Primary Research Questions Using HMOs To Serve The Medicaid
advertisement

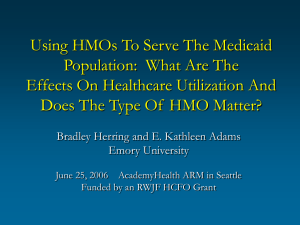
Using HMOs To Serve The Medicaid Population: What Are The Effects On Healthcare Utilization And Does The Type Of HMO Matter? Bradley Herring and E. Kathleen Adams Emory University Primary Research Questions • What are the effects of using HMOs for the Medicaid population? – Does enrollee access to care change? – Do utilization patterns change? – Do overall healthcare expenses change? • Are there different effects for commercial HMOs versus Medicaid-dominant HMOs? June 25, 2006 AcademyHealth ARM in Seattle Funded by an RWJF HCFO Grant State Motivation for Using Managed Care Background • Enrollees in some form of Medicaid managed care increased from 32.1% in 1995 to 60.7% in 2004 – Primary care case management – At risk health plans: “carve out” plans and HMOs • Enrollees in Medicaid HMOs increased from 14.1% in 1995 to 39.5% in 2004 • Little consistent or generalizable empirical evidence for access to care, utilization, or total expenses Might the Type of HMO Matter? • Commercial HMOs enrolling both Medicaid and privately insured populations: – Reduce “stigma” by integrating populations? – More likely to include “mainstream” providers? – Economies of scale? • Medicaid-dominant HMOs – more than 75% of enrollees in Medicaid: – Serve unique needs (economies of scope)? – More likely to include traditional “safety net” providers? – Inefficient due to “learning by doing”? • Improve access to care, at current expense: – Improve access to “mainstream” office-based providers? – Improve quality? • Reduce expense, while maintaining access: – – – – Improve use of cost-effective preventive services? Decrease unnecessary use of the ER? Better manage chronic conditions? Use bargaining power to achieve provider discounts? • Or perhaps yield predictable budgets? Prior Research • Early research summarized in Hurley et al. (1993) and Rowland et al. (1995) • More recent research: – State-specific analysis: CA, FL, OH, MN, TN, WI – Nationally-representative survey data: • State-level penetration or presence of MMC in a county – We compliment Duggan’s (2004) work on total state expenditures (i.e., capitation rates) by focusing on underlying utilization-based expenses 1 Our Empirical Approach • Community Tracking Study in 60 U.S. markets – Household Survey for ‘96-‘97, ‘98-‘99, ‘00-‘01, and ‘03 – We limit to the 51 urban MSAs • MSA measures of Medicaid HMO penetration using CMS and InterStudy data for ‘96, ‘98, ‘00, and ‘02 – CMS lists all Medicaid HMOs and the counties served – We link to InterStudy data to determine whether each HMO is commercial or Medicaid-dominant – Penetration rate: the percentage of all Medicaid enrollees in that HMO type Our Empirical Approach (cont.) OUTCOMEit = f (ßHMO XHMO,it + ßI XI,it + ßAREA XAREA,it + γMSA MSAi + γYEAR YEARt, ε) where OUTCOMEit = a specific outcome measure for Medicaid enrollee i during time t = measures of commercial and XHMO,it Medicaid-dominant HMO penetration = a set of individual characteristics XI,it XAREA,it = a set of local area characteristics = a set of MSA indicator variables MSAi YEARt = a set of year indicator variables ε = an error term Medicaid Enrollees in the CTSCTS-HS: Three Sets of Dependent Variables (cont.) Office-based physician visits Any mental health services Inpatient stays Inpatient surgeries Variables: HMO (both types) penetration rate Commercial HMO penetration rate Medicaid-dominant HMO penetration rate 1996 1998 2000 2002 24.7% 35.9% 32.4% 42.1% 8.5% 14.3% 12.4% 12.1% 16.2% 21.6% 20.0% 30.0% Source: Complied CMS and InterStudy data Medicaid Enrollees in the CTSCTS-HS: Three Sets of Dependent Variables • Sample: 9134 non-elderly with Medicaid in the CTS-HS – Includes children in SCHIP – Adults and children both together and separate • 1st set: Access measures: – – – – Usual source of care other than the ER Usual source of care is the ER Having a difficulty in obtaining care Being satisfied with one’s primary care doctor Medicaid Enrollees: Independent Variables • Variables of interest: • 2nd set: utilization measures: – – – – Medicaid HMO Penetration Rates of Urban CTS Markets by Period – – – – Medical practitioner visits ER visits Inpatient nights Outpatient surgeries • 3rd set: “synthetic” estimate of total healthcare expenses using CTS-HS utilization & the MEPS: – 1996-2003 MEPS to regress actual expense on utilization – The MEPS coefficients are essentially “unit prices” – Commercial HMO penetration rate – Medicaid-dominant HMO penetration rate • Individual controls: – Age and gender, family type (e.g., single with kids), family income, race/ethnicity, education, self-reported health status • Local-area controls: – PCCM, type of SCHIP expansion, Medicaid fee index, MDs/capita seeing Medicaid, hospital beds/capita, FQHC, private HMO penetration, median income, race/ethnicity • MSA fixed effects and time trend 2 Results for Commercial HMOs • Child enrollees: – No effect on access – No effect on utilization – No effect on expenses • Adult enrollees: – No effect on access – Increase only for mental health visits (p<0.05) – Decrease in expenses (p<0.10) Results for MedicaidMedicaid-Dominant HMOs • Child enrollees: – Decrease in usual source of care other than ER (p<0.10) – Increase in medical practitioner visits (p<0.10) Increase in ER visits (p<0.05) – Increase in healthcare expenses (p<0.05) • Adult enrollees: – Increase in using the ER as a usual source of care (p<0.10) – Increase in medical practitioner visits (p<0.05) Decrease in inpatient surgeries (p<0.001) Decrease in outpatient surgeries (p<0.05) – No effect on healthcare expenses Magnitude of the Effect of MedicaidMedicaid-Dominant HMOs • We simulate the independent effect of the increase in the Medicaid-dominant penetration rate of 16.2% in 1996-1997 to 30.0% in 2002-2003: – Proportion reporting a (non-ER) usual source of care: Reduced from 86.2% to 84.8% – Number of visits to the ER: Increased from 0.654 per year to 0.732 per year – Total healthcare expenses (in 2003$): Increased from $3004 to $3163 (a 5.3% real increase) Conclusions • Increase in penetration by commercial HMOs: – – – – No change in access to care Little change in utilization patterns No increase in expenses (perhaps a decrease for adults) (Our other work: increase in physician participation) • Increase in penetration by Medicaid-dominant HMOs: – – – – Worse access to care Many changes in utilization Increase in expenses for children; No change for adults (Our other work: no change in physician participation) Policy Implications • What’s the real motivation for contracting with HMOs? – Welfare improvements from either improved access and maintained expense -or- lower expense and maintained access • Our results suggest that – States may have seen small welfare improvements by contracting with commercial HMOs before their exit – States have seen (and will see) decreases in welfare by contracting with Medicaid-dominant HMOs • Attention needed in setting capitation rates and fees – Exits by commercials & pressure from Medicaid-dominants 3