Document 11186897
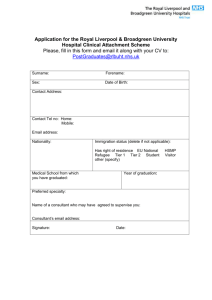
advertisement

Contents Introduction by chief executive 1 About us 2 Equality and diversity 4 Our performance 7 Summary of national survey programme 2013 8 Local hospital patient surveys 14 Benchmarking data 15 How we did against our 2013/2014 priorities • Goal 1: Reducing mortality: We will implement robust systems to improve mortality and improve patient outcomes • Goal 2: Avoiding harm to patients • Goal 3: Deliverying patient centred care, treating all patients with dignity and respect and obtaining feedback that more than 75% of patients would recommend this Trust to a family member or friend 22 26 26 29 Review of quality performance: Safety • Division of Medicine: Reducing risk in Gastroenterology. • Division of Surgery: Abdominal Aortic Aneurysm [AAA] Screening Programme 31 31 33 Review of quality performance: Effectiveness • Division of Medicine. Telemedicine: Stroke Thrombolysis. • Division of Core Clinical and Support Services. Bone Marrow Transplant services Joint Accreditation Committee Europe (JACIE) • Division of Surgery. Pain Management Services 35 35 37 Review of quality performance: Experience • Division of Medicine. Multi Disciplinary Team (MDT) Approaches to supporting patients with alcoholic liver disease. • Division of Surgery: Enhanced recovery programme for patients with Hepato-biliary disease. • Division of Core Clinical Support Services: End of life care: Introducing the role of the volunteer. 40 40 41 Participation in clinical audits 45 Participation in clinical research 47 Commissioning for quality and innovation (CQUIN) framework 50 Data quality 52 Consultation on our Quality Account 55 Priorities for Improvement 2013/14 Goal 1: To reduce mortality Goal 2: Reducing avoidable harm to patients Goal 3: Delivering patient centred care, treating all patients with dignity and respect and obtaining feedback that more than 75% of patients would recommend this Trust to a family member or friend Goal 4: Improving services for patients with learning disabilities 56 57 58 60 Care Quality Commission 64 External Statements 65 1 39 43 62 Introduction by chief executive I am delighted to share with you our fifth Quality Account. This covers the aspect of our services, care and treatment, which matters most to us all – the quality of care we offer to our patients. This year’s Quality Account once again assesses the quality of our services and is here to assure our patients, the public, our commissioners and other partners that we rigorously assess and monitor the quality of the care and treatment we provide to our patients. Over the past year, we have continued to build on local quality measures on aspects of our services which matter most to you. The Board of Directors has been assured about the data and information in this report. We continue to involve the public and our patients in the development of our quality measures. We work hard to ensure that all of our stakeholders have the opportunity to influence what services we focus on in the future. We value and welcome all of the feedback and suggestions that we receive. I hope that you will continue to offer your thoughts on how we can improve further. In the report, you can read about our excellent stroke service, improvements to the way we care for people with alcoholic liver disease, our award-winning enhanced recovery programme and the new Abdominal Aortic Aneurysm screening programme. It has been a challenging year and there are some areas where we need to improve the way we care and treat patients. We are working to ensure patients don’t get an infection when they come into our hospitals and to reduce the numbers of patients waiting for more than four hours to be admitted, transferred or discharged from our Emergency Department. During the year, we commissioned an external review about the way we collect data about Venous Thromboembolism (VTE or blood clot) assessments and to ensure that our processes were robust and that we were being open and transparent. All the achievements we have made on improving the quality of our services for patients could not have happened without the hard work and commitment of our staff. They have well and truly led the way when it comes to making things better. On behalf of the Board of Directors, I would like to thank them for their dedication and enthusiasm. I hope you enjoy reading the Quality Account and please do get in touch if you have any feedback. Aidan Kehoe Chief executive 2 About us We are one of the busiest university teaching hospital trusts in North West England. We manage three hospitals based on two sites: the Royal Liverpool University Hospital, Liverpool University Dental Hospital and Broadgreen Hospital. Our hospitals have often been at the forefront of medical breakthroughs during our long history at the heart of the city. We became an NHS Trust in 1995 and we are currently applying to become a foundation trust. We are the major adult university teaching hospitals for Merseyside and Cheshire; we provide general hospital services to the adult population of Liverpool. We also provide a range of specialist health services, including cancer services for Merseyside, Cheshire and beyond. We are also a centre for clinical research and lead teaching and training in a variety of health professions. We provide a comprehensive range of specialist services to 750,000 people each year within a total catchment population of more than two million people in Merseyside, Cheshire, North Wales, the Isle of Man and beyond. In the past year, we cared for over 87,000 people in our emergency department, around 90,000 day case and inpatients and over 574,000 outpatient appointments. As one of the largest employers in the city, we employ over 5,500 staff as well as staff in services such as catering. Our annual budget is over £430 million. Many of our services are highly regarded both nationally and internationally. These include ophthalmology, pancreatic surgery, gastroenterology, pathology, vascular surgery and interventional radiology. We are a specialist centre for nephrology, renal transplantation, nuclear medicine, haematology, lithotripsy, dermatology, urology and dental services. The long-term plan for the Trust for the Royal Liverpool University Hospital to focus on emergency and complex care, with Broadgreen Hospital to focus on non-emergency care, including specialist services for older people, elective surgical care and dermatology plus a range of outpatient services. We have the largest Emergency Department in the city and we are a Major Trauma Centre, part of the Major Trauma Centre Collaborative for Merseyside and Cheshire. We provide care and treatment for patients with major trauma, who have life threatening injuries and patients with serious illnesses such as strokes and heart attacks. We also provide care for patients with more routine illnesses and injuries, such as simple fractures. The Liverpool University Dental Hospital supports dental teaching and provides specialist dental services and emergency care for the local community. As a major teaching hospital trust we have significant relationships with all the universities in Liverpool, but in particular the University of Liverpool’s medical and clinical schools and Liverpool John Moores University, for the training of nurses. We are a major centre for the diagnosis, treatment, care and research of cancer. We provide a range of cancer services from our renowned Linda McCartney Centre. We are a regional cancer centre for pancreatic, urology, haematology, ocular oncology, testicular, anal, oesophago-gastric, specialist palliative care, specialist radiology, and specialist pathology and chemotherapy cancer treatment services. We are a national centre for ocular oncology (eye cancer). We also have excellent local cancer treatment services, including skin, breast and colorectal, head, neck and thyroid and lung cancer. We host a Macmillan Cancer Information and Support Service, with centres on both of our sites. We have the only National Institute for Health Research funded Biomedical Research Unit in the UK, which is dedicated to pancreatic disease, in collaboration with the University of Liverpool. We have a dedicated Clinical Research Facility and are currently running over 400 clinical research studies. During 2013/14 we remained the host organisation for the Comprehensive Research Network for Cheshire and Merseyside. From April 1 2014, we became the host organisation for the North West Coast Comprehensive Research Network. We continue to look at ways to develop our research and development programme to identify improved treatment and care for our patients and patients across the world. 3 Equality and diversity Our commitment to inclusion, equality, diversity and human rights and improving health and employment outcomes for all continues. We ensure compliance with the Equality Act 2010 via participating in the Equality Delivery System (EDS) (a national tool for reviewing and assessing equality performance with stakeholders, bringing equality into core business and identifying future priorities and actions), setting equality objectives, conducting equality impact analyses and publishing equality information on our website. We aim to achieve equality of outcomes for all irrespective of protected characteristics (age, gender, race, disability, religion or belief, marital or civil partnership status, sexual orientation, gender reassignment, pregnancy and maternity) The four goals of the EDS are: • Better health outcomes for all • Improved patient access and experience • Empowered, engaged and well supported staff • Inclusive leadership at all levels. EDS progress is reviewed annually with stakeholders, the Trust improved on nine outcomes in 2013. Full results can be viewed on the equality and diversity section of our website www.rlbuht.nhs.uk/Equality%20and%20Diversity/Pages/ Equality%20Delivery Six equality objectives were set in April 2012 to be reviewed in 2016. Progress is monitored through the Equality & Diversity sub-committee. Objective Progress To extend patient profiling (equality monitoring) data collection to all protected characteristics by April 2013 Red, Amber, Green Rating We collect and record equality data for patients across each of the nine protected characteristics. In 2013 we set a target of 95% complete equality data for new patients across all protected characteristics. We consulted the community to identify barriers to equality monitoring and increase public awareness of the rationale/benefits for monitoring and are working collaboratively with other NHS trusts to establish an equality monitoring media campaign to continue to raise public awareness and improve response rates. 4 To introduce robust equality performance reporting and monitoring on all protected characteristics by April 2013 We monitor patient equality data annually to understand the demographics of patients accessing services in comparison to the population served, and analyse patient survey results from an equality perspective and equality monitor formal complaints. This allows us to identify if all areas of the community are accessing services and monitor performance outcomes to identify any differences in experience and outcomes between people from different groups. Reporting currently covers gender, age, ethnicity, religion and belief and marital/civil partnership status and will be extended to cover disability and sexual orientation when sufficient equality data is available. This data shows that we have higher `Did not attend’(DNA) rates for Black and minority ethnic (BME) patients, and a shorter average length of stay. We consulted via Merseyside Black History month to try and identify any underlying reasons for the higher DNA rates and are trialling using the telephone interpreting service to remind patients that do not speak English about their appointments. To develop readily available An accessible publications policy was introduced in 2013. This accessible patient policy is used to determine which accessible formats we will information including routinely provide information in to meet diverse patient needs. patient information leaflets, corporate reports and appointment letters To conduct an equal pay audit in 2012 An equal pay audit was completed and findings investigated. Actions have been agreed to improve the quality of employee data across all protected characteristics to over 75% disclosure by January 2015. To set workforce diversity targets to develop a more representative workforce by April 2013 A workforce diversity disclosure target of over 75% has been set for the protected characteristics of sexual orientation, religion and belief and disability to reduce the number of staff who have stated that they `do not wish to disclose’ this information by January 2015. For all other protected characteristics we have over 90% disclosure. We are taking action to encourage staff to update and disclose their equal opportunities monitoring through an on-going campaign explaining the benefits of equality monitoring and asking staff to check and update their details. 5 In 2013 a health and employment positive action initiative in recruitment was developed with local NHS partners, Skills for Health and Job Centre Plus targeted at BME, older and disabled applicants for employment to address disproportionality identified in short-listing and appointing applicants from this group to give them additional support with completing application forms, and interview skills/techniques. The Trust aims to secure funding to continue with this. To develop skills and competence of staff through new equality and human rights training strategy A new Equality and Human Rights Training Strategy was agreed in 2012. Completion of E&D training is constantly over 90% for all staff. Last year we came in the top 20% of NHS trusts nationally for staff completing equality and diversity training. This year we implemented visual impairment, deaf awareness and lesbian, gay, bisexual and transgender awareness training and will introduce unconscious bias training in 2014. Additional progress this year: • DisabledGo access reports driving improvements to disabled facilities • Hate Crime campaign with Merseyside Police to raise awareness and reporting • Further promotion campaigns • Promotion of employment opportunities in the community • Appointed to the national Equality and Diversity Council • Improvements to interpreting and translation policy and procedures • Bronze award in the Employers Forum Network of Equality and Inclusion benchmarking exercise in respect of policy and practice for staff and patients across the nine protected characteristics under the Equality Act 2010 • Stonewall Health Equality Index top performer for second year running and seventh nationally for demonstrating how our services meet the needs of lesbian, gay and bisexual patients • Successful renewal of the Two Ticks positive about disabled people accreditation with the Department of Work and Pensions, for positive employment practice for disabled people. • Improved ranking in the Stonewall Workplace Equality index by 68 ranks, 119th out of 379 entrants 6 Our performance The table below highlights some of our key indicators, the majority of which are nationally mandated. Performance indicator 2012/13 performance. 2013/14 target 2013/14 performance MRSA bacteraemia (Trust attributable) Achieved 0 8 Clostridium Difficile (Trust attributable) Achieved 35 51 Cancelled operations (on day of surgery for non medical reasons) Achieved 0.6% 0.47% Cancelled operations (patients not treated within 28 days following cancellation) Achieved 0% 0.4% Referral to treatment targets (% within 18 weeks). This has three components specific to the patient’s pathway. Achieved Monthly achievement all 3 components Achieved throughout 2013/14 Cancer: 31-day wait from diagnosis to first treatment Achieved 96% Achieved all quarters Cancer: 31-day wait for second or subsequent treatment - surgery - anti-cancer drug treatments Achieved Achieved 94% 98% Achieved all quarters Cancer: 62-day wait for first treatment - from urgent GP referral - from consultant screening service referral Achieved Achieved 85% 90% Achieved both components for all quarters Cancer: two week wait from referral to date first seen (urgent GP suspected cancer referrals and symptomatic breast patients) Achieved 93% Achieved all quarters Emergency Department waiting times within 4 hours Achieved 95% 94.1% Delayed Transfers of Care Achieved 2.1% 1.35% Percentage of patients admitted with stroke spending at least 90% of their stay on a stroke unit Achieved 80% 90.8% Venous Thromboembolism (VTE) Risk Assessment Achieved Monthly achievement of 90% Below target since September 2013 For all performance elements not met this year the Trust has clear actions agreed to deliver improvements. 7 Summary of national patient survey programme This year we have had results from two surveys, one that reviewed the experience of our patients who were in hospital for at least one night and one from our patients who attended the hospital for cancer care and treatment. National Inpatient Survey key findings There are ten sections in the national inpatient survey and the table below highlights where our trust was rated in comparison with the national average. There are no areas where the Trust was rated worse than other Trusts and one area that we were rated as better than other Trusts. Overall the change from the 2012 survey has not shown any significant changes. 8 Section 1: Emergency Department There were improvements, with more patients feeling they had been given the right amount of information and more patients feeding back that they were treated with dignity and respect whilst they were in our Emergency Department. Section 2: Waiting list or planned admission There was some improvement across all questions for the second year in a row. This indicates that our patients are increasingly being offered choice of where to have their first hospital appointment and that the hospital is less likely to change admissions dates. In two of the questions, we performed better than the best performing trusts. Section 3 and 4: Hospital and ward In relation to waiting for a bed and ward, we were well within the average range. There was some improvement in relation to cleanliness, which has been consistently high for a number of years and in relation to patients being given the opportunity to choose their food. We need to make improvements to the quality of our food as this is consistently lower despite changes to our meal service. This year we will undertake some more in depth work to understand this in more detail. Section 5 and 6: Doctors and nurses There has been a very small decline in positive responses here for all questions however we remain in the higher range of average for other Trusts. Section 7: Care and treatment Patients report that they have enough privacy when being examined or treated. Overall there has been a small decline, though we performed about the same as other Trusts, across the remaining questions in this section. There was a small decline in the number of patients feeling they have someone to talk to about their worries or fears, we will review this. Section 8: Operations and procedures The Trust reported better than the best performing trusts in explaining to patients after their operation or procedure how things had gone. The remaining questions were about the same as the best performing trusts. Section 9: Leaving hospital We performed the same as the best performing Trust in this area and better on one question about receiving printed information about medications. Section 10: Overall There needs to be improvement in how our patients feel they can give their views and understand how to raise a complaint. On the whole our patients rate us the same as the best performing hospitals in relation to their overall experience. In moving forward we have agreed our priorities for improvement from the national survey in 2013 and these are: 1.Improving our patient’s mealtimes 2.Reviewing why patients don’t feel they can talk to staff about worries and fears. We will monitor this at department level to highlight any trends so we can support improvements 3.We will continue to review how we can improve noise at night for patients and investigate new ways of working to ensure maximum rest is available 4.We will review pain management as our Trust surveys highlight that over 90% of our patients report that their pain is managed effectively. Our question is slightly different form the national inpatient survey in that we ask for a yes or no response. The reason for this is that we felt there was no in between with this and to expect someone to be content with pain only being managed some of the time is not our aspiration. In the national survey only 73% of our respondents said their pain was definitely managed well. 9 National Cancer Survey Key Findings 2013 Introduction The National Cancer Patient Survey was undertaken by the Quality Health and included patients who had been diagnosed with cancer and treated between 1 September 2013 and 30 November 2013. Patients were asked their opinion on every aspect of the cancer care they had received. This ranged from their first visit to the GP, to them receiving their treatment, and included questions on communication, compassion and support. Patients were also given the opportunity to add any additional information they felt was important. The survey included about 116,525 NHS patients who had 13 different types of cancer. 621 patients from this Trust were identified and sent a survey with 384 questionnaires completed and returned, giving a response rate of 64% compared to the national average of 68%. This response rate was down from 71% last year. Percentage Scores The questions in the cancer survey have been summarised as the percentage of patients who reported a positive experience. For example, ‘Percentage of patients who were given a complete explanation of their diagnostic tests’ and ‘Percentage of patients who said that nurses did not talk in front of them as if they were not there’. Neutral responses, such as ‘Don’t know’ and ‘I did not need an explanation’ are not included when computing the score. The Survey Outcome Report Overall the responses to the survey have shown an improvement on the previous year which helps to show the action plans put in place last year are working. There have been improvements in the question relating to improving communication with patients regarding diagnostic tests and in particular ‘staff explained completely what would be done during test’ . This question showed a statistically significant improvement in the previous year. Two other areas where there were statistically significant improvements were in reference to day case/out patients: – ‘Hospital staff definitely gave patients enough emotional support’ and ‘Doctors had the right notes and other documentation with them’. We maintained a 91% rating for ‘patients’ given name of the Clinical Nurse Specialist (CNS) in charge of their care’, and this is something that we aim to improve on and will continue to build on the action plan for this year. We improved on other areas of CNS contact, such as patients feeling they were being listened to by their CNS, which is testament to last year’s action plan. Other areas which have also shown an improvement from the previous year include: • • • • • • • • Patients given written information about the type of cancer they had Getting understandable answers to important questions all/almost all of the time Patient given a choice of different types of treatment Patients given written information about side effects Staff gave complete explanation of what would be done Given clear written information about what they should/should not do post discharge Staff told patient who to contact if worried after discharge GP given enough information about patient’s condition and treatment. We do however, need to improve on the support we offer for people with cancer. Staff need to improve the way information is passed on to patients, with regard to support groups and impact of cancer. We will include these into the action plan for the coming year. The completion of our new Well-being Centre should mean an improvement in this area. The action plan for this year will include a programme for training for ward nurses to facilitate their ability to answer questions and support cancer patients in their care. 10 The following action plan will be monitored and evaluated will enable the Trust to continue to move towards all answers in the green (top 20%). It focuses on the following areas: • To continue to improve communication with patients about their care and treatment • To continue improving patient’s experience of having a key worker / CNS • Improved quality of and access to, patient information for patients with a diagnosis of a rarer cancer • Improve ward staff knowledge and understanding of cancer. NHS Staff Survey 2013 ‘If a friend or relative needed treatment, I would be happy with the standard of care provided by this organisation’ Our Trust Results: 2012 = 66%, 2013 = 71%, national average 2013 = 64%. The NHS Staff Survey is an annual requirement of all NHS Trusts in England. Improving the staff survey results and staff engagement is a key priority. We opted to survey all staff rather than the required sample of about 850 staff for a Trust our size. Our response rate was 58%, 2% less than 2012. However, 3066 staff took part in the survey and the views of over 3000 staff are significant. The national average was 49% in 2013. Our ambition is to reach 70%, which we will strive for by excellent communication on why the survey is important and what we have done as a result, briefings, prizes and recognition for staff. The staff survey is an excellent indicator of progress on leadership and staff engagement. The overall staff engagement score is better than 2012 and average compared to other Trusts. There are four questions which make up the combined response for “would you recommend the Trust as a place to work or receive treatment”, and we have seen improvement in every question from 2012, and when compared to other similar trusts. The staff survey results demonstrate that where we have focused attention through staff engagement, results have improved. For example, clear planned goals (up 3%), staff able to make suggestions to improve their area of work (up 4%) staff able make improvements happen in their place of work (up 3%), receive recognition for good work (up 4%) satisfied with amount of responsibility (up 2%), staff feeling valued by the Trust (up 3%), recommend Trust as a good place to work (up 6%). Whilst we have areas we would like to improve, e.g. appraisal uptake, hand washing, reporting errors, near misses and incidents, the staff survey results provide valid and reliable evidence to demonstrate that staff engagement is having a significant impact on the well-being of staff. We plan to build on this during the next year by improving how we recognise and reward staff. Staff Engagement We have built on existing staff engagement work and implemented a new model ‘Going Local – Six Steps to the Stars’ where divisions and corporate teams are empowered to implement their own ideas and solutions to improving services for patients, their families and for themselves. Great ideas include improved team working and local expectations of each other, new ways of working in the storage and retrieval of case notes, and streamlined processes between sterile services and the Dental Hospital leading to a faster turnaround. This year, we are using ‘big conversation’ listening events, to address key issues and learning for the Trust such as learning from Operation ‘Fresh Start’, which was a Trust wide strategic initiative to look at how we can work differently to support timely, safe, effective discharge planning. We have reviewed our reporting culture for incidents, errors and near misses, and within teams to address local cultures and behaviours. 11 Staff are kept up to date on staff engagement progress with items at Team Brief and local briefings in their own workplace on issues which matter to them. Articles are included in the staff newsletter Insight and our Staff Awards recognises those staff who have made a difference to patient care and services and impacted on the working lives of staff. We will improve on the spread of reward and recognition for staff this year through divisional-led local celebrations of achievement, and through our new ‘Share and Learn’ quarterly celebration events. Spread and adoption of listening to staff and supporting them to take action on their ideas is critical to success as we move towards our new hospital. Transforming our services also requires us to transform how we recruit, appraise and develop our staff, together with how we utilise their skills and talents to create the fit for purpose workforce our patients and their families need and our staff deserve as a valued and motivated member of their team. 12 Local hospital patient surveys Patient feedback is very important to us in helping to identify where we are doing well, but more importantly those areas our patients feel we could improve upon. Each month our volunteers visit each ward and use a questionnaire with our patients to record their experiences. There are number of areas that we focus on and these include: • Areas where we as an organisation feel we need to improve • Mandatory questions such as the Friends and Family Test • Areas where our national survey highlights the need for improvement. These will be discussed in more detail in our review of 2013-14 priorities. Rating your experience in our Hospital One of the questions we ask our patients is how they would rate the care they receive in hospital. We report the percentage of patients who report that they had Good, Very Good or Excellent experiences. Over 12 months, we surveyed 4661 patients and the overwhelming majority report a good to excellent experience with 81.92% of patients rating very good or excellent. Every month we review our care on the wards or departments where a patient reports either a fair or poor experience to assess if there are any trends that we need to address. These areas are identified in our monthly quality performance report and staff are then able to respond to this. 13 Benchmarking data The Department of Health has asked that in our Quality Account we share information on a core set of indicators. All trusts are required to report against these indicators using a standard format. The following data is made available to National Health Service trusts and NHS foundation trusts by the Health and Social Care Information Centre. In all benchmarks we have used the latest data available from the centre. Patient Reported Outcome Measures (PROMS) PROMS are a series of measures recorded by patients’ before and after their operation that measure how their quality of life and health outcomes have improved following their surgery. The data below helps us to understand how well we are performing against our peers. We then use this information to plan how improvements. This is discussed and monitored in the division of surgery’s performance meetings. There are two types of standard measures EQ-5D and EQ-Vas explained below and some areas have condition specific measures. EQ-5D looks at five areas; mobility, self-care, usual activities, pain/discomfort and anxiety/depression, with questions that ask the patient to score themselves on three levels; these are no problems, some problem or severe problems. Formulas are added to produce a score with one being the best. EQ-VAS is line marked from 0-100, 0 being the worst health state and 100 being the best. The patient is asked to mark a point in the line to indicate how they feel about their state of health. We report PROMS measures scores for (i) groin hernia surgery, (ii) varicose vein surgery, (iii) hip replacement surgery, and (iv) knee replacement surgery, during the reporting period. PROMS reporting period: 1 April 2011 to 31 March 2012 PROMS reporting period: 1st April 2012 to 31st March 2013 We do not have a national benchmark for the PROMS indicators. The current PROMS data we receive monthly indicates we are within expected limits for hernia, knee replacement and hip replacement. Varicose vein procedures are no longer performed at our hospitals. We are working to improve the outcome for hip replacements, particularly with regard to EQ-5D (measuring health outcomes form a patient’s perspective) as results have been poor in the past but have shown improvement in the data available for March 2013 to September 2013. 14 Patient Safety Incidents This section reports the number and rate of patient safety incidents reported within the Trust during the reporting period, together with the number and percentage of such patient safety incidents that resulted in severe harm or death. Our performance is compared against similar NHS trusts. 1st October 2012 to 31st March 2013 1 April 2013 to 30 September 2013 Please note that at the time of publishing this account national averages had not been made available. We acknowledge incident reporting is below the national average and we are working on improving our reporting culture. There have been delays in reporting incidents to the National Reporting and Learning System (NRLS) we are slightly over (by 5 days) the national average of 30 days. We are taking the following actions to further improve our reporting arrangements: • Reviewing our incident category and sub categories in order to ensure all patient safety incidents are reported correctly to the NRLS. • Improving the timelines of uploading data to the NRLS on a monthly basis, no later than 30 days after the incident. • The degree of harm in the Trust is below the national average. The National Patient Safety Agency (NPSA) reports that not all organisations apply the national coding of degree of harm in a consistent way. We report all patient safety incidents based on the degree of actual harm caused. • We have a system in place where divisions share lessons learned on a quarterly basis and we have introduced a weekly meeting to review/ events that resulted in harm and to review no harm/near misses to identify themes. We communicate key messages to all staff to learn from incidents. 15 Venous Thromboembolism (VTE) Venous Thrombo-Embolism (VTE) is the formation of a blood clot in a vein (venous thrombosis), which can dislodge from its site of origin. Most thrombi (clots) occur in the deep veins of the legs and result in Deep Vein Thrombosis (DVT). Dislodged thrombi may travel to the lungs and cause a Pulmonary Embolus (PE). (National Institute for Health and Clinical Excellence, Clinical Guideline 46, (April 2007) This section reports the percentage of patients who were admitted to hospital and who were risk assessed for venous thromboembolism during the reporting period. Trust performance 2013/2014 VTE monthly performance Please note that in 2013 the Trust commissioned an external review of our data collection methods for VTE assessment. This was due to anecdotal evidence suggesting our methods could be strengthened. The Trust has now moved to a full electronic data collection method to ensure complete transparency and consistence. Our local CQUIN target for 2012/13 was that 90% of patients should have a VTE risk assessment on admission and we did meet this target. Our CQUIN target for 2013/14 was that 95% of patients should have this assessment on admission and we did not achieve this using the new electronic model. We did however, achieve over 90% compliance and aim to improve this figure for 2014/15. For 2013-2014 the rate is currently at 93.7% (May 2014). 16 Clostridium Difficile (CDT) This section reports the rate per 100,000 bed days of cases of CDT infection reported amongst patients aged two or over during the reporting period. New cases of CDT infection identified are reported directly to the infection prevention and control team who co-ordinate investigations, care and mandatory reporting via a dedicated database to Health Protection England (formerly Health Protection Agency). This information is shared with and further checked by our clinical information department to ensure it is accurate. We have taken the following actions to improve this rate and so the quality of its services by strengthening collaborative links between local hospitals and community teams. In addition, we are continuing to develop links between the infection prevention and control team and the University of Liverpool team conducting CDT research to improve care. We are focusing on identifying patients at risk of CDT infection and a focus on preventing other infections which may result in patients requiring antibiotic treatment. Some of the other improvements we have introduced are: • Prompt identification and isolation of patients with CDT infection supported by a specialist infectious disease team • Close working relationship between infection prevention and control, hotel services and domestic contractors to ensure high standards of cleanliness including thorough cleaning when patients are discharged • Formal root cause (RCA) analyses to identify areas for improvement including antibiotic prescribing • Monthly antimicrobial prevalence audits • Improved consultant engagement at RCA meetings. Mortality The next chart is our Standard Hospital Mortality Index (SHMI) which excludes palliative (patients who are dying) care coding comparing our performance to other acute Trusts in the North West. The Summary Hospital-level Mortality Indicator (SHMI) is an indicator which reports on mortality at trust level across the NHS in England using a standard and transparent methodology. It is produced and published quarterly as an experimental official statistic by the Health and Social Care Information Centre (HSCIC) with the first publication in October 2011. The SHMI is the ratio between the actual number of patients who die following hospitalisation at the trust and the number that would be expected to die on the basis of average England figures, given the characteristics of the patients treated there. Our SHMI currently stands at 1.07 which is the average for the region. It is lower than our closest neighbour Aintree University Hospital Foundation Trust which serves a similar population. 17 The SHMI has fluctuated since 2010 when we first began to report it. The most recent quarterly figure is 1.03. (Dr Foster: Mortality comparator until June 2013). We currently only one period report for this information The Royal Liverpool and Broadgreen University Hospitals NHS Trust considers that this data is as described for the following reasons. The Trust value was 1.07 which is within the expected range. The SHMI includes deaths up to 30 days after discharge and does not include any correction for social deprivation and other factors. It is notable that out of 22 acute trusts in the North West only three have an SHMI of 1.00. Our mortality rates are better than our neighbouring acute trust. The Royal Liverpool and Broadgreen University Hospitals NHS Trust has taken the following action to improve care and safety of our services by establishing processes to report mortality alerts identified using Dr Foster systems for any diagnosis or procedure on a quarterly basis to the Trust Medical Director. These alerts are reviewed by our medical director and patient safety leads and independently by the Trust audit leads, to determine the best course of action, such as case note audits or coding investigations. These have been reviewed by Clinical Coding, Data Quality and the clinical teams. Palliative Care Coding The percentage of patient deaths with palliative care coded at either diagnosis or specialty level for the trust for the reporting period is reported below. It is important for trust to identify the level of palliative care coding as some Trusts may care for a higher number of patients who are at the end of their life and therefore death is not unexpected. In year, data from Dr Foster showed we had an increase in palliative care coding between 2008 and 2012 at a greater rate than the national norm. A thorough review of coding for palliative care episodes was undertaken by the specialist palliative care team and our qualified clinical coding staff to ensure our best practice meets national standards. Our coding always represents what has been written by clinicians in the notes and is not changed retrospectively by clinicians. The review concluded, as with other Trusts who provide access to specialist palliative care services to an increasing population, that our palliative care coding is an accurate reflection of palliative care activity and does not impact inappropriately on the reporting of mortality. 18 Readmissions This section reports the percentage of patients aged — 15 or over, readmitted to a hospital which forms part of the trust within 28 days of being discharged from a hospital, which forms part of the trust during the reporting period. The Trust does not report re-admission data for 0-14 years as it is unlikely that patients in this age group are re-admitted following discharge. We have compared ourselves against similar trusts. The 2012-13 data was not available at the time of publishing this account. Actions taken We have developed a strategy to reduce readmissions. A steering group was established in 2012 and work began in identifying the key areas to focus on 2012/13. We have seen a reduction in readmissions in 2012, which is not highlighted within this specific data. For 2013 -14 a target of 50% for some speciality specific conditions has been. Patient Experience This section reports the Trust’s responsiveness to the personal needs of its patients during the reporting period. The data is based on the number of complaints received. The lower the score the better. The comparison of the highest and lowest performing trusts is within the North West. This data is presented in this manner so that Trusts can assess how we can perform alongside other Trusts. We can then use this information to deliver improvements. A full action plan is in place and monitored by the patient experience group and the quality governance committee. NB: Highest/Lowest is of all English Trusts. Our Trust is ranking higher than the national average however we have focussed on ensuring our patients are able to raise their concerns and welcome the opportunity to utilise feedback for improvement. 19 How we did against our 2013/2014 priorities Goal 1: Reducing Mortality: We will implement robust systems to improve mortality and improve patient outcomes Aim: Implementation of systems to support reduction in mortality Priorities 2013-14 a) To improve recognition, escalation and management of the deteriorating by a 10% reduction in cardiac arrest calls and increase by 10% calls to our Acute Response Team (ART) b) Improve sepsis recognition and response with increased calls to the ART team. Outcome: On Track Achieving a reduction of mortality is a three year plan and each year there are a number of priorities. This year we have made excellent progress in relation to ensuring we reduce mortality but work is on-going. For each of our goals outlined above a short summary of progress made will be provided below. Mortality benchmarking is provided in more detail in the benchmarking section of this report. We have undertaken a review of patient safety in 2013-14 and has introduced the new ‘Mortality and Patient Safety’ Sub Committee (MAPS) where all aspects of mortality and patient safety will be monitored. Progress made in 2013-14 includes: - Appointment of a consultant clinical patient safety lead and operational lead to support the patient safety - Lead advanced nurse practitioner supporting operational delivery of sepsis management - Compliance audits to be led by the Acute Response Team (ART). Proforma developed to support identification, and to guide diagnosis and treatment - Simulation training and human factors training course implemented. Sepsis recognition and surviving sepsis guidance - Implementation of Medical Microbiology and Infectious Disease consultant led ward rounds - Re-launch of the Surviving Sepsis project under development, across both emergency and inpatient areas, coordinated by patient safety leads, Intensive Therapy Unit (ITU) leads, Mortality and Patient Safety Sub Committee (MAPS) steering group and Acute Response Team. 20 Priority A - Recognising and managing deteriorating patients There has been a 9.73% increase in the number of calls made to our Acute Response team in 2013-14 which is an indication our deteriorating patients are being identified sooner. In relation to the reduction in cardiac arrest calls this has not been achieved. The graph opposite demonstrates whilst there was a slight rise in the % of cardiac arrests in 2013 compared with 2012 there is a larger decrease compared with 2011. Although we have not met our aim to reduce cardiac arrest calls by 10% there has not been a decrease in performance overall. It may also be an indicator that we have seen many more patients being admitted extremely unwell. 21 National Comparison NCAA quarterly report: 17- Mar-14 (Date range = 01-Apr-13 to 31-Dec-13) The graph above which illustrates where our organisation sits in relation to the rest of the country. We may have had slightly more cardiac arrests than the previous year but according to the National Cardiac Arrest Audit (NCAA) the number of individuals who had a cardiac arrest and were discharged from hospital was virtually the same as those predicted to survive to discharge by NCAA. (Please note the data above has been risk adjusted by NCAA) Priority B - Improve Sepsis Recognition and response What we have achieved: During 2013, we have strengthened the processes implemented in 2012, they included: • Increasing the number of case note reviews performed following a cardiac arrest. (94% of patients suffering a cardiac arrest had their case notes reviewed during 2013) • The above reviews are now reported weekly where lessons learned and additional measures are implemented where necessary in real time • A preliminary review of our Track and Trigger system has resulted in our senior doctors being informed earlier of patients who are showing signs of deteriorating. An in-depth review is taking place, which will result in significant changes in the way we detect, record and escalate patients who are showing signs of deterioration. 22 Next steps Our next steps during 2014/15 are • Implement the National Early Warning System (NEWS) • Complete an in depth review of the way in which our organisation responds to the deteriorating patient • Develop an implementation strategy for an electronic Track and trigger system • Ensure resuscitation attempts within the organisation are appropriate • Improve the quality of data supplied to the National Cardiac Arrest Audit which in turn will provide a rich and accurate source of information. 23 Goal 2 – Reduction of Avoidable Harm to our Patients Aim Reduction of avoidable harm to patients Priorities 2013-14 a) To reduce harm across a range of indicators. b) Improving dementia care for patients over 70 in line with the National Dementia Strategy c) Improving our discharge processes and communication with GPs. 90% of inpatients will have their discharge communicated to GPs within 24 hours. Outcome: On Track As part of the overall plan to reduce harm to patients we set some clear objectives as part of a three year strategy. Progress has been made in most of the priority areas. However, there are some elements that require on going focus. Priority A: Reducing harm across a range of indicators The priorities within this section are: • To reduce grade 2-4 Hospital Acquired Pressure Ulcers (also known as bed sores). • Reducing harm from falls • Reducing Catheter Associated Urinary Tract Infections (CAUTIs) • Venous Thromboembolisms (VTEs) and completion of root cause analysis (RCAs). Tissue Viability – reduce hospital acquired pressure ulcers to no more than 0.30% average per month/ aim for Zero Grade 3 and 4 pressure ulcers. Although we achieved our plan to have no more than an average rate of 0.30% grade 2- 4 hospital acquired pressure ulcers in 2013-14, we did not meet our Zero target for Grade 3 and 4 Hospital acquired pressure ulcers. These pressure ulcers are seen as deep tissue damage to the skin which is why we set a zero target. We will continue to review this in the next year. 24 Reducing harm from falls – in previous years we focused on reducing falls, whilst we still monitor this we recognise that it is important to focus more on the reduction of harm. There has been some fluctuation in the number of moderate to severe harms reported but a small downward trend noted. Every moderate to severe harm is fully reviewed to ensure everything possible has been done to reduce risk and that lessons learned are shared with staff. Catheter Associated Infection (CAUTIs) – our aim was to report no more than a rate of 0.6% and this has been met each month. Venous Thrombo-Embolic Events (Blood clots) – our target this year was to ensure every patient who developed a blood clot in hospital had their case fully reviewed to ensure we were picking up any lessons learned. This process is in place and now electronic, which supports improved reporting. Quarterly reports have been taken to patient safety meetings to ensure lessons are learned. The Mortality and Patient Safety Sub Committee (MAPS) will monitor and report these outcomes for 2014-2015 Priority B: Improving dementia care for patients over 70 in line with the national dementia strategy The focus this year was to • Ensure patients admitted over 75 are screened for any risk factors that may indicate dementia • Ensure the right tests are taken to diagnose Dementia and then refer patients to specialist centres for diagnosis and on going care • Raise awareness of dementia and provide a wide range of educational programmes that will equip our staff to manage and support patients and their families. 25 Screening and diagnosis There has been an extensive amount of work undertaken with our staff to ensure they fully understand the importance of completing the initial screening so that we could identify patients who may need extra support. Although we have made real progress we have not achieved the 90% performance indicator. Training and raising awareness Currently over 1000 staff completed training utilising Power Point presentation, SCIE Dementia Gateway and Higher education (University courses). All staff groups have been trained and this will continue. There have been a number of consultation events to obtain feedback from families and carers about what they need. We expect to continue to deliver improvements though our revised Dementia Strategy and the strategic Dementia Steering group. Priority C: Improving our discharge processes and communication with GPs. 90% of patients will have their discharge communicated to GPs within 24 hours (inpatient areas) This performance element will be reported as part of the CQUINs overview. 26 Goal 3: That more than 75% of patients will recommend this hospital to a family member or friend Aims: Patients will feel respected and treated with dignity, they will feel involved in their care and supported in preparing for discharge Priority areas 2013-14 a) 95% or more of our patients will report that they were treated with respect and dignity b) To ensure that 95% of our patients report that their pain is managed effectively. c) Over 80% of our patients will report that they were involved in their discharge planning d) 95% of our patients will report that their medications have been provided in a timely manner and fully explained e) To establish daily senior doctor reviews in all wards to lead safe on-going care and effective discharge plans. Outcome: On track. As part of our three year plan to improve patient experience we are aiming for 75% of our patients to rate extremely likely to recommend our hospital to friends and family. Patient feedback is the most important indicator of how well an organisation is doing. We undertake regular feedback surveys with our patients in a variety of ways. The introduction of the friends and family test last year gave us an opportunity to understand in more detail how patients were feeling about their experience. To help improve our friends and family test rating we decided to focus on the five priorities outlined above. Friends and family results 2013-14 We did not achieve a rating of 75% of patients recommending this hospital to friends and family in year one so remain focussed on delivering this by the end of 2014-15. We did see an improvement in year with up to 53% of patients saying they were extremely likely to recommend this hospital to family members or friends. Responses: Each month there was an average of 82% of patients who said they were either extremely likely or likely to recommend the hospital and our inpatient surveys found that consistently patients felt treated with dignity and respect. Our overall net promoter score has returned a maximum rating of 53% with an average of 50.3% over the year. 27 Overall Patient Feedback: The chart below highlights results in relation to priorities A-D above. On the whole we have achieved really good feedback for all questions. These are based on surveys undertaken on a monthly basis by our volunteers and represent feedback from 1461 patients in 2013-14. Implementation of Daily Consultant Reviews We have made significant progress in ensuring that patients are reviewed daily by a consultant to ensure safe and effective discharge planning seven days a week. Over the next 12 months we will continue to ensure this happens on all wards. 28 Review of quality performance: Safety Subject Matter: Patient Safety: reducing risk in Gastroenterology Aim: Early detection and prevention of C.diff in the ward area Goal: No CDT on ward area that could have been prevented Outcome: Outcome Met In the Gastroenterology and Hepatology wards there was a significant increase in the number of C.diff cases identified in 2013. There were two peaks on one of the wards in July and the second peak on the other ward in October. All incidences of C.diff are thoroughly reviewed by the infection prevention and control team alongside the ward nursing, medical and pharmacy staff. After the first peak in July, improvements were put in place and lessons learned were shared with staff to reduce risk. Areas that were looked at as part of the whole team review included: • The environment • Increased environmental monitoring • The provision of an additional isolation room by converting an office • The skills of staff • The prescribing of antibiotics (as certain antibiotics can increase the chance of developing C.diff) • Antibiotic prevalence audits • Testing patients with symptoms of diarrhoea as soon as possible to reduce the risk of contact with other patients. The matron for the ward area at the time also decided to look at other issues with her team such as: • The matron attending the acute medical admission unit (AMAU) every morning to identify gastroenterology patients and review them. If a patient is admitted with loose stools (diarrhoea) then a a sample of the patients stool is taken prior to transfer to the ward. A side room is identified for high risk patients, and discussion undertaken with the patient to ensure they understand the risk of cross infection and the importance of washing hands amongst other factors • All planned admissions (these are patients we know are being admitted from home for a particular reason, so we have more time to plan their admission) are assessed by the matron and allocated a side room if necessary. The team also reviewed the admission pathways and looked at how they could reduce any chance of cross contamination (where one patient may come into contact with another and cause infection) and changed how they plan and admit certain patients and where they are located across the two wards. 29 This has helped to reduce the movement of patients across the two wards and has contributed to the zero cases since the last peak in October. It is really important to ensure we ‘think outside the box’ at every opportunity and never assume ‘there is nothing else we can do. The team in Gastroenterology alongside our Infection prevention and control team did just that and the results so far seem to indicate that it works. 30 Review of quality performance: Saftey Abdominal Aortic Aneurysm (AAA) Screening Programme Aim: The Abdominal Aortic Aneurysm (AAA) Screening programme aims to reduce AAA related mortality by providing a systematic population-based screening programme for the male population during their 65th year and, on request, for men over 65 Goal: To introduce an AAA screening service across Cheshire and Merseyside by 1 April 2014 Outcome met - a screening programme is now in place in Cheshire and Merseyside What is Abdominal Aortic Aneurysm Screening? Ultrasound screening in the community for aortic aneurysm is offered to all men registered with an NHS GP shortly after their 65th birthday, but older men can volunteer for a scan. This is a free programme, funded by the NHS. The ultrasound scan is done in community venues and measures the width of the aorta (a large blood vessel in the abdomen). Ruptured abdominal aortic aneurysm deaths account for 2.1% of all deaths in men aged 65 and over. This compares with 0.8% in women of the same age group. The mortality from rupture is high, with nearly a third dying in the community before reaching hospital. Of those who undergo AAA emergency surgery, the post-operative mortality rate is around 50%, making the fatality rateafter rupture 82%. This compares with a post-operative mortality rate in high quality vascular services of 3-8% following planned surgery. How have we done this year? In 2013/14 we have: • Established 20 screening locations across Cheshire and Merseyside • Invited nearly 6,000 men for an appointment of which 4700 attended for screening • Referred six men for assessment for life saving surgery • 130 men are being followed up with repeat scans (surveillance) • Formed a partnership with Everton Football Club and Radio Merseyside to promote the service leading to 500 self-referrals • Been the pilot site for the AAA image storage software • Reduced failed appointments [DNAs] in clinics from 36% to 15% • Improved experience for patients by moving clinics to locations with better access. 31 Targets for 2014/15 • To invite 16000 men for screening appointments during this year • To further promote the service by joining the healthy stadia initiative in sports venues in St Helens, Tranmere, Warrington and Widnes • To increase patient participation within the programme. The programme’s activity is overseen by a Programme Board, consisting of public health commissioners, quality assurance leads, a vascular surgeon from another hospital, Arrowe Park Hospital and a patient representative (who had an AAA identified and repaired by the service). 32 Review of quality performance: Effectiveness Telemedicine Stroke Thrombolysis Service Aim: Improve ‘door to needle’ times in Stroke Thrombolysis Goal: To thrombolyse over 80% of patients presenting out of hours within one hour of arrival Outcome: Outcome Met Thrombolysis is a clot busting treatment to break down the acute blockages in the brain’s blood vessel which cause strokes. One million brain cells are damaged for every minute thrombolysis is delayed. International guidelines suggest 80% of patients should be thrombolysed within one hour of hospital arrival. In 2012 30% of Stroke patients presenting out of hours were thrombolysed within one hour of arrival. In April 2013 the Stroke Service launched an innovative telemedicine videoconferencing system to facilitate out of hours thrombolysis. This reduces transit time for the on call consultants, improves productivity and streamlines the thrombolysis process. In the last three months to April 2014, 100% of patients receiving thrombolysis have done so in less than an hour. Patient and carer feedback regarding the telemedicine system has been universally positive. Thrombolysis performance data is reviewed on a weekly basis and benchmarked against national Stroke Audit data. Having surpassed the target of thrombolysing over 80% of patients within one hour of arrival, the Stroke Service now aims to further improve quality and outcomes by reducing the average door to needle time further. Dr Paul Fitzsimmons [near the screen] Clinical Director for Gerontology and Stroke 33 Review of quality performance: Effectiveness Bone Marrow Transplant Services JACIE Accreditation Aim: Improving service effectiveness through accreditation compliance Goal: To achieve accreditation with the Joint Accreditation Committee Europe Outcome: Outcome Met We provide a Bone Marrow Transplant (BMT) service to patients across the North West and further afield. All BMT services must be accredited through the Joint Accreditation Committee Europe (JACIE). This is a non-profit body that was established in 1998 for the purpose of assessment and accreditation in the field of Haematopoietic Stem Cell Transplantation (HSCT). Its primary aim is to promote high-quality patient care and laboratory performance in haemopoietic stem cell collection and processing (EBMT 2012). In order to achieve accreditation, the transplant centre has to demonstrate high-quality performance and service excellence. The Transplant Unit spent 18 months preparing for submission of their evidence to demonstrate that we provide services and care to the required standard. This involved reviewing all aspects of clinical practice and developing standard operating procedures to ensure all essential aspects of quality are adhered to. These standard operating procedures are reviewed annually to ensure they remain compliant with up-to date practice. The JACIE standards are very clear about the level of qualifications and training that staff should have and that they should be trained in the procedures they regularly perform. Each member of staff undertaking procedures is assessed to ensure on- going competency and these assessments are recorded and held by the staff and their managers. Competency assessments were developed for both medical and nursing staff and this is supported by a wide range of teaching activities. What this means to our patients is assurance that staff are trained well, that there are the right levels of resources to provide a safe and effective service and that we are recognised as a centre of excellence. The transplant unit registered its submission to JACIE in May 2012 and was inspected in October 2013. The final report from the inspectors was received in February 2014. The programme achieved 100% compliance with all the standards and only minor recommendations were made. A response to these recommendations is being submitted in May 2014 and we hope to have our certificate of JACIE accreditation shortly after. Our Bone Marrow Transplant Team 34 Review of quality performance: Effectiveness Pain Management Services Aim: To reduce the outpatient waiting times and also develop a multi-disciplinary approach in the management of acute and chronic pain services. Goal: To improve both the patient’s experience and well-being. Outcome: Outcome Met We received 34% of all new pain management referrals in Merseyside, - 2,020 new referrals in 2013/14 and 16% of all patients with chronic pain attend our Emergency department. We have, in partnership, with Liverpool Clinical Commissioning Group developed a plan to increase our capacity, nonrecurrently, for new patient referrals to reduce the waiting time. This was successful in reducing the waiting time from 34 weeks in July 2013 to four weeks in April 2014. We are implementing a multi-disciplinary team for pain management services. This development will significantly improve patient experience and on-going clinical management which also achieves the National Pain Audits standards for the delivery of pain services. In addition, we will also implement hot clinics for patients to provide rapid access following, or avoiding Emergency Department attendances. We will also hold multi-disciplinary ward rounds for patients who are inpatients with acute or chronic pain. We will be working in partnership with Liverpool Clinical Commissioning Group to implement a pilot community pain management service and the aim of this is to ensure a seamless service from the acute, chronic and community services. We continue to work in partnership with Liverpool Commissioning Group, as well as implementing the business plan to develop the multi-disciplinary service in 2014/15. 35 Review of quality performance: Experience Improving experience for patients with Alcoholic Liver Disease Aim: To provide a clear pathway for patients with Alcoholic Liver Disease Goal: To reduce unnecessary hospital admission Outcome: Outcome Met In 2010, a joint position paper on behalf of British Society of Gastroenterology, the Alcohol Health Alliance UK, and the British Association for Study of the Liver highlighted that the most deprived lifestyle groups have up-to 15 times greater alcohol specific mortality and up to 10 times greater alcohol specific admissions to hospital. It therefore recommended that hospitals should develop a multidisciplinary approach to the care and management of people attending or admitted to hospital with an alcohol-related cause. We reviewed this guidance and reviewed all patients attending the Emergency Department or admitted to the hospital on more than six occasions in the previous six months. There was also a detailed review of three of our patients who were the most frequent attenders to our Emergency Department. The team investigated the reason for admission including medical and social reasons. They then reviewed how many people, across a range of professions, were involved in their care, discharge planning and aftercare. There were discussions with patients to try and understand why they chose to come to hospital and what they felt could be provided as an alternative. This was followed by the development of an electronic early warning system ensured that any patient admitted to the hospital would be referred to the alcohol team. This then led to an integrated alcohol and hepatology (liver) consultant led multidisciplinary team (MDT). The impact of this work highlighted that patients with alcoholic liver disease were being supported by a large number of key workers from a variety of voluntary agencies, housing agencies, GPs, primary care alcohol specialist nurses, social workers, homeless outreach, and specialist medical consultants from Psychiatry to Hepatology. However, much of this work was happening in isolation and at times with no one person reviewing the patient’s pathway. Importantly, the patients were unclear where to go for what, and were often utilising the Emergency Department as a failsafe when they were unsure or troubled. By utilising the MDT approach we have been able to direct patients appropriately so they know where to go for help. This has resulted in a significant reduction in hospital attendance and admission for this small but significant group of patients. 36 Review of quality performance: Experience Enhanced Recovery Programme (ERP) within Hepato-Biliary Department Aim: Implementation of ERP principles with Hepato-Biliary (HPB) Goal: To improve patient experience and streamline patient pathway Outcome: Length of stay reduced from 23 days to 13 days Outcome Met The Enhanced Recovery Programme has previously been implemented as a national programme within several specialties but never within HPB. As this cohort of patients experience a long length of stay the idea was to streamline the service to improve patient experience and length of stay. We are the regional pancreatic unit for the North West and committed to continually improving our service. Although there was no evidence to support the implementation of the enhanced recovery principles within HPB, the team felt that these patients would benefit from these practices. From the outset, we focussed on the entire patient pathway so the project team consisted of members from all specialties involved in the patient’s treatment. We reviewed the current processes in place and devised a new more streamlined pathway along with the development on the Pancreatic Enhanced Recovery Unit (PERU). By implementing on PERU the following benefits were achieved: • Increased ratio of nurses to patients • Reduction in the usage of critical care beds • Patients more actively involved in their treatment plan from diagnosis • By having the same cohort of patients in one area they are able to encourage and motivate each other in their recovery. The changes are now being sustained and improved upon. The team has been recognised for the fantastic work and were awarded the Health Service Journal award for Acute Sector Innovation 2013. The team accepting their Health Service journal Award in 2013. 37 Review of quality performance: Experience End of Life Care Aim: To ensure that patients are treated with care and compassion at the end of life and that patient, their relatives and carers are supported in the last hours or days of life with a trained volunteer. Goal: To support all requests for a volunteer so that no patient dies alone Outcome: Outcome Met We have a specialist palliative care service that aims to respond to patient needs directly as needed and indirectly by support and education to a cohort of trained Palliative Care Network nurses. We may only get one opportunity to get this right for our patients providing safe care and a positive lasting memory for those left behind once a loved one has died. Our volunteer role has really enhanced the care we provide and consists of trained and competent volunteers. They can be called upon to sit with a patient at the end of life or to provide support to the family. This does not replace the nursing role in the hospital but enhances what we can do to get it right at this vital time for patients and their families. The CQC acknowledged the excellent end of life care service during our Chief Inspector of hospitals inspection in 2013. CQC Good practice example: Royal Liverpool University Hospital “The end of life care service at the Royal Liverpool University Hospital has introduced several innovative models of care……… They have also trained volunteers who will sit with patients who are dying if nursing staff are unable to do so………..” Next Steps To consolidate and develop our volunteer programme to be seven days a week and out of hours service within our quality governance framework. We continue to respond to patient needs and support our network nurses to achieve the optimum care and compassion at the end of life in line with the six fundamental values - care, compassion, competence, communication, courage and commitment (the 6Cs) that resonate strongly with both staff and people who use our services, as outlined in: Compassion in Practice, Nursing, Midwifery and Care Staff, Our Vision and Strategy December 2012. 38 Participation in Clinical Audit During 2013/14, 31 national clinical audits and three national confidential enquiries covered NHS services that the Royal Liverpool and Broadgreen University Hospitals NHS Trust provides. During that period we participated in 94% of national clinical audits and 100% of national confidential enquiries which it was eligible to participate in. The national clinical audits and national confidential enquiries that the Royal Liverpool and Broadgreen University Hospitals NHS Trust were eligible to participate in during 2013/14 can be viewed in Appendix 1. The reports of 16 national clinical audits were reviewed by the provider in 2013/14 and the Royal Liverpool and Broadgreen University Hospitals NHS Trust intends to take the following actions to improve the quality of healthcare provided: • Oxygen prescribing guidelines have been updated and disseminated across the Trust following the publication of the Emergency use of Oxygen Audit • All Heart Failure patients are to be referred to the heart failure specialist nurse following the National Heart Failure report • Improvement in the uptake of the pulmonary rehabilitation programme after the patient has been discharged. To address this, our Chronic Obstructive Pulmonary Disease (COPD) nurses and the rest of the team will ensure that suitable patients are referred for pulmonary rehabilitation. For the following it was felt that we achieved comparably or better than nationally and no actions were identified: • Fractured Neck of Femur • Myocardial Infarction National Audit Project (MINAP) • National Vascular Database – abdominal aortic aneurysm outcomes Stroke Improvement National Audit Project (SSNAP) includes the National Sentinel Stroke Audit. It should be noted the national reports reviewed during 2013/14 are not explicit to the list of audits in Appendix 1 but are, however, the reports published during 2013/14. Also of note is this figure is in regards to reports reviewed at the Trusts Clinical and Cost Effectiveness Sub-Committee The reports of 144 local clinical audits were reviewed by the provider in 2013/14 and examples of actions to be taken by the Trust to improve the quality of healthcare provided are as follows: • All patients 65 or above admitted to clinical gerontology will have a cognitive screen • Increased frequency of syringe driver observations • Diabetic foot clinic to be set up to improve management of diabetic foot ulcers 39 • A vitamin D decision aid has been developed to help rationalise the frequency of testing • To devise a specific algorthythm for investigation and management of hyperprolactinaemia - to improve the pathway for investigation of patients with hyerprolactinaemia. Engagement in clinical audits Submission in national audits increased by 3% during 2013/14 During 2013/14 the clinical audit database continued to be developed and is now able to monitor both the progress and actions from clinical audit much more robustly. Audit symposia were again held in all three divisions and cumulated in a Trustwide symposium where an overall winner was announced. The annual clinical audit poster competition was also held. In 2014 we will promote Clinical Audit Awareness week and activities held to raise awareness of clinical audit within the Trust. 40 Participation in clinical research The number of patients receiving NHS services provided or sub-contracted by the Royal Liverpool and Broadgreen University Hospitals NHS Trust in 2013-14 that were recruited during that period to participate in both National Institute for Health Research (NIHR) and non-NIHR supported research was well above the NIHR target for that year. NIHR patient accrual 2013-2014 The new Royal Liverpool University Hospital represents a crucial step toward the development of a health and life sciences campus on site developing new treatments through research and a hub for the future of health science research in the North West. Our Clinical Research Unit has maintained Phase I accreditation, the first NHS unit in England and Wales to do so, which means we carry out first in human clinical trials. This has led to a strategic alliance with COVANCE (a global commercial research company) for early phase studies (which are used to measure the safety and efficacy of an investigational new drug before it is marketed to the general public). The unit has conducted ten of these very early phase trials in the past two years. We have strong links with the University of Liverpool including, sponsorship of national and international studies. 41 Pancreatic Biomedical Research Unit Major areas of research Infectious Diseases Cancer Diabetes Pharmacology Gastroenterology Eye Dental At the end of the financial year (March 2013) we had 197 leading researchers working on 461 active research studies of which 209 have NIHR support. Our increasing level of participation in clinical research demonstrates our commitment to improving the quality of care provided and making a significant contribution to wider health improvement. We are keen for public involvement in research and now have patient representatives on our Governance and research, development and research executive committees. Consent4Consent in healthy volunteers has been a huge success, we have about 3000 people signed up to the database, and it is now rolled out to patients within the hospital, with many patients in multiple specialist areas indicating that they are happy to be contacted if there is a research study that they may be suitable for. We hope this will give all interested patients the chance to take part in research and make a real difference to the lives of others in the future. In 2013/14, RD&I has focused on the development and implementation of an Intellectual Property and Innovation Framework. This framework provides a structure for the adoption and diffusion of innovations across the divisions and the commercialisation and exploitation of Intellectual property should any be identified. RD&I is working closely with the Service Improvement Team and external partners as required. 2013/14 saw the development of Liverpool Health Partners, an organisation that encompasses partners from across Liverpool including higher education institutes, NHS Trusts and the Clinical ommissioning Groups. A cross cutting theme of the Liverpool Health Partner is the development of a Joint Research Office, a number of partners have participated in the Joint Research Office pilot programme, primary focus of this is streamlining and sharing of best practice. Last year our Quality Accounts stated that it would report the following data this year: • In 2013/14 we met the target to increase the numbers of patients taking part in clinical research • The number of new studies opened during 2013/14 was 137 and we will continue to monitor and report on studies completed during 2013/14 • We have made significant progress with the use of the model clinical trial agreement by external sponsors and can report 76% of commercial studies have used this form of contract in the last 12 months. 42 Commissioning for quality and innovation (CQUIN) framework The framework is designed to help produce a system which actively encourages organisations to focus and to stretch themselves on quality improvement and innovation. CQUINs in 2013-2014 A proportion of the Royal Liverpool and Broadgreen University Hospitals NHS Trust income in 2013/2014, (4.4 million) was conditional on achieving quality improvement and innovative goals agreed between Royal Liverpool and Broadgreen University Hospitals NHS Trust and Liverpool Clinical Commissioning Group, our main commissioner, for the provision of NHS services through the CQUIN payment framework. We have made some excellent progress with many of our CQUIN targets and we are committed to continue to deliver any that were underperforming in 2014-15. Some of these are discussed in the main body of the report. Further details of the agreed goals for 2013/2014 and for the following 12 month period are available electronically at our website www.rlbuht.nhs.uk or by writing to our chief nurse, Mrs Lisa Grant. 43 CQUINs Performance 2013-14 44 Data quality Information Governance Toolkit (IGT) Within the IGT there are six initiatives with 45 standards. The initiatives include information governance management, confidentiality and data protection assurance, information security assurance, clinical information assurance, secondary use assurance and corporate information assurance. Our Information Governance Assessment report overall score for 2013/14 was 82%, and was rated as satisfactory. The IGT is available on the Health and Social Care Information Centre website https://www.igt.hscic.gov.uk/ A sub-set of the Information Governance Toolkit scores are also used to monitor compliance with standards required for the NHS Operating Framework, the NHS Care Records Guarantee and the Statement of Compliance. The table illustrates the distribution of scores achieved with 20 of the 45 standards at level 3. Scores Level 0 Level 1 Level 2 Level 3 2013/14 0 0 25 20 2012/13 0 0 22 23 The annual audit carried out by Mersey Internal Audit Agency for the October submission of the IGT gave a ‘significant assurance’ rating, based on the scores recorded at that time, and on the assumption that evidential gaps would be completed in all standards before the end of March 2014. This has been completed. There have been a total of 43 incidents logged within this fiscal year with only 2 level 1 incidents logged, the remainder being logged as level 0. It should also be noted that the structure of the recording of incidents had changed within the year. Level 1 incidents: 1. 13 Electronic reports for clients from Liverpool John Moores University were sent and printed out by University of Liverpool Occupational Health department. 2. Monthly activity sheets containing 136 sets of staff data (name, date of birth, case/NHS number, date sample taken and date result available and investigation) were sent to the incorrect location. Information Quality Our information quality team continues to monitor and investigate any data quality issues that are identified on our electronic patient administration system to assist in the delivery of high quality, reliable data. The team continues to report a range of key performance indicators, which assist in the monitoring of quality, providing assurance to the organisation on a quarterly basis to our Board of Directors. 45 NHS number and general medical practice code validity The NHS Number is a unique number that identifies an individual patient and is used to support patient care. It can identify patients in systems locally and nationally and is also used for ensuring patients are treated safely and correctly. Using the NHS Number is an indicator of good data quality and underpins world class care whilst improving patient safety: We will be taking the following actions to improve data quality: • Quarterly data quality report containing key performance indicators are shared with our Board of Directors • Both internal and external audits assist in assuring us of the quality of data held about the care we have provided to patients • We meet with and work closely with our commissioners to provide assurances that the quality of data submitted to the Secondary Uses Service (SUS) is high. We submitted records during April 2013 to January 2014 to the SUS for inclusion in the Hospital Episode Statistics, which are included in the latest published data. The percentage of records in the published data which included the patient’s valid NHS number was: • 99.9% for admitted patient care • 100%% for outpatient care • 99.4% for emergency care High NHS Number coverage has been maintained over recent years, with marked improvement seen since 2009/10 as per the table below (data taken from the SUS published Data Quality dashboards). 46 The percentage of records in the published data which included the patient’s valid General Medical Practice Code was: • 100% for admitted patient care • 100% for outpatient care and • 100% for emergency care 47 Consultation on our Quality Account Patient feedback is important to us. Over the course of the year we have had several opportunities to discuss the Quality Account (internally and externally) and what quality means to our stakeholders. To prepare this year’s Quality Account and discuss progress against last year’s priorities, we have consulted with a wide range of staff and stakeholders. We also consulted on the Quality Account at international nurses day events so that staff from all three hospital sites had the opportunity to provide feedback. The proposals for this year’s Quality Account has also been discussed at our Quality Governance Committee and members were asked to speak to their staff and provide feedback or comments. In addition to this, members of our Quality Improvement Council, Patients’ Council, and Board of Directors have all had the opportunity to contribute to the development of the content of this year’s Account. External consultation has also been undertaken with the following committees/groups: • Liverpool Healthwatch • Knowsley Healthwatch • Sefton Overview and Scrutiny Committee • Liverpool Clinical Commissioning Group. 48 Priorities for improvement 2014/15 The trust has reviewed its own strategic themes and has agreed some priorities for 2014-15 and these will impact upon the quality goals set last year. We will produce a full Quality strategy for 2014-15 that will reflect the Trust strategic themes and align with the 2014-15 priorities. Within this quality account we will highlight how our priorities link into the Trust overall strategic plan. Our Vision Delivering the highest quality of healthcare driven by world class research for the health and wellbeing of the population Our Values Patient centered Professional Open and engaged Collaborative Creative Strategic themes a. To deliver an exceptional patient experience, making the Trust one of the most sought after places to be treated anywhere in the world b. To improve the quality of life for our patients by providing excellent, safe and accessible healthcare, which puts patient’s wellbeing at the heart of all we do c. To develop a world-class workforce, recognized for its skills and level of engagement and founded on a culture of achievement, education, training and development d. To achieve international recognition for our research and innovation, bringing new therapies from the bench to the bedside e. To play a lead role in the development of a sustainable health system for the communities we serve. Our priorities for 2014-15 The focus this year is to ensure we provide: 1. A 7 day service ( Supporting strategic themes, A, B, E) 2. A patient safety culture (Supporting Strategic Themes, A,B,D,E) 3. The Right Staffing levels (Supporting all strategic themes.) 4. A Learning organisation (Supporting all strategic themes) 5. The Journey to 2018 programme (Supporting all strategic themes). 49 Quality Account Priority 1: Reducing mortality - to embed robust systems to improve mortality rate and improve patient outcomes How will we do it? Reducing mortality links into the Trust priorities for this year and in particular will be supported by: • Developing strong 7 day a week services to ensure consultant level review • Ensuring we have a strong patient safety culture where every opportunity is taken to share lessons learned. There are robust processes in place for undertaking multi-disciplinary reviews of all patient deaths in the hospital and we are strengthening how we share those lessons learned. Focusing our priorities To support the on-going work to reduce mortality rates in the hospital we have agreed to focus on 2 distinct clinical pathways. We will also continue with the work which was started in 2013-14 and ensure this good work is embedded in the Trust and continuing to have the impact we need. The implementation of pathway driven care has already delivered some excellent results, for example in enhanced recovery. In terms of improving patient outcomes this is a proven method and so we will replicate this across some key areas. 2013 - 14 priorities Improve recognition, escalation and management of the deteriorating patient and deliver improvements. This will result in a year on year reduction by at least 10% in resuscitation calls and a 10% or more increase to the ART. Improve sepsis recognition and response as evidenced by increase in calls to the ART. Implement the pneumonia pathway and deliver 95% compliance unless agreed deviations are documented. 2014 - 15 priorities Implement the heart failure and pancreatic pathways and deliver 95% compliance unless there are agreed deviations documented. Develop and implement pathways for Leukaemia and Lymphoma. 2015 - 16 priorities Deliver zero healthcare associated infections. Deliver improved Modified Early Warning System (MEWS) escalation and further improvements in recognising the deteriorating patient. 50 Quality Account Priority 2: We will continue to deliver reduction in harm to patients How will we do it? Reducing harm to patients in the Trust is underpinned by the following Trust priorities for 2014-15: • Developing strong 7 day a week services to ensure consultant level review and access to diagnostics • Ensuring we have a strong patient safety culture where every opportunity is taken to share lessons learned • Ensuring we have the right staff to provide the right level of care for our patients. Developing a culture where learning from incidents and complaints as a matter of course was highlighted in a number of significant reports in 2013. Professor Don Berwick produced a report on safety in the NHS in August 2013 titled ‘A promise to learn a commitment to act’ and provided 10 key recommendations that Trust should take to address patient safety. This trust already has many of these in place and has a full action pan to deliver on any not currently in place. Focusing on our priorities There are a number of key priority areas in the next two years and these are outlined below. We will continue to collate information on the four harms within the patient safety thermometer(*): • Pressure ulcers • Falls with harm that is moderate to severe • Catheter associated urinary tract infections (CAUTI) • Venous thrombolytic embolism (VTE) including strengthening how we work together to understand preventable causes and share lessons learned • Achieve no less than 97% harm free hospital care. Efficiency of care is also an area we will continue to monitor as this will ensure reductions in delays that could result in harm to patients. The focus this year will be to review how effective we are at supporting patients to access services in a safe and timely manner. This will include waiting times to access care but also on how we are improving access to tests and investigations and the speed and accuracy of when results are available. Outpatient efficiency is also part of this target as it is essential our patients are able to access their appointment in a timely manner and to ensure they feel they have been able to access the care they needed. * The patient safety thermometer is a survey that is undertaken every month on every patient in hospital for at least one night. We record if any patients are admitted with any of the four harms and report on harm free care. This is submitted on a national database for comparison against other hospitals. 51 2013 - 14 priorities Improving dementia care for patients over 70 years old in line with the National Dementia Strategy. Improving our discharge processes and communication with GPs Focusing on the reduction of harm to patients across a range of indicators. Rolling out enhanced recovery in agreed pathways. Improve access to services: • Reduction of waiting times to be admitted to hospital 2014 - 15 priorities • Efficiency of outpatient consultations, to collate information on how long past an appointment time our patients are waiting to be seen in our top 10 areas where delays have been identified. All areas must deliver a 10% improvement in year with further stretch targets agreed for 2015-16 • Reduce cancellations of appointments by the Trust by 30% • Use of MEDWORX system (software package which identifies appropriate use of clinical beds) to identify delays in care for patients. Agree targets to reduce delays in outpatient appointments across the top 10 specialities and monitor implementation. Maintain focus on reduction of harm to patients. 2015 - 16 priorities Continue to work with stakeholders to anticipate patient care requirements in vulnerable groups for example: • Dementia • Learning disabilities • Transitional care. 52 Quality Account Priority 3: Delivering patient centred care, treating all patients with dignity and respect and obtaining feedback that more than 75% of patients would be extremely likely to recommend this Trust to a family member or friend How will we do it? The experience of our patients is the most important thing and this quality account priority will be supported by all five of the Trust overall priorities for 2014-15. We have already developed a means of ascertaining feedback from patients regarding how likely they are to recommend our hospital to a family member or a friend though response rates and results have not been as high as we would like so more work is underway to improve this. We report our patient experience feedback in our monthly quality performance report and this included the ‘Friends and Family Test’ where patients are asked to rate how likely they are to recommend our Trust to family or friends. Response categories are: 1.Extremely likely 2.Likely 3.Neither likely nor unlikely 4.Unlikely 5.Extremely unlikely 6.Don’t know. Focussing on our priorities We have identified a number of areas where improvements to the patient experience are required and these are highlighted below. Keeping patients fully informed and ensuring every patient feels that they have been treated with dignity and respect is key to ensuring patient centred care. Our patients have the right to access the right member of staff to provide their on-going care regardless of the day of the week and so our work to increase real 7 day working patterns will continue, with real progress already made, we aim to embed this in the Trust and provide evidence of how it is working and the difference it is making. After a successful experience in hospital it is important that the discharge of our patients is planned well, with full involvement of the patient and any relevant family members or whoever the patient wishes to be involved. This is why we will increase our focus on this aspect of care and aim to have at least 90% of our patients saying they were fully informed. We will also undertake some post discharge surveys to ask patients how they felt the discharge planning was to ensure that it was a safe and effective discharge. 53 95% or more of our patients will report that they were treated with respect and dignity. To ensure that 95% of our patients report that their pain is managed effectively. 2013 - 14 priorities To establish daily senior reviews in all wards to facilitate safe on-going care and effective discharge plans, over 80% of our patients will report that they were involved in their discharge planning. To ensure that 95% of our patients feel that their medications have been provided in a timely manner and fully explained. 95% or more of our patients will report that they were treated with respect and dignity. To establish 7 day week working across the Trust. Examples of key features within the objective would be: 2014 - 15 priorities • Every patient to be reviewed by a consultant every day • Access to diagnostic tests to be the same every day of the week. To have 90% of our patient’s report that they feel involved in the planning of their discharge. As part of the Trusts review of how we undertake patient surveys ensure we ask patients how effective their discharge was. 95% of patients surveyed will say their discharge was safe and effective. 95% or more of our patients will report that they were treated with respect and dignity. 2015 - 16 priorities To deliver improvements in patients feeling informed and involved in their care with 80% or above reporting they do feel involved. To maintain improvements in all aspects of patient safety. 54 Quality Account Priority 4: To ensure that people with learning disabilities and/or autistic spectrum conditions (ASC) are able to access our services when necessary including making reasonable adjustments to services It is estimated that there are 1.5 million people diagnosed with learning disabilities. This is set to increase. There is a recognised inequality in relation to the access to health care treatment for those with a learning disability. When we link this to the fact that approximately one third of people who have a learning disability will also have an associated physical disability and one third will be likely to suffer from epilepsy, it is essential that we support these patients and their families to access our services at the right time. It is also essential to ensure we are able to support admission to hospital both a planned event and as an emergency, in a manner that meets the needs of these patients and their families. In a recent consultation event held by the Trust, which was attended by a wide range of stakeholders, there are some clear areas of priority that it is felt we need to address. These include: 1. Developing a strategy that works for everyone. This means it should: • Be a Multi-agency document • Support an Autism task group • Take into consideration the need for a learning disabilities nurse • Clarify entry points in A&E and across wider hospital • Clarify the skills required in Triage and address these • Be clear about how we recognise patients with a learning disability. Ensure that this is recorded on our systems • Flag up reasonable adjustments and ensure these are reviewed and agreement made regarding what can be done • Continue with collaboration. 2. Developing a clear role for our learning disability champions. This should include: • Allocation of this role to someone who has the time to be able to look at patient experience from the point of admission to discharge • The development of transition champions” and links into Alder Hey • Ensuring there is a role in the outpatient department so that families can liaise prior to the appointment • Consider how we develop our clinical nurse specialists who care for patients with learning disabilities • Be clear about how we will review the experience of our patients and their families to ensure lessons are learned. 55 Setting our priorities Based on the feedback from our consultation event we are able to highlight what is going well and also where our stakeholders wish us to focus more. For 2014-15 our key areas of work will be: 1. To complete our strategy by the end of July 2014 and have this approved at the Trust Learning Disabilities Steering Group 2. Ensure our electronic systems record every patient accessing our services with moderate to severe learning disabilities 3. Ensure all patients with a learning disability have a full risk assessment within 24 hours of admission using a recognised risk assessment tool. Undertake a monthly audit of compliance as part of our ward based audit programme 4. Identify a learning disabilities lead in the Trust 5. Agree a policy which identifies the process for making reasonable adjustments by August 31st 2014 6. Develop a programme of education about learning disabilities to be delivered to staff 7. Review the use of the ‘This is Me’ health passport and provide information regarding the utilisation of these. The aims above will be reviewed in the Learning Disabilities Steering Group and the action plan updated on a quarterly basis. 56 Statement of directors’ responsibilities in respect of the Quality Account The directors are required under the Health Act 2009 to prepare a Quality Account for each financial year. The Department of Health has issued guidance on the form and content of annual Quality Accounts (which incorporates the legal requirements in the Health Act 2009 and the National Health Service (Quality Accounts) Regulations 2010 (as amended by the National Health Service (Quality Accounts) Amendment Regulations 2011). In preparing the Quality Account, directors are required to take steps to satisfy themselves that: • the Quality Accounts presents a balanced picture of the trust’s performance over the period covered; • the performance information reported in the Quality Account is reliable and accurate; • there are proper internal controls over the collection and reporting of the measures of performance included in the Quality Account, and these controls are subject to review to confirm that they are working effectively in practice; • the data underpinning the measures of performance reported in the Quality Account is robust and reliable, conforms to specified data quality standards and prescribed definitions, and is subject to appropriate scrutiny and review; and • the Quality Account has been prepared in accordance with Department of Health guidance. During 2013/14, the Trust commissioned an independent and external review about the way we collect data about Venous Thromboembolism (VTE) assessments. This was to ensure that our processes were robust and that we were being open and transparent. The directors confirm to the best of their knowledge and belief they have complied with the above requirements in preparing the Quality Account. By order of the Board 27 June 2014 Date ............................................................ Chair 27 June 2014 Date ............................................................ Chief Executive 57 Care Quality Commission The Trust is required to register with the Care Quality Commission (CQC) and its current registration status is registered with full compliance with no conditions. The CQC has not taken enforcement action against the Trust during the reporting period 1 April 2012 to 31 March 2013. During the reporting period 1 April 2013 to 31 March 2014 the Trust received one CQC new wave inspection visit on two of its locations: the Royal Liverpool Hospital on 29 October 2013 and Broadgreen Hospital on 30 October 2013. On this occasion the Trust was found to be compliant with the five key areas with some areas identified as requiring improvement. We are working with our NHS partners to complete the CQC Action Plan we have put in place. 58 Patient’s Council Patient’s Council comments on the Trust Quality Accounts 2014 The Patients’ Council for the Royal and Broadgreen University Hospital Trust have received the Trust’s Quality Accounts and had the opportunity to make comments. We are happy that the following goals will be included in the 2014/15 priorities: 1. Reducing Mortality 2. Reduction in harm to Patients 3. Treating Patients with Dignity and Respect 4. To ensure that people with disabilities are able to access the services. The Trust continue to do excellent work and the Council receive continued support. Irene Kelly Chair, Patients’ Council 27 May 2014 59 The Royal Liverpool and Broadgreen University Hospitals NHS Trust - Quality Account Commentary 2013/14 Healthwatch Liverpool welcomes the opportunity to provide a commentary on this Quality Account. Engagement with the Trust has continued during 2013-14, with Healthwatch representatives regularly attending meetings at the Trust. This commentary only relates to the issues covered in the version of the Quality Account that was provided by the Trust. Overall this Quality Account provides a clear reflection of some of the achievements and challenges for the Trust during the past year. The priorities for 2013-14 are rightly seen as part of a longer-term strategy, and from the report appear to be mostly on track. There are many positive achievements and developments outlined in the Quality Account; Healthwatch Liverpool was particularly pleased to read about the work carried out to improve the experiences of patients with Alcoholic Liver Disease, as this work has provided better outcomes for individual patients through a multi-disciplinary, more person-centred approach, and has additional benefits in view of developing a more sustainable health system. We are also pleased to note that a relatively high number of the Trust’s patients were recruited to participate in health research, thus helping to identify new treatments for the future. Although most of the key indicator targets and the majority of CQUIN targets were met, it is clear that challenges remain. One example is that unfortunately the targets for MRSA and C Difficile were not met this year, although the positive work carried out in Gastroenterology to prevent C Difficile from taking hold and spreading on the wards is encouraging. Healthwatch Liverpool is pleased to see that steps have been taken to improve the reporting of incidents within the Trust. The priorities for improvement as a result from two national patient surveys are clearly identified in the report, and Healthwatch Liverpool looks forward to seeing the results once action plans have been implemented. Healthwatch Liverpool is pleased to note that the Trust has continued to progress on Equality Delivery System (EDS) outcomes, by identifying where some of the gaps are and working on trying to improve access and outcomes for all communities in Liverpool and beyond. The priorities for 2014-15, including providing 7-day a week services, right staffing levels and reducing mortality will be followed with interest by Healthwatch Liverpool. We are pleased to see that additionally the Trust will focus on access, and barriers to access, for people with a learning disability and/or autistic spectrum conditions. Healthwatch Liverpool looks forward to continuing engagement with The Royal Liverpool and Broadgreen University Hospitals in 2014/15. Stanley Mayne, Health and Social Care Ambassador for Healthwatch Liverpool 60 NHS Liverpool Clinical Commissioning Group Liverpool CCG welcomes the opportunity to comment on the Royal Liverpool and Broadgreen University Hospital NHS Trust Quality Account 2013/14. As Lead Commissioner of care services and on behalf of our co-commissioning CCGs and the local population, we believe this Quality Account demonstrates a commitment to quality improvement and high quality services. NHS England “Everyone Counts: Planning for Patients 2014-15 to 2018/19” sets out NHS England ambitions and commitment in ensuring high quality care for all, now and for future generations and describes quality as spanning three areas: safe, effective and personalised care. This Quality Account provides an overview of these areas and presents a true reflection of the provider’s achievement of quality of service delivery against the backdrop of a changing NHS. Delivering care and treatment in an organisation with a wide range of services requires commitment to continuously monitor and deliver high quality patient care. Liverpool CCG along with our Co-Commissioning CCGs, is aspiring through strategic objectives and 5 year plans to develop an NHS that delivers great outcomes, now and for future generations. That means reflecting the Government’s objectives for the NHS set out in their mandate to us, adding our own stretching ambitions for improving health and delivering better services to go even further to tailor care to the local health economy. Providing high quality care and achieving excellent outcomes for our patients is the central focus of our work and paramount to our success. It is felt that the priorities identified for the coming year are both challenging and reflective of the current issues across the health economy. The CCG recognises that the Trust acknowledges that improvements are required in certain areas and have referenced these in the report. The CCG looks forward to the implementation of these schemes to enhance the quality of service delivered. The CCG enjoys a conducive and productive working relationship with the Trust and looks forward to continuing this collaborative approach and to strive for excellence and deliver high quality care and treatment to our local population. Signed 12 June 2014 Katherine Sheerin Chief Officer 61 Independents auditor’s limited assurance report to directors of Royal Liverpool and Broadgreen University Hospitals NHS Trust on the annual quality account 62 63 64 65 Appendix 1: Mandatory Clinical Audit Programme List of Mandatory Audits applicable to the Trust • Acute coronary syndrome or Acute myocardial infarction (MINAP) • Adult asthma • Adult Bronchiectasis Audit* • Adult critical care (Intensive Care National Audit and Research Centre (ICNARC) Case Mix Programme Database • Bowel cancer (NBOCAP) • Cardiac Rhythm Management (CRM) • Diabetes (Adult) ND(A) • Elective surgery (National PROMs Programme) • Emergency Use of Oxygen (British Thoracic Society) • Falls and Fragility Fractures Audit Programme (FFFAP) • Gastrointestinal Haemorrhage (NCEPOD) • Head and neck oncology (DAHNO) • Inflammatory bowel disease (IBD)* • • • • • • • • • • • • • • • • • • • • Lower Limb Amputation (NCEPOD) Lung cancer (NLCA) National Audit of Seizures in Hospitals (NASH) National Cardiac Arrest Audit (NCAA) National Chronic Obstructive Pulmonary Disease (COPD) Audit Programme* National Comparative Audit of Blood Transfusion programme National Diabetes Inpatient Audit (NADIA National emergency laparotomy audit (NELA) National Heart Failure Audit National Joint Registry (NJR) National Pregnancy in Diabetes (NPID) National Vascular Registry* Oesophago-gastric cancer (NAOGC) Paracetamol overdose (care provided in emergency departments)* Renal replacement therapy (Renal Registry) Rheumatoid and early inflammatory arthritis* Sentinel Stroke National Audit Programme (SSNAP)* Severe sepsis & septic shock* Severe trauma (Trauma Audit & Research Network, TARN) Tracheostomy study (NCEPOD) 66 The national clinical audits and national confidential enquiries that The Royal Liverpool and Broadgreen University Hospitals NHS Trust participated in during 2013/14 are as follows: List of Mandatory Audits the Trust submitted • Acute coronary syndrome or Acute myocardial infarction (MINAP) • Adult asthma • Adult critical care (Intensive Care National Audit and Research Centre (ICNARC) Case Mix Programme Database • Bowel cancer (NBOCAP) • Cardiac Rhythm Management (CRM) • Diabetes (Adult) ND(A) • Elective surgery (National PROMs Programme) • Emergency Use of Oxygen (British Thoracic Society) • Falls and Fragility Fractures Audit Programme (FFFAP) • Gastrointestinal Haemorrhage (NCEPOD • • • • • • • • • • • • • • • • • • • • • Head and neck oncology (DAHNO) Inflammatory bowel disease (IBD)* Lower Limb Amputation (NCEPOD) Lung cancer (NLCA) National Audit of Seizures in Hospitals (NASH) National Cardiac Arrest Audit (NCAA) National Chronic Obstructive Pulmonary Disease (COPD) Audit Programme* National Comparative Audit of Blood Transfusion programme National Diabetes Inpatient Audit (NADIA National emergency laparotomy audit (NELA) National Heart Failure Audit National Joint Registry (NJR) National Vascular Registry* Oesophago-gastric cancer (NAOGC) Paracetamol overdose (care provided in emergency departments)* Renal replacement therapy (Renal Registry) Rheumatoid and early inflammatory arthritis* Sentinel Stroke National Audit Programme (SSNAP)* Severe sepsis & septic shock* Severe trauma (Trauma Audit & Research Network, TARN) Tracheostomy study (NCEPOD) 67 The national clinical audits that The Royal Liverpool and Broadgreen University Hospitals NHS Trust was eligible to participate in during 2013/14 but did not are as follows: Audit Title Bronchiectasis (British Thoracic Society) Reason for not participating Diabetes in Pregnancy There was lack of clarity in regards to which hospital should submit data to this audit. The hospital aims to run an internal audit to compare ourselves nationally. The number of eligible patients for audit is 6 and therefore was deemed not appropriate to participate 68 The enclosed information is available on request in alternative formats including community languages, easyread, large print, audio, braille, moon and electronically. Visit our website at www.rlbuht.nhs.uk for details about the Trust. Visit www.nhs.uk for information about waiting times for all clinical specialties at the Royal Liverpool and Broadgreen University Hospitals NHS Trust. This report has been produced by the Royal Liverpool and Broadgreen University Hospitals NHS Trust. For more copies, please contact the Communication and Marketing Department on 0151 706 5460, for Typetalk 18001 0151 706 5460, email equalityanddiversity@rlbuht.nhs.uk or ask at the main reception of the Royal Liverpool University Hospital. 69 Notes 70 71 72 The enclosed information is available on request in alternative formats including community languages, easyread, large print, audio, braille, moon and electronically. Visit our website at www.rlbuht.nhs.uk for details about the Trust. Visit www.nhs.uk for information about waiting times for all clinical specialties at the Royal Liverpool and Broadgreen University Hospitals NHS Trust. This annual report has been produced by the Royal Liverpool and Broadgreen University Hospitals NHS Trust. For more copies, please contact the Communication and Marketing Department on 0151 706 5460, for Typetalk 18001 0151 706 5460, email equalityanddiversity@rlbuht.nhs.uk or ask at the main reception of the Royal Liverpool University Hospital. The Royal Liverpool and Broadgreen University Hospitals NHS Trust Prescot Street Liverpool L7 8XP Tel: 0151 706 2000 www.rlbuht.nhs.uk Please recycle this document