Public Health
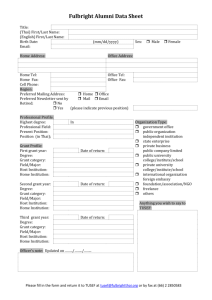
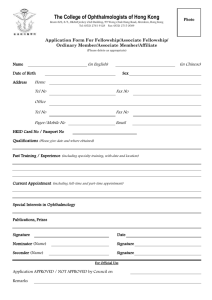
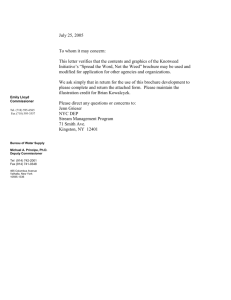
advertisement

Public Health Call for Papers Public Health Risks, Costs & Prevention Strategies Chair: Linda McKibben, Ph.D. Sunday, June 6 • 9:30 a.m.-11:00 a.m. ● Health Care Costs of Moderate and Severe Obesity Tatiana Andreyeva, M.A., Roland Sturm, Ph.D. Presented by: Tatiana Andreyeva, M.A., Doctoral Fellow, RAND Graduate School, 1700 Main Street, Santa Monica, CA 90401; Tel: 310.393.0411 Ext. 6047; Fax: 310.451.7040; Email: tatiana@rand.org Research Objective: Estimate the excess health care costs associated with moderate and severe obesity among individuals ages 50-69. Despite the sound evidence that obesity increases health care costs by more than a third, there is no data distinguishing how severe obesity differs from moderate obesity. As severe obesity increases at a much faster rate than moderate obesity, using average cost effects is unlikely to provide a good estimate to predict future health care costs. Study Design: This study uses the Health and Retirement Study, a nationally representative biennial longitudinal survey of 9,825 Americans in their 50’s at baseline in 1992, to analyze differential impacts of severity of obesity on health care utilization and costs. Dependent variables are total medical spending and three measures of health care utilization (number of ambulatory visits, hospital stays and the probability of hospitalization). We subset the analysis to individuals whose weight does not change by more than 10% between two adjacent waves to obtain a better measure of long-term weight. The results are adjusted for sociodemographic changes to isolate the unique effect of obesity category. Regressors include: age, educational achievement, racial minority, family income, insurance and marital status. We estimate models separately for men and women. Individuals are classified into weight categories based on the body mass index (BMI) calculated from self-reported weight and height. In addition to the standard obese category, defined as a BMI >= to 30 kg/m2, the groups of interest are more extreme categories: BMI: 35-40 and BMI>=40. The statistical analysis of medical expenditures uses a two-part model. We estimate probit and linear models for service utilization variables. Population Studied: Nationally representative adults ages 5069. Principal Findings: Among individuals ages 50-69, moderate obesity (BMI: 30-35) is associated with a 32% increase in annual health care costs among women and 16% among men, a BMI of 35-40 with an increase of 62% and 42%, a BMI of 40 or more with an increase of 98% and 74% respectively. In absolute terms, overweight implies an average increase of $447 per year in health care costs for men and $397 for women. Moderate obesity increases medical spending by $635 for men and - twice as much - $1,255 for women. The effects trend up as severity of obesity grows. Severe obesity increases medical spending by $2,433 per year for men and $1,814 for women. The largest effect is for the most obese segment, which is extra annual medical spending of $2,888 for men and $3,833 for women. There are also significant disparities in service utilization by weight category. Conclusions: The prevalence of severe obesity is increasing at a double-fold rate among US adults than obesity. As comorbidities and resulting service use are much higher among severely obese individuals, the widely published trends for overweight/obesity, including health care costs, underestimate the consequences for physician practices, hospitals, and health plans. We show that severe obesity increases average health care costs twice as much as moderate obesity and almost four times more in the very severe cases. Implications for Policy, Delivery or Practice: Average estimates hide all of the effects on health care system from the “obesity epidemic” in the US and underestimate future costs associated with obesity. Accurate estimates of obesity costs, however, have major implications for future outlays from Social Security programs and Medicare that already pay for almost a half of expenditures attributable to overweight and obesity. ● Is Some Physician Advice on Smoking Cessation Better than No Advice? An Instrumental Variable Analysis of the 2001 National Health Interview Survey Yuhua Bao, Ph.D., Naihua Duan, Ph.D., Sarah Fox, Ed.D. Presented by: Yuhua Bao, Ph.D., Health Economist, Department of Medicine, UCLA, 1100 Glendon Avenue, Suite 2010, Los Angeles, CA 90024; Tel: 310.794.3081; E-mail: yuhuabao@mednet.ucla.edu Research Objective: Of the more than thirty-three million smoking adults who visited their health providers during one year (2000-2001), about 65% received some advice to quit smoking. Health providers do not consistently advise smoking cessation partly because they lack confidence in the effectiveness of their advice and partly because the “best practice” identified by randomized controlled trials is usually too time and resource intensive for community practice. This study estimates the effect of provider advice as practiced in day-to-day clinical contacts on patients’ cessation outcome using non-experimental data. Study Design: We use the sample adult file from the 2001 National Health Interview Survey. We estimate a joint model of self-reported smoking cessation and ever having received advice in the past twelve months during medical visits to providers. Because providers tend to advise mostly heavier smokers and/or patients already diagnosed with smokingrelated conditions, we use provider advice for diet/nutrition and for physical activity reported by the same patient as instrumental variables for smoking cessation advice. A similar analysis is conducted on the sample without any smokingrelated conditions. We also exclude patients who reported receiving additional help to quit smoking such as counseling and medication (about 37% of those who received some advice) to estimate the effect of advice alone on the cessation of lighter smokers. Population Studied: Adult patients who either are current smokers (every day and some days) or quit during the last twelve months and who had some contact with the health care providers or facilities they most often go to for acute or preventive care. Principal Findings: We find that provider advice doubles the chances of success in (self-reported) smoking cessation by their patients. The probability of quitting by the end of the twelve-month reference period averaged across all smoking patients is increased from 8% to 16%, which is both statistically and practically significant (p<0.001). The effect size is similar when we restrict the analysis to patients without any smoking-related conditions. The effect of providing advice alone to patients who are lighter smokers and/or who have fewer smoking-related conditions is even larger (from 8% to 23%, p<0.001). Conclusions: Provider advice delivered in routine practice settings has a sizable effect on the success rate of smoking cessation among smoking patients. The effect size is larger than that of almost all other tobacco control policies made so far such as tax on tobacco products and clean in-door air laws. Implications for Policy, Delivery or Practice: Current rate of smoking cessation advice during clinical contacts is far below optimal, given the large effect of some provider advice found in this study. While it is not feasible or effective to adopt the “best practice” identified in clinical trials in every clinical context, providers can make a big difference by consistently providing advice and other help to all their smoking patients. Primary Funding Source: NCI ● The Impact of Obtaining Documented Informed Consent for Population-Based Voluntary Supplemental Newborn Screening in California Lisa Faulkner, Ph.D., Maura Hanlon, M.P.H., CHES, Lisa Feuchtbaum, Dr.PH, Fred Lorey, Ph.D., Kathleen Velazquez, M.P.D., M.A., George Cunningham, M.D., M.P.H. Presented by: Lisa Faulkner, Ph.D., Research Scientist, Genetic Disease Branch, Public Health Institute c/o California Department of Health Services, 850 Marina Bay Parkway, Room F175, Richmond, CA 94804; Tel: 510.412.1453; Fax: 510.412.1560; E-mail: lfaulkne@dhs.ca.gov Research Objective: To assess the impact of obtaining documented informed consent during an 18-month populationbased supplemental newborn screening research project using tandem mass spectrometry in California. Study Design: Using a prospective cohort study, we compared participation in voluntary supplemental newborn screening (which required written consent) to participation in mandatory newborn screening (which allows opt out for religious reasons only) in a prospective cohort. Population Studied: To assess the impact of the informed consent process on decision-making we conducted 5 focus groups with 31 pregnant women, a mail survey of prenatal care providers and a telephone survey with MS/MS program participants. Principal Findings: Less than half (354,000 or 47%) of the 756,000 California babies who received mandatory newborn screening also received supplemental screening for metabolic disorders. While 42,000 (6%) of parents refused supplemental screening; the remaining 360,000 (47%) had no documented consent or refusal. Only half the hospitals in the State submitted samples with documented consent for 50% or more of the babies born at their facilities. Only 17% of prenatal care providers handed out the educational materials and offered to answer questions while another 29% didn’t hand it out at all. The focus group discussions revealed the benefits and risks were not well understood. Conclusions: Population-based informed consent for newborn screening places a burden on hospitals and significantly reduces the population screened and the number of disorders detected in the newborn period. Informed consent does not appear to be feasible for population based screening and it didn’t achieve its presumed benefits of protecting subjects by enabling them to make informed decisions about participation in population-based research. Implications for Policy, Delivery or Practice: If applicable, obtain a waiver of written informed consent for population based newborn screening research or pilot projects with minimal risk. Investigate barriers to why prenatal care providers do not discuss with patients and try to increase their participation since most pregnant women appear to rely on them for advice about newborn screening. Improve educational materials to better convey risks and benefits. Primary Funding Source: HRSA ● Impact of Low Health Literacy on Medical Costs David Howard, Ph.D., Julie Gazmararian, Ph.D., Ruth Parker, M.D. Presented by: David Howard, Ph.D., Assistant Professor, Department of Health Policy and Management, Emory University, 1518 Clifton Road, N.E., Atlanta, GA 30322; Tel: 404.727.3907; Fax: 404.727.9198; E-mail: dhhowar@emory.edu Research Objective: Despite the prevalence of low health literacy and the number of studies documenting its impact on health outcomes, there is a paucity of information on the implications for medical costs. The objective of this study was to examine the impact of low health literacy on medical costs and resource use. Study Design: Costs incurred over a one year period were compared between persons with low and adequate health literacy using propensity scores. Propensity scores were based on age, race, income, education, and chronic conditions. Population Studied: A total of 3,260 non-institutionalized elderly persons enrolling in one of four Medicare managed health care plans (Cleveland, Ohio; Houston, Texas; South Florida; Tampa, Florida) in 1997. Principal Findings: Controlling for observed covariates, persons with low health literacy incur expenditures for emergency room care that are $86 (66% of the sample average emergency room expenditures) higher (1997 U.S. dollars) (P<0.01) than persons with adequate health literacy. Costs for outpatient care and prescription drugs are $137 (7%) lower (P = 0.42) and $27 (4%) higher (P = 0.60), respectively. The cost of inpatient care was $979 (18%) higher (P = 0.25) but statistically insignificant, possibly due to the extreme skewness of the inpatient spending distribution. When persons incurring inpatient expenditures above the 99th percentile were excluded, the difference was $1,017 (19%) and significant at the 5% level. Conclusions: Persons with low health literacy incur higher expenditures for emergency room care. Comparisons of the likelihood of using inpatient care, inpatient admissions, and costs with outliers excluded indicate that persons with low health literacy use more inpatient resources as well. Future research should seek data sources with larger sample sizes, examine the sensitivity of results to alternative models for comparing health spending, and determine whether results are consistent across different demographic groups. Implications for Policy, Delivery or Practice: Programs to improve health literacy and simplify communication of health information have the potential to reduce health care costs. Primary Funding Source: Pfizer Foundation ● Maternal Smoking and the 1998 Master Settlement Agreement Douglas Levy, M.P.H., Ellen Meara, Ph.D. Presented by: Douglas Levy, M.P.H., Ph.D. Candidate, Department of Health Care Policy / HMS, Harvard University, 180 Longwood Avenue, Boston, MA 02115; Tel: 617.432.4356; Fax: 617.432.0173; E-mail: delevy@fas.harvard.edu Research Objective: Immediately following the November 1998 Master Settlement Agreement (MSA) between the states' attorneys general and several large tobacco companies there was a large (45 cent) increase in the price of cigarettes that took effect nationally. Prior literature suggested that such a large price increase would reduce smoking among pregnant women by as much as 14% and would improve birth weight outcomes, preventing as many as 6,600 low birth weight outcomes (<2500g) per year. We sought to determine how the MSA affected smoking among pregnant women and whether the MSA affected birth weight outcomes. Study Design: We performed interrupted time-series analyses on data from the national Natality Detail Files, examining smoking participation, smoking intensity, birth weight, and low birth weight status (LBW) immediately before and after the MSA. Subgroup analyses were conducted by maternal age, race, and educational attainment. Population Studied: We included all singleton births conceived from March 1996 to February 1998 and from December 1998 to February 2000 to mothers 15 to 44 years old in the 47 states reporting maternal smoking and the District of Columbia. Pregnancies overlapping the announcement of the MSA were excluded. In total, our study population comprised 9,012,048 births. Principal Findings: The large increase in cigarette prices following the MSA had no substantive effect on smoking prevalence (log-odds post- vs. pre-MSA=0.000071, p=0.99) or smoking intensity (among smokers, 0.22 fewer cigarettes smoked per day post-MSA, p<.0001) reported by pregnant women. Furthermore, we found the MSA had no significant effect on birth weight outcomes (birth weights down an average of 1.6g post-MSA, p=0.125). Findings were similar across all subgroups we analyzed. Conclusions: Our analyses indicate most pregnant women are unlikely to change their smoking habits in response to price changes. It is possible that as public awareness of the dangers of smoking during pregnancy continues to increase and as prices have increased over the past fifteen years, the remaining core of women willing to smoke during pregnancy is particularly intransigent. Alternatively, it is possible that previous studies in this area, using state tobacco excise taxes as a proxy for price, captured state-level changes in policy and/or attitudes towards smoking coincident with the excise tax changes rather than a true price effect. Implications for Policy, Delivery or Practice: Efforts to reduce smoking and improve health outcomes by increasing cigarette excise taxes will not affect all populations identically. Targeted interventions may be necessary to prevent low birth weight morbidity associated with cigarette smoking. More rigorous studies using other outcomes and populations are needed to verify the health benefits of this popular tobacco control measure. Primary Funding Source: AHRQ Call for Papers Public Health Infrastructure: Identifying & Closing the Gaps Chair: Glen Mays, Ph.D., M.P.H. Monday, June 7 • 4:00 p.m.-5:30 p.m. ● Optimizing Use of Resources for Conducting Practicebased Immunization Assessments Margaret Coleman, Ph.D., Noelle-Angelique Molinari, Ph.D., Shannon Stokley, M.P.H., Hussain Yusuf, M.B.B.S., M.P.H., Mark Messonnier, Ph.D. Presented by: Margaret Coleman, Ph.D., Economist, HSREB, CDC/NIP, 1600 Clifton Road, N.E., MS-E52, Atlanta, GA 30333; Tel: 404.639.8801; Fax: 404.639.8614; E-mail: zby5@cdc.gov Research Objective: Assessment, feedback, information, and exchange (AFIX) is a practice-based strategy that promotes childhood immunizations and has been shown to improve medical provider vaccination coverage rates. The Centers for Disease Control and Prevention (CDC) recommends that federally funded immunization programs conduct annual AFIX site visits in at least 25% of provider offices. This project seeks to understand how grantees use funds to administer AFIX and determine what factors influence completion of AFIX assessments. Study Design: 2000 and 2001 CDC program funding records were compared with immunization program self-reported data of completed AFIX assessments. A Poisson model was estimated with maximum likelihood to determine what factors influenced the dependent variable, completed AFIX assessments. The independent variables were grantee vaccine purchase policies, full time equivalent employees (FTEs), perchild funding, and population of children. Population Studied: State and urban programs receiving grant monies to administer AFIX. Principal Findings: There was an extremely wide spread in per-assessment spending, i.e. 2000 federal spending ranged from $81 to $174,926. Median funding for AFIX programs was $106,551 in 2000 and $266, 387 in 2001, far less than average funding which was $240,056 and $501,629, respectively. The model results showed that numbers of completed AFIX assessments increased 30% with a 10% increase in FTEs and 8% when there was a 10% increase in AFIX site-visits combined with other required site visits for the Vaccines for Children (VFC) program. The funding perchild variable was significant in explaining numbers of completions. Conclusions: The wide range in per-assessment spending indicates that assessment process work practices need to be standardized. A standardized funding formula may need to be developed to more systematically distribute grant monies. Grantees should administer AFIX in conjunction with VFC site visits to the extent possible. Funding increases to grantees that support hiring and training more FTEs may result in increased numbers of completed assessments. Implications for Policy, Delivery or Practice: Standardizing assessment work practices and distributing grant monies more systematically will improve the quality of AFIX and assure policy makers that government funds are being appropriately spent. Primary Funding Source: CDC ● Racial/Ethnic Differences in Trust of Public Health to Respond Fairly After Bioterrorism David Eisenman, M.D., M.S.H.S., Cheryl Wold, M.P.H., Anna Long, Ph.D, M.P.H., Claude Setodji, Ph.D. Presented by: David Eisenman, M.D., M.S.H.S., Associate Natural Scientist, Behavioral Health, RAND Corporation, 1700 Main Street, Santa Monica, CA 90407; Tel: 310.393.0411 Ext. 6429; E-mail: david_eisenman@rand.org Research Objective: Public health departments’ effectiveness in the response phases of catastrophic terrorism will require diverse communities’ trust in their institutions and actions. This study describes variations in “trust”—perceptions about whether the public health system would respond fairly to one’s needs regardless of race/ethnicity, income, or other personal characteristics—by racial/ethnic and other demographic, household/neighborhood, and healthcare-related factors, in a large U.S. metropolitan population. Study Design: We analyzed data from the Los Angeles County Health Survey, a periodic, random-digit-dialed telephone population survey in Los Angeles County (LAC). The outcome variable (trust) was an affirmative response to the item: “If there is a bioterrorist attack in LA, do you think the County’s public health system will respond fairly to your health needs regardless of race, ethnicity, income or other personal characteristics?” Mantel-Haenszel chi-square tests were conducted to assess the prevalence of trust by variables that were selected because they were predictors of trust in previous studies or due to a priori reasoning: demographic (race/ethnicity, age, gender, education, income, interview language), household/neighborhood (household dependents, perceived neighborhood safety), healthcare-related (health status, insurance, perceived access to healthcare), and perceived risk of a terrorist attack. To examine the effect of race/ethnicity on trust we performed simple and multivariate logistic regression, adjusting for demographic and other variables associated with trust (perceived access to healthcare and perceived neighborhood safety.) Population Studied: Eligible participants were noninstitutionalized adults; spoke English, Spanish, or one of four Asian languages; and lived in LAC from October 2002— January 2003. A random sub-sample (n=1,041) of the 8,127 participants answered 12 additional items regarding terrorism. Principal Findings: Trust was associated with race/ethnicity (white 77%, Latino 73%, Asian/Pacific Islander 68%, African American (AA) 63%, p=0.001); advancing age (18-39 years 77%, 40-64 years 83%, 65 and older 85%, p=.03); language (English 80%, Spanish 86%, Asian languages 62%, p=0.01); perceived access to healthcare (more difficult over past year 76%, less difficult 89%, no change 82%, p=0.09); and perceived neighborhood safety (very unsafe 63%, somewhat unsafe 78%, somewhat safe 81%, very safe 84%, p=0.01). Compared to whites, AA’s were less likely to report trust (OR 0.4; 95% CI 0.2—0.7). Multivariate predictors of trust were AA race (aOR 0.5; 95% CI 0.3—0.9), age 18-39 (aOR 0.5; 95% CI 0.2—0.9), Asian language (aOR 0.3; 95% CI 0.1— 0.7) and greater perceived neighborhood safety (aOR 1.4; 95% CI 1.1—1.7). Conclusions: In this population-based study, trust in public health to respond fairly to bioterrorism was lower among African Americans, Asian language groups, younger adults, and residents of unsafe neighborhoods. Implications for Policy, Delivery or Practice: Public health officials charged with preparing and responding to a bioterrorist event must continue to develop institutional trust with African American and Asian/Pacific Islander communities. Addressing variations in trust by age, language, and perceived neighborhood safety also are important for designing and implementing strategies to improve trust and confidence in the public health system. Primary Funding Source: RAND ● Public Health Finance: An Investigation of Jurisdiction Funding Patterns and Performance Capacity Peggy Honore, D.H.A., M.H.A., Eduardo Simoes, M.D., M.Sc., M.P.H., Walter Jones, Ph.D., Ramal Moonesinghe, Ph.D., M.A., M.S. Presented by: Peggy Honore, D.H.A., M.H.A., Instructor, Rollins School of Public Health, Emory University, 3113-L Flowers Road, South, Atlanta, GA 30341; Tel: 770.234.9599; Fax: 770.220.1835; E-mail: PAHONORE@aol.com Research Objective: A field of study for public health finance has never been developed. Consequently, very little is known about the relationships, types, and amount of finances that fund the public health system in America. Research and analysis of the health care delivery system financial structures are studied in great detail; however, a comparable degree of routine analysis in public health simply does not exist. This research was an effort to illustrate practices for public health financial analysis that could serve as instruments to strengthen the financial foundation of the public health system while also aiding with defining a field of public health finance by building on the sparse knowledge available. Specific objectives were to investigate if different levels and types of revenues, expenditures, and other demographic variables in a public health jurisdiction are associated with performance of the 10 Essential Public Health Services. Study Design: The research utilized local public health system performance scores in each of the 10 Essential Public Health Services as calculated through the Local Public Health System Performance Assessment Instrument. In this correlational study, each of the participating local health systems are data points with a bivariate relationship between a specific financial or demographic indicator and an essential public health performance score. Population Studied: The population consisted of 50 local health agencies in a mid-west state. Principal Findings: One of the study’s most significant findings was the degree of synergism between public health jurisdiction taxes per capita and local public health system capacity. Statistically significant correlations were found in 6 of the 10 essential services performance scores. Analysis of the financial data also revealed that, on average, high scoring local public health systems had taxes per capita 38% greater than the lower scoring systems. However, an association between jurisdiction revenues per capita to higher performance was not observed. This suggests that flexible funding streams such as those under the direct control of jurisdictions like taxes are more effective with improving system performance. Conclusions: A vital component to performance improvement is the ability to collect, analyze and transform data into information. While this research was an attempt to illustrate the usefulness of such analysis, replication of it in other jurisdictions across the nation is hindered by the lack of available financial data such as public health jurisdiction tax rates, revenues, and expenditures. The significance of this research on strengthening the public health systems is supported by an IOM (2002) recommendation to experiment with increasing local funding flexibility. Implications for Policy, Delivery or Practice: Analysis to determine the adequacy and effectiveness of financial resources to sustain appropriate standards within the public health system should be routine, anticipated, and institutionalized as a collective responsibility throughout the system. If results showing increased performance capacity to be associated with higher taxes per capita are replicated nationally, it would provide a powerful analytical tool to policymakers for determining how to increase investments for the delivery of essential public health services. ● Competency of Public Health Nurses and Faculty in the Essential Public Health Services Michele Issel, Ph.D., Kathleen Baldwin, Ph.D. Presented by: Michele Issel, Ph.D., Clinical Associate Professor, School of Public Health, UIC, 1603 W. Taylor Street (MC 923), Chicago, IL 60612; Tel: 312.355.1137; Fax: 312.996.3551; E-mail: issel@uic.edu Research Objective: For public health nurses to contribute substantively to the health of the public, they need to be competent at performing the ten essential public health services. Their competence begins with their public health nursing education and, hence, public health nursing faculty also need to be competent in the ten essential public health services. Little information exists regarding the level of competency of either public health nursing staff or faculty, despite federal priorities and interest in advancing the education of nurses for population-based practice. This research sought to assess the self-reported level of competency of the public health nursing workforce in Illinois. Study Design: A questionnaire based on the ACHNE standards for public health nursing was developed and reviewed by an expert panel for readability and applicability to public health nurses. Competency in each essential public health service was scored on a 1 (need to be taught this) to 5 (do and teach this to others) Lickert scale, with 3 (do or can do this) or higher as being competent in the essential service. Alpha reliability for the essential public health services ranged from .89 to .97. Population Studied: Two independent samples in Illinois were used. For the public health nursing staff survey, a purposive sample was 50 local health departments in which the director of public health nursing and three of their public health nurses responded to the questionnaire. For the faculty survey, a purposive sample of 124 nurses who were deans and faculty currently overseeing or providing PHN education were surveyed. Principal Findings: Staff respondents (n=168) were mostly 48 year old, white females with a baccalaureate degree. Faculty respondents (n=47) were 50 years old, most had a doctorate, and annually teach community/public health for 8 semester hours. Both staff and faculty felt most competent in linking people to services (mean 3.4 and 4.2, respectively). This was the only essential service in which staff rated themselves as competent. Faculty rated themselves as competent in researching innovative strategies (mean 4.0), and monitoring population health (mean 4.0), and marginally competent in policy and planning skills (mean 3.1). Among the staff, higher education was correlated with higher competency scores in ensuring a competent workforce, developing polices and mobilizing community partnerships. Faculty with an educational background in public health nursing had higher competence in teaching about ensuring a competent workforce, mobilizing community partners, and policy and planning than did faculty without a public health nursing degree. Conclusions: Overall, competency in the essential public health services is low. The essential service of highest competency is individual focused and a uniquely nursing task. Higher education and work experience increase self-reported competency Implications for Policy, Delivery or Practice: The results suggest the need for broad state-wide educational offerings to increase the competency of public health nurses and faculty. Curriculum could be tailored to address the competencies rated lowest. Greater emphasis is needed in local health agencies and nursing programs on requiring and assisting public health nursing staff to acquire minimum competency in all ten essential public health services. ● Rural Hospitals’ Health Promotion and Disease Prevention Services: Relationships with External Forces and Hospital Characteristics Mei Zhao, M.S., Peter Olden, Ph.D., Henry Carretta, M.P.H. Presented by: Mei Zhao, M.S., Research Associate, Health Administration, Virginia Commonwealth University, P.O. Box 980203, Richmond, VA 23298; Tel: 804.827.1811; Fax: 804.828.1894; E-mail: mzhao@hsc.vcu.edu Research Objective: Examine organizational and environmental factors associated with provision of Health Promotion / Disease Prevention (HPDP) services by U.S. rural acute care hospitals in 2000, using Oliver’s strategic response theoretical framework. Study Design: Oliver’s framework identifies 5 internal and external constructs that may influence organizational response to external factors. Oliver’s constructs (and our variables) are cause (for-profit status); constituents (sum of dummy variables for HMO, PPO, Blue Cross, JCAHO, medical school, Medicare, hospital system, network, and alliance); content (sum of dummy variables for hospital mission and long-term plan for community health); control (ratio of HPDP services offered by all other hospitals in county to maximum number of such services that could be offered by them); and, context (sum of three dummy variables for hospital works with others to conduct community assessments, to assess appropriate capacity, and, to share clinical and health information). Total margin, total hospital staff per bed, volunteer department, per capita county income, number of staffed beds, and Medicare case mix index were included as control variables. The dependent variable (DV) was defined as number (0-18) of HPDP services offered by each hospital. Cross-sectional data from 2000 AHA Annual Survey of Hospitals, 1999 Medicare Cost Reports, February 2000 Area Resource File, and 2000 Center for Medicare and Medicaid Service Case Mix Index files were concatenated for the study population. After multicollinearity tests, two models were tested with both OLS and Poisson multivariate regressions. An un-weighted model used a simple count of the number of HPDP services as the DV. A second model weighted the number of HPDP services by the number of hospitals that do not offer the service in the entire study population. This gave more weight to services offered by fewer hospitals. Population Studied: 1,513 non-federal, rural, acute care general hospitals that responded to the AHA 2000 Annual Survey. Principal Findings: Mean percentage of hospitals offering an individual HPDP service ranged from 7.0% to 78.4%. Forprofit (cause) hospitals provided significantly less HPDP services than not-for-profit hospitals. The number of constituents, hospital goals (content), and their interconnectedness with external partners were all positively associated with more HPDP services (p<.05). HPDP penetration (control) was less significant (p=.09). All control variables, except total margin, were significant (p<.05). The OLS (weighted) and Poisson (un-weighted) analyses were similar except that for-profit status (cause) was not significant in the Poisson analysis, perhaps reflecting the importance of weighting HPDP services. Conclusions: Four of Oliver’s five constructs were useful predictors of organizational and environmental factors influencing rural hospital adoption of HPDP services. Market HPDP penetration (control) may be less important. Hospital total margin, staffing, volunteer department, staffed beds, and CMI, and, local per capita income are important to consider in models. Implications for Policy, Delivery or Practice: Rural health stakeholders have called for improved rural health, noting that it lags non-rural health. This study extends knowledge of factors influencing rural hospitals’ provision of HPDP, which could help improve rural health. Future studies should consider using weighted HDPD measures and the six control variables. Related Posters Poster Session A Sunday, June 6 • 6:45 p.m.-8:00 p.m. ● Predicting the Costs and Allocation of Public Health Nursing Services Kaye Bender, R.N., Ph.D., FAAN Presented by: Kaye Bender, R.N., Ph.D., FAAN, Dean and Professor, University of MS School of Nursing, 2500 North State Street, Jackson, MS 39216-4505; Tel: 601.984.6220; Fax: 601.815.5958; E-mail: KBender@son.umsmed.edu Research Objective: To design a probablility model for anticipating the allocation and costs of public health nursing services within a public health jursidiction. Study Design: The design for this study is a prospective modeling design which includes relative capability, ranked scoring, and predictive numerical estimations for public health nurse staffing for a given population. Modeling allows a public health jurisdiction to utilize a formula by which to predict and allocate staffing levels and costs of public health nursing services. Population Studied: A statistically significant sample of public health nurses from selected states and local jurisdictions across the United States is being developed. The final sample size will be determined by the anticipated power level for the study. Principal Findings: This research is currently underway, but will be concluded by May 2004. Findings are anticipated to lead to the testing of the predictive model, with adjustments based on a variety of jurisdictional sizes and public health needs. Conclusions: Conclusions will be developed as the final results of the study are analyzed. However, it is anticipated that the model will move public health administration forward in its approach to planning staffing levels and finances for the largest public health professional workforce, public health nurses, at a time when the national nursing shortage has been predcited to create workforce gaps for the already vulnerable public health infrastructure. Implications for Policy, Delivery or Practice: National organizations such as APHA, ASTHO, NACCHO, ANA, and others are predciting the most significant nursing shortage to occur between now and the year 2020. The potential impact of that shortage on the public health infrastrcuture is notable, given the fact that public health nurses constitute the single largest component of the governmental public health workforce. Historically, nursing shortages have also impacted the public health budgets, as salary increases have accompanied the quest for recruiting and retaining qualified public health nurses. The anticipated nursing shortage, coupled with the current concerns over state finances and budgets, create the potential for a crisis situation. The development and testing of a predictive model for forecasting staffing levels and costs of public health nursing services has the potential to guide state and local public health jursidictions toward sound workforce and financial planning. Primary Funding Source: State funds ● Developing Statewide Public Health Department Capacity for Response to Chemical Incidents Lisa Benton, M.D., M.P.H., Erica Weis, M.P.H, Kevin Chao, Ph.D., Robert Melton, M.D., M.P.H., Sharon Lee, Ph.D., Raymond Neutra, M.D., Dr.P.H. Presented by: Lisa Benton, M.D., M.P.H., Public Health Medical Officer, Division of Enviromental & Occupational Disease Control, California Department of Health Services, 1515 Clay Street, Suite 1700, Oakland, CA 94612; Tel: 510.622.4453; Fax: 510.622.4902; E-mail: lbenton@dhs.ca.gov Research Objective: Given the greater likelihood of their occurrences compared to a biological terrorist event, response to chemical terrorism or hazardous materials incidents demands coordination of health department capabilities with those of non-traditional partners. To strengthen capabilities of public health departments to respond to chemical emergencies, contemplation of contamination scenarios provides useful guidance for identifying needs, assets, and agency partners for preparedness. Study Design: To strengthen the California Department of Health Services’ (CDHS) capacity to respond to a chemical threat or disaster resulting in contamination, the Division of Environmental and Occupational Disease Control (DEODC) designed, implemented, and assessed practical processes focused on the unique immediate and long-term challenges presented by chemical emergencies and incidents. From December 2002 until now, the DEODC prioritized eight (8) public health response activities for chemical emergencies. Based on the state health department’s distinct expertise for acute and long-term environmental laboratory, toxicology, epidemiology, surveillance, risk communication, and guidance for worker health and safety, DEODC created a template --a public health functional working group, to facilitate health effects assessment and support interagency response. To integrate these functions: DEODC implemented a 24-hour oncall intra-agency response protocol operating within an interagency emergency notification algorithm; conducted key informant interviews with potential stakeholders at the local and county level to assess knowledge and needs; provided guidance, recommendations and technical assistance for public health laboratory directors; assessed worker health and safety information needs during a chemical incident; identified gaps in communication and offered solutions; developed modules for immediate and long-term community risk surveillance and studies; and created pathways to quickly produce toxicology and chemical fact sheets. Population Studied: Key informant individuals having distinct roles for emergency response to chemical incidents at the 62 local and county health departments, and state level in CA: first responders, health providers, environmental health scientists, industrial hygienist, toxicologists, law enforcement personnel, epidemiologists, community based organizations. Principal Findings: The need to evaluate methods for public health department response to chemical emergencies is essential. Many public health personnel often need to better define, plan, and implement concerns about long-term consequences to human and environmental health as well as contamination cleanup. Many agencies perceived by health departments to be stakeholders do not initially consider public health agencies as part of their integrated response plans. Because of the frequency of spills requiring hazardous materials teams to intervene, public health agencies should consider these models in planning and emergency response. Throughout California, many local health departments are requesting guidance and assistance for mitigation and recovery of spills involving chemicals and hazardous materials and do not have resources to address these threats. Conclusions: Compared to preparedness and response activities for biological events where public health departments have clear mandates and authorities for leadership, the roles for public health departments responding to chemical emergencies often appear to overlap with first responder entities and can often be unclear. Key informant interviews and regional workshops addressing management of chemical incidents are effective tools to prepare local health departments and laboratories to handle assessment of chemical contamination. Implications for Policy, Delivery or Practice: The resources dedicated for terrorism response should be evaluated in the context of creating added capacity to prepare for and respond to chemical threats. Since hazardous materials incidents occur frequently, they can serve as models for testing public health response capabilities and integrating intermediate and longterm interventions and coordination pertaining to contamination clean up and human health effects. Primary Funding Source: CDC ● Are Birth Outcomes Linked to Public Health System Performance? Michelyn Bhandari, M.P.H., F. Douglas Scutchfield, M.D., Evelyn Knight, Ph.D., Ann Kelly, M.H.A., I. Puiu Vasilescu, Ph.D. Presented by: Michelyn Bhandari, M.P.H., Research Associate, School of Public Health, University of Kentucky, 121 Washington Avenue, Room 105, Lexington, KY 405360003; Tel: 859.257.2821; Fax: 859.257.6644; E-mail: mwbhan2@uky.edu Research Objective: Much of published public health research has focused on evaluation of specific public health interventions, and very few studies have tested the relationship between public health system performance and health outcomes. This study examines the relationship of birth outcomes to public health system performance on the 10 essential public health services (EPHS) and to health departments’ offering certain maternal and child health programs. Answers to these questions will contribute to a better understanding of the particular contribution of public health functions to health status changes beyond what an individual program evaluation contributes. Study Design: This study uses data from three states that participated in the National Public Health Performance Standards Program test of the local assessment instrument (version 5b) in 2000. The performance data was matched by county to three additional databases: 1) the 1997 National Association of County and City Health Officials (NACHHO) profile of health departments, 2) Area Resource File (ARF) published by Health Resources and Services Administration’s (HRSA) Bureau of Health Professions in 2001, and 3) and the Community Health Status Indicators (CHSI) Project published by HRSA in 2000. Maternal child health program variables were obtained from the NACCHO profile, and birth outcome variables were obtained from the CHSI project. We explored the bivariate relationships between system performance on the 10 EPHS and maternal child health programs offered by the health departments, and between system performance and birth outcomes. This study also used multiple linear regression to assess the relationship between birth outcomes and system performance while controlling for other variables such as percent of persons below the poverty level and percent nonwhite population. Control variables were obtained from the ARF. Population Studied: This study use cross-sectional data from 152 county or city/county health department jurisdictions located within three states. Principal Findings: The mean public health system performance score on seven out of 10 of the essential services was higher among those jurisdictions offering childhood immunization programs than among those which did not offer such programs. However, system performance was inversely associated with five other maternal and child health programs provided by the HDs. Bivariate results indicated that both the infant mortality rate and percentage of low birth weight babies in our study population was statistically significantly related to public health system performance. However, after controlling for poverty and percent nonwhite, public health performance was not a significant contributor to these birth outcomes. Conclusions: Results indicate that performance of the system on the 10 EPHS is not related to birth outcomes when contextual factors are taken into account. Clearly, more research is required to determine the mechanism through which public health systems processes influence community health status. Further study using multilevel analysis will be done to explore alternative pathways of getting from system performance to community health status outcomes. Implications for Policy, Delivery or Practice: Clarification of relationships within the conceptual model of public health practice is warranted. Evidence that clearly demonstrates a pathway between public health performance and outcomes would likely generate support for performance management and quality improvement efforts in the practice sector. Primary Funding Source: CDC, ATPM ● Patterns of Alcohol Consumption within the Context of Hepatitis C Eleanor Stoller, Ph.D., Carol Blixen, Ph.D., Adam Perzynski, M.S., Joshua Terchek, BS, Stephanie Kanuck, M.S., Richard McCormack, Ph.D. Presented by: Carol Blixen, Ph.D., Associate Director for Research Program Development, Division of Clinical Research-NA-10, Cleveland Clinic Foundation, 9500 Euclid Avenue, Cleveland, OH 44195; Tel: 216.444.6254; Fax: 216.444.9275; E-mail: blixenc@ccf.org Research Objective: Research Objective: Alcohol use is discouraged or contraindicated for patients with a variety of medical illnesses. However, little is known about why patients continue to consume alcohol in the face of diagnoses that warrant a reduction in use or abstinence. The objective of this research was to explore the patterns of alcohol consumption among patients diagnosed with the Hepatitis C Virus (HCV). Study Design: Study Design: Cross sectional research design employing thematic analysis using N*Vivo, a software program for managing and coding qualitative data. Population Studied: Population Studied: Two sources of qualitative (textual) data were used: (1) 30 semi-structured interviews with currently nonproblematic drinkers (determined by the Alcohol Use Disorders Identification Test [AUDIT] scores) diagnosed with HCV at a metropolitan teaching hospital and (2) 307 illness narratives posted on Hepatitis Crelated sites on the Internet. Principal Findings: Principle Findings: We categorized decisions regarding alcohol consumption within the context of HCV into three categories: Compliance, Tailoring, and Noncompliance. Some compliant subjects quit immediately after diagnosis, whereas others quit drinking only after a delay (until they experienced disease symptoms and complications; because of negative reactions to alcohol; or for reasons not related to the diagnosis). Tailoring involved some change in drinking behavior following HCV diagnosis, most often decreases in the frequency or amount or a change in the type of alcohol consumed. Some individuals drank only on special occasions or in response to stress. Others tried to monitor their bodies for evidence of disease progression or employed strategies they believed would lessen the negative impact of alcohol. Finally, a number of individuals disregarded medical advice and continued to drink at pre-diagnosis levels (noncompliance). While some challenged recommendations of medical providers, others discounted the likelihood that alcohol-related risks applied to them. Others saw little reason to stop drinking, either because they believed there was no “cure” for HCV or because the perceived benefits of drinking outweighed the costs. Conclusions: Conclusions: Almost all of these informants were aware that alcohol consumption was contraindicated among people with a diagnosis of HCV and most could describe the negative impact of alcohol on liver function. Yet we found a proportion of HCV patients, even among these nonproblematic drinkers, who continued to consume alcohol, either at reduced or pre-diagnosis levels. Some people classified as Tailoring reported that they had “quit drinking,” but later described situations in which they still drank. Individuals often exhibited more than one pattern indicating that “adherence” may be a series of contextualized decisions that unfolded over time. Further analyses will determine the prevalence of these patterns among these respondents. Implications for Policy, Delivery or Practice: Implications for Policy, Delivery, and Practice: Abstinence from alcohol use represents a major opportunity to prevent a decline in the health and quality of life of patients with HCV and similar diseases. Information generated by this research will be incorporated into a tool designed to enhance the effectiveness of primary care providers in discouraging alcohol consumption among non-abusing/nondependent drinkers diagnosed with HCV. Primary Funding Source: NIAAA, ● The Association of Violence Perpetration and Victimization with Risky Sexual Behavior Laura Bogart, Ph.D., Rebecca Collins, Ph.D., William Cunningham, M.D., M.P.H., Robin Beckman, M.P.H., Daniela Golinelli, Ph.D., David Eisenman, M.D., Chloe Bird, Ph.D. Presented by: Laura Bogart, Ph.D., Social/Behavioral Scientist, Health, RAND Corporation, 1700 Main Street, P.O. Box 2138, Santa Monica, CA 90407; Tel: 310.393.0411Ext. 7109; Fax: 310.451.6930; E-mail: lbogart@rand.org Research Objective: Prior research has found that violence perpetration and victimization are related to greater engagement in high risk sexual behavior. However, the majority of studies have assessed overall perpetration, victimization, and risk behavior, rather than within the context of intimate or sexual relationships. Furthermore, research in this area has primarily focused on women and HIV-negative individuals. In the present study, we examined whether people with HIV who experience or perpetrate abuse within a close relationship are more likely to engage in unprotected intercourse with that same partner. We also assessed whether this association holds across women, men who have sex with men (MSM), and heterosexual men. Study Design: Data are from the Risk and Prevention (R&P) survey of the HIV Cost and Services Utilization Study (HCSUS). HCSUS used multistage national probability sampling to select a random sample of adults with known HIV infection who had at least one health care visit at a facility other than a military, prison, or emergency department from January 1996 to February 1996. The R&P sample was selected from the second HCSUS follow-up (September through December 1998); analyses were weighted to represent the entire surviving sample at second follow-up. Eight items assessed specific abusive behaviors within spousal or primary relationships (threaten to hit or throw something; push, grab, or shove; kick, bite or hit with fist; force to have vaginal or anal sex), separately for perpetration and victimization; these variables were combined and dichotomized into “any perpetration” or “any victimization” vs. none. Unprotected sex was defined as any anal or vaginal sex without a condom. Both had a “past six months” reference period. Logistic regressions were conducted predicting any unprotected sex with any perpetration or victimization, gender/orientation group (women, heterosexual men, MSM) and the gender/orientation group by perpetration/victimization interactions. Control variables included age, race, income, education, geographic region, and CD4 count. Population Studied: A total of 1421 people with HIV were surveyed. The present analyses focused on those in a close relationship (288 women, 148 heterosexual men, and 292 MSM). Principal Findings: Respondents who had perpetrated abuse within their close relationships were more likely than those who had not to report engaging in any unprotected intercourse in the past 6 months (OR = 2.54, 95%CI = 1.32-4.87, p < .01). Similarly, respondents who had been victims of abuse within their close relationships were more likely than those who had not to report engaging in any unprotected intercourse (OR = 3.01, 95%CI = 1.78-5.10, p < .001). Gender/orientation group did not moderate these effects (all ps > .10). Conclusions: Across all three gender/orientation groups, perpetrating violence and experiencing victimization within a close relationship was strongly and significantly associated with ever having unprotected sexual intercourse within that relationship. Implications for Policy, Delivery or Practice: Interventions for HIV positive individuals designed to prevent sexual transmission of HIV to close relationship partners need to take into account the sometimes abusive contexts in which sexual activity may occur, regardless of the gender/orientation group targeted. Primary Funding Source: NHLBI ● Community Social Capital, Individual Social Capital and Obesity Timothy Brown, Ph.D. Presented by: Timothy Brown, Ph.D., Assistant Director, Petris Center - School of Public Health, University of California at Berkeley, 2150 Shattuck Avenue, Suite 525, Berkeley, CA 94720-7380; Tel: 510.643.4103; Fax: 510.643.4281; E-mail: timbrownphd@yahoo.com Research Objective: This research seeks to determine the possible association between community-level social capital, individual-level social capital and an intermediate health state, obesity, in US metropolitan areas. Study Design: I examine the effects of lagged communitylevel social capital on body mass index both independently and interacted with all other variables in the model including individual-level social capital using multivariate regression analysis. I control for sex, race/ethnicity, age, marital status, education, physician office visits, smoking status, and aerobic exercise status. I test for the endogeneity of physician office visits, smoking status, aerobic exercise status, and individuallevel social capital by estimating two-stage least squares and using a Hausman-type test of endogeneity. The strength of the identifying variables in the first-stage regressions is tested using the Staiger-Stock criteria. The exogeneity of the identifying instruments in the first-stage regressions is tested using an overidentification test. Finally, the exogeneity of the social capital variables is tested using a new approach that does not require instruments: the De Luna-Johansson test. Population Studied: I study adults aged 18 years and older who live in US metropolitan areas using data from the 2000, 2001 National Health Interview Surveys and the 2000 County Business Patterns survey. Principal Findings: Individual body mass index (BMI) and community-level social capital are found to be negatively associated. Individual-level social capital is found to be positively related to BMI, but this association is attenuated in areas with higher levels of community-level social capital. Conclusions: Both community-level social capital and individual-level social capital may be important influences on individual BMI independent of sex, race/ethnicity, age, marital status, exercise, medical care, smoking, and education. Implications for Policy, Delivery or Practice: Public health professionals should further investigate possible mechanisms by which community-level social capital may affect health before making policy changes so that changes may be appropriately targeted and their effects appropriately measured. ● Systems Assessment of HIV Service Delivery in Chicago Title I EMA Douglas Bruce, M.S.W., Nathan Linsk, Ph.D., Linda Lesondak, Ph.D., Barbara Schechtman, M.P.H., Michael Bass, M.S.W., Chuck Bright, M.S.W. Presented by: Douglas Bruce, M.S.W., Jane Addams College of Social Work, Univ. of Illinois at Chicago, Midwest AIDS Training and Education Center, 1640 W. Roosevelt Road, Suite 511, Chicago, IL 60608; Tel: 312.996.0514; E-mail: dbruce@uic.edu Research Objective: To describe degree to which the primary care, mental health, and substance abuse treatment systems interact and collaborate in delivering services to persons living with HIV/AIDS; To identify obstacles to effective systems interaction; and To recommend modifications to improve systems interactions and collaborations. Study Design: Mixed methods study using semi-structured interviews of key informants from multiple service systems. Principal domains of inquiry in interview were: existing services in the systems described; gaps in services; systems linkages and interactions; existing and emerging patterns; development needs; and recommendations. First-level and second-level coding of qualitative data used to analyze responses and describe themes that emerged. Population Studied: Publicly funded systems of care providing services to persons living with HIV/AIDS, including medical care, mental health, substance abuse, case management, housing, child welfare, and corrections. Key informants included providers, administrators and consumers within these care systems. Principal Findings: There is a lack of coordination and collaboration among systems due to structural factors and different treatment paradigms. Structural factors include inconsistent eligibility criteria for clients, data reporting requirements that preculde effective collaboration among providers, and "turf battles." Divergent care models often results in a lack of knowledge among providers regarding the treatment delivered by other professional disciplines, as well as conflicting approaches to treatment. The HIV/AIDS service delivery model has shifted in recent years to a medical care model, while co-locating services in a single location is thought to improve patient access to care and present opportunities for improving coordination of care. Emerging policy changes affecting the systems of care include faithbased initiatives, decreased access to medications, and rapid testing mandates. Conclusions: Services for persons living with HIV/AIDS should be located within single locations as well as combined at the administrative level. Housing, mental health, and substance aubse services need to be expanded. A continuum of services including prevention, case finding, testing, and behavioral health services needs to be developed further. Improved collaboration, planning, and data systems are viewed as important mechanisms for eliminating duplication of services and maximizing resources. There is a need for the development of vision and leadership commitments among stakeholders to effect constructive change. Policy changes are needed at the local, state, and national level. Implications for Policy, Delivery or Practice: Developing integrated systems of care should be a priority. There is a need for coordinated data systems to better plan, coordinate, and evaluate care services. Policy issues that need to be addressed include lobbying for increased AIDS Drug Assistance Program (ADAP) funds, closer examination of disclosure issues regarding rapid testing, lobbying for expanding the maximum length of stay in residential substance abuse treatment. Providers from different disciplines and practice settings need to be crosstrained in order to overcome barriers to effective treatment coordination. Leadership from different disciplines need to have focal point discussions on how to examine HIV/AIDS care within larger care systems, and not as a free-standing system developed from dedicated federal and state funding. Primary Funding Source: HRSA, Local Title I Grantee ● Relationship of Attitudes towards Doctors and the Receipt of Preventative Services Andrea Cherrington, M.D., Donald Pathman, M.D., Giselle Corbie-Smith, M.D. Presented by: Andrea Cherrington, M.D., Research Fellow, Medicine, UNC/RWJ Clinical Scholars Program, 1004 West Trinity Avenue, Durham, NC 27701; Tel: 919.530.1164; Email: andrea_cherrington@med.unc.edu Research Objective: To examine whether an association exists between attitudes towards doctors and the receipt of preventative services. Study Design: We used data from a 2002-2003 telephone survey of adults living in 150 rural counties in 8 states of the U.S. southeast that queried respondents on their use of health services, their barriers to care and their opinions on access issues. For this study, primary independent variables were measured through four questions that were combined into two 2-item scales that assessed agreement with statements that one should (1) see doctors early and regularly and (2) avoid seeing doctors in preference of self-treatment. Chi-square analyses were used to look for associations between attitudes towards doctors and the receipt of preventative services. Findings were weighted to sampling and response probabilities. Population Studied: Individuals living in rural counties in the southeast. Minorities were oversampled. Principal Findings: Of the 4, 879 adult respondents, 54% were female, 70% were white and 27% were African American. Only half had graduated high school and 43% had an annual household income of less than $25,000. A total of 13.5% (n=656) didn´t believe in seeing doctors early and regularly and 18% (n=877) believed that one should delay or avoid seeing doctors. Persons who indicated that they don´t believe in seeing doctors early and regularly were less likely than those who do to have had a routine doctor visit in the previous year (66.1% vs 83.2%, p< 0.001), had a flu shot in the previous year (50% vs 69.9%, p=0.004), had a mammogram in the previous year (37.4% vs 60.4%, p<0.001), had a pap smear in last 3 years (81.2% vs 89.2%, p<0.001), had a cholesterol check in the last 5 years (61% vs 76.5%, p<0.00.1) or ever had endoscopic screening (34.9% vs 48.4%, p<0.001). Persons who agreed that they believe in avoiding/delaying seeing doctors also received fewer preventive services when compared with those who didn´t agree. Conclusions: Attitudes and beliefs about seeing doctors versus self-treatment are associated with the likelihood that a person will have received recommended preventative services. Implications for Policy, Delivery or Practice: Understanding individuals´ beliefs about health and the role of physicians in disease prevention will facilitate targeted interventions aimed at increasing uptake of preventative services Primary Funding Source: RWJF ● Geographic Variation in the Prescription of Schedule II Opioid Analgesics Among Outpatients in the United States Lesley Curtis, Ph.D., Jennifer Stoddard, B.A., B.S., Jasmina Radeva, M.A., Steve Hutchison, Ph.D., Raymond Woosley, Ph.D., Kevin Schulman, M.D. Presented by: Lesley Curtis, Ph.D., Assistant Research Professor, Center for Clinical and Genetic Economics, Duke Clinical Research Institute, Duke University Medical Center, PO Box 17969, Durham, NC 27715; Tel: 919.668.8101; Fax: 919.668.7124; E-mail: lesley.curtis@duke.edu Research Objective: Previous reports have examined the use of opioid analgesics, including oxycodone. However, no study has explored geographic variations in the use of these drugs systematically. We sought to measure geographic variations in opioid use in a large outpatient population. Study Design: We conducted a retrospective cohort study using the administrative claims database of a large pharmaceutical benefit manager. Main outcome measures were number of claims per 1000 total claims for opioid analgesics and oxycodone at state and county levels. We measured state-level variation using the weighted coefficient of variation and the systematic component of variation. We calculated county-level rates by dividing the number of claims for all opioid analgesics and for oxycodone by the total number of claims by zip code, which we mapped to counties to obtain aggregate figures. In univariate and multivariable analyses of county-level rates, we explored associations with explanatory variables, including sociodemographic characteristics, hospital admissions and surgeons per 1000, urban influence, and presence of state-level prescription monitoring programs. Population Studied: Subjects were included if their insurance carriers required the benefit manager to track claims at the subject level, excluding those whose plans used a single identifier for multiple family members. The data set consisted of 7,873,337 outpatients enrolled continuously from January through December 2000 and who filed at least 1 prescription drug claim during that period. Each subject's claims were linked using a unique identifier encrypted to ensure confidentiality. A total of 1171 insurers were represented, covering all 50 states, the District of Columbia, and US territories. Principal Findings: A total of 391,299 subjects (5.0%) filled a prescription for an opioid analgesic. Of almost 9 million claims, 567,778 (64.2 per 1000) were for an opioid analgesic. Claim rates varied by state from <20 to >100 claims per 1000. States with long-standing prescription monitoring programs had among the lowest rates for both opioid analgesics and oxycodone. In multivariable regression analysis of countylevel data, statewide prescription monitoring programs, number of surgeons per 1000, location in a metropolitan area, and poverty rate were independently associated with claim rates for all opioid analgesics. Monitoring programs, number of surgeons per 1000, location in a metropolitan area, and median age were independently associated with claim rates for oxycodone. Conclusions: Although there are important geographic variations in claim rates for oxycodone, they are consistent with variations in the use of other opioid analgesics. Prescription monitoring programs, number of surgical specialists, location in a metropolitan area, and poverty rate are associated with claims for oral opioid analgesics, including oxycodone. Implications for Policy, Delivery or Practice: Although prescription monitoring programs have been shown to reduce the use of opioid analgesics, some believe that physicians may under-prescribe these drugs in states with monitoring programs. Alternatively, monitoring programs may have a Hawthorne effect, whereby physicians prescribe more appropriately because their behavior is being observed. Better understanding of geographic variations will require detailed analyses of the costs, risks, and benefits of therapies and the circumstances in which they are used. Primary Funding Source: AHRQ ● The Effect of Income Question Design in Health Surveys on Family Income, Poverty and Eligibility Estimates Michael Davern, Ph.D., Holly Rodin, MPA, Timothy Beebe, Ph.D., Kathleen Thiede Call, Ph.D., Lynn Blewett, Ph.D. Presented by: Michael Davern, Ph.D., Research Associate, SHADAC, University of Minnesota, 2221 University Avenue, S.E., Suite 345, Minneapolis, MN 55414; Tel: 612.625.4835; E-mail: daver004@umn.edu Research Objective: To evaluate the differences between two methods of collecting family income information. The first method, termed “the omnibus approach,” asks for the total family income amounts with one central survey item and is used in health surveys such as the National Health Interview Survey (NHIS) and the Behavioral Risk Factor Surveillance System (BRFSS). The second method, used in the Current Population Survey Demographic Supplement (CPS-DS), sums specific amounts of income obtained from multiple income sources over everyone in the family. We call this the “summed income amounts” approach. We also assess whether there is a bias resulting from using the omnibus income item to estimate the number of people below a certain level of poverty or eligible for a public program. Study Design: We utilize the 2001 CPS-DS data because it contains both an “omnibus” and “summed income amounts” measure. First we compare the summed amount to the omnibus amount of family income. Second, we use the various sources of summed income to predict whether there is a mismatch between the omnibus and summed income amounts. Finally, if the summed amount is not within the omnibus amount range, we assign a new summed amount of income to the family that is restricted to be within the range of the omnibus amount. We compare tabulations based on the new restricted summed amounts to the previous summed income values and observe differences. Population Studied: The 2001 CPS-DS covers the noninstitutionalized US population. Principal Findings: We find a great deal of variation between the omnibus family income question and the summed income amounts from every source and every member within a family. These differences derive from predictable sources. For example, having children under 24 in the household with earned income is related to the mismatch. Furthermore, the percent of people estimated to be in poverty is higher using the omnibus income item relative to the estimates derived from the aggregated items. Conclusions: Income is often collected in health surveys as both a correlate of health insurance coverage and as a means to model public program eligibility. There are realistic constraints to including more than an omnibus income question in health surveys, such as survey administration costs, length of time per interview, and concerns about respondent sensitivity to lengthy segments of the survey focusing on income questions. However, analysts should be aware that the income data derived from such a survey is limited with respect to eligibility estimation because it tends to produce lower family income estimates and does not allow an analyst to adjust for various income disregards associated with many public programs. Implications for Policy, Delivery or Practice: The methodologies employed in this paper could be generalized to enhance health survey income data by statistically matching respondents from a survey with detailed income data to health survey data in order to have better estimates of income and the sources of income. This is important in order to develop more realistic program eligibility estimates using health survey data. Primary Funding Source: RWJF ● An Evaluation of Hazardous Materials Emergency Response Planning: Implications for Policy Improvement at the County Level in California Muntu Davis, M.D., M.P.H. Presented by: Muntu Davis, M.D., M.P.H., The California Endowment Scholars in Health Policy at Harvard University, The California Endowment, 10620 De Haven Avenue, Hansen Hills, CA 91331; Tel: 310.776.0406; E-mail: muntu_davis@post.harvard.edu Research Objective: 1. To evaluate the implementation of current federal and state hazardous materials emergency response planning policies at the county level 2. To determine the responsibilities of the different agencies involved in hazardous materials emergency response planning 3. To identify areas for improvement Study Design: Federal laws, California legislation, and emergency response planning guidelines were analyzed for legal precedence and current practice pertaining to hazardous materials emergency response planning. Data were obtained from the Department of Pesticide Regulation for pesticide incidents from the years of 1999 to 2001. Census data was obtained from the US Census Bureau for 2000. Structured interviews with State, County and Local government agencies responsible for planning and responding to hazardous materials accidents were conducted, as well as interviews with residents of Earlimart, Tulare county, California. Population Studied: Not applicable. Principal Findings: 1. California's budget cuts have limited the ability of emergency response agencies to prepare for hazardous materials accidents. 2. At minimum, emergency response plans are conducted undergo yearly reviews, which may simply include updating phone numbers. 3. Some agencies are able to conduct tabletop exercises with a limited number of their staff. These exercises do not test all skills required for an actual response effort. 4. No interagency drills are performed. 5. The public and its needs, e.g. linguistic, are not included in the planning process. 6. Bio-terrorism has a) increased funding for pre-hazard mitigation planning and b) heightened the awareness of the need to improve communication among different emergency response agencies at and between different levels of government. 7. Hazardous materials emergency response planning is not viewed the same as bio-terrorism preparedness despite the fact that the protocols are the same for both. Conclusions: The legislation and guidelines reviewed are theoretically very comprehensive and sound in terms of outlining the process of hazmat planning and response. However, as the number of agencies responding to a hazardous materials accident increases, the chance of an ineffective response increases. Considering this, a few recommendations can be made to improve the current hazardous materials emergency response system. Implications for Policy, Delivery or Practice: The key to effective emergency management is rapid, well planned responses. And as first responders, county and local agencies need to plan and to practice working together to ensure an effective response to any type of emergency. Therefore, I recommend the following: 1. Consolidate grant programs for emergency response efforts into larger partnership grants given to local governments with accountability provisions based on objective measures of outcomes or effectiveness. 2. More state or regional oversight over county planning and preparation, recognizing that local responders begin the process and activation of the emergency response system in the state. 3. Interagency drills every 2 or 3 years for improved interagency coordination and communication. 4. Ensure that resources used for bio-terrorism preparedness coincide with the needs for hazardous materials response planning and preparation. 5. Pesticide-related disasters are different in nature and risks compared with other emergencies, like a fire, flood or civil unrest. Yet, all can be very dangerous and involve a large number of people. 6. Inclusion of the public would enable emergency responders to assess needs, e.g. language needs, prior to an emergency. Primary Funding Source: The California Endowment ● UNC Certificate Program: Are We Training the Public Health Workforce? Mary Davis, Dr.PH, MSPH Presented by: Mary Davis, Dr.PH, MSPH, Program Planner and Evaluator, North Carolina Institute for Public Health, UNC School of Public Health, CB 8165, Chapel Hill, NC 27599; Tel: 919.843.5558; E-mail: mary_davis@unc.edu Research Objective: Public health workers need to be trained in the latest approaches of the core public health sciences. Developing distance-learning methods that use a lifelong learning framework to train the public health workforce has been identified as an essential strategy for improving the public health system infrastructure and meeting the public health needs of the nation. A number of schools and programs in public health have created public health worker training programs. The University of North Carolina at Chapel Hill School of Public Health (UNC SPH) created the on-line Certificate in Core Public Health Concepts with public health workers as the primary target audience. Public health worker participation in these programs, however, has yet to be examined. Additionally, there has been considerable debate as to who should be counted as a public health worker. The purpose of this research was to define and examine public health worker participation in the UNC SPH Certificate Program. Study Design: The National Public Health Performance Standards Program defines the public health systems as public, private, and voluntary entities that contribute to delivery of essential public health services within a jurisdiction. Using this definition, all Certificate programs applicants were assigned a job code by place of employment. Population Studied: Applicants were classified as: 1) Public Health Agency workers work for a state or local health department, only, 2) Public Health System workers work for healthcare providers such as hospitals or laboratories, human services and charity organizations, and 3) “Other” category work for organizations that are not among those listed above, e.g. temporary agencies. Applicants were also categorized by participation in the program: 1) Participants were current students or graduates of the program, 2) Nonparticipants enrolled in a course but subsequently withdrew from the program and those accepted who never enrolled in any courses. Principal Findings: Among 273 applicants examined, 147 (54%) were classified as Nonparticipants and 126 (46%) were classified as Participants. Of the total applicants, 36 (13%) have completed the program. Fifty three (19 %) of the applicants were classified as Public Health Agency Workers, 174 (64%) were classified as Public Health System Workers, and 46 (17%) were classified as being employed in the Other category. Among Nonparticipants, 31 (21%) were Public Health Agency Workers, 89 (61%) were Public Health System Workers, and 27 (18%) were classified in the Other category. Among Participants, 22 (17.5%) were Public Health Agency Workers, 85 (67.5 %) were Public Health System Workers, and 19 (15%) were classified in the Other category. Among graduates, 8 (22%) were Public Health Agency Workers, 22 (61%) were Public System Workers, and 6 (17%) were classified in the Other category. This paper will also present Participation satisfaction with the program and student performance. Conclusions: The Certificate applicants and enrollees include a number of government public health agency employees as well as public health system workers from more direct care settings. Implications for Policy, Delivery or Practice: While online programs reach the public health workforce, no specific benchmarks for participation have been established. This research provides insight into the participation of public health agency workers in training. ● Preparedness for Bioterrorist Events and Other Public Health Emergencies in Rural Florida Aram Dobalian, Ph.D., M.P.H., J.D., Jennie Tsao, Ph.D. Presented by: Aram Dobalian, Ph.D., M.P.H., J.D., Assistant Professor, Health Services Administration, University of Florida, P.O. Box 100195, Gainesville, FL 32610-0195; Tel: 352.273.6081; Fax: 352.273.6075; E-mail: adobalia@phhp.ufl.edu Research Objective: Approximately 80% of U.S. land is classified as rural. Rural communities are found in all states, and 65 million Americans live in these communities. Because of their remote locations and limited resources, rural communities have specific concerns that vary from urban communities when it comes to recovery from mass casualty events. Whereas existing studies have addressed medical needs such as injury or physical trauma, little is known about how rural health care providers will respond to the intermediate and longer-term health needs, particularly mental health needs, of rural communities following bioterrorist and other public health emergencies. Study Design: This study used key informant interviews to assess existing preparedness based on the structure, process and outcomes of care, as well as knowledge/awareness of preparedness among primary care providers. We evaluated which models are working with regard to quality of care, and which models promoted greater provider awareness of what to look for and who to ask for assistance following bioterrorist and other public health emergency events. We also examined special concerns of certain vulnerable, priority populations including women, children and families, and frail elders. Population Studied: To date, we have examined a mix of various organizations within rural communities in Northern Florida: community health centers and the public health system, primary care clinics, hospitals, individual providers, and a long-term care provider. Principal Findings: Bioterrorism was not perceived to be a significant threat to rural communities, and some interviewees expressed concern that resources are being diverted from what they perceived to be higher priority health needs. Providers did indicate some heightened interest from patients around the time of major news events (e.g., anthrax, SARS). Many interviewees were aware of the existence of bioterrorism preparedness plans, but few expressed familiarity with the details of those plans. Existing resources were viewed as inadequate to meet current mental health needs. Few providers identified PTSD as a likely consequence of bioterrorism. Conclusions: Public health emergencies were generally viewed as less important than the common chronic conditions that confront providers in rural communities. Existing resources may be inadequate to meet current health needs given comments by interviewees who stressed the need to address inadequate access to providers, especially specialty care (e.g., mental health, dental health), and patient-level barriers to care such as a lack of insurance, the cost and distance involved in transportation, and a lack of financial resources to pay for care. These issues would be exacerbated by a mass casualty event. Implications for Policy, Delivery or Practice: Greater education and training regarding mental health conditions that may result from or be exacerbated by major public health emergencies is necessary for primary care providers. This training may have the added benefit of assisting providers in decreasing unmet need for mental health care in rural communities. Primary Funding Source: AHRQ, Health Resources and Services Administration ● Adopting and Adapting Small Area Variation to Improve Clinical Quality of Care in Health Plans Huda Fadel, M.P.H., Ph.D. Presented by: Huda Fadel, M.P.H., Ph.D., Manager, Health Services Research, Center for Health Care Quality and Evaluative Studies, Blue Cross Blue Shield of Michigan, 600 East Lafayette, Mailcode J418, Detroit, MI 48226; Tel: 313.225.7175; Fax: 313.225.5993; E-mail: hfadel@bcbsm.com Research Objective: Small area variation (SAV) analysis in health care has been in use since the 1970s, and its findings of variation have spurred improvement in quality of care through evidence based medicine. Most SAV work has come from academia, relying on large Medicare or other national files and reporting findings with system-wide implications. Health plans can play an important role in reducing variation, however, it is only recently that they have begun to adopt SAV to diagnose problems, establish priorities and target resources in their health management programs. Although SAV has great potential, turning research into practical solutions has been a challenge Study Design: Blue Cross Blue Shield of Michigan (BCBSM), the state’s largest commercial health insurer, has adopted this approach to understanding utilization and improving quality of care for its population. Its atlases show extensive practice variation, in some health topics more than others. 1. In 2000, BCBSM, in conjunction with the Center for Evaluative Clinical Sciences, produced the Dartmouth Atlas of Health Care in Michigan, one of the first examinations of its kind in commercially-insured populations. The Atlas addressed variation in several medical conditions, surgical procedures, end-of-life care and pharmacy utilization and is published on the company’s website. 2. One of the Atlas’ most interesting findings was the wide variation in pediatric ADHD prescribing. In 2003, BCBSM collaborated with researchers at the University of Michigan Medical School to study quality of care for ADHD. A parallel investigation into the Michigan Medicaid population was included for comparison purposes. 3. In 2004, four BCBS plans will collaborate to produce an Atlas of pharmacy utilization and quality measures. This Atlas will provide empirical benchmarks and a national platform for sharing and discussion best practices in pharmacy programs Principal Findings: The empirical findings from these atlases have been excellent vehicles for educating consumers and providers. Corporate quality studies now include an SAV analysis and atlas in their plan; all results are published in the company’s newsletters and on its website. Over time, it is anticipated that variation will decrease for these topics. Similar efforts are being investigated for provider profiles and customer reports. Community coalitions use atlas findings to improve quality in their areas. This helps target resources and efforts in the areas where they are needed. BCBSM works closely with these groups. Another area under development is focused provider networks and centers of excellence, based on the practice of evidencebased medicine. Most progress to date has been on health issues for which medical science is clear (and variation is “unwarranted”). The issues for which guidelines are not available are problematic, though we know there is variation. Health plans struggle with the question of “which rate is right?” and appropriate actions. Meanwhile, variation continues to entails high cost. Conclusions: Most progress to date has been on health issues for which medical science is clear (and variation is “unwarranted”). The issues for which guidelines are not available are problematic, though we know there is variation. Health plans struggle with the question of “which rate is right?” and appropriate actions. Meanwhile, variation continues to entails high cost. Implications for Policy, Delivery or Practice: Large health plans have immense data assets that are well-suited for SAV studies. These activities are resource intensive, and are undertaken to improve health care. Although the method has generated a great deal of interest, turning research into practical solutions remains a challenge ● Proactive Recruitment of Health Plan Members into Smoking Cessation Counseling Jodi Summers Holtrop, Ph.D., Huda Fadel, M.P.H., Ph.D, Sam Vansen, MHSA, David Weismantel, M.D., M.S., William Wadland, M.D., M.S. Presented by: Huda Fadel, M.P.H., Ph.D, Manager, Health Services Research, Center for Health Care Quality and Evaluative Studies, Blue Cross Blue Shield of Michigan, 600 East Lafayette, Mailcode J418, , MI 48226; Tel: 313.225.7175; Fax: 313.225.5993; E-mail: hfadel@bcbsm.com Research Objective: The purpose of the study is to determine if delivery of proactive phone calls or postcards to health plan members currently using pharmacotherapy alone increases participation in smoking cessation counseling services and to assess the resource costs to the program of doing so Study Design: Health plan members filling pharmacotherapy claims were identified weekly from health plan pharmacy claims data and randomized into one of three groups: control, recruitment postcard, or recruitment phone call by a nurse counselor. Enrollment of study members to the smoking cessation program was tracked for one month Population Studied: Adult members of a large health insurer in Michigan. Subjects were enrolled in the PPO or indemnity product and had pharmacy coverage Principal Findings: Over a 5-month time period, 625 total individuals were identified for participation in the study with the following respective enrollments to the program: 0/157 control; 2/156 postcard; 66/312 phone call recruitment (p<0.0001). Over 50% of the prescriptions were for bupropion. Most of the members (53%) had quit by the time of the call. Members with lower confidence (p=0.02) and experiencing episodes of relapse (p<0.0001) were significantly more likely to enroll in the counseling services. The 2-month quit rates for the phone call participants were similar to other participants spontaneously calling to enroll during the same time period. Total costs for each intervention were: $3389 (phone) and $4766 (call). Incremental cost per intervention type shows $73.25 per participant receiving postcards and $24.56 per telephone participant Conclusions: Query of a pharmacy database to identify smokers filing claims for pharmacotherapy and proactive telephone recruitment by smoking cessation counselors of a health plan may be an effective way to reach smokers attempting cessation in a non-HMO environment. Although the total investment of personally contacting individuals by telephone is high, the resulting enrollment makes it the most cost-effective way of encouraging participation in quitlines Implications for Policy, Delivery or Practice: Compared to the use of pharmacotherapy alone, smoking cessation counseling provided to those making a quit attempt increases the likelihood of successfully quitting over no additional assistance. Many smokers attempting cessation do not access methods available to them that would increase their chances of successful cessation. Methods for encouraging participation in effective programs are needed and proactively contacting smokers may be one of them. Primary Funding Source: RWJF ● Combining the Benefits of Decision Science and Financial Analysis in Public Health Management: A County-Specific Budgeting and Planning Model Peter Fos, Ph.D., M.P.H., Danny Miller, M.B.A., CB.A., Brian Amy, M.D., MHA, M.P.H., Miguel Zuniga, M.D., DrPH Presented by: Peter Fos, Ph.D., M.P.H., Chief Science Officer, Mississippi State Department of Health, 570 E. Woodrow Wilson, Jackson, MS 39216; Tel: 601.942.8367; Email: Peter.Fos@msdh.state.ms.us Research Objective: Determine the benefit of combining the use of decision and financial analysis by developing a countyspecific budgeting and planning model, using multi-attribute utility methodology. Study Design: A modified Delphi technique was used to develop a decision support system to assist in budgeting and planning. The decision support system variables were based on three national sets of indicators:the CDC Health Objectives for the Nation Consensus Set of Health Status Indicators for the General Assessment of Community Health Status -United States; the UnitedHealth Group State Health Rankings, and the newly released Institute of Medicine 20 Key Areas to Transform Health Care System. An additive multi-attribute utility method is employed to develop a scoring system to rank statewide health status objectives according to a weighted numerical score. Four objectives related to health risks, health outcomes, health resources, and healthcare quality are used to measure each board's member’s perceptions of importance in each indicator. The four objectives were subdivided into 20 sub-objectives representing detailed health status data. A county-specific interactive computer based model was developed to determine the impact of changes in budgeting and planning on each county’s capability to achieve services delivery objectives. These services delivery objectives were determined following the Agency mission and vision, associated with financing issues and considerations. Population Studied: The state of Mississippi population was the target population for the study. Specifically, since the decision support system is a county-specific budgeting and planning model, each of the 82 counties in the State represented the unit of analysis. Group meetings of board members, district health officers and administrators were held to assess valuations and trade-offs across a set of objectives for health status assessment. Principal Findings: The county-specific budgeting and planning model is a reasonable decision support system for use in a public health agency. The model illustrates the impact on a county health department’s capability to deliver public health services, as well as indicates the expected change in health measures. One benefit is that the model allows for planning and budgeting, and the analysis or the associated effects, without the restrictions of categorical funding and financing. The decision support system can be used for real-time budgeting and planning, as well as simulations that can assist in strategic financial decision making. Conclusions: The county-specific budgeting and planning model allowed for better alignment of available resources to existing needs, which enhances individual county capacity. This promotes the highest utility decision making process for the Agency. In addition, local monies can be used to enhance local capacity, whereas Federal, State must be spread across the state evenly. The flexible use of discretionary monies allow the Agency, through the use of the county-specific budgeting and planning model, to identify achievable improvement in county capacity rather than expending scarce resources into unachievable, no matter how worthy or noble, pursuits. Deciding which partnerships and collaborations will be most successful for the State, and where these initiatives should occur, results in better outcomes and avoids those situations in which money is spent with less than favorable outcomes. Implications for Policy, Delivery or Practice: This information can be used to redesign processes of care, design quality improvement initiatives, and to guide policy formulation and implementation. Primary Funding Source: Mississippi State Department of Health. ● Local Preparedness Drills: Establishing Criteria Kristine Gebbie, Dr.PH, R.N., Patricia Hegadorn, M.P.H., R.N., Kristine Qureshi, DNSc, RN, Jacqueline Merrill, M.P.H., R.N. Presented by: Kristine Gebbie, Dr.PH, R.N., Associate Professor and Director, Center for Health Policy, Columbia University School of Nursing, 630 West 168th Street, M.B. 6, New York, NY 10032; Tel: 212.305.1794; Fax: 212.305.0722; E-mail: kmg24@columbia.edu Research Objective: As a part of a large project to establish criteria for evaluating local public health agency emergency preparedness drills and exercises, develop and validate an evaluation framework and methodology. Study Design: A qualitative method combining extensive literature review, expert panel assessment and response from the practice field. Population Studied: The ultimate population is the 2600 local public health agencies in the US; the population for the framework establishment is a deliberate panel of experts in emergency response and public health emergency response. Principal Findings: The initial framework developed from earlier studies of emergency preparedness is too general and non-quantifiable; combining the framework with key quality elements (structure, process, outcome) allows for identification of key points for quantifiable data. Conclusions: The expert draft framework is sufficient for a first round of testing with the 12 Project Public Health Ready pilot sites, adjustment based on findings, and testing with a larger sample of 60 sites. Implications for Policy, Delivery or Practice: Current assessment of emergency response exercises is generally impressionistic, done immediately after the drill (the FEMA 'hot wash') and does not allow for measurement of improvement over time or comparative research on components or methods of improvement Primary Funding Source: CDC ● Counting Public Health Workers: A Comparison of Data Sources Kristine Gebbie, Dr.PH, R.N., Jacqueline Merrill, M.P.H., R.N., Lorraine Sanders, M.S., RN, Eric Gebbie, M.A., MIA Presented by: Kristine Gebbie, Dr.PH, R.N., Associate Professor and Director, Center for Health Policy, Columbia University School of Nursing, 630 West 168th Street, M.B. 6, New York, NY 10032; Tel: 212.305.1794; Fax: 212.305.0722; E-mail: kmg24@columbia.edu Research Objective: Identify differences in reported numbers of key public health professionals in two widely used data bases, both of which have been criticized, and develop hypotheses that might be explanatory of the differences Study Design: Comparative display of data on key public health professions from the HRSA-sponsored Public Health workforce 2000 and the Department of Labor Bureau of Labor Statistics. Population Studied: Data reported on key public health professional groups in Public Health Workers Enumeration 2000 and 2002 Bureau of Labor Statistics report. Principal Findings: The numbers reported in Enumeration 2000 are consistently smaller than those included in the Bureau of Labor Statistics; the proportion of professionals within any one class reported as being federal, state or local varies widely as well. Conclusions: The reporting sources used for the two reports can account for much of the difference, but is not adequate to allow a choice between the two. Implications for Policy, Delivery or Practice: The public health policy-making community must make decisions about needed data and establish a routine for data collection and analysis that can be viewed as sufficiently reliable for policy use. ● Hepatitis C among Homeless Adults in Los Angeles Lillian Gelberg, M.D., MSPH, Marjorie Robertson, Ph.D., Lisa Arangua, M.P.P., Ronald Andersen, Ph.D., Barbara Leake, Ph.D., Hal Morgenstern, Ph.D. Presented by: Lillian Gelberg, M.D., MSPH, George F. Kneller Professor, Department of Family Medicine, David Geffen School of Medicine at UCLA, 50-071 CHS Box 951683, Los Angeles, CA 90095-1683; Tel: 310.794.6092; Fax: 310.794.6097; E-mail: lgelberg@mednet.ucla.edu Research Objective: Persons infected with the hepatitis C virus (HCV) are at high risk for serious long-term health problems, and they are potentially infectious to others. NIH’s national agenda for preventing the spread and consequences of hepatitis C includes early detection, treatment, and prevention efforts for high-risk and infected persons. Recent research by our team and others suggests that homeless adults in urban areas are at particularly high risk for HCV infection due to their high rates of risky drug use. Despite their apparent high risk, however, there are no population–based studies of hepatitis C in this group. For emerging infectious diseases, protecting the health of the community as a whole will depend on protecting the health of those most at risk. The objective of this study was to document the prevalence and correlates of hepatitis C infection among homeless adults, and to identify high-risk sub-groups that should be targeted for screening and subsequent treatment or prevention efforts. Study Design: We conducted a community-based probability survey of 500 homeless adults in 41 shelters and meal programs in the Skid Row area of Los Angeles, using a 2-hour face-to-face interview and blood testing for HCV, HBV, and HIV. Population Studied: 500 homeless adults. Principal Findings: Rates of lifetime infection were as follows: HCV (28.7%), HBV (ever infected 32.7%, currently infected 2.2%), HIV (3.7%); 47% had ever been infected with either of these three infections. Most adults with lifetime HCV infection (59%) also had been infected in their lifetime with HBV. HCV rates were higher among: lifetime IDUs (85%, but only 52% of HCV+s reported IDU), lifetime intranasal drug users (37%), sex workers for cash, but not for drugs) (46%), 3+ tattoos in lifetime (48%), transfusion before 1990 (41%), older adults (18-29 yrs 0%, 30-49 yrs 26%, 50+ yrs 37%), former prison inmates (52%), and among men who had sex with men (28%) (all p < .001). There was no significant variation in HCV by gender (men marginally higher), ethnicity (black, white, Latino), chronic homelessness, recruitment site (shelters vs. meal programs), blood transfusion history, or psychiatric hospitalization history. Despite their high HCV rates, only 37% of the overall sample had ever been tested for HCV. Among HCV+s, 50% had never been tested for HCV, only 24% knew they had HCV, and only 24% had ever been counseled about HCV. Conclusions: As expected, hepatitis C rates were high among the Los Angeles homeless population relative to the general population (28.7% vs. 1.8%). Persons infected with HCV were at high risk for being infected with HBV, suggesting the need for HBV vaccination programs for this high risk population of homeless adults. Consistent with the literature in other populations, injection drug use was the strongest risk factor for HCV infection. However, since only half of those infected reported IDU, other risk factors for HCV infection might also be important among homeless adults. Implications for Policy, Delivery or Practice: The findings from this study will be used to inform clinicians, health planners, and health policymakers regarding HCV screening, prevention, and treatment for homeless persons. Primary Funding Source: NIDA ● Factors Associated with Receipt and Adherence to Lifestyle Recommendations and Impact on Hypertension Control Mark Horng, M.D., LeRoi Hicks, M.D., M.P.H., Earl Francis Cook, SD Presented by: Mark Horng, M.D., General Medicine Fellow, Division of General Medicine, Brigham and Women's Hospital, 1620 Tremont Street, Boston, MA 02120-1613; Tel: 617.732.4815; Fax: 617.732.7072; E-mail: mhorng@partners.org Research Objective: To examine rates of adherence to suggested lifestyle modifications for HTN management and of associated blood pressure control Study Design: Nationally representative, cross-sectional survey using a stratified multistage probability sample of noninstitutionalized, civillian population of the US. Population Studied: The NHANES 1999-2000 survey participants aged 20 or older who were told they had HTN at least twice by a doctor or other health professional were included in logistic regression model to determine factors associated with adherence to therapies and rates of hypertension control. Principal Findings: Of aware hypertensive individuals (n=1244), 146 (13.1%) were only advised to take medications and 81 (7.3%) to alter lifestyles, while 846 (76.0%) were advised to do both. Patients advised to take medication only had higher adherence rates (84.2%), than those advised to modify their lifestyle only (54.3%), or advised to do both (53.9%). Hypertension is controlled in 36.6% of those taking medications, 56.8% of those following lifestyle changes, and 46.1% doing both. Individuals are less likely to receive lifestyle recommendations if they are aged 60 or greater (OR 0.25; CI 0.13-0.48), are white (OR 0.46; CI [0.23-0.89]), or have completed high school (OR 0.39; CI [0.19-0.81). Individuals who are obese (BMI>30) (OR 0.25; CI [0.150.42]), diabetic (OR 0.42; CI [0.20-0.89]), or hypercholesterolemic (OR 0.49; CI [0.30-0.80]), have lower odds of adhering to lifestyle recommendations, while higher odds of adhering to lifestyle recommendations were associated with being white (OR 1.76; CI [1.04-2.96]) or age 60 or older (OR 2.29; CI [1.33-3.96]). Conclusions: Despite higher adherence rates, prescribing medications alone has lower rates of hypertension control combined to prescribing both medications and lifestyle modification. Implications for Policy, Delivery or Practice: Clinicians should recommend and encourage adherence to both medications and lifestyle changes for optimal management of hypertension, and future research examining patterns of care for hypertension should examine rates of advising lifestyle modification as well as medication prescribing. Primary Funding Source: HRSA ● Bioterrorism-Related ED Utilization: NYC 2001 Nathaniel Hupert, M.D., M.P.H., Mary Koshy, MPA, Jason Cuomo, M.P.H., Neal Flomenbaum, M.D. Presented by: Nathaniel Hupert, M.D., M.P.H., Assistant Professor of Public Health and Medicine, Departments of Public Health and Medicine, Weill Medical College of Cornell University, 411 E. 69th Street, New York, NY 10021; Tel: 212.746.3049; Fax: 212.746.8544; E-mail: nah2005@med.cornell.edu Research Objective: To quantify surge emergency department (ED) admissions temporally and geographically related to the 2001 New York City anthrax attacks. Study Design: We examined ED admissions data from 9/01/01 to 12/31/01 as well as comparison data from the same time frame in years 2000 and 2002 from three hospitals in New York City located near midtown Manhattan (Hospital A), the Bronx (Hospital B), and Brooklyn/Queens (Hospital C). We compared ED admissions per day for all visits and for selected individual primary ICD-9 codes, including those for respiratory symptoms, chest pain, gastrointestinal symptoms, and malaise and fatigue. In addition, we pooled ED admissions by patient zip code to study geographic trends in admissions. We hypothesized that ED admissions for respiratory complaints would be higher at the study hospitals in October 2001 (the month of peak anthrax-related activity) than in other study months. Population Studied: Urban population in metropolitan area targeted by 2001 anthrax attacks. Principal Findings: The average daily ED census in 2001 at Hospital A was 119.9 (2000=114.4, 2002=114.2), at Hospital B was 363.4 (2000: 343.8, 2002: 372.6), and at Hospital C was 166.7 (2000=160.0, 2002=147.1). Hospital A experienced a significant rise in ED admissions during October 2001 compared to other months in 2001 as well as 2000 and 2002 (average daily census October 2001=129.3; other months in 2001=116.7, 2-tailed Student’s t-test p=0.0007; October ‘00/02=112.8, p<0.0001). Hospitals B and C did not experience a statistically significant rise in ED admissions in October 2001 compared to other months in 2001. The increase in ED admissions at Hospital A was not attributable to cases with primary ICD-9 codes for chest pain, respiratory ailments, gastrointestinal disturbance, or malaise and fatigue. However, there was a significant rise in cases coded as “V01.9, communicable disease contact NOS” (October, 2001=93, all other study months of 2001=70, Chi2=12.09, p value=0.0005). Hospitals B and C had insignificant numbers of V01.9 diagnoses (<10 for entire study period). Hospital A also had significantly more admissions arising from its local zip code during October 2001 compared to other months in 2001 (t-test p=0.02) and to October of ‘00/’02 (p<0.0001). Conclusions: The study hospital closest to the epicenter of the 2001 NYC anthrax attacks (i.e., midtown Manhattan) experienced a significant increase in ED admissions during October 2001. At least part of this surge appears to have been local attack-related admissions that were coded as “communicable disease contact.” In contrast, the two more distant study hospitals did not experience any significant surge in ED admissions during this time period. Implications for Policy, Delivery or Practice: This study provides the first quantitative assessment of potential overloading of hospital-based emergency services in the aftermath of the first lethal bioterrorist attack on U.S. soil. Our results do not support the notion of a generalized increase in ED utilization during the 2001 anthrax attacks. Rather, the impact of the attacks on ED utilization appears local even within an affected metropolitan area. This finding has important implications for planning of emergency response and health care resource allocation in the aftermath of future bioterrorist attacks or natural epidemics. Primary Funding Source: AHRQ ● Policy Implications of Dual Healthcare Use Across Medicare and VA Denise Hynes, Ph.D., R.N., Min-Woong Sohn, Ph.D., Kristin Koelling, M.P.H., Noreen Arnold, M.S., Larry Manheim, Ph.D., Fran Weaver, Ph.D. Presented by: Denise Hynes, Ph.D., R.N., Director, VA Information Resource Center, Edward Hines Jr. VA Hospital, 5th Avenue and Roosevelt Road, Building 1, Room C303, Hines, IL 60141; Tel: 708.202.2413; Fax: 708.202.2415; Email: hynes@research.hines.med.va.gov Research Objective: The Medicare and Department of Veterans Affairs healthcare systems represent the largest healthcare systems in the U.S. An increasing number of elderly use both systems of care. Such dual use has significant implications for coordination of care, quality of care, and economic impacts at the patient, provider and societal level. We linked data from the VA and the Centers for Medicare and Medicaid Services (CMS) to examine patterns of healthcare utilization and costs across systems. Study Design: We combined data from CMS and VA for calendar year 1999 to identify a cohort of dually eligible elderly. Using linked demographic, health care utilization and claims data across the two systems of care, we examined factors predictive of the healthcare system used. For risk adjustment, we used the Hierarchical Condition Categories (HCC) risk scores that will be used to adjust for differences in risks for Medicare reimbursement in 2004. Hierarchical categories in HCC are designed to allow for coding variations due to different financial incentives under the VA and Medicare. We compared VA-only use, Medicare-only use or dual usage patterns using multinomial logistic regression on a 5% random sample (N = 86,140). Population Studied: A cohort of 2.6 million elderly who were dually eligible for VA and Medicare in 1999. Principal Findings: Of all dually eligible veterans, 83.7% were enrolled in Medicare fee-for-service. Of these, 21.9% used only VA services, 30.3% used only Medicare services; 42.6% used both VA and Medicare services. Compared with Medicare-only users, VA-only users tended to have a high VA priority level (Odds Ratio [OR] = 20.85; P < 0.001) or lived less than 10 miles from a VA inpatient facility (OR = 2.09; P < 0.001), while dual users tended to be older (85 or older, OR = 2.23; P < 0.001; 75 – 84, OR = 1.40; P < 0.001). AfricanAmericans were more likely to be VA-only users, but, when their Medicare premiums were paid through state Medicaid programs, they tended to use both systems of care more than non African-Americans. Patients with high-risk scores (indicating poorer health status) were more likely to be dual users and those with the lowest risk scores were more likely to use VA alone. Conclusions: Adjusting for patient age, race, and other demographic factors, older and sicker elderly tended to use both systems of care more, while the least sick were more often users of VA services exclusively. Eligibility (e.g., VA priority score and Medicare state buy-in status) and access (e.g., distance to the nearest VA inpatient facility) were important determinants of dual use patterns. Implications for Policy, Delivery or Practice: Dually eligible may use heath care services from both VA and Medicare, creating the potential for fragmentation and duplication of care. Understanding how the elderly manage their health care is important for both systems of care. For example, low-income elderly with poor health status may benefit from improvements in continuity of care across the two systems of care. Future research should examine whether coordination of care between VA and Medicare providers can improve patient outcomes. Primary Funding Source: VA ● VA and Medicare Dual Use by Veterans with Colorectal Cancer Denise Hynes, Ph.D., R.N., Min-Woong Sohn, Ph.D., Ruth Perrin, M.A., Kristin Koelling, M.P.H., M. Rosario Ferreira, Ph.D., Charles Bennett, Ph.D. Presented by: Denise Hynes, Ph.D., R.N., Director, VA Information Resource Center, Edward Hines Jr. VA Hospital, 5th Avenue and Roosevelt Road, Building 1, Room C303, Hines, IL 60141; Tel: 708.202.2413; Fax: 708.202.2415; Email: hynes@research.hines.med.va.gov Research Objective: Veterans with colorectal cancer (CRC) require combination therapy including surgery, chemotherapy and/or radiation therapy, and long-term follow-up. To ensure CRC patients’ extensive healthcare needs are being met, understanding patterns of healthcare use between VA and Medicare-covered systems is important. Study Design: Of 2.6 million VA and Medicare dually eligible beneficiaries in CY1999, we identified CRC patients based on diagnosis coding. Using linked demographic, health care utilization and claims data across the two systems of care, we examined factors predictive of the healthcare system patients used. We performed multivariable regression analyses, including disease severity/risk category determined by Hierarchical Condition Categories (HCC). We compared VA-only use, Medicare-only use or dual usage patterns using multinomial logistic regression. Population Studied: We identified 33,001 patients with CRC who were age 65 or older and were dually eligible. Principal Findings: There were 33,001 veterans age 65 or older with CRC. VA only use, rather than dual use was more likely among CRC patients who had higher VA priority levels (Odds Ratio [OR] = 3.1, p < 0.001), were African American (OR = 2.8, p < 0.001), and lived <10 miles from VA hospitals (OR = 2.3, p < 0.001). Those who used only VA services, compared to those who used only Medicare services, were more likely to have poorer health (OR = 2.0, p < 0.001), be older (OR = 2.3, p < 0.001, for 85 and older compared to 65 to 74 years old), and African American with low incomes (OR = 2.6, p < 0.001). Conclusions: CRC patients with higher risk scores tended to use Medicare services more, but the sickest, poorest and minority CRC patients were most likely to use both Medicare and VA services. Implications for Policy, Delivery or Practice: Minority CRC patients in the VA with the poorest health status may benefit most from improvements in coordination of care throughout the continuum of care across systems. Coordination of prevention, early identification, and treatment improvements across health care systems are needed to benefit those most in need. Primary Funding Source: VA ● What Do Local Public Health Departments Do? Evelyn Knight, Ph.D., F. Douglas Scutchfield, M.D., Michelyn Bhandari, M.P.H., Ann Kelly, M.H.A., Mary Kay Rayens, Ph.D. Presented by: Evelyn Knight, Ph.D., Project Director, School of Public Health, University of Kentucky, 121 Washington Avenue, Room 107C, Lexington, KY 40536-0003; Tel: 859.257.9168; Fax: 859.257.6644; E-mail: eknig0@uky.edu Research Objective: Characterizing local public health departments and their programs in a standardized manner has become a national policy concern due to the lack of standardization. Programs to accredit local agencies are being discussed and the National Association of County and City Health Officials (NACCHO) is developing an “operational definition” of local public health agencies that would define the minimum requirements. This study sought to determine if patterns exist in the groups of programs offered by local health departments. Study Design: Using data from NACCHO’s 1997 National Profile of Local Health Departments, the programs offered by local agencies were studied. Factor analysis based on a tetrachoric correlation matrix was applied to create groups of programs that tended to be offered together. Programs selected for inclusion in the analysis were the 34 general programs included in the profile plus nine more specific chronic disease programs. Population Studied: A group of 152 health departments in three states were studied. These health departments had completed the 1997 NACCHO Profile as well as a test version of the NPHPSP performance assessment, indicating their interest (or that of their state public health agency) in performance improvement. Principal Findings: Since the factor analysis required variation in the programs offered, 13 programs were removed that were provided by 80% or more of the health departments. Four other programs were removed because they were offered by 20% or fewer health departments, and one was removed because a correlation was not calculable. For the remaining 25 programs three factor groups were identified: (1) ten “basic” programs, (2) seven “expanded clinical” programs, and (3) eight “outreach” programs. Conclusions: Public health programs offered in this sample of local health departments clustered into groups that seem to indicate specific policy direction. Further analysis on other, larger numbers of health departments, with more specific qualitative and quantitative information on the programs, may classify different types of local health departments based on their program offerings. Implications for Policy, Delivery or Practice: Development of a typology describing local health agencies based on their program offerings would enable more directed planning to enhance and standardize public health services available to all populations. This typology would assist decision makers assessing state and national initiatives to augment public health services provided locally. In addition, relationships of public health infrastructure and high performing agencies to the types of services offered by local agencies could be evaluated. Primary Funding Source: CDC, ATPM ● Preventing Unnecessary Hospitalizations: How is the U.S. Doing? Denise Kruzikas, Ph.D., H. Joanna Jiang, Ph.D., Denise Remus, Ph.D., R.N., Marguerite Barrett, M.S., Rosanna Coffey, Ph.D., Roxanne Andrews, Ph.D. Presented by: Denise Kruzikas, Ph.D., Health Researcher, Research and Pharma, Medstat, 4301 Connecticut Avenue, N.W., Suite 330, Washington, DC 20008; Tel: 202.719.7869; Fax: 202.719.7801; E-mail: Denise.Kruzikas@thomson.com Research Objective: To identify U.S. hospitalizations that may be avoided through high quality primary and preventive care and to investigate trends over time, by region and among priority populations, including children, older Americans, women, low-income individuals, and rural residents. Study Design: This project examines potentially avoidable hospitalizations across the U.S. using the AHRQ Prevention Quality Indicators (PQIs), which focus on 10 chronic and five acute conditions, as well as one obstetric outcome. The primary data source is the Healthcare Cost and Utilization Project (HCUP) Nationwide Inpatient Sample (NIS) hospital discharge database. Population-based hospitalization rates are calculated using data from the NIS, U.S. Census, Current Population Survey, and Claritas Census projections. Rates are adjusted for age and sex using direct standardization. Standard error calculations and bivariate significance tests account for sampling strategies of each database. Population Studied: U.S. population for 1994, 1997, and 2000. Principal Findings: Between 1994 and 2000, admission rates declined 71% for angina without procedure; 30% for uncontrolled, uncomplicated diabetes; and 30% for adult asthma. Rates rose 20% for chronic obstructive pulmonary disease and 13% for hypertension. Hospitalization rates vary by geographic region; the West has the lowest rates for 15 PQIs, while the Midwest has the highest rates for 11 PQIs. Admission rates are highest among very young children (0-4 years) and individuals 85 years and older. Compared with men, women are 2.5 times more likely to be admitted for adult asthma and 50% more likely to be admitted for hypertension, but are 50% less likely to experience diabetes-related lower extremity amputations. Girls are 35% less likely than boys to be hospitalized for pediatric asthma. Low-income residents have the highest admission rates for all PQIs. Rates vary 6278% between the lowest and highest income groups; differences are most pronounced among chronic conditions. Rural residents have higher hospitalization rates for nine PQIs. Conclusions: The U.S. health care system has reduced potentially unnecessary hospitalizations in a number of areas. During the study period, admission rates decreased significantly for specific health conditions including angina without procedure; uncontrolled, uncomplicated diabetes; and adult asthma. Western states consistently have the lowest hospitalization rates in the nation. These results suggest the potential for improvement in other areas. Higher rates among select conditions and regions need to be explored to determine which hospitalizations may be avoidable. Variations among sub-populations must be investigated further, particularly among low-income and rural residents, to understand why priority populations experience higher rates of hospitalization. Implications for Policy, Delivery or Practice: These results provide insight into the quality of primary and preventive care at national and regional levels. Policy makers may use these results to evaluate priority areas (e.g., diabetes and hypertension) and identify targets for health care system improvement or more extensive study. State and local leaders can incorporate the national and regional benchmarks into their quality improvement initiatives. These efforts may ultimately improve the quality of outpatient care and further prevent unnecessary hospitalizations. Because hospitalizations constitute the largest component of health care costs, reducing admissions through better quality primary and preventive care can result in substantial cost savings for the U.S. heath care system. Primary Funding Source: AHRQ ● Examining Public Health Financing in New York State: A Methodology for Evaluating Local and National Public Health Data Perri Leviss, MPM, Lloyd Novick, M.D., M.P.H. Presented by: Perri Leviss, MPM, Consultant, 40 Branford Road, Hastings-on-Hudson, NY 10706; Tel: 914.478.3468; Fax: 914.478.4876; E-mail: pleviss@earthlink.net Research Objective: This study uses data collected from local health departments in New York State for the period 2000- 2002 with the purpose of developing improved methods of collecting and analyzing this type of information. This study follows an initial investigation of trends in local public health funding in New York State. Information from this study was successfully used in support of policy recommendations made to the New York State Legislature by the New York State Association of County Health Officials (NYSACHO). However, differences in data collection and the array of services offered by individual local health departments, has led to the further examination of methodology and results reported here. Study Design: In an effort to understand fiscal trends for local health departments in New York State, the New York State Association of County Health Officials (NYSACHO) developed and administered a survey in December 2002 that collected data on spending and funding sources from CY 2000 – CY 2002. Of the 58 surveys distributed, NYSACHO had a response rate of over 75%. Findings from the survey included significant changes in public health programs and revenue streams across New York State during the 3 year period. Of the 51 responding counties, 6 counties’ data could not be used in any of the data analyses because it was too incomplete based on the screening criteria that was developed. Therefore the data below includes 45 of the 58 counties in New York State. In some cases, the actual N<45 because some counties may not have expended funds for specific public health programs, and therefore a portion of the data analyses was not performed. The responding counties included a relatively even distribution of small and large counties as well as urban/suburban/rural counties. All the State’s largest counties participated in the survey with the exception of New York City who could not participate due to data conversion issues. However, initial analysis of this data encountered problems of comparing “apples and oranges” because of a variation in the services offered by local health departments particularly in the areas of primary care, home health care and early intervention. A future follow-up study will examine basic public health funding and compare select groups of counties according to the pattern of services rendered. Principal Findings: Many of the findings noted below were difficult to interpret because the data collection and array of services between counties was not truly comparable. Reanalysis of the data and recommendations for a revised data collection instrument will be made as part of the follow-up study. The highest per capita expenditures were among smaller county health departments. The range in per capita expenditures among LHDs was relatively large, but smaller if you look at LHDs which are similar in size and scope. Some county health departments had similar total expense budgets, but varying per capita expenditures. The increase in Early Intervention (EI) expenditures may be limiting the availability of resources for other core public health services. Some LHDs spend a large percentage of their total expenditures on Early Intervention programs. The counties with the smallest total EI expenditures also had the smallest EI percentages of total budgets in 2001. Some counties had similar total EI expenditures, but very different percentages of the total budget. Many LHDs maintain large home health/home care programs. In some cases, LHDs in NYS may have supported other core public health functions through home care revenues, limiting the need for local tax levy. Some of the largest home care programs reside in both large and small LHDs. The small counties rely most heavily on State Aid as a percentage of total revenues and these LHDs are most vulnerable to budget reductions. Population is one factor in determining the reliance on State Aid as a revenue source, but it appears that there are other factors influencing the data as well. The analysis may underestimate the true impact of a reduction in State Aid upon core public health services because the denominator includes revenues from EI and Home Care Services. Therefore, some small LHDs are even more reliant on State Aid for the provision of core public health services. Those counties with the largest per capita State Aid funding were not the counties most reliant on State Aid as revenue source (as a percentage of LHD revenue). Conclusions: There are distinct differences in the mix and levels of public health services that are provided by LHDs across New York State. In the NYSACHO survey, this was demonstrated by the lack of consistency in what counties call their public health services and the fact that almost no two LHDs provided the same array of services. This variability contributes to the differences in impact of proposed budget reductions on LHDs. In New York State, there is a loose definition of the minimum set of public health services that are required in order to be considered a LHD. In a time of constrained budgets, states must clearly define and enforce the range of required services and provide guidelines about the distribution of funds among these public health programs, leaving some room for individual modifications. Finally, returns from the NYSACHO survey demonstrate that reductions in local support/local tax levy are increasing concern and compounds issues of State Aid losses. Further examination of this issue as well as some of the others listed above is required. Implications for Policy, Delivery or Practice: The survey instrument developed and then subsequently revised by NYSACHO, presents a national model for States and local public health departments to evaluate their own resources/needs and to promote information exchange within and between localities. With limited resources, local public health officials must make difficult choices about their programs and activities. By encouraging localities to collect uniform financial data sets, public health will be better suited to support its case for stable and sufficient funding. LHD’s across the country must come together to address the issues of state financing for core public health functions and to ensure that the basic infrastructure of public health is not destroyed at a time when the demands on public health are greater than they ever have been before. Budget deficits at both state and local levels are sharply reducing public health support at a time of unprecedented challenge. The Sudden Acute Respiratory Syndrome, bioterrorism preparedness, smallpox vaccination, and other emerging diseases including West Nile Virus calls for increased public health capacity, not a lessoning of this vital function. Diseases do not know of boundaries and the assurance of one’s health requires many states and localities to work together. National organizations that represent local public health have an obligation to assist LHDs in this long and uphill battle. The small amount of funds spent on public health activities across the country now will provide for a lifetime of good health. ● The Public Health Workforce: A Six State Case Study Jean Moore, B.S.N., M.S.N., Peter House, MHA, Robert Wood, M.P.H., Elizabeth Mertz, M.P.A. Presented by: Jean Moore, B.S.N., M.S.N., Deputy Director, SUNY School of Public Health, Center for Health Workforce Studies, One University Place, Rensselaer, NY 12144; Tel: 518.402.0250; Fax: 518.402.0252; E-mail: jmm04@health.state.ny.us Research Objective: The research objective was to conduct a study of the public health workforce. The study focused on governmental public health agencies at the state and local levels and particularly on public health physicians, dentists and nurses as well as workers with formal public health training. The study also assessed the role that schools of public health play in assisting these public health agencies to recruit, retain or provide continuing education to their workforce. Major goals of this study included: 1)assessing the adequacy of the supply of these workers in relation to the demand for them; 2)quantifying differences in staffing in light of organizational responsibilities and relationships as well as the size of the population served by the agency; and 3)understanding the role that schools of public health play in addressing public health workforce needs of these agencies. Study Design: The study had three main components: 1. A six state case study that included surveys and interviews with staff of state and local public health agencies in those states on their most pressing health workforce issues. 2. Identification and analysis of available data on the workforce of public health agencies in the six states studied. 3. Convening a Project Advisory Committee to provide guidance on the overall study methodology, the issues to be discussed and the questions to be asked of state and local public health agencies, and to assist with the interpretation of findings. The six states selected for study were New Mexico; Montana; Georgia; California; Texas; and New York. The states were selected to assure representation of the four organizational models described in Local Public Health Practice: Trends and Models, (APHA, 2000) which represent different relationships between the state and local public health agencies. The four models are 1)Centralized - a state operated public health system (New Mexico); 2)Decentralized – a public health system operated by local government (Montana); 3)Shared – a public health system jointly operated by state and local government (Georgia); and 4)Mixed - a public health system with differing levels of state and local involvement (California, Texas, New York). Population Studied: Using the case study methodology, five local public health agencies and/or district offices in each of the case study states were selected to participate in the study, including at least one urban, one rural, one suburban, and where appropriate, one local agency on an international border. A survey of district/local public health agencies was conducted, with topics including: general workforce issues; staffing and function; recruitment and retention issues for public health nurses, public health physicians; the oral health workforce; supply of and demand for workers with formal public health training; training and continuing education needs; and collaborations with educational institutions, including Schools of Public Health. Interviews were conducted with key public health stakeholders in the six case study states, including state, district and local public health leaders and managers. Interviews focused on the topics included in the survey. Principal Findings: Public Health Nurses (PHNs) o Public health agencies in all six case study states reported difficulty recruiting PHNs, especially in rural areas, but less difficulty retaining them. o Reasons for the recruitment difficulties included: budget constraints, a general shortage of RNs, non-competitive salaries and lengthy processing time for new hires. o A wide range of PHN training needs were identified; the greatest unmet need was for public health oriented training o Lack of access to baccalaureate nursing, masters of public health, and other advanced training programs is a significant barrier to upgrading existing staff, particularly in rural areas. Public Health Physicians (PHPs) o PHPs play different roles in public health agencies, depending upon the size of the agency. o Formal public health education for PHPs is often a preference rather than a requirement. o Rural public health agencies in all six case study states reported difficulty recruiting PHPs. o Barriers to recruiting PHPs include non-competitive salaries and rural locations. Oral Health Staff o There are very few dentists and dental assistants, and even fewer hygienists in the public health workforce. o Many dental public health programs are run by PHNs or other dental staff (dental hygienists or dental assistants) and utilize volunteer or contract dentists only for services requiring their expertise. o Recruitment of dentists into public health is difficult, but those who choose it tend to stay. o The lack of oral health services in most LDHs is more often a function of lack of funding for services than a lack of staff, although staffing can be problematic as well. Workers with Master’s of Public Health (MPHs)/Schools of Public Health (SPHs) o MPHs most commonly worked in state health departments or as top managers in large public health agencies; they were needed, but rare in smaller public health agencies. o MPHs who worked in LHDs often had clinical skills and duties. o LHD staff who got MPHs often left the LHD to work in larger organizations that offered better opportunities. o Public health agencies in the six case study states reported greater need for training in core public health concepts than for MPHs. o SPHs, in general, have done a poor job collaborating with public health agencies; however, there are models of successful collaborations. o More opportunities for public health training and education should be accessible to senior staff of public health agencies, particularly those in leadership positions. Additional o Budget constraints is the single biggest barrier to adequate staffing of governmental public health agencies. o Public health agencies in the case study states reported workforce shortages across a variety occupations, including: health educators, nutritionists, social workers, clerical staff, epidemiologists, dental hygienists, dental assistants, laboratory personnel and home health aides. o Rural public health agencies in most states reported drawing their staff from the local labor market and had more difficulty recruiting more educated, skilled public health workers. o Public health agencies in border counties identified a need for public health workers who are bi-lingual; are culturally competent; and have up-to-date knowledge of tropical diseases, such as dengue, murine typhus. o Some public health agencies are concerned about losing senior staff to retirement in the next five years and reported a need for succession planning. Conclusions: This study documents the difficulty experienced by the public health system in recruiting the workers it needs. In addition, many of these workers lack formal public health training and in many instances, this training is either not affordable or accessible to them. The public health system is undergoing many changes, faced with declining resources, emerging diseases, new roles and new technology. There is a need to develop strategies that assure an adequate supply of well-prepared public health professionals in order to maintain an effective public health system in America. Implications for Policy, Delivery or Practice: There is a need continue to study trends in the public health workforce, to better understand the issues that impact on the recruitment and retention of an adequately trained workforce. It may also be helpful to conduct a functional enumeration of public health workers, to develop benchmarks based on job functions, which include direct patient services, populationbased services and program management. In addition, there is a need to develop strategies to address some of the finding of this study, including the use of scholarships and career ladders, among others. Schools of public health and other educational programs must find avenues to create accessible and affordable educational opportunities to the existing public health workforce. Primary Funding Source: HRSA ● Bridging the Chasm: How Hospitals are Taking on Public Health Responsibilities Peter Weil, Ph.D., Reed Morton, Ph.D., Richard Bogue, Ph.D., Paul Halverson, Dr.P.H. Presented by: Reed Morton, Ph.D., Associate Director, Research & Development, American College of Healthcare Executives, 1 N. Franklin, Suite 1700, Chicago, IL 60606; Tel: 312.424.2800; Fax: 312.424.0023; E-mail: RMorton@ache.org Research Objective: In the U.S., community hospitals have traditionally had very little to do with improving the health status of their communities. Instead, they provided the structure for the provision of acute care, delivered by privately employed physicians to patients many of whom had private insurance and lived near the hospital. But beginning in the mid 80s, hospitals began to reach out to their community for either marketing purposes or to satisfy their requirement to provide "community benefit" that allowed them to maintain their favored tax status. From the public side, the Institute of Medicine noted that a public health system neither can nor should be achieved by public helath professionals alone. It urged public health agencies to cultivate relationships with physicians and other private sector groups. We conducted this study to assess what kinds of activities hospitals were undertaking to build relationships with public health agencies in their communities. A useful structure to examine the relationship is provided by the "essential services of public health" issued in 1994. These ten services were developed by a number of public health groups to show how public health agencies carry out their role to promote physicial and mental health and prevent disease, injury and disability. Thus, the purpose of the study was to examine what types of essential public health services leading hospitals are providng either alone or in concert with public health agencies. Study Design: Seven "leading hospitals" were identified by reviewing the literature, contacting professional associations, obtaining data from a mailed survey and validating these through follow-up fax surveys and 30 minute telephone interviews with hospital CEOs. A national advisory committee selected those hospitals that appeared to have initiated novel management practices that promoted community health. Twoday site visits were then scheduled by two researchers. Each visit consisted of semi-structured interviews with between 10 and 14 individuals, including the CEO, the current board chair, the board secretary, the senior vice president or chief operating officer, the medical staff president, the head of fundraising or the foundation and the vice president with responsiblity for community health. Interviews were also conducted with the executives of two ro three community organizaitons involved in community health partnerships with the hospital or health system and others based on the initiatives and corporate structure of the leading practice sites. Through 63 detailed on-site interviews, we identified 24 distinct practices some of which contribute to the ten essential public health services. Population Studied: This was a qualitative study designed to elicit best practices in providing public health services by hospitals. Eligible were any general, medical surgical, short term hospitals in the U.S. Using the methods described above, seven leading hospitals were studied on site. Principal Findings: None of the hospitals appear to participate in the essential service related to enforcement and regulation. All leading hospitals participate in essential public health service 1 (Monitor health status to identify and solve community health problems), 3 (Inform, educate and empower people about health issues) and 4 (Mobilize community partnerships and action to identify and solve health problems). We illustrate how the leading hospitals contribute to achieving nine of the ten essential public health services. Conclusions: Our findings show that only those essential public health functions that are specifically regulatory are excluded from the agenda of leading hospitals. Hospitals under both public and not-for-profit auspices are collaborating with public health agencies and other community groups. They fulfill in whole or in part, essential public health services. Implications for Policy, Delivery or Practice: The paper contributes to our understanidng of the blurring of lines between the public and private health sectors and shows that managers of certain hospitals promote a broader view of the hospital's role in the community. The problem today is to find ways to ensure that not just leading hospital executives, but all hospital executives take responsibility to provide or ensure that their community has each essential public health service. Suggested are:(1) providing education to hospital executives and aspiring executives about methods to achieve public health services; (2) evaluating executives' performance based in part, on their public health achievements; (3) giving award to hospital leaders accomplish the public health services alone or who collaborate with public health agents in their community; and (4) including the ten essential public health services in protocols that evaluate communities as desirable places to in which to live. Primary Funding Source: WKK ● Evolving Relationships between Turning Point Partnerships and Public Health Institutes Bud Nicola, M.D., M.H.S.A, Joseph Kimbrell, MA, LCSW, Chris Kinabrew, M.S.W., M.P.H., Stephen M. Padgett, R.N., M.S., Betty Bekemeier, M.S.N., M.P.H. Presented by: Bud Nicola, M.D., M.H.S.A, Senior Consultant, Turning Point National Program Office, 6 Nickerson Street, Suite 300, Seattle, WA 98109; Tel: 206.616.8410; Fax: 206.616.8466; E-mail: bnicola@u.washington.edu Research Objective: (1) Describe the relationships between state-level Turning Point partnerships and Public Health Institutes in states which have both, and (2) develop models that represent the variety of those relationships. Study Design: Turning Point is a program funded by The Robert Wood Johnson Foundation, involving 21 state-wide initiatives and 2 ‘linked’ states which formed multi-sector collaborative partnerships for public health systems change. In 18 of those states, there are also free-standing Public Health Institutes, which either preceded or resulted from Turning Point. Key participants in those state partnerships and institutes, and staff at the National Network of Public Health Institutes and the National Program Office of Turning Point, were interviewed to elicit perspectives on the relationship between the two structures. These interviews were analyzed to identify and illustrate the historical and continuing relationships among state health agencies, Public Health Institutes, and Turning Point partnerships. Population Studied: 18 states with both a Turning Point partnership and a Public Health Institute, either emerging or established. Principal Findings: Both Turning Point and Public Health Institutes represent efforts to reform and modernize public health systems, and to institutionalize those changes. The relationships of Turning Point state partnerships with their respective Public Health Institutes have taken many shapes. In some cases the state health agency developed the Turning Point partnership, which in turn led to the establishment of a Public Health Institute. In other cases, the Public Health Institute preceded the Turning Point initiative, and may or may not have been involved with Turning Point activities. In still other cases, state health agencies were less involved in the formation of either the Turning Point partnership or the Public Health Institute. Participants reported more administrative flexibility with Public Health Institutes, and greater opportunities for policy development and advocacy, than is usually possible within state government. Along with this flexibility, however, free-standing institutes also have greater uncertainty about funding streams, and in some cases, are perceived as more distant from policy implementation. Participants generally recommended complementary, rather than competitive, roles for Public Health Institutes in relation to state health agencies and other organizations. Conclusions: Turning Point state partnerships and Public Health Institutes share a number of goals regarding public health systems change, and often involve alliances with similar partners. Public Health Institutes represent a more flexible administrative structure, with a greater ability to pursue independent funding and advocacy work. Factors that influence the choices and sequencing of these options are largely related to local contexts, and political and economic resources. Many of the Turning Point participants perceived Public Health Institutes to be a useful ‘successor’ organizational form for the process of public health systems change. While the establishment of Public Health Institutes was generally considered beneficial, there are many viable paths toward this goal. Implications for Policy, Delivery or Practice: Successful and sustainable public health systems change requires continuing relationships with multiple partners, and careful assessment of needs and resources. Decisions about appropriate administrative structures and governance models should reflect local histories, build on existing relationships when possible, and extend these when necessary. States considering the development of a public health institute may look to the experiences of Turning Point partnerships for useful lessons on the opportunities and challenges posed by public health institutes. Primary Funding Source: RWJF ● Cost-Effectiveness Comparison between a Free Nicotine Replacement Therapy Program and a Smoke-Free Workplace Policy Campaign for the State of Minnesota Michael Ong, M.D., Ph.D., Stanton Glantz, Ph.D. Presented by: Michael Ong, M.D., Ph.D., VA Ambulatory Care Fellow, Medicine, Stanford University, 117 Encina Commons, CHP/PCOR, Stanford University, Stanford, CA 94305-6019; Tel: 650.723.1503; Fax: 650.723.1919; E-mail: mikeong@stanford.edu Research Objective: Public health tobacco control programs are increasingly being asked to consider individual-based smoking cessation programs beyond quitlines, particularly free nicotine replacement therapy (NRT) programs. Budget limitations force public health tobacco control programs to choose between individual-based programs and more traditional population-based programs, such as smoke-free workplace campaigns. This analysis compares the benefits and costs of a free NRT program with a smoke-free workplace campaign. Study Design: We simulated the benefits and costs of both programs generated after one year. Benefits are calculated in number of quitters generated and in quality-adjusted life years (QALYs). We estimated the number of smokers interested in quitting and in using NRT from a 1999 survey conducted by the Minnesota Partnership for Action Against Tobacco. Key assumptions of our free NRT program model include the chance of cessation success with each NRT attempt is 7.1%, that individuals will have a maximum of 2 cessation attempts in one year, that NRT equally assists both heavy and light smokers (<15 cigarettes/day), and there is a 35% relapse rate. Costs of free NRT programs are based on costs of patch and gum NRT therapy used in quit attempts, and we assume minimal distribution costs. Key assumptions of our statewide smoke-free workplace policy include an absolute smoking prevalence reduction of 3.7%, a 35% relapse rate, and that these policies are 90% effective. Costs of our smoke-free workplace policy include enactment campaign costs and media enforcement costs. Population Studied: For our free NRT program model, we use a hypothetical cohort of all smokers for the state of Minnesota based on 2001 Census Bureau population estimates and 2001 smoking prevalence data from the Centers for Disease Control (CDC). For our smoke-free workplace policy model, we use a hypothetical cohort of indoor workers from Minnesota who smoke based on the 2001 Occupational Employment Survey and 2001 smoking prevalence from the CDC. Principal Findings: After one year, a smoke-free workplace policy induces 10,400 quitters at a cost of $8.3 million. This ratio of $798 per quitter translates into a cost-effectiveness ratio of $505 per QALY. After one year, a free NRT program induces 30,900 quitters at a cost of $121 million. This ratio of $3,900 per quitter translates into a cost-effectiveness ratio of $2,470 per QALY. Conclusions: A free NRT program produces more quitters than a smoke-free workplace policy. However, it does so at nearly fifteen times the overall cost and with a nearly five times higher cost-effectiveness ratio. As it is unclear whether light smokers actually benefit from NRT, a free NRT program may generate fewer quitters than our estimation. Implications for Policy, Delivery or Practice: While free NRT programs are cost-effective, smoke-free workplace policies are more cost-effective and cost less overall. Given budget limitations, smoke-free workplace policies should be a funding priority for public health programs. ● Understanding the Financing and Functions of Metropolitan Health Departments: A Key to Improved Public Health Response Alonzo Plough, Ph.D., M.P.H. Presented by: Alonzo Plough, Ph.D., M.P.H., Professor, Health Services, School of Public Health and Community Medicine, University of Washington, 999 3rd Avenue, Suite 1200, Seattle, WA 98104; Tel: 206.296.1480; E-mail: Alonzo.Plough@METROKC.GOV Research Objective: To describe and better understand the specific financing issues facing large Metropolitan Health Departments. Such departments are not well described in previous studies but play a major role in the provision of local public health services to nearly 50% of the U.S. population. Study Design: The study design is a descriptive, case study drawing on data collected by the National Association of City and County Health Officials and in-depth financial information from a representative Metropolitan Health Department Population Studied: This study focuses on the organizational and financial characteristics of an estimated 50 MHD’s out of the 3000 local health departments in the country. Principal Findings: An analysis of the large metropolitan health departments suggest that current assumptions about local health department capacities and financing challenges mistakenly equate the characteristics of the average LHD with the financial and organization characteristics of the health departments which serve most of the US population; the MHD. Conclusions: Large metropolitan health departments play a very significant role in public health service delivery and have financial, and organization capacities and challenges which are not well understood or reflected in federal public health financing strategies. Implications for Policy, Delivery or Practice: Health disparity reduction, chronic disease prevention and public health preparedness efforts must better understand and more appropriately fund Metropolitan Health Departments to have significant impacts on urban populations. The traditional statecentric approach to funding may not appropriately fund to a scale to achieve measurable outcomes or clear replicable models of prevention. ● Evaluation of Strategic Workforce Development in a Local Public Health Agency Margaret Potter, J.D., M.S., Molly Eggleston, M.P.H., CHES, Gerald Barron, M.P.H., G. Daniel Bednarz, Ph.D., Christine E. Ley, Ph.D., M.P.H., M.S.W., Carl I. Fertman, Ph.D., M.B.A., CHES Presented by: Margaret Potter, J.D., M.S., Associate Dean and Director, Center for Public Health Practice, University of Pittsburgh, 3109 Forbes Avenue, Pittsburgh, PA 15260; Tel: 412.383.2400; Fax: 412.383.2228; E-mail: mapotter@pitt.edu Research Objective: Measure the impact of a strategicallydesigned training program on participating workers and on their organizational employer. Study Design: Through a strategic assessment process, a local public-health agency identified for performance improvement a prioritized list of essential services. Trainers designed a 30hour program to improve competencies of the agency’s employees in three domains (analytic, cultural, and communications), which were related to those essential services with the highest priority for strategic improvement. Outcome evaluation of this training program included both organizational and individual-trainee indicators. The primary organizational indicator was application of appropriate evaluation methods in the agency’s annual program plans. The individual-trainee indicators were: 1) change in attitudes, beliefs, awareness, and knowledge over the course of training; 2) usefulness of course topics and effectiveness of training methods; and 3) uptake of new skills into work and resulting program improvements nine months after training. Population Studied: The trainees were 77 employees (about 20% of all staff) representing all thirteen program divisions of the 400-employee agency. One program division (food safety) sent every professional and field-staff member to the training. Other program chiefs selected employees on the basis of need for training and other unspecified factors. Principal Findings: Impacts of the training appear in each of the three competency-domains and at both the organizational level and the individual-trainee level. For the analytic competencies, a comparison of annual program plans pretraining and post-training by the agency’s senior management showed improved use of appropriate outcome indicators; and, nine-months after training, a trainee sample confirmed the uptake of analytic skills. Results of the trainees’ evaluations revealed inadequacies in the cultural-competency module; consequently, the agency later devoted an additional half-day of training to that subject for all 400 employees. For the communications competencies, trainees initially questioned the training approach but nevertheless demonstrated acquisition of the skills that were taught. At nine-month follow-up, they not only acknowledged the usefulness and impact of the communications training but also called for agency-wide policies and procedures to incorporate the underlying communications principles. Conclusions: Strategically-designed competency-based training can improve individual work-products and skills in the analytic, cultural, and communications domains. Such training can also improve an agency’s performance of targeted essential public-health services. However, the impact of such training depends not only on trainees’ participation and uptake of new skills but also on the organization’s sustained commitment to learning and its implementation of competency-based policies and procedures. Implications for Policy, Delivery or Practice: Federal public-health agencies, along with academic trainers and state and local-agency partners, are currently investing unprecedented levels of funding, time, and expertise into development and training programs for the existing public- health workforce. This evaluation of one such program provides evidence of positive outcomes when the training design is strategically focused on essential-service related competencies. Primary Funding Source: HRSA ● The Effect of Liability Reform on the Supply of Practicing Physicians Dov Rothman, Ph.D., Jason Snyder, MA, Tim Simcoe, M.A. Presented by: Dov Rothman, Ph.D., Assistant Professor, Department of Health Policy and Management, Columbia University, 600 West 168th Street, 6th Floor, New York, NY 10032; Tel: 212.342.4521; E-mail: dbr2104@columbia.edu Research Objective: A number of states passed liability reform legislation in the 1970’s, 1980’s and 1990’s. These reforms capped the damages that individuals can collect from physicians in malpractice lawsuits. This study examines whether and how these reforms affected: (1) the supply of practicing physicians, and (2) health care utilization rates. In particular, we focus on the supply of OBGYN’s, and utilization rates of pregnant women (number of prenatal visits). Study Design: We construct an annual county-level dataset from three sources: The Bureau of Health Professions Area Resource File, Insurance industry publications, and the annual United States Natality Detail File. The main variables in our dataset include (at the county-level): the number of practicing physicians, the number of practicing OBGYN’s, average per capita income, average number of prenatal visits per pregnancy, and population. We estimate the effect of tort reform on our outcomes of interest using two estimation strategies. First, we use a difference-in-differences estimator. This estimator compares changes in our outcomes of interest in states that adopted liability reform to changes in our outcomes of interest in states that did/had not adopted liability reform. In this approach, states that did/had not adopted liability reform serve as control groups for states that adopted liability reform. Second, we use a county-level matching estimator. We implement this in two steps. In the first step, we use observable county-level demographic, economic and political variables to match counties in states that adopted liability reform to “very similar” looking counties in states that did/had not adopted liability reform. In the second step, we compare changes in our outcomes of interest across these matches. In this approach, the counties in the states that did/had not adopted liability reform serve as control groups for their matches in the states that had adopted liability reform. Principal Findings: We find that 1990’s liability reforms are associated with increases in the supply of total physicians per capita, and the supply of practicing OBGYN’s per capita. We also find that 1990’s liability reforms are associated with decreases in the average number of prenatal visits per pregnancy. We are in the process of implementing a number of robustness checks. Conclusions: The results described above are consistent with the arguments that medical liability creates negative incentives for physicians to practice in areas where they are more vulnerable to malpractice lawsuits, and that medical liability creates positive incentives for physicians to practice defensively. In future research, we will examine whether and how liability reforms affected utilization patterns other than prenatal visits, and whether and how liability reforms affected health care outcomes for specific populations. Implications for Policy, Delivery or Practice: Our results suggest that limiting physician liability should increase the supply of practicing physicians and might lower costs associated with physicians practicing defensively. ● What Does It Take to Be Prepared for Terrorism and Other Public Health Emergencies? Lucy Savitz, Ph.D., M.B.A., Michael Allswede, DO, Samuel Watson Presented by: Lucy Savitz, Ph.D., M.B.A., Senior Health Services Researcher, Health Care Quality and Outcomes, RTI, 3040 Cornwallis Road, RTP, NC 27709; Tel: 919.316.3301; Fax: 919.541.7384; E-mail: savitz@rti.org Research Objective: The role of government is to protect and ensure the health of the population; while the role of hospitals is to treat the infirmed. Thus, hospitals play a central role in preparedness. Our work with hospital executives suggests that preparedness is a daunting task, and it is considered relative to many competing priorities. Targeted tools that inform decision making and guide rational resource allocation are needed. In order to address expressed needs, our work: (1) creates a common language for communicating hazard information; (2) supports evidence-based, planning and investment; and (3) promotes surge and augmented capacity partnering for regional preparedness and response. Study Design: This exploratory study provides retrospective cost analyses over a 3-year period together with real-time expert ratings for four pathogen threats—aerosol anthrax, aerosol smallpox, staph enterotoxin B, and cholera food contamination. Based on foundational work to create a pathogen score—composite measure based on key attributes of communicability, effectiveness of treatment, and availability of medical treatment—we engaged two expert panels to independently assign scores across a continuum of victim load and time of release. These ratings are displayed in a tool referred to as the Pittsburgh Matrix. Intervention costs associated with command and control, capacities and resources, and disease-specific assets were captured using a standardized tool. Three years worth of data were pooled and analyzed in developing a series of Bio Terrorism Unit (BTU) cost metrics. Population Studied: Two integrated delivery systems (IDSs) participated in this study—UPMC Health System and Intermountain Health Care—drawing expert panels from these two sites. Evidence for threat-specific clinical manifestations of exposure were abstracted from peer-review literature and available military reports. Cost information on preparedness investments was gathered from financial analysts, using cost accounting system data at these IDSs (n=41 hospitals over 3 states). Principal Findings: Pathogen scores assigned by independent, expert panels were highly correlated for all four threat scenarios studied. Investment in implementing targeted, preparedness interventions in these health systems were relatively equal across acquisition/development and operational costs with $3.4 million invested by a single system and $1 in annual maintenance. However, we found that the majority of investment was made in command and control infrastructure (67%) versus key capacities and resources (35%) or disease-specific assets (1%). Conclusions: Health care is legislated as a right, funded as a commodity, and hospitals are expected to offer their services as public goods in a time of need. We know that hospitals operate in a fiscally constrained environment and face competing resource allocation decisions. We also know that they are integrally involved with public health in response to such threats. Findings from this study beg a discussion around the responsibility and accountability for funding hospital preparedness. Implications for Policy, Delivery or Practice: Results support hospitals’ evidence-based, capacity assessment, focusing on salient resources. The need for coordinated planning among public safety and hospitals is supported by a common language of threat-specific, pathogen scores. Results can inform policy makers in creating hospital preparedness incentives and understanding required hospital investments needed to support preparedness. Primary Funding Source: AHRQ ● Practicing Public Health: The Relationship between Public Health System Performance and Programs Offered F. Douglas Scutchfield, M.D., Evelyn Knight, Ph.D., Michelyn Bhandari, M.P.H., Ann Kelly, M.H.A., I. Puiu Vasilescu, Ph.D., Mary Kay Rayens, Ph.D. Presented by: F. Douglas Scutchfield, M.D., Principal Investigator, School of Public Health, University of Kentucky, 121 Washington Avenue, Room 105B, Lexington, KY 405360003; Tel: 859.257.6504; Fax: 859.257.6644; E-mail: scutch@uky.edu Research Objective: Relationships between local public health system performance on the 10 essential public health services (EPHS) and variation in agency outputs, defined as programs offered by the local public health agency, were studied to strengthen the understanding of how performance effects the practice environment. Study Design: This cross-sectional study used local public health system performance data from the National Public Health Performance Standards Program (NPHPSP) assessment (test version 5b) collected in 2000. The health system performance scores include a score for each of 10 EPHS plus a total score. Outputs were measured using data from the National Association of County and City Health Officials’ (NACCHO) 1997 National Profile of Local Health Departments, in which respondents checked programs offered by their agency from a standard list. To reduce the data for 43 selected programs, factor analysis was used to create three groups within the 25 programs for which there was variation across the sample. Bivariate relationships were analyzed between each of the three factor scores and the 10 EPHS and total performance scores. Population Studied: A sample of 152 public health departments/systems from three states was studied. These public health jurisdictions had completed the 1997 NACCHO Profile as well as the 5b test version of the NPHPSP performance assessment, and represented over 70% of the jurisdictions in these states. Principal Findings: Of the 33 bivariate relationships evaluated between three program group scores and 11 performance scores, 10 were significantly positive, five were significantly negative, and 18 were not significant. There were no significant relationships between the first group of 10 “basic” programs and the 11 health system performance scores. There were five significant negative correlations for the second group of seven “expanded clinical” programs with performance scores for EPHS #2 through 6. However, for the third group of eight “outreach” programs, 10 of the performance scores had a significant positive relationship. Conclusions: Local health departments whose systems score higher on performance measures are likely to offer more outreach programs. Lower public health system performance was related to offering more programs with a clinical focus on chronic disease. With more specific information on the quantity and quality of programs offered by health departments, it may be possible to more accurately predict the impact of higher health system performance on public health departments and practices in their communities. Implications for Policy, Delivery or Practice: These results emphasize the population health orientation of the ten essential services, as reflected in community oriented programs. As local public health practice moves toward implementation of the essential services as the basis for health system performance improvement, a shift may occur in the nature of programs offered at the local level. This may have important implications where public health provides the medical care safety net for a community. Assuring the public’s health will then require a close examination of the role of clinical programs in the larger arena of public health practice and pursuing highly performing public health systems. Primary Funding Source: CDC, ATPM ● Mifepristone: Diffusion of Innovation Michelle Dawn Seelig, M.D., Lisa Rubenstein, M.D., MSHS, Lillian Gelberg, M.D., M.S.HS, Paula Tavrow, Ph.D., Martin Lee, Ph.D. Presented by: Michelle Dawn Seelig, M.D., Primary Care Research Fellow, Family Medicine, UCLA School of Medicine, 924 Westwood Boulevard, Suite 650, Los Angeles, CA 90095; Tel: 310.794.6049; Fax: 310.794.6097; E-mail: mseelig@mednet.ucla.edu Research Objective: To explore the self-reported factors that predict a physician being unlikely to offer medical abortion with Mifepristone. We will use this information to identify potential interventions to help interested physicians who are not currently offering abortion services to overcome the obstacles that prevent them from offering medical abortion with Mifepristone to their patients as an alternative to surgical abortion in the event of unwanted pregnancy. Study Design: We conducted secondary analysis of data collected from a national telephone survey of physicians who participated in a study conducted by the Kaiser Family Foundation, KFF, entitled, National Survey of Women’s Health Care Providers on Reproductive Health: Views and Practices on Medical Abortion. Population Studied: The KFF survey was a national random sample of 790 health care providers, consisting of 595 obstetrician-gynecologists, OBGYN, and 195 family practitioners, internists, and general practitioners - referred to as general practice physicians, GPP. Data were collected between May 15 and August 28, 2001. Because we were interested in determinants of provider behavior among potential adopters of Mifepristone, physicians were selected from the original sample if they indicated that they were not currently offering Mifepristone and were not personally opposed to medical abortion. Principal Findings: Less than one percent of the total sample currently offered Mifepristone. Of the potential adopters, 24 percent were likely to offer Mifepristone. Controlling for age, gender, the percentage of women of reproductive age in the physician's practice, location, and training, legal concerns related to FDA requirements and other matters, practice policies prohibiting medical abortion, providers’ lack of interest in offering abortion services, and being a primary care physician, GPP, were significantly associated, p<0.05, with being unlikely to offer Mifepristone. Conclusions: Since FDA approval in September 2000, less than one percent of physicians have begun to offer medical abortion using Mifepristone. Because medical abortions can be performed in GPP’s offices without surgical equipment, the diffusion of medical abortion services could significantly increase access to abortion in the United States. Most physicians were not personally opposed to abortion, but were discouraged by barriers such a legal requirements that are potentially remediable through educational and policy initiatives. Increased understanding of these barriers is critical for ensuring patient access to safe, medically supervised abortion. Implications for Policy, Delivery or Practice: Extending participation in medical abortion to new providers by addressing the factors associated with being unlikely to offer Mifepristone is essential for overcoming the problem of access to abortion for women living in the 87% of US counties without an abortion provider. Primary Funding Source: HRSA ● Social Networks Analysis Methods to Define and Quantify Dimensions of Public Health Systems Sergey Sotnikov, Ph.D., Deborah Gibbons, Ph.D. Presented by: Sergey Sotnikov, Ph.D., Economist, PHPPO, Centers for Disease Control and Prevention, 4770 Buford Highway., N.E., Mail Stop K-39, Atlanta, GA 30341-3724; Tel: 770.488.2528; Fax: 770.488.2474; E-mail: ann0@cdc.gov Research Objective: The recent report from Institute of Medicine (IOM), “The Future of the Public’s Health in the 21st Century,” emphasizes the need for a “systems” approach to public health. “Public health system” in that report is defined as a complicated web of different entities that include the governmental public health infrastructure, community organizations, health care delivery systems, employers and businesses, media, and academia. The multiplicity of interactions between these elements of the public health systems was recognized, but no framework for quantitative evaluation of these ties proposed. This study developed a method to measure and quantify dimensions of public health systems. Study Design: An extensive literature review enabled identification and description of quantitative indicators of the dimensions of the public health systems that are new to public health. Different approaches to measuring aspects of public health systems were classified, described, and documented. Survey and interview instruments were then developed and purified through interviews with public health experts. Population Studied: We used the National Library of Medicine (NLM) Gateway to search multiple on-line databases and identify relevant methodologies both within and beyond the realm of public health (public administration, operations research, management, etc.) that can be used to measure interorganizational networks in public health. Principal Findings: Two approaches to evaluation and measurement of public health partnerships have been identified. Qualitative description of interorganizational cooperation in public health reveals the importance and nature of some linkages, but it does not allow to assess structural aspects of public health systems or test the effects of interorganizational cooperation on public health system performance. The new methods that enable quantitative assessment of networks of linkages within complex public health systems were identified and their usefulness for public health has been evaluated. Conclusions: Proposed methods of measuring the public health systems will make it possible to assess the effects of cooperation within interorganizational networks on systems’ performance and facilitate appropriate interventions to improve public health service delivery coordination. An optimal strategy in practical application of these new methods is to utilize a mix of different quantitative performance indicators and measures. For example, density measures can be used to reveal the extent of decentralized cooperation that is occurring among member organizations. Centrality measures can be used to identify network leaders, potential for rapid information saturation, and the level of hierarchy within the network. Equivalence measures will show the extent to which certain participants occupy similar positions and serve similar functions, or roles, within the network structure. Implications for Policy, Delivery or Practice: Public heath policymakers and practitioners can use our methods to measure and evaluate health system structure. A new typology of public health systems based on quantifiable system characteristics can be created. Quantifying the dimensions of public health systems will also provide a metric for evaluation of organizational capacity that influences efficient functioning of the public health infrastructure. Finally, by identifying weaknesses in public health system networks, policymakers can target appropriate interventions. Primary Funding Source: CDC ● Turning the Tide: A Community Based Approach to Developing Successful Intervention Strategies for At-Risk Adolescents Patricia Sweeney, R.N., M.P.H., J.D., Ralph Ricci, M.S. Presented by: Patricia Sweeney, R.N., M.P.H., J.D., Visiting Assistant Professor, Center for Public Health Practice, University of Pittsburgh, 3109 Forbes Avenue, #210, Pittsburgh, PA 15260; Tel: 412.383.2231; Fax: 412.383.2228; E-mail: psweeney@pitt.edu Research Objective: To review community studies, reports and data sets reporting on the prevalence of risk factors which are precursors to adolescent substance abuse, pregnancy, school dropout, delinquency, and violence. The findings and data from these sources were compared to national and state data and were synthesized into a strategic plan outlining intervention tactics and modalities to assist at-risk adolescents and their families. Study Design: Representatives from government, juvenile justice, social services, health care, law enforcement, education, religion, ethnic and minority groups, civic organizations, public health, media and families, were intentionally recruited to join the community planning team. The 120 member team was divided into 6 work groups. Data was collected and analyzed to identify the most significant risk factors present in the community. Community assets to address risk factors were assessed, the juvenile justice system decision making processes were analyzed, and the legal and policy issues constraining cross system collaboration were studied. Plenary meetings were held to synthesize the finding of each team and then a strategic plan of intervention tactics and modalities was developed. Population Studied: The target population was the youth and families residing in Mahoning County, OH, an economically challenged community of 240,000 in Northeast Ohio. Principal Findings: The reviews of evidence analyzed by the teams showed that the four issues posed the greatest risk for youth and families in Mahoning County, Oh include: 1) extreme economic deprivation, 2) parental involvement in the problem behavior, 3) early and persistent antisocial behavior, and 4) youth who feel disenfranchised and as a result demonstrate alienation and rebelliousness. With minor exceptions, social and community services were adequately available to meet these youth and family needs. However, systemic issues were identified which universally affected commitment to reducing risk: community acceptance of crime, systemic community prejudice and isolationism. Conclusions: The need to create a set of strategies to address the issues reported in the Findings was the paramount conclusion of the planning team. Specifically, this study shows that adequately addressing adolescent risk factors requires cross-system, cross-community cooperation to identify and alter existing institutional and attitudinal barriers. Such systematic changes are required to build trust and change the community culture away from a culture of acceptance and tolerance of crime and prejudice to a culture that exemplifies strong character and quality of life for all members of the community. Implications for Policy, Delivery or Practice: Community planning efforts which focus solely upon the direct service needs of youth and families fail to address the societal conditions which underlie the risk factors. Developing strategic intervention to address these issues far exceed traditional community planning initiatives. Funders and community planners need to recognize that such systematic changes require long term assistance and support and a long term commitment from community leaders. In Mahoning County, Ohio, this commitment to address systemic and attitudinal problems has resulted in increased community capacity to collaboratively address community issues, and successfully secure funding for needed services and has resulted in the successful implementation of the identified strategic interventions. Primary Funding Source: U. S. Department of Justice and Ohio Department of Youth Services ● The Effect of Financial Incentives on Smoking Cessation Program Attendance and Completion Kevin Volpp, M.D., Ph.D., Andrea Gurmankin, Ph.D., David Asch, M.D., J. Murphy, M.D., H. Sox, M.D., C. Lerman, Ph.D. Presented by: Kevin Volpp, M.D., Ph.D., Assistant Professor of Medicine and Health-Care Systems, Philadelphia VAMC, University of Pennsylvania, CHERP, University and Woodland Avenues, Philadelphia, PA 19104; Tel: 215.573.0270; Fax: 215.823.6330; E-mail: volpp70@mail.med.upenn.edu Research Objective: Approximately 70 percent of smokers want to quit smoking, but only about 3 percent of smokers quit each year. Smoking cessation programs are an underutilized cost effective way to help people quit smoking. Our objective was to determine whether modest financial incentives increase the rate of smoking cessation program enrollment, completion, and quit rates. Study Design: Eligible patients were randomized into incentive and non-incentive groups. Both groups were invited to join a 5-class smoking cessation program at no out-ofpocket cost. In addition, the incentive group was offered $20 for each class attended and $100 if they quit smoking (biochemically confirmed). Subjects were blinded as to the existence of the other group. Intention to treat analysis was used for each of the outcome variables. Chi-Square tests were used to test for significant differences in enrollment and completion between the two groups. Population Studied: 179 patients at the Philadelphia Veterans Affairs Medical Center who reported smoking at least 10 cigarettes per day and who did not have any contraindications to nicotine patch utilization. Principal Findings: Subjects had smoked an average of 29.8 years, with a mean consumption of 23.4 cigarettes per day. There were no significant differences between the incentive and enrollment groups in the number of cigarettes smoked per day, the length of time patients had been smoking, degree of addiction, quitting intentions, risk perception of smokingrelated risks, sociodemographic characteristics, and distance from the VA hospital. The incentive group had higher rates of program enrollment (43.3% vs. 20.2%, p<.001) and program completion (25.8% vs. 12.2%, p=.02). Data on quit rates 30days post-program completion will be collected for the entire cohort by the end of January, 2004. Conclusions: Modest financial incentives are associated with significantly higher rates of smoking cessation program enrollment and completion. Implications for Policy, Delivery or Practice: The use of financial incentives could be an effective strategy for increasing tobacco cessation rates. Since tobacco quit rates are low and smoking-related illnesses are a leading cause of death in the United States, this should be further considered. Primary Funding Source: VA ● Hepatitis C, Whose Diagnosis Are We Missing? Barbara Yawn, M.D. M.Sc. Presented by: Barbara Yawn, M.D. M.Sc., Director of Research, Olmsted Medical Center, 210 Ninth Street, S.E., Rochester, MN 55904; Tel: 507.287.2758; Fax: 507.287.2758; E-mail: yawnx002@umn.edu Research Objective: Hepatitis C is reported to be present in 1 to 4 % of all Americans according to estimates based on information from the National Health and Nutrition Survey (NHANES). In previous studies of diagnosed cases of hepatitis C in Olmsted County, Minnesota, the prevalence was only 1/10 that reported from NHANES. The purpose of this study was to see if additional community members had identified risk factors for hepatitis C but had no HCV testing. Study Design: This study used an electronic summary of the routine yearly self adminsitered health histories used in all Olmsted County medical facilities to identify people who might be at risk for hepatitis C. This list was compared to the list of those who have been tested for hepatitis C and those with a diagnosis of hepatitis C. This comparison allowed identification of a cohort that might be at increased risk of hepatitis C but have not been screened for the infection. Population Studied: All adults in Olmsted County who attended any office, emergency department or were hospitalized at any medical care facility in Olmsted County during 2000 and 2001. Principal Findings: A total of 58,481 adult residents of Olmsted County had at least one health history completed or updated during 2000 or 2001. Of those individuals, 643 people (1.1%) were identified as reporting one or more risk factors for hepatitis C during 2000 or 2001. Of these people 300 (0.5%) reported having tattoos done by non-professionals, 346 (0.6%) reported use of injectable drugs at some time in their life, 185 (0.3%) reported use of a "substance like intranasal cocaine" and 402 (0.7%) reported having more than 6 sexual partners during some year of their life. Over 8.6% (5037 adults) did not answer yes or no to one or more of these questions. There were no gender differences in the number of people with risk factors who had not been tested for HCV. However, those with risk factors and no testing for HCV were primarily less than 40 years of age (82%). Most of the people reporting risk factors of tattoos (84%) and multiple sex partners (78%) who were tested for HCV also had a history of intravenous drug use (IVDU) at some time in the past. All (100%)of those that were diagnosed with HCV and reported risk factors of multiple sex partners or tattoos also had a history of IVDU. Conclusions: In Olmsted County almost 40% of people who reported any potential risk factors for hepatitis C had not been tested for HCV. However, the percent not tested varied considerably by the type of risk factor. For those with IVDU history only 16% had no records of being tested. The percentage of not screening was much higher in risk factors with less likelihood of HCV transmission such as tattoos or multiple sex partners. Since most of the people in these categories who were tested for HCV (and all that were HCV positive) also had a history of IVDU, it appears that reported IVDU is the prime driver of HCV testing. Implications for Policy, Delivery or Practice: A simple self administered history sheet can identify additional people at increased risk for hepatitis C. These forms should be used by all clinics and public health services to identify people willing to report hepatitis C risk factors. Those with risk factors should be evaluated and tested to increase recognition and therapeutic opportunities for this treatable disease. Primary Funding Source: Scherring Plough Invited Papers Public Health & Disaster Preparedness Chair: Robert Valdez, Ph.D., M.H.S.A. Tuesday, June 8 • 11:15 a.m.-12:45 p.m. • Panelists: Kristine Gebbie, Columbia University; Nicole Lurie, RAND; Carmen Nevarez (no abstracts provided)