Quick Reference for Statistics in Medicine
advertisement

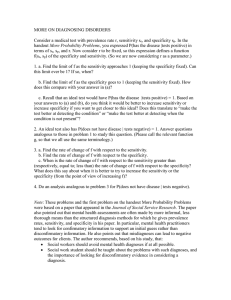
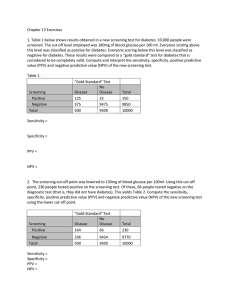
Quick Reference for Statistics in Medicine Developed from material on the SIM website by Lynsay Lane (Meds 2010) Study Designs What is it? Here, you draw a random sample of people and record information about their Crosshealth in a systematic sectional manner. You can surveys compare characteristics of people with and Observational (the researcher without a disease. studies but does These are like surveys Cohort not alter what that extend over time. (aka occurs) longitudinal This allows you to study changes and to or prospective) establish a timesequence – e.g., between cause and disease. This is a retrospective study. You begin at the CaseStudy end, by selecting control Designs people with the disease, studies and then work backwards to hunt for possible causes. Normally used in testing new drugs and treatments. A sample of patients with the condition, who meet selection criteria, are RCT randomly allocated to receive either the new treatment or the control Experimental (the researcher (standard or placebo) intervenes to treatment. Results are change reality, recorded. then observes Here, there is an what happens) intervention (ex. reduced coverage of certain services), but it is often not completely Quasiexperiments planned by the researcher. Also, people not allocated to experimental & control groups randomly. Advantages Quick; can cover whole population, giving representative information whether or not people are seeking care Prospective, so can establish causal sequence; can estimate incidence Disadvantages Based mainly on self-report (biases?); diagnostic information usually inaccurate; can’t establish causal sequence Timeconsuming; costly; attrition of cohort? Relatively cheap way of investigating causal factors Requires recall of past events (inaccurate?); controls may not be equivalent to cases This design Ethical controls for all concerns in main forms of etiological bias; good for applications; both often uses etiological selected and evaluative populations, so research issue of generalizability of the results May be more practical than RCT; can use “natural experiments” Allocation bias often significant (experimental and control groups not equivalent) Patterns observed before and after the intervention are compared. Some Concepts in Statistics Measures of central tendency: Mean – the average of a set of values Median – the value of the middle observation in a rank-ordered distribution of values. Half the observations will fall below the median and half above Measures of dispersion of a set of values: Range – the highest value minus the lowest. The simplest indicator of spread, but only considers 2 of the values; may be affected by an extreme value Variance – the average of the squared distance between each value and the mean of all values. This improves on the rage by including information form every observation Standard Deviation (SD) – the square root of the variance. It has the property that in a “normal” distribution, roughly ⅔ of all observations fall within 1 SD of the mean. In addition, roughly 95% of all observations will fall within ± 2 SD. Confidence Intervals (CI) – a range within which the true value of a parameter probably lies. The idea is that you have calculated a value from studying a sample, and want to show how accurate this estimate is for the whole population. Research reports often contain statements such as “the prevalence of inebriation among law students was 13.5% (95% CI 10.1%, 16.9%). This means that your study found 13.5% of students were drunk, and you’re 95% confident that the true prevalence lies somewhere between 10.1 and 16.9%. The bigger the sample size (n), the narrower the CI (because with a bigger sample we have more confidence in the result) Measures of Association: Relative Risk (RR) – the ratio of the risk of disease among people with a risk factor to those without. It indicates the strength of a risk, or causal factor. An RR of 1.0 means that the two incidence rates (disease among those with, and those without, the risk factor) are equal, so the factor has no effect. An RR of 2.0 would indicate that the exposed people were twice as likely to get the disease; conversely an RR of 0.5 means they were half as likely, so the exposure protected them from disease (e.g. Eat your veggies!!) Odds Ratio (OR) – in a case-control study, the OR provides an estimate of the RR. This is required because you CANNOT calculate incidence in a case-control study. As with the RR, an OR above 1.0 indicates increasing risk related to the factor, while values below 1 indicate protective effect Chi-square test – a statistical test of the association between two categorical variables Correlation coefficient – a statistical measure that shows how closely two numerical variables lie in a linear association. That is, if you know one of the values, how accurately could you predict the other by means of a straight line interpolation? The correlation coefficient can range from -1 to +1, the two extremes denoting a perfect linear relationship and 0 denoting a complete absence of relationship. Regression analysis – a family of analytical methods that extend correlations and show how much change occurs in the dependent variable for each unit change in a predictor variable. In medicine, the dependent variable is typically an aspect of health, like BP, while the independent (or predictor) variable could be a determinant of health (like the number of cigarettes smoked daily). In multiple regression, you can see how 2 or more variables can influence the dependent variable: how much effect do body-weight, cigarettes and amount of exercise affect BP? Measures of Statistical Difference: t-test – a test for comparing the mean values from two samples. It shows how confident we can be that the two mean values differ in the populations from which the samples were drawn. This could be used to evaluate the results of a drug trial for antihypertensives: how confident are we that the results of this study indicate that there would be a similar difference when the drug is applied to other samples of patients? Basic Definitions Incidence – the frequency with which something, such as a disease, appears in a particular population or area. In disease epidemiology, the incidence is the number of newly diagnosed cases during a specific time period. Prevalence – the proportion of individuals in a population having a disease. It is a statistical concept referring to the number of cases of a disease that are present in a particular population at a given time. Power – refers to the ability of a study to detect a difference that is real. Power is directly proportional to sample size. Reliability – refers to consistency or dependability. More formally, it refers of the amount of random error that occurs in making a measurement. Validity – refers to what conclusions we can draw from the results of a study, or of a measurement. When referring to a screening test, validity is commonly reported in terms of sensitivity and specificity. Sensitivity – refers to what fraction of all the actual cases of disease are detected by a test. Sensitivity is low if a test generates “false negatives” (people score negatively on the test when they should score positively). This can be serious if early treatment would have saved the person’s life. SeNsitivity is inversely associated with false Negative rate Specificity – refers to whether the test identifies only those with the disease. Specificity is low if a test generates “false positives” (people without the disease test positive for it). This can lead to worry and expensive further investigations. SPecificity is inversely associated with false Positive rate Positive Predictive Value (PPV) – probability that a positive score is a true positive Negative Predictive Value (NPV) – probability that a negative score is a true negative PPV and NPV depend on prevalence of disease, so must be determined for each clinical setting because it is variable. As prevalence goes down, PPV goes down and NPV rises (i.e. greater chance of not having the disease) Likelihood Ratio (LR) – is the likelihood that a given test result would be expected in a patient with the disease compared to the likelihood that the same result would be expected in a patient without the disease. 2 x 2 Table for Testing a Test Disease present Disease Absent Positive Test Negative Test Validity: a (TP) c (FN) b (FP) d (TN) Predictive Values: PPV = a / (a+b) NPV = d / (c+d) Sensitivity = a / (a+c) Specificity = d / (b+d) *** T = true, F = false, P = positive, N = negative False Negative rate = (1- seNsitivity), how many cases are missed by the screening test? False Positive rate = (1-sPecificity), how many are falsely classified as having the disease? Pretest Probability of Disease (prevalence of disease among the sample) = (a+c) / N, can also be expressed as… Odds of disease (based on sample) = (a+c) / (b+d), if the disease is rare. LR for positive test = Sensitivity / (1-specificity) LR for negative test = (1-sensitivity) / specificity