This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike License. Your use of this
material constitutes acceptance of that license and the conditions of use of materials on this site.
Copyright 2007, The Johns Hopkins University and Damian Walker. All rights reserved. Use of these materials
permitted only in accordance with license rights granted. Materials provided “AS IS”; no representations or
warranties provided. User assumes all responsibility for use, and all liability related thereto, and must independently
review all materials for accuracy and efficacy. May contain materials owned by others. User is responsible for
obtaining permissions for use from third parties as needed.
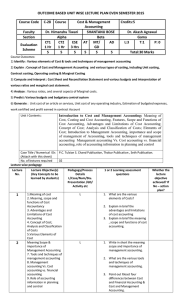
Types of cost data
Lecture 4
Damian Walker
Aim of lecture
To provide conceptual and practical insight into
how to do costing in an economic evaluation
Structure of lecture
What do we mean by cost?
Identify which costs to include
How to measure resource use?
How to value resource use?
How to analyse/present cost data?
Why consider costs?
There are not, never have been and never will be
enough resources to meet all of society’s needs
or wants
Scarcity implies choice between alternatives
Cost is one factor which enables choice
What do we mean by
cost?
Opportunity costs
Opportunity cost = economic cost
Cost is foregone benefit of a resource in it’s best
alternative use
Cost = market price only when price reflects value of
marginal product (perfect competition)
Need to estimate shadow prices / social value of
resources:
no market price: donated goods, volunteer time
distorted price: MP of labour ≠ wage
unstable prices: inflated / deflated exchange rates
where goods have a yield over a period of time: capital
goods (Wednesday’s lecture)
Opportunity cost
As simple as the opportunity cost concept is, it
is one of the most important in microeconomics
and economic evaluation
The art in applying the concept correctly lies in
being able to recognize the most valuable
alternative that is sacrificed by the pursuit of a
given activity
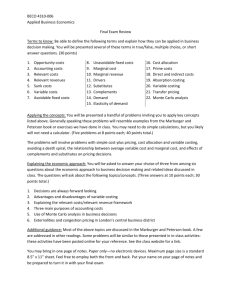
Pop quiz
You won a free ticket to see an Eric Clapton concert
(which has no resale value). Bob Dylan is performing on
the same night and is your next-best alternative activity.
Tickets to see Dylan cost $40. On any given day, you
would be willing to pay up to $50 to see Dylan. Assume
there are no other costs of seeing either performer. Based
on this information, what is the opportunity cost of seeing
Eric Clapton?
a) $0, (b) $10, (c) $40, or (d) $50.
Remember
The opportunity cost of an activity is the value
of everything you must sacrifice to pursue it
So if you are willing to pay as much as $50 to see
Dylan and the cost of a ticket to see Dylan is
$40, what is the opportunity cost of seeing
Clapton?
Reference
Farraro PJ, Taylor LO. Do economists
recognise an opportunity cost when they see
one? A dismal performance from the dismal
science. Contributions to Economic Analysis & Policy
2005; 4(1)
Which costs to
include?
Julien Harneis
freedryk
andyinsouthamerica
The Crownless King
How can we categorise
these costs?
Classification of costs
Capital items: those that last longer than a year
or have a unit price > $100
Recurrent items: those that are used up in the
course of a year and are usually purchased
regularly
Examples?
Classification of costs
Fixed costs
Semi-fixed costs
Variable costs
do not change when the quantity of output produced
changes
change according to how much output produced
Examples?
In the long-run it is assumed that all costs are
variable
Activities as inputs
If one activity is clearly separate from the others,
both financially and administratively, it may be
easier to record the total cost
E.g. start-up, training and social mobilisation
activities are treated as categories of inputs and
included along with personnel, vehicles etc.
it is assumed that all the resources required for
the activity are included in that category and not
under the separate categories
Shared costs
The resources that you are costing may not be
fully used in the specific cost centre that is being
examined
In this case, a decision needs to be made about
what proportion of the resources should be
allocated to the specific cost centre that is being
costed and the way it should be allocated
Shared costs
What are some examples of typical shared costs?
What allocation rules might be used to distribute
these costs to specific cost centres? E.g. in a
hospital, how might we allocate the costs of the
kitchen to different wards?
Methods for allocating shared costs:
direct allocation
step-down allocation
Other costs?
So far focussed on programme costs
What other costs might we consider in, for
example, an economic evaluation of vaccines
against rotavirus?
Classification of costs
Direct
Indirect
Intangible
Health sector
Other sectors
Patient / family
Productivity losses
Future
Which costs to include?
Perspective of analysis
Societal
broad
Other agencies
Health service
Patient
narrow
Which costs to include?
Perspective of analysis
Range of costs
Perspective
Inpatient days & Special education
outpatient visits
Days off work
Health service
✔
✖
✖
Health service &
other agencies
✔
✔
✖
Societal
✔
✔
✔
Which costs to include?
Time-frame of analysis
Suitable for disease and intervention in question
days: prophylactic drugs for diarrhoea
months: chemo-prophylactic drugs for malaria
life-time: drugs for HIV/AIDS
Which costs to include?
Future costs
Life-years normally Gained life-years
lived
Related medical and
non-medical costs
Incorporate
Incorporate
Unrelated medical
and non-medical
costs
Leave out of the
analysis
May be incorporated
at analyst’s discretion
in a sensitivity
analysis
Which costs to include?
Quantitative importance
big-ticket items first
will inclusion of additional costs affect the
conclusions?
Attribution
does the resource use consumed relate to the disease
(intervention)?
How to measure
resource use?
How to measure resource use?
Different study designs
Possible vehicles for resource use data:
Best source of data depends on:
RCTs
observational studies
literature
administrative databases
expert opinion
study question
research resources
Economic evaluations usually use a
range of methods
Most reliable
Least reliable
How to measure resource use data?
Advantages of RCTs
‘Economic analyses … are likely to be most
helpful when undertaken as part of large,
unblinded, pragmatically designed, randomised
trials based as closely as possible on regular
clinical practice’
(Freemantle & Drummond 1997)
How to measure resource use data?
Advantages of RCTs
Randomisation ensures internal validity
Facilitates prospective data collection
accurate
unbiased
Can link with measurement of health outcome
Uses individual patient data
can use standard tests of significance
How to measure resource use?
Disadvantages of RCTs
Often too short in duration
May lack external validity
May include protocol driven costs
Will need to extend study to measure others
costs
How to measure resource use data?
Data collection techniques
Case report forms
Medical records
Questionnaires
Patient diaries
DeMTAP pictorial diaries
Consumption and
expenditure data
Health and non-health
12-month period
Includes home-produced
consumption
Prompts in the form of a
checklist and aide
mémoire
Lesong Conteh
Source: Wiseman V, et al. Using diaries to collect data in resource-poor settings: questions on design and implementation.
Health Policy Plan 2005;20:394-404. Used with permission. Copyright 2005 Oxford University Press. All Rights Reserved.
Source: Wiseman V, et al. Using diaries to collect data in resource-poor settings: questions on design and implementation.
Health Policy Plan 2005;20:394-404. Used with permission. Copyright 2005 Oxford University Press. All Rights Reserved.
How to measure resource use?
How detailed to go?
Micro costing vs. gross costing (Gold et al.
1996)
Top-down vs. bottom-up (Drummond et al.
2005)
Choice depends on need for specific estimation
vs. research costs
Precision vs. pragmatism
How to value resource
use?
How to value resource use?
Principles involved
Opportunity cost
value of next best use of resources
perfectly competitive market, price = opportunity cost
prices in health care often unavailable or distorted
caution in using prices derived from health care
‘markets’
need to use shadow prices
Well, that’s the theory at least …
In practice, most studies use unadjusted market
prices and / or use cost-to-charge ratios
Costs vs. charges
In the USA, a common method for estimating
the economic cost of medical services is to
adjust the charges through the use of cost-tocharge ratios
Cost-to-charge ratios are coefficients developed
by expert panels to convert charges for medical
services to their true economic costs
Applying cost-to-charge ratios to medical service
charges produces average estimates of true costs
How to value resource use?
Principles involved
Average vs. marginal cost?
Marginal costs only cover the costs of producing
one additional unit of output
Choice depends on time-frame of analysis
short-term, few items are variable, e.g. drugs, tests
long-term, all items are variable including labour and
capital
Economists often take long-run perspective
In long-run can use average cost = marginal cost
Definitions
Average cost = TC / Q, the average cost per
unit of output
Marginal cost = (TC of x + 1 units) – (TC of x
units), the extra cost of producing one extra unit
of output
Average marginal cost = (TC of x units – TC of
y units) / (x units – y units), where x > y
Incremental cost = extra cost incurred by one
programme over another
Example
Say, for example, 60% of children in Nepal are
fully vaccinated at a cost per child of $15
The National Immunisation Programme in Nepal
aims to fully vaccinate 85% of children: do you
think the average marginal cost per additional
child fully vaccinated will be <, = or > than $15?
Why?
How to value resource use?
Sources for health service unit costs
Administrative databases (DRGs, reference
costs), e.g.
www.who.int/choice/country/en/index.html
Manuals, e.g.
www.pssru.ac.uk/uc/uc2006contents.htm
Published literature
Specific estimation
How to analyse and present cost
data?
Present resource use separately from unit cost
Present distribution of costs
Despite the usual skewness in the distribution
of costs, it is the arithmetic mean that is the
most informative measure
Measures other than the arithmetic mean do
not provide information about the cost of
treating all patients, which is needed as the
basis for healthcare policy decisions
Issues in analysis of costs
Parametric statistics assume normal distribution
Costs may not be normally distributed
So either:
use standard approaches such as t tests
OR use non-parametric techniques (such as
bootstrapping)
May not have power to detect difference in costs
Critique of published costing studies
A review of 45 randomised trials that included
economic evaluations and were published in 1995
showed serious inadequacies in the use of
statistical methods for costs (Barber & Thompson
1998)
A re-review of these studies found that the costing
methods were of poor quality (Graves et al. 2002)
Graves et al. (2002) concluded that “No amount
of statistical analysis can compensate for poor
quality cost data”
Conclusions
Good costing needs to:
be explicit about assumptions
define the perspective adopted
apply the opportunity cost principle
recognise the importance of the time-frame
Conclusions
Issues for debate include
which perspective should be adopted?
how long should the time-frame be?
whether to include future costs?
precision vs. pragmatism: how detailed should cost
measurement be?
References
Barber JA, Thompson SG. Analysis and interpretation of cost
data in randomised controlled trials: review of published studies.
BMJ. 1998; 317: 1195-1200
Freemantle N, Drummond M. Should clinical trials with
concurrent economic analyses be blinded? JAMA. 1997; 277(1):
63-64
Graves N, Walker D, Raine R, Hutchings A, Roberts JA. Cost
data for individual patients included in clinical studies: no
amount of statistical analysis can compensate for inadequate
costing methods. Health Econ. 2002; 11(8): 735-739.
Wiseman W, Conteh L, Matovu F. Using diaries to collect data
in resource-poor settings: questions on design and
implementation. Health Policy Plan. 2005; 20(6): 394-404