Document 11270055
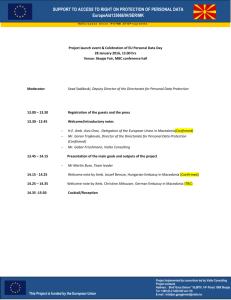
advertisement

Exploiting Fitness Trade-offs to Prevent Antifungal Drug Resistance by MASSACH ETT \N TITUTE OF TECHNOLULGY Benjamin Matteson Vincent JUL 0G 2015 B.S., Biological Sciences Stanford University (2008) LIBRARIES Submitted to the Program in Microbiology in partial fulfillment of the requirements for the degree of DOCTOR OF PHILOSOPHY in MICROBIOLOGY at the MASSACHUSETTS INSTITUTE OF TECHNOLOGY February 2015 Massachusetts Institute of Technology 2015. All rights reserved. Signature redacted Author _ _...............................................g ,Program in Microbiology Certified by Signature redacted r ell, Susan Lindquist Department of Biology Thesis Supervisor Signature e a t d .................................... i n t r redacted Accpteby by ...... S Accepted Michael T. Laub Department of Biology Chairman, Microbiology Graduate Committee 1 2 Exploiting Fitness Tradeoffs to Prevent Antifungal Drug Resistance By Benjamin Matteson Vincent Submitted to the Program in Microbiology on January 9 th, 2014 in partial fulfillment of the requirements for the Degree of Doctor of Philosophy in Microbiology ABSTRACT The evolution of drug resistance in pathogenic microorganisms is typically viewed as an inevitable consequence of the selective pressures imposed by antimicrobial agents. However, although certain drugs rapidly lose efficacy in the clinic, others remain refractory to resistance. In my thesis, I tested the hypothesis that antifungal drug resistance is the outcome of diverse tradeoffs between the fitness benefits of resistance mutations and their costs upon the adaptive cellular factors that enable the evolution of new traits. I also pursued the discovery of novel small molecule inhibitors of fungal drug resistance to further delineate the cellular processes required to support this phenotype. First, I examined the mechanisms underlying the exceptionally low incidence of resistance to the polyene antifungal amphotericin B (AmB), a mainstay of antifungal therapy for over 50 years. Genome sequencing of AmB-resistant clinical isolates and mutants evolved in the laboratory revealed several loss-of-function mutations in ergosterol biosynthesis as causes of resistance. However, deeper phenotypic profiling of these mutants revealed that they all carried massive costs for the ability to tolerate environmental stressors and deploy virulence factors. I concluded that these costs sharply limit the emergence of resistance to AmB in the clinic. AmB is also extremely toxic to patients, a feature seen in many other resistancerefractory drugs. Collaborating with a synthetic chemistry team headed by Martin Burke (University of Illinois), we demonstrated that new, nontoxic AmB analogs with improved selectivity for the target (ergosterol) still retain the extremely valuable property of evading drug resistance. This finding countered the assumption that narrowing the target specificity of a drug would enable more routes to the emergence of resistance. Separately, I conducted a high-throughput screen for small molecule inhibitors of drug resistance in Candida. This screen identified a fungal-selective inhibitor of cytochrome bcl of the electron transport chain. Collaborating with chemists (JeanBaptiste Langlois and Stephen Buchwald) and structural modelers (Raja Srinivas and Bruce Tidor), we optimized the potency and fungal selectivity of this compound. Moreover, these studies provided insight into the role of mitochondrial respiration in fungal host adaptation, immune evasion, and virulence in an animal model. Finally, in the appendix I describe work in progress on the discovery and characterization of a compound that selectively kills Candidaby targeting the mitochondrial phosphate transporter. Resistance to this agent sensitizes fungi to azoles and bears severe fitness costs, reminiscent of the case of AmB. Thesis supervisor: Susan Lindquist Title: Professor of Biology 3 4 Acknowledgments Completing the work described in this thesis was only possible through the tremendous support of many generous people. First, Susan Lindquist has been an encouraging and supportive advisor and scientific guide to me. She has taught me to focus my efforts on the most important implications of my research and not get sidetracked with minor concerns. She has also made it possible for my work to have the greatest impact it can through enabling some remarkable collaborations for me. I am extremely lucky as a graduate student to have worked on such important projects with the full support of many other talented researchers, and she has made all of that happen. I am also indebted to Sue for creating a wonderful lab environment. The person most responsible for this is Brooke Bevis, who works tirelessly to make the lab run smoothly. I can't even begin to thank Luke Whitesell for the amazing technical training, scientific guidance, and simply good-natured generosity he has provided to me. Ruthie Shouval also went to great lengths to help me when I needed it. The Lindquist lab has been a remarkable place for camaraderie and lighthearted fun over these past five and a half years. As time passes, I will remember the great friendships I've made here as the best part of my experience. But even more than that, the science that my labmates do on a daily basis inspires me to do better with my own work. I would also like to thank other MIT faculty, most importantly my thesis committee, for offering such constructive and supportive comments during our meetings. I would also like to thank Alan Grossman for starting the Microbiology Ph.D. program and keeping such a humble and approachable personality. Finally, above all, I am most indebted to my parents. As they both earned doctorates some 40 years ago, they instilled in me that the pursuit of knowledge is the highest aspiration of mankind. They also know the struggles and pains of surviving graduate school, and kept me afloat all of these years. Mom and Dad invested in my education from an early age. They have supported everything I have ever sought to do, not because they want me to be someone in particular, or want me to be successful, but only out of love. The greatest joy of my life is to know that my achievements serve to honor my parents, their parents, and everyone that came before and made all of this possible. 5 6 Table of Contents Page Summary 3 Acknowledgments 5 Table of Contents 7 Chapter One: Introduction 11 Chapter Two: Fitness Trade-offs Restrict the Evolution of Resistance to Amphotericin B Abstract Introduction Results Discussion Methods References Figures 36 37 39 41 54 58 68 73 Chapter Three: Non-toxic Antimicrobials that Evade Drug Resistance Abstract Introduction Results Discussion Methods References Figures 98 99 99 101 108 109 119 124 Chapter Four: A Fungal-Selective Cytochrome bcl Inhibitor Impairs Virulence and Prevents the Evolution of Drug Resistance Abstract Introduction Results Discussion Methods References Figures 129 Chapter Five: Conclusions and Future Directions 179 Appendix A: Selective Targeting of the Mitochondrial Phosphate Carrier Yields an Antifungal Therapeutic Strategy that Evades Resistance 191 Appendix B: Curriculum Vitae 205 7 130 131 134 146 149 168 171 8 List of Figures and Tables Page Figures Chapter Two Figure 2.1: Mechanisms of AmB resistance in Candida 73-74 Figure 2.2: AmB-resistant strains critically depend on high levels 75 of Hsp90 function for survival Figure 2.3: Constitutive stress response activation in AmB-resistant 76-77 strains Figure 2.4: AmB-resistant strains are hypersensitive to the stresses 78-79 of the host environment Figure 2.5: AmB-resistant strains are defective in filamentation 80-81 and adhesion Figure 2.6: AmB-resistant strains are avirulent in a mammalian model 82-83 of disseminated candidiasis Figure S2.1 Transposon insertion and heterozygosity analysis in 84 AmB-resistant C. albicans Figure S2.2 : AmB-resistance mutations and heterozygosity analysis in AmB-resistant C. tropicalis 85-86 Figure S2.3 : Heterozygosity analysis of in-vitro-evolved series 87-88 Figure S2.4 : Minimal inhibitory concentrations of Hsp90 inhibitors 89-90 and cytotoxic compounds Figure S2.5 : Validation of additional mutant strains 9 91-92 Table S2. 1: Strains used in this study 92-93 Table S2.2: Oligonucleotide sequences used in this study 94-97 Chapter Three Figure 3.1: Synthesis of AmB urea derivatives 124 Figure 3.2: Sterol binding, antifungal, and human cell toxicity 125 of AmB ureas Figure 3.3: Efficacy and toxicity of AmB ureas in mice 126 Figure 3.4: Characterization of mechanisms and costs of resistance to AmB ureas 127-128 Chapter Four Figure 4.1: Discovery of Inz-266 by high-throughput screening 171 Figure 4.2: Inz-266 is a fungal-selective cytochrome B inhibitor 172 Figure 4.3: Structural analysis of Inz-266 binding to cytochrome bc 1 173 Figure 4.4: Optimization of Inz-266 through medicinal chemistry 174 Figure 4.5: JBL- 182 renders fluconazole cidal and reduces the 175 emergence of resistance Figure 4.6: Inhibition of cytochrome bc 1 by JBL- 182 prevents 176 adaptation to suboptimal carbon sources Figure 4.7: Loss of cytochrome bc 1 severely reduces fungal virulence 177 and fluconazole tolerance, but increases brain colonization Figure 4.8: Broad-Spectrum activity of JBL- 182 10 178 Chapter One: Introduction 11 FUNGAL PATHOGENS OF HUMANS Epidemiologv and Pathogenesis of Fungal Infection Fungi are ubiquitous residents of the human body. In healthy humans, the skin, oral cavity, gastrointestinal tract and genital mucosa harbor a great diversity of fungal communities [1]. Fungal outgrowth in these non-sterile sites results in some of the most frequent infections of otherwise healthy humans. Worldwide, nearly 2 billion people are afflicted annually with superficial infections of the scalp, nails, and skin (Brown et al, 2012). Over half of women experience vaginal yeast infections at some point in their reproductive years [2]. Oral yeast infections (thrush) are a common occurrence in both healthy babies and denture-wearers. Although infections of these bodily surfaces are unpleasant, they are generally quite minor medical concerns and typically resolve with brief and facile treatment. Invasive fungal infections of sterile body sites, on the other hand, are among the most morbid and severe maladies of mankind. Current estimates suggest that over 1.5 million people worldwide die of invasive fungal infections annually, placing fungi among the most deadly pathogens on earth [3]. Such invasive fungal infections are most common in severely immunocompromised individuals, including those with uncontrolled HIV, patients taking immunosuppressants for solid organ transplants, hematopoietic stem cell transplant recipients, or chemotherapy patients. However, fungi can also invade the bloodstream of (relatively) healthy patients undergoing abdominal surgery or central venous catheter implantation [4]. Depending on the fungal species responsible, infections can target the lungs, brain, bloodstream, kidneys, or liver, and cause lethality due to either major organ failure or sepsis. Mortality rates for invasive fungal infections 12 range from 30%-90%, depending on the species, body site, and underlying condition of the patient [5]. This high rate of mortality reflects several problems in the clinical management of these diseases. Diagnosis of the precise infecting pathogen typically comes too late or not at all, and clinicians are forced to rely on broad-spectrum empiric therapy [3]. More importantly, available antifungal drugs suffer from a litany of limitations in their patterns of systemic distribution, fungicidal efficacy, and patient toxicity [6]. Fungal pathogens often hide in niches that are poorly penetrated by these agents, deploy adaptive stress responses to tolerate drug-induced toxicity, and even acquire mutations that desensitize them to the action of the drug [7-9]. Although a wide variety of fungal species can cause invasive infections, more than 90% of deaths are caused by members of the Cryptococcus, Aspergillus, and Candida genera [3]. Cryptococcus neoformans and Cryptococcusgattii are yeast-like fungi that typically enter the body through inhalation and then invade the central nervous system in susceptible hosts. These pathogens successfully evade host defenses by hiding within a thick polysaccharide capsule that is invisible to cells of the immune system. Aspergillus species are ubiquitous environmental molds inhaled by most humans daily, but in the severely immunocompromised, they cause a chronic pulmonary disease that is rarely treatable. Disseminated Aspergillus infections also kill thousands of transplant recipients annually [10]. Candidaalbicans, however, is the fungal species responsible for the greatest number of invasive fungal infections, and is the main focus of my work. 13 Biology and Virulence of Candida albicans C. albicans is remarkable among pathogens for the great diversity of surfaces and organs it readily infects. Unlike most other fungal pathogens, C. albicans has no wellestablished environmental niche, but mainly exists as a commensal of warm-blooded animals [11]. C. albicans is present in large numbers in the gastrointestinal flora, but can also be detected in the mouth and vagina of healthy individuals. In these sites, Candida is typically in equilibrium with host immune factors that limit fungal growth [1]. However, changes in the structure and composition of these environments can lead to rapid and robust fungal outgrowth. In HIV patients, the decline in CD4+ cell counts tips the balance in favor of fungi and leads to frequent cases of thrush. Treatment with broadspectrum antibacterial drugs also allows Candidato surpass its competitors and dominate certain niches, causing secondary infections [12]. Although C. albicans is considered a model fungal pathogen, its genetics and reproductive cycle of are highly complex, and for many years this complexity limited the progress of research. C. albicansgenerally grows as an obligate diploid, but haploid strains of C. albicanshave been described recently [13]. However, all known haploid strains are slow-growing and avirulent. Meiosis has never been observed in C. albicans. Instead, a cryptic mating process proceeds through the joining of two different diploid cell types, white and opaque, and the formation of a tetraploid intermediate [14]. This tetraploid then loses chromosomes by a poorly understood process, regenerating the diploid. Although the lack of a haploid stage in its life cycle has hindered the development of genetic tools for this organism, the creation of auxotrophic markers has enabled the generation of deletion mutants and heterologous expression sites [15]. 14 Nevertheless, diploidy prevents facile loss-of-function genetic screens, and partially as a result, the vast majority of gene products are poorly understood. Further difficulties include a modified genetic code and the absence of stably replicating plasmids. Despite these difficulties, the growing importance of C. albicans as a pathogen has fueled the pace of research. ANTIFUNGAL DRUGS: MECHANISMS OF ACTION AND RESISTANCE Azoles Azoles are by far the most widely used antifungal agents due to their safety and oral bioavailability, which enables outpatient and prophylactic use. They are generally split into two groups. The first of these is the imidazoles (including clotrimazole, ketoconazole, and miconazole), which are only useful for the treatment of skin, hair, and vaginal infections. The second group comprises the first-generation triazoles, including fluconazole, which is extremely broadly used in the treatment of mucosal candidiasis. Newer triazoles (in particular voriconazole) have a broader spectrum of activity, and have transformed the treatment of life-threatening aspergillosis [16]. Azoles act through inhibition of Erg IIp (lanosterol 14-alpha-demethylase), also known as Cyp5 1 p [6]. This heme-containing protein catalyzes the removal of a methyl group from lanosterol in the sterol biosynthetic pathway. Blocking Erg IIp function causes the accumulation of 14-alpha-methylated sterols, which perturb diverse membrane functions and prevent cell growth. While newer azoles are fungicidal against Aspergillus, they are generally only fungistatic drugs against most pathogenic fungi, especially 15 Candida. The inability of azoles to kill Candidaallows these infections to persist and evolve resistance to treatment. Resistance to Azoles The broad use of azole antifungals to treat recurrent thrush at the height of the AIDS epidemic (before the broad introduction of improved antiretroviral therapy) led to frequent reports of resistance [17]. As Candidais a commensal, rarely spreads between patients, and appears to lack horizontal gene transfer, resistance typically evolves de novo [18]. However, the broad use of azoles against agricultural pathogens appears to select for mutants in Aspergillusfumigatuswith reduced susceptibility to these drugs, causing grave clinical concern and a dire need to understand mechanisms of resistance [19]. Azole resistance emerges through multiple mechanisms. Alterations in the azole binding site of Ergi lp, including the R467K and G464S mutations, are frequently detected in resistant isolates [18]. These mutations (and many others) alter the interaction between azoles and the heme cofactor of the target enzyme, decreasing its affinity for the drug [20]. Mutations in the transcription factor Upc2, which controls sterol biosynthesis, can also contribute to azole resistance [21]. Increased copy number of ERG] 1, which can occur through formation of a specific isochromosome, is another mechanism frequently detected in clinical isolates [22]. The most intractable form of azole resistance occurs through upregulation of multidrug efflux pumps, specifically members of the ATPbinding-cassette (ABC) family and the major facilitator superfamily. Upregulation of ABC efflux pumps, including Cdrlp and Cdr2p in C. albicans, can occur through gain of function mutations in the Taclp transcription factor that cause constitutive activation 16 [23]. All of these mechanisms appear to have generally neutral effects on the fitness and virulence of C. albicans, explaining their frequent emergence [24]. Although it has been studied much less than Candida,Aspergillus evolves resistance to azoles through many of these same mechanisms. Resistance to azoles can also occur through loss of function mutations in the ERG3 gene, encoding sterol delta 5-6 desaturase. These mutations result in the detoxification of the methylated sterol produced when Ergi ip is inhibited [25]. However, these mutations are rarely observed in the clinic, likely because they reduce the virulence of C. albicansin most, but not all, strain backgrounds [26,27]. Polyenes Amphotericin B (AmB) is the only polyene used for invasive fungal infections. It has the broadest spectrum and the most rapid fungicidal activity of any antifungal agent. Amphotericin has an unusual mode of action for an antimicrobial: direct small moleculelipid interaction, targeting the fungal sterol ergosterol [28]. Whereas the antibacterials daptomycin and colistin also directly bind to lipids and can insert themselves in the membrane, recent work suggests AmB acts differently [29]. It had long been assumed that AmB kills fungi by forming ion channels within the plasma membrane. However, chemical synthesis revealed that ion channel formation and cell killing are dissociable [30]. Further detailed mechanistic studies revealed that AmB does not insert into membranes, but instead remains on their surface, where it forms large aggregates. These aggregates have a high affinity for ergosterol and rapidly extract the sterol from fungal membranes, permeabilizing and killing cells [29]. Key features of this "sterol sponge" 17 model, including proof of existence of AmB aggregates in vivo and elucidation of their structure, remain to be demonstrated. Nevertheless, it presents an attractive explanation for many of the unexplained phenomena observed with this drug. An inescapable aspect of the clinical experience with AmB, however, is its severe, dose-limiting, and occasionally fatal toxicity to patients [31]. AmB is only partially selective for ergosterol over its human analog, cholesterol [32]. AmB binding to cholesterol in cell membranes can cause irreversible renal damage, which presents a challenge as many patients with fungal infections already have limited kidney function. Newer formulations of AmB in combination with lipids have mitigated, but not eliminated this issue. In addition, due to its narrow therapeutic index, blood levels of AmB must be kept very low, which runs counter to the high and repeated dosing strategies used with most antimicrobials [33]. Resistance to Polyenes AmB is unique amongst antifungals (and antimicrobials in general) in that resistance to this agent is exceptionally rare. Repeatedly, large-scale resistance surveillance studies have identified very few isolates with strong resistance (<1% of all isolates) [34]. The rarity of resistance is remarkable when it is considered that AmB has been administered to millions of patients over a span of 50 years, and almost always as monotherapy. Previous studies of AmB resistance have revealed that disruption of ergosterol biosynthesis genes (including ERG6 and ERG3/ERG 1I simultaneously) can confer resistance in vitro [35]. These isolates produced altered membrane sterols, which presumably have lower affinity for AmB. Several studies have also revealed rare 18 Candida mutants recovered in the clinic with amphotericin resistance and altered sterol profiles. However, the relevance of these mutations to the outcome of therapy in the patient remains unclear [36,37]. Echinocandins Echinocandins are natural product derivatives that target the Fks Ip and Fks2p protein complex that synthesizes beta-1,3 glucan, a major component of the fungal cell wall [38]. These agents lack oral bioavailability and central nervous system penetration, and have a generally narrower spectrum of activity than other agents. Plasma membrane protein complexes that synthesize large polysaccharides are notoriously difficult to study. Hence, little is known about the direct action of echinocandins on their target. However, their potent fungicidal activity against Candidahas rendered them the drug of choice for severe invasive candidiasis. One aspect of echinocandin activity that likely improves their efficacy is their synergistic activity with the host immune system. Inhibition of beta- 1,3 glucan synthesis exposes polysaccharides that are normally buried, rendering the fungi more immunogenic. This leads to hypersecretion of cytokines when these cells are encountered by macrophages [39]. This effect likely enhances both innate and adaptive responses to pathogenic fungi, promoting clearance of the infection. Resistance to Echinocandins Although they have only been in clinical use for 10 years, resistance to echinocandins is becoming a major clinical issue in certain species (particularly Candidaglabrata). The most commonly observed mechanism of resistance derives from mutations in two "hot- 19 spot" regions of the FKS 1 gene encoding the glucan synthase target [40], which decrease the sensitivity of glucan synthase activity to the drugs. Several of these mutations decrease the virulence of C. albicanswhen homozygous, which may prevent their dissemination [41]. Recent efforts have also demonstrated that increased chitin synthesis, mediated through induction of cell wall stress response pathways, protects fungi from echinocandins [42,43]. NEW IDEAS TOWARDS THE DISCOVERY OF ANTIFUNGAL AGENTS Introduction to the problem Clinical therapy of invasive fungal infections currently relies on agents originally discovered decades ago. The newest class, the echinocandins, were discovered in the 1970's and spent nearly 30 years in development prior to approval [33]. Azoles were discovered even earlier, and have been in use since the 1980's. AmB entered the clinic in 1963, before many of the transplant procedures and diseases that predispose to invasive fungal infection even existed. None of these agents are ideal in terms of patient toxicity, spectrum of activity, prevention of resistance, ease of dosing, and rapid fungicidal efficacy against the most obdurate pathogens. But despite the high clinical demand for improved agents, no new classes of antifungal have even reached phase III trials in the last 12 years. Economics and regulatory challenges certainly deserve some of the blame for the paucity of new antifungals. However, even promising preclinical agents are rarely descried, suggesting that scientific difficulties are the main limitation. New ideas and methodologies are certainly in order. 20 In this section I will briefly outline the difficulties encountered in the pursuit of novel antifungals (and antimicrobials in general), and the limitations of commonly employed strategies. I will then shift to a discussion of new approaches in antifungal discovery including 1) ideas to reinvigorate natural product discovery, 2) targeting virulence factors, 3) targeting microbial stress responses, and 4) disabling fungal adaptation to nutrient deprivation by the host. I will then revisit many of these issues in the conclusion of this thesis to discuss them in light of my findings. Challenges with traditional approaches to the discovery of antimicrobials Throughout the golden age of antibiotic and antifungal discovery in the 2 0 th century, arguably every class of agent was discovered by phenotypic screening for, or serendipitous observation of, growth-inhibitory effects on whole cells. However, in the 1990's and 2000's, the availability of whole-genome sequences and essential gene lists ushered in a paradigm-shift in antimicrobial discovery strategies [44]. The new approach sought to identify gene products that were essential for viability, present in a broad spectrum of fungi, absent in humans, and amenable to high-throughput screening for small molecule inhibitors. However, this approach has failed to generate even one novel class of FDA-approved antibacterial or antifungal [6]. Though few accounts of antifungal drug discovery efforts in this arena are documented in the literature, substantial detail is available on the failure of targeted approaches to discovering antibacterials [45]. Strangely, the rate of hit identification in screens against purified bacterial proteins has been much lower than for purified mammalian proteins. This unexpected finding may reflect intrinsic differences in 21 bacterial protein structure. More interestingly, it might be the result of evolutionary pressures these proteins have been subjected to in the wild, where they must evade inhibition by secondary metabolites secreted by competitor organisms. Nevertheless, a number of effective inhibitors of essential microbial enzymes with excellent potency in vitro have been discovered, yet never became drugs. A consensus explanation for these failures is the difficulty posed in engineering the microbial cell permeability upon these compounds. Known antimicrobial classes have highly discordant physical properties compared to the scaffolds present in synthetic libraries used in high-throughput screening [33,46]. The capacity to pass through microbial cell walls and membranes while avoiding drug efflux pumps is rare in purely synthetic molecules. Indeed, the only purely synthetic classes of antifungals or antibacterials in broad use are azoles, oxazolidinones, sulfonamides, and quinolones (with the exception of anti-tuberculosis agents). Alas, in advancing novel classes of antifungals and antibacterials to approval, whole-cell phenotypic screens have failed as well [45,47]. Novel synthetic molecules with useful single-agent antimicrobial activity appear to be lacking in pharmaceutical screening collections, perhaps due to their limited structural diversity and the physical properties of these compounds. Certainly, natural products are a much better source of chemical diversity, and the production of secondary metabolites that kill nearby competitors is a common survival strategy in the microbial world. Moreover, these compounds are naturally capable of passing through microbial membranes, and their biosynthesis may have evolved to prevent resistance mechanisms. Hence, it is extremely disappointing that natural product-based screening efforts have also come up short [47]. The complexity of natural product extracts frequently 22 complicates the initial screening process. Many hits contain substructures that cause unfavorable pharmacological properties in man, and their chemical complexity renders them intractable to synthetic optimization. Most alarmingly, the vast majority of natural product screening efforts now result in the rediscovery of known classes of antimicrobials, or new structures active on old targets. Reinvigorating Natural Product Discovery Despite the difficulties delineated above, great hope for the future of antimicrobial natural product discovery lies, ironically, in genomics. Recent advances have enabled prediction of the structures of secondary metabolites produced by an organism by sequencing the DNA that encodes its polyketide synthases and other biosynthetic clusters [48]. Using these methods, the biosynthetic potential of DNA extracted from any environmental source can be computationally determined, enabling researchers to harness new sources of chemical diversity from unculturable organisms. The DNA can then be transformed into tractable host strains for the production and isolation of potentially useful biosynthetic products, then tested for antimicrobial effects [49]. Though still unproven in its clinical utility, the potential of this method to expand the universe of useful antimicrobial chemical matter is immense. In addition, advances in diagnostics may enable more natural product antifungals to reach the clinic. The inability to rapidly diagnose the species infecting a patient has restricted antifungal discovery efforts to the development of broad-spectrum agents. Due to this requirement, potent natural product antifungals with narrow-spectrum activity have been discovered and promptly abandoned [47]. These agents could be resurrected if 23 rapid, sensitive, and affordable diagnostic procedures to identify the infecting organism reach the clinic and gain wide use. New diagnostic technologies utilizing sequencing and RNA probe-based methodologies may enable the realization of this goal [50]. Targeting Virulence Factors Historically, non-essential targets and compounds that lack significant singleagent growth-inhibitory activity in vitro have been ignored in the development of antimicrobial agents (with the exception of beta-lactamase inhibitors). However, many more factors are required for microbial pathogenesis in vivo than are required for mere growth in vitro, opening up many more targets and potentially much more chemical space for drug discovery. There are generally two broad types of non-essential targets that could be exploited: "active" mechanisms that enable damage of host tissue (including adhesion, invasion, and toxin secretion) and "passive" mechanisms that simply enable microbial survival within host environments [51]. Inhibitors of active virulence processes promise a tremendous advantage: they might not select for resistance, since many virulence strategies are not required for the growth of the individual cells employing them. However, targeting active virulence factors in pathogenic fungi may prove insufficient. Many of the most dangerous fungal pathogens are adapted to life outside of the host environment. These pathogens cause disease simply by growing and consuming host tissues; they have not evolved elaborate virulence mechanisms. Moreover, since invasive fungal infections typically occur in patients with very limited immune function, antifungal agents need to actively kill their target pathogen to be curative. Nevertheless, 24 a virulence-factor-targeted agent, such as an inhibitor of filamentation in Candida albicans, could be useful in combination with a more traditional growth-inhibiting antifungal [52]. Extracellular adhesins such as Als3 that mediate tissue invasion could also present excellent targets for tractable monoclonal antibody therapies, which could prevent C. albicans from reaching protected niches such as the brain [53]. Unfortunately, many of these active virulence processes are not broadly conserved across fungal species. Given the severe limitations in precise diagnosis of infecting organisms before the initiation of therapy, identifying broad-spectrum anti-virulence strategies is of the highest importance. Targeting Stress Responses More promising are strategies targeting highly conserved stress response proteins that enable adaptation to challenges encountered in the host environment. The large scale identification of genes essential in vivo has recently been enabled by barcode-tagging methods [54]. More targeted approaches, examining individual stress response pathways, have also contributed greatly to our understanding of stress adaptation within the host. One such pathway is the HOG (High Osmolarity Glycerol) MAP kinase pathway [55]. This pathway transduces changes in osmolarity and oxidative stress into a broadly adaptive transcriptional program, through increased synthesis of osmolytes and other protective factors [56]. Loss of Hogi renders C. albicanscompletely avirulent in mice, even though it has no effect on growth under normal conditions in vitro. Of greatest promise as targets, however, are stress-response proteins that are not only required for survival in vivo but also for tolerance of (and resistance to) antifungal 25 treatment. Two such proteins that have emerged in the literature are calcineurin and protein kinase C (PKC) [57-59]. Calcineurin is a Ca2+/Calmodulin activated phosphatase that responds to membrane perturbation and other stresses by dephosphorylating substrate proteins, including the transcription factor Crz . In C. albicans, deletion of the catalytic subunit of calcineurin renders the fungus avirulent, and even prevents survival in serum [60]. Deletion of calcineurin (or inhibition with FK-506 or cyclosporine) also renders typically fungistatic ergosterol biosynthesis inhibitors fungicidal [61]. Many of these same phenotypes are also seen in cells lacking PKC1, a critical regulator of the cell wall integrity pathway [57]. Critical to the function of PKC, calcineurin, and other signal transduction pathways is Hsp90 [62]. Hsp90 is a broadly conserved and highly abundant molecular chaperone that aids in the folding and stabilization of a long list of metastable client proteins [63]. This list is highly enriched for signal transducers and proteins that undergo a conformation change in response to stimulation by a ligand or activating partner. In yeast, Hsp90 is produced in great excess of the amount needed for survival under normal conditions, and may act as a protein homeostasis buffer that allows for rapid adaptation to stress [64,65]. The excess buffer of Hsp90 also enables novel mutations to have immediate phenotypic consequences, including oncogenic mutations in kinases [66]. By responding to the increased demand for signaling from stress response proteins, Hsp90 enables resistance pathways to multiple antifungals. Inhibition of Hsp90 blocks the emergence of azole resistance in C. albicans, and restores sensitivity to azoles in mutants that had previously evolved resistance in the clinic [67]. Hsp90 also promotes resistance to echinocandins in fungi separated by a billion years of evolution [68]. High 26 levels of Hsp90 are also required for fungal virulence in mice (in the absence of antifungal treatment) in both C. albicans and A. fumigatus [69,70]. Attempts to pharmacologically target these pathways, however, have not yet proven fruitful. PKC, Calcineurin, and Hsp90 have central roles in cell-mediated immunity in humans, and their inhibition during a severe infection would likely be counterproductive. As such, fungal-selective inhibitors are needed, and these have not yet advanced to the clinic. Targeting Metabolic Adaptation Unexpectedly, the work in this thesis uncovered a critical and pharmacologicallytargetable role for central carbon metabolism and mitochondrial respiration in the pathogenesis and drug resistance of C. albicans. Recent work from many groups has established that carbon deprivation is an underappreciated form of stress that fungal pathogens encounter in the course of infection [71,72]. C. albicans is capable of colonizing such nutritionally disparate body sites as the mouth, vagina, bloodstream, kidney, brain, skin, nails, and eyes. Moreover, even within a single niche, Candidacan encounter rapidly fluctuating environmental conditions, including infiltration by immune cells. As the ability to convert environmental nutrients into biomass and ATP (and thus new cells) is the fundamental selective pressure on all organisms, a litany of mechanisms exist to enable fungi to optimally exploit their surroundings. Such mechanisms may present promising new opportunities for selective therapeutic intervention. Fermentable sugars, such as glucose, are the preferred general carbon source of yeasts. However, sugars are rarely abundant in host microenvironments (typically 0.1- 27 0.2%), and in some niches they are completely absent [73]. Though the dominant carbon source in each niche is poorly defined, they include lactate, acetate, amino acids, and fatty acids [74]. In the absence of abundant sugars, Candida relies heavily on gluconeogenesis from these suboptimal carbon sources for many vital processes. One such process is the biosynthesis of the carbohydrate-rich cell wall. In fact, carbon source utilization dictates the very structure of the fungal cell wall and thus has critical consequences for stress tolerance and immunogenicity [75]. Candidaencounters the most severe nutrient deprivation upon engulfment into phagocytic immune cells (macrophages or neutrophils), where sugars are absent [76]. To tolerate this environment and escape, C. albicans induces the glyoxylate cycle, enabling metabolism of non-fermentable 2-carbon compounds including acetate [77]. Indeed, the role of this pathway is underscored by its deployment by both bacterial and fungal pathogens, in which it is required for full virulence. A critical requirement for the successful utilization of all non-fermentable carbon sources is ATP production from the mitochondrial electron transport chain. In high-glucose conditions, the inhibition of mitochondrial respiration only partially impairs proliferation in C. albicans [78]. However, when sugars are scarce, mitochondrial function is required to fuel the TCA cycle, enable gluconeogenesis, and produce ATP through oxidative phosphorylation. Given the high conservation of most mitochondrial proteins from fungi to humans, they are rarely mentioned as putative antifungal targets. Previous efforts have focused on identifying mitochondrial proteins unique to fungi, including the Goal protein unique to the Candidaclade, or the glyoxylate cycle, which exists across diverse microbial pathogens but is absent in mammals [77,79-81]. 28 However, efforts to unlock therapeutic value through pharmacological targeting of these metabolic processes have been limited. Many pathogen-specific mitochondrial proteins are not conserved across a broad enough spectrum of fungi, or are not druggable by small molecules. Moreover, given the impressive metabolic flexibility of many pathogenic fungi, inhibiting any one pathway of metabolic adaptation may be rapidly bypassed by upregulation of others. Indeed, mutants lacking the glyoxylate are attenuated, but not avirulent [82]. Proteins with central, conserved, and irreplaceable roles in multiple metabolic pathways, such as electron transport chain complexes, may present more attractive targets. Unfortunately, these factors are generally highly conserved from yeast to man. Nevertheless, ample evidence exists from the history of available antifungals and antibiotics that targeting processes still present in humans can yield therapeutics with tremendous clinical value. For example, the target of azoles is well conserved in humans, many classes of antibiotics target the ribosome, and the new anti-tuberculosis agent bedaquiline targets ATP synthase. Identifying the atomic-level differences in such central and essential proteins between their pathogen and human homologs would provide a critical path forward for the development of new agents. SUMMARY Decades of study have provided valuable insights into the mechanisms by which pathogenic fungi cause disease, the mechanisms by which antimicrobial drugs kill fungi, and the mechanisms that allow fungi to resist these agents. Yet, our understanding of why resistance emerges rapidly to some drugs and not others remains limited. Moreover, feasible strategies for the discovery of new agents active against drug resistant pathogens 29 are lacking. In this thesis, I explore the fitness costs of drug resistance mutations as both an evolutionary explanation for the clinical rates of resistance and also a powerful tool to inform the discovery of new agents. I also used unbiased screening to discover new small molecules that disarm the adaptive cellular responses that enable resistance. With this work, I seek to provide both a fundamental understanding of the tradeoffs inherent in the evolution of drug resistance as well as specific targets and strategies for development of new agents. Examining drug resistance as a form of adaptation to genetic and environmental change thus provides deep insight into the mechanisms that promote and restrict the rapid evolution of new traits. References 1. Underhill DM, Iliev ID (2014) The mycobiota: interactions between commensal fungi and the host immune system. Nat Rev Immunol 14: 405-416. 2. Sobel JD (2007) Vulvovaginal candidosis. Lancet 369: 1961-1971. 3. Brown GD, Denning DW, Gow NA, Levitz SM, Netea MG, et al. (2012) Hidden killers: human fungal infections. Sci Transl Med 4: 165rv1 13. 4. Andes DR, Safdar N, Baddley JW, Playford G, Reboli AC, et al. (2012) Impact of treatment strategy on outcomes in patients with candidemia and other forms of invasive candidiasis: a patient-level quantitative review of randomized trials. Clin Infect Dis 54: 1110-1122. 5. Horn DL, Fishman JA, Steinbach WJ, Anaissie EJ, Marr KA, et al. (2007) Presentation of the PATH Alliance registry for prospective data collection and analysis of the epidemiology, therapy, and outcomes of invasive fungal infections. Diagn Microbiol Infect Dis 59: 407-414. 6. Odds FC, Brown AJ, Gow NA (2003) Antifungal agents: mechanisms of action. Trends Microbiol 11: 272-279. 7. Desai JV, Mitchell AP, Andes DR (2014) Fungal biofilms, drug resistance, and recurrent infection. Cold Spring Harb Perspect Med 4. 8. Cowen LE, Sanglard D, Howard SJ, Rogers PD, Perlin DS (2014) Mechanisms of Antifungal Drug Resistance. Cold Spring Harb Perspect Med. 9. Kontoyiannis DP (2012) Invasive mycoses: strategies for effective management. Am J Med 125: S25-38. 10. Neofytos D, Fishman JA, Horn D, Anaissie E, Chang CH, et al. (2010) Epidemiology and outcome of invasive fungal infections in solid organ transplant recipients. Transpl Infect Dis 12: 220-229. 30 Chen C, Noble SM (2012) Post-transcriptional regulation of the Sefl transcription factor controls the virulence of Candida albicans in its mammalian host. PLoS Pathog 8: e1002956. 12. Xu J, Schwartz K, Bartoces M, Monsur J, Severson RK, et al. (2008) Effect of antibiotics on vulvovaginal candidiasis: a MetroNet study. J Am Board Fain Med 21: 261-268. 13. Hickman MA, Zeng G, Forche A, Hirakawa MP, Abbey D, et al. (2013) The 'obligate diploid' Candida albicans forms mating-competent haploids. Nature 494: 55-59. 14. Forche A, Alby K, Schaefer D, Johnson AD, Berman J, et al. (2008) The parasexual cycle in Candida albicans provides an alternative pathway to meiosis for the formation of recombinant strains. PLoS Biol 6: el 10. 15. Noble SM, Johnson AD (2005) Strains and strategies for large-scale gene deletion studies of the diploid human fungal pathogen Candida albicans. Eukaryot Cell 4: 298-309. 16. Perfect JR, Marr KA, Walsh TJ, Greenberg RN, DuPont B, et al. (2003) Voriconazole treatment for less-common, emerging, or refractory fungal infections. Clin Infect Dis 36: 1122-1131. 17. Rex JH, Rinaldi MG, Pfaller MA (1995) Resistance of Candida species to fluconazole. Antimicrob Agents Chemother 39: 1-8. 18. Sanglard D, Odds FC (2002) Resistance of Candida species to antifungal agents: molecular mechanisms and clinical consequences. Lancet Infect Dis 2: 73-85. 19. Chowdhary A, Kathuria S, Xu J, Meis JF (2013) Emergence of azole-resistant aspergillus fumigatus strains due to agricultural azole use creates an increasing threat to human health. PLoS Pathog 9: e1003633. 20. Lamb DC, Kelly DE, White TC, Kelly SL (2000) The R467K amino acid substitution in Candida albicans sterol l4alpha-demethylase causes drug resistance through reduced affinity. Antimicrob Agents Chemother 44: 63-67. 21. Hoot SJ, Smith AR, Brown RP, White TC (2011) An A643V amino acid substitution in Upc2p contributes to azole resistance in well-characterized clinical isolates of Candida albicans. Antimicrob Agents Chemother 55: 940-942. 22. Selmecki A, Forche A, Berman J (2006) Aneuploidy and isochromosome formation in drug-resistant Candida albicans. Science 313: 367-370. 23. Coste AT, Karababa M, Ischer F, Bille J, Sanglard D (2004) TAC 1, transcriptional activator of CDR genes, is a new transcription factor involved in the regulation of Candida albicans ABC transporters CDR1 and CDR2. Eukaryot Cell 3: 16391652. 24. Lohberger A, Coste AT, Sanglard D (2014) Distinct roles of Candida albicans drug resistance transcription factors TAC 1, MRR1, and UPC2 in virulence. Eukaryot Cell 13: 127-142. 25. Jackson CJ, Lamb DC, Manning NJ, Kelly DE, Kelly SL (2003) Mutations in Saccharomyces cerevisiae sterol C5-desaturase conferring resistance to the CYP51 inhibitor fluconazole. Biochem Biophys Res Commun 309: 999-1004. 26. Vale-Silva LA, Coste AT, Ischer F, Parker JE, Kelly SL, et al. (2012) Azole resistance by loss of function of the sterol Delta(5),(6)-desaturase gene (ERG3) in Candida albicans does not necessarily decrease virulence. Antimicrob Agents Chemother 56: 1960-1968. 11. 31 27. Chau AS, Gurnani M, Hawkinson R, Laverdiere M, Cacciapuoti A, et al. (2005) Inactivation of sterol Delta5,6-desaturase attenuates virulence in Candida albicans. Antimicrob Agents Chemother 49: 3646-3651. 28. Gray KC, Palacios DS, Dailey I, Endo MM, Uno BE, et al. (2012) Amphotericin primarily kills yeast by simply binding ergosterol. Proc Natl Acad Sci U S A 109: 2234-2239. 29. Anderson TM, Clay MC, Cioffi AG, Diaz KA, Hisao GS, et al. (2014) Amphotericin forms an extramembranous and fungicidal sterol sponge. Nat Chem Biol 10: 400406. 30. Palacios DS, Dailey I, Siebert DM, Wilcock BC, Burke MD (2011) Synthesisenabled functional group deletions reveal key underpinnings of amphotericin B ion channel and antifungal activities. Proc Natl Acad Sci U S A 108: 6733-6738. 31. Safdar A, Ma J, Saliba F, Dupont B, Wingard JR, et al. (2010) Drug-induced nephrotoxicity caused by amphotericin B lipid complex and liposomal amphotericin B: a review and meta-analysis. Medicine (Baltimore) 89: 236-244. 32. Wilcock BC, Endo MM, Uno BE, Burke MD (2013) C2'-OH of amphotericin B plays an important role in binding the primary sterol of human cells but not yeast cells. J Am Chem Soc 135: 8488-8491. 33. Roemer T, Krysan DJ (2014) Antifungal drug development: challenges, unmet clinical needs, and new approaches. Cold Spring Harb Perspect Med 4. 34. Pfaller MA, Espinel-Ingroff A, Canton E, Castanheira M, Cuenca-Estrella M, et al. (2012) Wild-type MIC distributions and epidemiological cutoff values for amphotericin B, flucytosine, and itraconazole and Candida spp. as determined by CLSI broth microdilution. J Clin Microbiol 50: 2040-2046. 35. Sanglard D, Ischer F, Parkinson T, Falconer D, Bille J (2003) Candida albicans mutations in the ergosterol biosynthetic pathway and resistance to several antifungal agents. Antimicrob Agents Chemother 47: 2404-2412. 36. Kelly SL, Lamb DC, Kelly DE, Manning NJ, Loeffler J, et al. (1997) Resistance to fluconazole and cross-resistance to amphotericin B in Candida albicans from AIDS patients caused by defective sterol delta5,6-desaturation. FEBS Lett 400: 80-82. 37. Eddouzi J, Parker JE, Vale-Silva LA, Coste A, Ischer F, et al. (2013) Molecular mechanisms of drug resistance in clinical Candida species isolated from Tunisian hospitals. Antimicrob Agents Chemother 57: 3182-3193. 38. Steinbach WJ, Perfect JR (2003) Newer antifungal therapy for emerging fungal pathogens. Int J Infect Dis 7: 5-20. 39. Wheeler RT, Fink GR (2006) A drug-sensitive genetic network masks fungi from the immune system. PLoS Pathog 2: e35. 40. Pfaller MA, Boyken L, Hollis RJ, Messer SA, Tendolkar S, et al. (2006) In vitro susceptibilities of Candida spp. to caspofungin: four years of global surveillance. J Clin Microbiol 44: 760-763. 41. Ben-Ami R, Garcia-Effron G, Lewis RE, Gamarra S, Leventakos K, et al. (2011) Fitness and virulence costs of Candida albicans FKS 1 hot spot mutations associated with echinocandin resistance. J Infect Dis 204: 626-635. 32 42. Walker LA, Gow NA, Munro CA (2013) Elevated chitin content reduces the susceptibility of Candida species to caspofungin. Antimicrob Agents Chemother 57: 146-154. 43. Munro CA, Selvaggini S, de Bruijn I, Walker L, Lenardon MD, et al. (2007) The PKC, HOG and Ca2+ signalling pathways co-ordinately regulate chitin synthesis in Candida albicans. Mol Microbiol 63: 1399-1413. 44. Roemer T, Jiang B, Davison J, Ketela T, Veillette K, et al. (2003) Large-scale essential gene identification in Candida albicans and applications to antifungal drug discovery. Mol Microbiol 50: 167-181. 45. Payne DJ, Gwynn MN, Holmes DJ, Pompliano DL (2007) Drugs for bad bugs: confronting the challenges of antibacterial discovery. Nat Rev Drug Discov 6: 2940. 46. Lipinski CA, Lombardo F, Dominy BW, Feeney PJ (2001) Experimental and computational approaches to estimate solubility and permeability in drug discovery and development settings. Adv Drug Deliv Rev 46: 3-26. 47. Roemer T, Xu D, Singh SB, Parish CA, Harris G, et al. (2011) Confronting the challenges of natural product-based antifungal discovery. Chem Biol 18: 148-164. 48. Medema MH, Blin K, Cimermancic P, de Jager V, Zakrzewski P, et al. (2011) antiSMASH: rapid identification, annotation and analysis of secondary metabolite biosynthesis gene clusters in bacterial and fungal genome sequences. Nucleic Acids Res 39: W339-346. 49. Walsh CT, Fischbach MA (2010) Natural products version 2.0: connecting genes to molecules. J Am Chem Soc 132: 2469-2493. 50. Barczak AK, Gomez JE, Kaufmann BB, Hinson ER, Cosimi L, et al. (2012) RNA signatures allow rapid identification of pathogens and antibiotic susceptibilities. Proc Natl Acad Sci U S A 109: 6217-6222. 51. Clatworthy AE, Pierson E, Hung DT (2007) Targeting virulence: a new paradigm for antimicrobial therapy. Nat Chem Biol 3: 541-548. 52. Lo HJ, Kohler JR, DiDomenico B, Loebenberg D, Cacciapuoti A, et al. (1997) Nonfilamentous C. albicans mutants are avirulent. Cell 90: 939-949. 53. Liu Y, Filler SG (2011) Candida albicans Als3, a multifunctional adhesin and invasin. Eukaryot Cell 10: 168-173. 54. Noble SM, French S, Kohn LA, Chen V, Johnson AD (2010) Systematic screens of a Candida albicans homozygous deletion library decouple morphogenetic switching and pathogenicity. Nat Genet 42: 590-598. 55. San Jose C, Monge RA, Perez-Diaz R, Pla J, Nombela C (1996) The mitogenactivated protein kinase homolog HOGI gene controls glycerol accumulation in the pathogenic fungus Candida albicans. J Bacteriol 178: 5850-5852. 56. Alonso-Monge R, Navarro-Garcia F, Roman E, Negredo Al, Eisman B, et al. (2003) The Hogl mitogen-activated protein kinase is essential in the oxidative stress response and chlamydospore formation in Candida albicans. Eukaryot Cell 2: 351-361. 57. LaFayette SL, Collins C, Zaas AK, Schell WA, Betancourt-Quiroz M, et al. (2010) PKC signaling regulates drug resistance of the fungal pathogen Candida albicans via circuitry comprised of MkcI, calcineurin, and Hsp90. PLoS Pathog 6: e1001069. 33 58. Sanglard D, Ischer F, Marchetti 0, Entenza J, Bille J (2003) Calcineurin A of Candida albicans: involvement in antifungal tolerance, cell morphogenesis and virulence. Mol Microbiol 48: 959-976. 59. Cruz MC, Goldstein AL, Blankenship JR, Del Poeta M, Davis D, et al. (2002) Calcineurin is essential for survival during membrane stress in Candida albicans. EMBO J 21: 546-559. 60. Blankenship JR, Wormley FL, Boyce MK, Schell WA, Filler SG, et al. (2003) Calcineurin is essential for Candida albicans survival in serum and virulence. Eukaryot Cell 2: 422-430. 61. Onyewu C, Blankenship JR, Del Poeta M, Heitman J (2003) Ergosterol biosynthesis inhibitors become fungicidal when combined with calcineurin inhibitors against Candida albicans, Candida glabrata, and Candida krusei. Antimicrob Agents Chemother 47: 956-964. 62. Diezmann S, Michaut M, Shapiro RS, Bader GD, Cowen LE (2012) Mapping the Hsp90 genetic interaction network in Candida albicans reveals environmental contingency and rewired circuitry. PLoS Genet 8: e1002562. 63. Taipale M, Jarosz DF, Lindquist S (2010) HSP90 at the hub of protein homeostasis: emerging mechanistic insights. Nat Rev Mol Cell Biol 11: 515-528. 64. Borkovich KA, Farrelly FW, Finkelstein DB, Taulien J, Lindquist S (1989) hsp82 is an essential protein that is required in higher concentrations for growth of cells at higher temperatures. Mol Cell Biol 9: 3919-3930. 65. Jarosz DF, Taipale M, Lindquist S (2010) Protein homeostasis and the phenotypic manifestation of genetic diversity: principles and mechanisms. Annu Rev Genet 44: 189-216. 66. Xu Y, Lindquist S (1993) Heat-shock protein hsp90 governs the activity of pp60v-src kinase. Proc Natl Acad Sci U S A 90: 7074-7078. 67. Cowen LE, Lindquist S (2005) Hsp90 potentiates the rapid evolution of new traits: drug resistance in diverse fungi. Science 309: 2185-2189. 68. Singh SD, Robbins N, Zaas AK, Schell WA, Perfect JR, et al. (2009) Hsp90 governs echinocandin resistance in the pathogenic yeast Candida albicans via calcineurin. PLoS Pathog 5: e1000532. 69. Cowen LE, Singh SD, Kohler JR, Collins C, Zaas AK, et al. (2009) Harnessing Hsp90 function as a powerful, broadly effective therapeutic strategy for fungal infectious disease. Proc Natl Acad Sci U S A 106: 2818-2823. 70. Lamoth F, Juvvadi PR, Soderblom EJ, Moseley MA, Asfaw YG, et al. (2014) Identification of a key lysine residue in heat shock protein 90 required for azole and echinocandin resistance in Aspergillus fumigatus. Antimicrob Agents Chemother 58: 1889-1896. 71. Brown AJ, Brown GD, Netea MG, Gow NA (2014) Metabolism impacts upon Candida immunogenicity and pathogenicity at multiple levels. Trends Microbiol. 72. Ene IV, Brunke S, Brown AJ, Hube B (2014) Metabolism in Fungal Pathogenesis. Cold Spring Harb Perspect Med. 73. Lorenz MC, Fink GR (2002) Life and death in a macrophage: role of the glyoxylate cycle in virulence. Eukaryot Cell 1: 657-662. 34 74. Ramirez MA, Lorenz MC (2007) Mutations in alternative carbon utilization pathways in Candida albicans attenuate virulence and confer pleiotropic phenotypes. Eukaryot Cell 6: 280-290. 75. Ene IV, Adya AK, Wehmeier S, Brand AC, MacCallum DM, et al. (2012) Host carbon sources modulate cell wall architecture, drug resistance and virulence in a fungal pathogen. Cell Microbiol 14: 1319-1335. Jimenez-Lopez C, Lorenz MC (2013) Fungal immune evasion in a model host76. pathogen interaction: Candida albicans versus macrophages. PLoS Pathog 9: e1003741. 77. Lorenz MC, Fink GR (2001) The glyoxylate cycle is required for fungal virulence. Nature 412: 83-86. 78. Sun N, Fonzi W, Chen H, She X, Zhang L, et al. (2013) Azole susceptibility and transcriptome profiling in Candida albicans mitochondrial electron transport chain complex I mutants. Antimicrob Agents Chemother 57: 532-542. 79. Li D, Chen H, Florentino A, Alex D, Sikorski P, et al. (2011) Enzymatic dysfunction of mitochondrial complex I of the Candida albicans goal mutant is associated with increased reactive oxidants and cell death. Eukaryot Cell 10: 672-682. 80. Qu Y, Jelicic B, Pettolino F, Perry A, Lo TL, et al. (2012) Mitochondrial sorting and assembly machinery subunit Sam37 in Candida albicans: insight into the roles of mitochondria in fitness, cell wall integrity, and virulence. Eukaryot Cell 11: 532544. 81. Shingu-Vazquez M, Traven A (2011) Mitochondria and fungal pathogenesis: drug tolerance, virulence, and potential for antifungal therapy. Eukaryot Cell 10: 13761383. 82. Barelle CJ, Priest CL, Maccallum DM, Gow NA, Odds FC, et al. (2006) Nichespecific regulation of central metabolic pathways in a fungal pathogen. Cell Microbiol 8: 961-971. 35 Chapter Two: Fitness Tradeoffs Restrict the Evolution of Resistance to Amphotericin B *This chapter has been published previously: Vincent BM, Lancaster AK, Scherz-shouval R, Whitesell L, Lindquist S. Fitness tradeoffs restrict the evolution of resistance to amphotericin B. PLoS Biology 2013;11(10). 36 Fitness Trade-offs Restrict the Evolution of Resistance to Amphotericin B Benjamin Matteson Vincent", Alex Kelvin Lancaster 2', Ruth Scherz-Shouval 2, Luke Whitesell 2 , Susan Lindquist 2 ,3 1 Microbiology Graduate Program, Massachusetts Institute of Technology, Cambridge, Massachusetts, United States of America, 2 Whitehead Institute for Biomedical Research, Cambridge, Massachusetts, United States of America, 3 Howard Hughes Medical Institute, Department of Biology, Massachusetts Institute of Technology, Cambridge, Massachusetts, United States of America E-mail: Lindquist admingwi.mit.edu Current address: Department of Pathology, Beth Israel Deaconess Medical Center and Center for Biomedical Informatics, Harvard Medical School, Boston, Massachusetts, United States of America * Abbreviations: AmB, Amphotericin B; CFU, colony-forming-unit; ERG, ergosterol; FCZ, fluconazole; Hsp90, heat shock protein 90; HUVEC, human umbilical vein endothelial cell; TNF-a, tumor-necrosis-factor alpha, WT, wild-type ABSTRACT The evolution of drug resistance in microbial pathogens provides a paradigm for investigating evolutionary dynamics with important consequences for human health. Candida albicans, the leading fungal pathogen of humans, rapidly evolves resistance to two major antifungal classes, the triazoles and echinocandins. In contrast, resistance to the third major antifungal used in the clinic, amphotericin B (AmB), remains extremely rare despite 50 years of use as monotherapy. We sought to understand this long-standing evolutionary puzzle. We used whole genome sequencing of rare AmB-resistant clinical isolates as well as laboratory-evolved strains to identify and investigate mutations that confer AmB resistance in vitro. Resistance to AmB came at a great cost. Mutations that conferred resistance simultaneously created diverse stresses that required high levels of 37 the molecular chaperone Hsp90 for survival, even in the absence of AmB. This requirement stemmed from severe internal stresses caused by the mutations, which drastically diminished tolerance to external stresses from the host. AmB-resistant mutants were hypersensitive to oxidative stress, febrile temperatures, and killing by neutrophils and also had defects in filamentation and tissue invasion. These strains were avirulent in a mouse infection model. Thus, the costs of evolving resistance to AmB limit the emergence of this phenotype in the clinic. Our work provides a vivid example of the ways in which conflicting selective pressures shape evolutionary trajectories and illustrates another mechanism by which the Hsp90 buffer potentiates the emergence of new phenotypes. Developing antibiotics that deliberately create such evolutionary constraints might offer a strategy for limiting the rapid emergence of drug resistance. Author Summary The evolution of drug resistance in human pathogens is considered an inevitable consequence of the selective pressures imposed by antimicrobial drugs. Yet resistance to one antifungal drug, amphotericin B (AmB), remains extremely rare despite decades of widespread use. Here we explore the biological mechanisms underlying this conundrum. By examining natural and experimental populations of Candidaalbicans, we identify multiple mutations that confer resistance to AmB in vitro. As with the evolution of resistance to other antifungals, we find that the chaperone protein Hsp90 is involved in enabling the evolution of resistance to AmB. We also discover, however, that mutations that confer AmB resistance impose massive costs on other aspects of fungal pathogenicity; strains that are resistant to AmB are hypersensitive to attack by the host immune system and are unable to invade and damage host tissue. Thus, the evolution of resistance to AmB is restricted by a tradeoff between tolerance of the drug and the ability to cause disease. We propose that developing new antibiotics for which resistance presents such dire tradeoffs may be a promising strategy to prevent the evolution of resistance. 38 Introduction Understanding how organisms rapidly evolve novel traits is a central problem in both evolutionary biology and the treatment of infectious diseases. The emergence of drugresistant pathogens not only provides a model for studying the evolution of new phenotypes but also poses a grave challenge to human health. Antibiotic treatment selects for rare mutations that alter cellular processes and, thereby, either mitigate the toxicity of the drug or bypass it altogether. Sometimes resistance mechanisms are completely orthogonal to the normal biology of the cell, as is the case for the amplification of efflux pumps or the horizontal acquisition of drug-detoxifying enzymes in bacteria. But often the mutations that confer resistance alter basic cellular processes in such a way as to create a variety of new stresses. The latter is especially relevant in eukaryotic pathogens, where the rarity of genetic exchange within and between populations necessitates the de novo evolution of resistance [1,2]. Candida albicans is the leading fungal pathogen of humans and the fourth most common cause of all hospital-acquired infections [3,4]. Normally a harmless commensal, changes in host immune status allow C. albicans to become pathogenic. Infections range from superficial thrush to life-threatening systemic disease. Mild to moderate infections are currently treated with triazoles, which inhibit Ergi1 (lanosterol 14a-demethylase), preventing ergosterol biosynthesis [5]. Life-threatening systemic infections require treatment with echinocandin or polyene agents. Echinocandins inhibit the synthesis of the cell wall polymer (1,3)-p-D-glucan, resulting in loss of cell integrity [5]. The third most commonly employed antifungal is the polyene drug amphotericin B (AmB), which was the standard of care for -40 years [6]. Its potent fungicidal activity 39 derives from its ability to selectively bind the major sterol of fungal membranes, ergosterol [7,8]. Among other effects, this binding induces pore formation in the plasma membrane and results in rapid cell death. While AmB is extremely effective at killing fungi, its clinical utility is impaired by several liabilities. First, pharmacokinetics and distribution are poor, allowing some fungi to hide in niches where drug exposure is limited [9]. Second, AmB induces idiosyncratic systemic reactions involving fever and tremors. Third, and still more problematic, AmB's cumulative, dose-dependent renal toxicity limits use in many patients. Despite these limitations, a remarkable advantage of AmB is that it has been exceptionally refractory to the evolution of resistance. After 50 years of use as monotherapy, the acquisition of AmB resistance in C. albicans remains extremely rare. For comparison, the antifungal drug 5-flucytosine was introduced several years later than AmB, but resistance rendered this drug obsolete against Candida in less than 20 years [10]. In a recent study of 9,252 clinical isolates of C. albicans, 99.8% remained AmBsensitive [11]. Although the less toxic triazoles and echinocandins have recently replaced AmB as the frontline therapy, AmB still retains frequent use in many settings, particularly when an infection resists treatment with other drugs [12]. Indeed, resistance to triazoles emerges frequently and, although echinocandins are relatively new to the clinic, resistance to echinocandins is also already arising [13- 18]. The best-validated mechanism of resistance to AmB observed in clinical isolates of C. albicans to date involves a double loss of function in both ERG3 and ERG]] (C-5 sterol desaturase and lanosterol 14a-demethylase, respectively), identified by biochemical analysis of membrane sterol composition [19- 21]. In other fungal 40 pathogens, sterol analysis of rare AmB-resistant isolates has identified resistant strains lacking ERG2, encoding C-8 sterol isomerase, and ERG6, encoding C-24 sterol methyltransferase [22 -24]. However, there has been no systematic analysis of AmB resistance mutations in Candida using matched isogenic strains. More importantly, the consequences of these mutations upon the biology and pathogenicity of Candida remain largely unexplored. Here we thoroughly explore mutations that can confer AmB resistance in C. albicans with the goal of understanding why resistance emerges so rarely in the clinic. Our results establish that the evolutionary constraints imposed by AmB are distinct from those of other antifungals. They provide insights into the mechanisms by which external and internal biological stresses restrict evolutionary trajectories. In addition, our work broadens the role of protein homeostasis regulators as potentiators for the emergence of new traits. Finally, our findings suggest a general strategy for antimicrobial drug development that might be broadly useful in limiting the emergence of resistance. RESULTS Whole Genome Sequencing of AmB-Resistant Clinical Isolates implicates ERG2 and ERG3/11 As a first step towards understanding the evolution of resistance to AmB in Candida, we sought to broaden and validate the list of mutations that allow the fungus to tolerate this drug. As AmB-sensitive parental strains from which rare AmB-resistant isolates evolved are not available, the identification of mutations conferring resistance has proven challenging. Nevertheless, we sequenced the entire genome of two 41 independent clinical isolates that had evolved resistance to AmB, one from C. albicans and one from the closely related species C. tropicalis. For comparison, we also resequenced the AmB-sensitive C. albicansreference strain SC5314. Using paired-end reads, we achieved over 50-fold coverage of these genomes, which allowed us to detect simple polymorphisms as well as complex genome rearrangements. As expected, the strains differed from each other and from the reference strain at more than 20,000 sites. To identify the variants responsible for resistance, we took advantage of previous work and inspected candidate genes acting in the ergosterol biosynthesis pathway. In the C. albicans AmB-resistant isolate, we detected a high density of mispaired reads at the ERG2 (ORF19.6026) locus (Figure 1A). Further analysis revealed that both copies of the ERG2 gene in this strain carried an insertion of the TCA2 retrotransposon (Figure Si A). Whole-genome analysis of polymorphisms indicated that the strain carried a high level of heterozygosity across its entire genome, with only two small regions of homozygosity. Strikingly, one of these included the transposon insertion in ERG2 (Figure SlB). In the C. tropicalis isolate, the sequence of ERG2 was identical to that of the AmB-sensitive reference strain, MYA-3404. However, a mutation was observed in ERG3 (CTRG_04480), another enzyme involved in sterol synthesis (Figure S2A). Specifically, phenylalanine replaced serine 257, a residue that is absolutely conserved in this protein from fungi to mammals (Figure S2B). In addition, the ERG]] (CTRG_05283) ORF of this isolate harbored a deletion of 170 nucleotides (Figure S2C). Again, despite generally high levels of heterozygosity in other regions of the genome, the 42 regions surrounding both ERG3 and ERG]] had become homozygous (Figure S2D). These results suggest that selective sweeps had operated to fix new mutations to a homozygous state in both clinical isolates. But, of course, the sequencing of many more AmB-sensitive and resistant isolates would be necessary to establish this conclusion. Validation of erg2 and erg3/1J in Laboratory Strains To validate that either loss of ERG2 or the combined loss of ERG3 and ERG]] function is sufficient to confer resistance to AmB, we created them anew in a wild-type background. Because C. albicans is an obligate diploid, we used auxotrophic markers to sequentially delete the loci, creating homozygous mutations in ERG2 and double homozygous mutations in ERG3 and ERG1. To confirm the inactivation of these genes in both lab strains and clinical isolates, we exploited the unique spectral characteristics of ergosterol. These result from conjugation of the double bonds C5-C6 and C7-C8, formed and isomerized by Erg3 and Erg2, respectively. We prepared sterol extracts from both of the clinical isolates and both of the laboratory mutants along with the isogenic wild-type control. Extracts from the wild-type laboratory strain exhibited the double-peaked spectrum between 240 and 300 nm characteristic of the conjugated bonds (Figure 1 C). Extracts from both the laboratory mutants and the clinical isolates did not. Next, we determined the minimal inhibitory concentration (MIC) of AmB in the knockout strains and compared it to the wild-type laboratory strain and the clinical isolates. AmB resistance levels in the two newly created laboratory strains matched those of the corresponding clinical isolates. For the erg2 mutants this was a 10-fold increase in MIC (Figure 1 D), and for the erg3 erg]] mutants it was a 20-fold increase. We were 43 unable to obtain further transformants in these mutants for technical reasons, thus precluding any attempt at complementation of the phenotype. However, we verified our results with an additional independent mutant in each background (Figure S5). Thus, laboratory-generated mutants successfully reproduce the resistant phenotypes observed in clinical isolates. Laboratory Evolution of AmB Resistance Implicates ERG6 Mutations To discover other mutations that could confer AmB resistance in Candida, we next employed in vitro evolution. The drug-sensitive reference strain SC5314 was not suited to this analysis because we repeatedly found that the resistance that emerged in selections with this strain was highly unstable. Another strain, C. albicans ATCC- 10231, proved to be less susceptible to this problem. To isolate resistant variants, this strain was inoculated in liquid media containing a low concentration of AmB and serially passaged seven times into media with a 2-fold higher concentration of AmB at each step. Surviving cells from each passage were isolated and saved. We then used whole genome sequencing and alignment of the parental strain with strains from the third, fifth, and seventh passages to identify the mutations emerging as strains developed resistance. Alignment of genome sequences and algorithmic detection of novel polymorphisms emerging within the series revealed a trajectory of mutations in the ERG6 (ORFJ9.1631) gene, encoding A(24)-sterol C-methyltransferase (Figure 1B). Notably, the parental strain had been heterozygous for a premature stop codon that replaced the codon for Glu70. A mutation in the other allele of ERG6, AspJ80Gly, appeared at the second step in the series. In the third step, the copy number of the Q70Stop allele increased to a 3:1 ratio relative to the Aspl80Gly allele. Finally, a loss of heterozygosity 44 event, unique to the left arm chromosome 3 where ERG6 resides, resulted in homozygosity of the nonsense allele (Figure S3A-B). Several independent selections with this strain-with either a similar gradual selection process or with selection regimes employing immediate shifts to high drug concentrations-all involved additional mutations in ERG6 (unpublished data). Finally, we validated the capacity of ERG6 mutations to create AmB resistance by using auxotrophic markers to delete the gene in the SC5314 reference strain background. This resulted in a 12-fold increase in the AmB MIC (Figure 1 D). Systematic Analysis of AmB Resistance in Late-Stage Ergosterol Biosynthesis Mutants To systematically define genes whose inactivation might confer AmB resistance in vitro, we used homologous site-directed recombination to generate isogenic diploid deletion mutants for all seven nonessential genes acting in the latter half of the ergosterol biosynthesis pathway (the steps after cyclization of squalene to lanosterol). Only the deletion of ERG2, ERG6, or of ERG3 and ERG]] together conferred more than a 3-fold increase in the AmB MIC (Figure ID). While other mutations conferring resistance to AmB may exist, these three are the most critical, as they have all been detected in the clinic and validated in the laboratory. Thus, we focused our efforts to explain the exceptional rarity of clinical AmB resistance on understanding the broader biological consequences of mutations in ERG2, ERG6, or ERG3 and ERG]]. AmB-Resistant Mutants Have an Unusual and Extreme Dependence on Hsp90 We previously reported that the emergence and maintenance of resistance to triazole and echinocandin antifungals critically depends on the molecular chaperone 45 Hsp90 (ORF19.6515) [25]. Hsp90 is one of the most abundant proteins in eukaryotic cells, constituting ~1% of total cellular protein, and acts as a protein homeostasis buffer. Although Hsp90 is an essential protein, its activity can be reduced up to 10-fold without impairing normal growth [25- 27]. Previous work has suggested that phylogenetically diverse organisms use this excess reservoir of protein-folding capacity to promote the rapid evolution of new traits through a litany of mechanisms [25,27,28]. These include binding and stabilizing mutant proteins with novel activities, promoting the folding and maturation of metastable signal transduction proteins that respond to harsh environmental conditions, and allowing for the release of cryptic genetic variation upon stress. In pathogenic fungi, we have shown that mild compromise of Hsp90 function prevents the de novo emergence of resistance to triazoles and, in fact, reverses the resistance of strains of which had previously evolved triazole and echinocandin resistance in the clinic [25,29,30]. Hsp90 promotes antifungal drug resistance by stabilizing calcineurin and protein kinase C, two signal transducers that promote resistance by mitigating the stress to the cell wall and membrane that is induced by these drugs [25,30,31]. We asked if Hsp90 also plays a role in the evolution of resistance to AmB, taking advantage of two structurally unrelated natural products with high specificity for Hsp90 (geldanamycin and radicicol). We examined mutants that had evolved AmB resistance under drug pressure in the clinic (Figure 2A-B), mutants created deliberately by targeting genes in the sterol pathway (Figure 2C), and mutants arising at each step in our in vitro selection (Figure 2D). We spotted drug-resistant and control isolates on media containing no drug, fluconazole, or AmB, in either the presence or in the absence of the Hsp90 inhibitors. 46 As previously described, modest inhibition of Hsp90 completely blocked fluconazole resistance (Figure 2A, middle panel). It did not affect growth of the fluconazole-resistant isolate in the absence of fluconazole (Figure 2A, top panel). Modest inhibition of Hsp90 also abrogated AmB resistance (Figure 2A, bottom panel). Surprisingly, however, low concentrations of either of the Hsp90 inhibitors completely blocked the growth of all of the AmB-resistant strains, even in the absence of AmB (Figures 2A-D and S4B). Perturbations in ergosterol biosynthesis can lead to general increases in the accumulation of diverse small molecules. This raised the possibility that the hypersensitivity to Hsp90 inhibitors might simply be due to an increase in their intracellular accumulation. To investigate, we determined the MICs of a panel of seven chemically and mechanistically distinct cytotoxic agents (that do not act through Hsp90) in all of the resistant strains. These MICs were compared to the MICs of geldanamycin and radicicol, as well as two synthetic Hsp90 inhibitors from completely different chemical scaffolds. AmB-resistant mutants were, indeed, generally more sensitive than wild-type cells to many of the cytotoxic compounds. The decrease from the wild-type in the MIC of any of these cytotoxic agents ranged from 2- to 8-fold in the erg2 or erg6 mutants and 4- to 16-fold in the erg3 erg]] mutant (Figure S4A-C). But the decreases in MIC of the four Hsp90 inhibitors were 18- to 48-fold for the erg2 mutants, 85- to 109fold for the erg6 mutants, and 222- to 480-fold for the erg3 erg]1 mutants (Figure S4BC). Thus, the hypersensitivity of AmB-resistant strains to Hsp90 inhibitors cannot simply be attributed to a general increase in drug accumulation. 47 Rather, the growth of these mutants must critically depend on maintaining very high levels of Hsp90 function even in the absence of AmB. Was the effect of the Hsp90 inhibitors restricted to growth inhibition, or did they actually cause cell death? We previously showed that Hsp90 inhibition renders the typically cytostatic drug fluconazole cytocidal, killing the fungus instead of simply blocking its growth [29]. Indeed, low concentrations of Hsp90 inhibitors were cytocidal to the AmB-resistant mutants (Figure 2E). But, once again, in contrast to the fluconazole resistant strains, Hsp90 inhibition killed AmB-resistant cells even in the absence of AmB. Thus, the mutations that confer AmB resistance cause a novel and critical dependence on Hsp90 for the simple maintenance of normal viability. AmB-Resistant Strains Exhibit Constitutive Activation of Stress Responses Hsp90 promotes the maturation of a diverse array of metastable signal transduction proteins, including kinases, phosphatases, and ubiquitin ligases (known as Hsp90 clients) [32]. These function in many stress response pathways. Thus, the simplest explanation for the extreme dependence of AmB-resistant strains on Hsp90 is that these normally nonessential client proteins are required to tolerate the perturbations in cellular homeostasis caused by mutations in ergosterol biosynthetic enzymes. To investigate, we first tested our AmB-resistant strains for constitutive transcriptional activation of a variety of stress response genes. These include targets of the known HSP90 client calcineurin [30,33], as well as genes involved in the response to iron starvation or oxidative stress, two stresses tightly linked to membrane sterol homeostasis. To provide a point of comparison, we exposed wild-type strains to external stresses known to induce these responses. 48 The AmB-resistant mutants indeed exhibited a constitutive activation of diverse stress responses (Figure 3A, left panel). Pathways of iron starvation were constitutively active, most strongly in the erg3/erg]] and erg6 mutants, as evidenced by the high expression of RBT5 (ORF19.5636), FET34 (ORF19.4215), FTRJ (ORF19.7219), and FTH1 (ORF19.4802), and SIT] (ORF19.2179). Genes responding to general plasma membrane and oxidative stressors also showed generally broad elevation [including CAT] (ORF19.6229), GPX1 (ORF19.86), CRH]1 (ORF19.2706), and DDR48 (ORF19.4082)]. Induction of calcineurin targets [UTR2 (ORF19.1671), RTA2 (ORF19.24), ECM331 (ORF19.4255)] was observed at varying levels as well, most strongly in the various lab strains [33,34]. The level of constitutive activation of these pathways in AmB-resistant strains was in many cases comparable to levels seen in wildtype strains exposed to severe external stresses (Figure 3A, right panel). Intriguingly, the AmB-sensitive, fluconazole-resistant erg3 mutant did not show dramatic upregulation of any of the responses tested, but only a weak induction of several iron starvation genes. These data suggest that the mutations that confer resistance to amphotericin concomitantly exert an array of stresses to cellular membrane and redox homeostasis. Nonessential Stress Responses Become Essential in AmB-Resistant Strains Hsp90-dependent stress-response pathways are not essential for growth of wild-type strains. In pathogenic fungi, validated Hsp90 clients include calcineurin, the MAP-Kinase Hogl, and Protein Kinase C (PKC) [30,31,35]. To test whether they become essential in the resistant mutants, we took advantage of the high conservation of these proteins: highly selective drugs targeting their human homologs have been developed for diverse therapeutic purposes, and these are active on the fungal proteins as well. These chemical 49 probes allowed us to selectively reduce the activities of these proteins in the genetically intractable clinical isolates. In laboratory strains, these compounds allowed us to bypass the difficulties inherent in maintaining mutations expected to exhibit synthetic lethalities. To inhibit calcineurin, we used FK-506 and Cyclosporin A, two structurally and mechanistically distinct inhibitors of the phosphatase. To inhibit PKC, we used enzastaurin, a synthetic PKC inhibitor with high selectivity for this kinase, and confirmed our findings with cercosporamide, a natural product fungal-specific inhibitor of PKC [31,36]. Treatment with either calcineurin inhibitor inhibited growth of all of the Amphotericin-resistant strains, with complete growth inhibition of erg2 and erg6 mutants (Figure 3B). The erg3 erg]] strains were slightly less sensitive to calcineurin inhibitors, but showed a dramatically increased sensitivity to PKC inhibition. We also asked if wild-type cells rely on Hsp90-dependent stress responses to defend themselves from the toxic effects of AmB. To do so, we created genetic knockouts of these normally nonessential genes in a wild-type background. Indeed, hog] mutants were hypersensitive to AmB, while strains lacking calcineurin [cnb1(orfl9.4009)] were not (Figure 3C). Mild inhibition of Hsp90, which is sufficient to impair calcineurin activity, did not change the AmB MIC. However, more extensive inhibition of Hsp90, which would destabilize Hogl [35], did sensitize cells to the antifungal. Thus, HogI is required to tolerate the stress imposed by drug treatment, while the calcineurin and PKC pathways are required to tolerate the stress imposed by resistance mutations. Next, we tested the role of Hsp90, Hogl, and calcineurin in the de novo emergence of AmB resistance. To do so, we generated ERG2/erg2 heterozygotes in a 50 wild-type background and in strains lacking HogI or calcineurin. We then selected for loss of the remaining allele of ERG2 by plating on media containing AmB. As expected, ERG2/erg2 heterozygotes that were otherwise wild-type produced resistant colonies at a rate of ~_1 05 (Figure 3D). Low concentrations of the Hsp90 inhibitor geldanamycin completely eliminated the emergence of such colonies. Strains lacking calcineurin also failed to produce resistant colonies, and hog] strains produced only a few small, slowgrowing colonies. We conclude that Hsp90-dependent stress responses are required to enable the de novo emergence of AmB resistance. AmB-Resistant Mutants Are Hypersensitive to Stresses Encountered in the Host Although we have successfully validated the ability of several ergosterol biosynthesis mutations to confer resistance to AmB in vitro, resistance rarely evolves during the treatment of infected patients. We wondered if the phenotypic benefit of AmB resistance might be undermined by fitness costs imposed by the mutations. That is, the high levels of internal stress that burden the AmB-resistant mutants might make them unable to withstand the additional external stresses imposed by the host. To investigate, we tested the ability of the resistant mutants and wild-type control to tolerate a range of stresses encountered in host environments, including (1) elevated temperatures (fevers are a universal response to systemic fungal infection and a common side-effect of AmB treatment); (2) hydrogen peroxide, hypochlorous acid, and nitric oxide (used by neutrophils to kill Candida); and (3) serum, iron deprivation, and antimicrobial peptides, as these are other common sources of stress in the host. While AmB-resistant strains grew similarly to wild-type strains at 37 'C and 39 'C, they grew more poorly at 41 'C (Figure 4A). Resistant mutants were hypersensitive 51 to the presence of peroxide, hypochlorous acid, and the nitric oxide donor DPTANONOate (Figure 4A-C). Resistant mutants also proliferated moderately more slowly than wild-type cells in the presence of an iron chelator (Figure 4D). Resistant strains were also sensitive to growth in 100% bovine serum (Figure 4F) at elevated temperature, but were not more sensitive to the neutrophil-associated antimicrobial peptide Calprotecin/S 1 OOA (Figure 4E). Next, we tested their susceptibility to attack by neutrophils, the most critical component of the innate immune system in combating acute fungal infection. We isolated human neutrophils from whole blood to 99% purity and activated them by treatment with recombinant TNF-a. Wild-type or AmB-resistant C. albicans strains were co-cultured with neutrophils for 6 h, at which point neutrophils were lysed and fungal growth was measured. The hog] mutant, previously reported to be hypersensitive to neutrophil attack [37,38], was included as a positive control. AmB-resistant mutants were indeed significantly hypersensitive to neutrophil attack, exhibiting at least as strong of a defect as the hog] mutant (Figure 4G). AmB-Resistant Mutants Are Defective in Filamentation and Tissue Invasion Another potential fitness cost of AmB-resistance mutations could be a compromise of pathogenic virulence mechanisms. C. albicans responds to several stimuli in the host environment by undergoing dramatic morphological changes, including the adoption of filamentous hyphal forms. Filamentation enables penetration and invasion of host tissue, and is a highly validated virulence factor for this pathogen [39,40]. We asked if our AmB-resistant mutants can filament effectively when exposed to 10% fetal bovine serum in RPMI culture media. After 4 h of incubation, wild-type strains exhibited long and 52 robust filaments (Figure 5A). The fluconazole-resistant erg3 mutant exhibited a mild lay in hyphal protrusion but still formed substantial filaments. However, the erg2 mutant could only form short and amorphous filaments. The erg6 and erg3 erg]] strains and clinical isolates were entirely unable to form hyphal extensions, and remained mainly in the yeast form. We then asked if this defect in filamentation reduced the capacity of the pathogen for tissue invasion. Monolayers of primary human endothelial cells were established in culture, and infected with the C. albicans strains. Lysis of the endothelial cells was monitored by assaying the release of cytosolic lactate dehydrogenase (LDH). All amphotericin-resistant mutants showed dramatic defects in their ability to damage the monolayer (Figure 5B). AmB-Resistant Mutants Are Avirulent in Mice Finally, we compared the virulence of our AmB-resistant laboratory and clinical strains with that of wild-type and fluconazole-resistant (erg3) strains in a mouse model of Candida fungemia. To provide a rigorous test, we used a relatively high intravenous inoculum of 4x 106 fungal cells in young Balb/c mice. At the time of sacrifice, both kidneys were isolated from each mouse. One was analyzed for fungal burden by homogenization and plating of CFU; the other was submitted for histological analysis. The wild-type strain killed all infected mice within 1-2 d (Figure 6A). Necropsy revealed high viable fungal burden in the kidney, extensive filamentous fungal morphology, and moderate tissue damage (Figure 6B-C). The erg3 mutant demonstrated reduced virulence as previously reported [41-43], but still killed all mice in an average of 53 3-4 d. At the time of death, mice infected with this mutant had extremely high kidney fungal burdens, filamentous fungal morphology, and extensive kidney necrosis. All AmB-resistant mutants, including the clinical isolate, were completely avirulent. Some mice showed mild weight loss in the first day after inoculation. But within a few days all infected mice recovered and appeared healthy. Kidney fungal burdens at 12 d postinoculation were at least three orders of magnitude lower than those of mice infected with wild-type Candidaor the fluconazole-resistant strain (Figure 6B). Thus, the resistant strains failed to tolerate the host environment or immune attack and colonize this organ, let alone damage it. Histological analysis demonstrated healthy kidneys with some signs of resolving acute inflammation, suggesting that innate immune attack may have contributed to the clearance of these strains (Figure 6C). The lack of morbidity in mice infected with the clinical isolate suggests that this strain was recovered from the patient harboring it not because it was virulent but simply because it had survived AmB treatment. DISCUSSION The emergence of drug resistance has diminished the utility of nearly every class of antimicrobial drug. Yet, 50 years after its introduction, AmB remains as effective as ever. The failure of fungi to evolve resistance to AmB presents a considerable evolutionary puzzle with important consequences for human health. Our work offers a mechanistic solution. In a comprehensive search for mutations that can produce AmB resistance, we sequenced rare resistant clinical isolates, evolved resistant strains in the laboratory, and targeted candidate genes by site-directed recombination. Every mutation 54 that was capable of conferring robust AmB resistance came at great cost to the pathogen. They all diminished Candida's ability to survive the diverse array of stresses that are inherent to growth in a mammalian host, crippled a major virulence factor required for invasive disease (filamentation), and eliminated the capacity to kill mice. Certainly, AmB therapy often fails, but not because the fungus acquires resistance to the drug [44,45]. Instead, treatment failure is linked to other factors, including the inability of the drug to penetrate certain niches of the body, dose-limiting renal toxicity, or the underlying disease of the patient [6,7,9]. While a small number of AmB-resistant clinical isolates have been reported in large surveys of clinical strain collections, we suspect that many (if not all) of these will prove to be avirulent, as was the one we tested. That is, they may have survived in a superficial niche less exposed to the stresses of the bloodstream but would not be capable of mounting a virulent systemic infection. Such strains might persist in patients with extreme immune system deficiencies. However, resistance to AmB is rare even in patients receiving myeloablative therapies that eliminate immune function [6,7]. Even in the absence of stress from the immune system, the lack of filamentation and hypersensitivity to other aspects of the host environment (such as fever or iron deprivation) likely restricts the virulence of resistant strains. Certainly, other explanations have been put forth for the rarity of AmB resistance and may also be relevant. For example, drugs that target lipids are not susceptible to resistance caused by substitutions in drug-binding pockets, a common occurrence with drugs that target proteins. In addition, because AmB acts on the plasma membrane, it is not susceptible to resistance mediated by increased drug efflux. Nevertheless, our work indicates that several deletion or loss of function mutations can readily arise in Candida 55 and confer resistance to AmB in vitro. But these mutants do not become prevalent in the clinic. It might be argued that AmB resistance is rare because it is dosed intravenously and is not often employed in the types of long-term prophylaxis that breed resistance. However, the structurally similar polyene nystatin, which has the same ergosterol-binding mechanism of action as AmB, is widely used as a topical agent in the prevention of thrush in immunocompromised patients and the treatment of superficial rashes in neonates. Although there has been ample opportunity for resistance to emerge and become a clinical liability, it has not. Our work also elaborates on the central role played by Hsp90 in potentiating the evolution of new phenotypes, but here it takes on a novel character. As previously reported, Hsp90 plays a critical role in the evolution of drug resistance in Candida and Aspergillus [25]. Hsp90 allows drug-resistant mutants to survive stresses imposed by triazoles and echinocandins, but is not required to tolerate the mutations conferring resistance to those drugs alone. Such is not the case for AmB. The alterations in sterol structure that confer AmB resistance cannot be achieved without causing a high level of constitutive stress. High levels of Hsp90, then, become essential to simply support viability, even in the absence of the drug. Thus, our findings illustrate yet another way that Hsp90 enables the acquisition of dramatic new phenotypes. Given its conservation, we suggest its role in supporting stress responses operates very broadly in the evolution of phenotypic diversity, allowing organisms to acquire mutations that confer novel phenotypes but simultaneously create stresses that otherwise would not be tolerated. The clinical experiment of 50 years of AmB use indicates that the emergence of drug resistance, which widely plagues antimicrobial therapeutics, is not inevitable [46]. 56 By elucidating the mechanisms that restrict the evolution of virulent AmB-resistant Candida, our work suggests a strategy that might be applied more broadly to prolong the ever-shortening window of efficacy encountered with new antibiotics: the development of compounds that exploit the high costs of resistance mechanisms. This strategy need not require the targeting of lipids. Advances in structural biology and medicinal chemistry have enabled the design of enzyme inhibitors that are less susceptible to resistance mediated by point mutations or by drug efflux [47- 50]. Resistance to these agents may require the microbe to make more complex changes to its physiology and these, too, may come at a high cost. How might we discover targets that could induce such constraints upon resistance? One possibility is to focus on essential genes that also play critical roles in stress responses or virulence processes, for which rewiring of pathways may fundamentally alter pathogenicity. In any case, fungal-selective inhibition of Hsp90 presents an attractive mechanism to prevent the emergence of drug resistance to all three antifungal classes in clinical use. Rooted in ancient and conserved biological processes, a similar strategy may prove useful in cancer, where resistance has greatly limited the efficacy of targeted therapeutics. Indeed, pharmacological inhibition of Hsp90 is now being explored as a strategy to forestall the emergence of resistance in diverse malignancies [28]. Investigating the mechanisms that support rapid evolutionary change with an eye to the constant challenges that cells face in their host environment presents a problem of broad biological interest with important clinical implications. 57 MATERIALS AND METHODS Ethics Statement All animal protocols were conducted in accordance with the Guide for the Care and Use of Laboratory Animals of the National Institutes of Health. All animals were maintained according to the guidelines of the MIT Committee on Animal Care (CAC). These studies were approved by the MIT CAC (protocol #0312-024-15). All efforts were made to minimize suffering. Media and Growth Conditions C. albicans and C. tropicalis strains were routinely maintained at 30 'C in YPD (2% Bacto peptone, 2% dextrose, 1% yeast extract). Stocks were maintained in 15% glycerol at -80 'C. For generation of deletion mutants, transformants were selected on synthetic medium (2% dextrose, 0.67% Difco yeast nitrogen base with ammonium sulfate) with an amino acid dropout mixture. RPMI 1640 media (Gibco) was buffered with 165 mM MOPS, pH 7.0, and supplemented with 2% dextrose. Whole genome sequencing, alignment, mapping, and variant calling. Using an Illumina HiSeq platform with paired-end reads, we obtained an average coverage of 50fold. After quality control filtering, reads from each sequenced genome were aligned against the Candidaalbicans SC5314 reference sequence, unless otherwise specified (Assembly 21, downloaded from the Candida genome project on June 27, 2011, available here: http://www.candidagenome.org/download/sequence/CalbicansSC5314/Assembly21/ar chive/C albicansSC5314_versionA2 1 -sOl -mO 1 -r03_chromosomes.fasta.gz) using the BWA aligner [51]. This was followed by variant calling with respect to this Candida 58 albicans reference using the UnifiedGenotyper from version 1.0.5974 (the version we used throughout these analyses) of the Genome Analysis Toolkit (GATK) [52]. (To ensure that lower quality SNPs that are present in both a parental and derived strain were correctly identified as being common, we disabled the maximum deletion fraction in the - call to the UnifiedGenotyper module. The specific parameters used were: "-dcov 1000 standemitconf 10.0 -standcallconf 50.0 --maxdeletionfraction 1.0.") For the Candidatropicalis genome (strain OY5), only a preliminary assembly consisting of 24 scaffolds for the reference example, Candida tropicalis MYA 3404, is currently available. We downloaded assembly "ASM633vl" from NCBI (https://www.ncbi.nlm.nih.gov/nuccore?term=GG692395:GG692418[PACC] on December 20, 2012). Alignment and SNP calling for the C. tropicalisgenome was performed as per the C. albicansgenomes. All reads will be available at NCBI under BioProject accession numbers PRJNA194436 (http://www.ncbi.nlm.nih.gov/bioproject/l94436) for C. albicans and PRJNA1 94439 (http://www.ncbi.nlm.nih.gov/bioproject/194439) for C. tropicalis;the umbrella project accession number is PRJNA195600 (http://www.ncbi.nlm.nih.gov/bioproject/195600). Finding Unique Strain-Specific Variants To identify variants (including SNPs and indels) unique to a strain, we compared the "parental" strain to individual "derived" strains. We used a combination of custom code and the GATK's CombineVariants and SelectVariants features to locate, and then rank by quality, the SNPs and indels detected in open reading frames that were present only in derived strains. From the previously generated VCF files for each of the parental and derived strains as described above, the CombineVariants module was used to create a 59 single list of SNPs (specifically we set the module options "-priority" to the name of the derived strain and the option "-genotypeMergeOptions" to "UNIOUIFY"). With this output VCF file, we employed the SelectVariants module to detect variants unique to the derived strain via the option: "-select "set==<derived-strain>". Additionally, to find cases where heterozygotes become homozygotes, or vice versa, we again used the SelectVariants by using the intersection feature: "-select 'set==Intersection". The merged genotype calls within each common SNP were then further filtered to find high-quality calls where the zygosity changed. Alignments of the reads for the ranked SNPs and indels were then visually inspected in the Integrative Genomics Viewer (IGV) for quality control [53]. In the case of the clinical isolates, we did one pairwise comparison: between the SC5314 ("derived"). wild type and the ATCC 200955 AmB-R clinical isolate For the in vitro selection experiments, we defined the first isolate (#1) as parental, and compared the subsequent three serially derived isolates (#2, #3, #4) back to this parental isolate. Loss-of-Heterozygosity (LOH) Visualization To visualize the LOH events in the in vitro selection series (BVO 1 -BV05), we performed multisample SNP calling using the GATK UnifiedGenotyper module to generate a VCF file containing all SNPs in all four strains (UnifiedGenotyper options: "-glm SNP -nt 1 -downsample tocoverage 100000"). Following quality filtering of SNPs, from this VCF file, we created a Python script to generate a list of positions of SNPs (relative to reference), if present in any of the four strains. For each SNP position in each of the strains, we were then able to classify whether it was homozygous for the reference base (blue), homozygous for the variant base (red), or heterozygous (white). The resulting 60 "heterogram" for all chromosomes was visualized using the quilt.plot function from the R "fields" package [54]. Regions where a LOH event is likely to have occurred show up as blocks of blue and red SNPs (regions of high homozygosity) against the backdrop of white (heterozygous SNPs). Sliding Window Heterozygosity Analyses For each SNP in a given strain, we extracted the counts of reads containing the reference and variant base from the allele depth ("AD") VCF annotation at that position. Using only SNPs of quality 1,000 or more, we then computed the "base ratio" at each position by dividing the count of reads for the minor allele base by the total number of reads for both bases at that SNP position, resulting in values of between 0 (complete homozygosity) and 0.5 (complete heterozygosity). We then averaged these base ratios over a 1 kb sliding window for each chromosome. We performed these analyses for the in vitro evolution series (BVO1-BV04) of C. albicans as well as the single C. tropicalis isolate (OY5). Spectrophotometric Analysis of Membrane Ergosterol Content Sterols were extracted and analyzed as previously described [55]. Equal weights of cell pellets were used across strains. Absorption patterns were recorded by scanning between 240 and 300 nm at 0.5 nm intervals. Strain Construction Strains and primers are listed in Tables Si and S2. Deletion strains were constructed as described in [56], using HIS1, LEU2, and ARG4 markers (the URA3 marker was not used, and all strains used were URA3 wild type). Briefly, PCR products containing approximately 350 nucleotides of upstream and downstream homology for each gene 61 were generated, and fusion PCR was used with a selectable auxotrophic marker to generate the knockout construct. Proper insertion of the auxotrophic marker and loss of the endogenous gene were confirmed by PCR. Two heterozygotes were selected from each initial knockout transformation for the knockout of the second allele, from which two knockout strains were tested for each (four total strains). The erg3 erg] mutant was constructed as previously described [21]. These four strains were compared for phenotypic concordance in filamentation and stress resistance to minimize the effect of secondary mutations; additional data on a second mutant strain for key mutants is presented in Figure S5. Minimum Inhibitory Concentration and Growth Assays Antifungal susceptibility was determined in flat bottom, 96-well microtiter plates (Costar) using a broth microdilution protocol as described [25]. Overnight cultures were grown at 30 'C in YPD for at least 16 h, and cell density was measured by OD600 before seeding approximately 103 cells per well in YPD or RPML media, at 30 'C or 37 'C, as indicated in figure legends. Growth was measured at 24 or 48 h postincubation by alamar blue (Invitrogen) fluorescence with excitation at 550 nm and emission at 590 nm, and in certain cases confirmed by measurement of OD600 after agitation using a spectrophotometer (Tecan). MIC80 was defined as the concentration of drug reducing growth by 80% relative to the wells containing no drug. For susceptibility to AmB and stress response inhibitors (Figures ID, 3B-C, and S5A), growth scores were determined by normalization of the values for each sample to the values obtained for the wild-type strain in the absence of AmB (or in the DMSO negative control for Figure 3B). For these assays (Figures 1D, 3B-C, and S5A), each condition was tested in duplicate and 62 Relative growth data were quantitatively repeated on at least two different days. displayed in color using Java TreeView 1.1.3 (http://itreeview.sourceforge.net). Sensitivity to stressors (Figure 4B-E) was similarly determined by microplate dilution and reading of alamar blue dye fluorescence; here, growth scores were calculated by dividing the growth value of the mutant by the growth value of the wild type in each particular stress condition. For stress assays (Figures 4B-E and S5B-C), data represent the mean of six wells, pooled from experiments performed on two separate days. Statistical significance was determined in Graphpad Prism 5.0 using the Student's t test function. Error bars represent the SEM for each group. Serum sensitivity was performed as previously described [57]. Cidal and static effects of Hsp90 inhibition were tested generally as previously described [29]. Cells were grown overnight in YPD and diluted to a concentration of 104 cells/mL at 30 'C in YPD containing Hsp90 inhibitors at the indicated concentrations. After 24 h, cells were plated onto YPD at two dilutions and colonies counted. Drugs used in growth assays included AmB (Fungizone, Invitrogen), fluconazole (TCI chemicals), radicicol (A.G. Scientific), geldanamycin (A.G. Scientific), Cyclosporin A (CalBiochem), FK-506 Enzastaurin (LC Labs). (A.G. Scientific), Cercosporamide (Sigma-Aldrich), and All drugs were dissolved in DMSO, with the exception of fluconazole (H 20) and AmB, which was obtained as an aqueous suspension with sodium deoxycholate. Agar Plate Growth Assays Spotting assays were performed by growing overnight cultures of strains in YPD at 30 'C, washing in PBS, and resuspending in PBS at a concentration of 5x 106 cells/mL. Four 63 5-fold serial dilutions were performed before spotting. All RPMI-agar plates were used within 6 h of pouring due to the potential instability of AmB and peroxides; it is recommended to test a range of AmB concentrations in agar plates due to potential chemical instability. Selection of AmB-resistant colonies was performed using ERG2/erg2i heterozygotes in wild-type, cnbAz, or hogli/ backgrounds on RPMI- agar plates containing 0.4 gg/mL AmB; the wild-type was also selected on media containing AmB and 2.5pM geldanamycin. Strains were grown overnight in YPD at 30 'C, washed in PBS, and plated at a density of 8x 106 cells per plate, and incubated for 2 d at 37 'C before photographs were taken. In Vitro Gradual Selection of AmB Resistance ATCC 10231 was grown overnight at 30 'C in YPD and 2x 108 cells were inoculated into one liter of YPD containing 0.25 [tg/mL AmB at 30 'C. Cultures were grown shaking for 24-48 h until turbidity was observed; cells were then removed, washed in PBS, and split for freezing glycerol stocks or reinoculation into media with a 2-fold higher concentration of AmB at the same cell density. The process was repeated until the concentration of AmB reached 32 pg/mL. The process was repeated in three independent selections. Strains were then thawed from glycerol stocks and struck to single colonies for future MIC assays. Neutrophil Killing Assay Neutrophils were prepared fresh from the blood of a healthy human donor following standard protocols, using Histopaque 1077 density gradient centrifugation and hypotonic erythrocyte lysis [58]. After isolation, neutrophils were activated by treating with recombinant TNF-a (10 ng/mL). Killing assays were performed essentially as described 64 in [38,59]. Briefly, neutrophils were co-cultured with log-phase C. albicans strains at a 1:1 ratio, with both cell types at a concentration of 10 4/mL. Control wells were inoculated in the identical conditions but without neutrophils added. Plates were incubated at 37 'C in a humidified incubator for 6 h, at which point neutrophils were lysed by adding one volume of water containing 0.1% Tween-20 and a 1:40 dilution of Alamar blue; wells were vigorously pipetted up and down. Alamar blue fluorescence was measured after 90 min of incubation at 37 'C. Relative growth was measured by dividing values obtained in the presence of neutrophils by those obtained in their absence for each strain. Control wells lacking C. albicans were included to verify that this treatment does not quantify growth of the neutrophil cells. Results from three separate plates are shown; growth of each mutant strain is presented as a fraction of the wild-type growth from the same plate. Statistical analysis was performed using paired Student's t test in Microsoft Excel. Filamentation Assay Hyphal induction was performed by growing C. albicans overnight at 30 *C in YPD, washing in PBS, and diluting 1:100 into RPMI + 10% fetal bovine serum at 37 'C (Sigma-Aldrich). After 2 or 4 h, cultures were briefly concentrated by centrifugation and visualized by DIC microscopy. Endothelial Cytotoxicity Assay Endothelial cell invasion assays were performed with human umbilical vein endothelial cells (HUVEC's, Lonza) as previously described [60]. Monolayers were infected with C. albicans strains at a 1:1 HUVEC:fungus ratio and assayed for cytotoxicity with the CytoTox-96 Lactate dehydrogenase assay (Promega) after 6 h of co-incubation. 65 Cytotoxicity was quantitated as the fraction of LDH release relative to a 100% value of wells treated with 1% Triton X-100 and a baseline value of HUVEC cells not infected with Candida. Error bars are indicative of the standard error of the mean for each group. Error bars indicate SEM. Results pooled from two experiments are displayed (six replicate wells per experiment). Statistical analysis was performed using unpaired Student's t test in Microsoft Excel. Quantitative RT-PCR Expression Analysis For measurement of the expression of stress response genes, strains were grown overnight in YPD 30 'C and diluted to OD600 of 0.15 in YPD, then grown for 5 h to mid-log phase and either centrifuged without treatment or subjected to different stresses. For stressed wild-type cells (SN250 strain), the conditions were as follows: AmB treatment with 1 ptg/mL AmB for 15 min, Osmotic shock with 0.3M NaCl for 10 min, Nitrosative stress with 2 mM DPTA-NO (Cayman Chemical) for 15 min, calcium shock with 150 mM calcium chloride for 10 min, oxidative stress with 10 mM tert-butyl peroxide for 10 min, and iron chelation with 500 iM bathophenanthroline sulfonate for 4 h. Cultures were centrifuged at 1,500 g for 5 min and quickly flash frozen in liquid nitrogen. Total RNA was isolated with an RNeasy column kit (Qiagen), normalized to equal amounts of total RNA across samples, and reverse transcribed for 120 min with the high capacity reverse transcription kit (Applied Biosystems). qPCR was performed with SYBR green mastermix (Applied Biosystems) on an Applied biosystems AB17900 thermal cycler, using oligonucleotides described in Table S2. Each measurement was obtained from an average of four wells, including two biological replicates and two technical replicates. Expression analysis was performed by the comparative ACt 66 quantitation method, comparing mutant or stress-treated strains to wild-type untreated strains, using nomalization to four internal control genes: TDH3, ACTi, TEF3, and RPP2B; the mean value obtained from the four normalizations was used. For representation by heatmap (Treeview), relative expression levels were determined by dividing each value by the maximum expression level for that gene in any tested condition, with the untreated wild-type samples set as the baseline (as certain genes were induced over 50-fold and others were not induced greater than 4-fold in any condition). Murine Model of Systemic Infection We utilized 7-9-wk-old female Balb/c mice from Charles River laboratory (n = 8 mice for WT, 10-14 mice for mutant strains). Each strain was tested in two independent experiments (performed at different times), and data were pooled. Strains to be injected were grown overnight in YPD, diluted, and grown for 5 h into mid-log phase at 30 'C, then washed twice in phosphate buffered saline (PBS), counted by hemocytometer and plating of dilutions, and resuspended in PBS at a concentration of 4xl07 cfu/mL. We used 100 [tL of each suspension to inject mice by lateral tail-vein injection. Mice were weighed daily and monitored for signs of morbidity and sacrificed when body weight decreased by more than 20%. Kidneys were removed and either homogenized in PBS and plated for viable colony units (in duplicate) or submitted for fixation and staining with Periodic-acid Schiff stain. A veterinary pathologist was consulted for histological analysis. All experimental procedures were carried out according to NIH guidelines and MIT protocols for the ethical treatment of animals. 67 Acknowledgments The authors express gratitude to M. Brophy and L. Nolan for purified Calprotectin, J_ Love and T. Volkert for genome sequencing, J. Kohler and C. McLellan for useful discussions, V. Vyas for strains, and J. Funt for custom Python code used in the generation of heterozygosity plots from VCF files. References 1. Tibayrenc M, Ayala FJ (2012) Reproductive clonality of pathogens: a perspective on pathogenic viruses, bacteria, fungi, and parasitic protozoa. Proc Natl Acad Sci U S A 109: E3305-3313. 2. Xu J, Ramos AR, Vilgalys R, Mitchell TG (2000) Clonal and spontaneous origins of fluconazole resistance in Candida albicans. J Clin Microbiol 38: 1214-1220. 3. Brown GD, Denning DW, Gow NA, Levitz SM, Netea MG, et al. (2012) Hidden killers: human fungal infections. Sci Transl Med 4: 165rv1 13. 4. Pfaller M, Neofytos D, Diekema D, Azie N, Meier-Kriesche HU, et al. (2012) Epidemiology and outcomes of candidemia in 3648 patients: data from the Prospective Antifungal Therapy (PATH Alliance(R)) registry, 2004-2008. Diagn Microbiol Infect Dis 74: 323-331. 5. Odds FC, Brown AJ, Gow NA (2003) Antifungal agents: mechanisms of action. Trends Microbiol 11: 272-279. 6. Gallis HA, Drew RH, Pickard WW (1990) Amphotericin B: 30 years of clinical experience. Rev Infect Dis 12: 308-329. 7. Brajtburg J, Powderly WG, Kobayashi GS, Medoff G (1990) Amphotericin B: current understanding of mechanisms of action. Antimicrob Agents Chemother 34: 183188. 8. Gray KC, Palacios DS, Dailey I, Endo MM, Uno BE, et al. (2012) Amphotericin primarily kills yeast by simply binding ergosterol. Proc Natl Acad Sci U S A 109: 2234-2239. 9. Paterson PJ, Seaton S, Prentice HG, Kibbler CC (2003) Treatment failure in invasive aspergillosis: susceptibility of deep tissue isolates following treatment with amphotericin B. J Antimicrob Chemother 52: 873-876. 10. Vermes A, Guchelaar HJ, Dankert J (2000) Flucytosine: a review of its pharmacology, clinical indications, pharmacokinetics, toxicity and drug interactions. J Antimicrob Chemother 46: 171-179. 11. Pfaller MA, Espinel-Ingroff A, Canton E, Castanheira M, Cuenca-Estrella M, et al. (2012) Wild-type MIC distributions and epidemiological cutoff values for amphotericin B, flucytosine, and itraconazole and Candida spp. as determined by CLSI broth microdilution. J Clin Microbiol 50: 2040-2046. 12. Mora-Duarte J, Betts R, Rotstein C, Colombo AL, Thompson-Moya L, et al. (2002) Comparison of caspofungin and amphotericin B for invasive candidiasis. N Engl J Med 347: 2020-2029. 68 13. Garcia-Effron G, Kontoyiannis DP, Lewis RE, Perlin DS (2008) Caspofunginresistant Candida tropicalis strains causing breakthrough fungemia in patients at high risk for hematologic malignancies. Antimicrob Agents Chemother 52: 418 14183. 14. Ghannoum MA, Rice LB (1999) Antifungal agents: mode of action, mechanisms of resistance, and correlation of these mechanisms with bacterial resistance. Clin Microbiol Rev 12: 501-517. 15. Pfeiffer CD, Garcia-Effron G, Zaas AK, Perfect JR, Perlin DS, et al. (2010) Breakthrough invasive candidiasis in patients on micafungin. J Clin Microbiol 48: 2373-2380. 16. Sanglard D, Odds FC (2002) Resistance of Candida species to antifungal agents: molecular mechanisms and clinical consequences. Lancet Infect Dis 2: 73-85. 17. Walker LA, Gow NA, Munro CA (2010) Fungal echinocandin resistance. Fungal Genet Biol 47: 117-126. 18. White TC, Marr KA, Bowden RA (1998) Clinical, cellular, and molecular factors that contribute to antifungal drug resistance. Clin Microbiol Rev 11: 3 82-402. 19. Kelly SL, Lamb DC, Kelly DE, Manning NJ, Loeffler J, et al. (1997) Resistance to fluconazole and cross-resistance to amphotericin B in Candida albicans from AIDS patients caused by defective sterol delta5,6-desaturation. FEBS Lett 400: 80-82. 20. Martel CM, Parker JE, Bader 0, Weig M, Gross U, et al. (2010) A clinical isolate of Candida albicans with mutations in ERG 1I (encoding sterol 14alphademethylase) and ERG5 (encoding C22 desaturase) is cross resistant to azoles and amphotericin B. Antimicrob Agents Chemother 54: 3578-3583. 21. Sanglard D, Ischer F, Parkinson T, Falconer D, Bille J (2003) Candida albicans mutations in the ergosterol biosynthetic pathway and resistance to several antifungal agents. Antimicrob Agents Chemother 47: 2404-2412. 22. Hull CM, Bader 0, Parker JE, Weig M, Gross U, et al. (2012) Two clinical isolates of Candida glabrata exhibiting reduced sensitivity to amphotericin B both harbor mutations in ERG2. Antimicrob Agents Chemother 56: 6417-6421. 23. Vandeputte P, Tronchin G, Larcher G, Ernoult E, Berges T, et al. (2008) A nonsense mutation in the ERG6 gene leads to reduced susceptibility to polyenes in a clinical isolate of Candida glabrata. Antimicrob Agents Chemother 52: 370 13709. 24. Young LY, Hull CM, Heitman J (2003) Disruption of ergosterol biosynthesis confers resistance to amphotericin B in Candida lusitaniae. Antimicrob Agents Chemother 47: 2717-2724. 25. Cowen LE, Lindquist S (2005) Hsp90 potentiates the rapid evolution of new traits: drug resistance in diverse fungi. Science 309: 2185-2189. 26. Borkovich KA, Farrelly FW, Finkelstein DB, Taulien J, Lindquist S (1989) hsp82 is an essential protein that is required in higher concentrations for growth of cells at higher temperatures. Mol Cell Biol 9: 3919-3930. 27. Jarosz DF, Lindquist S (2010) Hsp90 and environmental stress transform the adaptive value of natural genetic variation. Science 330: 1820-1824. 28. Whitesell L, Santagata S, Lin NU (2012) Inhibiting HSP90 to treat cancer: a strategy in evolution. Curr Mol Med 12: 1108-1124. 69 29. Cowen LE, Singh SD, Kohler JR, Collins C, Zaas AK, et al. (2009) Harnessing Hsp90 function as a powerful, broadly effective therapeutic strategy for fungal infectious disease. Proc Natl Acad Sci U S A 106: 2818-2823. 30. Singh SD, Robbins N, Zaas AK, Schell WA, Perfect JR, et al. (2009) Hsp90 governs echinocandin resistance in the pathogenic yeast Candida albicans via calcineurin. PLoS Pathog 5: e1000532. doi:10.1371/joumal.ppat.1000532 31. LaFayette SL, Collins C, Zaas AK, Schell WA, Betancourt-Quiroz M, et al. (2010) PKC signaling regulates drug resistance of the fungal pathogen Candida albicans via circuitry comprised of Mkcl, calcineurin, and Hsp90. PLoS Pathog 6: e1001069. doi: 10.1371/joumal.ppat.1001069 32. Taipale M, Krykbaeva I, Koeva M, Kayatekin C, Westover KD, et al. (2012) Quantitative analysis of HSP90-client interactions reveals principles of substrate recognition. Cell 150: 987-1001. 33. Karababa M, Valentino E, Pardini G, Coste AT, Bille J, et al. (2006) CRZ1, a target of the calcineurin pathway in Candida albicans. Mol Microbiol 59: 1429-1451. 34. Jia Y, Tang RJ, Wang L, Zhang X, Wang Y, et al. (2012) Calcium-activatedcalcineurin reduces the In vitro and In vivo sensitivity of fluconazole to Candida albicans via Rta2p. PLoS One 7: e48369. doi: 10.1371/joumal.pone.0048369 35. Diezmann S, Michaut M, Shapiro RS, Bader GD, Cowen LE (2012) Mapping the Hsp90 genetic interaction network in Candida albicans reveals environmental contingency and rewired circuitry. PLoS Genet 8: e1002562. doi:10.1371/joumal.pgen.1002562 36. Sussman A, Huss K, Chio LC, Heidler S, Shaw M, et al. (2004) Discovery of cercosporamide, a known antifungal natural product, as a selective Pkc 1 kinase inhibitor through high-throughput screening. Eukaryot Cell 3: 932-943. 37. Arana DM, Alonso-Monge R, Du C, Calderone R, Pla J (2007) Differential susceptibility of mitogen-activated protein kinase pathway mutants to oxidativemediated killing by phagocytes in the fungal pathogen Candida albicans. Cell Microbiol 9: 1647-1659. 38. Miramon P, Dunker C, Windecker H, Bohovych IM, Brown AJ, et al. (2012) Cellular responses of Candida albicans to phagocytosis and the extracellular activities of neutrophils are critical to counteract carbohydrate starvation, oxidative and nitrosative stress. PLoS One 7: e52850. doi:10.1371/joumal.pone.0052850 39. Lo HJ, Kohler JR, DiDomenico B, Loebenberg D, Cacciapuoti A, et al. (1997) Nonfilamentous C. albicans mutants are avirulent. Cell 90: 939-949. 40. Mitchell AP (1998) Dimorphism and virulence in Candida albicans. Curr Opin Microbiol 1: 687-692. 41. Miyazaki T, Miyazaki Y, Izumikawa K, Kakeya H, Miyakoshi S, et al. (2006) Fluconazole treatment is effective against a Candida albicans erg3/erg3 mutant in vivo despite in vitro resistance. Antimicrob Agents Chemother 50: 580-586. 42. Chau AS, Gurnani M, Hawkinson R, Laverdiere M, Cacciapuoti A, et al. (2005) Inactivation of sterol Delta5,6-desaturase attenuates virulence in Candida albicans. Antimicrob Agents Chemother 49: 3646-3651. 43. Vale-Silva LA, Coste AT, Ischer F, Parker JE, Kelly SL, et al. (2012) Azole resistance by loss of function of the sterol Delta(5),(6)-desaturase gene (ERG3) in 70 Candida albicans does not necessarily decrease virulence. Antimicrob Agents Chemother 56: 1960-1968. 44. Park BJ, Arthington-Skaggs BA, Hajjeh RA, Iqbal N, Ciblak MA, et al. (2006) Evaluation of amphotericin B interpretive breakpoints for Candida bloodstream isolates by correlation with therapeutic outcome. Antimicrob Agents Chemother 50: 1287-1292. 45. Rex JH, Pfaller MA, Barry AL, Nelson PW, Webb CD (1995) Antifungal susceptibility testing of isolates from a randomized, multicenter trial of fluconazole versus amphotericin B as treatment of nonneutropenic patients with candidemia. NIAID Mycoses Study Group and the Candidemia Study Group. Antimicrob Agents Chemother 39: 40-44. 46. Read AF, Lynch PA, Thomas MB (2009) How to make evolution-proof insecticides for malaria control. PLoS Biol 7: e1000058. doi:10.1371/journal.pbio.1000058 47. Altman MD, Ali A, Reddy GS, Nalam MN, Anjum SG, et al. (2008) HIV- 1 protease inhibitors from inverse design in the substrate envelope exhibit subnanomolar binding to drug-resistant variants. J Am Chem Soc 130: 6099-6113. 48. Li XZ, Nikaido H (2009) Efflux-mediated drug resistance in bacteria: an update. Drugs 69: 1555-1623. 49. Nakashima R, Sakurai K, Yamasaki S, Nishino K, Yamaguchi A (2011) Structures of the multidrug exporter AcrB reveal a proximal multisite drug-binding pocket. Nature 480: 565-569. 50. Zhou T, Commodore L, Huang WS, Wang Y, Thomas M, et al. (2011) Structural mechanism of the Pan-BCR-ABL inhibitor ponatinib (AP24534): lessons for overcoming kinase inhibitor resistance. Chem Biol Drug Des 77: 1-11. 51. Li H, Durbin R (2009) Fast and accurate short read alignment with Burrows-Wheeler transform. Bioinformatics 25: 1754-1760. 52. DePristo MA, Banks E, Poplin R, Garimella KV, Maguire JR, et al. (2011) A framework for variation discovery and genotyping using next-generation DNA sequencing data. Nat Genet 43: 491-498. 53. Thorvaldsdottir H, Robinson JT, Mesirov JP (2012) Integrative Genomics Viewer (IGV): high-performance genomics data visualization and exploration. Brief Bioinform. 54.Fields Development Team (2006). fields: Tools for Spatial Data. National Center for Atmospheric Research, Boulder, CO. URL http://www.image.ucar.edu/GSP/Software/Fields/index.shtml 55. Arthington-Skaggs BA, Warnock DW, Morrison CJ (2000) Quantitation of Candida albicans ergosterol content improves the correlation between in vitro antifungal susceptibility test results and in vivo outcome after fluconazole treatment in a murine model of invasive candidiasis. Antimicrob Agents Chemother 44: 20812085. 56. Noble SM, Johnson AD (2005) Strains and strategies for large-scale gene deletion studies of the diploid human fungal pathogen Candida albicans. Eukaryot Cell 4: 298-309. 57. Blankenship JR, Wormley FL, Boyce MK, Schell WA, Filler SG, et al. (2003) Calcineurin is essential for Candida albicans survival in serum and virulence. Eukaryot Cell 2: 422-430. 71 58. Nauseef WM (2007) Isolation of human neutrophils from venous blood. Methods Mol Biol 412: 15-20. 59. Ermert D, Niemiec MJ, Rohm M, Glenthoi A, Borregaard N, et al. (2013) Candida albicans escapes from mouse neutrophils. J Leukoc Biol 94: 223-236. 60. Uppuluri P, Chaturvedi AK, Srinivasan A, Banerjee M, Ramasubramaniam AK, et al. (2010) Dispersion as an important step in the Candida albicans biofilm developmental cycle. PLoS Pathog 6: e1000828. doi: 10.1 371/joumal.ppat. 1000828 61. White TC (1997) Increased mRNA levels of ERG16, CDR, and MDR1 correlate with increases in azole resistance in Candida albicans isolates from a patient infected with human immunodeficiency virus. Antimicrob Agents Chemother 41: 14821487. 72 J - ~AL ~ A SC5314 Wild-Type ATCC 200955 AmB-R Clinical isolate Chr2: 153368 Chr2: 157825 ERG2 B i #1 in vitro selection WTIQ7OStop DIBOG/QO7Stop #2 for AmB resistance fI #3 D180G/Q70Stop (1:3) #4 Q7QStop/Q7OStop ERG6 Chr3: Chr3: 466245 465115 [AmB] D Total Sterol Extract C C. albicans Wild-Type C. albicans Clinical isolate erg2 1.00.8.0 35 0.1 0.2 (pgfmL) 0.4 0.8 1.6 erg3 0.6- erg4 0.4. erg5 0.2' erg3.ergll erg6 erg24 0 0240 280 260 300 Wavelength - WT - erg2 - C. tropicalis Clinical C. tropicalis Wild-Type C. tropicalis Clinical Isolate erg3;ergll C. albicans Clinical 0.0 0.25 0.50 0.75 1.0 Relative Growth 73 Fi2ure 1. Mechanisms of AmB resistance in Candida. (A) Alignment of reads from whole-genome sequencing of C. albicans wild-type strain SC5314 and AmB-resistant clinical isolate ATCC 200955 demonstrates transposon insertion in ERG2 in the clinical isolate. The ERG2 locus is shown. Colored reads are indicative of mate-pairs that do not both map to the same chromosome, but instead one end to ERG2 and the other end to the TCA2 locus (elaborated in Figure SlA). Reads were visualized with the integrative genomics viewer (IGV) [53]. (B) Alignment of selected strains from whole-genome sequencing of in vitro-evolved AmB-resistant series identifies causal mutations. Mutations in ERG6 ORF are highlighted, and the corresponding amino acid changes are indicated. Strain #1, 0 generations (founder); Strain #2, 60 generations; Strain #3, 120 generations; Strain #4, 240 generations. Two segments of IGV visualization for ERG6 were joined to allow visualization of both mutations in one image; point of joining indicated by "::". (C) Spectrophotometric analysis of sterols reveals lack of C5-C6:C7- C8 conjugation in AmB-resistant clinical isolates as well as laboratory-generated erg2 and erg3 erg]] mutants. Sterols were isolated by saponification and heptane extraction and analyzed spectrophotometrically between 240 and 300 nm, following established methods [55]. (D) AmB susceptibility of clinical isolates and laboratory-generated mutants in every nonessential gene in the latter half of the ergosterol biosynthesis pathway (after cyclization of squalene to lanosterol). Mutants were generated in SN152 strain background using HIS 1, LEU2, and ARG4 markers [56]. AmB susceptibility was determined by microplate dilution in RPMI at 37 'C for 24 h, repeated in duplicate; growth was normalized to wild-type in the absence of AmB. 74 A B A0.5pM Geldanamycin C. tropicalis WT C. tropicalis AmB-R Geldanamycin - Wild-Type FCZ-Resistant AmB-Resistant 0.5pM - C. tropicalis WT C. tropicafis AmB-R Wild-Type FCZ-Resistant AmB-Resistant 8 pg/mL 1 pg/mL AmB L C - FCZ L Wild-Type 1 pglmL AmB FCZ-Resistant AmB-Resistant Hsp9O inhibitor MIC (AM) E Radicicol MIC Geldanamycn MIC -0- Amphotein MIC D Wild-Type erg3AA arg2A/A erg6A/ erg3A/A erg11AlM Clinica -A- -4- -15o Amphotericin r 1 28 MC (sgImL) 11.00 25. -0.75 4. 3. 2. *0.50 4 ; 5 Sequential Isolate Number Geldanamycin erg2MA erg6NA erg3/I1IA Clinhal 104. 102m Fold Population Change 7 101K 10. j1 10-2. -0.28 3 0.25 pM AmB Wild-Type 3-A 2 0.4 pgimL 105. 40. 351 1 No Drug (RPMI, 37-C) 10-4 10-8 ; N Geldanamycin E Radicicol Figure 2. AmB-resistant strains critically depend on high levels of Hsp90 function for survival. (A) Mild inhibition of Hsp90 not only reverses AmB resistance but selectively kills AmB-resistant isolates. Spot assays (5-fold serial dilutions) of wild-type (SC5314), fluconazole-resistant (Isolate #2, [61]), and AmB-resistant (ATCC 200955) C. albicans on RPMI media containing antifungals and/or Hsp90 inhibitors at the indicated concentrations. (B) Increased dependence on Hsp90 for AmB resistance is conserved in a C. tropicalis clinical isolate. Spot assays of C. tropicalis reference strain MYA-3404 (AmB-sensitive) and ATCC 200956 (AmB-resistant) on media containing AmB, geldanamycin, or both compounds. (C) Isogenic, laboratory-generated AmB-resistant mutants also show an increased dependence on Hsp90. Spot assay of laboratorygenerated mutants on AmB and geldanamycin. Fluconazole-resistant erg3 mutant and AmB-resistant clinical isolate are provided for reference. Full MIC data in liquid culture for all strains are provided in Figure S4. (D) In vitro selection for AmB resistance leads to hypersensitivity to Hsp90 inhibition. 24-hour MIC80 (drug concentration reducing growth by 80 percent) of geldanamycin, radicicol, and AmB for each isolate from in vitro evolution series, tested in YPD at 30 'C. Note the discontinuity in the left y-axis due to the dramatic decrease in Hsp90 inhibitor MIC. (E) Hsp90 inhibition is cidal to AmBresistant strains. Viability assays of wild-type and AmB-resistant C. albicans strains in the presence of the Hsp90 inhibitors geldanamycin or radicicol. Strains were incubated in liquid culture for 24 h with the drugs and then plated for surviving colony-forming units. Drugs were used at 5 ptM in all strains. Error bars indicate SEM; each measurement was performed in duplicate. 75 A oo fe. of Wild-Type AmB erg3AIA NaCl erg3, 1A/A Fe Chelator erg2A/A DPTA-NO Clinical Ca erg6AIA Peroxide U_ Is L + 2 -1.00 -0.83 -0.6 -0.50 -0.33 -0.16 0.00 0.16 0.33 0.50 0.86 0.83 1.00 Relative Expression DMSO G dA RAD B Hsp90 FK506 CsA CRD ENZ Calcineurin PKC AmB (pg/mL) C 0 C.a. Wild-Type Wild-Type C.a. Clinical cnbIA/A C.a. erg2 0.05 0.10 0.20 0.40 hog1A/ A C.a. erg6 1pM GdA C.a. erg3/11 SpM C.t. Clinical GdA C.t. Wild-Type 0.00 0.25 0.50 0.75 1.00 Relative Growth 0.00 0.25 0.50 0.75 1.00 Relative Growth Wild-Type hogIA/A cnb1IA 76 Wild-Type; 2.5 pM Geldanamycin Figure 3. Constitutive stress response activation in AmB-resistant strains. (A) AmB resistant mutants constitutively express diverse stress response genes at high levels in the absence of any external stressors. qRT-PCR profiling of stress response genes in wildtype, fluconazole-resistant (erg3), and AmB-resistant mutants of C. albicans grown in rich (YPD) media with no added stressors (left panel), compared with wild-type strains treated with a variety of acute stressors known to activate these stress response pathways (right panel). Strains were grown to mid-log phase in YPD, and RNA was isolated by established methods. For stress treatment of wild-type strains (right panel), the indicated stressors are: AmB, 1 pg/mL AmB; NaCl, 0.3 M NaCl; Fe Chelator, 500 pM bapthophenanthroline disulfonate; DPTA-NO, 2 mM DPTA-NONOate; Ca , 150 mM CaCl 2 ; Peroxide, 10 mM tert-butyl peroxide. Expression levels of diverse stress response genes were quantified and normalized to four internal control genes: TDH3, TEF3, ACT1, and RPP2B; the mean value obtained from these four normalizations was used. To generate quantitative comparisons for color visualization, the relative expression level of each gene in each sample was divided by its maximal expression level observed (in any of the deletion strains or stress conditions; see Materials and Methods for further description). (B) Calcineurin and PKC pathways are differentially required for survival of AmB-resistant strains. Growth of AmB-resistant laboratory mutants and clinical isolates, as well as wild-type controls, in the presence of small molecule stress response inhibitors at the following concentrations: Geldanamycin and Radicicol, 2 pM; FK-506, 5 tg/mL; Cyclosporin A, 5 pg/mL; Enzastaurin and Cercosporamide, 5 pg/mL. Growth was assayed after 24 h; values indicate means of duplicate measurements, normalized to wildtype in DMSO. (C) Hogl, but not calcineurin or PKC, is required for wild-type levels of AmB tolerance in the absence of ergosterol biosynthesis mutations. Wild-type, cnbi, and hog] strains, as well as wild-type with 1 or 5 pM geldanamycin, were tested for AmB MIC by microplate dilution. Growth was assayed after 48 h to highlight differences in drug tolerance between strains; values indicate means of duplicate measurements, normalized to the wild type in the absence of AmB. (D) Hogl, Cnbl, and high levels of Hsp90 are required for the de novo emergence of AmB-resistant colonies. ERG2/erg2 heterozygotes from wild-type, cnb], or hog] backgrounds were plated at a density of 8x 106 cells per plate on media containing 0.6 ptg/mL AmB. The wild-type was also plated on media containing AmB and 2.5 pM geldanamycin. Plates were photographed after 3 d. 77 A - - Wild-Type CM erg3A/A erg2A/A - erg6A/A erg3, 11A/A Clinical 37'C 41'C 39'C Hypochlorous Acid B 1.00- 37'C 39'C 0.5mM 0.25mM Peroxide Peroxide DPTA-NONOATE (NO donor) C 1 1.00T Relative Growth 0.75- 0.75 0.50-. Relative Growth 0.50. 0.25- 0.25- 0.00 1 I 0.081 Tf 441 E Calprotectin/S1OOA9 Peptide BPS (Iron Starvation) 1.25- 1.00Relative Growth 0.75. Relative 1.00Growth 0.75- 0.50- 0.50- 0.25] 0.25- T 0.00 G F Neutrophil:Candida Co-Culture Serum Proliferation, 39.5*C 1.00- +0 WT CFUImL + erg2AIA 1 erg6A/A Relative 0.75- erg3A/Aerg11A/A + Clinical + Growth 0.50- 102 0.25- 0 4"M Ulp 0.00 48 Tim (hr) ~&I" / 4 78 Figure 4. AmB-resistant strains are hypersensitive to the stresses of the host environment. (A) AmB-resistant strains are sensitive to very high febrile temperatures and extremely sensitive to oxidative stress, especially at elevated temperature. Wild-type and AmB-resistant strains were spotted by serial dilution on RPMI media with or without tert-butyl peroxide at the concentrations indicated. (B-E) AmB-resistant strains are hypersensitive to stresses encountered in the host environment. Wild-type and AmBresistant strains were grown in RPMI media containing 2 mM of hypochlorous acid (B) or 4 mM of the nitric oxide donor DPTA-NONOATE (C), two neutrophil-secreted products that are the critical final effectors of anti-Candidaimmunity. Sensitivity to iron deprivation was tested by growth in RPMI + 500 iM of the iron chelator bathophenanthrolinedisulfonic acid (D). No increase in sensitivity to the antimicrobial peptide Calprotectin (10 pg/mL) (E) was observed. Growth values were obtained by normalization to wild-type growth in the same condition. All mutant strains were significantly more sensitive than wild-type to the tested concentrations of hypochlorous acid, DPTA-NONOate, and BPS at 37 'C (**p < 0.01, two-tailed Student's t test), but not to calprotectin. Values indicate the mean of two independent experiments of three replicates each; error bars indicate SEM. (F) AmB-resistant strains proliferate more slowly than wild type in serum at elevated temperature. Wild-type and AmB-resistant strains were inoculated in 100% fetal bovine serum at 39.5 'C, and viable colony-forming units were determined by plating dilutions on YPD after 24 and 48 h. Error bars indicate SEM. (G) AmB-resistant strains are hypersensitive to killing by neutrophils. Human neutrophils were isolated from whole blood (see Materials and Methods) and activated by treatment with recombinant TNF-a. Candida were added to wells containing neutrophils at a 1:1 effector:target ratio and incubated at 37 'C for 6 h, at which point neutrophils were lysed and Candidagrowth was quantitated with Alamar blue. Percent growth for each strain was calculated as the fraction of growth in the presence of neutrophils to growth in the absence of neutrophils; mutants were normalized to growth of the WT on each plate. The experiment was performed with a total of three biological replicates from two separate days; error bars indicate mean and SEM. 79 YPD, 30 0C Serum/37 0 C Serum/37 0C 2 hr 4 hr A WildType erg3AA erg2lA erg6AA erg3AIA erglI A AmB-R Clinical Isolate 40- -TPercent 30Cytotoxicity (LDH Release) * B F,,i1 2010- 40 0 80 Figure 5. AmB-resistant strains are defective in filamentation and tissue invasion. (A) AmB-resistant mutants fail to properly induce filamentous growth upon stimulation. Wild-type strains and resistant mutants were grown in YPD and then inoculated into RPMI media containing 10% fetal bovine serum at 37 'C. Strains were analyzed by DIC microscopy after 2 and 4 h. (B) AmB-resistant strains cause much less damage to endothelial monolayers than wild type. Monolayers of HUVECs (human umbilical vein endothelial cells) were established and infected with C. albicans. After 6 h, endothelial cell cytotoxicity was assayed by quantifying LDH release, using uninfected cells as a negative control and cells lysed with 1% Triton X-100 as 100% lysis control. Data were pooled from two independent experiments with six replicate wells each; error bars indicate SEM. All mutant strains were significantly less cytotoxic than wild type (*p < 0.05, **p < 0.01, two-tailed paired Student's t test). 81 Mouse Tall Vein Infection 100. - - A -u- WT + erg3AIA Percent 75 Survival erg2AI4 erg6AIA erg3A/Aerg1 IAIA + Clinical 50 -+- 250. - 1 0 1 B . 2 3 4 7 . . 5 5 7 3 9 Time (days) . 10 11 12 Kidney Colony Forming Units at Sacrifice 107Total CFU 104105* 103102101. own -7*.. AA vY0 AA I>' *44~~4 C C Wild-Type erg3AA erg2AA erg6AA 82 erg3AA;ergllAA Clinical Isolate AmB-resistant strains are avirulent in a mammalian model of Figure 6. disseminated candidiasis. (A) AmB-resistant mutants do not cause morbidity even when injected into mice at a high inoculum. Wild-type, erg3, and AmB-resistant mutants were grown into log phase for 5 h in YPD, counted, and 4x 106 cells of each strain were injected into the tail vein of 7-9-wk-old Balb/c mice (n = 8-14 mice per strain). Mice were monitored for weight loss and sacrificed after a >20% drop in body weight or appearance of morbidity. All surviving mice were sacrificed after 12 d. (B) AmBresistant strains are unable to colonize the mouse kidney. Colonies were counted after homogenization and plating in duplicate of viable candida from one kidney of each infected mouse at the time of sacrifice. As wild-type, erg3, and other mutants survived for different periods of time before sacrifice, direct comparisons cannot be made between these groups based on CFU values. However, the extremely low CFU values from AmBresistant strains are typically indicative of sterilization. (C) AmB-resistant strains do not damage the mouse kidney. Kidneys from each infected mouse were fixed and stained with periodic acid-Schiff stain to visualize Candida and kidney pathology. Wild-type and erg3 strains demonstrated filamentous growth and severe kidney pathology, which was even greater in the erg3 strain. Examples of sites where fungi are observed are highlighted with a black arrow; fungi appear as long filaments with a purple color. No viable Candida were seen in sections from mice infected with AmB-resistant strains. Scale bar, 50 gm. 83 Insertion region A WildType I *, i~' AmphB- Transposon Resistant Mate pairs -.- ~ ------ t~1 TCA2 Transposon Endogenous Locus (Chromosome 7) ERG2 (Chromosome 1) B Chri Chr2 Chr3 Chr4 Chr5 Chr6 Chr7 ChrR 0.4 Mean Heterozygosity 0.1 ERG2 (Chrl:155,291 to 154,638) Supporting Information Figure S1. Trasposon insertion and heterozygosity analysis in AmB-resistant C. albicans. (A) Insertion of TCA2 retrotransposon into ERG2 locus. Mapping of reads from wild-type (SC5314) and AmB-resistant (ATCC 200955) C. albicans. Left, ERG2 locus on chromosome 1; right; TCA2 locus on chromosome 7. Mate-pairs of reads in the AmB-resistant strain in which one mate maps to ERG2 and the other to TCA2 (identified by long insert sizes) are depicted in the lower panel. All screenshots were generated by the Integrative Genomics Viewer (IGV) [53]. (B) Whole-genome heterozygosity analysis of C. albicans ATCC 200955. Single-nucleotide-polymorphisms (SNPs) were analyzed for base ratio at each variant site to determine an allelic ratio; the mean heterozygosity value for total heterozygosity is 0.5, and for total homozygosity the value is 0.0. Base ratios were averaged over a 1 kb sliding window for each chromosome. 84 S258F ERG3 B C. A. H. LHKPHHKWIVCTPFASHAFHPVDGFFQSLPYH LHKPHHKWIMPSPFASHAFHPLDGWSQSVPYH LHKPHHIWKIPTPFASHAFHPIDGFLQSLPYH albicans fumigatus sapiens C ERG11 C. tropicaliscontigs (unassembled) D a aa a z zz z S 00 528 0 0 03 1 a a a a 5, 2, Z Z Z Z 5, 8, 1 06 05 07 08 a 2, 09 0.4- Mean Heterozygosity 0.1 ERG3 ERG11 85 a a z z 2 10 1 Figure S2 AmB-resistance mutations and heterozygosity analysis in AmB-resistant C. tropicalis. (A) Mutation in ERG3 changing conserved serine 275 residue to phenylalanine in C. tropicalis ATCC 200956. (B) S275 is universally conserved in Erg3 homologs. Alignment of protein sequence surrounding S275 from Erg3 homologs of C. albicans, A. fumigatus (XP_747563), and H. sapiens (BAA33729). (C) 170-nucleotide deletion from ERG]] of C. Tropicalis ATCC 200956, detected as the complete absence of reads mapping to this region of the gene. Unnecessary lines generated by IGV (not representative of data) were removed. (D) Heterozygosity analysis of ATCC 200956; the incomplete assembly of the C. tropicalis genome requires the use of smaller sequence contigs. 86 .. . .... .. .. ..... ... ........... .................... A cd cd chri ews chrS d"r B chtR - U chi7 Ca21chr3_C albicansSC5314 I 0 Isolates CW) 6 #1 #2 0 #3 6 #4 E- 2e+05 6e+05 4e+05 position 87 8e+05 Figure S3 Heterozygosity analysis of in vitro-evolved series. (A) Whole-genome analysis of loss of heterozygosity events across four sequenced isolates from in vitro-evolved series (from Figure 1B). A list of all SNP positions in the four strains was compiled and then analyzed for heterozygosity by base ratio (see Materials and Methods). Sites homozygous for the reference base are depicted in blue, homozygous for the variant base in red, and heterozygous in white. The loss of heterozygosity is focused on the left arm of chromosome 3, which contains ERG6. (B) Heterozygosity analysis of chromosome 3 demonstrates loss of heterozygosity in isolate #4. Sliding-window analysis of base ratio along chromosome 3 depicts loss of heterozygosity in the left arm of chromosome 3. 88 A Wild-type CE1 efg2-1Ml Clinical isolate M erg6-1- & MIC, PM - 643216. -il 2- erg3erg 11- U.5. 0.250.125 0.0625 0.03125 19\1 B N Wild-type 32 MIC, PM pM 32 - 4 2 11 0.5 0.25 0.1250.0625- 19N C U F ~] U* U* U* 1024- 4? <1. Fold Sensitivity Ratios (WT MIC/Mutant MIC) Compound/Strain Anisomycin Benomyl Nocodazole MNNG 4NQO Mycophenolic Acid Nourseothricin Geldanamycin Radicicol NVP-AUY922 SNX-2112 erg2-/4.00 2.00 2.00 2.00 4.00 1.67 8.00 32.14 24.00 27.31 21.33 ATCC200955 4.00 2.00 2.00 3.00 2.00 5.00 8.00 28.80 18.00 27.31 21.33 89 erg6-/- erg3, 11-/8.00 5.33 4.00 2.00 8.00 4.00 6.00 3.00 8.00 4.00 10.00 2.50 16.00 8.00 480.00 96.00 384.00 96.00 222.61 109.40 256.00 85.33 erg2-/clinical isolate erg6-/erg3ergll-- Figure S4 Minimal inhibitory concentrations of Hsp90 inhibitors and cytotoxic compounds. (A) Sensitivity of AmB-resistant mutants to diverse cytotoxic compounds. MIC80 of each strain against each compound was determined by microplate dilution assay in YPD at 30 'C. (B) MIC80 of strains to four Hsp90 inhibitors in YPD at 30 'C. (C) Fold sensitization, relative to wild-type, of mutant strains to cytotoxic agents and Hsp90 inhibitors (Hsp90 inhibitors highlighted in red for clarity). Table indicates the value obtained when the MIC80 for each compound in the wild-type strain is divided by the MIC80 for that compound in that mutant strain. 90 0 A 0.05 0.1 0.2 0.4 0.8 1.6 [AmB] (pg/mL) Wild-type erg2A/A #2 erg6A/A #2 0.00 0.25 0.50 0.75 1.00 Relative Growth erg3/ergllA/A #2 c B DPTA-NONOATE (NO donor) Hypochlorous Acid In 1.00-. 1.00- Relative Growth Relative 0.75. Growth 0.50- 0.60- 0.25n nn 0.75- 0.25- II ,_ I e ** .*-- ~r~i *r 499 At- A D YPD, 30"C RPMl+FBS, 37-C, 4hr Wild-Type erg2A/A #2 erg6AIA #2 erg3AIA erg1IA/A #2 91 Figure S5 Validation of additional mutant strains. (A) AmB susceptibility of a second, independently generated laboratory deletion mutant in ERG2, ERG6, or ERG3 and ERG]], performed as described in Figure 1D. (B) Sensitivity of each additional mutant to hypochlorous acid (B) and DPTA NONOate (C), performed and analyzed as described in Figure 4B-C (**p < 0.01, Student's t test). (D) Filamentation of each additional mutant in response to stimulation by fetal bovine serum at 37 'C in RPMI media, performed as described in Figure 5A. Strain Name/Name in Genotype Source Prototrophic (naturally erg2/erg2) ATCC Prototrophic (naturally erg3/erg3, erg]I/erg1) Prototophic ATCC Prototrophic As ATCC 10231, erg6 D1 80G As ATCC 10231, erg6 D1 80G (3:1) As ATCC 10231, erg6 Q70stop/Q70stop Prototrophic ATCC This study This study This study White TC, 1997 LEU2/leu2A HIS1/his1A arg4A/arg4A URA3/ura3A::imm 434 IRO1/iroIA: :imm 434 leu2A/leu2A his1A/hislA arg4A/arg4A URA3/ura3A: :imm 434 Noble et al, 2005 Text ATCC 200955 (AmB-R Clinical C. albicans) ATCC 200956 (AmB-R Clinical C. tropicalis) MYA-3404 (C. tropicalis WT reference strain) ATCC 10231/in vitro #1 AmB-R#2/in vitro #2 AmB-R#3/in vitro #3 AmB-R#4/in vitro #4 Fluconazole-R #2 (CaCi-2) SN250/Wild-Type SN152 ATCC Noble et al, 2005 IRO1/irolA::imm434 BV06/erg2A/z BV07/ erg3J/ BV08/ erg4A/A BV09/ erg5AI/A As SN 152, erg2A::C.d.HIS]/erg2A:C.m.LEU2 As SN 152, erg3A::C.d.HIS/erg3A:C.m.LEU2 As SN152, erg4A::C.d.HIS/erg4A:C.m.LEU2 As SN152, 92 This study This study This study This study BV10/ erg6l/ BV1 1/ erg3A/A erg] zA/A erg5A::C.d.HISJ/erg5A:C. m.LEU2 As SN 152, erg6A::C.d.HISJ/erg6A:C.m.LEU2 As SN152, erg3A::C.d.HIS/erg3A:C.m.LEU2 This study This study erg]JA:C.d.ARG4/ergl lA/C. d.ARG4 BV12 /erg24/z BV13/ cnbi/zI BV14/ hogzI/z BV16/ WT, ERG2/erg2A BV17/ cnb z/zA, ERG2/erg2A As SN152, erg24A.C. dHISJ/erg24A:C.m.LEU2 As SN152, cnblA::C.d.HIS/cnbIA:C.m.LEU2 As SN152, hogIA::C.d.HIS/hogIA:Cm.LEU2 As SN250, ERG2erg2A::C.d.ARG4 As SN152, cnbi A::Cd. HISJ/cnbi A:C.m.LEU2; This study This study Noble et al, 2010 This study This study ERG2/erg2A::C.dARG4 BV18/ hogl/A, ERG2/erg2A As SN152, hogIA::C.dHIS/hogIlA:Cm.LEU2; ERG2/erg2A::C.dARG4 Table S1 Strains used in this study. List of strains used in this study. 93 This study Name Use Sequence SN-2 bridging primer for all deletions ccgctgctaggcgcgccgtgACCAGTGTGATGGATATCTGC ERG2-del-upF bridging primer for all deletions Upstream deletion fragment ERG2-del-upR Upstream deletion fragment SN-5 ERG3-del-upF Downstream deletion fragment Downstream deletion fragment Check insertion of deletion checking loss of endogenous gene checking loss of endogenous gene Upstream deletion fragment ERG3-del-upR Upstream deletion fragment ERG2-del-dnF ERG2-del-dnR ERG2-delupcheck ERG2intcheck-F ERG2intcheck-R ERG4-del-upF Downstream deletion fragment Downstream deletion fragment Check insertion of deletion checking loss of endogenous gene checking loss of endogenous gene Upstream deletion fragment ERG4-del-upR Upstream deletion fragment ERG3-del-dnF ERG3-del-dnR ERG3-delupcheck ERG3intcheck-F ERG3intcheck-R gcagggatgcggccgctgacAGCTCGGATCCACTAGTAACG AGTAATGGTTGCTCCGGTTG CACGGCGCGCCTAGCAGCGGTGATACGTTTCGGTTCTCTGTC GTCAGCGGCCGCATCCCTGCTAATAGAGGGGGCACGGATT ATCCATGGCAACAAATGAAA AATCGTATCCCTTCGTCGTC CCACGGCCATTATGATTGAT GATTGATCCAGTACCAGCATGA CCTTTGCATTTGCTAAAATCTG CACGGCGCGCCTAGCAGCGGAAAATTGGCTAAACCGAATCC GTCAGCGGCCGCATCCCTGCCATCTTTGTTTTGGACCATTGA CAAAGCCAACCAGATCATCA TGTGCAGGAATGCAATTGTT GATTTCCCAAGTCTCCCAAA GGAAGAACCCATCAACTGGA AAT GAC GTC TCC CCC TCT TT CAC GGC GCG CCT AGC AGC GGT GTT GAT GGT TGT AAA ATG AAA AA 94 ERG5-del-upF Downstream deletion fragment Downstream deletion fragment Check insertion of deletion checking loss of endogenous gene checking loss of endogenous gene Upstream deletion fragment ERG5-del-upR Upstream deletion fragment ERG4-del-dnF ERG4-del-dnR ERG4-delupcheck ERG4intcheck-F ERG4intcheck-R ERG6-del-upF Downstream deletion fragment Downstream deletion fragment Check insertion of deletion checking loss of endogenous gene checking loss of endogenous gene Upstream deletion fragment ERG6-del-upR Upstream deletion fragment ERG5-del-dnF ERG5-del-dnR ERG5-delupcheck ERG5intcheck-F ERG5intcheck-R ERG6-del-dnR ERG6-delupcheck ERG6intcheck-F ERG6intcheck-R ERG 1-delupF Downstream deletion fragment Downstream deletion fragment Check insertion of deletion checking loss of endogenous gene checking loss of endogenous gene Upstream deletion fragment ERGL 1-delupR Upstream deletion fragment ERG 1-deldnF ERGI1-deldnR ERGL 1-delupcheck ERGI 1intcheck-F ERGI1intcheck-R ERG24-delupF Downstream deletion fragment Downstream deletion fragment Check insertion of deletion checking loss of endogenous gene checking loss of endogenous gene Upstream deletion fragment ERG24-delupR Upstream deletion fragment ERG24-deldnF ERG24-deldnR Downstream deletion fragment Downstream deletion fragment ERG6-del-dnF GTC AGC GGC CGC ATC CCT GCT TGC TAA GCT ACA TAA TAT CAA AAT CA CCA CTG GTC CAA AAC AAC AA CCA CTG GTC CAA AAC AAC AA GCT GGG GTT CCA TTC AGT TA AAT GGA GAT CCA AAC CCA CA GCAACGCGTAACAACACACT CACGGCGCGCCTAGCAGCGGAAAGTGAATGTTTTGTGGTTTTTG GTCAGCGGCCGCATCCCTGCGAGGGAAATAAGTAGGTCAAAACAA CGAGGTTGCTCCATCAATTT GTTCCGGTTGGATCGAATTA TGCTTCATCTCGTGATTTGG AATGATCGGGAAATTGACCA CGATGGCCGTAGTTCTTACA CACGGCGCGCCTAGCAGCGGGAAAATGAAAGGTTCTTTAACTTGA GTCAGCGGCCGCATCCCTGCGGGGCTTGACAAACAACAAG GCTAAGCCCATTTTCAGTGG CCGAAATATCATTGGGAACG GTGGTGTAGGTGGTCCTGGT GTTGTTTGTCAAGCCCCATT TTTGAGAACAGCCACACGAC CACGGCGCGCCTAGCAGCGGTGAGTTATGATCTTCTTGAAAAGAAAC GTCACCGGCCGCATCCCTGCCGGCAACTTTCTTTCGATTC AGCAGATGATGCTGGAACCT GCCGGGAATAACTGAGAAAA TTTGACCGTTCATTTGCTCA TAGCTTTGGCAGCAGCAGTA TTGAACCCCATCCAAATTGT CACGGCGCGCCTAGCAGCGGAACTTTGGTTAGTTATTTTGTGGAAA GTCAGCGGCCGCATCCCTGCAAAACAAACAAGGAAAGCGAAT AAATGATGCCGAAATCGAAC 95 ERG24-delupcheck ERG24intcheck-F ERG24intcheck-R CNBl-del-upF CNB1-delupR Check insertion of deletion checking loss of endogenous gene checking loss of endogenous gene Upstream deletion fragment Upstream deletion fragment CNBl-del-dnF Downstream deletion fragment CNBl-deldnR CNB1-delupcheck CNB1intcheck-F CNB1intcheck-R Downstream deletion fragment Check insertion of deletion checking loss of endogenous gene checking loss of endogenous gene YHB1-RT-F RTPCR AAGTTGCTCCTCCTGCTGGTAAT YHB1-RT-R RTPCR TCCTTGTCTGTAGCTGGGTCATAGA RBT5-RT-F RTPCR GTTCTGTTGAATCTTTGGCCAC RBT5-RT-R RTPCR AGCCTTAGCCAAAGCGTCA FET34-RT-F RTPCR ATGAGGAGGAGGAAGAACAAAGC FET34-RT-R RTPCR GGGCTAGAAGAGGAACCAGTTG FTRT-RT-F RTPCR TATCATTGCCACGGTCTTGA FTR1-RT-R RTPCR GGACCAGAACCGTTTTCAGA FTH1-RT-F RTPCR CCCAACTGAATCTGATGACCTTAC FTHI-RT-R RTPCR GCCAACACAGCAGCATTTAC SITI-RT-F RTPCR CTGCCAGTCAACCCGTCTATG SIT1-RT-R RTPCR AACTCCAAACGACCAAGGACAT CRHI-RT-F RTPCR CCAGTTCTTCATCCAGCTCA CRH II-RT-R RTPCR CCAATCAATGCAACAAAGCC DDR48-RT-F RTPCR TTCGGTAAAGACGACGACAAAGA DDR48-RT-R RTPCR GCCAAATGAAGAGGATCCATAAGA STP4-RT-F RTPCR TCCTTTCAAGAACATCGATTCA STP4-RT-R RTPCR TTATGCATCCAATCATCGACA CAT1-RT-F RTPCR TTG GTC AAC ACG GTC CAT T CAT1-RT-R RTPCR CCA TAA GCA CCG GAA CCT T GPX1-RT-F RTPCR ATG GCA AGA ACC AGG CAC TA GPX1-RT-R RTPCR CTG GAT CTG CTT GTT CAC CA UTR2-RT-F RTPCR CCATGCTGTTCTCAATTTGGTA UTR2-RT-R RTPCR TCTAGGCATAGGCATACAAGCA RTA2-RT-F RTPCR AAG AGC CAC ACA AGC GAT TT RTA2-RT-R ECM331-RTF ECM331 -RTR RTPCR TCC CGT GAA TAA CCA CCA AT RTPCR GAGTATTCTCAACTCCCCATCG RTPCR AAATCGCAAAGGAAGGTAATGA TEF3-RT-F RTPCR CCA CTG AAG TCA AGT CCG TTG A TEF3-RT-R RTPCR CAC CTT CAG CCA ATT GTT CGT AAGGTTTCCAGACATTCCACA TGGCTGGCCTATTTAGCTTG ACGACCAATGAACCAATCGT TTCTGGTGGCTCATTCTTTG GGGAAGAGAATTGAACAGGTTG CACGGCGCGCCTAGCAGCGGTTGTCAGTAGTTGTTGAAGTCGAA GTCAGCGGCCGCATCCCTGCCAACAGTTTTGGTTTAGTTCATGT TTGTTGAGCAGGTTGCTGTC TAAAGATGGGTCAGGGCAAA CGTCCAAATCAGCTTCCATT 96 ACT1-RT-F RTPCR GCT TTT GGT GTT TGA CGA GTT TCT ACT1-RT-R RTPCR GTG AGC CGG GAA ATC TGT ATA GTC TDH3-RT-F RTPCR ATC CCA CAA GGA CTG GAG A TDH3-RT-R RTPCR GCA GAA GCT TTA GCA ACG TG RPP2B-RT-F RTPCR ACT TAG CTG CTT ACT TAT TGT TAG Table S2 Oligonucleotide sequences used in this study. Oligonucleotide primer sequences used in the generation of mutants and RT-PCR experiments. 97 Chapter Three: Non-Toxic Antimicrobials that Evade Resistance *This chapter has been submitted for publication and is under peer review **My contribution included designing and performing the experiments included in Figure 4, as well as writing the text describing these experiments and portions of the abstract and discussion 98 Non-toxic antimicrobials that evade drug resistance Stephen A. Davis', Benjamin M. Vincent 2,3, Matthew M. Endo', Luke Whitesell 3 , Karen Marchillo, David R. Andes5 , Susan Lindquist 3,4 *, and Martin D. BurkeI* 1Howard Hughes Medical Institute, Roger Adam Laboratory, Department of Chemistry, University of Illinois at Urbana-Champaign, Urbana, IL 61801, United States. 2Microbiology Graduate Program, Massachusetts Institute of Technology, Cambridge, Massachusetts, United States of America 3 Whitehead Institute for Biomedical Research, Cambridge, Massachusetts, United States of America, 4 Howards Hughes Medical Institute, Department of Biology, Massachusetts Institute of Technology, Cambridge, Massachusetts, United States of America 5Departments of Medicine and Medical Microbiology and Immunology, University of Wisconsin, Madison, Wisconsin, United States. *To whom correspondence should be addressed ABSTRACT Drugs that act more promiscuously provide fewer routes for the emergence of resistant mutants. But this benefit often comes at the cost of serious off-target and dose-limiting toxicities. The classic example is the antifungal amphotericin B (AmB), which has evaded resistance for more than half a century. We report dramatically less toxic amphotericins that nevertheless evade resistance. They are scalably accessed in just three steps from the natural product, and bind their target (the fungal sterol, ergosterol) with far greater selectivity than AmB. Hence, they are less toxic and far more effective in a mouse model of systemic candidiasis. Surprisingly, exhaustive efforts to select for mutants resistant to these more selective compounds revealed that they are just as impervious to resistance as AmB. Thus, highly selective cytocidal action and the evasion of resistance are not mutually exclusive, suggesting practical routes to the discovery of less toxic, resistance-evasive therapies. Introduction Less selective pharmacological action is generally associated with decreased vulnerability to resistance, but also with increased toxicity" 2 . The classic example is amphotericin B (AmB), an exceptionally resistance-evasive but also highly toxic antifungal agent that has remained the last line of defense in treating invasive fungal infections for over half a century 3 . An excess of 1.5 million people die from such 99 I infections each year 4, in large part because the extreme toxicity of AmB is dose-limiting'. Extensive efforts to develop a clinically viable less toxic amphotericin have been made, but without success5 . Moreover, it has remained unclear whether such a decrease in toxicity would come at the cost of an increase in vulnerability to pathogen resistance. For decades the pursuit of a less toxic amphotericin was guided by the widely accepted model in which AmB (Fig. la) kills cells via ion channel-mediated membrane permeabilization5 ' 6 . This model suggests that improving the therapeutic index of this drug requires the selective self-assembly of oligomeric ion channels in yeast vs. human cells, a problem that has been very challenging to approach rationally. Contrary to this model, it was recently shown that AmB primarily exists as a large extramembranous aggregate which kills yeast by simply binding 7 and extracting8 ergosterol, and likely kills human cells by similarly binding cholesterol 9 . Ergosterol is critical for many different aspects of yeast physiology 0-14 , and mutations that alter sterol biosynthesis in a manner that confers resistance abrogate fungal virulence15 , explaining the failure of fungi to evolve AmB resistance in the clinic. This new sterol sponge model enabled efforts to improve the therapeutic index of AmB to focus on the simpler problem of selectively binding sterols, and this yielded the recent discovery of a new derivative, C2'deoxyAmB (C2'deOAmB) (Fig. la) that binds ergosterol but not cholesterol and is toxic to yeast but not human cells9 . Limited synthetic access to this derivative, however, has hindered its further development and the determination of whether this improvement in therapeutic index is coupled to a decreased capacity to evade resistance. To rationalize the greater ergosterol-selective binding observed with C2'deOAmB we took into consideration several new structural insights regarding these prototypical small 100 molecule-small molecule interactions. First, the mycosamine appendage is critical for binding both ergosterol and cholesterol1 6 . Recent solid-state NMR evidence also confirms direct contact between the A and B rings of ergosterol and the AmB polyene motif in the sterol sponge complex8 . Furthermore, a recent crystal structure of an AmB derivative1 7 (Fig. Ic) reveals a water-bridged hydrogen bond between the C2' and the C13 hydroxyl groups. We propose that such intramolecular hydrogen bonding fixes the relative positions of the mycosamine appendage and the polyene motif enabling AmB to bind both ergosterol and cholesterol, and that deletion of the C2' hydroxyl group favors a shift to an alternate conformer that selectively binds ergosterol. Alternatively stated, this model predicts that a protein-like' 8 -22 ligand-selective allosteric effect underlies these small molecule-small molecule interactions. Guided by this model, and further encouraged by previous reports of modest but promising improvements in therapeutic index 5, we pursued more synthetically accessible disruptions of a putative similarly ground state-stabilizing intramolecular salt bridge between the C41 carboxylate and C3' ammonium ions (Fig. la). RESULTS Three-step synthesis of AmB ureas All previously reported derivatives of AmB have maintained a C I6-C41 carboncarbon bond5 . Enabling us to explore a new chemotype, we discovered that treatment of a minimally protected variant of AmB (1) with diphenyl phosphoryl azide (DPPA) cleanly promotes a stereospecific Curtius rearrangement in which the C16-C41 bond is cleaved and the resulting isocyanate is intramolecularly trapped by the neighboring C15 alcohol23 101 to form an oxazolidinone 2 (Fig. ld). This particular oxazolidinone, in turn, is surprisingly reactive to ring-opening with primary amines under mild conditions to yield a new class of urea containing amphotericins (3) having a C16-nitrogen bond. Interestingly, the parent heterocycle, 2-oxazolidinone, is unreactive under the same conditions. We further found that 1 can be directly converted to 3 in a scalable one-pot operation involving serial addition of DPPA, an amine, and aqueous acid. Starting with 1 g of fermented AmB and using methyl amine as the nucleophile, this overall three-step sequence yields 264 mg of AmB methyl urea (AmBMU) (Fig. le). Employing ethylene diamine produces 236 mg of AmB amino urea (AmBAU), and in a four step-variant, reaction with P-alanine allylester followed by deallylation yields 124 mg AmB carboxylatoethyl urea (AmBCU). This chemistry thus provides rapid, efficient, and scalable access to these new derivatives starting with the natural product that is already fermented on the metric ton scale. AmB ureas are selectively toxic to yeast With this new series of AmB derivatives in hand, we first determined their sterol binding properties via isothermal titration calorimetry (ITC) (Fig. 2a)9 . AmB binds both ergosterol and cholesterol, but the aglycone, amphoteronolide B (AmdeB), binds neither sterol 16 . Like C2'deOAmB 9, all of the new C16 urea-containing derivatives retain the capacity to bind ergosterol but, within the limits of detection of this experiment, show no binding to cholesterol. This sterol binding selectivity translated into a major improvement in therapeutic index in vitro (Fig. 2b). Specifically, we determined the minimum inhibitory 102 concentration (MIC) against Saccharomyces cerevisiae and the minimum hemolytic concentration (MHC) against human red blood cells for AmB, a series of previously reported C41 and/or C3'-modified derivatives5 , and the new AmB ureas. AmB is a potent antifungal (MIC 0.5 gM), but is also highly toxic to human red blood cells (MHC 8.6 RM) (entry 1). AmdeB is non-toxic to both (entry 2)9,24. Previously reported modifications including methyl esterification (AmBME)25,26, carboxylic acid reduction (C41MeAmB) 24 , methyl amidation (AmBMA) 27, and double modification to form a triazoloethyl amide bis-aminopropyl derivative (AmBTABA) 28 produce modest improvements in therapeutic index (entries 3-6), with the best results obtained with AmBTABA (MIC 0.25 pM, MHC 49 pM) (entry 6). In contrast, all of the AmB urea derivatives retained antifungal activity but show dramatically reduced toxicity to human red blood cells. The MHC of AmBMU and AmBAU exceeds the limits of solubility in this assay (500 pM) (entries 7,8). Remarkably, the only structural difference between AmBMA (entry 5) and AmBMU (entry 7) is the insertion of a protonated nitrogen atom between the C16 and C41 carbons (Fig. la,c). The activities of the AmB urea derivatives were further tested against a series of pathogenic Candida strains (Fig. 2c) 29 . Both AmBMU and AmBAU demonstrate potent antifungal activity against all strains tested. AmBCU retained activity, but was in general somewhat less potent. The compounds were also tested for toxicity against human renal proximal tubule epithelial cells (RPTEC), the critical site of toxicity for AmB in patients. They all showed little or no toxicity to hTERT1 RPTEC 30 , and substantially reduced . toxicity to the more sensitive primary RPTEC 31 103 AmB ureas are more efficacious and less toxic in mice Based on all of these results, AmBMU and AmBAU were judged to be especially promising and thus further evaluated for efficacy and toxicity in vivo (Fig. 3a-d)32 . In a mouse model of disseminated candidiasis both AmBMU and AmBAU were substantially more effective than AmB at reducing fungal burden in the kidneys at all three tested doses (1, 4 and 16 mg/kg, intraperitoneal injection). The differences in efficacy were most pronounced at the 16 mg/kg dose at 24 hours post inoculation. Relative to AmB, AmBMU reduced the fungal burden by 1.2 log units (p < 0.0001), and AmBAU reduced the fungal burden by nearly 3 log units (p < 0.0001). We speculate that an improved pharmacological profile, potentially due to a >20 fold increase in water solubility relative to AmB, may contribute to this unexpected dramatic improvement in antifungal activity for the new compounds in vivo. Acute mouse toxicity was determined by single intravenous administration of AmB or its derivatives to healthy, uninfected mice and monitoring for lethality (Fig. 3d). All mice in the 4 mg/kg AmB dosage group died within seconds. AmBAU was drastically less toxic with >50% lethality only observed at the 64 mg/kg dosage group. Strikingly, all mice dosed with even 64 mg/kg AmBMU survived with no observable toxicity. AmB ureas still evade resistance We next investigated the impacts of increased ergosterol selectivity on the development of resistance to these analogs. Due to its unique mode of action7, AmB is not susceptible to most of the common mechanisms of resistance to other antimicrobials. Its lipid target is not as readily mutable as proteins or RNA; it is unaffected by efflux pumps; and its polyene macrolide structure is not a substrate for secretion via drug- 104 detoxifying enzymes. Moreover, ergosterol plays a central role in many aspects of yeast physiology' 0 ~4 . Mutations in genes involved in ergosterol biosynthesis can change sterol structures in ways that confer AmB resistance in vitro34, however, these mutations have enormous fitness costs in vivo, crippling fungal virulence". Consequently, resistance rarely, if ever appears in the clinic35 . We asked if the improved sterol selectivity of AmBMU and AmBAU rendered them more vulnerable to the evolution of resistance. We first determined the MIC of AmB, AmBMU and AmBAU against a panel of labgenerated strains carrying mutations in all seven of the non-essential C. albicans latestage ergosterol biosynthesis genes (Fig. 4a)'. Surprisingly, AmBMU and AmBAU displayed an in vitro resistance profile that was very similar to AmB (Fig. 4a). As for AmB, only erg2, erg6 or erg3/ergll mutants showed substantial resistance to AmBMU and AmBAU, and all of these mutants are known to be avirulent15 . Thus, known ergosterol biosynthesis mutations do not appear to be a threat to the efficacy of AmBAU and AmBMU. We next used exhaustive unbiased selections for survival in the presence of the compounds to ask if any other mutations could confer resistance to AmBMU or AmBAU. One-step selections on plates containing 8X the MIC of AmB, AmBMU or AmBAU yielded no colonies with stable resistance to any of the drugs, even after ethyl methanesulfonate mutagenesis. We then utilized a gradual resistance-selection protocol in liquid culture, with serial two-fold increases in drug concentration. Most serial selections ended in extinction of the lineage. However, we did recover 5-8 mutants for each drug that exhibited a ;>4-fold increase in MIC. Importantly, all of these substantially resistant 105 mutants were cross-resistant to all three compounds, suggesting no new mechanisms of resistance unique to AmBMU or AmBAU (Supplementary table I). To identify the mutations responsible for resistance in these selections, we used whole genome sequencing of the WT strain as well as all 11 of the in vitro-evolved resistant mutants, including both strongly and weakly-resistant isolates (Supplementary table 1). Most mutants with strong resistance to AmB or the derivatives contained mutations in the ERG2 or ERG6 locus that subsequently underwent a loss of heterozygosity (Fig. 4b)'. Unexpectedly, we also identified 3 independent mutants with low-level (~2-fold) AmB resistance mediated through a recurrent substitution in ORF19.7285 (D216Y), an uncharacterized WD40 repeat protein conserved across fungi. However, these mutants were no more resistant to AmBMU and AmBAU than to AmB (Supplementary table I). We then asked if any of the mutants with substantial resistance to AmBMU or AmBAU (>4-fold MIC increase) could elude the dramatic fitness defects previously demonstrated for AmB-resistance. As previously reported 5 , all AmB-resistant mutants are extremely sensitive to oxidative stressors, which are continually encountered during the course of infection. In addition, they become highly dependent on the molecular chaperone Hsp90, which supports diverse fungal stress responses' . All of the mutants resistant to AmBMU or AmBAU were likewise severely sensitized to the oxidative stressor tert-butyl hydrogen peroxide and the Hsp90 inhibitor geldanamycin (Fig. 4c,d). Previous work has also demonstrated that AmB-resistance mutations disable filamentation, a key driver of virulence in Candida15 . Again, in response to stimulation 106 with fetal bovine serum at 370 C, all mutants with strong resistance to AmBMU or AmBAU were unable to form the filaments observed in the wild-type (Fig. 4e). We next asked if resistance to AmBMU or AmBAU reduces competitive fitness in vivo. To do this, we infected mice with a pool of strains, consisting of the wild-type parent (AmBMU and AmBAU-sensitive) and 15 AmBMU or AmBAU-resistant mutants (with each strain comprising 1/ 1 6 th of the total population). After allowing the infection to proceed for four days (in the absence of drug treatment), we euthanized the mice and tested the drug sensitivity of fungal colonies isolated from in the kidneys to determine the AmBMU and AmBAU-resistant fraction of the final population. Indeed, even over this short period of infection, the percentage of the surviving population resistant to AmBMU or AmBAU dropped dramatically and the drug-sensitive parent rapidly overtook the population (Fig. 4f). Finally, we tested if any of our AmBMU or AmBAU-resistant mutants retained the capacity to cause lethal infection. To do so, we inoculated mice with pools of resistant mutants and compared their survival to mice infected with wild-type strains. At a low inoculum (to match that of an individual resistant strain) the wild-type strain killed all infected mice (Fig. 4g). Wild-type strains subjected to the same mutagenesis and in vitro passaging used to generate the resistant strains also killed all of the mice. In stark contrast, all mice infected with pools of mutants selected for resistance to AmB, AmBMU or AmBAU survived the infection (Fig. 4g). Thus, AmBMU and AmBAU are no more vulnerable to resistance than AmB, which has evaded resistance despite widespread clinical utilization for over half a century. DISCUSSION 107 Our findings collectively reveal that selective antimicrobial action and evasion of resistance are not mutually exclusive. Here, compounds that bind with high selectivity to a pathogen-specific lipid evade the emergence of virulent resistant strains, suggesting major costs in fitness are caused by even small changes in the structure of this lipid. This is likely because ergosterol is a central molecular node 36 in yeast physiology, being critical for the function of membrane proteins10, endocytosis", vacuole fusion12 membrane compartmentalization", and pheromone signaling 4 Our results further suggest that AmBMU and AmBAU are exceptionally promising candidates for replacing AmB as a less toxic treatment for invasive fungal infections. These new derivatives bind ergosterol but not cholesterol, are substantially more effective and less toxic than AmB in vivo, yet still evade resistance. Moreover, these compounds are accessed in just three steps from AmB, which is already fermented and commercially available on the metric ton scale. All of the reagents used in their synthesis are already employed on the process scale to prepare other pharmaceuticals, including diphenyl . phosphoryl azide 37 39 Our results also support a novel ligand-selective allosteric-effect model for guiding the rational development of other non-toxic amphotericins. This model predicts that disruption of intramolecular polar interactions between functional groups on the macrolide core and the mycosamine appendage cause a conformational shift in the molecule, from one that binds both ergosterol and cholesterol to one that selectively binds ergosterol. Strikingly, the portion of AmB that contains all of these functional groups, i.e., the module comprised of C13-C23, is 100% conserved in every member of the mycosamine-bearing polyene macrolide family of natural products40 . This includes a 108 collection "aromatic polyenes" that are reported to be orders of magnitude more potent . than AmB 4 1 and effective against even very challenging to treat Aspergillus infections4 2 Thus, synthesizing the analogous urea derivatives of other polyene macrolide natural products could lead to ultrapotent and/or broader spectrum yet still minimally toxic new antifungal agents. More broadly, our results show that targeting pathogen specific and polyfunctional lipids represents a promising blueprint for achieving the highly sought combination of low toxicity and evasion of resistance. Intriguingly, nisin, which binds a bacterial polyfunctional lipid, lipid II, has similarly evaded resistance despite half a century of use as a food preservative . It was recently discovered that binding of the same lipid underlies the action of defensin peptides 44, critical components of innate immunity that have retained antibiotic activity over more than two billion years of evolution. Other recent studies increasingly show that specific lipid-transmembrane protein interactions are critical for diverse cellular functions4 5 . Thus, as new microbe-specific and polyfunctional lipids are discovered4 6 , they present outstanding targets for the rational development of other non-toxic yet still resistance-evasive antibiotics. Methods General Reaction Conditions Due to the light and air sensitivity of amphotericin B (AmB), all reactions were performed in oven or flame dried glassware under an atmosphere of argon under low light conditions. Compounds were stored under an anaerobic atmosphere. All solvents were dispensed from a solvent purification as described by Pangborn and coworkers 47 109 (THF, Et2 0: dry neutral alumina; DMSO, DMF, CH 30H : activated molecular sieves). Triethylamine and pyridine were freshly distilled under nitrogen from CaH2. Camphorsulfonic acid was recrystallized from ethanol. Water was doubly distilled or obtained from a Millipore (Billerica, MA) MilliQ water purification system. Reactions were monitored by RP-HPLC using an Agilent 1200 Series HPLC system equipped with an Agilent Zorbax Eclipse C 1 8 3.5-pm, 4.6 x 75 mm column with UV detection at 383 nm at 1.2 mL/min, or an Agilent 6230 ESI TOF LC/MS system equipped with an Agilent Zorbax Eclipse C18 1.8-pm, 2.1 x 50 mm column with UV detection at 383 nm at 0.4 mL/min. Full experimental details and characterization for new compounds appear in the Supplementary Information. Extinction Coefficient Determination Extinction coefficients (L mol~1 cm') were determined as previously reported 117,000), C41MeAmB 121,000), AmBMU (6406 = (6406 = (6406 164,000), AmdeB 102,000), AmBMA = 87,000), AmBAU (6406 (6406 (6406 = = 102,000), AmBME 114,000), AmBTABA = 87,000), AmBCU (6406 (6406 - and were as follows: AmB (6406 = = 58,000). Isothermal Titration Calorimetry ITC was performed as previously reported. Growth Conditions for S. cerevisiae. S. cerevisiae was maintained with yeast peptone dextrose (YPD) growth media consisting of 10 g/L yeast extract, 20 g/L peptone, 20 g/L dextrose, and 20 g/L agar for 110 solid media. The media was sterilized by autoclaving at 250'F for 30 min. Dextrose was subsequently added as a sterile 40% w/v solution in water (dextrose solutions were filter sterilized). Solid media was prepared by pouring sterile media containing agar (20 g/L) onto Coming (Coming, NY) 100 x 20 mm polystyrene plates. Liquid cultures were incubated at 30'C on a rotary shaker and solid cultures were maintained at 30'C in an incubator. Growth Conditions and MIC Assay for C. albicans, C. tropicalis, C. parapsilosis, and C. glabarata. The organisms were maintained, grown, subcultured, and quantified on Sabouraud dextrose agar (SDA; Difco Laboratories, Detroit, MI). Twenty-four hours prior to the study, the organisms were subcultured at 35'C. Minimum Inhibitory Concentration (MIC) Determination MIC determinations were performed in duplicate on at least two occasions using . the Clinical and Laboratory Standards Institute M27-A3 microbroth methodology 48 Hemolysis Assays Hemolysis experiments were performed following known procedures9 . Whole human blood (sodium heparin) was purchased from BioreclamationlVT (Westbury, NY) and stored at 4'C and used within two days of receipt. WST-8 Cell Proliferation Assays 111 Primary Renal Proximal Tubule Epithelial Cells Preparation. Primary human renal proximal tubule epithelial cells (RPTECs) were purchased from ATCC (PCS-400-010, Manassas, VA) and immediately cultured upon receipt. Complete growth media was prepared using renal epithelial cell basal medium (ATCC, PCS-400-030), renal epithelial cell growth kit (ATCC, PCS-400-040), and penicillinstreptomycin (10 units/mL and 10 ug/mL). Complete media was stored at 4'C in the dark and used within 28 days. Primary RPTECs were grown in CO 2 incubator at 37 'C . with an atmosphere of 95% air/5% CO2 TERT1 Renal Proximal Tubule Epithelial Cells Preparation. TERTI human renal proximal tubule epithelial cells (RPTECs) were purchased from ATCC (CRL-4031, Manassas, VA) and immediately cultured upon receipt. Complete growth media was prepared using DMEM:F12 media (ATCC, 30-2006), triiodo-L-thyronine (Sigma, T6397), recombinant human EGF (Life Technologies, PHG03 11), ascorbic acid (Sigma, A4403), human transferrin (Sigma, T8158), insulin (Sigma 19278), prostaglandin El (Sigma, P7527), hydrocortisone (Sigma, H0888), sodium selenite (Sigma, S5261), and G418 (Sigma, A1720). Complete media was stored at 4C in the dark and used within 28 days. TERTI RPTECs were grown in CO 2 . incubator at 37'C with an atmosphere of 95% air/5% CO 2 WST-8 Reagent Preparation. WST-8 cell proliferation assay kit (10010199) was purchased from Cayman Chemical Company (Ann Arbor, MI) and stored at -20'C and used within 6 months of 112 receipt. WST-8 reagent and electron mediator solution were thawed and mixed to prepare the WST-8 reagent solution. The solution was stored at -20'C and used within one week. WST-8 Assay. A suspension of primary or TERTI RPTECs in complete growth media was brought to a concentration of 1 x 105 cells/mL. A 96-well plate was seeded with 99 pL of the cell suspension and incubated at 37'C with an atmosphere of 95% air/5% CO 2 for 3 hours. Positive and negative controls were prepared by seeding with 100 [tL of the cell suspension or 100 pL of the complete media. Compounds were prepared as 5 mM (AmB) and 8 mM (AmBAU, AmBMU, AmBCU, and AmdeB) stock solutions in DMSO and serially diluted to the following concentrations with DMSO: 8000, 6000, 4000, 3000, 2000, 1500, 1000, 800, 600, 400, 300, 200, 100, 50, 25, 10, 5, 2.5, 1, 0.5, 0.25, and 0.1 pM. 1 pL aliquots of each solution were added to the 96-well plate in triplicate, with each column representing a different concentration of the test compound. The 96-well plate was incubated at 37*C with an atmosphere of 95% air/5% CO 2 for 24 hours. After incubation, the media was aspirated and 100 pL of serum-free media was added and 10 pL of the WST-8 reagent solution was added to each well. The 96-well plate was mixed in a shaking incubator at 200 rpm for 1 minute and incubated at 37'C with an atmosphere of 95% air/5% CO 2 for 2 hours. Following incubation, the 96-well plate was mixed in a shaking incubator at 200 rpm for 1 minute and absorbances were read at 450 nm using a Biotek HI Synergy Hybrid Reader (Wanooski, VT). Experiments were performed in triplicate and the reported cytotoxicity represents an average of three experiments. 113 Data Analysis. Percent hemolysis was determined according to the following equation: % cell viability = Abs ap- Abs-ng. neg. X xsample 100% Abs.pos.- Abs-neg. Concentration vs. percent hemolysis was plotted and fitted to 4-parameter logistic (4PL) 49 dose response fit using OriginPro 8.6. The MTC was defined as the concentration to cause 90% loss of cell viability. Ethics Statement All animal procedures were approved by the Institutional Animal Care and Use Committee at the University of Wisconsin according to the guidelines of the Animal Welfare Act, The Institute of Laboratory Animal Resources Guide for the Care and Use of Laboratory Animals, and Public Health Service Policy. In Vivo Murine Efficacy Study All studies were approved by the Animal Research Committee of the William S. Middleton Memorial VA Hospital (Madison, WI). Efficacy was assessed by CFU count in the kidneys of neutropenic mice with a disseminated fungal infection as described previously by Andes et a,''0 5 1 . A clinical isolate of Candida albicans (K-1) was grown and quantified on SDA. For 24 hours prior to infection, the organism was subcultured at 35'C on SDA slants. A 106 CFU/mL inoculum (CFU, colony forming units) was prepared by placing six fungal colonies into 5 mL of sterile, depyrogenated normal (0.9%) saline warmed to 35'C. Six-week-old ICR/Swiss specific-pathogen-free female mice were obtained from Harlan Sprague Dawley (Madison, WI). The mice were 114 weighed (23-27 g) and given intraperitoneal injections of cyclophosphamide to render neutropenia (defined as <100 polymorphonuclear leukocytes/mm 3). Each mouse was dosed with 150 mg/kg of cyclophosphamide 4 days prior to infection and 100 mg/kg 1 day before infection. Disseminated candidiasis was induced via tail vein injection of 100 tL of inoculum. AmB, AmBAU, or AmBMU were reconstituted with 1.0 mL of 5% dextrose. Each animal in the treatment group was given a single 200 pL intraperitoneal (ip) injection of reconstituted AmB, AmBAU, or AmBMU 2 hours post-infection. Doses were calculated in terms of mg of compound/kg of body weight. At each time point (6, 12, and 24 hours post-infection), three animals per experimental condition were sacrificed by CO 2 asphyxiation. The kidneys from each animal were removed and homogenized. The homogenate was diluted serially 10-fold with 9% saline and plated on SDA. The plates were then incubated for 24 hours at 35'C and inspected for CFU viable counts. The lower limit of detection for this technique is 100 CFU/mL. All results are expressed as the mean logio CFU per kidney for three animals. In Vivo Murine Toxicity Study All studies were approved by the Animal Research Committee of the William S. Middleton Memorial VA Hospital (Madison, WI). Uninfected Swiss ICR mice were used for assessment of infusion toxicity. Groups of five mice were treated with single intravenous doses of AmB, AmBAU, AmBMU (reconstituted with 1.0 mL of 5% dextrose), or sterile pyrogen-free 0.85% NaCl administered via the lateral tail vein over 30 seconds. Dose levels studies included 0.5, 1, 2, 4, 8, 16, 32, and 64 mg/kg. Following administration mice were observed continuously for one hour and then every 6 hours up 115 to 24 hours for signs of distress or death. Resistance Studies Minimum Inhibitory Concentration and Growth Assays Susceptibility of wild-type and resistant strains to AmB, AmBAU, AmBMU, tertbutyl peroxide (Sigma-Aldrich), geldanamycin and radicicol (A.G. Scientific) was determined in flat bottom, 96-well microtiter plates (Costar) using a broth microdilution protocol adapted from CLSI M27-A3. Overnight cultures (14-20hr) were grown at 30'C in YPD, and approximately 5x10 3 cells were seeded per well. For AmB, AmBAU, and AmBMU, MIC assays were performed at 37'C in RPMI buffered with MOPS (0.165M) with 10% fetal bovine serum (Sigma-Aldrich) added; for tert-butyl peroxide, geldanamycin, and radicicol, MIC's were determined in YPD at 30'C. MIC's were determined after 24h incubation as the concentration of compound resulting in no visible growth in wells. For quantitative display of growth at drug dilutions, OD 60 0 was measured in a spectrophotometer (Tecan) and displayed as heat maps using Java TreeView 1.1.3 (http://jtreeview.sourceforge.net). Media and Growth Conditions C. albicanswas generally grown and maintained as described previously". Stocks were stored in 15% glycerol at -80*C; strains were generally grown in YPD media at 30'C. Drugs were added directly to media from DMSO stocks. 116 In Vitro Gradual Selection of AmB, AmBAU, or AmBMU Resistance Selection of resistance to AmB, AmBAU, and AmBMU was performed as follows. 1 mL overnight (14-20hr) cultures of SC5314 (WT) were washed in PBS, then treated with 3% EMS (Ethyl Methanesulfonate, Sigma-Aldrich) for 45 min. Cells were then washed 4x in YPD and resuspended in YPD and allowed to recover for 3h. Cells were then inoculated to an OD600 of approximately 0.025-0.05 in 10OmL YPD containing 0.25ptM AmB or AmB-AU, or 0.375pM AmB-MU. After 24-72 hours, a lmL aliquot was removed from any culture that had grown to saturation and subjected to another round of mutagenesis in the same manner as described above. After recovery, cells were then inoculated into a new YPD flask containing 2x higher concentration of the same drug. Cultures that grew were subjected to one more round of EMS mutagenesis before inoculating into a 2-fold higher drug concentration (total of 3 rounds of EMS mutagenesis) and then passaged at 2-fold higher increments of drug concentration until reaching 2pM AmB or AmB-AU, or 3gM AmB-MU. Cultures were passaged once more at 2pM AmB or AmBAU or 3pM AmBMU, then plated onto YPD media and frozen in glycerol stocks before further evaluation. Filamentation Assay Hyphal induction was performed by growing C. albicansovernight at 30'C in YPD, washing in PBS, and diluting 1:100 into RPMI+10% fetal bovine serum (SigmaAldrich) at 37'C in a culture tube on a rotating wheel. After 3h, cultures were washed in PBS and resuspended in 250gg/mL Calcofluor white in a microcentrifuge tube, and shaken at 30'C for 10 min. Cells were then washed twice in PBS, concentrated 10-fold, 117 briefly sonicated in a water bath, and mounted on slides for visualization under a DAPI filter set at 60X magnification. Murine Model of Systemic Infection All animal protocols were performed in accordance with the Guide for the Care and Use of Laboratory Animals of the National Institutes of Health. Animals were maintained according to the guidelines of the MIT Committee on Animal Care (CAC). These studies were approved by the MIT CAC (protocol #0312-024-15). We used 7-12week-old female Balb/c mice ordered from Taconic farms for all mouse virulence studies. All strains were prepared for inoculation by diluting overnight cultures (14-20h) 1:100 into YPD and growing into log phase for 4-5 hours, then washing 3x in PBS before. Strains were injected into the lateral tail vein in a volume of 100 pl. For mouse survival experiments, strains were grouped as follows: The wild-type Mutagenized pool consisted of 5 SC5314 colonies subjected in parallel to mutagenesis and passaging (as described above) without drug exposure, injected as of 1.6x10^5 cfu per strain (8x10^5 cfu total inoculum per mouse); the Wild-type low inoculum was the SC5314 parental strain injected at 1.6x10A5 cfu. AmB-Resistant, AmBAU-Resistant, and AmBMU- resistant pools were comprised of strains isolated from each selection in the presence of the indicated drug, using strains that exhibited >4-fold MIC increase for the drug used. Individual resistant strains were present in the pools at 1.6x1 0 A5 cfu per mouse (8x 1 0 A5 total inoculum per mouse when pooled). Each strain or pool of strains was tested in at least two independent experiments, and data were pooled. Mice were weighed daily and monitored for signs of morbidity and sacrificed when body weight decreased by 20%, or 118 when signs of extreme distress were apparent. For the competitive infection with quantification of kidney burden, a pool comprised of 16 strains at equal fraction of the population, one SC5314 wild-type and 5 strains each from selections for resistance to AmB, AmBAU, and AmBMU was used, with 3x1OA4 cells of each strain inoculated per mouse (4.8x10A5 total inoculum). Three mice were used per experiment, in a total of two experiments. 4d after infection, mice were sacrificed and kidneys were removed aseptically, homogenized, and plated onto YPD plates. Pools of the inoculum immediately before injection were also plated. 184 colonies were randomly selected from the pre-infection and 184 from the post-infection plates and tested for growth in 96-well plates in the presence of 1 pM AmBAU or 1.5 gM AmBMU, and the fraction of wells from the pre and post-infection pools exhibiting growth in either drug was determined. Whole Genome Sequencing, Alignment, Mapping, and Variant Calling . Whole genome sequencing and analysis was performed as previously described 5 References 1. 2. 3. 4. 5. 6. 7. Li, J. et al. Colistin: the re-emerging antibiotic for multidrug-resistant Gramnegative bacterial infections. Lancet Infect. Dis. 6, 589-601, (2006). Cortes, J. E. et al. A Phase 2 Trial of Ponatinib in Philadelphia ChromosomePositive Leukemias. New. Engl. J. Med 369, 1783-1796, (2013). Ellis, D. Amphotericin B: spectrum and resistance. JournalofAntimicrobial Chemotherapy 49, 7-10, (2002). Brown, G. D. et al. Hidden Killers: Human Fungal Infections. Science TranslationalMedicine 4, 165rv1 13, (2012). Volmer, A. A., Szpilman, A. M. & Carreira, E. M. Synthesis and biological evaluation of amphotericin B derivatives. Nat. Prod. Rep. 27, 1329-1349, (2010). L. N. Ermishkin, Kasumov, K. M. & Potzeluyev, V. M. Single ionic channels induced in lipid bilayers by polyene antibiotics amphotericin B and nystatine. Nature 262, 698-699, (1976). Gray, K. C. et al. Amphotericin primarily kills yeast by simply binding ergosterol. Proc. Natl. Acad. Sci. USA 109, 2234-2239, (2012). 119 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. 18. 19. 20. 21. 22. 23. 24. Anderson, T. M. et al. Amphotericin forms an extramembranous and fungicidal sterol sponge. Nat. Chem. Biol. 10, 400-406, (2014). Wilcock. B. C.. Endo. M. M.. Uno. B. E. & Burke, M. D. C2'-OH of Amphotericin B Plays an Important Role in Binding the Primary Sterol of Human Cells but Not Yeast Cells. J Am. Chem. Soc. 135, 8488-8491, (2013). Zhang, Y.-Q. et al. Requirement for Ergosterol in V-ATPase Function Underlies Antifungal Activity of Azole Drugs. PLoS Pathog6, e1000939, (2010). Heese-Peck, A. et al. Multiple Functions of Sterols in Yeast Endocytosis. Molecular Biology of the Cell 13, 2664-2680, (2002). Kato, M. & Wickner, W. Ergosterol is required for the Sec 1 8/ATP-dependent priming step of homotypic vacuole fusion. The EMBO Journal20, 403 5-4040, (2001). Klose, C. et al. Yeast Lipids Can Phase-separate into Micrometer-scale Membrane Domains. J. Biol. Chem. 285, 30224-30232, (2010). Jin, H., McCaffery, J. M. & Grote, E. Ergosterol promotes pheromone signaling and plasma membrane fusion in mating yeast. The Journalof Cell Biology 180, 813-826, (2008). Vincent, B. M., Lancaster, A. K., Scherz-Shouval, R., Whitesell, L. & Lindquist, S. Fitness Trade-offs Restrict the Evolution of Resistance to Amphotericin B. PLoS Biology 11, e1001692, (2013). Palacios, D. S., Dailey, I., Siebert, D. M., Wilcock, B. C. & Burke, M. D. Synthesis-enabled functional group deletions reveal key underpinnings of amphotericin B ion channel and antifungal activities. Proc. Natl. Acad Sci. USA 108, 6733-6738, (2011). Jarzembska, K. N. et al. Controlled Crystallization, Structure, and Molecular Properties of Lodoacetylamphotericin B. Cryst. Growth Des. 12, 2336-2345, (2012). Changeux, J. P. & Edelstein, S. J. Allosteric receptors after 30 years. Neuron 21, 959-980, (1998). Koike, K. et al. Multiple membrane-associated tryptophan residues contribute to the transport activity and substrate specificity of the human multidrug resistance protein, MRP1. J. Biol. Chem. 277, 49495-49503, (2002). Knight, Z. A. & Shokat, K. M. Features of selective kinase inhibitors. Chemistry & Biology 12, 621-637, (2005). Neant-Fery, M. et al. Molecular basis for the thiol sensitivity of insulin-degrading enzyme. Proc. Natl. Acad Sci. USA 105, 9582-9587, (2008). Duggan, K. C. et al. (R)-Profens are substrate-selective inhibitors of endocannabinoid oxygenation by COX-2. Nat. Chem. Biol. 7, 803-809, (2011). Maeda, H., Suzuki, M., Sugano, H. & Matsumoto, K. A Facile Synthesis of (S)Isoserine from (S)-Malic Acid. Synthesis 5, 401-402, (1988). Palacios, D. S., Anderson, T. M. & Burke, M. D. A Post-PKS Oxidation of the Amphotericin B Skeleton Predicted to be Critical for Channel Formation Is Not Required for Potent Antifungal Activity. J. Am. Chem. Soc. 129, 13804-13805, (2007). 120 Bonner, D. P., Mechlinski, W. & Schaffner, C. P. Polyene Macrolide Derivatives .3. Biological Properties of Polyene Macrolide Ester Salts. J. Antibiot. 25, 261262, (1972). Keim, G. R., Poutsiaka, J. W., Kirpan, J. & Keysser, C. H. Amphotericin B Methyl Ester Hydrochloride and Amphotericin B: Comparative Acute Toxicity. Science 179, 584-585, (1973). Tevyashova, A. N. et al. Structure-Antifungal Activity Relationships of Polyene Antibiotics of the Amphotericin B Group. Antimicrob. Agents Chemother. 57, 3815-3822, (2013). Paquet, V., Volmer, A. A. & Carreira, E. M. Synthesis and in vitro biological properties of novel cationic derivatives of amphotericin B. Chem. Eur. J. 14, 2465-2481, (2008). Pfaller, M. et al. Epidemiology and outcomes of candidemia in 3648 patients: data from the Prospective Antifungal Therapy (PATH Alliance@) registry, 20042008. Diagn. Micr. Infec. Dis. 74, 323-331, (2012). Ellis, J. K. et al. Metabolic response to low-level toxicant exposure in a novel renal tubule epithelial cell system. Mol. Biosyst. 7, 247-257, (2011). Zager, R. A. Polyene antibiotics: Relative degrees of in vitro cytotoxicity and potential effects on tubule phospholipid and ceramide content. Am. J. Kidney Dis. 36, 238-249, (2000). Andes, D., Stamsted, T. & Conklin, R. Pharmacodynamics of Amphotericin B in a Neutropenic-Mouse Disseminated-Candidiasis Model. Antimicrob. Agents Chemother. 45, 922-926, (2001). Pfaller, M. A. Antifungal Drug Resistance: Mechanisms, Epidemiology, and Consequences for Treatment. The American JournalofMedicine 125, S3-S 13, (2012). Sanglard, D., Ischer, F., Parkinson, T., Falconer, D. & Bille, J. Candida albicans Mutations in the Ergosterol Biosynthetic Pathway and Resistance to Several Antifungal Agents. Antimicrob. Agents Chemother. 47, 2404-2412, (2003). Pfaller, M. A. et al. Wild-Type MIC Distributions and Epidemiological Cutoff Values for Amphotericin B, Flucytosine, and Itraconazole and Candida spp. as Determined by CLSI Broth Microdilution. J. Clin. Microbiol. 50, 2040-2046, (2012). Pinto, J. P., Machado, R., Xavier, J. G. & Futschik, M. E. Targeting molecular networks for drug research. Frontiersin Genetics 5, (2014). Tudhope, S. R. et al. Development of a Large-Scale Synthetic Route to Manufacture (-)-Huperzine A. OrganicProcessResearch & Development 16, 635-642, (2012). Yue, T.-Y. et al. Stereoselective Process for a CCR3 Antagonist. OrganicProcess Research & Development 10, 262-271, (2006). Grongsaard, P. et al. Convergent, Kilogram Scale Synthesis of an Akt Kinase Inhibitor. Organic ProcessResearch & Development 16, 1069-1081, (2012). Dailey, I. Synthesis and Function of the ConservedMotif ofMycosamineContainingPolyene Macrolides Ph. D. thesis, University of Illinois at UrbanaChampaign, (2012). % 25. 26. 27. 28. 29. 30. 31. 32. 33. 34 35. 36. 37. 38. 39. 40. 121 41. 42. 43. 44. 45. 46. 47. 48. 49. 50. 51. Kotler-Brajtburg, J. et al. Classification of Polyene Antibiotics According to Chemical Structure and Biological Effects. Antimicrob. Agents Chemother. 15, 716-722, (1979). Moonis, M., Ahmad, I. & Bachhawat, B. K. Liposomal Hamycin in the control of experimental Aspergillosis in mice - relative toxicity, therapeutic efficacy and tissue distribution of free and liposomal Hamycin. Indian Journalof Biochemistry & Biophysics 29, 339-345, (1992). Hasper, H. E. et al. An Alternative Bactericidal Mechanism of Action for Lantibiotic Peptides That Target Lipid II. Science 313, 1636-1637, (2006). Schneider, T. et al. Plectasin, a Fungal Defensin, Targets the Bacterial Cell Wall Precursor Lipid II. Science 328, 1168-1172, (2010). Laganowsky, A. et al. Membrane proteins bind lipids selectively to modulate their structure and function. Nature 510, 172-175, (2014). Han, X., Yang, K. & Gross, R. W. Multi-dimensional mass spectrometry-based shotgun lipidomics and novel strategies for lipidomic analyses. Mass Spectrom. Rev. 31, 134-178, (2012). Pangborn, A. B., Giardello, M. A., Grubbs, R. H., Rosen, R. K. & Timmers, F. J. Safe and Convenient Procedure for Solvent Purification. Organometallics15, 1518-1520, (1996). Clinical and Laboratory Standards Institute (CLSI). Reference method for broth dilution antifungal susceptibility testing of yeasts; approved standard, 3rd ed. CLSI document M27-A3. Clinical and Laboratory Standards Institute, Wayne, PA. (2008). Sebaugh, J. L. Guidelines for accurate EC50/IC50 estimation. Pharm. Stat. 10, 128-134, (2011). Andes, D. & van Ogtrop, M. Characterization and Quantitation of the Pharmacodynamics of Fluconazole in a Neutropenic Murine Disseminated Candidiasis Infection Model. Antimicrob. Agents Chemother. 43, 2116-2120, (1999). Andes, D. & van Ogtrop, M. In Vivo Characterization of the Pharmacodynamics of Flucytosine in a Neutropenic Murine Disseminated Candidiasis Model. Antimicrob. Agents Chemother. 44, 938-942, (2000). 122 Acknowledgements Portions of this work were supported by the National Institutes of Health (R01GM080436, R01GM080436-S), Howard Hughes Medical Institute (HHMI), and The Mathers Foundation. M.D.B is an HHMI Early Career Scientist and S.L. is an HHMI Investigator. Author Contributions S.A.D., B.M.V., L.W., D.R.A., S.L., and M.D.B. conceived the study and designed the experiments. S.A.D., B.M.V., M.M.E., and K.M. performed the experiments. S.A.D., B.M.V., S.L., and M.D.B. wrote the manuscript. Author Information www.nature.com/reprints. Reprints and permissions Correspondence information and requests is available at for materials should be addressed to M.D.B. (mdburkegillinois.edu) or S.L. (lindquist@wi.mit.edu). Competing Financial Interest The University of Illinois has filed patents on amphotericin ureas. 123 a OH / 13 OH OH "Me e 'cIntramolecular OH OH 0,,, 0 1 Me, Me 41 C0 2 putative j R salt bridge NH 3 2' 0 R= OH amphotericin B (AmB) H C2'deoxy AmB (C2deOAmB) HO HH N .OH ergosterol Me,. Me mycosamine 131A Me d OH O- O,, _ H cholesterol OH N>2 OH OHOH O, ,OH 0 N.Me NN' H H 1. FmocONSuccinimide 0 O AmBMU OH '~--Me OH NH 2 OH 264 mg 64% average yield per step 2. CSA, MeOH 3. DPPA, Et3N; H2NCH 2CH 2 NH2 ; HCO 2H, H 20 OH OH OH 0,.N o- OH ,OH ~O N H H -- Me OH NH2 AmBAU OH 236 mg 61% average yield per step _NH2 H OHNH OH 1. FmocONSuccinimide 2. CSA, MeOH 3. DPPA, Et3N; P-Alanine Allylester; HCO 2 H, H 20 4. Thlosallcyllc Acid, Pd(PPh3 )4 ig OH N' R H N 3 AmB 1. FmocONSuccinlm 2. CSA, MeOH 3. DPPA, Et3N; H2NMe; HCO 2H, H 20 .1OH 0, H20OH NH 2R H AH H', H 20 \5ONHFmoc I OH 2 OH Me Me OMe MSOH ,OH _,,H H HO OMe Me Me Me r, H me / polyene Me , / // .,OH HO: M HO b HO 0 Me,, OH OH 0,, ,OH OO 0 N H 0 N H OH OOH AmBCU NH 2 Kr 124 mgOH 58% average yield per step Figure 1: Synthesis of AmB urea derivatives a. Chemical structures of AmB and C2'deOAmB. b. Chemical structures of ergosterol and cholesterol c. X-ray crystal structure of N-iodoacylAmB showing an intramolecular water bridged hydrogen bond between the C2' and C-13 hydroxyl groups. d. General scheme for synthesis of AmB ureas. e. Synthesis of AmBMU, AmBAU and AmBCU from AmB in only 3 or 4 steps. 124 a b Ergosterol Bindng -10 I -20 -30 -40 .50' -60 i * I m--a -U- AnBAU -- AMBCU * NS L- entry * ergceterol-containing LUVs AmBMU AmdeB 7 NS jh, 10 OH R AmDCU C4~AnB AMe AmM NS NS mycosamine 0.5 8.55 2.20 -\H >500 >500 mycosamine 025 30.67 5.38 mycosamlne 0.5 22.03 t 6.26 mycosamine 0.25 15.32 * 3.39 0.25 48.5 8.7 mycosamie 0.5 >500 NH2 nycosamine 0.25 >500 10H~ mycosamine OH 2 AmdeB A AmBAU R' OH 1 OMe 0 M AMBMEA -20 0 sterol-f roe LUVs E cholest eroI-containing LUVs -25 CAmBA 4e0 -30 C 3 MTC (pM) MIC (Ig/rnL) C. C. sic&')s gwwata 700 KI1 AmB AmBMU AmBAU AmBCU MHC (pM) MIC (PM) S. creWsiae red blood cells . - OH OR' -I- (Ipcd) 0 .' 0 o sterol-fee LUVs AmB HO OH O' OH OH Me Cholesterol Binding 5.- H - 0 2hI (Wcal) AmBMU AmdeB AmB H M,, 0 - 10 0.25 0.5 0.5 0.5 0.06 0.25 0.25 1 C. C. NET trcPcis pf Psloia hRTE TE 22019 5810 0.06 1 1 2 0.06 0.25 0.25 1 ~W Rimar TE 6.4 t 1.3 2.4 t 0.3 44.4 t 2.1 >80 37.6 4.8 11.3 0.4 >80 >80 HH N Me AmBMU .. ...-'.. NNH 2 H 2N 0 mBAU H H Aan!CU - -1 ~ H4 3 323.8 30.2 O Figure 2: Sterol binding, antifungal, and human cell toxicity of AmB ureas a. Total net isotherms from ITC showing AmB or derivatives binding to ergosterol (top) or SD. *, cholesterol (bottom). Values represent the mean of at least three experiments (MIC) concentration inhibitory Minimum b. significant. not p:0.05, **, p<0.001; NS, 90% causing (MHC) against S. cerevisiae and minimum hemolytic concentration hemolysis against human red blood cells. c. MIC against clinically relevant yeast pathogens (C. albicans, C. glabrata, C. tropicalis, C. parapsilosis) and minimum toxic concentration (MTC) causing 90% toxicity against human hTERT 1 renal proximal tubule epithelial cells (RPTEC) and human primary RPTECs. 125 C b a I mgfkg I) L 16 ntkg 4 mrg +Contmi 7.0- -- 6.5- +AmBMU 6.0- -- AmBAU AmB 5.55.04.5. 4.03.5 I -1--------------U ~ 12 18 6 24 0 Tism (houn) d U 12 Thm (houM) 18 24 0 6 12 Tis (hours) 18 24 Drug Lettialy by Does 100 so- i6 a -e- AmB so- -J a- AmBAU - C + 40- AmBMU 20- u~w l'6 32 4 64 Dose (mg") Figure 3: Efficacy and toxicity of AmB ureas in mice. Quantification of the fungal burden in the kidneys of C. albicansinfected neutropenic mice 2, 6, 12 and 24 hours after a single IP injection of AmB, AmBMU or AmBAU at dosages of a. 1 mg/kg b. 4 mg/kg or c. 16 mg/kg. P-values are relative to AmB at each indicated time point, *, p<.05, **, p<0.001, ***, p<0.0001, d. Dose response toxicity assessed via determination of lethality upon single IV injection of AmB, AmBMU and AmBAU to healthy mice at doses of ranging from 0.5 to 64 mg/kg (5 mice per dosage). Mice were monitored for survival up to one day. 126 a AmBAU AmBMU AmB 0.00 WT 0.17 - erg2A erg3AA 0.33 erg4AA 0.50 0.67 ewg5&A/ rg6IA 0.83 1.00 *rg3/11hA erg24WA U N 0U N 0I N 0I 0 0 00 0in aI 0 In0 0 0 0 0 ,(m NN N 0; CN 4 (M C3 NNN3o b Peroxide Sensitivity C WT 4 3 AmB-R#10 1 1e 1 1 AmBMU-R#7 0 12 8 4 dAMBMU MIC (pM) AmBAU-R#1 16 Geldanamycin Sensitivity 9 I AmBAU-R#3 AmBAU-R#7 30 20 0 0 0 AmBAU-R#10 Competitive Fitness CL C 16 1A00m - AmBMU and AmBAU Resistant 0.8 12 Mbuse Overall Survival: Pooled Infection g AmBMU and AmBAU Sensitive 1.0 8 AmBMU MIC (IM) ERG2 e 4 - 75- - - 0.6 - 50 AmB-Resistant pool AmBMU-Resistant pool AmBAU-Resistant pool WT-Low Inoculum WT-Mutagenized Pool 0 0.4 CL 25- 0.20* 0.0Injected Pool In Kidney after 4d 0 2 127 4 8 6 Time (days) 10 12 14 Fig 4: Characterization of mechanisms and costs of resistance to AmB ureas. a. Activity of AmB, AmBMU and AmBAU against C. albicans ergosterol biosynthesis mutants. Growth (as judged by ODonn at 24 h) is shown relative to WT with no compound added. Scale bar indicates relative growth ranging from bright green (equal to WT growth, 1.00) to black (zero growth, 0.00). b. Complete genome sequencing of parental wild-type (SC5314) and mutants selected for resistance to AmB, AmBMU or AmBAU. ERG2 ORF is shown; color coded mutations represent blue=C, red=T, brown=G, green=A in the mutant strain. c,d. MIC of tert-butyl peroxide and geldanamycin compared to AmBMU for all resistant isolates selected; each point indicates one or more isolates. e. Filamentation in response to serum at 37'C. Representative images of wildtype and mutants selected in AmB, AmBMU or AmBAU, (all cross-resistant), stained with Calcofluor White. Scale bar = 10 Em f. Competitive infection of mice with 16 different strains (1 WT and 15 that are resistanct to AmBMU and AmBAU). 3x10 4 cells of each strain injected per mouse (4.8x 105 total inoculum). Fraction of pool sensitive or resistant to AmBMU and AmBAU determined before tail-vein injection and 4d later after isolation from kidneys. g. Mouse overall survival after tail-vein injection. Mice were injected with a pool of 5 passaged and mutagenized WT strains each at 1.6x10 5 (8x10 5 total inoculum), 1.6x10 5 cells of parental WT (WT-Low), or pools of 5 resistant mutants with 1.6x1 05 cells of each mutant. 128 Chapter Four: A Fungal-Selective Cytochrome be 1 Inhibitor Impairs Virulence and Prevents the Evolution of Drug Resistance *This chapter is currently in preparation for submission 129 A Fungal-Selective Cytochrome bcl Inhibitor Impairs Virulence and Prevents the Evolution of Drug Resistance Benjamin M. Vincent, Jean-Baptiste Langlois, Raja Srinivas, Alex K. Lancaster, Ruth Scherz-Shouval, Luke Whitesell, Bruce Tidor, Stephen L. Buchwald, Susan Lindquist Affiliations 1 Microbiology Graduate Program, Massachusetts Institute of Technology, 77 Massachusetts Avenue, Cambridge, Massachusetts, 02139, United States of America, 2 Whitehead Institute for Biomedical Research, 9 Cambridge Center, Cambridge, Massachusetts, 02142, United States of America, 3 Department of Chemistry, Massachusetts Institute of Technology, Cambridge, Massachusetts 02139, United States 4 Howard Hughes Medical Institute, Department of Biology, Massachusetts Institute of Technology, Cambridge, Massachusetts, 02139, United States of America ABSTRACT To cause disease, a pathogen must adapt to the challenges of its host environment. The leading fungal pathogen Candidaalbicans readily colonizes nutrient-poor bodily niches, withstands attack from the immune system, and can tolerate treatment with azole antifungals, often evolving resistance. To discover agents that block these adaptive strategies, we screened 300,000 compounds for inhibition of azole tolerance in a drugresistant Candida isolate. We identified a novel indazole-based compound that converts azoles from fungistatic to fungicidal drugs by selective inhibition of mitochondrial ) cytochrome bcl. We synthesized >100 derivatives to optimize potency (to 0.4 pM IC 50 and fungal selectivity (>25-fold over human). In addition to reducing azole resistance, targeting cytochrome be 1 prevented C. albicans from adapting to the nutrient-deprived macrophage phagosome, and greatly curtailed its virulence in mice. Inhibiting mitochondrial respiration and restricting metabolic flexibility with this synthetically tractable chemotype provides an attractive therapeutic strategy to limit both fungal virulence and drug resistance. 130 INTRODUCTION Many pathogens have evolved to optimally exploit very particular niches within the host. But rigid specialization comes with several costs. Specialist pathogens struggle to adapt to the dramatic differences in nutrient composition, immunological surveillance, and drug exposure that characterize different host niches. Because of this, hyper- specialized pathogens fail to disseminate and colonize new niches, which limits their reproductive fitness. Furthermore, when perturbations of host physiology cause dramatic changes in local environmental conditions, pathogen populations that cannot adapt go extinct. In such circumstances, the adaptive plasticity of generalist pathogens provides strong evolutionary benefits. Candida albicans provides a paradigm for the study of a flexible and resilient pathogen. It is the most common cause of fungal infection in humans worldwide. In healthy humans, C. albicans thrives as a harmless commensal of the oral cavity and gastrointestinal tract [1]. Immunocompetent patients can suffer from recurrent infections (e.g. diaper rash and vaginal infections), but they typically resolve quickly. Mild to moderate immunosuppression often leads to more significant C. albicansinfections of the oropharynx, esophagus, and other superficial sites. In severely immunocompromised patients, Candida and other fungal pathogens can invade the bloodstream and internal organs, causing sepsis, multi-organ system failure, and death in up to 40% of patients [2]. Invasive fungal infections are now responsible for over 1.5 million deaths per year worldwide [3]. The incidence of such infections is increasing due to climate change and the expansion of human populations into new environments, which exposes them to 131 new pathogenic fungi [4]. Exacerbating the problem, the increasing use of immunosuppressive therapies and the rapidly rising rate of diabetes and other immunosuppressive systemic illnesses renders human populations ever more susceptible to fungal infection. Compounding the problem yet further, the relatively recent evolutionary divergence of humans from fungi (relative to their divergence from bacteria) reduces the number of targets available for selective therapeutic intervention. Indeed, only three classes of antifungal drug are broadly used in the clinic-and none is ideal [5]. Azoles are the most widely used antifungals in the clinic due to their safety and good oral bioavailability. They block fungal growth by disrupting ergosterol biosynthesis (through inhibition of the Erg 11, lanosterol 14-alpha demethylase enzyme) [6]. Other synthetic compounds with single-agent, broad-spectrum antifungal activity have not been approved for systemic or mucosal infections, despite extensive efforts to discover and develop them [5]. Though safe and highly effective in certain settings, azoles do have several drawbacks. First, their activity is fungistatic, not fungicidal, against Candida and most other fungal pathogens. This limited activity allows pathogens to persist, creating ideal conditions for the emergence of resistant strains. Indeed, azole resistance is increasing in prevalence, and is typically driven by pump-mediated drug efflux or by mutations in ERG 1, the drug target [7]. A second major liability of azoles is their inability to clear most types of disseminated fungal infection in patients with limited immune function. These patients require intravenous treatment with either polyenes or echinocandins, large natural product-derived molecules with fungicidal activity. However, these agents are limited by poor therapeutic index (in the case of the main polyene, amphotericin B) or limited brain 132 penetration and species spectrum (in the case of echinocandins). Even with optimal treatment, the mortality rate from invasive fungal infections remains extremely high (4090% depending on the species) [3]. Clearly, new therapeutic strategies are sorely needed. In the treatment of bacterial infections, combination therapy has proven highly effective and slowed the emergence of resistance. This has not been possible with the agents approved for the treatment of fungal infection, due to in large part to antagonistic antimicrobial activites. Given the safety and efficacy of azoles, agents that render them fungicidal (in combination) and limit the emergence of resistance would have tremendous clinical utility. Promising targets for such intervention include two signal transduction proteins that enable survival of azole-induced membrane stress, calcineurin and protein kinase c (PKC) [8-10]. These metastable proteins require high levels of the molecular chaperone Hsp90 for function [11,12]. Inhibition of Hsp90, calcineurin, or PKC all render azole treatment fungicidal and dramatically reduce the emergence of resistant strains. However, the human homologs of these highly conserved proteins play critical roles in host stress tolerance and immune responses, necessitating fungal-selectivity if they are to be used in the context of an active infection. Selectivity has been difficult to realize. Other potential strategies for reducing azole resistance [13] have not been pursued in drug development or successful in the clinic. Here we took another approach: unbiased high-throughput phenotypic screening for agents that bestow fungicidal activity upon azoles. Out of more than 300,000 compounds screened, we discovered a novel, fungal-selective inhibitor of cytochrome bcl (complex III) of the electron transport chain that had particularly promising properties. Exploring the effect of inhibiting cytochrome bcl revealed a critical role for 133 mitochondrial respiration in fungal virulence. The chemical tractability of the indazole scaffold allowed us to improve its potency, fungal selectivity, and stability. Our findings suggest that the selective targeting of fungal respiration represents a promising approach for restricting the emergence of drug resistance and sensitizing fungi to attack by the immune system. RESULTS Identification of novel small molecules that reverse fluconazole resistance in C. albicans To find new agents that might be useful in antifungal combination therapy, we screened for compounds that are fungicidal in combination with fluconazole and prevent the emergence of fluconazole resistance. We employed a previously reported isolate of C. albicans(referred to as CaCi-2) that had evolved resistance to fluconazole during the treatment of an HIV-infected patient [11,14]. We screened this isolate at 8 pg/ml fluconazole, which slows, but does not stop, its growth (Figure IA). Of 302,509 compounds screened, 1654 compounds (0.5%) inhibited growth >75% in combination with fluconazole (Figure IB). Hits were filtered for potency (IC50 < 1 pLM), lack of toxicity to mouse 3T3 fibroblasts (IC50 > 26pM), and lack of single-agent activity without fluconazole (IC50 > 26pM). Next we filtered the screen hits for compounds with activity against a clinical isolate that had emerged later in the treatment of the same patient and had higher levels of resistance (CaCi-8; [14]). We then eliminated chemically reactive compounds, compounds with metal-chelating motifs, and promiscuous compounds that hit multiple 134 other assays run using the same chemical library. 30 candidates were advanced and retested from dry powders, and 3 were chosen for structure-activity relationship studies. Detailed information on the primary screen is freely available at the PubChem database (Pubchem AID 2007). An indazole derivative (Inz-266) was chosen for target identification and further development due to its chemical tractability. Inz-266 Blocks Mitochondrial Respiration by Targeting Cytochrome bcl To better understand the effects of Inz-266 on fungal cells, we generated a profile of compound-induced phenotypes under a variety of growth conditions and in the presence of various stressors. These conditions included high salt, oxidative stress, nutrient deprivation, and exposure to diverse toxic agents. We then compared the profile of phenotypes induced by Inz-266 to that of other small molecules that sensitize C. albicans to azoles, including inhibitors of Hsp90, Calcineurin, PKC, histone deacetylases, PKA, and ARF cycling [8,10,13]. Inz-266 produced a unique phenotypic profile (Figure IC). Most intriguingly, Inz-266 potently inhibited growth of both C. albicans and the model yeast S. cerevisiae in media containing glycerol as the sole carbon source, while only mildly slowing growth in glucose (Figure 1 D). While fungi can ferment glucose and other sugars, utilizing glycerol as the sole carbon source requires cellular respiration. This result suggested that Inz-266 might interfere with mitochondrial function. As a way to identify the target of Inz-266, we exploited its potent, single-agent inhibition of respiratory growth to select resistant mutants for whole-genome sequencing. A wild-type S. cerevisiae strain (BY4741) was plated on media containing glycerol as carbon source and 1 OpM Inz-266. After 7 days of incubation, two colonies with robust 135 growth were isolated. The resistance of these isolates was confirmed and their genomes were sequenced together with that of the parental BY4741 strain. Alignment of mutant and parental genomes followed by polymorphism discovery (Materials and Methods) revealed that both resistant mutants contained an identical mutation in the cytochrome b (COB) gene of the mitochondrial chromosome (Figure 2A). This mutation replaced phenylalanine 90 with tyrosine (F90Y) in the mitochondrial cytochrome B protein, which is the core enzymatic subunit of cytochrome bc 1 (Complex III) of the election transport chain. Cytochrome bc 1 is an 11-protein complex embedded in the mitochondrial inner membrane that couples the oxidation of ubiquinol to the reduction of cytochrome C [15]. Cytochrome B, which bears the mutation that conferred resistance to Inz-266, forms the core catalytic component of the bel complex. The enzymatic activity of the complex is to convert ubiquinol and oxidized ferricytochrome C into ubiquinone and reduced ferricytochrome c, which simultaneously transporting two protons into the mitochondrial intermembrane space. This enzymatic activity is critical to oxidative phosphorylation in two ways. First, it establishes and maintains the proton gradient along the mitochondrial inner membrane, thus enabling ATP synthase activity through chemiosmotic coupling. Second, by producing a reduced form of cytochrome C, it enables complex IV (cytochrome C oxidase) to utilize molecular oxygen as the terminal electron acceptor in mitochondrial respiration. Taken together with the specific inhibition of respiratory growth by Inz-266, the resistance conferred by the cytB F90Y mutation suggested that cytochrome bc 1 might be the direct target of Inz-266. 136 Inz-266 Inhibits Cytochrome bcl Activity in Isolated Yeast Mitochondria To determine if Inz-266 inhibits cytochrome bc 1, we used a well-established in vitro assay of its enzymatic activity using purified yeast mitochondria, permeabilized with Triton X- 100 [16]. This assay exploits a spectral shift in cytochrome C upon its reduction by cytochrome bcl and ubiquinol. Indeed, Inz-266 exhibited dose-dependent inhibition of cytochrome bcl from both S. cerevisiae and C. albicans IC50's of 2.5 and 8.0 ptM, respectively (Figure 2B-E). To provide yet stronger proof that cytochrome B is the relevant target of Inz-266, we performed the same assay with mitochondria purified from the indazole-resistant cytochrome b F90Y mutant and asked if the enzymatic activity was resistant to Inz-266. Indeed, a four-fold higher concentration of Inz-266 was required to achieve 50% inhibition of the F90Y mutant enzyme than for WT (Figure 2B). This 4-fold increased resistance to Inz-266 in the enzymatic activity of the F90Y mutant mitochondria closely parallels the 4-fold increased resistance to growth inhibition by Inz266 in this mutant (Figure 2C). To confirm that loss of cytochrome B function confers azole sensitivity in C. albicans, we used genetic tools to disable the complex. Methods to selectively mutate the mitochondrial genome in C. albicans are unavailable. Instead, we deleted a nuclearencoded gene, RIP], which encodes a conserved member of the complex that is required for cytochrome bc 1 function [17]. We knocked out both copies of the RIP] gene in the CaCi-2 background, and reconstituted the gene to control for potentially extraneous effects of the deletion. riplA/A mutants from both backgrounds were indeed hypersensitive to azole treatment, mimicking the effects of Inz-266 (Figure 2D). 137 Inz-266 is selective for yeast over human cytochrome bcl The cytochrome bel complex is highly conserved from fungi to humans. To determine the relative fungal selectivity of Inz-266, we tested it on mitochondria purified from HEK293 human embryonic kidney cells. Inz-266 inhibited human cytochrome bcl activity with an IC50 of 45 pM, 8.3-fold higher than the IC50 for the fungal homolog (Figure 2E). We then interrogated the toxicity of Inz-266 to respiring mammalian cells. In tissue culture, most mammalian cell lines do not require mitochondrial respiration for proliferation. To force respiration, we cultured cell lines in media containing galactose instead of glucose [18]. We used a luminescent assay of cellular ATP content as a stringent test for inhibition of mitochondrial respiration (the dominant source of ATP production in these conditions) in HepG2 hepatocellular carcinoma cells and NIH-3T3 mouse fibroblasts. Inz-266 inhibited proliferation in these cell lines under forced respiration conditions only at 32 pM (the solubility limit), and only mildly at that (Figure 2F). These results suggested that the inhibition of respiration by Inz-266 is at least moderately selective for fungal over human cells. Mutational and Structural Analysis Suggests Inz-266 Binds the Cytochrome B Qo Site Cytochrome b is a large protein with multiple deep binding pockets. To investigate regions critical for Inz-266 activity, we isolated additional Inz-266-resistant mutants and sequenced their mitochondrial cytochrome B genes. From these selections, we identified P270L and L275S mutations to confer resistance to Inz-266 (Figure 3A). Along with F90Y, P270L and L275S map to a small region of the previously solved 138 crystal structure of the protein, known as the Quinol-oxidizing (Qo) pocket (Figure 3B-C, Hunte et al, 2000). This site is the target of the antimalarial drug atovaquone, which, unlike Inz-266, is a ubiquinol substrate analog (Trumpower et al, 2000). An alignment of the structures of the Qo site from the yeast and mammalian (bovine) homologs revealed several key differences that could be exploited for selective inhibition (Figure 3C). Most prominently, L275 in the fungal enzyme is replaced in the mammalian enzyme with a bulkier phenylalanine residue, which protrudes into of the central cavity of the Qo site. To determine if this residue is involved in the fungal selectivity of Inz-266, we tested a previously-described yeast L275F mutant [19]. This mutation conferred ~4-fold resistance to Inz-266. We also noted that the previously described G143A mutant conferred strong resistance to Inz-266 (Figure 3A). We conclude that the Qo pocket is the site for Inz-266 binding. Moreover, differential interactions with fungal L275 and human F275 residues in this site are at least partially responsible for the fungal selectivity observed (Figure 3A). To better define the binding mode of Inz-266, we used computational docking of the compound onto the structure of cytochrome b. Inz-266 was docked into a 16A grid surrounding the Qo site, using a previously solved structure of the cytochrome bc 1 complex (PDB: 1EZV). After sampling possible conformations of Inz-266 and their position within the active site, a lowest energy structure was computed (Figure 3D). Notably, in this conformation, Inz-266 made close contacts with Gly143, Pro270, and Leu275, all of which confer resistance to the compound upon mutation (Figure 3C). Taken together, these data very strongly suggest that the Qo pocket is the binding site for Inz-266. While this site is the known target of several agricultural fungicides, 139 none have been pursued for the treatment of human fungal infections due to their lack of selectivity for fungi, poor pharmacological properties. or inactivity against relevant human pathogens [20]. The low molecular weight and chemical tractability of Inz-266, combined with its potency and fungal selectivity, made it an attractive lead for further development through medicinal chemistry efforts. Optimization of Inz-266 Through Medicinal Chemistry To improve the potency and selectivity of Inz-266, we synthesized and tested a total of 125 analogs (Selected compounds described in Figure 4). We noted that substitution of the phenyl group of Inz-266 with fluorine and trifluoromethyl groups conferred 37-fold enhanced potency against the fungal enzyme, but only 9-fold enhanced potency against the human enzyme (JBL-202, JBL-22, and JBL-84, Figure 4). Substituting a methyl group or fluorine atom at the 7 position of the indazole ring also improved potency 5-fold (JBL-94). Combining these modifications produced JBL-140, which demonstrated good potency and selectivity (IC50 0.026 jiM, 40-fold fungal selective). Unfortunately, all of these compounds contain a highly labile ester group, which is susceptible to hydrolysis in the presence of serum esterases. However, we determined that a more stable methyl-tetrazole (JBL- 114) or pyrazine (JBL-218) moiety at this position retained moderate antifungal activity. Combining this substitution with JBL- 140 yielded JBL-182, which displayed strong antifungal activity (IC50 0.38 gM vs CaCi-2 with fluconazole), and almost 30-fold fungal selectivity (IC50 10.59 JIM vs respiring HepG2 cells). While the fungal selectivity of JBL-182 may require further optimization, 140 we note that the clinically useful antimalarial drug atovaquone (which targets cytochrome bcI) was to ic to respiring HepG2 cells with an IC50 of 12.2 pM, a concentration that it typically achieves in patients [21]. This indicates that partial inhibition of the Qo site of cytochrome bcl can be tolerated in humans. Inhibition of Cytochrome bel Prevents the Emergence of Fluconazole Resistance and Renders Fluconazole Fungicidal This potent, selective, and more stable compound provides a valuable tool that allowed us to investigate the role of mitochondrial respiration in diverse aspects of fungal pathogenesis. We first interrogated the effect of cytochrome B inhibition on the emergence of resistance to fluconazole. We plated C. albicans on media containing fluconazole, JBL-182, or both drugs (Figure 5A). Resistant colonies emerged at a high rate (-0. 1 %) on the plates containing fluconazole alone. Plates containing JBL- 182 alone exhibited reduced colony size, but no reduction in the total number of colonies. However, the combination of JBL- 182 with fluconazole completely abrogated the emergence of resistant colonies (Figure 5A). Up to this point, it was unclear whether JBL- 182 merely enhances the fungistatic activity of fluconazole, or if the combination renders cells inviable. To distinguish between these possibilities, we treated liquid cultures of C. albicanswith fluconazole, JBL- 182, or both compounds, and measured viable colony forming units recoverable from the culture over time. As expected, fluconazole alone slowed growth of the wildtype strain but did not cause a decrease in viability (Figure 5B). JBL-1 82 also partially 141 slowed growth alone. Importantly, combination of fluconazole with JBL-182 reduced the number of viable cells by 97%. The fungicidal effect of fluconazole was even stronger against the riplA/A mutant (Figure 5B). Thus, JBL-182 both prevents the emergence of new resistance to fluconazole and transforms fluconazole from a fungistatic compound to a fungicidal one. Inhibiting Cytochrome B with JBL-182 Restricts Carbon Source Utilization Having established the effects of JBL- 182 in combination with fluconazole, we explored the consequences of cytochrome bc 1 inhibition alone on the physiology and virulence of C. albicans. A key function of mitochondrial respiration across eukaryotes is to support ATP production and biomass expansion in the absence of sugars. In the laboratory, fungal pathogens are typically studied in high glucose conditions (2%), in which ATP can be readily produced from glycolytic fermentation without respiration. However, in host environments, sugars are much scarcer. In the bloodstream, readily fermentable sugars are present at 0.1-0.2%, and in other niches they are present at lower concentrations or completely absent [22]. Candidathus relies on utilization of suboptimal carbon sources, including lactate, acetate, fatty acids, and amino acids [23]. Might JBL- 182 restrict the metabolic flexibility of C. albicans by preventing utilization of these carbon sources? Under conditions of high glucose (and thus fermentation), JBL- 182 caused very little growth inhibition in a disc diffusion on agar plates (Figure 6A). In plates containing only fetal bovine serum as the source of nutrients (-0. 1-0.2% glucose), JBL- 182 caused slight growth inhibition. And in media containing the non-optimal sugar galactose, 142 which is abundant in the GI tract [24], JBL- 182 also caused moderate growth inhibition. But when non-fermentable carbon sources were tested, the iiihibitory effect of JBL-182 was dramatically stronger. On media containing amino acids, lactate, or acetate as the carbon source, JBL- 182 exhibited potent and profound growth inhibition (Figure 6A, bottom panel). Inhibition of Cytochrome bcl Sensitizes C. albicans to Macrophages Perhaps the most severe nutrient limitation that C. albicansencounters is upon engulfment into the macrophage phagosome [25]. Upon phagocytosis, C. albicans induces the glyoxylate cycle of 2-carbon metabolism and induces a morphogenetic program of filamentation, to enable escape. To determine if inhibition of fungal cytochrome B might impair this process, we co-cultured C. albicans engineered to express blue fluorescent protein (BFP) with mouse bone-marrow-derived macrophages, with or without JBL- 182. As expected, the macrophages phagocytosed the fungi within 30 minutes, with or without the compound (Figure 6B). The fungi showed filamentous growth and escaped the macrophages within 2 hours in the absence of JBL- 182. In contrast, with JBL- 182 C. albicans remained trapped in the phagosome (Figure 6B-C). Similar effects were observed when macrophages were infected with the rip]A/A mutant, confirming that loss of cytochrome B function is responsible for this phenotype (Figure 6B-C). We also asked if JBL- 182 would sensitize C. albicansto growth inhibition by macrophages. In a 14 hour co-culture, untreated wild-type C. albicans evaded macrophage attack and grew robustly (Figure 6D). Inhibition of cytochrome bc 1 by JBL- 143 182 (or deletion of RIP 1) sharply curtailed fungal growth in the presence of macrophages. These results suggest that inhibition of cytochrome bc 1 strongly synergizes with macrophages in blocking the growth of C. albicans. Cytochrome bcl Is Required for Fungal Virulence and Drug Resistance in Mice Given the effects of cytochrome bc 1 inhibition on properties key to fungal pathogenesis, we asked if its function is required for fungal virulence in a whole animal model. Pilot experiments determined that JBL- 182 will require further optimization of pharmacological parameters for to achieve sufficient target engagement for use in mice. As a surrogate for the effects of the compound, we examined our riplA/A mutant generated in the CaCi-2 fluconazole-resistant background. In the absence of drug treatment, CaCi-2 (and the riplA/A:RIP1 re-integrant strain) killed mice within several days, as expected (Figure 7A). In stark contrast, the rip]A/A mutant did not cause severe disease in the mice for over two weeks. However, after 17-20 days, mice infected with the rip]A/A strain exhibited agitated behavior and a head-tilt, suggestive of a possible central nervous system (CNS) infection, and were promptly euthanized. Indeed, the brains of these mice carried high fungal burden (data not shown). To quantitatively test if cytochrome bc 1 compromise increased colonization of the CNS in mice, we infected animals with a low inoculum of WT, rip]A/A, and the RIPl reconstituted strain. We allowed this infection to proceed for four days, then sacrificed the completely asymptomatic mice and quantified fungal 144 burden in the brain and kidney. While the rip]A/A mutant was almost completely defective in kidney colonization, it exhibited approximately 5-fold higher fungal burden in the brain than the wild-type or re-integrant strain (Figure 7B). Thus, while the riplA/A mutant does not kill mice through the typical means of kidney colonization, this mutant has an increased capacity to colonize the brain, where it can cause lethality. This might limit the utility of targeting cytochrome be 1 as monotherapy. Treatment with azoles is generally insufficient to cure disseminated candidiasis, as their fungistatic activity is insufficient to fully eradicate the fungus. We tested whether the fungicidal effects of disabling cytochrome bc 1 in the presence of azoles would enable a lasting cure of the infection. We infected mice with a high inoculum of fungus and treated them for 3 days with a standard dose of fluconazole that controls but does not eradicate the infection. We then stopped treatment and monitored for recurrence of the infection over the next four weeks. In mice infected with CaCi-2, severe infection recurred within 1-2 weeks of stopping treatment. Only 10% of these mice survived (Figure 7C). In mice infected with the riplA/A mutant, 90% survived, with only one mouse succumbing to neurological symptoms after more than 3 weeks. Given the increase in brain colonization in mice infected with strains lacking cytochrome function, we tested if this concern was eliminated by fluconazole treatment. We infected mice with a low inoculum of CaCi-2 or rip]A/A, allowed infection to proceed for four days, treated for 3 days with fluconazole, and then waited four more days before sacrificing mice. Quantification of fungal burden in both the brain and kidney established that fluconazole treatment eliminated brain colonization in these mice (Figure 7D). Thus, even if cells lacking cytochrome bc 1 function were to succeed in 145 colonizing the brain, they should remain highly susceptible to fluconazole. Thus, these two antifungal strategies strongly potentiate each other. JBL-182 Inhibits Fungal Pathogens Separated by Over a Billion Years of Evolution While we have focused on C. albicans, many other fungal pathogens that cause life-threatening invasive infections respond poorly to azoles and other available agents [3]. The Qo binding site for JBL- 182 is strictly conserved across these evolutionarily distant species, including the critical L275 residue, which dictates the fungal selectivity of this scaffold (Figure 8A). To determine if JBL-182 might have efficacy against a broad range of other fungal pathogens, we tested its effects on Scedosporium prolificans, Aspgerillus terreus, and Rhizopus oryzae. As a single agent, JBL-182 exhibited promising growth inhibition of all three fungi. When grown on media requiring respration, this activity was markedly enhanced (Figure 8B). Notably, these species are also closely related to agricultural pathogens that cause devastating crop failures. Hence, the fungal specificity afforded by the binding pocket of JBL- 182 may provide avenues for the pursuit of antifungals across diverse settings. Discussion The evolution of mechanisms that permit flexibility and resilience in the face of environmental challenges empowers many fungi to be extremely formidable pathogens. Currently, the chemical arsenal we have to combat them is severely limited, creating a dire need for new approaches. Here we demonstrate that mitochondrial respiration presents an attractive target for intervention because it is required for these adaptive 146 strategies. Surprisingly, despite its conservation from fungi to humans, our work demonstrates that it is possible to pharmacologically disable respiration across separated by a billion years of evolution without impairing respiration in human cells. We discovered and optimized a potent and fungal selective indazole-based inhibitor of cytochrome bc 1 that abrogates the ability of C. albicansto tolerate treatment with azole drugs and impairs their ability to evolve azole resistance. Disabling cytochrome bc 1 also prevents fungal adaptation to nutrient starvation, sensitizes C. albicansto macrophages, and curtails virulence in mice. Restricting the adaptive plasticity of fungal pathogens by inhibiting respiration may present a broadly useful approach to the development of sorely-needed combination therapies. Moreover, targeting cytochrome bc 1 may provide an avenue for the treatment of fungi that are refractory to treatment with azoles and other available agents. Considerable progress has been made to identify metabolic pathways that are absent in humans and might therefore present attractive therapeutic targets. One such example is the glyoxylate cycle, which enables diverse pathogens to survive carbon starvation [22,26,27]. However, given the formidable metabolic flexibility of C. albicans,the pharmacological targeting of any one metabolic pathway alone may prove insufficient as a therapeutic strategy. In support of this notion, mutants lacking a functional glyoxylate cycle exhibit only partially reduced virulence [27]. In contrast, the mitochondrial electron transport chain is a central molecular node in metabolic networks, and is required for many pathways of metabolic adaptation. It is thus unlikely that fungi can readily tolerate or bypass its inhibition and retain virulence [28]. We anticipate that mitochondria will prove essential to many other fungal virulence processes, as others too 147 have begun to reveal [29,30]. Although targeting such highly conserved proteins might initially seem unwise, there are certainly many examples of effective antimicrobials that exert their effects through proteins shared with man, such as azoles or ribosome-targeting antibiotics. Though promising, inhibiting fungal cytochrome bc 1 must overcome several challenges to be useful as a therapeutic strategy. One challenge is to design compounds that can target this hydrophobic pocket in the inner mitochondrial membrane, crossing both the plasma membrane and the outer membrane to do so, and yet retain sufficient water solubility for effective delivery. Recent advances in drug formulation may mitigate this concern [31]. In addition, a higher degree of fungal selectivity than we have achieved to date (40-fold) might be necessary to guarantee safety in patients. The successful use of the cytochrome bc I inhibitor atovaquone in antimalarial therapy suggests that such challenges can be overcome. Moreover, recent advances in the crystallization of fungal cytochrome bc I could aid in the structure-based design of agents with improved potency and selectivity [32]. The increased brain colonization of C. albicans with disabled cytochrome B (the rip]A/A mutant) could also present a challenge. However, the clinical relevance of this phenomenon is unclear [33], and combination therapy with azoles, which eliminate this colonization, would appear to greatly mitigate this concern. Another challenge will be to determine if mitochondrial inhibitors can be effective against Candidaglabrata, in which loss of mitochondrial respiration appears to increase azole resistance through induction of drug efflux pumps [34]. But even if targeting of mitochondrial respiration is ineffective 148 against C. glabrata, it may be effective in the treatment not only of C. albicans but also of diverse fungal pathogens that are refractory to treatment with current agents [3]. Most (arguably all) classes of antibiotics and antifungals of the 201h century were identified by phenotypic screening of natural product extracts and synthetic libraries, assaying simply for single-agent microbial growth inhibition (both intentionally and serendipitously). Yet, novel classes of natural product antimicrobials are increasingly hard to discover, and their development into drugs poses substantial challenges [35]. In the past two decades, efforts have swung toward target-based screening of purified proteins against synthetic chemical libraries. This approach has failed to deliver any novel classes of antifungals or antibacterials in clinical practice [6,36]. In part, this failure is due to the fact that synthetic compounds with good activity in cell-free assays fail to traverse microbial cell walls and membranes. Recent efforts have returned to phenotypic screening, using synthetic chemical libraries to search for single agents capable of inhibiting microbial growth. However, results suggest that the few chemical classes with useful activity as single agents have already been discovered [36]. As an alternative approach, we propose that unbiased phenotypic screening for growth inhibition in combination with older antimicrobials might uncover vast regions of chemical space with previously unknown therapeutic potential [37,38]. To this end, we hope that the discovery and optimization of JBL- 182 will provide a broadly applicable blueprint for similar efforts against other pathogens. Materials and Methods 149 High I hroughput Smaji Moiecule Screen Methods used in the high-throughput screen are described in depth in [39]. Fungal Growth and Strain Manipulation C. albicansand S. cerevisiae were maintained under standard conditions as described previously [28]. Assays of fungal growth were generally performed as described in [28], with the following specifications. Phenotypic profiling experiments were performed in 96-well flat-bottom plates by diluting overnight YPD cultures to a starting OD of 0.0003, then assaying growth in drug and stress conditions after 24 or 48 hours (as indicated) by reading OD600. In these experiments, drugs and concentrations included Conditions included 0.9M NaCl, 0.05 jg/mL aureobasidin, 80 piM bathophenanthroline disulfonic acid, 0.5pg/mL cerulenin, 2mM tert-butyl peroxide, 40 mg/L calcofluor white, 2 pg/mL tunicamycin, 0.1 pg/mL caspofungin, 25 gM simvastatin, and 0.008% SDS. Small molecule inhibitor odrugs were used at either 2.5 ptM (Brefeldin A), 5 ptM (Geldanamycin, FK-506, cercosporamide), 10 ptM (Trichostatin A, Inz-266), 15 pM MDL-12,330A), or 20 pM (rotenone). Synthetic media used a base of Difco YeastNitrogen-Base (YNB) with complete amino acid supplement, and addition of 2% glucose or 2% glycerol. Growth results were quantitatively displayed in heatmaps using Treeview as described in [28]. Minimal inhibitory concentration (MIC) assays were performed at 2 fold concentration increments in 96-well plates over 24-72 hours as described in figure legends. The MIC was defined as the lowest concentration that results in no visible fungal growth. 150 Alignment of Yeast and Bovine Cytochrome bcl Cytochrome bcl from Saccharomyces cerevisiae (PDB: 1P84) was aligned to cytochrome bel from Bos taurus (PDB: 1SQV), using the "align structures" feature in Pymol. Structural Docking (Raja Srinivas and Bruce Tidor) Ligands were docked into the active site using the GLIDE package (Schrodinger suite). The initial unbound ligand conformation was generated using a SMILES sequences,which was converted to a 3D structure using Ligprep (Schrodinger Suite). For docking, the native ligand, ubiquinol, was removed from the active site of the crystal structure (PDB Code: 1EZV). A grid of 16A was generated centered on the active site. To generate an improved bound conformation, we used an inverse design approach, which has been described in detail before. (Citations here-see below) In short, an ensemble of scaffold conformations is generated in the active site, with appropriate attachment points for the functional groups. The top docked conformation of Inz-266 was used to generate an initial conformation for the scaffold. We thoroughly sampled in both translation and rotation throughout the active site to generate an ensemble of possible scaffold position. We further sampled the bond between the Indazole and the benzene every degree (Bond shown in green). We rotamerized the functional group by enumerating all dihedrals every 30 degrees and employed a Dead-end Elimination/A* approach, which guarantees the global minimum energy conformation. Finally, we 151 rescored the top conformations using an energy model with increased accuracy as described before. Selection of resistant mutants and whole genome sequencing Selection of mutants resistant to Inz-266 was performed by plating 107 cells per plate on YNB-glycerol-agar plates containing Inz-266. Plates were incubated for 7 days before picking colonies and retesting their resistance in liquid media. Isolates were retested for resistance to cycloheximide to eliminate nonspecific efflux mutants. DNA extraction, whole genome sequencing and polymorphism detection was performed as described in [28]. Cytochrome B enzyme assay The cytochrome B enzyme assay was adapted from [16]. Briefly, compounds were diluted in a 2x reaction buffer containing 100mM Tris-Cl pH 7.4, 10mM sodium azide, 0.02% BSA, and 0.1% Tween-20. Mitochondria (-5 pg protein) and cytochrome C (final concentraion 50tM) were then added, and the reaction was initiated by the addition of ubiquinol (50pM), reduced from ubiquinone with dithionite. Reaction plates were incubated at room temperature for 10 minutes before reading absorbance at 550nm. IC50's were calculated in Graphpad Prism 6.0. Antimycin A (200nM) was included on every plate as a control for 100% inhibition. Mammalian Cell Respiration Toxicity Compounds were tested for toxicity to respiring mammalian cells as described in [18]. Cells were initially passaged in High-Glucose DMEM, then washed and resuspended in glucose-free DMEM with 10mM galactose and added to 96-well white tissue culture 152 plates at 10,000 cells per well. After 72 hours, ATP production was used as a surrogate for growth and assayed using Cell-titer-glo (Promega) at 1:5 dilution. Bone-Marrow Derived Macrophage Co-Culture Macrophages were isolated from GFP-tubulin Balb/c mice using standard methods [40]. After 7-9 days in culture, macrophages were added to 12-well plates containing glass cover slips at 3x10 5 cells/well, and fungi were added at an MOI of 4. Cells were fixed with 3% formalin before visualization by fluorescence microscopy. Fungal growth over 14hr in the presence of macrophages was assayed by Alamar Blue dye reduction (control experiments demonstrated very low background macrophage dye signal). Mouse infection experiments All mouse experiments were performed under MIT protocol 0312-024-15 and in accordance with NIH standard for the ethical treatment of animals. Mouse experiments were performed as described in [28] with the specific inoculum used noted in the figure legend. 7-12 week-old female Balb/C mice were used in all experiments. Fluconazole was prepared at 1 mg/mL solution in PBS and delivered intraperitoneally. Supplemental Chemical Synthesis Methods (Jean-Baptiste Langlois and Stephen Buchwald) General reagent information Commercial materials were purchased and used as received unless otherwise noted. Acetonitrile (anhydrous, 99.8%), carbon tetrachloride (anhydrous, 99.5%) and NN- 153 dimethylformamide (anhydrous, 99.8%) were purchased from Sigma-Aldrich. Acetone (ACS reagent, 99.6%) was purchased from Acros Organics. Tetrahydrofuran was purified and dried using a solvent purification system consisting of successive passage through alumina and Q5 reactant-packed columns. Deionized water was employed; this solvent was degassed by sonication under slight vacuum for 5 minutes, followed by backfilling with argon. Potassium carbonate (ACS reagent, 99.0%), tribasic potassium phosphate (reagent grade, 98%) and sodium azide (ReagentPlus®, 99.5%) were purchased from Sigma-Aldrich. Ammonium chloride (ACS reagent, 99.6%) was purchased from Acros Organics. Phosphorus (V) oxychloride (ReagentPlus@, 99%), hydrazine monohydrate (N 2H 4 64-65%, reagent grade, 98%), N-chlorosuccinimide (98%), N-bromosuccinimide (ReagentPlus@, 99%), bromoacetonitrile (97%), 2,2'-azobis(2-methylpropionitrile) (98%), 2-methylpyrazine (99%) and dimethylsulfate (99%) were purchased from SigmaAldrich. (Trimethylsilyl)diazomethane solution (2M in hexanes) was purchased from Sigma-Aldrich and kept in a fridge at -5 'C. 2-fluoro-5-(trifluoromethyl)-phenylboronic acid and 7-fluoro-1H-indazole were purchased from Combi-Blocks. 2-fluoro-3- methylbenzoic acid was purchased from Oakwood Chemicals. XPhos ligand was purchased from Strem and precatalyst P was prepared following a reported procedure.' Compounds described herein were purified by flash chromatography using Silicycle SiliaFlashP60 (230-400 mesh) silica gel. General analytical information All compounds described herein were characterized by 'H, 154 1C and ' 9F NMR (when applicable). 1H, 13 C and 19F NMR spectra were recorded on BrUker 400 MHz spectrometers. The samples were prepared in CDCl 3, and chemical shift (6) are given in parts per million (ppm) relative to the residual solvent peak (7.26 ppm for 1H and 77.16 ppm for for 13 C). 13 C). Few samples were prepared in d6 -DMSO (2.50 ppm for 'H and 39.51 ppm 19F NMR were performed with proton decoupling. Peak multiplicity is reported as: s (singlet), d (doublet), t (triplet), q (quartet), m (multiplet), dd (doublet of doublets), dt (doublet of triplets), ddd (doublet of doublets of doublets), td (triplet of doublets), br (broad), app (apparent). Coupling constants (J) are given in Hertz (Hz). Mass spectrometry analyses were performed for both chemical probes (X1 and X2). HRMS data were obtained using a direct analysis in real time (DART) ionization method on a BrUker Daltonics APEXIV 4.7 Tesla Fourier Transform Ion Cyclotron Resonance Mass Spectrometer (FT-ICR-MS). The relative purities of chemical probes X1 and X2 were determined using LC-MS analysis on an Agilent 1260 Infinity Chromatograph coupled with an Agilent 6120 Quadrupole Mass detector. The analyses were performed using an Eclipse XDB-C18 column (5 tm, 4.6x150 mm) using an isocratic mobile phase composed of 90% of acetonitrile, 9.9% of water and 0.1% of acetic acid (flow rate = 0.8 ml/min). Preparation of chemical probe X1 155 0 0 OH Me 2SO 4 , K 2CO 3 0. Acetone, r.t. Me Scheme 1. Me Preparation of methyl 2-fluoro-3-methylbenzoate 2. Methyl 2-fluoro-3-methylbenzoate 2: 2-fluoro-3-methylbenzoic acid 1 (2 g, 13 mmol, 1 eq) was charged into a 100-ml round-bottomed flask and dissolved in acetone (20 ml). Potassium carbonate (2.15 g, 15.6 mmol, 1.2 eq) was added in portions and the resulting suspension was stirred until the gas evolution ceased (10 min). Then, dimethylsulfate (1.23 ml, 13 mmol, 1 eq) was added and the reaction mixture was stirred for 1 hour at room temperature. The reaction was monitored by TLC (Hexanes/AcOEt 9/1, Rf() = 0.1, Rf(2 ) = 0.7). After complete consumption of the starting material, the reaction mixture was diluted with acetone (10 ml) and filtered on a plug of celite. The solid was rinsed twice with acetone (2x 10 ml) and the filtrate was concentrated using a rotary evaporator. The crude residue was triturated with hexanes (10 ml) and the resulting suspension was filtered on a plug of celite. The filtrate was concentrated using a rotary evaporator to yield the desired product as a pale yellow liquid (2.2 g, 99%). 'H NMR (400 MHz, CDCl 3 ): 6 7.66-7.70 (m, 1H), 7.52-7.57 (m, 1H), 7.18-7.22 (t, J= 7.7 Hz, 1H), 3.84 (s, 3H), 2.26-2.27 (d, J= 2.4 Hz, 3H). 13C NMR (125 MHz, CDCl 3): 6 164.2-164.2 (d, J= 3.2 Hz), 158.0-160.5 (d, J= 256.5 Hz), 136.1-136.2 (d, J= 5.9 Hz), 129.1, 125.9-126.1 (d, J= 17.5 Hz), 124.0-124.0 (d, J= 4.5 Hz), 117.9-118.0 (d, J= 10.9 Hz), 52.3, 14.114.1 (d, J= 4.6 Hz). 156 0 0 0/ F Me 2 N'NH2 N 2 H 4.H 20 MeOH 60 *C, 1.5 hr F H Me Scheme 2. Preparation of 2-fluoro-3-nethylbenzohydrazide 3. 2-fluoro-3-methylbenzohydrazide 3: methyl 2-fluoro-3-methylbenzoate 2 (2.2 g, 13 mmol, 1 eq) was charged into a 100-ml round-bottomed flask and dissolved in methanol (20 ml). Hydrazine monohydrate (3.15 ml, 65 mmol, 5 eq) was added and the flask was equipped with a reflux condenser. The flask was then placed in an oil bath preheated at 60 'C and the reaction mixture was refluxed for 1.5 hours. After this time, the reaction mixture was cooled to room temperature and volatiles were removed using a rotary evaporator. The crude residue was triturated in hexanes (20 ml) and the supernatant solution was removed with a pipet. The operation was repeated two times and the resulting gummy solid was dissolved in AcOEt, dried with Na2 SO 4 , filtered and concentrated using a rotary evaporator. The crude reaction mixture was dried in vacuum for 12 hours to give the desired product as a white solid (1.8 g, 83%). 'H NMR (400 MHz, d -DMSO): 6 9.48 (brs, 1H), 7.32-7.40 (m, 2H), 7.12-7.15 (t, J = 7.6 Hz, 1H), 4.51 (brs, 2H), 2.25-2.25 (d, J= 2.3 Hz, 3H). 3 1 C NMR (125 MHz, d6 -DMSO): 6 163.6, 156.2-158.7 (d, J= 248.1 Hz), 133.2-133.3 (d, J= 5.2 Hz), 127.3-127.3 (d, J= 3.2 Hz), 124.9-125.0 (d, J= 17.7 Hz), 123.9-123.9 (d, J= 4.2 Hz), 122.9-123.1 (d, J = 16.1 Hz), 14.1-14.2 (d, J= 4.2 Hz). 157 OH 0 N' NH2 H N 2H4.H20 sealed tube 140 *C, 15 hr Me 3 NN H Me Scheme 3. Preparation of 7-methyl-I H-indazol-3-ol 4. 7-methyl-1H-indazol-3-ol 4: 2-fluoro-3-methylbenzohydrazide 3 (1.5 g, 9 mmol, 1 eq) was charged into a sealed tube and suspended in hydrazine monohydrate (6 ml). The tube was sealed with a Teflon screw valve and placed in an oil bath preheated at 140 'C. The reaction mixture was placed behind a protective shield and stirred for 15 hours. After this time, the reaction mixture was cooled to room temperature and the protective shield was removed. The cooled mixture was poured into crushed ice and the mixture was stirred for 10 min. A white precipitate formed and was filtered off the suspension with a fritted funnel. The solid was washed twice with water (5 ml) and subsequently dried in vacuum for few hours to afford the desired product as a white solid (1 g, 75%). 'H NMR (400 MHz, d -DMSO): 6 10.52-11.12 (brm, 2H), 7.42-7.44 (d, J= 8.0 Hz, 1H), 7.07-7.09 (d, J = 6.9 Hz, 1H), 6.86-6.90 (dd, J = 6.9 and 8.0 Hz, 1H), 2.38 (s, 3H). '3 C NMR (125 MHz, d -DMSO): 6 156.6, 142.5, 127.0, 119.9, 118.9, 117.6, 112.3, 16.1. OH I Me NN N H Cl POC1 3 sealed tube 140 *C, 5 hr 4 N -N Me H 5 Scheme 4. P~reparation of 3-chloro-7-rnethyl- I H1-indazole 5. 158 3-chloro-7-methyl-1H-indazole 5: 7-methyl-1H-indazol-3-ol 4 (500 mg, 3.38 mmol, 1 eq) was charged into a sealed tube and suspended in phosphorus (V) oxychloride (2 ml). The tube was sealed with a Teflon screw valve, placed in an oil bath preheated at 140 'C and the reaction mixture was stirred at this temperature for 5 hours. After this time, the reaction mixture was cooled to room temperature and poured into crushed ice. The mixture was stirred for 30 min and an off-white precipitate formed. The solid was filtered off the suspension with a fritted funnel. The residual water was removed by azeotropic evaporation with toluene using a rotary evaporator. The resulting solid was dried in vacuum for few hours to afford the desired product as an off-white solid (565 mg, 99%). 'H NMR (400 MHz, CDC1 3): 6 7.47-7.49 (d, J= 8.1 Hz, 1H), 7.17-7.19 (d, J= 7.0 Hz, 1H), 7.09-7.13 (dd, J= 7.0 and 8.1 Hz, 1H), 2.53 (s, 3H). 13 C NMR (125 MHz, CDC 3 ): 6 141.6, 135.3, 128.1, 122.1, 120.7, 120.2, 117.0, 16.6. C1 Me N' H N C1 BrCH 2CN, K2CO3 DMF, 90 * 2 hr 5 N Me 6 N CN Scheme 5. Preparation of 2-(3-chloro-7-methyl-IH-indazol-1-yl)acetonitrile 6. 2-(3-chloro-7-methyl-1H-indazol-1-yl)acetonitrile 6: 3-chloro-7-methyl-1H-indazole 5 (300 mg, 1.81 mmol, 1 eq) and potassium carbonate (500 mg, 3.62 mmol, 2 eq) were charged into a test tube and suspended in DMF (5 ml). The tube was capped with a Teflon screw-cap septum. Bromoacetonitrile (0.25 ml, 3.62 mmol, 2 eq) was added via 159 syringe through the septum and the tube was placed in an oil bath preheated at 90 'C. The reaction was monitored by TLC (Hexanes/AcOEt 6/4, Rf(6 ) = 0.8). After complete consumption of the starting material (2 hours), the reaction mixture was cooled to room temperature, quenched with an aqueous solution of HCl (IM) and extracted with Et2 O. The organic layer was washed with brine, dried with Na 2 SO 4 , filtered and concentrated using a rotary evaporator. The crude residue was adsorbed onto silica gel, dried in vacuum and purified by flash chromatography (Hexanes/AcOEt 6/4, Rf(6) = 0.8) to afford the desired product as an off-white solid (350 mg, 94%). 'H NMR (400 MHz, CDC13 ): 6 7.54-7.57 (ddq, J= 0.7, 1.3 and 8.0 Hz, 1H), 7.26-7.28 (in, 1H), 7.17-7.21 (dd, J= 7.1 and 8.0 Hz, 1H), 5.43 (s, 2H), 2.79 (s, 3H). 13 C NMR (125 MHz, CDC13 ): 6 140.8, 136.5, 130.9, 123.3, 123.2, 120.3, 118.4, 114.6, 39.9, 18.6. F3 C B(OH) 2 F CI I N F CF3 P (5 mol %), K 3PO4 M CNTHF/degassed water 40 OC, 2hr CN Me 6 6 I N PCy2 i-Pr i-Pr FPd-XPhos N Me 7 7 NH 2 C CN P XPhos Scheme 6. Preparation of 2-(3-(2-fluoro-5-(trifluoromethyl)phenyl)-7-methyl-1H-indazol-1-yl)acetonitrile 2-(3-(2-fluoro-5-(trifluoromethyl)phenyl)-7-methyl-1H-indazol-1-yl)acetonitrile 7. 7: 2- (3-chloro-7-methyl-1H-indazol-1-yl)acetonitrile 6 (100 mg, 0.49 mmol, 1 eq), ), 2-fluoro5-(trifluoromethyl)-phenylboronic acid (152 mg, 0.73 mmol, 1.5 eq), tribasic potassium phosphate (212 mg, 1.0 mmol, 2 eq) and XPhos precatalyst P (18 mg, 0.025 mmol, 0.05 160 eq) were charged into a test tube, which was capped with a rubber septum. The vessel was successively evacuated and backfilled with argon. This operation was repeated three times and anhydrous THF (1 ml) was added via syringe through the septum followed by freshly degassed water (2 ml). The rubber septum was then replaced by a Teflon screwcap septum and the tube was placed in an oil bath preheated at 40 'C. After 2 hours, the reaction mixture was cooled to room temperature, quenched with water and extracted with AcOEt. The organic layer was dried with Na 2SO 4 , filtered and concentrated using a rotary evaporator. The crude residue was adsorbed onto silica gel, dried in vacuum and purified by flash chromatography (Hexanes/AcOEt 8/2, Rf(7) = 0.5) to afford the desired product as a yellow solid (147 mg, 90%). 'H NMR (400 MHz, CDC1 3 ): 6 8.06-8.08 (dd, J= 2.4 and 6.4 Hz, 1H), 7.70-7.74 (m, 1H), 7.63-7.66 (dd, J= 3.4 and 8.1 Hz, 1H), 7.347.39 (m, 1H) 7.25-7.28 (m, 1H) 7.18-7.22 (dd, J= 7.0 and 8.1 Hz, 1H), 5.58 (s, 2H), 2.86 (s, 3H). 13C NMR (125 MHz, CDC1 3 ): 6 160.6-163.1 (d, J = 255.6 Hz), 141.3, 140.5, 130.1, 128.9-129.0 (m), 127.7-127.9 (m), 127.3-127.6 (m), 124.3, 123.1, 121.2-121.4 (d, J= 16.0 Hz), 120.1, 120.0, 119.7-127.9 (q, J= 272.1 Hz), 117.1-117.3 (d, J= 23.3 Hz), 114.9, 40.1, 18.8. 9F NMR (376 MHz, CDC13 ): 6 -62.0 (s, 3F), -107.9 (s, IF). F 3C F3C F Me NH 4CI, NaN 3 F.IN N 15 hr Me 8 TMSCH 2N 2 THF, N DMF, 100 *C NN F3 C NH N:N 0 O C to r.t. 15 hr Scheme 7. Preparation of chemical probe X1. 161 N NN Me Xi N me N:N 3-(2-fluoro-5-(trifluoromethyl)phenyl)-7-methyl-1-((2-methyl-2H-tetrazol-5yl)methyl)-1H-indazole X1: 2-(3-(2-fluoro-5-(trifluoromethyl)phenyl)-7-methyl-1H- indazol-1-yl)acetonitrile 7 (100 mg, 0.3 mmol, 1 eq), ammonium chloride (32.4 mg, 0.6 mmol, 2 eq) and sodium azide (39 mg, 0.6 mmol, 2 eq) were charged into a test tube and suspended in DMF (1 ml). The tube was sealed with a Teflon screw-cap septum and placed in an oil bath preheated at 100 'C. The reaction mixture was stirred at this temperature for 15 hours. After this time, the reaction mixture was cooled to room temperature, quenched with an aqueous solution of HCl (IM) and extracted with Et2 0. The organic layer was dried with Na2 SO 4 , filtered and concentrated using a rotary evaporator to recover compound 8 as a yellow oil. The crude mixture (100 mg, 0.27 mmol, 1 eq) was charged into a test tube, which was subsequently closed with a Teflon screw-cap septum. The vessel was successively evacuated and backfilled with argon. This operation was repeated three times and anhydrous THF (2 ml) was added via syringe through the septum. The reaction mixture was cooled to 0 'C with an ice bath and a solution of (trimethylsilyl)diazomethane in hexanes (2M, 0.2 ml, 0.41 mmol, 1.5 eq) was added dropwise via syringe through the septum. Then, the ice bath was removed and the yellow reaction mixture was stirred for 15 hours. After this time, the excess (trimethylsilyl)diazomethane was quenched with few drops of tetrafluoroboric acid. When the gas evolution ceased, the reaction mixture was concentrated using a rotary evaporator. The crude residue was adsorbed onto silica gel, dried in vacuum and purified by flash chromatography (Hexanes/AcOEt 6/4, Rf(xl) = 0.7) to afford the desired product as a white solid (23 mg, 22% from 8). 'H NMR (400 MHz, CDC1 3 ): 162 8 8.06-8.08 (dd, J= 2.1 and 6.4 Hz, 1H), 7.65-7.69 (in, 1H), 7.59-7.62 (dd, J= 3.3 and 8.0 Hz, 1H), 7.30-7.35 (appt, J= 9.1 Hz, 1H), 7.18-7.20 (dt, J= 1.2 and 6.9 Hz, 1H), 7.11-7.14 (dd, J= 7.0 and 8.1 Hz, 1H), 6.14 (s, 2H), 4.28 (s, 3H), 2.83 (s, 3H). "C NMR (125 MHz, CDC1 3 ): 6 163.4, 160.6-163.2 (d, J= 256.0 Hz), 140.6, 139.9, 129.3, 129.1-129.3 (m), 127.0-127.4 (in, 2C), 123.8, 119.8-127.9 (q, J= 272.2 Hz), 122.2, 122.0-122.1 (d, J= 16.1 Hz), 120.7, 119.5-119.6 (d, J= 7.2 Hz), 116.8-117.1 (d, J= 23.5 Hz), 46.8, 39.7, 19.4. "F NMR (376 MHz, CDCl3 ): 6 -61.9 (s, 3F), -108.0 (s, IF). LC-MS: RT(x1) = 2.3 min (>98% purity). HRMS (m/z): [M+H] calculated for C 18H 15F 4N 6, 391.1289; found, 391.1277. Comment: The low isolated yield obtained after the methylation step was due to the concomitant formation of two additional regioisomers that were separated during the purification by flash chromatography. Preparation of chemical probe X2 CI N F / H N-chlorosuccinimide CH 3CN, 70 *C, 15 hr F 9 N H N 10 Scheme 8. Preparation of 3-chloro-7-fluoro-J H-indazole 10. 163 3-chloro-7-fluoro-1H-indazole 10: 7-fluoro-lH-indazole 9 (500 mg, 3.7 mmol, 1 eq) and N-chlorosuccinimide (500 mg. 3.7 mmol. 1 eq) were charged into a test tube equipped with a stir bar. Anhydrous acetonitrile (5 ml) was added and the tube was sealed with a Teflon screw-cap septum. The tube was then placed in an oil bath preheated at 70 'C and stirred for 15 hours. After complete consumption of the starting material, monitored by TLC (Hexanes/AcOEt 8/2, Rf(l) = 0.5; Rf(2 ) 0.7), the reaction mixture was cooled to room temperature and acetonitrile was removed using a rotary evaporator. The solid residue was dissolved in AcOEt and washed twice with an aqueous solution of NaOH (2M). The organic layer was dried with Na 2 SO 4 , filtered and concentrated using a rotary evaporator. The crude residue was adsorbed onto silica gel, dried in vacuum and purified by flash chromatography (Hexanes/AcOEt 8/2, Rf(2 )= 0.7) to afford the desired product as a white solid (540 mg, 85%). 'IH NMR (400 MHz, CDC1 3 ): 6 10.78 (brs, lH), 7.46-7.50 (m, 1H), 7.12-7.19 (m, 2H). 13C NMR (125 MHz, CDC1 3 ): 6 146.7-149.1 (d, J = 249.0 Hz), 136.2-136.3 (d, J= 4.0 Hz), 131.2-131.3 (d, J= 16.1 Hz), 124.2-124.3 (d, J 4.3 Hz), 122.3-122.4 (d, J= 5.3 Hz), 115.5-115.6 (d, J= 4.4 Hz), 112.2-112.4 (d, J= 15.5 Hz). '9F NMR (376 MHz, CDC 3 ): 6 -132.4 (s, IF). Comment: The isolated product was contaminated with a side-product stemming from additional chlorination in position 5 of the indazole (4% according to 19F NMR). 164 c1 -~N' (; F H N K 2 CO3 , 80 *C, Ci Br DMF 1 hr 10 N F N 12 N Scheme 9. Preparation of 3-chloro-7-fluoro- I -(pyrazin-2-ylrnethyl)- I H-indazole 12. Comment: The preparation of compound 12 requires the use of alkylation reagent 11, which is prone to decomposition in the contact of air at room temperature. To circumvent this problem, the following procedure has been devised to prepare reagent 11 as a solution in DMF that can be directly employed in the alkylation event. 3-chloro-7-fluoro-1-(pyrazin-2-ylmethyl)-1H-indazole 12: N-Bromosuccinimide (6.1 g, 34.5 mmol, 15 eq), and 2,2'-azobis(2-methylpropionitrile) (377 mg, 2.3 mmol, 1 eq) were charged into a 100-ml round-bottomed flask and suspended in carbon tetrachloride (30 ml). 2-methylpyrazine was added and the flask was equipped with a stir bar and a reflux condenser. The flask was then placed in an oil bath preheated at 80 'C and refluxed for 3 hours. After this period of time, a black precipitate formed. The clear supernatant was diluted with hexanes (20 ml), cooled to room temperature and filtered on a plug of celite. The dark solid was rinsed two times with hexanes (2x20 ml). DMF (20 ml) was added to the filtrate and low boiling solvents were removed using a rotary evaporator (hexanes and carbon tetrachloride). The resulting solution of 11 in DMF was transferred into a 1 00-ml round-bottomed flask containing potassium carbonate (3.8 g, 27.6 mmol, 12 eq) and 3chloro-7-fluoro-1H-indazole 10 (400 mg, 2.3 mmol, 1 eq). The flask was equipped with a reflux condenser and placed in the oil bath preheated at 80 'C. After 2 hours, the reaction 165 mixture was cooled to room temperature, quenched with water and extracted with Et 2 0. The organic layer was dried with Na2SO4 . filtered and concentrated using a rotary evaporator. The crude residue was adsorbed onto silica gel, dried in vacuum and purified by flash chromatography (Hexanes/AcOEt 7/3, Rf(4) = 0.4) to afford the desired product as a yellow solid (466mg, 77%). 1H NMR (400 MHz, CDC13 ): 6 8.49-8.52 (brm, 2H), 8.39 (brs, 1H), 7.44-7.49 (in, 1H), 7.08-7.16 (in, 2H), 5.82 (s, 2H). '3 C NMR (125 MHz, CDC13 ): 6 152.0, 146.9.149.4 (d, J= 248.3 Hz), 144.4, 144.2, 143.4, 135.1-135.1 (d, J= 3.0 Hz), 130.9-131.0 (d, J= 13.3 Hz), 125.5-125.5 (d, J= 4.0 Hz), 122.3-122.4 (d, J= 5.7 Hz), 116.0-116.0 (d, J 4.4 Hz), 112.8-112.9 (d, J= 16.9 Hz), 54.6-54.7 (d, J= 4.2 Hz). 'F NMR (376 MHz, CDC13 ): 6 -133.6 (s, IF). Comment: The 2,5-dichloro-7-fluoro-1H-indazole initially present in substrate 10 underwent the alkylation reaction with similar efficiency to afford a side-product that we did not manage to remove from product 12 (96% pure according to 19F NMR). B(OH) 2 F 3C F C IFN N F 12 NHPCy ,H 2 SF CF3 P (5 mol %), K PO 4 THF/degassed 3water 40 *C, 2 hr N IN NN F X2 N Nz \/ C P N Scheme 10. Preparation of chemical probe X2. 166 i-Pr i-Pr Pd-XPhos i-Pr XPhos 2 7-fluoro-3-(2-fluoro-5-(trifluoromethyl)phenyl)-1-(pyrazin-2-ylmethyl)-1H-indazole X2: 3-chloro-7-fluoro-1-(pyrazin-2-ylmethyl)-1H-indazole 12 (400 mg, 1.52 mmol, 1 eq), 2-fluoro-5-(trifluoromethyl)-phenylboronic acid (475 mg, 2.28 mmol, 1.5 eq), tribasic potassium phosphate (645 mg, 3.04 mmol, 2 eq) and XPhos precatalyst P (55 mg, 0.076 mmol, 0.05 eq) were charged into a 100-ml Schlenk tube, which was capped with a rubber septum. The vessel was successively evacuated and backfilled with argon. This operation was repeated three times and anhydrous THF (8 ml) was added via syringe through the septum followed by freshly degassed water (16 ml). The rubber septum was then replaced by a Teflon screw valve and the tube was placed in an oil bath preheated at 40 'C. After 2 hours, the reaction mixture was cooled to room temperature, quenched with water and extracted with AcOEt. The organic layer was dried with Na2 SO 4 , filtered and concentrated using a rotary evaporator. The crude residue was adsorbed onto silica gel, dried in vacuum and purified by flash chromatography (Hexanes/AcOEt 8/2, Rf(xl)= 0.4) to afford the desired product as a white solid (482 mg, 81%). 1 9F NMR analysis of the isolated product revealed the presence of the side-product carried out during all this synthetic sequence. The product was consequently further purified by preparative HPLC to yield pure compound X2 (384 mg, 65%). The purification was performed on an Agilent 1260 Infinity instrument coupled with a diode-array detector. An Agilent prepC18 column (5 pm, 212x150 mm) was employed with an isocratic mobile phase composed of 90% of acetonitrile, 9.9% of water and 0.1% of acetic acid (flow rate = 20 ml/min, RT(x2) = 3.0 min). 'H NMR (400 MHz, CDC13 ): 8 8.47-8.60 (brm, 2H), 8.348.46 (brs, 1H), 8.09-8.11 (dd, J= 2.3 and 6.6 Hz, 1H), 7.67-7.77 (m, 1H), 7.57-7.60 (ddd, J= 1.1, 3.5 and 7.8 Hz, 1H), 7.32-7.37 (ddd, J= 0.9, 8.7 and 9.6 Hz, 1H), 7.08-7.18 (m, 167 2H), 5.99 (s, 2H). "C NMR (125 MHz, CDC 3 ): 6 160.5-163.0 (d, J= 255.5 Hz), 152.4, 147 2-149 6 (d, J= 2473 Hz), 144.4 144.1, 143.3, 140.3, 130.7-130.9 (d, J= 12.8 Hz), 128.8-129.0 (m), 127.5-127.7 (m), 127.2-127.9 (qd, J= 3.2 and 32.9 Hz), 126.8-126.8 (d, J= 3.7 Hz), 122.4-122.5 (dd, J= 1.4 and 5.5 Hz), 121.4-121.5 (d, J= 15.8 Hz), 119.7127.7 (q, J= 270.1 Hz), 117.6-117.8 (dd, J= 4.4 and 8.0 Hz), 117.0-117.2 (d, J= 23.4 Hz), 111.9-112.1 (d, J = 16.9 Hz), 54.8-.54.8 (d, J = 4.4 Hz). 'F NMR (376 MHz, CDC13 ): 6 -62.0 (s, 3F), -108.1 (s, IF), -134.1 (s, IF). LC-MS: RT(x2) = 3.0 min (>99% purity). HRMS (m/z): [M+H] calculated for C19 H 12 F 5N 4 , 391.0977; found, 391.0971. References 1. Calderone R, Odds FC, Boekhout T (2009) Candida albicans: fundamental research on an opportunistic human pathogen. FEMS Yeast Res 9: 971-972. 2. Pfaller MA, Diekema DJ (2010) Epidemiology of invasive mycoses in North America. Crit Rev Microbiol 36: 1-53. 3. Brown GD, Denning DW, Gow NA, Levitz SM, Netea MG, et al. (2012) Hidden killers: human fungal infections. Sci Transl Med 4: 165rv1 13. 4. Byrnes EJ, 3rd, Li W, Lewit Y, Ma H, Voelz K, et al. (2010) Emergence and pathogenicity of highly virulent Cryptococcus gattii genotypes in the northwest United States. PLoS Pathog 6: e1000850. 5. Roemer T, Krysan DJ (2014) Antifungal drug development: challenges, unmet clinical needs, and new approaches. Cold Spring Harb Perspect Med 4. 6. Odds FC, Brown AJ, Gow NA (2003) Antifungal agents: mechanisms of action. Trends Microbiol 11: 272-279. 7. Cowen LE, Sanglard D, Howard SJ, Rogers PD, Perlin DS (2014) Mechanisms of Antifungal Drug Resistance. Cold Spring Harb Perspect Med. 8. Sanglard D, Ischer F, Marchetti 0, Entenza J, Bille J (2003) Calcineurin A of Candida albicans: involvement in antifungal tolerance, cell morphogenesis and virulence. Mol Microbiol 48: 959-976. 168 9. Cruz MC, Goldstein AL, Blankenship JR, Del Poeta M, Davis D, et al. (2002) Calcineurin is essential for survival during membrane stress in Candida albicans. EMBO J 21: 546-559. 10. LaFayette SL, Collins C, Zaas AK, Schell WA, Betancourt-Quiroz M, et al. (2010) PKC signaling regulates drug resistance of the fungal pathogen Candida albicans via circuitry comprised of Mkc 1, calcineurin, and Hsp90. PLoS Pathog 6: e1001069. 11. Cowen LE, Lindquist S (2005) Hsp90 potentiates the rapid evolution of new traits: drug resistance in diverse fungi. Science 309: 2185-2189. 12. Diezmann S, Michaut M, Shapiro RS, Bader GD, Cowen LE (2012) Mapping the Hsp90 genetic interaction network in Candida albicans reveals environmental contingency and rewired circuitry. PLoS Genet 8: e1002562. 13. Epp E, Vanier G, Harcus D, Lee AY, Jansen G, et al. (2010) Reverse genetics in Candida albicans predicts ARF cycling is essential for drug resistance and virulence. PLoS Pathog 6: e1000753. 14. White TC (1997) Increased mRNA levels of ERG16, CDR, and MDR1 correlate with increases in azole resistance in Candida albicans isolates from a patient infected with human immunodeficiency virus. Antimicrob Agents Chemother 41: 14821487. 15. Hunte C, Palsdottir H, Trumpower BL (2003) Protonmotive pathways and mechanisms in the cytochrome bcl complex. FEBS Lett 545: 39-46. 16. Gutierrez-Cirlos EB, Trumpower BL (2002) Inhibitory analogs of ubiquinol act anticooperatively on the Yeast cytochrome bcl complex. Evidence for an alternating, half-of-the-sites mechanism of ubiquinol oxidation. J Biol Chem 277: 1195-1202. 17. Beckmann JD, Ljungdahl PO, Lopez JL, Trumpower BL (1987) Isolation and characterization of the nuclear gene encoding the Rieske iron-sulfur protein (RIP1) from Saccharomyces cerevisiae. J Biol Chem 262: 8901-8909. 18. Marroquin LD, Hynes J, Dykens JA, Jamieson JD, Will Y (2007) Circumventing the Crabtree effect: replacing media glucose with galactose increases susceptibility of HepG2 cells to mitochondrial toxicants. Toxicol Sci 97: 539-547. 19. Hill P, Kessl J, Fisher N, Meshnick S, Trumpower BL, et al. (2003) Recapitulation in Saccharomyces cerevisiae of cytochrome b mutations conferring resistance to atovaquone in Pneumocystisjiroveci. Antimicrob Agents Chemother 47: 27252731. 20. Gao X, Wen X, Esser L, Quinn B, Yu L, et al. (2003) Structural basis for the quinone reduction in the bcl complex: a comparative analysis of crystal structures of mitochondrial cytochrome bc 1 with bound substrate and inhibitors at the Qi site. Biochemistry 42: 9067-9080. 21. Hughes W, Dorenbaum A, Yogev R, Beauchamp B, Xu J, et al. (1998) Phase I safety and pharmacokinetics study of micronized atovaquone in human immunodeficiency virus-infected infants and children. Pediatric AIDS Clinical Trials Group. Antimicrob Agents Chemother 42: 1315-1318. 22. Ene IV, Brunke S, Brown AJ, Hube B (2014) Metabolism in Fungal Pathogenesis. Cold Spring Harb Perspect Med. 169 23. Ramirez MA, Lorenz MC (2007) Mutations in alternative carbon utilization pathways in Candida albicans attenuate virulence and confer pleiotropic phenotypes. Eukaryot Cell 6: 280-290. 24. Brown AJ, Brown GD, Netea MG, Gow NA (2014) Metabolism impacts upon Candida immunogenicity and pathogenicity at multiple levels. Trends Microbiol. 25. Lorenz MC, Fink GR (2001) The glyoxylate cycle is required for fungal virulence. Nature 412: 83-86. 26. Lorenz MC, Fink GR (2002) Life and death in a macrophage: role of the glyoxylate cycle in virulence. Eukaryot Cell 1: 657-662. 27. Barelle CJ, Priest CL, Maccallum DM, Gow NA, Odds FC, et al. (2006) Nichespecific regulation of central metabolic pathways in a fungal pathogen. Cell Microbiol 8: 961-971. 28. Vincent BM, Lancaster AK, Scherz-Shouval R, Whitesell L, Lindquist S (2013) Fitness trade-offs restrict the evolution of resistance to amphotericin B. PLoS Biol 11: e1001692. 29. Shingu-Vazquez M, Traven A (2011) Mitochondria and fungal pathogenesis: drug tolerance, virulence, and potential for antifungal therapy. Eukaryot Cell 10: 13761383. 30. Sun N, Fonzi W, Chen H, She X, Zhang L, et al. (2013) Azole susceptibility and transcriptome profiling in Candida albicans mitochondrial electron transport chain complex I mutants. Antimicrob Agents Chemother 57: 532-542. 31. Fahr A, Liu X (2007) Drug delivery strategies for poorly water-soluble drugs. Expert Opin Drug Deliv 4: 403-416. 32. Birth D, Kao WC, Hunte C (2014) Structural analysis of atovaquone-inhibited cytochrome bc 1 complex reveals the molecular basis of antimalarial drug action. Nat Commun 5: 4029. 33. Liu Y, Mittal R, Solis NV, Prasadarao NV, Filler SG (2011) Mechanisms of Candida albicans trafficking to the brain. PLoS Pathog 7: e1002305. 34. Ferrari S, Sanguinetti M, De Bernardis F, Torelli R, Posteraro B, et al. (2011) Loss of mitochondrial functions associated with azole resistance in Candida glabrata results in enhanced virulence in mice. Antimicrob Agents Chemother 55: 18521860. 35. Roemer T, Xu D, Singh SB, Parish CA, Harris G, et al. (2011) Confronting the challenges of natural product-based antifungal discovery. Chem Biol 18: 148-164. 36. Payne DJ, Gwynn MN, Holmes DJ, Pompliano DL (2007) Drugs for bad bugs: confronting the challenges of antibacterial discovery. Nat Rev Drug Discov 6: 2940. 37. Ejim L, Farha MA, Falconer SB, Wildenhain J, Coombes BK, et al. (2011) Combinations of antibiotics and nonantibiotic drugs enhance antimicrobial efficacy. Nat Chem Biol 7: 348-350. 38. Spitzer M, Griffiths E, Blakely KM, Wildenhain J, Ejim L, et al. (2011) Cross-species discovery of syncretic drug combinations that potentiate the antifungal fluconazole. Mol Syst Biol 7: 499. 39. Youngsaye W, Hartland CL, Morgan BJ, et al. ML212: A small-molecule probe for investigating fluconazole resistance mechanisms in Candida albicans. Beilstein J Org Chem. 2013;9:1501-7. 170 40. Weischenfeldt J, Porse B. Bone Marrow-Derived Macrophages (BMM): Isolation and Applications. CSH Protoc. 2008;2008:pdb.prot5080. 171 B A~ \ Fluconazole resistant C. albicans einI F~..conaw 1654 screen hits i 1014 Non-toxic to Fibroblasts CHpk~ 622 active with IC50 < 1pM 48hr 296 Non-toxic alone, active vs Caci-8 300.000 Compounds 30 Non-Promiscous Scaffolds 3 Candidates for SAR J' 8 E .1 C S I I. -S I Inz-266 C :5 I- High NaCl Aureobasidin BPS Cerulenin Peroxide Calcofluor White Tunicamycin Caspofungin Simvastatin AA D I Inz-268 concentration (pM) A -> A A ARf IRA Glucose S. cerevislae Glycerol Glucose C. albicans Glycerol Figure 1. Discovery of Inz-266 by high-throughput screening. A) Schematic of the high throughput screen for inhibitors of azole tolerance. B) Triage of hits from the screen. C) Profiling of fungal growth in stress conditions in the presence of Inz-266 and other small molecules. D) Effect of Inz-266 on growth of S. cerevisiae and C. albicans in media containing glucose or glycerol as carbon source. 172 A Parental WT lnz-266Resistant #1 lnz-266Resistant #2 C B Growth In 8-lycerol Media Cytochrome B Enzyme Actvity 1.0- 1o -- cytocwome C RedUction +- ~-Type Relative WC-T9pe CtB F90Y Growth COS F90Y 0.1 0.I 00. -1 IN 0.4 0~In-W 0 1 logonz-2661 p .1 1a 2 [Fluconazole] pjg/mL D 0 0.12 0.25 0.5 1.0 2.0 4.0 8.0 WT WT+tnz-266 riplt/A 0-00 0.25 0-50 0.75 1-00 F E CyEoclwome B Enzyme Assay Cell Prollferatlon 0. 401.4 + 5, Human C. albcans Relatlv ATP L"vl - HepG2 - 3T3 Fibroblast 10 -w C. abicans . O.S. 0.4 lo [ .1 0 1 109 onz-2"s "e Pn&-2661 2 Figure 2. Inz-266 is a fungal-selective inhibitor of mitochondrial cytochrome bcl. A) Cytochrome B mutation in two Inz-266-resistant isolates, visualized by the Integrative Genomics Viewer (IGV). B) Inhibition of yeast cytochrome B enzymatic activity by Inz266 in both wild-type and F90Y mutant mitochondria. C) Resistance of F90Y mutant to growth inhibition by Inz-266. D) Fluconazole tolerance in C. albicansCaCi-2 WT, treated with Inz-266, or riplz/A deletion mutant. E) Comparison of inhibition of cytochrome B activity in C. albicans and human (HEK293) mitochondria. F) Comparison of the effect of Inz-266 on proliferation of HepG2 and NIH-3t3 cells under respiring conditions (DMEM-galactose) with inhibition of C. albicansin presence of 8 ptg/mL fluconazole. 173 B A P270(L/ - Qi pocket M7- Qo pocket Bovine= Brown Yeast = Green D C Nnmal Inhbitory Concentradon WT I L275F Cytochrome B P27OL Mutation LIGSOF 1147V G143A 4 i 431 -f Inz-266, pM . Figure 3. Structural analysis of Inz-266 binding to cytochrome bcl. A), Structure of yeast cytochrome bc 1 indicating location of Qi and Qo pockets. B) Structural aligment of yeast and bovine cytochrome bcl and indication of location of mutations that confer resistance to Inz-266. C) MIC of Inz-266 under respiratory growth conditions against mutants of the Qo pocket. D) Computational docking of Inz-266 onto Qo pocket of yeast cytochrome bc 174 0.005 0.007 0.016 0.020 1.25x Atovaquone 3.79 1.88 >32 12.72 <0.5x Inz-266 8.092 45.32 1.655 >32 >19.3x JBL-202 2.972 35.98 1.013 >32 >31.5x JBL-22 1.058 8.655 0.722 >32 >44.3x JBL-84 0.1448 4.622 0.305 >32 >104.9x JBL-94 1.005 21.28 0.398 >32 >80.3x JBL-140 0.026 1.044 0.080 >32 >398.4x JBL-218 5.423 83.81 25.87 >32 >1.2x 22.63 109 4.987 >32 >2.4x JBL-36 0.141 10.78 0.758 12.98 17.1x JBL-182 0.289 6.507 0.381 10.59 27.7x Antimycin A JBL-114 N"- C Figure 4. Optimization of Inz-266 through medicinal chemistry. Compounds were synthesized and tested as described in materials and methods. 175 A DMSO Fluconazole DMSO JBL-182 B Time Kill Analysis Fluconazole +I- JBL-182 Proliferation (CFU/mL) 1071 + Wild-type 10 + ip1A/A + Wild-Type + JBL-1 82 Wild-Type + FCZ riplA/A+FCZ + Wild-Type+ FCZ + JBL-182 1o 10 10 -Ing 0 24 Time (Hours) 48 Figure 5. JBL-182 renders fluconazole cidal and reduces the emergence of resistance. A) 106 C. albicans wild-type (SC5314) cells were plated on media containing 64 mg/L fluconazole, IOpm JBL-182, or a both compounds in combination. Photos were taken after 4d incubation. B) 5x10 3 C. albicans SC5314 cells were incubated in the presence of 32 mg/L fluconazole, 10 [tM JBL-182, or both compounds, and C. albicans rip1iz/ were incubated in the presence and absence of 32 mg/L fluconazole. Dilutions were plated on YPD after 24 and 48 hr. 176 A 2% Glucose Amino acids Galactose Serum Lactate Acetate B Wild Type + DMSO Wild Type +INZ-182 npN 30' 120 C D Fungal Survival In Co-culture Filawentatlon In Macrophages Percent PerentPercent (1201 wrf Hyphalof 225 DMSO Inz-182 tiplAiA DMSO Inz-182 riplIA Figure 6. Inhibition of cytochrome bcl by JBL-182 prevents adaptation to suboptimal carbon sources. A) Growth of_10 4 C. albicans SC5314 cells on agar plates containing various carbon sources in the presence of a filter disc containing DMSO or 10pg JBL- 182. B) Co-culture of BFP-labeled C. albicans and GFP-tubulin-labeled mouse bone-marrow-derived macrophages. C) Quantification of effects observed in (B) D) Fungal survival quantified by alamar blue dye reduction after 14 hr co-culture at MOI of 0.125 in the presence of bone marrow macrophages. 177 Mouse Tall Vein Infection A CaCi-2 CaCi-2 rplA/A --CaCi-2 niplA/A + RIP1 Percent survival Is* 2S. A A5 I* S 0 2S Days Kidney and Brain Colonization No Drug Treatment B Total Recovered CaCi-2 CaCi-2 riplA/L CaCi-2 rip1A/A + RIPI 2.0o10 CFU 2.00101 *90 0 0 2.01021 _:. 2.0010 el 13 flulifts LnWoIDOeoon (20CR)) Brain Kidneys Recurrence of Fluconazole-Resistant infection C - CaCi-2 - CaCi-2 rip 1/A - CaCi-2 riplA/A 1-09 Percent survival + RIPI 2 0cilL5 24 mngazg Fluconazote D Days Kidney and Brain Colonization After Fluconazole Treatment Total 2.03,101 * CaCi-2 CFU Recovered CaCi-2 riplA/A 2.001 2.0a1 2.031 Brain Kidneys (20 CFUJ1 Figure 7. Loss of cytochrome bcl severely reduces fungal virulence and fluconazole tolerance, but increases brain colonization. A) Tail-vein infection of Balb/C mice with 5x105 fungal cells of indicated strains. N = 7 mice per strain. B) Viable fungal burden isolated from brain 4d after infection with 6x104 cfu of indicated strains. N = 6-7 mice per strain. C) Survival of mice infected with 106 cfu of CaCi-2 then treated for 3d with 24 mg/kg fluconazole. N = 6-10 mice per strain. D) Mice were infected with 6x104 cfu of the indicated strains, treated for 3d with 24 mg/kg fluconazole, monitored for 4 more days, then sacrificed and fungal burden in kidney and brain was quantified. 178 A PASIVPEWYLLPFYAILRSIPDKLLGVIT PPSIVPEWYLLPFYAILRSIPDKLGGVIA PPAIVPEWYLLPFYAILRSIPNKLLGVIA PASIVPEWYLLPFYAILRSIPDKLGGVIA PPSIVPEWYLLPFYTILRSIPNKLLGVVG PPHIKPEWYFLFAYTILRSVPNKLGGVLA Saccharomyces cerevisiae Candida albicans Aspergillus fumigatus Rhizopus oryzae Cryptococcus neoformans Homo Sapiens B 294 266 RPMI, 0.2% Glucose YNB, 2% Glucose YNB, 2% Glvcerol Rhizopus oryzae Aspergillus terreus Scedosporium prolificans Figure 8. Broad-spectrum activity of JBL-182. A) Alignment of a contiguous segment of Qo site of cytochrome bel from indicated species. Mutations conferring resistance to indazoles are indicated in bold; residues conserved in all of these fungi but not humans are indicated in red. B) Activity of JBL-182 against indicated species. ATCC reference strain of each species was grown on potato-dextrose-agar plates, then 4 resuspended in water with 0.1% Tween, counted, and 10 cells were plated on indicated media with filter discs containing DMSO or I Ogg JBL-182 and incubated at 35*C. Images were taken after 24 hr (Rhizopus) or 48 hr (Aspergillusand Scedosporium). 179 Chapter Five: Conclusions and Future Directions 180 AMPHOTERICIN B AND THE CONSTRAINTS OF EVOLUTION In this thesis, I investigated the mechanisms that promote and restrict the evolution of resistance to antifungal drugs in the clinic. My work establishes that mutations that confer resistance to AmB impose a strict requirement for high levels of Hsp90 function, sensitize Candidato stresses encountered in the host environment, and disarm the virulence factors of this pathogen. I suggest it is the sum of these effects that has prevented the emergence of resistance to AmB in the clinic. These specific mechanisms further our understanding of the role of stress responses in the rapid evolution of new traits. They also might inform the design of novel resistance-refractory antimicrobial agents. Here I discuss the broader implications of my main conclusions as well as future directions to extend this work. Expanding the role of Hsp90 and stress responses in the evolution of new traits Hsp90 is a highly abundant chaperone whose activity governs the folding and function of diverse metastable proteins, especially those involved in signal transduction (including kinases, steroid hormone receptors, and ubiquitin ligases) [1]. Importantly, its activity is intimately linked to environmental conditions. Although Hsp90 is normally produced far in excess of cellular demands, stressful conditions can overburden Hsp90's folding capacity. This protein folding burden modulates the output of the pathways in which Hsp90 client proteins function. These properties position Hsp90 to have powerful effects on the emergence of new traits. At least five different ways in which Hsp90 can affect rapid evolutionary change have been described. First, Hsp90 directly binds and stabilizes novel mutated proteins 181 that might otherwise misfold and be degraded, enabling them to have immediate phenotypic consequences [2,3]. Second, Hsp90 buffers pre-existing genetic variation, keeping it cryptic until it is released by the broad effects of stress on the proteome [4-6]. Third Hsp90 can regulate epigenetic factors [7]. Fourth, overburdening of Hsp90 can release transposons [8]. Fifth, Hsp90 enables the evolution of drug resistance by supporting stress responses that mitigate drug toxicity [9]. Our studies on the emergence of resistance to AmB now provide evidence for a sixth mechanism by which Hsp90 mediates evolutionary change: empowering cells to respond to, and withstand, the stressful consequences of disruptive new mutations. The ergosterol biosynthesis mutations that enable AmB resistance severely perturb membrane physiology by altering the structure of a key lipid that regulates fluidity, permeability, and transmembrane protein functions. As such, the survival of AmB-resistant mutants becomes strictly dependent on the capacity of Hsp90 to mature certain stress response proteins, including calcineurin. This mechanism is distinct from previous studies of Hsp90's role in azole and echinocandin resistance. For azole and echinocandin resistance, the mutations resistance mutations are not the source of stress; instead stress comes as a direct effect of toxicity induced by the drug. Our findings indicate that Hsp90 may have an even broader role in in evolutionary processes: allowing cells to tolerate the drastic and disruptive physiological changes inherent in novel traits. 182 Extending the evolutionary breadth of the AmB resistance-virulence tradeoff One major question that was not addressed in our work is how broad the tradeoff between resistance to AmB and virulence is across evolutionarily diverse species. Our work focused primarily on C. albicans for several reasons. First, C. albicans has been the most common fungal pathogen in hospitals for many decades, and certainly has been given broad enough exposure to AmB for resistance to evolve. Second, ample evidence is available from large surveillance studies of this species to establish that clinical resistance to AmB is extremely rare [10]. Third, as this species is genetically tractable, we were able to demonstrate with genetically matched strains that every mutation known to confer strong resistance completely abrogates virulence in mice. With this foundation, it is now important to determine how broadly our findings extend to fungal pathogens other than C. albicans. One of the main mechanisms underlying the avirulence of AmB-resistant C. albicansis the loss of filamentation in resistant mutants. However, many pathogenic fungi are not filamentous, but grow as yeasts. Are these pathogens more likely to evolve resistance to AmB? Isolates of the evolutionarily distant non-filamentous fungus Candidaglabratawith ergosterol biosynthesis mutations have been described in a handful of cases [11]. It is not known if these mutants are merely bystanders that survived amphotericin resistance, or in fact retain virulence. However, given the haploid nature of C. glabrata,if loss of function mutations in ERG2 or ERG6 did not carry major fitness costs, nearly every population would be expected to rapidly evolve resistance to AmB. Another non-filamentous species of interest is the extremely distant yeast Cryptococcus neoformans. Amphotericin B resistance has been reported in isolates from 183 several HIV patients with cryptococcosis, but resistance still remains exceedingly rare [12,131. Thus, it appears likely that even in non-filamentous fungi, the modifications of ergosterol biosynthesis that confer AmB resistance carry severe selective disadvantages. These defects may include the deficiencies in stress tolerance and host adaptation that we demonstrated for C. albicans. Although AmB has at least moderate inhibitory activity against virtually every fungus, some species are intrinsically more resistant than others. Aspergillus terreus is generally considered to be insusceptible to AmB (but is killed by high concentrations of the drug). Previous work has suggested that both heightened oxidative stress responses and limited drug accessibility to the plasma membrane could contribute to the intrinsic AmB resistance of A. terreus [14,15]. Further study is warranted to elucidate how this fungus eludes killing by AmB, especially in light of the new "sterol sponge" model of AmB action [16]. Deepening our understanding of the tradeoff between resistance and virulence Returning to C. albicans, another interesting avenue of research will be to exploit the availability of genetic tools and mouse models of infection to further probe the fitness costs of resistance to AmB in vivo. One intriguing possibility is that AmB-resistant mutants lose systemic virulence but retain the potential to colonize specific host niches. Many of the strains tested in antimicrobial susceptibility surveillance studies come from cases of thrush. Given the low rate of AmB resistance in these studies, AmB-resistant fungi appear unlikely to cause disease in the oropharynx. However, it is possible that AmB-resistant strains could persist as commensals of the gastrointestinal tract or other 184 niches, depending on their selective disadvantage compared to AmB-sensitive strains. It is tempting to speculate that resistance to AmB merely shuts down the capacity of this fungus for virulence, but not for other forms of host colonization. As such, the selective pressure to evolve AmB resistance would remain low, since it would only prove beneficial during the treatment of a terminally ill patient (and lead to death of the host, for that matter). If this is true, the resilience of AmB????may be attributed to the tendency of the drug to select for an avirulent population, indirectly achieving the desired goal of approaches that seek to directly inhibit virulence factors [17]. It may also be interesting to determine if there are mechanisms that bypass the virulence defects of amphotericin-resistant C. albicans. Recent work has described several fluconazole-resistant erg3 mutants that retain fully wild-type filamentous growth and virulence, unlike previous isolates lacking erg3 that exhibited moderate fitness defects [18]. This result demonstrates that it is possible for cells to buffer the fitness costs of certain ergosterol mutations. However, the fitness costs of AmB-resistant erg2, erg6, and erg3/erg] mutants were much more severe than those observed for fluconazole-resistant erg3 mutants in the strains we constructed. One approach to determining the potential of new mechanisms to buffer these mutations would be to passage an amphotericin-resistant deletion mutant through several rounds of infection in a mouse. If such passaging selected for mutants that increased its fitness and virulence, it would be possible to sequence the genome of the resulting strains and identify the mutations responsible for buffering the parental phenotype. 185 Lessons from AmB for the Design of Resistance-Refractory Therapeutics The ability to design drugs that are inherently refractory to resistance would have extraordinary value in the treatment of many types of infections. Our work points to one such novel design strategy. Specifically, searching for compounds for which resistance can evolve only via mechanisms that bear substantial fitness costs. Predicting apriori whether a specific compound or drug target will evade resistance is extremely difficult. To shed light on new ideas for the design of resistance-refractory agents, it is important to first put our findings with amphotericin in the context of other antimicrobial drugs, in particular antibacterial agents, for which resistance currently presents an enormous societal challenge. Admittedly, comparisons of resistance rates and mechanisms between antibacterial and antifungal agents are difficult to make. Bacterial drug resistance often involves the rapid and efficient horizontal transfer of resistance mechanisms, while antifungal drug resistance spreads much more slowly, and must often evolve de novo. Nevertheless, it is useful to first examine how AmB compares with different antibacterials with regards to the mechanisms and costs of resistance. As most antibacterials are natural products, mechanisms to detoxify them have previously evolved in the natural world, sometimes in the species that produces the antibiotic itself. The most prevalent and worrisome resistance mechanisms involve the activity of enzymes that modify the drug itself, such as aminoglycoside acetyltransferases or beta-lactamases [19]. In general, such drug detoxification mechanisms carry only miniscule fitness costs. However, if a particular antibiotic is kept out of use for many years, the cost of maintaining the genes encoding these resistance determinants (especially if they are encoded on a plasmid) tends to decrease their prevalence [20]. 186 Remarkably, although AmB is a natural product, no drug-detoxifying enzymes are known to act upon it. This is a possible consequence of the unusual polyene structure of AmB, which does not resemble any cellular metabolites. Thus, there are no enzymes acting on similar molecules that could evolve the ability to degrade AmB through subtle changes in substrate specificity. Indeed, synthetic antibacterials that do not closely resemble cellular metabolites, including oxazolidinones and fluoroquinolones, remain generally insusceptible to resistance by enzymatic modification [19]. Another common mechanism of antibiotic resistance that must be evaded in bacteria and fungi alike is pump-mediated efflux. Overexpression of multidrugresistance (MDR) efflux pumps in certain species, including Pseudomonas aeruginosa, does appear to have some negative consequences for virulence in certain models [21]. However, the frequent isolation of MDR Pseudomonas (and other gram negative bacteria) in the clinic suggests that these costs can either be buffered by compensatory mechanisms, or still permit virulence in humans. Drug efflux is also a major mechanism of antifungal drug resistance, to the azoles. As AmB does not need to enter cells to be active, it is not susceptible to such a mechanism of resistance. Thus, although targets on the cell surface are few in number, they present this highly attractive benefit of evading efflux. Yet another important mechanism of resistance is changes in the drug target These can occur through, amino acid substitutions in the drug-binding site of the target protein, post-translational modification of the target protein (typically methylation), or alteration of the structure of non-protein targets such as lipids [19]. Modifications of amino acid side chains can readily occur without significant fitness costs in most cases, 187 and single mutations that confer resistance must be avoided. One approach to designing agents that are not susceptible to resistance through point mutation is to design inhibitors that fit within the "substrate envelope" of the target. Using this approach, mutations that abrogate drug binding also abrogate substrate binding and thereby enzymatic function [22]. Cellular components that present fewer opportunities for modification than proteins (and ribosomal RNA) are better targets for resistance-refractory agents. Importantly, when such cellular components are central and highly conserved, their modification bears more severe fitness costs for the pathogen. Advantages and limitations of targeting Lipids Combining all of these previous observations with my own results with AmB suggests that lipids are ideal targets for resistance-refractory antimicrobial agents. First, they are less amenable to modification than other biomolecules. Their relatively small and simple structures are not readily modified without severe consequences for cellular membrane structure. As many lipids are abundant and conserved, membrane proteins have evolved to function in concert with their structures. As such, even small modifications in lipid structure can have drastic consequences for the function of many such proteins. Second, cell-surface lipids can be targeted without the potential for resistance mediated by efflux. Finally, as drugs targeting lipids can rapidly kill cells through immediate permeabilization, the pathogen may have insufficient time to deploy enzymatic modification of such compounds prior to cell death. Available antibacterial drugs targeting membrane phospholipids have also remained effective over time, albeit not quite as refractory to resistance as AmB. The 188 polymyxin-based drug colistin is regaining clinical use against gram negative bacteria, which it kills by binding to the outer membrane. However, resistance has repeatedly emerged through modification of the structure of outer membrane lipopolysaccharide [23]. This mechanism may reflect that the bacterial outer membrane acts mainly as a sieve from the exterior world, separated from the bacterial cytoplasm by a cell wall and inner membrane. As such, the structures of outer membrane lipids, which are already much larger and more complex than sterols, can be readily modified without the phenotypic consequences inherent in modifying the eukaryotic plasma membrane. Daptomycin acts on the membrane of gram positives (interior to the cell wall), and is generally refractory to resistance, but is slowly losing efficacy. Resistance to daptomycin appears to occur through complex modifications of phosphatidylglycerol that are still poorly understood [24]. The ability of bacteria to evolve resistance to these two agents may reflect their greater tolerance for perturbation of membrane structure compared to fungi. It may also reflect a greater diversity of large, complex, and modifiable lipid structures in bacterial membranes than in fungal membranes. Another possibility is that the resistancerefractory nature of AmB is a property of targeting sterols, not phospholipids; these two classes of lipid have highly distinct structures and functions. Unfortunately, bacterial membranes are generally devoid of sterols. Nevertheless, the further characterization of bacterial membrane components might serve to identify a similarly irreplaceable target, and thus present a promising target for intervention. 189 FUTURE PROSPECTS The evolutionary history of life on earth suggests that over time, populations will adapt to nearly any challenge they encounter. However, ecological studies suggest that focused adaptation to one extreme condition often diminishes the ability of an organism to tolerate other stresses. Our work suggests that AmB exploits this evolutionary conundrum by imposing a tradeoff between resistance and adaptation to the host environment. Finding new ways to impose evolutionary conflicts on pathogens is a promising strategy to stop the global challenge posed by drug resistance. References 1. Taipale M, Jarosz DF, Lindquist S (2010) HSP90 at the hub of protein homeostasis: emerging mechanistic insights. Nat Rev Mol Cell Biol 11: 515-528. 2. Xu Y, Lindquist S (1993) Heat-shock protein hsp90 governs the activity of pp60v-src kinase. Proc Natl Acad Sci U S A 90: 7074-7078. 3. Taipale M, Krykbaeva I, Koeva M, Kayatekin C, Westover KD, et al. (2012) Quantitative analysis of HSP90-client interactions reveals principles of substrate recognition. Cell 150: 987-1001. 4. Rutherford SL, Lindquist S (1998) Hsp90 as a capacitor for morphological evolution. Nature 396: 336-342. 5. Queitsch C, Sangster TA, Lindquist S (2002) Hsp90 as a capacitor of phenotypic variation. Nature 417: 618-624. 6. Jarosz DF, Lindquist S (2010) Hsp90 and environmental stress transform the adaptive value of natural genetic variation. Science 330: 1820-1824. 7. Sollars V, Lu X, Xiao L, Wang X, Garfinkel MD, et al. (2003) Evidence for an epigenetic mechanism by which Hsp90 acts as a capacitor for morphological evolution. Nat Genet 33: 70-74. 8. Speechia V, Piacentini L, Tritto P, Fanti L, D'Alessandro R, et al. (2010) Hsp90 prevents phenotypic variation by suppressing the mutagenic activity of transposons. Nature 463: 662-665. 9. Cowen LE, Lindquist S (2005) Hsp90 potentiates the rapid evolution of new traits: drug resistance in diverse fungi. Science 309: 2185-2189. 10. Pfaller MA, Diekema DJ (2007) Epidemiology of invasive candidiasis: a persistent public health problem. Clin Microbiol Rev 20: 133-163. 190 11. Hull CM, Bader 0, Parker JE, Weig M, Gross U, et al. (2012) Two clinical isolates of Candida glabrata exhibiting reduced sensitivity to amphotericin B both harbor mutations in ERG2. Antimicrob Agents Chemother 56: 6417-6421. 12. Kelly SL, Lamb DC, Taylor M, Corran AJ, Baldwin BC, et al. (1994) Resistance to amphotericin B associated with defective sterol delta 8-->7 isomerase in a Cryptococcus neoformans strain from an AIDS patient. FEMS Microbiol Lett 122: 39-42. 13. Pfaller MA, Messer SA, Boyken L, Rice C, Tendolkar S, et al. (2005) Global trends in the antifungal susceptibility of Cryptococcus neoformans (1990 to 2004). J Clin Microbiol 43: 2163-2167. 14. Blum G, Hortnagl C, Jukic E, Erbeznik T, Pumpel T, et al. (2013) New insight into amphotericin B resistance in Aspergillus terreus. Antimicrob Agents Chemother 57: 1583-1588. 15. Blum G, Perkhofer S, Haas H, Schrettl M, Wurzner R, et al. (2008) Potential basis for amphotericin B resistance in Aspergillus terreus. Antimicrob Agents Chemother 52: 1553-1555. 16. Anderson TM, Clay MC, Cioffi AG, Diaz KA, Hisao GS, et al. (2014) Amphotericin forms an extramembranous and fungicidal sterol sponge. Nat Chem Biol 10: 400406. 17. Clatworthy AE, Pierson E, Hung DT (2007) Targeting virulence: a new paradigm for antimicrobial therapy. Nat Chem Biol 3: 541-548. 18. Vale-Silva LA, Coste AT, Ischer F, Parker JE, Kelly SL, et al. (2012) Azole resistance by loss of function of the sterol Delta(5),(6)-desaturase gene (ERG3) in Candida albicans does not necessarily decrease virulence. Antimicrob Agents Chemother 56: 1960-1968. 19. Alekshun MN, Levy SB (2007) Molecular mechanisms of antibacterial multidrug resistance. Cell 128: 1037-1050. 20. Andersson DI, Hughes D (2010) Antibiotic resistance and its cost: is it possible to reverse resistance? Nat Rev Microbiol 8: 260-271. 21. Olivares J, Alvarez-Ortega C, Linares JF, Rojo F, Kohler T, et al. (2012) Overproduction of the multidrug efflux pump MexEF-OprN does not impair Pseudomonas aeruginosa fitness in competition tests, but produces specific changes in bacterial regulatory networks. Environ Microbiol 14: 1968-1981. 22. Chellappan S, Kiran Kumar Reddy GS, Ali A, Nalam MN, Anjum SG, et al. (2007) Design of mutation-resistant HIV protease inhibitors with the substrate envelope hypothesis. Chem Biol Drug Des 69: 298-313. 23. Wright MS, Suzuki Y, Jones MB, Marshall SH, Rudin SD, et al. (2014) Genomic and transcriptomic analyses of colistin-resistant clinical isolates of Klebsiella pneumoniae reveal multiple pathways of resistance. Antimicrob Agents Chemother. 24. Bayer AS, Schneider T, Sahl HG (2013) Mechanisms of daptomycin resistance in Staphylococcus aureus: role of the cell membrane and cell wall. Ann N Y Acad Sci 1277: 139-158. 191 Appendix A: Selective Targeting of the Mitochondrial Phosphate CarrierYields an Antifungal Therapeutic Strategy that Evades Resistance *This chapter is currently in preparation for submission. 192 Selective Targeting of the Mitochondrial Phosphate Carrier Yields an Antifungal Therapeutic Strategy that Evades Resistance Benjamin M. Vincent" 2 , Willmen Youngsaye 3 , Catherine Hartland3 , Alex K. Lancaster2 Ruth Scherz-Shouval 2, Luke Whitesell 2, Susan Lindquist24 Affiliations 1 Microbiology Graduate Program, Massachusetts Institute of Technology, 77 Massachusetts Avenue, Cambridge, Massachusetts, 02139, United States of America, 2 Whitehead Institute for Biomedical Research, 9 Cambridge Center, Cambridge, Massachusetts, 02142, United States of America, 3 Chemical Biology Platform and Probe Development Center, Broad Institute of MIT and Harvard, 7 Cambridge Center, Cambridge, MA 02142, USA 4 Howard Hughes Medical Institute, Department of Biology, Massachusetts Institute of Technology, Cambridge, Massachusetts, 02139, United States of America ABSTRACT Novel approaches to the treatment of drug-resistant fungal infections are sorely needed. Here we describe the discovery of FT-350, a highly potent thiohydantoin derivative that kills fungi by targeting the mitochondrial phosphate carrier. A single residue of the mitochondrial phosphate carrier (Asni 84) is responsible for a >500-fold difference in potency of FT-350 against fungal and human cells. Resistance to FT-350 emerges primarily through deletions in mitochondrial DNA that disable respiration, but render cells hypersensitive to widely-used azole antifungals. These data suggest that selective targeting of mitochondrial phosphate transport could provide an avenue to the development of an antifungal combination therapy that evades resistance. INTRODUCTION Although many complex natural products that selectively kill fungi have been described, tractable synthetic compounds with potent and selective antifungal activity are exceedingly rare [1,2]. Indeed, azole antifungals targeting Erg IIp are the only agents of purely synthetic origin to have gained broad clinical use against fungal infections (with 193 the exception of topical agents). Although small, synthetic compounds with useful antifungal activity are very difficult to find, they have great advantages over natural product-based agents. First, their chemical tractability allows for repeated rounds of optimization for important therapeutic parameters, including potency, selectivity, spectrum of activity, off-target effects, in vivo half-life, and oral bioavailability. Second, small synthetic agents are better than large natural products at penetrating hard-to-reach niches in which fungal pathogens can hide and resist treatment [3]. Third, scale-up and production of synthetic agents is generally a much simpler and more predictable process than it is for natural products. Most importantly, a small synthetic agent would be an ideal candidate for an oral combination therapy with azoles that could clear fungal infections more rapidly and prevent the emergence of resistance. RESULTS Identification of a Thiohydantoin Derivative with Potent Antifungal Activity In a high-throughput screen for small molecules that reverse azole resistance in C. albicans (described in detail in chapter 4), we identified a thiohydantoin-based scaffold (Figure IA, left panel) with potent antifungal activity as a single agent (MIC = 0.3 pM). This compound was a hit in less than 1% of other screening assays in which it was tested (by other investigators), suggesting it does not act promiscuously [4]. Initial structureactivity relationship studies performed around this scaffold identified a fluorinated derivative with 5-fold improved potency, which we named FT-350 (Figure 1A, right panel). Under standard susceptibility testing conditions, FT-350 exhibited surprisingly strong antifungal activity against the azole-resistant strain CaCi-2 as a single-agent (MIC 0.0625-0.125ptM) (Figure IB). Antifungal activity was even more potent in the presence 194 of fluconazole (MIC 0.015-0.03pM). Extensive details on the testing and structureactivity relationships of the thiohydantoin scaffold are available online in the indicated reference (MLPCN probe ML316) [4]. Initial studies with FT-350 showed an unusual pattern of antifungal activity against S. cerevisiae and C. albicans. FT-350 potently inhibited the growth of S. cerevisiae on media containing glycerol, but not glucose, as a carbon source (Figure 1 C). This result indicated that it might act as an inhibitor of mitochondrial respiration. However, FT-350 inhibited growth of C. albicans under both fermenting and respiring conditions (glucose and glycerol) with equal potency (Figure ID). Although S. cerevisiae represses respiration in the presence of glucose and C. albicansdoes not, respiration is not required for growth of C. albicans [5]. Taken together, these results indicated that FT-350 did not act as a straightforward inhibitor of the electron transport chain. To determine the fungal selectivity of FT-350, we tested it against two mammalian cell lines, mouse NIH-3T3 fibroblasts and human HepG2 hepatocellular carcinoma cells. As our fungal data suggested that this agent targets respiration, we tested the toxicity of FT-350 under forced respiration conditions, using media with galactose as the primary sugar and quantifying cellular ATP levels [6]. Under these conditions, we noted no toxicity to the HepG2 cells at 32 pM, and only mild toxicity to NIH-3T3 fibroblasts at 16 and 32 pM (Figure lE). These data suggest that FT-350 exhibits a therapeutic index of at least 500-fold in cell culture. 195 Loss of Mitochondrial Complex IV Confers Resistance to FT-350 In an attempt to identify the target of FT-350, we selected mutants resistant to this compound to be used for whole-genome sequencing. Selection of resistant mutants in C. albicans on media containing 2% glucose and 5pM FT-350 resulted in a high rate of emergence (~ 10-) of slow-growing colonies that, upon retesting, were completely unaffected by treatment with FT-350. Genome sequencing of one of these mutants along with the parental strain revealed that it contained a large deletion in the mitochondriallyencoded core enzymatic subunit of cytochrome C oxidase, COX (Complex IV of the election transport chain) (Figure 2A). Two other mutants with the same phenotype also harbored deletions in the mitochondrial COX gene (data not shown). Cytochrome C oxidase is a highly conserved protein complex that acts directly after cytochrome bc 1 (ubiquinol cytochrome C reductase, described in chapter four) in the electron transport chain. However, since cytochrome C oxidase is not required for fungal growth, and its deletion confers resistance to FT-350. Thus, FT-350 cannot kill fungi through inhibition of FT-350. Rather, loss of cytochrome C oxidase appears to detoxify the effects of FT350. Indeed, we also noted that deletion of RIP] of complex III also conferred resistance to FT-350 (data not shown). Further analysis is needed to determine which mitochondrial proteins and complexes must be present and functional for FT-350 to be toxic. The finding that loss of mitochondrial respiration is a major mechanism of resistance to FT-350 is particularly interesting because loss of mitochondrial respiration renders fungi hypersensitive to azole antifungals (chapter four). To demonstrate pursue the potential of these two compounds in combination, we monitored their effects on the CaCi-2 fluconazole-resistant strain and the FT-350-resistant isolate derived from CaCi-2. 196 We tested these two strains on media containing fluconazole, FT-350, or both compounds, as well as under respiring conditions (glycerol media) (Figure 2B). As expected, the FT-350-resistant cytochrome C oxidase mutants were unable to grow on glycerol media and were also acutely hypersensitive to fluconazole. Thus, as the dominant mechanism of resistance to FT-350 leads to hypersensitivity to fluconazole, these two agents could be used in a combination therapy that poses very high barriers to resistance. A Point Mutation in the Mitochondrial Phosphate Carrier Confers Resistance to FT-350 Our selections for resistance to FT-350 on glucose-containing media allowed for the emergence of respiration-deficient mutants and thus did not reveal the target. To identify mutants that bypass this mechanism of resistance, we selected for colonies on media containing FT-350 with glycerol as the sole carbon source, so that cells that lose respiration would be unable to grow, and only respiration-competent FT-350-resistant mutants could emerge. Under these conditions, mutants emerged at a much lower rate (<108), and were not slow-growing. Genome sequencing of three independently-selected mutants resistant to FT-350 revealed that they all carried an identical heterozygous mutation in MIR], which encodes the mitochondrial phosphate carrier protein [7,8] (Figure 3A). This mutation replaced asparagine 184 of the protein with threonine (henceforth referred to as Ni 84T). Miri p is localized to the inner membrane of mitochondria and transports phosphate into the mitochondrial matrix [9,10]. It is the sole source of phosphate for the production of ATP from ADP by ATP synthase. Intriguingly, no small molecule 197 inhibitors of this protein have been identified, and only low-affinity, non-selective, thiolreactive agents (such as mersalyl and N-ethylmaleimide) have been used to inhibit its activity in vitro [11]. Mirip is required for respiration of S. cerevisiae, but not for fermentation, and it has not been studied in C. albicans or other fungal pathogens [7]. We compared the sequence surrounding the resistance-determining N 184 residue of the mitochondrial phosphate carrier protein homologs across various fungi as well as the human homolog of the protein. Intriguingly, asparagine is present at position 184 in all species sensitive to FT-350, but threonine is present in this position in all species resistant, including humans (human homolog is named SLC25A3) (Figure 3B). These data suggest that the presence of asparagine and not threonine at position 184 of the Mirip protein dictates the activity of FT-350. To confirm that the Ni 84T mutation is critical for the activity of Miri p, we cloned it into an integrating C. albicans expression vector and transformed the construct into a wild-type strain [12]. Indeed, transformants expressing the Ni 84T mutation exhibited a 512-fold increased MIC for FT-350 (Figure 3C). Importantly, while cell culture assays for mammalian cell cytotoxicity are liable to artifacts, the extremely strong resistance conferred by replacing a single residue of fungal Mirip with the corresponding residue of the human homolog provides compelling evidence for the fungal selectivity of this compound. To further this analysis, we perturbed the copy number of MIR] in C. albicans, and tested its effects on growth inhibition by FT-350. Deletion of one copy of the MIR] gene caused a 2-fold decrease in the MIC for FT-350, supporting that it may be the target of the compound on the principle of induced haploinsufficiency [13,14] (Figure 3C). 198 Adding one additional copy of the MIR] gene resulted in a ~2-fold increase in resistance to FT-350, also supporting that Mirlp could be the drug target. However, demonstration that FT-350 inhibits mitochondrial phosphate uptake in mitochondria purified from wildtype C. albicans, but not strains expressing the Ni 84T mutant, would be required to confirm Mirlp as the target. DISCUSSION FT-350 presents a novel and intriguing mechanism of action for a small molecule. The questions raised by our unexpected findings with this compound may lead to a deeper understanding of the poorly studied mitochondrial phosphate carrier. An initial question concerns why this drug is potently toxic to C. albicans as a single agent, when other inhibitors of mitochondrial respiration complexes do not kill this species. Several hypotheses could explain this result. First, inhibition of the phosphate carrier could depolarize the inner membrane proton gradient, as this protein co-transports phosphate with protons. Evidence for such a mechanism of killing by FT-350 would be bolstered by demonstrating that treatment with the compound directly depolarizes the mitochondrial membrane potential (using potential-sensitive dyes), and that other uncouplers such as FCCP or 2,4 DNP also kill C. albicans. Second, it is possible that inhibition of phosphate transport into mitochondria would induce an osmotic shock that renders mitochondrial membranes swollen and permeable, and could trigger pathways of programmed cell death. Third, inhibition of phosphate accumulation in the mitochondrial matrix could cause a rapid and severe buildup of ADP, which might be toxic on its own. Finally, it is important to note that while mitochondrial ATP production is not required 199 for survival, mitochondria perform other essential activities in the cell, including lipid biosynthesis and redox regulation. Thus, FT-350 could kill cells by disrupting one of these other activities. Nevertheless, the finding that loss of electron transport chain components (in particular cytochrome C oxidase) confers resistance to FT-350 bolsters a toxic "gain of function" mechanism for its antifungal activity. Whatever the mechanism, FT-350 provides the first chemical tool for studying this poorly understood yet broadly conserved protein, and reveals an unexpectedly vital role of the phosphate carrier in cell survival. Moreover, the potent, single-agent activity of FT-350 and its multilevel synergy with fluconazole suggest that this compound or others like it may hold great promise for the treatment of drug-resistant Candidainfections. MATERIALS AND METHODS Fungal Growth Assays in Liquid Culture Toxicity of FT-350 to fungal cells was tested as described in chapter four, with the following specifications. For glucose/glycerol comparison, media consisted of yeast nitrogen base and complete amino acid mix (Difco) supplemented with 2% glucose or 2% glycerol. Growth was determined by OD600 at 24 hr (C. albicans glucose or glycerol, S. cerevisiae glucose) or 48hr (S. cerevisiae glycerol). Relative growth was normalized to a no-drug control. MIC testing and growth inhibition of strains with varying levels of MIR] was performed in RPMI media with 0.2% glucose, testing for 24hr. Mammalian Cell Cytotoxicity 200 Toxicity to HepG2 and NIH-3t3 cell lines was tested exactly as described in chapter four, recording results at 72hr, and normalizing to DMSO control. Genome sequencing and polymorphism discovery Genome sequencing and polymorphism discovery were performed as described in [15] and chapter four. Spot assays Fungal growth on agar plates was performed by standard methods as previously described [15]. Cloning of MIRI and Transformation of C. albicans The MIR] ORF was cloned from wild-type or Ni 84T mutant strains into the pDIS3 integrating vector [12] using the following oligonucleotides: MIR1-975up-f, tattatcgatTGGACAGGACTAACCCCAAC; MIRi-950dn-r, tatacccgggCAACAATCTTGAATCCGGGTA. MIR] heterozygotes were generated by deleting one copy of MIRI using the HIS3 marker [16] and the following oligonucleotides: MIR I-updel-fATTTGCCTGCCAGAATCAAA; MIRI-updel-r, CACGGCGCGCCTAGCAGCGGGAGGGAATTTTTGGTTGGAA; MIRi-dndel-f, GTCAGCGGCCGCATCCCTGCCCATGAATGAATAAGGGAAAGC, MIRI-dndel-r, CCATGAATGAATAAGGGAAAGC. Transformation of C. albicanswas performed using standard protocols [16]. REFERENCES 1. Roemer T, Krysan DJ (2014) Antifungal drug development: challenges, unmet clinical needs, and new approaches. Cold Spring Harb Perspect Med 4. 201 2. Roemer T, Xu D, Singh SB, Parish CA, Harris G, et al. (2011) Confronting the challenges of natural product-based antifungal discovery. Chem Biol 18: 148164. 3. Odds FC, Brown AJ, Gow NA (2003) Antifungal agents: mechanisms of action. Trends Microbiol 11: 272-279. 4. Hartland CL, Youngsaye W, Pu J, Vincent B, Mosher CM, et al. (2010) Probing Metabolic Requirements for Fungal Virulence - Probe 1. Probe Reports from the NIH Molecular Libraries Program. Bethesda (MD). 5. Sun N, Fonzi W, Chen H, She X, Zhang L, et al. (2013) Azole susceptibility and transcriptome profiling in Candida albicans mitochondrial electron transport chain complex I mutants. Antimicrob Agents Chemother 57: 532-542. 6. Marroquin LD, Hynes J, Dykens JA, Jamieson JD, Will Y (2007) Circumventing the Crabtree effect: replacing media glucose with galactose increases susceptibility of HepG2 cells to mitochondrial toxicants. Toxicol Sci 97: 539547. 7. Murakami H, Blobel G, Pain D (1990) Isolation and characterization of the gene for a yeast mitochondrial import receptor. Nature 347: 488-491. 8. Wohlrab H, Briggs C (1994) Yeast mitochondrial phosphate transport protein expressed in Escherichia coli. Site-directed mutations at threonine-43 and at a similar location in the second tandem repeat (isoleucine-141). Biochemistry 33: 9371-9375. 9. Phelps A, Wohlrab H (2004) Homodimeric mitochondrial phosphate transport protein. Transient subunit/subunit contact site between the transport relevant transmembrane helices A. Biochemistry 43: 6200-6207. 10. Phelps A, Briggs C, Mincone L, Wohlrab H (1996) Mitochondrial phosphate transport protein. replacements of glutamic, aspartic, and histidine residues affect transport and protein conformation and point to a coupled proton transport path. Biochemistry 35: 10757-10762. 11. Phelps A, Wohlrab H (1991) Mitochondrial phosphate transport. The Saccharomyces cerevisiae (threonine 43 to cysteine) mutant protein explicitly identifies transport with genomic sequence. J Biol Chem 266: 19882-19885. 12. Gerami-Nejad M, Zacchi LF, McClellan M, Matter K, Berman J (2013) Shuttle vectors for facile gap repair cloning and integration into a neutral locus in Candida albicans. Microbiology 159: 565-579. 13. Xu D, Jiang B, Ketela T, Lemieux S, Veillette K, et al. (2007) Genome-wide fitness test and mechanism-of-action studies of inhibitory compounds in Candida albicans. PLoS Pathog 3: e92. 14. Roemer T, Boone C (2013) Systems-level antimicrobial drug and drug synergy discovery. Nat Chem Biol 9: 222-231. 15. Vincent BM, Lancaster AK, Scherz-Shouval R, Whitesell L, Lindquist S (2013) Fitness trade-offs restrict the evolution of resistance to amphotericin B. PLoS Biol 11: e1001692. 16. Noble SM, Johnson AD (2005) Strains and strategies for large-scale gene deletion studies of the diploid human fungal pathogen Candida albicans. Eukaryot Cell 4: 298-309. 202 A U* * - FT350: MIC=0.06 pM Hit: MIC=0.3 pM B Relative Growth1.00 FT-350 Alone FT-350 + 8 pg/mi Fluconazole 0.25 0.c 02 0.004 0.006 0.016 0.031 0.063 0.125 0.250 0.500 1.000 [FT-350, IMI C Relative Growth 0.75 - S. cerevisiae, Glucose - S. cerevisiae, Glycerol 0.50 0.004 0.250 0.063 0.616 1.000 [FT-350], pM D Relative Growth -* 0.75, C. albicans, Glucose C. albicans, Glycerol 0.50' 0.2& 0.004 0.250 0.063 0.016 1.000 [FT-350, pM E Relative Growth 1.00. (Galactose Media) 0.7& - Human HepG2 - Mouse 3t3 Fibroblasts 0.50' 0.25 0.5 0.50 1 2 a 4 16 32 [FT-350, 1 M] Figure 1. A thiohydantoin derivative with potent, fungal-selective growth inhibition. A) Structures of initial hit compound and derivative FT-350. B) Growth inhibition of C. albicans CaCi-2 strain in RPMI media by FT-350. C-D) Growth inhibition of S. cerevisiae and C. albicans on glucose or glycerol media. E) 72 hr growth inhibition of HepG2 hepatocellular carcinoma cells or NIH-3T3 mouse fibroblasts by FT350 in DMEM-galactose media, quantified by Cell titer-glo ATP assay. 203 A FT350-R COX(mtDNA) I Glucose + B Glucose Glycerol Fluconazole FCZ-R DMSO FT350-R FCZ-R 0.25 gM FT350 FT350-R Figure 2. Loss of cytochrome oxidase confers resistance to FT-350 but sensitivity to fluconazole. A) Genome sequence and alignment of a FT-350-resistant mutant with a large deletion in the mitochondrial COX gene. B) Serial dilution spot assay of CaCi-2 ("FCZ-R") and the FT350-resistant mutant sequenced above. Plates were photographed at 48hr after spotting yeast. FT-350 was added at 0.25 pM; fluconazole was added at 16 pg/mL. 204 A WT R2 R3 MIR1 B 173 S. Cerevisiae C. C. C. C. A. Glabrata Albicans albicans-R Neoformans Funigatus H. Sapiens 188 FTPILFKQIPYNIAKF FTPILFKQIPYNIAKF FTPILFKQIPYNIAKF FTPILFKQIPYTIAKF FGPILFKQVPYTMAKF FGPILFKQIPYTMAKF GVAPLWRQIPYTMMKF [FT-350 pM C 0 0.0010.003 0.007 0.015 0.0310.062 0.125 0.25 0.5O 1 2 4 8 16 MIR1/MIR1 MI/mirlA MIR1/MIRI+pMIR1 MIR1/MIRI+mir1N184T 0.00 0.25 0.50 0.75 1.00 Figure 3. The mitochondrial phosphate carrier Mirip is a potential target of FT350. A) Alignment of MIR] sequence from wild-type and three independent FT-350resistant mutants, indicating heterozygous N184T mutation in mutants. B) Alignment of protein sequence of amino acids 173-188 from the Mirip homologs of indicated species. Sequences were obtained by BLAST search of the S. cerevisiae Mirip sequence against the non-redundant protein database for each of the indicated species. C) Genetic manipulation of MIR] determines susceptibility to FT-350 in C. albicans. Strains indicated are SN152 wild-type transformed with pDIS3 vector (empty), SN152 wild-type with one copy of MIR] deleted and transformed with pDIS3 vector, SN 152 wild-type transformed with a wild-type copy of MIR] in the pDIS3 vector, and SNI 52 wild-type transformed with the pDIS3 containing the mirJNl84Tmutation. Growth inhibition in media containing a serial dilution of FT-350 was assessed at 24hr and normalized to a nodrug control. 205 CURRICULUM VITAE Benjamin Matteson Vincent benjvinc(agmail.com EDUCATION Massachusetts Institute of Technology, Cambridge, MA Ph.D. Candidate, Microbiology Thesis Advisor: Professor Susan Lindquist September 2008 - December 2014 Stanford University, Stanford, CA Bachelor of Science, Biology September 2004-June 2008 AWARDS AND FELLOWSHIPS NSF Graduate Research Fellowship, 2009-2012 Deans Award for Academic Accomplishment, Stanford University, 2008 Weinstein Award, Department of Biology, Stanford University, 2008 PUBLICATIONS Vincent, B.M., Youngsaye W., Hartland, C., Lancaster, A.K., Whitesell, L., and Lindquist, S. Selective inhibition of the mitochondrial phosphate carrier yields an antifungal therapeutic strategy refractory to the evolution of resistance. In preparation. Vincent, B. M., Langlois J. B., Youngsaye W., Lancaster A. K., Scherz-Shouval R, Whitesell L, Buchwald S, Lindquist S. A Fungal-Selective Cytochrome bcl Inhibitor Impairs Virulence and Prevents the Evolution of Drug Resistance. In preparation. Davis S.A., Vincent B.M., Endo M.M., Whitesell L.W., Marchillo K., Andes D.R., Lindquist, S.* and Burke, M.D.* Non-toxic antimicrobials that evade the emergence of drug-resistance. Submitted. Vincent, B. M., Lancaster, A. K., Scherz-Shouval, R., Whitesell, L., & Lindquist, S. (2013). Fitness trade-offs restrict the evolution of resistance to amphotericin B. PLoS Biology, 10, e1001692. Youngsaye, W., Hartland, C. L., Morgan, B. J., Ting, A., Nag, P. P., Vincent, B., Mosher, C. A., Bittker, J. A., Dandapani, S., Palmer, M., Whitesell, L., Lindquist, S., Schreiber, S. L., & Munoz, B. (2013). ML212: A small-molecule probe for investigating fluconazole resistance mechanisms in Candida albicans. Beilstein Journalof Organic Chemistry, 1501-1507. 206 Youngsaye, W., Dockendorff, C., Vincent, B., Hartland, C. L., Bittker, J. A., Dandapani, S., Palmer,. M., Whitesell, L., Lindquist, S., Schreiber, S. L., & Munoz, B. (2012). Overcoming fluconazole resistance in Candida albicans clinical isolates with tetracyclic indoles. Bioorganic & Medicinal Chemistry Letters, 9,3362-3365. & Youngsaye, W., Vincent, B., Hartland, C. L., Morgan, B. J., Buhrlage, S. J., Johnston, S., Bittker, J. A., MacPherson, L., Dandapani, S., Palmer, M., Whitesell, L., Lindquist, S., Schreiber, S. L., & Munoz, B. (2011). Piperazinyl quinolines as chemosensitizers to increase fluconazole susceptibility of Candida albicans clinical isolates. Bioorganic medicinal chemistry letters, 18, 5502-5505. CONFERENCES Keystone Conference: The Chemistry and Biology of Cell Death Selective targetingof mitochondrialrespirationyields a therapeuticstrategy refractory to the evolution of resistance Poster presentation Santa Fe, NM, February 2014 Gordon Conference: Stress Proteins in Growth, Development and Disease TargetingStress Responses to Prevent Antifungal Drug Resistance Oral presentation Lucca, Italy, July 2011 TEACHING EXPERIENCE Teaching assistant, Professor Alan Grossman, MIT, Microbial Genetics and Evolution, Fall 2009. Teaching assistant, Professor Robert Sapolsky, Stanford University, Human Behavioral Biology, Spring 2008. 207