Background Impact of an antidepressant adherence program in a managed care organization
Impact of an antidepressant adherence program in a managed care organization
Kara Zivin Bambauer, PhD
Stephen Soumerai, ScD
Alyce Adams, PhD
Fang Zhang, PhD
Rick Weisblatt, PhD
Neil Minkoff, MD
Andrea Grande, RPh
Dennis Ross-Degnan, ScD
Harvard Pilgrim Health Care and Harvard Medical School
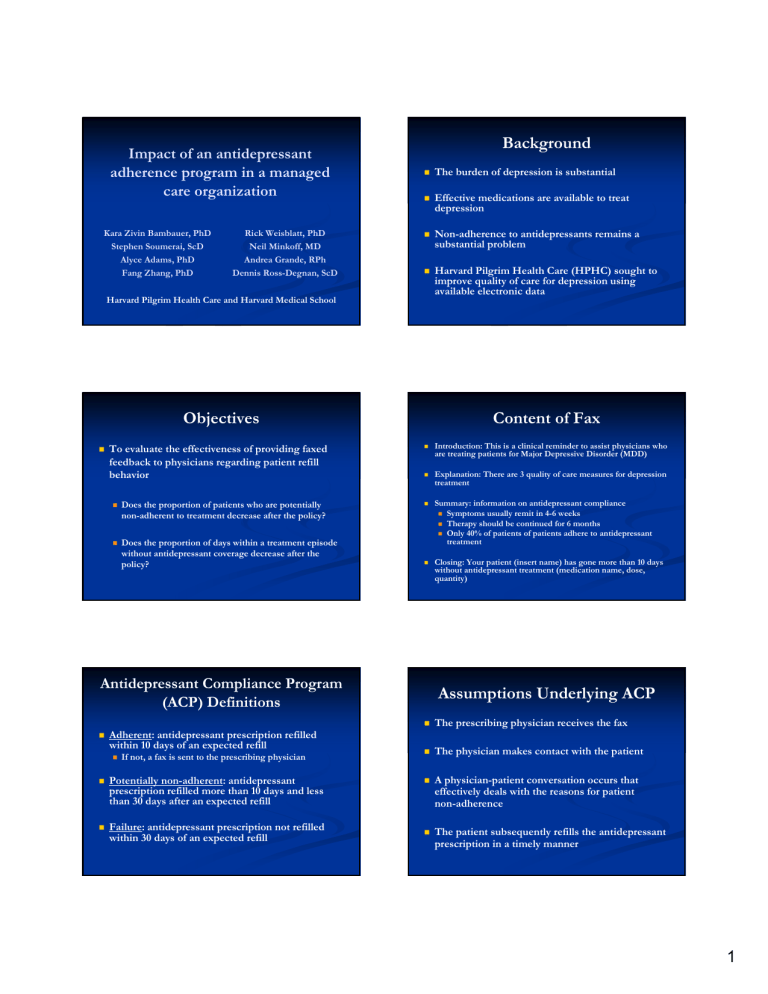
Background
The burden of depression is substantial
Effective medications are available to treat depression
Non-adherence to antidepressants remains a substantial problem
Harvard Pilgrim Health Care (HPHC) sought to improve quality of care for depression using available electronic data
Objectives
To evaluate the effectiveness of providing faxed feedback to physicians regarding patient refill behavior
Does the proportion of patients who are potentially non-adherent to treatment decrease after the policy?
Does the proportion of days within a treatment episode without antidepressant coverage decrease after the policy?
Content of Fax
Introduction: This is a clinical reminder to assist physicians who are treating patients for Major Depressive Disorder (MDD)
Explanation: There are 3 quality of care measures for depression treatment
Summary: information on antidepressant compliance
Symptoms usually remit in 4-6 weeks
Therapy should be continued for 6 months
Only 40% of patients of patients adhere to antidepressant treatment
Closing: Your patient (insert name) has gone more than 10 days without antidepressant treatment (medication name, dose, quantity)
Antidepressant Compliance Program
(ACP) Definitions
Adherent: antidepressant prescription refilled within 10 days of an expected refill
If not, a fax is sent to the prescribing physician
Potentially non-adherent: antidepressant prescription refilled more than 10 days and less than 30 days after an expected refill
Failure: antidepressant prescription not refilled within 30 days of an expected refill
Assumptions Underlying ACP
The prescribing physician receives the fax
The physician makes contact with the patient
A physician-patient conversation occurs that effectively deals with the reasons for patient non-adherence
The patient subsequently refills the antidepressant prescription in a timely manner
1
Inclusion Criteria
All HPHC members were eligible
All types of providers were included
Each patient needed to be enrolled for 6 months before and 6 months after first antidepressant use
Patients were included who used a select subset of antidepressants usually indicated for treatment of depression
New users of antidepressants (no use in previous 100 days)
First episode of antidepressant treatment for each person
Age ≥ 18
Timeline
Methods
Interrupted time-series (ITS) analysis using SAS PROC AUTOREG
Used to evaluate rates of change in adherence due to the ACP
Look at slope and level changes
ITS is one of the strongest quasi-experimental designs for studying policy changes
Characteristics of Study Participants
(N=13,128)
Mean age (sd): 42 (11)
Gender: 69% female
Policy Variables
Adherent: 18%
Potentially non-adherent: 29%
Failure: 53%
No significant differences in pre-policy and post-policy patients
Percent of Non-Adherent Patients Who Proceed to
Adherence Failure
100%
90%
80%
70%
60%
50%
Pre-ACP period
First year of
ACP
40%
30%
20%
10%
Phase-in period
0%
May-02 Aug-02 Nov-02 Feb-03 May-03 Aug-03 Nov-03 Feb-04 May-04
% w/gaps & fail model expected
Mean Percent of Treatment Days Not Covered
100%
90%
80%
70%
60%
50%
Pre-ACP period
First year of
ACP
40%
30%
20%
10%
Phase-in period
0%
May-02 Aug-02 Nov-02 Feb-03 May-03 Aug-03 Nov-03 Feb-04 May-04
% coverage model expected
2
Limitations and Implications
Electronic reminder systems, while popular, may not improve patient adherence
Success of such interventions requires a complex chain of events to occur
We cannot determine from electronic data whether communication between physicians and patients addresses reasons for patient non-adherence
Stand alone interventions targeting adherence are not successful
Conclusions
The ACP was not successful at increasing antidepressant adherence rates in HPHC members
Additional research should re-examine assumptions underlying the ACP to identify ways to improve future antidepressant adherence interventions
Effectiveness of electronic interventions should be carefully evaluated before widespread implementation
3