INTRODUCTION Therapy Disruptions and Physical Restraints in ICU Settings: Implications for Quality Initiatives
advertisement

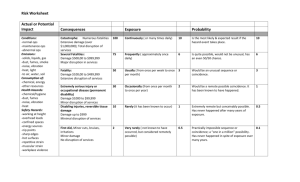
INTRODUCTION Therapy Disruptions and Physical Restraints in ICU Settings: Implications for Quality Initiatives Lorraine C. Mion, PhD, RN, FAAN Ann F. Minnick, PhD, RN, FAAN Rosanne Leipzig, MD, PhD Cathy Catrambone, DNSc, RN Mary E. Johnson, PhD, RN • JCAHO, CMS, and FDA minimize use of physical restraint in patient care. • NQF: restraint is a nurse sensitive quality indicator. • Majority of physical restraint use in hospitals is in critical care. • ICU RNs & MDs use physical restraint to prevent patient-initiated therapy disruption of medical devices; less often to keep from falling out of bed. Funded by NIH R01 AG019715 INTRODUCTION • Few studies have examined rate, contexts or consequences of therapy disruption and/or association with physical restraint. • Society of Critical Care Medicine: more knowledge is needed to enable an evaluation of risk-to-benefit ratio of restraining versus nonrestraining interventions in ICUs METHODS • Design: Prospective prevalence • Settings: 49 adult ICUs from 39 hospitals selected at random from 6 geographic areas of U.S; average daily census > 99 – – – – – – Texas New York Illinois Colorado Ohio Arizona OBJECTIVES • To describe the rate and contexts related to TD in ICUs • To examine factors associated with TD rates in ICUs • To describe the consequences of ICU TD to patient and staff Variables • Outcome Variable: disruption Types and rate of therapy – Rate = (# therapy disruption episodes/total patient days) x 1000. • Unit-Level Contextual Variables: Census, proportion of days: men, physical restraint (excludes side rails), ventilator, and elderly. • Patient-Level Contextual Variables: Demographics, cognition, sedating medications, presence of restraint at time of disruption. DATA COLLECTION PROCEDURES Variables (continued) • Patient Consequences: Adverse events as direct consequence of TD (e.g., hemorrhage) • 2003 - 2005 • Trained ICU RNs, daily rounds • Therapy disruption ascertainment – nurse initiated reporting card – daily interview with nurses – chart abstraction. • Chart abstraction to describe disruption episode, patient contextual variables, and consequences. • Staff Consequences: Unprotected exposure to body fluids, violence or physical harm. • Resource Consequences: Additional resources (procedures, therapies) as direct consequence of the therapy disruption Rates of TD Episodes and Devices RESULTS • # patient episodes with one or more TDs: 1,097 TD episode rate: 22.1 episodes/1000 days (0 to 102.4) • Rates by ICUs: • ICU Profile: 49 ICUs: size 8 – 42 beds: 26 General, 12 MICUs, 11 SICUs - General = 23.6 • Number of Patient-Days: 49,482 Unit range: 172 – 2,155 patient-days - 0.51 to 0.02 - 0.37 to 0.19 - 0.37 to 0.20 - 0.28 to 0.29 General = 33.1 Surgical = 26.0 Patient Factors At Time of the Disruption (N = 1,097) Correlation of Unit-Level Risk Factors with Unit-Level TD Rate 95% CI Surgical = 16.1 • # devices terminated/disrupted: 1,638 • TD device rate: 33.1 devices/1000 days (0 to 168.9) • Rates by ICUs: – MICU = 39.8 Variable r-value (Proportion of days accounted for by) Ventilator: r = - 0.26 Men: r = - 0.10 Age 65+: r = - 0.09 Restraints: r = 0.01 MICU = 23.4 • • • • Age: 63.2 (± 17.7) Range: 11 – 98 years Men: 57% Day shift: 46% Restraint at the time: 45% • Alertness/Cognition – Lethargic 27% – Agitated/anxious 58% – Disoriented 54% • Occurred with patient fall 1.7% Patient Factors At Time of the Disruption (N = 1,097) Percentage of episodes Most Frequently Disrupted Devices (N = 1097 episodes) • Medications 24 hours prior: – – – – Narcotic 43% Benzodiazepine 34% Neuroleptic 14% Neuromuscular blocking agent 1.6% – Any of above: 25 20 15 10 5 0 NG 70% Device Restart Rates (> 40%) Percentage of Devices 30 en yg Ox * IV Te le* T ET Patient Consequences: Harm as Direct Result of Disruption (N = 1,097) 100 • None noted: • Minor: 80 60 77.2% 15.9% – No therapy or treatments required (bruising) • Moderate: 40 6.0% – Requires therapy, but harm not life threatening (e.g., sutures) 20 • Major: 0 le en Te xyg O IV ley AP ing Fo CP ress D NG ctio a Tr n T ne EG ET l Li P tr a n Ce • Deaths: -0- Additional Treatment/ Resources Staff Consequences • Unprotected exposure to blood/body fluids 74 ( 7%) • Experienced violence (hitting, kicking, etc) 30 ( 3%) • Physically injured 15 ( 1%) 0.9% – Major medical/surgical procedures (e.g., blood transfusions) • • • • • • • • Additional/new restraints Additional/new sedation X-ray/imaging Increased monitoring Dressings Consultations Surgical procedure Labs 320 (29%) 219 (20%) 140 (13%) 84 ( 8%) 69 ( 6%) 42 ( 4%) 38 ( 3%) 31 ( 3%) CONCLUSIONS • TD not rare but varies among units • No significant relationship by proportion of men, elderly, ventilator, or use of physical restraint • Most experience no harm, but clinically significant number incur minor to moderate harm and/or need device restarted • Further study to examine patient- and unitrisk factors