Chronic Care Delivery
advertisement
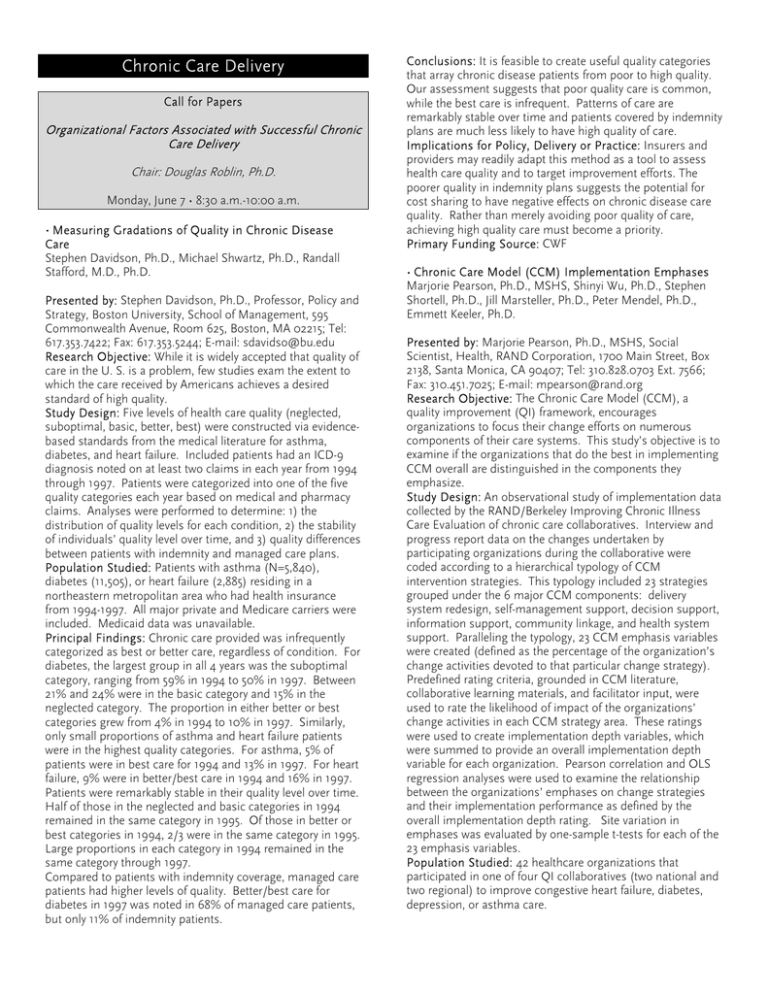
Chronic Care Delivery Call for Papers Organizational Factors Associated with Successful Chronic Care Delivery Chair: Douglas Roblin, Ph.D. Monday, June 7 • 8:30 a.m.-10:00 a.m. • Measuring Gradations of Quality in Chronic Disease Care Stephen Davidson, Ph.D., Michael Shwartz, Ph.D., Randall Stafford, M.D., Ph.D. Presented by: Stephen Davidson, Ph.D., Professor, Policy and Strategy, Boston University, School of Management, 595 Commonwealth Avenue, Room 625, Boston, MA 02215; Tel: 617.353.7422; Fax: 617.353.5244; E-mail: sdavidso@bu.edu Research Objective: While it is widely accepted that quality of care in the U. S. is a problem, few studies exam the extent to which the care received by Americans achieves a desired standard of high quality. Study Design: Five levels of health care quality (neglected, suboptimal, basic, better, best) were constructed via evidencebased standards from the medical literature for asthma, diabetes, and heart failure. Included patients had an ICD-9 diagnosis noted on at least two claims in each year from 1994 through 1997. Patients were categorized into one of the five quality categories each year based on medical and pharmacy claims. Analyses were performed to determine: 1) the distribution of quality levels for each condition, 2) the stability of individuals’ quality level over time, and 3) quality differences between patients with indemnity and managed care plans. Population Studied: Patients with asthma (N=5,840), diabetes (11,505), or heart failure (2,885) residing in a northeastern metropolitan area who had health insurance from 1994-1997. All major private and Medicare carriers were included. Medicaid data was unavailable. Principal Findings: Chronic care provided was infrequently categorized as best or better care, regardless of condition. For diabetes, the largest group in all 4 years was the suboptimal category, ranging from 59% in 1994 to 50% in 1997. Between 21% and 24% were in the basic category and 15% in the neglected category. The proportion in either better or best categories grew from 4% in 1994 to 10% in 1997. Similarly, only small proportions of asthma and heart failure patients were in the highest quality categories. For asthma, 5% of patients were in best care for 1994 and 13% in 1997. For heart failure, 9% were in better/best care in 1994 and 16% in 1997. Patients were remarkably stable in their quality level over time. Half of those in the neglected and basic categories in 1994 remained in the same category in 1995. Of those in better or best categories in 1994, 2/3 were in the same category in 1995. Large proportions in each category in 1994 remained in the same category through 1997. Compared to patients with indemnity coverage, managed care patients had higher levels of quality. Better/best care for diabetes in 1997 was noted in 68% of managed care patients, but only 11% of indemnity patients. Conclusions: It is feasible to create useful quality categories that array chronic disease patients from poor to high quality. Our assessment suggests that poor quality care is common, while the best care is infrequent. Patterns of care are remarkably stable over time and patients covered by indemnity plans are much less likely to have high quality of care. Implications for Policy, Delivery or Practice: Insurers and providers may readily adapt this method as a tool to assess health care quality and to target improvement efforts. The poorer quality in indemnity plans suggests the potential for cost sharing to have negative effects on chronic disease care quality. Rather than merely avoiding poor quality of care, achieving high quality care must become a priority. Primary Funding Source: CWF • Chronic Care Model (CCM) Implementation Emphases Marjorie Pearson, Ph.D., MSHS, Shinyi Wu, Ph.D., Stephen Shortell, Ph.D., Jill Marsteller, Ph.D., Peter Mendel, Ph.D., Emmett Keeler, Ph.D. Presented by: Marjorie Pearson, Ph.D., MSHS, Social Scientist, Health, RAND Corporation, 1700 Main Street, Box 2138, Santa Monica, CA 90407; Tel: 310.828.0703 Ext. 7566; Fax: 310.451.7025; E-mail: mpearson@rand.org Research Objective: The Chronic Care Model (CCM), a quality improvement (QI) framework, encourages organizations to focus their change efforts on numerous components of their care systems. This study’s objective is to examine if the organizations that do the best in implementing CCM overall are distinguished in the components they emphasize. Study Design: An observational study of implementation data collected by the RAND/Berkeley Improving Chronic Illness Care Evaluation of chronic care collaboratives. Interview and progress report data on the changes undertaken by participating organizations during the collaborative were coded according to a hierarchical typology of CCM intervention strategies. This typology included 23 strategies grouped under the 6 major CCM components: delivery system redesign, self-management support, decision support, information support, community linkage, and health system support. Paralleling the typology, 23 CCM emphasis variables were created (defined as the percentage of the organization’s change activities devoted to that particular change strategy). Predefined rating criteria, grounded in CCM literature, collaborative learning materials, and facilitator input, were used to rate the likelihood of impact of the organizations’ change activities in each CCM strategy area. These ratings were used to create implementation depth variables, which were summed to provide an overall implementation depth variable for each organization. Pearson correlation and OLS regression analyses were used to examine the relationship between the organizations’ emphases on change strategies and their implementation performance as defined by the overall implementation depth rating. Site variation in emphases was evaluated by one-sample t-tests for each of the 23 emphasis variables. Population Studied: 42 healthcare organizations that participated in one of four QI collaboratives (two national and two regional) to improve congestive heart failure, diabetes, depression, or asthma care. Principal Findings: The organizations significantly varied in emphasis on each CCM strategy (p<0.01). Only 4 of the 23 CCM emphasis variables, however, were significantly correlated with the overall implementation depth ratings. The organizations with greater depth of implementation included an emphasis on organizing and engaging a practice team (Pearson correlation coefficient 0.46, p < 0.01), involving patients in collaborative decision-making (0.37, p <0.05), or encouraging provider participation in the QI efforts (0.31, p < 0.05). However, sites that emphasized traditional patient education (as distinct from patient activation and selfmanagement support) showed poorer implementation performance (-.41, p <0.01). Our parsimonious regression equation model shows that three variables – practice team, collaborative decision-making, and patient education (negative effect) – explained 43% of variance in the depth rating (model significant at p <0 .001 level). Conclusions: Of 23 change emphases, only 4 distinguished the best CCM implementers (i.e., the organization whose change activities were most likely to have impact, according to CCM principles). These key emphases included organizing and engaging practice teams, collaborative decision making with patients, encouraging provider participation in QI efforts, and de-emphasis on traditional patient education. Implications for Policy, Delivery or Practice: To successfully implement CCM, organizations should be encouraged to emphasize practice teams, patient collaboration, and provider participation in their QI strategies and to not over emphasize traditional patient education. Collaborative facilitators and organization leaders should consider if increased training and resources are needed to support interventions in these areas. Primary Funding Source: RWJF • The Effect of Primary Health Care Orientation on Chronic Illness Care Management Julie Schmittdiel, M.A., Stephen Shortell, Ph.D., Thomas Rundall, Ph.D. Presented by: Julie Schmittdiel, M.A., Ph.D. Candidate/Graduate Student Researcher, Health Services and Policy Analysis, University of California, Berkeley, 1421 Tilia Street, San Mateo, CA 94402; Tel: 650.572.9416; Fax: 650.572.2760; E-mail: jschmittdiel@yahoo.com Research Objective: To determine whether there is a relationship between greater levels of primary health care orientation in physician organizations and organizations’ implementation of chronic illness care management. Study Design: A cross-sectional telephone survey of 1,590 physician organizations throughout the U.S. conducted from September 2000 to September 2001. The resulting response rate was 70%. Population Studied: 1,040 physician organizations with 20 or more practicing physicians whose physicians treat at least one of the following chronic illnesses: asthma, diabetes, depression, or CHF. Principal Findings: Of the eight measures of primary health care orientation (severity of disease treated in primary care; health promotion practice; health education practice; accepted risk for hospitalization costs; required reporting to outside organizations; rate of primary care practitioner turnover; use of electronic medical record; use of electronic standardized problem list), six are significantly related to physician organization overall use of 11 measures of chronic care management. This finding is valid after adjustment for numerous control variables including age of organization, size of organization, capital available, practice type, ownership, and environment. Conclusions: Organizations that emphasize the use of primary health care, which emphasizes comprehensive health services within primary care and a commitment to overall patient health, appear to have greater use of chronic care management practices. Implications for Policy, Delivery or Practice: Policies that help organizations to strengthen their commitment to primary care may also help these organizations increase their use of chronic care management. Recent research suggests that the primary care setting is the ideal home for improved chronic care delivery. This study gives empirical weight to this health care approach, and gives policy makers and other stakeholders a potential way to help close the “quality chasm” in chronic illness care. Primary Funding Source: RWJF • A Meta-Analysis of Interventions to Improve Chronic Illness Care Alexander Tsai, M.A., Sally Morton, Ph.D., Emmett Keeler, Ph.D. Presented by: Alexander Tsai, M.A., Epidemiology and Biostatistics, Case Western Reserve University, 2511 Overlook Road, Suite 6, Cleveland Heights, OH 44106-2459; Tel: 216.321.5496; E-mail: act2@case.edu Research Objective: The Chronic Care Model is a recently developed framework aimed at improving chronic illness care. While the Chronic Care Model in its entirety has not been evaluated in controlled studies, there have been many trials of interventions that have incorporated one or more elements. We sought to use empirical data from the literature to address two related research questions: 1) do interventions that incorporate one or more elements of the Chronic Care Model result in improved outcomes of interest for specific chronic illnesses; and 2) are any elements essential or superfluous? Study Design: To identify studies that incorporate one or more elements of the Chronic Care Model, we reviewed bibliographies of previously published systematic reviews and meta-analyses relevant to this topic, searched the MEDLINE database (1998-2003), and consulted with experts. Data were extracted on study characteristics and intervention effects on clinical outcomes, quality of life, and processes. Studies were characterized by the elements of the chronic care model in their intervention. Population Studied: We identified randomized and nonrandomized controlled trials of interventions compared to a control or usual care group for four conditions of interest: asthma, congestive heart failure, depression, and diabetes. Principal Findings: Of 1,345 abstracts screened, 112 studies contributed data to the random-effects meta-analysis: 27 asthma studies, 21 congestive heart failure studies, 33 depression studies, and 31 diabetes studies. Interventions that contained one or more elements of the chronic care model led to a pooled effect size of –0.17 (95% CI, –0.24 to –0.11) on clinical outcomes and 0.11 (95% CI, 0.02-0.21) on quality of life, and a pooled relative risk of 1.19 (95% CI, 1.10-1.28) on key processes. No single element was found to be essential or superfluous for effectiveness. We detected evidence of publication bias for studies of congestive heart failure (all outcome measures) and asthma (clinical outcome measure). Conclusions: Interventions that contain one or more elements of the Chronic Care Model improve clinical outcomes and processes -- and to a lesser extent, quality of life -- for patients with chronic illnesses. The elements most responsible for these benefits cannot be determined from existing data. Implications for Policy, Delivery or Practice: Interventions that contain one or more elements of the Chronic Care Model do improve outcomes and processes. An evaluation of three Institute for Healthcare Improvement (IHI) Breakthrough Series Collaboratives is currently underway to determine whether or not the Chronic Care Model is an effective intervention when implemented as a package. Primary Funding Source: RWJF • Sustainability and Spread of Chronic Illness Care Improvement Shin-Yi Wu, Ph.D., Marjorie Pearson, Ph.D., Emmett Keeler, Ph.D., Stephen Shortell, Ph.D., Peter Mendel, Ph.D., Jill Marsteller, Ph.D. Presented by: Shin-Yi Wu, Ph.D., Associate Engineer, Health, RAND Corporation, 1700 Main Street, Santa Monica, CA 90401; Tel: 310.3930411; Fax: 310.3934818; E-mail: shinyi@rand.org Research Objective: To assess the sustainability and spread of Chronic Care Model (CCM) implementation efforts initiated during quality improvement (QI) collaboratives and to examine the relationships between CCM implementation intensity and QI sustainability and spread. Study Design: Observational study of data collected by the RAND/Berkeley Improving Chronic Illness Care Evaluation (ICICE). ICICE found that, during the collaboratives, the study organizations implemented multiple change strategies suggested by the CCM, a QI framework that encourages change across six areas: delivery system redesign (DSR), patient self-management support (SM), decision support (DS), information support (IS), community linkages (CL), and health system support (HSS). To examine if these change activities were sustained and spread, we interviewed key contact persons in each organization one year after the collaborative and qualitatively coded the interview transcripts to create variables for the post-collaborative status of their QI activities (continued and expanded, maintained at collaborative level only, or declined) and their reported success at spread (any and type). We then used ordinal regression models to examine whether successful QI sustainability and spread were associated with the intensity (quantity and depth) of the organizations’ CCM implementation during the collaborative (overall and in specific CCM areas), controlling for organization type (public vs. nonpublic), disease focus, and the organization’s baseline congruence with CCM (measured by Assessment of Chronic Illness Care instrument). Population Studied: 42 organizations participating in two national and two regional collaboratives to improve care for congestive heart failure, diabetes, depression, or asthma. Principal Findings: The majority of the organizations (57%) reported continuing and expanding their QI efforts after the collaborative, while 25% maintained at their collaborative level and 14% did not sustain their efforts. Seventy-nine percent reported successfully spreading these changes: 42% within their site, 30% to additional sites, and 27% to other chronic conditions. The intensity of many of their change activities during the collaborative was positively associated with both sustainability and spread (p<.05). The best prediction models for sustainability (judged by the highest Nagelkerke psudo Rsquare) were those that included the depth of CCM implementation overall or the depth of changes to obtain HSS (leadership support, provider participation, or coherent system improvement), followed by depth in IS (patient registry system, use of information for care management, or feedback of performance data). The best prediction models for spread included the quantity of changes to improve DS (guideline institutionalization, provider education, or expert consultation) or the quantity of changes overall. Conclusions: One year later, large proportions of healthcare organizations report sustaining and spreading the CCM change efforts they initiated during a QI collaborative. The intensity of the organization’s CCM implementation efforts during the collaborative relates to successful sustainability and spread. Efforts to acquire health system support and build information support are particularly critical to sustaining QI activities, while increased decision support capabilities can facilitate successful spread. Implications for Policy, Delivery or Practice: To maximize continuation and spread of CCM changes, collaborative and organizational leaders should encourage high intensity of change efforts (in both quantity and depth) during the initial collaborative period. Primary Funding Source: RWJF Call for Papers Innovative Strategies to Integrate Patients into Chronic Care Delivery Chair: Michael Von Korff, Sc.D. Monday, June 7 • 10:30 a.m.-12:00 p.m. • Evidence-Based Checkup for Patient Education Web Sites Suzanne Boren, M.H.A., E. Andrew Balas, M.D., Ph.D., Zaynab Mustafa, B.A. Presented by: Suzanne Boren, M.H.A., Associate Director, Center for Health Care Quality, University of Missouri, 324 Clark Hall, Columbia, MO 65211; Tel: 573.882.1492; Fax: 573.884.0474; E-mail: BorenS@health.missouri.edu Research Objective: To assist the development and selection of better patient education web sites through identification of essential issues to be covered by them based on the results of pertinent randomized clinical trials. Study Design: Checklist development: Systematic searches in MEDLINE, HealthSTAR, and CINAHL were conducted for patient education randomized controlled trials. Four eligibility criteria were applied: (i) targeted clinical area, (ii) randomized clinical trial, (iii) patient focused educational intervention tested versus control, and (iv) measurement of the outcome of care. Substantiated educational content items and achieved improvements were abstracted into checklists. Web site evaluation: Through extensive searches European and American web sites were identified with the following eligibility criteria: (i) academic health sciences center, (ii) comprehensive patient information on the web, and (iii) focus on a targeted clinical area. Provided web site information was compared with the evidence-based checklists. Population Studied: The targeted clinical areas of this study included diabetes, asthma, and congestive heart failure. Principal Findings: One hundred and seventy eligible patient education trials were analyzed (11,760 patients in 88 diabetes studies; 3,353 patients in 12 congestive heart failure studies; 10,857 patients in 70 asthma studies). Using the evidence linking tested interventions to improved outcomes, there were 25 substantiated educational content items identified for diabetes, 15 educational content items for congestive heart failure, and 23 educational content items for asthma. The web sites of 46 academic health science centers and referral sites missed several essential content items. In diabetes, 59.7 percent of content items were missed; 44.8 percent of content items were missed in congestive heart failure; and 65.5 percent of content items were missed in asthma. Conclusions: With the rapidly accumulating results of clinical trials, Internet-based patient education programs could be redefined with evidence linking specific content items to better outcomes. While many academic health centers offer valuable information, there is a surprising lack of several critical items in prestigious patient education web sites. Implications for Policy, Delivery or Practice: Educating patients and providers about good chronic care needs to be based on scientifically sound evidence. Patient education involves more than telling people what to do or giving them instructional material to read. Packaging of educational messages and alternative delivery techniques should be analyzed in the future. Primary Funding Source: , National Library of Medicine; Information Society General Directorate of the European Commission • Evaluating Concordance to American Diabetes Association Standards of Care for Type 2 Diabetes through Group Visits in an Uninsured or Inadequately Insured Patient Population Dawn Clancy, M.D., Dennis Cope, M.D., Kathryn Marley Magruder, Ph.D., Peng Huang, M.D., Tamara Wolfman, M.D. Presented by: Dawn Clancy, M.D., Assistant Professor of Medicine, Medical University of South Carolina, 1614 Regimental Lane, Johns Island, SC 29455; Tel: 843.953.8986; Fax: 843.953.8980; E-mail: clancyd@musc.edu Research Objective: To evaluate the effectiveness of a managed care approach to health care delivery, group visits, in the management of uninsured or inadequately insured patients with type 2 diabetes. Study Design: One hundred twenty patients with uncontrolled type 2 diabetes were randomly assigned to receive their care in group visits or usual care for 6 months. After 6 months, concordance with 10 process-of-care indicators recommended by the American Diabetes Association (ADA) standards of care1 was evaluated through chart abstraction. The 10 items evaluated were: up-to-date HbA1c levels and lipid profiles, urine for microalbumin, appropriate use of angiotensin converting enzyme inhibitor or angiotensin receptor blockers, use of lipid lowering agents where indicated, daily aspirin use, annual foot examinations, annual referrals for retinal examinations, and immunizations against streptococcal pneumoniae and influenza. Population Studied: Uninsured and underinsured patients with type 2 diabetes in an outpatient general medicine clinic that serves predominantly disadvantaged African Americans. Principal Findings: Patients who received care in group visits showed statistically significant improvement in concordance with these 10 process-of-care indicators (p<0.001). 76% of the patients who received care in group visits had at least 9 of these 10 items up to date as compared to 23% of control patients; 86% of patients in group visits had at least 8 of the 10 indicators as compared to 47% of control patients. Conclusions: Group visits proved more effective in promoting concordance with ADA standards of care than usual care in the treatment of uninsured or inadequately insured patients with type 2 diabetes. Implications for Policy, Delivery or Practice: Primary care providers caring for patinets with type 2 diabetes may want to consider using groups to provide education and care for people with type 2 diabetes because it may be both more costefficient and effective than individual consultations. Primary Funding Source: RWJF, Agency for Healthcare Quality and Research • Managing Old-Age Diabetes: The Effect of Health Club Enrollment and Use on Medical Costs and Outcomes among Older Adults Kun (Sue) Gao, Ph.D. student, M.A., MAJ Marsha Patrick, Ph.D., M.H.A., Matthew Maciejewski, Ph.D., James LoGerfo, M.D., M.P.H. Presented by: Kun (Sue) Gao, Ph.D. student, M.A., Research Assistant, Department of Health Services, University of Washington, 1959 N.E. Pacific Street, Seattle, WA 98195; Tel: 206.484.2620; E-mail: suekgao@u.washington.edu Research Objective: The purpose of this study was to examine the effect of health club enrollment and use on the healthcare costs and outcomes in an older population with diabetes. Study Design: This nested retrospective cohort study used healthcare utilization and cost data with a sample size of 3,183. Annualized total cost, inpatient cost, primary care cost and prescription drug cost were compared using health club enrollment status and actual health club weekly visits. The generalized linear model with the gamma distribution and log link was used for all cost analyses. Ordinary least-squares regression was used to examine the effect of health club enrollment and use on disease outcome as measured by the HbA1c level. Age, sex, co-morbidity, duration of participation, baseline costs and baseline physical measures were included in all models to control for possible selection bias, and data were weighted according to the length of enrollment. Population Studied: From a larger cohort of all 6,583 Medicare+Choice enrollees at Group Health Cooperative of Puget Sound who chose a free health club benefit (HCB) and 19,749 age and sex matched controls, we selected all 758 diabetics from the HCB group and the 2,425 diabetics from the control group. HCB is a health club benefit that is used by several major managed Medicare programs in the U.S. Principal Findings: HCB enrollees and controls had comparable chronic disease score (CDS) and baseline Hba1c level. HCB enrollees scored higher in almost all baseline medical costs. In the follow-up period HCB enrollees had significantly higher primary care costs (ratio=1.17, p< .001) but lower adjusted HbA1c levels than controls (7.42% vs. 7.57%, p< .001). In terms of actual health club use, the low users who averaged less than one visit per week showed the same pattern as the total HCB enrollees, while the high users averaging one or more weekly visits had significantly lower adjusted total cost compared to both controls (ratio= 0.97, p< .05) and the low users (ratio= 0.80, p< .01). The high users and low users did not differ much in terms of HbA1c levels (7.31% vs. 7.44% respectively), yet both were significantly lower than controls (7.57%). Conclusions: Enrollment in HCB alone did not result in significant cost-savings, however, enrollees did perform better in terms of disease outcomes. Moreover, enrollees who averaged one or more health club visits per week had significantly lower annual total healthcare costs. Implications for Policy, Delivery or Practice: Cost saving and better management of diabetes could be potentially achieved by promoting more actual health club use on top of the membership benefit. More behavioral experimental studies are also needed to identify motivational factors that would encourage diabetic older adults to engage in higher levels of exercise. Primary Funding Source: CDC • Collaborative Care Needs and Preferences of Primary Care Patients with Multimorbidity Polly Noel, Ph.D., Michael Parchman, M.D., M.P.H., John Williams, Jr., M.D., M.H.Sc., John Cornell, Ph.D., B. Chris Frueh, Ph.D., Anne Larme, Ph.D., Lewis Kazis, Sc.D., Austin Lee, Ph.D., Jacqueline Pugh, M.D. Presented by: Polly Noel, Ph.D., Associate Director/Assistant Professor, Medicine, VERDICT Center of Excellence/STVHCS & UTHSCSA, 7400 Merton Minter Boulevard, San Antonio, TX 78229; Tel: 210.617.5110; Fax: 210.567.4423; E-mail: pollyh@verdict.uthscsa.edu Research Objective: To describe the health care experiences of patients with multimorbidity and their collaborative care needs and preferences. Study Design: Combined qualitative/quantitative methods. First, we conducted focus groups at 8 primary care clinics in 4 states. A general interview guide included open-ended questions derived from the 4 collaborative care elements proposed by Von Korff and colleagues to enhance the management of chronic illness (identification of patientcentered problems, targeting & goal-setting, self-management needs, and active sustained follow-up). Identified themes were used to finalize a mailed survey to examine the difference in collaborative care needs and preferences among 360 primary care patients with multimorbidity and 360 patients with only 1 chronic illness. Population Studied: Primary care patients with multiple chronic illnesses served by the Veterans Health Administration. Principal Findings: Focus Group: Sixty patients with two or more chronic illnesses participated. Patient-identified problems included negative effects on physical and emotional functioning, work/leisure, and relationships. Polypharmacy was a major concern and affected patients’ lives in a number of areas. Problematic interactions with providers and the health care system were also mentioned, often in relation to specialty care. These health care system “hassles” included long waits for referrals, difficulty accessing nonscheduled urgent care, poor continuity of care between primary and subspecialty clinics, and juggling multiple appointments. Patients were more likely to blame the system, as opposed to individual providers, for these problems, but several patients related incidents in which providers had overlooked or ignored their concerns or provided conflicting advice. Most participants, however, expressed overall satisfaction with their care and their primary care providers. Many said they lacked knowledge or skills needed to manage their chronic illnesses. Patients were willing to use technology for monitoring or educational purposes as long as it did not preclude human contact. Patients were also very receptive to receiving care or monitoring from nonphysician providers as long as they were used to augment, not eliminate, a physician’s care. Survey: 422 surveys were returned. Patients with multimorbidity reported significantly more health care hassles and problems with polypharmacy, but greater satisfaction with their primary care providers. Patients with multimorbidity were more likely than patients with only a single chronic illness to have been monitored between appointments, participated in health education, or been seen by a nonphysician provider in the prior 6 months, but the overwhelming majority did not receive these services. Patients with multimorbidity were also more likely to express a desire to learn a variety of self-care skills, including strategies to manage their medications, improve their ability to communicate with their providers, lose weight, manage their pain, and improve their sexual relationships. Conclusions: The needs and preferences of patients with multimorbidity are consistent with the basic tenets of patientcentered, collaborative care. In spite of their general satisfaction, patients with multimorbidity are more likely to report health care system “hassles.” Educational support and monitoring for these patients appears suboptimal. Implications for Policy, Delivery or Practice: Multimorbidity creates an enormous burden for these patients. Clinics that organize and deliver services in accordance with a collaborative care approach may best meet the needs of these complex patients. Primary Funding Source: VA • Motivational Interviewing to Support Antiretroviral Treatment Adherence Angela Thrasher, M.P.H., Carol Golin, M.D., Jo Anne Earp, Sc.D. Presented by: Angela Thrasher, M.P.H., Doctoral Student, Cecil G. Sheps Center for Health Services Research, University of North Carolina at Chapel Hill, 725 Airport Road, CB# 7590, Chapel Hill, NC 27599-7590; Tel: 919.824.4794; E-mail: angela_thrasher@unc.edu Research Objective: Although research explicitly linking motivational interviewing (MI) -- a client-centered counseling style shown to effectively improve the health behavior of individuals -- to behavior change exists, few studies report on MI’s quality or examine how quality influences effectiveness. We studied the relationship between MI quality and adherence to antiretroviral therapy (ART) in the context of the PACT study, a randomized, controlled trial of an MI-based intervention with 158 HIV-infected patients failing their current regimen to an educational control. Study Design: Among the first 48 people randomized to receive the MI-based intervention, we evaluated the quality of professionally-transcribed audiotaped MI sessions. The Motivational Interviewing Skill Code (MISC), a standardized MI coding scheme, globally assesses patient-counselor interactions and counts specific recommended communication behaviors of therapist and client. We used the MISC to measure the proportion of interactions that achieved a standardized quality level for 22 specific, counseling behaviors and 6 global measures. We assessed ART adherence using electronic bottle cap monitor and pill count data at 4, 8, and 12 weeks follow-up. We then correlated ART adherence and specific MI counseling behaviors. Population Studied: HIV-positive patients who have failed antiretroviral therapy and are attending a university-based infectious-disease clinic. Principal Findings: The sample (n=48) was predominantly male (70%) and minority (90%), with an average age of 40 years and an average adherence level at exit of 85% (range: 5100%). On 4 of 5 behavioral indicators, the majority of MI sessions achieved the targeted quality level: 67% achieved it for global therapist rating; 88% for reflections to questions ratio; 33% percent for using open-ended questions; 96% percent for complex reflections; 100% for MI-consistent statements. On a 7-point scale, interviewers were rated highest on “genuineness” (5.3) and “warmth” (5.3), lowest on “egalitarianism” (4.0). Interviewer behaviors significantly associated with or trending towards an association with ART adherence were: total number of facilitative comments (r=.42, p=.026), total number of paraphrases (r=.35, p=.069), number of open-ended questions asked (r=.34, p=.077), and ratio of reflections given to questions asked (r=.32, p=.097). Conclusions: High quality MI can be conducted within the structure of a randomized, controlled trial. Moreover, MI quality affect effectiveness. Further studies should concentrate on teasing out the specific counseling behaviors most closely associated with behavioral change. Implications for Policy, Delivery or Practice: Program fidelity is a key aspect of intervention success. Using the MISC along with regular feedback to the interviewers is an effective way of assessing and increasing MI program fidelity. Primary Funding Source: Society for General Internal Medicine Call for Papers Issues in Chronic Care Delivery & Quality Chair: Sherrie Kaplan, Ph.D., M.P.H. Tuesday, June 8 • 9:15 a.m.-10:45 a.m. • Persistent High Out-of-Pocket Costs among Medicare Beneficiaries Wenke Hwang, Ph.D, Jennifer Wolff, Ph.D, Gerard Anderson, Ph.D Presented by: Wenke Hwang, Ph.D, Assistant Research Scientist, Department of Health Policy and Management, Johns Hopkins University, 624 North Broadway, Room 307, Baltimore, MD 21205; Tel: 410.614.3199; Fax: 410.955.2301; Email: whwang@jhsph.edu Research Objective: Medicare’s cost-sharing requirements and benefit limits leave some beneficiaries with high out-ofpocket (OOP) costs in any given year. We explore the extent to which high OOP costs tend to persist over time among Medicare beneficiaries, and what types of health services are primarily responsible for persistent high OOP costs. Study Design: The Medicare Current Beneficiary Survey was used to examine OOP costs for beneficiaries who were continuously surveyed from 1997 through 1999. Out-ofpocket spending reflects cost-sharing for Medicare covered services and direct medical spending for Medicare noncovered services. High out-of-pocket expense was defined as the highest decile (top 10%) of out-of-pocket spending in any given year. Beneficiaries were assigned to three categories: (1) those with consistent high out-of-pocket expenditures over all three years (“always high”), (2) those with one or two years of high out-of-pocket expenditures (“intermittent high”), and (3) those without high out-of-pocket expenditures in any year (“never high”) OOP costs. Logistic regression was used to examine baseline characteristics associated with being categorized in the “always high” OOP group. Characteristics that were considered include age, gender, race, supplemental health insurance, place of residence (community versus institution), and numbers of self-reported chronic conditions. Population Studied: Institutional and community-dwelling Medicare beneficiaries age 65 and older (N=3,052). Principal Findings: Beneficiaries with “always high” OOP costs were on average 91 years of age, predominantly female (79%), white (95%), and incurred an average of $16,067 annually in direct medical spending, and another $1,292 in health insurance premiums. Total personal health care costs for individuals with “always high” OOP costs were four times higher than beneficiaries with “intermittent high” OOP costs ($3,860), and more than 20 times higher than beneficiaries with “never high” OOP experience ($735). For beneficiaries with “always high” OOP costs, more than 85% of personal spending was for institutional care compared to 33% for beneficiaries with “intermittent high” OOP costs, and 3% for the “never high” OOP group. Overall, Medicare contributed 51% of total health care costs for its beneficiaries, but its contribution was less than 25% of total health care costs for those with “always high” OOP costs. After adjusting for age, gender, race, and insurance status, beneficiaries residing in an institution were 20 times (OR = 23.33, 95% CI, 11.9 – 43.24) more likely to have “always high” OOP costs than beneficiaries living in communities; and beneficiaries with multiple chronic conditions were 2.7 times (OR = 2.69, 95% CI 1.5-4.4) more likely to have “always high” OOP costs compared to beneficiaries with no or only one chronic condition. Conclusions: Medicare beneficiaries who have multiple chronic conditions or incur institutional long-term care were much more likely to have persistent high OOP costs. Implications for Policy, Delivery or Practice: These data suggest that Medicare is unable to fulfill its intended role of spreading risk to buffer individuals from financially devastating consequences related to health care need. As increasing number of beneficiaries grow older, Medicare needs a substantial reform in its benefit design in the areas of chronic and long-term care. Primary Funding Source: RWJF • Measuring Quality of Care in People with Arthritis Sarah Sampsel, M.P.H., Catherine MacLean, M.D., Ph.D., Philip Renner, M.B.A., Russell Mardon, Ph.D. Presented by: Sarah Sampsel, M.P.H., Senior Health Care Analyst, Quality Measurement, National Committee for Quality Assurance, 2000 L Street, NW, Suite 500, Washington, DC 20036; Tel: 202.955.1716; Fax: 202.955.3599; E-mail: sampsel@ncqa.org Research Objective: Arthritis is one of the leading causes of disability in the United States, yet no standard set of measures currently exists to measure the quality of arthritis care and bring effective care processes to the attention of health care providers, hospitals and health plans. To develop new clinical performance measures to assess care of patients with arthritis. Study Design: Observational study conducted in five health plans. A clinical expert panel was convened to develop measure specifications based on guidelines and evidence supporting critical aspects of arthritis care. Four aspects of care were assessed during the summer of 2004: DMARD utilization for patients with rheumatoid arthritis; appropriate gastrointestinal prophylaxis for patients utilizing NSAIDS; comprehensive osteoarthritis care; and comprehensive symptom assessment. Population Studied: Five health plans participated in the study by providing patient-level administrative and medical record data. The enrollments of these plans ranged from nearly 1 million to approximately 150,000. The plans included network and staff models, and were located in several geographic regions of the country. Plan products included commercial, Medicare and Medicaid. Principal Findings: We found that the implementation of performance measures for key aspects of arthritis care is challenged by the availability of administrative data. However, we identified the potential for improvement in each of the four areas studied. For the Initiation of DMARD Therapy for Patients with Rheumatoid Arthritis, two of three health plans showed performance higher than 51%; the range was 31 – 76 %, with a mean rate of 66.7%. Performance on the prophylaxis against gastrointestinal bleeding among high-risk patients treated with nonsteroidal anti-inflammatory drugs measure ranged from 22.6% to 40.8% with a mean performance rate of 35.9%. For the arthritis symptom assessment measure, performance ranged from approximately 50 - 90 % for the pain assessment (mean rate of 79.6%) and 50 - 60% (mean rate of 62.0%) for functional assessment. Finally, the comprehensive osteoarthritis treatment measure which required reporting of three components, had the following mean rates by component: recommendation for weight loss – 48.4%, recommendation for physical activity/therapeutic exercise – 42.5%, and first line acetaminophen use – 15.1%. Conclusions: The key challenge to the feasibility of arthritis performance measures is the lack of administrative data to identify the eligible population. Administrative data capture suffers as a result of under-coding and under-recognition of arthritis. Developing measures that can be specified at the provider or provider group level can facilitate quality improvement in patient care, however, it is not known if such efforts would also improve the appropriate diagnosis and coding to improve data capture. This project has provided meaningful and useful information to NCQA to pursue the development of provider level measurement and promote use in pay for performance modules. Implications for Policy, Delivery or Practice: Consensus around a single set of measures creates a powerful tool for focusing on key components of arthritis care as a basis for quality improvement and allows for a valid comparison of care within and across health care settings. However, in the absence of reliable and available administrative data, quality improvement and performance measurement activities might best be focused at the provider or provider group level. Primary Funding Source: Corporate Grant - Pharmaceutical Sponsor • Adverse Maternal Outcomes among Asthmatic Women Nancy MacMullen, Ph.D., APN/CCNS, Jay Shen, Ph.D., Jay Shen, Ph.D., Catherine Tymkow, ND, APN, CWHNP Presented by: Jay Shen, Ph.D., University Professor, Health Administration, Governors State University, One University Parkway, University Park, IL 60466; Tel: 708.534.3144; Fax: 708.534.8041; E-mail: j-shen@govst.edu Research Objective: Limited research has been done on adverse maternal outcomes of asthmatic women who are more susceptible to poorer outcomes. This study examines differences in adverse maternal outcomes between women with asthma and women without asthma. Study Design: Twelve adverse maternal outcome measures examined were pre-term labor, hypertensive disorders of pregnancy (3 measures), gestational diabetes, antepartum hemorrhage (2 measures), membrane disorders (2 measures), cesarean section, postpartum hemorrhage and pregnancy longer than 42 weeks. Maternal age, ethnicity, health insurance status, the income level and comorbidities were adjusted. Population Studied: A total of 7,777 asthmatic patients identified from 563,621 women aged from 13 to 55 who had a delivery in 2001, abstracted from the National Inpatient Sample. Of the women who delivered, 1.4 percent had asthma. 31,108 (four times of 7,777) patients were randomly selected from 541,719 non-asthmatic women as the comparison group of the asthmatic patients. Principal Findings: Compared to non-asthmatic women, women with asthma had a higher risk of having preterm labor (Odds Ratio (OR) [95% Confidence Interval, CI] 1.22 [1.06, 1.41]), pre-eclampsia (OR [CI], 1.50 [1.25, 1.81]), transient hypertension of pregnancy (OR [CI], 1.34 [1.10, 1.63]), pregnancy-induced hypertension (OR [CI], 1.45 [1.27, 1.66]), gestational diabetes (OR [CI], 1.68 [1.47, 1.92]), placenta previa (OR [CI], 1.52 [1.05, 2.21]), infection of the amniotic cavity (OR [CI], 1.53 [1.27, 1.84]), cesarean section (OR [CI], 1.34 [1.26, 1.43]) and pregnancy term longer than 42 weeks (OR [CI], 1.15 [1.02. 1.30]). Women with asthma had a lower risk of having abruption placenta (OR [CI], 0.07 [0.01, 0.66]), and had comparable risk of having premature rupture of membrane (OR [CI], 0.20 [0.03, 1.38] and postpartum hemorrhage ((OR [CI], 0.19 [0.02, 1.83]. Conclusions: In comparing adverse maternal outcomes of non-asthmatic women, asthmatic women had poorer outcomes in nine of the 12 measures, better outcome in one measure, and comparable outcomes in two measures. Asthmatic women were clinically much more vulnerable to having adverse maternal outcomes, especially pre-eclampsia, pregnancy-induced hypertension, gestational diabetes, placenta previa and infection of the amniotic cavity. Implications for Policy, Delivery or Practice: Health care providers should be aware of adverse pregnancy outcomes resulting from etiological factors related to asthma. Preventive interventions such as educational programs, symptom and medication management, and avoidance of environmental and stress related triggers will assist women to co-manage their asthma during pregnancy. Primary Funding Source: AHRQ • Does Literacy Impact the Effectiveness of a Disease Management Program in Congestive Heart Failure? Brad Smith, Ph.D, Autumn Dawn Galbreath, M.D., Robert Ellis, M.D., Emma Forkner, R.N., Richard Krasuski, M.D., Gregory Freeman, M.D. Presented by: Brad Smith, Ph.D, Statistician, UTHSCSA Disease Management Center/Altarum Institute, 4243 Piedras Drive E., Suite 240, San Antonio, TX 78228; Tel: 210.567.9708; Fax: 210.567.9712; E-mail: smithp5@uthscsa.edu Research Objective: To investigate whether the effectiveness of disease management in congestive heart failure (CHF) patients is influenced by a patient’s literacy level, as measured by educational attainment. Existing studies of the efficacy of disease management (DM) programs have largely been conducted on group-insured populations that tend to be employed and have above average levels of education. Consequently, we have little idea whether such programs will be effective as they expand to more diverse, and possibly less-well-educated, patient populations. Study Design: For this study, primary outcomes included mortality, time to first emergency department visit and New York Heart Association (NYHA) functional class. Secondary outcomes included daily sodium intake (in milligrams) and patient confidence in self-management of symptoms (scale: 0100). The key independent variable examined was literacy for which educational attainment (measured ordinally) served as a proxy. Contingency tables and Mantel- Haenszel chi-squared test statistics assessed whether the rate of improvement across outcome variables differed across educational strata. To determine whether the size of improvement varied by educational attainment, one-way ANOVA was employed. Logistic regression analysis assessed whether education had effects on outcomes net of gender, age and type of heart failure. Population Studied: Data were collected through telephone interviews, periodic clinic visits and a chart review conducted among a sample of 646 patients enrolled in the DM arm of a community-based study of CHF patients. Principal Findings: Education strongly influences improvement in sodium intake: 80% of patients who had completed some college coursework or better showed a decrease in daily sodium intake while only 69% of patients with a high school degree or less reduced dietary sodium intake (p=.003). Differences in the magnitude of improvement in dietary habits were also apparent. The least-well-educated patients reduced their sodium intake by 505 milligrams daily while the patients with at least some college education reduced their intake by 734 milligrams daily (p=.001). For confidence in self-management of symptoms, approximately 52% of patients with at least a college degree reported feeling more confident about managing their disease while 43% of patients with a high school degree or less felt more confident (p=.008). The difference in the magnitude of improvement was modest: the less-well-educated group added 2.2 points on the confidence scale compared to the 2.6 points added by the better educated (p=ns). In multivariate analyses, education was a statistically significant predictor of both decreased sodium intake as well as improved self-confidence, net of controls. No statistically significant relationships were observed between education and primary study outcomes including mortality, time to first emergency department visit, rates of health care utilization and improvement in NYHA functional class. Conclusions: These results suggest that literacy, as measured by educational attainment, has an important impact on the secondary, but not primary, goals of a disease management program for CHF patients. Implications for Policy, Delivery or Practice: Those who provide disease management services to the chronically ill may be able to further improve important clinical and patient satisfaction outcomes by paying special attention to literacy levels, and education more generally. Primary Funding Source: Direct federal appropriation • Is Managed Care Superior to Traditional Fee-For-Service among HIV-Infected Beneficiaries of Medi-Cal? David Zingmond, M.D., Ph.D., Susan Ettner, Ph.D., William Cunningham, M.D., M.P.H. Presented by: David Zingmond, M.D., Ph.D., Visiting Assistant Professor of Medicine, Division of General Internal Medicine and Health Services Research, UCLA School of Medicine, 911 Broxton Plaza, Los Angeles, CA 90095-1736; Tel: 310.794.0786; Fax: 310.794.0732; E-mail: dzingmond@mednet.ucla.edu Research Objective: Medicaid is the single largest payer for healthcare services for HIV-infected Americans. Since the 1997 Balanced Budget Amendment, Medicaid has encouraged the adoption of managed care approaches to control costs. The adoption of managed care for HIV-infected Medicaid enrollees has been controversial with primary concerns for maintaining access to HIV specialists and initiation of effective HIV treatments. Little is known regarding the relative success or failure of such programs. California’s Medicaid program (Medi-Cal) has instituted mandatory and optional managed care enrollment on a county-by-county basis. The goal of this study was to examine whether HMO enrollment impacted use of antiretroviral therapy, hospitalizations, and mortality among Medi-Cal beneficiaries. Study Design: Retrospective longitudinal study of Medi-Cal beneficiaries with HIV/AIDS. We used linked Medi-Cal enrollment files, Medi-Cal claims, hospital discharge abstracts from the Office of Statewide Health Planning and Development, death records, and California AIDS Registry records to perform patient level analysis of mortality, disease progression (AIDS or death), hospitalization, and use of highly active antiretroviral therapy (HAART) among HIV-infected Medi-Cal enrollees. Multivariate probit analyses predicting the impact of HMO-enrollment on outcome controlled for patient demographics and disease characteristics. In order to account for unmeasured severity, sensitivity analyses using a treatment selection model (e.g. bivariate probit) based upon county Medi-Cal enrollment policy were performed. Relative risks were based upon model predictions with confidence intervals estimated by bootstrap. Population Studied: Medi-Cal beneficiaries with HIV/AIDS enrolled in Medi-Cal as of January 1999 and with continuous enrollment til January 2002 or death. Principal Findings: A total of 22,761 HIV-infected patients were enrolled continuously from January 1, 1999 til death or the end of the observation period. Of these, 3,183 (14%) were enrolled at study entry in a Medi-Cal HMO, and the remainder in traditional FFS Medi-Cal. By county, 6.9% of enrollees resided in counties with primarily mandatory HMO enrollment, 85.3% were in counties with optional HMO enrollment, and the remainder lived in rural counties without HMOs. Enrolled patients were heterogeneous by gender (70% male), race (43% white, 28% black, 19% Latino, 3% Asian, and 8% other/unknown), age (8% < 30 years, 68% between 30 and 49, and 24% 50 and older), and disease stage (51% with confirmed AIDS). Among AIDS patients at baseline, 54% were receiving HAART and 86% were receiving some kind of antiretroviral therapy (19% and 44% respectively for non-AIDS patients). By the end of 2001, 18% of AIDS patients and 9% of non-AIDS patients had died. For both groups of patients, HAART use at baseline was less likely for HMO-enrolled patients (AIDS patients: relative risk (RR) 0.85, 95% confidence interval (CI) 0.79 to 0.92 and non-AIDS patients: RR 0.77, 95% CI 0.67 to 0.91). HMO-enrollment did not predict differences in three-year mortality or hospitalization. Using treatment selection models, HMOenrollment was not associated with any differences in medication use or outcomes for AIDS or non-AIDS patients. Inclusion of patients with non-continuous enrollment does not impact these results. Conclusions: Managed care models for the care of Medicaid enrollees infected with HIV have similar outcomes as traditional Medicaid Fee-For-Service models in California when a separate HIV drug benefit is provided. Other aspects of care, including overall cost, patient satisfaction, and access to outpatient specialty care should also be considered as factors in deciding whether managed care models should be adopted for the care of HIV-infected enrollees in Medicaid. Implications for Policy, Delivery or Practice: The adoption of managed care approaches for chronically ill Medicaid populations can be as clinically effective as those in traditional FFS Medicaid. Wholesale adoption of a managed care approach should thus be based on alternative considerations, such as cost, satisfaction, and longer term outcomes. Primary Funding Source: UCLA Center for AIDS Research Related Posters Poster Session B Tuesday, June 8 • 7:30 a.m.-8:45 a.m. • Patient-Provider Communications Regarding Self-Care Management During Medical Encounters: A Contextual Assessment Framework Nedal Arar, Ph.D., Juan Rosales, MA, Jackie Pugh, M.D. Presented by: Nedal Arar, Ph.D., Ass. Professor, Medicine, UTHSCSA, SA, TX 78229-3900; Tel: 210.567.0075; Fax: 210.567.4423; E-mail: ararn@uthscsa.edu Research Objective: Self-care management (SCM) support is an essential element for achieving high-quality chronic illness care. Effective communication between providers and patients remain at the center of health-care delivery. Our objectives are to (1) describe the content and the process of patientphysician exchanges regarding SCM during outpatient primary care encounters, (2) develop and test a tool to asses the intensity of these exchanges, and (3) develop a framework that considers the improvement of patient-provider communications regarding SCM. Study Design: Cross-sectional, observational study design. Methods: 50 encounters involving six physicians at a Veterans Health Care System in SA, TX. were videotaped, coded, and analyzed for verbal content and process related to SCM. Content analysis of these observations focused on patientphysician exchange regarding: awareness of symptoms associated with a chronic illness and its complications, monitoring activities (e.g. home glucose monitoring), use of medications, management of emergencies, diet, exercise, alcohol use, cigarette smoking, family support, and management of illnesses’ psychosocial impact Data analysis included both qualitative and quantitative approaches using Atlas.ti and SPSS 9.0 software packages respectively. Population Studied: Outpatient Veterans Principal Findings: The average length of the encounter was 22.6 minutes, (range: 5-47, SD=8.9). The average number of patient visits observed per physic was 8 (range: 3-12, SD=3.2). The most common disease observed was diabetes (22, 44%), followed by heart diseases (9, 18%), hypertension (8, 16%), depression (6, 12%) and cancers (5, 10%). 35% (18) had one disease, 14 (27%) two, 11 (22%) between 3 and 6 diseases. We found that issues pertaining to different facets of self-care management were discussed in every physician-patient interaction. The total number of complete exchanges regarding self-care management topics in all the 50 encounters was 484. The highest number of SCM exchanges discussed was related to medication (195, 40.3%), followed by disease symptoms (79, 16.3%), diet (58, 12%), exercise (47, 9.7%), monitoring activities (44, 9.1%), smoking (20,4.1%) and family support (19, 3.9%). Community resources (30, 0.6%), management of emergencies (5, 1%) and drinking (8, 2.9%) were the least discussed issues. Using the Third Party Assessment-Self-care Management (TPA-ScM) tool, we measured the intensity of SCM communication between patients and their physicians. Weighted kappa was calculated using SAS (SAS Institute, Cary, NC) software, and it was based on a four point ordinal scale: (0) indicated the evaluator perceived that the item was not discussed (least desirable); (1) indicated that item discussion was considered poor; (2) indicated that item discussion was considered adequate; and (3) indicated that item discussion was considered exceptional. The overall Kappa for all subscales = 0.75. Patient-physician exchanges regarding SCM were found to be barely adequate (patients score= 1.9, physicians score=2). We also present a new analytical framework: Contextual Assessment Framework (CAF) that has informed the content analysis presented herein. This framework allows for comparing patients’ and physicians’ questions and responses exchanged during the encounters concerning SCM. It views the patients as being active in giving and receiving feedback on their progress, and physicians as being instrumental in helping patients within the context of patients’ experiences with chronic illnesses. Conclusions: In any given encounter, only a few aspects of SCM were emphasized. Patient-physician exchanges regarding SCM were barely adequate. The CAF contrasts patients’ and providers’ concepts of illnesses, and considers the improvement of communications within the dynamic process of clinical interactions. Implications for Policy, Delivery or Practice: Improving SCM will enhance patients’ centeredness and foster a highquality chronic illness management. Further studies evaluating the impact of patient-centered approach on improving the care for chronically ill patients is justified. Primary Funding Source: VA • Are Clinical Measures of Quality Related to Consumer Satisfaction and Reported Experience with Care? An Analysis of Diabetic Medicare Beneficiaries in Medicare Fee-for-Service Shulamit Bernard, Ph.D., R.N., Erica Brody, M.P.H., Celia Eicheldinger, M.S. Presented by: Shulamit Bernard, Ph.D., R.N., Director, Program on Health Care Quality and Outcomes, Health Quality Program, RTI International, 3040 Cornwallis Road, Research Triangle Park, NC 27709; Tel: 919.485.2790; Fax: 919.990.8454; E-mail: sbernard@rti.org Research Objective: To examine whether consumer reports and ratings of health care are correlated with clinical indicators of quality. Study Design: We used data from the 2000 National Medicare Fee-for-Service (MFFS) CAHPS® survey, conducted for the Centers for Medicare and Medicaid Services (CMS). The sample of beneficiaries, drawn from a sampling frame constructed from the CMS Enrollment Data Base (EDB) resulted in 103,551 (64%) completed surveys. MFFS survey data was merged with 1999-2001 Medicare claims data. This analysis includes 16,532 diabetic beneficiaries identified by ICD 9 codes. Using ICD-9 and CPT codes, and data from the twelve months preceding the survey response date, we constructed 4 clinical indicators of quality including eye exam, physiological test (including hemoglobin A1c, microalbumin, and cholesterol), diabetic education and self blood glucose monitoring, and disease progression. In addition, estimated case-mix adjusted means for 5 CAHPSTM measures, were constructed using the CAHPS Macro version 3.4. The casemix adjusted means were stratified by the clinical quality indicators and two-sample tests for mean differences were performed. Due to large sample sizes the Gaussian distribution was assumed. Population Studied: Diabetic beneficiaries enrolled in Medicare fee-for-service during 2000. Principal Findings: We found no differences in mean CAHPS scores among beneficiaries experiencing disease progression. Having a diabetes-related physiological exam (such as Hemoglobin A1c) is associated with higher mean CAHPS scores for the three composites estimated (Getting Care Quickly, Good Communication, and Getting Needed Care) as well as the two ratings estimated (Rate Plan and Rate Health Care). Beneficiaries having an eye exam report higher mean scores for the two ratings and the getting needed care composite while the self care indicator is associated with higher plan ratings but no other CAHPS measure. Conclusions: Our findings suggest that overall, diabetic beneficiaries receiving preventive services are more likely to report higher levels of satisfaction and better experience with the Medicare program. Diabetic beneficiaries experiencing worsening of their disease do not differ in their reports of satisfaction or experience suggesting that they do not attribute disease progression to availability of services or the plan performance. Implications for Policy, Delivery or Practice: The findings suggest that, among a chronically ill population, subjective ratings and reports are correlated with quality of care as demonstrated by process measures. Further, this analysis suggests that ratings and reports are a direct result of the quality of care received and may be used to monitor clinical quality as well as satisfaction and experience with care. Primary Funding Source: CMS • Disease Management Success Stories: Chronic Disease Management in Uninsured, Underserved and Rural Populations. Jane Nelson Bolin, Ph.D., J.D., R.N., Larry Gamm, Ph.D., Donna Zazworsky, R.N., M.S., Michael Reis, M.D., Paul Shelton, Ph.D., Bita Kash, M.B.A. Presented by: Jane Nelson Bolin, Ph.D., JD R.N., Assistant Professor, Health Policy & Management, Texas A & M School of Rural Public Health, 3000 Briarcrest Avenue, Suite 310, Bryan, TX 77802; Tel: 979.862.4238; Fax: 979.862.8371; E-mail: jbolin@srph.tamushsc.edu Research Objective: To identify and examine outcomes of chronic diabetes disease management efforts in uninsured, underserved, and rural populations. Study Design: Disease management outcomes data from health plans offering Diabetes Disease Management in Arizona, Texas and Illinois are examined. Statistical comparisons and analyses are conducted to examine both clinical and financial outcomes of diabetes disease management members of the individual health plans. Key dependent variables are (1)) Key laboratory tests acquired; (4) Key exams performed; (5) Changes in costs for in-patient charges, (6) Changes in total costs per-member per-year (PMPY) and (7) Differences in outcomes across urban and rural patient populations. Population Studied: Adult participants of Diabetes Disease Management programs in health plans in Arizona, Texas and Illinois. Principal Findings: In Arizona’s DM program for the uninsured key clinical measures and exams were obtained routinely, and a majority of the time, with improvement noted in outcome measures for HgbA1c, LDL, urine proteins and other key indicators. Health Plans in Texas and Illinois saw significant improvement in both patient-level clinical indicators as well as a reduction in patient costs. These health plans serve underserved, uninsured and rural patients. Conclusions: Diabetic disease management resulted in improvement of key clinical and patient level indicators as well as improved financial indicators such as in-patient costs and overall per-member per-year costs. Implications for Policy, Delivery or Practice: Managed care plans, community health systems and private or public insurers can cost-effectively support the treatment needs in diabetic patients in underserved, uninsured and rural populations. Primary Funding Source: HRSA, Office of Rural Health Policy • Use of Complementary and Alternative Medicine Practitioners By People with Physical Disabilities: Estimates from a National Survey Matthew Carlson, Ph.D., Gloria Krahn, Ph.D., M.P.H., Phillip Beatty, M.A. Presented by: Matthew Carlson, Ph.D., Assistant Professor, Sociology, Portland State University, P.O. Box 751, Portland, OR 97207; Tel: 503.725.9554; Fax: 503.725.3957; E-mail: carlsonm@pdx.edu Research Objective: To estimate the prevalence and determine symptoms and reasons for CAM practitioner use among insured adults with physical disabilities. Study Design: Panel survey data collected in 2000 and 2001. Estmates are based on cross-sectional analysis of the 2001 survey and bivariate analyses of CAM practitioner use among people with physical disabilities. Population Studied: 830 persons with physical disabilities obtained through a multi-modal sampling technique including a random sample of members of disability organizations (51%), a purposive sample recruited through disability publications, websites, and provider practices, (40%), and a snowball sample (9%). Principal Findings: CAM practitioners were used by 19% of the sample. CAM use was more prevalent among women than men (24% vs. 10%), in the Western US (30%) compared to the Midwest (20%) Northeast (14%), and South (10%) and among prior users (62%) compared to non-users (8%). Common symptoms treated were pain (80%), decreased functioning (43%), and lack of energy (24%). Common reasons for using CAM practitioners included lifestyle choice (67%) and because they are more effective (44%). Conclusions: People with physical disabilities are a heterogeneous group who use CAM modalities at similar or higher rates than the general population, for similar symptoms, and for reasons similar to the general population. Implications for Policy, Delivery or Practice: Results from the current survey suggest that CAM treatments represent a substantial proportion of the medical care obtained by Americans with chronic health conditions and highlight the need for more consistent regulation as well as integration with traditional medicine. Primary Funding Source: US Department of Education, National Institute on Disability and Rehabilitation Research • Comorbid Physical Conditions and Quality of Depression Care Among Elderly Medicare Beneficiaries Usha Sambamoorthi, Ph.D., Stephen Crystal, Ph.D., Wenhui Wei, M.A., M.S., Mark Olfson, M.D., Stephen Crystal, Ph.D. Presented by: Stephen Crystal, Ph.D., Research Professor, Institute for Health, Health Care Policy, and Aging Research, Rutgers University, 30 College Avenue, New Brunswick, NJ 08901; Tel: 732.932.8579; Fax: 732-932-8592; E-mail: scrystal@ihhcpar.rutgers.edu Research Objective: This study evaluates the relationship between comorbid physical conditions and depression care among elderly persons using eight years of a large, nationally representative survey of Medicare beneficiaries. Study Design: We used merged survey and Medicare claims data from the Medicare Current Beneficiary Survey. The elderly with diagnosed depression were identified on the basis of ICD-9-CM codes recorded in health care claims. Pharmacological treatment for depression was derived from detailed self-reports of prescribed medication use and psychotherapy for depression was identified from Medicare claims. Population Studied: Medicare beneficiaries aged 65 and over living in the community, enrolled in fee-for-service Medicare throughout the year. Principal Findings: Rates of diagnosed depression were positively associated with increasing levels of physical comorbidity overall and for all examined subgroups. However, among those diagnosed with depression, treatment for depression was not related to level of physical comorbidity. Conclusions: These findings call into question the concept that concurrent general medical conditions tend to impede the management of depressive disorders. Implications for Policy, Delivery or Practice: Access to specialty care treatment needs to be expanded for elderly with concurrent physical illness and depression. Primary Funding Source: NIMH • Patient Adherence: Lessons from Five Decades of Research Robin DiMatteo, Ph.D. Presented by: Robin DiMatteo, Ph.D., Professor, Psychology, University of California, 900 University Avenue, Riverside, CA 92508; Tel: 909.787.5734; Fax: 909.787.3985; E-mail: robin@ucr.edu Research Objective: A major limiting factor in the success of chronic care delivery involves the reluctance of patients to accept and follow through with recommendations from their physicians and other health professionals. The literature on patient adherence is very extensive, and although only about 10 percent of the published papers on this topic are empirical articles, there are over 1000 studies. Summarizing what we currently know about the causes and consequences of nonadherence requires an analysis of the entire adherence literature, and the building of data-driven models from metaanalyses. Issues of measurement are critically important, as well. Researchers and clinicians have devised various strategies for assessing patient adherence, yet how these methods relate to each other, whether they over- or underestimate adherence, and how various factors affect adherence research results need to be examined. Study Design: This paper presents a coherent, data-driven model of the results of multiple meta-analyses of the entire literature on predictors, outcomes, and measurement of patient adherence to chronic disease regimens. Moderating variables included definitions of adherence, specific regimens and diseases of concern, and methods of adherence measurement. Population Studied: All empirical articles on adherence published in peer-reviewed, English language journals from 1948 through 2002 were included. Studies examined adherence to exercise, diet, medication, health related behavior, screening, vaccination, and appointments (prescribed by a nonpsychiatrist physician). Each article was coded according to: recency, disease condition of patient sample; illness severity and health status; type of adherence measurement method; type of treatment or recommendation requiring adherence; operational definition of adherence; sample size; percentage of patients adhering for each method of adherence assessment, and “r” (correlation) effect size between methods of adherence assessment, as well as between adherence and the following variables: physician humanistic and communication skill, patient beliefs, anxiety, depression, practical and emotional social support, family cohesiveness, and family conflict, and the outcome of medical treatment Principal Findings: Adherence to treatment relates significantly to treatment outcomes. Adherence is positively predicted by physician humanism, and by patients’ efficacy beliefs, family cohesiveness, and social support. Adherence is negatively predicted by family conflict and patient depression. Conclusions: The strong effects in this research suggest that in the context of limited resources, patient adherence to chronic disease regimens can best be achieved by improving health professional-patient communication and by insuring that patients believe in the necessity and efficacy of treatment, and have adequate support for adherence. Screening for, and reducing, patient depression and family conflict likely can improve patient adherence. Implications for Policy, Delivery or Practice: Estimates suggest that nonadherence costs the US health care system several hundred billion dollars per year. Interventions to improve adherence should be targeted to factors that are known, from quantitative reviews of adherence research, to relate to adherence with strong effects sizes. Primary Funding Source: AHRQ • Use of COX-2 Nonsteroidal Anti-Inflammatory Drugs in Ambulatory Care, 2000-2001 Sheila Franco, Alan Cohen, M.A., Amy Bernstein, Sc.D. Presented by: Sheila Franco, Staff Fellow, National Center for Health Statistics, 3311 Toledo Road, Hyattsville, MD 20782; Tel: 301.458.4331; Fax: 301.458.4037; E-mail: sfranco@cdc.gov Research Objective: Since 1999, a new class of nonsteroidal anti-inflammatory drugs (NSAIDs) has been introduced, the so-called COX-2 NSAIDs. COX-2 NSAIDs are similar in efficacy to traditional NSAIDs but were believed to have a lower incidence of gastrointestinal side effects than traditional NSAIDs. COX-2 drugs are also among the most heavily marketed and are generally more expensive than traditional NSAIDs. This paper examines the use of COX-2 NSAIDs in ambulatory care visits by age, sex, and selected diagnoses. Study Design: Using data from the National Ambulatory Medical Care Survey (NAMCS) and National Hospital Ambulatory Medical Care Survey (NHAMCS) Hospital Outpatient Department Component, visit records were examined to determine NSAID and COX-2 NSAID visits. Visit records include up to six prescription and non-prescription drugs ordered or continued during the ambulatory care visit. Bivariate analyses and multivariate logistic regressions were used to determine the predictors of the use of a COX-2 NSAID among NSAID visits. Population Studied: Visits by persons age 18 and over to U.S. office-based physicians’ practices (NAMCS) and hospital outpatient departments (NHAMCS) are included. Data years 2000 and 2001 are combined. Principal Findings: In 2000-01, COX-2 NSAIDs accounted for 45 percent of NSAID ambulatory care visits among adults 18 years and older, almost equaling the use of traditional NSAIDs. The use of COX-2 NSAIDs increases with age. For visits for those aged 18-44, 29% of NSAID visits were for COX2, compared with 46% for those aged 45-64, 58% for those 6574, and 62% for those 75 and older. Patients with rheumatoid (RA) or osteoarthritis (OA) often take NSAIDs on a long-term basis, and therefore may be more prone to gastrointestinal side effects. COX-2 use was more prevalent among visits with a recorded diagnosis of rheumatoid or osteoarthritis, with 61% of NSAID visits with an OR or RA diagnosis including a COX-2, compared to 43% of those without such a diagnosis recorded. Logistic regression controlled for the effects of age, sex, race, and a diagnosis of rheumatoid or osteoarthritis. Age and a diagnosis of rheumatoid or osteoarthritis remained significant predictors in the multivariate analysis of having a COX-2 NSAID prescribed during an NSAID visit. Men were more likely than women to have a COX-2 prescribed, after controlling for other factors. Race was not significant predictors of COX-2 use. Conclusions: Since the introduction of the first COX-2 NSAIDs, they have dominated the market. COX-2 NSAID use increases as age increases and is more common for men and for patients with a diagnosis of rheumatoid or osteoarthritis. Implications for Policy, Delivery or Practice: COX-2 NSAIDs were heralded when introduced because it was believed they offered analgesic and anti-inflammatory relief with fewer gastrointestinal side effects. While some NSAID users do develop GI complications, it is a small proportion of all patients. Further, as COX-2 drugs are more widely used, the evidence of their lower incidence of side effects has been mixed and controversial. It is unclear if the increased use of COX-2 NSAIDs is warranted given their substantially higher cost. • Diabetes Care Management Participation in a Primary Care Setting and Subsequent Hospitalization Risk Anthony Greisinger, Ph.D., Rajesh Balkrishnan, Ph.D., Rahul Shenolikar, M.S., Oscar Wehmanen, M.S., Shahid Muhammad, M.D., P. Kay Champion, M.D. Presented by: Anthony Greisinger, Ph.D., Vice President for Research and Development, Kelsey Research Foundation, 7800 Fannin, Suite 209, Houston, TX 77054; Tel: 713.442.1214; Fax: 713.442.1229; E-mail: ajgreisinger@kelsey-seybold.com Research Objective: There exists scant evidence examining the impact of participation in primary care diabetes management programs and their educational components on the risk of subsequent significant patient morbidity. This study examined the association between participation in a diabetes management program in a primary care setting, and the risk of subsequent hospitalization. Study Design: In this cohort study, information in the year preceding the hospitalization was obtained on several demographic, clinical, and diabetes care management participation related variables. Multivariate logistic regressions were used to examine the relationship between primary care diabetes management participation, as well as individual educational components on the likelihood of subsequent-year hospitalization. Population Studied: 10,980 patients with diabetes mellitus receiving some type of treatment in a large primary care clinic network in Houston, TX were examined for incidence of hospitalization in the year 2002. Principal Findings: Patients participating in some type of primary care diabetes management were 16% less likely to have an incidence of hospitalization (p=0.05). When individual educational components of the diabetes care management program were examined, diabetes education sessions were more beneficial than certified diabetes educator visits in reducing the incidence of hospitalization. Patients with controlled blood glucose levels and a diabetes education session seemed to have the most significant hospitalization risk reduction (Odds ratio (OR) =0.62, 95% CI: 0.40, 0.95). Conclusions: There seems to be beneficial effects associated with participation in primary care diabetes management programs in terms of reduced hospitalization risk. Implications for Policy, Delivery or Practice: Attendance in diabetes educational sessions in primary care settings coupled with maintenance of blood glucose control seems to be associated with greatest risk reduction. Primary Funding Source: Kelsey Research Foundation • A Qualitative Assessment of Best Practice Implementation for Diabetes Management in Primary Care Bryan Weiner, Ph.D., Christian Helfrich, M.P.H., Lucy Savitz, Ph.D., M.B.A., Kathleen Swiger, M.S., M.P.H., Christian Helfrich, M.P.H. Presented by: Christian Helfrich, M.P.H., Doctoral candidate, Health Policy and Administration, University of North Carolina at Chapel Hill, CB #7411, Chapel Hill, NC 27599-7411; Tel: 919.968.6150; E-mail: helfrich@unc.edu Research Objective: To examine how physician practices adopt and implement strategies for Type 2 diabetes management (DM). In particular, we explored how organizational factors and strategy characteristics affect adoption and implementation processes. Study Design: Replicated, holistic case studies, using qualitative interviews and quantitative surveys. Population Studied: Six physician group practices purposively sampled from a survey of 166 primary care physicians affiliated with managed care organizations in the state of North Carolina who provided care to ten or more privately ensured diabetes patients in 2001. Principal Findings: Two distinct phases were observed: 1) adoption and 2) implementation. The adoption phase included an "agenda setting" stage where parameters were established for searching for and evaluating the DM strategy, and a "matching" stage where the strategy was compared with the organization's needs. The implementation phase included a "redefining/restructuring" stage, where both the organization and the strategy were mutually adapted and a "routinizing" stage where the strategy ceased to have a distinct identity and simply became part of the routine way things were done. All sites reported a routine forum for identifying problems, opportunities, and strategies for improving diabetes care. In some cases, a "performance gap" triggered the search for a new strategy, and in all cases sites engaged in opportunistic surveillance rather than routine, comprehensive scanning. Sites did not vary in terms of the external sources of information considered in the adoption of new DM strategies; and all sites reported using their own practice experience to “reality test” information gathered from external sources. In all cases, the DM strategies underwent considerable adaptation after they were adopted. Even “fixed” innovations, such as an in-office HbA1c testing machine, were adapted as physicians defined the appropriate frequency of testing and optimal range of values for diabetes management. Cases that succeeded in routinizing their DM strategy made lasting changes to organizational policies and procedures concerning factors such as appointment scheduling, office workflow, and documentation. They did not require institutional incentives or punitive measures. Conclusions: A reasonably consistent innovation process was observed across the six cases, which matches well with organizational theory and previous empirical studies. While a great deal of variation exists within the general process, several specific factors emerged that may help other efforts aimed at adopting and implementing innovative strategies in primary care settings. Routine forums for identifying problems, local tailoring, and ease of administration are shared attributes of successful interventions. Further, an innovation champion is essential for implementation of the strategy. Implications for Policy, Delivery or Practice: Understanding the adoption and implementation process can help researchers and policy makers identify key points for delivering support to promote adoption and implementation of evidence-based strategies. Primary Funding Source: CDC • Adherence to Clinical Guidelines for End Stage Renal Disease Anemia Management: Implications for Cost and Quality of Care Denise Hynes, R.N., M.P.H., Ph.D., Kevin Stroupe, Ph.D., James Kaufman, M.D., Domenic Reda, Ph.D., Amy Peterman, Ph.D., Margaret Browning, Ph.D. Presented by: Denise Hynes, R.N., M.P.H., Ph.D., Senior Health Scientist, Midwest Center for Health Services and Policy Research, Edward Hines, Jr VA Hospital, P.O. Box 5000 (151V), Hines, IL 60141; Tel: 708.202.2413; Fax: 708.202.2415; E-mail: hynes@research.hines.med.va.gov Research Objective: Patients with end-stage renal disease (ESRD) require chronic dialysis to replace lost kidney function, using substantial healthcare resources. A costly component of ESRD care is anemia management with erythropoietin (EPO). National Kidney Foundation (NKF) clinical practice guidelines recommend that EPO be administered subcutaneously (SC) rather than intravenously (IV). Since reimbursement for EPO differs for federal vs. private-sector dialysis centers we hypothesize different use patterns by facility type. Using data from a multi-site prospective observational study of patients with ESRD, 1) we examined how well this guideline was followed for hemodialysis patients in VA or private-sector facilities; and 2) we determined implications of following this recommendation for EPO dose, cost, and anemia management. Study Design: 1) We determined route of EPO administration monthly over 6-12 months of patient follow-up and compared the proportion of patients receiving SC versus IV administration based on predominant route. 2) We compared EPO dose for patients receiving predominantly SC EPO versus IV, adjusting for baseline factors (age, race, comorbidities, months on dialysis, baseline hemoglobin); we compared average yearly EPO cost per patient for SC versus IV administration, using the Medicare reimbursement rate of $8/1000 units of EPO; we assessed anemia management by comparing hemoglobin at closeout for patients receiving SC EPO versus IV. Population Studied: 332 ESRD patients receiving hemodialysis enrolled in a study from 2001-2003. Principal Findings: Of the 332 patients 183 received dialysis in a VA facility and 149 in a private-sector facility. We found greater adherence to the clinical guideline in VA facilities. SC route of administration was used predominantly for 53% of patients in VA facilities (97 patients) versus 16% in privatesector facilities (24 patients) (p < 0.001). Average weekly dose was 35% lower for patients receiving SC EPO compared to IV, adjusting for baseline clinical factors: 13,789 units for SC (95% CI: 7,842 to 19,737) versus 21,064 for IV (95% CI: 15,660 to 26,467) (p < 0.01). Average weekly SC dose (adjusting for clinical factors) did not differ between VA and private-sector facilities (p = 0.91) nor did IV dose (p = 0.75). The average yearly EPO cost per patient (adjusted for clinical factors) was $3,027 lower for patients receiving SC EPO: $5,736 for SC versus $8,763 for IV. Closeout hemoglobin was not different between SC and IV groups: 11.85 gm/dL for both groups. Conclusions: We found greater adherence to the NKF guideline recommending SC use for administration of EPO among patients treated at VA facilities compared to the private sector. By following the guideline, we estimate that facilities could use 35% lower doses at a savings of $3,027 per patient annually without compromising anemia management. However, overall adherence to this guideline is low. Implications for Policy, Delivery or Practice: Given the high costs of ESRD care, it is important to determine where costs can be saved without compromising patient care. The NKF recommendation for SC EPO was found to provide cost savings without impacting anemia management. Future research should investigate whether there are other clinical outcomes associated with the use of SC administration of EPO that might augment or offset these findings. Primary Funding Source: VA • Medication Related Factors Affecting Health Care Outcomes and Costs in Patients with Psoriasis Rajesh Balkrishnan, Ph.D., Amit Kulkarni, M.S., David Richmond, M.S., Daniel Pearce, M.D., Steven Feldman, M.D., Ph.D. Presented by: Amit Kulkarni, M.S., Doctoral Student and Graduate Research Assistant, Management, Policy,and Community Health, University of Texas School of Public Health, 1200 Herman Pressler, Suite E-331, Houston, TX 77030; Tel: 713.500.9181; Fax: 713-500-9171; E-mail: akulkarni@sph.uth.tmc.edu Research Objective: Psoriasis is one of the most common skin diseases. Owing to its non-life threatening nature, psoriasis is not considered as serious as many other medical conditions. However, the degree of morbidity faced by these patients has been shown to be comparable to other major chronic diseases. Approximately $1.6 to $3.2 billion is spent annually in the United States for treatment of psoriasis, a large portion of it on controller medications. Patients suffering from psoriasis have low health status and a constant cost associated with the treatment of psoriasis owing to its chronic and recurring nature. This study examined the relationship between factors related to medication use and associated health status and costs associated with the treatment of psoriasis in the United States. Study Design: Cross sectional cohort study using the 2000 United States Medical Expenditure Panel Survey (MEPS) Database. Estimates of health care service utilization and costs, and demographic and clinical patient variables were obtained from the database files. Self-reported health status in the MEPS is measured using the EuroQoL (EQ-5D) instrument. Population Studied: Data for approximately 1.1 million patients (weighted sample size) with psoriasis in the 2000 MEPS database was analyzed using multivariate weighted analyses. Principal Findings: Medications accounted for nearly 50% of the psoriaisis-specific health care costs in patients. The average number of annual psoriasis prescription refills was 3.8. 57.1% of patients were being treated with topical corticosteroids, 27.5% with other medications, and 15.4% were not receiving any pharmacological treatment. The multivariate models examining predictors of health care costs and health status (EQ-5D summary score) explained 61% and 50% of the variance respectively. Among medication-related factors, use of topical corticosteroid therapy was associated with a decrease in psoriasis-specific health care costs (60% lower costs among users compared to non users, p=0.036) and better health status (29% improvement in EQ-5D summary scores among users compared to non users, p=0.004). The use of other medications was not associated with any significant reduction in costs or improvements in health status compared to patients receiving no pharmacological treatment. Increased psoriasis prescription refill rates were associated with an increase in psoriasis-specific health care costs (p<0.001). Conclusions: Use of controller medications such as topical corticosteroids is the most important driver of reduced health care costs and improved health status in patients with psoriasis. Prescription costs are an important component of total psoriasis-specific health care costs. There seems to be a differential beneficial impact of topical corticosteroids compared to other medications for treatment of psoriasis on health care outcomes and costs. Implications for Policy, Delivery or Practice: Controller medication use is an important cornerstone of successful psoriasis management. The availability of many inexpensive topical corticosteroids should encourage payers and physicians to encourage increased adoption of controller medications in order to decrease patient costs, and improve patient outcomes. Primary Funding Source: The Center for Dermatology Research is funded by a grant from Galderma Inc. • Modifying the SF-36V Physical Functioning Scale For Use with Persons with SCI Stephen Luther, Ph.D., Debra Rosenberg, Ph.D., Jeffery Kromrey, Ph.D., Gail Powell-Cope, Ph.D., AR.N.P, Audrey Nelson, Ph.D, R.N., Patricia Quigley, Ph.D., R.N. Presented by: Stephen Luther, Ph.D., Evaluation Methodologist, Measurement & Evaluation Team, Veterans Integrated Services Network 8, 11605 North nebraska Avenue, (118M), Tampa, FL 33612; Tel: 727.580.7477; Fax: (813) 5583990; E-mail: steve.luther@med.va.gov Research Objective: The purpose of this study was to modify the SF-36V Physical Functioning (PF) Scale for use with Spinal Cord Injured veterans. Study Design: The project consisted of two phases. In the first phase a focus groups were conducted with veterans with SCI and their caregivers to identify alternative wording for SF-36 PF items that might be comparable to items that are worded inappropriately (i.e. "Climbing one flight of steps") for persons with SCI. The pool of alternative items was then included with the original SF-36 items, measures of activities of daily living, Information about level of injury, information about physical functioning, and demographic information in a written questionnaire. After pilot testing the questionnaire was mailed to all persons with SCI who have the James A. Hailey Veterans Medical Center as their medical provider (n=787). Approximately 400 usable questionnaires were obtained through this process. We employed Item Response Theory strategies (as recommended by Ware) to compare the psychometric properties of the original SF-36V items and the new SCI sensitive items. The characteristic of the new items across varying levels of function is also explored. Finally convergent and divergent validity of the resultant scales are described. Population Studied: A cross sectional survey of all veterans with SCI that receive their care at the James A. Hailey Veterans Medical Center as their medical home (n=787). Principal Findings: Equivalent items employing wording appropriate for persons with SCI were identified. A discussion of modification to the scales to be appropriate for persons with different levels of injury and function will be described. Conclusions: A set of items with comparable psychometric properties to those on the original PF scale but being more appropriate for persons with SCI was identified. Implications for Policy, Delivery or Practice: The SF-36V is widely used by the Veterans Administration Healthcare System monitor outcome of patient populations. A appropriately worded and psychometrically sound version of the SF-36V PF Scale will ensure that values for persons with SCI will comparable to those of other patients. Primary Funding Source: VA • Success of Implementation and Maintenance of Quality Improvement for Depression Lisa Meredith, Ph.D., Peter Mendel, Ph.D., Marjorie Pearson, Ph.D., Shin-Yi Wu, Ph.D., Emmett Keeler, Ph.D., Jurgun Unutzer, M.D., M.P.H. Presented by: Lisa Meredith, Ph.D., Senior Behavioral Scientist, Health, RAND Corporation, 1700 Main Street, Santa Monica, CA 90407-2138; Tel: 310.393.0411 Ext. 7365; Fax: (310)451-7004; E-mail: seidel@rand.org Research Objective: To describe the changes made and examine factors associated with the success of implementation, maintenance, and spread of practice-based quality improvement (QI) efforts to put promising new primary care practice models for depression into place locally. Study Design: Cross-sectional analysis of qualitative data coded from monthly progress reports completed throughout QI implementation and telephone interviews conducted with key team leaders 18 months following implementation. Implementation success was evaluated using measures of change activities, changes that teams rated a success, maintenance of changes, and spread of changes. Other variables evaluated were reported barriers and facilitators to change, and organization and community characteristics. Population Studied: We evaluated the QI process of 17 multidisciplinary QI teams (11 public community health centers and 6 private health care practices) participating in the Improving Chronic Illness Care and Institute for Healthcare Improvement's Breakthrough Series for depression in 2001. Principal Findings: Implementation of change activities was varied with some changes made by only 1 or 2 organizations (planned visits, community linkages) while other changes were made by all (proactive follow-up, patient education, patient registry, and patient management information systems). Organizations most commonly reported success for changes to delivery and information system changes (59% and 53%) and more sites sustained these changes over time (59% and 94%). Organizational structure and leadership support were the most common facilitators while staff resistance, time, and information technology were the most common barriers. Different strategies for success varied with different sets of barriers Conclusions: Despite the challenges associated with QI for depression, we observed broad success across 17 different multi-disciplinary teams. Implications for Policy, Delivery or Practice: Detailed findings about QI implementation such as these should be helpful in guiding future efforts to improve chronic illness care. Primary Funding Source: RWJF • How Often Do Patients with Chronic Illnesses Fail to Receive Recommended Monitoring for Their Conditions? James Reschovsky, Ph.D., Hoangmai Pham, M.D., M.P.H. Presented by: Hoangmai Pham, M.D., M.P.H., Senior Health Researcher, Center for Studying Health System Change, 600 Maryland Avenue, S.W., Suite 550, Washington, DC 20024; Tel: 202.554.7571; Fax: 202-484-9258; E-mail: mpham@hschange.org Research Objective: To measure the extent that patients diagnosed with common chronic conditions fail to receive regular monitoring by a physician or other health professional as recommended in prevailing clinical guidelines and to assess factors associated with the receipt of regular monitoring care. Study Design: The study uses nationally representative survey data from the Round 2 (1998-1999) Community Tracking Study Household Survey. For a set of prevalent chronic conditions, adult survey respondents were asked if they were ever diagnosed with the condition. Diagnosed patients were then asked if they saw a physician or other health professional for that condition during the previous two years. We identify chronic conditions for which regular monitoring (at least every two years) is recommended by prevailing clinical guidelines. The frequency of regular monitoring care is measured and patient, insurance, and delivery system factors are assessed in bivariate and multivariate analyses. Population Studied: Adults ever diagnosed with hypertension, hypercholesterolemia, or diabetes (n=15,592). Principal Findings: A significant number of diagnosed patients failed to receive regular care for their chronic conditions over the preceding two years: 39% for hypertension, 33% for hypercholesterolemia, and 15% for diabetes. Multivariate factors associated with greater monitoring generally are consistent across specific conditions: diagnosis with multiple conditions, poorer self-reported health status, greater age, African American race, self-reported risk aversion, not being a smoker, being insured (especially by Medicare), seeing the same provider at a usual source of care, and having a physician as the regular provider. Patients’ educational level was only associated with receipt of monitoring in bivariate analyses. Finally, patients who reported their regular provider was good at explaining things were more likely to get regular monitoring care. Conclusions: Large proportions of diagnosed patients fail to receive regular monitoring for chronic conditions, as recommended by clinical guidelines. Patient characteristics appear to be the most important factors, although continuity of care and proper patient education by providers also are also influential. Implications for Policy, Delivery or Practice: Failure to receive regular monitoring can potentially increase the seriousness of chronic conditions, resulting in extra morbidity, cost, and preventable hospitalization. We identify the types of patients that are at greatest risk of not receiving regular followup care for chronic conditions. Providers should target these patients with greater educational efforts. In addition, administrative systems that permit the making of appointments well into the future, systems to remind patients to make appointments at times recommended by clinical guidelines, and systems that remind patients to keep appointments that have been made could all contribute to greater compliance with guidelines for the treatment of chronic conditions. These are likely to be key components for successful disease management programs. Primary Funding Source: RWJF • Prescription Drug Benefit Dispensing Restrictions: A Barrier to Managing Chronic Conditions and Costs? Kathryn Phillips, Ph.D., Su-Ying Liang, Ph.D., Jennifer Haas, M.D., Brian Alldredge, Pharm.D., Marilyn Stebbins, Pharm.D. Presented by: Kathryn Phillips, Ph.D., Associate Professor of Health Economics and Health Services Research, School of Pharmacy & Institute for Health Policy Studies, University of California San Francisco, 3333 California Street, Box 0613, San Francisco, CA 94143; Tel: 415.502.8271; Fax: 415-502-0792; Email: kathryn@itsa.ucsf.edu Research Objective: Chronic disease management is a major issue for health care quality and costs. Adherence with longterm prescription drug regimens is central to disease management. Although it is known that many health plans limit prescriptions to a 30-day supply when filled at community pharmacies, there is virtually no research on dispensing patterns for these types of medications. The objective of this research was to examine dispensing patterns for five drug classes commonly prescribed for chronic conditions. Study Design: This study utilized data from the 1996 and 2000 Medical Expenditure Panel Survey. Drugs were chosen based on following criteria: (a) typically used for chronic conditions, (b) in most cases can be safely dispensed for more than 30 days, (c) have consistent dosing patterns, and (d) have variations by relevant populations: gender, age, and how continuously taken. Five drug classes were examined: anti-epileptic drugs (AED), beta -blockers (BB), hormone replacement therapy (HRT), oral contraceptive pills (OCP), and selective serotonin reuptake inhibitors (SSRI). Drug names and quantity dispensed were reviewed and categorized to indicate whether prescriptions were filled for <=30 days or > 30 days. We used chi-square tests to examine the associations of insurance, use of mail order, and individual characteristics with dispensing patterns. Population Studied: The study population contained a nationally representative sample with appropriate age and gender groups for the drug classes analyzed (both genders and all ages for AED and SSRI, ages 18+ for BB, female ages 50+ for HRT, female ages 18-35 for OCP). Principal Findings: Almost three-quarters of prescriptions for the drug classes examined were dispensed for 30 days or less in both 1996 and 2000. Among the five drug classes, the percentage of prescriptions dispensed for 30 days or less varied widely from 66%-67% (BB and HRT) to 82%/84%/86% (OCP, AED, SSRI) (p<.01). Individuals who were younger, non-White, less educated, uninsured or publicly insured, or with poorer access to care were more likely to obtain prescriptions for <=30 days. Conversely, individuals with Medicare coverage were more likely to obtain prescriptions for >30 days. However, among privately insured individuals, those with drug coverage were more likely to obtain prescriptions for <=30 days than those without coverage. The percentage of individuals who reported having ever used mail order services, which is the most commonly used method to obtain >30 day supplies, increased only slightly from 19962000 (from 8%-10%). Conclusions: Almost three-quarters of prescriptions for five commonly used drug classes for chronic conditions were dispensed for <=30 days. Individuals who are more disadvantaged were more likely to get prescriptions for <=30 days. Although there can be clinical and economic reasons to dispense drugs for <30 days in selected instances, dispensing > 30 day drug supplies is often more effective and less costly. Implications for Policy, Delivery or Practice: Our results suggest that dispensing restrictions are a potentially serious challenge to more effective and less costly care. These results have implications for debates over Medicare prescription drug benefits, as benefit structure appears to influence whether patients get <=30 day or > 30 day supplies. Further research is needed to consider the influence of dispensing restrictions and mail order prescription services on the costs and outcomes of care. Primary Funding Source: NCI, AHRQ • Measuring the Quality of Care in Indian Health Diabetes Education Programs Yvette Roubideaux, M.D., M.P.H., Carolyn Noonan, M.S., Jack Goldberg, Ph.D., Lorraine Prucha, M.P.H., Lorraine Valdez, R..N., M.P.A., CDE, Kelly Acton, M.D., M.P.H. Presented by: Yvette Roubideaux, M.D. M.P.H., Assistant Professor, Mel and Enid Zuckerman Arizona College of Public Health, University of Arizona, 500 N. Tucson Boulevard, #110, Tucson, AZ 85716; Tel: 520.318.7280; Fax: (520) 318-7017; Email: yvetter@u.arizona.edu Research Objective: The purpose of this study is to examine the relationship between the level of diabetes education program services and the quality of diabetes care. Study Design: Cross-sectional study of the quality of diabetes care among patients in the Indian Health Service. Diabetes programs were invited to participate in the IHS Integrated Diabetes Education and Care Recognition Program and rank the level of comprehensiveness of their services into one of three groups ranging from the lowest (developmental) to the highest (integrated). The quality of care was determined using the 2001 IHS Diabetes Care and Outcomes Audit, which is a systematic random sample of medical records of 8274 patients with diabetes seen in the 86 participating programs. The quality indicators included recommended yearly examinations, education, and laboratory tests. Results were compared among programs of differing comprehensiveness of services. Population Studied: American Indians/Alaska Natives Principal Findings: In the 86 participating programs, the mean age of patients with diabetes was 54.21 years and the mean duration of diabetes was 8.26 years. The majority of programs were classified at or below the developmental level of program comprehensiveness and only 9 programs (10%) were at the higher program levels (educational and integrated). After adjustment for patient characteristics, program factors and clustering of data within programs, more comprehensive programs were associated with greater completion rates of diet education, yearly cholesterol tests, and a1c tests (p< 0.05). Other quality of care indicators such as yearly foot and eye exams, routine laboratory tests and immunizations showed better outcomes for the higher level programs but these differences were not statistically significant after adjustment for data clustering, patient and program characteristics. Conclusions: System-wide improvements in diabetes education are associated with better diabetes care outcomes. Implications for Policy, Delivery or Practice: This study provided information for the Indian Health National Diabetes Program and suggests that development of more comprehensive diabetes education programs can improve care and could reduce morbidity for patients with diabetes. The results of this study could help inform the development of diabetes education programs in minority and non-minority populations. Primary Funding Source: AHRQ • Predictors of Risk Status of Managed Care Patients with Chronic Conditions: Implications for Chronic Care Disease-Management Jayashri Sankaranarayanan, M.Pharm., Ph.D. Candidate, Holly Mason, Ph.D. Presented by: Jayashri Sankaranarayanan, M.Pharm., Ph.D. Candidate, Graduate Research Assistant, Pharmacy Practice, Purdue University, Heine Pharmacy Building, 575 Stadium Mall Drive, West Lafayette, IN 47907-2091; Tel: 765.743.2423; Fax: 765.494.7880; E-mail: jysan@purdue.edu Research Objective: Patient-risk status prediction in chronic conditions has implications for designing efficient and effective self-management education programs and guiding management-decisions. In the context of limited empirical data, the objective was to study the association of patientreported demographic, clinical, psychosocial, health-behavior and health-outcome factors with the risk-status of managedcare patients in chronic conditions. Particularly, association between patient’s readiness to adopt self-management behavior and patient risk-status was also studied, controlling for clinical, health-behavior and health-outcome variables. Study Design: Randomized cross-sectional mail survey. Population Studied: Enrollees (n=4730) from a centralIndiana (U.S.A) based health plan were surveyed (JuneSeptember 2003). Inclusion criteria: Adult patients, 18 years or older with at least one of four chronic conditions (asthma, diabetes, high-cholesterol or hypertension) using ICD-9-CM codes. Based on Andersen’s conceptual behavioral utilization framework (1995,2002), measures of demographics (gender, age, people per household, marital-status, employment-status, and insurance-status, number of information-support sources, income), clinical (disease-type, duration), psychosocial (stress, coping, self-efficacy, goal-setting, patient readiness), health-behavior (summated score of a 22-item selfmanagement behavior inventory) and health-outcomes [ShortForm 12 physical and mental health summary scores(PCS, MCS), 1-item satisfaction with care] were examined for their associations with patient risk-status. Patients with high medical service use and medical care costs were defined as “high-risk.” Patient readiness for each of four selfmanagement domains was derived from a patient-reported transtheoretical model-based staging-algorithm. This was the checked stage response (1=pre-contemplation, 2=contemplation, 3=preparation, 4=action or 5=maintenance) for each of four 1-item self-management domains: participation with doctor; general self-management; lifestylemanagement; and medical care. Stress, coping, self-efficacy, and goal-setting were measured by summated-scale scores. Principal Findings: Usable response rate: 12.9% [High-risk (n=102), low-risk (n=507)]. Gender, age, people per household, education, marital-status, employment-status, insurance-status, income, patient readiness to adopt lifestylemanagement, total medical conditions, maximum duration of the four conditions, stress, coping, self-efficacy, goal-setting, and PCS were significant for patient risk-status [univariate logistic-regressions, p=0.05]. Six variables were significant predictors of low-risk patient-status [stepwise multiple logisticregression, p=0.05]: Increased number of persons per household (OR=1.6, 95%CI=1.02-2.62) and health-status score (PCS-OR=1.1, 95%CI=1.07-1.16), and being full-time employed than retired (OR=4.5, 95%CI=1.36-14.73) increased odds of being low-risk. Having multiple-provider insurance compared to private insurance only (OR=0.1, 95%CI=0.04-0.38), having low information-support sources (OR=0.7, 95%CI=0.59-0.90) and being in precontemplation compared to maintenance stage in terms of patient-readiness for participation with doctor (OR=0.1, 95%CI=0.02-0.62) decreased odds of being low-risk. Being in action compared to maintenance stage for patient readiness to adopt lifestyle-management increased odds of being low-risk (OR=2.6, 95%CI=1.37-5.09), controlling for clinical variables (total medical conditions, maximum duration of the four conditions), self-management behavior, and health outcomes. Conclusions: Demographic (people per household, information-support sources), enabling (insurance, employment), psychosocial (patient-readiness for participation with doctor), and health-status outcome (PCS) factors were important predictors of patient risk-status. Patient readiness to adopt lifestyle-management was significant for patient risk-status, controlling for clinical, health-behavior and health-outcome measures. Implications for Policy, Delivery or Practice: Other than demographic and enabling factors, this study highlights the implications for considering psychosocial (patient readiness) factors in patient risk-stratification to aid health-providers in appropriate targeted self-management education interventions for optimal chronic disease-management. Primary Funding Source: Purdue Research Foundation, Purdue University • An Evaluation of an Adult Asthma BTS Collaborative: Process of Care and Outcomes Matthias Schonlau, Ph.D., Rita Mangione-Smith, M.D., Mayde Rosen, R.N., B.S.N., Kitty Chan, Ph.D., Shan Cretin, Ph.D., Emmett Keeler, Ph.D. Presented by: Matthias Schonlau, Ph.D., Statistician, Statistics, RAND, 1700 Main Street, Santa Monica, CA 90407; E-mail: matt@rand.org Research Objective: To examine whether a collaborative to improve asthma care positively influences process and outcomes of care in adult asthmatics. Study Design: Post-intervention evaluation of 11 sites that chose to participate in the evaluation of the Institute for Healthcare Improvement Breakthrough Series (BTS) Collaborative for asthma care. Control sites were identified for four of these sites. Population Studied: 185 adults with asthma with at least one asthma related visit in the prior 12 months in one of 15 primary care clinics: 11 collaborative participants and 4 control clinics. Principal Findings: Patients in the intervention group were more likely than patients in the control group to monitor their peak flow (57% vs 24%, p=0.04) and to have a written action plan (43% vs 27%, p=0.047). Patients in the BTS collaborative were significantly more likely to be satisfied with provider communication (62% vs 39%, p=0.02). Conclusions: The intervention improved some aspects of process of care. Patients benefited through increased satisfaction with communication. Follow-up of patients who participated in the intervention may have been too brief to detect significant improvement in the other health-related outcomes examined. Primary Funding Source: RWJF • Medicare Beneficiaries with Alzheimer’s Disease: Access to Mental Health Services Chandrakala Ganesh, B.S. Pharmacy, Dennis Shea, Ph.D. Presented by: Dennis Shea, Ph.D., Department Head and Professor, Health Policy and Administration, The Pennsylvania State University, 104C Henderson Building, State College, PA 16802; Tel: 814.863.5421; Fax: 814.863.2905; E-mail: dgs4@psu.edu Research Objective: The objectives of this research are: (1) to describe patterns of psychotropic drug use, physical and mental co-morbidities, mental health visits and prescription drug coverage among Medicare beneficiaries with AD; (2) to determine the factors responsible for differences in psychotropic drug use and visits to mental health providers among Medicare beneficiaries with AD. Study Design: The research uses data from the 1999 Medicare Current Beneficiary Survey (MCBS). Odds ratios are calculated using logistic regression. Two dependent variables are prescription of donepezil and mental health visit by Medicare beneficiaries. The independent variables include self report or claims diagnosis of mental health conditions, comorbid physical health conditions, age, census, race and gender. Population Studied: The study sample includes community based Medicare beneficiaries who reported AD in the survey or claims records of the 1999 MCBS. Principal Findings: Over 70% of beneficiaries with AD had atleast one other chronic health condition (50% arthritis, 43% hypertension, 38% heart disease & 11% depression). Less than 20% of beneficiaries visited a mental health specialist for mental health care. Beneficiaries more likely to visit a mental health specialist are white, over 75 years and live in the Northern or Western census regions. Only 16% of beneficiaries with AD are prescribed donepezil. The key predictors of a prescription are age over 75 years, diagnosis of mental illness, from the South census region South and being African American. Conclusions: A significant number of Medicare beneficiaries with AD do not receive mental health services. They have lower levels of treatment, especially the use of acetyl cholinesterase inhibitors. Implications for Policy, Delivery or Practice: There are 4 million Americans suffering from AD. Though AD can be effectively managed with pharmacological and behavioral therapy, there is an underutilization of mental health services by Medicare beneficiaries with AD. Medicare policy should emphasize appropriate diagnosis and treatment guidelines for this vulnerable population. Primary Funding Source: NIMH, Summer Training in Aging ResearchTopics- Mental Health (START-MH) 2003 • Making the Business Case to Employers for Cardiovascular Health Benefits: A Summary of the Worksite Literature and Selected Case Studies Karen Shore, Ph.D., Steven Garfinkel, Ph.D., Dyann Matson Koffman, Dr.PH, Victoria Anwuri, M.P.H., Diane Orenstein, Ph.D., Lori Agin, B.A. Presented by: Karen Shore, Ph.D., Senior Research Scientist, American Institutes for Research, 1791 Arastradero Road, Palo Alto, CA 94304; Tel: 650.843.8121; Fax: 650-858-0458; E-mail: kshore@air.org Research Objective: CDC’s cardiovascular health (CVH) program provides public health leadership to improve cardiovascular health for all, and reduce the burden of and eliminate disparities associated with heart disease and stroke. In support of those goals, we developed a Cardiovascular Health and Business Toolkit. State health department staff will use the Toolkit to influence employers to purchase prevention related benefits and services for their employees to prevent heart disease and stroke. Through a literature review, expert panel recommendations, and worksite case studies, we identified interventions that improve health and reduce costs associated with heart disease and stroke among employees. Study Design: We conducted a literature review of worksite efforts to reduce heart disease and stroke, specifically by controlling high blood pressure and high blood cholesterol risk factors. We also gathered extensive background information on the programs of multiple companies from the literature and from expert panel recommendations. Using a list of criteria such as successful risk factor outcomes, we selected six companies for detailed telephone case study interviews. We gathered information on various aspects of the organization, CVH program components, and efforts to evaluate the CVH program. Population Studied: The six case study organizations ranged in size from 225 to over 1 million employees and had locations throughout the U.S. Industries represented were direct marketing/distribution, manufacturing (health care, clothing, automotive), higher education, and poultry processing. Principal Findings: The literature review suggested that for those at risk for heart disease and stroke, 1) a minimal screening and referral program offered at the worksite will positively affect about 25% of those at-risk, 2) individual follow-up counseling will significantly improve risk factor outcomes, and 3) plant-wide environmental interventions show a small positive effect on outcomes, but aren’t comparable to individual follow-up counseling and education. The case studies revealed a variety of promising practices employers are currently implementing to reduce heart disease and stroke. Programs ranged from general health promotion programs (for the smaller employers) to CVH-specific programs, and all were designed to reduce blood pressure and/or cholesterol. Health program components included HRAs, feedback, and follow up; newsletters; and interactive websites. Specific approaches to address high risk employees include disease management programs, telephone and inperson counseling, and vouchers to pay for physician office visits. Conclusions: Case study interviewees identified senior management support and a culture supporting wellness and CVH, as well as resourceful and committed program staff as key organizational components of an effective program. Consistent with the literature review, interviewees identified HRAs and screenings, follow up counseling, plantwide/environmental changes (cafeteria foods, fitness centers), plant-wide policy changes (non-smoking facilities), health education information and classes, financial or other incentives (gift cards, lower health insurance premiums), efforts to reach populations “where they are”, and consistent yet frequent communication with simple messages as key program components. Implications for Policy, Delivery or Practice: This study identified interventions that had the most impact for preventing heart disease and stroke, are cost-effective, and can be implemented in all sizes and types of worksites. Primary Funding Source: CDC • Patient Satisfaction and Utilization of VA versus PrivateSector Healthcare Services by Veterans Kevin Stroupe, Ph.D., Denise Hynes, Ph.D., Anita GiobbieHurder, M.S., Eugene Oddone, M.D., Morris Weinberger, Ph.D., William Henderson, Ph.D. Presented by: Kevin Stroupe, Ph.D., Research Scientist, , Midwest Center for Health Services and Policy Research, PO Box 5000 (151H) 5th Avenue and Roosevelt Road, Bldg 1B260, Hines, IL 60141; Tel: 708.202.3557; Fax: 708-202-2316; E-mail: stroupe@research.hines.med.va.gov Research Objective: Chronically ill patients who are not satisfied with their care may change healthcare providers or systems, which could disrupt continuity of care and impede management of their conditions. In this study, we determined the VA and private-sector healthcare utilization of veterans with chronic conditions, and we tested the hypothesis that veterans who were less satisfied with their care were more likely to use private-sector services. Additionally, we examined this hypothesis among a sub-group of veterans with greater access to private-sector care: those who were Medicareeligible. Study Design: Data came from a multi-center randomized trial of increased access to primary care. We assessed patient satisfaction along 11 dimensions prior to randomization, and we determined VA and private-sector utilization over the subsequent 6 months, using VA and Medicare administrative data, private-sector billing data, and patient interviews. We used multivariable logistic regression analyses to examine whether baseline patient satisfaction was associated with private-sector inpatient or outpatient use over the 6-month period following baseline. Because the 11 satisfaction subscales were correlated, we estimated separate regression models for each satisfaction subscale. We conducted the same analyses for the subgroup of Medicare-eligible veterans. Population Studied: Patients hospitalized on the General Medicine Service of 9 VA medical centers between 1992 and 1994 were eligible if they had a diagnosis of diabetes mellitus, chronic obstructive pulmonary disease, and/or congestive heart failure. Principal Findings: Of the 1,375 study patients, 174 (13%) used private-sector healthcare. Patients with private-sector healthcare use were older and lived farther from a VA medical center. Ninety-five percent of patients with private-sector use continued to receive some VA healthcare. For 6 of the 11 satisfaction subscales, the odds of private-sector use decreased as patient satisfaction increased, ranging from a 21% decrease (OR = 0.79; 95% CI: 0.63, 0.99) to a 32% decrease (OR = 0.68; 95% CI: 0.53, 0.87) (p < 0.05). Findings were even stronger among the sub-group of Medicare-eligible veterans. For 8 of the 11 satisfaction subscales, the odds of private-sector use decreased as satisfaction increased, ranging from a 29% decrease (OR = 0.71; 95% CI: 0.53, 0.94) to a 39% decrease (OR = 0.61; 95% CI: 0.40, 0.92) (p < 0.05). In contrast, among Medicare-ineligible veterans, greater satisfaction at baseline was associated with lower odds of private-sector use for only 2 of the 11 satisfaction subscales (p < 0.05) Conclusions: Higher baseline satisfaction was associated with less subsequent private-sector healthcare use. Moreover, the association between patient satisfaction and private-sector use was strongest among Medicare-eligible veterans. Implications for Policy, Delivery or Practice: Patient satisfaction was associated with private-sector, particularly among Medicare-eligible veterans. While availability of Medicare gives these veterans greater flexibility in response to patient satisfaction, differences in VA and Medicare benefit structures (such as the previous lack of a Medicare drug benefit) might encourage dissatisfied veterans to continue receiving some VA care. Indeed, 95% of private-sector users continued receiving some care at the VA. This dual use of VA and private-sector care may impede efforts to ensure continuity of care for their chronic conditions. Thus, improvements in patient satisfaction may lead to enhanced continuity of care. Primary Funding Source: VA • VA and Medicare-Covered Private-Sector Healthcare Use by Veterans with End Stage Renal Disease Kevin Stroupe, Ph.D., Denise Hynes, Ph.D., Kristen Koelling, M.S. Presented by: Kevin Stroupe, Ph.D., Research Scientist, Midwest Center for Health Services and Policy Research, PO Box 5000 (151H) 5th Avenue and Roosevelt Road, Bldg 1B260, Hines, IL 60141; Tel: 708.202.3557; Fax: 708-202-2316; E-mail: stroupe@research.hines.med.va.gov Research Objective: Veterans with end stage renal disease (ESRD) need chronic dialysis to replace lost kidney function, requiring substantial healthcare resources. Many VA users also obtain private-sector healthcare. Such dual use may enhance flexibility; however, it can potentially make comprehensiveness and continuity difficult to achieve. Dual use may be particularly prevalent among ESRD patients because most become Medicare eligible after initiating dialysis, regardless of age. To determine which ESRD patients are most likely to have continuous rather than fragmented care, we examined the financial, geographic, sociodemographic, and health status factors that predict exclusive use of VA care. We hypothesized that patients with better financial and geographic access to VA were more likely to use VA exclusively. Study Design: We submitted Social Security Numbers (SSNs) of the 6.1 million VA users or eligible users in 1999 to the US Renal Data System (USRDS), a national repository for Medicare and other information for ESRD patients. USRDS identified all ESRD veterans and provided their Medicare claims and demographic data, which we linked with VA administrative data. We obtained local healthcare market factors from the Area Resource File. We performed multivariable logistic regression analyses with regional fixed effects to examine the effect of financial (e.g., whether patients were subject VA copayments and whether patients were eligible for Medicaid), geographic (e.g., whether patients lived <10 miles from VA or non-VA hospitals), socio-demographic (e.g., age, race, and gender), and health status factors on exclusive VA healthcare use. Health status was measured using Hierarchical Condition Categories (HCC) where higher scores indicate worse health status. Population Studied: Our study included all veterans with ESRD in 1999 who were eligible for both VA and Medicarecovered private-sector care. Principal Findings: There were 25,667 veterans with ESRD in 1999 eligible for VA and Medicare-covered private-sector services. Fifty-nine percent were >= 65 years old. Ten percent used VA services only, 32% used private-sector services only, and 58% used both. Exclusive VA use increased for patients without VA medical copayments (OR = 6.5) but decreased for Medicaid-eligible patients (OR = 0.28). Exclusive VA use increased when VA hospitals were <10 miles from patients (OR = 2.15) but decrease when non-VA hospitals were <10 miles (OR = 0.71). Exclusive VA use decreased among patients >= 65 (OR = 0.67) and decreased as HCC scores increased (e.g., scores above the fourth quartile OR = 0.08). Conclusions: Patients with greater financial (e.g., no VA medical copayment) and geographic access (e.g., VA hospitals <10 miles) to VA were more likely to use VA exclusively. Patients with greater financial (e.g., Medicaid eligibility) and geographic access (e.g., non-VA facilities <10 miles) to privatesector services were less likely to use VA exclusively. Older patients with worse health status were less likely to use VA exclusively. Implications for Policy, Delivery or Practice: ESRD patients require extensive healthcare and may benefit from improvements in continuity and coordination of care. Financial factors were found to affect exclusive VA use. Consequently, it might be useful to examine whether altering financial incentives (such as copayments) and benefit structures in VA and Medicare might promote healthcare use in a single system. Primary Funding Source: HRSA • Using Claims Data to Estimate the Burden of Mood Disorder Services among Women Diagnosed with Tubal Infertility Guoyu Tao, Ph.D., F. Chowdhury, M.D., T. Chorba, M.D., G. Fricchione, M.D., K. Irwin, M.D. Presented by: Guoyu Tao, Ph.D., Health Scientist, Division of STD, cdc, 1600 Clifton Road, MS-E80, Atlanta, GA 30333; Tel: 404.639.8180; Fax: (404)639-8607; E-mail: gat3@cdc.gov Research Objective: Tubal infertility is one of the sequelae of untreated bacterial STD infection. Little is known about the use of medical services for mood disorder by women with tubal infertility. Infertility may result in common mood disorders (e.g., depression and anxiety) if reproductive efforts fail, and mood disorders may reduce the frequency of intercourse, thereby reducing fertility. The objective of this study is to determine if an excess of medical services for mood disorders is observed before and after the diagnosis of tubal infertility. Study Design: Using the MarketScan database for the years 1998 to 1999, we examined medical claims for women enrolled in health plans of large U.S. employers. ICD-9 codes were used to identify patients with tubal infertility and mood disorders (major depressive disorder, anxiety, phobic disorders, neurotic depression, brief or prolonged depressive reaction, or adjustment reaction with anxious mood or mixed emotional features). Population Studied: women who had tubal infertility or mood disorders. Principal Findings: More than 335,000 women aged 19-44 years were continuously enrolled in these health plans from 1998 through 1999; 105 (0.2%) had claims for tubal infertility and mood disorder. Of these, 51 (49%) were diagnosed with a mood disorder before being diagnosed with infertility, and 54 (51%) were diagnosed with infertility before being diagnosed with a mood disorder. The percent with a mood disorder was significantly higher among enrollees with infertility claims than among enrollees without infertility claims (16% versus 12%) (p<0.001). Conclusions: Services for mood disorders may be more common in patients with infertility because of the possible causal effects of infertility on mood disorders or mood disorders on reduced fertility. Alternatively, enrollees with coverage for infertility services may be more likely to have mental health coverage that allows generation of mood disorder claims because more costly health plan products tend to cover both more comprehensive infertility and mental health services. Among women diagnosed with infertility and mood disorder, about half were diagnosed with a mood disorder before their infertility diagnosis. Analyses that attempt to estimate the degree to which tubal infertility causes mood disorders must consider that both diagnosed and undiagnosed mood disorders may precede infertility diagnoses and represent pre-existing conditions rather than outcomes of infertility per se. Implications for Policy, Delivery or Practice: Clinicians who care for infertility patients should be aware that many infertility patients receive mood disorder services before or after their infertility diagnosis and should consider mental health risk assessment and management for infertility patients. Primary Funding Source: CDC • Evaluation of the Quality Payment Demonstration Program for Increasing the Cure Rate of Tuberculosis Wen-Chen Tsai, Dr.PH, Pei-Tseng Kung, Sc.D. Presented by: Wen-Chen Tsai, Dr.PH, Assistant Professor, Health Services Management, China Medical University, 11 Ln16 Sec.3 Chungching Road, Taya, Taichung, 428; Tel: 886.4.25603149; Fax: 886-4-25603149; E-mail: wtsai@mail.cmu.edu.tw Research Objective: The tuberculosis is one of leading causes of death in Taiwan and the annual number of death of tuberculosis is the the highest among all infectious diseases. In order to increase cure rate of tuberculosis, improve treatment quality, and give more health care responsibilities to health care providers, the Bureau of National Health Insurance (BNHI) has implemented the "quality payment" demonstration programs for tuberculosis in Taiwan since 2001. The BNHI hopes to furnish the patients with comprehensive health care services that emphasize health care outcomes and quality. The purpose of this study was to evaluated the tuberculosis demonstration program of quality payment. This study evaluated the differences of cure rates, treatment times, treatment expenditures, and patient satisfaction for tuberculosis patients between the demonstration program and current fee-for-services payment programs. The factors influencing the successful treatment to tuberculosis, were analyzed. The physicians' attitudes and opinions to the demonstration program were surveyed. Study Design: This study is a retrospective study. It consists of two parts. In the first part, the study used the structured questionnaire to interview tuberculosis patients, and we also used questionnaire to survey the relative physicians’ opinions for the demonstration program. The descriptive statistics were used to compare patients’characteristics, treatment expenditure, satisfaction of medical services, treatment times, and cure rate between the demonstration programs and feefor-services program. Multiple regression analysis was conducted to explore the relative factors that influenced the patients’ satisfaction with treatment process and outcomes, and logistic regression analysis was applied to examine the factors that significantly affected tuberculosis patients if they could be cured within 9-month treatment. In the second part, based on NHI medical claim data this study conducted statistical analyses for comparing the spending, cure rate, and treatment time for tuberculosis patients between demonstration program and fee-for-service program. Population Studied: The study period was from January 2001 to December 2002. The samples comprised all tuberculosis patients who were new cases and were cured in demonstration program or fee-for-services program in 2002, and those who were new tuberculosis patients and were also cured in 2001 before the implementation of demonstration program. Principal Findings: The results showed that tuberculosis patients in the demonstration program indeed had shorter treatment times. According to the consequences of analyzing NHI medical claim data, there was 83.81% cure rate in terms of 9-month treatment for those participating in the demonstration program, and 57.60% cure rate for nonparticipants. The average treatment time for cured patients under the demonstration program was 224 days, which was shorter than that of non-participants. The demonstration program had higher average treatment expenditure for one cured tuberculosis patient in terms of 9-month treatment, but had similar average treatment expendiutre in terms of 18month treatment. The patients in the demonstration program felt more satisfaction with treatment services. The main problems for many tuberculosis patients were a long period of medication and the side effects of medicines. For physicians, most physicians believed the demonstration program is helpful to increase cure rate, but they showed less satisfaction with claim procedures and payment structures. Conclusions: The quality payment demonstration program was significantly helpful to increase the cure rate of tuberculosis. The study results recommend the BNHI entirely implements the quality payment program for tuberculosis treatment. Implications for Policy, Delivery or Practice: Health care payment policy for increasing the successful tuberculosis treatment Primary Funding Source: Center of Disease Control, Taiwan • Effect of Services in Drug Treatment Clinics on Emergency Department Use Christine Laine, M.D., M.P.H., Barbara Turner, M.D., MSEd, Walter Hauck, Ph.D Presented by: Barbara Turner, M.D., MSEd, Professor, Medicine, University of Pennsylvania, 1123 Blockley Hall, 423 Guardian Drive, Philadelphia, PA 19104-6021; Tel: 215.898.2022; Fax: 215.573.8779; E-mail: bturner@mail.med.upenn.edu Research Objective: To examine the relationship of medical care and other health care services in drug treatment clinics with repeated emergency department (2+ ED) visits. Study Design: A survey of a stratified random sample of drug treatment clinic directors (N=125)in New York linked to Medicaid claims for clinic patients. Survey in 1998 asked about services in 1997 and addressed: linkage to medical care, staffing, available drug and alcohol treatment, accessibility, on-site medical preventive services, social support services, HIV services, and academic affiliation. The dependent variable was 2+ ED visits in 1997 and models adjusted for clustering of patients. Population Studied: 8,397 Medicare-enrolled patients who received regular (6+ months) drug treatment at a surveyed clinic in 1996-97 Principal Findings: Repeated ED use occurred for 14.4%. Drug treatment clinics with on-site medical services had lower odds of 2+ ED visits (0.79 [95% CI 0.68, 0.91]. After adjustment, an interaction between onsite medical services and the weekly number drug users seen (grouped by quartile) revealed showed that this benefit occurred only for smaller volume clinics: lowest quartile (0.64 [0.47, 0.88]), middle two quartiles (0.79 [0.64, 0.97]) but top quartile (1.27 [0.81, 1.97]). Offering more medical preventive services such as PAP smears was the only other clinic characteristic associated with less ED use (0.62 [0.44, 0.88]. Conclusions: Onsite provision of medical services in small and moderate sized drug treatment programs is associated less demand for ED care. The additional protective association of preventive services may indicate clinics with more comprehensive medical services. Implications for Policy, Delivery or Practice: To reduce ED use by drug users in treatment, policymakers should consider supporting a more complete array of medical services in drug treatment clinics. Lack of benefit of onsite medical services in large drug treatment programs may indicate poorer ability to manage patient demand or poorer quality care. Primary Funding Source: NIDA • Long Term Survival Post Treatment of a Nationwide Cohort of Elderly Veterans with Colorectal Cancer Katherine Virgo, Ph.D., M.B.A., Mary Valentine, M.P.H., Lucille Dauz, M.A., Lan Marietta, M.A., Sangita Devarajan, M.P.H., Frank Johnson, M.D. Presented by: Katherine Virgo, Ph.D., M.B.A., Professor, Department of Surgery, Saint Louis University & St. Louis VAMC, 3635 Vista at Grand Boulevard, Saint Louis, MO 631100250; Tel: 314.289.7023; Fax: 314.289.7038; E-mail: virgoks@slu.edu Research Objective: The research objective was to identify a nationwide cohort of patients diagnosed with colorectal cancer and follow them from the period pre-diagnosis through diagnosis, initial curative intent treatment, adjuvant therapy, post-treatment follow-up, to the final endpoint of either death or loss to follow-up using a merged VA-Medicare database. This permits the researcher to capture a more complete picture of patient management, disease recurrence, and outcomes than possible in studies which do not account for patients utilizing multiple systems of health care. Study Design: A retrospective analysis of 13 years of nationwide Medicare and VA inpatient and institutional outpatient data beginning with the three years pre-diagnosis (1986-1990) through a minimum of five years post-diagnosis (1994-1998) was conducted. Death data were available through December 2003. Data were also extracted from tumor registry files, Computerized Patient Record System Files, and paper medical records at each VA. Population Studied: The population studied included all VA patients diagnosed with colorectal cancer and surgically treated for cure during the five-year period 1989-1993, who were Medicare-eligible at diagnosis, and survived the index admission. Principal Findings: Of the 6612 patients treated with curative intent during the five-year period, 4902 (74%) could be staged. Of these, 4535 (93%) were deemed eligible for the study. Of the eligible patients, 77% were diagnosed with colon cancer and 23 percent with rectal cancer. The majority (88%) had adenocarcinoma. The histopathologic grade was moderately differentiated for 54% and well differentiated for 19%. As of December 2003, 74% had died. Including all stages (0- IV), the average survival in months after treatment was 75 (median=61). Survival by stage was also calculated. Identification of significant predictors of survival is underway. Conclusions: This rich database provides a wealth of data for subgroup analyses of survival, recurrence patterns, and particularly, of health services utilization patterns within and across systems of care. Implications for Policy, Delivery or Practice: Continuity of care may be lacking for users of multiple systems of care. In addition, diagnostic tests may be repeated needlessly further increasing costs both the patient and to society. Primary Funding Source: VA • Congestive Heart Failure Care Management: Utilization and Factors Associated with Its Implementation in Physician Organizations Margaret Wang, M.P.H., Thomas Bodenheimer, M.D., Robin Gillies, Ph.D., Stephen Shortell, Ph.D. Presented by: Margaret Wang, M.P.H., Doctoral Candidate, Health Services and Policy Analysis, University of California, Berkeley, 1340 Arch Street, Berkeley, CA 94708; E-mail: mcywang@uclink.berkeley.edu Research Objective: Existing literature provides evidence that multi-disciplinary care management processes (CMPs) for patients with congestive heart failure (CHF) improve clinical outcomes and reduced healthcare costs. However, little is known about the utilization of these processes or factors affecting their implementation in physician organizations (POs). This study aims (1) to assess the use of CMPs to manage CHF patients; and (2) to identify organizational and environmental factors affecting the extent of their implementation in POs. Four types of CMPs are examined: (a) case management; (b) provider feedback; (c) clinical practice guidelines; and (d) disease registry. Study Design: This study analyzed data collected by the National Study of Physician Organizations (NSPO), a crosssectional census survey (response rate = 70%) of POs in the U.S. (September 2000 through September 2001). CMP implementation was assessed by asking the PO how many of the four CMPs does the PO employ to manage CHF patients. Multivariate linear regression was performed to determine how environmental and organizational factors affect the extent to which POs implement these CMPs. Population Studied: The studied population consisted of 1,104 POs (67% medical groups and 33% IPAs) employing 20 or more physicians in the U.S. Analyses were restricted to those POs report treating CHF patients, resulting in a sample size of 798 POs. Principal Findings: On the average, POs report implementing approximately one CMP to manage CHF patients. Multivariate linear regression results indicate that environmental factors including external incentives to improve quality, percentage of county HMO penetration, and percentage of hospital financial risk assumed by the PO are all positively associated with the extent to which CMPs are utilized to manage CHF patients. In addition, a PO’s participation in CHF quality improvement activities, the sophistication of clinical information technology infrastructures, systematic assessment of patient satisfaction, having an appointment scheduling system to allow for patient group visits and follow-up, IPA-status (MG as referent group), and being single specialty (multispecialty as referent group), all have positive relationships with the degree of CMP implementation. Conclusions: Even though CMPs for CHF have been shown to improve outcomes and reduce costs, we found that POs have adopted these CMPs to only a minor extent. In addition, our results suggest that the extent to which POs implement CMPs to manage CHF patients is affected by a combination of environmental incentives and organizational structural capabilities. Consistent with prior findings, most noteworthy of these facilitators include the presence of incentives to improve quality in the PO’s external environment and the sophistication of clinical information technology adopted by the PO. Implications for Policy, Delivery or Practice: This study provides the first national assessment of CMPs implemented by POs to manage CHF patients, as well as factors associated with the extent of their use in POs. Given that CHF has been the most common discharge diagnosis for Medicare beneficiaries and has significant healthcare cost and resource implications, it is crucial to elucidate environmental and organizational factors associated with CMP implementation. A deeper understanding provides policy makers and practitioners information on how to facilitate CHF care management, thereby improving the healthcare quality for CHF patients. Primary Funding Source: RWJF • Using the Ecology Model to Assess Healthcare in Asthma Barbara Yawn, M.D. M.Sc., George Fryer, Ph.D., Robert Phillips, M.D., Susan Dovey, Ph.D., David Lanier, M.D., Larry Green, M.D. Presented by: Barbara Yawn, M.D. MSc., Director of Research, Research, Olmsted Medical Center, 210 Ninth Street, S.E., Rochester, MN 55904; Tel: 507.287.2758; Fax: 507.287.2722; E-mail: yawnx002@umn.edu Research Objective: To test the value of the ecology model in assessing changes in the patterns of healthcare contact in people with asthma. Explicitly, to assess the ability of the ecology model to reveal changes in patterns, identify specific populations who experience barriers to care and describe how asthma affects healthcare contacts. Study Design: The ecology model was used as the analytic framework to display the health care contacts of case and control subjects. Risk ratios were used to compare the healthcare contacts of cases and controls across multiple settings and combinations of settings. Population Studied: Children and adults who participated in the 1999 U.S. Medical Expenditure Panel Survey. Cases were school-aged children (6 to 17 years) and young adults (18 to 44 years) with self-reported asthma. Controls were people from the same age groups who have no self-reported asthma or other chronic conditions. Principal Findings: In 1999, the presence of asthma increased the likelihood of an ambulatory care visit (risk rations 1.2 and 1.3 for children and adults respectively) and more than doubled the likelihood of making one or more visits to the emergency department (risk ratios >2.7). The ecology models highlights the 18.8% of children and 14.5% of adults with asthma who had no ambulatory care visits for asthma in 1999. In addition, about one quarter of this group (5.2% of children and 3.69% of adults with asthma) were seen in the emergency department or hospital but had no ambulatory care during the year. These Americans were more likely to be uninsured, have no usual source of care and live in metropolitan areas. Conclusions: The ecology model confirmed that asthma increases contact in all health care settings but also demonstrated a change in the pattern of contacts. More importantly, the ecology model identified an uninsured, urban subgroup of people with no usual source of care but with asthma who sought emergent or hospital services but appear to have barriers to ambulatory care access. Implications for Policy, Delivery or Practice: The ecology model identified people with apparent access barriers to care that would be missed in reviews of HMO data, emergency room records and medical records of large health care organizations. The ecology model can provide the necessary context for policy and practice evaluation and modification related to care of chronic diseases. Primary Funding Source: AHRQ • Practical Quality Indicators for Asthma Management Barbara Yawn, M.D., M.Sc. Presented by: Barbara Yawn, M.D. MSc., Director of Research, Olmsted Medical Center, 210 Ninth Street, S.E., Rochester, MN 55904; Tel: 507.287.2758; Fax: (507) 287-2758; E-mail: yawnx002@umn.edu Research Objective: Asthma is common and management guidelines are availble, yet many reviews of asthma care suggest that the care provided does not meet the recommended standards. Most of the currently used quality measures and report cards directed back to physicians provide little information on how to improve compliance with the quality standards assessed. This study is designed to develop quality measures that relate directly to care functions in the primary care physicians office. Study Design: Retrospective medical records of an entire county population. A set of quality measures that assess basic history and physical functions for asthma care were compared to the docmented care for all asthma visits in the two community health care systems for a one year period. Quality measures had to be present or met at only one visit during that year to be counted as completed. Population Studied: The clincians caring for all children and adults making an asthma related visit to any health care facility in Olmsted County in 2000. Principal Findings: The quality measures developed and studied and the percent meeting the indictor (%) are as follows. 1. Percent of visits with an asthma ICD-9 code (493.xx) that had a written diagnosis other than asthma such as RAD or wheezy bronchitis in people > 3 years of age (24%). 2. Percent of visit notes with daytime symptoms documented (54%). 3. Percent of visits with nighttime symptoms documented (33%). 4. Percent of charts with absteenism or reduced activity days recorded (12%). 5. Percent of visits with triggers or allergies mentioned or evaluated (9%). 6.Percent of patients with non-urgent visit in a year (11%). and 7. Percent of patients with an ambulatory follow-up visit within one month after emergency department visit or a hospitalization (75%). The goal for measure 1 was 0% and was 100% for all of the rest of the indicators. Conclusions: Many medical records do not contain the information necessary to assess asthma severity, asthma control or triggers that may effect control. Without these basic pieces of data it is difficult to believe that current guidelines can be followed. Each measure has a direct solution that can be incorporated into the care system of people with asthma. Implications for Policy, Delivery or Practice: These quality measures may facilitate translation of guidelines into practice more effectively than current guidelines that have such outcomes as the ratio of rescue to controller prescriptions or the percent of people on controller medications, neither of which suggest immediate and simple solutions. Primary Funding Source: AHRQ • Risk Adjustment for Children with Special Health Care Needs Hao Yu, M.Sc., Andrew Dick, Ph.D, Peter Szilagyi, M.D., M.P.H. Presented by: Hao Yu, M.Sc., Ph.D Candidate, Community and Preventive Medicine, University of Rochester, 601 Elmwood Avenue, Box 644, Rochester, NY 14642; Tel: 585.275.3432; Fax: 585.461.4532; E-mail: hao_yu@urmc.rochester.edu Research Objective: While most studies of risk-adjusted capitation focused on Medicare’s reimbursement to managed care plans, few risk-adjustment models have been estimated separately for children. This study aims to fill the information gap by estimating risk-adjustment models for children, especially for children with special health care needs (CSHCN), and examining the potential profit that plans could hypothetically gain by using additional information to select low-cost enrollees under different risk-adjusted capitation rates. Study Design: The data were extracted from the Medical Expenditure Panel Survey (MEPS), a nationally representative survey of health services use and cost. This study tested five sets of adjustors using a modification of the RAND two-part model, in which the first part used logistic regression to estimate the probability of using health services in 2000, and the second part used a generalized linear model with gamma distribution to estimate the total expenditures in 2000. Crossvalidation of the estimated models was performed using a split-sample method with bootstraping. Plan’s revenue was defined as the sum of risk-adjusted capitation payment, and its profit as the difference between the revenue and the actual health expenditures in 2000. The profit rate was the profit divided by the revenue. We quantify plans’ incentive for risk selection by assuming that plans could use additional information to exclude individuals whose predicted expenditures were higher than the capitation rate under each of the estimated models. Population Studied: The study included 4,896 children less than 18 years old, who were screened using the CSHCN Screener through the MEPS 2000 Parent Administered Questionnaire. The sample was linked with MEPS 1999 to obtain information about health services use and expenditure in 1999. Principal Findings: Socio-demographic factors explained 2% of the variance in annual expenditure. Together with sociodemographic factors, CSHCN status explained 6%; the five detailed questions of CSHCN Screener explained 12%; health status measures explained 14%; and prior year use and expenditures explained 20%. All the adjusters together explained 22%. If the socio-demographic factors were used to adjust capitation rates, plans could use CSHCN status as additional information to enroll only the profitable individuals whose expected expenditures were not higher than the adjusted capitation payment, and could achieve a profit rate of 45%. In the extreme case of favorable selection, the profit rate would be 50%. Conclusions: Each of the risk adjustment models explained only a small proportion of the variance of annual total expenditure. Adding CSHCN status as an adjuster tripled the proportion explained by socio-demographic factors alone. The five questions of CSHCN Screener had explained the variation similarly to health status. The CSHCN information could help reduce discrimination facing CSHCN in a competitive health plan market. The plans’ incentive to select low-cost children was substantial. Implications for Policy, Delivery or Practice: Further research in the area of adjustment models for children is needed. Given the imperfection of risk-adjustment capitation system, future studies need to focus on a mix of capitation payment and cost-based reimbursement system to reduce selection incentives. Primary Funding Source: The Maternal Child Health Bureau