Mandatory HAI Reporting in Pennsylvania: One Year and Counting Stephen Ostroff, MD
advertisement

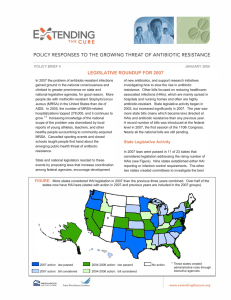
Mandatory HAI Reporting in Pennsylvania: One Year and Counting Stephen Ostroff, MD PA Department of Health Disclosure: Nothing to disclose “An optimist is one who makes opportunities of his difficulties while a pessimist is one who makes difficulties of his opportunities.” Harry Truman “The nice thing about being a pessimist is that you are constantly either being proven right or are pleasantly surprised.” George Will 70% of states/DC have reporting requirements in place California and Pennsylvania are currently the only states that have legislatively mandated reporting from both hospitals & LCTFs along with MRSA screening. Outline • Background • PA legislation • Implementation – Resources – Status • Data • Benefit & value Pittsburgh Regional Health Initiative 32 hospitals in SW Pennsylvania 68% reduction in CLABSI PA Legislation • In 2004, PA became 2nd state (IL 1st) to mandating HAI reporting & public disclosure • Through PA Healthcare Cost Containment Council (PHC4) • Publish annual report PA Healthcare Cost Containment Council 2006 Report Healthcarerelated infection Yes www.phc4.org No No. 30,237 1.5 m Fatal 12.3% 2.1% LoS (days) 19.3 4.4 Charge $176k $33k Healthcare Associated Infections in Pennsylvania • Fueled perception that HAIs were/are: – Out of control – Expensive – Easy to prevent Rx for PA (Jan 2007) Governor’s Office of Healthcare Reform Quality Component: - Hospitals must implement procedures to eliminate virtually all HAIs - Require reporting via uniform electronic surveillance system - Fund regional best practice training - Eliminate perverse incentives for paying added costs of HAIs - Nursing facilities to report HAIs Act 52 (Aug 2007) (Implement Rx for PA) • All facilities submit inf. control plan – 255 Acute Care Facilities – 722 Long term Care Facilities – Include MRSA/MDRO screening • “Qualified” electronic surveillance system – Incentives for implementation • Facility-wide reporting of HAIs – For hospitals, use all modules in CDC’s NHSN patient safety component – 180 days post-enactment (Feb 14, 2008)* – Nursing home dates/system not specified *Only 33 hospitals used NHSN at time of enactment Act 52 of 2007 (2) • All HAIs reported as serious events to Patient Safety Authority (PSA) • PADOH to report: – Facility-specific time trends – Compare rates among like facilities – Compare Pennsylvania to national data • Annual benchmark reduction targets – 10% reduction in 1st year – Subsequent annual targets set by DOH • Corrective action plan/fines if target unmet Implementation • 1200+ facilities (ACHs, LCTFs, ASCs) submitted Infection Control Plans – Only 3 fined for late submission • 100% compliance with Feb 08 deadline • 14 Electronic systems “qualified” – 79% of eligible hospitals now using a QES Benchmarking Conditions for Hospitals • Catheter-associated urinary tract infection • Central line-associated bloodstream infections • Surgical site infections • Abdominal hysterectomies • Hip & knee replacements • Cardiac surgeries HAI Reporting Long term care facilities • Developed reporting criteria based on modified McGeer criteria • Stand-alone electronic system for reporting • Phased implementation began two weeks ago Data Reports into NHSN from 255 Pennsylvania facilities Category Total Mean/month 2/08-12/08 36,819 3,506 1/09-4/09 5,738 1,435 Represents approx 10% of all facilities and reports in NHSN Healthcare-associated Infections Pennsylvania, (n = 42,617) All others 2358, 6% Resp 4994, 12% UTIs 16491, 39% BSIs 4816, 11% SSIs 6940, 16% 7018, 16% GI HAIs Benchmarking Conditions • Catheter Assoc UTIs • Central line BSIs • Surgical site infections 12,120 3,224 – Cardiac surgery – Hip replacement – Knee replacement – Abdominal hysterectomy All others 495 350 358 278 25,792 Data Analysis & Reporting • Use of Standardized Infection Ratios • Maximizes potential for risk adjustment • Reported no. of infections • Complex determination of no. expected • Ratio of observed to expected • Statistical significance Example: CAUTIs Medical ICUs Statewide Facility A Facility B Catheter days 250,000 1,000 23,500 No. infections 1,200 4 200 Rate per 1,000 4.8 4.0 8.5 Expected x 4.8 112.8 SIR 1.00 0.83 1.77 Estimated Cost/Time for Acute Care Facilities Assumptions • Personnel cost of $50/hr • Enrollment & training on NHSN – 2 persons/facility x 2 weeks • Non-benchmark conditions – 30 minutes to gather data & enter • Benchmark conditions (incl denominators) – 60 minutes to gather data & enter Data collection costs & person-hours • Training – $1,020,000 – 40,800 person/hrs • Non-benchmark (25,792 reports) – $644,800 – 12,896 person/hrs • Benchmark (16,825) – $841,250 – 16,825 person/hrs Totals (15 months): $2.5 million 70,500 person/hours Cost/Personnel Estimates • Does not include – DOH/PSA/HC4 costs – Data quality monitoring efforts – Long term care facilities – Added modules in NHSN – Required MRSA/MDRO screening costs • Lab testing costs • Isolation and care costs Questions • Does mandatory reporting add value? – Does this motivate facilities to implement practices they otherwise would not implement? – Examples in PA of reductions independent of reporting requirement – CMS Deficit Reduction/never events approach – More targeted/efficient reporting approaches • • • • • Can consumers understand the data? Will consumers/others use these data? Cost effectiveness of approach? Ability of institutions to further HAI reductions? How to evaluate impact of mandatory reporting?