Atherosclerotic Quantifying Function Multi-Year
advertisement

2007 IEEE/ICME International Conference on Complex Medical En2ineerin2
Quantifying Human Atherosclerotic Plaque Growth
Function Using Multi-Year In Vivo MRI and
Meshless Local Petrov-Galerkin Method
Dalin Tang 1, Chun Yang2, Joseph D. Petruccelli 1, Chun Yuan 3,
Fei Liu 3, Tom Hatsukami 4, Sayan Mondall, Satya Atluri5
Mathematical Sciences Department
Worcester Polytechnic Institute
Worcester, MA 01609, USA,
dtang(wpi.edu
508-831-5332, fax: 508-831-5824
2Mathematics Department, Beijing Normal University, Beijing, China
3Deparment of Radiology, University of Washington
Seattle, WA 98195 USA
4Division of Vascular Surgery, University of Washington, Seattle, WA. 98195 USA
5 Center for Aerospace Research & Education, University of California, Irvine
Irvine, CA 92612 USA
However, this Low-Shear-Stress (LSS) mechanism cannot
fully explain why advanced plaques continue to grow under
elevated flow shear stress conditions [32]. The study of
atherosclerotic plaque progression and rupture is limited by
the complexity of the disease and lack of available
computational models based on in vivo patient data.
Atherosclerotic plaques often rupture without warning and
cause subsequential acute syndromes such as heart attack and
stroke [15-17, 28-29]. Current screening and diagnostic
methods are insufficient to identify the victims before the
event occurs [28]. It is extremely important to be able to
model and predict plaque progression and assess potential
rupture risk so that proper treatment can be suggested at an
early stage of the disease to prevent possible heart attack and
stroke.
Abstract - Atherosclerosis is a disease in human circulation
system affecting a large percentage of people, especially elderly
people in the developed countries. To better predict plaque
progression and prevent potential rupture, multi-year MRI
patient-tracking data were obtained to quantify human
atherosclerotic plaque progression. MRI-based 2D/3D models
with multi-component plaque structure and fluid-structure
interactions (FSI) were developed and solved by numerical
methods based on the meshless local Petrov-Galerkin (MLPG)
method (2D) and finite element method (2D/3D) to quantify
plaque growth functions which can be used to simulate plaque
progression for early prediction and diagnosis of atherosclerosisrelated cardiovascular diseases. For the first time, quantitative
human plaque growth functions were determined using structure
stress and flow shear stress data. Use of multi-year data leads to
verifiable simulations and improved accuracy of predictions. Our
initial results support the new hypothesis that plaque progression
has negative correlation with structural stress and flow shear
stress conditions. Plaque growth functions using both structure
stress and flow shear stress leads to much better agreement with
patient plaque progression data than using either of them. More
data and validations are needed to confirm our findings.
Multi-contrast magnetic resonance imaging (MRI)
techniques have been developed by Yuan and Hatsukami et al.
[36-38] to quantify plaque size, shape, and components
(fibrous, lipid, and calcification, inflammation, etc.) that allow
for the classification of lesions according to American Heart
Association (AHA) pathological guidelines [1-2,15-16].
While current diagnosis and surgery decisions for plaque
removal are mainly based on plaque morphology (stenosis
severity), mechanical forces play an important role in plaque
rupture and progression and should be taken into
consideration. MRI-based computational models with fluidstructure interactions and a computational plaque vulnerability
index (CPVI) for human atherosclerotic plaques have been
introduced by Tang et al. for plaque assessment and potential
clinical applications. Plaque assessment by CPVI method had
an impressive 900o agreement with histopathological
classifications [34]. Image-based computational modeling and
mechanical image analysis are adding a new spectrum of
Key words: Atherosclerosis; carotid artery; plaque progression;
blood flow; meshless method; fluid-structure interaction.
I. INTRODUCTION
Cardiovascular disease (CVD) is becoming the No. 1 killer
in the world and was responsible for 4000 of all deaths in the
United States in 2000 [1,2,22]. Much progress has been
reported on atherosclerosis initiation and early-stage
development related to endothelial cell activities [13,17-18,2324, 30-31]. It has been well-accepted that atherosclerosis
initiation and progression correlate positively with low and
oscillating flow wall shear stresses [13-14,17,23-24,30].
1-4244-1078-9/07/$25.00 c2007 IEEE.
546
2007 IEEE/ICME International Conference on Complex Medical Engineering
b)
indices (in additional to plaque morphological characteristics)
which may lead to more accurate assessment and predictions.
To better predict plaque progression and prevent potential
rupture, multi-year MRI patient-tracking data were obtained to
quantify human atherosclerotic plaque progression. We
hypothesize that plaque progression depends on structural
stress/strain conditions, plaque composition, and flow shear
stress conditions. MRI-based 2D/3D models with multicomponent plaque structure and fluid-structure interactions
(FSI) were developed and solved by numerical methods based
on the meshless local Petrov-Galerkin (MLPG) method (2D)
[3-6] and finite element method (2D/3D) to quantify plaque
growth rate functions which can be used to simulate plaque
progression for early prediction and diagnosis of related
cardiovascular diseases.
d)
c)
e)
II. MODELS AND METHODS
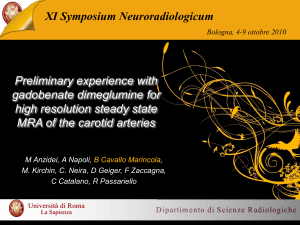
Fig. 1. 3D plaque samples re-constructed from in vivo MR images. (a)-(b):
Data from one patient at two time points showing plaque growth; (c)-(e): one
patient taking Statin showing plaque reduction. Time interval: 18 months.
Red: lumen; Yellow: lipid; Dark blue: calcification; light blue: outer wall.
Data Acquisition
Multi-year MRI data sets were acquired from 9 patients
with explicit consent obtained (See Fig. 1 for two examples).
MRI scans were conducted on a GE SIGNA 1.5T whole body
scanner using the protocol outlined in Yuan and Kerwin.[36].
A carotid phased array coil was used for all scans. Multicontrast images in TI, T2, proton density (PD), time-of-flight
(TOF), and contrast-enhanced (CE) TI weightings of carotid
atherosclerosis were generated to characterize plaque tissue
composition, luminal and vessel wall morphology [12,36-38].
A computer package CASCADE (Computer-Aided System for
Cardiovascular Disease Evaluation) developed by the
Vascular Imaging Laboratory (VIL) at the University of
Washington (UW) was used to perform image analysis and
segmentation. CASCADE allows for all contrast weightings
to be simultaneously displayed, indexed relative to the carotid
bifurcation, and analyzed serially along the length of the
carotid artery, CASCADE provides manual and automatic
analysis tools for accurate lumen and wall boundary detection,
and image registration. A histologically validated automated
in vivo plaque composition algorithm - MEPPS (MorphologyEnhanced Probabilistic Plaque Segmentation) facilitates the
analysis of plaque components which include lipid-rich
necrotic core (including intraplaque hemorrhage),
calcifications, loose matrix (including all tissues that were
loosely woven, such as proteoglycan rich fibrous matrix,
organizing thrombus, and granulomas), and others [25]. Upon
completion of a review, an extensive report is generated and
segmented contour lines for different plaque components for
each slice are stored as digital files for 3D geometry
reconstruction.
A.
B.
The Solid and Fluid Models
Both artery wall and plaque components were assumed to
be hyperelastic, isotropic, incompressible and homogeneous.
No-slip and natural boundary conditions (continuity of
displacement, balance of stresses) were specified at all
interfaces. Pressure conditions were set using patient-specific
data. All of these lead to (summation convention is used):
p ui,tt = cij j , i,j= 1,2,3; sum overj,
(1)
=
+
(2)
Fij ( ui± uj,i )/2, i,j =1,2,3
wall
=0,
ij nj Iout
(3)
arij njlinterface=sij * nj interface,
(4)
u interface=U interface,
(5)
where 6 is stress tensor (superscripts indicate different
materials), c is strain tensor, u is solid displacement vector,
and f . stands for derivative of f with respect to the jth
variable. Equations (1)-(5) apply to all solid models for
normal tissue and all plaque components except that the
material parameters will be different for each material.
Material densities for fluid, vessel and plaque components
were assumed to be the same for simplicity. The MooneyRivlin (M-R) model was used to describe the nonlinear
material properties of the vessel wall and plaque components
with parameters chosen to fit experimental data from our
studies and literature [8,10,20,27,35]. The strain energy
function for the modified Mooney-Rivlin model is given by
[7,33-34]:
(6)
W=c1(ll -3)+ c2( 2 -3) + D1 [ exp(D2 (I1 -3)) -1],
where h1 and '2 are the first and second strain invariants, c1 and
D, are material constants chosen to match experimental
measurements. The stress/strain relations can be found by:
(ij8=(W/Fij ±+W/OFji)/2,
547
(7)
2007 IEEE/ICME International Conference on Complex Medical Engineering
-11, _
0 0 oo o
_~
00 0 0C 0' 00 0
y test
00 00 0 0
00 0 00 0 c
00 0
0
00
0 000 0 0
00 000 0 0
0
0
0 0000 0 oo0
0o0 000 0 OO g
00 ggg0
0
000 0 °c°o°00
0 ° 00 0 00
00 0 0
q
0 oo o o
00
o0g~%o
0
0
00 0 0 0
0 0000
0
000 * ooo0o 0o 0C0
0
aQ
0
00 000
ti0 0000 O000000
where aij are the second Piola-Kirchhoff stresses, Fj, are the
Green-Lagrange strains. The incremental material law is
evaluated by further differentiation as,
Cijrs = (0(ij/GF,rs + 8ij/O,sr)/2.
Q
0o
(8)
The incremental generalized Hooke's law is given by
(9)
yij Cijrs -rs
Modified Mooney-Rivlin Models have been used in our
previous studies and by other authors [8,10,20,27,35] which
demonstrate the stiffening behavior of arteries and match well
with experimental measurements [9,11,20,26-27].
For the 3D model with fluid-structure interactions, the
flow was assumed to be laminar, Newtonian, viscous and
The Navier-Stokes equations with an
incompressible.
arbitrary Lagrangian-Eulerian (ALE) formulation were used as
the governing equations [21]. No-slip boundary conditions
were specified at all interfaces. Pressure conditions were set
using patient-specific data. All of these lead to the following:
X000
(10)
V-v=O,
VIF = X/8t ,
(1 1)
0
Let Qs be a sub-domain of Q, with an arbitrary shape and
contain a point x in question. Starting from (1), the
asymmetric local weak formulation of the problem is:
1 dQx +
fv, piidQx - 7ji1i
Qs
Qs
f(ui
f
+
-
u-
)vi dF,
=
fvi f dQx
(15)
Qs
_
where v is the test function, dQx means the integration is in
the current configuration. a is a penalty parameter to impose
the essential boundary condition (a >> 1). The symmetric
local weak formulation is:
0J,
JVipiidQ,
+
f|t1
r
Jvij0ui dQx viJvi%njdFx
-
Qs
Qs
s
-F. Jv1 ojn dF
+ o jku- u1 )v1dFx
Ls
s
viffdQx
(16)
Qf
The Meshless Local Petrov-Galerkin (MLPG) Method
While finite element method (FEM) has gained great
popularity in recent years, it has some serious drawbacks.
One of them is tedious meshing and re-meshing [5]. The
MLPG method has the advantage that it is truly meshless so
that no meshing or remeshing is needed. It has great potential
to replace FEM for problems with complex geometries and
frequent re-meshing. The basic ideas and key points for the
MLPG method are explained below. The MLPG and FEM
formulations are parallel except that the integration for MLPG
method is over a sub-domain, and trial and test functions can
be chosen independently (MLPG1-MLPG6, [3-6]). For
simplicity, notations used in this section are consistent with
those in [3,5] whenever possible.
Let Q be the global domain, {Xi, i=1, , N} be selected
nodal points, Q, be a sub-domain (marked as Q_x_trial in Fig.
2) and a trial function u be defined as,
C.
jEaj(x),
00
;)
Fig. 2. Schematics of the MLPG method
=
u(x)
0 v
Q _x_trial
(12)
(13)
P outlet Pout(t),
P inlet Pin(t),
where v and p are fluid velocity and pressure, vg is mesh
velocity, F is vessel inner boundary.
The 3D FSI model was solved by a commercial finite
element package ADINA (ADINA R & D, Inc., Watertown,
MA, USA). The 2D solid model was solved by MLPG method
and also by ADINA for validation purpose.
8v8n inlet, outlet
00000
00
o-=v 0 00 0
=
p(8v/8t + ((v - vg) * V) V ) = - Vp + IV2 v,
0000%0
where Fsu= Qs nu, Fst=Qsn Ft, Ms
(16) can be re-written as
Ls U Fsu U Fst'
JvPii dQx + Jvi,7ividQ- JvviinidFx
Qs
Qs
-
1s
JviniinjdFx +a F_JuiVidFx
L,
=
JvifidQx + Jv1tidFx +a Ju1vidFx
Q!
(17)
Ft
1F_
Substituting (2) and (6)-(9) into (17) leads to a local weak
form given in terms of displacement variables. This leads to a
system of equations which are solved to get the displacements,
stress and strain variables. Details can be found from [4]. A
Meshless Finite Volume Method (MFVM) was used in this
paper in which both strains and displacements were
interpolated using the same shape function [4]. The nodal
values of strains are expressed in terms of the independently
interpolated nodal values of displacements, by simply
enforcing the strain-displacement relationships directly by
collocation at the nodal points. The MFVM method, based on
the MLPG mixed approach, is more suitable for nonlinear
problems with large deformations [4-5].
(14)
j=l ,M
where aj are undetermined coefficients, qO are admissible
shape functions which take desired values at xj (similar to
FEM), and {xj} are nodal points covered by Q,
548
2007 IEEE/ICME International Conference on Complex Medical Engineering
WTI= a + b cG = 0.0631- 0.000943 cG, (R2=0.405).
(18)
where cG=Stress-Pl. The daily plaque growth rate function
(daily WTI denoted by dWTI) (scan interval 525 days) is:
dWTI = 1.20e 4 -1.796e 6 GC.
(19)
where the unit for dWPI is cm/day, and unit for cG is KPa.
III. RESULTS
Plaque Growth Functions Using Stress from 2D Models
Fig. 3 gives stacked segmented MRI slices (Fig. 3 (a)-(c))
obtained from a patient at three time points (only internal
carotid branch is shown) and corresponding slices selected for
analysis (Fig. 3 (d)-(f)). For 2D models, the computational
starting geometries (with zero stress/strain) were obtained by
shrinking in vivo MRI geometries 15-20% so that the vessel
would expand to its in vivo geometries with specified lumen
pressure. For each patient, a data set was generated which
included (for every node selected for analysis): vessel wall
thickness, values of maximum principal stress (Stress-PI) and
all other stress/strain components for all time points and slices.
For each (cross-section) slice, 100 equally spaced nodes were
selected on the lumen boundary. In this paper, vessel wall
thickness increase (WTI) was selected as the measure for
plaque progression. The statistical analysis package SAS was
used to determine possible correlation between WTI (between
successive times) and Stress-P1.
A.
(a) 1st scan
(b) 2d scan
(a) WTI vs. Stress-P1(7 slices)
(b) WTI vs. Stress-P1(6 slices)
W T I (cm)
>
0. 1-
Pearson correlation
coefficient= - 0.3773
f
0. 1-
00o~.
a
"I-
0
400
Pearson correlation
coefficient - 0.637
=
-.2
0
100
200
300
Stress-P1 (KPa)
Stress-P1 (KPa)
Fig. 4: Human carotid plaque progression (measured by WTI) correlates
negatively with Stress-P1. (a) Including the bifurcation slice, 700 points,
Pearson correlation coefficient PC = - 0.373, (p<0.0001); (b) excluding the
bifurcation slice, 600 points, PC = -0.637 (p<0.0001).
(c) 3rd scan
PC values from the other 8 patients are -0.497, -0.467, -0.156,
-0.388, -0.233, -0.228, -0.438, and -0.325, respectively, all
with p<0.001, indicating negative correlations between WTI
and Stress-P1 and that correlation coefficients vary from
patient to patient.
Plaque Growth Functions Using Solid Stress and Flow
Shear Stress from 3D FSI Model
Fig. 5 gives the plaque sample we used to construct the
3D FSI model and slices selected for data analysis. Fig. 6
gives plots of WTI vs. Stress-P1 and fluid maximum shear
stress (MSS, for definition, see [7]) using results from the 3D
FSI model (320 data points from 8 slices, time interval: 304
days). Stress-P1 at Time 2 and MSS at Time 1 were used
because they gave better correlations. The Pearson correlation
(PC) coefficients were -0.435 (p<0.0001) for Stress-P1 and 0.401 (p<0.0001) for MSS, respectively. Using MSS Time 2
values, we have PC = - 0.179 (p=0.0057). For individual
slices (internal carotid only), PC= -0.651 (p<0.0001), -0.457
(p=0.0031), - 0.453 (p=0.0033), -0.640 (p<0.0001), - 0.778
(p<0.0001) for Stress-P1, and PC= - 0.623(p<0.0001), - 0.766
(p<0.0001), - 0.784 (p<0.0001), 0.303 (p=0.057), and 0.283
(p=0.077) for MSS, respectively. The linear approximations
given by the least squares method are:
WTI= 0.0537 - 0.000572 c, (R2=0.190).
(20)
WTI= 0.0454 -0.000422xr, (W=70.161),
(21)
where x=MSS and values of Stress-P1 at Time 2 and MSS at
Time 1 were used because they gave better correlations.
Noticing WTI has statistically significant negative correlations
with both Stress-P1 and MSS, multi-variable regression
analysis was performed using both variables which led to the
following formula (units: Stress-P1: KPa; MSS: dyn/cm2) with
considerable improvement on Ri value:
WTI=0.0937-0.000761 cG - 0.000580 x (R2=0.474). (22)
The daily WTI (scan interval 304 days) is given by:
B.
(d) It Scan
(e) 2ndScan
(f) 3rd
200
*
W T I (cm)
Scan
Fig. 3. Segmented in vivo MRI data of a carotid plaque showing progression.
Magenta: lipid core; red: loose matrix; blue:Calcification; yellow: fibrous
tissue. The beginning slice is the start of bifurcation. Time interval between
two scans: 18 months.
Fig. 4 gives plots of WTI vs. Stress-P1 from 2D model
with/without the bifurcation slice (700/600 data points from
7/6 slices). The 6-slice data set gives much better correlation.
The Pearson correlation coefficient PC =-0.637 (p<0.0001)
which indicates a significant negative correlation. The PC
values for the 6 slices analyzed individually are (starting from
the bifurcating slice) -0.43 8, -0.46 1, -0.628, -0.754, -0.653 and
-0.502 respectively, all with p<0.0001.
The linear
approximation obtained for this patient (600 points) using the
least squares method is:
549
2007 IEEE/ICME International Conference on Complex Medical Engineering
model (it takes several months) due to the complexity of
plaque geometries and mesh generation process. Correlation
analysis using 2D models provides insight and motivation for
further 3D investigations [32-33].
It should be kept in mind that plaque progression is a
multi-faceted process. Other than mechanical factors, plaque
type, component size and location, cell activities, blood
conditions such as cholesterol level and other chemical
conditions, inflammation and lumen surface condition may all
have considerable impact on plaque progression.
Investigations could follow different channels from different
disciplines and use different modalities. Findings from all the
channels could be integrated together to obtain better and
more thorough understanding of the complicated
atherosclerotic progression process.
The long term goal of our research is to develop models
and non-invasive methods to better understand the
mechanisms governing plaque progression and rupture, and
make predictions which can be used in patient screening and
other potential clinical applications. The 3D model based on
in vivo MRI data and the proposed new hypotheses for plaque
progression could serve as starting points for many further
investigations. Measurements of plaque component material
properties, circumferential zero-stress condition and
anisotropic properties were not included because they are not
available under in vivo conditions with current technology and
were not included in the current model. Overall, in vivo
patient-specific data are normally limited by what is available
from current technology and in clinical practice. We are still
at the modeling and feasibility study stage, introducing proper
models, performing sensitivity studies, gathering initial data
for further investigations.
(23)
dWTI=0.000308-2.50e&6 CG_ 1.91 e6 x.
Using only the 5 internal carotid slices (200 points), we have
better correlations (all with p<0.0001):
WTI= 0.0637 - 0.000897 cG, (PC=-0.528, P7=0.279). (24)
WTI= 0.0619 - 0.000578 T, (PC=-0.525,R=0.276), (25)
WTI=0.111 - 0.00103 c - 0.000663 x, (RP=0.637). (26)
(a) Time 1 patient scan
_
i.
I~~~~~~~~
Lipi
\
(b) Time 2 scan, 10 month 1 Later
.
.
Lumen
.Z
(e StesP .plot... .
Max
(c) 3D view
.
...re
.
Min Scal
..X
Ma..j
(d) Flow Velocity Plot
)id
tre
Fig. 5. A human carotid plaque sample used to construct 3D FSI model.
(a) WTI vs. structure Stress-P1
(b) WTI vs. flow MSS
WTI (cm)
WTI (cm)
.::
0.10-
0.10
0.05
.
WTI= 0.0537
- 0.000572
Stress-P1
|.PC=-0.435,
>
0.10-
005g
A
WTI= 0.0454
0.10
!
- 0.000422
Stress-P1
....PC=-0.
'0' 401,
',(p<0.0001)
V. CONCLUSION
0.000
=.05
-.05
1.
0
100
Stress-P1 (KPa)
*.
0
For the first time, quantitative human plaque growth
functions were determined which will be used to simulate
plaque progression in our next step investigations. Use of
multi-year data leads to verifiable simulations and improved
accuracy of predictions. Our initial results support the new
hypothesis that plaque progression depends on both structural
stress/strain conditions and flow shear stress conditions.
Results presented are preliminary. More data and validations
are needed to confirm our findings.
I
50
100
150
MSS (dyn/cm2)
200
Fig. 6. Results from 3D FSI model indicate that human carotid plaque
progression (measured by WTI) correlates negatively with both structure
Stress-P1 and flow maximum shear stress (at wall).
IV. DISCUSSION
ACKNOWLEDGEMENT
Our initial results obtained from the 9 patient serial MRI
data sets indicate that low wall stress (LWS) has positive
correlations with plaque progression as measured by wall
thickness increase (WTI), and may create favorable
mechanical conditions in the plaque for further plaque
progression. Our results using 3D FSI models further indicate
that both solid stress and fluid shear stress contribute to plaque
progression and that plaque growth function using both solid
stress and fluid shear stress leads to much better agreement
with patient-tracking data than using only one of the two
(P7=0.637 for both vs. P7=0.279 for solid stress only and
P7=0.276 for flow only). Only one 3D case was included
because it is very time-consuming to construct the 3D FSI
This research was supported in part by NSF/NIGMS DMS0540684 and NIH/NIBIB-RO1 EB004759.
REFERENCES
[1] American Heart Association. Heart Disease and Stroke
Statistics - 2003 Update. Dallas, TX. American Heart
Association; 2003.
[2] American Heart Association. Heart Disease and Stroke
Statistics - 2005 Update.
[3] S. N. Atluri, The Meshless Local-Petrov-Galerkin Method for
Domain & BIE Discretizations, Tech Science Press, Forsyth,
GA, 2004.
550
2007 IEEE/ICME International Conference on Complex Medical Engineering
[4] S. N. Atluri, Z. D. Han, A. M. Rajendran, "A new
implementation of the meshless finite volume method, through
the MLPG "Mixed" approach," CMES: Computer Modeling in
Engineering & Sciences, 6 (6): 491-513, 2004.
[5] S. N. Atluri and S. P. Shen, The Meshless Local Petrov-Galerkin
(MLPG) Method, Tech Sciences Press, Encino, CA, 2002.
[6] S.N. Atluri, S.P. Shen, "The basis of meshless domain
discretization: the meshless local Petrov-Galerkin (MLPG)
method," Advances in Comput.Mathe, 23 (1-2):73-93, 2005.
[7] K. J. Bathe, Finite Element Procedures. Prentice Hall, 1996.
[8] D. Beattie, The mechanics of heterogeneous arteries:
implications for human atherosclerosis. Ph.D thesis, Georgia
Institute of Technology, Atlanta, GA, 1996.
[9] D. Beattie, C. Xu, R. P. Vito, S. Glagov S, M. C. Whang,
"Mechanical analysis of heterogeneous, atherosclerotic human
aorta," J. Biomech. Engng., 120: 602-607, 1998.
[10] L. J. Brossollet and R. P. Vito, "An alternate formulation of
blood vessel mechanics and the meaning of the in vivo
property," J. Biomechanics. 28:679-687, 1995.
[11] L. J. Brossollet and R. P. Vito, "A new approach to mechanical
testing and modeling of biological tissues, with application to
blood vessels," J. Biomech. Engng., 118:433-439, 1996.
[12] J. M. Cai, T. S. Hatsukami, M. S. Ferguson, R. Small, N. L.
Polissar, and C. Yuan. "Classification of human carotid
atherosclerotic lesions with in vivo multicontrast magnetic
resonance imaging," Circulation. 106:1368-1373, 2002.
[13] M. H. Friedman, "Arteriosclerosis research using vascular flow
models: From 2-D branches to compliant replicas," J. Biomech.
Engng. 115:595-601, 1993.
[14] M. H. Friedman, C. B. Bargeron, 0. J. Deters, G. M. Hutchins,
and F. F. Mark, "Correlation between wall shear and intimal
thickness at a coronary artery branch," Atherosclerosis, 68: 2733, 1987.
[15] V. Fuster, Co-Editors: J. F. Cornhill, R. E. Dinsmore, J. T.
Fallon, W. Insull, P. Libby, S. Nissen, M. E. Rosenfeld, W. D.
The
Vulnerable
Atherosclerotic
Wagner,
Plaque:
Understanding, Identification, and Modification, AHA
Monograph series, Futura Publishing, Armonk NY, 1998.
[16] V. Fuster, B. Stein, J. A. Ambrose, L. Badimon, J. J. Badimon,
J. H. Chesebro. "Atherosclerotic plaque rupture and thrombosis,
evolving concept," Circulation. 82 Suppl. II:II-47--II-59, 1990.
[17] D. P. Giddens, C. K. Zarins, and S. Glagov, "The role of fluid
mechanics in the localization and detection of atherosclerosis,"
J. Biomech. Engng. 115:588-594, 1993.
[18] D. P. Giddens, C. K. Zarins, and S. Glagov, "Responses of
arteries to near-wall fluid dynamic behavior," Appl. Mech. Rev.
43:S98-S102, 1990.
[19] J. H. Gillard, T. S. Hatsukami, M. Graves, C. Yuan, Editors,
Carotid Disease: The Role of Imaging in Diagnosis and
Management, Cambridge Univ Press, England, 2006.
[20] H. Huang H, R. Virmani, H. Younis, A. P. Burke, R. D. Kamm,
and R. T. Lee, "The impact of calcification on the
biomechanical stability of atherosclerotic plaques." Circulation,
103:1051-1056, 2001.
[21] T. Hughes, W. K. Liu, T. Zimmermann, "Lagrangian-Eulerian
finite element formulation for incompressible viscous flows,"
Computer Meth. in Applied Mech. Engng. 29:329-349, 1981.
[22] J. D. Humphrey, Cardiovascular Solid Mechanics, SpringerVerlag, New York, 2002.
[23] D. N. Ku, "Blood Flow in Arteries," Annu. Rev. Fluid Mech.
29:399-434, 1997.
[24] D. N. Ku, D. P. Giddens, C. K Zarins, and S. Glagov, "Pulsatile
flow and atherosclerosis in the human carotid bifurcation:
[25]
[26]
[27]
[28]
[29]
[30]
[31]
[32]
[33]
[34]
[35]
[36]
[37]
[38]
551
positive correlation between plaque location and low and
oscillating shear stress," Arteriosclerosis. 5:293-302, 1985.
F. Liu, D. Xu, M. S. Ferguson, B. Chu, T. Saam, N. Takaya, T.
S. Hatsukami, C. Yuan and W. S. Kerwin, "Automated in vivo
segmentation of carotid plaque MRI with morphology-enhanced
probability maps," Magn Reson Med. 55:659-668, 2006.
H. M. Loree, A. J. Grodzinsky, S. Y. Park, L. J. Gibson, and R.
T. Lee, "Static circumferential tangential modulus of human
atherosclerotic tissue," J. Biomechanics, 27(2): 195-204, 1994.
H. M. Loree, B. J. Tobias, L. J. Gibson, R. D. Kamm, D. M.
Small, and R. T. Lee, "Mechanical properties of model
atherosclerotic lesion lipid pools," Arterioscler Thromb.
14(2):230-4, 1994.
M. Naghavi, P. Libby, E. Falk, S. W. Casscells, S. Litovsky, J.
Rumberger, J. J. Badimon, C. Stefanadis, P. Moreno, G.
Pasterkamp, Z. Fayad, P. H. Stone, S. Waxman, P. Raggi, M.
Madjid, A. Zarrabi, A. Burke, C. Yuan, P. J. Fitzgerald, D. S.
Siscovick, C. L. de Korte, M. Aikawa, K. E. Juhani Airaksinen,
G. Assmann, C. R. Becker, J. H. Chesebro, A. Farb, Z. S. Galis,
C. Jackson, I. K. Jang, W. Koenig, R. A. Lodder, K. March, J.
Demirovic, M. Navab, S. G. Priori, M. D. Rekhter, R. Bahr, S.
M. Grundy, R. Mehran, A. Colombo, E. Boerwinkle, C.
Ballantyne, W. Insull Jr., R. S. Schwartz, R. Vogel, P. W.
Serruys, G. K. Hansson, D. P. Faxon, S. Kaul, H. Drexler, P.
Greenland, J. E. Muller, R. Virmani, P. M. Ridker, D. P. Zipes,
P. K. Shah, J. T. Willerson, From vulnerable plaque to
vulnerable patient: a call for new definitions and risk assessment
strategies: Part I. Circulation. 108(14):1664-72, 2003.
M. Naghavi, (same as above). From vulnerable plaque to
vulnerable patient: a call for new definitions and risk assessment
strategies: Part II. Circulation. 108(15):1772-8, 2003.
R. M. Nerem, "Vascular fluid mechanics, the arterial wall, and
atherosclerosis," J. Biomech. Engng. 114:274-282, 1992.
R. M. Nerem, "Hemodynamics and the Vascular Endothelium,"
J. Biomech. Engng., 115:510-514, 1993.
D. Tang, "Modeling Flow in Healthy and Stenosed Arteries,"
Wiley Encyclopedia of Biomedical Engineering, editor: Metin
Akay, John Wiley & Sons, Inc., New Jersey, Article 1525: 1-16
(2006).
D. Tang, C. Yang, J. Zheng, P. K. Woodard, G. A. Sicard, J. E.
Saffitz, and C. Yuan, "3D MRI-Based Multi-Component FSI
Models for Atherosclerotic Plaques a 3-D FSI model," Annals of
Biomedical Engineering, 32(7):947-960, 2004.
D. Tang, C. Yang, J. Zheng, P. K. Woodard, J. E. Saffitz, J. D.
Petruccelli, G. A. Sicard, and C. Yuan, "Local Maximal Stress
Hypothesis and Computational Plaque Vulnerability Index for
Atherosclerotic Plaque Assessment," Annals of Biomedical
Engineering, 33(12):1789-1801, 2005.
S. D. Williamson, Y. Lam, H. F. Younis, H. Huang, S. Patel, M.
R. Kaazempur-Mofrad, and R. D. Kamm, "On the sensitivity of
wall stresses in diseased arteries to variable material properties,"
J. Biomechanical Engineering, 125, 147-155, 2003.
C. Yuan and W. S. Kerwin, "MRI of atherosclerosis," J Magn
Reson Imaging. 19(6):710-9, 2004.
C. Yuan, L. M. Mitsumori, K. W. Beach, and K. R. Maravilla,
"Special review: Carotid atherosclerotic plaque: noninvasive
MR characterization and identification of vulnerable lesions,"
Radiology. 221:285-99, 2001.
C. Yuan, L. M. Mitsumori, M. S. Ferguson, N. L. Polissar, D. E.
Echelard, G. Ortiz, R. Small, J. W. Davies, W. S. Kerwin, and T.
S. Hatsukami. "In vivo accuracy of multispectral MR imaging
for identifying lipid-rich necrotic cores and intraplaque
hemorrhage in advanced human carotid plaques," Circulation.
104:2051-2056, 2001.