Increased Tympanostomy Tube Use Contrasts with Fewer Ambulatory 1996 – 2006
advertisement

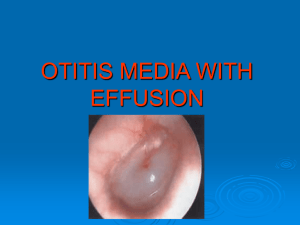
Increased Tympanostomy Tube Use Contrasts with Fewer Ambulatory Visits for Otitis Media in the US: 1996 – 2006 Lawrence C Kleinman, MD, MPH Leonardo Trasande, MD, MPP Salomeh Keyhani, MD, MPH Mount Sinai School of Medicine New York, NY Dr. Kleinman has no financial or other conflicts to disclose Outline Overview of Otitis Media Context: Studies of TT Appropriateness Data and Analysis Findings Conclusion Otitis Media Most common illness in Children in US Two distinct syndromes – Acute otitis media (AOM) – Otitis Media with Effusion (OME) OM is Ubiquitous – 67% of children have >1 AOM, by 2 years old * – 90% of closely observed children have > 1 episode OME by 2 years † * Teele DW, Klein JO, Rosner BA and the Greater Boston Otitis Media Study Group. JAMA 1983, PEDIATRICS, 1984. † Paradise et al. PEDIATRICS, 1997. Tympanostomy Tubes Most common surgery in children Benefits are uncertain in many cases – High levels of inappropriateness found twice Appropriateness Findings National sample of insured children*, 1990-91 – 23% Inappropriate (i.e. Risks > Benefits) Five NY City area hospitals†, 2002 – 1994 Academies’ Guidelines on OME (for subsample 1 through 3 y.o. with isolated OME) Recommended 7.5 % Not Recommended 92.5 % – 2004 Academies’ Guidelines on OME (not published) Recommended 5.6 % Not Recommended 94.4 % •Kleinman et al, The Medical Appropriateness of Tympanostomy Tubes Proposed for Children Under 16 in the United States. JAMA, 1994 † Keyhani, Kleinman, Rothschild, et al. Overuse of Tympanostomy Tubes in New York metropolitan area: evidence from 5 hospital cohort. BMJ, 2008 Study Data Children Age 0 through 16 Years Sources – Population Data: US Census – Surgical procedures National Survey of Ambulatory Surgery (NSAS) – Available for 1994 - 96, and 2006 – Medical visits (annual) National Ambulatory Medical Care Survey (NAMCS) – Doctors offices National Hospital Ambulatory Medical Care Survey (NAMCS) – Hospital Clinics and EDs Analysis Absolute and Relative Measures – Total Counts – Per Capita: Tympanostomies per 1000 children – Per 100 ambulatory otitis media visits (OMV) Time series regression analysis – Analyze changes from 1994-96 and 1996-2006 in single model using SAS Proc AutoReg OMV Decreasing Otitis Media Visits By Year: 1994 - 2006 30,000,000 20,000,000 10,000,000 0 1994 1996 1998 2000 2002 2004 2006 1994 – 1996: Slope = -670,977 (± 1.184 M), p = 0.58 1996 – 2006: Slope = -667,008 (± 199,114), p = .007 Use of TT now increasing US Children < 16 years 1994 – 1996: Slope = -24,912 p = .09 TT Surgeries per Year 650,000 1996 – 2006 Slope = 17,304 p = .02 400,000 1994 1995 1996 2006 TT per capita and per 100 OMV, US 6 TT per 1000 children 8 4 2 TT per 1000 children TT per 100 OMV 4 1994 – 1996: Slope = - 0.46 (± .04) p = .06 1996 – 2006: Slope = 0.22 (± .01) p = .02 TT per 100 OMV 1994 – 1996: Slope = - 0.09 (± .13) p = .61 1996 – 2006: Slope = 0.18 (± .03) p = .09 0 0 1994 1995 1996 2006 12 8 TOTAL PRIVATE PUBLIC NONE Table of Pairwise p-values (larger of pair in bold) 1996 Private vs Public Private vs. No Insurance Public vs No Insurance .09 <.001 <.001 2006 Private vs Public Private vs. No Insurance Public vs No Insurance Pairwise from 1996 to 2006 Private (increase) <.001 Public (decrease) .19 No Insurance (decrease) <.001 2006 1996 2006 1996 2006 1996 0 2006 4 1996 Surgeries per 1000 Children Increase is only among privately insured children .001 <.001 <.001 Summary of Findings Population 0-16 Increased slightly – Increased 4.4 % (66.5 M → 69.4 M) Ambulatory Visits for OM 1996 – 2006 – Decreased 27% (24.0 M → 17.5 M) 667,008, p=0.007 Tympanostomy Tubes 1996 – 2006 – Increased 35% (493K – 668K) 17,304 per year, p=0.02 – Increased 28% per capita – Increased 85% relative to Ambulatory Visits for OM Conclusions Utilization for Otitis Media is decreasing Tympanostomy Tube use is increasing Increase in TT is – disproportionate to either population growth or ambulatory medical service utilization for OM – disproportionate in that it was all among privately insured children TT use among publicly insured and uninsured actually decreased 1996 to 2006 Final Thoughts Context: Tympanostomy Tubes Overused – We don’t know why practice deviates from criteria Epidemiological Trend: Disproportionate increase in TT use – In other of our data: No associated decrease in antibiotic use Did focus on reducing antibiotic use unintentionally increase use of TT for children with OM – Passive : Less focus on surgical management, or – Active: Clinical belief that more surgery would reduce antibiotic use Is the United States experiencing an epidemic of Tympanostomy Tube Surgery? Evidence suggests: Yes, at least for privately insured children Alternative: We know so little about treating the most common disease in children with tubes that we can’t say Either way: urgent need for – HSR and HPR to understand why, followed by – Quality management to implement what we learn regarding the use of tympanostomy tube Thank you Major Indication for TT is OM Insured children, 1990-91* – 23% Recurrent AOM – 29% Persistent OME – 45% Both, 3% Neither Children from 5 NYC Hospitals, 2002† – 21% Recurrent AOM – 60% Persistent OME – 11% Eustachian Tube Dysfunction, 3% Both OME and AOM * Kleinman et al, The Medical Appropriateness of Tympanostomy Tubes Proposed for Children Under 16 in the United States. JAMA, 1994 † Keyhani, Kleinman, Rothschild, et al. Overuse of Tympanostomy Tubes in New York metropolitan area: evidence from 5 hospital cohort. BMJ, 2008 YEAR Variable 1 Variable 2 1994 0 0 1995 1 0 1996 2 0 1997 2 1 1998 2 2 1999 2 3 2000 2 4 2001 2 5 2002 2 6 2003 2 7 2004 2 8 2005 2 9 2006 2 10 Regress Outcome on V1 and V2 1994: Y = β0 1995: Y = β0 + β1, Δ= β1 1996: Y = β0 + 2*β1, Δ= β1 2006: Y = β0 + 2*β1 + 10*β2 , Δ=10*β2 Slope 1994-96 = β1 Slope 1996-06 = β2 YEAR Variable 1 Variable 2 1994 0 0 1995 1 0 1996 2 0 1997 - - 1998 - - 1999 - - 2000 - - 2001 - - 2002 - - 2003 - - 2004 - - 2005 - - 2006 2 1 Regress Outcome on V1 and V2 1994: Y = β0 1995: Y = β0 + β1, Δ= β1 1996: Y = β0 + 2*β1, Δ= β1 2006: Y = β0 + 2*β1 + β2 , Δ= β2 Slope 1994-96 = β1 Slope 1996-06 = β2 /10 New York State Chidlren Under 16 with Ambulatory Tympanostomy Tube Insertions: New York State 1996-2006 25000 20000 15000 10000 5000 0 1996 1998 2000 2002 2004 2006 Appropriateness, 1990-91* Definition: of Appropriateness “expected health benefits exceed the expected negative health consequences by a sufficiently wide margin that the tympanostomy is worth performing ‘ Insured children, 1990-91 – Using Explicit Criteria from an expert multidisciplinary panel 42% Appropriate (i.e. Benefits > Risks) Appropriateness, 2002* Explicit Criteria Concordant Appropriate Uncertain Not Concordant Inappropriate All Children (N=682) 7.0 % 22.3 % 69.7 % OME (N= 452) 8.6% 10.8 % 80.6 % Recommended Not Recommended 1994 Guidelines (N=172) 7.5 % 92.5 % 2004 Guidelines 5.6 % 94.4 % Academy’s Guidelines 2004 OME Guideline 2 months to 12 years old Tympanostomy Tubes – Otherwise healthy: Consider them after 4 months if persistent symptoms / hearing loss, recommended after 6 months – Sooner in “at Risk” children hearing loss independent of OME language or speech disorder autism and other developmental symptoms Down syndrome or other craniofacial syndromes visual impairment cleft palate developmental delay – Structural damage to the tympanic membrane or middle ear Clinical Findings - - OME 50 % of effusions were present for less than 3 months at the time surgery was proposed 25 % of children with OME did not have any effusion documented before the day surgery was proposed 75 % of children with effusion did not have documented hearing loss Typical Inappropriate Indication Child less than three years old Effusion documented for less than 1 month No recurrent otitis media With or without a trial of antibiotics Comparing Recommendations AHCPR Guideline more restrictive: 1447 UR Firm Criteria more restrictive: 5 Criteria Development (1994) Panel of 9 national experts – 5 Pediatricians, 4 Otolaryngologists Considered 80 potential indications for tympanostomy 2 round process: literature + judgment Indications rated on 9 point scale 1 2 3 4 5 6 INAPPROPRIATE EQUIVOCAL 7 8 9 APPROPRIATE Prospective Utilization Review 6429 cases January 1990 – June 1991 Step 1: Nurse Review – Interviews office staff for clinical data – Computer guided If found inappropriate at step 1: – Step 2: Physician Review Step 2 Physician Review Board certified reviewers Verify step 1 data accurate and complete Identify new clinical data Identify extenuating circumstances Overturn or sustain step 1 finding of inappropriate Explicit Criteria Clinical factors: OME – Age of patient – Duration of effusion – Otoscopic findings – Hearing Loss – Results of antibiotic treatment Clinical factors: Recurrent OM – Frequency of recurrence – Failure of antibiotic prophylaxis