Unmet Need for Symptom Management from Breast Cancer Treatment
advertisement

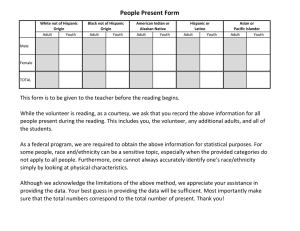
Unmet Need for Symptom Management from Breast Cancer Treatment Jean Yoon, Jennifer Malin, Diana Tisnado, May Lin Tao, Patricia Ganz, Katherine Kahn Los Angeles Women’s Study RAND, Santa Monica UCLA General Internal Medicine and Health Services Research Background Treatment and early detection of breast cancer has improved patient survival. Quality of life and symptom management have become important for patients with breast cancer. Symptoms vary by patient characteristics and type of treatment. Previous Research Most quality of breast cancer care studies focus on whether women received screening, timely diagnosis, and appropriate interventions. Several studies examined pain management for cancer patients. Few studies have analyzed whether patients have received appropriate management of other symptoms. - IOM describes one aspect of quality of care and desirable health outcomes as management of physical and psychological symptoms Study Design Los Angeles Women’s Study conducted in 2000. Population-based study. Patients identified through Rapid Case Ascertainment. 1,219 women responded to survey with 63% response rate. Defining Unmet Need Had symptom severe enough that it interfered with mood or functioning Arm problems, nausea/vomiting, hot flashes, vaginal dryness, problems with sleep. Wanted help for her symptoms Did not receive any help for her symptoms Analysis Bivariate and multivariate analyses of unmet need by patient characteristics. - Patient characteristics included age, race, language, education, income, marital status, working status, insurance coverage, treatments received, number of severe symptoms, health status, comorbid conditions, stage at diagnosis. Bivariate analysis of reasons for unmet need by race/ethnicity. Results weighted for non-response and adjusted for clustering at hospital level. Sample Race/Ethnicity White Black Hispanic Spanish Hispanic English Other N 834 112 104 103 66 % 65 12 9 8 6 Sample Characteristics Mean age (SD) 67 (14) % with at least one comorbidity 83% Stage at diagnosis: In situ (13%), I (38%), II (30%), III (5%), IV (2%), Unknown (11%) Prevalence of Unmet Need N Have severe symptom Wanted help for symptoms Received help for symptoms % Difficulty sleeping Hot flashes Nausea / vomiting Vaginal dryness Arm problems Any symptom 353 248 158 148 138 577 28 19 12 11 11 46 68 74 78 66 77 77 70 51 91 48 69 75 Symptom Prevalence by Race/Ethnicity N % 112 104 43 44 66 35 White 834 47 Hispanic English language 103 49 Black Hispanic Spanish language Other Chi-square p-value 0.0626 Unmet Need Prevalence by Race/Ethnicity Black Hispanic Spanish language Other N % 24 21 60 55 9 44 White 104 34 Hispanic English language 13 32 Chi-square p-value <0.0001 Race/Ethnicity as Predictors of Unmet Need Black Hispanic Spanish language Other White Hispanic English language Odds Ratios 3.61* 2.69* 1.37 1.00 0.94 * P<0.05 Model included age, education, income, working status, health status, comorbid condition, treatments received, stage at diagnosis, and number of severe symptoms. Reasons for Unmet Need by Race/Ethnicity Patient Report of Black/Hisp Span/Other N=54 White/Hisp Eng N=117 Pvalue MD didn’t think Rx would benefit patient 27 14 0.0056 MD didn’t know about Rx 20 11 0.035 MD didn’t know about problem 37 30 0.2397 MD didn’t appreciate how much problem was bothering patient 17 14 0.4651 Conclusion Prevalence of unmet need varied by type of symptom. Black and Hispanic Spanish-speaking women were less likely to report having a symptom and more likely to report an unmet need. Among women with an unmet need, more black, Hispanic Spanish-speaking, and other women reported the reasons as the MD did not think treatment would benefit her and the MD did not know about treatments. Limitations Survey relied on patient self-report of severe symptoms, and the variability of symptom severity among patients was not determined. Results are not generalizable to premenopausal women. Asian American women 60-75 years of age were allocated to another study and not able to be included. Implications for Practice and Policy Symptoms cannot always be cured but can be managed. Providers should systematically evaluate symptoms and their effects on function and quality of life. Research continues to highlight the need to address the causes of unequal treatment