vs. above 75th) 1.02 0.96, 1.08 0.525 *Full model controlled for 39 patient variables including age, comorbidities, sex, source of admission, fracture location, injury characteristics, race, income, and 21 significant interactions. Hypothesis (1): Black patients with hip fracture receive care at hospitals that are more likely to pursue non-operative management. Odds of non-operative care within individual hospitals: conditional logistic regression* Parameter Odds Ratio 95% CI P Race: Black (vs. white) 1.53 1.38, 1.66 <0.0001 Income: Below 25th Percentile (vs. above 75th) 1.10 1.01, 1.19 0.028 *Full model controlled for individual hospital effects, 39 patient variables including age, comorbidities, sex, source of admission, fracture location, injury characteristics, race, income, and 21 significant interactions. Hypothesis (2): Black patients with hip fracture are more acutely ill than whites. I. Non-operative patients: survival to 7 days Alive (Row %) Dead (Row %) Black 694 (92%) 60 (8.0%) White 7249 (73.7%) 1831 (18.6%) II. Odds of survival to 7 days: black vs. white Odds Ratio 95% CI Unadjusted 2.92 2.23, 3.82 Adjusted for hospital 2.44 1.79, 3.34 (Mantel-Hanszel) 1.0 Operative 0.9 SURVIVAL 0.8 0.7 Non-Operative 0.6 0.5 0.4 0 30 60 90 120 DAYS AFTER ADMISSION Black White 150 180 Conclusions • Black race associated with 80% increased odds of non-operative treatment • Controlled for comorbidities, source of admission, fracture characteristics, and income • Controlling for hospital, odds of non-operative treatment increased 57% among black patients • Pattern not explained by acuity of illness, as black patient survival exceeds white patient survival in non-operative cases Implications • Clinical model allows for examination of differences in care delivered to a large sample of patients with similar indications for intervention • Further research needed to validate and describe causes of this potential disparity • Identification of patient-level factors and socio-environmental effects that may influence patterns of operative care Collaborators • Lee A. Fleisher, MD (PENN • Orit Even-Shoshan, MS (Center for Outcomes Research, CHOP) • Lanyu Mi, MS (Center for Outcomes Research, CHOP) • Jeffrey H. Silber, MD, PhD (Center for Outcomes Research, CHOP; PENN) • Funding: NIDDK #R01 DK073671 (JHS); RWJFCSP (MDN)