Prevention Guidelines and the Risk of Nursing Lifestyle -
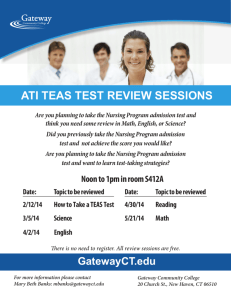
advertisement

Prevention Guidelines and the Risk of Nursing Home Admission Prevention Guidelines Clinical preventive services are “a ubiquitous part of primary care practice” practice”. LifestyleLifestyle-related risk factors Berg AO, Allan JD. Am J Prev Med 2001;20 (3 Suppl):3Suppl):3-4. Guidelines US Preventive Services Task Force National High Blood Pressure Education Program National Cholesterol Education Program Other national groups Elmira Valiyeva, Ph.D., Rutgers Louise Russell, Ph.D., Rutgers Jane Miller, Ph.D., Rutgers Monika Safford, M.D., U Alabama/Birmingham Primary: Primary: Smoking, inactivity, obesity Intermediate: Intermediate: blood pressure, cholesterol, diabetes Impact on death and disease well studied Impact on hospitalization: JE Miller, LB Russell, DM Davis, et al. Med Care. Care. 1998;36:4111998;36:411-421 Impact on nursing home admission likely, but not studied in representative populations that include the middlemiddle-aged Funded in part by AHRQ grant HS11477 NHANES I Epidemiologic Followup Study NHANES I Large nationally representative sample CommunityCommunity-dwelling adults aged 4545-74 Baseline (1971(1971-1975) largely predated current prevention campaigns Comprehensive risk factors by interview, physician exam Analysis strategy NHEFS tracked outcomes, including nursing home admission, through 1992 Cox proportional hazards regression analysis of periods of time (spells) at risk of nursing home admission MiddleMiddle-aged adults (45(45-64 at baseline) and elderly (65(65-74) analyzed separately Linked to lifestylelifestyle-related risk factors and control variables present at baseline Sample Size Age at baseline 45-64 Respondents Respondents with 1+ admission Spells at risk Spells ending in admission Person-years of observation 3,526 65-74 2,936 230 728 (6.5%) (24.7%) 3,660 3,303 282 900 58,027 37,420 1 LifestyleLifestyle-related risk factors Thresholds taken from national guidelines: Smoking: Smoking: current Inactivity: Inactivity: < very active in usual day and/or recreation Obesity: Obesity: Body Mass Index (BMI) ≥ 30 kg/m2 Blood pressure: pressure: systolic BP ≥ 140 mm Hg Cholesterol: Cholesterol: ≥ 240 mg/dl Diabetes: Diabetes: ever diagnosed by doctor Prevalence of control variables LifestyleLifestyle-related risk factor prevalence, % Risk factor Current smoker Inactive Body mass index 30+ Systolic blood pressure 140+ mm Hg Total cholesterol 240+ mg/dl Diabetes Age at baseline 45-64 65-74 38.6 19.2 51.0 64.4 17.8 18.0 42.2 65.5 41.6 48.1 4.6 8.8 (% except age) Risk factor Age in years Female Underweight (BMI <19) Heart attack/heart failure Stroke Cancer Arthritis Chronic lung disease Fracture Policy and Clinical Significance Attributable Fractions (based on NHANES III prevalences) Relative risks of nursing home admission Age at baseline 45-64 65-74 54.0 68.9 52.3 57.4 4.0 3.5 6.4 13.4 3.0 4.9 3.0 5.0 33.3 48.9 21.5 24.4 7.9 10.4 Inactive 1.40 (1.05, 1.87) 1.14 (0.92, 1.42) Body mass index 30+ 1.35 (0.96, 1.89) 1.31 (1.07, 1.60) Systolic blood pressure 140+ 1.35 (1.06, 1.73) 1.29 (1.06, 1.56) Total cholesterol 240+ 1.14 (0.89, 1.44) 0.90 (0.77, 1.06) Diabetes 3.25 (2.04, 5.19) 1.50 (1.07, 2.11) Prevention guidelines have identified risk factors, and risk factor levels, that have major impacts on the risk of nursing home admission. Prevention could reduce that risk 45-64 65-74 D ia be te s 1.32 (1.08, 1.61) BP 14 C 0+ ho le st er ol 24 0+ 1.56 (1.23, 1.99) BM I3 0+ Smoker In ac ti v e 65-74 years 18 16 14 12 10 8 6 4 2 0 Sm ok er 45-64 years Percent ( P<0.05, 95% CIs) Better quality of life. Lower costs for families and thirdthird-party payers. 2 Authors’ Authors’ affiliations Elmira Valiyeva, Ph.D. Jane Miller, Ph.D. Louise Russell, Ph.D. Monika Safford, M.D. Institute for Health, Rutgers University, New Brunswick NJ Deep South Center on Effectiveness at the Birmingham VA Medical Center and University of Alabama at Birmingham, AL 3