This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike License. Your use of this
material constitutes acceptance of that license and the conditions of use of materials on this site.
Copyright 2007, The Johns Hopkins University and Jonathan Weiner. All rights reserved. Use of these materials
permitted only in accordance with license rights granted. Materials provided “AS IS”; no representations or
warranties provided. User assumes all responsibility for use, and all liability related thereto, and must independently
review all materials for accuracy and efficacy. May contain materials owned by others. User is responsible for
obtaining permissions for use from third parties as needed.
Session 1
Overview of Health Insurance
& Managed Care Principles
& History
Jonathan P. Weiner, Dr. P.H.
Professor or Health Policy & Management
Goals of Session
• To introduce some basic principles of
health insurance and managed care.
• To provide a brief history and
overview of health insurance and
managed care in the US.
• To identify some key trends
3
Growth in US Health Care Spending:
1962-2007
2000
1800
Dollars (billions)
1600
1400
1200
1000
800
600
400
200
0
1962 1966 1970 1974 1978 1982 1986 1990 1995 1998 2000 2007
Source: HCFA, CMS
Year
4
Paying for Health Care: Alternative
Approaches
• Government employed providers
• Government “social insurance”
– Mandatory buy-in
– Entitlement for special populations
• As “benefit” of employment
– Insurance
– Direct care or access to contract providers
•
•
•
•
Union/worker collectives
Private “indemnity” health insurance
Out of pocket
Charity care
5
Definition of Insurance
• A social device where a group of persons
transfers risk to an insuring entity in order to
combine loss experience.
• This theoretically permits the ability to
actuarially predict these “losses” and to
calculate the premium payments that will need
to be contributed by all members of the risk
pool.
6
Some characteristics of an “ideal”
private insurance market
• Large risk pool
• Predictable, but “random” event
• Potential high cost of insurable event
• Event not controllable by parties
– “moral hazard”
• Market economically feasible
7
Approaches for Sharing and Bearing
Insurance “Risk”
• Consumers
– Premiums,cost sharing (deductibles,co-pays,co-insurance,
coverage threshold)
• “Intermediary” (Insurance/managed care entity)
– Inclusions/exclusions, thresholds, re-insurance
• Providers
- Capitation, risk-sharing arrangements,employment
• Employers
– Premiums, self-insurance, re-insurance
8
Patient Cost, Use, and Insurance
Coverage
Patient Cost of Care
Total Cost for
Uninsured Patient
Out-of-pocket cost for
insured patient, net of
insurance premium
Co-insurance
applies
Use of Care
Deductible
Out-of-Pocket
Limit
External Plan
Maximum
Adapted from Chollet DJ. Mapping Insurance Markets. State Coverage Initiatives, AcademyHealth, 1997.
9
Why Employer’s Got Involved In Health
Care
• Healthy employees are productive employees
• European immigrant / Union expectations
• Vacuum existed in the 1930-50’s, now “stuck” in
this role.
• Tax advantage
• Attracts good employees
• “Self Insurance” (ERISA) is now big factor
10
US Health Insurance: Some Historical
Footnotes
• 1930’s -- Blue-Cross/ Blue Shield and Hospital
Association.
• 1930’s – Prepaid-Group Practices (PGPs) and
Union/Employers
• 1950’s – Commercial insurers get into the act
• 1960’s -- Federal “great society” – Medicare and
Medicaid
• 1970’s - The “Health Maintenance Organization” (HMO)
Act (the unholy alliance of AMA sponsored IPAs and
PGPs)
11
Proportion of Americans with Health
Insurance: 1940-2005
100
90
70
60
50
40
30
20
05
20
00
20
95
19
90
19
80
19
75
19
70
19
65
19
60
19
55
19
50
19
45
19
40
10
0
19
% Insured
80
Year
12
Health Care Financing and Coverage
(Approx) in the US
Private Ins.
Population
67%
Payment
44%
Medicare
10
16
Medicaid
9
14
14
-
16
10
Uninsured
Out-of -Pocket
Other
13
Who Pays for Health Care 1965-2001
Public Total
Private Insurance
Private Other
Private Out-of-Pocket
100%
90%
29%
80%
60%
23%
25%
35%
5%
6%
6%
5%
42%
41%
46%
45%
1975
1985
1995
2001
6%
20%
10%
33%
30%
50%
30%
14%
44%
70%
40%
15%
22%
25%
0%
1965
CMS Office of the Actuary, National Health Statistics Group. Figures may not
add due to rounding.
14
The “Actuarial Cycle” -Cost / premium see-saw
Image from CMS Health Care Industry Market Update. March 24, 2003.
15
Insurance premiums vs. earnings and
inflation
Health Insurance Premiums
Overall Inflation
Workers' Earnings
20%
18%
18.0%
16%
14%
14.0%
13.9%
12.9%
12%
12.0%
11.2%
10.9%
10%
9.2%
8.5%
8%
8.2%
6%
5.3%
4%
2%
0.8%
0%
1988
1989
1990
1993
1996
1999
2000
2001
2002
2003
2004
2005
Kaiser/HRET Survey of Employer-Sponsored Health Benefits: 1999-2005; KPMG Survey of Employer-Sponsored Health
Benefits: 1993, 1996; The Health Insurance Association of America (HIAA), 1988, 1989, 1990; Bureau of Labor Statistics,
Consumer Price Index, U.S. City Average of Annual Inflation (April to April), 1988-2005; Bureau of Labor Statistics, Seasonally
Adjusted Data from the Current Employment Statistics Survey (April to April), 1988-2005.
16
The Late 1980’s: medical inflation is out
of control
• The bankrollers of the system
said enough was enough, and
the era of “managed care”
was born. HMOs and their
techniques served as the
model.
17
Managed Care’s Approximate Share of the
Health Insurance Market in 1988 & 2007
MCO
FFS
120%
100%
15%
80%
60%
75%
85%
40%
20%
25%
0%
1988
2007
18
The Key “Ingredients” of Managed Care
• Care “management”
– aka, utilization/disease management
• Vertical integration / coordination
• Financial risk sharing with providers
• Attempts at instilling a market
19
Definition of Managed Care
An integrated system that manages
health services for an enrolled
population rather than simply
providing or paying for them.
Services are usually delivered by
providers who are under contract to, or
employed by the plan.
20
The Health Insurance Models
• Traditional (Fee-for-Service) Indemnity
• “Managed” Indemnity Plan
• Preferred Provider Organization (PPO)
• Health Maintenance Organization (HMO)
21
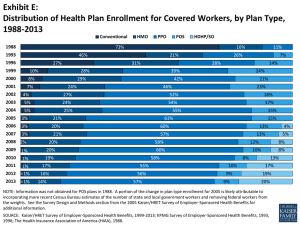
Shift in Employment-Based Plan Type
1988 - 2002
HMO
POS
PPO
100%
14%
90%
9%
8%
38%
41%
25%
22%
7%
5%
48%
52%
22%
18%
23%
26%
2001
2002
27%
80%
46%
70%
60%
Indemnity
35%
73%
28%
50%
26%
40%
14%
24%
31%
27%
28%
29%
1996
1998
1999
2000
30%
20%
10%
11%
16%
7%
21%
0%
1988
1993
Source: Kaiser/HRET Survey of Employer-Sponsored Health Benefits, 2002
22
Managed Care Is Mainstream
Managed Care = US Health Care
23
INGREDIENTS SIMMERING IN TODAY’S
PRESSURE COOKER
• Health care cost spiral is inevitable.
• “We”consumers and providers want it “all.”
• Uninsured likely to grow, government not able
(willing?) to tackle head-on.
• Other than MCOs, no party is willing (able?) to
come to grips with resource limitations.
24