Using the Critical Incident Technique to Better Understand Patient Presented by:

Using the Critical Incident Technique to Better Understand Patient
Experiences of Ambulatory Care
Presented by:
Kristin L. Carman, Ph.D.
American Institutes for Research
Presented at:
Academy for Health Services Research
Annual Meeting, San Diego, CA June, 2004
Project Team
Roger Levine, PhD
Managing Research Scientist, AIR
Karen K. Shore, PhD
Senior Social Scientist
Margarita Hurtado, PhD
Principal Research Scientist
Kristin L. Carman, PhD
Principal Research Scientist
Judy Mitchell, MS
Senior Research Scientist
Steven A. Garfinkel, PhD
Managing Research Scientist
San Keller, PhD
• Principal Research Scientist
Funding
Agency for Healthcare Quality and
Research
• Part of the CAHPS II grant
Partners
HMSA, Hawaii
Humana, Chicago
Purpose of our project
To develop an A-CAHPS Survey
To use Critical Incident data in novel ways to address issues related to:
Instrumentation
Quality improvement
Reporting, and
Cultural comparability
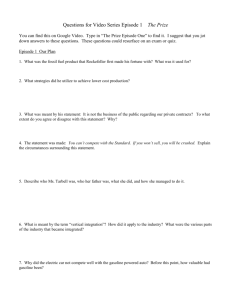
Critical Incident (CI) Technique
Critical Incident
“Incident”=an observable, specific behavior
“Critical”=means incident was crucial to the outcome of interest
Organized structure for data collection; focuses on observable behavior
Used to collect and analyze reports of behaviors associated with specific outcomes
Qualitative method; in-depth interviews
Methods and data
200 interviews; 40 providers and 260 patients
Patient respondents divided equally among four different racial/ethnic groups
Open-ended responses are transcribed
Each interview usually generates 10 incidents; we’ll have 2000+ incidents
CI data management and processing
Gathering extensive data
Using qualitative software to create and manage a very complex data base
Developed a very careful data processing protocol
Raw data is open-ended responses, transcribed
Data is transformed into “incident write ups”
These two types of data are the sources for analyses
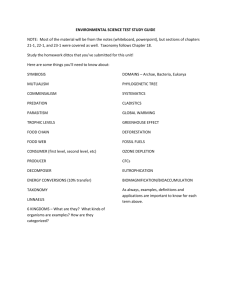
Specific Goals
Instrumentation goals
Develop a complete taxonomy of the components of quality ambulatory health care, based on both patient and clinician perspectives
Confirm that the domains measured by the draft
CAHPS® instrument are salient to patients and providers and can be assessed by patients
Determine whether the domains are salient and measurable for both men and women, for individuals with different levels of education, and across a range of racial and ethnic groups
Identify additional domains that should be measured
Instrumentation goals (cont’d)
Identify CAHPS® item content that can result in a spread of scores at the high end of the score distribution to minimize ceiling effects
Generate objective patient reports of health care experience
Create items for Ambulatory CAHPS® for which a positive rating would be rare
Instrumentation analysis
Developing the taxonomy
Randomly select at least 200 incidents
Two teams classify incidents into major categories, then subcategories
Iteratively validate and refine the taxonomy with additional set of incidents
Instrument analysis (cont’d)
Using incidents as the unit of analysis, then respondents, we investigate statistical associations between personal characteristics and the way people conceive of quality of care
Tabulation of respondent characteristics by taxonomy categories which are quality of care themes (e.g., coordination of care)
Regress taxonomy categories on respondent characteristics
Instrument analysis (cont’d)
Logistic Regression
Simple and multiple
Dependent Variable=taxonomy category
Independent Variables=
Individual demographics
Respondent: provider or patient
Quality improvement goals
Identify physician behaviors associated with excellent and poor quality of care based on experiences of patients and clinicians
Identify combinations or co-occurrences of behavior
Identify key facilitators and barriers to quality of care, specifically related to CAHPS domains
Create tools for QI interventions to improve
CAHPS scores
Quality improvement analysis
Analyze interview and CI files
Conduct additional coding of data
Focus on which behaviors or actions by clinicians co-occur to create positive (or negative) experiences for patients
Compare findings by respondent characteristics
Cultural Comparability goals
Identify variations in taxonomic structure for different racial/ethnic groups
If differences exist, identify the implications for:
Supplemental domains, concepts and items
CAHPS domain labels and explanatory vignettes
Culturally appropriate interventions to improve care
Reports goals and analysis
Identify narratives (phraseology) that clearly and effectively explains CAHPS measures in reports
Next steps
Complete interviews
Complete analyses
Disseminate findings
For more information, contact:
Kristin L. Carman, PhD
Principal Research Scientist
American Institutes for
Research
1000 Thomas Jefferson
Washington, DC 20007
(202) 342-5090
Kcarman@air.org
www.air.org
Karen K. Shore
Senior Research Scientist
American Institutes for
Research
ADDRESS
Palo Alto, CA (ZIP)
PHONE NUMBER kshore@air.org
www.air.org
Transcript
[CI 1-1]
[CI 1-3]
[CI 1-2]
[CI 2-1]
[CI 2-2]
Episode 2
[CI 3-1]
Episode 3
[CI 3-2]
Critical Incident behaviors
Database Creation
CIs for Interview
Critical Incident
Forms
Episode 1
CI 1-1
Separate CIs
CI 1-1
CI 1-2
CI 1-3
CI 2-1
CI 1-2
CI 1-3
CI 2-1
Verbatim Transcript
Marked by interviewer for Episode # and for CI behaviors (not numbered —only numbered here for illustration) in Atlas/ti
Links are logical only: episode # in CI # allows analyst to trace back to transcript
CI Forms filled out by cut and paste from
Transcript, numbered to reflect source episode.
This takes place in Word
CI forms cut into separate text files for sorting into
Taxonomy
Both transcript and concatenated CI files are assigned to doc families for respondent demographics
(See next page for detail)
Transcript
[CI 1-1]
[CI 1-3]
[CI 1-2]
[CI 2-1]
[CI 2-2]
Episode 1
Final Atlas/ti Database
Concatenated CIs
P-01-M-JM-1-1-A
TAX-Communicates
CI 1-1
P-01-M-JM-1-2-B
TAX-Clarifies
CI 1-2
Episode 2
Taxonomy codes are assigned by autocoding
CI 1-3
The ID code includes #’s for episode and CI.
Since ID #’s include identifiers for referents, they are assigned to demographic code families for referents
(See next page for detail)
[CI 3-1]
Episode 3
CI 2-1
[CI 3-2]
At this stage, the finalized concatenated CI file, with taxonomy codes embedded, is imported into Atlas/ti. Taxonomy codes are
“autocoded” by searching for
Taxonomy codewords. At this point, hypertext links can be created between CI forms and episodes in the transcript. If desired, Taxonomy codes may be applied manually to the transcript.
RESPONDENT DEMOGRAPHICS
Respondent demographics are represented by placing
“primary documents” in “PD Families” or sets:
Example:
Gender::Male = {PD1; PD4; PD5; PD8…}
Gender::Female = {PD2; PD3; PD6; PD7…}
Age::20s = {PD1; PD2…}
Age::30s = {PD4; PD8…}
Age::40s = {PD3…}
Age::50s = {PD6…}
Age::60s = {PD5; PD7…}
Imported in a table:
PD1
PD2
PD3
PD4
PD5
PD6
PD7
PD8
…
Gender
Male
Female
Female
Male
Male
Female
Female
Male
Age
20s
20s
40s
30s
60s
50s
60s
30s
Dataset can be parsed according to Boolean combinations of set-memberships, for example, to restrict a query to documents that belong in both the Male and 20s sets.
REFERENT DEMOGRAPHICS
Referent demographics are represented by placing CI ID codes into “Code Families” or sets. The logic is the same as for PD families, but at present there is no table import feature and assignment is made with the “code family manager” tool in Atlas/ti.
Again, set memberships can be used to focus queries on different classes of referents.
Strategies for associating data at episode or interview levels
Layered IDs:
Since ID’s are layered, a hierarchy of ID codes can be created in
Atlas/ti. For example, a hierarchy could be structured as follows:
Interview ID
+--Episode ID
+--CI ID
+--Referent ID
Code Families:
A code family that included all the CI ID codes for a given episode would enable searching by episode in the concatenated CI files.
Hypertext:
Hypertext links can be created from the CI forms to the episodes in the transcript, or even to the specific descriptions of behaviors from which the CIs are derived.