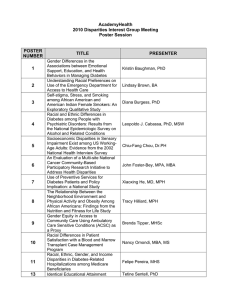
Disparities
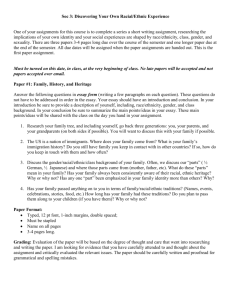
advertisement

Disparities Call for Papers Findings in Health Care Disparities on the Road Less Traveled Chair: Vanessa Sheppard, Georgetown University Medical Center Sunday, June 26 • 10:30 am – 12:00 pm ●Disparities in the Management of Early Breast Cancer among Asian Americans and Pacific Islanders Rebecca P. Gelber, M.D., James W. Davis, Ph.D., Todd B. Seto, M.D., MPH Presented By: Rebecca P. Gelber, M.D., General Internal Medicine Fellow, Internal Medicine, Harvard Medical School, Massachusetts Veterans Epidemiology Research and Information Center; University of Hawaii John A. Burns School of Medicine, 790 Boylston Street, 24F, Boston, MA 02199; Tel: (808)382-7767; Email: rgelber@hsph.harvard.edu Research Objective: Despite consensus guidelines for the management of breast cancer, many patients do not receive standard therapy. Although this discrepancy may be partly related to patient ethnicity, little is known about breast cancer care among Asian Americans and Pacific Islanders (AAPIs). Objective: To evaluate the management of early stage breast cancer among AAPI women. Study Design: Retrospective analysis using data from the Hawaii Tumor Registry, a Surveillance, Epidemiology, and End Results (SEER) Program population-based registry, linked to administrative data from Hawaii's largest health insurer. Population Studied: We studied the first course of therapy for 2038 women (937 Japanese, 144 Chinese, 236 Filipino, 295 Hawaiian, 426 white; mean age, 59+/-13 years) diagnosed with early stage breast cancer (stages I, IIA or B, IIIA) in Hawaii from 1995-2001. We evaluated the use of standard-of-care treatments as defined by NCI/NIH guidelines, including (1) breast-conserving surgery (BCS); (2) radiation therapy following BCS; and (3) chemotherapy for women with nodal spread. We used logistic regression to examine the association between ethnicity and quality of care. Principal Findings: Overall, 1227 (60.2%) women had stage I disease, 752 (36.9%) stage IIA or B, and 59(2.9%) stage IIIA. Only 1623 (79.6%) of all women received BCS, and 64.9% of these received radiation therapy. Of those with node-positive disease (n=526), 82.7% received chemotherapy. Japanese and Hawaiian women were significantly less likely than whites to receive BCS after controlling for age, year of diagnosis, rural residence, tumor size, grade, nodal status, estrogen-receptor status, history of prior cancer, Charlson comorbidity index, health plan typ (HMO, fee-for-service, Medicare), and income (OR, 95%CI: 0.61, 0.42-0.88, for Japanese; 0.63, 0.40-0.98, for Hawaiians; 0.76, 0.42-1.35, for Chinese; 0.68, 0.42-1.10, for Filipinos). Filipino women were significantly less likely than whites to receive radiation after BCS (OR, 0.60; 95%CI, 0.390.91), while other AAPIs were treated similarly to whites (OR, 95%CI: 0.84, 0.61-1.16, for Japanese; 1.06, 0.69-1.62, for Hawaiians; 1.46, 0.83-2.56, for Chinese). AAPI women were as likely as white women to receive chemotherapy for nodepositive disease (OR, 95%CI: 1.94, 0.84-4.48, for Japanese; 0.92, 0.36-2.33, for Hawaiians; 0.64, 0.19-2.12, for Chinese; 0.81, 0.32-2.10, for Filipinos). Conclusions: We found significant disparities in the management of early stage breast cancer among AAPI women, with Japanese, Hawaiians, and Filipinos being particularly less likely to receive standard-of-care treatment, as compared to white women. Implications for Policy, Delivery, or Practice: Further study is needed to determine the reasons for the observed differences in care and to examine the impact of these disparities on health outcomes. Primary Funding Source: AHRQ ●Medicare+Choice Enrollment and Plan Benefits Among Black, Hispanic and White Medicare Enrolled VA-Using Veterans in CY2000 Dolly A. John, MPH, Raji Sundaravaradan, Jessica Davila, Ph.D., Iris I. Wei, DrPH, Margaret Byrne, Ph.D., Laura Petersen, M.D., MPH, Debora A. Paterniti, Ph.D., Nora Osemene, PharmD, Robert O. Morgan, Ph.D. Presented By: Dolly A. John, MPH, Project Coordinator, MEDVAMC (152), Houston Center for Quality of Care and Utilization Studies, 2002 Holcombe Boulevard, Houston, TX 77030; Tel: (713) 794-8663; Fax: (713) 748-7359; Email: dollya.john@med.va.gov Research Objective: Prior studies examined enrollment of Medicare enrolled VA-using veterans (MEVV) in Medicare+Choice (M+C, now called Medicare Advantage) plans but not enrollees’ plan benefits. We examined enrollment in M+C plans of all MEVV in CY2000 and enrollees’ monthly premiums, prescription drug coverage and plan benefit packages. We compared these across race/ethnicity groups. Study Design: VA-using (any use between CY1996 and CY2000) veterans were matched to CY2000 Medicare Denominator, Group Health Plan and Benefits Information Form (BIF) plan benefits data to identify veterans (age>=65) enrolled in Medicare and in a M+C plan in CY2000. CMS’s plan service area data identified 261 active M+C contracts operating in 817 counties. Generosity of benefits was scored on a combination of physician and hospital co-pays, prescription drug and supplemental benefits (vision, dental, hearing and podiatry) available for that plan. We predicted enrollment in a M+C plan using univariate and multivariate logistic regression models. We also controlled for income, VA priority level and metropolitan status of the county. Population Studied: 1,919,790 Black, Hispanic and White MEVV in CY2000; 282,939 were M+C enrollees who represent 87% of all Black, Hispanic and White MEVV enrolled in any type of Medicare managed care plan. We excluded from our analyses those in other race/ethnic groups and those in hospice. Principal Findings: Compared to 60% of all White MEVV living in a county with an active M+C plan, a greater proportion of Black (72%) and a smaller proportion of Hispanic (51%) enrollees lived in a county with an active M+C plan in CY2000. Overall, among those with an active M+C plan in their county, 25% of White (n=251,596), 21% of Black (n=26,639) and 34% of Hispanic (n=4,704) MEVV were enrolled in a M+C plan. Even after adjusting for the presence of multiple plans, availability of benefits ($0 monthly premium, prescription drug and supplemental benefits), age, gender, income, Medicare state buy-in, VA priority status, CY2000 VA use and the metro status of their county of residence, Black enrollees were less likely (OR=.73, 95%CI: .71.74) and Hispanic enrollees were more likely (OR=1.62, 95%CI: 1.56-1.69) to be enrolled in a M+C plan than White enrollees. Furthermore, more Black and Hispanic enrollees than White enrollees were in plans with a $0 monthly premium (80% and 83% versus 70%, p<.0001), some drug coverage (96% and 94% versus 85%, p<.0001) and a high benefits package (82% and 91% versus 78%, p<.0001) than White enrollees. Conclusions: The majority of MEVV enrolled in a M+C plan in CY2000 paid nothing, had some drug coverage and a high benefits package. Compared to White M+C enrollees, Black and Hispanic M+C enrollees were more likely to be in plans without monthly premiums, with some prescription drug coverage and a high benefits package. Implications for Policy, Delivery, or Practice: Black and Hispanic VA-using veteran M+C enrollees may have been more vulnerable to M+C plan cost increases and benefit reductions in recent years than White enrollees. How this may have impacted their continuity and quality of care and whether this results in disparities in health services use and health outcomes needs further exploration. Primary Funding Source: VA ●Racial Disparities In Primary Care and Utilization of Health Services at the End of Life Andrea Kronman, M.D., Jim Burgess, Ph.D., Arlene Ash, Ph.D. Presented By: Andrea Kronman, M.D., Internal Medicine, Boston University Medical Center, 91 E Concord Street MAT 2, Boston, MA 02118; Tel: (617)414 6811; Fax: (617)414 6817; Email: andrea.kronman@bmc.org Research Objective: To determine the role of primary care in the racial disparities of healthcare utilization at the end of life. Study Design: This study is analyzes Medicare data to examine racial differences in primary care visits and hospitalizations for ACSC during the last 18 months of life. Hospital admissions for two specific ACSC: diabetes (DM) and congestive heart failure (CHF) were drawn from the final 6 months of life, while outpatient visit frequencies were from the 12 months prior to that period. Utilization data was obtained from the MedPAR, carrier and hospice files of beneficiaries who died in the last 6 months of 2001, and linked to NDI records to determine cause of death. Demographics were obtained from the CMS 2000 Denominator file. Univariate and bivariate analysis was used to assess differences between races. Population Studied: The study population of Medicare beneficiaries who died in the last 6 months of 2001 was obtained from a random sample of 1 million beneficiaries stratified by decedent status and race. Beneficiaries excluded from the study were less than 66 years of age, not entitled to both Medicare A and B, and not enrolled in a Medicare Fee for Service plan continuously. Principal Findings: Study sample (n=162,992) characteristics: mean age 81 (range 66 - 98), female 56%, black 36%, Hispanic 10%, Other 14%. Racial differences were found in hospice use (24% white, 18 % black, 20 % Hispanic, p <0.0001) and in-hospital deaths (38 % white, 46 % black, 52 % Hispanic, p<0.0001). Outpatient visits differed significantly between races; particularly among those who had not had any ambulatory care visits (16 % white, 26 % black, 24 % Hispanic p<0.0001) or primary care visits (30 % white, 39 % black, 37 % Hispanic, p < 0.0001). DM was the cause of 4% of the 49,598 beneficiaries with DM who were hospitalized. There were significant differences between races for those hospitalized for DM (whites 2.7%, blacks 5.1 %, Hispanic 5.0 %, p<0.0001) and those hospitalized more than once (whites 7.7%, blacks 10.1 %, Hispanics 7.1 %, p<0.0001). CHF was the cause of 18% of the 48,770 hospitalized beneficiaries with a CHF diagnosis. There were racial differences for those hospitalized for CHF (white 16%, black 18%, Hispanic 21%, p<0.0001) and those with more than one admission (white 23 %, black 26%, Hispanic 26%, p <0.0001). Conclusions: There are significant disparities between races in frequency of primary care visits toward the end of life. There are also significant racial disparities in the use of hospice, and hospitalizations for diabetes mellitus and congestive heart failure during the last six months of life. Implications for Policy, Delivery, or Practice: This study implies that receipt of primary care may contribute to differences in care and higher costs of minorities at the end of life. Increasing the provision of primary care to elderly minority groups could improve management of chronic disease, decrease costs, and improve care quality at the end of life. The relationship between primary care and health care utilization at the end of life warrants further study. Primary Funding Source: No Funding ●Racial Disparities Among Medicaid Beneficiaries with Mental Disorders Mihail Samnaliev, Ph.D. Presented By: Mihail Samnaliev, Ph.D., Project Associate, Commonwealth Medicine Center for Health Policy and Research, University of Massachusetts Medical School, Center for Health Policy and Research, University of Massachusetts Medical School, 222 Maple Avenue, Chang Building, Shrewsbury, MA 01545; Tel: (508) 8561765; Email: Mihail.Samnaliev@umassmed.edu Research Objective: The ECA study and the National Health Interview Survey (NHIS) have documented lower prevalence of mental disorders among African Americans and Hispanics compared to Caucasians. Yet, it is unclear if and to what extent these disparities are the result of state healthcare system factors as opposed to confounding ethnic differences in health behavior and in the epidemiology of mental disorders. In this study we explore interstate variation in rates of diagnosis of mental disorders among racial and ethnic groups. Second, we explore correlation patterns between Medicaid eligibility, detection and service utilization rates. We study all racial and ethnic groups, however, the primary focus in this article is on the Hispanic population. Study Design: A quasi-experimental design where states represent the ‘experimental’ units. As a baseline for comparison we use the 1999 NHIS which is a nationally representative report of occurrence of mental disorders by race. States were selected in a stratified sampling mode to capture the variation in Medicaid programs regarding health care coverage. Mental disorders were identified using ICD-9 codes and prescribed medications in 1999. Logit models were used to estimate the probability of mental health diagnosis and hospitalization. Population Studied: Medicaid beneficiaries with mental disorders in six states: Arkansas, Colorado, Georgia, Indiana, New Jersey, and Washington in 1999. Principal Findings: (1) Beneficiaries from Hispanic origin had much lower rates of diagnosis with mental illness, compared to Caucasians. This difference was as large as 12% and for most states it was much larger than the approximately 2% difference documented in the NHIS. There was a significant interstate variation in rates of diagnosis of Hispanic beneficiaries, ranging from 2.5% (in Georgia) to 11.9% (in Arkansas). (2) Rates of diagnosis with mental illness among Hispanics were positively correlated with the proportion of Hispanics who were classified as ‘Disabled’ in the Medicaid eligibility category. However, this finding should be viewed with caution because of missing data on race in some of the states. (3) Compared to Caucasians, the probability of hospitalization was significantly greater among Hispanics and there was a well expressed pattern where lower rates of diagnosed mental illness among Hispanics was correlated with greater probability of hospitalization for Hispanics vs. Caucasians. Conclusions: The greater disparities between Caucasians and Hispanics as compared to findings from nationally representative surveys, suggests that State Medicaid policies can play an important role in alleviating or perpetuating existing racial disparities. Significant interstate variation in diagnosis rates further suggests that Medicaid programs in some states are more effective than others in identifying the Hispanic population with mental disorders. Further research needs to explore the extent to which racial disparities are driven by State disability standards. The correlation between rates of diagnosis and probability of hospitalization raises a question of whether underdiagnosis of MI among Hispanics may have an adverse effect on health outcomes. Implications for Policy, Delivery, or Practice: States with relatively low detection rates of mental illness among the Hispanic population may benefit from a more assertive approach in identifying mental disorders among the Hispanic population. Primary Funding Source: RWJF ●Racial/Ethnic Disparity in Access to New Prescription Drugs Junling Wang, MS, C. Daniel Mullins, Ph.D., MS Presented By: Junling Wang, MS, Doctoral Candidate and Research Assistant, Pharmaceutical Health Services Research, University of Maryland, 515 West Lombard Street, Room 272, Baltimore, MD 21201; Tel: (410)706-1418; Fax: (410)706-5394; Email: jwang005@umaryland.edu Research Objective: To determine whether there are racial or ethnic disparities in the utilization of new prescription drugs and to examine the impact of the generosity of drug coverage on these disparities. Study Design: This is a non-experimental study. Population Studied: The main data sources were Medical Expenditure Panel Survey (1996-2001) and Mosby’s GenRx Database. The former provided information on patient characteristics and, for each prescribed medicines event (when prescribed medicines were purchased or otherwise obtained), drug name, NDC and payment sources; the later provided information on drug approval dates. Drugs were considered “new” if approved fewer than or equal to five years ago at the time of survey data collection. A negative binomial model was used to test the disparities across racial/ethnic groups when controlling for other covariates; the dependent variable was number of prescribed medicines event; the independent variables were dummy variables for (1) black, non-Hispanics, and (2) white Hispanics (white, non-Hispanics was the reference group); generosity (percentages of drug cost paid by health insurance); interaction terms between generosity and the dummy variables for racial/ethnic groups; age; gender; marital status; education; and dummy variables for census regions, metropolitan statistical area, poverty status, and self-perceived health status. The interaction terms between generosity and racial/ethnic groups were included in order to test whether effects of generosity differed across racial/ethnic groups. Sensitivity analyses were performed using variable definitions for the number of years post-launch that a drug is considered new. Principal Findings: Among 47,115 prescription users, 31,853 were white, non-Hispanics, 5,904 were black, non-Hispanics, and 7,337 were white Hispanics. According to the least stringent five-year criterion for defining new drugs, the mean numbers of prescribed medicines events were 1.67, 1.36, and 1.07 among white, non-Hispanics, black, non-Hispanics, and white Hispanics, respectively. The differences between white, non-Hispanics and the two minority populations were significant in the main model and most of the sensitivity analyses. The negative binomial model showed that the number of prescribed medicines events was 29-45% lower (depending on the criterion for defining new drugs) among black, non-Hispanics than among white, non-Hispanics (P<0.01); the number of events among white Hispanics was 10-23% lower than among white, non-Hispanics but it was not always significant. The interaction terms between racial/ethnic groups and generosity were not significant, suggesting that the effects of insurance generosity did not differ across racial/ethnic groups. The gap between white, non-Hispanics and black, non-Hispanics widened when the criteria for new drugs became more stringent and the gap between white, non-Hispanic and white Hispanics narrowed. However, neither trend in the gaps was found significant in a nested model. Conclusions: There are racial disparities in the use of new drugs but no ethnic disparities are confirmed. The generosity of drug insurance coverage is positively correlated with the use of new drugs and this correlation is fairly consistent across racial/ethnic groups. Implications for Policy, Delivery, or Practice: New prescription drugs have potential benefits in improving life expectancy and quality of life. Thus, measures should be taken to address the racial/ethnic disparities in the use of new drugs. Primary Funding Source: No Funding Call for Papers Can Quality Improvement Programs Reduce Health Disparities? Chair: Kaytura Felix-Aaron, Bureu of Primary Health Care Monday, June 27 • 9:00 am – 10:30 am ●Racial and Ethnic Differences in Use of High Volume Hospitals and Surgeons Andrew Epstein, MPP, Ph.D., Mark Schlesinger, Ph.D., Bradford Gray, Ph.D. Presented By: Andrew Epstein, MPP, Ph.D., Assistant Professor, Health Policy and Administration, Yale University, 60 College Street, New Haven, CT 06520; Tel: (203)785-6924; Fax: (203)785-6287; Email: andrew.epstein@yale.edu Research Objective: To quantify the direction and magnitude of racial and ethnic differences in use of high volume hospitals and surgeons among New York City-area residents undergoing one of 10 procedures for which a volume-mortality association has been identified for both hospitals and surgeons. Study Design: Using New York state hospital discharge data from 1995-96 and 2000-01, we classified hospitals and surgeons as high volume based on thresholds published in volume-mortality studies. Linear probability models were used to assess the overall independent association between patient race/ethnicity and treatment by a high volume provider for each time period, controlling for patient sex, age, admission type/source, insurance status and number of comorbidities. To decompose the influence of inter- and intra-hospital referral patterns, patient residence ZIP Code fixed effects were included in both hospital and surgeon use models, distance to the closest hospital and closest high volume hospital were included in the hospital use model, and hospital fixed effects were included in the surgeon use models. Population Studied: Adults living in New York City, Nassau County or Westchester County treated at hospitals in the same area for: abdominal aortic aneurysm repair, carotid endarterectomy, percutaneous coronary intervention, coronary artery bypass graft surgery, total hip replacement, or for surgery for pancreatic, breast, colorectal, gastric or lung cancer. Principal Findings: Black, Latino and Asian patients were significantly less likely to use high volume hospitals in 8-9 of the 10 procedures during 2000-2001. Although these differences were reduced with the inclusion of patient residence ZIP Code fixed effects, minorities remained less likely to use high volume hospitals for 5-8 procedures. Similar patterns were found for use of high volume surgeons: black patients were significantly less likely to be treated by high volume surgeons for all 10 procedures, Asian patients for 6, and Latino patients for 7. After controlling for patient ZIP Code and hospital fixed effects, the number of procedures with significant racial differences (2, 3 and 3 respectively) and the magnitudes of the differences became smaller. Ongoing work explores the influence of specific hospital and neighborhood characteristics on the use of high volume providers. Analysis of the 1995-96 data yielded the same pattern of findings. Conclusions: For a range of surgical procedures for which prior research suggests a volume-mortality association, minority patients in the New York City area are less likely to use high volume hospitals and surgeons. This relationship can be attributed primarily to racial/ethnic differences in the geographic distributions of patients and providers. For a small number of procedures, however, minority patients are less likely to be treated by high volume surgeons than are white patients from the same ZIP Code admitted to the same hospital. Implications for Policy, Delivery, or Practice: Given substantial differences in referral patterns by patient race/ethnicity, strategies for centralization of surgical procedures may have disproportionate effects for minorities. An alternative strategy for improving survival for minority patients would focus on quality improvement interventions among providers primarily serving minorities. Primary Funding Source: RWJF ●Disparities in Inpatient Quality of Care Measures by Race and Ethnicity Romana Hasnain-Wynia, Ph.D., David W. Baker, M.D., MPH, Raj Behal, M.D., MPH, Joe Feinglass, Ph.D., David Nerenz, Ph.D., Joel S. Weissman, Ph.D. Presented By: Romana Hasnain-Wynia, Ph.D., Senior Director, Research and Evaluation, Health Research and Educational Trust, One North Franklin, 30th floor, Chicago, IL 60606; Tel: (312)422-2643; Fax: (312)422-4568; Email: rhasnain@aha.org Research Objective: This study addresses quality of care in hospitals. Evidence indicates that quality measurement initiatives, when linked to data on race and ethnicity, can improve quality and reduce disparities. This study of 89 hospitals nationwide examines inpatient quality measures for three conditions by race and ethnicity to see whether disparities in care exist. This measure set is serving as the basis for the national RWJF disparities initiative in cardiac care. Study Design: The study examines racial disparities in 18 inpatient quality of care measures for acute myocardial infarction, heart failure, and pneumonia. Eighty-nine hospitals are reporting the measures with patient race/ethnicity as part of CMS’s overall Hospital Quality Initiative. We examined mean rates and median times (in minutes for continuous measures) for each of the measures for White, Black, Hispanic, and Asian groups focusing on meaningful clinical differences. For adjustment of the data, we examine breakdowns by age, sex, admission source, admission type, and payor type. We conduct multivariate analyses and estimate separate models for each of the measures. Population Studied: Eighty-nine hospitals reported measures to the University Healthsytem Consortium from the third quarter of 2002 to the first quarter of 2004 for a total of 118,279 admissions. Principal Findings: In preliminary analyses we found differences in mean rates and median times for measures requiring personal interaction with patients. For patients with heart failure, rates for providing discharge instructions varied by race/ethnicity (White, 36.8%, Asian, 30.8%, Black, 26.1% and Hispanic, 24.3%), as did rates for smoking cessation counseling (White, 54.3%, Asian, 47.9%, Black, 47.8% and Hispanic, 39.2%). For acute myocardial infarction, times and rates varied for the following measures: time to thrombolysis in minutes (Asian 68, White 105, Hispanic 220, and Black 476); time to PTCA in minutes (White 515, Asian 678, Blacks 878 and Hispanic 913); and rates for smoking cessation counseling (White, 77.4%, Asian 68.6%, Black, 64.8% and Hispanic 63.4%). For community acquired pneumonia, rates for administration of pneumococcal vaccination varied by race/ethnicity (White 26.3%, Hispanic 21.8%, Black 20.9% and Asian 15.4%). Differences in rates of prescribing essential medications (e.g., beta blockers for myocardial infarction) were similar across racial/ethnic groups, in part because compliance with these measures was near 100%. Conclusions: This is the first study to look at differences in quality of care by race/ethnicity for conditions measured by the CMS Quality Initiative. Additional analyses are needed to determine the statistical significance of these findings after adjustment for potential confounders and to understand whether these differences are explained by racial/ethnic differences in where patients receive care or whether there are disparities within institutions. Implications for Policy, Delivery, or Practice: Hospitals’ efforts to reduce disparities should focus on procedures and patient education and counseling. Hospitals should routinely monitor disparities in quality of care for these indicators and initiate interventions to reduce disparities. Standardizing care plans to ensure high levels of compliance with recommended processes of care may be the best strategy to eliminate disparities. Primary Funding Source: CWF ●Racial Disparities Remain As Quality Improves in Medicare Managed Care Sarah Scholle, MPH, DrPH, Beth Virnig, Ph.D., Sarah Shih, MPH, Russ Mardon, Ph.D. Presented By: Sarah Scholle, MPH, DrPH, Asst Vice President, Research and Analysis, National Committee for Quality Assurance, 2000 L Street NW, Suite 500, Washington, DC 22031; Tel: (202) 955 1726; Fax: (202) 955 3599; Email: scholle@ncqa.org Research Objective: To determine whether secular trends in quality of care for Medicare managed care enrollees between 1998 to 2003 differed for whites versus blacks. Previous studies of Medicare managed care demonstrated significant disparities in quality of care between black and white beneficiaries. While managed care performance on key indicators has improved since these reports, the impact on racial disparities is unclear. Study Design: This longitudinal panel study uses member level data on HEDIS effectiveness of care measures submitted to NCQA. These data were linked with CMS enrollment data on race/ethnicity and region. Trends in performance on health care quality indicators were analyzed using direct standardization methods to control for patient age and sex. Multivariate regression methods were used to control for region. Performance rates adjusted for age, sex, and region are reported. Population Studied: Enrollees in Medicare managed care organizations on performance measures for calendar years 1998 to 2003. The number of health plans available for analyses ranged from 346 in 1998 to 170 in 2003 with Medicare managed care enrollment between 5.4 to 7.5 million members per each year. The number of patients varied by measure; for example, analyses on diabetes care included approximately 120,115 members in 2003. Principal Findings: Quality of care improved for both Black and white Medicare beneficiaries during the time period studied, however, the pattern of improvement varied by the type of measures. In measures addressing preventive and screening services, quality generally improved and the gap in performance between whites and blacks sometimes closed. For example, hemoglobin A1c screening rates for diabetics improved from an adjusted rate of 0.78 in 1999 to 0.82 in 2003 among whites and from 0.73 to 0.82 for blacks during the same time period. For measures addressing control of hemoglobin A1c and lipid levels, quality improved but the racial disparity remained. For example, the rate of control for lipid levels (LDL <130) increased from 0.58 to 0.62 for whites and from 0.44 to 0.57 for blacks. For behavioral health measures, improvement over time was negligible, and the disparity between whites and blacks remained. For example, the rate of outpatient follow-up within 30 days of a mental health hospitalization changed from 0.53 to 0.56 for whites and 0.37 to 0.40 for blacks. Further analyses will address additional measures and control for socioeconomic status. Conclusions: Quality performance in Medicare managed care plans has improved for blacks and whites, however, the disparity in performance remains, particularly for measures assessing control of clinical outcomes and behavioral health. Implications for Policy, Delivery, or Practice: Despite high level attention and efforts to address health care disparities between blacks and whites, disparities persist. A better understanding of the source of disparities and new approaches are needed to reduce these inequities in care. Primary Funding Source: The California Endowment ●Solving Racial Disparities in Quality of Medicare Managed Care: Geography Reconsidered Sarah Scholle, DrPH, MPH, Beth Virnig, Ph.D., Russell Mardon, Ph.D., Rich Mierzejewski, MS, MBA, Sarah Shih, MPH Presented By: Sarah Scholle, DrPH, MPH, Assistant VP, Research and Analysis, NCQA, 2000 L Street NW, Suite 500, Washington, DC 20036; Tel: 202-955-1726; Fax: 202-955-3599; Email: scholle@ncqa.org Research Objective: To examine whether the variation in quality of care for Medicare managed care enrollees observed in earlier reporting years persists in the most current 2004 reporting year and whether geographic disparity is greater or less than racial disparity. Study Design: This cross-sectional study uses individual-level data for seven HEDIS effectiveness of care measures that is linked with Medicare demographic information. Estimates of rates of preventive care are calculated separately for blacks and whites, overall and for each of nine census regions using direct standardization controlling for age and sex. Population Studied: The individual-level HEDIS data set contains over 6 million records. We were able to link over 95 percent of records submitted by managed care plans to Medicare information. The analysis is limited to persons whose race is black or white. The number of individuals included in analysis varies from measure to measure; for example, there were 17,292 individuals included in analysis of beta blocker use after heart attack. Principal Findings: For all seven preventive services measures, we observed overall racial disparity with blacks receiving less care than whites. For example, the rate of beta blocker after heart attack—BBH-- for whites was 90.2 percent compared to 83.3 percent for blacks. Similarly, the disparities in rate of 30-day follow-up after hospitalization for mental illness were 55.2 percent for whites and 37.2 percent for blacks. In addition to a global racial difference, we observed racial differences within each census region. We also observed considerable region-to-region variation. For example, for BBH, the overall racial effect was a difference of 6.9 percent. The lowest performing region had a rate of 75.4 percent while the highest performing region had a rate of 93.9 percent. The OR comparing the lowest and highest performing regions was 1.26 while the OR for blacks compared to whites was 1.08. Likewise, for 30-day follow-up, the OR for race was 1.48 while the OR comparing highest and lowest regions was 1.84. In both cases, the regional level of performance was inversely correlated with the percentage of the managed care population that was black. Further analyses will examine additional HEDIS effectiveness of care measures and control for additional patient and plan factors. Conclusions: Racial disparity in quality of care continues to be observed in Medicare managed care plans and is consistently found in measures of effectiveness of care. However, there is also considerable regional variation in quality that is independent of race but is correlated with higher black populations. Implications for Policy, Delivery, or Practice: While overall and within region racial differences cannot be ignored, the large region-to region variation and its correlation with minority population suggest that equalizing regions may prove to be an important strategy for improving preventive services received by elderly black managed care Primary Funding Source: California Endoment Foundation ●The Effect of Quality Improvement on Racial Disparities in Diabetes Care Thomas Sequist, M.D., MPH, Alyce Adams, Ph.D., Fang Zhang, MS, Dennis Ross-Degnan, Sc.D., John Ayanian, M.D., MPP Presented By: Thomas Sequist, M.D., MPH, Instructor in Medicine and Health Care Policy, Department of Health Care Policy, Harvard Medical School, 180 Longwood Avenue, Boston, MA 02459; Tel: (617)432-3447; Email: tsequist@partners.org Research Objective: Since 1997 Harvard Vanguard Medical Associates (HVMA) has implemented quality improvement (QI) programs for diabetes including a new electronic medical record (EMR), electronic physician reminders, disease registries, and patient mailings. We evaluated whether these QI programs were associated with changes in racial disparities in care. Study Design: We identified diabetic patients > 18 years old using insurance claims and EMR data. We assessed 5 quality measures based on American Diabetes Association guidelines: annual retinopathy screening, annual HbA1c testing, annual LDL cholesterol testing, and rates of appropriate HbA1c control (< 7.0%) and LDL cholesterol control (< 130 mg/dL). To assess changes in racial disparities for each indicator, we used logistic regression to adjust for race, year, race-year interactions, age, and sex, with general estimating equations to control for repeated measures among patients. Population Studied: We identified adult diabetic patients receiving primary care during 1997 to 2001 within HVMA, a large multi-speciality group practice in Massachusetts. Among 7,216 diabetic patients, 5,180 were white and 2,036 were black, with a mean age of 58 years and 51% female. Principal Findings: Two quality measures demonstrated relatively low overall baseline scores and subsequent large improvement. The proportion of all patients receiving annual LDL cholesterol testing increased from 40% in 1997 to 64% in 2001, while the white-black disparity decreased from 13% to 3% (p<0.001 for change in disparity). The proportion of all patients with an LDL cholesterol < 130 mg/dL increased from 15% in 1997 to 43% in 2001, and the white-black disparity decreased from 9% to 6% (p<0.001 for change in disparity). The proportion of all patients with a HbA1c < 7.0% remained low from 1997 (31%) to 2001 (33%), and the white-black disparity remained constant at 10% (p=0.34 for the change in disparity). Two quality measures demonstrated relatively high baseline scores, and blacks were not less likely than whites to receive services at baseline. The proportion of all patients receiving annual HbA1c testing remained stable from 1997 (76%) to 2001 (77%), and there was no change in the whiteblack difference (p=0.34). The proportion of patients receiving annual retinopathy screening exams decreased slightly from 1997 (74%) to 2001 (70%), and there was no change in the white-black difference (p=0.83). Conclusions: Racial disparities were diminished following successful QI efforts in cholesterol management, but persisted following comparable QI efforts in glycemic control that had limited impact. Implications for Policy, Delivery, or Practice: Generalized quality improvement programs can result in reduced disparities when overall quality of care improves rapidly, but reducing other persistent disparities may require a specific focus on minority health. Primary Funding Source: Harvard Medical School Center of Excellence in Minority Health and Health Disparities Call for Papers Disparities in Cardiac Care - New Lessons Chair: David Nerenz, Henry Ford Health System Monday, June 27 • 11:00 am – 12:30 pm ●Information and Quality Sorting by Ability to Pay in the Market for Heart Surgeons Rachel Kreier, Ph.D. Presented By: Rachel Kreier, Ph.D., Professor, Economics, Hofstra University, Barnard Hall, Hempstead, NY 11549; Tel: (516)463-5659; Email: ecorek@hofstra.edu Research Objective: This paper examines disparities in the effects of New York's coronary artery bypass graft (CABG) mortality rate reporting program. Study Design: The investigation uses the 1988-1999 SPARCS (Statewide Planning and Research Cooperative System) administratively releasable in-patient data set, which contains demographic, medical, and insurance coverage information for patients discharged from New York hospitals. A strength of the investigation is that it makes use of the relatively rich information about primary and secondary insurance coverage in the SPARCS data set. There are approximately 200,000 observations. Three separate econometric approaches are applied to the data (OLS, binary logit using patient-surgeon match as the unit of observation, and multinomial logit). The investigation is informed by a theoretical model of quality sorting (stratification) by ability to pay. Population Studied: Patients undergoing CABG procedures in New York State during the 1988-1999 period. Principal Findings: Quality sorting of surgeons' services by income group and type of insurance coverage increased during the decade following the reporting program's inception. Being African American also is a significant predictor of seeing a surgeon with a poorer mortality rate in the later years. The basic results are robust across econometric specifications. Furthermore, the average performance of the surgeons treating those in the lowest income group shows negligible improvement, while the average performance of surgeons treating upper income groups shows substantial improvement. Conclusions: The findings strongly suggest that the reporting program has facilitated quality sorting by ability-to-pay. In addition, there is cause for concern that the poor have not shared in across the board quality improvements over time, and that the reporting program may promote the continued widening of the quality gap across income groups and groups with different insurance coverage. Implications for Policy, Delivery, or Practice: At least in this market, performance reports appear to exert significantly disparate effects on patients with different incomes, racial backgrounds, and insurance coverage. Payment policies, such as quality adjusted disproportionate share payments, or Medicaid payments might offset this tendency if appropriately designed, although they would also greatly strengthen the incentives for providers to attempt to game the rating system through patient selection. Furthermore, the theoretical model is relevant in a variety of contexts. These include, in addition to quality reporting programs, managed competition approaches to delivering health care, such as the Medicare + CHOICE/Medicare Advantage program. These programs rely on market mechanisms and consumer choice to implement quality/cost trade offs. There is strong theoretical reason to expect them to lead to quality stratification by ability to pay, as well. Primary Funding Source: No Funding ●Do Physicians Discriminate Among Patients of Different Race when Referring to High Quality Cardiac Surgeons? Dana Mukamel, Ph.D., David Weimer, Ph.D., Alvin Mushlin, M.D. Presented By: Dana Mukamel, Ph.D., Associate Professor & Senior Fellow, Center for Health Policy Research, University of California, Irvine, 111 Academy Way, Irvine, CA 92697; Tel: (949) 824-8873; Fax: (949) 824-3388; Email: dmukamel@uci.edu Research Objective: Prior studies found that Blacks in New York State receive CABG surgery from cardiac surgeons of lower quality, when quality is measured by the surgeon’s riskadjusted mortality rate (RAMR). The objective of this study was to investigate whether this phenomenon can be explained by 1) the fact that Blacks are seen by physicians whose referrals in general are to lower quality surgeons or 2) whether referring physicians refer their white and black patients to different surgeons. Study Design: Medicare claims data were used to identify the surgeon performing the CABG surgery and the referring physician. RAMRs for each surgeon were obtained from the New York State Cardiac Surgery Report. A comparison of the average surgeons’ RAMRs for referring physician who referred only white patients and those who referred both blacks and whites was made to answer the first question. To answer the second question, hierarchical linear models were estimated to predict the surgeon’s RAMR, allowing for both a random intercept and a random race slope. The random race coefficient was conditioned on characteristics of the referring physician. Population Studied: 22,571 New York State fee-for-service Medicare enrollees having CBAG surgery in 1997-1999. Principal Findings: The findings confirm both hypotheses. 1) Physicians with patients of both races refer all their patients to surgeons with higher RAMR compared to physicians who have only white patients (p<0.000). The difference is about 10% of the state average mortality rate. 2) Physicians with patients of both races refer their black patients to surgeons with higher RAMR (p<0.002) compared with the surgeons to which they refer their white patients. This disparity is not modified by the age or specialty of the referring physician. It does, however, decrease (i.e. less disparity relative to white referrals) with the number of black patients in the practice of the referring physician and if the surgeon practices in the hospital to which the referring physician makes most of her cardiac referrals (not only CABG). These analyses controlled for other potential explanations for differential referrals, including patient gender, age, co-morbidities, emergency procedure, distance, education, and income. Conclusions: The disparity in access of Blacks to high quality cardiac surgeons is explained by several aspects of the referral process. About half of the disparity can be explained by who the referring physician is and the other half is due to differential treatment of minority patients by same physician. Implications for Policy, Delivery, or Practice: Because racial disparities in access to high quality surgeons are caused by several factors, policy interventions should be multifaceted. Interventions, such as education or feedback of information about referral patterns, should be aimed at referring physicians who refer their white and black patients differently. Minority patients should be educated about the referral patterns of their physicians. A “referral report card” might serve as a vehicle for disseminating information about referral patterns. Further research is required to understand why physicians with a racially mixed practice refer all their patients to lower quality surgeons. In particular, geographic distribution of patients, referring physicians and surgeons should be examined. Primary Funding Source: NIA, Commonwealth Fund & NCMHD ●Surgeons' Experience with a new Cardiac Surgery Technique and Patient Race Dana Mukamel, Ph.D., Laurent Glance, M.D., David Weimer, Ph.D., James Jackson, Ph.D., Thomas Pearson, M.D., Ph.D., Todd Massey, M.D., Jeffrey Gold, M.D., Sheldon Greenfield, M.D., Alvin Mushlin, M.D., M.Sc. Presented By: Dana Mukamel, Ph.D., Associate Professor & Senior Fellow, Center for Health Policy Research, University of California, Irvine, 111 Academy Way, Irvine, CA 92697; Tel: (949) 824-8873; Fax: (949) 824-3388; Email: dmukamel@uci.edu Research Objective: CABG surgery performed on a beating heart without the use of cardiopulmonary bypass (off-pump CABG) has been recently been introduced as an alternative to conventional CABG surgery. The objective of this study is to determine whether non-white patients treated by surgeons who are inexperienced with this new, off-pump, technique are more likely to undergo off-pump CABG compared with white patients treated by the same surgeons. Study Design: Retrospective analysis of the New York State Cardiac Surgery Reporting System data for 1999. These data include type of surgery, clinical risk factors that are likely to influence the choice of off-pump vs. on-pump surgery (e.g. degree of occlusion by vessel type), patient race and ethnicity, and surgeon identifier. We estimated logistic models predicting the use of off-pump vs. on-pump procedure. These models controlled for clinical risk factors, patient race and ethnicity, and surgeon volume of off-pump cases. To account for clustering of patients within surgeons we estimated mixed models with random physician effects. Patient race and ethnicity were interacted with a variable indicating the experience of the surgeon, measured by the number of offpump surgeries the surgeon performed. Population Studied: All patients undergoing isolated CABG procedures in NYS in 1999. Principal Findings: Black and white patients treated by experienced surgeons, with a high volume of off-pump surgeries, had the same probability of undergoing off-pump surgery. However, Blacks treated by surgeons with low volumes of off-pump procedures were 1.9 times (p<0.01) more likely to have off-pump surgery compared with Whites treated by the same surgeons, after controlling for patient risk factors. Similar trends were observed for Hispanics. Controlling for the number of Black patients treated by the surgeon did not change the study findings. Conclusions: The finding that Blacks that are treated by surgeons with low off-pump volume are more likely to undergo off-pump surgery than Whites cannot be explained by patient risks or the racial composition of the surgeon practice. Implications for Policy, Delivery, or Practice: This study suggests that surgeons who are inexperienced with the offpump procedure preferentially perform this new procedure on non-White patients. Since less experienced surgeons are likely to have worse outcomes, especially given that off-pump CABG surgery is more technically demanding than on-pump CABG surgery, this practice may increase the risk of poor CABG outcomes for non-White patients. This practice raises ethical concerns about disparities that should be addressed in further research to understand its causes and to allow development of appropriate policy interventions. Primary Funding Source: NIA, Commonwealth Fund, and NCMHD ●Regional Patterns of Cardiac Procedure Use Following Acute Myocardial Infarction Among American Indians Thomas Sequist, M.D., MPH, Alan M. Zaslavsky, Ph.D., James M. Galloway, M.D., John Z. Ayanian, M.D., MPP Presented By: Thomas Sequist, M.D., MPH, Instructor in Medicine and Health Care Policy, Department of Health Care Policy, Harvard Medical School, 180 Longwood Avenue, Boston, MA 02115; Tel: (617)432-3447; Email: tsequist@partners.org Research Objective: The prevalence of coronary heart disease is rising among American Indians (AI), but there is limited evidence describing processes of care for AI with acute myocardial infarction (AMI). We compared rates of cardiac catheterization, percutaneous coronary intervention (PCI), and coronary artery bypass graft surgery (CABG) between AI and whites with AMI. Study Design: We combined data from the Nationwide Inpatient Sample and the Indian Health Service National Patient Information Reporting System to identify AI receiving care in both federal and non-federal hospitals during 1998 to 2001. Admissions for AMI were defined by a primary International Classification of Diseases 9th Revision (ICD-9) diagnostic code of AMI. Cardiac catheterization, PCI, and CABG were identified using ICD-9 major procedure codes. We fit multivariate logistic regression models to compare rates of cardiac procedure use between AI and whites after adjusting for age, gender, and Charlson comorbidity index. We constructed similar models stratified by geographic region and by the presence of diabetes, as well as restricted the analysis of rates of PCI and CABG to patients undergoing cardiac catheterization. Population Studied: We identified 2,511 AI and 316,526 whites over the age of 30 years admitted with AMI during the study period. There were substantial admissions for AI in four geographic regions, including the Eastern region (n = 662), West North Central region (n = 447), West South Central region (n = 562), and the Mountain region (n=840). Principal Findings: AI were less likely than whites to undergo cardiac catheterization in 3 of 4 geographic regions, including the West North Central region [odds ratio (OR) 0.57, 95% confidence interval (CI) 0.44-0.76], the West South Central region (OR 0.32, 95% CI 0.24-0.43), and the Mountain region (OR 0.52, 95% CI 0.37-0.72). AI were less likely than whites to undergo PCI in these same regions, with odds ratios ranging from 0.43 (95% CI 0.31-0.57) in the West South Central region to 0.69 (95% CI 0.53-0.89) in the West North Central region. Nationally, AI were less likely than whites to undergo CABG (OR 0.76, 95% CI 0.60-0.95), however there was no regional variation in this difference. The presence of diabetes did not modify differences in cardiac catheterization or PCI, however AI were less likely than whites to undergo CABG among diabetic patients (OR 0.48, 95% CI 0.32-0.73), but not among non-diabetic patients (OR 0.90, 95% CI 0.72-1.12). There were no differences in rates of PCI and CABG between AI and whites among those receiving cardiac catheterization. Conclusions: Differences in cardiac procedure use are concentrated in western regions of the country and are especially related to access to cardiac catheterization. Future research is needed to elucidate the mechanisms of these differences. Implications for Policy, Delivery, or Practice: Health disparities research has often excluded American Indians due to data limitations. This study demonstrates the importance of evaluating this population, as well as highlights access to cardiac catheterization as a significant mediator of differences in access to coronary revascularization among American Indians. Future research is needed to further understand the mechanisms of this disparity and its impact on health outcomes. Primary Funding Source: No Funding Source ●Impact of Hospital Volume on Racial Disparities in Cardiovascular Procedure Mortality Amal Trivedi, M.D., MPH, Thomas D. Sequist, M.D., MPH, John Z. Ayanian, M.D., MPP Presented By: Amal Trivedi, M.D., MPH, Research Fellow, Health Care Policy, Harvard Medical School, 180 Longwood Avenue, Boston, MA 02139; Tel: (617)945-0887; Email: trivedi@hcp.med.harvard.edu Research Objective: Hospital volume is a powerful predictor of mortality for many procedures. We assessed the relative contribution of hospital volume to overall disparities in cardiovascular procedure mortality. Study Design: We analyzed 719,679 hospital discharges from the Nationwide Inpatient Sample from 1998 to 2001 with principal procedure codes for abdominal aortic aneurysm (AAA) repair, coronary artery bypass graft (CABG), percutaneous transluminal coronary angioplasty (PTCA), or carotid endarterectomy (CEA). For each procedure we compared in-hospital postoperative mortality rates for Blacks, Hispanics, and Whites, adjusting for comorbid illness using the Elixhauser method. The adjusted relation of race to receiving care in low-volume hospitals(below median) was assessed in logistic regression models controlling for age, sex, median income, location (urban/rural), payer, admission type (elective/urgent/ emergent), and comorbidity. We analyzed the impact of hospital volume on racial disparities in riskadjusted outcomes by predicting mortality with and without adjusting for hospital volume. All analyses used SAS-callable SUDAAN to account for the complex sampling and clustering of patients by hospital. Population Studied: The Nationwide Inpatient Sample (NIS) is a population-based sample of nearly 1000 nongovernmental acute care hospitals in the U.S. Principal Findings: Blacks had greater risk-adjusted mortality than Whites following elective AAA repair (OR 1.84, 95%CI 1.20-2.84), CABG (OR 1.19, 95%CI 1.06-1.33), and CEA (OR 1.56, 95%CI 1.07-2.27), but not PTCA. Hispanics had greater mortality following AAA repair (OR 1.43, 95%CI 1.08-1.89), but not other procedures. After adjusting for multiple demographic and clinical characteristics, Blacks were significantly more likely than Whites to receive AAA repair (OR 1.78, 95%CI 1.47-2.17), CEA (OR 1.77, 95%CI 1.60-1.97) and CABG (OR 1.18 95%CI 1.12-1.24) in low-volume hospitals. Blacks were not more likely to receive PTCA in low-volume hospitals. Hispanics had significantly increased odds of receiving all four procedures in low-volume hospitals relative to Whites with adjusted ORs ranging from 1.72 (95%CI 1.671.78) for PTCA to 2.64 (95%CI 2.40-2.90) for CEA. Asians had the highest use of low-volume hospitals with an increased odds relative to Whites ranging from 1.96 (95%CI 1.84-2.08) for PTCA to 3.28 (95%CI 2.76-3.89) for CEA. Hospital volume was a significant predictor of mortality with hospitals in the lowest volume quartile having a 28% (CABG) to 130% (AAA) increase in risk-adjusted mortality relative to high-volume hospitals. Adjusting for hospital volume, however, had little effect (<6% change) on the relative odds of death for Blacks and Hispanics versus Whites. Conclusions: Though minority patients are more likely to undergo cardiovascular procedures in low-volume hospitals, this racial difference in hospital volume is unlikely to explain a large portion of the racial and ethnic gap in post-procedure outcomes. Implications for Policy, Delivery, or Practice: Additional research is needed to determine why minorities are more likely to receive care in low-volume hospitals and experience higher mortality independent of hospital volume. Primary Funding Source: NRSA Institutional Training Grant Call for Panels Crossing the Cultural Chasm to Improve Quality of Care & Reduce Health Disparities Chair: Lisa Cooper, Johns Hopkins University Monday, June 27 • 2:30 pm – 4:00 pm ●Understanding Barriers to Healthcare Among Latinos: the Effects of Ethnicity, Culture Change and Discrimination Debra Joy Pérez, MA, MPA, Ph.D. Presented By: Debra Joy Pérez, MA, MPA, Ph.D., Program Officer/WKKELLOGG Fellow in Health Policy Research/Multicultural Mental Health Research Fellow/NIMH mentee, Research & Evaluation Unit/Interfaculty Program in Health Policy at Harvard, The Robert Wood Johnson Foundation/Harvard University, PO Box 3311, Princeton, NJ 08543; Tel: (609)627 5966; Email: djperez@fas.harvard.edu Research Objective: This study tests the hypothesis that changes due to acculturaion and discrimination are associated with variation in reporting barriers to care among Latinos and Non-Hispanic whites. Healthcare barriers are defined as unmet healthcare needs and postponement of needed care. A financial barrier is defined as trouble paying medical bills. The cultural change factors assessed are components of acculturation: language, identity, nativity, recency (generation) and duration in the US. The discrimination factors include perceived personal or group experience of discrimination. Logistic Regression Models are used to test the key relationships between cultural factors, discrimination and three barriers to care. Study Design: The data for this study was collected by the Kaiser Family Foundation/The Pew Hispanic Center in their 2002 National Survey of Latinos from April 4 to June 11, 2002. A nationally representative sample of 4,214 adults, 18 years and older were selected at random for this phone survey. The Random Digit Dial sample includes sub-samples of Mexicans, Puerto Ricans, Salvadorans, Dominicans, Colombians and Cubans. Of the total sample, 2,929 were self-identified Latino or Hispanic. The sample was weighted to reflect the distribution of adults in the US by country of origin, age, gender and region. There are 1008 non-Hispanic whites in the sample and 171 African Americans. Samples were stratified into three groups: total sample of whites and Latinos (3937 cases), total Latino sample (2929 cases) and Immigrant sample (2014). Analyses were conducted using chi square and logistic regression. A complex multiple imputation procedure was used to impute income values for 255 missing cases. Population Studied: Latinos: Immigrants and nonimmigrants. Substantial subsamples of Puerto Ricans, Cubans, Mexicans, Dominicans, Central Americans, South Americans and Whites. Principal Findings: Being Latino was not associated with an increased likelihood of reporting financial barriers but it was associated with a 1.86 likelihood of reporting unmet healthcare needs and a .86 likelihood of reporting postponement of care compared to whites. Latinos as a whole were no more likely to report financial barriers as compared to whites (p=.37444.) However, stratification by immigrant status revealed that nonimmigrant Latinos were statistically more likely to report financial barriers compared to Whites (p=0.05). As a group Latinos were more likely to report having unmet healthcare needs compared to whites (p=.0100.) Perceptions of postponement of care had an peculiar relationship to race/ethnicity. Whites were more likely than Latinos to report postponement of care and Non-immigrant Latinos were more likely to report postponement of care compared to immigrants. Latinos who have been in the US for more generations report higher rates of all three barriers. Latinos with a college degree were more likely than Whites with a college degree to report unmet healthcare needs but they were as likely to report financial barriers and postponement of care as Whites. Latino rates of barriers increase with each generation. Latinos in the 1st generation reported less barriers to care than Latinos in older generations. First generation Latinos reported a lower rate of financial barriers, unmet healthcare needs and postponement of care compared to Latinos in 2nd generation and beyond. Twenty percent of 1st generation Latinos reported financial barriers compared to 28% of 3rd/4th generation (p= .0172.) Thirteen percent of 1st generation Latinos compared to 20% of 3rd/4th generation reported having unmet healthcare needs (p=.0093.) Seventeen percent of 1st generation Latinos reported postponing care compared to 32% of 3rd/4th generation (p< .000.) Logistic regression showed that discrimination is a significant predictor of reporting healthcare barriers. Persons who reported discrimination were three times as likely to report an unmet healthcare need. Conclusions: This study reveals the importance of cultural components such as immigrant status and number of generations in the US in reporting barriers to care. The generation results suggest that perceptions of barriers in the US change overtime. The increase in barriers among nonimmigrants was associated with increased exposure and acculturation/integration to American mainstream. This suggests that early immigrant status is protective of barriers. The reduced reporting of barriers among immigrants may be an indication of fewer attempts at receiving care rather than fewer actual barriers. These findings suggest that organizations interested in servicing Latinos may need to develop different interventions to improve healthcare delivery and quality of care for different generations of Latinos and at different stages of their acculturation process. Implications for Policy, Delivery, or Practice: Expansion of healthcare access through insurance has been the preferred policy solution to reducing racial disparities in barriers to care between Latinos and Non-Hispanic Whites (Hargraves and Hadley, 2003; Zuvekas and Taliaferro, 2003). Yet, insurance only explains part of disparities. Other non-financial and “unobserved factors” such as culture and discrimination are significant predictors of access to and satisfaction with care (Sver et. al.; Zuvekas and Taliaferro, 2003; IOM, 2002). The findings suggest that policy orientation may need to adapt to the mult-dimensional acculuration process of the Latino population. First generation Latinos may need access-oriented policies and interventions. Second generation Latinos may be out of alignment compared to whites in identifying need and seeking appropriate medical care. They may require consumer activation policies and interventions. Third generation and beyond may benefit from efforts to improved the provider patient relationship and policies that reduce discrimination in the healthcare setting. The mechanisms explored in this research could help identify avenues for policy change to eliminate racial/ethnic disparities in healthcare. Primary Funding Source: WKK, NIMH ●Cultural Concordance Between Patient and Primary Care Provider and Cervical Cancer Screening Ninez Ponce, MPP, Ph.D., Melissa Gatchell, MPH, Jan Liu, MPH, Juanita Dimas, Ph.D., Kelvin Quan, MPH, JD Presented By: Ninez Ponce, MPP, Ph.D., Assistant Professor, Health Services, UCLA School of Public Health, 31-254 B CHS, Los Angeles, CA 90095; Tel: (310)206-4021; Email: nponce@ucla.edu Research Objective: This study examines the impact of cultural concordance, measured by language, racial and gender matches between patients and their providers on cervical cancer screening rates. We hypothesize that a language, racial and/or gender match will increase screening rates, resulting in fewer missed opportunities for detecting a virtually preventable cancer. We examine this question using Medicaid managed care data from one of the most racially diverse counties in California. Study Design: We fit multivariate logistic models to test the effect of language, ethnic, and/or gender match on Pap tests for the most commonly spoken Medicaid beneficiary languages: Vietnamese, Spanish, Farsi and English. We adjusted for beneficiary characteristics: age, medically needy designation; and provider characteristics: international medical graduate, years worked at site, medical school graduation year, specialty, and city of practice. We also estimated random effects models with PCPs as the second level, but found low intraclass correlation at the PCP-level. Relative risks and predicted probabilities from the one-level models were computed to evaluate effect sizes. Population Studied: Female members of Alameda County’s local Medicaid managed care plan, ages 25 to 64 with at least 11 months coverage in 1999 and 2000, and whose primary care physicians (PCPs) were office-based (n=1140 beneficiaries, 21 PCPs). Beneficiary profiles were linked to laboratory data on Pap test screening and to provider-level information. For provider level data, we drew on two sources: proficiency in languages other than English was assessed from a provider language survey conducted by the Medicaid managed care plan; medical training institution, specialty, and year of graduation was derived from the American Medical Association master files. Principal Findings: A language match improved the likelihood of receiving a Pap test among Spanish speaking women (RR 2.17; 95% CI 1.93, 2.43), decreased the likelihood for Vietnamese speakers (RR 0.88; 95% CI 0.84, 0.93), and had no effect for Farsi-speakers. Having a female doctor was important for Spanish speaking women, but only if that doctor also spoke Spanish: the predicted probability for a Pap test increased from 50% (gender match) to 85% (gender match and language match). Racial concordance had the strongest effect for African American women (RR 1.36; 95% CI 1.30, 1.41). There was no racial concordance effect for Latinas. Conclusions: Our findings suggest that contracting with Spanish bilingual providers benefits Spanish-speaking women. While language match conferred a negative or nil benefit to Vietnamese and Farsi speakers, a majority of these women had PCPs who spoke their primary languages. This suggests that efforts to raise screening rates for this group need to target their bilingual providers. Racial concordance had the most profound effect for African American women, inferring a strong cultural component in the patient-physician encounter. The lack of a measured effect on racial concordance for Latino women resulted from the scarcity of Latino providers in the sample, reflecting the under-representation of Latino physicians in California. Implications for Policy, Delivery, or Practice: Our study provides evidence that improving provider-patient cultural concordance can benefit some groups, and identifies training, reimbursement and educational areas needed to raise the quality of provider-patient encounters. Primary Funding Source: California Cancer Research Program ●Treatment Nihilism: Exploring Attitudinal Factors that may Contribute to Disparities in Health Care Dana Gelb Safran, Sc.D., Sara L. Thier, MPH, Ira B. Wilson, M.D., SM, William Bender, MPH, Theresa Sommers, BA, William H. Rogers, Ph.D. Presented By: Dana Gelb Safran, Sc.D., Director, The Health Institute, Institute for Clinical Research and Health Policy Studies, Tufts-New England Medical Center, 750 Washington Street, Box 345, Boston, MA 02458; Tel: (617)636-8611; Fax: (617)636-8351; Email: dsafran@tufts-nemc.org Research Objective: To explore attitudes of “treatment nihilism” expressed by Medicare beneficiaries aged 65 and older, and to examine whether these attitudes differ by race and ethnicity. Extensive research documents treatment differences that are associated with patients’ socioeconomic characteristics – most notably, race and ethnicity. However, little is understood about the mechanisms by which treatment differences arise, and in particular, the extent to which they represent clinicians’ deference to patient preferences as opposed to other factors. Study Design: A longitudinal observational study of Medicare beneficiaries aged 65 and older from 13 states nationwide (MA, NY, PA, FL, IL, MN, TX, NM, AZ, CO, CA, OR, WA). From 1998 to 2002 we monitored participants’ primary care relationships and health outcomes using a combination annual surveys and administrative data obtained from the Centers for Medicare and Medicaid Services (CMS). The 2002 questionnaire asked a series of questions concerning the subject’s likely actions if told by their primary physician that they had a “serious medical illness such as cancer or heart disease.” Analyses presented here evaluate responses to an item asserting: “I would seek as little medical care as possible and let nature take its course.” We term this treatment nihilism (TN). Population Studied: Respondents to the 2002 questionnaire (n=3449) are included in analyses that model “treatment nihilism” as a function of patients’ age, sex, race (white, African-American, Asian, other), Hispanic ethnicity, years of education, household income, functional health status, number of chronic conditions, and trust in their primary physician. Principal Findings: Overall, 10.5% of seniors revealed attitudes of TN. African-American and Hispanic elderly were more likely to report TN than non-Hispanic whites (23.9%, 22.5%, 9.7%, respectively, p<.001). Among those with less than a high school education, 24.0% expressed TN, compared with 8.9% among high school graduates (p<.001). In multivariate models controlling only for age, sex and race/ethnicity, TN was significantly associated with older age (OR=1.07 per year, p=.001), African-American race (OR=3.60, p=.001) and Hispanic ethnicity (OR=3.06, p=.001). However, after controlling for socioeconomic status (education, income), health (functional status, disease count), and patient trust, the effects of race and ethnicity were mitigated substantially (p>.06). Low educational attainment, low household income, low mental health status and older age were significantly associated with TN (p<.001). Patients with more chronic conditions were less likely to express TN (p<.01), as were those with more trusting primary care relationships (p<.001). Conclusions: Attitudes of TN are not rare among elderly adults, and are significantly higher in select subgroups. Socioeconomic factors (education, income), mental health and age emerged as the principal characteristics associated with preferring to “letting nature take its course” rather than seeking medical treatment. When these variables are masked or ignored, the attitudes appear to be attributes of AfricanAmerican race and Hispanic ethnicity. Implications for Policy, Delivery, or Practice: The findings highlight that, with extensive evidence of treatment disparities in health care, attention must turn to understanding and addressing the mechanisms by which these occur. For clinicians and health care organizations, the findings underscore that there is no short cut to knowing the values and preferences that patients hold, but rather, these must be uncovered, discussed and sometimes negotiated with each individual patient and each episode of illness. Primary Funding Source: AHRQ, Robert Wood Johnson Foundation ●Disparities in Access to Care and Health Care Utilization: Does Provider-Patient Race/Ethnicity Mix Matter? Evidence from MEPS 2002 Jaeun Shin, Ph.D., Sangho Moon, Ph.D. Presented By: Jaeun Shin, Ph.D., Professor, KDI School of Public Policy and Management, 207-43 Cheongnyangri2-dong, Dongdaemoon-gu, Seoul, 130-868; Tel: (822) 3299-1037; Fax: (822) 3299-1240; Email: jshin@kdischool.ac.kr Research Objective: Racial and ethnic disparities in access to care and health care utilization are well documented. Health insurance status and socioeconomic characteristics are often known to produce barriers to care and use of health care services among racial minorities. However, these factors do not explain racial disparities. Though previous research has raised the possibility that provider-patient race/ethnicity mix may cause this disparity, few studies examine this issue empirically. The purpose of this study is to understand differences in access to care and health care utilization between individuals with providers of identical race/ethnicity and those with providers of different race/ethnicity, and to assess the health policy implications for reducing racial/ethnic disparities in the health care provision. Study Design: Race/ethnicity mix is identified for respondents to the 2002 Medical Expenditure Panel Survey (MEPS) and their usual source of care (USC) provider. The access-to-care variables are measured by its distinguishing attributes – confidence in the USC provider (total 4 indicators) and satisfaction with the USC provider (total 6 indicators). The health care utilization variables include office-based service use, hospital outpatient and inpatient services use, ambulatory care use, dental service use, home health service use and prescription drug use (total 11 service types). Statistical significance of the differences in means is calculated using t-tests. Population Studied: The population studied includes respondents of all ages from the 2002 MEPS who identify a USC provider. The respondents are divided into two groups according to the provider-patient racial/ethnic mix (PPMIX): identical race/ethnicity (Hispanic-Hispanic, Black-Black, and White-White, I-PPMIX) and diverse race/ethnicity (Hispanicnon Hispanic, Black-non Black, and White-non White, DPPMIX) for further analysis. Principal Findings: Compared with respondents with DPPMIX, those with I-PPMIX are significantly (p<0.05) more likely to have confidence in the provider (3 out of 4 indicators): whether the person would go to the USC provider (1) for new health problems, (2) for preventive health care, and (3) for ongoing health problems. The satisfaction with the provider also is positively and significantly (p<0.01) associated with having I-PPMIX (all 6 indicators): (1) whether the provider generally listens to the person and seek person’s advice when choosing between treatments, (2) whether the provider asks about and show respect for treatments other doctors may give the person, (3) whether the provider asks the person to help make decisions, (4) whether the provider gives the person some control over treatment, (5) whether the provider explains options to the person, and (6) whether the provider speaks the person’s language or provide translator services. Having I-PPMIX has no significant relationship with the level of hospital outpatient total visits and total doctor visits. Compared with respondents with D-PPMIX, hospital inpatient total number of discharge (p<0.01) and total night stays (p<0.1), total number of emergency room visits (p<0.01), and home health total days and total agency-sponsored care days (p<0.05) are significantly lower for those with I-PPMIX, while office-based total visits and total doctor visits, total dental visits, and total number of prescription drug refills are significantly (p<0.01) higher for those with I-PPMIX. Conclusions: This study provides preliminary evidence that diverse race/ethnicity provider-patient mix may produce barriers to care, represented as weak confidence in and low satisfaction with the provider. With the identical providerpatient race/ethnicity mix, individuals may use more health care services in the settings where the provision of medical treatments involves the direct interaction between the provider and patients, such as office-based services, dental service and drug prescription service. Higher use of ambulatory service and hospital inpatient services among those with D-PPMIX may be contributed by the delayed delivery of necessary medical care. The reluctance of patients to encounter the provider due to the cultural discomfort in personal interaction may lead to lack of the usual source of care, consequently forcing the patients to depend on intensive and emergent care. Also, the potential perceived racism on the provider side against patients from different cultural background may possibly be the reason for the disparity in health care. Implications for Policy, Delivery, or Practice: Policy makers can use results from this study in developing and improving health care provision environments to reduce racial/ethnic disparity in access to care and health care utilization. Further research should pay attention to examine the influence of provider-patient race/ethnicity mix and health outcomes of the patients. Primary Funding Source: KDI School of Public Policy and Management; Sungkyunkwan University, Korea (South) ●Are Resident Physicians Prepared to Deliver Quality Care to Diverse Population? Joel Weissman, Ph.D., Joseph Betancourt, M.D., Elyse Park, Ph.D., Minah Kim, Ph.D., Eric G. Campbell, Ph.D., Brian Clarridge, Ph.D. Presented By: Joel Weissman, Ph.D., Associate Professor, Institute for Health Policy, MGH/Harvard, 50 Staniford Street, 9th floor, Boston, MA 02114; Tel: (617) 724-4731; Email: jweissman@partners.org Research Objective: The Institute of Medicine Report “Unequal Treatment” cited cross-cultural training as a mechanism to address racial and ethnic disparities in health care, but little is known about residents' preparedness to provide quality care to diverse populations or the barriers they face in practice. This study explores residents' perceptions of 1) their preparedness to deliver care to diverse patients; 2) the barriers they face in delivering such care; and 3) the educational climate for cross-cultural training at their institution. Study Design: National survey of over 2000 residents in seven specialties in their final year of training. Population Studied: Residents in six specialties in their final years of training. Principal Findings: 97% of residents felt that it is “moderately” or “very important” for physicians in their specialty “to consider the patient’s culture when providing care”. Residents reported that cross-cultural patient issues “often” resulted in longer than average visits (41% of residents), non-compliance with treatment (20%), and delays obtaining consent (18%). Although only 8% of respondents felt unprepared to care for different cultures generally, many felt unprepared to deliver specific components of crosscultural care, including caring for patients with health beliefs at odds w/ western medicine (25%), who were new immigrants (25%), or whose religious beliefs affect treatment (19%). In addition, 24% felt they lacked the skills to identify relevant cultural customs. Major barriers to delivering crosscultural care included lack of time (56% saying it was a moderate or big problem), inadequate training (31%), and lack of role models (31%). 1/3 to 1/2 of Residents received little or no instruction in specific areas of cross-cultural care beyond what was learned in med school, and 41% (family medicine) to 83% (surgery and OB/GYN) received little or no evaluation on cross-cultural issues during their residencies. Conclusions: Resident physicians preparedness to deliver cross-cultural care lags well behind preparedness to provide other key components of health care. Furthermore, our results suggest that residents received mixed educational messages. Although the topic of cross-cultural care was perceived to be important, there was little clinical time to address cultural issues, little training, and little to no formal evaluation or role modeling of cross-cultural skills. Implications for Policy, Delivery, or Practice: If eliminating racial/ethnic disparities is in part contingent on cross-cultural education, there is significant room for improvement in this area. Training environments need to augment formal and informal training mechanisms to enhance residents’ preparedness to deliver cross-cultural care to achieve the goals set by the IOM. Primary Funding Source: The California Endowment Call for Papers Communication & Care: The Role of Language & Health Literacy Chair: Anne Beal, The Commonwealth Fund Monday, June 27 • 4:30 pm – 6:00 pm ●Understanding Adverse Events in Patients with Limited English Proficiency Chandrika Divi, MPH, Andrew Chang, JD, MPH, Jerod M. Loeb, Ph.D. Presented By: Chandrika Divi, MPH, Associate Project Director, Center for Patient Safety, JCAHO, One Renaissance Boulevard, Oakbrook Terrace, IL 60181; Tel: (630)792-5918; Fax: (630)-792-4918; Email: cdivi@jcaho.org Research Objective: To examine the epidemiology of adverse events attributable to patient-provider communication problems in limited English proficient (LEP) patients. Study Design: Adverse event data were collected from hospital incident reporting systems in 6 JCAHO accredited hospitals from March 1, 2004 to August 31, 2004, and stratified by English-speaking and LEP patients. Each hospital provided de-identified incident reports pertaining to all LEP patients and a random sample of 30 incident reports pertaining to English-speaking patients. Each incident report was examined and the adverse event was deconstructed using the JCAHO Patient Safety Event Taxonomy (PSET), and classified according to the primary, secondary, tertiary and quaternary nodes of the classification scheme. Each classified incident report was reviewed by three project team members for concurrence on the classification categories used. Classified incident reports that team members disagreed over or required clinical interpretation, were further reviewed and classified by a physician. All classified adverse events pertaining to limited English proficient patients were examined for language related causative or contributive factors. The frequency of incidents categorized by the quaternary, tertiary and secondary nodes of the PSET were tabulated and compared between LEP and English-speaking patients. Population Studied: Adverse events related to Englishspeaking and limited English proficient adult patients in the hospital setting. Principal Findings: A total of 146 reported incidents met the inclusion criteria for data review, and were classified and recorded. Of these incidents, 38%(56)pertained to LEP patients. For LEP patients, under the primary classification category of Impact, “no harm” was recorded for 20%(11) incidents and “some harm” was recorded for 80%(45) incidents. Comparatively, for English speaking patients, “no harm” was recorded for 26%(23) incidents and “some harm” was recorded for 74%(67) incidents. Under the primary classification of Type, “communication” was most commonly recorded for incidents pertaining to LEP patients and Englishspeaking patients, 42%(24) and 45%(41), respectively. Under the primary classification of Cause, for incidents pertaining to LEP patients, 42%(24) incidents were due to organizational factors and 39%(22) incidents were due to practitioner related factors. For incidents pertaining to English speaking patients, 47%(42) incidents were due to organizational factors and 33%(30) incidents were due to practitioner related factors. Conclusions: Results indicate that language issues can impact patient-provider communication and contribute to adverse events that harm hospitalized patients. However, more data are required to validate the association between the degree of harm and LEP status.This impact, nonetheless, contributes towards the disparities in patient safety for vulnerable patient populations experiencing language barriers in the health care setting. Implications for Policy, Delivery, or Practice: A review of the literature has shown that that very few studies address the role of language barriers in the occurrence of adverse events in LEP patient populations. This project provides information on the impact of LEP status on the nature and occurrence of adverse events in hospitalized patients and identifies potential preventive strategies. These findings will inform, guide and facilitate the enhancement of accreditation standards directly related to culturally and linguistically appropriate health care services. Primary Funding Source: CWF ●Is What We Have Here A Failure to Communicate? A Statewide Evaluation of the Adequacy of Hospital Interpreter Services for Patients with Limited English Proficiency Glenn Flores, M.D., Sylvia Torres, Linda Holmes, Debbie Salas-Lopez, M.D., Sandy Tomany-Korman, MS, Mara Youdelman, JD, LLM Presented By: Glenn Flores, M.D., Director, Center for the Advancement of Underserved Children, Pediatrics, Medical College of Wisconsin/Children's Hospital of Wisconsin, 8701 Watertown Plank Road, Milwaukee, WI 53226; Tel: (414)4564454; Fax: (414) 456-6385; Email: gflores@mail.mcw.edu Research Objective: 47 million Americans speak a nonEnglish language at home and 21 million (including 4 million children) are limited in English proficiency (LEP). With 11% of its population LEP, New Jersey (NJ) is a model state for studying interpreter issues. The study aim was to assess the adequacy of interpreter services (IS) in NJ hospitals in meeting LEP patients’ needs, and to make actionable policy recommendations on how best to meet the needs of NJ’s LEP patients. Study Design: Cross-sectional survey in which representatives at all 122 NJ hospitals were contacted to answer 37 questions on hospital and patient features, IS, and resources/policies needed to provide quality interpreter services to LEP patients. Population Studied: Hospitals in the state of New Jersey. Principal Findings: 67 hospitals completed surveys (55% response rate). A median of 9% of staff and 33% of MDs are bilingual. A median of 93 patients per hospital need interpreters (range=0-15,000), and the median IS budget is $10,063 (range=$0-458,000). 97% of hospitals use phone IS. 87% of hospitals have no IS department, 19% offer no written translation services, and 31% lack multilingual signs. Only 3% of hospitals have a full-time interpreter, for a ratio of 1 interpreter per 235,769 LEP persons in NJ. 80% of hospitals offer no staff training on working with interpreters. The proportion of non-white patients is associated with providing written translation (P<.01) and with staff training on working with interpreters (P<.02), and the proportion of Medicare patients is associated with having multilingual signs (P<.04). Three hospitals had model programs with more extensive IS. Hospitals stated the following would improve IS at their institutions: more funding; federal/state interpreter certification and guidelines; more MD/staff education on interpreter use; listing locally available interpreters; and identifying bilingual staff. Most said 3rd-party reimbursement for IS would be beneficial, by reducing costs, adding full-time interpreters, freeing staff for other services, meeting future population growth, and improving communication and education. Conclusions: Most NJ hospitals have no formal interpreter services department, 97% have no full-time interpreter, 80% provide no staff training on working with interpreters, and deficiencies exist in hospital signage and translation services. Most NJ hospitals said 3rd-party reimbursement for interpreter services would benefit their hospitals. Implications for Policy, Delivery, or Practice: Based on these findings, we suggest NJ provide third-party reimbursement of IS statewide. If restrictive state budgetary challenges preclude full implementation of third-party reimbursement, we suggest considering one or more of the following: 1) Provide Medicaid/SCHIP reimbursement for IS in the emergency department; 2) Use federal Medicaid and SCHIP matching reimbursement funds to train more qualified medical interpreters; 3) Negotiate bulk discounts with telephone interpreter services; 4) Consider using funds from the state’s Office of Refugee Resettlement and/or English as a Second Language Program; 5) Utilize employer pressure to encourage greater access to healthcare services for LEP employees; 6) Utilize innovative, cost effective technologies to improve access to trained medical interpreters, such as remote simultaneous interpretation and telemedicine networks; 7) Consider implementing licensure requirements and state regulations mandating adequate access to IS for LEP patients; and 8) If other measures fail, consider legal options to enforce compliance with Title VI of the Civil Rights Act. Primary Funding Source: Office of Minority and Multicultural Health, New Jersey Department of Health and Senior Services ●Pap Test Use Among English, Spanish, Cantonese, Mandarin, Korean, Vietnamese, and Khmer Speaking Women: Is there a Language Divide? Ninez Ponce, MPP, Ph.D., Neetu Chawla, MPH, Susan Babey, Ph.D., E. Richard Brown, Ph.D., Nancy Breen, Ph.D. Presented By: Ninez Ponce, MPP, Ph.D., Assistant Professor, Health Services, UCLA School of Public Health, 31-254B CHS, Los Angeles, CA, CA 90095; Tel: (310)206-4021; Fax: (310)4559475; Email: nponce@ucla.edu Research Objective: Racial and ethnic disparities exist in cervical cancer screening . We examined whether primary language use, measured by language of interview, contributes to disparities in Pap test rates using a population-based sample of California women. Study Design: This study used data from the 2001 California Health Interview Survey (CHIS). CHIS 2001 is a random-digit dial (RDD) telephone survey of 55,428 households drawn from every county in California and is the largest statewide health survey conducted in the United States. The sample was designed to provide estimates for California's overall population, its major racial and ethnic groups, and a number of ethnic subgroups. CHIS 2001 was conducted in six languages: English, Spanish, Chinese (Cantonese and Mandarin dialects), Korean, Vietnamese, and Khmer. Multivariate logistic regression analyses were used to determine factors associated with three-year Pap test use. Factors studied include race/ethnicity and language of interview, marital status, income, educational attainment, level of acculturation, insurance status, usual source of care, smoking status, area of residence, and health status. Population Studied: The population studied was California women, ages 25 to 64, who did not report a cervical cancer diagnosis or a hysterectomy (n = 23,387). Principal Findings: Adjusting for all other covariates, we found that Asian women speaking English (RR 0.91; 95% CI 0.87, 0.95), Cantonese (RR 0.82; 95% CI 0.67, 0.93), Mandarin (RR 0.78; 95% CI 0.62, 0.91), Khmer (RR 0.73; 0.33, 0.99), and Korean (RR 0.92; 0.81, 1.00) were significantly less likely to have had a Pap test in the past three years than Englishspeaking white women. In addition, multivariate results showed that Spanish-speaking White women (RR 1.09; 95% CI 1.04, 1.10) and Spanish-speaking Latinas (RR 1.06; 95% CI 1.05, 1.07) were the most likely to be screened. Conclusions: Large language disparities in cervical cancer screening are present in California, where Asian women speaking Cantonese, Mandarin, Khmer, and Korean had the lowest rates of Pap tests compared to English-speaking Whites. However, even English-speaking Asians had considerably lower screening rates, suggesting that both cultural and language barriers exist. Spanish-speaking women are the most likely to report three-year Pap test use and Vietnamese-speakers had screening rates comparable to English-speaking White women. Implications for Policy, Delivery, or Practice: Although Federal civil rights law and policy require that most health care providers make interpretation services available to patients who need it, such laws and policies are difficult to enforce so that barriers due to language may still exist. Our findings suggest that in addition to English and Spanish, cancer screening services should be available in multiple languages, particularly Asian languages. Furthermore, patient and provider awareness campaigns need to consider both linguistic and cultural bridging strategies to raise the screening participation among Asian women. Spanish and Vietnamese language access efforts may have broader coverage and comprehensiveness in promoting Pap test use than similar efforts in other languages. These efforts could serve as a model for improving screening rates among Cantonese, Mandarin, Khmer, and Korean speakers in California and in the United States. Primary Funding Source: NCI, The California Endowment ●Reducing Disparities in Mental Health Care by Targeting Language and Insurance Barriers Tetine Sentell, Ph.D., Martha Shumway, Ph.D., Lonnie Snowden, Ph.D. Presented By: Tetine Sentell, Ph.D., Postdoctoral Fellow, Psychiatry, UCSF, 2727 Mariposa Street, Suite 100, San Francisco, CA 94110; Tel: (415)437-3075; Fax: (415)437-3020; Email: tsentell@itsa.ucsf.edu Research Objective: Untreated mental illness is a significant policy problem with high fiscal and social costs, particularly among racial/ethnic minorities. This study compared four potential policy actions to address disparities in mental health treatment: (1) providing health insurance, (2) providing health insurance and minimizing language barriers, (3) providing health insurance with mental health coverage, and (4) providing health insurance with mental health coverage and minimizing language barriers. Study Design: Using the 2001 California Health Interview Survey (CHIS), a representative sample of 55,428 California adults, logistic regressions were estimated to predict unmet need and to compare the statewide impact of the four policy actions. Population Studied: The sample included adults aged 18 to 64 who self-reported a mental health need (n=6,994; 16% of non-elderly adult respondents). To maximize impact, predictive models were estimated specifically for Californians most likely to need, and least likely to receive, mental health care (e.g., poor, limited education, limited English proficiency). Principal Findings: Forty-two percent of respondents had an unmet mental health need. Race/ethnicity, lack of English proficiency, and lack of insurance were significant barriers to care. Fifty-three percent of Whites, 42% of African Americans, 31% of Asians, and 24% of Latinos received needed care. Fifty percent of proficient English speakers received needed services versus 9% of those with limited English proficiency. Insured adults were twice as likely to have received needed care than the uninsured when other variables were controlled. Policy action 1— providing health insurance— increased receipt of needed services dramatically among African Americans, but did not greatly benefit Latinos and Asian/PIs. Policy action 2 —providing health insurance and minimizing language barriers — did increase receipt of needed services among Latinos and Asian/PIs. Policy action 3— providing insurance with mental health coverage— was particularly beneficial to Asian/PIs, increasing receipt of needed services to 93%. But policy action 4— providing health insurance with mental health coverage and minimizing language barriers— had the greatest benefit for Asians/PIs and Latinos specifically, as well as overall, increasing receipt of services by all disadvantaged Californians to 67%. Conclusions: A high level of unmet need for mental health care persists, particularly among minority groups with limited English proficiency. Policy action appears to decrease disparities among those who need care, though actions do not equally benefit all groups. Tested policy actions appear to particularly benefit Asian/PIs. Only 31% of Asian/PI CHIS respondents received needed mental health services, but under the final hypothetical policy action an estimated 97% would receive needed care. Although tested policy actions almost double receipt of needed services among Latinos from 24% (in the CHIS) to 45% (with the final policy action), almost half of Latinos would still have unmet mental health needs, suggesting the presence of other barriers that perpetuate disparities among Latinos. Implications for Policy, Delivery, or Practice: Improving access to insurance and decreasing language barriers are policy actions that appear to reduce racial/ethnic disparities in unmet need for mental health services, indicating that seeking mental health treatment, though a deeply personal choice, can be influenced by large-scale, systemic changes amenable to policy action. Primary Funding Source: NIMH ●Improving Patient Safety through Informed Consent in Populations with Limited Health Literacy Helen Wu, M.Sc., Robyn Y. Nishimi, Ph.D., Christine M. PageLopez, Kenneth W. Kizer, M.D., MPH Presented By: Helen Wu, M.Sc., Program Director, National Quality Forum, 601 13th Street NW, Suite 500N, Washington, DC 20005; Tel: (202)783-1300; Fax: (202)783-3434; Email: hwu@qualityforum.org Research Objective: In 2003, the National Quality Forum, NQF, endorsed as voluntary consensus standards a set of 30 safe practices that have been demonstrated to improve patient safety. This project evaluated number 10 of those safe practices, which relates to informed consent and which is particularly important in populations with limited health literacy. This project sought to identify strategies to facilitate widespread adoption of Safe Practice 10. Study Design: The main component of Safe Practice 10 calls for providers to ask each patient, or his/her legal surrogate, to recount what he or she was told during the informed consent discussion, with the objective of ensuring the patient understands the proposed treatment and its potential consequences. Also known as teach back, this practice has been shown to improve patient recall and understanding, and it allows providers to gauge patient understanding and whether informed consent was actually achieved. Additional specifications of Safe Practice 10 address other components of the informed consent process, including consent forms, verbal discussion, and the use of interpreters. The project had three components: 1. an in-depth assessment of the experiences of four hospitals that had implemented teach back as a standard practice; 2. phone interviews with providers that had not adopted Safe Practice 10 so as to identify major barriers to implementation of the practice; and 3. a multi-stakeholder workshop to review and refine preliminary project findings. Population Studied: Patients undergoing invasive, noninvestigational, non-emergent procedures, with a special focus on patients with limited health literacy - defined as those with limited English proficiency, low literacy, and other difficulties understanding healthcare terminology and concepts. Principal Findings: Providers who used teach back demonstrated numerous benefits of the practice: surgical errors and serious adverse events were avoided, efficiency was improved and costs were lowered due to substantially lower rates of surgical cancellations/delays, and trust was improved between providers and patients. Teach back was found to be an important practice to improve patient safety, quality, and communication. Overall, these benefits far outweighed the perceived time burden of asking patients to recount information related to the informed consent. Healthcare providers may face challenges in successfully adopting and implementing Safe Practice 10, such as buy-in from physicians about the importance of the practice, but those challenges can be overcome if a sufficient case is made for the importance of proper informed consent and the benefits of teach back. Conclusions: Safe Practice 10 provides an evidence-based, feasible, and usable strategy to enhance the safety of the caregiving process. Implications for Policy, Delivery, or Practice: Providing informed consent is an ethical, professional, and legal duty of physicians, but one that is often overlooked or given short shrift. Patients who are well informed are more satisfied with their care, more likely to have a good outcome, more trusting of their providers, and more able to make decisions that reflect their personal preferences and values. Effective communication between providers and patients is central to informed consent. Use of Safe Practice 10 increases the effectiveness of provider-patient communication and may reduce potentially adverse events. Primary Funding Source: CWF Call for Papers Can the Appropriate Consumption of Health Care Reduce Disparities? Chair: Marsha Lillie-Blanton, The Henry J. Kaiser Family Foundation Tuesday, June 28 • 8:30 am – 10:00 am ●Racial/Ethnic Disparities in Behavioral Counseling: the Case of Hispanic/White Difference in the Receipt of Smoking Cessation Advice Yuhua Bao, Ph.D. Presented By: Yuhua Bao, Ph.D., Division of General Internal Medicine and Health Services Research, David Geffen School of Medicine, UCLA, 1100 Glendon Avenue, Suite 2010, Los Angeles, CA 90024; Tel: (310)794-3081; Email: yuhuabao@mednet.ucla.edu Research Objective: Racial/ethnic differences in health behaviors and lifestyles likely account for a substantial amount of the racial/ethnic disparities in health. There is strong evidence that provider behavioral counseling can be effective in helping patients change certain health behaviors. Disparities in behavioral counseling, if any, can thus aggravate racial/ethnic disparities in the prevalence and burden of diseases. This paper discusses some of the issues in studying racial/ethnic disparities in behavioral counseling by using the example of Hispanic/white difference in the receipt of smoking cessation counseling. Study Design: We define primary (secondary) behavioral counseling as counseling delivered to patients who do not yet have (already have) behavior-related health conditions. We first conceptually discuss why overall disparity (or the lack of it) could be a misleading depiction of possible disparities in primary or secondary counseling. To provide an empirical example, we then estimate the Hispanic/white difference in the receipt of smoking cessation advice from their regular healthcare providers during the past 12 months. We use the 2001 National Health Interview Survey Sample Adult File and stratify the logistic regression analysis of receiving some provider advice to quit smoking by the presence of smokingrelated health conditions. These conditions include myocardial infarction/coronary heart disease/stroke, less serious heart conditions, emphysema/chronic bronchitis/asthma, and some types of cancer. Population Studied: Adult patients (Hispanic or nonHispanic white according to self identification) who were current smokers and who had some contact in the past 12 months with the health care providers or facilities they most often went to for acute or preventive care. Principal Findings: Overall, the rate of receiving some smoking cessation advice was lower among Hispanic patients than among white patients (52.6% vs. 69.5%). After adjusting for essential demographic information, the intensity of smoking and the presence of smoking-related health conditions, the difference remained at 9 percentage points (p<0.001). However, results of stratified analysis indicated that the overall disparity was almost entirely accounted for by the disparity in primary counseling: the adjusted Hispanic/white ratio in the probability of primary smoking cessation advice was 0.77, reflecting an absolute difference of 15 percentage points (p<0.001). Meanwhile, the difference among patients with smoking-related conditions was negligible and not statistically significant. Conclusions: The Hispanic/white disparity in smoking cessation counseling was mainly a result of the much lower rate of counseling among Hispanic patients before the onset of smoking-related conditions. Since primary behavioral counseling is more discretionary and often receives less priority than diagnostic or therapeutic services, factors pertaining to the care process such as provider stereotyping and the uncertainty in assessing minority patients’ preventive care need could have given rise to the disparity. Implications for Policy, Delivery, or Practice: Racial/ethnic disparities in primary behavioral counseling could eventually lead to or aggravate the disparities in disease prevalence; disparities in secondary counseling may mean disproportionate burden of morbidity and mortality associated with the conditions. Future studies will need to investigate behavioral counseling in the primary vs. secondary context separately to provide relevant implications for closing the racial/ethnic disparities in health and healthcare. Primary Funding Source: NIH EXPORT Center ●Identifying Racial and Ethnic Disparities in Ambulatory Care Sensitive Conditions among Medicare Beneficiaries Arthur Bonito, Ph.D., Celia Eicheldinger, MS, Linda Greenberg, Ph.D., Arthur Meltzer, Ph.D. Presented By: Arthur Bonito, Ph.D., Research Triangle Institute, Box 12194, 3040 Cornwallis Road, Research Triangle Park, NC 27709; Tel: (919)541-6377; Fax: (919)990-8454; Email: ajb@rti.org Research Objective: Hospital and emergency room treatment for ambulatory care sensitive conditions, or ACSCs, may serve as a marker for inadequate access to or use of standard ambulatory health care services. The objective of this study was to more accurately assess the occurrence of racial and ethnic disparities in the proportion of Medicare beneficiaries with selected ACSCs in 2002. Study Design: As a precursor to this study, we developed an algorithm employing surname, geographic location, common first names, and information on the Medicare Enrollment Database to improve the race and ethnicity coding of Hispanic and Asian and Pacific Island Medicare beneficiaries. Using the improved race and ethnicity code, we selected a stratified random sample of Medicare beneficiaries. Stratification was disproportionate by race and ethnicity to include large enough numbers to allow reliable investigation of disparities. We used Medicare claims to identify hospital and emergency room discharges for persons having principal diagnoses for five chronic ACSCs: diabetes mellitus, chronic lung disease, congestive heart failure, hypertension, and seizures. Population Studied: The study sample of nearly two million beneficiaries was weighted in our analyses to represent the approximately 28 million Medicare beneficiaries in the traditional fee-for-service plan for the entire CY 2002, including Whites, Blacks, Hispanics, and Asians and Pacific Islanders. Principal Findings: Using White beneficiaries’ rates as the basis for comparison, the rates of treatment for ACSCs for Blacks ranged from 10 percent greater than Whites for chronic lung disease to almost four times higher for diabetes and hypertension. For Hispanics, the rates ranged from no different on three ACSCs -- seizures, congestive heart failure, and chronic lung disease -- to twice as high or more for hypertension and diabetes. For Asians and Pacific Islanders, the rates were comparable to Whites for diabetes, about 20 percent higher for hypertension, and about half as much for chronic lung disease, congestive heart failure, and seizures. In summary, Blacks had the highest rates for all five ACSCs. Whites had the lowest rate for only one of the ACSCs, hypertension. Whites and Asians and Pacific Islanders had virtually the same lowest rate for diabetes mellitus. Asians and Pacific Islanders alone had the lowest rates for the other three ACSCs. Conclusions: Our analyses found patterns of differences among racial and ethnic groups for five chronic ACSCs. Of the four racial and ethnic groups, Blacks have the worst access to ambulatory care. Asians and Pacific Islanders have as good or better access to services as Whites. Hispanics’ access to primary care is better than Blacks, but worse than Whites. Implications for Policy, Delivery, or Practice: We have identified disparities in ACSCs among four racial and ethnic groups based on a more complete identification of Medicare beneficiaries by race and ethnicity. Study findings hold promise for more valid and reliable assessment of health disparities among the racial and ethnic minorities enrolled in Medicare. Also, they provide policy makers with information to more effectively target efforts to racial and ethnic groups most in need, and to identify, monitor, and assess progress toward elimination of health disparities. Primary Funding Source: CMS ●To Voice or to Exit: Racial Differences in Consumer Responses to Problematic Health Care Experiences Lisa C. Gary, MS, MPH, Mark Schlesinger, Ph.D. Presented By: Lisa C. Gary, MS, MPH, Doctoral Candidate, Health Policy, Yale University, 60 College Street P.O. Box 208034, New Haven, CT 06510; Tel: (203)787-9943; Email: lisa.gary@yale.edu Research Objective: To identify health system characteristics (e.g.- managed care) and patient characteristics (e.g.-level of patient trust) that are associated with active consumer empowerment. Study Design: Background: Managed care has a significant impact on the way health care is delivered in the US. In fact most consumers with employer sponsored health insurance are enrolled in a health plan with some type of managed care practice such as prior authorization rules, utilization review, closed panels of providers, and primary care provider requirements. Current research shows that managed care has led to diminished consumer trust in health systems and low levels of patient satisfaction. These findings are particularly salient in light of the vast racial health care disparities we see. The data are overwhelming that minorities in the U.S. receive significantly lower quality care across a range of diseases e.g.cancer, cardiac care, pain management, and some preventive care. Low patient trust may be indicative of feelings of disempowerment and alienation in the health care system especially for minorities and other vulnerable groups. The consumer empowerment behaviors under study are voicing and exit. Voicing refers to instances when consumers express their concern over negative health care encounters. The targets for voicing may be informal or formal such as talking with family and friends or registering complaints with the health plan or a government authority. Exit refers to a consumer’s decision to change health plans or physicians in response to unsatisfactory health care episodes. Data Source: Data are from the Yale/New York Academy of Medicine Survey of Consumer Experiences in Health Care, a telephone survey of approximately 5000 individuals representing the US non-institutionalized population. The racial/ethnic groups represented include African Americans, Hispanics, Whites, Asians, and other racial groups. Population Studied: Methods: We use logistic regression, ordered logistic regression, and bivariate probit models with selection (the dichotomous version of Heckman selection models) to determine if race is a significant factor in the degree of trust in physicians and health plans, likelihood of experiencing negative health care episodes, and type of consumer self-advocacy controlling for various psychosocial and health system factors including perceived vulnerability, informational social support, health system knowledge, and several managed care health plan practices . Principal Findings: For the analysis on consumer empowerment behaviors, blacks were less likely to voice dissatisfaction about problematic health care encounters compared to whites. We examined voicing in three domains 1) voicing to family, friends, or an employer, 2) voicing to the health plan, and 3) voicing to one’s physician. Blacks were less likely to voice to any of these entities compared to whites after controlling for educational status, health plan characteristics, perceived vulnerability, and informational social support. Blacks were significantly less likely to voice dissatisfaction to their personal physicians. Interestingly, blacks were more likely to “exit” as a result of negative health care experiences than whites. Blacks tend to exert control or exhibit agency by simply leaving these bad situations; however, it is unclear whether these exit decisions will lead to better care in the new health plan or physician relationship. This type of empowerment behavior may be futile and silent in many ways and in fact it indicates that effective consumer voice may not be a real option for many African Americans. In light of the low levels of trust in physicians and health plans, these minority consumers may fear retribution, limited system response to their concerns, or be subjected to disrespect and alienation for voicing their opinions so they simply exit. Implications for Policy, Delivery, or Practice: The development of culturally relevant consumer empowerment health promotion tools could be very useful for improving clinical and administrative interactions for minority patients. Primary Funding Source: NIMH, Aspen Institute ●Mediators of Race Effects on Risk of Potentially Avoidable Maternity Complications among MedicaidInsured Mothers Sarah Laditka, Ph.D., MA, MBA, James N. Laditka, D.A., Ph.D., Janice C. Probst, Ph.D. Presented By: Sarah Laditka, Ph.D., MA, MBA, Associate Professor and MHA Program Director, Health Services Policy and Management, University of South Carolina, 800 Sumter Street, HESC Building, Room 116F, Columbia, SC 29201; Tel: (803)777-1496; Fax: (803) 777-1826; Email: sladitka@gwm.sc.edu Research Objective: Studies have found that African American women receive less prenatal care than do white women, and are more likely to have pregnancy complications. We examined both the risks of pregnancy complications and factors associated with these risks focusing on differences by race and ethnicity, using state-level data from South Carolina. The data provide detailed individual-level information such as marital status, income, and education. Such information is not commonly available in administrative datasets. We used the Potentially Avoidable Maternity Complication (PAMC) indicator to evaluate pregnancy outcomes associated with access to prenatal care of reasonable quality. PAMCs, defined by a panel of obstetricians and health services researchers, are identified through combinations of primary and secondary hospital diagnoses at delivery, such as both a urinary tract infection and a complication known to be associated with such infections. Study Design: Delivery hospitalization data for the year 2000 for Medicaid-insured women were obtained from the South Carolina Budget and Control Board. We supplemented these data with information from the 2000 Area Resource File and the 2000 annual survey of the American Hospital Association. Analyses included chi-square and multilevel logistic regression. Controls included age, educational attainment, marital status, income, comorbidities, and characteristics of mothers’ residence counties and delivery hospitals. Population Studied: 26,869 delivery hospital discharges for Medicaid-insured women in South Carolina, year 2000. Principal Findings: Not controlling for other factors, African American mothers had higher odds of having a PAMC than did white women (OR 1.26, p<.001). In the multivariate model, the odds of experiencing a PAMC did not differ between African American and white mothers. Notable PAMC predictors were (odds ratios in parentheses): being single (1.58, p<.0001), having income below the poverty threshold (1.30, p<.001), being disabled (1.51, p=.05), having diabetes (2.29, p<.001), and living in a rural county (1.96, p=.05). Bivariate analyses showed that, compared with whites, African Americans were more likely to (odds ratios in parentheses, all p<.0001): be single (2.45), have income below the poverty threshold (1.66), be disabled (1.54), have diabetes (1.82), and live in a rural county (1.29). Thus, risk factors disproportionately affecting African Americans contributed notably to PAMC risk at the population level. Conclusions: The greater PAMC risk of African Americans mothers at the population level is notably attributable to specific measurable risk factors. Single African American Medicaid beneficiaries and those with diabetes are at particularly high risk of avoidable pregnancy complications. Implications for Policy, Delivery, or Practice: PAMC analyses can suggest efficient approaches to addressing disparities in pregnancy outcomes associated with the accessibility and qualities of prenatal care. Healthy Start programs, community health centers, and rural health clinics may be particularly useful for addressing pregnancy risks associated with poverty, single parent status, and chronic disease. Particularly in rural areas, poor, disabled, and single pregnant women may benefit from transportation and other forms of proactive support to attend prenatal care. Prenatal care for African American Medicaid beneficiaries should stress diabetes control. Primary Funding Source: HRSA ●Racial/Ethnic Differences in the Use of Health Information to Self-Advocate During the Medical Encounter: Is Having Health Information Enough? Jacqueline Wiltshire, MPH, Ph.D., Kate Cronin, MPH Presented By: Jacqueline Wiltshire, MPH, Ph.D., PostDoctoral Fellow, Center for Women's Health Research, University of Wisconsin Medical School, 202 South Park Street, 6W, Madison, WI 53715; Tel: (608)-267-5566; Fax: (608)-267-5575; Email: wiltshire@wisc.edu Research Objective: Patients with self-advocacy orientation gain maximum benefit from the medical encounter. However, little research has been conducted on how patients’ knowledge and use of health information influence the medical encounter. Moreover, little is known about the racial/ethnic differences in the use of health information to self-advocate during the medical encounter. The purpose of this study is to examine (1) whether health information empowers midlife women to self-advocate during the medical encounter, and (2) whether self-advocacy differs by race/ethnicity. Study Design: Study data were drawn from the 2000-01 Household Component of the Community Tracking Study, a nationally representative survey. To operationalize health information, sources of acquiring health information in the past 12 months (internet, friends, TV or radio, books/magazine/other source, and health care professional/organization) was aggregated. Self-advocacy was operationalized through yes/no responses to the following questions: “Did the doctor order a test, procedure, or prescription for you mainly because of information that you mentioned or showed to him or her?; During the past 12 months, have you mentioned information to a doctor about a medical condition or treatment for you that you found out about yourself or were told by others?” All regression analyses accounted for complex survey design and were adjusted for race/ethnicity, age, marital status, rural/urban, education, health status, employment, federal poverty level, and insurance type. Population Studied: The sample included 6,234 Whites, 858 African American, 507 Hispanic, and 207 Native/Asian/Pacific/Other women aged 45 to 64 with at least one doctor visit. Principal Findings: Overall, 47.5% of the women reported getting medical information (49.3% of Whites, 39.6 of African Americans, 44.1% of Native/Asian/Pacific/Other and 41.4 of Hispanics). Seventeen percent of all women mentioned medical information to doctor and 8.1% reported that the doctor used the information to order a test, procedure, or prescription. After multivariable adjustment using logistic regression, women who had obtained health information were 5 times more likely to mention information to their doctor (OR=5.00, 95% CI: 4.25-5.89) and 4 times more likely to get a test/procedure/prescription from their doctor (OR=4.23, 95%CI: 3.36-5.33). African Americans were less likely to mention information to a doctor (OR=0.55, 95%CI: 0.39-0.79) and there were no significant differences in race/ethnicity with regards to doctor ordering a test. Moreover, when Whites were removed from the analysis (n=1,635), Native/Asian/Pacific/Other and Hispanics were more likely to mention information to a doctor (OR=2.05, 95%CI: 2.05, 1.263.32, OR=2.05, 95%CI: 1.61, 1.07-2.42, respectively); and Hispanics were more likely to get a test/procedure/prescription ordered from their doctor (OR=1.82, 95%CI:1.05-3.17). Conclusions: While health information empowers midlife women to self-advocate, African American women are least likely to self-advocate using previously acquired health information. Factors or barriers that may impede the ability of African American women to self-advocate need to be identified. Implications for Policy, Delivery, or Practice: Every health care encounter should be seen as an opportunity to foster an environment which promotes self-advocacy among patients. Primary Funding Source: NIA Related Posters Poster Session B Monday, June 27 • 6:15 pm – 7:30 pm ●Medicare: An Investigation of Inequalities in Access Jean Accius, Master's in Aging Studies Presented By: Jean Accius, Master's in Aging Studies, Doctoral Student, School of Public Affairs, American University, 4400 Massachusetts Avenue NW, Washington, DC 20016; Tel: (850) 321-7917; Email: acciusj@hotmail.com Research Objective: Given well-documented racial healthdisparities, access to care within the healthcare system amongst racial groups is a primary concern. Medicare, one of the largest government-sponsored health programs, has the potential to reduce these health disparities. However, whether racial minorities receive the care they need through Medicare is unknown as previous research on the topic has focused on the relationship between access to care and health status, and not race. Study Design: This research paper contributes to the literature by examining the disparities that exist within the Medicare Program between black and non-black beneficiaries within the area of access to care. More specifically, is the Medicare program relatively inaccessible to the needs of blacks in comparison to non-blacks in terms of access to care? My hypothesis is that the Medicare Program is not sufficient in meeting the needs of blacks relative to their counterparts. Population Studied: This paper uses data from the 1993 Medicare Beneficiary Survey. The MCBS, collected by the Office of Strategic Planning of the Center for Medicare and Medicaid Services, is a continuous, multipurpose survey of a nationally representative sample of aged, disabled, and institutionalized Medicare beneficiaries. Beneficiaries are sampled from the Medicare enrollment files and interviewed in person three times a year using computer-assisted personal interviewing. Newly admitted beneficiaries are added to the sample once a year and deaths or refusals are depleted from the sample. The response rate for the 1993 survey was 87 percent, yielding a sample size of 12,895. The analysis sample constituted of 11, 177 observations. Principal Findings: Preliminary bivariate results suggest that blacks were more satisfied with the availability of care than non-blacks. Primary Funding Source: No Funding Source ●Patient Preferences for Participatory Decision-making: Patient Race, Education and Physician Perceptions Gbemisola Adeseun, BS, MPH, Lisa A. Cooper, M.D., MPH, Presented By: Gbemisola Adeseun, BS, MPH, Medical Student, Welch Center for Prevention, Epidemiology & Clinical Research, Johns Hopkins University, 2024 East Monument Street, Suite 2-500, Baltimore, MD 21287; Tel: (410) 303-9428; Email: gadeseun@jhmi.edu Research Objective: Participatory decision-making is linked to positive patient outcomes, including satisfaction, adherence, and continuity of care. Previous studies suggest that ethnic minorities and less educated patients experience less participatory visits with physicians. However, little work examines whether patient preferences for participatory decision-making (PDM) and physician perceptions of those preferences differ across patients’ race/ethnicity or education. We examined whether: 1) patients’ race and educational level are associated with their preferences for PDM and 2) physicians’ perceptions of patient preferences for PDM are influenced by patients’ race and education. Study Design: We conducted a brief cohort study of patients and physicians in primary care practices serving managed care and fee-for-service patients in Baltimore, MD, Washington DC, and Northern VA areas in 2002. Our main outcomes of interest, collected from pre- and post-visit questionnaires, were: 1) patient preferences for PDM, measured before the visit using an item from the Autonomy Preference Index and 2) physicians’ predictions of individual patient’s preferences for PDM measured after the visit. We used logistic regression with generalized estimating equations to account for the clustering of patients by physicians and adjusted for patient, age, gender, and health status and physician race in multivariate models. Population Studied: Two-hundred and six patients seeing 30 physicians participated in the study. Patients had an average age of 51 years; they were 65% women; 55% African American and 45% white; and 38% had less than high school (HS) education, 32% were HS graduates, and 31% had some college education. Principal Findings: The probability of preferring PDM was similar for white and African-American patients (72% vs. 62%, P=0.09). Individuals with less than high school education, high school graduates, and some college education and beyond were equally likely to desire PDM (Pr 0.65, 0.61, 0.73, respectively; P >0.05). Physicians perceived that: 1) white and African-American patients were equally likely to desire participatory decision-making (Pr 0.65 and 0.67, respectively; P=0.42) and 2) individuals without a high school diploma were less likely to desire PDM compared to individuals with some college education and beyond (Pr 0.54 vs. 0.76, respectively; P =0.03). Conclusions: Patient preferences for participatory decisionmaking do not differ by race or education. While physicians do not perceive ethnic minorities as preferring less participation in care, they do misperceive individuals with less than high school education as desiring less active roles in decision-making. Implications for Policy, Delivery, or Practice: Interventions to increase physicians’ PDM behaviors with patients regardless of educational level may better meet less educated patients’ needs to play active roles in medical decisionmaking. Primary Funding Source: CWF, National Center or Minority Health Disparities ●Differences in Neonatal Mortality among Whites and Asian Subgroups: Evidence from California 1991-2001 Laurence Baker, Ph.D., Christopher Afendulis, Ph.D., Amitabh Chandra, Ph.D., Elena Fuentes-Afflick, M.D., Shannon McConnville, MA, Ciaran Phibbs, Ph.D. Presented By: Laurence Baker, Ph.D., Associate Professor, Health Research and Policy, Stanford University School of Medicine, HRP Redwood Building, Room 110, Stanford, CA 94305-5405; Tel: (650)723-4098; Fax: (650)725-6951; Email: laurence.baker@stanford.edu Research Objective: The number of Asian-American newborns has grown rapidly over the past 20 years, but there is relatively little evidence about health outcomes for AsianAmericans as a group or for national origin subgroups of the larger Asian-American population. Data limitations have left previous studies able to study only small numbers of AsianAmerican newborns and precluded detailed comparisons across a large number of subgroups. The objective of this study is to provide new data on Asian-American births and outcomes, comparing most Asian-American subgroups with large and detailed data. Study Design: Cross-sectional and longitudinal comparisons of birth outcomes among nine Asian-American subgroups (Cambodian, Chinese, Filipino, Indian, Japanese, Korean, Laotian, Thai, and Vietnamese) and Whites. We use data linking birth certificates, death certificates, and hospital discharge records for newborns and mothers. We compare birthweights, newborn complications, comorbidities, and other risk factors across the various groups. We use logistic regression to examine differences in neonatal mortality. For the mortality models, the dependent variable was 28 day mortality and maternal race/ethnicity was the primarily independent variable. Some models include only basic controls. Others include extensive controls for maternal age, education, nativity, and prenatal care use; newborn gender, birth weight and neonatal and maternal risk factors. Comparing results across models with and without the additional controls allows us to assess the impact of including the risk factors on the estimated mortality differences across the various groups. Population Studied: 2.4 million births in California for 19912001 for non-Latina White and Asian women from the nine subgroups. Principal Findings: Birthweights and risk factors vary noticeably across the various groups. Mortality rates also vary. In unadjusted comparisons, infants born to Chinese, Japanese, and Korean women had significantly lower neonatal mortality rates than infants born to White women, while Thai infants had significantly higher rates. Observable risk factors account for some of the differences, but not all. After controlling for risk factors, the mortality risk for Japanese newborns was about one-third lower than the risk for Whites, and the risk for Filipino infants was about one-sixth lower (both p<0.05). After adjustment, Thai infants had mortality risk nearly twice as high as Whites (p<0.05). Some differential trends over time were also observed, with infants born to Filipina women experiencing the greatest decline. Conclusions: : In California, the risk of neonatal mortality varies by Asian national origin subgroup. Observable risk factors explain some, but not all of the differences across groups. Implications for Policy, Delivery, or Practice: Further efforts to reduce neonatal mortality among Asians should identify and address the needs of high-risk subgroups. Much current work groups all Asian Americans together, but efforts to collect more detailed data and include more detailed categories in analyses could be valuable. Primary Funding Source: National Institute on Child Health and Development ●Access to Neonatal Intensive Care and the Black-White Newborn Outcomes Difference Laurence Baker, Ph.D., Christopher Afendulis, Ph.D., Amitabh Chandra, Ph.D., Elena Fuentes-Afflick, M.D., Shannon McConnville, MA, Ciaran Phibbs, Ph.D. Presented By: Laurence Baker, Ph.D., Associate Professor, Health Research and Policy, Stanford University School of Medicine, HRP Redwood Building, Room 110, Stanford, CA 94305-5405; Tel: (650)723-4098; Fax: (650)725-6951; Email: laurence.baker@stanford.edu Research Objective: Among low birthweight newborns, Black newborns have better survival than White newborns for a given birthweight. This birthweight-specific survival advantage has never been fully explained. One previously unexplored possibility is differential access to high-level neonatal intensive care units (NICUs), which have been shown to contribute to improved outcomes. This paper compares the use of NICUs by race/ethnicity and examines relationships between access to NICUs and differences in birthweight-specific mortality. Study Design: The first part of the study consists of crosssectional and longitudinal comparisons of access to NICUs among Asian, Black, Hispanic and White newborns. We use data linking birth certificates, death certificates, and hospital discharge records for newborns and mothers. We calculate the distance from residence zip code to the nearest hospitals with high-level and lower-level NICUs, and compare distances across race/ethnicity groups and over time. We use multinomial logistic models to examine the probability of being born in hospitals with different NICU levels. The independent variables in these models were race/ethnicity, maternal and newborn demographics, and maternal and neonatal risk factors. In the second part of the study, we use the same data to model infant mortality. We estimate logistic regression models of 28-day mortality, as a function of race/ethnicity, controlling for a range of risk factors including birthweight, maternal characteristics, and a detailed set of controls for health status. We investigate the impact of controlling for use of a NICU on the estimated variations in mortality rates by race and ethnicity. Population Studied: All births in California between 1990 and 2000 in work to date. We expect to add data from Wisconsin, Missouri, and New Jersey in the near future. Principal Findings: Black newborns are more likely to live close to, and be born in, hospitals with large tertiary NICUs than White infants. 43% of Black newborns under 2500g are born in high level NICUs, compared with 31% of Whites. However, despite evidence from other studies that higher NICU use rates reduce mortality for high-risk newborns, the higher rate of use of high-level NICUs by Black newborns explains only a small portion of the observed Black-White birthweight-specific mortality difference. We found only small variations in use of NICUs among Asian, Hispanic and White newborns. Conclusions: There are large racial/ethnic disparities in use of NICUs. Opposite much of the disparities literature, in which Blacks are less likely to have access to advanced therapies, Black infants were more likely to be born in hospitals with high level NICUs than White infants. Differential access to technology does not, however, explain the favorable outcomes among Black infants. Implications for Policy, Delivery, or Practice: Differential access to technologies is an important policy consideration, but can be complex. Findings from some settings that Black patients receive less intensive care do not extrapolate uniformly to all settings. Assuming that differential technology use will necessarily drive outcome differences may also be unwarranted. Primary Funding Source: National Institute on Child Health and Development ●Disparities in Perinatal and Infant Health Among Rural AI/ANs and Rural Whites: Is the Gap Narrowing? Laura-Mae Baldwin, M.D., MPH, Eric Larson, Ph.D., Elise Murowchick, Ph.D., Holly Andrilla, M.S., L. Gary Hart, Ph.D. Presented By: Laura-Mae Baldwin, M.D., MPH, Professor, Family Medicine, University of Washington School of Medicine, Box 354982, Seattle, WA 98195; Tel: (206) 685-4799; Fax: (206) 616-4768; Email: lmb@u.washington.edu Research Objective: To examine whether disparities in perinatal care and birth outcomes among rural American Indians/Alaska Natives (AI/ANs) and rural whites have decreased during the decade and a half of national and statelevel policy change to improve access to prenatal and infant care. Study Design: Cross-sectional study using the National Linked Birth-Death Database to compare prenatal care receipt, low birthweight rates, neonatal and postneonatal death rates, and causes of death among rural AI/ANs and whites in three time periods: 1985-1987, 1989-1991, 1995-1997. Multivariate logistic regression examined whether the AI/AN-white differences diminished over the three time periods. Population Studied: 217,064 AI/AN and 5,032,533 white, nonHispanic singleton births to women living in rural U.S. counties in the three time periods. Principal Findings: Prenatal care use increased substantially and comparably for both AI/ANs and whites over the three time periods, with the greatest improvement between 19891991 and 1995-1997 (AI/AN rates of inadequate care 33.9% in 1989-91, 26.3% in 1995-97; whites 13.5% in 1989-91, 10.0% in 1995-97). The adjusted 2.5 times greater risk of receiving an inadequate pattern of prenatal care among AI/ANs compared to whites did not diminish over time. Postneonatal death rates of AI/ANs were higher than whites in each of the time periods, although the adjusted odds decreased from 1.76 in 1985-1987 to 1.60 in 1995-1997. The most common causes of postneonatal death for rural AI/ANs and whites were SIDS, congenital anomalies, infectious disease, and unintentional injuries and accidents, with AI/ANs having significantly higher rates of SIDS, infections, and injuries/accidents throughout the study period. In 1995-1997, there were over three times as many infectious disease-related postneonatal deaths among rural AI/ANs compared to whites (54 AI/AN deaths, but only 16 white deaths in a same sized population). Conclusions: Significant improvements in access to prenatal care and postneonatal death rates among both rural AI/ANs and whites between the mid-1980s and late-1990s are encouraging. There were minimal gains in closing the gaps between AI/ANs and whites in these measures, however. Three of the four most common causes of postneonatal death include preventable components. Implications for Policy, Delivery, or Practice: The fact that perinatal outcomes of both AI/ANs and whites improved during a time of expanding Medicaid eligibility and enrollment, increased provision of support services and case management, and efforts such as the Back to Sleep campaign suggests that these types of programs can be successfully applied in diverse populations. Changes over the past two decades in the organization of AI/AN health services, with increased tribal autonomy, provide excellent opportunities for culturally appropriate interventions to further improve perinatal outcomes. Persistent disparity in the per capita annual health care funds available to the Indian Health Service compared to that spent on the average U.S. citizen threatens these opportunities, however. Redoubled efforts and adequate funding are needed to ensure that populations with higher rates of adverse perinatal outcomes, such as AI/ANs, continue to experience improvements. Without these efforts and funding, it will be difficult for AI/ANs to meet the Healthy People 2010 objectives, in which AI/ANs and whites are expected to reach the same goals. Primary Funding Source: No Funding Source ●Physician and Patient Characteristics in Outpatient Breast Cancer Screening Rajesh Balkrishnan, Ph.D., Stephen V. Samuel, M.D. Presented By: Rajesh Balkrishnan, Ph.D., Merrell Dow Professor, College of Pharmacy and School of Public Health, 500 West 12th Avenue, Columbus, OH 43201; Tel: (614)2926415; Fax: (614)292-1335; Email: rbgws@sbcglobal.net Research Objective: Breast cancer is the most common cancer among women and is the second leading cause of cancer death in the United States. However, death rates from breast cancer have been declining in recent years and these decreases are believed to be the result of earlier detection and improved treatment. Earlier detection of breast cancer is primarily achieved through screening methods. Typically, screening for breast cancer consists of breast self examination (BSE), clinical breast exam (CBE), and mammography. The main objective of this study was to examine the factors that are associated with physician recommendations for breast cancer screening in United States outpatient settings. Study Design: Analysis of cross sectional nationally representative survey. Population Studied: Data from the National Ambulatory Medical Care Survey (NAMCS) database, a national probability sample administered by the Division of Health Care Statistics, National Center for Health Statistics (NCHS), Center for Disease Control and Prevention (CDC) were used. This study sample consisted of 2.04 billion female patients aged 18 and older who visited physicians based in outpatient settings in the US from 1996 to 2001. Multiple logistic regression analyses were used to examine predictors of breast self exam, mammography, and clinical breast exams in outpatient settings during the 6 year time period. Principal Findings: Women who paid for their office visit with public insurance (Medicare/Medicaid), or other insurance, or had no insurance were less likely to be offered breast self exam counseling, clinical breast exam, or mammography than women who had private insurance. In addition, primary care physicians (family practice, general practice, and internal medicine only) were less likely to offer breast self exam counseling and less likely to perform a clinical breast exam than their non-primary care counterparts. Furthermore, women who were 65 years or older were significantly less likely to receive the three screening methods when compared to women between the ages of 35-49. Conclusions: The findings of the study reveal several factors that play a role in the physician recommendation of breast cancer screening. These findings also indicate that there are certain disparities regarding the recommendation of breast cancer screening and further research needs to be conducted to determine the best methods to bridge these gaps in patient care. Implications for Policy, Delivery, or Practice: These findings contribute to the existing information about breast cancer screening and highlight the physician and patient factors that affect breast cancer screening in outpatient settings in the United States. Policies designed to target factors associated with higher risk of non-screening in primary care settings may eventually lead to earlier detection and treatment of breast cancer resulting in decreased mortality from breast cancer. Primary Funding Source: No Funding Source ●Health Literacy and Metabolic Syndrome Risks: A Pilot Study with Deaf Adults who Communicate with American Sign Language Steven Barnett, M.D., Robert Pollard, Ph.D. Presented By: Steven Barnett, M.D., Assistant Professor, Department of Family Medicine, University of Rochester, 1381 South Ave, Rochester, NY 14620; Tel: (585)506-9484 x110; Fax: (585)473-2245; Email: steven_barnett@urmc.rochester.edu Research Objective: To examine the health-related knowledge and risk factors of deaf adults who communicate with American Sign Language. Study Design: We worked with a convenience sample of deaf adults attending a social activity in Rochester NY. ASL-fluent researchers (hearing and deaf) reviewed the research project with potential participants and obtained consent. Each adult completed a single page low English literacy questionnaire; ASL-fluent researchers answered any questions. The questionnaire asked demographic and health information. Participants also completed a modified REALM, which asked them to circle words they recognized and understood. After participants completed the survey we measured blood pressure, height, weight and waist circumference. Population Studied: Deaf people who communicate in American Sign Language (ASL) comprise an understudied and medically underserved language minority community. Deaf people who communicate in ASL experience health disparities, including poorer health and less access to health information and healthcare services than those in the general population. The low literacy of many adults deaf since childhood contributes to disparities. Limited access to health information and healthcare services may put deaf adults at risk for health problems related to lifestyle choices such as diet and physical activity. There is little research on health and deaf people who communicate in ASL. Health literacy measures such as the REALM use pronunciation to assess health literacy. It is unlikely that adults deaf since childhood have heard these words pronounced. Principal Findings: Sixty-one deaf adults participated, 30 (49%) were women. Fifty-one knew they became deaf before age 3 years and 47 (77%) reported ASL as their one best language. The median age was 46 (range 21-89; SD=13). Forty-eight (79%) graduated college (associate degree or higher) but 38 (69%) scored in the highest REALM category (high school reading level). Only 39 (64%) rated their health as “good.” Seven (13%) were current smokers. Twenty-six (43%) thought they were “too heavy.” Seventeen (28%) were obese with a body mass index (BMI) > 30 and another 26 (43%) were overweight (BMI 25-29.9). Seventeen women (57%) and 11 men (38%) had abdominal obesity by waist circumference. Thirteen participants (21%) thought their blood pressure was “too high,” 12 (20%) knew they took medicine for blood pressure, while 25 (46%) participants’ blood pressure was elevated (systolic > 124 or diastolic > 84). The presentation will include other data as well as national general population data for comparison. Conclusions: We should learn more about health literacy, health knowledge, health and risk behaviors of deaf people who communicate in ASL. This is essential in order to promote health and prevent disease in deaf people and their family members. In order to do this we need to adapt and evaluate existing research tools for use in ASL. Implications for Policy, Delivery, or Practice: Many adults deaf since childhood became deaf in utero during the rubella pandemic of the early 1960s and they, like other adults their age, will have increasing age-appropriate preventive services needs. One of the goals of Healthy People 2010 is to improve health and access to health research for people with disabilities. Primary Funding Source: CDC ●Relationship Between Local Unemployment Rate and Hospital-Level Outcome Raj Behal, M.D., MPH, Sarah Kinsella Presented By: Raj Behal, M.D., MPH, Medical Director, Clinical Effectiveness & System Redesign, University HealthSystem Consortium, 2001 Spring Road Suite 700, Oak Brook, IL 60523; Tel: (630)954-4892; Email: rbehal@uhc.edu Research Objective: To assess whether the proportion of hospital admissions that are length of stay outliers is affected by the socioeconomic status of local population. Study Design: A binary logistic regression model was developed to determine the independent effect of population characteristics on the proportion of LOS outliers after controlling for case mix. Variables obtained from 2000 census data included proportion of local population that was Black, Hispanic, over age 65, under age 18, with Bachelor's degree, foreign born, below poverty level; median household income; hospital-level variables included annual case volume, % patients dying within 2 days of admission, and mean predicted LOS (using RDRG grouper to assign severity of illness to each patient). Population Studied: Discharges from 59 hospitals in the state of Massachusetts in year 2000 were included in the study. Principal Findings: Local unemployment rate was an independent predictor of proportion of cases that were LOS outliers (c-index 0.764, Hosmer Lemeshow p value = 0.97). Conclusions: After adjusting for various social and demographic characteristics of the local population, and case mix for each hospital, unemployment rate appears to be positively correlated with hospital-level outcome of LOS outliers. Implications for Policy, Delivery, or Practice: Further research is required to fully elucidate the effect of prevalent unemployment rate in the community on disparities in hospital-level outcomes. Primary Funding Source: No Funding Source ●Should We Continue to Blame Obesity on Urban Sprawl? Stephanie Bernell, Ph.D., Andrew Plantinga, Ph.D. Presented By: Stephanie Bernell, Ph.D., Assistant Professor, Public Heatlh, Oregon State University, 319 Waldo Hall, Corvallis, OR 97331-6406; Tel: (541)737-9162; Fax: (541)7374001; Email: Stephanie.Bernell@oregonstate.edu Research Objective: Recent studies emphasize the connection between obesity and development patterns associated with urban sprawl. Empirical analyses have found higher obesity rates among residents of sprawling areas. Some researchers have proposed changes in urban design to reduce obesity and other health problems linked to physical inactivity. An important assumption implicit to this line of reasoning is that urban form is exogenous to an individual’s weight. In particular, it is assumed that when urban development patterns produce low levels of physical activity, individuals have a greater tendency to become obese. In this study, we consider the possibility that weight affects an individual’s choice of the type of neighborhood to reside in. Specifically, we test the hypothesis that an individual’s weight and the urban form of the area where they live are determined simultaneously. If true, the assumption that urban form is exogenous to weight is incorrect. This would imply that earlier empirical results are invalidated by simultaneity bias and challenges the idea that obesity can be addressed through urban design modifications. Study Design: Our econometric model is a two-equation system with BMI and a latent variable determining residence in a high or low sprawl county as endogenous variables. The exogenous variables are the other individual attributes and the region of residence. Parameter estimates are derived using a simultaneous equations probit estimator. Population Studied: Our main data source is the National Longitudinal Survey of Youth 1979 (NLSY79), which tracks a nationally representative sample of individuals who were ages 14 to 22 years in 1979. We use data from the NLSY79 for the year 2000 to measure body mass index (BMI), other individual attributes (race, gender, smoking and marital status, income, number of children, age, educational attainment), and county and region of residence in 2000. An individual is considered obese if their BMI exceeds 30. We categorize counties as having a high or low degree of sprawl. Our final sample includes 3,867 respondents to the NLSY79 who reside in counties for which the sprawl index was measured and for whom we have complete observations of the individual attributes. Principal Findings: Consistent with earlier studies, individuals with higher probability of living in high sprawl counties are found to have greater BMI. However, we also find that greater BMI increases the probability that individuals live in high sprawl counties. Conclusions: Uur results suggest that causality between weight and urban form runs in both directions. That is, we find evidence for the simultaneity of BMI and urban form, implying that parameter estimates in earlier studies are biased. Implications for Policy, Delivery, or Practice: Our finding that higher BMI increases the probability of residence in a high sprawl county raises doubts about whether obesity can be reduced through modifications of urban form . Building compact, walkable communities may simply attract individuals who are already physically active. Alternatively, modifying existing communities to promote exercise—for example, by building parks and installing sidewalks—may have little effect if current residents are predisposed to physical inactivity. Primary Funding Source: No Funding Source ●Why are Some Individuals Food Insecure?: The Role of County Level Factors Stephanie Bernell, Ph.D., Bruce Weber, Ph.D., Mark Edwards, Ph.D. Presented By: Stephanie Bernell, Ph.D., Assistant Professor, Public Health, Oregon State University, 319 Waldo Hall, Corvallis, OR 97331-6406; Tel: (541)737-9162; Fax: (541)7378001; Email: Stephanie.Bernell@oregonstate.edu Research Objective: This study attempts to untangle the multiple sources of food insecurity by examining the roles of household demographics, local economic and social conditions and federal food security programs in explaining the likelihood of household food insecurity in Oregon, the state with the highest hunger rate in the nation in four of the last five assessments. We believe this is the first study that has examined the role of local (county-level) contextual factors in explaining food insecurity. Study Design: We use a multivariate logit model to estimate the probability of household food insecurity. Maximum likelihood coefficients and marginal effects are presented. In addition, based on the multivariate model results, we calculate and present predicted probabilities of food insecurity for composite individuals living in different settings. Population Studied: In this study, food insecurity is modeled as a function of personal characteristics and county-level contextual variables. The analyses are based on the 2000 Oregon Population Survey data, supplemented by data from the 2000 Census and other sources identified in Table 2. The Oregon Population Survey contains information on food insecurity and on personal and household characteristics of Oregon residents. The supplemental data contains county specific information on wages, unemployment, program use, and community affiliations and participation. Principal Findings: Controlling for individual and household demographics, local economic conditions (local wages and unemployment) have a significant effect on the likelihood that a given household will be food insecure. Also, whether one lives in a rural or urban environment matters greatly. Moving from a completely urban environment to a completely rural environment reduces the probability of food insecurity by about 5 percentage points, holding all else constant. The county food stamp level is also significant determinant of food insecurity. The empirical analysis does not suggest that high county-level rent is associated with a significantly higher probability of food insecurity. Evidence does suggest, however, that very low-income households located in high-rent counties have an increased probability of food insecurity. Conclusions: Our results suggest food insecurity is much more than a problem with individual choices. It is the case that that the local community food security infrastructure (food stamp outreach, wages and employment opportunities and housing costs) significantly affects the likelihood that families will be food insecure. Implications for Policy, Delivery, or Practice: Local actions that strengthen this infrastructure may be expected to have stronger effects in states like Oregon where the influence of contextual factors is relatively strong. Primary Funding Source: No Funding Source ●Identifying New Target Areas for Reducing Racial/Ethnic and Gender Disparities in Health Care for the Medicare Population Sarita Bhalotra, M.D., Ph.D., Mathilda Ruwe, M.D., MPH, John Capitman, Ph.D., Elise Desjardins, MBA Presented By: Sarita Bhalotra, M.D., Ph.D., Assistant Professor, Heller School, Brandeis University, 415 South Street, Waltham, MA 02454; Tel: (781)736-3960; Email: bhalotra@brandeis.edu Research Objective: To provide a framework for integrating health disparity perspectives with current clinical care and public health practice, we reviewed the evidence for racial/ethnic and gender disparities in access, prevention and treatment for five health conditions: depression, colorectal cancer, stroke, coronary heart disease and major joint replacement. We determined availability of evidence-based treatment and existence of interventions to reduce racial/ethnic or gender disparities. Study Design: We conducted a thorough search from multiple scholarly sources; eligible reports were: studies involving the target populations; published between 19992003, involving population aged 65 years and over; addressing target health condition in the target populations, or access to preventive care or treatment, and possible interventions to reduce disparities in colon or rectal cancer preventive services; studies meeting minimal methodology standards; a stepwise methodology that eliminated reports systematically yielded a total of 327 qualified studies. Population Studied: Elders 65 years and over who were: Asian-Americans, African-American or Hispanic/Latina, American-Indians, Pacific Islanders, Rural residents, Disabled, Low Income or Dual Eligible Principal Findings: We found racial/ethnic and gender differences in access, prevention and treatment for all five conditions. Racial/ethnic disparities for depression were for both receiving a diagnosis and treatment. Although the data on gender differences in access to invasive cardiac procedures was somewhat inconsistent the weight of the evidence showed that women and racial/ethnic minorities tend to underuse and have access to these procedures at a later stage, while white males tend to overuse the procedures. Gender disparities also resulted from differences in clinical presentation. Although colorectal cancer is a largely preventable disease, racial/ethnic minorities are less likely to be screened. Racial/ethnic minority elders were less likely to be offered and to participate in primary preventive activities for stroke, such as weight loss/diet improvements, smoking cessation, and physical activity. Females and African American elders were less likely to receive carotid endartectomy (CEA). There are racial/ethnic differences in rates of joint replacement despite small differences in osteoarthritis and musculoskeletal conditions. Women tend to undergo joint replacement surgeries more frequently, experience more disability at the time of total hip arthroplasty, and do not perform as well after one year as compared to men. We found no evidence of interventions to reduce gender and racial/ethnic disparities in access or treatment of these conditions. There were not enough studies rural/urban, dual eligible to allow conclusions on disparities. Conclusions: Women and racial/ethnic minority elders can benefit from interventions to reduce underuse of available primary and secondary preventative services for colorectal cancer, stroke, and depression and coronary heart disease. However, national guidelines and interventions for reducing disparities are currently not available for these conditions. More studies on rural/urban and dual eligible differentials are required. Implications for Policy, Delivery, or Practice: Race/ethnicity and gender encompass social and contextual variables that are associated with lifetime exposure to behavioral and contextual/genetic risks that can influence health outcome disparities. Current health care system attributes also influence health disparities. Health outcome disparities can arise in each phase of prevention and treatment. If Healthy People 2010 disparity goals are to be achieved, interventions must be multifaceted and address the complex causation of disparities Primary Funding Source: CMS ●Trends in Geographic Disparities in the Context of Technology Adoption and Diffusion. Mythreyi Bhargavan, Ph.D., Jonathan Sunshine, Ph.D. Presented By: Mythreyi Bhargavan, Ph.D., Director of Research, American College of Radiology, 1891 Preston White Drive, Reston, VA 20191; Tel: (703)715-4394; Fax: (703)2642443; Email: mythreyib@acr.org Research Objective: To measure disparities in the utilization of diagnostic imaging across states, to examine how these disparities vary across imaging modalities (such as X-ray, CT, MR) – specifically whether the disparities are greater among new technologies -- and to examine whether these gaps narrow over time. Further, we measure if state demographic characteristics and physician supply affect the adoption and rate of spread of technologies. Study Design: We use Medicare summarized physician claims data (Part B claims for non managed care enrollees) for 1997-2003. We group the diagnostic imaging claims by imaging modality (X-ray, ultrasound, CT, MRI, etc.), and by state. We obtain state level statistics (from a variety of sources), i.e., counts of radiologists, population, Medicare enrollees, average income and per capita health spending by state etc. We use the coefficient of variation for a simple comparison of variability across states by modality and observe trends over time. To measure the effect of the adoption of new technology, we examine if this variability across states is significantly different for newer technologies (CT, MRI) than it is for older technologies (X-ray), and we measure if these differences persist when we control for state demographics and state physician supply. To measure the effect of the diffusion of technology, we test if the variation in per capita utilization of each imaging modality decreases over time, overall and with controls for state characteristics that affect demand for imaging state physician supply. Population Studied: We study Medicare Part B fee-for-service enrollees during the period 1997-2003. Principal Findings: Preliminary estimates show that for all the years examined, the coefficient of variation was higher for MR and CT than for mammography and general radiology. In virtually all modalities, the coefficient of variation decreased during the period 1995-2001. We expect to find similar trends for the period 1997-2003. Conclusions: Small area variation needs to be viewed in the light of the technology diffusion and adoption literature. Though small area variation has been studied for over 30 years, this important perspective has been missing. Implications for Policy, Delivery, or Practice: Very widespread geographic variation in the use of many individual health care services and in the total volume of services has been extensively documented for over 30 years, beginning with pioneering studies by Wennberg. However, there has been relatively little explanation of the variation, and attempts to explain the variation have not focused upon technology adoption and diffusion, although that is relevant to a fast changing field like health care. Past studies specifically of the utilization of diagnostic imaging showed wide variation in per capita imaging use across states, particularly for new imaging modalities. Because technology change is particularly prominent in imaging, a study of imaging is especially promising for investigating the role of technology adaptation and diffusion in geographic variation. Primary Funding Source: No Funding Source ●The Relationship of Acculturation to Disparities in Perceived Health Between Latinos and non-Latino Whites Jeanne Black, MBA, Ninez Ponce, Ph.D. Presented By: Jeanne Black, MBA, Doctoral Candidate, Health Services, UCLA, 4396 Keystone Avenue, Culver City, CA 90232; Tel: (310)836-8876; Email: jtblack@ucla.edu Research Objective: Self-reported health status is widely used as an indicator of population health, based on the question, “In general, would you say your health is excellent, very good, good, fair, or poor?” Using this measure, Latinos report significantly worse health than non-Latino Whites. The objective of this study is to examine whether acculturationrelated factors explain this disparity in addition to the previously demonstrated effect of socioeconomic status (SES). Study Design: This cross-sectional study used data from the random-digit-dial California Health Interview Survey 2001. We used weighted logistic regression to examine the impact of health conditions, SES, and acculturation on the odds of reporting fair or poor health. Acculturation-related factors were English proficiency (LEP), language(s) spoken at home, years in the US, citizenship status, and immigrant generation. Regression coefficients were compared using the Wald test. Population Studied: 10,942 Latino and 25,679 non-Latino White non-elderly adults residing in California. Principal Findings: Latinos had 4 times the odds of perceiving their health to be fair or poor, adjusting for age and gender (p<0.0001). These odds remained unchanged when BMI and chronic conditions were added to the regression model, although being obese, or having been diagnosed with asthma, arthritis, diabetes, hypertension, heart disease, or cancer each had an odds ratio of at least 2.0 (p<0.0001 for all). Adding acculturation-related variables reduced the odds from 4.1 to 1.98. Increased odds were associated with LEP (OR=3.7, p<0.0001); not speaking English at home (OR=1.3, p<0.0001); and not being a US citizen (OR=1.3, p=0.012). The odds also increased with length of residence. Speaking Spanish and English at home, being a naturalized citizen, and immigrant generation were not significant. When education and poverty status were added to the model, the SES variables had a greater effect than acculturation (F=60.1 vs. F= 7.25), and the OR for Latinos was reduced further to 1.4. The only acculturation-related variable to remain significant was LEP; its associated odds decreased from 3.7 to 2.0 (p<0.0001). Conclusions: Some factors associated with lower levels of US acculturation appear to increase Latinos’ odds of reporting fair/poor health status. However, acculturation level also is associated with SES factors such as income and education. The only acculturation-related factor to remain robust when SES was added to the model is LEP. Despite the significant contributions of health conditions and SES to perceived health, there remains considerable disparity between Latinos and non-Latino whites. This finding and the robustness of LEP may indicate that self-reported health is a culturally-mediated perception. Alternatively, since other acculturation-related variables had diminished effects when SES variables were added, the LEP effect may signal language barriers: Latinos with LEP may have unreported chronic conditions because they lack language access to the medical care that would diagnose these conditions. Implications for Policy, Delivery, or Practice: English language proficiency explains a significant portion of the difference in perceived health between Latinos and non-Latino Whites, independent of socioeconomic status. Therefore, efforts to reduce this disparity should focus not only on health insurance coverage and tax credits, but should also address language access in health care. Primary Funding Source: No Funding Source ●A Method to Improve Medicare Coding of Race and Ethnicity: Implications for Health Disparities among Medicare Beneficiaries Arthur Bonito, Ph.D., Celia Eicheldinger, MS, Linda Greenberg, Ph.D., Arthur Meltzer, Ph.D. Presented By: Arthur Bonito, Ph.D., Program on Health Care Org, Del, and Access, RTI International, Box 12194, Research Triangle Park, NC 27709; Tel: (919) 541-6377; Fax: (919) 9908454; Email: AJB@RTI.ORG Research Objective: Historically, analyses of racial and ethnic groups generally have been limited to comparisons of White, Black, and All Other Medicare beneficiaries combined. The objective of this study was to assess the validity and accuracy of race and ethnicity coding on the Medicare Enrollment Data Base, or EDB, and develop a method to improve coding of Hispanics and Asians or Pacific Islanders so these groups may be more validly represented in analyses identifying health disparities. Study Design: We pooled existing random samples of Medicare fee-for-service and managed care beneficiaries who responded to three annual CAHPS Medicare Satisfaction Surveys for 2000 through 2002. The pooled sample consisted of 830,728 unique beneficiaries who self-reported their race and ethnicity. These self-reports constituted the gold standard measure against which we assessed the existing EDB race and ethnicity coding as well as our own effort to improve EDB coding. Our approach to improve EDB coding was based in part on algorithms we developed using US Census lists indicating how frequently specific surnames belonged to persons identifying themselves as Hispanic or Asian or Pacific Islander. Population Studied: Medicare beneficiaries enrolled in traditional fee-for-service or managed care plans with particular focus on Hispanics and Asians or Pacific Islanders. Principal Findings: We developed an algorithm employing surname, geographic location, common first names, and information on the EDB that dramatically improved upon existing EDB race and ethnicity coding. Sensitivity increased from 29.5 to 76.6 percent for Hispanics and from 54.7 to 79.2 percent for Asians and Pacific Islanders, with no loss of specificity. Kappa coefficients reached 0.80. The impacts of improved race and ethnic coding on health service utilization differed by condition, type of service, and whether estimating a count, a rate, or an average. We illustrate the impact of the improved race and ethnicity coding on identification of diabetics and the use of diabetes related services. Conclusions: Our study dramatically improved the validity of Medicare race and ethnicity coding for Hispanics and Asians or Pacific Islanders, increasing the number of Hispanics by 300 percent and of Asians or Pacific islanders by more than 30 percent. This improvement results in an enhancement of the analytic capability and policy potential of Medicare administrative data to provide more valid estimates of potential disparities involving racial and ethnic minorities’ use of and access to health services. Implications for Policy, Delivery, or Practice: This study developed an algorithm to recode the Medicare EDB race and ethnicity variable that more accurately identified Hispanic and Asian or Pacific Islander beneficiaries. Our results have important implications for research on health disparities among the Medicare beneficiaries and increasing our knowledge of service use by minority groups. Our recoded race and ethnicity variable can be substituted for the existing EDB variable to allow more valid assessment of potential health disparities among Hispanics and Asians or Pacific Islanders. Primary Funding Source: CMS ●A Sign of Our Times: Creating Effective Multilingual Signage in a Children's Hospital by Integrating Input from Hospital Staff, Administrators, and Families Jane Brotanek, M.D., MPH, Glenn Flores, M.D., Suzanne Strugalla Presented By: Jane Brotanek, M.D., MPH, Assistant Professor, Community Pediatrics, Medical College of Wisconsin, 8701Watertown Plank Road, MS 756, Milwaukee, WI 53226; Tel: (414) 456-5778; Fax: (414) 456-6385; Email: jbrotane@mail.mcw.edu Research Objective: 4 million US children are limited in English proficiency (LEP), but research has not examined barriers posed to LEP patients and their families by monolingual English hospital signs, nor informed processes for creating multilingual signage in a children's hospital. The study objective was to determine the barriers and priorities in developing multilingual hospital signage as identified by key hospital personnel, administrative staff, and parents. Study Design: The Children's Hospital of Wisconsin recently approved conversion of English signage to multilingual signage for the 2 major non-English language groups, Spanish and Hmong. The Interpreter Services Advisory Committee (ISAC) met to discuss barriers and priorities in implementing multilingual signage. The ISAC is a group of 13 hospital staff, including the Director of Public Relations, an outreach specialist, a clinical learning specialist, and 2 pediatricians. The ISAC, together with Latino and Hmong families, conducted several hospital walk-throughs to evaluate current signage and priorities for multilingual signs. Participant observation techniques were used to record themes noted in the discussions and walk-throughs, and a summary of themes was compiled using grounded theory. Population Studied: Key hospital and administrative staff of the Children's Hospital of Wisconsin, along with Latino and Hmong families Principal Findings: The ISAC and families initially considered comprehensively translating all hospital signs. Consensus was reached on prioritizing multilingual sign placement in hightraffic areas using a comprehensive approach spanning from the parking garage to multiple end destinations, with maps provided in different languages. The group agreed that the most efficient use of resources would be to post separate signs in Hmong and Spanish next to/below existing signs, rather than changing current signs. The importance of responding to future needs also was raised, including consideration of electronic systems, computer kiosks, removable signs, and consultation with signage experts from other industries. Conclusions: Children's Hospital staff, administrators, and families identified the following priorities in creating multilingual signage in a children's hospital: multilingual sign placement in high-traffic areas using a comprehensive approach; multilingual maps on each hospital floor; separate signs in Hmong and Spanish alongside/below existing signs; and the importance of creating signage systems responsive to future changes and needs. Implications for Policy, Delivery, or Practice: This comprehensive approach integrating the perspectives of key stakeholders could serve as a model for other children's hospitals considering implementing a multilingual signage system. Primary Funding Source: Medical College of Wisconsin, Department of Pediatrics ●Urban African American Men with HIV/AIDS: Exploring Association of Stigmatization, Health Systems Barriers with Overall Life Functioning and Life Satisfaction Dr. Aaron Buseh, Ph.D., MPH, MSN, Kelber, S., MSc, Stevens, PE, Ph.D., RN, FAAN, Park, C. Gi., Ph.D. Presented By: Dr. Aaron Buseh, Ph.D., MPH, MSN, Assistant Professor, College of Nursing, University of WisconsinMilwaukee, 1921 East Hartford Avenue, Room 569, Milwaukee, WI 53211; Tel: (414) 229-5462; Fax: (414) 229-5504; Email: aaronbg@uwm.edu Research Objective: In 2000, the death rate for black males attributed to AIDS was 5 times that of white men. African American men whose lives are extended with antiretroviral therapies face an array of challenges: lack of finances, lack of access to medical care, and social stigma due to HIV/AIDS. In order to develop effective intervention programs for black males living with HIV, it is essential to identify the factors associated with the overall functioning and quality of life of this population. The purpose of this study was to examine the association and relationships between socio-demographic variables, stigmatization, health systems barriers, and life satisfaction and overall functioning as self-reported reported among an urban sample of HIV infected black males. Study Design: Cross-sectional descriptive survey design was used to examine selected socio-demographic variables, their association and influence on the quality of life among a sample of urban African American males. Data were analyzed using descriptive statistics, followed by correlations and hierarchical multiple regressions statistics. Population Studied: Participants included a convenience sample of black males (18 years or older) who self-reported as having been diagnosed with HIV infection (n = 55) and were recruited through a local African American community-based organization in a Midwest metropolitan area. A survey questionnaire pertaining to socio-demographic indicators, subjective health status, stigmatization, health systems barriers, provider engagement and trust, life satisfaction and overall functioning were combined into one survey instrument and was administered to the participants. Principal Findings: Barriers to health care was inversely associated with the participants’ perception of their health; the poorer the health of the participants the greater their perception of the degree of barriers to obtaining health care. Provider trust was positively associated with education; the higher the level of education, the higher the level of trust in the provider. All of the variables measuring stigma and health system barriers were inversely associated with quality of life; as barriers to health care and perceived stigma increased, quality of life decreased. Stigmatization and health systems barriers were associated. After adjusting for the demographic variables of age, income, education, length of diagnosis, sexual orientation, and health status, the factors significantly impacting quality of life in our model were: personalized stigma and barriers to health care- accounting for 55% of the variance in quality of life. Also, after adjusting for length of diagnosis, age, income and clinical status, the factors of engagement with health provider and barriers to health care accounted for 39% of variance in overall functioning. Conclusions: African Americans are disproportionately represented among existing and new cases of HIV infection. The importance of factors examined in this study cannot be understated. Understanding the experiences of African American males living with HIV/AIDS will assist health care professionals in working with this population in maximizing the management of their disease and improving overall quality of life. Implications for Policy, Delivery, or Practice: Assessing social stigma and health systems barriers in relation to overall functioning and health-related quality of life among African American males has important implications in developing programs that will enable this population to live well. The levels of social stigmatization and health system barriers can be modified and are important influences on adaptation processes that may enhance overall quality of life of urban African American men living with HIV/AIDS. Primary Funding Source: Sigma Theta Tau International Honor Society of Nursing, Eta Nu Chapter ●Ethnicity and Employer-Sponsored Insurance as Predictive Factors of Uninsurance Among Hispanics in Nebraska Erin Carlson, MPH, Jane Meza, Ph.D., Katherine Jones, Ph.D., PT Presented By: Erin Carlson, MPH, Health Data Analyst, Preventive and Societal Medicine, University of Nebraska Medical Center, 984350 Nebraska Medical Center, Omaha, NE 68198-4350; Tel: (402) 559-8406; Fax: (402) 559-7259; Email: ekcarlso@unmc.edu Research Objective: To provide information to policymakers for expanding coverage to Nebraska’s growing Hispanic population by determining whether Nebraska’s Hispanics are less likely to have employer-sponsored insurance (ESI) than are other racial/ethnic groups in Nebraska and to identify whether a correlation exists between Hispanic ethnicity, ESI, and uninsurance in Nebraska. Study Design: The 2004 Nebraska State Planning Grant (NSPG) random-digit dialed telephone survey identified characteristics of Nebraska’s uninsured and sources of coverage for the insured. A translated survey was administered to Spanish-speaking respondents. Descriptive and bivariate analyses described differences between Hispanics and non-Hispanics in employment status and predictive factors of uninsurance; multivariate regression analysis detected association between uninsurance, ethnicity, and ESI. Four of 13 NSPG focus groups also provided data. Key contacts recruited participants for all groups and comoderated the Hispanic groups in Spanish. Group proceedings were audio-recorded and transcribed for coding and analysis. Population Studied: The telephone survey interviewed 3750 adults under age 64 across the state. Hispanics were over- sampled. The 448 surveys of Hispanics were compared to non-Hispanics. Most of the two Hispanic groups’ 27 participants were uninsured and employed. The two employer groups included 12 participants with one group conducted in a rural community and the other in an urban community. Principal Findings: Hispanics were more likely than nonHispanics to be employed and to have ESI available. Ten percent fewer Hispanics than non-Hispanics were enrolled in available ESI. Only .2% of Hispanics whose employer offered health insurance said they were not enrolled because they “did not need/want” health insurance. The most common reason (23%) given for why Hispanics were not enrolled in ESI was “don’t know.” Hispanics (21.7%) and non-Hispanics (20.0%) responded similarly that they did not enroll in ESI because contributions were “too expensive.” When controlling for age, marital status, and poverty level, ethnicity was not found to be a significant predictor of ESI (p=.275). Uninsurance was more strongly associated with poverty status (p=.001) than ethnicity or ESI. Hispanics whose jobs did not offer ESI were more likely to be uninsured than were those with ESI available (OR=1.11). Hispanic focus group participants valued health insurance but said they could not afford the employee contributions. Both groups offered they would pay 10% of their paycheck for family coverage. Many participants believed ESI was their only insurance option, but said it was difficult to obtain and use primarily due to lack of information and cost, in addition to other factors. Employer participants indicated that ESI was not a factor in recruiting and retaining Hispanic employees because Hispanic workers preferred money over benefits and thus seemed to not value ESI. Conclusions: Uninsurance among Nebraska’s Hispanics is due to poverty rather than ethnicity or availability of ESI. Implications for Policy, Delivery, or Practice: Policies to mitigate uninsurance among Nebraska’s Hispanic population should make ESI affordable for low-wage workers. Information about how Nebraska’s employers explain ESI and enroll Hispanic workers is necessary to better inform employees about ESI. Research is needed to define the economic contribution the Hispanic workforce makes to Nebraska’s economy to support policies that improve health access for this population. Primary Funding Source: HRSA growing trend towards the utilization of paid caregivers in hospice, such as aids or various nursing staff. Studies show that terminally-ill minorities with low income are more in need of paid caregivers. The objective in this study was to determine whether and how two variables in hospice care, the race of the patient and the type of caregiver (paid vs. unpaid), were related to the trend of shorter stays in hospice. Study Design: To model the risk of dying within one month after admission to hospice care, we used the Cox proportional hazard because it allows for both non-normal distributions (to account for the well-known highly skewed length of stay) and censoring (to account for patients discharged alive). Patient characteristics (age, gender, and death place), clinical characteristics (referral source and diagnostics at discharge) and hospice characteristics (profit/nonprofit) were factored in to the model. Population Studied: In this retrospective study, we looked at a sample of patients over the age of 65 who died or were discharged alive (N=3,142) from hospice care from National Home and Hospice Care Survey (pooled data for 1998-2000). Principal Findings: There were no main effects of race and type of caregiver, but there was a significant racial effect, depending on the type of caregiver. Minorities with paid caregivers were 39% more likely than non-Hispanic whites with paid caregivers to die within one month (p=0.0206). In contrast, racial disparity in the risk was not found when both groups were taken care of by their relatives/ unpaid caregivers (p=0.2088). Conclusions: Racial disparity in outcomes between hospice patients was found in only one subgroup: between minorities and whites taken care of by paid caregivers, but not found when both groups were taken care of by their relatives/ unpaid caregivers. This suggests that the dying minority elderly may only achieve similar timely access to hospice care as compared to whites if they are cared for by their relatives. Implications for Policy, Delivery, or Practice: We need to examine policy interventions that might benefit minority hospice patients that have to rely on paid caregivers. We should also explore why elderly minority hospice patients are more susceptible as a group to delayed access to hospice care than non-Hispanic whites when they both have to rely on paid caregivers. These questions are important, considering our finding that there was no racial disparity when taken care of by relatives/unpaid caregivers. Primary Funding Source: Retirement Research Foundation ●Disparities for Minority Elderly in Receipt of Timely Hospice Care Kyusuk Chung, Ph.D., Ross Mullner, Ph.D., Audrey K. Gordon, Ph.D., Duck-Hye Yang, Ph.D., Joseph Lee, M.D. ●Effect of Retirement on Body Mass Index among the Near Elderly Sukyung Chung, MPH Presented By: Kyusuk Chung, Ph.D., University Professor, Health Administration, Governors State University, One University Parkway, University Park, IL 60466; Tel: (708) 5344047; Fax: (708) 534-8041; Email: k-chung@govst.edu Research Objective: Although the use of hospice care among the terminally-ill elderly has tripled over the last decade, there has been a growing concern about the steady increase in the proportion of hospice patients with short stays (less than one month). Short stays in hospice may be troublesome as it can prevent the full benefit of hospice care. Though the majority of hospice patients are still taken care of by unpaid primary caregivers (such as family or friends), there has been a Presented By: Sukyung Chung, MPH, Graduate Student, Health Policy and Administration, University of North Carolina at Chapel Hill, 1103B McGavran-Greenberg Hall, CB#7411, Chapel Hill, NC 27599-7411; Tel: (408)746-0916; Email: sukyungc@email.unc.edu Research Objective: Retirement changes the availability of financial resources and leisure time, and could act as either an opportunity or a barrier to the maintenance of healthy body weight. This study investigates the causal effect of retirement on BMI to help determine the population of priority for interventions to halt the growth of obesity and related health care costs. The role of wealth and the relative importance of quantity and content of leisure time in the BMI response to retirement are also explored. Study Design: Retirement in this study is defined as currently not working and self-considered as retired. To get consistent estimate of retirement, not induced by health conditions, the fixed effects with instrumental variable method is employed. Eligibilities for defined-benefit pension and Social Security benefit were used as instruments for retirement. Subsamples based on total household wealth were compared to examine the role of wealth in the BMI response to retirement. The relative importance of retirement-related changes in quantity and content of leisure time is examined by estimating the effect of reduced working hour on BMI among workers, and the effects of retirement on BMI as compared to working in physical jobs and sedentary jobs. Population Studied: This study uses six panels of the Health and Retirement Study (HRS) conducted every two years from 1992 to 2002 with age ranged from 51 to 71 (n=41,725). The HRS is a national survey including all genders and racial groups. Principal Findings: The mean BMI of the sample was 28.5 and retirement increases BMI by 0.4 points on average compared to currently working status either full time or part time. The BMI response to retirement was greater, 1.0 in BMI, among those with lower wealth, but disappeared among the wealthier group. Retirement significantly increased BMI as compared to working in sedentary jobs or physical jobs. However, reduced working hour or increasing leisure time did not change BMI for current workers. The weight gain effect was persistent in the model using a broader definition of retirement. Conclusions: Retirement causes the greatest gain in BMI for those with less wealth. Two pieces of evidence – gain in BMI with retirement compared with working, regardless of job types, and no effect on BMI from reduced working-hours among workers – suggest that change in content of leisure time with retirement lead to BMI gain. Changing leisure time health behavior, such as physical activity and diet, with retirement, and differences in these responses between people with different socioeconomic status should be further explored. Implications for Policy, Delivery, or Practice: The modest marginal weight change with retirement has a sizable impact on the population obesity rate because the majority of people in their fifties and sixties are overweight prior to retirement. The impact of BMI gain with retirement on public health and Medicare costs will accelerate with the expanding retired population. Interventions to improve leisure time health productivity of retired people in low wealth status should be among the highest priorities in public health policy. Primary Funding Source: No Funding Source ●The Utilization of Dental Services by Diabetics in Colonias on the Texas/Mexico Border Martha Conkling, MSPH Presented By: Martha Conkling, MSPH, Graduate Assistant, Health Policy and Management, School of Rural Public Health, 3000 Briarcrest, Suite 300, Bryan, TX 77802; Tel: (979)458-3031; Email: mctromp@srph.tamhsc.edu Research Objective: One-third of people with diabetes have severe periodontal disease. Recent evidence suggests a two way association between chronic periodontal inflammation and diabetes. This study was conducted to investigate if individuals with diabetes in the colonias near McAllen, Texas have lower realized access to dental services than those individuals without diabetes. It is hypothesized that diabetics are more likely to have seen a health care provider than to have seen a dentist in the last year. Study Design: Baseline household survey data collected from December 2002 to April 2003 in the colonias near McAllen, Texas was used for this study. Multiple logistic regression was performed to assess whether diabetics in this population have lower realized access to dental services than those individuals without diabetes. Population Studied: Four hundred and forty-six adults were interviewed. A blood sugar test or screening had been received by 231 participants. These people were included in the study. Eighty four of the adult participants reported having diabetes. As a population residents of colonias are known to be poor, uneducated, and overweight. Principal Findings: Seventy-eight percent of people with diabetes reported that they had an education at the 8th grade level or less and 72 percent live in households with an income less than 8,000 dollars per year. People with diabetes were 86 percent less likely to have seen a dentist in the last year, than those without diabetes (p-value 0.024). People who had seen a health provider were 11 times more likely to have seen a dentist (p-value 0.033). Participants over 65 years were 96 percent less likely to have seen a dental health provider in the last year. Participants reporting a low perception of their health were 85 percent less likely to have seen a dentist in the past year (p-value 0.006). Conclusions: A clear relationship has been demonstrated between those who have realized a dental provider visit in the last year and diabetes status. This disparity is caused to some degree by the lack of dental insurance in this population and must also be affected by the extreme poverty of the households that diabetics reside in. A minimum of education is a factor since an ability to obtain access to health services is contingent on basic literary skills. Implications for Policy, Delivery, or Practice: The interrelationship between diabetes and periodontal inflammation suggests that preventive dental care may be important in preventing complications of both diseases. The Centers for Disease Control recommends that diabetic patients see a dentist at least once every 6 months, with more frequent dental visits for those with periodontal disease. The American Diabetes Association’s standards for treating diabetic patients include an examination of the oral cavity as part of the patient’s initial visit. However, periodic oral examinations are not included as a standard of continuing care. It is hoped that new strategies to control diabetes by improving dental care in the colonias can be devised. An inability to consume foods due to unhealthy gums and lost teeth could result in untimely deaths. Primary Funding Source: RWJF, HRSA ●A Cultural Competence Organizational Model: Lessons from the Safety Net Linda Cummings, Ph.D., Donna Sickler, MPH, Ed Martinez, MPA, Marsha Regenstein, PhD, Jennifer Cromwell Presented By: Linda Cummings, Ph.D., Director of Research, , National Association of Public Hospitals and Health Systems, 1301 Pennsylvania Avenue, NW, Suite 950, Washington, DC 20004; Tel: (202) 585-0100; Fax: (202) 585-0101; Email: lcummings@naph.org Research Objective: The largest concentration of LEP patients in the American health care setting is in the public hospital system. These hospital systems care for a highly diverse patient population. Some of the nation’s largest safety net hospitals and health systems receive interpreter services requests in over 60 languages. A variety of cultural competence practices have been developed to better serve culturally and ethnically diverse patients who often are also low-income and uninsured. Much has been written about the goals of culturally and linguistically appropriate practices, but few models exist that offer practical examples to guide work in this area. This study focused on cultural competence practices at Woodhull Medical and Mental Health Center, part of the largest public hospital system, the New York City Health and Hospital Corporation, in the most diverse city in the nation. Study Design: Woodhull Medical Center was selected for a comprehensive case study because it is a mature, complex health care system that has integrated cultural competence practices throughout the organization, operationalizing these practices into quality improvement initiatives on a sustained basis. Researchers conducted in-depth interviews during an extensive site visit at Woodhull with the chief executive officer, chief medical officers, human resource director, director of communications, patient care coordinators, and other key staff. Researchers visited programs and reviewed materials developed to support cultural and linguistic services at the medical center. Population Studied: Major safety net hospital in New York City. Principal Findings: Researchers found cultural competence programs and policies at Woodhull to be integrated into key aspects of hospital operations including administrative/medical leadership, human resources, interpreter services, customer service, infrastructure, and community relations. Cultural competence practices and policies at Woodhull are closely linked with quality improvement efforts. Despite the considerable resource constraints affecting safety net organizations, leadership commitment and ingenuity are instrumental in building a culturally competent organization and effective approaches, especially with new or difficult-to-reach patient populations. Conclusions: This study found that cultural competence practices at one large safety net hospital can be systematically described to provide guidance to other health care organizations as they begin implementation of these practices. This study offers a practical model for implementing culturally and linguistically appropriate practices that identifies unique features of the safety net setting and the challenges or barriers to implementation. Implications for Policy, Delivery, or Practice: For safety net providers, this case study offers a model for implementing significant cultural competence practices and embedding them in hospital practices, despite considerable resource constraints. The study offers valuable lessons for the health care system as a whole, given the nation’s changing demographics. These findings have relevance for a variety of hospitals and health care systems that are experiencing an influx of new immigrant groups or retooling practices to better serve a diverse patient population. Primary Funding Source: Other, National Association of Public Hospitals and Health Systems ●Use of Adjuvant Chemotherapy and Radiation Therapy for Colorectal Cancer among Asian Americans and Pacific Islanders James W. Davis, Ph.D., Todd B. Seto, M.D., MPH Presented By: James W. Davis, Ph.D., General Internal Medicine Fellow, Internal Medicine, Harvard Medical School, Massachusetts Veterans Epidemiology Research and Information Center; 790 Boylston Street, 24F, Boston, MA 02199; Tel: (808)382-7767; Research Objective: Consensus guidelines and randomized trials support the use of chemotherapy for stage III colon cancer and chemotherapy with radiation therapy for stages II and III rectal cancer to improve survival. While the use of these treatments may be partly related to patient ethnicity, the management of Asian Americans and Pacific Islanders (AAPIs) with colorectal cancer remains largely unknown. Objective: To evaluate the use of chemotherapy and radiation therapy for colorectal cancer among AAPIs. Study Design: Retrospective analysis using data from the Hawaii Tumor Registry, a Surveillance, Epidemiology, and End Results (SEER) Program population-based registry, linked to administrative data from Hawaii´s largest health insurer. Population Studied: We studies the first course of therapy for 602 patients (336 Japanese, 46 Chinese, 74 Filipino, 48 Hawaiian, 98 white; mean age 67+/-13 yrs) diagnosed with stage III colon cancer (n=347) or stages II (n=109) or III (n=146) rectal cancer in Hawaii from 1995-2001. We evaluated the use of standard-of-care treatments as defined by NCI/NIH guidelines: (1) chemotherapy for stage III colon cancer and stages II or III rectal cancer, and (2) radiation therapy for stages II or III rectal cancer. We used logistic regression to examine the association between ethnicity and quality of care. Principal Findings: Overall, 71.6% (n=431) of patients received chemotherapy. Only 57.6% (n=147) of patients with rectal cancer received radiation therapy. Chemotherapy rates were similar among all ethnicities (from 67.6% of Filipinos to 77.1% of Hawaiians, P=0.8). Adjusting for tumor stage and site, age, gender, year of diagnosis, rural residence, cancer history, grade, Charlson comorbidity index, health plan (HMO, fee-for-service, Medicare), and income, chemotherapy was used significantly less often among older patients (OR, 0.02; 95%CI, 0.01-0.06, for age >/=85 vs. <55) and those with prior cancer (OR, 0.53; 95%CI, 0.29-0.99) or stage II rectal cancer (OR, 95%CI: 0.37, 0.21-0.65, for stage II rectal; 1.66, 0.92-3.01, for stage III rectal vs. stage III colon). Radiation rates were low among all ethnic groups (from 52.9% of Chinese to 77.8% of Hawaiians, P=0.26). Hawaiians were more likely than whites to receive radiation in adjusted analyses (OR, 95%CI: 4.61, 1.25-16.99, for Hawaiians; 1.30, 0.54-3.12, for Japanese; 0.91, 0.29-2.82, for Filipinos; 0.95, 0.25-3.57, for Chinese). Significant predictors of lower radiation use included advanced age (OR, 0.09; 95%CI, 0.02-0.47, for age >/=85 vs. <55) and prior cancer (OR, 0.28; 95%CI, 0.11-0.74). Conclusions: We found low rates of standard treatments for colorectal cancer among all ethnic groups in our population, without significant disparities among AAPIs. Implications for Policy, Delivery, or Practice: Further study is needed to determine the reasons for the observed low use of chemotherapy and radiation therapy in our population. Primary Funding Source: AHRQ ●Disparities Changes in the United States: Findings from the National Healthcare Disparities Report Elizabeth Dayton, MA, Dwight McNeill, Ph.D., MPH, Ernest Moy, M.D., MPH, Ed Kelley, Ph. D. Presented By: Elizabeth Dayton, M.A., Junior Service Fellow, Department of Health and Human Services, Agency for Healthcare Research and Quality, 540 Gaither Road, Rockville, MD 20850; Tel: (301)427-1320; Fax: (301)427-1341; Email: edayton@ahrq.gov Research Objective: Our objective is to begin describing changes in disparities in American healthcare and to draw interpretations and make recommendations for improvement. Study Design: This study is based on research from the National Healthcare Disparities Report (NHDR), a Congressional mandated report that annually analyses healthcare differences by race/ethnicity and socioeconomic status across about 250 measures from three-dozen sources. Sources include 7 databases sampling the civilian, noninstitutionalized population; 5 sampling healthcare facilities and providers; 7 extracting from data systems of healthcare organizations; 4 surveillance and vital statistics systems databases. Data for minority and poorer populations are compared with data for whites and higher-income populations, respectively. Annual rates of change are determined for measures with multi-year data. Disparities are considered meaningful if relative differences are at least 10% and statistically significant with p<0.05, assessed using ztests. Population Studied: The national U.S. population. Principal Findings: The 2004 NHDR reports some disparities changes, though overwhelmingly disparities persist, with minorities and poorer populations receiving worse care than whites and higher income groups, respectively. Some disparities exhibit improvement. For example, in 1998 elderly Asian and Pacific Islander Medicare beneficiaries had lower rates of influenza vaccination than whites; in 2000 no significant difference was observed. In 1999 blacks and Asians were less likely than whites to report a source of ongoing care; in 2000 a significant difference was not evident. In 2000 black children age 19-35 months had lower rates of measles-mumps-rubella vaccination than whites, and Hispanic children had lower rates of Haemophilus influenzae vaccination than non-Hispanic whites; a significant difference was not evident in 2002. In 1992 black women had a higher rate of late stage breast cancer than whites; 2001 rates were similar due to falling rates among blacks coupled with rising rates among whites. However, overall disparities changes from 2000 to 2001 observed in the NHDR are moderate. About 3% of measures for blacks improved; about 5% deteriorated. About 14% of measures for Hispanics improved; about 3% deteriorated. About 6% of measures for Asians improved; none deteriorated. American Indians and Alaskan Natives saw no measures improve; about 5% deteriorated. In sum, minorities’ healthcare quality improved for about 6% and deteriorated for about 3% of measures. The poor were the only income group with any significant change, experiencing improvement for about 5% of measures. Conclusions: The national average rate of change for healthcare disparities is slow, but these analyses illustrate that improvement is possible. Some changes parallel specific improvement efforts. For example, elimination of some vaccination disparities for minority children may be partly related to the CDC National Immunization Program. Elimination of the disparity for late stage breast cancer between black and white women may be partly attributable to the CDC National Breast and Cervical Cancer Early Detection Program and improving rates of mammography among blacks. Implications for Policy, Delivery, or Practice: Improvement, deterioration, and disparities highlight best practices and components and populations in healthcare where targeted improvement efforts are most needed and would garner the greatest results; understanding trends in healthcare quality and disparities may play a key role in improving healthcare. Primary Funding Source: AHRQ ●Racial/Ethnic Differences in Tumor Stage at the Time of Diagnosis in Managed Care Settings for Cancers Detectable by Screening. Chyke Doubeni, M.D., MPH, Terry S. Field, D.Sc., Diana Buist, Ph.D., Shelley Enger, Ph.D., Eli Korner, Ph.D., Lois Lamerato, Ph.D. Presented By: Chyke Doubeni, M.D., MPH, Assistant Professor, Family Medicine and Community Health, Meyers Primary Care Institute/University of Massachusetts, 55 North Lake Avenue, Worcester, MA 01655; Tel: (508)334-7772; Fax: (508)595-2200; Email: chyke.doubeni@umassmed.edu Research Objective: Racial/ethnic differences in the stage of tumor at the time of diagnosis contribute to disparities in cancer survival rates. Limited data are available examining the association between race/ethnicity and cancer stage at diagnosis in racially diverse populations in settings where health insurance is not a barrier. We examined this association among patients who were diagnosed with breast, cervical, prostate or colon/rectum cancer while enrolled in one of six geographically diverse managed care organizations (HMO). Study Design: This is a repeated cross-sectional study. Population Studied: This population-based study was conducted on patients diagnosed with breast, cervical, prostate or colon/rectum cancer between 01/01/93 and 12/31/98, who were identified from tumor registries associated with six HMOs. Patients with cancers of unknown tumor stage were excluded. We further restricted our sample to patients identified as non-Hispanic white (“white”), nonHispanic black (“black”), Hispanic, or Asian. Principal Findings: This study was comprised of a total of 24,225 patients with breast, 1,396 with cervical, 22,456 with prostate and 13,741 with colon/rectum cancer. In multivariable logistic regression models that adjusted for age at diagnosis, year of diagnosis, study site and duration of enrollment with the health plan prior to diagnosis, black women were much more likely to have advanced breast ((adjusted odds ratio [OR] (95% confidence interval [CI]): 1.62 (1.42-1.84)) or cervical (OR (95% CI): 1.35 (0.90-2.01) cancer at the time of diagnosis compared to white women. Black men were also more likely to have advanced prostate cancer (OR (95% CI): 1.15 (1.01-1.31)) compared to white men. Hispanic women were slightly more likely to have advanced breast (OR (95% CI): 1.09 (0.94-1.26)) or cervical (OR (95% CI): 1.11 (0.78-1.57)) cancer at the time of diagnosis compared to white women but these associations were not statistically significant. Asian women were less likely to have advanced breast cancer (OR (95% CI): 0.87 (0.73-1.03)), but were more likely to have advanced cervical cancer (OR (95% CI): 1.51 (1.01-2.26)) compared to white women. In logistic regression models that also adjusted for sex, blacks, Hispanics and Asians were slightly more likely to have advanced colon/rectum cancer at diagnosis compared to whites, although the associations did not reach statistical significance. However, Black men with colon/rectum cancer were significantly more likely to have advanced disease at diagnosis compared to white men. Conclusions: Our study found pervasive racial/ethnic differences in stage of cancer at diagnosis even in settings where financial barriers to healthcare access may not exist. More research is needed to better understand the causes of these differences. Implications for Policy, Delivery, or Practice: Elimination of financial barriers alone may not eliminate racial/ethnic disparities in cancer stage at diagnosis. Primary Funding Source: NCI ●The Socio-Economic Gradient in Health and Functioning Among Children and Youth Lisa Dubay, ScM Presented By: Lisa Dubay, ScM, Principal Research Associate, Health Policy Center, The Urban Institute, 2100 M Street NW, Washington, DC 20037; Tel: (202)261-5667; Fax: (202)2231149; Email: ldubay@ui.urban.org Research Objective: The socio-economic gradient in morbidity, mortality, and overall health status at various points across the lifespan has been well documented in the medical, public health, economic, and sociology literatures. There is also a body of literature that argues that a life-course perspective is critical to understanding disparities associated with socio-economic position (SEP). This view derives from evidence that children’s health and functioning and the physical, social and psychosocial environments in which they reside at critical developmental junctures, particularly early childhood and adolescence, are associated with health status in adulthood. Surprisingly, there is scant evidence of a socioeconomic gradient in health and functioning in childhood and adolescence in the US. Perhaps more important to the development of policies to reduce disparities, or gradients, there is a paucity of research that examines the pathways through which SEP affects child health and functioning or examines multiple dimensions of health and functioning within the same study. This paper attempts to close this critical gap in the literature. Study Design: Data for this paper are derived from the recently released 1997 and 2002 Child Development Supplement to the Panel Survey of Income Dynamics (PSID). The Child Development Supplement (CDS) is uniquely suited to examine these issues because of the survey’s breadth and depth of content. Using the PSID, a new measure of socioeconomic position, based on Britain’s National Statistics-Socio-economic Classification (NS-SEC), is used to examine the extent of the SEP gradient in child and adolescent health and physical, cognitive, and emotional functioning and to assess whether this gradient increases as children age. The paper documents the extent to which SEP is negatively associated with exposures to family, school, and neighborhood environments that threaten children’s health and functioning and positively associated with potential mediating and adaptive mechanisms. Descriptive, multivariate, and factor analyses are used in this paper. Population Studied: A nationally representative sample of children ages 0-12 were drawn from participants in the PSID in 1997 (n=2907) and were interviewed and re-interviewed five years later in 2002. Principal Findings: The results suggest that a SEP gradient exists in child health and physical, cognitive, and emotional functioning and that these gradients grow as children age. Furthermore, children of lower SEP are more likely to live in family, school, and neighborhood environments that threaten rather than promote child health and functioning. Conclusions: Understanding the pathways through which SEP affects child health and functioning is critical to developing effective primary and secondary interventions that can reduce SEP disparities. Implications for Policy, Delivery, or Practice: The current policy focus on reducing health disparities through the health care system may be necessary but is an insufficient mechanism for eliminating health disparities. Unless the fundamental disparities in children’s family, school, and neighborhood environments are ameliorated, the gradient in health disparities will continue to exist and to grow over the life-course of these children. Primary Funding Source: Other ●Willingness to Participate in Clinical Trials Among Elderly Whites and African Americans Raegan Durant, M.D., Roger B. Davis, Sc.D., Edward Marcantonio, M.D., MSc, Marcie B. Freeman, MEd, Bruce E. Landon, M.D., MBA Presented By: Raegan Durant, M.D., General Medicine Fellow, Division of General Medicine and Primary Care, Beth Israel Deaconess Medical Center, 330 Brookline Avenue, Rose 111, Boston, MA 02130; Tel: (617)667-0487; Fax: (617)667-2751; Email: rdurant@bidmc.harvard.edu Research Objective: Despite National Institutes of Health mandates for minority inclusion in clinical research, African Americans are underrepresented in clinical trials. Many have hypothesized that African Americans are less willing to participate in clinical trials partially due to higher levels of distrust in the health care system. We sought to determine the differences in willingness to participate in clinical trials among elderly whites and African Americans and the factors that influence their willingness to participate. Study Design: We assessed willingness to participate in 3 hypothetical clinical trials with increasing levels of risks (diet trial for obesity, antihypertensive trial for HTN, chemotherapy trial for cancer) on an ordinal scale from 1 (“not willing”) to 5 (“very willing”). We created a mean willingness to participate scale calculating the mean score for each respondent based on responses to the 3 vignettes (Cronbach’s alpha 0.74). For analysis, each respondent was categorized as less (mean score < 4) or more (mean score > or = to 4) willing. We assessed trust in one’s primary care provider (PCP) and trust in clinical research separately using two previously validated scales. We also assessed sociodemographic factors, comorbidities, health status, previous exposure to clinical research, personal experiences with discrimination, and attitudes toward potential barriers and incentives associated with trial participation. We performed bivariable analyses to examine the associations between these factors and willingness to participate. Those factors significantly associated with the outcome were used to create a multivariable logistic regression model. Population Studied: We surveyed, via mail, 1412 eligible community dwelling elderly (age >50) whites and African Americans in the Boston metropolitan area. Principal Findings: We received responses from 755 eligible persons (53% response rate). The study population was 63% white and 37% African American. African Americans were not significantly more distrustful of their care providers (46.3% vs. 44.6%, p=0.66) or clinical research (3.2% vs. 3.0%, p=0.84). In unadjusted analyses, whites were slightly more likely to be more willing (32.8% vs. 29.9% p=0.13) to participate in clinical trials compared to African Americans. In the multivariable model, male gender (OR 2.40, 95% CI 1.58,3.64), having dependent care responsibilities (OR 1.96, 95% CI 1.16,3.32), previous trial participation (OR 1.84, 95% CI 1.24,2.74), and the endorsement of the importance of participant benefit from trial participation (OR 2.16, 95% CI 1.24,3.76) were all associated with an increased willingness to participate. Respondents who thought it would be important for their own PCP to ask them to be in a trial were less willing to participate (OR 0.60, 95% CI 0.37,0.96). Neither race nor distrust was independently related to willingness to participate in the final multivariable model. Conclusions: African Americans were not significantly less willing to participate in clinical trials compared to whites. Distrust was not an independent predictor of willingness to participate in clinical trials. Low representation of African Americans in clinical trials may be due to factors other than a lower willingness to participate. Primary Funding Source: NIA ●Effects of Medicare Beneficiary Race/Ethnicity, SocioEconomic Status, and Coverage Type on Mammography Screening: Comparison of a Diverse Group of Medicare Advantage and Fee-for-Service Enrollees Kelle Eason, MPH, Ashley Antler, BA, Michelle Fernandez, MPH, Susan Merrill, PhD, MPH Presented By: Kelle Eason, MPH, Healthcare Data Analyst, Scientific Affairs, Lumetra, One Sansome Street, Suite 600, San Francisco, CA 94104; Tel: (415)677-2168; Fax: (415)6778436; Email: keason@caqio.sdps.org Research Objective: Evidence suggests patients enrolled in Medicare Advantage (MA) (Medicare managed care, formerly known as Medicare+ Choice) may be more likely to receive regular preventive care than their counterparts with Fee-forService (FFS) coverage. Furthermore, older women, non-white women, and women in lower socio- economic strata are less likely to receive mammograms. The primary objective of this study is to identify patterns in mammography screening among diverse populations in both MA and FFS settings. The aim is to compare mammography rates and patterns in each setting while controlling for demographic factors associated with receipt of mammography; race/ethnicity, age, dualeligibility (enrollment in both Medicare and Medicaid), and socio-economic factors such as income and education, in order to determine if these factors alone or in combination account for variance in mammography screening rates between settings with different funding and organizational structures. We hypothesized that the MA population would have consistently higher mammography rates than women enrolled in FFS, and that mammography screening patterns would differ between the MA and FFS populations. Study Design: Health Plan Employer Data and Information Set (HEDIS) mammography population data (2001-2002) and Centers for Medicare and Medicaid Services (CMS) (20012002) Medicare administrative claims data were used to assess screening status of female MA and FFS Medicare enrollees in California. Demographic variables for both populations were obtained from CMS enrollment data, and 2000 Census data were used to estimate socio-economic factors of the beneficiary neighborhood by zip code. Analyses examined individual demographic characteristics that were associated with the receipt of biennial mammography in each population, and those that had an inverse effect. Combined and interactive effects were also evaluated, and differences in mammography patterns between the two populations were identified. This study does not include comparisons between managed care plans or physician offices. Population Studied: Study population includes women aged 50-67 as of January 2001 and their mammography screening status during January 2001-December 2002. Principal Findings: Overall, MA mammography rates were higher (76.4%) than those in FFS (45.8%). In the MA population, dual eligibility and/or Hispanic race/ethnicity were both independently associated with not receiving a mammogram. In the FFS population, dual eligibility was not as significant, but any non-white race/ethnicity (Black, Hispanic, Asian, Native American, and Other) was associated with not having received a mammogram during the two-year measurement period. Conclusions: Contrary to our initial hypothesis that the MA population would have consistently higher mammography rates compared to women enrolled in FFS, our findings suggest that this pattern may not hold true across all demographic groups. Dually eligible women had a lower mammography rate in both settings, a finding consistent with previous studies indicating that lower income women are less likely to receive a mammogram. However, the disparity in rates between dually eligible and non-dually eligible women in MA was twice that observed in the FFS population, suggesting that the pattern of better preventive services in MA does not necessarily apply to lower income women. When analyzed by race/ethnicity, similar patterns were observed for MA and FFS women. Non-White women in both settings experienced lower rates of mammography screening than their White counterparts in the same setting. Comparison of rates between settings revealed that White, Black and Asian women in MA were more likely to receive a mammogram than their counterparts in FFS. Surprisingly, a different pattern was observed for Hispanic women, who were no more likely to have received a mammogram in the MA versus FFS setting. Implications for Policy, Delivery, or Practice: When patterns within the MA and FFS settings are identified and compared, a more complex picture of the effects of demographics begins to emerge. Providers and administrators may consider special breast cancer education and mammography reminder programs with particular attention to coverage type and population diversity. Providers in both settings may share best practices to improve mammography screening among their respective patients. The patterns observed in this study may have larger implications for the future of Medicare mammography screening, as the diversity of this study population mirrors predicted changes in the Medicare population nationwide. Primary Funding Source: CMS ●Differences In Symptom Presentations and Screening of African Americans and Whites for Benign Prostatic Hyperplasia (BPH) Bennett Edwards, Ph.D., Daniel Howard, Ph.D., Kimberly Whitehead, Ph.D., Ahinee Amamoo, MS, Yhennekko Jallah, MS, Paul Godley, M.D., Ph.D., MPH Presented By: Bennett Edwards, Ph.D., Associate Professor, Allied Health Professions, Shaw University, 118 East South Street, Raleigh, NC 27601; Tel: (919)231-2501; Fax: (919)7434693; Email: bedwardssu@aol.com Research Objective: To determine whether there are racial differences over time in symptoms, screening, and health care-seeking behaviors for BPH Study Design: Four common urinary symptoms evaluated were: pushed or strained to urinate; urinated again shortly after urination; stopped and started several times when urinating; and dribbled urine after initial urination period. Severe urinary symptoms (incontinence, and prostate problem prevented urination) were also evaluated. Screening was measured by whether the respondents received regular digital rectal exams (DRE) by a physician (MD). Respondents' were asked if they regularly go to a MD and if they put-off care quite often, which were used to measure the health care-seeking behaviors of the respondents. In addition to these factors, information on respondents' socioeconomic factors, health conditions, and MD characteristics were also collected. Comparisons between AA and W elders' responces to common and severe symptons, screening behaviors, and health care seeking behaviors were compared using Fisher's exact tests. Generalized Estimating Equations (GEE) were used to determine the racial effects over time between urinary symptoms and BPH, adjusting for socioeconomic factors, health conditions and MD characteristics. Population Studied: The study population included male respondents, ages 65-85, from Waves 3 (1994-African Americans (AA)=482; Whites (W)=407 and 4 (1998-AA=253; W=237) of the Established Populations for the Epidemiologicic Studies of the Elderly (EPESE). Principal Findings: W reported all four common symptoms more frequently than AA in 1994 and 1998, with stopped and started several times when urinating (p=0.002); and dribbled urine after initial urination period (p=0.034) being significant. However, AA were more likely to report severe symptoms, with incontinence being statistically significnat over time (p=0.002). AA were less likely than W to have a regular DRE in both 1994 and 1998 (p=0.008 and p<0.001, respectively) and less likely to see an MD in 1994 (p<0.014).Futhermore, over time AA were more likely to not have a regular rectal exam because they were not bothered by their symptoms (p=0.016). GEE statistics for AA over time demonstrated significantly more No Named Physician responses than W. Those that regularly had a DRE by an MD were less likely to live in a rural area(OR=0.301;p<0.004) and less likely less likely to put off health care (OR=0.295; p=0.004), when adjusted for other socioeconomic, health conditions and MD characteristics. AA had significantly more incidences of diabetes than W in 1998 (p=0.023). Conclusions: Whites reported common urinary symptoms more often although, African Americans appear to present severe symptoms differently and are less likely to see an MD. The lack of access to a MD or lack of bother may contribute to their advanced BPH symptoms. In addition, Diabetes may confound and/or mask BPH symptoms. Implications for Policy, Delivery, or Practice: A continued effort is needed to increase early MD visits with African American males males to decrease the number of those presenting with severe BPH symptoms. Primary Funding Source: AHRQ, NIH National Center on Minority Health and Health Disparities/R24 MD00167/P60 MD000239 ●Racial Disparities in Lipid Management in Patients with Diabetes Jennifer Elston Lafata, Ph.D., Manel Pladevall, MPH, M.D., Jan Simpkins, MA, Kaan Tunceli, Ph.D., George Devine, Ph.D., L. Keoki Williams, MPH, M.D. Presented By: Jennifer Elston Lafata, Ph.D., Director, Center for Health Services Research, Henry Ford Health System, 1 Ford Place, Suite 3A, Detroit, MI 48202; Tel: (313)874-5454; Fax: (313)874-7137; Email: jlafata1@hfhs.org Research Objective: To describe lipid management over time in a cohort of patients with diabetes (DM) and evaluate whether care receipt differed between African American and White populations in an equal access environment. Study Design: Automated claims and clinical databases were used to identify a cohort of patients with DM in 1997/1998 that was retrospectively followed through 2002 (mean follow- up = 42.1 months). Overall and race stratified rates of hypercholesterolemia screening, treatment and goal achievement were estimated in each follow-up year. Treatment was determined by a claim for lipid lowering agents and goal attainment was defined as low density lipoprotein cholesterol (LDL-C) less than 100 and 130 mg/dL. Population Studied: Retrospective cohort of 11,411 HMO enrollees aged 18+ years (50.8% female; 53.2% White, 43.1% African American, and 3.7% other), with DM who were continuously enrolled during 1997/1998. Principal Findings: During follow-up, rates of testing, treatment and goal attainment improved over time for both races. Racial disparities favoring the White cohort were evident for all rates in each year. Rates of testing increased from 60.7% in 1999 to 76.8% in 2002 for Whites and 48.2% to 71.1%, respectively for African Americans. Rates of treatment increased from 34.6% in 1999 to 53.4% in 2002 for Whites and 26.1% to 45.7%, respectively for African Americans. Rates of goal achievement at LDL-C <100 mg/dL increased from 34.9% in 1999 to 42.5% in 2002 for Whites and 23.9% to 30.8%, respectively for African Americans. Rates of goal achievement at LDL-C <130 mg/dL increased from 71.2% in 1999 to 79.7% in 2002 for Whites and 59.1% to 67.6%, respectively for African Americans. Among patients treated with lipid lowering agents, rates of goal achievement over the same period improved from 67.3% to 75.5% when using a goal of LDL-C <130 mg/dL but only 34.1% to 40.3% when using the currently recommended goal of LDL-C <100 mg/dL. Conclusions: Our preliminary findings show that racial disparities in rates of testing tended to decrease over time, while those associated with LDL-C goal achievement and treatment with lipid lowering drugs tended to persist over time. Overall gains in all rates were achieved between 1999 and 2002 but the percentage of these high risk patients at the current recommended LDL-C goal (i.e., LDL-C <100 mg/dL) remains low regardless of race. We are in the process of evaluating these racial disparities adjusting for other factors. Implications for Policy, Delivery, or Practice: This research shows persistent underachievement of recommended LDL-C goal levels among those known to be at elevated risk for cardiovascular disease, especially among African Americans. Since appropriate use of preventive and early diagnostic interventions is key in reducing the health and economic burden of cardiovascular disease it is incumbent on health care delivery systems to address these disparities in treatment. Primary Funding Source: Blue Cross Blue Shield of Michigan ●Reducing Disparities in Diabetes Care among the Nation’s Most Vulnerable Patients Christopher Forrest, M.D., Ph.D., Kaytura Felix-Aaron, M.D., Jinlin Wang, MS, Amisha Pandya, MHS, Elvan Daniels, M.D., Leiyu Shi, Dr.PH. Presented By: Kaytura Felix-Aaron, M.D., Chief, Clinical Quality Data Branch, Division of Clinical Quality, Bureau of Primary Health Care, 5600 Fisher Lane, Room 17C-26, Rockville, MD 20857; Tel: (301) 594-4306; Fax: (301) 594-5224; Email: KFelix-Aaron@hrsa.gov Research Objective: Low-income patients are disproportionately affected by diabetes, one of the most prevalent and costly chronic conditions affecting the US population. The federal government funds health centers (HCs) to provide services to vulnerable patients residing in medically underserved communities. One of the primary goals of HCs is to provide high quality services to all patients according to their needs, rather than their insurance status, race/ethnicity, or poverty status. This study was done to examine the costs and quality of diabetes care in HCs to assess whether they are fulfilling their goal of reducing healthcare disparities. Study Design: Cross-sectional analysis using sociodemographic, encounter, and practitioner data from 2002 and readily available from HCs’ management or clinical information systems. A standardized charge obtained from the Medicare fee schedule was applied to each procedure code in the encounter file. Morbidity burden and risk adjusted charges were obtained using the Johns Hopkins ACG case-mix system. We used generalized estimating equations (GEE) to control for age, sex, morbidity burden, and delivery site effects. Population Studied: The study was conducted in the Sentinel Center Network (SCN), a newly formed, national network of 52 health centers that share clinical data on all their patients to inform policy and improve practice for the health center safety-net. Data from a total of 962,011 patients (about 10% of all HC patients in the nation) comprise the SCN database. The diabetes patient study sample includes 58,519 adults age 18 and older. Principal Findings: Overall, 9.2% of the adult patient population, 8.1 % of white, 10.8% of black, 10.0% of Asian, and 9.2% of Hispanic had diabetes. Compared with those without diabetes, patients with diabetes had 2-fold higher morbidity burden (ACG risk score 2.99 v 1.46, p<.001); higher primary care expenditures/patient ($598 v $340, p<.001); and, higher visit rates/patient (7.81 v 3.81, p<.001). Multivariable analysis showed charges for uninsured patients were comparable to privately insured diabetes patients, whereas those for Medicaid and Medicare patients were significantly higher. In addition, charges for black and white patients were comparable, but those for Hispanic and Asian patients with diabetes were higher than those for whites. Charges for patients with diabetes whose income was below the federal poverty level (FPL) were similar to those between 101-200% of FPL and higher than those above 200% of FPL. With respect to quality of diabetes care overall, 57.8% of adult patients with diabetes had 1+ Hemoglobin A1C tests, 45.4% 1+ LDL tests, and 40.3% both tests done during 2002. The adjusted odds of having both tests performed was highest for the uninsured compared with those with public or private insurance, and the odds for ethnic minorities was higher than whites. Conclusions: We found no disparities in the costs or quality of diabetes care by insurance payer, race/ethnicity, or family income in the nation’s health centers. Implications for Policy, Delivery, or Practice: Health centers are achieving their goal of eliminating disparities by matching services according to patients’ needs. This equitable model of primary care service delivery is likely a result of the unique organization and financing of health centers, their governance and mission, including their responsiveness to local needs, and the health professionals who staff them. The health center model of primary care should be considered more broadly as a policy option for eliminating disparities throughout the nation. Primary Funding Source: HRSA ●Racial Segregation of Nursing Home Staff and Residents Zhanlian Feng, Ph.D., Mary Fennell, Ph.D., Vincent Mor, Ph.D. Presented By: Zhanlian Feng, Ph.D., Project Analyst, Center for Gerontology and Health Care Research, Brown University, 2 Stimson Avenue, Providence, RI 02912; Tel: (401) 863-9356; Fax: (401) 863-9219; Email: Zhanlian_Feng@brown.edu Research Objective: Previous research has documented persistent racial and ethnic disparities in various health care outcomes for elderly patients in long-term care settings. Yet, until recently little attention has been given to the issue of unequal access to nursing home care, which suggests that minority residents, particularly African Americans, are at far greater risk of residing in facilities with limited resources and historically poor performance than are whites. There is a lamentable dearth as well of available data on the racial/ethnic mix of nursing home staff. The purpose of this study is to describe the extent of racial segregation in the distribution of nursing home staff vis-à-vis residents. Study Design: The facilities under study represented a subsample from a national sample of nursing homes which participated in a study of organizational strategy and performance, in which data were collected on race/ethnicity of nurse aides. The subsample was comparable to national averages in terms of urban location, fairly close to national averages on percent of residents on Medicaid and percent self-pay, and these facilities were somewhat less likely to be for-profit or chain affiliated. Responses were matched with concurrent Minimum Data Set (MDS) resident assessments to obtain information on race/ethnicity of residents. The black-white Dissimilarity Index was used to depict the patterns of racial segregation of both facility staff and residents. Population Studied: The sample included 19,874 long-stay nursing home residents and 2,130 nurse aides from 145 freestanding facilities in 8 states in 1995. Principal Findings: Nearly 36% (N=52) of the study facilities had no black residents, whereas a few facilities (N=6) had over 50% black residents. Over 80% of all black residents resided in just under 20% of all facilities. The Dissimilarity Index was .648 for residents and .653 for staff, meaning about 65% of all black residents (or staff) would have to be relocated to achieve a perfectly even proportion of black residents (or staff) across all facilities. The correlation between the proportions of black residents and of black staff was fairly strong (.7), suggesting that homes with more black residents are heavily concentrated with black staff, and vice versa. Furthermore, facilities that were highly concentrated with black residents were more likely to be those with poorer resources as indicated by a substantially higher proportion of Medicaid residents and a lower proportion of private-paying residents. Conclusions: Access to nursing home care is marked by considerable racial/ethnic segregation, as evidenced by the high concentration of black residents in a small number of facilities. The racial/ethnic composition of nursing home staff also exhibited a similar pattern of segregation. Implications for Policy, Delivery, or Practice: Additional research is needed to assess the extent to which racial segregation of staff and residents in nursing homes mirrors residential segregation patterns in the local community, or is associated with other community or market characteristics. The primary question generated by these findings is what difference this high degree of racial segregation makes in the quality of care provided the average non-white nursing home resident. Primary Funding Source: NIA ●Social Identity and the Perceived Efficacy of and Engagement in Health Behaviors among a Low-Income, Minority Community Sample Tracy Finlayson, BS, Shawna Lee, MSW, MPP, Daphna Oyserman, Ph.D. Presented By: Tracy Finlayson, BS, Research Assistant, Health Management and Policy, University of Michigan School of Public Health, 109 South Observatory, Ann Arbor, MI 481092029; Tel: (734)615-5131; Email: tfinlays@umich.edu Research Objective: This research seeks to explore new frontiers in the determinants of health disparities by examining why risky and protective health behaviors are differentially related to social class. We investigate the interface between social identity and health, and develop a process model that accounts for when health messages and behaviors are judged as relevant for socially disadvantaged Americans and motivate health-related behavioral changes. We postulate that the idea of health in this country is socially represented by white, middle-class images, values, lifestyles, and behaviors that are not meaningful for people in other social groups. We aim to show that common health messages advocating certain health-promoting behaviors in the realms of oral health, physical health, and mental health are not perceived as relevant to many minority groups and socio-economically disadvantaged Americans, and are not effective in bringing about a change in behavior. Study Design: We held focus groups to inform the development of a survey on personal engagement in behaviors and perceptions about social identity and behaviors. Following a standard priming methodology, to make salient stigmatizing social identity membership (being reminded that one is a poor minority) participants were randomly assigned to prime or no prime survey conditions. ANOVA and regression analyses were performed to examine if making social identity salient altered efficacy ratings of various types of health behaviors and reported engagement in those behaviors, controlling for the individual’s level of identification with that social identity (Group Belongingness). Population Studied: We surveyed a community sample of primarily low-income African-American women attending the weekly job fair at a state social service agency in Michigan. 121 surveys were collected during Summer 2004. Principal Findings: Strongly identifying with one’s social group (High Group Belongingness) predicted participants’ beliefs that other members of their social group smoked often and were not likely to eat fruits/vegetables regularly. It also predicted a decreased likelihood of flossing in the past week. Low Group Belongingness was a significant predictor of lower self-rated oral health and of decreased likelihood of having eaten fresh fruits/vegetables in the past week. Results also indicated that being in the social identity prime condition (reporting on social identity at the beginning of the survey) and being high in Group Belongingness interacted to predict whether respondents currently smoke. Additionally, perceiving that utilization of mental health services was relevant to one’s social group was positively correlated with perceptions related to preventive oral health and physical health behaviors. Conclusions: Several behaviors were related to how strongly individuals identified with their social identity. The overall level of Group Belongingness influenced respondents’ endorsement of their personal engagement with health behaviors related to smoking, oral health, and diet. Implications for Policy, Delivery, or Practice: These findings can inform the development of targeted, culturally sensitive health education and intervention efforts intended to reduce existing health disparities by extending accurate health information and services to hard-to-reach high-risk subpopulations. Primary Funding Source: Walter J. McNerney Award ●Health Services Utilization in Canadian Ethnic Populations Andrew Fong, B.Comm., BA, Hude Quan, M.D., Ph.D., Jianli Wang, M.D., Ph.D., William Ghali, M.D., MPH, Richard Musto, M.D., Tom Noseworthy, M.D. Presented By: Andrew Fong, BA, Senior Research Analyst with the Calgary Health Region, Community Health Science, University of Calgary - Graduate Student, 1403 - 29th Street NW, Calgary, T2N 2T8; Tel: (403) 944-8926; Fax: (403) 9448950; Email: Andrew.Fong@calgaryhealthregion.ca Research Objective: Racial disparities in health care utilization and outcome have been extensively studied in the United States. These studies found that visible minorities have a lower likelihood of receiving effective procedures and certain beneficial medications such as preventive care services and referral to specialists for evaluation. Moreover, visible minorities in the United States are more likely to receive delayed care and/or poorer quality care. In Canada, ethnic differences and related disparities in Canada's health care system have not been studied extensively and is not understood sufficiently. This study assesses the health services utilization in ethnic populations residing in Canada. Study Design: This study analyzed data from the Canadian Community Health Survey (cycle 1.1). This national crosssectional telephone survey collected self-reported ethnicity and utilization of family doctor, specialist and in-hospital stay in the last 12 months and cancer screening test in their life time as of 2001. The sampling weights endorsed by Statistics Canada were used to calculate estimates. Population Studied: Of 131,535 respondents, 3665 (2.8%) aboriginal and 6558 (5.0%) unspecified ethnicity data were excluded. This resulted in a data set that included 7057 visible minority. Of visible minority, 29.9% were Chinese, 0.29% Japanese or Korean, 20.5% South Asian, 13.8% South East Asian, 7.2% West Asian/Arabic, 14.4% Black and 5.9% South American. Principal Findings: Visible minorities had similar frequencies of visit with family doctors with 78.4% of both Caucasion and Visible minorities visiting a family doctor within a 12 month period. In contrast, Visible minorities had lower frequencies of consultations with medical specialist (48.3% vs. 54.7% of Caucasian), lower length of stay in hospital (5.5 vs 8.3 days with Caucasian), lower psa test amongst men aged 40 years and older (30.4% vs 44.7% of Caucasian), lower mammogram and PAS smear test for women aged 35 years and older (53.9% vs. 65.7% of Caucasian) and ( 78.4% vs 90.2% of Caucasian) respectively. Conclusions: The level of health services utilization varies by type of service among Canadian ethnic populations. Visible minorities appear to under-utilize health care that is accessible through physician's referral compared with Caucasians. The reasons for under-utilization of specialty, in-hospital care and cancer screening test in visible minorities should further be studied. Implications for Policy, Delivery, or Practice: Despite Canada's universal health care system, ethnic diversity in health services utilization still exits. Primary Funding Source: No Funding Source ●Heart Disease Risk Factors: Diagnosis Differences Sheila Franco Presented By: Sheila Franco, Staff Fellow, National Center for Health Statistics, CDC, 3311 Toledo Road, Hyattsville, MD 20782; Tel: (301)458-4331; Fax: (301)458-4038; Email: sfranco@cdc.gov Research Objective: Heart disease is the leading cause of death in the United States. Hypertension and high cholesterol are independent risk factors for cardiovascular disease. People with multiple risk factors are at greater risk for heart disease than those with a single risk factor and risk increases as the number of risk factors increase. For those without insurance, these risk factors may go undiagnosed, and therefore untreated, leading to increased morbidity from heart disease. Those without insurance may also be less likely to afford treatment, including drug therapy, even if these conditions are diagnosed. This paper examines multiple heart disease risk factors by age, sex, race/ethnicity, health insurance, and poverty status. Study Design: This analysis used data from the National Health and Nutrition Examination Survey (NHANES). NHANES collects data from physical exams and information on family characteristics during interviews. Bivariate analysis was used to examine multiple risk factors for heart disease. The multivariate analysis is ongoing. Population Studied: Persons age 20 and over are included. A person with undiagnosed hypertension is defined as not being told by a doctor they have hypertension but having measured elevated blood pressure. A person with undiagnosed high serum cholesterol is defined as not being told by a doctor they have high cholesterol but having measured total serum cholesterol greater than or equal to 240 mg/dL. Principal Findings: In 1999-2000, 14 percent of adults aged 20 and over had either undiagnosed hypertension or undiagnosed high serum cholesterol. Of those with high cholesterol, 15 percent were undiagnosed. Of those with hypertension, 30 percent were undiagnosed. Undiagnosed hypertension was more common for those without insurance (35%) than those with some form of coverage (29%). Undiagnosed high cholesterol was also more common for those without insurance (24%) than those with insurance coverage (15%). Among those lacking health insurance coverage, poverty status, gender, and age were not predictors of having undiagnosed hypertension, among those with hypertension. Among those with hypertension but without insurance coverage, undiagnosed hypertension was more common for Mexicans (45%) than black non-Hispanics (37%) and white non-Hispanics (32%). Conclusions: The lack of insurance is related to having undiagnosed high cholesterol or hypertension. Notably, among those with hypertension but without insurance, Mexicans were significantly more likely to undiagnosed than white or black non-Hispanics. Implications for Policy, Delivery, or Practice: Screening for hypertension and high cholesterol is effective in identifying and improving treatment for these conditions. Those lacking health insurance may be less likely to be screened, diagnosed, or treated for these conditions. Treatment of heart disease risk factors can reduce morbidity and health care utilization. If those without health insurance are less likely to be diagnosed with these important heart disease risk factors, then they are also less likely to get treatment for these conditions. This may lead to increased morbidity and health care utilization and costs in later years. Primary Funding Source: CDC ●Ethnic Disparities in Health and Health-Related Behaviors among Homeless Women Lillian Gelberg, M.D., MSPH, Austin Erika, Ph.D., Ronald M. Andersen, Ph.D. Presented By: Lillian Gelberg, M.D., MSPH, George F. Kneller Professor, Department of Family Medicine, UCLA, 50-071 CHS Box 951683, Los Angeles, CA 90095-1683; Tel: (310) 794 6092; Fax: (310) 794 6097; Email: lgelberg@mednet.ucla.edu Research Objective: Limited empirical research has focused on ethnic differences in the health of homeless women. Using a probability sample of homeless women in Los Angeles, we employ the Behavioral Model for Vulnerable Populations to examine the predisposing, enabling, and need factors associated with health and health-related behaviors in this population. Study Design: A community-based probability Sample of 974 homeless women in 66 Los Angeles County shelters and meal programs underwent a one hour structured face-to-face personal interview. Population Studied: Homeless women. Principal Findings: Numerous ethnic differences in the correlates of health and health-behavior exist among homeless women. White women are especially vulnerable to poor health, reporting more gynecological symptoms, limitations on physical functioning, history of drug and alcohol abuse, and history of psychiatric hospitalization. White women’s experience of homelessness is also more severe compared to African Americans and Hispanics; White women had been homeless longer on average and reported more exits from homelessness. No significant ethnic differences exist in key sociodemographic factors including income, health insurance coverage, work status, or receipt of food stamps. Conclusions: The experience of homelessness differs by ethnicity, as do the correlates of health and health-related behaviors. Notably, White women in this population experience poorer health than African American and Hispanic women on a number of measures. These ethnic differences must be considered when using the Behavioral Model for Vulnerable Populations to examine health outcomes. Implications for Policy, Delivery, or Practice: Ethnic disparities may differ in various vulnerable populations. While homeless women of all ethnic backgrounds experience poorer health compared to housed women, our findings suggest that white homeless women experienced poorer health relative to Hispanics and African American women. While most homeless women have health disparities, our findings that white homeless women had the greatest disparity on many measures suggest that this subgroup also needs to be targeted by program planners and policy makers to improve their health and access to care. Primary Funding Source: NIDA, Robert Wood Johnson Foundation, NIAAA, AHRQ ●Inner City Adolescents At Highest Risk of Health Consequences of Obesity Roy Grant, MA, Marian Larkin, M.D., Alan Shapiro, M.D., Sandra Goldsmith, MS RD, Basma Faris, MS RD, Presented By: Roy Grant, MA, Director of Research, Research, The Children's Health Fund, 317 East 64th Street, New York, NY 10021; Tel: (212)535-9400; Fax: (212)535-7699; Email: rgrant@chfund.org Research Objective: Obesity (BMI => 95th percentile) more than doubled from 1980-2000 among children 6-11 years old and tripled for adolescents 12-19. Associated health conditions including type 2 diabetes (T2DM) and hypertension also increased. Black and Hispanic children and youth are disproportionately affected. Adult obesity, T2DM and cardiovascular disease (CVD) are more firmly associated with adolescent than childhood obesity. Our objective was to refine a protocol to target patients at highest risk for health consequences of obesity for weight management interventions. Using this protocol, we sought to describe the characteristics of this highest risk group, for whom weight management intervention would be medically necessary. Study Design: An algorithm was developed for use at comprehensive physical exams to identify these risk factors: race-ethnicity, family history, BMI, physical findings, lab results. Identified patients were referred for further lab testing, nutrition counseling, and endocrinology consultation if needed. Only patients Tanner II or higher and age 12-19 were included to describe patients at the highest risk. Data quality was checked by retrospective chart review. Population Studied: Based on retrospective chart review of a random sample of 200 patients who had a comprehensive physical examination between June 1 and December 31, 2003, prevalence among patients age 6-19 years in our predominantly Hispanic South Bronx Health Center is 19% overweight (BMI 85th to 94th percentile) and 25% obese (BMI at or above 95th percentile). With 2,226 patients 6 to 19 years old, this indicates that approximately 1,000 are at risk of overweight, obesity, and related health consequences. Principal Findings: For the first 75 identified patients: Demographics, 71% Hispanic, 29% Black; 56% male; mean age, 14.7 years; BMI: 91% obese, 9% overweight, mean, 33.5; Other risk factors: 87% family history of diabetes; 70% acanthosis nigricans; 35% dyslipidemia; 24% elevated blood pressure (BP). On chart review, nutrition notes were found in 48% of charts. Dyslipidemia and elevated BP had been underidentified by about half. Conclusions: In an inner city community health center, prevalence of pediatric overweight and obesity is high. To make better use of scarce resources, a protocol to identify patients at the most immediate risk is useful. This protocol is effective in getting high risk patients to a nutritionist and identifying patients with insulin resistance and incipient CVD. The prevalence of obesity with complications suggests that weight management interventions are medically necessary for these patients. Implications for Policy, Delivery, or Practice: For practice: primary care providers should consistently reference lab results received after the visit in determining patient risk status. BP readings should be consistently checked for ageappropriate norms. For policy: the profile of patients at the highest risk of T2DM and CVD identified in this population may serve as the basis for a diagnostic entity of “adolescent obesity syndrome” for which nutrition counseling and other weight management services should be reimbursed as medically necessary. The short-term increase in health expenditures is anticipated to be small in relation to the eventual savings achieved by preventing early onset diabetes and heart disease. Primary Funding Source: Bristol-Myers Squibb ●Racial Differences in Attitudes Toward Innovative Medical Technology Peter Groeneveld, M.D., MS, Seema S. Sonnad, Ph.D., Anee K. Lee, BA, David A. Asch, M.D., MBA, Judy A. Shea, Ph.D. Presented By: Peter Groeneveld, M.D., MS, Assistant Professor of Medicine, Center for Health Equity Research and Promotion, Philadelphia VA Medical Center, 3900 Woodland Ave, Philadelphia, PA 19104-4155; Tel: (215) 898-2569; Fax: (215) 573-8779; Email: peter.groeneveld@med.va.gov Research Objective: Patient "innovativeness," defined as the propensity to adopt and use new technology, is likely to be an important component of healthcare decision-making. Our goal was to measure differences in innovativeness between black and white patients. Pronounced racial variation in attitudes may explain differences in both patient preferences for particular technologies and in utilization rates. Study Design: We constructed a self-administered survey instrument that combined previously validated survey components for general innovativeness (i.e. 6 questions about patients' attitudes toward new ideas and ways of living) and content-specific innovativeness (i.e. 5 questions regarding patients' attitudes toward medical technology). We also presented a brief vignette describing a hypothetical implantable medical device, and we subsequently asked a series of 8 questions about patients' reactions to the technology. All questions were in Likert scale format. Population Studied: The survey was administered to a convenience sample of 81 primary care patients (50 black, 31 white) at the Philadelphia Veterans Affairs Medical Center. Principal Findings: There were no significant differences in age (mean 55, range 32-85), educational attainment, and prior exposure to medical technology between white and black respondents, although whites reported higher incomes. Cronbach's alpha was 0.62 for the six general innovativeness questions, 0.59 for the five content-specific innovativeness questions, and 0.72 for the eight vignette questions. The overall Cronbach's alpha was 0.82 for the entire instrument, indicating high overall consistency. With responses scaled from 0 (resistant to innovation) to 4 (highly innovative), there was no racial difference in general innovativeness (blacks: 2.3, whites: 2.3, p=0.86). However, whites had greater innovativeness in regard to medical technology (blacks: 2.2, whites: 2.6, p=0.01). We found no racial differences in attitudes toward use of the hypothetical medical device presented in the vignette (blacks: 2.5, whites: 2.4, p=0.39). The response of black patients to the specific technology in the vignette was significantly more innovative (p=0.04) than their response to medical technology in general. Conclusions: There were no measurable differences between white and black veterans in their attitudes toward new ideas or ways of thinking, yet white veterans were more favorably disposed toward new medical technology. The lower level of healthcare-technology-specific innovativeness among blacks surprisingly did not result in a more negative response by blacks to a hypothetical example of a new implantable medical device. Implications for Policy, Delivery, or Practice: Blacks and whites respond differently to innovative medical technology. The lack of a racial difference in the response to the vignette might have been due to the manner in which the technology was presented, which may have allayed concerns and encouraged greater innovativeness among black respondents. Primary Funding Source: VA ●Primary Care for Low-Income Populations: A Comparison of Health-Care Delivery Systems Ellie Grossman, M.D., Anna T.R. Legedza, Sc.D., Christina C. Wee, M.D., MPH Presented By: Ellie Grossman, M.D., Fellow, Div of General Medicine and Primary Care, Beth Israel Deaconess Medical Center, 330 Brookline Avenue, Rose 105, Boston, MA 02215; Tel: (617) 667-1960; Fax: (617) 667-2751; Email: egrossma@hsph.harvard.edu Research Objective: In an effort to cut health-care costs, some states have considered shifting primary care for lowincome populations from hospital-based practices to community health centers (CHCs). To explore ramifications of these proposals, we examined quality measures at different types of primary-care sites. Study Design: This study is a secondary analysis of the 20002002 National Health Interview Survey (NHIS). We described low-income patients (pts) who receive primary care at hospital clinics, physician (MD) offices or HMOs, or CHCs, and compared 1) emergency-room (ER) visits; 2) delays in medical care due to office/clinic constraints (appointment availability, office wait time, and accessibility of scheduling staff), and 3) influenza and pneumococcal vaccinations. Multivariable logistic regression models adjusted for age, sex, race/ethnicity, education, language, region, employment, insurance, transportation accessibility, and illness burden (self-reported health status, hospitalizations and office visits, comorbidities and disabilities, mood disturbances and need for mental health care). All analyses were performed using SUDAAN and were appropriately weighted to account for the complex sampling. Population Studied: Adult NHIS participants with family income less than 200% of the poverty threshold (n = 38,329). Principal Findings: More than half of our sample (59%) received primary care at an MD office or HMO, while 20% went to a CHC and 3% to a hospital clinic; 18% did not identify any of these three sites as a source of primary care. There were significant demographic differences between the pts at the three site types (p<.001 for all comparisons). The mean pt age was 49 years (y) at MD offices / HMOs, 48y at hospital clinics, and 41y at CHCs; 31% of MD office / HMO pts were racial minorities, vs. 61% of hospital-clinic pts and 48% of CHC pts. Only 13% of MD office / HMO pts were uninsured - compared to 29% of hospital-clinic pts and 33% of CHC pts. Hospital-clinic pts were more likely to have a higher illness burden. We found significant differences across sites for our quality measures of interest – even after adjustment for sociodemographic and health-status factors. Hospitalclinic pts were more likely to report > 1 ER visit in the past year than CHC pts (OR 1.8; 95% CI 1.4, 2.3) or MD office / HMO pts (OR 1.9; 95% CI 1.5, 2.4). However, hospital-clinic pts were no more likely to report a delay in care than pts at CHCs (OR 1.2; 95% CI 0.9, 1.6). Hospital-clinic pts were more likely than CHC pts to be vaccinated for influenza (OR 1.3; 95% CI 1.1, 1.7) or pneumococcus (OR 1.4; 95% CI 1.1, 1.8); vaccination rates at MD offices / HMOs were similar to those at CHCs. Conclusions: Our results suggest that no one type of primary care site delivers clearly higher quality care for low-income populations. Further studies will need to examine additional quality indicators. Implications for Policy, Delivery, or Practice: Quality issues should be considered as we decide how best to deliver care to vulnerable populations. Primary-care sites which may be perceived as ‘low-cost’ may actually deliver mixed-quality care. Primary Funding Source: HRSA ●Racial Differences in Hospice Use Among Non-Hispanic Blacks and Whites Beth Han, M.D., Ph.D., MPH, Robin Remsburg, Ph.D. Presented By: Beth Han, M.D., Ph.D., MPH, Health Scientist, Centers for Disease Control and Prevention, National Center for Health Statistics, 3311 Toledo Road, Hyattsville, MD 20782; Tel: (301)458-4137; Fax: (301)458-4032; Email: hih9@cdc.gov Research Objective: Despite many benefits, hospice appears to be underutilized. We examined differences in hospice use rates among younger and older non-Hispanic Blacks and Whites between 1991 and 2000 and investigated racial differences in hospice patient characteristics. We tested differences in length of hospice survival between hospice enrollment and death in hospice among non-Hispanic Blacks and Whites. Study Design: Series of cross-sectional studies using the 1991-2000 annual Underlying and Multiple Cause-of-Death Files and the 1992-2000 National Home and Hospice Care Surveys. Chi-Square tests, linear regression methods, the Kaplan-Meier method, and Cox proportional hazards models were used. Population Studied: We examined data from the 1991-2000 annual Underlying and Multiple Cause-of-Death Files, providing cause-of-death information reported by all 50 states and the District of Columbia from 1991 to 2000. We also investigated 19,547 hospice patients from the 1992, 1994, 1996, 1998, and 2000 National Home and Hospice Care Surveys, which provide nationally representative data on U.S. home and hospice care agencies and their patients. Principal Findings: Hospice use rates doubled for nonHispanic Whites and tripled for non-Hispanic Blacks between 1991 and 2000. In 1999/2000, differences in hospice use rates between younger non-Hispanic Whites and Blacks diminished, whereas differences between elderly non-Hispanic Whites and Blacks increased. Non-Hispanic Black hospice patients were more likely to be younger; have Medicaid-only; have HIV/AIDS; and to be referred by hospitals than their White counterparts. In 1999/2000, 25% of non-Hispanic Whites and 25% of non-Hispanic Blacks died within 7 days after hospice enrollment. After adjustment for covariates, non-Hispanic Black and White hospice patients had similar length of hospice survival between 1991 and 2000. Conclusions: Hospice use rate for elderly non-Hispanic Blacks was at least 9% lower than for elderly non-Hispanic Whites in 1999/2000. Despite differences in hospice patient characteristics, non-Hispanic Blacks and Whites had similar length of hospice survival during the 1990s. Many patients who entered hospice care did so late in the trajectory of their terminal illnesses. Implications for Policy, Delivery, or Practice: Future research is needed to understand why hospice use rate for elderly non-Hispanic Blacks was at least 9% lower than for elderly non-Hispanic Whites in 1999/2000. Hospice agencies should understand characteristic differences between nonHispanic Black and White hospice patients in order to address their needs more sensitively and effectively. Strategies are needed to improve length of hospice survival among both non-Hispanic White and non-Hispanic Black hospice patients. Primary Funding Source: CDC ●Racial and Ethnic Disparities in Access to Vision Care among Children with Special Health Care Needs in the United States Kevin Heslin, Ph.D., Richard S. Baker, M.D., Magda Shaheen, M.D., Ph.D., Richard Casey, M.D. Presented By: Kevin Heslin, Ph.D., Assistant Professor, Research Centers in Minority Institutions, Charles R. Drew University of Medicine and Science, 1731 East 120th Street, Los Angeles, CA 90059; Tel: (310)761-4726; Fax: (310)631-1495; Email: keheslin@cdrewu.edu Research Objective: All children should receive periodic vision screening and, if indicated, vision care services to address impaired functioning. The purpose of this study was to examine racial and ethnic disparities in access to vision care using secondary survey data on a representative sample of children with special health care needs (CSHCN) in the United States. Study Design: The National Survey of Children with Special Health Care Needs was a cross-sectional survey conducted from October 2000 to April 2002. A random-digit-dial sample of households with children under age 18 was selected from the 50 states and the District of Columbia. Respondents were parents or guardians who knew the most about the index child’s health. Unmet need for vision care was assessed by asking, “During the past 12 months, was there any time your child needed eyeglasses or vision care?” and then: “Did your child receive all the eyeglasses or vision care that he or she needed?” If the respondent answered “yes” to the first question and “no” to the second, the child was categorized as having unmet need for vision care. We used multivariate logistic regression to estimate the independent association of race and ethnicity with unmet need. Control variables included child gender, age, disability status, insurance coverage, illness severity, mother’s educational achievement, cultural competence of the child's primary care physician (as perceived by the respondent), and a count variable of unmet needs for other types of health services that ranged from 0 to 13. Odds ratios (ORs) and 95% confidence intervals (CIs) were calculated. The Stata software program was used to estimate population prevalence parameters and, in the multivariate analysis, to adjust standard errors for the complex survey sampling design. Population Studied: 14,070 children with special health care needs. Principal Findings: Of the estimated 3,321,870 CSHCN represented in this analysis, 6% had unmet need for vision care. Approximately 5% of whites had unmet need, compared with 9% of African Americans, 10% of Latinos, 14% of multiracial children, and 8% of children of “other” racial and ethnic backgrounds (p<0.0001). Multivariate analysis showed that, compared with whites, African Americans had twice the odds (OR = 2.01; 95% CI = 1.37, 2.96) and children of multiracial backgrounds had three times the odds (OR = 3.06; 95% CI = 1.62, 5.75) of having unmet need for vision care. Latino children and those of “other” racial and ethnic backgrounds did not differ from whites in the multivariate analysis. Conclusions: Outreach programs should target CSHCN in underserved racial and ethnic minority communities to reduce disparities in access to vision care. Primary Funding Source: AHRQ ●Rural/Urban Differences in Access to Health Care: Does Universal Coverage Reduce Inequalities in Health? Nicole Huang, Ph.D., Winnie Yip, Ph.D., Hong-Jen Chang, M.D., MS, MPH, Yiing-Jenq Chou, M.D., Ph.D. Presented By: Nicole Huang, Ph.D., Assistant professor, Department of Health Education, National Taiwan Normal University, 162 Heping East Road, Section 1, Taipei, 106; Tel: 886-2-23636880 x220; Fax: 886-2-23630326; Email: nhuang@cc.ntnu.edu.tw Research Objective: Rural-urban disparities in access to health care have always been a focus of concern. Considerable literature has documented that rural residents are at especially high risk of inadequate and delayed access to health care due to both demand-side and supply-side factors. Some speculate that introduction of a single-payer health-care system, which has monospony power to take care of both demand and supply issues, may substantially reduce ruralurban health disparities. However, whether a single-payer universal coverage eliminates disparities in access to care among rural population remains unknown. The objective of this paper is to compare the changes in rates of ruptured appendicitis between rural and urban residents in Taiwan from 1996 to 2001. As ethnic disparity in access to care under the NHI program is also a focus of rural health policy, we also conducted additional analyses on disparities between aborigine and non-aborigine populations. Study Design: Ruptured appendicitis was used as an indicator of access-induced health outcome. The NHI hospital discharge ICD-9-CM codes were used to define hospitalization for ruptured (ICD-9-CM code 540.0 and 540.1) and non-ruptured appendicitis (ICD-9-CM codes 540.9). Of 309 townships in Taiwan, 30 mountainous areas are proclaimed “rural areas.” The patients living in these 30 mountainous towns were identified as rural residents while the patients living in other areas were identified as urban residents. Other variables such as age, gender, aborigine status, socioeconomic status, health status, and hospital characteristics were also included in the analyses. Population Studied: The NHI enrollment files, hospital discharge data, and the household registry were three main data sources. We identified all 128,930 patients undergoing appendectomy for which either a normal or perforated appendix was the principal diagnosis in Taiwan between 1996 and 2001. Principal Findings: During the first 3 years under the NHI program, although the differences between the rural and urban areas were apparent, the differences were narrowing. As the downward trends continued, in looking at the trends since 1999, we found very few discernible differences between the rural and urban areas. After adjusting for demographic, SES, health status, and hospital characteristics, the ruptured rate among rural residents was decreasing significantly faster (1.1%) than that among urban residents over time. More specifically, the children showed a significantly steeper narrowing trend (3.4%) in the rural-urban disparities under the NHI program than adults. Furthermore, unlike the significant gap narrowing observed between rural and urban areas, the pace of reduction in ruptured rate among aborigine people was only 0.5% faster than that among non-aborigine people and the difference was not significant. Conclusions: Our findings demonstrate the significant narrowing of health disparities between rural and urban populations since the implementation of the NHI program. In particular, of all age groups, the most dramatic narrowing of the gap was observed among children after adjusting for a variety of patient and hospital characteristics. Implications for Policy, Delivery, or Practice: In conclusion, while many countries are discussing the option of single-payer universal coverage system, our findings add new knowledge in that effectiveness of single-payer universal insurance program ameliorates rural-urban disparities in health and provide an important reference to their discussion. Primary Funding Source: Other, National Health Research Institute and National Science Council ●Reducing Disparities in Healthcare Access: The CostEffectiveness of Non-Emergency Medical Transportation Paul Hughes-Cromwick, BS, MA, Ph.D. Candidate, Richard R. Wallace, BS, MS, Ph.D. Candidate, Hillary J. Mull, BA, MPP Presented By: Paul Hughes-Cromwick, BS, MA, Ph.D. Candidate, Senior Analyst, Health Solutions Division, Altarum Institute, 3520 Green Court, Ann Arbor, MI 48105; Tel: (734)302-4616; Fax: (734)302-4994; Email: paul.hughescromwick@altarum.org Research Objective: We hypothesize that that improving access to healthcare for the transportation-disadvantaged population will lead to improved quality of life, potential enhancements in life expectancy, and a decrease in health costs nationally. This decrease may exceed the incremental increase in transportation costs. Study Design: Millions of Americans are considered to be “transportation disadvantaged.” Members of this population, due to low income, physical or mental disability, inability to drive, or some other reason, cannot transport themselves or are unable to purchase transportation services. This dependency reduces access to essential healthcare services. In some cases this access disparity leads to lost opportunities for early detection or decreases in health status. The Transportation Research Board of the National Academies of Science launched the project, “Cost Benefit Analysis of Providing Non-Emergency Medical Transportation.” Arising from this project, the current study estimates the size of the transportation-disadvantaged population that misses care due to a lack of non-emergency medical transportation (NEMT), and analyzes the cost-effectiveness of providing the missed transportation in terms of improved health status (measured as quality adjusted life years, or QALYs) relative to increased transportation costs. Cost-effectiveness is demonstrated two different ways: (1) at a macroscopic level and (2) at a microscopic level for two critical conditions that affect the transportation disadvantaged: asthma and heart disease. Population Studied: This is a nationally representative study of those we estimate to be transportation-disadvantaged relative to accessing healthcare. We identify relevant individuals using multiple years of the National Health Interview Survey and the Medical Expenditure Panel Survey. Principal Findings: Our results indicate that at least 3.6 million Americans miss medical care due to a lack of transportation in a given year. They are disproportionately female, poorer, and older; have less education; and are more likely to be minorities than those who do not miss care due to a lack of NEMT. While adults who miss care are spread across urban and rural areas like the general population, children lacking transportation are more concentrated in urban areas. These 3.6 million suffer from co-morbidities at a much higher rate than do their peers. Many of the conditions they face, however, can be managed if appropriate care is made available. Based on our macroscopic cost-effectiveness analysis, we found that only small health benefits (about 1/50th of a QALY per person) are needed to balance the added costs; furthermore, at the microscopic level, we found that providing missing NEMT to asthma and heart disease patients is highly cost effective. Conclusions: Based on our findings, we see great promise for net societal benefits from improving the quality of life of this population by increasing its access to transportation. Implications for Policy, Delivery, or Practice: We recommend modifications to national healthcare and transportation data sets to allow more direct assessment of the magnitude of this problem and of the benefits that could be achieved by remedying it. We believe that transportation adds a novel dimension to health services research on healthcare access and disparities. Primary Funding Source: Transportation Research Board of the National Academies of Science ●Quality of Hospital Care among Hispanics: Does primary language make a difference? Margarita Hurtado, Ph.D., MHS, January Angeles, MPP Presented By: Margarita Hurtado, Ph.D., MHS, Principal Research Scientist, American Institutes for Research, 10720 Columbia Pike, Silver Spring, MD 20901; Tel: (301) 592-2215; Fax: (301) 593-9433; Email: mhurtado@air.org Research Objective: To determine whether the quality of hospital care reported by Hispanic patients differ according to the primary language they speak, with an emphasis on communication-related aspects of service delivery. Study Design: We derived patients’ primary language using two variables: (1) primary language spoken at home; and (2) language in which the questionnaire was administered. When language indicated for both variables was the same, that language was chosen as the respondent’s primary language. In cases where the language indicated differed, individuals were designated as bilingual. We conducted regression analyses of responses to the HCAHPS survey on quality of hospital care controlling for potential confounders, including age, sex, education, overall health status and admission status (medical, surgical, and obstetrics). We also accounted for correlated error by including the hospital as a random effect in mixed effects models. Population Studied: The study sample includes 1,806 Hispanics who had an inpatient hospital stay. Data were collected in three states – Arizona, Maryland, and New York – through the HCAHPS pilot test. Of the entire sample, 80% were female, almost half (48%) were between the ages of 18 to 34, one-third (29%) did not graduated from high school, and only 14% were college graduates. Forty-four percent were identified as primarily English-speaking, 32% primarily spoke Spanish, and 23% were bilingual. Principal Findings: Quality of hospital care reported by Hispanic patients did not differ significantly by language group for any of the HCAHPS composite measures (communication with nurses, communication with doctors, communication about medication, nursing services, discharge information, pain control and physical environment). Global ratings of nurses, physicians, and the hospital also did not show any significant differences. Analyses of individual item analysis, however, revealed significant differences between language groups for an important component of physicianpatient communication: providing explanations that are easy to understand. Those who spoke Spanish as their primary language were significantly less likely than those who primarily spoke English to report that doctors explained things in a way they could understand (p=0.02). Both Spanish-speaking and bilingual Hispanics were less likely than English-speaking Hispanics toi report having nurses explain things clearly to them, but the difference was only significant for bilingual Hispanics (p=0.01). There were no significant differences with respect to having doctors or nurses listen carefully to them. Conclusions: This study suggests that those who do not speak English as their primary language experience greater difficulty communicating with clinicians than their Englishspeaking counterparts. With respect to other aspects of care, Hispanic patients report similar experiences with the quality of their hospital care regardless of the language they predominantly speak. Implications for Policy, Delivery, or Practice: This study points out an important component of care that hospitals need to examine and improve in order to provide better care to non-English speaking patients. Further work is needed to define the most effective ways of doing so. Primary Funding Source: AHRQ ●Health Related Quality of Life and Direct Medical Care Cost of Prostate Cancer Patients Ravishankar Jayadevappa, Ph.D., Bernard S. Bloom, Ph.D., Sumedha Chatre, Ph.D., Kenneth M. Fomberstein, S. Bruce Malkowicz, M.D. Presented By: Ravishankar Jayadevappa, Ph.D., Research Assistant Professor, Department of Medicine, University of Pennsylvania, Room # 224, 3615 Chestnut Street, Philadelphia, PA 19104; Tel: (215)898-3798; Fax: (215)573-8684; Email: jravi@mail.med.upenn.edu Research Objective: Introduction and Objective: Multiple factors (demographic, clinical, social, economic and environmental) influence the medical care cost and health related quality of life (HRQoL) of patients with prostate cancer (PCa). It is important to assess the factors associated with variations in health resource utilization, costs and their relationship to outcomes for effective management and policy decision. We evaluated generic and prostate-specific HRQoL and direct medical care cost for men with PCa. Study Design: Methods and Statistical Analysis: We conducted a prospective cohort study of newly diagnosed PCa patients. Additionally, we recruited matched controls (cancer free) from same hospitals. All cases completed SF-36 and UCLA-PCI surveys prior to treatment, and at 3, 6, 12 and 24 months after surgery. Controls completed surveys at baseline only. Direct medical care cost (DMC) data were obtained from a hospital based administrative database and clinical data were obtained via structured medical chart review. Demographics and HRQoL were compared using T-test, Fisher Exact and Chi-sq. Wilcoxon and log-T tests were used to compare DMC. Multivariate regression models were used to assess incremental cost of PCa and the predictors of 24 months PCa specific HRQoL. Population Studied: Newly diagnosed PCa patients, recruited from the Urology clinics of a large academic health care system and VA hospital. Principal Findings: Results: We recruited total of 521 PCa patients and achieved a retention rate of 85%. PCa patients showed significant variations in baseline characteristics, treatment pattern and HRQoL by hospitals, age and ethnicity. For PCa patients who had 24 months follow-up, mean annual medical care cost was $4,160 for the treatment year and mean length of stay was 3.5 days. Baseline physical function for cases was 9 points higher than controls (72.6 vs.61: p =.0107) and score on bodily pain was higher, indicating lower pain (91.5 vs. 76.9 p=.0054). For baseline prostate specific HRQoL (UCLA- PCI), cases had better functions on sexual function (71.5 vs 48.7 p=.0009), bowel bother (96.9 vs 86 p=.0160) and sexual bother (89.1 vs. 69.4 p=.0160). At 12 months post treatment, cases had generic HRQoL similar to their baseline values and those of controls for all domains. Urinary function (80.1 vs.93.9: p .0019), sexual function (39.4 vs. 71.5: p<.0001), urinary bother (83.1 vs. 94.1: p.0319) and sexual bother (35.5 vs. 89.1: p<.0001) were lower at 12 months for cases than baseline values, while rest of the PCI domains were comparable. At 24 months of post treatment, generic HRQoL of cases returned to their baseline values. Urinary function (77.2 vs. 93.9: p=.0014), sexual function (42.7 vs. 71.5: p=<.0001), and sexual bother (41.1 vs. 89.1: p<.0001) were lower and rest of the PCI domains were comparable. In a multivariate log-linear regression, marital status was a significant predictor of sexual, urinary and bowel functions at 24 months. Conclusions: Conclusions: PCa patients reported weaker sexual function, urinary function and sexual bother at 24 months post treatment compared to their baseline values. Baseline characteristics, treatment pattern and HRQoL vary across age, ethnicity and hospital settings. Implications for Policy, Delivery, or Practice: There exists a significant opportunity for improving HRQoL of men with PCa that requires multisystem approach. Primary Funding Source: Department of Defense ●What Happens Ehen You Leave? Outcomes of Patients who Leave Hospital Against Medical Advice Yan Jin, MA, Donald Schopflocher, Ph.D. Presented By: Yan Jin, MA, Project Consultant, Alberta Health and Wellness, 22nd Floor, TPNT, 10025 Jasper Avenue, Edmonton, T5J 2N3; Tel: (780)415-0210; Fax: (780)422-2880; Email: yan.jin@health.gov.ab.ca Research Objective: Although many studies have been conducted on patients leaving hospital against medical advice (AMA), few examined mortality as an outcome of AMA discharge. The purposes of our retrospective study used a large-scale dataset to identify patient’s characteristics associated with AMA discharge and compare not only readmission but also mortality rates between patients with AMA and formal discharges. Study Design: The data used in this study are from the Canadian Institute for Health Information’s (CIHI) Inpatient Discharge Abstract Database (DAD) for Alberta and from the Alberta Health Care Insurance Plan (AHCIP) Registry File. A large range of variables related to patients’ characteristics, socio-demographics, Charlson comorbidity index, substance abuse, and admission category were included. Data linkage was conducted to obtain death status and the defined variables. We applied logistic regression and Cox proportional hazard models in the analysis. Population Studied: We defined the study cohort as index discharges or the first discharges in 2000/01 from all Alberta acute hospitals for Alberta residents over age 18 who left hospital alive. Principal Findings: Of the 343,309 hospital discharges, 171,043 met our selection criteria. Of these, 169,163 were formal discharges with: an average length of stay (ALOS) of 6.2 days, mean age of 50 and 63.7% female. In contrast, there were 1,880 AMA discharges with: an ALOS of 4.6 days, mean age of 42 and 44.9% female. The odds ratios for AMA discharge were 1.25 for patients younger by 10 years, 1.58 for males, 2.59 for patients on welfare, 4.05 for First Nation patients, 1.65 for patients living alone, 2.59 for patients with elective admission via emergency department or ambulance, 5.45 for patients with urgent/emergency admission, 3.36 for patients with drug related diagnosis, and 2.96 for patients with alcohol related diagnosis. Within one year of index discharge, AMA discharged patients had 49% higher risk of being readmitted to hospital and 26% greater risk of death, compared to patients formally discharged. Conclusions: Leaving hospital AMA is associated with: (1) being younger, male, First Nations or on welfare; (2) living alone; (3) having substance abuse problems; and, (4) having an urgent/emergency admission. Patients leaving hospital AMA are at greater short-term risk of adverse outcomes including readmission and death. Implications for Policy, Delivery, or Practice: Aappropriate intervention strategies for patients leaving hospital AMA could improve spending in the health care system and the health status of individuals. Primary Funding Source: No Funding Source ●Ethnicity and Other Social Determinants in Pap Testing Among Canadian Immigrant Women Arminee Kazanjian, Dr.Sc., Alice Chen, MC, MS, Arminee Kazanjian, Dr.Sc. Presented By: Arminee Kazanjian, Dr.Sc., Professor, Health Care & Epidemiology, University of British Columbia, 5804 Fairview Avenue, Vancouver, BC, V6T 1Z3; Tel: (604)8224618; Fax: (604)822-4994; Email: a.kazanjian@ubc.ca Research Objective: Many studies reported that ethnic minorities and immigrants in North America are less likely to receive Papanicolaou (Pap) smears, a recommended screening test for cervical cancer. At the same time, there is also evidence that some of these groups experience higher rates of cervical cancer incidence and mortality. The underutilization of Pap screening by immigrants and minority groups is of particular concern in the province of British Columbia (BC), Canada where 26% of its population in 2001 were immigrants. Moreover, more than one-third of these immigrants arrived within the previous ten years and the predominant majority of them are of non-European origins. The objectives of the present study are: (1) To compare the rates of Pap testing among recent immigrants of different ethnic origins in BC (2) To examine the socio-demographic factors that affect the probability of Pap testing among immigrant women Study Design: This study is a retrospective analysis of administrative databases. A database of immigrants who landed in Canada in 1985-2000 and destined for BC was linked to the province’s administrative health databases as part of a national immigrant health project. The control group was randomly selected from the general population of BC and individually matched to the immigrants by sex, age and health region. Receipt of Pap testing was estimated from the physicians’ claims for service database for the years 19992001. Socio-demographic factors examined were marital status, educational level and the ability to communicate in English. Population Studied: The study population consists of women between the ages of 18 and 69 and enrolled in BC’s health plan for any time in 1999-2001. Six subgroups of immigrants were selected for this study based on their place of birth: those from China, South Asia, Philippines, Western Europe, South and Central America and the USA. A total of over 100,000 immigrant women were included. Principal Findings: All subgroups of immigrants were less likely than the control group to receive Pap testing, with an overall odds ratio of 0.46. Ethnic differences were significant, with South Asian, Chinese and Filipino women showing the lowest probability of receiving Pap tests. All the sociodemographic factors studied were found to have an effect on the probability of Pap testing among immigrant women. Conclusions: Immigrant women are less likely to receive Pap testing than the non-immigrant population. The difference is especially profound for ethnic minority immigrant women. Marital status, education and English ability all contribute to the probability of Pap testing in immigrant women. Implications for Policy, Delivery, or Practice: Given the risk for advanced stages of cervical cancer when screening services are not received, targeted efforts are necessary to increase the utilization of Pap testing by Asian immigrant women. Primary Funding Source: Canadian Population Health Initiative ●Cancer Risk Perception and Preventive Screening by Women of Diverse Populations Sue Kim, Ph.D., MPH, Sabrina Wong, Ph.D., RN, Celia Kaplan, Dr.PH, Judith Walsh, M.D., MPH, George Sawaya, M.D., Eliseo Pérez-Stable, M.D. Presented By: Sue Kim, Ph.D., MPH, Postdoctoral Scholar, Medicine, University of California, San Francisco, 3333 California Street, Suite 335, San Francisco, CA 94143; Tel: (415)502-4078; Fax: (415)502-8291; Email: sekim@medicine.ucsf.edu Research Objective: Inaccurate perceptions of risk compromise informed decision-making and may have important behavioral and psychological consequences. Few studies have addressed if ethnic differences in cancer risk perception exist. This study examines the perception of breast, cervical, and colorectal cancer risk and compare the actual risk and screening behavior of a sample of women from various ethnic groups. Study Design: A sample of women, aged 50 to 80, who have made a visit to a primary care physician in the past two years were recruited from ambulatory practices. Trained interviewers administered an initial screening telephone survey and a follow-up in-person interview in English, Spanish or Chinese. Women’s risk perception was examined using different response formats (e.g. numerical scales, word scales, and assessment of cancer risk relative to other risks). Multivariate regression models examined ethnic differences in risk perception and screening, controlling for education, age, income, previous cancer history, and family history of cancer. Population Studied: 536 women completed the survey: 282 non-Latino White (52.6%), 72 African-American (13.4%), 81 Latina (15.1%), and 101 Asians (18.1%). Principal Findings: Latina perceived themselves to have the highest risk for getting cancer (estimating their lifetime risk to be 37.1%), compared to African-American (29.8%), White (21.0%), and Asian (22.0%) (P<.01). Multivariate results showed that compared to White women, Latina women perceived higher risk of cervical (OR, 2.08; 95% CI, 1.14-4.15) and colorectal cancer (OR, 2.49; 95% CI, 1.36-4.56). African American perceived higher colorectal cancer risk (OR, 2.20; 95% CI, 1.21-3.98) and Asian women perceived lower breast cancer risk compared to White women (OR, 0.48; 95%CI 0.260.89). Having a college degree was related to a lower cervical cancer risk perception (OR, 0.45; 95% CI, 0.26-0.89) and family history of cancer was related to higher breast (OR, 2.56; 95% CI, 1.70-3.83) and colorectal cancer risk perception (OR, 1.91; 95% CI, 1.27-2.88). In regards to cancer screening, there were no differences in cervical and breast cancer screening rates. Higher percentages of Latina (15.00%) and Asian (17.82%) women never had any colorectal cancer screening compared to White women (11.39%) (P<.01). Conclusions: All women did not have an accurate understanding of their cancer risk. Yet, ethnic differences persisted in cancer risk perception even after controlling for education, age, income, and cancer history (self and family). Having a higher risk perception was not directly related to higher screening rates. We are currently collecting more data to run detailed analyses comparing the four ethnic groups. Implications for Policy, Delivery, or Practice: It’s important to consider ethnic differences when communicating with patients about cancer risk. It appears that there is a difference in cancer risk perception among women and may reflect their screening behavior. When clinicians communicate with patients about risk information, the traditional percentage and numeracy information may not be as effective in all diverse populations. Primary Funding Source: AHRQ ●The Role of Medical Education in Reducing Health Care Disparities: the Drew/UCLA Medical Education Program Michelle Ko, M.D., Ronald Edelstein, EdD, Kevin Heslin, Ph.D., LuAnn Wilkerson, EdD, Lois Colburn, Kevin Grumbach, M.D. Presented By: Michelle Ko, M.D., Internal Medicine Resident, Internal Medicine, UCLA Center for Health Sciences, 16-155 CHS, 10833 LeConte Avenue., Los Angeles, CA 90095; Tel: (310)825-8307; Email: jassmine@ucla.edu Research Objective: The Drew/UCLA Medical Education Program selects students for their demonstrated commitment to underserved areas. Students receive basic science instruction at UCLA and complete their required clinical rotations in South Los Angeles, an impoverished urban community. We examined the association between graduation from Drew/UCLA and subsequent practice in a medically underserved area, incorporating the potential confounding predictors of student demographics, socioeconomic status markers, and specialty choice. Study Design: A retrospective cohort study. Population Studied: Graduates of the UCLA School of Medicine and the Drew/UCLA Medical Education Program from 1985-1995, in active practice, with a self-reported mailing address in California from the American Medical Association (AMA) Physician Masterfile. Principal Findings: Twenty-nine percent of all graduates studied are practicing in medically underserved areas. Fiftythree percent of Drew/UCLA graduates are practicing in underserved areas, in comparison to 26.1% of UCLA graduates. In multivariate analyses, only underrepresented minority race/ethnicity (OR: 1.572; 95% CI: 1.096-2.255) and participation in the program (OR: 2.466; 95% CI: 1.586-3.832) were predictive of practice in underserved areas. Conclusions: Physicians who participated in the Drew/UCLA Medical Education Program are more likely to practice in underserved areas than those who completed a traditional medical school curriculum. This may be attributed to the selection of committed students, as confirmed by the association of race/ethnicity and practice. Our results also indicate an independent program effect, perhaps by providing a supportive learning environment in a medically underserved urban community. Implications for Policy, Delivery, or Practice: Investment in the development of medical education programs targeting underserved areas can help to alleviate disparities in health care delivery. Primary Funding Source: National Center on Minority Health and Health Disparities ●A Provider-Friendly Screening Tool to Identify Patients Who Lack Physician Trust David Kuykendall, Ph.D., MBA, Michael Kallen, Ph.D., MPH Presented By: David Kuykendall, Ph.D., MBA, Director, METRIC, Department of Veterans Affairs, VAMC (152), 2002 Holcombe Boulevard, Houston, TX 77030; Tel: (713) 794-8514; Email: david.kuykendall@med.va.gov Research Objective: To develop an easy-to-use screening tool for the identification of primary care patients who enter a medical encounter with low physician trust. Study Design: Consecutive patients waiting for appointments at outpatient clinics were asked to provide demographic information and then to complete a battery of scales about their health and health care. Average scores on the 11-item Trust in Physician Scale were calculated and used to categorize patients as high trust, i.e., average responses favorable, or lacking trust, i.e., average responses neutral or unfavorable. To the extent that initial levels of physician trust are based on life experiences, groups with different life experiences should exhibit different levels of trust. Modeled proxies for patients’ previous life experiences included gender, income, age, ethnicity, education, and pain. The study tested whether the number of these predisposing factors, each of which the literature has shown to be associated with low physician trust, could explain physician trust as well as a complex, multivariable model that included predisposing factors as main effects and significant interactions involving ethnicity. Population Studied: Participants came from one private, one public, and one VA clinic. One hundred fifteen African American and 148 White American patients participated: 44% were females; 54% had incomes <= $20,000 per year; 37% completed high school or less; 41% experienced moderate to severe pain during the previous 4 weeks. Principal Findings: Logistic regression identified patient characteristics associated with entering the clinic having low physician trust. Similar accuracies were achieved using number of predisposing factors present as the sole predictive variable and the more complex multivariable model that included multiple main effects and a significant interaction: sensitivity=.474 vs .368; specificity=.855 vs .932; positive predictive value=.514 vs .636. The percentage of patients who lacked physician trust escalated as the number of predisposing factors per patient increased. Overall, 25% of respondents lacked physician trust. With one predisposing factor, 32% of respondents lacked physician trust; with three predisposing factors, 50% lacked trust; and with five predisposing factors, 67% lacked trust. Conclusions: Identification of patients who lack physician trust can be achieved by considering the number of predisposing factors pertaining to a given patient. The approach is as accurate as the multivariable logistic model with main and interaction effects, and is simple to implement, calculate and interpret. Implications for Policy, Delivery, or Practice: Disparities in quality of care can result from a lack of physician trust existing prior to scheduled medical encounters. Patients with a propensity toward lack of trust possess multiple proxies for previous life experiences that are known to influence trust, i.e., low income, African American, low education, poor health, men, older. A simple screening tool to identify patients who lack physician trust, based on readily available measures, can help providers identify patients who may have special concerns. Understanding these concerns is a first step toward addressing root causes of low physician trust and toward improving delivery processes for vulnerable populations. Primary Funding Source: AHRQ, Department of Veterans Affairs ●Help Seeking Among Individuals with Inadequate Health Literacy Shoou-Yih Lee, Ph.D., Julie A. Gazmararian, Ph.D., Ahsan M. Arozullah, M.D., MPH Presented By: Shoou-Yih Lee, Ph.D., Assistant Professor, Health Policy and Administration, University of North Carolina at Chapel Hill, 1101 McGavran-Greenberg Hall (CB# 7411), Chapel Hill, NC 27510-7411; Tel: (919) 966-7770; Fax: (919) 966-6961; Email: sylee@email.unc.edu Research Objective: We know very little about how individuals with inadequate health literacy cope with literacy problems and the effects of the coping behavior. Thus, the study examines (1) the relationship between health literacy and help seeking behavior and (2) how the assistance received is related to health status and health care utilization. Study Design: Health literacy was measured using the short version of the Test of Functional Health Literacy in Adults (STOFHLA). The score ranged from 0-100 and inadequate health literacy was defined as score < 67. Health status was measured with self-reported general health status and SF-12 (physical and mental health). Health care utilization included regular physician visits and hospitalization. Individuals were asked if they received the following assistance: (1) help with reading medical information from doctors and hospitals, (2) being reminded to do things to stay healthy, and (3) tangible social support (i.e., help when bed-ridden, help with doctor visits, help with preparing meals, help with daily chores, and informational help to understand situation). Individual attributes (age, gender, ethnicity, educational attainment, and marital status) were included as controls in multivariate analysis. Population Studied: The sample consisted of 3,260 Medicare enrollees, age 65 or older, at four sites of the Prudential HealthCare Plans (853 in Cleveland, 498 in Houston, 975 in South Florida, and 934 in Tampa); 2,956 spoke English and 304 spoke Spanish as their native language. Principal Findings: Compared to those with adequate health literacy, individuals with inadequate health literacy were more likely to seek and receive assistance with reading medical information (20.2% vs. 3.7%) and to be reminded to do things to stay healthy (46.4% vs. 41.3%); but they perceived less tangible social support available to them (p<0.0001). Multivariate analysis showed that among individuals with inadequate health literacy skills, reading assistance and healthful reminders were negatively related to physical and mental health status while tangible social support was positively related to health status. Receiving healthful reminders was positively related to routine physician visits. No other association was found between information/assistance and health care utilization. Furthermore, tangible social support appeared to reduce the negative impact of inadequate health literacy on self-reported general health status. Conclusions: Individuals with inadequate health literacy seek and receive various types of assistance in dealing with health problems. The assistance they receive has differential impact on health outcomes and health care utilization. Interestingly, informational assistance appears to have negative correlations with health status, possibly due to the quality of information received. Tangible social support, on the other hand, is positively associated with health status and appears to reduce the adverse effect of inadequate health literacy on health status. Implications for Policy, Delivery, or Practice: Interventions to reduce the adverse consequences of inadequate health literacy focus mostly on providing informational and communicative support (e.g., simplifying medical information) and on improving individuals’ ability to use health information. Tangible support in the individual’s social environment is largely ignored and should be emphasized in interventions and clinical practices. Primary Funding Source: AHRQ ●Determinants of Diabetes Control Among African Americans and White Veterans Judith A. Long, M.D., Joshua P. Metlay, M.D., Ph.D. Presented By: Judith A. Long, M.D., Physician Researcher, Philadelphia VA CHERP, 1201 Blockley Hall, 423 Guardian Drive, Philadelphia, PA 19104; Tel: (215)898-4311; Fax: (215)5738778; Email: jalong@mail.med.upenn.edu Research Objective: Compared to whites, African Americans (AA) have worse diabetes control, and more complications from diabetes mellitus (DM). The objective of this study was to determine if socio-demographic, self-care, or clinical factors help explain why AAs have worse diabetes control than whites. Study Design: This project is a clinic-based, case-control study. Using hospital administrative and clinical records, we identified veterans living in Philadelphia with DM diagnosed after age 30 and having a HbA1c drawn at the VA within 3 months of the date of sampling. Cases were defined as diabetic veterans with a HbA1c = 8% and controls were diabetic veterans with a HbA1c < 8%. Each participant completed a telephone survey and had their VA medical chart reviewed. We performed bivariate and multivariate analyses to determine predictors of diabetes control and after adjusting for clustering by provider, sequential logistic regressions to determine if groups of variables helped explain the association between diabetes control and race. Population Studied: Diabetic Veterans Principal Findings: 433 veterans (67% of those contacted and eligible) participated in the study (147 cases, 286 controls, 317 AAs, and 116 whites). Among AA, only 61% had good diabetes control, compared to 81% among whites (p < 0.001). In unadjusted analyses, the odds for AAs, compared to whites, of having good diabetes control was 0.35 (95% CI 0.19-0.64). In the final adjusted model, in addition to race, the following were associated with good control: older age, an unchanged or better financial situation compared to the previous year, having no additional health insurance, better diabetes self-care as determined by the Diabetes Care Profile Self-Care Adherence Scale, better self-rated general health, a total cholesterol under 200 mg/dl, and having had diabetes for fewer years. After adjusting for these factors, the odds for AAs, compared to whites, of having good control was 0.34 (95% CI 0.19-0.63). Conclusions: In these analyses, we show that predictors of diabetes control include socio-demographic, self-care, and clinical factors; however, these factors did little to explain the disparities in control between AA and white diabetic veterans. Implications for Policy, Delivery, or Practice: Until we better understand reasons for racial differences in diabetes control we are unlikely to eliminate this large disparity. Primary Funding Source: VA ●Processes and Outcomes in the Transition of Care for Youth with Chronic Childhood Illness Debra Lotstein, M.D., Moira Inkelas, Ph.D., Ronald Hays, Ph.D., Neal Halfon, M.D., MPH Presented By: Debra Lotstein, M.D., Assistant Professor of Pediatrics, Pediatrics, UCLA, 10833 Le Conte Avenue, 12-358 MDCC, Los Angeles, CA 90095; Tel: (310)825-9346; Email: dlotstein@mednet.ucla.edu Research Objective: As children with chronic medical conditions grow into adulthood, they lose support from childspecific systems, and comparable adult programs do not exist. There is evidence that young adults with chronic conditions have difficulty transitioning to adulthood, and that assistance with the transition process can improve access to health care and health-related outcomes. The purpose of this study is to describe the health care quality and outcomes for young adults with chronic illnesses who have aged out of eligibility for a child-specific care coordination and payment program, and to describe the relationship of these outcomes to prior assistance with the transition process. Study Design: We conducted a cross-sectional survey of former clients of a federally-funded case management and medical care payment program for children with serious medical conditions. Descriptive statistics were calculated to describe socio-demographic and medical characteristics of this sample. To measure transition support, subjects reported on assistance in four domains of transition (medical care, insurance, self-care skills and school/job planning). Measured outcomes included health–related quality of life measures and education, vocational and social status. Access measures included interruption in care and insurance coverage since leaving the program. Also, we estimated bivariate relationships between childhood factors and both transition processes and outcomes. Population Studied: Potential subjects were identified using archival records from the San Bernardino County, California Title V program. One hundred former clients of the program, aged 21-24 (mean age=23 years), without cognitive impairment, completed the survey. Principal Findings: Survey respondents had a broad range of medical conditions, of which 28% were congenital. Prior to age 21, half had Medicaid and most received care from an academic setting. Only 31% of respondents had discussed the need for an adult-oriented physician with their pediatric providers, and only 25% received assistance in finding an adult provider. About 25% reported a current unmet need for medical care. Over 40% have had an interruption in insurance coverage since turning 21, and 22% were uninsured at the time of the interview. Almost half were unemployed and 25% had not completed high school. Conclusions: Transition assistance for this population of youth with chronic conditions falls short of national recommendations. Access to appropriate adult-oriented medical care is also sub-optimal. These youth report substantial unmet needs for medical care. Implications for Policy, Delivery, or Practice: An improved transition process could decrease the discontinuties seen in care across the life span. Public agencies, as well as specialty and primary care providers, should improve transition planning and assistance to youth with chronic childhood conditions. Primary Funding Source: RWJF ●Differences in Health Literacy Among Subgroups of Medicare Beneficiaries Lauren McCormack, Ph.D., MSPH, Jennifer Uhrig, Ph.D., Carla Bann, Ph.D. Presented By: Lauren McCormack, Ph.D., MSPH, Program Director, Health Communication, RTI International, 3040 Cornwallis Road, RTP, NC 27709; Tel: (919) 541-6277; Fax: (919) 990-8454; Email: Lmac@rti.org Research Objective: To measure health literacy of beneficiaries enrolled in the Medicare program and to examine factors that predict health literacy levels. Study Design: Analysis of the Medicare Current Beneficiary Survey (MCBS). Working in collaboration with the Centers for Medicare and Medicaid Services, we developed and tested two types of survey questions to measure health literacy among Medicare beneficiaries – health insurance terminology questions (n= 10) and reading comprehension and numeracy questions (n= 17), creating an index for each set of questions (Cronbach’s alpha = .76 and .85, respectively). The reading comprehension and numeracy questions were based on excerpts from the Medicare & You 2001 handbook about various topics including information available on the Medicare hotline, how to interpret a Medicare claims notice, an overview of the Medicaid program for dual eligibles, and exercises related to choosing a health plan. The questions were fielded in Round 36 of the MCBS using in in-person interview format. Population Studied: Nearly 1,000 elderly and disabled Medicare beneficiaries residing in community settings. Principal Findings: Terms that all beneficiaries were least likely to correctly define include “provider network” (39 percent), “formulary” (42 percent), and “Medigap” (55 percent). Nearly nine out of every 10 respondents knew what a “primary care doctor” is. After reading a short overview, only about half of respondents correctly indicated that the purpose of the Personal Plan finder is to help beneficiaries choose a health plan. About 60 percent of beneficiaries correctly reported that Medicaid is a joint Federal/state program despite this being directly stated in a reading comprehension paragraph. Respondents also had difficulty interpreting some data in the claims notice, particularly the amount paid to the doctor and the amount of deductible met. Based on descriptive statistics, some of the more typical vulnerable subgroups of Medicare beneficiaries also had significantly lower levels of health literacy relative to their counterparts. This includes disabled beneficiaries and those in the oldest age group (85+), non-whites, Hispanics, those with less than a high school education, and those in fair/poor health. Controlling for these and other factors in our multivariate analysis, we examined the determinants of health literacy, modeling the two indices separately. Preliminary results suggest that older beneficiaries and those with less education and income had significantly lower levels of health literacy in both indices. Non-whites had significantly lower health terminology levels. Conclusions: Selected subgroups of Medicare beneficiaries appear to have lower levels of health literacy based on questions that address health related terminology and navigation of the Medicare program. Implications for Policy, Delivery, or Practice: Efforts need to continue to inform and educate Medicare beneficiaries, with consideration given to how address lower levels of health literacy particularly among selected subgroups. Additional research is needed to refine this initial set of health literacy measures and to examine the factors that affect health literacy in the Medicare population. Primary Funding Source: CMS ●Racial/Ethnic Differences In CAM Use For Chronic Medical Conditions Shannon Mitchell, Ph.D. Presented By: Shannon Mitchell, Ph.D., Associate Research Scientist, Epidemiology and Public Health, Yale University, 240 East 86 #15H, New York, NY 10028; Tel: (212)706-2751; Email: shannon.mitchell@yale.edu Research Objective: This project examines an important and heretofore largely unexamined aspect of racial/ethnic disparities in health services utilization--the use of complementary and alternative medicine for chronic health conditions. Although CAM is increasingly used by Americans, little is known about patterns of CAM use for treatment of common medical conditions among racial/ ethnic minorities. Specifically the study examines whether there are racial/ethnic disparities in1) the prevalence of overall CAM use and provider based vs. self-administered CAM therapies for chronic medical conditions (including cardiovascular disease, diabetes, cancer, back pain/problems, arthritis, chronic pain, anxiety/depression, mobility problems, and obesity), 2) CAM use as a complement or substitute for conventional medical care, 3) the importance of CAM therapies in maintaining health and well-being, and 4) perceived effectiveness of CAM therapies in treating chronic medical conditions. Study Design: The study employs a cross-sectional design to examine racial/ethnic disparities in CAM using data from the 2002 National Health Interview Survey (NHIS). The NHIS is a nationwide, personal interview household survey conducted annually through the National Center for Health Statistics, which contains a representative sample of the civilian, noninstitutionalized population of the United States. In 2002, the NHIS included an Alternative health/ Complementary and Alternative Medicine supplement implemented as part of the Sample Adult Core. Respondents were asked about their use of 17 non-conventional therapies during the last 12 months. Interviews were conducted in English and Spanish and had a final sample response rate of 74 percent. Logistic regression analysis was used to determine the amount of disparities in the use of CAM for chronic medical conditions, importance of CAM in maintaining health and well-being, and perceived effectiveness between Whites, African-Americans, and Hispanics controlling for other respondent demographic characteristics including insurance status. Separate models of CAM use were estimated for individual chronic conditions as well as any chronic condition. Population Studied: The sample of patients included in the study consists of those persons included in the 2002 NHIS adult sample core (N=31,044). Principal Findings: Preliminary analyses show that Whites are more likely to report any CAM use and provider-based CAM use for chronic medical conditions. However, patterns of use, importance of CAM, and perceived effectiveness vary among racial/ethnic minorities. African Americans and Hispanics were more likely to use specific self-administered CAM therapies for the treatment of chronic medical conditions compared to Whites. There were racial/ethnic disparities in the importance and perceived effectiveness of CAM therapies in the treatment of chronic medical conditions. Conclusions: Because the analysis is still in the preliminary stages, we do not offer conclusions at this time. Implications for Policy, Delivery, or Practice: The broad goal of this study is to further our understanding of how CAM utilization might contribute to eliminating disparities in health. Given that racial/ethnic minorities are more likely to suffer from many chronic medical conditions, have poorer health status and health outcomes, understanding racial/ethnic differences in the use of multiple healing practices, would further serve to improve cultural competency in health care delivery and may reduce disparities in health. Through better understanding of racial/ethnic disparities in CAM use, importance of CAM and perceived effectiveness in the treatment of chronic medical conditions, the study provides information and direction to strategies for improving quality of care and cultural competency. Primary Funding Source: National Center for Complementary and Alternative Medicine, NIH ●Evaluation of the Single Item Health Literacy Screener Nancy Morris, Ph.D., APRN, Charles D. MacLean, MDCM, Benjamin Littenberg, M.D. Presented By: Nancy Morris, Ph.D., APRN, Associate Professor, Nursing, The University of Vermont, 228 Rowell, 106 Carrigan Drive, Burlington, VT 05405; Tel: (802) 656-3057; Fax: (802) 656-8306; Email: nancy.morris@uvm.edu Research Objective: Reading ability, an aspect of health literacy, is important to knowledge about health care: health information, management of one’s health, utilization of services, and outcomes. A short, simple measure to screen for limited health literacy would allow for targeted interventions to enhance communication and optimize patient understanding when appropriate. Our aim was to assess the diagnostic accuracy of the Single Item Literacy Screener (SILS) as compared with the Short Test of Functional Health Literacy in Adults (STOFHLA). Study Design: Cross-sectional survey, with in-home interviews of patients recruited from primary care practices participating in the Vermont Diabetes Information System. The STOFHLA is a valid, reliable and widely used 7-minute timed test of reading comprehension to measure health literacy. Results are categorized into inadequate (0-16 correct answers), marginal (17-22 correct answers), and adequate health literacy (23-36 correct answers). The SILS is a single brief question that can be asked by a health care professional or clerk: “How often do you need to have someone help you when you read instructions, pamphlets, or other written material from your doctor or pharmacy?” Responses of “sometimes,” “often,” or “always” are considered a positive result and suggest further assessment of health literacy is warranted. A “never” or “rarely” response is negative. Population Studied: 766 outpatient adults with diabetes confirmed by their Primary Care Provider, receiving primary care in Vermont or northern New York. Principal Findings: Of the 766 persons screened, 142 (18%) had limited health literacy [marginal or inadequate (STOFHLA score of 0-22), blind, or otherwise unable to read]. Six hundred (78%) screened negative on the SILS and 546 of these subjects had adequate health literacy (negative predictive values=91% (95% confidence interval 88%, 93%)). Of the 166 who scored positive on the SILS, 73 had limited literacy (positive predictive value = 44% (.36, .52)). The sensitivity of the SILS was 54% (95% confidence interval 45%, 62%) and the specificity was 85% (82%, 88%). The area under the Receiver Operative Characteristic Curve (ROC) was 0.74 (0.69, 0.78). Conclusions: The SILS is a simple means to discriminate between limited and adequate health literacy in ambulatory adults with diabetes. Implications for Policy, Delivery, or Practice: An ideal screening instrument has a high level of sensitivity, acceptable specificity, ease of administration, reasonable costs, and negligible risk and minimal burden to the patient. Although not very sensitive, the SILS can easily exclude patients who do not need further assessment. This allows providers to target additional assessment of health literacy to the subset of the population most in need. Primary Funding Source: , National Institute of Diabetes and Digestive and Kidney Diseases ●Providing Health Education to People with Disabilities Jill Morrow, M.D., MBA Presented By: Jill Morrow, M.D., MBA, Medical Director, Public Welfare, Office of Mental Retardation, Commonwealth of Pennsylvania, 512 Health and Welfare Building; North 7th and Forster Street, Harrisburg, PA 17108; Tel: (717)787-5110; Fax: (717)772-0012; Email: jmorrowgor@state.pa.us Research Objective: People with mental retardation (MR) often have complex medical problems, but limited ability to understand health education materials designed for the general public. Multiple people support them and need to understand their medical conditions. We sought to identify whether or not we could deliver health information to a broad group of stakeholders across a geographically diverse state. We also asked if that health information would impact the health of this population. The Pennsylvania Health Care Quality Unit (HCQU) initiative aims to address this. Study Design: We designed a demonstration project to create HCQUs to provide health training and gather health data. Groups of counties collaborated to develop proposals to create HCQUs based on a template. Surveys of need related to health care issues guided the proposals and initial activities of the HCQUs. Eight HCQUs were created across the Commonwealth representing all of Pennsylvania’s 67 counties. HCQU clinical staffing includes registered nurses and consultant primary care and psychiatric physicians. Additional staffing includes individuals with a mental health background, IT support, and a designated training coordinator. HCQUs average about 10 employees each. We measured the ability to provide training at the appropriate level for the audience and used the health data to assess the impact of that training. Population Studied: We targeted the population of people receiving licensed residential services through the Office of Mental Retardation, Commonwealth of Pennsylvania and the people who support them including families, case managers, and staff providing direct care. The individuals with MR live in group homes, Intermediate Care Facilities for the Mentally Retarded (ICF/MR), and family living. Adults comprise over 95% of this population of 15,504 Principal Findings: HCQUs provided 2199 trainings to people from every county in the Commonwealth in quarters 3 and 4 of fiscal year 2003-2004. This involved 3309 hours and 21,112 people. The distribution of stakeholders receiving training included 68% direct care staff, 10% supports coordinators, 2% family members, 5% consumers, 10% health care workers, and 5% other. Basic, intermediate and advanced training levels comprised 75, 22, and 3% respectively. Training topics consisted of general health topics including nutrition, diabetes, medications, and bipolar disorder. The training topics also included those that are more common in people with MR like seizures, Trisomy 21, lifting and body mechanics, and dysphagia. Trainees indicate an overall training satisfaction over 90%. Preliminary impact data indicates that nutrition is one of the most frequently delivered topics and that the number of overweight individuals with a weight reduction program increased by 5% from fiscal years 2001-2002 to 2003-2004. Conclusions: We demonstrated that small units can effectively deliver health information to a wide audience across a large geographic area. Trainees overall demonstrate satisfaction with training. The data shows impact on behavior related to weight reduction for overweight individuals. Implications for Policy, Delivery, or Practice: Policy makers should consider this model for similar populations in other areas and other groups of individuals with disabilities. Definitive assessment of the impact of this approach on knowledge of health information and change in behavior requires additional study Primary Funding Source: No Funding Source ●Impact of Health Education on Weight in People with Disabilities Jill Morrow, M.D., MBA Presented By: Jill Morrow, M.D., MBA, Medical Director, Public Welfare, Office of Mental Retardation, Commonwealth of Pennsylvania, 512 Health and Welfare Building; North 7th and Forster Street, Harrisburg, PA 17108; Tel: (717)787-5110; Fax: (717) 772-0012; Email: jmorrowgor@state.pa.us Research Objective: The prevalence of obesity in the general population is known through public health surveillance surveys. However, these surveys typically either cannot identify those with disabilities or do not capture a large enough sample of that population. This study identifies the prevalence of obesity and overweight in a population of people with mental retardation (MR) and assesses the impact of modified health education on this condition. Study Design: b. We gathered measurements of weight, height, diet, and physical activity on a random sample of people with MR. A standardized instrument called the Health Risk Profile was used and the data gathered from residential medical records by registered nurses. The data was gathered in two fiscal years 2001-2002 and 2003-2004. Training about nutrition occurred between those two years. The general population prevalence rates were used as a control. Population Studied: c. People with MR receiving licensed residential services including group homes, Intermediate Care Facilities for the Mentally Retarded (ICF/MR), and family living through the Office of Mental Retardation (OMR), Commonwealth of Pennsylvania make up a population of 15,504. We used a random sample of 1286 adults; 748 in 2001-2002 and 538 in 2003-2004. We excluded 58 individuals for incomplete data. Principal Findings: d. We used height and weight to calculate Body Mass Index (BMI) for all individuals in the sample. BMI was categorized using the CDC guidelines for obesity groups. We had complete data for 1228 people. During the first year 30% of people fell into the overweight category and 32% in the three CDC obesity categories making a total of 62% in both categories. In the second year 28% made up the overweight category and 32% the obese ones for a total of 60%. This is comparable to existing Pennsylvania prevalence of 60%, but somewhat higher than the 24% in the obese categories. We noted a difference of 4% in the proportion of people in the overweight or obese categories who had a weight reduction program between 2001-2002 and 2003-2004. We demonstrated an increase of 8% between those two years in the proportion of people with a weight loss program who lost at least 5 pounds in the last year. A difference did not exist in the proportion of people who had an exercise program; 38% in 2001-2002 and 40% in 2003-2004. Conclusions: e. Obesity and overweight impact individuals with MR to the same extent as the general population. Our data shows that individuals with MR can participate in weight reduction programs and lose weight. Our results indicate that training about nutrition lead to weight loss and potentially the impact of obesity on chronic health conditions. Implications for Policy, Delivery, or Practice: f. Policy makers should consider the application of this model to other disability groups and to other health conditions. Further research is needed to assess the longevity of the effects of the training on weight. Primary Funding Source: No Funding Source ●Social Cohesion, Social Support and Health Among Latinos in the United States Norah Mulvaney-Day, Ph.D., Margarita Alegria, Ph.D Presented By: Norah Mulvaney-Day, Ph.D., Associate Director, Cambridge Health Alliance, Center for Multicultural Mental Health Research, 120 Beacon Street, 4th Floor, Somerville, MA 02472; Tel: (617) 503-8448; Fax: (617) 5038430; Email: nmulvaney-day@charesearch.org Research Objective: Understanding the source of health disparities among Latinos is complicated by the heterogeneity of this group. Social supports have been found to have a positive influence on health in the general population. This analysis examines the relationships between different forms of social support (neighborhood social cohesion, family support and friend support) and self-rated physical and mental health in a population of Latinos. Study Design: Two dichotomous variables were created to represent a poor/fair self-rating of (1) general physical health and (2) mental health as the dependent variables. Logistic regressions using weighted data were conducted in order to observe the main effects of the levels of social cohesion, family support and friend support on these two dependent variables. Control variables were age, sex, poverty, education and marital status. The sample was stratified across nativity (U.S. born versus non-U.S. born) in order to observe differences. Population Studied: The data set for this analysis is from the National Latino and Asian American Study (NLAAS), a nationally representative household survey of Latinos and Asians living in the United States. The sample consists of 2554 Latinos from four distinct subgroups: 577 Cuban; 495 Puerto Rican; 868 Mexican; and 614 Other Latino. Principal Findings: High levels of family support, social support and social cohesion all had negative relationships with poor/fair self-rated general health in the combined sample. Family support and friend support were also negatively related to poor/fair mental health, although social cohesion did not emerge as a factor in the mental health model. When models were stratified across nativity, family and friend support remained significant for those born outside the U.S. but not for those in the U.S., and social cohesion approached significance for those born in the U.S. (p<.10) but not for those born outside. For self-rated mental health, family support was the only significant support variable across both nativity groups. Conclusions: Family support, friend support and social cohesion represent distinct characteristics of social interaction that impact health in different ways across nativity status. For new immigrants, health is dependent upon family and friend support networks, and not necessarily upon relationships of trust and cohesion with unrelated others in one’s neighborhood. For US-born Latinos, social cohesion is more important, suggesting that if family and friend supports break down over time, the level of social cohesion is more critical to individual health. Implications for Policy, Delivery, or Practice: This study suggests that there may be different pathways toward health for different generations of Latinos and also across general versus mental health. This complexity indicates that it is critical to avoid mental health and health care policy development aimed at Latinos as a uniform group. Further, the importance of community level support for Latinos born in the U.S. should to be taken into account by primary care clinicians. Community interventions that emphasize neighborhood level cohesion may be a vehicle for reducing health disparities. Finally, the relationship between family support and self-rated mental health should be considered in mental health treatment plans for Latinos. Primary Funding Source: National Institute of Mental Health ●Do Racial and Ethnic Disparities Exist in Unmet Needs for Specialty, Dental, Mental, and Allied Health Care among Children with Special Health Care Needs? Emmanuel Ngui, DrPH, MSc, Glenn Flores, M.D. Presented By: Emmanuel Ngui, DrPH, MSc, Assistant Professor of Pediatrics, Epidemiology and Health Policy, Center for the Advancement of Underserved Children, Department of Pediatrics, Medical College of Wisconsin, 8701 Watertown Plank Road, Milwaukee, WI 53226; Tel: (414)4564302; Fax: (414)456-6385; Email: engui@mail.mcw.edu Research Objective: To examine racial/ethnic disparities in reported unmet needs for specialty, dental, mental, and allied health care, and to identify factors associated with unmet needs among racial/ethnic CSHCN. Study Design: We analyzed data from the 2001 National Survey of CSHCN (NS-CSHCN). For each outcome, unmet need was defined as parental report of the child not receiving all needed health care in the past year. Covariates examined included child’s age, gender, residence, maternal education, insurance coverage, poverty status, availability of a personal doctor or nurse, language of interview, the child’s condition severity, and whether the condition is stable or changes all the time. Population Studied: A nationally representative sample of 38,886 CSHCN <18 years old participating in the 2001 NSCSHCN. Principal Findings: Black and Hispanic CSHCN were significantly (p<.05) more likely than white CSHCN to be poor (29% vs. 32% vs. 9%). Black CSHCN also were significantly more likely than white CSHCN to have no personal doctor or nurse (14% vs. 9%) and to have conditions that change all the time (9% vs. 6%), whereas Hispanic CSHCN were significantly more likely than white CSHCN to be uninsured (9.3% vs. 4.5%). The prevalence of reported unmet needs among CSHCN ranged from 7% for specialty care to 18% for mental health care. Compared to white CSHCN, black CSHCN had significantly more unmet needs for specialty (10% vs. 7%), dental (16% vs. 8.7%), and mental health care (27% vs. 17%), and Hispanic CSHCN had more unmet dental care needs (16% vs. 9%). Except for unmet mental health care needs among Hispanic CSHCN (OR, 0.6; 95% CI, 0.40 0.96) all other racial/ethnic disparities in unmet needs disappeared after multivariate adjustment. Black female CSHCN, however, were disproportionately more likely to have unmet mental health care needs than all other groups (41% vs. 13-20%), and had significantly greater adjusted odds of unmet mental health care needs than black male CSHCN (OR, 2.2; CI, 1.2-4.0). For each racial/ethnic group and for CSHCN overall, the most significant determinants of unmet needs included lack of insurance, poverty, lack of a personal doctor or nurse, and having conditions that change all the time. Conclusions: Racial/ethnic disparities exist in unmet specialty, dental, and mental health care needs among CSHCN, but disappear after adjustment, except for unmet mental health care needs among black female CSHCN. Within and across racial/ethnic groups, key factors associated with disparities in unmet needs included lack of insurance coverage, poverty, lack of a personal doctor or nurse, and having conditions that change all the time. Implications for Policy, Delivery, or Practice: Our findings suggest the need for universal mental health screening of black female CSHCN. In addition, because minority children are disproportionately more likely than white children to live in poverty, be uninsured, and lack a personal doctor or nurse, eliminating disparities in unmet specialty, dental, and mental health care needs for all CSHCN, and especially minority CSHCN, will require greater efforts to reduce the number of poor and uninsured CSHCN, and to ensure that all CSHCN have a medical home. Primary Funding Source: No Funding Source ●Are There Racial and Ethnic Disparities in Satisfaction with Care Among Parents of Children with Special Health Care Needs (CSHCN)? Emmanuel Ngui, DrPH, MSc, Glenn Flores, M.D. Presented By: Emmanuel Ngui, DrPH, MSc, Assistant Professor of Pediatrics, Epidemiology and Health Policy, Center for the Advancement of Underserved Children, Department of Pediatrics, Medical College of Wisconsin, 8701 Watertown Plank Road, Milwaukee, WI 53226; Tel: (414)4564302; Fax: (414)456-6385; Email: engui@mail.mcw.edu Research Objective: To examine whether racial/ethnic disparities exist in parental satisfaction with care among CSHCN, and to identify factors associated with these disparities. Study Design: Bivariate and multivariate analyses of data from the 2001 National Survey of CSHCN (NS-CSHCN). Covariates included sociodemographic factors, insurance, language of interview, condition severity and stability, ease of using services, provider-patient communication factors (PPC), and having a personal doctor/nurse. PPC measures included parental ratings of the healthcare provider as never/sometimes: spending adequate time with the child (inadequate time), listening carefully to parents (inadequate listening), being sensitive to the family’s values/customs (cultural insensitivity), providing needed information to families (inadequate information), and helping parents feel like partners in care (inadequate partnership). Population Studied: Nationally representative sample of 38,886 CSHCN < 18 years old. Principal Findings: Nationally, 8% of parents of CSHCN were dissatisfied or somewhat dissatisfied with their children’s healthcare, with Hispanic (16%) and black (13%) parents more dissatisfied than white parents (7%). Dissatisfaction was greater among parents of CSHCN who were poor, uninsured, publicly insured, had no personal doctor/nurse, had a mother who had not graduated from high school, interviewed using a non-English survey, and with conditions that change frequently. Minority parents were significantly more likely than white parents to report problems in ease of using healthcare services and PPC. Black and Hispanic parents were significantly more likely than white parents to be dissatisfied (odds ratio [OR], 2.3; 95% confidence interval [CI], 1.6-3.3; OR, 2.6; CI, 1.8-3.8, respectively), but these disparities disappeared after multivariate adjustments. Among all parents of CSHCN, inadequate listening (OR, 2.4; 95% CI, 1.6-3.5), information (OR, 1.8; CI, 1.3-2.6), time (OR, 1.7;CI, 1.2-2.4), and partnership (OR, 1.6; CI, 1.1-2.3), difficulty using services (OR, 3.4; CI, 2.54.8), language barriers (OR, 2.1;CI, 1.1-4.4), and condition severity (OR, 1.1; CI, 1.06 -1.2) were significantly associated with dissatisfaction. Within racial/ethnic groups, unique factors associated with dissatisfaction included cultural insensitivity among blacks (OR, 2.7; CI, 1.2-5.9), language barriers among Hispanics (OR, 2.7; CI, 1.2-6.15), and lack of insurance (OR, 1.8; CI, 1.1-3.1) and inadequate time (OR, 1.7; CI, 1.1-2.6) among whites. Inadequate partnership was significantly associated with dissatisfaction among Hispanics (OR, 5.2; CI, 2.2-12.4) and white parents (OR, 1.7; CI, 1.1-2.6) but not black parents. Conclusions: Racial/ethnic disparities exist in satisfaction with care among parents of CSHCN, but disappear after adjustment. Across racial/ethnic groups, key factors associated with dissatisfaction included inadequate listening and information, condition severity, and difficulty using services. Factors associated with dissatisfaction that were unique to specific racial/ethnic groups included provider cultural insensitivity for black parents, language barriers for Hispanic parents, and lack of insurance, and inadequate time with the provider among white parents. Inadequate partnership with the provider was associated with dissatisfaction among Hispanic and white but not black parents. Implications for Policy, Delivery, or Practice: Regardless of race/ethnicity, satisfaction with care among the parents of CSHCN can be improved by enhancing the ease of using services and the quality of provider-patient communication, particularly provider listening skills, information provision, and a greater focus on condition severity. Greater satisfaction among parents of Hispanic CSHCN may be achieved by addressing language barriers, such as by providing adequate interpreter services and bilingual staff. For all CSHCN, and particularly minority CSHCN, greater satisfaction with care might be achieved by implementing more family-centered healthcare that incorporates improved provider listening skills, adequate information and time with patients and their families, fewer language barriers, cultural sensitivity, and easier access to services. Primary Funding Source: No Funding Source ●A Survey on Drug Utilization Pattern in the Health Care System of India. Bhagirath Patel, Ph.D., Paresh Shah, Ph.D., Rames Goyal, Ph.D. Presented By: Bhagirath Patel, Ph D., Pharmacologist, Shri B M Shah College of Pharmacy, College Campus, Modasa, 383315; Tel: +91 2774 249475; Email: bk121@rediffmail.com Research Objective: Drug utilization pattern is an important factor determining the efficiency of a health providing set up. An efficient set up requires usage of quality drugs at an affordable price. For this purpose it is essential to collect data to evaluate the drug utilization pattern and to effect necessary interventions and policy changes to eliminate the shortcomings present, if any. Study Design: A model study was conducted at retail pharmacy outlets in rural and urban areas of North Gujarat, India. Data (1796) were collected by author and qualified pharmacist who were trained in survey procedures, using specially prepared and pre-tested questationnaires. The collected data were tabulated and analyzed by using normal proportion test. Population Studied: Total population is around 2 millions in the area of North Gujarat, India. Principal Findings: Broad spectrum antibacterial, compound with analgesics, antipyretic and anti-inflammatory effects, antacids/antiulcer and nutritional products constituted a high proportion of prescription in both urban and rural areas. Based on WHO criteria, most of the drugs (57%) prescribed in the rural areas were non-essential, compared with (48%) in urban areas. Conclusions: Use of fixed dose combinations, frequency use of antibiotics, vitamin tonic and poly pharmacy was the trend identified through this study. Indiscriminate use of antibiotics is leading to cause resistance development. Implications for Policy, Delivery, or Practice: The results of this study emphasize the need for comprehensive measures, including training, information, legislation and education at all level of drug purchase to rationalize the drug through by improving prescribing patterns. Primary Funding Source: State Government ●The Prevalence of Discrimination among Latinos in the US: Cultural and SES Correlates Debra Joy Pérez, MA, MPA, Ph.D., Margarita Alegria, Ph.D., Lisa Fortuna, M.D., MPH Presented By: Debra Joy Pérez, MA, MPA, Ph.D., Program Officer/WKKELLOGG Fellow in Health Policy Research/Multicultural Mental Health Research Fellow/NIMH mentee, Research & Evaluation Unit/Interfaculty Program in Health Policy at Harvard, The Robert Wood Johnson Foundation/Harvard University, PO Box 3311, Princeton, NJ 08543; Tel: (609)627 5966; Email: djperez@fas.harvard.edu Research Objective: Numerous studies established a relationship between discrimination and physical & mental health. Yet, we know little about the likelihoods of discrimination among Latinos in different socio demographic strata. Few studies have shown the prevalence or severity of discrimination experiences among Latino and Latino subgroups. Most of the existing literature focuses on Black/White differences. This paper examines the prevalence and severity of perceived discrimination among US Latinos. This study will address the following questions: What is the rate and severity of self-reported perceived discrimination among Latinos and Latino subgroups in the US? Do subgroup difference remain when accounting for difference in income and education? How do cultural factors vary perceived discrimination? Do Cubans, Puerto Ricans or Mexicans attribute discrimination to the same causes? How does the rate or severity of discrimination vary for Latinos in different generations or different stages of acculturation? Study Design: Data are from the National Latino and Asian American Study (NLAAS). The NLAAS is based on a stratified area probability sample design of persons 18 years of age and older in the non-institutionalized population of the 50 states and Washington D.C. The sampling frames and sample selection procedures selected for this study are common to the University of Michigan Survey Research Center’s (SRC) National Sample Design. Through the following four step sampling process, a probability sample of respondents for screening interviews was selected; 1) primary stage sampling of US Metropolitan Statistical Areas (MSAs) and counties, 2) second stage sampling of area segments, 3) third stage sampling of housing units within the selected area segments, 4) random selection of respondents from the sample housing units. Additionally, the NLAAS sample design includes two components; 1) an NLAAS core sample which is designed to provide a nationally representative sample of all national origin groups regardless of geographic residential patterns and 2) the NLAAS-HD supplements which are targeted oversampling of geographic areas with a moderate to high density (5 %+) of targeted Latino and Asian households. The supplements were added to the sample plan as a cost reduction strategy to obtain the desired sample of national origin groups not widely dispersed in the US (e.g. Puerto Rican, Cuban, Chinese, Filipino, and Vietnamese). The Mexican subgroup did not require supplemental over sampling. Individuals residing in the high-density areas had two chances of selection, one under the NLAAS Core sample and the other under the NLAAS-HD sample. This sample design requires weighting corrections for joint probabilities of selection. The NLAAS uses validated measures of sociocultural factors like acculturative distress, measures of ethnic identity, information regarding immigrant and generational status and language proficiency. The NLAAS is the largest national mental health study of Latinos and ever conducted for understanding mental health and services needs in these communities. All NLAAS subjects are interviewed in person regarding mental health diagnoses and the socio-cultural variables examined in this study. The target population for this investigation includes all Latino adults (ages 18 and over) in the NLAAS criteria for eligibility. The average final weighted response rates for the NLAAS first respondents was 75%. The NLAAS battery includes a nine-item scale of self-perceived discrimination. This discrimination scale measures the frequency of routine experiences of unfair treatment in general. Respondents indicate how often they experience the following situations: 1.) being treated with less courtesy that other people, 2.) being treated with less respect than other people, 3.) receiving poor service than other people at restaurants or stores, 4.) people acting as if they think the respondent is not smart, 5.) people acting as if they are afraid of respondent, 6.) people acting as if they think respondent is dishonest, 7.) people acting as if they think the respondent is not as good as they, 8.) being called names or insulted and 9.) being threatened or harassed. These nine items were taken from the Detroit Area Study (DAS), (Jackson & Williams, 1995; Williams, Yu, Jackson, and Anderson, 1997). The 6 response categories range from Almost Everyday (1) to Never (6). The prevalence of each item is assessed separately for each of the analysis proposed in this paper. he items in the scale had a standardized Cronbach alpha score of .9105. This study uses logistic regression and chi-square to test the various hypotheses. Population Studied: Latinos, Puerto Ricans, Mexicans, Cubans, Other Latinos Principal Findings: The overall rate of discrimination among Latinos was 34%. Rates of any perceived discrimination varied by ethnicity and demographic characteristics. Puerto Ricans were more likely to report any discrimination than other Latinos. Over forty percent of Puerto Ricans (43%) reported some experience of discrimination compared to 33.6% of Mexicans and 34.8% of other Latinos (p=0.022.) Cubans were significantly less likely than all other groups to report any discrimination (20.3%; p=0.022). Age and Gender: More men than women reported any discrimination (39.4% compared to 28.8%; p<.000). Age was inversely associated with reporting any discrimination. Younger Latinos were significantly more likely than older Latinos in any other age group to report any discrimination. There is an almost perfect linear relationship between increase in age and decrease reporting of perceived discrimination ranging from 50.3% at 18 to 24 year olds compared to 10.9% of Latinos age 65 and over; p<.000). Reports of any discrimination increased with more education, just over a quarter of Latinos with less than a high school degree reported any discrimination compared to 43% of Latinos with some college or better (p<.000.) Socioeconomic Factors:Latinos in higher income ranges were also more likely to report any discrimination. Less than a third of Latinos living in households with less than 15K per year reported any discrimination while approximately 40% of Latinos in households earning more than 75K reported any discrimination (p=0.0289.) Cultural Factors: We found that English proficient Latinos were more likely than Spanish dominant Latinos to report any discrimination (45.3% v. 22.5%, p <0.000). More US born Latinos reported higher rates of discrimination compared to immigrant Latinos. Nearly half of native-born Latinos (45.9% reported any discrimination) compared to only a quarter of immigrants (25.5%; p<.000). Just under a quarter of Latinos who indicated that associations with his/her own ethnic groups were very important reported higher rates of perceived discrimination compared to nearly forty percent of Latinos who rated these associations as less important (24.27% vs. 37.65%; p <.000.) A quarter of first generation Latinos (25.47%) reported any discrimination compared to 38.96% of Latinos in the second generation, 47.24% of third generation Latinos and 51% of fourth generation Latinos (p<.000.) Similarly, possessing a strong ethnic identity and having less than a high school diploma was also associated with a decreased mean on the severity scale of perceived discrimination. Being English proficient and being a 3&4 generation Latino was also associated with an increased probability of reporting perceived discrimination after adjusting demographic and cultural factors. Conclusions: The results showed that being Cuban was associated with lower rates of perceived discrimination. One explanation may be that Cuban immigrants have a good infrastructure for transition into the US of any other Latino group (Rumbaut 1994). In addition, the effects of living in an ethnic enclave may provide protection against the perception of discrimination if not protection against discriminatory acts. As hypothesized increases in exposure to groups in cultural conflict was associated with increases in perception of discrimination. Indeed, as some studies on African Americans have demonstrated gains in education were associated with increases in the rate of perceived discrimination. The proportion of Latinos with college degrees who perceived discrimination supports this theory. Another important conclusion is that a clear acculturation pattern emerges with regard to generation change and perceptions of discrimination. Third and fouth generation Latinos report much higher rates of any discrimination than Latinos in first generations. For all cultural factors tested, this low acculturation-high discrimination relationship was consistent except for ethnic identity. Latinos with the highest ethnic identity reported the lowest rates of perceived discrimination compared to Latinos with lower ethnic identity. Ethnic identity may be protective against initial perception of discrimination. Strong ethnic identity may reduce the exposure to perceived discrimination because individuals who strongly identify are less likely to be exposed to different ethnic group members. They may also be less hyper-vigilant or sensitive than those who are more ethnically isolated. Implications for Policy, Delivery, or Practice: Latinos will have increasing impact on the healthcare system and health policy issues. People who care about how the health care system operates should care about how the prevalence of discrimination in the larger society might impact perceptions of fairness in healthcare setting. Organizations need to be responsive to the perception of discrimination by this population. Reducing discrimination can improve the patient/provider relationship and lead to a welcoming environment that in turn can improve compliance and followup. Understanding how discrimination correlates with English proficiency and generation have implications for service delivery. Knowledge of the prevalence of discrimination could lead to changes in healthcare provider training. Primary Funding Source: WKK, NIMH ●Racial and Ethnic Disparities in Rural Mental Health Treatment Stephen Petterson, Ph.D., Emily J. Hauenstein, Ph.D., LCP, APRN, Douglas Wagner, Ph.D., Virginia Rovnyak, Ph.D., Elizabeth Merwin, Ph.D., MSN, Barbara Heise, MSN, NP Presented By: Stephen Petterson, Ph.D., Assistant Professor, School of Nursing, University of Virginia, P.O. Box 800782, Charlottesville, VA 22908; Tel: 434-243-9832; Fax: 434-9821809; Email: smp4n@virginia.edu Research Objective: To assess racial and ethnic differences in mental health treatment rates and pathways to care among Mexican American, African American and Non-Hispanic white non-elderly adults residing in rural areas. Study Design: This study uses data from the Medical Expenditure Panel Survey (MEPS) to estimate racial and ethnic disparities in mental health treatment in rural areas, as well as compare urban and rural group differences. Three calendaryear measures of mental health treatment are examined: any medical visit related to a mental health condition, the number of visits and any specialized mental health care visit. Several measures of rurality are examined, including the urban-rural continuum and the proportion of a county that is classified as rural. Binary logistic and linear regression analyses were performed to estimate differences in mental health treatment, adjusting for demographic, need, and access variables. Separate models are estimated for rural subsamples of Mexican Americans, African Americans and non-Hispanic whites. Variance estimation is based on the clustered survey design of the MEPS; the weights and design variables take multiple observations of an individual into account. Population Studied: The MEPS is a large nationallyrepresentative panel survey of households designed to provide estimates of the use of health services, medical expenditures and sources of payment. Data is collected in five interviews over a two-year period. Our sample consists of adults aged 18 to 64 in the first four panels of the MEPS, covering a period from 1996 to 2000. The sample size is 34,299 respondents; this figure includes 5,765 rural non-Hispanic whites, 234 rural Mexican Americans and 745 rural African Americans. Principal Findings: Our findings show that rural minorities are significantly less likely than rural whites to obtain needed mental health care despite their having significantly poorer mental health,. For instance, multivariate results indicate that, all else being equal, the odds that rural whites obtain any treatment are nearly 1.7 times greater than the odds for rural Mexican Americans and 2.6 times greater than rural African Americans. A surprising result is that while rural minorities are at a considerable disadvantage relative to non-Hispanic whites, there are no urban-rural differences among either Mexican Americans or African Americans. By contrast, the odds of mental health treatment are 20% greater for urban non-Hispanic whites than for rural non-Hispanic whites. Conclusions: Minorities are underserved by the rural mental health system, reflecting among other factors, restricted access to mental health services, high poverty rates and low levels of insurance coverage. Implications for Policy, Delivery, or Practice: Rural residents, particularly from minority groups, are at greater risk of mental health problems. Low levels of treatment may heighten that risk. Primary Funding Source: NIMH ●Healthcare Barriers and Deaf People: Facilitating a Cross-Cultural Dialogue Brian Piotrowski, M.D., Steven Barnett, M.D. Presented By: Brian Piotrowski, M.D., National Center for Deaf Health Research, University of Rochester, 1331 East Victor Road, Victor, NY 14564; Tel: (585) 924-2100; Fax: (585) 9245920; Email: bepiotrowski@hotmail.com Research Objective: To create an environment for respectful cross-cultural discussion in order to identify barriers to healthcare for deaf people and their families. Study Design: The Deaf Heath Task Force (DHTF) was a thirty-member group that included a unique mix of representatives of local hospitals and health systems, schools, service agencies, clinicians, and community-based deaf organizations. A goal of the DHTF was to identify and prioritize barriers to health care. This information would then be used in realistic mapping strategies for meaningful change in improving health care access for deaf individuals. We used various group process techniques modified for use with a bilingual group (ASL and spoken English). Population Studied: Members of culturally distinct minority groups often have to deal with challenges in health care access and utilization. Deaf people who communicate in American Sign Language (ASL) comprise a sometimes unrecognized cultural minority group. The city of Rochester, NY - with the highest per capita population of deaf individuals in the United States - has both dynamic deaf community leaders as well as many heath care providers passionate about improving the health of the deaf community. Despite this, there are few settings in which hearing and deaf individuals may meet and discuss these issues - bringing together perspectives from both consumers and providers. Principal Findings: The DHTF met monthly in a round-table setting. Deaf culture and the mechanics of working with ASL interpreters were constantly reinforced. Initially, the group generated a list of barriers to health care access and organized them in terms of both importance to improving health care access and relative difficulty of affecting change in them. These barriers included economic, cultural, and logistic components. The DHTF later published a report on these barriers and created a plan to share this information the local community. In addition, the members and the work of the DHTF were instrumental in securing funding for the NCDHR, the first CDC-funded prevention research center focused on health promotion and disease prevention with a disability population. Conclusions: We will describe the process of creating the DHTF and negotiating the bilingual/bicultural group process. We will share the list of barriers, their ranking, and the blueprint for addressing those barriers. We will also discuss observations of the dynamics of the group process in the context of diversity (including language, race, sex, education and experience). Implications for Policy, Delivery, or Practice: While this particular project deals with health care access for deaf individuals, there is no reason that a similar technique (with modifications) could not be used to address other issues (e.g. schools, unemployment) in other socially/linguistically distinct populations (e.g. immigrant communities) Primary Funding Source: CDC, ATPM ●Does Race Matter in the Use and Outcomes of Hematopoietic Stem Cell Transplantation (HSCT) in Children with Cancer? Jasmina Radeva, MA, Lesley H. Curtis, Ph.D., Philip P. Breitfeld, M.D. Presented By: Jasmina Radeva, MA, Clinical Research Manager, Center for Clinical and Genetic Economics, Duke Clinical Research Institute, 2400 Pratt Street Room 0311 Terrace Level, Durham, NC 27705; Tel: (919)668-8654; Fax: (919)668-7124; Email: radev001@dcri.duke.edu Research Objective: Hematopoietic stem cell transplantation (HSCT) is an established treatment approach for many malignant and non malignant diseases in children. Stem cells can be derived from three sources: autologous (patient’s own), allogeneic (unrelated donor), or syngeneic (identical sibling). The success of unrelated donor stem cell transplant is related to the number of donor’s and recipient’s matching human leukocyte-associate antigens. Although the number of donors is increasing overall, individuals from certain ethnic and racial groups still have a lower chance of finding a matching donor. Our objective was to determine if race is associated with the likelihood of undergoing HSCT form any source and autologous HSCT in children hospitalized with cancer and whether race impacts length of stay (LOS) and mortality during HSCT. Study Design: Using the 2000 Kids Inpatient Database and Clinical Classification Software, we identified all childhood cancer encounters and those involving HSCT procedures. Cancer encounters were defined as encounters with primary or secondary CCS diagnosis code between 1 and 45. HSCT was defined as primary or secondary CCS procedure code of 64. Encounters with HSCT procedures were further categorized as allogeneic, autologous, bone marrow transplant not otherwise specified, and multiple HSCT procedures on the basis of primary and secondary ICD-9-CM procedure. Comorbidities were also identified using primary and secondary ICD-9-CM diagnosis codes. Logistic regression was used to model the probability of undergoing HSCT from any source or from autologous source controlling for demographic characteristics, clinical variables, and hospital characteristics. Ordinary least squares model was used to model LOS and death during HSCT admission. Likelihood ratio and Wald tests were used to evaluate the inclusion of certain hospital characteristics in the models. Population Studied: Cancer-related hospital encounters for patients up to the age of 18 excluding neonatal encounters were selected from the KID 2000 data. The KID is part of the Healthcare Cost and Utilization Project. After excluding cases where gender was missing, the study sample included 49,994 cancer-related encounters for patients of age 18 and younger excluding neonatal encounters. Principal Findings: Compared to whites, blacks and Hispanics were less likely to undergo HSCT from any source (Odds Ratio [OR] = 0.54, marginal effect [ME] = -0.0076, p<0.001 for black; OR = 0.71, ME = -0.0047, p= 0.003 for Hispanic) and less likely to undergo autologous HSCT (OR=0.47, ME = -0.0045, p<0.001 for black; OR= 0.69, ME = 0.0026, p= 0.022 for Hispanic). Regression analysis suggests neither black nor Hispanic race has impact on LOS during HSCT. The positive coefficient on black however had statistical significance when evaluating inpatient death during an HSCT procedure (coefficient: 0.069, p=0.039). Conclusions: This analysis supports that, compared to whites, blacks and Hispanics are less likely to undergo any form of HSCT, not just allogeneic procedures. Black race was significantly associated with inpatient mortality during HSCT. Implications for Policy, Delivery, or Practice: In the future, these analyses should be controlled for patient level clinical data including disease stage and severity and data on parent/guardian perceptions of health care. Primary Funding Source: No Funding Source ●Disparities in Glycemic Control among Patients with Diabetes Receiving Care in Public Hospital Systems Marsha Regenstein, Ph.D., Jennifer Huang, MS, Dean Schillinger, M.D., Daniel Lessler, M.D., MHA, Brendan Reilly, M.D. Presented By: Marsha Regenstein, Ph.D., Director, National Public Health and Hospital Institute, 1301 Pennsylvania Avenue NW, Suite 950, Washington, DC 20004; Tel: (202) 585-0100; Fax: (202) 585-0101; Email: mregenstein@naph.org Research Objective: Public hospitals provide care to many of the country’s most vulnerable residents and share a commitment to eliminate barriers to care based on race, ethnicity, or ability to pay. While these organizations provide significant amounts of inpatient, outpatient, emergent and supportive services to patients, little is known about the care of patients with diabetes across public hospitals, or the extent to which disparities in diabetes outcomes exist within these systems. Study Design: In 2002-3, the National Public Health and Hospital Institute assembled a quality improvement consortium involving 7 public hospital systems that provide care to over 125,000 patients with diabetes on an annual basis. We obtained demographic, clinical, and utilization data over a 3-year period on a random sample of 3,000 patients with diabetes from each system.To be included, patients had to be *18 years old and have made 2 or more outpatient visits during the study period with an associated ICD-9 code of diabetes (excluding gestational diabetes). Six of the 7 sites reported race/ethnicity data on >98% of patients. Using patients' last HbA1c value, we measured the proportion of patients with poor glycemic control (HbA1c *9%, a standard benchmark), and explored whether glycemic control varied by race/ethnicity, insurance status, or use of outpatient services. Population Studied: Adult patients who received care at 7 public hospital systems during the period Jan 1 2000 through Dec 31 2002. Overall, 69% of patients were non-White minorities, and 42% were uninsured. Principal Findings: Over the 3-year period, 34% of patients rarely made outpatient visits (2-4 visits/3 yrs), 26% made occasional visits (5-10 visits/3 yrs) and 39% made regular visits (>10 visits/3 yrs). Overall, 26% of patients had poor glycemic control. Poor glycemic control was more common among Blacks (29%) and Hispanics (31%) than Whites (19%) or Asians (16%) (P<.001) and was greater among the uninsured (33%) than those with Medicaid (24%), commercial insurance (24%) or Medicare (17%) (P<.001). Adjusting for age, sex, race/ethnicity, insurance, and outpatient utilization, Blacks and Hispanics had worse glycemic control as measured by mean HbA1c (8.3% and 8.2%) than Whites or Asians (7.8% and 7.9%), as did the uninsured (8.2%) compared to Medicaid (8.0%), commercially insured (7.9%) and Medicare (7.5%) (P<.001). In adjusted models, there was a graded relationship between extent of ambulatory use and glycemic control with rare, occasional, and regular users having mean HbA1c levels of 8.4%, 8.1% and 7.8%, respectively (P<.001). Conclusions: Despite limited resources and the challenges posed by caring for diverse and vulnerable populations, public hospital systems perform at a level comparable to other health systems with regard to glycemic control. Our results suggest that public hospital systems should target access for the uninsured, continuity of care for all patients, and quality of care for minority populations. Implications for Policy, Delivery, or Practice: Given their shared missions and the availability of electronic data systems, public hospital systems have the opportunity to collaborate in quality of care benchmarking and crafting innovative diabetes improvement initiatives. Primary Funding Source: CWF ●A Comparison of Cancer Patients Visits to Physician’s Offices with Visits to Hospital Outpatient Departments Lisa Richardson, M.D., MPH, Florence Tangka, Ph.D. Presented By: Lisa Richardson, M.D., MPH, Medical Officer, Division of Cancer Prevention and Control, Centers for Disease Control and Prevention, 4770 Buford Highway NE, MS K-55, Atlanta, GA 30341; Tel: (770) 488-4351; Fax: (770) 488-4639; Email: lfr8@cdc.gov Research Objective: To compare the characteristics of cancer patients who made ambulatory visits to physician’s offices (POs) with the characteristics of those who made ambulatory visits to hospital outpatient departments (OPDs). Study Design: We analyzed data collected during the 2001 and 2002 National Ambulatory Medical Care Survey (NAMCS) of POs and National Hospital Ambulatory Medical Care Survey (NHAMCS) of OPDs. Sampling weights that accounted for multistage sample design and nonresponse of in-scope practitioners were used to obtain national estimates for the number of PO or OPD visits made by patients with cancer. We examined cancer-related and personal characteristics of patients by the visit setting (PO versus OPD). Population Studied: Patients with a primary diagnosis of cancer made a total of 3,116 visits to a PO or an OPD in 2001 or 2002. Principal Findings: We estimated that 7,856,379 patients made 27,456,800 cancer-related ambulatory visits in 2001 and 2002, 15% to an OPD and 85% to a PO. We also found that the characteristics of patients varied by setting type. The proportion of cancer-related visits for lung cancer and leukemia/lymphoma (10% and 35%, respectively) were higher in OPDs than in POs (8% and 11%, respectively). In contrast, the proportion of visits for breast and prostate cancer were higher in POs (23% and 19%, respectively) than in OPDs (14% and 6%, respectively). Anti-cancer drugs were ordered or administered in 11% of all visits, with similar proportions in POs and OPDs, although patients indicated that intravenous chemotherapy was the main reason for 10% of OPD visits but only 2% of PO visits. Patients younger than 45 accounted for a much higher proportion of cancer-related visits to OPDs (19%) than to POs (2%); while those older than 45 were more likely to be seen in POs. Blacks and Hispanics accounted for a higher percentage of visits to OPDs (14% and 12%, respectively) than to POs (9% and 3%, respectively), and Medicaid paid for more visits to OPDs (17%) than to POs (4%). Patients who had made six or more cancer-related medical visits in the previous year accounted for 56% of all OPD visits but only 25% of all PO visits. Conclusions: Minority and Medicaid-insured cancer patients are more likely than other cancer patients to make ambulatory visits to OPDs. Although the percentage of visits associated with anti-cancer drugs in OPD settings is similar to that in PO settings, intravenous chemotherapy is far more likely to be listed as the main reason for cancer-related visits to OPDs than visits to POs. Implications for Policy, Delivery, or Practice: These results confirm recent findings that black and Hispanic cancer patients and cancer patients insured by Medicaid are more likely to be served in hospital-based clinics than are other cancer patients (Richardson et al., accepted to AJPH). Because little research has been done to determine whether the location of cancer treatment is a causal factor in cancerrelated health disparities, future studies should examine the content and quality of the cancer care delivered in each treatment location. Primary Funding Source: CDC ●Racial and Ethnic Disparities in Access to Meantal Health Services Patrick Rivers, Ph.D., MBA, Saundra Glover, Ph.D., Kai-Li Tsai, Ph.D. Presented By: Patrick Rivers, Ph.D., MBA, Associate Professor & Director, Health Care Management, Southern Illinois University Carbondale, CASA -6615, Carbondale, IL 629016615; Tel: (618)453-8842; Fax: (618)453-7020; Email: privers@siu.edu Research Objective: To assess and categorize the impact of structural, financial and severity barriers on differential access of mental health services among adults by race. This study examined the influence of health insurance, availability of community medical resources, transportation, and access to care, on the racial and ethnic variations in utilization of mental health services. Study Design: We performed the following analyses: (1) descriptive analysis to estimate population size and weighted percent; (2) Chi-square analysis to examine the association between mental health services and the explanatory variables; (3) logistic regression analysis to show the pattern of mental health service-seeking behavior relative to race and ethnicity; and (4) stratified analysis to determine how factors differently affect mental health service visits by race/ethnicity. The major independent variable used in this model was race (i.e., White, African American, Asian/Pacific Islander, and Hispanic). Selfreported mental health visits served as the dependent variable. Population Studied: The authors conducted secondary data analysis from the 1998-1999 Community Tracking Study (CTS) household survey. Principal Findings: Persons from the lower income population make fewer visits to mental health care facilities than people with higher incomes. Significant effects of race/ethnicity remained when the data was examined for those individuals diagnosed with depression. Conclusions: Results of this study support the findings of the 2003 U. S. Surgeon General report documenting the unmet mental health needs of minorities in America. Racial/ethnic minorities face financial and structural barriers in accessing mental health services. Implications for Policy, Delivery, or Practice: Policies that will extend mental health coverage to the working poor are needed. Additional funding is needed to expand communitybased mental health clinics to improve access and quality of care, particularly for minority populations. Primary Funding Source: No Funding Source ●Outpatient Diabetes Care For Homeless and Housed Veterens: More Equal Than Not? Stefan Kertesz, M.D., MSc, Monika M. Safford, M.D., Stephanie A. Rose, M.D., Katri P. Palonen, M.D., Katharine Kirk, Ph.D., Catarina I. Kiefe, Ph.D., M.D. Presented By: Jewell H. Halanych M.D., MSc, Division of Preventive Medicine, University of Alabama at Birmingham, 1530 3rd Avenue South MT608, Birmingham, AL 35294; Tel: (334)444-5396; Fax: (205)935-7959; Email: jhalanych@mail.dopm.uab.edu Research Objective: National data suggest limitations in homeless persons' access to ambulatory care. No studies, however, compare utilization of ongoing care for homeless and housed outpatients in health systems designed to serve both groups. We used Veterans Health Administration (VHA) data to compare primary care entry, and utilization of ongoing care for homeless and housed VHA users with diabetes. Study Design: The proportion of VHA users achieving 1 or more Primary Care Visits (PC1) reflected entry to care. Ongoing care endpoints were proportions with 4 or more Primary Care Visits (PC4), and 1 or more Eye Clinic Visits (Eye). We made unadjusted comparisons between homeless and housed veterans using Chi-squared tests. The 3 multivariable logistic regressions adjusted for age, race, illness burden (Diagnostic Cost Groups (DCG)), mental illness, alcohol and drug abuse. Population Studied: All patients in 2003 national VHA data with >1 diabetes-related diagnosis were considered to have diabetes (n=735,897). “Homeless” patients were those using VHA homeless services or carrying an “absence of housing” diagnosis (n=8855, 1.2%). Principal Findings: Homeless persons were younger (mean (sd) age 54 (9) vs. 67 (11) years, for homeless vs. housed, respectively), had higher illness burden (DCG score 1.9 (1.6) vs. 1.0 (1.3)), and higher proportions with alcohol abuse (43% vs. 3%), drug abuse (36% vs. 1%) and mental illness (71% vs. 25%) (all p<.0001). While modestly fewer homeless (vs. housed) patients achieved primary care entry (PC1) (92% vs. 97%), more of the homeless obtained ongoing care: PC4 (59% vs. 47%), Eye (56% vs. 53%) (all p<.0001). After multivariable adjustment, the homeless had reduced odds ratios (OR) for PC1 (0.68, 95% CI 0.63-0.75), somewhat increased OR for PC4 (1.05, 95% CI 1.00-1.10) and modestly reduced OR for Eye (0.89, 95% CI 0.85-0.93). Models including all significant interactions did not qualitatively alter the findings. Conclusions: Homeless and housed diabetic VHA users had high (>90%) proportions entering primary care, although the homeless were moderately disadvantaged for this endpoint. In contrast, we did not find major disadvantages to homeless patients in measures of ongoing care. Our operational definition for homelessness probably selected for individuals with strong connections to VHA services. Implications for Policy, Delivery, or Practice: While national data indicate that not all homeless veterans obtain VHA services, our study suggests the VHA is able to achieve nearparity in utilization of ongoing care for diabetic homeless veterans who do. These findings should reinforce efforts to connect homeless veterans to VHA care. Primary Funding Source: VA, National Institute on Drug Abuse ●Rural-Urban Disparities in Access to Care for CYSHCN: A Tale of Two States Virginia Sharp, MS, ABD Presented By: Virginia Sharp, MS, ABD, Senior Research Associate, Center for Children with Special Needs, Children's Hospital & Regional Medical Center, 1100 Olive Way, Suite 500, Seattle, WA 98101; Tel: (206) 987-5311; Fax: (206) 9875741; Email: ginny.sharp@seattlechildrens.org Research Objective: The primary objectives of this research project were to (1) develop and test a methodology for identifying rural-urban differences in access to care for children and youth with special health care needs (CYSHCN) using the National Survey of Children with Special Health Care Needs (NS-CSHCN), and (2) evaluate rural-urban differences in access to care for CYSHCN between two seemingly similar states, Oregon and Washington. Study Design: Zip code level Rural Urban Commuting Area (RUCA) codes were linked to zip code of residence recorded for all Oregon and Washington respondents to the NSCSHCN and grouped into four categories--urban, suburban, large town, small town/rural. These RUCA groupings were used to analyze variables related to access to care and unmet service needs in the NS-CSHCN. Population Studied: The population included all children identified as CYSHCN in the NS-CSHCN residing in Oregon (n=745) and Washington (n=746). CYSHCN were identified using the CSHCN Screener, a set of five multi-part questions that identify children as having special health care needs based on the consequences of their health condition, rather than a list of specific diagnoses. Principal Findings: The NS-CSHCN includes information on need for and receipt of 14 types of child health services and 4 family support services. At the state level, Oregon and Washington look very similar, with no statistically significant differences between the states for any of these 36 variables. However, when the RUCA codes are used to disaggregate each state's data, different patterns of access to care and unmet needs appear for the two states. For child health services generally, in Oregon children living in suburban areas tend to be less likely to receive all needed routine preventive care, dental care and vision services. In Washington, children residing in large towns are more likely to have unmet child service needs, especially for dental care, specialized therapies, mental health care, and vision services. These same patterns also hold true for family services. In Oregon, suburban families have more unmet needs, while in Washington, families in large towns have more unmet needs. Comparing RUCA categories across the two states uncovers additional interesting differences in CYSHCN care needs and patterns of care. Conclusions: Even though Oregon and Washington are generally perceived to be very similar socially, politically, geographically and in other ways, they are not similar in terms of rural-urban disparities in access to care for CYSHCN. While the state sample sizes in the NS-CSHCN were too small to produce statistically significant differences for most access to care variables, those rural-urban disparities that were significant exhibited distinctly different patterns in the two states. Implications for Policy, Delivery, or Practice: This analysis indicates that the two states need to focus their resources for CYSHCN services differently to reduce access disparities related to rural-urban locational differences. More importantly, it highlights the need for more research on both intra- and inter-state patterns of health care resource distribution and access to those resource. Primary Funding Source: Oregon & Washington Departments of Health, CSHCN Programs ●Out-of-Pocket Health Spending Between Low- And Higher-Income Populations: What Factors Influence Financial Burden? Yu-Chu Shen, Ph.D., Joshua R. McFeeters, MPP Presented By: Joshua R. McFeeters, MPP, Graduate School of Business and Public Policy, Naval Postgraduate School, 555 Dyer Road, Code GB, Monterey, CA 93943; Tel: (831) 656-2951 Research Objective: In this paper, we explore the characteristics of adults and their families with low, moderate, and high financial burden from out-of-pocket health care spending. We focus on the following questions: 1. What are the social demographic determinants of financial burden for out-of-pocket spending? 2. Does private or public insurance coverage protect individuals from having a high burden of outof-pocket spending? 3. Does local health care market infrastructure help to reduce high out-of-pocket burden? Study Design: We obtained data on out-of-pocket health care spending, income, and other demographic and health insurance information primarily from the 2002 National Survey of America’s Families (NSAF). Health care financial burden was defined as the ratio of out-of-pocket health care spending to family income, and grouped into low, moderate, and high categories. Descriptive analyses compared the distribution of financial burden and demographic characteristics between low-income and higher-income populations. A multinomial logit model was used to examine the relative risk of having a high financial burden to a low burden for given individual and area characteristics. Separate multinomial logit models were done for low-income and higher-income populations because of the different spending patterns of the two groups. Population Studied: The population studied was 38,594 noninstitutionalized adults, ages 18 to 64 and their families who maintained the same type of health insurance coverage (employer-sponsored, private non-group, public or other) for the previous twelve months. The population was divided into two groups: low-income (income less than 200 percent of the Federal Poverty Level, FPL) and higher-income (income greater than or equal to 200% FPL). Principal Findings: 1. The effect of having unhealthy family members on financial burden is larger for higher-income adults than for low-income adults. 2. Employer-sponsored health insurance keeps the higher-income population from being in the high financial burden group relative to the uninsured higher-income population. However, low-income adults with employer-sponsored health insurance have a higher risk of being in the high financial burden group than uninsured, low-income adults. 3. Adults and families living in areas with high HMO enrollment have lower odds of high financial burden. For the low-income population, Federally Qualified Health Centers reduce the odds of high financial burden. Conclusions: 1. Low-income adults with family members in fair or poor health may be less willing and more constrained to spend on health care relative to higher-income adults with family members in fair or poor health. 2. Low-income adults and families with employer-sponsored coverage or all adults and families with private, non-group coverage have better health outcomes compared to uninsured adults and families, but are not protected from high financial burden. 3. Higher HMO enrollment and the presence of Federal Qualified Health Centers reduce the risk of high financial burden. Implications for Policy, Delivery, or Practice: It is important to understand factors that are associated with increasing or decreasing risks of high out-of-pocket health burden for adults and their families. Identifying these factors would help to more effectively target policies that reduce the financial burden of health care for both low-income and higher-income families. Primary Funding Source: RWJF ●Who are the Patients? Collection of Race, Ethnicity and Primary Language across U.S. Hospitals Donna Sickler, MPH, Marsha Regenstein, PhD Presented By: Donna Sickler, MPH, Research Analyst, National Public Health and Hospital Institute, 1301 Pennsylvania Avenue NW, Suite 950, Washington, DC 20004; Tel: (202)585-0100; Fax: (202)585-0101; Email: dsickler@naph.org Research Objective: Previous studies have attempted to determine the extent to which hospitals systematically collect information on patients’ race and ethnicity, but low response rates have impeded efforts to understand national practices. This study uses a more aggressive research methodology to survey acute care hospitals to develop estimates of data collection practices vis-à-vis race, ethnicity, and primary language. The study also examines operational aspects of data collection and the ways that race/ethnicity data is currently being used by clinical and administrative hospital staff. Finally, it identifies common barriers to data collection efforts. Study Design: Senior leaders from a representative sample of 500 acute care hospitals in the United States were surveyed by telephone in January/February 2005. The survey methodology and instrument were designed based on findings from an informal telephone survey of two dozen hospital CEOs who provided input into the content, proposed length, and preferred respondent for a successful response rate. Based on the CEO input, we identified chief financial officers and chief information officers to be the preferred respondents for the survey. The representative sample was drawn from the American Hospital Association database of U.S. hospitals. Findings were weighted to reflect the true distribution of hospitals by location in terms of urban/rural and census divisions. Population Studied: Acute care hospitals in the United States. Principal Findings: (Findings available March, 2005) Early evidence suggests that the majority of U.S. acute care hospitals collect some information on the race and ethnicity of patients, although the practices are highly variable and inconsistent within and across organizations. Fewer hospitals collect information on patients’ primary language, and only a small number of hospitals use this information in quality improvement efforts. Hospitals identified a number of barriers that serve as impediments to data collection efforts. Conclusions: Despite significant interest in disparities in health care both within and across institutions, current practices suggest that hospitals are only in their infancy in terms of data collection practices. Clearer direction from hospital leadership could substantially expand data collection efforts, which are often technologically possible but are not considered organizational priorities. Implications for Policy, Delivery, or Practice: Opportunities exist to improve data collection efforts to develop more robust sources of information about the quality of care received by individuals of different races and ethnicities. Given the nation’s strong interest in improving health information technology (HIT) and the overwhelming evidence of the existence of disparities in nearly all aspects of health care delivery, policies that encourage better and more consistent data collection, reporting, and analysis by race/ethnicity, within the context of improvements in HIT, could have a direct and immediate impact on the quality of care for all patients. Primary Funding Source: RWJF ●Differences in Utilization and Access Among Latinos and Asians in Alameda County Paula Song, MHSA, MAE, Catherine G McLaughlin, Ph.D. Presented By: Paula Song, MHSA, MAE, Doctoral Student, Department of Health Management and Policy, University of Michigan, 555 South Forest Street, Ann Arbor, MI 48105; Tel: (734)647-9604; Fax: (734)998-6341; Email: phsong@umich.edu Research Objective: While there have been numerous studies studying observed health disparities between Latinos and Whites and between Asians and Whites, there has been relatively little research investigating disparities between Latinos and Asians, particularly among the immigrant population. This paper helps fill that gap by examining differences in perceived health status and access, as well as self-reported utilization, among Latino and Cantonesespeaking Asian immigrants participating in a demonstration program in Alameda County, California. Study Design: We conducted a multi-wave telephone survey of enrollees in the Alameda Alliance Family Care health plan, part of the Robert Wood Johnson Foundation’s Communities in Charge (CIC) program. Surveys were conducted in English, Spanish, and Cantonese at three different times, at enrollment and at 6 and 12 months after enrollment. We analyze these data, comparing demographic, access, and utilization data at baseline and again after one year in the program. Population Studied: From August 2001 to January 2002, all new enrollees in the FamilyCare program were contacted. Over 80% participated. The sample for this research consists of 302 Asian and Latino adults who responded to all three waves of the survey. As required by the program, all adults were low-income uninsured parents of children who participated in Medi-Cal (S-CHIP). The two primary sources of enrollees were an Asian and a Latino health clinic. Reflecting this recruitment strategy, 97% of the sample population are immigrants. Principal Findings: Asian and Latino enrollees differed along several demographic characteristics. On average, Asians were older, more educated, and had higher household incomes than Latinos. Asians were significantly less likely than Latinos to have experienced a physician, emergency department (ED), or inpatient visit, and receive several preventive services. Controlling for individual characteristics, Latinos were more likely to utilize the ED. In addition, Latinos were significantly more likely to report more unmet needs and to have a usual source of care, both of which were significant predictors of ED use. Utilization levels for all services, except ED visits, increased significantly for both groups after enrollment. Asians continued to use the ED at significantly lower levels than Latinos, but differences in other types of utilization were no longer statistically significant. The percent of Asians reporting unmet needs did not change after enrollment, although the number of those reporting fair/poor health and having a chronic condition did increase. Conclusions: Prior to enrollment, Asians and Latino immigrants had different utilization patterns and perceptions of access to health services. After participating in a managed care program, these differences in utilization patterns were no longer significant, with the exception of ED visits. However, Latinos continued to report having more unmet needs, despite having similar utilization levels and fewer chronic conditions than Asians, suggesting more subtle cultural differences may account for differences in perception of access to care. Implications for Policy, Delivery, or Practice: Aggregating immigrants or ethnic groups may result in ineffective programs targeted at low-income uninsured immigrant groups. Programs that do not take into consideration differences in utilization and perceptions may not design the “right” program to address the needs of the uninsured and immigrant population. Primary Funding Source: RWJF ●Outcomes for Rural Patients who Travel for Care Sharon Sweeney Fee, RN, Ph.D. Presented By: Sharon Sweeney Fee, RN, Ph.D., Assistant Professor, College of Nursing, Montana State UniversityBozeman, P.O. Box 173560, Bozeman, MT 59717; Tel: (406) 994-2705; Fax: (406)994-6020; Email: sfee@montana.edu Research Objective: The purpose of this research was to look at the impact of distance on hospital outcomes for rural patients using risk adjustment to understand the relationship between distance and risk adjusted patient health outcomes. Study Design: Regression analysis was used to identify variations in outcome between groups of patients who traveled between 30 and over 800 miles for care. The outcomes measured included number of procedures and length of stay. Patient characteristic used in the study included payer, type of admit and source of admit and hospital size, diagnosis related group (DRG), type of service, the number of therapeutic and diagnostic services, and the number of secondary diagnoses. Population Studied: Using GIS technology, one year of Arizona hospital discharge data was analyzed and resulted in 20,926 cases of rural patients who traveled over 30 miles for health care between July of 2001 and June of 2002. Principal Findings: When controlling for age, distance was significant at the p = .01 level for the outcomes of number of procedures and length of stay. The negative Beta (-.03) in the procedures analysis demonstrates that the farther the patients travel, the fewer number of procedures they receive and the greater the length of stay. Significance (p<.01) was also found between a majority of the patient characteristics and both outcomes demonstrating the variation in type of rural dweller that travels for health care. Conclusions: The results of this study demonstrate that new characteristics may need to be part of rural health research and federally funded projects. Both outcomes were significantly related to distance traveled. These outcomes demonstrate new opportunities to develop more effective and efficient interventions for rural patients. Implications for Policy, Delivery, or Practice: In 2005, the IOM endorsed the overriding principle that “all rural Americans should have access to the full spectrum of highquality, appropriate health care.” This study demonstrates one method toward an improved understanding of health outcomes for rural Americans. Primary Funding Source: No Funding Source ●Educational Attainment And Cancer Mortality, 1959 2001: Patterns, Trends, And Pathways Elizabeth Tarlov, Ph.D., Robert Kaestner, Ph.D., Richard Warnecke, Ph.D. Presented By: Elizabeth Tarlov, Ph.D., Post-doctoral Fellow, Midwest Center for Health Services and Policy Research, Hines VA Hospital, PO Box 5000 (151H), Hines, IL 60141; Tel: (708)202-2254; Email: elizabeth.tarlov@med.va.gov Research Objective: A substantial body of empirical research evidence supports the existence of a causal link between educational attainment and health but little is known about the relationship between education and cancer. This study examined associations between educational attainment and cancer mortality in the United States between 1959 and 2001 and interpreted findings in light of changing technological, policy, and cultural contexts. Examining the relationship in an historical context can provide valuable insight into the involved pathways which are incompletely understood. Study Design: Census and mortality data on gender-race-agespecific subpopulations within states were used to estimate the effect of educational attainment on cancer mortality in five decennial time periods (1959-1961 to 1999-2001). Dependent variables were deaths due to lung, colon, breast, and prostate cancer and to all cancers combined. Estimates were obtained in gender-specific models using negative binomial regression and accounted for age, income, marital status, and timevarying state effects. Robust standard errors accounted for clustering within states. Population Studied: U.S. White and Black adults aged 45 years and older in the last four decades of the 20th century. Principal Findings: In 1959-1961, education had positive effects on lung and breast cancer mortality among women and on all cancers combined, lung, colon, and prostate cancers among men. There were no education effects in the following three time periods among women. Positive but nonlinear effects for lung and breast cancer re-emerged in the 1999-2001 data. Among men, education had less positive effects in later decades and in 1999-2001 education had a negative effect on mortality due to prostate cancer and to all cancers combined. Conclusions: Education effects varied by gender, cancer site, and over time and were often nonlinear. Based on theory and existing research evidence, it was hypothesized that time trends in education effects would be negative and that education effects on cancer mortality in 2000 would be negative and graded. However, time trends in education effects, although generally negative between 1960 and 1970, were characterized by a variety of patterns and changes in direction in subsequent years. Further, there was no evidence of a gradient in education effects on cancer mortality. Trends in the correlation between education and proximate determinants of cancer or cancer outcomes (for example, health behaviors and utilization of early detection services) may explain some of the patterns observed but the mechanisms that produced others remain unclear. Implications for Policy, Delivery, or Practice: The results suggest that education effects on cancer do not parallel those found for all-cause and cardiovascular disease mortality and for other measures of health and functioning such as selfrated health. Further refinement of theoretical pathways linking societal context, educational attainment, and cancer will be important to future progress in understanding these relationships and reducing social and economic disparities in health. Finally, research on the relationship between social position and cancer is hindered by the absence of socioeconomic information in large cancer datasets. An additional contribution of this study, therefore, is its demonstration of the advantages and limitations of using non-cancer datasets within a sound research design to address questions related to education and cancer. Primary Funding Source: Pre-doctoral traineeship ●A Comparative Evaluation of the Cost Effectiveness of Treating the Metabolic Syndrome in the African American and General Population Joseph Tasosa, MS, MBA, Richard Schuster, M.D., MMM, John McAlearney, Ph.D. Presented By: Joseph Tasosa, MS, MBA, Research Assistant, Community Health, Health Systems Management, Wright State University, 3139 Research Boulevard, #205, Kettering, OH 45420; Tel: (937) 258-5555; Fax: (937) 258-5544; Email: joseph.tasosa@wright.edu Research Objective: To assess the cost effectiveness of early treatment of three Metabolic Syndrome (MS) risk factors in the African American and general population. To compare the cost-effectiveness of early treatment of three MS risk factors in the African American and general population. Study Design: A cost effectiveness analysis was carried out using a Markov decision model to compare early treatment and late treatment of three MS risk factors (hyperlipidemia, diabetes and hypertension) in African Americans and the general population. The main outcome measure was the incremental cost per Quality Adjusted Life Year (QALY). Population Studied: African American population and the general population in the United States. Principal Findings: With the exception of early treatment of hyperlipidemia in African Americans ($187,462/QALY), early treatment of individual MS risk factors at age 30 was found to be cost effective (<$27,000/QALY) for both African Americans and the general population. The incremental cost of treating hyperlipidemia, diabetes and hypertension simultaneously in African Americans and the general population at age 30 was $53,140/QALY and $63,926/QALY respectively. With the exception of treatment of hyperlipidemia, early treatment strategies targeted at African Americans were found to be more cost effective than those targeted towards the general population. Sensitivity analyses indicated that age and cost of treatment were the most influential factors in the model. The cost effectiveness of early treatment of MS risk factors in blacks and the general population compares favorably with similar health care interventions. Conclusions: Early treatment of MS risk factors saves lives in a cost effective manner. The study supports a growing body of literature that indicates the cost effectiveness of providing preventative services to apparently healthy individuals. Our study also shows that disparate access to quality health care makes African Americans especially susceptible to the adverse effects of MS. We show that reducing these racial disparities by providing early treatment is cost effective. Implications for Policy, Delivery, or Practice: Proactive health policies that provide preventative services early are more beneficial and more cost effective than reactive policies that provide services later. Proactive policies may help reduce health disparities between African Americans and the general population. Primary Funding Source: No Funding Source ●Barriers to Vaccination Against Influenza in CommunityDwelling Veterans With Dementia: The Role of Caregiver Depression Joshua Thorpe, MPH, Betsy Sleath, Ph.D., RPh, Courtney VanHoutven, Ph.D., Lawrence Landerman, Ph.D., Elizabeth Clipp, Ph.D., RN Presented By: Joshua Thorpe, MPH, Doctoral Candidate, Pharmaceutical Policy and Evaluative Sciences, UNC - Chapel Hill, 323 Columbia Place East, Chapel Hill, NC 27516; Tel: (919) 928-8757; Email: thorpej@unc.edu Research Objective: The primary aim of this study is to examine the association between informal caregiver depressive symptoms and access to annual influenza vaccination in community-dwelling elderly with dementia. We hypothesize that greater levels of caregiver depression are associated with decreased likelihood of patient vaccination. A secondary aim of this study is to determine whether depression mediates the relationship between other predisposing, enabling, and need variables and access to flu shots. Study Design: Independent variables were collected as part of the first wave of the National Longitudinal Caregiver Sample, a longitudinal investigation of primary informal caregivers of elderly (age 60 and older) male U.S. veterans with dementia. The NLCS identified a national sample of veterans with at least one outpatient visit for dementia to a VA facility in 1997. Independent variables, collected in early 1998, were used to predict veterans’ receipt of flu shots during the 1998 influenza vaccination season. We examined VA Outpatient Data Files for visits occurring between September 1 and December 31, 1998 with a clinic stop code or CPT code indicating flu shot administration. Our primary independent variable was caregiver depressive symptoms as measured by the Center for Epidemiologic Studies Depression Scale short Boston form. The CES-D scale ranges from 0-20, with higher scores indicating greater depressive symptomatology. The selection of other independent variables was guided by the Andersen behavioral model of health service use. Predisposing variables included caregiver (CG) age, CG education, CG race, CG relationship to veteran, and veteran age. Enabling variables included CG perceived financial adequacy, veteran insurance coverage, CG physical health, CG social support, and region of country. Medical need variables included veteran behavioral disturbance, duration of dementia symptoms, and comordid conditions. A structural equation model was used to estimate direct and indirect path coefficients between independent variables, caregiver depression, and veteran vaccination against influenza. Population Studied: 1,424 community-dwelling male veterans with dementia and their informal caregivers. Veterans less than 65 years of age, those with no VA outpatient visits in the previous year, and those who died or entered a nursing home anytime during the flu shot season were excluded. Principal Findings: Results support our hypothesis that greater caregiver depressive symptoms are associated with a decreased likelihood of dementia patient vaccination against influenza. Further, CG depressive symptoms mediated the relationship between several predisposing, enabling, and need variables and the likelihood of vaccination. The following independent variables had a significant indirect effect on likelihood of vaccination via their influence on caregiver depression: CG social support, CG physical health, CG perceived financial adequacy, veteran depressive symptoms, and veteran level of irritability/aggression. Conclusions: We found that informal caregivers' depressive symptoms decreased the likelihood of vaccination against influenza in community-dwelling elderly with dementia. Results also showed that several independent variables exert their effects on likelihood of vaccination by influencing caregiver depression. Implications for Policy, Delivery, or Practice: Access to medical care in community-dwelling dementia patients may be improved directly by detecting and treating caregiver depression, and indirectly by addressing pathways to caregiver depression. Primary Funding Source: AHRQ, American Foundation for Pharmaceutical Education ●Do Black Patients Still Have Lower 30-day Mortality Than White Patients Within VA? Kevin Volpp, M.D., Ph.D., Roslyn Stone, Ph.D., Aashish Jha, M.D., Judith Lave, Ph.D., Mark Pauly, Ph.D., Heather Klusaritz, MSW Presented By: Kevin Volpp, M.D., Ph.D., Assistant Professor of Medicine and Healthcare Systems, School of Medicine and the Wharton School, University of Pennsylvania, 1232 Blockley Hall, 423 Guardian Drive, Philadelphia, PA 19104; Tel: (215) 573-0270; Fax: (215)573-8778; Email: volpp70@mail.med.upenn.edu Research Objective: Several studies have shown that Black patients hospitalized within the VA system have lower 30 day mortality than White patients. We examined whether these differences (1) exist for conditions for which hospital admission is generally not discretionary; (2) persist over time; and (3) are due to within hospital differences in outcomes as opposed to a non-random distribution of patients between facilities of differing average outcome. Study Design: We conducted an observational study using VA data in the National Patient Care Database on 30-day mortality for six conditions over a 7-year period. We used random effects logistic regression to assess differences in 30-day mortality between Black and White patients hospitalized with each of these conditions, with hospital site as the random effect and covariate adjustment for age, gender, fiscal year, and 30 comorbidities. We assessed interactions involving race and time, and assessed whether the racial disparities varied across hospitals by including a random coefficient for race. Population Studied: 340,982 Black or White patients hospitalized with one of the following conditions at VA hospitals nationwide between fiscal years 1996 and 2002: acute myocardial infarction, congestive heart failure, gastrointestinal bleeding, hip fracture, pneumonia, or stroke. Principal Findings: For each condition, Black patients had consistently lower 30-day mortality than White patients, with an estimated odds ratio (OR) of 30-day mortality of 0.84 (95% CI: 0.76-0.92) for acute myocardial infarction, OR=0.71 (95% CI: 0.66-0.76) for congestive heart failure, OR=0.89 (95% CI: 0.81-0.98) for gastrointestinal bleeding, OR=0.66 (95% CI: 0.53-0.82) for hip fracture, OR= 0.93 (95% CI: 0.88-0.99) for pneumonia, and OR=0.89 (95% CI: 0.82-0.97) for stroke (p<0.02 for each). The ORs of black to white mortality did not change substantially when adjustments for site were added, indicating that the overall racial difference in outcomes is predominantly due to within-site differences in outcomes between Whites and Blacks. The hypothesis that the ORs of black to white mortality were consistent in each year between 1996 and 2002 could not be rejected for any condition (p>0.26 for each condition). Conclusions: Black patients had lower 30-day mortality than White patients for six common conditions treated in VA hospitals between 1996 and 2002. The degree of reverse disparity appears to reflect within-site differences in outcomes by race rather that the possibility that Blacks may be treated in hospitals with lower mortality rates and was consistent over this time period for all conditions. Implications for Policy, Delivery, or Practice: Lower mortality rates exist for blacks than whites within the VA system. Determining the degree to which this is due to selection as opposed to treatment effects is important to understanding how well the VA is treating health disparities. Primary Funding Source: VA ●Marital Status and Cancer Screening Disparities among Older Latina and Non-Latina Women Melanie Wasserman, Ph.D, Melissa A. Clark, Ph.D., William Rakowski, Ph.D. Presented By: Melanie Wasserman, Ph.D, Post-doctoral fellow, Center for Gerontology and Health Care Research, Brown University, 2 Stimson Avenue, Box G-St311, Providence, RI 02912; Tel: (401)863-9036; Fax: (401)863-3489; Email: Melanie_Wasserman@brown.edu Research Objective: Women who do not follow traditional gender roles may be at a disadvantage in accessing preventive health services. Unmarried status is often used as a control variable in multivariate analyses of cancer screening, but has rarely been studied in and of itself as a source of health care disparities. This study examined disparities in utilization of cervical, breast, and colorectal screening as well as availability of a usual source of care by marital status, comparing Latinas and non-Latinas. Study Design: Cross-sectional analysis of 2003 Behavioral Risk Factor Surveillance System (BRFSS) data. Bivariate tabulations were done of marital status (married, never married, divorced/ separated, widowed, member of unmarried couple) against recent cervical, breast and colon cancer screening and availability of a usual source of care. Tabulations were stratified by ethnicity (Latina, non-Latina) and language (Spanish, English). Multivariate analyses were used to control for confounders (age, insurance, having a regular doctor, delayed care due to financial considerations, health status). Analyses were adjusted for sampling weights and survey design. Population Studied: Married and unmarried women between the ages of 40 and 75 who were interviewed in English or Spanish for the 2003 BRFSS. Analyses of cervical cancer screening were restricted to women who had not had a hysterectomy. Analyses of colorectal cancer screening were restricted to women over 50. Principal Findings: For all three populations (non-Latinas, Latinas and Spanish-speaking Latinas), access to a primary care doctor is highest for married women, followed by the widowed, divorced or separated, and never married, with the greatest disparity affecting members of unmarried couples. There was a 30 percentage point gap between married nonLatinas and Spanish-speaking Latinas who were members of an unmarried couple (92% vs. 62%). Cervical cancer screening rates were high (between 80 and 85%) for married women in all three groups, with only slightly lower rates (between 77 and 82%) for the unmarried. Colon cancer screening rates were low for all groups (44% for all groups combined). Latinas, particularly Spanish speakers, remained at a disadvantage in breast and colon cancer screening relative to non-Latinas, and being married remained the category with the highest utilization of cancer screenings for all three subpopulations. Marital status operated differently for breast and colon cancer screening, as well as for Latinas vs. nonLatinas. Members of unmarried couples had the lowest colon cancer screening rates among all three subpopulations, but Latina members of unmarried couples had the highest breast cancer screening rates of any group (66%). Disparities persisted after controlling for confounding factors. Conclusions: Unmarried women, both Latina and non-Latina, are less likely than their married counterparts to use cancer screening services. Marital status operates differently among Latinas and non-Latinas. Implications for Policy, Delivery, or Practice: Providers of cancer screening services should target their outreach efforts to unmarried women. Further research is needed to better design outreach strategies specific to never married, divorced, widowed, or separated women. The effect of marital status on cancer screening is different among Latinas, and should be studied separately for this population. Primary Funding Source: AHRQ, ●Disability and Clinical Preventive Services Wenhui Wei, Ph.D., Patricia Findley, DrPH, MSW, Usha Sambamoorthi, Ph.D. Presented By: Wenhui Wei, Ph.D., Assistant Reserach Professor, Institute for Health, Health Care Policy, and Aging Reserach, Rutgers University, 30 College Avenue, New Brunswick, NJ 08901; Tel: (732)932-0365; Fax: (732)932-8592; Email: wwh@rci.rutgers.edu Research Objective: Individuals with disabilities constitute 21% of the overall U.S. population and 53% of individuals with disabilities are women. Low utilization of clinical preventive services among people with disabilities may lead to poor health and decreased independence and hamper the fullparticipation of these individuals in the society. The objective of the study is to examine patterns of clinical preventive services use among adults with disabilities and compare these patterns to adults without disabilities. Study Design: Secondary data analyses of longitudinal household component of the Medical Expenditure Survey (MEPS) for the calendar years 1999 through 2001. Disabled individuals were identified as those who had difficulty in any area of activity of daily living as a result of their impairment or problems in body function, including psychological functions for two calendar years. Recommended preventive health services consisted of cervical and breast cancer screening for women, colorectal, cholesterol screening and annual influenza immunization for both men and women. Group differences were tested with chi-square statistic. Multiple regressions were used to examine patterns of clinical preventive services use. Population Studied: Study sample included 3,067 community-dwelling individuals who were aged 51 to 64, followed for two years, and alive at the end of follow-up period. Principal Findings: Overall, 21% of the study sample reported having a functional limitation for two calendar years. Among disabled individuals, 77% reported receiving mammogram, 75% Papanicolaou (Pap) test, 88% received cholesterol screening within the recommended period and 45% reported annual influenza immunization. Only a third of the study sample reported ever receiving colorectal cancer screening. Multivariate regressions revealed that disabled individuals were more likely to receive annual influenza immunization and less likely to receive Pap tests. We did not find significant differences in receipt of other preventive services. Among disabled individuals significant demographic and socioeconomic differences were found. Conclusions: Disabled women were less likely to receive some of the cancer screening services suggesting barriers to accessing health care services for women with disabilities. Some of the clinical preventive services care remained below targeted goals for Healthy People 2010. Implications for Policy, Delivery, or Practice: Interventions to promote cervical cancer screening among women with disabilities are needed. Primary Funding Source: Institute of Child Health and Disability. Medical Rehabilitation ●Testing Theories of Discrimination in Health Care: Evidence from New York’s CABG Report Card Rachel Werner, M.D., Ph.D. Presented By: Rachel Werner, M.D., Ph.D., Assistant Professor, Department of Medicine, Univeristy of Pennsylvania, Blockley Hall, Room 1208; 423 Guardian Drive, Philadelphia, PA 19104; Tel: (215) 898-9278; Fax: (215) 5738778; Email: rwerner@wharton.upenn.edu Research Objective: Evidence suggests that disparities in health care utilization stem in part from discrimination in the physician-patient interaction. Two theories have been suggested to explain why this discrimination exists. The first hypothesizes that physicians are biased against minority patients and thus treat black and white patients differently (also called taste-based discrimination). The second suggests that imperfect information causes clinical uncertainty about an individual patient’s treatment benefit. Therefore, physicians categorize patients by racial or ethnic group and base treatment decisions on the group’s average treatment benefit rather than an individual’s treatment benefit. Also called statistical discrimination, this theory suggests that disparities exist because physicians believe that minority patients have less treatment benefit on average compared to white patients. The objective of this study is to test these two theories of discrimination. Study Design: In December 1991, New York began publishing coronary artery bypass graft (CABG) report cards, which publicly rate cardiac surgeons on their patients’ risk-adjusted mortality rates following CABG surgery. Using this exogenous shock, I test for changes in disparities in CABG use to test these theories of discrimination. If racial and ethnic differences in CABG use stem from clinical uncertainty, and surgeons believe that racial and ethnic minorities will have worse outcomes than white patients, surgeons will preferentially treat white patients after report cards are released, increasing racial and ethnic differences in CABG use. Alternatively, if differences in CABG use are only due to tastebased discrimination, and clinical uncertainty plays no roll in these differences, CABG report cards will not change racial and ethnic differences in CABG use. To test these hypotheses, I use multivariate regression to estimate differences in CABG rates between white versus black and Hispanic patients in New York before and after New York’s first CABG report card was released, compared to rates of CABG surgery between white versus black and Hispanic patients over the same time period in 12 control states. I also estimate differences in cardiac catheterization and percutaneous transluminal coronary angioplasty (PTCA) rates and in-patient mortality rates. Population Studied: All patients hospitalized with a principal diagnosis of acute myocardial infarction (AMI) were identified in hospital discharge data from New York and the Nationwide Inpatient Sample (HCUP-3) during the study period (1988 to 1995). A total of 928,551 patients were identified: 310,412 from New York and 618,139 from the control states. Black and Hispanic patients accounted for 13.7% of patients in New York and 9.8% of patients in the control states. Principal Findings: Racial and ethnic differences in CABG use rose significantly in New York after New York’s CABG report card was released compared to changes in racial and ethnic differences in the control states. At the same time there were no significant changes in the rates of cardiac catheterization and PTCA. Despite the increase in racial and ethnic differences in CABG use in New York, there was no detectable change in in-patient mortality rates following AMI in New York compared to the control states. Conclusions: The increase in racial and ethnic differences in CABG use following the release of New York’s CABG report card is consistent with statistical discrimination as a cause of racial and ethnic disparities in health care utilization, rather than taste-based discrimination or bias. In this case, statistical discrimination did not impact in-patient mortality rates. Implications for Policy, Delivery, or Practice: Future interventions aimed to decrease disparities from discrimination in the physicians-patient interaction should address the mechanism of clinical uncertainty in statistical discrimination. Primary Funding Source: AHRQ ●What do the Disabled Report about their Experience with Medicare? ADL Disability and CAHPS Measures among Medicare Fee-for-Service Beneficiaries Nathan West, MPA, Celia Eicheldinger, MS, Shulamit L. Bernard, Ph.D., RN Presented By: Nathan West, MPA, Health Research Associate, Health Services and Social Policy Research, RTI International, 3040 Cornwallis Road, RTP, NC 27709; Tel: (919)541-6816; Email: nathanwest@rti.org Research Objective: To examine patterns of reported experiences and satisfaction with health care services among Medicare Fee-for-Service beneficiaries with difficulty or inability in performing activities of daily living (ADL). We differentiate between disability as defined by Medicare entitlement and reported disability as measured by ADL functioning. Study Design: Data come from the 2003 Medicare CAHPS Fee-for-Service survey, a cross sectional, national survey of Medicare beneficiaries that includes 107,893 survey respondents. We exclude beneficiaries with ESRD and those under 65 without disability as original reason for entitlement. The regression models included two variables created from survey responses and information provided from the Enrollment Database: ADL limitation and Medicare Entitlement. The ADL limitation variable has three levels: no ADL difficulties, mild ADL difficulties, and severe ADL difficulties. The Medicare Entitlement variable also has three levels: greater than or equal to 65 and Aged into Medicare; less than 65 and Medicare Entitlement by Disability; and greater than or equal to 65 and Medicare Entitlement by Disability. Case-mix variables race, ethnicity, insurance status, and whether or not the beneficiary had a personal doctor were also added to the regression models. All models were weighted to reflect the full Medicare Fee-for-Service population. Population Studied: Beneficiaries enrolled in the Medicare Fee-for-Service program during 2003. Principal Findings: In general, we found a linear relationship between extent of disability and CAHPS scores. Regardless of a beneficiary’s original Medicare entitlement status, the greater the level of difficulty with ADL functioning, the lower Medicare beneficiaries rate the Medicare program and their overall health care. We found this also to be true for composite measures of beneficiaries’ experiences with health services in Medicare, particularly whether or not they received needed care and had good communication with their providers. Conclusions: Our findings suggest that the severity of a disabling condition, as measured by ADLs, does account for variation in expectations and satisfaction in the Medicare program. Even among beneficiaries whose reason for entitlement was disability, there was a linear trend between functional disability and satisfaction and experience. While prior work demonstrated that disabled Medicare beneficiaries reported worse experience with their health care, this study suggests that even among the disabled those with functional disability report lower satisfaction and worse experience. Implications for Policy, Delivery, or Practice: The findings suggest that despite the insurance coverage offered by the Medicare program, beneficiaries with ADL functional limitations and potentially the greatest health care needs experience more barriers and delays to obtaining health care services. Primary Funding Source: CMS ●Ensuring Low-Literate Adult Access to Online Health Information: Developing a Research Program Pamela Whitten, BSM, MA, Ph.D., Michael Mackert, BS, MA, Brad Love, BS Presented By: Pamela Whitten, BSM, MA, Ph.D., Associate Professor, Telecommunication, Michigan State University, 409 Comm Arts Building, East Lansing, MI 48824; Tel: (517)432-1332; Fax: (517)355-1292; Email: pwhitten@msu.edu Research Objective: Researchers at Michigan State University studied the potential for a website to deliver health information to adults with low levels of literacy. Study Design: MSU researchers created a website to provide diabetes information to adults with low literacy levels. The website was designed with Flash technology to provide the health information primarily via images, animations, and audio. The website performed like a slideshow, controlled play, pause, and reverse controls. Even research participants who had never used a computer before were able to successfully navigate and control the website. Research participants were tested for diabetes knowledge before and after viewing the website to determine if the site increased their knowledge of diabetes. Subjects also completed the short version of the Test of Functional Health Literacy in Adults (TOFHLA). To conclude their participation in the study, subjects were interviewed in-depth to learn more about their experience using the website. Population Studied: Research subjects were recruited from a variety of outlets to find adults with lower levels of literacy, including community neighborhood centers and health outreach support groups. Many of these individuals were from lower income groups that would typically be eligible to receive Medicaid support. Principal Findings: Results show that subjects, in general, improved their diabetes knowledge as a result of going through the website. Interview results made it clear that participants approved of and enjoyed the website, particularly an interactive component that allowed subjects to assess their possible risk of developing diabetes. Conclusions: This pilot project helps to demonstrate that lowliterate populations can receive health information via websites that are designed with this group in mind. Some participants even said they prefer receiving information from such a website, citing greater privacy and ease of access. Further research to develop websites based on feedback received from participants, as well as confirming the results with other health information, will be a useful next step. Implications for Policy, Delivery, or Practice: It is evident that even adults with low levels of literacy can benefit from the provision of health information online, and it is possible that such material could be vastly more useful to certain adults than traditional print materials that are used in patient education. Further research needs to be conducted to learn more about what works and what does not in using websites to deliver health information to this underserved population, but the potential cannot be ignored and could quickly become a valuable tool for patient education. Primary Funding Source: Medicaid Office in the State of Michigan ●Racial Disparities in Pneumococcal Vaccination Among Managed Care Seniors Carla Winston, Ph.D., MA, Adrienne Mims, M.D., MPH, Michael Blue, MHSA, Kecia Leatherwood, MS, Pascale Wortley, M.D., MPH Presented By: Carla Winston, Ph.D., MA, National Immunization Program, Centers for Disease Control and Prevention, 1600 Clifton Road NE Mailstop E-52, Atlanta, GA 30333; Tel: (404)639-6248; Fax: (404)639-8614; Email: ctw3@cdc.gov Research Objective: One-time pneumococcal vaccination is recommended for all persons age 65 years and older, yet marked racial/ethnic differences in pneumococcal vaccine coverage exist. According to 2004 National Health Interview Survey (NHIS) data for persons over age 64 years, 61.6% of non-Hispanic Whites compared to 34.5% of non-Hispanic Blacks have received pneumococcal vaccine. We surveyed managed care patients to assess disparities in pneumococcal vaccination and reasons for nonvaccination among older African Americans and Whites in a managed care population. Study Design: We randomly sampled from five general medicine clinics 1198 Atlanta, Georgia HMO members over age 64 years whose electronic medical records indicated they were unvaccinated. Patients were asked, “Have you ever had a pneumonia shot?” and if unvaccinated, “What would you say is the main reason you have not had a pneumonia shot?” Unvaccinated patients were told they were indicated for pneumococcal vaccination and that vaccination was a covered benefit of their managed care insurance with no copayment. Unvaccinated patients were asked, “Would you like to get a pneumonia shot?” and had the opportunity to schedule a clinic visit for vaccination. Patients were asked to self-report race, ethnicity, and education level, since these variables were not in medical records. Population Studied: 850 (71%) sampled patients were surveyed by telephone in August 2004 regarding pneumococcal vaccination and attitudes towards pneumococcal vaccine. 61% of respondents were female; 48% were non-Hispanic Black; mean age was 72.2 years. Principal Findings: 377 patients (44%) reported that they had previously received pneumococcal vaccine. One quarter of patients reporting prior vaccination had recently been vaccinated after receiving a mailed reminder. Vaccinated patients were older than the unvaccinated (73.2 v. 71.5 years, p < 0.0001) but there was no significant difference in length of HMO enrollment, gender, or educational attainment. However, non-Hispanic Blacks were significantly less likely to report prior vaccination than non-Hispanic Whites (33% v. 51%, p < 0.0001). Overall, 41% of the unvaccinated did not know they needed a pneumococcal shot, 14% were concerned the shot would make them sick, 14% did not want the shot, and 9% stated they were not at risk for pneumonia, with no significant differences by race. When the pneumonia shot was offered, 63% of Whites stated they would like to get the shot versus 55% of Blacks (p = 0.10). Black patients were more likely than Whites to say they were unsure whether they would like to get the shot (17% v. 9%, p = 0.03). The percentage of patients who subsequently scheduled a clinic visit for vaccination did not differ statistically by race (44% of Whites v. 37% of Blacks, p = 0.15). Conclusions: Little is currently known about why racial disparities exist in managed care populations with presumably equal access to care. We will follow patients for six months to determine which patients are vaccinated and what factors are predictive of patients completing a scheduled clinic visit. Vaccination outcomes through February 2005 will be presented. Implications for Policy, Delivery, or Practice: Data from this study will be used to improve clinical outreach and education to patients regarding pneumococcal vaccination. Primary Funding Source: CDC, Kaiser Permanente, Atlanta, GA ●What’s Behind the Observed Disparity of Health Care Use and Expenditure? Diana Wobus, Ph.D. Presented By: Diana Wobus, Ph.D., Senior Analyst, Survey Operations, Westat, 1650 Research Boulevard, Rockville, MD 20850; Tel: (240) 453-2967; Fax: (301) 294-2038; Email: dianawobus@westat.com Research Objective: This study is an investigation on explanations for disparities observed in health care use and expenses found in a previous study. In a study, the utilization and expenditures of health care services was found different among people of different incomes. As a follow-up, clinical information on the study population was used to determine whether or not the disparity results from different levels of need for health care. Study Design: The 2001 Medical Expenditure Panel Survey data were used. The analysis unit is at person level. Linear regressions were used to determine if the differences of use and expenses among people of different incomes result from health status or medical conditions for which health care services were sought. The dependent variables are the number of visits (for ambulatory care) or hospital nights (for inpatient care) and the expenses (i.e. payments) associated with the services. The independent variables are household reported diagnosis (based on ICD-9 condition codes), selfreported health status in addition to a number of economic and demographic characteristics. Population Studied: The study population included the U.S. uninstitutionalized population. MEPS collects data on health care services from nationally representative samples. Principal Findings: The null hypothesis is that health status and conditions do not explain the disparity; thus the disparity observed in the previous study results primarily from economic or demographic characteristics, such as income or race. The alternate hypothesis is that the disparity is a function of health needs controlling for economic (resulting in insurance disparity) or demographic characteristics. The preliminary findings reveal that people of lower incomes used the health care services less frequently than people of higher incomes. However, for those people of lower incomes who used the health care services, average payment for their services tend to be higher for hospital services but lower for office-based visits. Analyses of use and expenses based on medical conditions and controlling for income levels and insurance confirmed that a major portion of the disparity is a direct function of the need for services as it relates to the severity of health problems. Conclusions: Claims on disparity of health care use and expenditures based entirely on demographic characteristics can be misleading if clinic information is ignored. By controlling for need for health care, interpreted in diagnosis or procedures, the study on disparity can reflect the real world. Primary Funding Source: Westat ●Standardized Measurement and Assessment of Health Disparities and Culturally and Linguistically Appropriate Services in Managed Care – a Feasibility Study Lok Wong, MHS, Sarah Hudson Scholle, MPH, DrPH, Alexandra Love, MPH Presented By: Lok Wong, MHS, Senior Health Care Analyst, Quality Measurement, National Committee for Quality Assurance, 2000 L Street, NW, Suite 500, Washington, DC 20036; Tel: (202)955-1784; Fax: (202)955-3599; Email: wong@ncqa.org Research Objective: This research study aims to explore and identify feasible methods for monitoring and measuring health disparities and the delivery of culturally and linguistically appropriate services (CLAS) by managed care organizations (MCOs) to diverse populations. The research objective is to understand the current state of evidence supporting common quality expectations in managed care and inform the field on potential methods for standardized measurement and assessment. Study Design: We identified key concepts and areas for potential evaluation and measurement based on a literature review on health disparities and CLAS and through an expert panel consensus process. We conducted qualitative key informant interviews to understand the feasibility of proposed evaluation areas identified and quantitative analysis of Medicare HEDIS data by race/ethnicity and CAHPS patient experience of care to examine the feasibility of reporting standardized performance measures by race/ethnicity or language. Population Studied: Populations including commercial, Medicare, Medicaid managed care. Interviews with managed care plans, purchasers, researchers, and consumer/advocacy groups. Principal Findings: Topics for potential evaluation of managed care organizations were identified under three broad areas: Linguistic Access, Cultural Competence and Reducing Health Care Disparities; specific topics included, infrastructure for data collection and quality improvement, ability to conduct subgroup analyses by race/ethnicity, providing effective language access, culturally competent care at the point of care, engaging communities and qualified interpretation services. These topics and areas resonated with key informants, including health plans, but operational definitions of common quality expectations and evaluation approaches need further refinement and flexibility to be feasible across all plans and gain consensus in all stakeholder groups. Conclusions: Managed care plans are interested in evaluating the quality of services received by culturally, linguistically and racially diverse populations and identifying opportunities for quality improvement. Informing MCOs of approaches feasible for monitoring the quality of health care services received by diverse populations may furnish MCOs with needed tools to begin to address and understand disparities and issues of CLAS within their organization, such as understanding health care needs of their diverse populations. Encouraging MCOs to use standardized measurement and assessment tools to assess potential disparities and services to diverse populations may her facilitate our understanding of gaps in quality of care received by diverse populations in managed care. Implications for Policy, Delivery, or Practice: Introduction of standardized measurement and assessment of MCOs may lead to accountability to the health of diverse populations, and improve the quality of care and services delivered through managed care. Primary Funding Source: The California Endowment ●Improving Use of Prescription Medications Helen Wu, M.Sc., Robyn Y. Nishimi, Ph.D., Christine M. PageLopez, Kenneth W. Kizer, M.D., MPH Presented By: Helen Wu, M.Sc., Program Director, National Quality Forum, 601 13th Street NW, Suite 500N, Washington, DC 20005; Tel: (202)783-1300; Fax: (202)783-3434; Email: hwu@qualityforum.org Research Objective: Poor patient adherence to prescription medication use instructions is both common and costly, affecting the majority of U.S. healthcare consumers. Despite attempts by many entities to address this problem, large-scale improvement has not occurred. There is an acute need to identify and widely deploy standardized metrics to improve consumer use of prescription medications. This project sought to identify a national action plan to increase consumer adherence to recommended use of prescription medications, focusing especially on populations with low literacy and limited English proficiency. Study Design: The project involved three elements: 1) reviewing the literature to identify practices that have been demonstrated to improve adherence; 2) developing a comprehensive national framework for evaluating and implementing practices to increase patient adherence; and 3) holding a multi-stakeholder workshop to reach agreement on a national action plan for broadly improving prescription medication use. Population Studied: All individuals using prescription medications, with a special focus on those at increased risk of non-adherence due to communication challenges with providers - e.g., those with limited English proficiency or low health literacy. Principal Findings: There is a complex array of factors related to non-adherence, and those that stem from unintentional reasons (e.g., lack of patient understanding, language barriers) are particularly well positioned for action and improvement. Multiple evidence-based strategies exist to effectively improve consumer adherence with the recommended use of prescription medications, many of which are centered on better communication between patients and providers. Basic steps can be taken to address the needs of patients with communication challenges, such as providing medication labels and packaging inserts in multiple languages and simplified verbiage. A wealth of data is also available that could be used to facilitate provider follow-up to promote improved adherence, such as prescription fill and refill tracking. National standards can and should be promulgated to identify a comprehensive set of practices and performance measures for improving the communication and care processes involving prescribers, pharmacists, and consumers, which will in turn substantially improve adherence. Conclusions: A combination of strategies is needed to effectively improve the use of prescription medications at the system, organization, and individual levels. Establishing national consensus standards to address non-adherence, based on existing evidence and data, will be an important first step. The recommended national action plan calls for a broad group of healthcare stakeholders to step forward in addressing these critical issues. Implications for Policy, Delivery, or Practice: Systematic implementation of a comprehensive set of national standards for improving medication use could have a substantial positive impact on safety, efficiency, effectiveness, equity, and other domains of healthcare quality. Primary Funding Source: California Endowment ●Effects of Patient Obtained Medical Information (POMI) on Healthcare Services Utilization in U.S. Counties Bin Xie, Ph.D, David Dilts, Ph.D, MBA Presented By: Bin Xie, Ph.D, Management of Technology, Vanderbilt University, 801 Inverness Avenue Apartment B16, Nashville, TN 37204; Tel: (615)322-8494; Email: bin.xie@vanderbilt.edu Research Objective: Patient obtained medical information (POMI) has attracted considerable attention as the Internet becomes a major source of medical information, but the impacts of such POMI on healthcare utilization and equality of healthcare are not clear. Would patients with POMI have higher healthcare utilization than patients without POMI? Would counties with higher portion of patients with POMI have higher per capital healthcare utilization? What are the implications for equality of healthcare? This paper addresses these questions. Study Design: We performed a cross-sectional analysis of 41485 individuals in 306 counties using data from the 20002001 Community Tracking Study Household Survey and the 2003 Area Resource File. Surgery rate and numbers of physician visits are used as indicators for healthcare utilization, and t-test, ANOVA and multiple regression are used to analyze the impacts of POMI on healthcare utilization. Population Studied: A national representative sample of 41485 individuals in 306 counties in the 2000-2001 Community Tracking Study Household Survey. Principal Findings: Of 41485 individuals, 16296 (39%) have POMI, 7190 (17%) sought POMI from the Internet. Of patients with similar characteristics, patients with POMI have higher surgery rate (for patients with excellent health, 0.18 vs. 0.11, p<0.001) and higher numbers of physician visits (for patients with excellent health, 3.03 vs. 2.05, p<0.001) than patients without POMI. In 306 counties, average portion of patients with POMI is 37.5%, with a range from 9% to 71%. As the portion increases in a county, surgery rate and numbers of physician visits tend to increase as well, although not monotonically. As the portion increases from 9% to 71%, surgery rate increases from 0.18 to 0.29, although it remains at the 0.22 level when the portion increases from 33% to 50% (p<0.001). Numbers of physician visits show similar pattern, increasing from 3.41 to 4.66 as the portion increases from 9% to 71%, although it remains at the 4.00 level when the portion increases from 29% to 50% (p<0.001). Surgery rate by patients without POMI also increases in a county as the portion of patients with POMI increases, although the trend is not monotonic. It increases from 0.16 to 0.26 as the portion increases from 9% to 71%, although it remains at the 0.19 level when the portion increases from 33% to 50% (p=0.07). Numbers of physician visits by patients without POMI, on the other hand, do not change much as the portion increases, as it remains at the 3.40 level as the portion increase from 9% to 71% (p=0.79). Conclusions: Per capital healthcare utilization in a county increases as the portion of patients actively seeing medical information increases, but the relationship between per capital utilization and the portion of informed patients in a county is not linear nor monotonic; per capital utilization increases suddenly when the portion of informed patients crosses some critical values, and remains stable otherwise. Further research is needed to ethics, policy and practical implications of this phenomenon. Implications for Policy, Delivery, or Practice: Firstly, we should pay more attention to traditional channels (such as TV/Radio and Books/Magazines) in delivering medical informatio to patients. Secondly, there is no evidence that disparities in access to medical information are causing disparities in healthcare utilization. Finally, differences in access to medical information may contribute to the regional variances in healthcare utilization. Primary Funding Source: No Funding Source ●Regional Variations of Aggressive Medicare Treatments in VA and Medicare Hospitals Wei Yu, Ph.D., Ariel Hill, AB, Samuel Richardson, BA Presented By: Wei Yu, Ph.D., Health Economist, Health Economics Resource Center, Department of Veterans Affairs, 795 Willow Road, Menlo Park, CA 94025; Tel: (650) 493-5000 x23157; Fax: (650) 617-2639; Email: wyu2@stanford.edu Research Objective: Researchers have observed a positive relation between healthcare utilization and medical capacity, suggesting that demand is induced by supply. However, we know little about how much of the variation is explained by other factors such as practice pattern. This study analyzes the variation in aggressive medical treatments near the end of life in the Department of Veterans Affairs (VA) and Medicare hospitals. Because the VA budget is allocated based on the number of patients, VA hospitals have little financial incentive to induce demand for aggressive treatments. Thus, variations within the VA and the difference between VA and Medicare hospitals could reveal the impact of other factors on medical treatments. Study Design: We retrospectively extracted healthcare utilization provided by the VA or Medicare hospitals during the final 2 years of life and analyzed variations between 21 VA integrated service networks (VISNs) in the utilization of five aggressive medical treatments: intensive care unit (ICU), mechanical ventilator, pulmonary artery monitor, cardiac catheterization, and dialysis. We grouped Medicare hospitals into the 21 VISNs by their location. We compared treatment variations among acute hospital stays during the final 30 days, the final year, and the second year before death with bivariate and multivariate methods. We examined the regional effects using a Probit regression model, controlling for demographics, principal diagnosis, and severity of comorbid conditions measured by the Charlson Comorbidity Index. Population Studied: Veterans who died between October 1, 1999 and September 30, 2001, were over age 67 at death, and used the VA system during their final 2 years of life (N=169,314). We excluded people under 67 at death so that all subjects were eligible for both VA and Medicare during the study period. Principal Findings: Use of aggressive treatments varied considerably among the 21 VISNs in both VA and Medicare hospitals. During hospital stays within the final 30 days of life, ICU use varied from 23.3% to 47.5% in VA and from 31.9% to 50.5% in Medicare, ventilator use varied from 9.0% to 20.1% in VA and from 14.3% to 24.5% in Medicare, pulmonary artery monitor use varied from 1.4% to 6.5% in VA and from 1.5% to 2.9% in Medicare, cardiac catheterization use varied from 0.7% to 3.4% in VA and from 1.9% to 3.8% in Medicare, and dialysis use varied from 2.5% to 5.6% in the VA and from 2.6% to 7.0% in Medicare. These variations persisted after controlling for other factors and in all the three time periods in regression analysis. The aggressiveness of care was not consistent between Medicare and VA facilities in the same region. Conclusions: Regional practice patterns could significantly affect the intensity of medical treatments and could be a significant factor of the variation observed in the private sector. The difference in practice patterns between VA and Medicare hospitals suggests that financial incentives is also involved in medical decisions. Implications for Policy, Delivery, or Practice: Reducing variation in medical treatments could enhance the quality of care near the end of life. As practice pattern is also a significant factor in medical decisions, evidence-based guidelines may improve the quality of care. Primary Funding Source: VA ●Ambulatory Care Sensitive Conditions, Community Factors, and Urban Low-Income Adults: Adapting a Conceptual Framework Wanqing Zhang, M.D., Med, Keith Mueller, Ph.D. Presented By: Wanqing Zhang, M.D., Med, Analyst, Preventive and Societal Medicine, University of Nebraska Medical Center, 984350 University of Nebraska Medical Center, Omaha, NE 68198-4350; Tel: (402)559-8441; Fax: (402)559-7259; Email: wazhang@unmc.edu Research Objective: Preventable hospitalization for ambulatory care sensitive conditions (ACSCs) has been the subject of multivariate analysis efforts for a decade. However, researchers currently lack a theoretical framework for much of their work. Using a conceptual framework, we explored the relationship between access outcomes and community factors among low-income adults residing in metropolitan statistical areas (MSAs), and we examined community-based measures of appropriate use of the health care system among a lowincome population. Study Design: Research has shown that individuals of lower socio-economical levels and some community factors are associated with a higher rate of hospitalization for ACSCs. But how do policy and community intervention modify these factors? The conceptual framework for the effects of community factors on access to ambulatory care for lowincome populations has been suggested by Davidson and colleagues. That framework divides health access and outcomes into three categories: potential access, realized access, and access outcomes. In this study, we examined the relationship between access outcome (ACSCs) and community determinants for urban low-income adults. We used the framework as a basis for constructing community variables hypothesized to influence access outcome. Hospital discharge data for ACSCs was obtained from the Health Cost and Utilization Project’s (HCUP) National Inpatient Database, which is maintained by the Agency for Health Care Research and Quality (AHRQ). Thirteen quality indicators for preventable conditions, developed by AHRQ, were drawn from PQI software. The community variables that reflect the population difference were based primarily on data from the U.S. Census Bureau’s Current Population Survey, and the Bureau of Health Professional’s Area Resource File. The financial support variable for safety-net services was from the Center for Medicare & Medicaid Service’s Medicare cost report. Population Studied: We studied a large national sample of U.S. hospitalized patients in the United States in 2002 - adults 18 or older with income <$25,000 in 33 MSAs. Principal Findings: Hospital discharge for ACSCs varies greatly among low-income adults from 33 selected MSAs (from 3.4% to 45.5 %). For discharge-level factors, Black adults had the highest odds for preventable hospitalizations due to ACSCs after case-mix adjusting (OR=1.51, P<0.001). Being uninsured also increased the odds for preventable hospitalization due to ACSCs (OR= 1.20, P<0.001). As we hypothesized, several community factors dramatically increased the likelihood for preventable hospitalization. A higher proportion of non-citizen immigrants and non-White population increased the likelihood of preventable hospitalization due to ACSCs by 5 and 10 times respectively. Uncompensated care costs were inversely related to preventable hospitalization due to ACSCs (OR=0.76, P<0.001). Conclusions: Guided by a conceptual framework, we found that community and public policy factors were significantly related to preventable hospitalization for ACSCs among urban low-income adults. Implications for Policy, Delivery, or Practice: The results suggest that care management and other interventions (e.g., language assistance, cultural sensitivity and awareness) are needed in communities with a higher proportion of noncitizen immigrants and non-White population. Meanwhile, preventable hospitalization due to ACSCs as a measure of health outcome is important in determining how to target community-wide interventions for improving community health and reducing health disparities. Primary Funding Source: Departmental funds