Achieving National Quality Measurement and Reporting: A Purchaser Perspective
advertisement

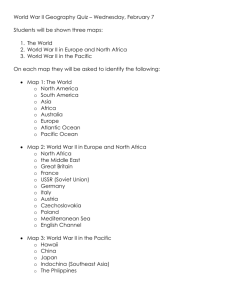
Achieving National Quality Measurement and Reporting: A Purchaser Perspective David S. P. Hopkins, Ph.D. Pacific Business Group on Health AcademyHealth ARM June 5, 2007 IOM Performance Measurement Principles “A performance measurement system should provide information for multiple uses, including: Provider-led improvement efforts Public reporting Payment and benefit design Population health initiatives.” -- excerpted from Performance Measurement: Accelerating Improvement, p. 48 2 © Pacific Business Group on Health, 2007 Consumer-Purchaser Disclosure Project: Performance Measurement Seen Through Consumers’ & Purchasers’ Eyes Scope and pace of measure development and implementation too narrow and slow Pressing sense of urgency Real consumer/patient choices being made with little real information Cost pressures leading to benefit designs and purchasing strategies too often “value-blind” Robust performance dashboard essential Consumer engagement requires relevant and adequate information Plan designs, payment systems and networks must recognize quality and efficiency Performance information must be valid and rapidly available: don’t let perfection be the enemy of the public good. 3 © Pacific Business Group on Health, 2007 Consumers and Purchasers Guidance on Measure Development Criteria Reasonable scientific acceptability Based on consumer’s perspective, not academic perfection Feasible Favor measures that can be populated with currently available electronic data Relevant to consumers and purchasers Important and actionable: full “STEEEP” dashboard Enable consumer choice Show high variation in performance Affect large numbers of patients or total health care spending Shed light on overall, cross-cutting, or condition-specific performance Provide better understanding of disparities Capture outcomes Reflect continuum of care 4 © Pacific Business Group on Health, 2007 How well have early standardization efforts delivered a robust measure set (per IOM 6 domains)? (* = minimal measure set; ** = partial measure set; *** = robust measure set) Measure Type Robust Measure Set Effectiveness/Timeliness Wide set of conditions Process Coordination of care Effectiveness – Outcomes Mortality/morbidity/ functional health status Wide set of conditions Safety NQF Safe Practices (Leapfrog) Infections/errors AHRQ Patient Safety Indicators Nursing Indicators Patient Centeredness C-CAHPS/H-CAHPS + other important domains Shared decision-making Coordination of care Safety/errors Equity Measures for population subgroups Cost-Efficiency Cost to payers Resource use Multiple time frames 5 NQF-Endorsed Measures (as of 6/1/07) ** * * ** 0 0 © Pacific Business Group on Health, 2007 National Efforts Lagging Local/Regional Initiatives Leapfrog Hospital Rewards – NQF-endorsed quality measures + resource efficiency measures Bridges to Excellence – systematic office processes + demonstrated excellence in 3 clinical areas HealthPartners Optimal Diabetes Care – patient-centered view leads to “all-or-none” measurement Mass. General Insurance Commission – physician-level clinical quality + cost-efficiency using best in class vendor tools Hospital Infections Reporting (PA, MO, FL) 6 © Pacific Business Group on Health, 2007 Better Quality Information (BQI) Pilots 6 Pilots: CA, AZ, IN, MA, MN, WI Selected through competitive RFP managed by AQA (formerly Ambulatory Quality Alliance) Focus is on aggregating Medicare and commercial data to measure and report on physician practice performance Intended for use by consumers and providers Contracted with CMS Limited scope of work: 5 nationally-endorsed quality measures initially, building to 12 3 measurement cycles: 2 in 2007, 1 in 2008 7 © Pacific Business Group on Health, 2007 Goals for the BQI Pilots Demonstrate effective public/private partnership Combine public and private data to achieve large “n” for measurement Inform the expansion of consensus measures nationally Demonstrate feasibility of collection of AQA endorsed performance measures Test additional measures that are feasible to collect and conform to AQA measure principles Speed adoption and reporting of valid, robust performance measures for use by: 8 Physicians and hospitals Consumers Purchasers Payers © Pacific Business Group on Health, 2007 BQI Challenges Measures Seeking a robust set – quality + cost-efficiency Many specialties, not just 1° care Consumers and purchasers want to choose/pay based on outcomes Data Chart review not scalable at statewide level (40,000+ practicing physicians) CPT-II codes good in concept, but lacking a path to implementation need both CMS and private sector Limited by what is electronically available today: claims, Rx, some lab 9 © Pacific Business Group on Health, 2007 Dynamic Tensions in Physician Performance Measurement Provider desires for “actionable” measures vs. consumer primary interest in outcomes Provider demands for precision (p<0.05) vs. consumer tolerance for some misclassification Milstein, et al., Health System Change, 2007 majority of consumers surveyed willing to accept >5% inaccuracy in physician performance ratings; 20+% willing to accept 20-50% inaccuracy Feasibility: measures requiring new coding vs. measures driven off available electronic data 10 © Pacific Business Group on Health, 2007