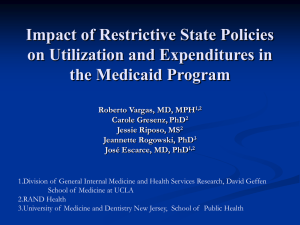
Background Impact of Restrictive State Policies on Utilization and Expenditures in
advertisement

Background Impact of Restrictive State Policies on Utilization and Expenditures in the Medicaid Program Roberto Vargas, MD, MPH1,2 Carole Gresenz, Gresenz, PhD2 Jessie Riposo, Riposo, MS2 Jeannette Rogowski, Rogowski, PhD3 José José Escarce, MD, PhD1,2 For state Medicaid programs, the Deficit Reduction Act eliminated Need to offer all benefits to all enrollees Requirement of states to get federal waivers before limiting benefits or imposing coco-pays and cost sharing Mandatory periods of public comment prior to implementing such changes 1.Division of General Internal Medicine and Health Services Research, David Geffen School of Medicine at UCLA 2.RAND Health 3.University of Medicine and Dentistry New Jersey, School of Public Health Restrictive Policies and Medicaid Restrictive drug policies have been associated with lower rates of prescription filling and more intensive use of acute care, nursing homes and higher overall costs Cost sharing and limits on physician visits in Medicaid have varying effects on physician visits rates but no significant impact on overall costs. Aims To examine the effects of restrictive policies on use of care by a nationally representative sample of Medicaid enrollees over a sixsix-year period Data Sources State Medicaid Summaries from 19971997-2002 services and coco-pays) Adults 1818-64 with at least one full calendar year of data in MEPS Summaries of state plan benefits including scope of medical care (Limits on visits and Study Sample We excluded: Patients who were pregnant The Medical Expenditure Panel Survey Had additional forms of insurance (MEPS), 19971997-2002 Were enrolled inn Managed care or HMO’ HMO’s 1 Study Design Outcomes Cross sectional, yearly analytic files of respondents Multivariate regression models and simulations Estimate the impact of state policy variation Controlling for individual characteristics, health care market factors, and community contextual factors Utilization: Outpatient officeoffice-based physician visits Outpatient office visits (non(non-physician and physician) Emergency room visits Inpatient acute care hospital admissions Expenditures: Prescription drug expenditures Total healthcare expenditures excluding vision and dental services Key Independent Variables: Medicaid Restrictive Policies Any physician visit coco-pay Any emergency room visit coco-pay Any prescription drug coco-pay Inpatient admission coco-pay for stay of greater than $21 Any inpatient coco-pay charged daily OfficeOffice-based physician visit limit Less than or equal to three prescription limit per month Regression Models: OfficeOffice-based visits: Negative binomial model Any emergency room: Logit model Any inpatient night: Logit model Expenditures: selected TwoTwo-part models Simulations: Descriptive Data: Individual Characteristics IndividualIndividual-Level Variables Female Analysis We simulated values for the utilization and expenditures weighted for the MEPS sampling design Descriptive Data: Outcomes Utilization and Expenditures 64% Mean (Std Err)/ % NonNon- Hispanic Black 28% # OfficeOffice-based physician visits 5.70 (0.33) Hispanic 21% # Total officeoffice-based visits Any emergency room visit % 8.03 (0.69) Other NonNon-White 5% NonNon-Hispanic White 46% Prescription expenditures $1098.28 (56.92) SSI Recipient 41% Total medical expenditures $4575.92 (320.53) Income<poverty 59% Less than high school 48% Any inpatient admission % 24% 14% 2 Descriptive Data: Restrictive Medicaid Policies Policy Regression Results 1997 Any Physician Visit Co pay 18 Limit on number of Physician Visits 17 Any Emergency Room Co pay 4 Prescription Co pay 29 Limit on number of prescriptions per month 11 Inpatient Admissions Co pay 14 Inpatient Daily Co pay 5 Visit limit policies had no significant impact on visits that included nonnon-physician care, emergency room visits, or inpatient hospital stays Limiting prescriptions to three per month had no significant effect on any of our utilization or expenditure measures Per day inpatient coco-pay was not associated with hospitalization rates or expenditures Regression Results Regression Results CoCo-pays for physician visits Lower Any ER visit rate (20% compared to 25%; p<0.10) Higher rates of inpatient hospitalization (18% compared to 13%; p<0.05) Higher average total expenditures ($5,431 compared to $4,271; p<0.05) Prescription drug coco-pays: Lower expenditures ($4,145 compared to $5,088; p<0.05) Prescription drug coco-pays: Significantly lower average number of physician officeoffice-based visits (5.58 compared to 6.70; p<0.05) Fewer Admissions (9% compared to 15%; p<0.10) ER visit coco-pays Regression Results Inpatient admission coco-pays of greater than $21 Lower total expenditures ($3,719 compared to $4,665; p<0.01) Conclusions Some coco-pays were associated with lower expenditures and utilization Visit limit policies, no significant impact on either outcomes of interest Certain restrictive policies are associated with unintended consequences such as the association of physician visit coco-pays with higher hospitalization rates and costs 3 Implications Efforts to reduce costs through restrictive policies have varying effects on utilization and expenditures Supplemental Slides As states consider greater use of restrictive policies there is a need to monitor the impact of restrictive policies for unintended consequences Results States Level Restrictive Policies Simulation Physician Office- Physician and NonValue Based Visits Physician Visits Any ER Visit Mean Std Err Mean Std Err Mean Std Err Any Office-Based Doctors Visit 0 6.29 (0.37) 8.59 (0.62) 0.23 (0.02) 1 6.00 (0.48) 8.35 (0.84) 0.24 (0.02) Any Inpatient Hospital Night Mean Std Err 0.15 (0.01) 0.13 (0.01) Any Physician Visit Co pay 0.13** 0.18** Simulation Variable Any ER visit Co pay 0 1 0 1 6.08 6.38 6.24 4.88 (0.36) (0.59) (0.34) (0.71) 8.68 8.07 (0.68) (0.84) 8.52 7.94 (0.62) (1.39) 0.25* 0.20* 0.23 0.24 (0.02) (0.02) (0.01) (0.05) Any Prescription Drug Expenditure (Spec 1) Mean SE 1109.85 (53.88) 1158.08 (59.87) Any Expenditure (Spec 1) Mean SE 4367.27 (314.30) 4953.56 (472.73) (0.01) 1115.04 (49.85) 4270.69** (267.43) (0.02) 1152.68 (87.88) 5430.74** (546.01) 0.14 0.14 (0.01) 1120.45 (39.32) 4664.96* (0.01) 1254.47 (146.76) 3718.50* (255.82) (686.33) Any Prescription Co pay 0 1 6.70** 5.58** (0.47) (0.37) 8.75 8.18 (0.75) (0.69) 0.22 0.25 (0.02) (0.02) 0.15 0.14 (0.01) 1108.34 (57.79) 5087.92** (397.68) (0.01) 1151.77 (62.87) 4144.60** (303.82) Limit of Three Rx per Month 0 1 6.15 7.15 (0.33) (1.47) 8.51 7.56 (0.61) (1.53) 0.23 0.29 (0.01) (0.09) 0.14 0.15 (0.01) 1126.5 (37.46) 4589.28 (0.05) 1364.48 (432.14) 5565.32 (256.60) (2042.71) Any Inpatient Admission Co pay greater than $21 Per Stay 0 1 - 0.15* 0.09 (0.01) (0.02) (261.84) (726.14) - - - 4671.56 3778.01 Policy Level Variables 1997 1998 1999 Any Physician Visit Co pay 18 18 18 17 17 19 Limit on number of Physician Visits 17 17 17 17 17 17 Physician Visit and Co pay Restriction 7 7 7 8 7 7 2000 2001 * 2002 *Data missing for one state *p<0.10; **p<0.05 State Level ER Restrictive Policies State Level Inpatient Admission Policies Policy Level Variables Policy Level Variables 1997 1998 1999 2000 2001 * 1997 1998 1999 2000 * 2001 2002 Inpatient Admissions Co pay 14 16 16 15 15 15 2002 Any Emergency Room Co pay 4 4 4 4 4 4 Inpatient Daily Co pay 5 5 5 5 5 5 Limit on number of Emergency Room Visits 4 4 4 4 4 4 Inpatient Stay Limit 12 12 12 12 10 10 Emergency Room Co pay and Visit Restriction 1 1 1 1 1 1 *Data missing for one state *Data missing for one state 4 State Level Prescription Drug Policies Policy Level Variables 1997 1998 1999 Prescription Co pay 29 29 30 31 30 31 Limit on number of prescriptions per month 11 12 12 12 10 10 Both Rx Co pay and limit 5 6 6 7 5 5 2000* 2001 2002 *Data missing for one state 5