Asthma Medications and Devices Krista D. Capehart, PharmD, MSPharm, AE-C
advertisement

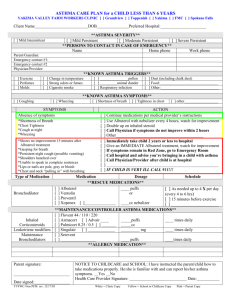
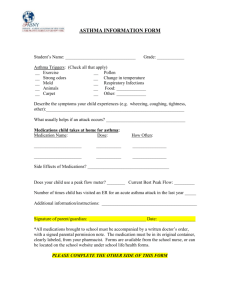
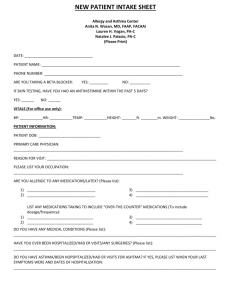
Asthma Medications and Devices Krista D. Capehart, PharmD, MSPharm, AE-C Assistant Professor of Pharmacy Practice University of Charleston School of Pharmacy Objectives • Identify quick relief and controller medications for asthma. • Discuss the different delivery devices for inhaled asthma medications. • Demonstrate how to assist in administering asthma medications. Quick Relief Medications • Medications that are used to help relieve symptoms of an asthma attack • Albuterol is one of the most commonly used quick-relief medications that works to relax the airways and make it easier to breath • Can start to work in 5-15 minutes after use for symptoms Bronchodilators – Beta 2 Agonists – Nebulized: every 4-6 hours as needed* Albuterol (pre-mixed) Ventolin, Proventil, Accuneb Albuterol (concentrate) Levalbuterol Levalbuterol (concentrate) Xopenex 0.63mg/3mL unit dose vial 1.25mg/3mL unit dose vial 2.5mg/3mL unit dose vial 2.5mg/0.5mL – must be mixed with saline or another solution 0.31mg/3mL unit dose vial 0.63mg/3mL unit dose vial 1.25mg/3mL unit dose vial 1.25/0.5mL – must be mixed with saline or another solution * Per NHLBI:EPR3 Guidelines for “Home” management of asthma exacerbations – Up to two nebulized treatments 20 minutes apart may be administered, assessing condition throughout both treatments to determine if emergency transport/emergency department treatment is necessary. Bronchodilators – Beta 2 Agonists – Metered Dose Inhalers (MDIs) every 4-6 hours as needed* Albuterol Levalbuterol Ventolin HFA, Proventil HFA, ProAir HFA Xopenex HFA Pirbutrol Maxair 2-6 puffs per dose (always use a spacer) 2-6 puffs per dose (always use a spacer) 2-6 inhalations per dose (breath activated – do not use spacer) * Per NHLBI:EPR3 Guidelines for “Home” management of asthma exacerbations – Up to two treatments 20 minutes apart may be administered, assessing condition throughout both treatments to determine if emergency transport/emergency department treatment is necessary. Bronchodilators – Anti-cholinergics – Metered Dose Inhalers (MDIs) every 4-6 hours as needed – Not for use alone in asthma Ipratropium bromide Atrovent HFA 4-8 puffs every 20 minutes as needed up to 3 hours for exacerbation * Per NHLBI:EPR3 Guidelines for “Home” management of asthma exacerbations – Up to two nebulized treatments 20 minutes apart may be administered, assessing condition throughout both treatments to determine if emergency transport/emergency department treatment is necessary. Errors in inhaler use • Requires coordination & skill for MDI • In a study that examined inhaler (MDI & DPI) use over 1 month, half made at least one error & 76% using MDI made an error • Critical errors resulted in almost no drug being administered and those occurred in 11% of those using DPI & 28% in those using MDI Spacer Devices • Advantages – Reduces need for patient coordination – Reduces pharyngeal deposition • Disadvantages – Inhalation can be more complex for some patients – Can reduce dose available if not used properly – More expensive than MDI alone – Less portable than MDI alone – Integral actuation devices may alter aerosol properties Ensure that each student has a Personal Written Asthma Action Plan Ensure that each student has a Personal Written Asthma Action Plan Management of Asthma Exacerbations: School Treatment (Per National Asthma Education Prevention Program) • The following slides are the suggested Emergency Nursing Protocol for Students with Asthma Symptoms who don’t have a personal asthma action plan. • A student with asthma symptoms should be placed in an area where he/she can be closely observed. Never send a student to the health room alone or leave a student alone. Limit moving a student who is in severe distress. Go to the student instead. Management of Asthma Exacerbations: School Treatment (Per National Asthma Education Prevention Program) Management of Asthma Exacerbations: School Treatment (Per National Asthma Education Prevention Program) Management of Asthma Exacerbations: School Treatment (Per National Asthma Education Prevention Program) Long-acting Controller Medications • These are medications that are taken daily to help prevent symptoms of asthma by decreasing inflammation and will NOT treat an asthma attack • Inhaled corticosteroids like fluticasone (Flovent®) and budesonide (Pulmicort®) and oral medications like montelukast (Singulair®) and zafirlukast (Accolate®) are the drugs that used most often to prevent symptoms of asthma • Must be taken as prescribed even if you are not having symptoms every day Routine Maintenance Inhaled Medications “Controller medications” Dosages listed are from NHLBI EPR3 Guidelines for ages 5- 11 year old unless otherwise noted Beclomethasone HFA 40 or 80mcg/puff QVAR Budesonide DPI 90mcg, 180mcg, or Pulmicort Flexhaler Low dose: 80-160mcg total per day to be divided and given every 12 hours Medium dose: >160mcg320mcg total per day to be divided and given every 12 hours High dose: >320mcg total per day to be divided and given every 12 hours Low dose: 180-400mcg total per day to be divided and given every 12 hours Medium dose: > 400-800mcg total per day to be divided and given every 12 hours High dose: >800mcg total per day to be divided and given every 12 hours Routine Maintenance Inhaled Medications “Controller medications” Dosages listed are from NHLBI EPR3 Guidelines for ages 5- 11 year old unless otherwise noted Budesonide inhalation suspension for nebulization 0.25mg/2ml,0.5mg/2ml, and 1mg/2mL Pulmicort Respules Low dose: 0.5mg total per day to be given in one or two treatments Medium dose: 1mg total per day to be given in one or two treatments High dose: 2mg total per day to be given in two treatments Mometasone DPI 110mcg/puff, 220mcg/puff Asmanex Twisthaler 1 puff in the evening Routine Maintenance Inhaled Medications “Controller medications” Dosages listed are from NHLBI EPR3 Guidelines for ages 5-11 year old unless otherwise noted Fluticasone HFA 44mcg, 110mcg, 220mcg/puff Flovent HFA Fluticasone DPI 50mcg, 100mcg, or 250mcg per inhalation Flovent Diskus Low dose:88-176mcg total per day to be divided and given every 12 hours Medium dose: > 176-352mcg total per day to be divided and given every 12 hours High dose: >352mcg total per day to be divided and given every 12 hours Low dose: 100-200mcg total per day to be divided and given every 12 hours Medium dose: > 200-400mcg total per day to be divided and given every 12 hours High dose: >400mcg total per day to be divided and given every 12 hours Combination Medications Inhaled – Beta2 Agonist and Corticosteroid Fluticasone/Salmeterol Advair Diskus DPI 100mcg-50mcg Fluticasone/Salmeterol Advair HFA HFA 45mcg-21mcg 115mcg-21mcg 230mcg-21mcg Budesonide/formoterol Symbicort HFA HFA 80mcg-4.5mcg 1 inhalation twice daily (12 hours apart) Not approved for children <12 years 2 puffs twice daily (12 hours apart) Long Acting Beta 2 Bronchodilators – not recommended for use alone in asthma without an inhaled corticosteroid Salmeterol DPI 50mcg/inhalation Formoterol DPI 12mcg/single use capsule for inhalation Serevent Diskus Foradil 1 inhalation every 12 hours Inhale the contents of one capsule every 12 hours Oral Medications • Oral Corticosteroids Methylprednisolone 2, 4, 8, 16, 32mg tablets Prednisolone 5mg tablets 5mg/5mL liquid 15mg/5ml 10mg ODT (Oral disintegrating tablet) 15mg ODT 30mg ODT Prednisone 1, 2.5, 5, 10, 20, 50mg tablets 5mg/mL 5mg/5mL Medrol Prelone, Pediapred Prelone, Orapred Orapred ODT 0.25-2mg/kg daily in single morning or every other day as needed for control 0.25-2mg/kg daily in single morning or every other day as needed for control 0.25-2mg/kg daily in single morning or every other day as needed for control Leukotriene Receptor Antagonist (LTRAs) Montelukast 4mg or Singulair 5mg chewable tablet, 10mg tablet Zafirlukast 10mg, Accolate 20mg 5mg at bedtime (614 years of age) 10mg twice daily (711 years of age) Food and Drug Administration (FDA) Decision • March 31, 2005 – FDA rules that manufacturers needed to phase out production and sale of CFC MDI by December 31, 2008 • Manufacturers began to develop HFA MDI for both “quick relief” medications (albuterol and levalbuterol) and for “longterm controller” medications (inhaled corticosteroids) Differences between CFC and HFA MDIs Component CFC HFA Dose delivery from near empty container Variable Consistent Variable ambient temperature Variable Consistent (-20C) Force of spray More forceful Softer Mist Temperature Colder Warmer Mist Volume Higher Lower Taste Different Different Breath-holding < important with CFC > Important with HFA Priming General guidelines for all Very specific to product Cleaning Periodic cleaning necessary Stressed as REGULAR cleaning necessary Hess DR, Myers TR, Rau JL. A Guide to Aerosol Delivery Devices. Access at http://www/AARC.org/aerosol_delivery on July 25, 2008. Softer, warmer plume may cause patients to think the HFA inhalers do not work as well as the CFCs. The HFA inhalers deliver 108 mcg of albuterol sulfate, which is equivalent to 90mcg albuterol base. This is the same amount of active medication as is in the CFC albuterol MDIs. http://www.google.com/imgres?q=image+HFA+vs+CFC+plume&hl=en&client=firefox-a&hs=GND&sa=X&rls=org.mozilla:enUS:official&biw=1280&bih=579&tbm=isch&prmd=imvns&tbnid=ry2nJQGuKZghPM:&imgrefurl=http://www.expertreviews.com/doi/pdf/10.1586/17476348.2.2.149&docid=qSjR7QNpJcZOM&w=120&h=67&ei=F81wToruLMHcgQem4_EQ&zoom=1&iact=hc&dur=3717&page=1&tbnh=58&tbnw=104&start=0&ndsp= 21&ved=1t:429,r:2,s:0&tx=44&ty=31&vpx=486&vpy=217&hovh=58&hovw=104 Accessed September 2011 Priming… • Each of the HFA metered-dose inhalers must be “primed” • What does “priming” mean? • How many times for different inhalers?!? Examples of HFA priming guidelines Medication When to prime # of sprays Proventil HFA (albuterol) Prior to 1st use 2 wks of non-use 4 4 Ventolin HFA (albuterol) Prior to 1st use 2 wks of non-use 4 4 ProAir HFA (albuterol) Prior to 1st use 2 wks of non-use 3 3 Flovent HFA (fluticasone) Prior to 1st use With < 3 weeks of non-use With > 3 weeks of non-use 4 1 4 QVAR (beclomethasone) Prior to 1st use With 10 days of non-use 2 2 Advair HFA (fluticasone and salmeterol) Prior to 1st use With 4 weeks of non-use 4 2 Atrovent HFA (ipratropium) Prior to 1st use With 3 days of non-use 2 2 Inhalation technique for the HFA MDIs 1. 2. 3. 4. 5. Remove mouthpiece cover and check for foreign objects. Shake the inhaler well immediately before use. Prime if necessary. Breath out normally through the mouth, getting as much air out of the lungs as possible. Place the mouthpiece between the lips and teeth. 6. Breath in slowly and press MDI canister down once at the beginning of the inhalation. 7. Hold breath as long as possible, up to 10 seconds. 8. Remove inhaler from mouth and breath out slowly 9. Wait 30-60 seconds between doses. 10. Rinse mouth and spit with ICSs. Cleaning HFA MDIs • All HFAs state actuator needs to be cleaned at least once a week and as needed • Clean by removing the canister and running warm water through the top and air dry overnight if possible Dry powder inhalation (DPI) devices • • • • • No propellants Built-in dose counters Breath actuated Formoterol – individual capsules Diskus (salmeterol & fluticasone) – blister strip • Budesonide and mometasone– drug reservoir Technique for Diskus • • 1. 2. Diskus expires 1 month from the day the pouch is opened Open, Click, Inhale Open by placing the thumb on the thumb grip and push away from you until the mouthpiece appears and snaps into position. Hold the Diskus FLAT with the mouthpiece toward you and slide the level as far as it will go until it clicks. 3. Inhale – – Exhale fully while holding the Diskus away from your mouth and FLAT. Never breath into the mouthpiece – Put the mouthpiece to your lips and inhale quickly and deeply through your mouth (not nose). – Remove the Diskus from your mouth and hold your breath for about 10 seconds. Exhale slowly. – Rinse your mouth with water and spit after breathing in the medicine. – Close the Diskus when you are finished. Technique for budesonide DPI • • • • • Prime before using for the 1st time ONLY Hold the inhaler so that the white part is pointing up and remove the cover by lifting up Hold the inhaler by the brown grip and grasp the inhaler in the middle, still holding it upright Twist the brown grip as far as possible to one direction then fully back again in the other direction until it stops The device is now primed and does NOT need to be primed again • Load the dose – Twist the cover and lift off – Hold inhaler in upright position and grasp brown grip – Place other hand in the middle of the inhaler – Twist all the way in one direction and then fully back again in the other direction until it clicks • Keep inhaler vertical until ready to use – Exhale completely (not into the inhaler) – Place mouthpiece in your mouth, close lips around it, inhale deeply and forcefully through the inhaler – Remove the inhaler from your mouth and exhale – Replace the cover – Rinse mouth with water and spit. Technique for mometasone DPI • Remove inhaler from pouch – throw away 45 days after opening or when dose counter reads “00” • Open the inhaler – Hold inhaler straight up with colored portion on the bottom. – Holding the colored base twist the cap counterclockwise to remove it. Removing cap loads the dose • Inhale the dose – Breathe out fully – Place the inhaler in your mouth holding it horizontally, closing your mouth firmly around the inhaler – Take in a fast, deep breath. Do not cover the ventilation holes – Do not breath into the inhaler. Remove the inhaler from your mouth and hold your breath for 10 seconds. – Rinse mouth with water and spit. Nebulizers • Nebulizers uses ampules of medication that is put in a special cup and usually air is used to make the solution into a breathing treatment • It usually takes about 5-10 minutes to complete a breathing treatment of 3 mL of medication. How do we see if the medications are working? • Peak flow meters • Spirometry Other asthma resources for you at school • The National Heart Lung and Blood Institute – National Asthma Education and Prevention Program has a large assortment of resources available online at http://www.nhlbi.nih.gov/health/public/lung/ index.htm#schools References • • • • • • • • • • • • • • • • Kelly HW and SorknessCA. Asthma. In: Dipiro JT, Talber RL, Yee GC, Matzke GR, Wells BG, Posey LM, eds. Pharmacotherapy: A Pathophysiologic Approach, 6th ed. New York: McGraw-Hill Co; 2005. p. 503-535. Blake K and Kelly WH. Asthma. In: Helms RA, Quan DJ, Herfindal ET, Gourley DR, eds. Textbook of Therapeutics: Drug and Disease Management, 8th ed. Philadelphia (PA): Lippincott Williams & Wilkins; 2006. p. 877-918. Global Initiative For Asthma: Global Strategy for Asthma Management and Prevention. Revised 2006. http://www.ginasthma.com/Guidelineitem.asp??l1=2&l2=1&intId=60 National Heart Lung and Blood Institute. National Asthma Education and Prevention Program; Expert Pane Report 3:Guidelines for Diagnosis and Management of Asthma; Full Report 2007. http://www.nhlbi.nih.gov/guidelines/asthma/index.htm Kavuru MS. Diagnosis and management of asthma. 4th ed. Professional Communications, Inc. West Islip, NY: 2008. http://www.google.com/imgres?q=image+HFA+vs+CFC+plume&hl=en&client=firefox-a&hs=GND&sa=X&rls=org.mozilla:enUS:official&biw=1280&bih=579&tbm=isch&prmd=imvns&tbnid=ry2nJQGuKZghPM:&imgrefurl=http://www.expertreviews.com/doi/pdf/10.1586/17476348.2.2.149&docid=qSjR7QNpJcZOM&w=120&h=67&ei=F81wToruLMHcgQem4_EQ&zoom=1&iact=hc&dur=3717&page=1&tbnh=58&tbnw=104&start =0&ndsp=21&ved=1t:429,r:2,s:0&tx=44&ty=31&vpx=486&vpy=217&hovh=58&hovw=104 Accessed September 2011 Hess DR, Myers TR, Rau JL. A Guide to Aerosol Delivery Devices. Access at http://www/AARC.org/aerosol_delivery on July 25, 2008. Leach CL. The CFC to HFA transition and its impact on pulmonary drug development. Resp Care 2005;50:1201-1206. Busse WW, Brazinsky S, Jacobson K, Schmitt K, Vanden Burgt J, et al. Efficacy response of inhaled beclomethasone dipropionate in asthma is proportional to dose, and is improved by formulation with a new propellant. J Allergy Clin Immunol 1999;104:1215-1222. Hess DR, Myers TR, Rau JL. A Guide to Aerosol Delivery Devices. Access at http://www/AARC.org/aerosol_delivery on July 25, 2008. Prescribing information for Asmanex Twisthaler 2008, Advair Diskus 2008, Spiriva 2008, Pulmicort FlexHaler 2007, Proventil HFA 2007, Ventolin HFA 2008, ProAir HFA 2006, Foradil Aerolizer 2006, QVAR 2006 Use of Ozone Depleting Substances: Removal of Essential Use Designation; Final Rule. Federal Register April 4, 2005;70(63):17167-17192. Questions and answers on final rule of Albuterol MDI’s. at http://www.fda.gov/cder/mdi/mdifaqs.htm access August 8, 2008. OptHolt T and Philibosian D. Inhalation Therapy Device Workshop. Delivered at the Association of Asthma Educators Annual Meeting in San Francisco July 18-21, 2008. FDA Public Health Advisory: National Transition from Chlorofluorocarbon (CFC) Propelled Albuterol Inhalers to Hydrofluroalkane (HFA) Propelled Albuterol Inhalers. Accessed at http://www.fda.gov/cder/mdi/albuterol.htm Accessed on August 8, 2008. http://www.nhlbi.nih.gov/health/prof/lung/asthma/sch-emer-actplan.pdf