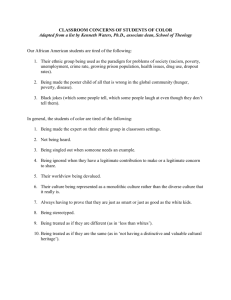
Has pay-for-performance decreased access for minority patients? Andrew Ryan, Ph.D.
advertisement

Has pay-for-performance decreased access for minority patients? Andrew Ryan, Ph.D. Schneider Institute for Health Policy, The Heller School for Social Policy and Management, Brandeis University Acknowledgements • Support • Agency for Healthcare Research and Quality • Jewish Healthcare Foundation 2 Outline • Potential unintended consequences of pay-for-performance • Pay-for-performance and disparities • Methods • Results • Policy implications 3 Patient avoidance in pay-for-performance • Patient avoidance, or “cream skimming”, occurs when providers determine that it is in their interest to avoid treating patients who are likely to reduce provider performance on a publicly reported or financially incentivized quality measure • In the absence of complete risk adjustment, providers may engage in statistical discrimination: the applying of perceived group characteristics to individuals (McGuire et al. 2008) • Documented extensively in the public quality reporting literature (Burack et al. 1999; Dranove et al. 2003; Epstein 2006; Narins et al. 2005) 4 Minority patients may be avoided in pay-for-performance • Racial and ethnic minority patients may be perceived to have higher unmeasured risk than non-Hispanic White (henceforth "White") patients, in P4P and public quality reporting programs. • A study by Werner, Asch, and Polsky (2005) found that disparities in rates of CABG procedures increased for Black and Hispanic patients, relative to White patients, after the implementation of the New York CABG public quality reporting program. • Despite concerns raised by several authors (Casalino et al. 2007, Chien et al. 2007; Hood 2007), there is no empirical evidence on the effect of P4P programs on patient avoidance. 5 The Premier Hospital Quality Incentive Demonstration (PHQID) • • • • • • Collaboration between Premier Inc. and CMS Implemented in 4th quarter of 2003, continues today Of the 421 hospitals (approximately 12% of IPPS hospitals) asked to participate in the PHQID, 266 (63%) chose to participate (Lindenauer et al. 2007) Pays a 2% bonus on Medicare reimbursement rates to hospitals performing in the top decile of a composite quality measure Pays 1% bonus for hospitals performing in the second decile (80th 90th percentile) of a composite measure Incentivized conditions • Acute myocardial infarction (AMI) • Heart failure • Community-acquired pneumonia • Coronary-artery bypass graft (CABG) • Hip and knee replacement Data and Methods 7 Data • Medicare fee-for-service inpatient claims and denominator files (2000-2006) • Primary diagnoses for which beneficiaries were admitted • Secondary diagnoses, demographics, and type of admission for risk adjustment • Zip codes to link beneficiaries to HRRs in which PHQID hospitals operated • Source of inpatient admission • Medicare provider of service files (2000-2006) • Hospital characteristics 8 Methods • • • Evaluate the avoidance of minority patients with AMI, heart failure, and pneumonia Use patient and hospital zip codes to identify Medicare beneficiaries living in hospital referral regions (HRR) of PHQID hospitals. For each condition for each race (White, Black, Hispanic, Other race): • Use linear probability model to estimate conditional probabilities that patients living in these HRRs receive care at PHQID hospitals before and after the program as a function of: • Beneficiary characteristics (Age, gender, race, Elixhauser comorbidities) • HRR fixed effects • Test difference-in-differences: • (Minority post – Minority pre) – (White post – White pre) 9 Methods continued • • • Hospital admission can occur through three sources: • Emergency department • Physician referral • Transfer from other facility Use multinomial logit model to estimate conditional probability that patient is admitted from each source (ED, referral, or transfer) to PHQID or non-PHQID hospital (6 outcomes) before and after program as a function of: • Beneficiary characteristics (age, gender, race, Elixhauser comorbidities) For each source of admission, test difference-indifference-in-differences: • [(Minority PHQID post – Minority PHQID pre) – (Minority non-PHQID post – Minority non-PHQID pre)] – [(White PHQID post – White PHQID pre) – (White non-PHQID post – White non-PHQID pre)] 10 Standard Error specification • Multiple observations from same HRRs over time give rise to group-level heteroskedasticity • Cluster-robust standard errors are estimated (Williams 2000) 11 Results 12 Descriptive statistics AMI n Age (mean) White Black Hispanic Other race Non-White 1,190,474 139,785 24,149 31,048 194,982 75.7 71.7 74.3 73.4 72.3 Female (%) Comorbidities (mean) 47.9 56.1 49.3 44.6 53.4 1.69 1.94 1.89 1.76 1.90 Admission through ED (%) 63.7 70.3 71.6 62.4 69.2 2,361,893 561,146 65,163 62,897 689,206 77.6 69.7 74.0 73.6 70.5 Heart failure n Age (mean) Female (%) Comorbidities (mean) 56.0 58.6 56.0* 52.7 57.8 1.92 2.07 2.11 1.97 2.07 Admission through ED (%) 67.1 72.6 75.2 65.2 72.1 2,226,619 288,399 50,732 66,648 405,779 76.6 70.7 74.2 74.7 71.8 Pneumonia n Age (mean) Female (%) Comorbidities (mean) 54.3 55.1 53.5 49.0 53.9 2.63 2.66 2.60 2.49 2.62 Admission through ED (%) 69.1 73.8 74.1 64.7 72.3 Note: *p >.05 Note: Test performed is Wald test of difference versus White 13 Proportion of admissions in PHQID hospitals 0 .05 .1 .15 .2 Adjusted Proportion of Admissions to PHQID hospitals: AMI .208 .211 .209 .214 .213 .206 .207 .2 .176 .179 .002 White Black .001 Hispanic Pre Post -.015 Other -.001 Minority DID Note: Orange triangle denotes significant effect 14 Proportion of admissions in PHQID hospitals 0 .05 .1 .15 .2 Adjusted Proportion of Admissions to PHQID hospitals: Heart Failure .175 .177 .183 .188 .179 .17 .167 .158 .161 .003 White Black Pre .183 .001 Hispanic Post -.005 Other .002 Minority DID 15 Proportion of admissions in PHQID hospitals .05 .1 .15 .2 Adjusted Proportion of Admissions to PHQID hospitals: Pneumonia .163 .163 .166 .168 .16 .163 .151 .153 .145 .138 .008 .002 .003 0 .002 White Black Pre Hispanic Post Other Minority DID 16 Source of Admission Analysis: AMI .6 Emergency Department Emergency Department .559 .569 Proportion of AMI patients .2 .4 .533 .531 Referral Referral .162 .154 .152 .142 .127 .129 .102 .096 .037 .035 .031 .032 .011 .006 -.005 0 .003 White Non-PHQID Pre PHQID Post -.016 -.02 Other Non-PHQID Post DID PHQID Pre DIDID 17 Summary of findings • Analysis shows small reduction in the proportion of “other race” patients admitted to PHQID hospitals for AMI after the program. • No effects observed for other races • No effects observed for heart failure or pneumonia • Reduction in admissions driven by: • Reduction in PHQID hospital ED use for “other race” patients, although not significant 18 Conclusions & Policy implications • Little evidence of minority patient avoidance in the PHQID • Patient avoidance may vary based on design of P4P program • P4P may have other unintended consequences • Unintended consequences of P4P should continue be monitored 19