Full Text: PDF (211.68KB)
advertisement

Published By Science Journal Publication
Science Journal of Medicine & Clinical Trial
ISSN: 2276-7487
http://www.sjpub.org/sjmct.html
© Author(s) 2013. CC Attribution 3.0 License.
Research Article
doi: 10.7237/sjmct/248
Hot Deck Propensity Score Imputation For Missing Values
Dr. Benjamin Mayer
Institute of Epidemiology and Medical Biometry, Ulm University, Schwabstr. 13, 89075 Ulm, Germany.
e-mail: benjamin.mayer@uni-ulm.de, Phone: +49-731-5026896, Fax: +49-731-5026902
Accepted 22th May, 2013
ABSTRACT
The adequate handling of missing data in medical research still
constitutes a major problem of statistical data analysis. Although
different imputation strategies and methods have been
developed in recent years, none of them can be used
unhesitatingly in arbitrary missing data situations. A commonly
observed drawback of the established imputation methods is
their sensitivity against the number of missing values in the
analysis set, the underlying missing data mechanism and scale
level of the incomplete variable. The extent of this sensitivity is
indeed different for individual methods. A novel approach for the
imputation of missing data was proposed here which especially
does not depend on the scale level of the variable that is affected
by missing values. This approach in a multiple imputation setting
was based on the calculation of propensity scores and their usage
in creating adequate imputation values, resting upon a Hot Deck
principle. In the course of a real-data based simulation study, the
proposed method was compared to a standard multiple
imputation approach and a complete case analysis strategy. The
results showed that there was a dependency of imputation’s
goodness from the assumed missing data proportion, too.
However, the developed imputation method generated
consistent estimations of the width of confidence intervals and
could be applied for different kinds of incomplete variables
straightforwardly, which is not possible with other imputation
approaches that easily in general.
KEYWORDS: Hot deck imputation; Missing values; Multiple
Imputation; Propensity Score.
1.0 INTRODUCTION
In medical research, the adequate handling of
missing values still constitutes a major problem.
Despite extensive methodological research on this
topic, there is still no uniform solution for the
handling and imputation of missing data yet. This
circumstance is also reflected in relevant guidelines
for clinical trials which indeed summarize the
problematic aspects of missing values and present
different approaches for their imputation
meanwhile. However, it has not been possible to
formulate uniform advices so far. Hence, it is much
more important to improve the existing methods
and to develop novel approaches for imputing
missing data. Within the latter, it is worthwhile to
investigate a preferably wide range of missing data
“situations”, which arise from different missing data
mechanisms and different types of variables which
are affected by missing values.
The problems if some values of a dataset cannot be
observed are substantial. First of all, each missing
value stands for a loss of information. The
generalization of study results is therefore limited
to a certain extent, depending on the amount of
missing items in the dataset on the one hand and
which variables are affected on the other hand. Just
ignoring those subjects with missing information
for one or more analysis variables may lead to a
considerable loss of statistical power, especially
when the number of analysis variables and thus the
probability for a missing observation is high. This
so called complete case analysis (CCA) strategy only
leads to convincing results if the missing data arise
independently of the underlying study conditions.
The most serious problem with missing values is
biased parameter estimates, however. Missing
values may destroy a generated structural equality
between comparison groups, for example, with the
result that an investigated treatment effect includes
some bias. With respect to the stated problems of
data analysis and interpretation, a methodological
examination of alternative approaches to handle
the missing data problem apart from only ignoring
them has been necessary.
There is a well established and accepted missing
data theory which can be significantly traced back
to Allison (2001), Little (2002) and Rubin (1987).
According to this theory, the occurrence of missing
data can be divided into three so called missing
data mechanisms, which describe the relation
between observed and missing values. The term
“Missing Completely At Random” (MCAR)
characterizes a situation where the incomplete
cases with missing values are a random sample of
the whole dataset, so the occurrence of missing
Corresponding Author: Dr. Benjamin Mayer
Institute of Epidemiology and Medical Biometry, Ulm University, Schwabstr. 13, 89075 Ulm, Germany.
e-mail: benjamin.mayer@uni-ulm.de, Phone: +49-731-5026896, Fax: +49-731-5026902
Science Journal of Medicine & Clinical Trial ISSN: 2276-7487
data is independent of other variables in the
dataset. An example for MCAR would be a patient
who is dying in the course of a clinical trial, but this
event is totally independent of the participation on
the trial. The second mechanism is called “Missing
At Random” (MAR) and describes the situation
where the occurrence of missing data can be
explained by other variables of the dataset which
are observed (e.g. patient fulfils exclusion criteria in
the course of a trial). If one has to assume that the
occurrence of missing values is in addition to it
related to unobserved variables, the missing data
mechanism is “Missing Not At Random” (MNAR).
One may think of a patient diagnosed with
depression who does not report about his actual
mental constitution because he is afraid of potential
consequences like inpatient treatment.
Numerous imputation methods have been
developed, whereas none of them is really
applicable in a MNAR situation. They can be
separated into either Single Imputation (SI) or
Multiple Imputation (MI) methods. The crucial
distinction between both strategies is that all SI
methods impute each missing by one value,
whereas the MI methods replace each missing value
by m (m > 1) imputation values. The main
advantage of MI over SI is that the imputation
values are estimated more precisely, since the
imputation itself as an additional source of
variability is explicitly considered at the estimation
of the variance. Therefore, MI approaches are
considered to be state of the art today (Schafer and
Graham, 2002). An example of a basic SI approach
is imputation by the mean of the observed values.
Often used MI methods are the Markov Chain
Monte Carlo (MCMC) method and a MI using
chained equations (White et al., 2011). However, as
already mentioned, there is still no uniform
solution for the handling and imputation of missing
data yet (European Medicines Agency, 2010).
A popular method of the SI strategy is, in a simple
version, the so called Hot Deck imputation that
includes a variety of approaches. According to the
Hot Deck principle, a missing value of an
incomplete variable is imputed by an observed
value of the same variable where the selection of
this observed value can be randomly or pursuant a
defined criterion. Often the imputation value for a
study participant is a random choice from a set of
observed values, where the participants show
similarities
with
respect
to
particular
characteristics. Different options to create this so
2
called “donor pool” are summarized and discussed
in Andridge and Little (2010).
Defining subjects similarly may be a complex
procedure in general. The investigated medical
problem strongly determines the most relevant
factors for such a definition. From a methodological
point of view usually multivariate approaches are
required. For a descriptive example one may think
of observational studies where patients are not
randomized to the treatment arms. Covariables and
potential confounders possibly are not equally
distributed to the comparison groups, so respective
analysis methods are required to avoid biased
effect estimates. A well-known approach in such a
situation to make patients more comparable and to
get adjusted effect estimates is the propensity score
(PS). It describes the conditional probability for a
patient to be exposed (e.g. belonging to the
treatment group) under a given covariate structure.
In this way the partially extensive information on a
patient can be reduced to a scalar value. Patients
with the same profile of covariables will have the
same conditional probability to be exposed.
The PS can then be used, for example, to adjust the
effect estimator for potential confounding in the
course of a regression analysis or to conduct a PSbased matching of exposed to non-exposed
patients. If the exposure status would be defined as
an indicator for the presence of missing values of an
analysis variable, then the PS can be used to assess
the similarity of patients with and without missing
values.
Within this paper, it is described how the two
concepts of propensity score estimation and Hot
Deck imputation can be combined to create a
flexible multiple imputation method. This approach
is called the Hot Deck Propensity Score (HDPS)
method. Related approaches are described in
Andridge and Little (2010), Mittinty and Chacko
(2004), Little (1986), Haziza and Beaumont (2007)
and Allison (2000). The proceeding is not
illustrated in detail in Andridge and Little, while
Mittinty and Chacko provide a nearest neighbor
imputation based on PS in a Single Imputation
setting only. The papers of Little and Haziza and
Beaumont, however, also rather describe Single
Imputation approaches, whereas they use the
Propensity Score to create imputation classes,
which is not the scope of this article. Allison indeed
describes a PS-based Multiple Imputation
procedure which is called “approximate Bayesian
bootstrap”, but this approach also rests upon
How to Cite this Article:Dr. Benjamin Mayer “Hot Deck Propensity Score Imputation For Missing Values,” Science Journal of Medicine and Clinical Trials,
Volume 2013 (2013), Article ID sjmct-248, Issue 2, 18 Pages, doi: 10.7237/sjmct/248
Science Journal of Medicine & Clinical Trial ISSN: 2276-7487
imputation classes and not on a nearest neighbor
approach.
The paper is organized as follows. After a short
presentation of the example data set which was
used for the simulation study, some theoretical
aspects of Hot Deck imputation and the calculation
of propensity scores are given. The presentation of
the HDPS method is additionally endorsed by a
simulation study which has been conducted to
investigate the performance of the method with
respect to effect estimation for different missing
data situations. Respective simulation results for a
complete case analysis and a standard multiple
imputation approach are also given to which the
HDPS results can be referred to.
2.0 Data Example
The SPICE data set (Holubarsch et al, 2008) was
derived from a cohort study in the field of
cardiology. This clinical trial investigated the
efficacy and safety of Crataegus extract in patients
with congestive heart failure. In an extended
evaluation of the SPICE data (Mayer et al., 2013), a
multivariate Cox regression analysis was
performed to find risk factors for a cardiac event,
which was a composite endpoint of cardiac death,
non-fatal myocardial infarction and hospitalization
due to progressive heart failure.
This analysis was based on 2170 patients who had
complete values in all necessary variables for the
regression model. The mean age of the patients was
59.8 years (SD 10.5) with a higher amount of male
patients (84%). Most relevant risk factors for
getting a cardiac event had been the intake of
cardioactive
medications
(glycosides,
antiarrhythmics, nitrates, diuretics, beta blockers,
and calcium antagonists), the extent of clinical
parameters (left ventricular ejection fraction
(LVEF), New York Heart Association (NYHA)
functional class) and the age of the patients. The
hazard ratios for those variables were significantly
different from 1.
The results of the multivariate Cox regression
analysis are presented more detailed in Table 2.
Parts thereof should be contrasted to the results of
the simulation study which will be described in the
following section 3, to capture the effect of a
missing value imputation via the proposed Hot
Deck Propensity Score method, and other strategies
to handle missing data.
3
3.0 Materials and Methods
Before the concepts of Hot Deck imputation,
propensity scores and a combination of both to
impute missing values are discussed, an
appropriate notation is introduced. This should
support a clear description of the algorithm for
HDPS imputation.
In the following, V=(V1,…,Vn)T denotes the
incomplete target variable from which missing
values have to be imputed, where n is the number
of subjects in the dataset. For a first view on the
method’s properties, it is assumed that only one
variable is affected by missing values. An
application of the proposed method for more than
one incomplete variable is then discussed within
section 5. Further, Xi=(Xi1,…,Xip) denotes the vector
of p completely observed variables for subject
i=1,…,n. Thus, X=(X1,…,Xn)T is the (n×p) matrix of
observed variables of the dataset. Furhtermore, let
R=(R1,…,Rn)T with Ri=1 if Vi is missing and Ri=0 if Vi
observed for all i=1,…,n be a missing data indicator
variable for V. Above that, the target variable V can
easily be separated into two components, the
observed part and the incomplete part: V=
(Vobs,Vmis). Consequently, the indicator variable R is
also separated into R=(R0,R1).
The main objective is to present a procedure for
missing value imputation. The introduced notation
should therefore not be interpreted in a way that
the regression of V on X is the aim, so V has not
necessarily to be the outcome variable of the final
analysis model. Instead, the aim is to conduct a
regression of the missing value indicator R on X to
estimate the conditional likelihood for each subject
to have a missing value in V. How the propensity
score is subsequently used to multiply impute the
missing values according to a Hot Deck approach is
described in section 3.3. Based on the completed
dataset, the final analysis model, for example a Cox
regression as in section 2, can be conducted.
3.1 The Concept of Hot Deck Imputation
According to the Hot Deck principle, every missing
value v* of a variable V (v* as a part of Vmis) is
imputed by an observed value v (v as a part of Vobs).
At this, the subject with the missing v* is often
labelled “recipient” whereas the subject who
provides the imputation value is called “donor”
(Andridge and Little, 2010). In general, one has to
differentiate two approaches: random Hot Deck
procedures choose a donor value v randomly out of
How to Cite this Article:Dr. Benjamin Mayer “Hot Deck Propensity Score Imputation For Missing Values,” Science Journal of Medicine and Clinical Trials,
Volume 2013 (2013), Article ID sjmct-248, Issue 2, 18 Pages, doi: 10.7237/sjmct/248
Science Journal of Medicine & Clinical Trial ISSN: 2276-7487
an underlying donor pool, and, by contrast,
deterministic Hot Deck methods select v according
to certain criteria. One searches for donor values,
for example, whose donors are preferably similar to
the recipient. For this decision, several approaches
which are able to capture the similarity between
subjects are possible.
In contrast to the so called Cold Deck principle
where the potential donor pool is based on data
which don’t origin from the actual analysis dataset,
the Hot Deck approaches go back to observed
values v of Vobs for the generation of the imputation
values. Since Hot Deck imputation is usually applied
in a SI setting, its general drawback is that the
amount of variability that can be traced back to the
imputation itself is not explicitly considered at the
imputation, so the variance is underestimated by
tendency, and confidence intervals are estimated to
narrow. The HDPS approach therefore aims to
implement the Hot Deck principle in a Multiple
Imputation setting by creating an appropriate
donor pool from which the imputation values are
chosen randomly.
3.2 The Calculation and Usage of Propensity
Scores
Basically, propensity scores describe the
conditional probability P( T=1 | X=x) to be exposed
with respect to a defined event, given the specific
covariable structure for a subject (Rosenbaum and
Rubin, 1983). The exposure status may indicate the
belonging to an intervention group or the presence
of a certain event like, for example, a missing value.
According to D’Agostino (1998), the PS are usually
estimated by a logistic regression model
logit P (T=1 | X=x) = ln (P/(1-P)) = β0 + β1x1 + … + βpxp.
The propensity score summarizes the partially
extensive information of a whole set of covariables
to a scalar value. This reduction of dimension could
be beneficial if the PS is used again within further
analyses.
In observational studies, for example, propensity
scores are frequently used to correct for potential
confounding variables which affect the estimation
of treatment effects negatively (Guo and Fraser,
2010). A major problem of observational studies
concerns the possible lack of structural equality of
comparison groups due to a not-feasible
randomization. By calculating an individual
conditional probability (on the particular covariate
4
structure) for each subject it is possible to adjust
for an unequal distribution of confounders in
comparison groups. The final analysis model,
whatever it is, has to consider the calculated PS as
an adjustment variable. Basically there are two
procedures to make use of the propensity score
(Guo and Fraser, 2010), either including it in the
final analysis model (e.g. as additional covariable in
a regression model) or to interpose a subject
matching according to the PS before a postmatching analysis is done (e.g. stratification based
on matched sample).
The PS approach is applicable to any type of
multivariate data when a binary, or even
multinomial, response variable is investigated.
Defining a binary missing data indicator variable R
as response, the PS methodology can be used to
estimate the chance for each study participant to
have a missing value in V, given the individual
structure of covariables X. The validity of this
likelihood is essentially dependent on the quality
and completeness of the covariables X. At that,
study participants with a similar covariable
structure have similar PS, so a matching of study
participants according to their calculated
conditional likelihoods can be made, for example.
Just that approach should be applied to create an
appropriate donor pool for study participants with
missing values in the course of a Hot Deck
imputation.
3.3 The Hot Deck Propensity Score (HDPS)
Approach
The objective of the HDPS method is to find a
respective donor element v of Vobs for each missing
value v* of Vmis. The approaches of Hot Deck
imputation and propensity score estimation are
combined for this purpose. According to the Hot
Deck principle, donors and recipients should be
preferably similar. The application of a missing data
indicator variable R enables to use a PS approach to
find appropriate pairs of donors and recipients, if R
defines the dependent
variable of the
corresponding logistic regression model and all
completely observed variables are used as
predictors. The strength of similarity is represented
by the PS of the subjects at this. Since a missing data
indicator variable is used which denotes the
presence or absence of the values of the target
variable V, the HDPS approach is not restricted to
an imputation of just certain variables in a sense
that there are no limitations with respect to the
scale level of V.
How to Cite this Article:Dr. Benjamin Mayer “Hot Deck Propensity Score Imputation For Missing Values,” Science Journal of Medicine and Clinical Trials,
Volume 2013 (2013), Article ID sjmct-248, Issue 2, 18 Pages, doi: 10.7237/sjmct/248
Science Journal of Medicine & Clinical Trial ISSN: 2276-7487
To avoid the general drawback of deterministic Hot
Deck procedures that each missing value is imputed
by just one donor value, the HDPS proposal rests
upon the creation of a donor pool from which an
imputation value is randomly chosen. In this way,
the HDPS approach can be implemented as a
Multiple Imputation method and is given through
the following algorithm:
1.
2.
3.
Calculate the PS via P(R=1 | X=x) where X is
the matrix of all completely observed
variables of the original data set and R is
the missing data indicator variable for the
target variable V
For all v* in Vmis search vi in Vobs, i=1,…,10:
Di | PS v* PS vi | 0
with min {Di:
i=1,…,10} := D1 ≤ D2 ≤ … ≤ D10
Do a MI (m = 5) by choosing randomly vi,
i=1,…,10 as imputation value for v*
PS
PS
vi
v* and
Here,
are
the
corresponding
propensity scores of v* and vi, respectively. For each
missing element of V (i.e. for each subject with a
missing in V) one has to search for a set of observed
values of the target variable (i.e. from all subjects
with observed values for V) such that the calculated
individual propensity scores show an absolute
deviation which tends to zero. The aim is to find
PS
vi
those propensity scores
which result in the ten
most minimal absolute differences when
PS
v* . In doing so, a donor
subtracting them from
pool of ten observed values of V is created. For each
missing value of the target variable then m = 5
elements of this pool are chosen randomly as
imputation values. The preferably high similarity
between subjects with missing values and observed
values is characterized and obtained by an absolute
deviation of their propensity scores which tends to
zero. The establishment of a donor pool allows
performing a MI, which has substantial advantages
over deterministic Hot Deck procedures which are
only able to conduct a SI. Simultaneously the
intended similarity between donors and recipients
is ensured by minimizing the absolute difference in
PS. The size of the donor pool has been set to a
number of ten potential donor values to guarantee a
sufficient variability among the imputation values
on the one hand, and to preserve an acceptable
extent of similarity on the other hand. The choice of
5
m = 5 corresponds to the established opinion with
respect to the number of imputations which are
sufficient (Rubin, 1987).
The HDPS approach is very intuitive. Initially one
investigates the relationship between the target
variable (by the respective missing data indicator
variable R) and all completely observed variables of
the data set. Using the PS as a scalar measure of
similarity of subjects, an adequate donor can be
identified easily. The consideration of the absolute
difference guarantees that the potential donor
subjects could have either smaller or larger PS
values. A priori one would expect that the ability of
the logistic regression model to capture a relation
between the missing data indicator and all observed
variables is high, especially if the data are missing
not completely at random (i.e. in case of MAR).
3.4 Simulation Study
To evaluate the proposed HDPS approach with
respect to its ability to impute missing values of
different scale levels properly, a real data-based
simulation study has been performed. On the basis
of the presented example dataset in section 2,
missing values have been artificially simulated and
imputed afterwards again. Therefore, the original
results of the Cox regression model (Table 2) can be
compared to results after imputation. Different
missing data situations have been investigated
which arise from different missing data mechanisms
and various proportions of missing values in the
dataset. Two alternative approaches to handle
missing data have also been applied to allow for a
comparison of the HDPS results to established
methods. The simulations have been performed
with the statistical software SAS.
3.4.1 Missing Data Situations
The simulation study has been set up to investigate
a number of different missing data situations. The
two missing data mechanisms MCAR and MAR have
been created, so the application of the HDPS
approach is restricted to so-called “ignorable”
missingness. Additionally, distinct proportions of
missing values in the dataset (5%, 10%, 20%, 30%,
40%, and 50%) have been examined. Although
there is no recommendation up to which rate of
missing values an imputation can, or should be
performed, a proportion higher than 50% seems
problematic in general with respect to data quality.
For that reason higher percentages have not been
considered for simulation. The investigated missing
How to Cite this Article:Dr. Benjamin Mayer “Hot Deck Propensity Score Imputation For Missing Values,” Science Journal of Medicine and Clinical Trials,
Volume 2013 (2013), Article ID sjmct-248, Issue 2, 18 Pages, doi: 10.7237/sjmct/248
Science Journal of Medicine & Clinical Trial ISSN: 2276-7487
rates represent more realistic scenarios which may
arise in practice. For each missing data situation,
1000 simulations have been run.
Hot Deck Propensity Score imputation is a flexible
approach since it is not restricted to a certain scale
level of the variable to be imputed. To show its
applicability for different types of variables, the
simulations have been run for both, one continuous
(LVEF) and one binary variable (glycosides intake).
3.4.2 Creation of Missingness
To create missing values according to the MCAR
mechanism, for both variables a simple random
sample has been chosen from the complete dataset
(2170 cases). For every patient a random number
generator has been used which indicated if the
respective value of LVEF or glycosides should be
deleted, where the likelihoods for deletion or not
were equal.
For generating the MAR mechanism a random
number generator has been used, too. But here the
likelihood for a value of LVEF or glycosides,
respectively, to be deleted was based on the values
of the variable NYHA class, and is therefore not
completely random. It has been assumed that
patients with a higher NYHA class are more likely to
have a missing in LVEF or glycosides. This
assumption might be realistic, since patients with a
higher NYHA class are severely ill and are, maybe,
more likely to miss an appointment for LVEF
examination, or do not know exactly if they ingest
glycosides besides all other medications. Overall,
the likelihoods for deleting a value or not have been
unequal, but resulted in the desired missing data
proportion for each simulation scenario.
3.4.3 Investigated Approaches to Handle
Missing Data
The incomplete datasets were subsequently treated
with three different approaches. The presented
HDPS method has been applied to the data, as well
as a standard multiple imputation approach
(Markov Chain Monte Carlo method (MCMC) or
Logistic method). Moreover, a complete case
analysis has been conducted. For the HDPS method,
the SAS macro “%hdps.sas” has been created which
implements the algorithm presented in section 3.3.
The MCMC method is default for the SAS procedure
PROC MI for the imputation of continuous variables
(LVEF). The imputation of binary variables
6
(glycosides) requires the Logistic method which is
also available in PROC MI. According to the HDPS
method, a number of 5 imputations have been
performed with the MCMC method and the Logistic
method, respectively. The Cox regression, as the
final analysis model, includes only completely
observed cases by default, so the performance of
CCA was straightforward by analyzing the
incomplete data sets directly.
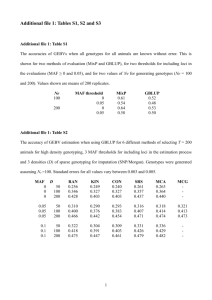
3.4.4 Evaluation of Simulation Results
To evaluate the applicability of the proposed HDPS
method, the same Cox regression which created the
original results of Table 2 have been performed
again with all imputed datasets. The parameters of
primary interest for the two incomplete variables
were the hazard ratios with their corresponding
95% confidence intervals. The comparison between
the original results and those which have been
created after missing value imputation based on
these parameters. Since for every missing data
situation 1000 simulation runs have been
conducted, the mean and standard deviation over
all simulation results for every parameter estimate
was calculated for the particular missing data
situation.
The c-statistic of the logistic regression model to
calculate the propensity scores has additionally
been recorded for informative purposes. This value
serves for describing the ability of the logistic
regression to model the relationship between the
completely observed covariables and the missing
data indicator variable. Higher values of the cstatistic indicate a better selectivity of the logistic
regression model. Therefore, in simulation
scenarios where the completely observed variables
fit well to the missing data indicator variable, higher
c-values and more precise imputations are
expected. Evaluation of the results after imputing
the binary variable (glycosides) is also based on
capturing the fraction of accordances among
original and imputed values.
4.0 Results
4.1 General Remarks
In the following, the results of the real data-based
simulation study, which has been described within
the last section, are presented. The main objective
was to investigate the impact of a missing value
imputation, with respect to the estimated hazard
ratios and corresponding 95% confidence intervals
How to Cite this Article:Dr. Benjamin Mayer “Hot Deck Propensity Score Imputation For Missing Values,” Science Journal of Medicine and Clinical Trials,
Volume 2013 (2013), Article ID sjmct-248, Issue 2, 18 Pages, doi: 10.7237/sjmct/248
Science Journal of Medicine & Clinical Trial ISSN: 2276-7487
of the two target variables: LVEF and glycosides. No
efforts have been undertaken at the generation of
the HPDS results which explicitly affected the
goodness of the logistic regression model
(expressed by the c-statistic). The calculation of the
propensity scores, which subsequently were used
for choosing the surrogate values, was based on all
observed variables of the example data set. First of
all, salient differences between the particular
simulation scenarios should be investigated with
respect to different proportions of missing values
and missing data mechanisms.
Since the simulation has been conducted for two
different types of variables, the results were
presented in two parts. Beside the hazard ratios and
95% confidence intervals, the value of the c-statistic
was also given for those simulation scenarios where
the HDPS method has been used to impute missing
data. The analysis of the binary variable was a bit
more extended by presenting additionally the rate
of correctly imputed missing items (i.e. accordance
of original and imputed value) for the HDPS and MI
method. It has to be kept in mind that the presented
results were the mean values over all 1000
simulation scenarios.
4.2 Continuous Simulation Variable
The simulation results for the continuous variable
(LVEF) confirmed some previously formulated
expectations and brought out interesting findings
with respect to the intended comparison of the
HDPS method for imputing missing values with CCA
and Multiple Imputation approaches.
First of all, according to Table 3, the use of MI led to
almost unbiased estimates of the hazard ratio and
corresponding 95% confidence interval for LVEF.
This holds for both investigated missing data
mechanisms, MCAR and MAR, and proved again the
very good properties of the MCMC method in
imputing missing values. Moreover, it seemed that
there is no considerable impact of the rate of
missing values in the data set on the precision of
estimation. The maximal deviation of the MI
estimator from the original hazard ratio (0.985)
was 0.9863 (MAR, 50% missing values).
The HDPS method, however, generated slightly
inaccurate estimates of the hazard ratio and the
confidence limits for missing value rates of 20% and
higher. Further, precision of estimation depended
on the underlying missing data mechanism,
whereas the estimation was more precise in case of
7
a MCAR mechanism. The maximum difference
between original and simulated hazard ratio of
LVEF could be observed again for a MAR
mechanism and a missing value rate of 50% (0.985
vs. 0.9933). The upper and lower confidence limits
were estimated too large compared to the original
limits. Overall, strength of the estimated effect sizes
for LVEF was too high.
The CCA strategy resulted in relatively robust
estimations of the hazard ratio for both, MCAR and
MAR, but much more sensitive estimations of the
confidence limits. The maximal deviation of the
estimated hazard ratio was 0.9688. While both
confidence limits were estimated too large by
applying the HDPS method, the CCA strategy
brought out smaller estimators for the lower
confidence limit and larger estimators for the upper
confidence limit. The broadest confidence interval
was given for a MCAR mechanism and 50% missing
values.
The MI and HDPS methods were both able to
generate consistent estimations of the confidence
intervals’ width in every simulation scenario. The
MI estimations were generally very consistent, even
with respect to both interval limits, but not only
regarding the width of the interval. Although both
confidence limits were estimated too large by the
HDPS method, the width of the interval stayed
relatively consistent.
As already described, the inaccurate estimation of
confidence limits by the CCA strategy differed
considerably from the biased estimation of the
confidence limits by HDPS. Whereas the HDPS
method generated too large values of both
confidence limits, CCA estimated confidence
intervals which were too wide, especially for higher
rates of missing values. The significant impact of
LVEF to the occurrence of a cardiac event was kept
up by applying a MI approach to the incomplete
data, since the estimation of the upper confidence
limit was below 1 in each scenario. For missing
value rates of 20% and higher, the HDPS and CCA
strategies suggested that LVEF was not a significant
predictor of a cardiac event, since the 95%
confidence interval of the hazard ratio included 1.
Table 4 shows the mean c-statistic of each HDPS
simulation scenario. As expected, the c-value which
can be used to describe the ability of the logistic
regression model to model the relationship between
the completely observed covariables and the
missing data indicator variable, was just above 50%
How to Cite this Article:Dr. Benjamin Mayer “Hot Deck Propensity Score Imputation For Missing Values,” Science Journal of Medicine and Clinical Trials,
Volume 2013 (2013), Article ID sjmct-248, Issue 2, 18 Pages, doi: 10.7237/sjmct/248
Science Journal of Medicine & Clinical Trial ISSN: 2276-7487
(0.54-0.59) in case of a MCAR assumption. The
extent of the c-value was negatively correlated with
the number of missing values in the data set.
Assuming a MAR mechanism, the expectation of
higher values of the c-statistic was also confirmed
(0.79-0.82), whereas there seemed to be no
correlation with the rate of missing data.
Another very important finding was that the HDPS
and MI approaches are both able to estimate the
hazard ratios and corresponding confidence
intervals of all other variables consistently, while
CCA led to severely biased estimates for higher
rates of missing values (see Appendix).
4.2 Binary Simulation Variable
The simulations for the dichotomous variable
‘glycosides intake’ resulted in -at least- slightly
biased estimates of the hazard ratio and confidence
interval limits. All investigated strategies to handle
missing data revealed precision problems even for
smaller rates of missing data.
HDPS underestimated glycosides effect size by
tendency, as well as the corresponding upper and
lower limits of the confidence interval. The extent
depended on the underlying missing data
mechanism, whereas the results were a bit more
biased in case of MCAR (maximal deviation is
1.3919 vs. 1.970). The width of the confidence
interval, however, was estimated consistently for
almost every scenario. For the highest rates of
missing values, the width was estimated a bit too
narrow, and the interval did not contain the true
effect size anymore.
The MI approach also underestimated the effect size
in all scenarios, and the confidence interval as well.
8
Like for HDPS, the Multiple Imputation method also
brought out consistent estimations for the width of
the confidence interval, even for high amounts of
missing values. Moreover, there seemed to be no
substantial impact of the assumed missing data
mechanism on precision of estimation.
In contrast to HDPS and MI, the CCA strategy
generated effect sizes which were overestimated,
especially if the missing data mechanism was MAR
and the amount of missing data was high.
Additionally, the corresponding confidence limits
were biased and led to interval widths which were
too large (maximum at 50% and MAR).
Again, as in case of a missing value imputation of
LVEF, HDPS and MI approaches led to nearly
unbiased estimations of the hazard ratios and
confidence intervals of the other predictor variables
of the Cox regression model, whereas the CCA
strategy generated substantially biased estimates,
especially for higher amounts of missing data in
‘glycosides intake’ (see Appendix).
The values of the c-statistic were similar to those
from the imputation of LVEF. For MCAR, the range
was again 0.54 to 0.59 and confirmed again the
expectation that the logistic regression model was
not able to find a meaningful relationship between
the predictor variables and the missing data
indicator variable when the data were MCAR. In
case of MAR, the values ranged from 0.79 to 0.83.
For the dichotomous variable ‘glycosides intake’
additionally the fraction of accordances among
original and imputed values was investigated. This
rate was negatively correlated with the amount of
missing data for both, HDPS (0.51 to 0.95) and MI
(0.75 to 0.98), whereas the MI approach brought
out more accordance. Overall, these values were
higher in case of a MAR mechanism.
Table 1: Patient characteristics of the analysis set for the extended evaluation of the SPICE study
How to Cite this Article:Dr. Benjamin Mayer “Hot Deck Propensity Score Imputation For Missing Values,” Science Journal of Medicine and Clinical Trials,
Volume 2013 (2013), Article ID sjmct-248, Issue 2, 18 Pages, doi: 10.7237/sjmct/248
Science Journal of Medicine & Clinical Trial ISSN: 2276-7487
Gender (n(%))
Female
Male
Age (mean (SD)) [years]
Smoking (n(%))
9
Complete cases of the SPICE data set
(n=2170)
345 (16%)
1825 (84%)
59.8 (10.5)
Non-smoker
986 (45%)
Smoker
953 (44%)
Ex-smoker
NYHA class
I
II
III
Body mass index (mean (SD)) [kg/m²]
Left ventricular ejection fraction (mean (SD)) [%]
Cardioactive medications (n (%))
231 (11%)
8 (0.4%)
1225 (56%)
937 (43%)
26.8 (3.7)
23.8 (6.6)
Glycosides
1228 (57%)
Nitrates
1224 (56%)
Beta Blockers
1395 (64%)
Antiarrhythmics
Diuretics
Calcium antagonists
476 (22%)
1859 (86%)
26 (1%)
Table 2: Explanatory variables for the risk of a cardiac event in patients with congestive heart failure
How to Cite this Article:Dr. Benjamin Mayer “Hot Deck Propensity Score Imputation For Missing Values,” Science Journal of Medicine and Clinical Trials,
Volume 2013 (2013), Article ID sjmct-248, Issue 2, 18 Pages, doi: 10.7237/sjmct/248
Science Journal of Medicine & Clinical Trial ISSN: 2276-7487
Explanatory variable
10
Glycosides (yes vs. no)
increased
risk for
yes
1.970
[1.636 , 2.372]
<0.0001
NYHA class (III vs. II)
class III
1.602
[1.357 , 1.892]
<0.0001
Diuretics (yes vs. no)
yes
Antiarrhythmics (yes vs. no)
yes
Nitrates (yes vs. no)
yes
Age
yes
Calcium antagonists(yes vs. no)
yes
LVEF
95% CI
1.947
low LVEF
p-value
[1.636 , 2.317]
1.426
older age
Beta Blockers (yes vs. no)
HR
[1.203 , 1.690]
1.775
[1.249 , 2.521]
1.015
[1.007 , 1.023]
1.312
[1.105 , 1.559]
2.233
[1.316 , 4.136]
0.985
[0.974 , 0.997]
<0.0001
<0.0001
0.0014
0.0004
0.0020
0.0037
0.0177
Table 3: Simulation results for the continuous variable LVEF. Denoted are (averaged over all simulations)
the hazard ratio and corresponding 95% confidence interval for LVEF
HR
MCAR
LCL
HR
0.997
0.985
Original results
0.985
5%
HDPS
0.9861 0.9742 0.9981
CCA
0.9854 0.9729 0.9981
10%
20%
30%
CCA
MI
HDPS
MI
CCA
HDPS
MI
0.974
0.9855 0.9733 0.9978
0.9855 0.9736 0.9975
0.9867 0.9748 0.9988
0.9854 0.9735 0.9974
0.9855 0.9722 0.9989
0.9881 0.9761 1.0001
0.9854 0.9735 0.9975
CCA
0.9855 0.9712 0.9999
MI
0.9854 0.9734 0.9975
HDPS
MAR
LCL
UCL
0.9893 0.9774 1.0014
0.974
UCL
0.997
0.9856 0.9733 0.9980
0.9863 0.9744 0.9984
0.9855 0.9736 0.9976
0.9858 0.9731 0.9987
0.9874 0.9755 0.9994
0.9856 0.9737 0.9977
0.9862 0.9724 1.0002
0.9894 0.9774 1.0015
0.9859 0.9740 0.9979
0.9863 0.9714 1.0015
0.9905 0.9785 1.0027
0.9859 0.9740 0.9979
How to Cite this Article:Dr. Benjamin Mayer “Hot Deck Propensity Score Imputation For Missing Values,” Science Journal of Medicine and Clinical Trials,
Volume 2013 (2013), Article ID sjmct-248, Issue 2, 18 Pages, doi: 10.7237/sjmct/248
Science Journal of Medicine & Clinical Trial ISSN: 2276-7487
40%
50%
11
CCA
0.9854 0.9701 1.0010
0.9868 0.9703 1.0036
MI
0.9852 0.9732 0.9973
0.9858 0.9739 0.9978
HDPS
0.9907 0.9787 1.0028
CCA
0.9923 0.9802 1.0045
0.9853 0.9685 1.0024
HDPS
0.9868 0.9703 1.0037
0.9919 0.9799 1.0040
MI
0.9933 0.9812 1.0055
0.9852 0.9733 0.9974
0.9863 0.9744 0.9983
Table 4: C-statistic from the logistic regression model. Denoted is (averaged over all simulations) the cvalue of the logistic regression model before HPDS imputation for LVEF.
C-statistic
MCAR
MAR
5%
10%
20%
30%
40%
50%
0.591
0.567
0.550
0.543
0.541
0.540
0.804
0.810
0.824
0.790
0.826
0.820
Table 5: Simulation results for the binary variable glycosides intake. Denoted are (averaged over all
simulations) the hazard ratio and corresponding 95% confidence interval for glycosides intake.
MCAR
Original results
5%
10%
20%
CCA
HDPS
MI
CCA
HDPS
MI
CCA
HDPS
MI
CCA
MAR
HR
LCL
UCL
HR
LCL
UCL
1.970
1.636
2.372
1.970
1.636
2.372
1.9719 1.6297 2.3860
1.8938 1.5762 2.2753
1.9533 1.6226 2.3516
1.9726 1.6217 2.3995
1.8212 1.5189 2.1837
1.9369 1.6093 2.3311
1.9749 1.6040 2.4316
1.6956 1.4190 2.0261
1.8954 1.5761 2.2794
1.9780 1.5833 2.4712
1.9759 1.6321 2.3921
1.8974 1.5781 2.2812
1.9566 1.6252 2.3557
1.9836 1.6270 2.4185
1.8159 1.5129 2.1796
1.9371 1.6096 2.3312
2.0062 1.6192 2.4856
1.6797 1.4033 2.0106
1.9019 1.5821 2.2864
2.0196 1.6037 2.5434
How to Cite this Article:Dr. Benjamin Mayer “Hot Deck Propensity Score Imputation For Missing Values,” Science Journal of Medicine and Clinical Trials,
Volume 2013 (2013), Article ID sjmct-248, Issue 2, 18 Pages, doi: 10.7237/sjmct/248
Science Journal of Medicine & Clinical Trial ISSN: 2276-7487
30%
40%
50%
12
HDPS
1.5832 1.3290 1.8859
1.5779 1.3212 1.8846
CCA
1.9855 1.5606 2.5262
2.0456 1.5867 2.6373
MI
HDPS
MI
CCA
HDPS
MI
1.8649 1.5520 2.2410
1.4855 1.2503 1.7650
1.8421 1.5332 2.2134
1.9898 1.5277 2.5918
1.3919 1.1742 1.6499
1.8040 1.5017 2.1672
1.8768 1.5624 2.2544
1.4767 1.2387 1.7604
1.8423 1.5339 2.2128
2.0658 1.5608 2.7342
1.3959 1.1730 1.6612
1.8228 1.5173 2.1900
Table 6: Biased CCA estimates of confidence interval width due to 50% missing data in LVEF under
MAR assumption.
Explanatory variable
Glycosides (yes vs. no)
increased
risk for
yes
imputation
method
yes
class III
MI
1.980 [1.644 , 2.384]
CCA
MI
CCA
HDPS
Nitrates (yes vs. no)
yes
1.970 [1.636 , 2.372]
2.046 [1.585 , 2.641]
HDPS
NYHA class (III vs. II)
95% CI
CCA
HDPS
Antiarrhythmics (yes vs. no)
HR
MI
CCA
HDPS
1.981 [1.645 , 2.385]
1.947 [1.636 , 2.317]
1.925 [1.502 , 2.467]
1.947 [1.636 , 2.318]
1.945 [1.634 , 2.315]
1.602 [1.357 , 1.892]
1.617 [1.253 , 2.086]
1.618 [1.370 , 1.912]
1.603 [1.357 , 1.894]
1.426 [1.203 , 1.690]
1.381 [1.088 , 1.754]
1.425 [1.202 , 1.690]
How to Cite this Article:Dr. Benjamin Mayer “Hot Deck Propensity Score Imputation For Missing Values,” Science Journal of Medicine and Clinical Trials,
Volume 2013 (2013), Article ID sjmct-248, Issue 2, 18 Pages, doi: 10.7237/sjmct/248
Science Journal of Medicine & Clinical Trial ISSN: 2276-7487
Diuretics (yes vs. no)
13
yes
MI
1.419 [1.197 , 1.682]
CCA
1.777 [1.154 , 2.739]
HDPS
Age
older age
MI
CCA
HDPS
Beta Blockers (yes vs. no)
yes
MI
CCA
HDPS
Calcium antagonists (yes vs. no)
yes
MI
CCA
HDPS
LVEF
low LVEF
MI
CCA
HDPS
MI
1.775
[1.249 , 2.521]
1.797
[1.265 ,2.553]
1.777 [1.251 , 2.524]
1.015 [1.007 , 1.023]
1.015 [1.004 , 1.026]
1.014 [1.006 , 1.022]
1.014 [1.006 , 1.022]
1.312 [1.105 , 1.559]
1.268 [0.992 , 1.620]
1.316
[1.108 , 1.564]
2.233
[1.316 , 4.136]
1.320
2.540
2.333
2.322
[1.111 , 1.569]
[1.212 , 5.347]
[1.316 , 4.137]
[1.309 , 4.119]
0.985 [0.974 , 0.997]
0.986 [0.970 , 1.003]
0.993 [0.981 , 1.005]
0.986 [0.974 , 0.998]
Table 7: Biased CCA estimates of confidence interval width due to 50% missing data in glycosides
intake under MAR assumption.
How to Cite this Article:Dr. Benjamin Mayer “Hot Deck Propensity Score Imputation For Missing Values,” Science Journal of Medicine and Clinical Trials,
Volume 2013 (2013), Article ID sjmct-248, Issue 2, 18 Pages, doi: 10.7237/sjmct/248
Science Journal of Medicine & Clinical Trial ISSN: 2276-7487
Explanatory variable
Glycosides (yes vs. no)
14
‘
increased
risk for
yes
imputation
method
CCA
HDPS
Antiarrhythmics (yes vs. no)
yes
MI
CCA
HDPS
NYHA class (III vs. II)
class III
MI
CCA
HDPS
Nitrates (yes vs. no)
yes
MI
CCA
HDPS
Diuretics (yes vs. no)
yes
MI
CCA
HDPS
Age
older age
MI
CCA
HDPS
Beta Blockers (yes vs. no)
yes
MI
HR
95% CI
1.970
[1.636 , 2.372]
1.395
[1.173 , 1.661]
2.065
1.822
1.947
1.921
1.866
1.894
1.602
1.627
1.634
1.612
1.426
1.372
1.379
1.420
1.775
1.782
2.180
1.869
1.015
[1.560 , 2.734]
[1.517 , 2.190]
[1.636 , 2.317]
[1.459 , 2.529]
[1.568 , 2.221]
[1.592 , 2.255]
[1.357 , 1.892]
[1.192 , 2.223]
[1.383 , 1.931]
[1.365 , 1.904]
[1.203 , 1.690]
[1.053 , 1.787]
[1.163 , 1.635]
[1.197 , 1.684]
[1.249 , 2.521]
[1.120 , 2.839]
[1.546 , 3.075]
[1.318 , 2.651]
[1.007 , 1.023]
1.015 [1.003 , 1.028]
1.013 [1.005 , 1.021]
1.014 [1.005 , 1.022]
1.312
[1.105 , 1.559]
How to Cite this Article:Dr. Benjamin Mayer “Hot Deck Propensity Score Imputation For Missing Values,” Science Journal of Medicine and Clinical Trials,
Volume 2013 (2013), Article ID sjmct-248, Issue 2, 18 Pages, doi: 10.7237/sjmct/248
Science Journal of Medicine & Clinical Trial ISSN: 2276-7487
15
CCA
1.256
[0.957 , 1.647]
MI
1.291
[1.087 , 1.534]
HDPS
Calcium antagonists (yes vs. no)
yes
CCA
HDPS
LVEF
low LVEF
MI
2.233
2.615
2.320
2.281
0.985
CCA
0.987
MI
0.984
HDPS
5.0 Discussion
1.221
0.984
[1.029 , 1.449]
[1.316 , 4.136]
[1.175 , 5.866]
[1.308 , 4.115]
[1.286 , 4.047]
[0.974 , 0.997]
[0.968 , 1.005]
[0.972 , 0.996]
[0.972 , 0.996]
The presence of missing data is a common problem
in medical research. However, there is no unique
How to Cite this Article:Dr. Benjamin Mayer “Hot Deck Propensity Score Imputation For Missing Values,” Science Journal of Medicine and Clinical Trials,
Volume 2013 (2013), Article ID sjmct-248, Issue 2, 18 Pages, doi: 10.7237/sjmct/248
Science Journal of Medicine & Clinical Trial ISSN: 2276-7487
proposal to handle missing values yet which is
supposed to be appropriate in every kind of
‘missing data situation’. This circumstance is
especially reflected in a respective guideline
(European Medicines Agency, 2010) which just
summarizes the problems of missing values for data
analysis and some established strategies and
methods which can be applied to incomplete data.
Therefore, improving the existing methods and
developing new ones, respectively, should be aimed
in this important research field of medical statistics.
According to literature, methods of the MI strategy
are viewed as state of the art today (Engels and
Diehr, 2003; Newman, 2003; Schafer and Graham,
2002; White et al., 2011) because they lead to less
biased results with respect to the behaviour of
parameter estimates and respective confidence
intervals. In contrast, pragmatic SI methods, like
mean or regression imputation, are not proposed
anymore since they underestimate variance by
tendency. MI overcomes this problem by imputing
missing values m > 1 times, so the imputation itself
as an additional source of variance is explicitly
considered at the estimation process (Rubin, 1987).
Whenever missing values are present, an
imputation strategy is indeed much more
reasonable than just deleting incomplete cases from
the data set, although Vach and Blettner (1991)
showed that this CCA strategy generates unbiased
estimates in case of a MCAR mechanism. However,
the loss of statistical power can be tremendous
when the number of examined variables is high.
Major restrictions to available imputation methods
are their inappropriateness in case of a MNAR
mechanism and their sensitivity against the number
of missing values in a data set, whereas common MI
methods even work well in case of higher amounts
of missing values up to 50% (Engels and Diehr,
2003; Mayer, 2011). Further, each of the established
imputation methods is only applicable for a certain
kind of scale level. The MCMC method, for example,
can only be applied to continuous variables with
missing items, and the Logistic method is only
appropriate for imputing binary variables. In
practice, often more than one variable are affected
by missing values, so one has to apply different
imputation methods to fill the data set. These
distinct methods, however, have different
presumptions with respect to the structure of the
data set which may lead to a complex imputation
process in total. Moreover, many researchers are
not too familiar with possibilities to impute missing
data, so the utilization of different imputation
methods maybe confusing. On the other hand, there
16
is the Fully Conditional Specification (FCS) method
(van Buuren, 2007) which can perform a MI for
variables with either continuous or categorical scale
level, but this approach is some kind of a black box
since the underlying algorithm is quite complex.
Knowing these facts, the development of new and
easily understandable methods for imputing
missing values should preferably include a MI
methodology which can be applied to variables of
different scale levels. The proposed HDPS method
for missing value imputation combines both. A
propensity score approach is used to create a
respective donor pool of possible imputation values
for each missing observation of the data set, so the
HDPS method can be implemented in a MI setting
by multiply choosing one donor value (at random)
out of the pool. On the one hand, the donor pool
which is generated by those 10 donors which have a
PS most next to the respective PS of the recipient
must not be too large because then the similarity
assumption does not hold anymore. On the other
hand, however, the donor pool must not be too
small since there should be enough variability in the
donor data to get valid MI estimates. Choosing those
10 donors’ PS which are most next to the respective
recipient PS seemed to be an acceptable approach
for the initial implementation of the HDPS
procedure.
The simulation study showed that the HDPS method
can easily be applied to different types of
incomplete variables. To apply a standard MI
approach instead, the implementation of different
methods (MCMC or Logistic) is necessary. However,
the validity of parameter estimation is much better
for standard MI approaches which are almost
unbiased, even in case of high amounts of missing
data. Especially the simulations for the binary
variable show that HDPS and MI generate rather
conservative estimations by tendency in contrast to
a CCA approach which estimates higher hazard
ratios and confidence intervals in nearly all
scenarios. But although HDPS, as well as MI, leads to
hazard ratio estimates that are too low, the width of
the corresponding confidence intervals is validly
estimated. In comparison, CCA produces severely
biased estimates of the confidence interval widths.
This mainly traces back to the reduced sample size
for the respective analysis. Another very important
finding is that HDPS, also as well as standard MI
approaches, is able to generate unbiased parameter
estimates for all other variables which are included
in the original Cox regression model (see Appendix),
How to Cite this Article:Dr. Benjamin Mayer “Hot Deck Propensity Score Imputation For Missing Values,” Science Journal of Medicine and Clinical Trials,
Volume 2013 (2013), Article ID sjmct-248, Issue 2, 18 Pages, doi: 10.7237/sjmct/248
Science Journal of Medicine & Clinical Trial ISSN: 2276-7487
whereas CCA produces invalid estimations for most
of the other variables instead.
For both simulation variables, the c-values are
negatively correlated with the number of missings
in the data set in case of a MCAR mechanism. There
are much higher values in case of a simulated MAR
mechanism, but that was the expectation in advance
since the mechanism has been created artificially
from the data. However, there seems to be no
relation between the goodness of fit of the logistic
regression model (i.e. the ability of the model to
separate cases with missing items from those with
complete data by doing a regression of the missing
data indicator variable and all completely observed
covariates) and the validity of estimation. Besides,
the fraction of correctly imputed values in case of
the binary simulation variable is negatively
correlated with the number of missing values in the
data set. Thus, the HDPS method can produce valid
imputations for binary variables only in case of
lower amounts of missing data.
In practice, it is unlikely that only one variable is
affected by missing values, so the handling of
missing data in multiple variables is an important
issue. Thus, an application of the proposed HDPS
approach in such data situations should be
discussed at least. For this initial implementation of
the method and the conducted simulation study,
respectively, only one variable was assumed to have
missing items. The main focus of the article was to
present the newly developed procedure for missing
value imputation, so the first setting of the
simulation study was restricted to only one partially
missing variable to see the properties of HDPS
imputation. The conception of HDPS allows from a
theoretical point of view quite easily its application
in situations with multiply incomplete variables. As
already showed, the method can deal with different
types of missing data variables by using a missing
data indicator variable to create propensity scores
on the basis of all completely observed variables of
a data set. This proceeding can be conducted
repeatedly for each incomplete variable without
further theoretical problems regarding the
imputation procedure. However, one has to discuss
the presumptions with respect to available data in
general. The presented data set includes a huge
number of cases, and therefore the implementation
of the logistic model is unproblematic. If the
investigated data set is much smaller, however, a
valid estimation of PS may be doubtful. But it is
actually very difficult to give an advice at this point
up to which amount of observations the HDPS
17
method can be applied validly. Further research is
necessary here where the proposed method should
be applied to data sets of different sizes.
The simulations showed that there seems to be no
relation between goodness of fit of the logistic
regression model and the validity of estimations for
the HDPS procedure. Otherwise, one should has
been able to observe an increase of estimation
precision in case of MAR compared to MCAR since
the c-values have been much higher for MAR.
However, it should at least be examined within
further investigations what happens to estimation
precision, if the establishment of the logistic
regression model is modified with respect to the
included predictors. Moreover, the performance of
the HDPS procedure in a MNAR setting would give
useful advices regarding the extent of bias of
parameter estimates. And above that, of course,
efforts to prove the method’s ability to produce
acceptable estimations in case of multiply
incomplete
analysis
variables
should
be
undertaken.
The main conclusion of this article is that the
proposed HDPS approach can be easily applied to
different types of incomplete variables regarding
their scale level, which is a major advantage against
most of the established imputation methods which
are one only applicable to certain types of variables.
Although the simulation results showed that HDPS
estimations for the imputed variable were rather
conservative in a sense that the real effect was
underestimated by tendency, the method was able
to produce unbiased estimates for all other included
covariates of the original analysis model. Further
investigations are needed, however, to check for
possible improvements with respect to estimation
precision, for the method’s performance in data sets
of different structures, and for its application in
estimating distinct outcome variables.
Acknowledgements
The study was funded by the young scientists
program of the German network 'Health Services
Research Baden-Wuerttemberg' of the Ministry of
Science, Research and Arts in collaboration with the
Ministry of Employment and Social Order, Family,
Women and Senior Citizens, Baden-Wuerttemberg.
The data for the simulation study have been kindly
provided by Dr Willmar Schwabe Pharmaceuticals,
Karlsruhe, Germany. Thank you very much for that.
I also appreciate the support of Silvia Sander at the
implementation of the SAS macro for HDPS
How to Cite this Article:Dr. Benjamin Mayer “Hot Deck Propensity Score Imputation For Missing Values,” Science Journal of Medicine and Clinical Trials,
Volume 2013 (2013), Article ID sjmct-248, Issue 2, 18 Pages, doi: 10.7237/sjmct/248
Science Journal of Medicine & Clinical Trial ISSN: 2276-7487
imputation. Finally, I thank the independent
reviewers for their valuable comments which really
improved the manuscript.
References
1.
2.
3.
4.
5.
6.
7.
Allison, P.D. Multiple imputation for missing
data: A cautionary tale. Sociological Methods and
Research 2000; 28: 301–309
Allison, P.D. Missing Data. Sage University
Papers Series on Quantitative Applications in
the Social Sciences, Thousand Oaks, CA, 2001,
07-136
Andridge, R.R. and Little, R.J.A. A Review of Hot
Deck Imputation for Survey Non-response.
International Statistical Review 2010, 78, 1: 4064
D’Agostino, R.B. Propensity Score Methods for
Bias Reduction in the Comparison of a
Treatment to a non-randomized Control Group.
Statistics in Medicine 1998, 17, 2265-2281
Engels, J.M. and Diehr P. Imputation of missing
longitudinal data: a comparison of methods.
Journal of Clinical Epidemiology 2003, 56: 968976
European Medicines Agency. Guideline on
Missing Data in Confirmatory Clinical Trials.
2010
Guo, S., Fraser, M.W. Propensity score analysis:
statistical methods and applications. SAGE
Publications, Inc., Thousand Oaks, 2010
18
11. Little, R.J.A. and Rubin, D.B. Statistical Analysis
with Missing Data. John Wiley & Sons, Hoboken,
New Jersey, 2002
12. Mayer, B. Missing Values in clinical longitudinal
studies – Handling of Drop-outs. Dissertation at
the University of Ulm (in German), 2011
(http://vts.uniulm.de/docs/2011/7633/vts_7633_10939.pdf)
13. Mayer, B., Holubarsch, C., Muche, R., Gaus, W.
Prognostic Factors for Patients with Congestive
Heart Failure – An Extended Evaluation of the
SPICE-Study. In revision at British Journal of
Medicine and Medical Research 2013
14. Mittinty, M., Chacko, E. Imputation by Propensity
Matching. Proceedings of the Survey Research
Methods Section, ASA 2004: 4022-4028
15. Newman, D.A. Longitudinal Modelling with
Randomly and Systematically Missing Data: A
Simulation of Ad Hoc, Maximum Likelihood and
Multiple Imputation Techniques. Organizational
Research Methods 2003, 6: 328
16. Rosenbaum, P.R., Rubin, D.B. The central role of
the propensity score in observational studies for
causal effects. Biometrika 1983, 70: 41-55
17. Rubin,
D.B.
Multiple
Imputation
for
Nonresponse in Surveys. John Wiley & Sons,
Hoboken, New Jersey, 1987
18. Schafer, J.L., Graham, J.W. Missing data: our view
of the state of the art. Psychological Methods
2002, 7: 147-177
Haziza, D., Beaumont, J.F. On the Construction of
Imputation Classes in Surveys. International
Statistical Review 2007, 75: 25-43
19. Vach, W., Blettner, M. Biased estimation of the
odds ratio in case-control studies due to the use
of ad hoc methods of correcting for missing
values for confounding variables. American
Journal of Epidemiology 1991, 134: 895-907
10. Little, R.J.A. Survey Nonresponse Adjustments
for Estimates of Means. International Statistical
Review 1986, 54: 139-157
21. White, I.R., Royston, P., Wood, A.M. Multiple
imputation using chained equations: Issues and
guidance for practice. Statistics in Medicine
2011, 30: 377-399
8.
9.
Holubarsch C.J.F., Colucci W.S., Meinertz T., Gaus
W., Tendera M. The efficacy and safety of
Crataegus extract WS® 1442 in patients with
heart failure: The SPICE trial. European Journal
of Heart Failure 2008, 10: 1255–1263
20. van Buuren S. Multiple imputation of discrete
and continuous data by fully conditional
specification. Statistical Methods in Medical
Research 2007, 16: 219-242
How to Cite this Article:Dr. Benjamin Mayer “Hot Deck Propensity Score Imputation For Missing Values,” Science Journal of Medicine and Clinical Trials,
Volume 2013 (2013), Article ID sjmct-248, Issue 2, 18 Pages, doi: 10.7237/sjmct/248