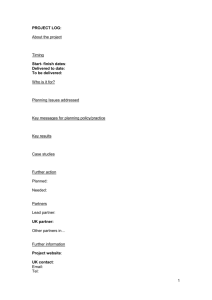
Public Health Systems
advertisement

Public Health Systems Call for Papers Towards a Better Understanding of Public Health Chair: Kristine Gebbie, Columbia University Monday, June 27 • 11:00 am – 12:30 pm ●How Americans Feel About Terrorism Security: Three Years After Sepember 11 Roy Grant, MA, Irwin Redlener, M.D., David Markenson, M.D., David A. Berman, Paula Madrid, PsyD Presented By: Roy Grant, MA, Director of Research, Research, The Children's Health Fund, 317 East 64th Street, New York, New York, NY 10021; Tel: (212)535-9400; Fax: (212)535-7699; Email: rgrant@chfund.org Research Objective: To determine, three years after the terror attacks of 9/11/01, Americans’ concern about another terrorist attack, their confidence in government and health care system to protect and respond, and their disaster preparedness. To compare results with data from our 2002 and 2003 surveys to track trends. Study Design: A survey was conducted by the Marist Institute for Public Opinion on behalf of the National Center for Disaster Preparedness (Mailman School of Public Health, Columbia University) and The Children’s Health Fund. Telephone interviews in English and Spanish were conducted between July 19th and 26th, 2004. Telephone numbers were selected based on a complete list of telephone exchanges selected to ensure that each region of the continental U.S. was represented in proportion to its population. A national random digit dial Equal Probability Selection Method using Random A methodology was used to draw the telephone numbers. Margin of error is +/- 3%. Population Studied: A nationally representative sample of 1,234 adults 18 years or older of whom 407 were parents of children 18 years or younger. Principal Findings: Three-fourths (76%) of Americans are concerned that another terrorist attack will occur in the United States. This degree of concern nationally is slightly less than the 81% level of concern in New York City. The lowest regional level of concern was in the west (71%), where no terrorist attacks have occurred. Nationally, only 39% think their own community has an adequate emergency response plan, and half (53%) are confident in the ability of the American government to protect the area in which they live from a terrorist attack. Only 39% of Americans are confident in the ability of the health care system to respond to an act of terrorism, a decline from 53% confident in 2002 and 46% in 2003. Yet two-thirds, 63%, of Americans have no family emergency preparedness plan at all. Barely one-fourth (24%) of Americans have a plan that meets the minimal criteria for preparedness, with at least two days of food and water, a flashlight, a portable radio and batteries, emergency phone numbers, and a family meeting place. Compared with identical questions and survey methodology from 2003, concern about another attack is unchanged (76%), trust in government to protect declined (53% in 2004 vs. 62% in 2003), and family preparedness is unchanged (24% vs.23%). Conclusions: There is a disconnect between concern and preparedness which constitutes a public health and disaster preparedness problem that must be addressed. The ubiquitous nature of concern of another attack where one lives indicates that there is no “psychological ground zero” where terrorism is concerned. Implications for Policy, Delivery, or Practice: Building psychological resilience is integral to terrorism preparedness. It involves active individual and family disaster planning. Making mental health services available primarily to the community that suffered the attack following an act of terrorism, as was done in New York City after 9/11, misses large segments of the affected population. Government must more effectively communicate risk and protective actions available to all citizens. Primary Funding Source: Other Foundation ●Evaluating Tuberculosis Surveillance and Action in an Urban and Rural Setting Kristine Lykens, MPA, Ph.D., Patrick Moonan, MPH, Anita Kurian, MPH, Steve Weis, DO Presented By: Kristine Lykens, MPA, Ph.D., Assistant Professor, Health Management and Policy, Unversity of North Texas Health Science Center, 3500 Camp Bowie Boulevard, Fort Worth, TX 76107; Tel: (817)735-2325; Fax: (817)735-2446; Email: klykens@hsc.unt.edu Research Objective: As a nation, we are moving closer toward Tuberculosis (TB) elimination. It is recognized that this goal will require a realignment of practices and resources by public health departments. To guide this realignment, starting in 2005, the CDC is requiring all public health departments receiving tuberculosis funds to conduct program evaluation. As part of a CDC funded project to develop a “toolkit” for TB program evaluation, CDC staff and researchers from the University of North Texas Health Science Center are developing and piloting such an evaluation model. This study examines the implementation of this evaluation model in one urban and one rural setting in North Texas. Study Design: A logic model for tuberculosis surveillance and action, developed by CDC staff provided the framework for the study. A process was developed for the public health departments involved in the project to select their most important performance indicators based upon a set of indicators developed by the Tuberculosis Epidemiology Study Consortium utilizing focus groups of program staff. Data was collected from the sites through medical record abstraction, administrative records, and interviews of key personnel. Population Studied: The population studied comprised the tuberculosis program staff, and the patients, suspects and contacts served by these programs. The urban site was Tarrant County (Fort Worth) Texas and 38 rural counties which are served by a regional office of the state health department. Principal Findings: Very different public health service delivery models for tuberculosis surveillance and action are employed in the urban and rural sites. The Tarrant County site has a centralized Tuberculosis clinic serving an urban and suburban population. Key performance indicators such as treatment completion and testing of contacts of TB suspects were very high, exceeding national and state goals. One weakness identified was in data management. The rural counties are served by sub-offices of a regional office located in Arlington, TX. Each sub-office provides a large range of services including TB to several rural counties. Initial assessments and contact investigations are conducted by public health nurses and case management is provided by them. Physicians services are provided by local primary care physicians. Directly observed therapy is conducted by the public health nurses, contracted local nurses and paraprofessionals. A statewide database for TB is used for data management. Treatment compliance rates are high but constrained by the mobility of patients, particularly immigrants, which also impact contact investigation and testing. Conclusions: Tuberculosis surveillance and action is conducted through very different delivery models in the urban and rural settings. Treatment completion is high in both settings. The centralized urban model allows for highly trained tuberculosis specialists where the rural model relies of local physicians backed up by regional tuberculosis consultants. Case management is very important in the rural setting since both public health and private providers are involved in care. Implications for Policy, Delivery, or Practice: The pilot implementation of the evaluation toolkit has been successful and adaptable to the substantially different rural and urban service delivery models. The pilot implementation is also planned for an additional large urban county and one suburban county. The primary “product” of this project is a refined evaluation “toolkit” which is adaptable to the different models of service delivery found throughout the U.S. Primary Funding Source: CDC ●Environmental Public Health Tracking: Linking Health, Environmental Hazard, and Exposure Data Ying-Ying Meng, DrPH, Rudolph P. Rull, Ph.D., Beate Ritz, M.D., Ph.D., Michelle Wilhelm, Ph.D., Marlena Kane, MSWc/MPHc Presented By: Ying-Ying Meng, DrPH, Senior Research Scientist, UCLA Center for Health Policy Research, 10911 Weyburn Avenue, Suite 300, Los Angeles, CA 900024; Tel: (310)794-2931; Fax: (310)794-2686; Email: yymeng@ucla.edu Research Objective: As part of the new national initiative on environmental public health tracking led by the Centers for Disease Control (CDC), we are developing a model surveillance system that links health effect data from a population-based survey to air pollution data from ambient monitors for identifying geographic patterns of chronic disease and environmental hazards. Study Design: Using US Census 2000 population densities at the block level, we identified the population-weighted centroid of each zip code for California Health Interview Survey (CHIS) respondents diagnosed with asthma. These centroids were linked to the nearest monitoring station within a 5-mile radius. We then estimated the annual ambient ozone and fine particulate matter (PM2.5) concentrations for each respondent. We estimated the effects of increases in annual ambient ozone and fine particulate matter (PM2.5) levels on uncontrolled asthma in the San Francisco Bay Area, San Joaquin Valley, and Los Angeles County regions of California. Uncontrolled asthma was defined as having daily or weekly symptoms or an asthma-related emergency room visit or hospitalization within the previous year. Population Studied: The population studied was 5,275 Californians, who reported that they had been diagnosed with asthma, including 1,961 from the San Francisco Bay Area, 1,502 from San Joaquin Valley, and 1,802 from Los Angeles County. Principal Findings: We observed an increase in the prevalence of uncontrolled asthma associated with ambient ozone levels in all three regions after adjusting for age, gender, race/ethnicity, poverty level, and health insurance status. For elevated ambient PM2.5 level, we only observed an increase of uncontrolled asthma for those residing in the San Joaquin Valley. The regional heterogeneity of the PM2.5 effect estimates may be related to variations in the characteristics of PM2.5. Conclusions: These findings contribute to our understanding of the role of air pollutants on the control of asthma after adjusting for individual-level socioeconomic status and access to care in different regions of California. The linkage of CHIS health data with air quality monitoring data provides a potential model for environmental public health tracking in other states. Implications for Policy, Delivery, or Practice: The environment plays an important role in our health. Many studies have linked exposures to environmental hazards with the development and exacerbation of specific diseases. However, no comprehensive systems exist at the state or national level to track many of the exposures and health effects that may be related to environmental hazards. We urgently need an Environmental Public Health Tracking system to collect and analyze non-infectious disease data and integrate that information with environmental hazard monitoring and exposure data. The availability of these types of data will enable researchers and health authorities to begin to understand the possible associations between the environment and adverse health effects. Primary Funding Source: CDC ●Increasing Influenza Vaccination and Reducing Mortality Among the Elderly Through Direct-to-Consumer Advertising Mitesh Patel, BSChem, Matthew M. Davis, M.D., MAPP Presented By: Mitesh Patel, BSChem, Medical Student, c/o Matthew Davis, M.D., MAPP, University of Michigan, 300 NIB, Ann Arbor, MI 48109-0456; Tel: (734) 615-3508; Fax: (734) 764-2599; Email: patelms@umich.edu Research Objective: Influenza-related mortality predominately and disproportionately impacts the elderly. Rates of annual influenza vaccination among the elderly are approximately 60%-65%, far below the Healthy People 2010 target of 90%. We examined the potential cost-effectiveness of a federal program of direct-to-consumer (DTC) advertising for influenza vaccine, as a method of increasing vaccination rates among persons aged 65 and older. Study Design: Published data regarding influenza-associated mortality rates and vaccine efficacy among US elderly were used to calculate the number needed to vaccinate (NNV) to prevent one all-cause death due to influenza. The NNV was then used to calculate the reduction in mortality expected from a 1% increase in the national elderly vaccination rate. Data regarding DTC advertising costs and effects for pharmaceuticals were used to inform estimates of DTC advertising costs necessary to increase vaccination rates by 1%. Published estimates of the value of one quality-adjusted life-year (QALY) and the utility of life for the average elderly person, in combination with the elderly population distribution from the Census and age-specific life expectancy for elderly persons from life tables, were used to calculate the average net present value of a life lost due to influenza mortality, discounted annually at 3%. This permitted calculation of the net present value of deaths prevented (lives saved) as a result of decreased influenza-related all-cause mortality in the setting of a 1% increase in the vaccination rate. Costs of the vaccine and vaccine administration were assumed to be covered by health insurance; adequate vaccine supply was also assumed. Population Studied: A hypothetical cohort of the US elderly population. Principal Findings: The US elderly population in 2003 was 35.9 million. For influenza among the elderly, the all-cause mortality rate was .001325 and vaccine efficacy against death was 68% (95% CI: 56%-76%). The NNV was 1110 (993-1348), resulting in 321 (264-359) elderly lives saved with a 1% increase in the vaccination rate. Based on base-case parameters of $200,000/QALY and utility=0.9 for the average elderly person, we estimated an average net present value of $1.9 million for an elder’s life lost to influenza. Total savings expected with a 1% increase in the influenza elderly vaccination rate were $610 million ($502m-$682m). At substantially more conservative parameter estimates of $50,000/QALY and utility=0.7 for a community-dwelling elder, the mortality savings were $118m ($98m-$133m). In comparison, DTC advertising would be expected to cost $30.9m to achieve a 1% increase in the elderly vaccination rate; i.e., DTC advertising for elderly flu vaccination was costsaving. Conclusions: DTC advertising regarding influenza vaccination for the elderly may represent a not only cost-effective but costsaving strategy for the federal government to pursue as a means of increasing vaccination rates. Implications for Policy, Delivery, or Practice: This is the first study to suggest potential benefits of DTC advertising in public immunization efforts. Primary Funding Source: No Funding ●From Theory to Practice: What Drives the Core Business of Public Health? Tina Smith, MPH, Chris Parker, MBBS, MPH, Beverly Tyler, Rachel Ferencik, MPA, Karen Minyard, Ph.D. Presented By: Tina Smith, MPH, Senior Research Associate, Georgia Health Policy Center, 14 Marietta Street NW, Suite 221, Atlanta, GA 30303; Tel: (404)651-0929; Fax: (404)6513147; Email: tsmith8@gsu.edu Research Objective: The Public Health Functions Steering Committee (1994) proffered a description of the Essential Public Health Services (Essential Services). There remain, however, questions about the relationship between the roles defined therein and public health practice at the state level. This research was undertaken to describe the current core business of public health in Georgia relative to the Essential Services and to elucidate the primary drivers of the core business, with a goal to better understand and address any misalignment between theory and practice. Study Design: A case study was conducted to examine Georgia’s public health system. The study design included embedded units of investigation related to district and local programs, flow of resources, stakeholder perceptions, state policies, relationships between state agencies, strategic visions, investments, and partnerships. Sources of data included interviews, focus groups, archival records, and site visits. Population Studied: The primary unit of analysis was Georgia’s $624M (2004) public health system. Individual interviews were conducted with 50 internal and external respondents including state, district, and local public health administrators, other health care providers, trade associations, legislators, agency board members, and state leaders. Focus groups were conducted in six geographically diverse communities across the state. Principal Findings: (1)The core business of public health is neither well-defined nor well-understood by internal and external stakeholders. (2)The current core business is dominated by the provision of direct services to individual patients, particularly those who are uninsured and Medicaid beneficiaries. (3)Resource utilization is significantly different from what public health leaders in the state and others in the field define as “ideal” for accomplishing the goal of improved health for the state’s population. (4)The primary drivers of the current core business of public health in Georgia were determined to be: (a)Source and categorical nature of funding; (b)Fragility of the health care safety net; (c)Rising numbers of uninsured individuals; (d)Need to measure performance and document short-term outcomes; (e)Regulatory environment; and (f)Philosophies of leadership. Conclusions: The core business of public health in Georgia is not aligned with the Essential Services. Continued growth in the number of uninsured, growing threats to the viability of safety net providers, and inflexible funding create challenges for state policy makers and public health leaders attempting to balance the Essential Services in the absence of broader state and national systemic policy interventions. Implications for Policy, Delivery, or Practice: Understanding the drivers of public health practice is essential to the development of effective public health policy and the implementation of effective public health systems. Based upon Georgia’s case study, it appears that public health systems in other states facing similar health care crises would also experience imbalance between their defined core business and the Essential Services. Broader state and national policy interventions may facilitate alignment. Findings from this research indicate the need for multi-state studies to understand (1) the drivers of the core business of public health in other states and (2) the impact on public health delivery and practice. Primary Funding Source: Georgia Department of Human Resources Call for Papers Contemporary Public Health Challenges Chair: Leslie Beitsch, Florida State University College of Medicine Monday, June 27 • 4:30 pm – 6:00 pm ●The Changing Impact of Smoking, Overweight and Obesity on Health Care Costs and Worker Absenteeism Curtis Florence, Ph.D., David Howard, Ph.D., Kenneth E. Thorpe, Ph.D., Kathleen Adams, Ph.D., Peter Joski, MSPH Presented By: Curtis Florence, Ph.D., Assistant Professor, Health Policy and Management, Emory University, Rollins School of Public Health, 1518 Clifton Road NE, Atlanta, GA 30322; Tel: (404) 727-2818; Fax: (404) 727-9198; Email: cfloren@sph.emory.edu Research Objective: Smoking, overweight and obesity have been shown to have substantial negative impacts on health outcomes. In recent years in the United States, the rate of smoking has declined, while the rates of overweight and obesity have increased dramatically. The purpose of this paper is to quantify the impact of these changes on health care costs and worker absenteeism for the employed population of the U.S. between the years 1987 and 2001. Study Design: We estimate annual number of work loss days and annual health care expenditures using the 1987 National Medical Expenditure Survey and the 2001 Medical Expenditure Panel Survey. These data contain detailed information on both of these outcomes, as well as current smoking status and body mass index (BMI). We define overweight as BMI>25 and <30, and obese as BMI 30+, using the guidelines developed by the Centers for Disease Control and Prevention. The impact of smoking, overweight and obesity on work loss days are estimated using a negative binomial regression model. The effect of these three factors on health care expenditures are estimated using a standard two-part model, where the likelihood of any expenditures is estimated by logit, while the level of expenditures are estimated by OLS with a logged dependent variable or with a generalized linear model, depending on the outcome of various specification test. We then use the predicted level of our outcomes from these regressions to calculate the attributable fraction of work loss days and health care expenditures for smoking, overweight and obesity in the two years. The changes in attributable fractions take into account both changes in the prevalence and the marginal effects of these risk factors. Population Studied: Working age adults age 18 to 64 in 1987 and 2001. Principal Findings: In 1987, 32.2% of workers ages 19 to 64 smoked, 30.3% were overweight and 13.5% were obese. By 2001, the rate of smokers had declined to 25.4%, while the rate of obese had increased to 35.4% and the rate of obese to 24.3%. We find that the decrease in smoking led to a decrease in the percentage of work loss days (12% to 9%)* and health care expenditures (6.6% to 4.0%) attributable to this risk factor. The increase in obesity is associated with an increase in attributable work loss days (5% to 7%)*, and an increase in attributable expenditures (0.6% to 6.1%)*. (*statistically significant changes at the 5% level) Conclusions: Our results show that the impact of this increase in weight has exceeded the benefits of reduced smoking (not including reductions in second-hand smoke). Implications for Policy, Delivery, or Practice: Public policy and workplace health promotion in the U.S. has focused an intense effort to lower the rate of smoking in recent years. While the rate of smoking has decreased substantially, there has been a concurrent increase in overweight and obesity. Both government and employers in the U.S. should devote more attention and resources to preventing weight gain and reducing obesity, while continuing to discourage smoking. Primary Funding Source: CDC ●Effects of Physical Activity on Medical Expenditures of US Adults Eric Keuffel, MPH Presented By: Eric Keuffel, MPH, Graduate Student- PhD, Health Care Systems Department, University of Pennslyvania, 6 Reaney Court, Philadelphia, PA 19103; Tel: (215) 546-9286; Email: ekeuffel@wharton.upenn.edu Research Objective: Regular physical activity improves clinical outcomes in coronary heart disease, hypertension, diabetes, stroke, obesity, osteoporosis, mental health disorders and other chronic conditions. While the epidemiological implications of regular physical activity (frequently defined as rigorously activity sustained for at least 30 minutes three times per week) are well-established, particularly in adults with chronic disease; the association between activity level and medical costs, even short-run medical costs, is poorly understood. Public and private health insurers may reevaluate or reconsider disease management exercise and physical activity programs on the basis of the treatment effect associated with physical activity programs. This study extends upon prior economic estimates by using cross-sectional data to quantify the effect of regular physical activity (defined as rigorously activity sustained for at least 30 minutes three times per week) on direct medical costs after adjusting for underlying health status, income, demographic characteristics and other relevant covariates. Study Design: The primary dependent variable in this analysis is log of total medical expenditures in year 2000 (excluding dental costs). Both unadjusted and adjusted regressions were conducted on cross sectional data. Independent variables in various OLS regressions generally include demographic characteristics, income, education, insurance coverage, behavioral covariates, health status measures and a dummy variable for physical activity. Health status was measured with 19 dummy variables that either reflect distinct diagnoses or conditions, summaries of domains of health and disability levels. Population Studied: The sample is comprised of Medical Expenditure Panel Survey (MEPS-Year 2000) respondents over age 17 who answered the question about whether or not they were physically active (n=17,423). The mean (median) total medical expenditure is $2,266 ($433). Unadjusted annual mean (median) medical expenditures are $2,914 ($565) for inactive adults (n=8,095) and $1,715 ($350) for active adults (n=9,328). Assuming no selection bias, initial examination of basic means and correlations are suggestive of a negative association between log medical cost and physical activity (Coeff= -.52, p<.01). The coefficient value translates into 40% lower medical costs for those who are physically active. Principal Findings: Controlling for health status and other patient characteristics eliminates the medical cost discount associated with physical activity. The association between participation in physical activity and log medical costs reverses sign and loses statistical significance (Coeff=+.07, p=.09). This effect is robust across subgroups as the same specification for those with particular types of insurance (public, private, uninsured) exhibit the same coefficient values and significance levels for the adjusted and unadjusted analyses. The effect also occurs when the dependent variable is redefined as the log of medical costs covered by insurance. Conclusions: This cross-sectional analysis suggests that short-run cost savings attributed to physical activity may be overstated in unadjusted analyses which do not account for health status of individuals. Implications for Policy, Delivery, or Practice: Public and private insurers seeking short-run returns may not benefit from cost reductions within the first year of disease management programs even if uptake is effective. Panel data over an extended time period is needed to more carefully identify the effect of physical activity on short and long run medical costs in US adults. Primary Funding Source: AHRQ, NRSA ●The Obesity Epidemic: Are Physicians Responding? Donna McAlpine, Ph.D., Amy R. Wilson, Ph.D., Anne D. Price, BA Presented By: Donna McAlpine, Ph.D., Assistant Professor, Health Services Research and Policy, School of Public Health, University of Minnesota, MMC 729, 420 Delaware Street SE, Minneapolis, MN 555455; Tel: (612)625-9919; Email: mcalp004@umn.edu Research Objective: The prevalence of overweight and obesity is increasing dramatically in the United States. Concomitantly, physicians are being called upon by major health organizations such as the United States Preventive Services Task Force to identify their obese patients and provide counseling services to help them to lose weight. This paper assesses whether physicians have responded. We examine the prevalence of obesity-related counseling (i.e., for diet/nutrition, exercise or weight loss) from 1996 to 2002. We describe the characteristics of patients, visits, and physicians that are associated with obesity-related counseling. The provision of counseling services to patients who may be most in need, including those who come to the doctor for weightrelated reasons, and those with diagnoses associated with obesity is examined. Study Design: Data come from the National Ambulatory Medical Care Survey, an annual survey of visits to nonfederally employed office-based physicians, from 1996 to 2002. We examine rates of counseling by patient (demographics, insurance, reason for visit, diagnosis), visit (duration, saw physician) and physician (specialty, new vs. established physician) characteristics. Population Studied: Analyses are restricted to visits for patients ages 18 and older. Sample sizes range from 17,542 to 24,929 over the study period. Data are weighted to adjust for non-response and to produce nationally representative estimates. Principal Findings: In 2002, approximately 14% of visits to physicians included counseling for diet/nutrition, 11% for exercise, and 4% for weight loss. For the total population, the prevalence of obesity-related counseling has not significantly changed since 1996. Patients who went to the doctor for weight-related concerns or with an obesity-related diagnosis were more likely to receive counseling for diet, exercise or weight reduction than the general population. However, even among patients who identified weight problems as the reason for visit, many were not counseled about behaviors linked to weight: in 2001/2002, 31% did not receive diet counseling, 48% did not receive exercise counseling, and 45% did not receive weight reduction counseling. Moreover, the prevalence of counseling during visits by patients with obesity-related complaints decreased significantly over the study period. Longer visits and visits with a primary care physician were associated with greater probability of obesity-related counseling. Conclusions: These results indicate discordance between what physicians are advised to do and what they report doing. Despite increasing recognition of and concern about the health consequences of obesity and the calls from major associations for increased detection and treatment, the proportion of physician visits that include counseling does not appear to be rising. Most importantly, rates of counseling appear to be declining for those most in need. Implications for Policy, Delivery, or Practice: Whether the failure of physicians to alter practice content in response to the increasing prevalence of obesity is due to competing demands during the patient-physician encounter, unease addressing weight issues or beliefs that treatment is not effective is not clear. However, the results do suggest a need go beyond medical solutions to obesity and toward environmental solutions. Primary Funding Source: No Funding ●Estimating Prevention Effectiveness: A Simulation Model Based on NHANES I and III Louise Russell, Ph.D., Elmira Valiyeva, Ph.D. Presented By: Louise Russell, Ph.D., Research Professor, Institute for Health, Health Care Policy and Aging Research, Rutgers University, 30 College Avenue, New Brunswick, NJ 08901; Tel: (732)932-6507; Fax: (732)932-6872; Email: lrussell@ihhcpar.rutgers.edu Research Objective: To make accurate estimates of the contribution of individual risk factors to population health outcomes, as a basis for estimating prevention effectiveness, analysts need to integrate information about single risk factors and diseases into a comprehensive picture of prevention and health. Each risk factor’s effect needs to be adjusted for other risk factors. This paper presents a simulation model designed to provide comparable estimates of the effects of major risk factors on mortality, hospital admissions, and nursing home admissions in a nationally representative sample of adults. Study Design: The simulation model uses projection equations that link baseline risk factors to mortality, hospital admissions, and nursing home admissions from all causes over the subsequent 20 years. The choice of risk factors in the model was based on reviews of epidemiological and medical research: all risk factors found by multiple studies to be statistically significant determinants of death and disease were included. Weibull regressions link time to death or end of followup, in days, to smoking, systolic blood pressure, physical activity, total cholesterol, body mass index, diet, and alcohol. The equations also control for age, sex, race, and conditions diagnosed at baseline, including diabetes. Negative binomial regressions link annual hospital and nursing home admissions to the same risk factors. Population Studied: Projection equations were estimated with data from the NHANES I Epidemiologic Followup Study (NHEFS), a representative cohort of U.S. adults aged 25-74 at baseline (1971-1975), whose admissions and deaths were tracked through 1992. Separate equations were estimated for six age-sex groups: men and women 25-44, 45-64, and 65-74; NHEFS excluded older persons. To estimate populationattributable fractions, the projection equations were applied to adults from NHANES III, conducted 1988-1994, which better reflects the current prevalence of risk factors. Principal Findings: First, we present tests of the model. Because decades of research document the risk factors, their statistical significance in the projection equations supports the model’s validity. Further, projection equations based on data through 1987 accurately forecast 1988-1992 mortality; hospital admissions were forecast less well due to the rapid growth of HMOs in the 1980s. Second, we present estimates of population-attributable fractions in NHANES III adults for several risk factors. For example, in NHANES III adults aged 45-74, smoking accounted for 6.4% of hospitalizations, 8.1% of nursing home admissions, and 14.5% of deaths. Comparable estimates for systolic blood pressures 140 mm Hg and over (despite treatment in some cases) were 2.3%, 3.2%, and 4.9%. Additional estimates will be included in the final paper. Conclusions: A simulation model based on two comprehensive, representative, and compatible national surveys, NHEFS and NHANES III, can provide comparable estimates of population-attributable fractions for individual risk factors. Implications for Policy, Delivery, or Practice: To set priorities for the use of prevention resources, policy makers need estimates of prevention effectiveness that are consistent and comparable. The simulation model presented here provides comparable estimates of population-attributable fractions as a basis for such estimates. Primary Funding Source: AHRQ ●Arkansas’s Response to Childhood Obesity: Update on Statewide Policy Implementation Kevin Ryan, JD, MA, Joseph W. Thompson, M.D., MPH, James E. Bost, MS, Ph.D., Jennifer L. Shaw, MAP, MPH, Margaret M. Harris, Ph.D. Presented By: Kevin Ryan, JD, MA, Associate Director for Policy and Projects, University of Arkansas for Medical Sciences, Arkansas Center for Health Improvement, 5800 West 10th Street, Suite 410, Little Rock, AR 72204; Tel: (501) 660-7584; Fax: (501) 660-7543; Email: ryankevinw@uams.edu Research Objective: In 2003, the Arkansas legislature passed Act 1220 to combat the growing epidemic of childhood obesity. Through this Act, all public schools were required to improve school nutrition, increase physical activity, and enhance awareness of obesity. Progress and challenges in implementing Act 1220 policies that may affect subsequent legislative activity in the recently opened 2005 general session are reviewed. Study Design: Act 1220 requires removal of vending machines from elementary schools, disclosure by school districts of all “pouring” contracts with soft drink companies, annual assessment by school districts of students’ body mass index (BMIs) to be confidentially reported to parents and formation of a Child Health Advisory Committee (CHAC) to set standards of nutrition and physical activity for Arkansas children. The Arkansas Center for Health Improvement (ACHI) undertook the task of measuring, collecting data, and reporting BMI to parents to comply with this legislation and has made systematic assessment of progress of other Act 1220 requirements. ACHI has systematically assessed the progress on all Act 1220 activities. Population Studied: The effected parties of this legislation include public school students and parents, schools, school districts, and healthcare professionals. Principal Findings: Act 1220 was fully implemented in the 2003-2004 school year and is now active in the 2004-2005 school year. Actions required by the Act include elimination of vending machines in elementary schools, disclosure of “pouring” contracts, and annual BMI assessments. Status assessments of these requirements are in progress. By the end of the 2003-2004 school year, BMI assessments were successfully completed and confidential Child Health Reports, including BMI-for-age, healthy lifestyle recommendations, and provider referral information, were mailed to parents. In addition, the CHAC developed recommendations for the Arkansas Department of Education for the 2004-2005 school year. These recommendations include nutrition education and standards, food service professional development, and physical activity standards. Acceptance and implementation of these recommendations will be determined in the currently active legislative session. Potential legislative changes to Act 1220 include a parental “opt-out” clause for BMI assessment that parallels other school health screenings. Conclusions: Act 1220 has enabled Arkansas to begin combating the childhood epidemic of obesity. Additional assessments regarding the effectiveness of programs developed as a result of Act 1220 are needed to inform local and national policies and programs. Implications for Policy, Delivery, or Practice: Implications of CHAC recommendations and BMI assessments also have the potential to affect health insurance coverage for obesityrelated conditions. Primary Funding Source: RWJF Related Posters Poster Session A Sunday, June 26 • 2:00 pm – 3:15 pm ●Communicating with Emergency Departments: What are the Capabilities? Angela Anderson, MPP, Gretchen Williams Torres, MPP Presented By: Angela Anderson, MPP, Research Manager, HRET/AHA, 1 North Franklin, 30th Floor, Chicago, IL 60606; Tel: (312) 422-2657; Fax: ; Email: aanderson@aha.org Research Objective: The purpose of the study is to identify the capabilities and processes emergency departments (EDs) use to communicate with local public health departments (LHDs). Study Design: Data were collected via a survey of 729 nonfederal, general hospitals with EDs in the 20 largest metropolitan areas in the United States. Respondents include ED administrators, nursing directors, and medical directors. The survey questionnaire addressed the following issues: methods of communication with the local health department (LHD); participation in various information systems, resourcesharing, and community-wide planning; and process of information dissemination. 191 (26%) of 729 hospitals responded to the survey. Data were weighted to control for potential non-response bias. Population Studied: Hospital emergency departments in the 20 largest metropolitan areas of the United States. Principal Findings: Landline communications methods (such as phone, fax, and touch tone service) were most important to EDs when communicating with LHDs (87%). 66% used webbased methods (such as email and internet site), and these were used in addition to landline methods, not to their exclusion (56% used both web and landline vs. 7% web only). With respect to EDs’ participation in disease surveillance with LHDs, 74% reported using both electronic and non-electronic systems. Most EDs (87%) had 24/7 contact information for their LHDs. Three-fourths (75%) of EDs were connected to the state’s Health Alert Network (HAN). Of these, about half receive alerts in the ED and distribute them on a 24/7 basis (54%) or have connections with the state that will work in case of circuit failure (53%). Survey respondents were asked about the EDs’ participation in four different types of information systems: 70% participated in syndromic surveillance; 65% participated in real-time bed/staff capacity at other EDs; 64% participated in community-wide resources (e.g. beds, staff, pharmaceutical) tracking systems; and 60% participated in centralized patient tracking systems. On average, EDs participated in 2.54 of these four types of information systems. One-tenth (10%) of the EDs participated in none of the four systems. Conclusions: Most EDs in major metropolitan areas rely on standard forms of communication (i.e., landline and telephone), even when they use web-based methods. The ability of EDs in large metropolitan areas to communicate with LHDs 24/7 is not universal; with significant proportions lacking contact information or being unconnected to the state’s Health Alert Network. Many of those that are connected to HAN do not receive and distribute them in the ED 24/7 basis and do not have a system that will work in the event of circuit failure. These raise the question of reliability in connecting EDs to appropriate response partners. Implications for Policy, Delivery, or Practice: Hospitals are integrating new information technologies and traditional modes of communication. This examined the communication systems of EDs in large metropolitan areas; the next challenge is to explore how EDs communicate with LHDs in smaller metropolitan and in rural areas. Primary Funding Source: CDC ●The Estimated Impact of Medicare Part D on Individuals Living with HIV/AIDS who are Dually Enrolled in Medicaid and Medicare Karyn Kai Anderson, Ph.D., MPH, MPH, William Clark Presented By: Karyn Kai Anderson, Ph.D., MPH, Social Science Research Analyst, Office of Research, Development and Information, DHHS, Center for Medicare and Medicaid Services, 7500 Security Boulevard, MS C3-20-17, Baltimore, MD 21244-1850; Tel: (410) 786-6696; Fax: (410) 786-5534; Email: kanderson2@cms.hhs.gov Research Objective: The wide array of antiretroviral treatment options is critical not only for controlling the clinical progression of HIV and AIDS, but also for preventing the spread of multi-drug resistant strains of HIV in the population. However, given that HIV/AIDS treatment medications are prohibitively costly without health insurance, public health agencies play an indispensable role. Medicaid and is one of the main sources of health insurance for individuals diagnosed with HIV or AIDS, a large fraction of whom are simultaneously “dually eligible” for Medicare, mostly due to qualifying as disabled beneficiaries under age 65. HIV/AIDS treatment medications for this dually eligible population are paid by state-specific Medicaid programs. However, next January 1, 2006 this prescription drug coverage will shift to Medicare when Part D of the Medicare Prescription Drug, Improvement and Modernization Act of 2003 (MMA) take effect. This study was conducted to estimate both the prevalence of HIV/AIDS among dually eligible individuals as well as the impact that this policy change will have on these individuals and the public health system. Study Design: This study used data from the Medicaid Analytic eXtract (MAX) database at the U.S. Department of Health and Human Services (DHHS) Centers for Medicare and Medicaid (CMS). MAX is the research-oriented adaptation of the Medicaid Statistical Information System (MSIS) administrative database. Files specific to calendar year 1999 were used since they are most recently available MAX data for all states. To attenuate typical weaknesses of administrative datasets (e.g., imperfect coding), a range of HIV/AIDS-specific diagnosis and procedure codes were used to capture as many HIV and AIDS cases as possible. The development of these criteria was informed by previous research on HIV/AIDS case-finding algorithms applied to this Medicaid database (Walkup et al., 2004; Thornton et al., 1997; Keyes et al., 1991). Population Studied: Individuals diagnosed with HIV or AIDS who are dually enrolled in Medicaid and Medicare. Principal Findings: The prevalence of HIV/AIDS among dually eligible individuals is presented nationally as well as by geographic area and state. Also presented are prescription drug utilization and expenditure findings. Taking into account the Medicaid policies that are specific to each state, a key focus of this analysis will be estimating the extent and direction to which dual beneficiaries’ cost-sharing obligations (e.g., co-pays) will shift after Medicare Part D takes effect. Conclusions: The study conclusions focus on estimated impact of Medicare Part D at both the individual level and the public health care systems level. Implications for Policy, Delivery, or Practice: The public health system has the grave responsibility of controlling the progression and proliferation of the HIV virus. With the bulk of all HIV/AIDS public health services in the U.S. managed by three major programs (Medicaid, Medicare, and the Ryan White CARE Act), it can be expected that a shift between any two is likely to have an effect on the third. This is especially true in the context of Medicare Part D given that Ryan White is the payer of last resort for HIV/AIDS care. It is hoped that the findings presented in this session will open a forum for discussion among health care analysts and decision makers. Primary Funding Source: CMS than the commensurate changes over two years (25%, p<0.10), and it is not significant in later periods. Conclusions: The benefits of physical activity for total health care costs are substantial and manifest across various sociodemographic groups, chronic health conditions and behaviors. Among people in late middle age, physical inactivity is associated with future health care costs that are on average almost a third above medical expenditure of active individuals. Given that almost every fourth American adult is sedentary, whereas late middle age people are even less active, millions of dollars could be saved in national health expenditure if Americans get more physically active. Implications for Policy, Delivery, or Practice: Physical inactivity imposes a substantial burden on the health care system. More thought is necessary in the research and policymaking world on how to promote active lifestyle and help reduce national health care costs. Primary Funding Source: No Funding Source ●Physical Activity and Future Health Care Costs among People in Late Middle Age Tatiana Andreyeva, MA, MPHil, Roland Sturm, Ph.D. Presented By: Prue Bagley, MA (Hons), Associate Lecturer, School of Public Health, La Trobe University, Bundoora, Victoria, 3086; Tel: 61 3 9479 3526; Email: p.bagley@latrobe.edu.au Research Objective: The research objective was to explore infrastructure requirements for population health services at the local level. Within Australia’s three-tiered system of government, states have, for historical and political reasons, organised the delivery of population health services in different ways. The result is a public health system with a complex and diverse organisational framework. This system is expected to both deal with existing concerns and respond to emerging issues. Whilst significant population health gains have been made, the system faces a number of challenges. Budget cuts in health have been borne disproportionately by infrastructure even as the range of what is considered population health business has expanded significantly. In this environment interest in the system’s capacity and performance has grown. The question of appropriate levels of infrastructure is a critical component of this interest. While something is known about infrastructure for population health at the national and state level, comparatively little is known about the level of infrastructure required at the local level. It is at this level that the majority of population health services are delivered through a diverse array of organisational arrangements. Study Design: To explore the question of infrastructure at the local level, senior population health managers in two Australian states were interviewed. These are Australia’s two most populace states. They also represent something of the diversity in the delivery systems for population health services. Population Studied: Senior population health managers Principal Findings: Respondents were asked to identify and reflect on the critical components of infrastructure required at the local level. These in-depth interviews revealed that senior managers have clear ideas about those elements of infrastructure they believe act as facilitators or barriers to the effective delivery of population health services, particularly in regard to systems for financing, planning and workforce development. Presented By: Tatiana Andreyeva, MA, MPHil, Doctoral fellow, RAND Graduate School, 1776 Main Street, Santa Monica, CA 90401; Tel: (310)393-0411 x6047; Fax: (310)2608155; Email: tatiana@rand.org Research Objective: The beneficial health effects of physical activity are well-established, yet commensurate differences in health care costs are less studied. This paper estimates the association between physical activity and future health care costs for a nationally representative sample of individuals ages 54-72 over 1996-2002. Study Design: The data is from the Health and Retirement Study, a nationwide biennial longitudinal survey of Americans in late middle age. The main outcome is total health care costs two and four years ahead from physical activity at baseline. Multivariate regression analysis corrects for the independent effects of socio-demographic and behavioral confounders. Sub-sample analyses include estimation across behavioral factors and chronic health conditions. Population Studied: Nationally representative adults ages 5472 surveyed over 1996-2002 (N=18,271). Principal Findings: Among adults ages 54-72 without physical limitations, active people have significantly lower average total health care costs than physically inactive individuals. In multivariate analyses, the average annual health care costs two years ahead from baseline are 29% higher for inactive persons than for active people (in 2003 dollars, $7,677 vs. $5,932; p<0.05). The increase in health care costs due to physical inactivity is higher for women (34%, p<0.05) than for men (27%, p=0.13). Across the chronic health conditions examined, vigorous physical activity is related to significantly lower future health care costs for people with cardiovascular disease, lung disease and back problems. Future health care costs are particularly high for inactive persons among smokers (33%, p<0.05). The effect of physical activity on health care costs four years ahead from baseline is less strong ●Infrastructure for Population Health at the Local Level Prue Bagley, MA (Hons), Professor Vivian Lin, DrPH Conclusions: Senior public health managers are able to readily identify those elements of infrastructure that are critical to their work. Infrastructure requirements may vary across delivery systems and organisational frameworks. The public health system is responsible for a variety of health issues and concerns. Infrastructure requirements may vary in response to these issues. Implications for Policy, Delivery, or Practice: This research suggests that diverse organisational structures may result in different requirements in terms of appropriate levels of infrastructure. In addition, it raises broader questions about reasonable expectations of a public health system. Given that this system is expected to respond to issues as diverse as disaster preparedness and the obesity ‘epidemic’, is it possible to specify what levels of infrastructure are required and what measure of capacity the system should contain? Primary Funding Source: Australian Research Council ●Building Emergency Health Workforce Surge Capacity-Reserach and Policy Analysis Marilyn Biviano, Ph.D., Atila Omer, MBA, Steve Tise, MA, James G. Hodge, Jr., JD, LLM Presented By: Marilyn Biviano, Ph.D., Director, Emergency System for Advance Registration of Volunteer Health Professionals Program, Health and Human Services, Health Resources and Services Administratiion, 5600 Fishers Lane, Room 13C-05, Rockiville, MD 20857; Tel: (301)443-0036; Fax: (301)443-4920; Email: mbiviano@hrsa.gov Research Objective: Develop comprehensive model for successful state-based Emergency Sytems for Advance Registration of Volunteer Health Professionals Study Design: Assess the entire spectrum of health professional volunteer advance registration components and policy issues and identify options and standards and definitions for advance credentialing of each health profession occupation. Then test the comprehensive model in 10 States. Population Studied: physicians, registered nurses, psychologists, clinical social workers, marriage and family therapists Principal Findings: Standards for credentialing and resource typing (per the National Incident Management System) developed for physicians, registered nurses, and behavioral health occupations. By varying the credentialing requirements through typing of health professional volunteers, emergency health personnel resources can be maximized, recruitment is improved and the cost of the states volunteer advance registry can be controlled. Conclusions: A state and regional system of advance registries of health workforce volunteers can form an effective, surge capacity that may be needed in a declared emergency. Implications for Policy, Delivery, or Practice: An effective, well thought-out set of emergency authorities and welldeveloped health professional volunteer advance registry system can provide an effective, qualified health workforce surge capacity for the state, region and nation. Primary Funding Source: HRSA ●The Integration of Hospitals into Community Emergency Preparedness Planning and Response: A National Baseline Assessment Barbara I. Braun, Ph.D., Nicole Wineman, MA, MPH, MBA, Nicole Finn, MA, Stephen Schmaltz, Ph.D., Jerod M. Loeb, Ph.D. Presented By: Barbara I. Braun, Ph.D., Project Director, Research, Joint Commission on Accreditation of Healthcare Organizations, 1 Renaissance Boulevard, DIVR, Oakbrook Terrace, IL 60181; Tel: (630)792-5928; Fax: (630)792-4928; Email: bbraun@jcaho.org Research Objective: To conduct a national baseline assessment of the existence of linkages among hospitals, public health agencies and traditional first responders in relation to community emergency preparedness. Specifically, to assess the prevalence of hospital participation in community-wide preparedness and response planning and test whether better linkages were associated with a perceived high number of community threats/hazards, experience in planning for a national event or responding to an actual event. Study Design: With input from an expert panel, a mailed questionnaire was utilized to conduct the cross-sectional assessment on linkage issues related to training and drills, equipment, surveillance, lab testing, surge capacity, incident management systems and communication mechanisms in early 2004. Population Studied: A nation-wide sample of 593 acute care hospitals. Respondents included hospital personnel responsible for environmental safety, emergency management, infection control, administration, emergency department services, quality improvement and other areas. Principal Findings: Of 1750 randomly selected general medical-surgical hospitals invited to participate, 678 agreed and 575 returned a completed questionnaire. Eighteen additional hospitals volunteered for the study. Eighty percent of responding hospitals had participated in community-wide training and 93% in drills. Fifty-eight percent had seen the community plan for distributing the Strategic National Stockpile (SNS); 27% had been involved in exercising the distribution of the SNS. Fifty-six percent had a direct electronic link into the state health alert network. Eighty-six percent of hospitals’ emergency response plans were built around an incident management system (IMS); 65% were developed in collaboration with the community emergency management agency. Multivariate logistic regression models identified factors associated with better linkages. Completion of a threat and vulnerability analysis together with community responders was associated with average daily census (ADC) and urban location. Presence of a community plan addressing acquisition of additional hospital supplies and decontamination capability was associated with prior preparation for a large scale event, but not number of community hazards, location or ADC. Sharing information among health care entities on the availability of ventilators and decontamination capacity was associated with ADC and having a high number of perceived community hazards. Sharing information on the availability of negative pressure rooms was associated with ADC, urban location and having a high number of perceived community hazards. Availability of a live answer 24/7 with public health (overall 43%) was associated with urban location. Conclusions: Responses suggesting the presence of strong linkages with the community were more commonly reported among large hospitals in urban areas, which is consistent with targeted funding for areas at higher risk. Across the sample, most hospitals are integrated, either directly or by representation, into community emergency preparedness and response planning. Nevertheless, opportunities for improving linkages exist, particularly in the areas of mass casualty logistics and communication. Implications for Policy, Delivery, or Practice: The first 72 hours of disaster response will be local. The effectiveness of hospital staff response is greatly enhanced by collaborative planning and assessment of integration into the community response process. Because this is among the first attempts to assess linkages, additional research is needed to evaluate the depth of relationships and adequacy of planning activities. Primary Funding Source: AHRQ ●Public Health Genetics: Assessing the State’s Role Gayle Byck, Ph.D., Amy A. Lemke, MS, Ph.D., Dale Lea, RN, MPH, APNG, Marianne B. Brennan, MA, Daniel Beckett, MA Presented By: Gayle Byck, Ph.D., Deputy Director, Institute for Health Research and Policy, Midwest Center for Health Workforce Studies, 1747 West Roosevelt Road, Suite 558, Chicago, IL 60608; Tel: (847)607-0319; Fax: (312)996-0065; Email: gaylebyck@comcast.net Research Objective: Advances in genetic knowledge and technology are presenting significant challenges to public health. Traditionally focused on maternal child health and newborn screening, state public health agencies are facing increasingly pressing questions about the role of genetics in all of their disease prevention and health promotion programs. At a national level, genetics/genomics has been positioned by the Institute of Medicine as one of eight key areas for public health education in the 21st century. Muin Khoury, Director of the CDC’s Office of Genomics and Disease Prevention, has argued for the integration of genetics and public health stating, “the new genetics will eventually change the face of public health.” At a local level, health departments face increasing public demand for information and services as mainstream news outlets cover stories of genetic health breakthroughs. In response, many states are re-evaluating their public health programs to determine their role in the shifting context of medical genetics. This project reports the findings of the Illinois Statewide Genetics Needs Assessment (2004), which assessed both the current status and future need for public health genetic services in Illinois, and the impact of emerging genetic information and services on the role and function of the state department of public health. Study Design: This project applied a mixed methods design, utilizing statewide surveys of genetic providers and local health department nurses, semi-structured key informant interviews with representatives of clinical genetics, general medicine and public health, and focus groups with representatives from consumer advocacy organizations. Surveys assessed genetics practice across the state and interviews and focus groups probed into issues of access, need, critical concerns, and the role of the state. N*Vivo was utilized in the analysis of the qualitative data. Population Studied: Public and private genetic service systems through samples that were drawn from five distinct populations: genetic providers (MD/PhD geneticists, genetic counselors, and genetic nurses), health care providers (representatives of general medicine and chronic disease specialties), local health department nurses (responsible for genetic or maternal/child health programs), public health administrators (from four key state agencies), and consumer/health advocacy organizations. Principal Findings: Preliminary review indicates a distinct role for the state department of public health in bridging public and private health care initiatives in genetics, addressing educational needs of the public and providers, responding to geographical and other access barriers, assuring increased screening capacity corresponds to actual availability of care, and ensuring public safety in the face of an increasingly complex array of technologies. Conclusions: This study identified a variety of clearly defined roles for state departments of public health with respect to public health genetics in the domains of education, training, service provision, surveillance, and integration. Implications for Policy, Delivery, or Practice: Genetics is becoming an increasingly central component of health promotion, care, and disease prevention. The speed with which genetics is affecting and altering the practice of health care is placing significant demands on the public and the public health system. The state department of public health will play a vital role in assuring the capacity, quality, and accessibility of future genetic services. Primary Funding Source: Illinois Department of Public Health ●State Sponsored Early Hearing Detection and Intervention Programs: Integrating Genetics Judith Cooksey, M.D., MPH, Judith Benkendorf, MS, CGC, Daniel Beckett, MA, Dale H Lea, MS, CGC, Cynthia Gordon, PhD, Helen Travers, MS, CGC Presented By: Judith Cooksey, M.D., MPH, Department of Epidemiology and Preventive Medicine, University of Maryland School of Medicine, 660 West Redwood Street, Baltimore, MD 21201; Tel: (410)706-1277; Email: jcookseyumuic@aol.com Research Objective: Severe congenital deafness, affects about one in every 500 newborns, about 80,000 babies each year. Early diagnosis and intervention enhances child’s language skills and social and cognitive development. In recent years, all states have established early hearing detection and intervention (EHDI) programs; the number of hospital newborns screened increased from 3% (1993) to 95% (2003). A striking finding is that 50% or more of these infants have a genetic basis (a gene mutation) for their deafness, yet genetics has not been a part of EHDI programs. Recent genomics advances now allow genetic testing to pinpoint the gene defect, and help guide the medical evaluation and management decisions. We studied the EHDI process to assess factors affecting the integration of genetics into established public health and medical care practice; our findings may be applicable to other new population-based screening. Study Design: An in-depth case study of the EHDI process conducted through qualitative research process using semi- structured interviews with key informants directly or indirectly involved with state sponsored EHDI programs. QSR NVivo qualitative analysis software was used to manage data, and assist with coding and analysis. Population Studied: Fifty-five key informants representing eight state health departments and two federal agencies (16), newborn nursery nurses, audiologists, speech-language pathologists (7), MD-otolaryngologists (8), clinical genetics professionals (15), and national leaders in research of hearing loss and genetics (9). Principal Findings: A conceptual framework for the five common steps in the EDHI process was developed and used to identify specific areas where genetics informants indicated genetic integration. We found varied approaches among state programs. Within health departments positive factors for stronger genetics integration included an organizational proximity between the EHDI program/staff and the state genetics program/staff; EHDI advisory committees that included geneticists; staff education on genetics; and combined reporting of newborn screening results by hospitals for both hearing screening and metabolic screening. Otolaryngologists varied across a spectrum of strong to weak interest in genetic evaluation as part of their medical evaluation. Factors that positively influenced genetics evaluation included their personal experience with referrals to geneticists, the level of genetics exposure during training, and the perspectives of leaders within their profession. Genetics research leaders predict that genetic evaluation and testing will be integrated into the medical evaluation step of the EDHI process. However, there were mixed opinions on integration of genetic testing into the newborn screening step. They noted that ongoing population-based research would help provide needed data on the population genetics of congenital deafness. However, several researches expect CHIP technology that tests for multiple gene defects may be available and affordable shortly. Conclusions: State EHDI programs have varied organizational and staffing arrangements and have limited genetics perspective or programmatic integration. Although EHDI programs do appear to be potential emerging areas for genetics services. Implications for Policy, Delivery, or Practice: Public health EHDI programs, like other several other public health programs for children with specific conditions (birth defects surveillance, Children with Special Health Care Needs), generally omit genetics evaluation from program design, despite a high prevalence of an underlying genetic cause for the condition. A better understanding of the process from multiple perspectives may guide efforts to bring useful genetics to these programs and improve patient and family outcomes. Primary Funding Source: HRSA, NHGRI-ELSi ●Evaluating Public Health Preparedness: Are We There Yet? Margo Edmunds, Ph.D. Presented By: Margo Edmunds, Ph.D., Adjunct Associate Professor, American Institutes for Research, Johns Hopkins Bloomberg School of Public Health, Department Health Policy and Management, 10720 Columbia Pike, Silver Spring, MD 20901; Tel: (301) 592-3373; Email: medmunds@air.org Research Objective: This evaluation was designed to assess regional communications and technology use during a twoday bioterrorism field exercise conducted in a mid-Atlantic metropolitan area during the summer of 2003. The evaluation produced recommendations for regional leaders in several cross-cutting areas, including interagency technology planning, mutual aid agreements across jurisdictions and organizations, and future training activities. Study Design: A multi-agency evaluation team met regularly for several months to develop a protocol for the evaluation and followed guidelines issued by the Department of Homeland Security in March 2003. The team developed a secure, Web-based survey tool that was completed by 86 trained evaluators who were observing response teams in a variety of field locations during the two-day exercise. Using a simple checklist format, the tool assessed the management of information flow, use of various kinds of communications equipment and devices, the availability of contact and other needed information, interactions with the media and the public, and other areas of activity. It also included an openended section for commentary and suggestions. All data were anonymized and aggregated to ensure that individuals and specific agencies were non-identifiable in the After Action Report. Population Studied: More than 1,200 people from dozens of agencies participated in the exercise, including a local elected official; state and local health departments; hospitals; other healthcare providers (clinics and a community health center); several other government agencies, such as transportation and public works; universities; and other private organizations. Principal Findings: On average, exercise participants had about 60% of the contact information they needed and actually reached about 40% of their target contacts. Few participants other than first responders relied on pre-existing response plans or protocols, such as Incident Command Systems (ICS). In general, response strategies were guided by verbal agreements among personnel who had worked together previously, and in 30-40% of the health departments and hospitals, there were no back-up personnel. Needs for information technology and equipment upgrades and training were widely noted. Conclusions: Evaluators commented on the high levels of professionalism they observed among the exercise participants, as well as the ingenuity of those who were able to work around problems they found. The exercise yielded timely and useful information, and much of it was actionable immediately. Exercising is a useful test of strengths and gaps in capacity and skills, with the added benefit of increasing regional awareness and support for coordinated all-hazards planning, training, and technology investments. Implications for Policy, Delivery, or Practice: Current CDC bioterrorism funding to states emphasizes the importance of drills and exercises, and jurisdictions that have conducted exercises are encouraged by U.S. Department of Homeland Security guidelines to disseminate lessons learned and promising practices. By sharing information about exercise design and evaluation, this presentation could assist with preparedness planning and capacity building among other agencies and organizations. Primary Funding Source: CDC, AHRQ, HRSA, several state and local agencies ●Economic Evaluation of HIV Rapid Testing Programs Paul G. Farnham, Ph.D., Angela B. Hutchinson, Ph.D., MPH Presented By: Paul G. Farnham, Ph.D., Associate Professor, Economics, Georgia State University, 14 Marietta Street NW, Room 531, Atlanta, GA 30303; Tel: (404) 651-2624; Fax: (404) 651-4985; Email: pfarnham@gsu.edu Research Objective: Although the annual number of new HIV infections cases has remained relatively constant at 40,000 and AIDS deaths at 16,000 since 1998, policy makers have been concerned about increases in HIV incidence in some communities. Many HIV-infected individuals do not get tested until late in their infections, and an estimated 25% of infected individuals are unaware of their serostatus. The development of new rapid HIV tests, such as OraQuick, which can be performed outside clinical settings and provide results in 20 minutes (though persons who test positive must return to the testing center for confirmatory results), offers new opportunities for individuals to learn their serostatus and gain access to prevention and treatment services. Because numerous questions exist regarding the costs and impacts of implementing rapid testing in various settings, this paper analyzes the economic evaluation studies of HIV rapid testing to summarize their results for policy makers. Study Design: This paper reviews economic evaluation studies from 1995 to 2004 focusing on the costs and effects of HIV rapid testing in various settings to catalog the assumptions, methodology, and results of the studies. Studies were selected through searches of several large electronic data bases, including AIDSLINE, Medline, and PsycINFO, using combinations of the following key words: HIV rapid tests, HIV counseling and testing, costs, costeffectiveness, HIV prevention, AIDS prevention, and HIV infection. Only peer-reviewed journal articles discussing interventions in the U.S. were included. Studies of mandatory HIV counseling and testing were excluded. Population Studied: HIV rapid testing programs in the following settings: HIV testing centers, sexually transmitted disease (STD) clinics, emergency departments and urgent care centers, and outreach settings. Principal Findings: Key variables in all of the studies were: the amount of time spent in pre- and post-test counseling sessions; the costs of screening and confirmatory tests; transportation, travel, and wait times; test sensitivity and specificity; seropositivity rates; and the probability of both infected and uninfected individuals receiving preliminary screening and confirmatory test results. Conclusions: In general, rapid testing procedures that provide results at the initial time of testing are more costeffective than conventional HIV testing programs that require a follow-up visit to obtain test results. Clients tested with rapid tests are more likely to receive their results than those with conventional testing. This conclusion is typically the strongest for HIV-uninfected clients, many of whom would not have returned to receive their test results with conventional testing. Implications for Policy, Delivery, or Practice: Because the use of rapid HIV testing typically eliminates the need for a return visit to learn test results, hospitals, health departments, and health care providers should increase their use of this testing process so that more individuals receive their test results and learn their HIV serostatus. These changes will help HIV-infected individuals access treatment and care for their illness and will further prevention efforts for both infected and uninfected individuals. Primary Funding Source: CDC ●The Effect of Workplace Smoking Restrictions on Cigarettes Consumed, Worker Absenteeism and Health Care Utilization Curtis Florence, Ph.D., Kathleen Adams, Ph.D. Presented By: Curtis Florence, Ph.D., Assistant Professor, Health Policy and Management, Emory University, Rollins School of Public Health, 1518 Clifton Road NE, Atlanta, GA 30322; Tel: (404) 727-2818; Fax: (404) 727-9198; Email: cfloren@sph.emory.edu Research Objective: Cigarette smoking has well known negative impacts on the health of both smokers and nonsmokers who are exposed to second-hand smoke. These adverse health effects have lead governments and employers to restrict, and in some cases ban, smoking in public areas. The effect of these restrictions in terms of reducing exposure to cigarette smoking and improving health outcomes is not well understood. This study examines the impact of workplace smoking restrictions on smoking and health outcomes for workers in the United States. Study Design: The National Health Interview Survey (NHIS) is used to gather nationally representative information on health status and health care utilization. The survey also gathers information on health risk factors such as cigarette smoking. In 1998, the NHIS contained a special prevention supplement which gathered information on workplace health promotion. Included in this supplement were questions on whether or not smoking was allowed in the workplace. If smoking was allowed, questions were asked concerning any restrictions on smoking in the workplace, such as limiting it to certain areas. This data is used to determine the percentage of workers who have a workplace smoking restriction. The effect of these restrictions is then found by estimating regression models for the following outcomes: the number of cigarettes smoked per day (conditional on smoking), the number of work days missed due to illness, and the likelihood of visiting a doctor or emergency room. The results show the impact of the smoking restrictions on both smoking behavior for smokers and health outcomes for all workers, therefore incorporating the effects of any reduction in second hand smoke exposure. Population Studied: Workers age 18 to 64 in 1998. Principal Findings: In 1998, 70.4% of workers had a workplace smoking ban, 14.1% had a workplace where smoking was limited to certain areas, and 15.5% had a workplace where there were no restrictions on smoking. 24.1% of workers reported being current smokers. Smokers who face a workplace ban smoke 8% fewer cigarettes a day than smokers who have no workplace restrictions. Smokers who face restrictions, but not bans, do not have significantly lower cigarette consumption than those who face no restrictions. Smokers who have some workplace restriction (either a ban or more limited restriction) have on average one less work day per year missed to illness, and have fewer doctors’ office and emergency room visits, than smokers who face no workplace restriction. Workplace smoking restrictions are not shown, however, to impact lost work days or health care utilization for non-smokers. Conclusions: Public policy and workplace health promotion in the U.S. has focused an intense effort to reduce exposure to cigarette smoke in the workplace. These restrictions help to reduce the number of cigarettes smoked by current smokers, and to improve health outcomes for smokers. The results of this study do not indicate, however, that workplace smoking restrictions also have positive health effects for non-smokers. Implications for Policy, Delivery, or Practice: These results suggest that future policy changes should focus on eliminating opportunities for smokers to smoke while at work to improve the health outcomes of smokers. Primary Funding Source: CDC ●The Role of Public Hospitals in an Era of Emerging Infectious Diseases- Taiwan’s Experience During the SARS Epidemic Yea-Jen Hsu, MS, Yiing-Jenq Chou, M.D., Ph.D., Shu-Fang Shih, MS, Nicole Huang, Ph.D. Presented By: Yea-Jen Hsu, MS, Research Assistant, Department of Social Medicine, National Yang Ming University, 155 Li-Nong Street, Section 2, Taipei, 112; Tel: 8862-28201458; Fax: 886-2-28261002; Email: yjhsu@ym.edu.tw Research Objective: The uproar of privatization and the declining availability of resources raise a series of debates on the role of public hospitals in today’s health care system. As privatization likely allows public hospitals to gain operating efficiency and effectiveness, many start to challenge the existence of public hospitals. Opponents of privatization defend the survival of public hospitals for these hospitals’ charitable and public missions. Previous studies have centered on the associations between hospital ownerships and quality of care, health care spending, and the effect of ownership type on firm conduct in hospital markets under regular situation. However, as we are facing an increasing number of emerging deadly infectious diseases, surprisingly, relatively little systematic attention has been devoted on the role of public hospitals in serving the needed under a large outbreak or other public emergency. It is important to consider how ownership would affect hospital’s responses during a large outbreak or public emergency, especially when public interests conflicts with financial interests of hospitals. The outbreak of the severe acute respiratory syndrome (SARS) in Taiwan in 2003 and the comprehensive data available offer an unique opportunity to evaluate whether hospital ownership plays any role in determining the provision of care to SARS patients in Taiwan during the SARS epidemic. Study Design: This study is a population-based descriptive study. Chi-square tests were used to test the difference of inpatient capacity, number of patients with infectious diseases treated, and the number and severity of SARS patients treated between public and private hospitals. Population Studied: All 3,005 reported SARS cases during the outbreak from March to July 2003 were observed. The National Health Insurance claims files and the hospital registry were two main data used. Principal Findings: Public hospitals treated 58% of total reported SARS cases, and 63% of the probable and suspected SARS cases while non-profit hospitals shared 31% and 27%, and private hospitals were only cared 11% and 10%. Compared to their market shares in all inpatients services (30%) or other infectious diseases (28%) under regular situations, public hospital took on exceedingly greater burdens by treating more and severe SARS patients during the epidemic. The differences were statistically significant. Conclusions: Due to the public’s fears of SARS, non-SARS patients avoided seeking care from the hospitals treating SARS patients and these hospitals could lose market shares in either outpatient or inpatient services. Under the emergency situation whereas public interests conflict with financial interests of hospitals, public hospitals were found to take on the major responsibility for treating SARS patients during the SARS epidemic. Implications for Policy, Delivery, or Practice: Over the past decades, government subsidies to public hospitals have been decreasing. According to the results of our study, public hospitals played a major role in nation’s response system to major outbreaks such as the SARS epidemic, while non-profit and private hospitals only shared small portions of the burden. Public hospital’s prompt responses to their public missions during such large outbreaks should not be overlooked in the discussions of privatization. Primary Funding Source: National Science Council ●How is Excess Body Weight Related to Health Service Utilization? I-Chan Huang, Ph.D., Albert W. Wu, M.D. Presented By: I-Chan Huang, Ph.D., Post-doctoral fellow, Health Policy and Management, Johns Hopkins University, 624 N Broadway, Room 663, Baltimore, MD 21218; Tel: (410)949-4238; Email: ichuang@jhsph.edu Research Objective: Studies have examined the impact of excess body weight on mortality, health-related quality of life, and cost. However, relatively little is known about the effects on health services utilization, and by what mechanism they may be related. We examined relationships of overweight and obesity to health service utilization using a sample from Taiwan. Study Design: This was a cross-sectional study. Body weight was classified using WHO Asian-Pacific body mass index definitions (BMI in kg/m2): normal (18.5-22.9), overweight (23-24.9), and obese (>=25). Utilization includes outpatient visits, hospitalization, emergency room visits, dental services, traditional Chinese medicine, and chiropractic services. For binary outcomes (e.g., use vs. none in the past month), we used logistic regression to examine the body weight-utilization relationships. For continuous outcomes (e.g., intensity of use), we used Tobit model that takes into account the skewed distribution of utilizations. In multivariable models, we adjusted for patient covariates including age, gender, education background, smoking status, chronic conditions, and self-reported heath status (SF-36 PCS and MCS). We used Sobel tests to examine whether chronic condition and health status mediate the relationships between body weight and utilization. Population Studied: A nationally representative adult sample (n=13,179) collected from the 2001 Taiwan National Health Interview Survey. Principal Findings: In this Taiwan sample, 49.7% were normal weight, 21.7% were overweight, and 28.5% were obese. In unadjusted results, obese people used more outpatient services, hospitalization, and emergency room visits than overweight and normal weight people (all P<0.05). For example, 40.1% of obese vs. 36.7% of overweight and 32.6% of normal weight visited a primary care physician during the past month. However, after adjusting for covariates, utilization patterns were similar among BMI groups for all types of health services (P>0.05). Sobel tests suggested that chronic conditions and physical health significantly mediate the relationship between body weight and utilization, particularly for outpatient visits, hospitalization, and emergency room visits (all P<0.05). The mediating effects were strong for people with hypertension, hyperlipidemia and coronary heart disease. Stratification by number of chronic conditions suggested that obese people with more chronic conditions utilized more outpatient, hospitalization, and emergency room visits than other subjects. However, overweight subjects with more chronic conditions tended to utilize more dental services, tradition Chinese medicine, and chiropractic services. Conclusions: Obesity and overweight are related to significant increases in various types of health services utilization. The influence of body weight on service utilization appears to be mediated by chronic conditions. Implications for Policy, Delivery, or Practice: Better management of chronic conditions for people with excess body weight may help to reduce the health services utilization. Primary Funding Source: No Funding Source sets used. MEPS is a nationally representative survey that includes data about medical spending, insurance status, and sociodemographic characteristics. NHIS captures height and weight, used to determine the Body Mass Index (BMI). The MEPS sampling frame is drawn from the previous year's NHIS. We created a unique person level file by merging MEPS data for the 1996 to 2000 years with the related NHIS data. A four-equation regression approach was then used to predict annual overweight- and obesity-attributable medical spending. The regressions included each person's BMI category, insurance category, and sociodemographics. Population Studied: Adults in the southern states, including Alabama, Arkansas, Florida, Georgia, Kentucky, Louisiana, Mississippi, North Carolina, South Carolina, Tennessee, Virginia, and West Virginia. The final sample included 20,307 adults. Principal Findings: Between 1996-2000, 36% of adults in the south were overweight and 19% were obese. Prevalence of obesity was highest among Medicaid enrollees (27%). per capital spending increase attributable to overweight was $261 (9.7%), inflated to 2003 dollars, and ranged between $78 for the uninsured and $414 for Medicare. Per capita spending increase attributable to obesity was $832 (30.3%) and ranged between $209 for the uninsured and $1,497 for Medicare. Aggregate spending attributable to overweight and obesity combined was $25.4 billion (8.5% of total spending) and ranged between 7.7% for Medicare and 9.9% for Medicaid. Conclusions: States and the federal government are paying heavily for obesity and its care. Implications for Policy, Delivery, or Practice: Much of the morbidity and mortality associated with obesity could be prevented through actions of the public health system to increase physical activity and promote healthy eating habits. State public health systems should use the findings to justify and further their efforts in the fight against obesity. Primary Funding Source: Southern Rural Development Center ●Overweight and Obesity Related Medical Spending in the South: Impact on Payers Amal Khoury, Ph.D., MPH, Jerome Kolbo, Ph.D., Wendy Bounds, Ph.D. ●How HMO Market Penetration Rates Affect Older Adults’ Prevention Behaviors Ying-Chun Li, Ph.D., Edward C. Norton, Ph.D. Presented By: Amal Khoury, Ph.D., MPH, Associate Professor, Health Services Research, Management & Policy, University of Florida, PO Box 100195, Gainesville, FL 32610; Email: akhoury@phhp.ufl.edu Research Objective: Two out of three US adults are overweight or obese. Prevalence of obesity has increased in the last two decades. Obesity is associated with several serious and costly chronic conditions and poses substantial challenges to the health of Americans, state budgets, the public health system, the healthcare system, and employers. Obesity rates are particularly high in the southern states, which also have fewer public health resources and tighter state budgets than other states. The objective of this study is to estimate medical spending attributable to overweight and obesity in the south for adults overall and for payers, including Medicaid, Medicare, private insurance, and out-of-pocket payments (which include payments by the uninsured). Study Design: The Medical Expenditure Panel Survey (MEPS) and the National Health Interview Survey (NHIS) are the data Presented By: Ying-Chun Li, Ph.D., Research Associate, Health Policy and Management, Harvard School of Public Health, 124 Mount Auburn Street, South 410, Cambridge, MA 02138; Tel: (617) 496-8851; Fax: (617) 496-8833; Email: ycli@hsph.harvard.edu Research Objective: Clinical prevention can reduce premature mortality for older adults, however, the observed rates of prevention services vary widely across states. We test the hypothesis that HMOs, which have a strong interest in providing prevention services, increase population rates of prevention services and thereby explain the variation across states. Furthermore, we predict that HMOs have both a direct and indirect effect influencing people's prevention behavior. Increased prevention by HMO enrollees may spillover to nonHMO enrollees either through changes of provider practice pattern or people's seeking care behavior. Study Design: This study evaluated six clinical prevention services (influenza vaccination, pneumococcal vaccination, mammography, pap smear test, colorectal cancer screening, and cholesterol screening) for older adults. We estimated separate logistic models with state fixed-effects for each of six clinical prevention utilizations. State HMO penetration rates were adjusted into quartile indicators for each observation. Population Studied: Two national data sets were linked at the state level. Individual-level information about the clinical prevention utilizations of 556,044 noninstitutionalized older adults were from Behavior Risk Factor Surveillance System 1994-2002. The state HMO penetration rates were measured based on information from the National Center of Health Statistics. The study assessed the clinical prevention utilization in past 12 months and ever had such service by elderly persons and aged 50–64 groups. Principal Findings: State HMO penetration rates have a significant positive effect on the probability of receiving most of the studied clinical prevention services. However, the positive HMO effects are stronger for older adults who ever had clinical preventions. One of the most significantly positive results is associated with vaccinations for elderly persons. Compared to people live in the lowest HMO penetration quartile areas, those elderly persons who live in the highest HMO penetration areas have a 70 percent higher probability of receiving an influenza vaccination in past 12 months or five times higher probability of ever having a pneumococcal vaccination. The magnitudes of the positive HMO effects on vaccinations for elderly persons are consistently higher for persons living in areas with higher HMO penetration. Conclusions: The empirical results support our hypotheses that HMO spillover effects may influence the clinical prevention utilization by older adults, but the positive HMO effects may not consistently exist in different HMO penetration quartiles for all of the studied clinical preventions. Implications for Policy, Delivery, or Practice: The results show that the rapid expansion Medicare beneficiaries into HMOs during the 1990s may have had positive health benefits for both HMO and non-HMO enrollees under public health system, at least for those living in areas with high HMO penetration. Primary Funding Source: No Funding Source ●Analysis of Vaccines for Children Quality Assurance Survey Data Pamela Mathison, MA, BSN, Lori Rizzo, MBA, BSN, Karen Hess Presented By: Pamela Mathison, MA, BSN, Senior Health Services Consultant, Business Development, Texas Medical Foundation, Barton Oaks Plaza Two, Suite 200, 901 Mopac Expressway South, Austin, TX 78746; Tel: (512) 329-6610; Fax: (512) 328-2921; Email: pamm@tmf.org Research Objective: 1. Utilize data abstracted from quality assurance site surveys at enrolled Vaccines for Children (VFC) providers over multiple years to assess the impact of VFC site visit feedback and education. 2. Utilize site survey data to identify significant indicators and trends that could affect provider-based immunization rates and determine the educational needs of providers. Study Design: Under contract with the Texas Department of State Health Services, the Texas Medical Foundation (TMF) has conducted quality assurance site visits for providers since September, 2001. The major purposes of the Vaccines for Children (VFC) site visits are to: 1. Improve the quality of immunization practices in VFC provider sites, 2. Increase the immunization levels in children under two years of age, and 3. Fulfill Centers for Disease Control and Prevention (CDC) contract/grant requirements. Feedback about site survey results is provided during the site survey, along with education and resources for quality improvement of immunization practices and immunization rates. In March, 2002, TMF staff implemented use of a newly-developed electronic site survey tool by TMF reviewers performing the site visits. This tool was used by TMF reviewers for 830 site surveys in 2002; for 2,408 surveys during 2003; and for 2,405 surveys during 2004. The electronic tool was also used by local and state health department staff in 2004 for an additional 222 site surveys conducted at public health department and Women, Infant and Children (WIC) clinics enrolled in the VFC Program. Data was drawn from these surveys for statistical analyses. Population Studied: The target audience for the quality assurance site surveys was providers enrolled in the Texas Vaccines for Children Program. While the vast majority of enrolled providers are private practice physicians, other types of VFC providers include public and private hospitals, local and state public health clinics, WIC providers, Federally Qualified Health Centers, Rural Health Centers, public and private schools, colleges and universities, pharmacies, local and state youth correctional facilities, and mobile clinics. Site visits are conducted every 9-15 months on all enrolled providers, beginning at least six months after they receive their first shipment of VFC-supplied vaccines. Principal Findings: Results indicate notable improvements in provider performance over time on immunization rates and several indicators of compliance with VFC regulations or recommended immunization practices. However, there were some reversions and variances that posed interesting questions to be addressed by further investigation. Conclusions: Quantitative analyses, coupled with other inputs (e.g., provider feedback), has provided indications of the site survey effectiveness. However, because quality assurance site visits are a once-a-year event and other variables could influence provider performance, a direct cause and effect relationship based on this data cannot be assumed. Implications for Policy, Delivery, or Practice: Conducting an individualized assessment of immunization practices and immunization rates provides the opportunity to present individualized feedback and offer education, resources and motivation to make changes in the provider’s system to improve those practices and, consequently, the provider’s immunization rate. These clinic-based improvements result in a higher level of protection against vaccine-preventable diseases for the general population. Primary Funding Source: CDC ●Sexual Violence Victims: Are Emergency Rooms Ready? Stacey Plichta, Sc.D., Tancy Vandecar Burdin, MS, Rebecca Odor, MS, Shani Reams, BA Presented By: Stacey Plichta, Sc.D., Associate Professor, School of Community and Environmental Health, Old Dominion University, 105 Spong Hall, Norfolk, VA 23529; Tel: (757) 683-4989; Fax: (757) 683-4410; Email: splichta@odu.edu Research Objective: This study explores the structure and process characteristics of emergency departments (ED’s) in Virginia as they relate to assisting victims of sexual violence. A state-wise survey estimates that roughly 27,000 people per year are victims of sexual violence in Virginia, yet only 10% of women and 2.2% of men seek medical care following an assault. Sexual violence has both immediate and long-term health consequences, and appropriate early intervention is critical to the recovery of victims and their families. Study Design: All 82 publicly accessible emergency departments in Virginia were surveyed via mail with a telephone survey follow-up for non-responders. The respondent ED’s (RR 75%) were distributed proportionately across the state. Questions about available services and resources were based upon the AMA's recommendations for the treatment and prevention of sexual assault, forensic Nursing guidelines and upon input from an expert panel from Virginia Sexual & Domestic Violence Action Alliance, the Virginia Department of Health and practicing forensic nurses. The expert panel, also reviewed and approved the final version of the survey. Population Studied: All 82 publically accessible emergency departmetns in Virginia, 62 (75%) responded. Principal Findings: ED’s serve an average of 36.5 victims per year (range 0-310). They generally report providing the recommended immediate care to victims of sexual violence, with most conducting a complete forensic exam or referring to a sister hospital. However, trained staff and critical linkages to the community are lacking. One-half report that they do not have a trained sexual assault nurse examiner (SANE/FNE) on staff, 60% are not part of a community sexual assault response team (SART) and one-quarter do not have a relationship with a rape crisis center. Further, both screening and followup could be improved. The majority do not screen for sexual violence unless it is suspected or disclosed. Training in sexual violence is an area where most ED’s could improve. Almost half do not have a formal training plan in place, over half do not provide training to new staff and the great majority (85%) have not provided training to medical staff in the past year. Conclusions: Emergency departments report serving many fewer victims than expected given estimates of the prevalence of sexual victimization in Virginia. It may be that victims in Virginia do not perceive the ED as a place that they can go to for help. The majority of the ED’s provide immediate care, but do not have the staff or training to provide comprehensive care to victims of sexual violence. Implications for Policy, Delivery, or Practice: There is a clear need to ensure that SANE/FNE staff are available at every hospital and that medical staff are trained on a regular basis. State agencies and sexual assault crisis centers need to partner with the ED’s to help them provide the care necessary to victims. Primary Funding Source: State of Virginia ●Local (public) Health Systems in the 21th century: Who Cares? -An Explorative Study on Health System Governance in Amsterdam Thomas Plochg, MSc, D. Delnoij, Ph.D., N.S. Klazinga, M.D. Ph.D., W. Hogervorst, M.D., P. van Dijk, M.D. Presented By: Thomas Plochg, MSc, Scientific Researcher, Department of Social Medicine, Academic Medical Center, University of Amsterdam, PO Box 22660, Amsterdam, 1100 DD; Tel: +31 20 5668719; Fax: +31 20 6972316; Email: t.plochg@amc.uva.nl Research Objective: It is argued that there should be a public health perspective to health system governance practices. Its intrinsic population health orientation provides the ultimate ground for determining the health needs and for governing collaborative care arrangements within which these needs can be met. However, population health concerns are not central in European health system reforms. Governments currently withdraw leaving governance roles to competing care providers and/or financiers. Incentives that trigger the uptake of a public health perspective are often ignored. The relevance of this issue can be illustrated by the current situation in the Dutch health system. Study Design: We explored whether there is a public health perspective to the governance practices of the municipality and the major care insurer in Amsterdam, The Netherlands. And if so, what the scope of this perspective is. We conducted document analysis of relevant municipal policy papers, 10 semi-structured interviews with key executives of the care insurer, and observations of public debates on local health policy. We analysed the data against the concept of 'community-based integrated care', which we used as an operationalisation of a public health perspective. Principal Findings: - There is a public health perspective to municipal health system governance, but its scope is limited. The municipality facilitates rather than governs health care provision in Amsterdam.- The insurer runs financial risks when adapting a public health perspective. It covers an population that partly overlaps the Amsterdam population. Returns on investments in population health are therefore uncertain. Conclusions: There seems to be a vacuum in the governance of the local health system in Amsterdam, as the municipality and insurer are cautious to take up a public health perspective. Consistent governance of the local (public) health system towards population health is therefore not assured. Implications for Policy, Delivery, or Practice: The described vacuum in governance is not an ideological problem but primarily a practical one, as both actors are willing but unable. This is illustrated by their collaborative activities in selected fields. In order to develop and maintain this collaborative governance, it is crucial to develop a shared vision, to invest in human resources, and to build trust. Moreover, the incentive structure should be made more supportive. Primary Funding Source: No Funding Source ●A Good Outbreak is Hard to Find: Seeking Performance Indicators for Evaluation of Preparedness Training Margaret A. Potter, JD, MS, Danielle Iulliano, MPH, Patricia Sweeney, RN, JD, MPH Presented By: Margaret A. Potter, JD, MS, Associate Dean and Director, Center for Public Health Practice, University of Pittsburgh Graduate School of Public Health, 3109 Forbes Avenue, Pittsburgh, PA 15260; Tel: (412)383 2400; Fax: (412)383 2228; Email: potterm@edc.pitt.edu Research Objective: As an academic center for public health preparedness, we must evaluate the practical results of training activities. The objective of this research was to identify performance-based indicators of timeliness and effectiveness in the detection and containment of infectiousdisease outbreaks. These indicators are intended for evaluation of performance in drills and exercises involving infectious-disease outbreaks. Study Design: We reviewed published medical-epidemiologic case reports describing the response to outbreaks caused by nine different pathogens between 1988 and 2004. This review focused on the processes and outcomes of response as indicated by pathogen-specific criteria, detection-phase criteria, and containment-phase criteria. The nine pathogens were selected because each had a public record of outbreak, including media and government reports in addition to the medical-epidemiologic reports, that was sufficient to construct a teaching case study: anthrax, brucellosis, hantavirus, hepatitis-A, monkeypox, plague, SARS, and West Nile virus. Population Studied: Each outbreak affected a different population; however, this study focused on the performance of clinical and public health professionals. Principal Findings: The outbreak reports were inconsistent in their detailing of performance-related process and outcome indicators. Usually included in the reports were pathogen characteristics relevant to the field epidemiologist and the clinician including route and source of exposure, incubation time, and symptoms. Inconsistently included were numbers relevant to overall response effectiveness such as secondary cases and health care workers infected. In the detection phase, decisions made by clinicians and public-health officials during the time elapsed between sample collection and diagnosis of the pathogen – such as how to treat affected persons, what to tell the public, and what precautions to recommend to health workers – would be crucial to the overall effectiveness of response. Nevertheless, few reports specified this time period or its associated activities. For practitioners seeking to improve performance in the containment phase, the quality and timing of advice given to the public, mitigation efforts, and inter-agency and inter-professional communication would be likely correlates of overall response effectiveness. However, virtually none of the reports included information about these activities. Conclusions: The outbreak reports for these nine pathogens emphasized epidemiologic information but had limited usefulness in identifying performance indicators for evaluating the training of public health practitioners. Future outbreak reports would better serve this need by including process and outcome indicators geared to population outcomes, timing, communications, and practical decision-making. Implications for Policy, Delivery, or Practice: The evaluation of preparedness training requires practical benchmarks to serve as standards for performance. Drills and exercises based on disease outbreaks should be evaluated on the basis of such outcomes, depending on the specific pathogen, as: time elapsed from first clinical observation to confirmed diagnosis; number of secondary cases; and appropriate communications among medical, public health, and law enforcement professionals. A body of authoritative case reports that include such outcomes would provide a foundation for systematic evaluation and improvement of practice in the detection and containment of disease outbreaks. Primary Funding Source: Centers for Disease Control & Prevention ●Closing The Gap Between Biological Agent Detection And Response Rasa Silenas, M.D., Janine C. Edwards, Ph.D., Ralitsa Akins, Ph.D., Josie Williams, M.D. Presented By: Rasa Silenas, M.D., Medical Director, Office of Homeland Security, Texas A&M University Health Science Center, PO Box 35399, Brooks City Base, TX 78235; Tel: (210) 534-7227 x 241; Fax: (210) 534-7238; Email: silenas@tamhsc.edu Research Objective: To assess infectious disease surveillance methods in use in a region of Texas for how they would affect delivery of health care in terrorism or natural disasters. Study Design: Case study, semistructured interviews, taped, transcribed and analyzed with ethnographic software. Population Studied: Public health officials in eight local offices, one regional office and at State level in the Texas Department of State Health Services, one federal (US Air Force) surveillance organization, and one local health department in a commmunity in Mexico which borders on a Texas subject community. Principal Findings: 1. Detection and analysis of disease surveillance are compartmentalized. 2. A major part of the surveillance system is an informal network of complex communications pathways. 3. Local public health workforce issues lead to underutilization of this insufficient resource. 4. Preparedness for orderly public health response and surge capacity are lagging in outlying areas. Conclusions: A number of opportunities to improve the effectiveness of disease surveillance and response to emerging health disasters are indentified. Implications for Policy, Delivery, or Practice: This study identifies at three broad categories of interventions, not necessarily expensive, that could optimize public health capabilities in infectious disease surveillance and response: workforce development and support, improved communications pathways and planning considerations. Specific recommendations will be discussed. Primary Funding Source: AHRQ ●Multivariate Methods for Aberration Detection: A Simulation Study Using the District of Columbia's Syndromic Surveillance Data Michael Stoto, Ph.D., Ronald Fricker, Ph.D., Arvind Jain, MS, John O. Davies-Cole, Ph.D., MPH ●Hospital Mortality Risk for Acute Myocardial Infarction Patients and the Effect of Adjustments for Diagnoses Present At Admission George Stukenborg, MA, Ph.D., Douglas P. Wagner, Ph.D., Frank E. Harrell, Jr., Ph.D., Alfred F. Connors, Jr., M.D. Presented By: Michael Stoto, Ph.D., Senior Statistical Scientist, RAND, 1200 South Hayes Street, Arlington, VA 22202-5050; Tel: (703)413-1100 x5472; Fax: (703)413-8111; Email: mstoto@rand.org Research Objective: Monitoring data from multiple hospitals and/or a variety of symptoms can improve the sensitivity of syndromic surveillance systems, but the number of false positives will increase with the number of series monitored. Multivariate detection algorithms combine the available data to achieve the optimal tradeoff among sensitivity specificity, and timeliness. The aim of this analysis is to investigate the improvement in performance characteristics of detection algorithms that might be expected with effective use of multiple data streams. Study Design: ER logs are faxed to the health department, where they are coded them on the basis of chief complaint. Our analysis focuses on four symptom groups (respiratory, gastrointestinal, unspecified infection, and rash) and on seven hospitals. We simulate a variety of disease outbreaks and test four classes of detection algorithms: (1) methods that analyze each series independently, controlling the probability that any of the series will flag; (2) summing the count in each symptom group across all hospitals; (3) combining the Pvalues from each individual series into an overall P-value; and (4) a multivariate detection algorithm that take into account the observed correlation among data streams. In each class we consider both algorithms that look at a single day’s data and methods such as CUSUM that integrate deviations over multiple days. Population Studied: ER visits in the District of Columbia. Principal Findings: Over a range of simulated outbreak types, the univariate and multivariate CUSUM algorithms performed more effectively. Both were nearly certain to detect an outbreak appearing in all hospitals and all syndrome groups on day 2, but when the simulated outbreak was limited to one syndrome group or hospital, 4 to 6 days were needed until it was likely that the algorithm would flag. The multivariate CUSUM was preferred to the univariate CUSUM for some outbreak types but not others. Conclusions: Multivariate detection algorithms offer only limited potential for improving the efficiency of statistical detection algorithms for syndromic surveillance. Given the number of days that even the best algorithms need to detect outbreaks, the value of syndromic surveillance may be highest for natural outbreaks such as influenza rather than for bioterrorism. Implications for Policy, Delivery, or Practice: Multivariate analysis of syndromic surveillance data cannot be recommended as a substitute for careful analysis of individual data series. Primary Funding Source: CDC Presented By: George Stukenborg, M.A., Ph.D., Associate Professor, Health Evaluation Sciences, University of Virginia School of Medicine, P.O. Box 800821, Charlottesville, VA 22908-0821; Tel: (434)924-8430; Fax: (434)924-8437; Email: gstukenborg@virginia.edu Research Objective: To develop a better in-hospital mortality risk adjustment model for use in studies of patients with fresh Acute Myocardial Infarction (AMI). Our new model adjusts for comorbid disease measured using secondary diagnoses reported as present at admission. We compare the statistical performance of the new model to other mortality risk adjustment models that use existing methods for measuring comorbid disease. Study Design: This is a retrospective observational cohort study using California hospital discharge abstract data. This study closely reproduces the study population selection criteria and mortality risk adjustment methods used in the 1996-1998 California Hospital Outcomes Project study of AMI. The original study population qualification and exclusion criteria are closely replicated and applied to publicly available California hospitalization data for 1996 through 1999. Record linkage using encrypted unique identifiers is used to define patient characteristics and hospitalization related events occurring during the patient’s episode of care. The original study population could not be exactly duplicated because several data elements used to define the original study population, including exact dates of admission, were not available for this study. Multivariable logistic regression analysis is used to develop a set of in-hospital mortality risk models using different methods of measuring comorbid disease. The set includes the mortality risk adjustment model developed in the original study, a model using the method of Elixhauser et al. to measure comorbid disease, and a model using present at admission diagnoses to measure comorbid disease. The discrimination between observed and predicted mortality achieved by each model was measured using the C statistic, and was validated by using the developed models to predict mortality outcomes in an identically defined independent study population. Population Studied: The study population included 120,706 AMI hospitalizations identified for the period from January 1996 through November 1998, which is 93.9% of the 128,509 cases identified in the original study. The mortality rate was 10.1%, which closely matches the 9.9% mortality rate reported in the original study. The distribution of patient demographic characteristics and other measured variables also closely matched the original study population. Principal Findings: The mortality risk adjustment model we developed using present at admission diagnoses to measure comorbid disease obtained a validated C statistic of 0.86. This level of statistical performance substantially exceed that achieved by any of the other models we evaluated. The model using the Elixhauser et al. method had a validated C statistic of 0.79. The model that was originally developed for use in the California study had a validated C statistic of 0.76 in our study population, which was nearly equivalent to the C statistic value of 0.77 reported in the original study. Conclusions: States that require hospitals to identify which secondary diagnoses are present at admission can use this information to substantially improve the statistical performance of AMI mortality risk models that adjust for patient differences in comorbid disease. Implications for Policy, Delivery, or Practice: Mortality risk adjustment models using present at admission diagnoses to measure comorbid disease can provide more accurate adjustments for patient differences in studies comparing observed to expected hospital mortality rates. Primary Funding Source: AHRQ, This project was supported by grant number R01 HS10134 and by grant number K02 HS11419 from the Agency for Health Care Research and Quality ●Hospital Response to Public Health Emergencies: A Study of Hospital Collaboration with Community Response Partners Gretchen Torres, MPP, Angela Anderson, MPP Presented By: Gretchen Torres, MPP, Deputy Director, Research & Evaluation, Health Research & Educational Trust, 1 North Franklin Street, 30th FLoor, Chicago, IL 60606; Tel: (312)422-2638; Fax: (312)422-4568; Email: gtorres@aha.org Research Objective: To identify collaborative strategies hospitals and public health partners can use in developing surge capacity for public health emergencies. Study Design: Data were collected via semi-structured interviews with 40 informants in hospitals, public health and EMS at state and community levels. Interview protocols explored public health and hospital planning for surge capacity, resource development, and inter-organizational relationships. Population Studied: Eight communities in 6 states, most with previous disaster experience, representing large and small urban and rural communities. Principal Findings: Most sites developed three-tiered response strategies that triage, stabilize and transfer patients to higher and lower level facilities. A predesignated hospital took on a regional coordinating role and interfaced with the public sector on behalf of all hospitals. Designated hospitals were often trauma facilities. In some cases, any hospital could volunteer. Some sites developed outpost models, which evacuated ambulatory, less acute, or infectious patients away from disaster sites. Outposts included rural hospitals, outpatient sites, or any hospital outside the disaster vicinity. Some collaborative planning processes were marked by tensions due to different perspectives of public and private entities or competitive hospital markets. Ensuring consistent planning across sectors was a universal concern that some states addressed through 1. unified health care-public health planning committees, 2. hospital-focused advisory groups to collect and disseminate information and connect public and private activities, or 3. subcontracts to hospital associations for hospital-specific planning and grant deliverables. Some communities created 501(c)3s to forge partnerships among a more diverse set of actors, creating access to more funding and neutral zones where usual competitors could collaborate in areas such as resource sharing. Preparedness planning provided an opportunity for some communities to break down barriers to working together. There was a universal sense that true preparedness required access to resources and expertise in all sectors. Many reported that planning’s true value was not the plans, policies and procedures that resulted, but the process itself because it facilitated communications across organizations and established working relationships through which to build trust, mutual understanding and shared worldviews. Conclusions: Despite histories of operating in silos, many stakeholders in hospitals and public health supported interorganizational preparedness planning. State and community context—resources, experience, and market conditions—highly influenced the planning process and nature of response systems that emerged. All study sites took a system-wide approach to developing surge capacity and preparedness planning more generally. Using federal resources to address gaps and build on existing infrastructure helped many sites avoid reinventing the wheel. Implications for Policy, Delivery, or Practice: The process of working across organizations and sectors is valuable in addressing the turf issues that impede progress on large systemic issues such as public health preparedness. Getting all players to the table and building the trust and shared experience productive, collaborative working relationships require is no small feat. It is important that the agents of any system-level change consider histories and existing infrastructure and create processes that 1. support and build on them where they are effective and 2. provide the flexibility to address gaps in a way that best connects and creates local and unique resources. Primary Funding Source: CDC ●Agroterrorism and Defending the Food Supply: State of Preparedness Rachel D. Vasconez, RD, MBA, MPH, Peter M. Ginter, Ph.D., Raymond William Bruer, MPH, MPA Candidate, Dugald C. A. Hall, Ph.D. Presented By: Rachel D. Vasconez, RD, MBA, MPH, Program Coordinator II, Health Care Organization and Policy, UAB South Central Center for Public Health Preparedness, RPHB 330 1530 3rd Avenue South, Birmingham, AL 35294; Tel: (205) 934-7122; Fax: (205) 934-3347; Email: rvascone@uab.edu Research Objective: This paper examines the issues and available discussions of recent agroterrorism conferences and meetings and provides a synthesis of the issues and recommendations. More specifically, the paper outlines why agroterrorism is an emerging issue of extreme importance to national security. It examines the vital issues inherent in the nation’s food supply, including producer control, fractured production and distribution systems, centralized processing, inadequate systems for monitoring, surveillance, screening and control of disease spread and lack of a nationwide integrated laboratory network system for diagnostic purposes. Discussion includes issues for both natural- and man-initiated events and the paper recommends specific courses of action to minimize the threat. Lastly, this paper discusses the planning and results of a pilot conference designed to initiate a multi-agency dialogue to minimize the impact of an agricultural event on the southeastern economy. Study Design: Literature, meeting and conference proceedings review. Implications for Policy, Delivery, or Practice: Presidential Directive/HSPD-9 established national policy to protect agriculture and the food supply from disasters, terrorist attacks, and other emergencies. This 2004 directive was the first public presidential-based acknowledgement that the U.S. food supply is at risk and should be regarded as critical infrastructure. Criticisms of the preparedness level of the nation’s food supply have been a topic of considerable debate since the September 11, 2001 terror attacks. The vulnerability of U.S. food production and distribution to attack and disruption became even more glaringly evident with outgoing Secretary of Health and Human Services, Tommy Thompson’s comment, "For the life of me, I cannot understand why the terrorists have not attacked our food supply because it is so easy to do.” Because of the significance of the food supply and the psychological and economic consequences of a successful disruption; federal and state agencies, producers, and consumers have been actively promoting the importance of implementing food supply protection measures. The importance of these issues are especially apparent in states in which a substantial portion of the gross state product is agriculturally based. The culmination of the attention and dialogue has resulted in an increasing emphasis placed on the nation’s food supply system and an understanding that a coordinated multi-agency initiative will be required to decrease its vulnerability level. A number informational sessions have been initiated to ensure the safety of the food supply, but little consensus has resulted despite nationwide attention. For example, there have been a number of conferences, proceedings, and meetings dedicated to agroterrorism including Biosecurity 2003, Louisiana Food and Agricultural Biosecurity: Producer Awareness Conference, National Multi-Hazard Symposium: “One Medicine” Approach to Health Security, New Mexico Biosecurity Conference, Agro-Security/Terrorism Work Conference, and the 2005 Alabama Agroterrorism Conference. To date, no comprehensive review or synthesis has been conducted of the discussions at these conferences or their proceedings. Primary Funding Source: Contract with State Health Department ●How Can the United States Prioritize the Targeted Testing of Tuberculosis? Steve Weiss, DO, Thaddeus Miller, MPH, Peter Hilsenrath, Ph.D., Kristine Lykens, Ph.D., Scott McNabb, Ph.D. Presented By: Steve Weiss, D.O., Professor, Department of Medicine, Unversity of North Texas Health Science Center, 3500 Camp Bowie Boulevard, Fort Worth, TX 76107; Tel: (817)321-4937; Fax: (817)321-4920; Email: sweis@hsc.unt.edu Research Objective: Improving efficiency of health spending is critical to controlling escalating national health care expenditures. Monitoring and evaluation activities can direct resources towards efficient use. Tuberculosis (TB) control policies in the U.S. emphasize prevention of Latent Tuberculosis Infection (LTBI) but do not guide efficient program design. Legal mandates exist for the screening of only some high risk populations, but it is not known if these mandates are directed toward the population most likely to yield efficient returns. The objective of this study is to determine the relative benefits and costs of a state law mandated TB screening program and a non state law mandated TB screening program in terms of cost, morbidity, treatment, and disease averted. Study Design: We conducted a retrospective comparison of the estimated costs and outcomes between the Tarrant County (TC), Texas homeless person TB screening program and the TC jail inmate screening program. This evaluation was part of the Tuberculosis Epidemiologic Studies Consortium, New Model for Assessing Tuberculosis Surveillance and Action Performance and Cost, funded by the Centers for Disease Control (CDC). The study period was from December 2001 to December 2003. Data were abstracted from monthly reports compiled by Tarrant County Public Health Department personnel. We gathered population information from the U.S. Census Bureau. We modeled risk reduction from LTBI treatment as a cumulative reduction of disease risk for these groups from the annual expected risk. Population Studied: Tarrant County, Texas homeless population residing in homeless shelters and Tarrant County jail inmates. Principal Findings: A non state mandated TB program for homeless persons in Tarrant County screened 4.5 persons to identify one with LTBI and 82 to identify one with TB. A statelaw mandated TB program for jail inmates screened 109 persons to identify one with LTBI and 3,274 persons to identify one with TB. The number of patients with LTBI treated to prevent one case of active TB case was 12.1 and 15.3 for the homeless and jail inmate TB programs, respectively. Treatment of LTBI by the homeless and jail inmate TB screening programs will avert 11.9 and 7.9 active TB cases at a cost of $14,350 and $34,761, respectively. Conclusions: Mandated TB screening programs should be risk-based, not population-based. Non mandated targeted testing for TB in congregate settings for the homeless was more efficient and effective than state law mandated targeted testing for TB among jailed inmates. Implications for Policy, Delivery, or Practice: TB screening is recommended in many situations by public health treatment guidelines and mandated in situations by legal statute. This study illustrates how monitoring and evaluation can be used to help set priorities so as to maximize return on public spending to TB interventions. By directing prevention and control programs towards reservoirs of latent disease and populations who risk makes them effective and efficient screening targets, we can improve our progress towards achieving TB elimination in the United States. Primary Funding Source: CDC