Factors that Influence Hospitalization for Chronic Medical Conditions SUMMARY AND POINTS OF DISCUSSION
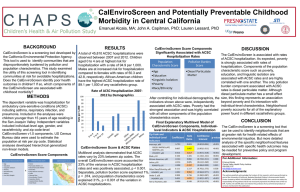
advertisement

Factors that Influence Hospitalization for Chronic Medical Conditions SUMMARY AND POINTS OF DISCUSSION P.O. Box 12194 · 3040 Cornwallis Road · Research Triangle Park, NC 27709 Phone: 202-728-1968 · Fax: 202-728-2095 · nmccall@rti.org · www.rti.org RTI International is a trade name of Research Triangle Institute. 1 Panel Summary Multivariate modeling of the trend in ACSC hospitalizations from 1993 to 2000 using Medicare claims data showed that changes in sociodemographic characteristics and health status among elderly Medicare FFS beneficiaries explained a substantial proportion of the observed positive trend in hospitalization rates for CHF, COPD, and PVD 2 Panel Summary Use of the emergency room strongly associated with hospitalization for COPD and modest association for CHF Evidence of substitution for PVD Rural areas that lost population Experienced declines in hospitalization rates for COPD and CHF 3 Panel Summary After controlling for changes in demographics, health status, and migration patterns, unexplained geographic variation in ACSC hospitalization rates remained Most notable for COPD and CHF in eastern half of United States This suggests factors not included in the trend analysis play an important role in hospitalization rate increases over time. 4 Panel Summary Cross-sectional multivariate analysis using the MCBS of likelihood of hospitalization in 2000 for an ACSC allowed for examination of factors not in claims data A previous hospitalization was found to be the strongest predictor of a subsequent hospitalization for the same chronic condition Having a usual source of care or supplemental insurance did not appreciably reduce likelihood of admission 5 Panel Summary In our third multivariate analysis, we used regional-level data aggregated to the level of HRRs to examine rates of change in acute care treatment for three chronic conditions between two time periods Allowed us to examine residual geographic variation observed in the trend analysis 6 Panel Summary Incorporated market-level information population characteristics hospital and post-acute care availability and usage physician and nurse supply factors supplemental insurance take-up general and M+C managed care penetration. 7 Panel Summary Beneficiary characteristics aggregated to the level of HRRs strongly influenced rates of acute care treatment for COPD, CHF and PVD Poverty appeared to have the strongest relationship with rate of hospitalization and its influence increased over time Significant regional concentration throughout the Appalachian Mountain Region and Gulf of Mexico 8 Panel Summary Positive association between rate of hospitalization for COPD and proportion of population that said they had not visited a physician due to cost in the latter part of the 1990s Supply factors related to SNF and rehabilitation care were associated with COPD and CHF hospitalization rates SNF + Rehab – High rates of home health visits positively associated with PVD admission rates 9 Panel Summary A descriptive analysis examined whether the incidence of an ACSC hospitalization was associated with self-reports of poor access to care or dissatisfaction with health care services among Medicare FFS beneficiaries No relationship between satisfaction with care or customer service Beneficiaries that had an ACSC hospitalization were modestly more likely to report problems getting needed medical care 10 Policy Implications Variation in the direction and strength of relationship between explanatory factors and hospitalization for the selected chronic conditions suggest that interventions employed to reduce hospitalization for ACSCs may have to be tailored to specific conditions to be effective 11 Policy Implications Rates of ACSC hospitalization are strongly influenced by health status within the Medicare FFS population Targeting hospitalized beneficiaries for disease management may be a reasonable strategy to reduce future admissions Decrease overall level of morbidity and presence of co-morbidities 12 Policy Implications A more aggressive approach to clinically managing beneficiaries with the studied chronic conditions may not be sufficient Poverty Living in rural areas Dual enrollment in Medicare/Medicaid 13 Policy Implications Observed regional clustering of COPD and CHF rates suggests interventions might be geographically targeted rather than national in scope 14 Policy Implications Lastly, use of ACSC hospitalizations as a quality measure may require further evaluation prior to widespread use Stark difference in trend in hospitalization rate for COPD and asthma – – – – Clinically difficult to distinguish Coding may be fungible Were there changes in treatment? Were there changes in payment? Creating indices may mask quality problems or quality improvement 15