Document 10980690
advertisement
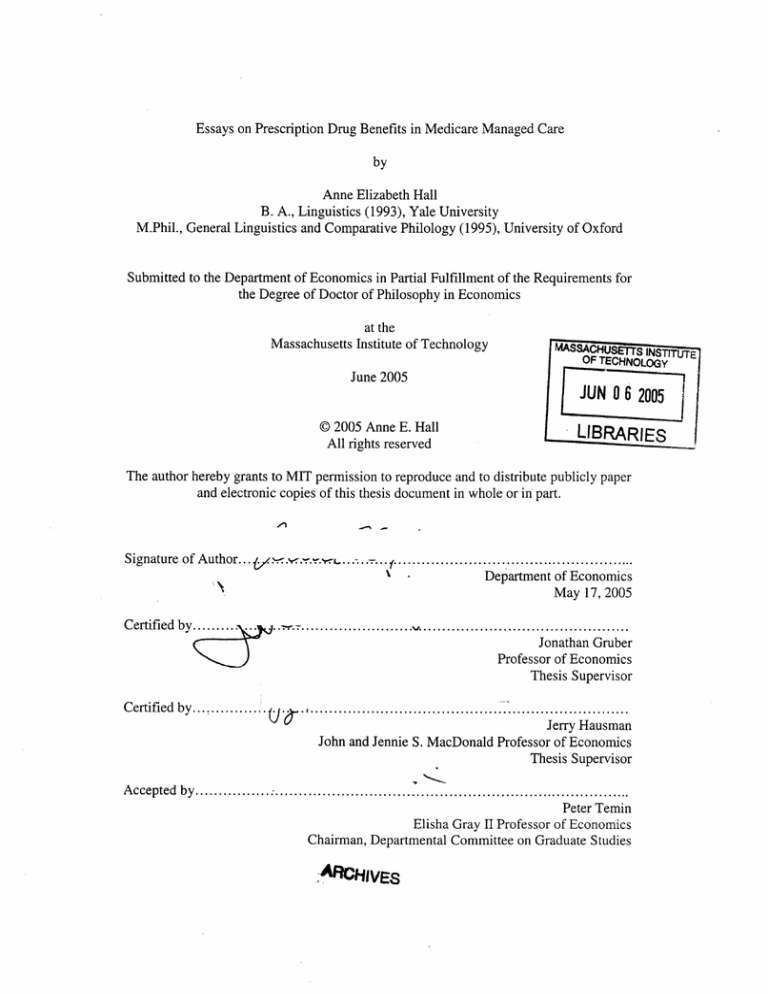
Essays on Prescription Drug Benefits in Medicare Managed Care
by
Anne Elizabeth Hall
B. A., Linguistics (1993), Yale University
M.Phil., General Linguistics and Comparative Philology (1995), University of Oxford
Submitted to the Department of Economics in Partial Fulfillment of the Requirements for
the Degree of Doctor of Philosophy in Economics
at the
Massachusetts Institute of Technology
iNS
OF TEHOO
E
Y
June 2005
JUN 06
LIB
( 2005 Anne E. Hall
RIES
All rights reserved
The author hereby grants to MIT permission to reproduce and to distribute publicly paper
and electronic copies of this thesis document in whole or in part.
x
Signature of Author....y
..........-.
.........
....................................................
x\
~~~~~~~~\>~~
~
Departmentof Economics
~May
17, 2005
Certified
by........................................................
Jonathan Gruber
Professor of Economics
Thesis Supervisor
Certified by .......
.i
....
Jerry Hausman
John and Jennie S. MacDonald Professor of Economics
Thesis Supervisor
Accepted by................
.............................................................................
Peter Temin
Elisha Gray II Professor of Economics
Chairman, Departmental Committee on Graduate Studies
-ARCHIVES
05
Essays on Prescription Drug Benefits in Medicare Managed Care
by
Anne Elizabeth Hall
Submitted to the Department of Economics in Partial Fulfillment of the Requirements for
the Degree of Doctor of Philosophy of Economics
ABSTRACT
In this thesis, I estimate a structural demand model for prescription drug benefits by
Medicare beneficiaries using data from the Medicare HMO program. I then use the utility
parameter estimates to explore other questions of interest relating to the elderly's demand
for prescription drug benefits.
In Chapter 1, I study the question of how much Medicare beneficiaries value prescription
drug benefits. Using data from the Medicare HMO program, I find that Medicare
beneficiaries are willing to pay $33 to increase their brand-name coverage limit by $100.
I also estimate marginal cost for each HMO and regress it on prescription drug benefits. I
find that raising brand-name coverage by $100 costs $30. These estimates suggest that
Medicare HMO enrollees are less than average prescription drug users and the results
give a lower bound for the welfare derived by the elderly from prescription drug benefits.
Chapter 2 addresses the question of how Medicare HMOs' choices of premiums and
benefits affect selection. Changes in demographic factors (a measure of risk based on
beneficiaries' characteristics) and risk scores (a measure based on beneficiaries' inpatient
diagnoses) in the fee-for-service sector are regressed on changes in premiums and
benefits in the HMO sector. The results show that increasing premiums and lowering
benefits raise the demographic factor but have no effect on the risk score, suggesting that
beneficiaries in more expensive demographic categories switch out of HMOs when
premiums rise and benefits fall but these beneficiaries are healthy for their demographic
category.
Chapter 3 measures the welfare loss from the withdrawals from the HMO program
following the Balanced Budget Act of 1997, using the utility parameter estimates from
Chapter 1. The changes to the Medicare HMO program in the Balanced Budget Act
triggered many plan withdrawals from the program. The welfare and costs are calculated
under two counterfactual scenarios. The results show that the Medicare HMO program
generates more welfare than costs and that the withdrawals resulted in a net loss for
society. The estimates of the loss range from $4.3 billion to $16.6 billion.
Thesis Supervisor: Jonathan Gruber
Title: Professor of Economics
Thesis Supervisor: Jerry Hausman
Title: John and Jennie S. MacDonald Professor of Economics
3
4
Acknowledgments
This thesis would not have been possible without the support and contributions of many
people and I would like to take this opportunity to acknowledge them in print.
My advisors, Jon Gruber and Jerry Hausman, both gave helpful advice and feedback
throughout all stages of researching and writing this thesis. I am deeply appreciative of the time
and effort they both put into advising me. In addition, their constant support and enthusiasm kept
my spirits up, and I never came out of a discussion with either of them without feeling more
inspired and hopeful about my work than when I came in.
Both of my parents gave me an enormous amount of support throughout graduate school,
even when I abandoned one Ph.D. and took up another. Not many parents would have been as
sympathetic to their children's career crises as mine were and I will always be grateful. Their
biggest contribution, however, was in raising me to enjoy learning and appreciate scholarly work.
My mother also contributed by reading drafts and providing feedback.
Ernie Berndt has always gone beyond the call of duty in giving me support and advice all
throughout graduate school, and by giving me the opportunity to teach and helping with my job
search. David Cutler and Jim Poterba were also particularly helpful with this thesis and
throughout my graduate career. Glenn Ellison and Joe Newhouse also gave helpful feedback for
Chapter
1.
My classmates at MIT and my graduate student colleagues at the NBER provided tons of
companionship, support and feedback. I'd particularly like to thank Melissa Boyle, Lesley Chiou,
Norma Coe, Dan Hungerman, Srikanth Kadiyala, Patricia Keenan, Joanna Lahey, Ha Yan Lee,
Byron Lutz, Grant Miller, Erich Muehlegger, and Cindy Perry. Their friendship has been
invaluable; they made graduate school bearable, and even occasionally fun.
The support staff at the NBER were amazingly helpful, particularly Donna Hicks and
Janet Stein, who administered my fellowship, and Dan Feenberg and Mohan Ramanujan, who
provided excellent computer support. Gary King at MIT was also incredibly helpful and always
shared his vast knowledge of how things work at MIT.
My brothers Chris, Jonathan, and Andrew, my stepmother Susan, my stepsister Sonja,
and her husband Evan, were all tremendously supportive throughout. My extended family was
also, particularly those who live in the Boston area: my cousin Cathy and her husband Johan, my
aunt Betty and uncle Pat, and my cousin Ch'uya and her husband Dave, all provided advice,
support, and endless free dinners.
My non-economist friends (and I'm amazed I still have some) have been incredibly
supportive and patient, even when I disappeared for months on end to study for generals or work
on my job-market paper. Thanks especially to Lois and Timur, Kasey, Chris, Mike, Renate,
Stephanie, Maria, and Ron. Thanks also to the other members of Chorus pro Musica for giving
me a life outside economics.
Finally, it would be species-ist of me not to recognize Persephone and Ulysses for
relieving stress, for getting me up in the morning, and for generally helping out, especially with
the important tasks of sleeping on my desk and walking across the computer keyboard when I am
trying to work.
Funding from the National Institute on Aging, through Grant Number T32-AG 00186 to
the National Bureau of Economic Research, is gratefully acknowledged.
5
6
Table of Contents
Chapter 1: Estimating the Demand for Prescription Drug Benefits by Medicare Beneficiaries
I. Introduction
9
II. Background: The Medicare HMO Program
III. A model of demand for Medicare HMO coverage and prescription drug
11
coverage
12
IV. Data on the Medicare HMO program
14
V. Data on prescription drug benefits
17
VI. Empirical strategy
20
VII. Demand parameter estimates
VIII. Welfare estimates
IX. The cost of supplying prescription drug benefits
23
27
32
X. Conclusion
References
Table 1a
Table 1b
Table 2a
Table 2b
Table 3
Table 4
Table 5
Table 6
36
38
40
41
42
43
45
45
46
49
Table 7
51
Table 8
52
Table 9
53
Table 10
54
Chapter 2: Medicare HMOs, Prescription Drug Benefits, and Selection
I. Introduction
II. Previous work
56
59
III. A model of plan choice by Medicare beneficiaries
IV. Data on Medicare HMOs and risk in the Medicare FFS sector
60
63
V. Empirical specification
VI. Results
VII. Discussion
VIII. Conclusion
References
Figure 1
65
68
74
75
77
79
7
Figure 2
Figure 3
80
80
Table 1
81
Table 2
82
Table 3
83
Table 4
84
Table 5
85
Table 6
86
Table 7
87
88
Table 8
Chapter 3: The Welfare Loss from Medicare+Choice
I. Introduction
II. Background: The Medicare HMO Program and the Balanced Budget Act of
1997
III. My approach to estimating welfare
IV. Estimating welfare in nested logit models
V. Applying welfare estimates to the Medicare HMO market
VI. Results of welfare and cost calculations
VII. Conclusion
References
Table 1
Table 2
Table 3
89
92
96
100
101
103
106
108
109
109
110
Table 4
113
Figure 1
117
Figure 2
118
8
Chapter 1: Estimating the Demand for Prescription Drug
Benefits by Medicare Beneficiaries
I.
Introduction
Medicare, when it was passed in 1965, did not include an outpatient prescription
drug benefit. Adding such a benefit has been under debate almost since the inception of
Medicare and the debate intensified during the 1990s. Medical spending during this
decade rose more quickly than GDP and prescription drug spending rose even more
quickly than overall medical spending. In 1999, for example, GDP rose 4.8%, medical
spending rose 7.1% and prescription drug spending rose 18.4% (Strunk and Ginsburg
2004). Medicare beneficiaries who do not have prescription drug coverage, however, as
part of their supplemental coverage have no protection against prescription drug costs,
even though prescription drugs have become a larger part of medical treatment.
In December 2003, Congress passed
the Medicare Prescription
Drug
Improvement and Modernization Act, which provides a partial, voluntary drug benefit for
Medicare beneficiaries starting in 2006. Much of the debate around passing this act
centered on the costs. Estimates of the cost of this benefit over the next decade are
uncertain and range from $395 billion (from the Congressional Budget Office) to $534
billion (from the Department of Health and Human Services). There has however been
very little discussion of the potential value of the benefit; while there appears to be a
consensus that providing such a benefit is good policy, without quantification of the
welfare derived from it, there is no way of knowing what the rate of return of spending on
the drug benefit will be.
9
In this paper, I will address the question
of how much value Medicare
beneficiaries derive from having prescription drug benefits by using data from the
Medicare HMO program to estimate the demand for, costs of, and welfare implications
of prescription drug benefits for Medicare beneficiaries who enroll in Medicare HMOs. I
will be employing methods developed for estimating demand for differentiated products
using market share data used previously by Berry (1994) and Town and Liu (2003),
among others. I find that Medicare beneficiaries, on average, are willing to pay $20 a
month for Medicare HMO prescription drug benefits, $28 a month to have their brandname drug coverage raised by $100, about $0.07 a month to lower their brand-name drug
co-payment by $1 and $8 a month to have coverage outside a plan's formulary, or list of
favored drugs. The benefits cost on average $146 per person per month to provide and it
costs plans $100 to raise brand-name coverage by $100, $129 to provide non-formulary
coverage, and $0.56 to lower the brand-name co-payment by $1. The discrepancy
between valuation and cost probably arises from either adverse selection or moral hazard
combined with regulation of HMOs that constrains their profit levels and causes them to
supply benefits at a cost higher than their value to beneficiaries.
While
there have been previous
studies on the plan choices
of Medicare
beneficiaries using data from the Medicare HMO program (Dowd et al. 2003, Town and
Liu 2003 and Atherly et al. 2004), my paper is the first to examine the welfare and cost
implications of providing different levels of drug benefits. Town and Liu discuss welfare
but they consider the welfare only from having or not having a benefit, not from different
levels of benefits, nor do they consider the costs of benefits. To predict the consequences
10
of providing such a benefit however, it is necessary to understand beneficiaries' response
to different levels of benefits and the associated costs.
Section II gives some background on the Medicare HMO program, Section III
presents a model of demand for Medicare HMOs and their drug benefits, Section IV and
Section V discuss the data, Section VI presents the empirical strategy, Section VII
presents the demand parameter estimates, Section VIII the welfare estimates and Section
IX the cost estimates. Section X concludes.
II.
Background: The Medicare HMO Program
Traditional Medicare has high requirements for patient cost sharing relative to
most modern private insurance plans. Currently, Medicare requires 20% co-insurance on
most outpatient services, a high deductible ($876) on hospital stays and only covers the
first 150 days of hospitalization per year. To cover the remaining costs, a large proportion
(87%
in 1999 [Medicare
Chartbook
2001])
of beneficiaries
have some kind of
supplemental insurance. In 1999, about a third had employer-sponsored
had private Medigap insurance,
coverage, 24%
11% were on Medicaid and 17% were enrolled in a
Medicare HMO.
The Medicare HMO program was created to take advantage of the supposedly
greater efficiency of managed care plans in caring for Medicare beneficiaries.
Commercial HMOs contract with the Center for Medicare and Medicaid Services (CMS),
the agency that runs Medicare, to provide health care for Medicare beneficiaries within a
defined service area (usually a county or group of contiguous counties). The contract,
which is revised and renewed each year, specifies benefits to be provided and possibly a
11
premium
that will be charged by the HMO to the beneficiary.
The government
reimburses the HMO at a flat rate that is set at a base level by county and then adjusted
for the individual beneficiary's
age, sex, Medicaid eligibility status and employment
status. The flat rate passes on the financial risk of the beneficiary's medical care to the
HMO. Beneficiaries are allowed to enroll in HMOs or remain in traditional Medicare as
they choose and are currently allowed to switch in and out or among HMOs whenever
they want. The HMOs must either accept all enrollees or close the plan completely.
From the beneficiary's point of view, the advantage of the HMOs is that they
require less cost-sharing for the beneficiary; co-payments for doctor visits, for example,
are usually about $10-$15 per visit which is less than traditional Medicare's
20% co-
insurance. Medicare HMOs also often cover benefits that are not covered by traditional
Medicare such as preventive care and outpatient prescription drugs. On the other hand,
they are managed-care plans and therefore usually place constraints on which providers
patients can see, which traditional Medicare does not.
III.
A model of demand for Medicare HMO coverage and prescription drug
coverage
To estimate the value of drug benefits to Medicare beneficiaries,
I will first
estimate a model of demand for HMOs and their associated benefits. To do this, I will use
methods for estimating the demand for differentiated products that have been developed
and used by Berry (1994) and Town and Liu (2003). Berry, following Cardell (1997),
lays out how to estimate logit and nested logit models of demand using data on market
shares and on prices and choice characteristics.
12
I will focus on the nested logit specification but will also present results from the
logit. In the nested logit model, plans are grouped into nests, within which utility is
correlated across plans. Similar to Town and Liu, I group the choices of Medicare
beneficiaries into HMOs with drug benefits, HMOs without drug benefit and traditional
Medicare.
Utility for person i in plan j in county m at time t in this model is given as:
Uijmt
m,
jmt, +jmt
jmt + igmt +(1
)£ijmt
(1)
Pjm,is the premium paid by the beneficiary, Xjm, is a vector of observed characteristics of
the plan,
j,,, is the unobserved quality of plan j and ejmt (distributed extreme value) is an
indclividual-specificshock.
igmt +(
-
)£uijm,
is the random component of utility and is
also distributed extreme value. Cardell derives the distribution of
individual-specific
,igmt'another
shock that is the same for each individual across all plans in the same
group g (HMO with prescription drug benefits or HMO without prescription drug
benefits). are [0,1) measures the correlation of within-group utility.
In the simple logit, both
and Cigequal 0, so ijmtis the only individual-specific
shock. This specification has the prediction that, if a plan exits the market, the plan's
members move to the plan with the largest market share. This prediction holds even if the
plan that they originally chose offered drug coverage and the plan that they are predicted
to move to does not. In the nested logit model, this prediction only holds within nests and
we will see that the nested logit model fits the data better.
13
Berry shows that if utility has the specification in (1), the parameters of the utility
function can be estimated with a linear regression (omitting the subscripts m and t for
clarity):
(2)
lns -Ins0 =apj +Xj,8+lnsjlg + :j
where sj is plan j's market share and so is the market share of the outside choice, which is
defined as the choice whose utility is normalized to zero. I define the outside choice as
choosing to remain in traditional Medicare. sjig is the plan's share within its nest and the
plan quality ~j is unobserved and comprises the error term.
Data on the Medicare HMO program
IV.
Data were collected for the years 1999-2002. Market shares for Medicare HMOs
come from the Medicare Managed Care Market Penetration State/County/Plan Data files,
which
contain enrollment
Reimbursement
in Medicare
managed care plans by plan and county.
levels come from the Medicare+Choice
base reimbursement
Payment Rate files; I use the
rate for the aged in each county. Benefit and premium data come
from the Medicare Compare database, which is the source of information for the online
plan chooser for Medicare beneficiaries. All of these data sources were obtained from the
Center for Medicare and Medicaid Services (CMS), the government agency that runs
Medicare.
I had to overcome a few difficulties with the data in order to use it. First, the
enrollment data do not report enrollment by county of service area of the HMO but rather
by county of residence for the beneficiary. While beneficiaries can only enroll in an
HMO if they live in that HMO's service area, they are usually allowed to retain coverage
14
if they subsequently move outside the plan's service area. The result is that there appear
to be many more HMOs in a county than there actually are HMOs available for
beneficiaries to enroll in. Most of the HMOs have very small enrollment, however. Like
other researchers who have used these data, therefore, I have only counted an HMO as
competing in a county if its enrollment is above a certain level (25 enrollees) and I have
also only included it if the Medicare Compare database shows the HMO as being in that
county since otherwise there is no benefit or premium data for it.
The enrollment data also only give enrollment by contract number within a
county. One contract may, however, cover more than one package of benefits since
HMOs are allowed to offer more than one within a county. Usually, the offerings consist
of a "basic" plan with an optional supplement for an extra premium. Since enrollment is
not split up by packages however, I attribute all of the enrollment to the HMO's "basic"
plan (the plan with the lowest premium). (Atherly et al. [2004] report that 87% of
Medicare HMO enrollees with prescription drug coverage receive it through the plan's
basic benefit package.)
The market share was calculated by dividing the HMO's enrollment by the
number of Medicare eligibles, adjusted to reflect state-level rates of Medicaid and
employer-sponsored plan participation. These rates were calculated by pooling the March
demographic supplements for the four years, identifying respondents reporting being
covered by Medicare and then tabulating the rates at which these respondents also report
being covered by Medicaid and employer-sponsored
insurance by state. It was necessary
to use state-level rates since the sample sizes for MSAs would not have been large
enough.
15
Table 1a shows, for each year, the number of contracts, the number of counties
with at least one Medicare HMO, the number of county-contract combinations
(observations) and total enrollment in the Medicare HMO program. All of these variables
decline sharply during the period of interest. Between 1999 and 2002, the number of
contracts drops from 290 to 143, the number of counties with at least one HMO drops
from 808 to 540, the number of observations drops from 1,964 to 962 and the number of
enrollees drops from 6.1 million to 4.8 million, a drop of 21%.
The drop in overall participation in the Medicare HMO program is due to the
large number of plan withdrawals during this period. These were in turn triggered by the
Balanced Budget Act of 1997, which went into effect in 1999. The Balanced Budget Act
adjusted the formula for the base reimbursement rates so that reimbursement did not
grow as fast for many areas and, as a result, many plans dropped out.
Table lb shows summary statistics for Medicare HMOs and counties by year. The
average Medicare HMO market share in a county climbed from 6.1% to 8.1% between
1999 and 2002; this increase is due to the greater likelihood of a plan withdrawing if it
had a smaller market share. Similarly, the average enrollment in a plan climbs from 3,107
to 5,033. The HMOs with the largest shares each year have shares from 47-48% and the
plans with the greatest enrollment have enrollments of 130,000-144,000.
Traditional Medicare's market share is on average about 85% in counties where
there are HMOs and only ever drops as low as 47%, so even in counties with high HMO
enrollment, traditional Medicare is still a dominant presence. The average number of
plans in a county, conditional on there being at least one plan in the county, is about 2.5
16
in 1999 and drops to 1.8 by 2002 and the number of plans in a county ranges from
to
12.
In addition to many HMOs dropping out of the program during this period, a
further effect of reducing the reimbursement
was that the HMOs who stayed in raised
premiums faster than the rate of inflation and reduced coverage. Table 2a shows the
average premium and percent of plans offering drug benefits by year. The average
premium nearly tripled between 1999 and 2002 while at the same time the percent of
plans offering prescription drug benefits dropped from 70% in 1999 to 60% in 2001 and
then rose again to 66% in 2002.
V.
Data on prescription drug benefits
Medicare HMOs vary the generosity of their drug benefits along several axes.
They can vary in what categories of drugs they cover, the coverage limits, the number of
tiers, the amount of the co-payments, the presence of a formulary (or list of drugs favored
by the plan), and whether the formulary is open or closed.
The main distinction in pricing among drugs is whether a drug is brand-name or
generic. Brand-name drugs are still under patent and are therefore priced much higher
than generic drugs. Table 4 contains national average drug prices for both the generic and
brand-name categories for 1999-2002, and, as it shows, brand-name drugs were typically
more than three times as expensive as generic drugs during this period.
In the data, plans fall into one of five categories with regard to what classes of
drugs they cover and whether or not there is a limit on coverage. Plans can have:
*
Limited generic coverage and no brand-name coverage;
17
* Unlimited generic coverage and no brand-name coverage;
* Limited generic and brand-name coverage;
* Unlimited generic coverage and limited brand-name coverage;
* Unlimited generic and brand-name coverage.
Table 2b shows the distribution of plans across the categories. The main way in
which plans reduced their generosity during this period was by removing brand-name
drug coverage. Between 1999 and 2002, there was a marked shift from the last three
categories into the second and the percent of plans with drug benefits offering brandname coverage dropped from almost 97% to 59%. Nominal coverage amounts within the
categories remained stable over the period although the real value of the coverage
declined since prescription drug prices were rising 5-10% a year.
The co-payment is the amount per prescription paid by the plan enrollee. Drugs
are grouped by co-payment into tiers, which are usually defined by the drugs' patent
status (brand-name or generic) and whether or not the drug is in the plan's formulary. The
formulary is a list of drugs that the plan obtains at lower prices and drugs on the
formulary have lower co-payments.
In the 1999-2000 data, a plan can have up to four tiers: generic non-formulary,
brand-name non-formulary, generic formulary and brand-name formulary. In the 20012002 data, a plan can also have a fifth tier: preferred brand-name formulary, and can also
specify different co-payments for when prescription drugs are mail-ordered. Few plans
have the maximum number of tiers, however, since plans do not always cover all
categories of drugs, and often formularies apply only to brand-name drugs.
18
Plans also vary in whether or not they have a formulary
and whether the
formulary is open or closed. A formulary is open if drugs not on the formulary are
covered (at a higher co-payment). The formulary is closed if drugs not on it are not
covered at all. I group plans without formularies and plans with open formularies together
into plans offering non-formulary coverage. There is no information in the data about
what drugs are included in the formulary; rather, the beneficiary is advised to contact the
plan directly about the formulary.
For the purposes of this study, since co-payments for the different tiers are highly
correlated, I only use one generic co-payment and one brand-name co-payment from each
plan. For each category, I use the lowest co-payment available (usually the generic
formulary co-payment and the preferred brand-name co-payment). Co-payments
remained more or less stable throughout this period, as Table 2a shows; the average
generic co-payment only rises slightly from $6.70 to $8.72 while the average brand-name
co-payment remains more or less constant at $15-$16.
The bottom rows of Table 2a report averages of measure of drug expenditure
covered by insurance and out-of-pocket spending for each plan; how I calculated these
will be discussed below.
Table 3 shows the average base rate for reimbursement by year for all counties
and counties containing HMOs. These range from about $400-500 a month to $700-800
across counties and over the period in question. The average rate for counties with HMOs
is about $40 higher than the average rate for all counties. This difference is not surprising
since studies of entry and exit in the Medicare HMO industry indicate that the level of
19
reimbursement is the most important factor in HMOs' decision to offer a Medicare plan
in a county (GAO 1999, Abraham 2000, Ellis and Gurol 2002, Pai 1999, Penrod 2001).
Empirical strategy
VI.
As discussed in Section III, the regression to be estimated is:
lnSjmt -Ilnsomt =
Pjmt+ X jmt, +
alnSjlgmt
+ jt
(3)
where s is the market share, j is the plan, m is the county and t is the year (1999-2002).
Xjmt
is a vector of drug benefit characteristics, the exact specification of which will be
discussed below.
5jmt
contains unobserved characteristics of the plan that are unobserved by the
econometrician but are observed by the beneficiaries and affect their valuation of the
plan. In this case, among other things, it might take the form of the extensiveness and
quality of the HMO's provider network, which we cannot observe.
Unobserved quality is correlated with both premium and the log of the nest share.
In order to overcome this problem, I use a strategy very similar to Hausman (1996), Nevo
(2001) and Town and Liu (2003). I use plan-county fixed effects, which capture the plancounty mean quality jm leaving the time-specific deviation in plan quality Ajm, as the
error term. The only potential bias therefore would arise from factors that change over
time for a given plan in a given county that affect both their premium and demand for
their product.
To deal with this remaining concern, I instrument for both premium and the log of
the nest share. I use two instruments for premiums. The first is created by calculating the
mean of the premiums charged by the plan's competitors for each of the other counties in
20
the plan's service area, and then calculating the mean of these means, weighted by the
number of Medicare eligibles in each county. The weighting takes into account the
relative importance of the other markets to the plans' pricing decisions.
For example, in 2002, Harvard Pilgrim Health Care offered a Medicare HMO
plan in Essex, Middlesex, Suffolk and Norfolk counties in Massachusetts (see Figure 1).
The instrument for the Harvard Pilgrim Health Care-Essex county-2002 observation
would be calculated by taking the means of Tufts and Blue Cross Blue Shield's premiums
in Middlesex county, of the same two plans' premiums in Suffolk county and of Tufts,
Blue Cross Blue Shield and Fallon in Norfolk county and then calculating the mean of
these three numbers weighted by the number of Medicare eligibles in each of the three
counties.
In using competitors' premiums, I differ from most previous work in this area
which use the firm's own prices in other geographic regions as instruments rather than
competitors'
prices. The assumption behind using own premiums
is that shocks to
marginal cost will be reflected in the firms' prices across counties. Their strategy
requires, however, the assumption that the different regions' deviations from the mean
valuation of the same good be independent of each other. This assumption can be
justified in the case where regions are geographically separated from each other and the
good that is being sold is the same across regions (as in the case of ready-to-eat cereal
being sold in different cities across the US). Medicare HMOs, however, tend to operate in
a group of counties that are contiguous and beneficiaries are likely to be crossing over
county boundaries to receive their medical care. In this case, a plan's time-specific
deviations from the means of quality for each county are not going to be independent of
21
each other in adjacent counties, limiting the applicability of the type of instrument used in
previous work. For example, if Harvard Pilgrim Health Care adds a Boston hospital to its
network, the time-specific deviation from its county means of quality will be correlated
across Suffolk, Middlesex and Norfolk counties since many residents of Middlesex and
Norfolk counties go into Boston in Suffolk county to receive hospital care.
Using competitors' premiums in other counties overcomes this problem.
Competitors' premiums are correlated with the premium because of the component of
marginal cost common to the region. They are, on the other hand, unlikely to be
correlated with the time-specific deviation from quality Ajm, because it is plausible to
assume that Medicare HMOs' pricing decisions in a county are based on factors specific
to that county, such as marginal cost and reimbursement. Marginal cost is derived from
exogenous supply-side factors such as the level of competition among providers and the
average health status of the elderly in the county while reimbursement is set according to
a formula. A more explicit model of pricing will be laid out in Section IX.
I also instrument for premiums with the county reimbursement rate since that is
an exogenous determinant of price.
To instrument for log of the nest share, Berry recommends using functions of the
characteristics of other firms in the same market. These variables will capture the part of
the firm's nest share that is determined by other firms' behavior but not the part that is set
by the firm's own characteristics. I use the mean of the drug expenditure covered by
each competing plan, weighted by each plan's market share.
Finally, to control for yearly shifts in demand for HMOs and their associated
medical care, I add year effects, where the omitted year is 1999.
22
VII.
Demand parameter estimates
Table 5 reports the results of estimating the demand equation for different
specifications of plan benefits. As mentioned above, no one has ever done a study of plan
choice with this level of detail in the drug benefit data. It is therefore not obvious how to
specify plan benefits. While theory can make a prediction about the sign of the effect of
plan benefits (that co-payments have a negative effect on demand, for example), there is
no theory on what functional form to use for benefits such as co-payments, coverage
amounts and non-formulary coverage.
I will therefore employ three specifications. The first one I use is a dummy for
prescription drug benefits alone. The second is a measure of how much prescription drug
expenditure is covered by the plan and the third has features of the plan, such as co-
payments and coverage limits, entering directly into the regression.
As canr be seen from Table 5, which specification I use does not significantly
affect the coefficients on premium or on the year dummies. The coefficient on premium
ranges from -. 007 to -0.005 (with a standard error of about 0.001) across specifications.
The year effects are significantly positive and rise over time, suggesting that demand for
Medicare HMOs rose steadily during this period. The coefficient on the log of the nest
share varies slightly more across specifications and is always significantly positive,
suggesting that the nested logit fits the data better then the ordinary logit. The OLS and
IV estimates tend to be quite similar.
The coefficients in these regressions report the percent change in the ratio of the
plan market share to the outside choice's market share resulting from a one unit change in
23
the right-hand-side variable. Since this measure is not very easily interpretable, I will
x
translate them into elasticities:
jmt
imi
where Xjmtis the variable of interest. In the
jmt
ordinary logit model, the elasticity is given by
on
X jmt.
In
the
nested
-[1-&jlgmt
-(1- 6)Sjmt]X
jmt
logit
(l - Sjmt )X jmtwhere
model,
the
elasticity
is the coefficient
is
given
by
where a is the coefficient on the log of the nest share.
In both cases, the elasticity is only defined if X jmt is greater than 0. Since about half of
the observations have a premium of zero, I calculate the semi-elasticity
jmlx
aXim
I
for
S jmt
the premium. I also calculate the semi-elasticity when calculating the effect of dummy
variables.
Table 6 shows the median elasticities and semi-elasticities. The premium
elasticity estimate of -0.18 to -0.31 means that doubling the premium is predicted to
cause the HMO's market share to drop by 18-31% and the semi-elasticity estimate of 0.005 to -0.008 that adding $10 to the premium causes the market share to drop by 5-8%.
These estimates are similar to Town and Liu's (2003) estimates of the median elasticity at
-0.29 and of the semi-elasticity at -0.009 and are higher in magnitude than Dowd et al.'s
estimate of -0.13.
Columns (1)-(4) of table 5 report the results from using only a dummy variable
for whether or not the plan offers prescription drug benefits. As expected, the effect of a
prescription drug benefit is significant and positive and the coefficient is estimated to be
0.108 in the IV nested logit specification.
24
Town and Liu estimate a significantly higher coefficient at 0.35 for the years
1997-2000. The difference may be due to several factors. First, plan generosity was
slightly higher on average in 1997-98 than in the period of my study as the Balanced
Budget Act did not take effect until 1999. Second, Town and Liu use the plan's own
premium in other counties as instruments. For reasons I discussed above, own premiums
may not be exogenous and using them as instruments will therefore not entirely remove
the upward bias of the coefficient on the indicator for drug benefits. As the elasticity
estimate in Table 6 shows, this coefficient is equivalent to the addition of a prescription
drug benefit raising the HMO's market share by 10.8%.
The second specification reported is a measure of drug expenditure for an average
prescription drug user covered by the plan. To calculate average drug utilization, I use
information from two sources. Moeller et al. (2004), using the Medical Expenditure Panel
Survey, find that the average elderly person filled 28.4 prescriptions annually in 2001
while Thomas et al. (2001) report that 34.3% of prescriptions written for elderly
prescription drug users were generic.
I calculate the average price of a prescription as being a weighted average of
average generic and brand-name prices, weighting the generic price with .343 and the
brand-name price with .657. Table 4 gives the weighted average price for each year.
Using these average prices, I calculate the cost of 2.4 prescriptions per month. I then
apply the rules of the plan to the total annual cost of the prescriptions
and split this
amount into out-of-pocket expenditure and expenditure covered by the plan.
For example, in 2001, the average prescription drug user is expected to spend 28.6
times $54.65 or $1,563.05 annually. Tufts HMO's Medicare HMO plan in Middlesex
25
County, Massachusetts, offered drug coverage in 2001 with an annual limit of $600. The
expenditure covered by this plan is therefore calculated to be $600 (since an average drug
user would use it all up) and the out-of-pocket expenditure for this plan is calculated to be
$1,563.05-$600=$963.05.
Another example is given by California Physicians'
Service in San Bernardino
County, California, in 2001, whose plan offers drug coverage with an annual limit of
$2000 and co-payments of $7 for generic drugs and $25 for brand-name drugs. In this
case, the out-of-pocket expenditure is calculated to be $538.42, or 28.6 times a weighted
average of the co-payments, where the weight for generic is .343 and that for brand-name
is .657. The expenditure covered by the plan is calculated to be $1,563.05-$538.42,
or
$1,024.63 since, in this plan, the average drug user does not use up all the coverage.
Table 2a reports summary statistics on out-of-pocket
and covered expenditure.
Average out-of-pocket expenditure rises from about $553 in 1999 to $1,079 in 2002, a
rise of 95% over three years. Average expenditure covered by the plan drops from $781
in 1999 to $567 in 2002, a drop of 27%.
Columns (5)-(8) of table 5 report the results for covered expenditure. As expected,
the effect on market share of increasing covered expenditure is significant and positive.
As Table 6 shows, when translated into an elasticity, the coefficient of .002 implies that
doubling the amount of covered expenditure is predicted to raise the HMO's market share
by 17.0%.
In the third specification, I allow the co-payments and coverage amounts to enter
directly into the regression. For plans that have unlimited coverage for brand-name drugs,
I set their coverage at the cost of 20 brand-name prescriptions a month. This puts the
26
coverage amount above the highest amount given in the data. I also deflate the coverage
amount using the Consumer Price Index for prescription drugs to 1999 levels.
Since there is a large amount of information in the Medicare Compare data, I had
to simplify it. As described above, I have already reduced the number of co-payment tiers
to two. I also found, through trial-and-error, that generic co-payments and coverage do
nriotseem to matter to plan choice at all so I only include brand-name co-payments and
coverage amounts if brand-name drugs are covered. Because the distribution of coverage
amounts is skewed, I allow it to enter in as a quadratic.
Columns (9)-(12) of Table 5 report the results of regressions using the brandname co-payment, the brand-name coverage amount and coverage amount squared, and a
dummy for non-formulary coverage. The parameters on brand-name co-payment and
non-formulary coverage have the expected signs but only the parameter on nonformulary coverage is significant. The parameter on coverage amount is significantly
positive and that on coverage amount squared is significantly negative.
Columns (9)-(12) of Table 6 convert these coefficients into elasticities and semielasticities. Doubling the coverage amount is predicted to increase the market share by
14.7% and adding non-formulary coverage is predicted to increase the market share by
7.1%. Doubling the brand-name co-payment lowers the market share by 0.4%.
VIII. Welfare estimates
The utility parameter estimates allow the estimation of welfare derived from
having different levels of prescription drug benefits. Welfare measures translate changes
in utility resulting from changes in benefits into monetary terms. These valuations
27
provide the benefit side for a cost-benefit analysis of adding a prescription drug benefit of
different levels of generosity.
Adding or changing the level of a drug benefit represents a change in the quality
of the plan. Small and Rosen (1981) give two ways of measuring welfare from such a
quality change in discrete-choice models. The first is to integrate over the change in the
share function resulting from a benefit to find compensated variation. Compensated
variation is the income change it would be necessary to give or take away to compensate
for the change.
The second way is to measure the price change necessary to keep the beneficiary
at the same level of utility after a benefit change; this measure is usually referred to as the
I will report both measures and they turn out to be very similar.
"willingness-to-pay".
The compensating variation for a change in benefits is given by:
-
fr Sjmt (Ujmt)dU
(4)
Intuitively, this result is analogous to the result for continuous choice that compensating
variation is found by integrating over the compensated demand function. Small and
Rosen give the details of derivation for this result for the discrete-choice case.
In the case of the nested logit model, the compensating variation of a quality
change is given by:
1
..
,
...
rUj
(5)
= IIn I
A
-Ag
Eexp( Uk -)
kEg
I-
I-C
28
This formula is derived by McFadden (1984). It is evaluated from Uto Uwhere U is
the utility of plan j before a change in plan j's benefits and U'I is the utility after the
change. g is the group or nest (HMOs offering drug benefits, HMOs not offering drug
benefits or traditional Medicare). The utility of traditional Medicare is normalized to
zero.
This result holds for more than one quality or price change made simultaneously;
U J is evaluated at the starting point before the changes and U'J is evaluated with all the
changes made.
To find the predicted welfare effect of a benefit change, such as adding a drug
benefit or raising the brand-name coverage amount, I calculate (5) for a hypothesized
market containing one HMO that offers drug benefits and traditional Medicare. The
HMO has the average characteristics (premium and unobserved quality) of all HMOs
offering drugs in the data.
It is important to note that equation (5) gives the average compensating variation
across all beneficiaries in the county. Benefit changes in HMOs will only affect a small
number of beneficiaries however: those beneficiaries in the plan and those that switch
into the plan because of the benefit change. (The benefit changes I consider are all
improvements so the change in enrollment will always be positive.) The average welfare
impact across these beneficiaries will be much larger. To calculate this welfare impact, I
find the total welfare change in the county using equation (5) and also calculate the
predicted share for the HMO before and after the change. When there is only one HMO
in the county, the share is given by:
29
exp(Uj)
(6)
j= 1+ exp(Uj)
I then divide the total welfare change by the predicted share after the change to
find the average impact on those actually affected by the change. Table 7 provides
estimates of welfare changes from adding a drug benefit and a number of hypothetical
benefit improvements.
The average compensating variation across all beneficiaries in the market from
adding a prescription drug benefit is calculated to be $1.95 but, when divided by the
market share, the compensating variation per enrollee is found to be $16.09. In other
words, enrollees would have to have $16.09 taken away from them to compensate for
adding the benefits.
The compensating variation of adding brand-name coverage, at $25.26, is higher
than that of a prescription drug benefit. The hypothetical coverage added has the average
characteristics of brand-name coverage in the data: a premium of $18, a brand-name co-
payment of $17 and a monthly brand-name coverage limit of $72.
Raising brand-name coverage by $100 from a base of $72 is estimated to have a
welfare effect of $25.49 and therefore has as much effect as adding the drug benefit.
Adding non-formulary coverage brings $8.60 per month in welfare. Doubling the
expenditure covered by the plan (from a base of $62, the mean value in the data) is
estimated to increase welfare by $19.36. Lowering the brand-name co-payment by $10
from $17 has an insignificant effect.
The willingness-to-pay measure gives an alternative measure of value for the
benefits. This measure gives the change in premium necessary to bring the beneficiary
30
down to the previous level of utility before the benefit change. To see this, assume that
before the change, utility is given by:
Uo =+ap+0 +
0 +o +o
If we assume a benefit change along with a compensatory price change, utility after the
change is given by:
U, = (p0 + Ap)+,8(X o +AX) + o + £o
Setting U0 equal to Ul gives:
Ap= -fAX
--
(7)
a
The change in p equals
a8 if X changes by one unit.
Table 8 reports estimates for willingness-to-pay for drug benefits based on the
coefficient estimates in Table 5. According to the IV nested logit parameter estimates, on
average, beneficiaries are willing to pay $18.00 per month for a prescription drug of
average value. They are willing to pay $28.60 for an additional $100 of covered
expenditure, $32.96 to raise monthly brand-name coverage by $100, $8.86 per month to
have non-formulary coverage and effectively zero to lower the brand-name co-payment.
Because brand-name coverage enters the regression as a quadratic, the willingness-to-pay
for this variable is given by
,am
+ Ja2 X amt and is evaluated at the median monthly
a
coverage amount of $27.50. These estimates are all qualitatively similar to the estimates
of compensated variation.
31
IX.
The cost of supplying prescription drug benefits
Using the parameters of the demand regression, it is possible to estimate marginal
cost for each HMO-county. To see this, consider equation (4), which gives the firm's
profit equation for a particular county:
rj = (pj +R)Msj ()-mcjMsj(mt)
(10)
where R is the county reimbursement rate, M is the number of Medicare eligibles in the
county and j5 is the vector of premiums in the county.
If we assume a constant marginal cost, the firm's first-order condition for profit
maximization is:
Sj
pj pj
= McJ
=mcj asi /' pj R
(9)
In the nested logit model:
Si1
as / pj
I- a
-
(10)
a(l- jig- ( - )Sj)
so we can invert equation (9) to give an expression for marginal cost in terms of the price,
the share, the reimbursement and the demand parameters:
mcj = pj +R+
(-,
1-ff
(11)
-(-)j)
Table 9 reports the summary statistics of the results of this calculation for each HMOcounty in the data. Estimated average monthly marginal cost rises from $360 in 1999 to
$457 in 2002 and the HMOs' estimated profit margin drops from 31% in 1999 to 27% in
2002.
32
In order to estimate how much it costs to supply prescription drug benefits, I
assume marginal cost is a function of benefits provided, county supply-side
characteristics, year effects and unobserved plan quality:
MCjm,= (Rx benefits) , + (County characteristics) y+ (Year effects) 6+ jmt
(12)
Regressing marginal cost on these variables will therefore give an estimate of the cost of
providing prescription drug benefits.
Correlation between the benefits and plan quality may be an issue however. While
I argued in Section V. that the benefits were uncorrelated with the time-specific deviation
J4jmt,
it is possible they are correlated with
jm t.
While this problem could be fixed with
plan-county fixed effects as in the demand regressions, I am unable to use them in this
regression because identification of the effect of benefits on marginal cost would only
come from plans that change their benefits over time and the decision to change benefits
may be endogenous to the level and cost of benefits.
To deal with the endogeneity problem therefore, I instrument for the level of
benefits with the average level of benefits offered by other plans in the county, the
average premium offered by other plans in the county and the Herfindahl index for
Medicare HMOs in the county. These variables all proxy for the level of competitiveness
in the county. Gurol and Ellis (2004) have demonstrated that competitiveness
in the
market is a determinant of whether or not HMOs offer prescription drug benefits, and it is
therefore probably also a determinant of the level of benefits.
Table 10 reports the results of regressing marginal cost on prescription drug
benefits, county characteristics and year dummies for both OLS and IV and for all three
of the specifications of drug benefits used in the demand regressions. Since marginal cost
33
is estimated using parameters from the demand regressions, the regressions are weighted
with the inverse of the standard deviation of that estimate. A probit was run for the first
stage of the binary endogenous variables (the dummy for drug benefits, the dummy for
non-formulary coverage and the dummy for generic-only coverage).
For county characteristics affecting marginal cost, I used the number of short-term
acute care hospitals, the number of beds in such hospitals, the number of doctors, the
number of medical and dental residents, the number of doctors engaged in teaching and
the number of doctors engaged in research as proxies for provider density and quality.
These variables are all divided by the number of Medicare eligibles in the county. As
Table 10 shows, the coefficients on these variables and on the year dummies differ
slightly between OLS and IV but do not differ significantly across drug benefit
specifications, suggesting that they are robust.
Columns (1) and (2) show the results when the drug benefits are specified with a
single dummy variable. The average cost of a drug benefit is estimated to be $21 with
OLS and $31 with IV. The increase in the cost of a drug benefit from OLS to IV suggests
that, conditional on the medical provider variables and year, the presence of prescription
drug benefits is negatively correlated with unobserved plan quality. This relationship may
be due to plans deciding to substitute prescription drug benefits for other plan benefits,
either to keep total costs down or to encourage favorable selection.
Columns (3) and (4) show the effect on marginal cost of raising the amount of
expenditure incurred by an average prescription drug user covered by the plan. Again, the
effect rises from OLS to IV and the effect is measured to be $0.28 with OLS and $0.43
with IV.
34
Columns (5) and (6) report the results for the specification using benefit
characteristics. Most coefficients have the expected sign and are significant. The effect of
raising the monthly brand-name coverage amount by $100 is estimated to be $32.33$2.58, or $29.75, while the effect on marginal cost of raising the brand-name co-payment
by $1 is estimated to be $1.31. The average cost of providing non-formulary coverage is
estimated to be $65 per month while the estimated cost of providing a generic-only
benefit is insignificantly different from zero.
These estimates of the effect of marginal cost of offering prescription drug
benefits allow us to make inferences about the level of prescription drug usage by
enrollees in HMOs and the estimates show the enrollees make extensive usage of them.
As discussed previously, the average elderly person fills about 2.4 prescriptions per
month, of which 34% are generic and 66% are brand-name.
HMOs offering drug
coverage cover, on average, about $60 of this average person's spending. If HMO
enrollees were average prescription drug users, the effect of offering drug coverage on
the plan's marginal cost would be about $60. Instead, as column (2) shows, the effect is
$31; HMOs with drug coverage are therefore covering $31 of drug spending per enrollee
per month.
Similarly,
in column
(4), if HMO enrollees
were average drug users, the
coefficient on covered expenditure would be 1. Instead, it is about .44, implying that
HMO enrollees with drug coverage spend 44% much as the average prescription drug
user.
The results in column (6) have similar implications. The cost of raising monthly
brand-name coverage by $100 costs about $30, implying that, in general, enrollees do not
35
take full advantage of the drug coverage. Non-formulary drug coverage, however, is
estimated to cost $65 on average, suggesting that enrollees in these plans are taking
advantage of the open formulary.
X.
Conclusion
In summary,
then, beneficiaries
are willing to pay on average $18 for a
prescription drug benefit and the benefit costs $31 to provide. Beneficiaries are willing to
pay $0.29 to increase the amount of expenditure of an average-level drug user by $1 and
increasing that amount by $1 costs the plan $0.44.
It is important to remember when comparing welfare and cost estimates that the
welfare estimates give the average welfare across the entire market, while the cost
estimates only apply to the enrollees who actually enroll in plans offering prescription
drugs. It is not surprising therefore that the cost estimates are slightly higher than the
welfare estimates. While we normally would not expect to see benefits being provided at
a higher cost than they are worth to consumers in the market, beneficiaries who actually
choose plans offering prescription drug benefits will value the benefits more than the
average beneficiary.
The welfare estimate, however, implies that the market the HMOs are drawing
upon seems to consist of less-than-average prescription drug users. If the average
beneficiary is only willing to pay $0.29 to raise the amount of expenditure of an average
user by $1, then the average beneficiary in the market HMOs are drawing upon uses
prescription drugs considerably less than average.
36
There are several factors that could give rise to this result. First, the Medicaideligible are excluded from the market definition and they are sicker than the average
Medicare beneficiary. Second, Medicare HMOs are known for deliberately targeting
healthier beneficiaries because they are paid with a flat reimbursement rate and therefore
have an incentive to enroll the beneficiaries who are expected to be less costly (Neuman
1998). Third, the market may appear to value prescription drugs less because while we
observe managed care without prescription drug benefits, we never observe prescription
drug benefits without managed care. A higher demand for prescription drug benefits,
however, is correlated with a lower demand for managed care, since people who are ill
both take more drugs and have a lower tolerance for the constraints of managed care. As
the demand for prescription drugs tends to be skewed, those beneficiaries in the tail of the
distribution, who are very ill, may also have a very great distaste for managed care and
would not choose to enroll in an HMO under almost any circumstances. The loss of the
tail of the distribution may explain why the welfare estimate implies that the value of
prescription drugs is so much lower than we would expect if the market represented a
random cross-section of Medicare beneficiaries.
The results presented here, however, are applicable to those Medicare
beneficiaries who did not have drug coverage before. This population is interesting
because they will be the ones to acquire prescription drug coverage when the Medicare
Modernization Act (MMA) comes into effect at the beginning of 2006. These estimates
provide a lower bound of the welfare effects of providing prescription drug coverage to
Medicare beneficiaries.
37
References
(1999). Medicare Managed Care Plans: Many Factors Contribute to Recent Withdrawals;
Plan Interest Continues, United States General Accounting Office: 69.
(2001). Medicare Chart Book, The Henry J. Kaiser Family Foundation.
Abraham, J., A. Arora, et al. (2000). "Enter at Your Own Risk: HMO Participation and
Enrollment in the Medicare Risk Market." Economic Inquiry 38(3): 385-401.
Arellano, M. (1987). "Computing Robust Standard Errors for Within-groups Estimators."
Oxford Bulletin of Economics and Statistics 49(4): 431-434.
Atherly, A., B. E. Dowd, et al. (2004). "The Effect of Benefits, Premiums, and Health
Risk on Health Plan Choice in the Medicare Program." Health Services Research
39(4, Part I): 847-864.
Berry, S. (1994). "Estimating Discrete-Choice Models of Product Differentiation." The
RAND Journal of Economics 25(2): 242-262.
Cardell, N. (1997). "Variance Components Structures for the Extreme Value and Logistic
Distribution with Applications to Models of Heterogeneity." Econometric Theory
13: 185-213.
Dowd, B. E., R. Feldman, et al. (2003). "The Effect of Health Plan Characteristics on
Medicare+Choice Enrollment." Health Services Research 38(1, Part I): 113-135.
Ellis, R. P. and I. Gurol (2002). Health Plan Entry and Exit in the Medicare Managed
Care Market. Boston University working paper 28.
Gurol, I. and R. P. Ellis (2004). Medicare Managed Care Choice of Benefits and
Premiums: Competition and Selection Incentives Really Matter. Boston
University working paper 27.
Hausman, J. (1997). Valuation of New Goods under Perfect and Imperfect Competition.
The Economics of New Goods, NBER Studies in Income and Wealth. T. F.
Bresnahan. Chicago, University of Chicago Press.
Hellinger, F. J. and H. S. Wong (2000). "Selection Bias in HMOs: A Review of the
Evidence." Medical Care Research and Review 57(4): 405-439.
McFadden, D. (1984). Econometric Analysis of Qualitative Response Models. Handbook
of Econometrics. Z. Griliches and M. D. Intriligator, Elsevier Science Publishers
BV. II: 1395-1457.
38
Moeller, J. F., G. E. Miller, et al. (2004). "Looking Inside The Nation's Medicine
Cabinet: Trends in Outpatient Drug Spending By Medicare Beneficiaries, 1997
And 2001." Health Affairs 23(5): 217-225.
Neuman, P., E. Maibach, et al. (1998). "Marketing HMOs To Medicare Beneficiaries."
Health Affairs 17(4): 132-139.
Nevo, A. (2001). "Measuring Market Power in the Ready-to-Eat Cereal Industry."
Econometrica 69(2): 307-342.
Pai, C.-W. and D. G. Clement (1999). "Recent Determinants of New Entry of HMOs into
a Medicare Risk Contract: A Diversification Strategy." Inquiry 36: 78-89.
Pauly, M. V. and Y. Zeng (2003). Adverse Selection and the Challenges to Stand-Alone
Prescription Drug Insurance. NBER WP 9919.
Penrod, J. D., T. D. McBride, et al. (2001). "Geographic Variation in Determinants of
Medicare Managed Care Enrollment." Health Services Research 36(4): 733-750.
Small, K. A. and H. S. Rosen (1981). "Applied Welfare Economics with Discrete Choice
Models." Econometrica 49(1): 105-130.
Strunk, B. C. and P. B. Ginsburg (2004). "Tracking Health Care Costs: Trends Turn
Downward In 2003." Health Affairs(Web Exclusive): W4-354-W4-362.
Thomas, C. P., G. Ritter, et al. (2001). "Growth In Prescription Drug Spending Among
Insured Elders." Health Affairs 20(3): 265-277.
Town, R. and S. Liu (2003). "The welfare impact of Medicare HMOs." The RAND
Journal of Economics 34(4): 719-736.
39
.
*CE
=E ILM
o Ct' OC'4)
-a0
0I
I~-
CD-CO - Co 0))
oOD
(D U0 I-
6
0
0
0
I-
41)
E
U)
4.- co
04)
0
z
0
t-(ON-C' )
E
O LO
I
cO
.r (C (,
lCU
o
'B
O
II
aQ
CO LO t
-
4)
CL
co
4) 0)
E, 0.4
4) 0.
z
4)0
'0
*o
)
.-
0
CO
(D - CO
,It It o
CooCM oC
)LO ) I'
CC)r-w
u'
0.1:
E
E
C,)
o) o C C)
m U)
C C00
Ez
m
0o0o
_D CD CD CD
E
o
o
0S
0
X 0O C\! 7q
CO 0
C) O0 r-.L~
c O, U) U- o
o
0
C~lIt
,O~ O a
E
0c)0) 0)0
It C CO ')
- C) CO
LO
0
a) 0)0a)0)
o) -
Ct
0
cJn .It
1--
C\jO O ,IO
([: 'I~ 0)jco
O 00
._
C0 C)
C
O C Oo
O'O O
x
CM
. CO
0
m
E
_Oq CO
L0U)
U)
C
C'l Cj C\j Cj CC0r- O ,t It LO LO
- - -oo -)0)-
(I)
.O
mB
I)
._
0
(U o
(a
-
a ac
(D O N-i-
'C
oS oS0
C")
o
'Ittr-Cco
(D Itt )
cot t ~CV)0)M
C6 C 'i
O U 13 Iq CV)
Ui CD o o co C", U C
0 Om ~-t
co
m t,IdC0co
) om
N -co
0 o6 3 o oo
CO 0) 0) cO
4-
E
E
z
t o '.(0
cs
M
r
o L)
,t
r- cm (O r
0
0)
r-
-
-. H
o
00
O
0)CD0o NC
0 O0
O O
(U )
(U O)
-
N C
C
cm CO C
- o C00
-0 00 O, ,-CD O
CO0
CO
0It o C o0It
O L)O - ',t
g) oCLO
coN
CO ' -Coi
OJ
N- O ') co -( o U) O0
C C\ - -
CD O _ N M)
- _) ) 0C0 N0
_CN 0)
) 00
0 00
0)
00C00 -0)000
0O
O
O
)0
00
0)000
OC
C
C
-- CM N
NC
I-
C"
0
0
I
.1.
C
0
0
0
0
o(U
C.)
4O
E
0
C.)
0
0
m
e-,
C.
-r
I.E
co
0
E
o0
(U)
m
(U
0)
C.)
(U
O
620
Ic
'1-
c
._.
(U
E
.5
w
co
UJI
(A
4)
._
a-
0
(L)
0
0
O
o
I-(_
O
.
(U
C
U)
ao.0
c
0
>
0C)
.'~~~~~~~~~~~~~~~~~~~~~.
c
O.
0
I-
0
E
Z
O
'4.
0(U
.0
0C.
aE
Z
0
C.
0
W..
.0
E
E
Z
z
CO ,t CO )
w cO
o o o LO LO cO O C 1 ) 0 ) Ocoo 'tcoO' C)O
cO
co
;; COLO
I'l LO CO
c
- CO
O CO
1G1G
G- N 'ct (O COD
N
69
6 G G 6
f 69 . 000
6
69
-: G~ G- GG 6e
G ;; ;9
;;
E
O
E
61g6)
E
,t > i, a)
0 0 0 0 0 0 0O
0OOt V.6
0 O00
0
CO U) 0)
OO1
69. V: 6g- 6G~
G~ 6 6 6 6. 60 t0
ft 0 OOOO1:~61.61:
6g)
69 ) 9
- -
E
CO
C
CM
a)
o
0
o co
-
(O
0
LO
0
o
(D
O) CO
(D O -
)C
CO
'-NC
e 6 Oi1C
N)
Z
CO LO t CO CO L) t
O r
CO -CO
'
t CO CO ,'* '
C
C)
C)
0o Cl)
0N 'T CO
N CO C
CO N
t
O C
-
CN
.
)O0
co N
C
C) C
OD
6 69
*
o
61) 0
) 0 t 0 0) 0
C CM0N
C N
CM C
0
C
C
C
C
C
C
CM CM CO CM CM
Cl
N
69.:
C
O Co)
N CMO- -co 0)
O CO
CD
CD co
' r r
6LO o;6;.e
61 6
6
LO
69
0)
0 T 0 0) 0 'T 0
CO C C C 0 CJ N C'J
C C N NC CMco N CM
z
000- 0 0)Oi0 - 0 0)
- "4
0) 000 0)000
0)0 000 0 CM0) 0'
0)
0
e)
0 00 00 o)
0 00
0)
00 0 0)
0)
0)000
aa. o4 oI o 0) 000
) 00
00
0
0)0
0
0
0
00
03000
OMO O irC N
- CNN
04 0
-
C
-
(0
C.)
4.'
CoM
CN4
C
0,.
a-
a)
a)
0)
a)
a)
.0
a-
.0
cco
'a
G)
i_
>a
')
O
0
.
*0
.
0
00
i-
a)
ca)
.0
cm
0.
a.c
-0)
a)
Ia)
0
0.
w
U)
c
0)
O
a)
a)
a)
cm
w
._-
m
0)
0.
CL
a)
0)
a)
C)
a)
.r
00.
(n
aC)
a)
zO
I-
ac)
0ta)
m
a)
0)
m
0
0)
*0
ol
L0
.o
ca)
6a)
cm
0.
0I-
0
a)
c
CD
0.
a)
a)
E
E
.E
E
0)
a.E
a..
a)
a)
L-
4)
a-
a)
E
so
m
.0
C
0
>a
Q
E
m
0
0
g.
0
._
._
L-
0m
._
c
O
3
E
0
0.
cm
a-
a)
0.
I-
a)
.10.
X
0t
m
0a)
00
a)
0
m
Q
ca)
0OL
;aa
0
4
0
2ca)
0f
(D
a)
.
x
w
Table 2b
Coverage amount by category of plan
Year
% of total plans with
prescription drug
coverage
Mean
coverage
amount
Minimum
coverage
amount
8
2.8%
$600
$250
$1,000
1
0.3%
n/a
169
58.5%
$942
$50
$3,600
87
30.1%
$1,359
$300
$4,500
24
8.3%
n/a
$500
$500
Types of plans
Maximum
coverage
amount
Lim. Gen. covge,
1999
no BN covge
Unlim. Gen.
covge, no BN
covge.
Lim. Gen. and BN
covge
Unlim. Gen.
covge, lim. BN
covge
Unlim. Gen. and
BN covge
Total
289
% offering BN
covge.
96.9%
Lim. Gen. covge,
2000
no BN covge
2
0.6%
$500
12
3.8%
n/a
149
46.6%
$802
$50
$3,600
113
35.3%
$1,199
$100
$4,000
44
13.8%
n/a
Unlim. Gen.
covge, no BN
covge.
Lim. Gen. and BN
covge
Unlim. Gen.
covge, lim. BN
covge
Unlim. Gen. and
BN covge
Total
320
% offering BN
covge.
95.6%
43
Table 2b (con.)
Coverage amount by category of plan
Year
Mean
Minimum
Maximum
% of total plans with
RX coverage
coverage
amount
coverage
amount
coverage
amount
6
2.7%
$383
$200
$500
33
14.7%
n/a
115
51.3%
$997
$200
$3,000
61
27.2%
$1,283
$250
$12,000
9
4.0%
n/a
$200
$1,000
Types of plans
Lim. Gen. covge,
2001
no BN covge
Unlim. Gen.
covge, no BN
covge.
Lim. Gen. and BN
covge
Unlim. Gen.
covge, lim. BN
covge
Unlim. Gen. and
BN covge
Total
224
% offering BN
covge.
82.6%
Lim. Gen. covge,
2002
no BN covge
16
7.3%
$583
75
34.1%
n/a
75
34.1%
$939
$200
$4,000
49
22.3%
$1,107
$250
$3,000
5
2.3%
n/a
Unlim. Gen.
covge, no BN
covge.
Lim. Gen. and BN
covge
Unlim. Gen.
covge, lim. BN
covge
Unlim. Gen. and
BN covge
Total
220
% offering BN
covge.
58.6%
44
E
C\I
L
:3Cl
C ,E co
*R
)
Lo)
o
Lo
Cl L
ao
eNr-9 ,-1!09CO
'3~6
m
0
0
E
0
E
02
'.
(0)
U
g
m(
E
.0
0n
0C
@'o
OD CDO
C)
N
CO
) ._
o
t t U)
.C )-O
61
6
6
0.
9
Io)
0a-a
c)
OD U) CM
C (D O It
C's Cl, Cl, 1
a)0
0
) Co
0
(0
a)
F) '
0
CO Co U) Nr
C,
0
U
CO -COl
.-
a
a)
E
0
.,
'~'''
°C)
M OO
6 O,C1
(D
m)t(D
E
C
0
O C O )
ZOcoc U-)
o
1- (D
'§a0.
.
-. 4--
E
n
m.- 0"
0
0*
0E
I
a)(l
I L
L
,E
w
'~
E._ ~~
C\ O,
C)
C
L)
a
C
Nt
O) oo
0
a
a)
.,
5
a)
3E roi o
.0 ,E
E
a)
a)
0)
a-
u-)
r-
CD
C
6qL09
I-Cl? t0 C?,)
a-
Cl, CM C
CM
)OOiC-e
(I9 6 6 649
a)t It0 00
0O'
0
0
O
a)
a)
U)
CO 0 U) t
r U)
L(DO LO
)
2
C? rlO=0.
a)CL
4'
E E qa)
0 0
0
0
0*-L-
.-
Q Q)
a-
0)E
. Q4 o)
a)C
. CD
LO (D CY)LO
cq 03
FQ C')
c 0) c) 9
_
8U
o 0.
o
o
Q 0)
0
_. 0
C
co
wo
co co
4)a- oN1 oCml oN-
>
O)'-X
..
O.
o
a) C)0)000
0)000
C
son
o0
Cl.
0a)
C
0
Cl)
Zt i t
CO
ao
X ._C
Q
O
ZC ~ It
t s6s
U)
69 6s
a)
C
O
a
,.
o-
.
C
0)
Cl ,
-,,
raCo
0
0o
C
CO 10CLO
,t It U) LO
a)
.2
w a).~
Q-0
om
r
C\
C D0s) C
(D
U
.-
0)
o
o.0
-
0) 04
0 .c
oa)
Q0D
0a
0
a- >)
C
CQ<
0
0)
0 (0 CMOD)GO a)
0 OO O)C)m C)
0m
0) 0
_
0
0)
0
<~ C: o rC) C) r
N CD
U) O O O 0
OO
C)
0
-o~
OOO OO_
O OOO6
SO0
O
ECD
/)
COa)
Z
.2 CZ
*
'4-
U
0)
.0
00r, 0
o o
C O1 O)
0)~cn]
',- O
00
COj a)
O'
O COCO I
O C
C) C) Coo
v5C
oo
O 'r- O Ck
·
o. oo
qc)c3
..
4-
.-E C
<
rco)
C)
nO C
LO
0
C]
I-
z
>
(0)
L
I- V
C
L.-
._.
qI)
0
0
E
4-W
0
C
a)c
I00
~c
C0
CZa
r
- 0l0
-j0 9oc0-0woc\Jc
°.
C) _C) 0°
Joo'o
v0
v3)o
o cLO
O0 O0s O0 T- O- ?- O. Ck O0 C
v
v
v
v
E
E CD)
-i
0
0
·a)0
~)
- 0_
-- OCQ
xlEn)El._
(D
CO
_ O
I'. oO- 0CO
oo r,.FO oCD-,el
C o
oo C U)
Ckl 00 0
o
o
-
r
cm
Ckl
CM
CN No O
w CO
o o o. o,-. oCD. C
o CO
o
, *9C>. C) C)
m. C) mC
.
LO
x 0 in0E
a)
a)-
0
O.
.0
Q O)
0
0
0) 0) 0.
0)
'CO
.C
C
LO0
0.I-
0)
.,E--,
_ ) 0)
aC
E
0)
t
a)
10
a)
cn
0
m
0)
0-
.-tC
-
a)
0)
c'o, V
2ncE (
-j0
OC0
0 c CI
0
m
C
4..d
0.
a-
a
a-
E
c-) C
'-- O)
0)
E
0)
0)
E.
CDC
eC
w
.0
0
0
zU)
C
0
2L
U)
a
_ 0))
_n
U)
>
0
a)
(n
4.
0.
.-0
0
oo
o
C)
CD
o-0 CM
00
CJ
CD
CDJ
C)
L-
a..
L
0)
0)
0)
m
0
0
U')
0)
4-
.o
?U
0 0=
0
-1
V
CL a)
a
--
0
a
0
0MNcc
0)0
CLZ.
0)
:
z
U
4D
o _CCa) a)
-nr._C0 o -
CZ
0
_ c
a)
(U
C
0
m LO
0 0 a
(
L 00O
~
C
L
CM
C\J0C\C~9l
c00O66666
Ooo_
O
oQ)
cTs
C0
0q C
_
C-
)
_U0
z
0
C/)
E U
:C
0 0 OE O C
a)
.-
L..
Lo
C)
-J
0
0c.
0y-0C'J0C
Q
)
F:ZF
U)
C\00
O)
. D O). 0 O
Q O-
r--
O c
0 '--
CO
0O -0
U')
*0
a
0)
o
,C)
U)
) E
x
(1)s 0
a
a)
0
0
N- O' - CJ (0 0)0
0
C,
o.C0 oo COC
°)
CD
O
-
-
o_
'6_
00s0
C
!.
CD
LO Cm "t Cj
C O) O
C
.) c
_
O) -
CO
0
_U-)°
z
c
C/) E
.0H
0
0
N- o-
.'i
2
'U) E.'
U
O CO
a)
-i
0
. 0
>)
LO 0
-J
OJ R0
0
o.0o6O
0 o--L-)o. CD Co
ooooo
-o
CJ CN00wC)-
C9 Cc C
OOLCU)
ca
6
CM
U)
a)
0(D,
x 0))
On
D
.0
0C
E
do)L-m)
0-
- _ECz
-
>-
inE
0
y
Q
"o
>1
U
U)
cn
m
(U
a)
O
oU)
a) O·a
(/O)
cn a) a1)
.U)
n 0
>
_
) -o
n
._
a)
0
X
0)
0O
.t E
o
a)
(_
0)
cn
¢D
a)
U
I.-
*0
*_-
o
-~
E
0)
0
-j
Ca)
O
O
I..
a)
aL.
U)
) Q)
.E 1.--)
E'-
a;
oU)
-0 C
(U
(o
-i_
i.
0
n
E
&-
CO
SN~
L.
'-
N
(UD
s
NIIl
CS
I-
ED
N~
II
a-
a)
0
a
a
0
(U
0.
.U
m
>1
s_
x
0
O
C
v
Q
0
¢DcU
...
J
._
>m
a
a)
¢ D
a).4-. a)
.0 N
¢D O
(U
O c: CZZ
._n
a)
.-- CZ
0ta)
o a) ._0
"r
O0
[OCZ
E-i--
cm
0
_ )
CZ
-oc-:
0j o
9oooZ
. 0"ooCoo)o oo&C\
_0C
co
4)
4)
4-
z
0) 0.
0.-)
966666o666666669?666m(
C)(. CC CM
t
C) C>
) o°. CO
t
a C)
C
LO U-)
OOC
O C) U-)
O C)
O LCD CoU)
M O C)
°.°) C)
C)
S0D
O0)
s0'It W
w
c) -nOC\I
P_
-
CA
_j
°
.
C)
O.
O 0
C0
CDCO
)C t
0 C)
0
C)lrtO-
O °. O O
O
cCL a) -O
.2
.
Us
C
0/).- W
Q
cn~
:)0)- I
op
4)
'4M
4)
<D"
rO(. ia CMjC Co :;"o
C) CD C) UML
t
o
M
vO N CO)
0 C
0 0 0
900cj-5J0\
4)
E
-
a)E
a)
M
CD
©
>~
C
_D
4-
0
0)
° O6OOO O O O6O
~0C\J
;,
4-
C
a)
_,.0..J
o _o o'o
o cV,
0 .000_
SC)0
o C)
cvcccc
U)
CM
C
cv
C)
a) :-
4_
'cn
- E
0--
O
0
*e
Q 0
) a) a
-U
r-
co^0 "t ia cm :;: , a
O w M U.) oqooCo
U-)sNM
69 6666666
-_
C
oM
co :;: P_ a r, R
0
0Cccoo
66
- C)
N r
COCm
· Cc
_c9
co
96OO00O
c)
C
a).
02-
u-E
=
- 3C
oC.)_=a
ZI-
o 0)c)C
co
U) )
o
CL
0
Ua
w
11--'
C
E
U)
0
CD
a)
"0
cn
E
U)
oE
O
0)
0C
E
o
.._
._
1,
,
o
U)
.oo
44)
C
4)
E
m
00C
.0
0
4.
.
C.)
E
0
E
E
0
=3
Mi
ob
L..,
E
0?.)
0)
0o
v,..
co
4)
H
00
E
0
4)
4)
O
00C
04)
a-
E
s-
0
·~
oD
o
CDJ
I-
4)
o
co
4)
_
_
4)
0()
!_
_
- O s'_
O
0"O
tn
E
C.
>
E
.0
=
<
*0
E
(D
_
<
W.
0
-
E
E
0
U) m->
) J,C a
S)
v
4)
E
o
a0)!) (1)
0
0) n0)S
(1)
0
ch..
4)
o
I_
IZ
4)
"0
4)0
C
nCo
a) 0)
C
aC
w
E a)
o
c
-)~0)
>-
0 0) F
U)
cmo
Ci2
a,o -4)U)o
)C
CZ
a)
CDEC
cn
co
a: o
E
00
v
z4)
.6-
0
Lo~C
C
Ci-
co
0
o
ocI
0~
) =
C0
c96
06C=
o-)
ioU);z-
66
C)
0
a)
R-
*-
o) o 9oo
-j .o
oo6
06
0
a.
CMj
co- .
x
a)
*0
a)
CD 0)
.-
z
)
a
0
U,'C.D CO
C'J (O
0) CM
C'J
tOo-
q
65 0
coN
doo
-0
-
-o
0
,
a)
n-
00
a
In.
a
._
0
-i
'r
6
-0
o'0 C
96
66C
O
-
)
CM
m(
z
I
E
0
wI
cn
i
0
C.)
a)
0q
U
__
*0-*
.-
.)
(I!
)
z
9o
0
-O
.
0
(0
a,
0 C'j
OC)
O0
.q
00 O
9o
00
0 d70
CO O
C) Cf
C)
E
(D
0
'a,~
a0)
.0
0.
C 06
0
U)
-J 0, o
9o
00
9
00
o.06
(ON-
0
C
3-
3w
M.
0
Z
ml
,0
C'
.0
m 0)
e
C
|'
m
v
a
0
..
0
E
E
-
0)
-J
0
-0
o o
0)
0) cr 0,) CV)
0
a) 0 c'J
0
o.
O
C
00:Z
z
U,
a)
I-
c) o
CZ
C
Un
C
-i0 906~
o°
69o
(DC'J
00
CM
a)
E
o C)
cn
0 0
'-
>6
>,
>
._-
.o
..
0
U)
Li
C
.
0a)
C
CE
)
w
._
q_.0
o
E
::
X
a)
SO
0
>6
E
'm--m m
..
.
a).
a4a)
'0-
,m...
m o
. _-
o
0a)
.
0Q)
w
w
._
._
(D
a)
>
'O
.__
0 H :-
a)
0¢t-a)2Q
._
- 0a.)
D
>
>,
. _-
I-
a
-
>
0
6
) O
0 C)>
>0
am Q
'a)
E
0
*._
0
C
a)
I..-
a
n
C
a
C)
E
CU a)
Q
a)
E
0
OCZ
a) a)
>
CZ
>6
.0
0),a)am
ma-a
00a)
U)
a)
Un
a)
E
0D
nn
!
0)
U)
..
a)
E
a)
CU._
En
E
*0-
am
COn
0a) a)
_
cn
-00
.6m
4) 0)
z
oo0
q q
9o
9
oo
C0 CO
0) 0,
,
00
00
)
) -
1-
_-
It-c\J
t
00~
0m
co
C.
A!
a4)
C.)
(U
(D (.
0)
0,
_
?
t t
6 C
~.dd~~~~~~~~~~~~~~~
t
Or- Ow~ 000
0 . vv-
q q CO
76666
o~~~~~I CDC
CC
-J
)C
cm.
0) in) _
C.)
C
e)
04)
0
Co)
CO
-J
0
0
CM, O
06C
00 o-00
O~O0
O
O0
0
- O
vIt
C - CM
OO0Z3
cooC
o~
0 ~ ~~ 66
0
Oo
9v~
z
P-Lo
0oO:00
0*,
~~
C
0
o'o
-0)
I=
coZ
00
O)
-i0
-
-
q
0
00
10:)C
I-
OCO
.~
O O
. 000
. .~C
0 v0000o
4)
o0
0
Cu1
4)
Cuw
:50
4).(
._~~~~~~~~~~~~~~~~~~u
o
._
0
0
W
0
0
>1
>.
>
0
0
0
w
w
a)
:5
._
_
E
0)
com
-
0
C
._
.-
E
.0
C
t._~
Q
0 ~~~~L
0)
:n
._
cm
-oP
0)
a)
o.2
n a)
0) E
a) c
._
0)
4)
0
C
'a-
0._
0
0)
(A
E
co
:-I
0
0
:5C
C
'IO6-
x
4)
>'
E
I-
0.
0
4)
0
CU
aQ
a-
C
4)
E
s/)W
C Cu
C
00
o0.
0
m
L.
4)
c)
4)
E
w
mF
C
*.
C
m
E
co
C
E
°C a)
0
4)
CZ C
l a)E
4.I
a
C
0 0
cn
0- U)
a
co1
C
iU
a-
C U
. ) -
0
O )O
.Em
--
Q3.2 a
E
O N-
CO
v
_
°6 -S
.- ~
ON
'-(0
cEI
CLO
CMj
6§
(D
C\n
(O o
o. c6
C)O
0o 6, r_
C!
cnO
r
C
6J
v
P00 CMj
co
69 69
0
0-
a)
L.
C
:F
C
o6
L.
C
E
a
L-
Lf
°9go
o o6 o
6o
(A) '0.
aL) -C
CO
-00:: -F
..
CO
Itc co
C\J gU)
CMO ·
a)
aC
E
im
ii
0
a
C
(0
O
O.
t OCO3
vi~
· O~
-cxM
'a.
4x
0
O
L
C
&W
t
co
'--
*0
L-
C
m(
00
a
)- m
gc
E
00
CD
=
(L
C
0
C
o\
0)0
(4
'cm C
6c8
io
M.
4a
O
00
7i
CX
CO
s._
0a2
C.)
*-E
C, )
0
-E
>0
.
C ccm 6g -4 _
LO
OO
C) oCO too,o-
cn
ci ur c5Cm
(0
a
==
co
O C)
a
6.
6cl
.C0
0M
69C
C'J
o~
69
C')C'
vNco
r-~
C 61
-CM
C w
NJ
6 =1
-
69
a)
-o
CZ
(O0
ICD U)
CM- CM-
o~~~~~~~~~~~~~~~~~~~~~~~69
e469n6#
GG 69
..
a)
uC.-
'0-
L
C
E
0.
a-
C\!s
a
c6 6
c)R t
~0
00 ,cl
'5
C
0
C
;C C)
C\ CJ
r-
L0
CMI
6g 6)
(D
CLO
-l
*'
G- CM ;-
6 603.
_ 6 6g
1_CJ
_
E
Q a
a,
a.
a)
a m
0)
0)
E
0
O
a0
a1)
E
a) .0
0 C.
SD
E
aa)
a)
-
0
Ct
.°~~~~~~~0
.'-'I
U)
E .2
r
a) 4
'--
0
0a-)
)D
Ua)
0'*M
E)E
.
a.)
'O
I.
IO
(D
oU)
L)
0
0 0"
._
a) n
E E
a0
E
U
0
X6
O.s
f
*0E-
o
1
. Q0
0a),-
o
=
0
0) W.
0
_
-'~
x(L)E
I-o
D C
0)
CJ C
(O
<
0.>
0
a)
2Ž
WE
0
°E
In w
00
a)
0
X 0 a)
a)
-j
C
a1)
0C.)
(L)
L.
.0
0
.r
0
*o
4,
L.
0
oC/)
-J
0
a)
0.
x
w
'o6
o o
.5,
a)
C
-4
(D
C CO
C
'a
a
00
.
C) C)
za)
(x o
" Co
00
4-,
0
Le)
00
.A
§
a1)
* -
C
.0
.
C
0
0
0
'6-
z
) (0
(.0
a)
0.
C
C
I
o _
*T.'
4d
C
c)(O
rs
C
In
N..
:66 Cl
0
Coc o10
o,-
za)
a)
a)
co o
C
a
am
'-a t
0
a1)
C
0
.6C.)
C-)
a)
a)
£-
0.
0
'I-
E
E
a
)
-j0
a-
-j
0
c)
z
'- 0
v)
C)
a0
o
CD
CM
0
OO11
0Cv,I
I
o i
C;CSotc
1r-
)
I.-
.-
Ui
a)
a)
C
F
co
a)
- D*
-4
Co
-O
s
0
N
10 ,N
-jC C~icv,
z
)
C
0rc
_
.o( LOC
-r (:
a)
C) cS
I'4c6
C;)
cn
Ca
c\
U
E
.-.
oo
0c
C: L6 aO
CO 6 C)co
U)
'a
a)
@a
4
~
0
I-
C
0.
0
a)
0.
U)
Qa)
mE o
W-
a)
6a) c
.
a)
0
a)a
C)
>1
E
a-
cn
'0 L,
N C
(D - LO
C
*-,
U
-0
ECZ
a)
0
CD
w
a) cO o
C
a
E
m
C
-6
C
E
>
9P
6
O
0a).
.0
-
E
c
C
-6
C
a
'o
CD
aECCD
CZO
Q -0
a)
>E
_ Co
°- ' Zo
o
- 6#Ira
C
co
C.
a)
0)
a)
a)Ea)
U )
Cn .0
U)
IIC
>j
0
,
c
0
0
c 4)C C(12 C)C
L._
(0
I-
0.02(D
0.C
CM Co
r-
C,)
*a-
(0
cOCL I'Iq oR Lq
LO 00 LO r-
L.
Cu
(D OD rl r_
69. 6A.69- 69
E
E
P-'t - t
E
E
C
O CO 0
I0
0
CO CD
C0
C q(O cV)
(D
C
s2 cMl (
(U
CM
C\J
4)
I-
'E
C 'CML OCF) U)
r CO It It
0
CU
0m
000
0_-CC000
0 0CC0
a)
I-
,I.) c
Cf0
0
LO~O..C a q a Cy
r0s c ICC)
.Cia (sCJ)
a).) tcI
b-
a)
(o
c-
e0 -. N
co
,t
Lo
,'co r- Lo co co
0.
x
a)
,(<c
t )00
O0
a)
La)
0
O
cn -
r-
CO
0
O
V
Cf
- I
c
w -C C
ocqLm O cr
O
-NCIO
r a)
O(OOc O
't
O
rs u
C
CV)
LO
u=
(DN Ino
CO
*-
°O t cor
o Cr
6t
LO
(.
o
C\i9CJ
E
0C 0 , ._
'~- 03
U)C
0(C) C 0
0 co
'D
IN
a)
CO ^
1L
OON., cL
0I OCSN
C) O
O
L
FIL0
.o .
O
C
6
o 0o
^
^
)
^--
^O
~--M ^1
-C
I-
CC
') 0 ON
)
00--(DV)Oc
'0t
C rN
C
U) 6 C 6 o
C\
CJ
N C)
j
.0
00
C; -
0
x
c a)
CO CU
a) 0
C (~CO
CO
--:.
0--- LOC
o
0
0C0
._
E
E Co
-i
a
0 1-
CM
c C\.O
W -Wt
Co t 0
D't
U-)v
CI I' Q
!. co
LO
r'ls~s O t0
0
Cf) O O
- C> -c
t
'
-C
OI 't C)
o ov
I t ) Co
O0
O U) O CM O U) C
I
.-
-
O
-
--
0
o
C
q
1
t
C r
,
o U) C
E
a)
0C(I)
LO
0). 2
oYcVO
. LL
_""E.'
CIO
co
E a) )
Cc
E)
E w
.
Csa
-
on oE00> I
01
4)
ao
OU
'-a
c"*;oAI
nC
3 -a) c'-
o
co
C
L-
C
C
E~
*5
c
E~~~~~~~-t-
C .~a ,x
e"
0
._
C
a)
0
.
a)
0)
a_
a,n
0
0
.0
0
.2
C
C._
a)
o 0
0
0.
..
a00.
E
a)
0
1-
20
a
0.
C.
0a)
a
a1,
x
0
-j
0
a)
'a
0-
.
E
a)
0a
CCD
a)
2
o
o~
0
CJ
0mJ
coO
c0> o 0.
.
0
.mEn
a)a)>
(D
)
a)~>
LC,
o~~~~c
x
a)
0
a)
-J
0
4)
0
>)
a
I,
N1
oD
O
CD
O
CD
cal
11
cml
11
cal
11
&.
&.
a,
G) a)
m
>. >-
0
&.
0a,
,I-
0
0
.
C
OcE
0U
0
0
2
CO
C
>1
C
~in
° -oo o)
a,
a)
4)
0
~0
1
00'a)a.._
0
E
o
.@
a,
0.
sa)
a)m,
z
-I)--a@o2 a 20a)
0~~~~0
0
C..
0cnC1) C(
Ua)>C
U)
C
0
a)
um
0
N
Oci:
U)
Table 10 (con.)
Marginal cost regressions
Benefit characteristics
OLS
IV
(5)
(6)
-70.734
-68.445
(0.923)
(0.985)
Log(Beds per 1000 Medicare eligibles)
40.166
38.949
Log(MDs per 1000 Medicare eligibles)
(0.550)
3.715
(0.798)
(0.595)
3.851
(0.834)
Log(Hospitals per 1000 Medicare eligibles)
Log(Residents per 1000 Medicare eligibles)
Log(MDs teaching per 1000 Medicare eligibles)
-0.872
-1.187
(0.342)
(0.345)
-5.649
-5.576
(0.465)
(0.462)
-2.042
(0.459)
-1.810
(0.460)
Year=2000
45.666
51.147
Year=2001
(2.496)
101.021
(2.648)
103.633
Year=2002
132.818
142.883
(2.842)
7.261
(3.992)
16.630
(2.422)
10.078
(2.037)
(3.238)
-4.341
(7.916)
Log(MDs doing research per 1000 Medicare
eligibles)
Dummy for generic-only benefit
Dummy for non-formulary coverage
Monthly brand-name coverage amount
(2.761)
(2.816)
65.364
(11.456)
32.329
(4.206)
Monthly brand-namecoverage amount squared
-0.694
-2.577
Brand-name co-payment
(0.141)
-0.051
(0.081)
(0.324)
-1.313
Constant
Observations
R2
0.783
(0.292)
0.778
(0.110)
(0.109)
5317
0.95
5317
Dependent variable: marginal cost derived from parameters in Column (12) of Table 5.
Notes: Regressions weighted by inverse of standard deviation of marginal cost estimates. First
stage of binary endogenous variables estimated with probit. Benefit variables are instrumented
in IV regressions. Instruments include the average benefits of competing plans in county, the
average premium charged by competing plans in county and the Herfindahl index for Medicare
HMOs in county.
55
Chapter 2: Medicare HMOs, Prescription Drug Benefits, and
Selection
I.
Introduction
Much of the literature on Medicare HMOs has focused on the question of whether
Medicare HMOs experience favorable selection and if so, how much (Atherly et al. 2004,
Ellis and Garcia-Goii 2004, Greenwald et al. 2000, Mello et al. 2002, Mello et al. 2003;
for a review of the pre-2000 literature, see Hellinger and Wong 2000). The consensus is
that Medicare HMOs do enroll beneficiaries who are on average significantly healthier
than the average Medicare beneficiary.
A related question that has not been very well explored, however, is how
Medicare HMOs' choices of their premiums and benefits affects selection differentially.
This is an interesting question because, in the past, policies have had a strong impact on
Medicare HMOs' behavior that was not predicted beforehand due to misunderstanding of
the market in which they operated. A key example is the exit of HMOs from Medicare
following the passage of the Balanced Budget Act of 1997. Starting in 1999, when the act
took effect, a large number of HMOs left the program or reduced their service areas, and
the exits continued for several years following. From 1999 to 2002, the number of HMOs
in the program declined from 290 in 1999 to 143 in 2002, the number of counties served
by the program declined from 808 to 540, and the number of enrollees declined from 6.1
million to 4.8 million.
It is not very well understood why the HMOs exited in such large numbers. The
primary reason HMO executives gave for exiting was that their reimbursement was not
56
high enough (Draper et al. 2002). The reimbursement
level does not explain however
why many HMOs chose to exit rather than raise their premiums and lower their benefits.
Most HMOs that stayed in the program did raise their premiums and lower their benefits
but a large number chose to exit instead.
Lake and Brown (2002) examined the factors contributing to HMOs' exit
decisions. They found that the most significant factors were reimbursement
level, the
profit status of the HMO (for-profit plans were more likely to leave) and whether the plan
was national (national plans were more likely to leave). They do not explore why the
HMOs that chose to exit did so instead of raising the cost sharing borne by enrollees.
A possible explanation for the HMOs' decision to exit is that raising premiums
and/or lowering benefits would have different effects on healthy and sick enrollees'
decisions, causing adverse selection. The risk of adverse selection could cause the HMOs
to exit since it might reduce their profit enough that offering a Medicare product would
no longer be profitable, given the fixed costs. As evidence of this hypothesis, HMO
executives of national plans cite adverse selection as a concern when discussing their
decisions to exit (Draper et al. 2002, Hurley et al. 2003).
On the face of it, it seems surprising that HMO executives should be concerned
about adverse selection when Medicare HMOs in general enjoy favorable selection.
Medicare HMOs do have features, however, that might make them attractive to sicker
beneficiaries. First, many of them offer prescription drug benefits, which would be
demanded more by beneficiaries with conditions requiring prescription drugs. Second,
while patients in general prefer fee-for-service when they are sick, Medicare HMOs are
sometimes the only supplementary plan available for beneficiaries who are neither
57
eligible for Medicaid nor have employer-sponsored retiree benefits. Murgolo (2002) finds
that the income distribution of Medicare HMO enrollees is more weighted towards the
lower middle, while the income distribution of fee-for-service (FFS) enrollees is more
weighted towards the extremes. Among beneficiaries not eligible for Medicaid therefore,
Medicare HMO enrollees will generally have lower incomes than FFS enrollees and
therefore both might find the supplementary benefits of HMOs more attractive and might
be in poorer health.
Theory therefore makes an ambiguous prediction about what enrollees will leave
Medicare HMOs first if the HMOs raise premiums or lower benefits. If the HMOs raise
premiums, the healthy could leave first because they are richer and do not value extra
benefits as much, or the sick could leave first because they have a higher disutility from
being in managed care. Similarly, if the HMOs lower benefits, the healthy could leave
first because the HMO has overall become less attractive or the sick could leave first
because the value of the benefits is no longer higher than the disutility of being in
managed care.
In this paper, I will address the question of how changing premiums and benefits
affects selection by looking at the effect of Medicare HMO premiums and benefits on the
level of risk in the FFS sector of each county. If a change in premiums or benefits causes
favorable selection in the HMO, we should observe an increase in the risk level of FFS
beneficiaries but if it causes adverse selection in the HMO, we should observe a decrease
in the risk level of FFS beneficiaries.
58
II.
Previous work
There have been two previous papers that addressed this question. Feldman et al.
(2003) study the effect of HMOs changing their drug benefits on the average risk level of
other HMOs in the market and find some evidence that higher benefits cause adverse
selection. Their study is limited in two ways, however. First, they take the total
enrollment in HMOs in a county as exogenous and only look at the change in relative risk
levels among the HMOs. Their analysis therefore precludes the possibility that HMOs'
benefits and premiums affects the overall level of selection in the HMO sector. Their risk
measures are also made at the plan level, not the plan-county level, and they are forced to
assume that average risk in a plan is equal across all counties in its service area.
The second paper, by Atherly et al. (2004), studies the choice of Medicare HMOs
at an individual level, using data from the Medicare Current Beneficiary Survey. With
individual data, they are able to interact beneficiary characteristics with plan choice to
find the effect of health status on plan choice and find some evidence that beneficiaries
with chronic illnesses choose an HMO with prescription drug benefits, conditional on
choosing an HMO. They only control for the presence of prescription drug benefits,
however, not the level. With regard to the choice of sector, they find that beneficiaries
choosing HMOs rate their health higher on average.
Neither paper addresses the question of how the level of drug benefits and
premiums offered by HMOs affects selection in the HMO sector relative to the FFS
sector.
59
III.
A model of plan choice by Medicare beneficiaries
The following section outlines a model of selection bias showing why the
direction of selection when Medicare HMOs raise their premiums or reduce their benefits
cannot be predicted.
Intuitively, this result comes from the unusual structure of Medicare beneficiaries'
choices. In conventional models of selection in health insurance (Cutler and Reber 1998,
Cutler and Zeckhauser 2000), it is assumed that choosers are choosing between two
plans, one that is more generous for all benefits and one that is less generous. Medicare
beneficiaries, however, are choosing between being in traditional Medicare (possibly
combined with a Medigap supplementary plan) and enrolling in a Medicare HMO.
Traditional Medicare has no constraints on utilization of services, which is attractive to
beneficiaries with health problems, but has high-cost sharing and does not cover
outpatient prescription drugs, which may drive away sicker beneficiaries. Medicare
HMOs, as managed care plans, have lower cost-sharing and often cover prescription
drugs but put constraints on utilization. The two choices therefore each have features that
will tend to influence selection in opposite directions and it is ambiguous exactly how
beneficiaries will respond when HMO premiums and benefits are changed.
To put the argument more formally, assume a market similar to that presented in
Rothschild and Stiglitz (1976) and Cutler and Zeckhauser (2000) where there are two
individuals, one high-risk and one low-risk. These individuals each derive utility from
their Medicare choices which is a function of the benefits provided, the premium paid,
and the level of strictness in management by the health plan:
U = U(b, p) -
(1)
60
where b = benefits, p = premium and
is a scalar measuring the disutility derived from
being in managed care. U(b, p) is a concave function that is increasing in b and
decreasing in p.
Figure
graphs the utility function against the level of benefits, holding the
premium and disutility for managed care constant. If we normalize the level of utility
derived from being in traditional Medicare to zero, as benefits drop, the beneficiary will
switch to traditional Medicare when benefits pass point A, since that is when her total
utility from being in an HMO drops below zero.
The high-risk and low-risk types can be assumed to have different relative
valuations of the HMO's benefits and of being in managed care. Let us assume that highrisk people value the HMO's benefits at a higher level but also have a higher disutility of
being in managed care. These assumptions alone do not predict which type will leave
managed care first when managed care benefits drop. To see this, consider Figures 2 and
3. Figure 2 graphs the utility functions of the high-risk and the low-risk types against
each other under the scenario where lowering the benefits causes favorable selection for
the HMO. The utility function for the high-risk type is given by Us(b,p)-4s and that for
the low-risk type is given by UH(b,p)-OH. In Figure 2, as b drops, the high-risk types
switch first to FFS, at B, and the low-risk types follow when b drops below A.
Figure 3 shows how the reverse can hold under the same assumptions. If the highrisk types' utility from drug benefits is higher relative to that of the low-risks, or their
disutility from being in managed care is less, the low-risk types will drop out first as b
drops, at A, and the high-risks follow when b drops below B, causing adverse selection in
the HMOs.
61
This model illustrates how which case holds can be tested by looking at the
change in the average risk levels of those enrolled in FFS Medicare. As benefits in HMOs
drop, there will be a shift from HMOs to FFS, and whether the HMOs experience
favorable or adverse selection will be shown by the effect on the risk level of those in
FFS, holding everything else equal.
In a simple model, where HMOs and FFS may be assumed to have the same
average risk level initially, the direction of selection can be directly inferred by the sign
of the change in average risk level in the FFS sector. If average risk in the FFS sector
rises as a result of benefit changes in the HMO sector, the beneficiaries switching into
FFS are sicker than average and that implies that the HMOs are experiencing favorable
selection as a result of the change. On the other hand, if average risk in the FFS sector
falls, the beneficiaries switching into FFS are healthier than average and the HMOs are
therefore experiencing adverse selection as a result of the change.
As mentioned above, however, HMOs in general experience favorable selection
and the initial average risk level in HMOs will be lower than that in the FFS sector. The
interpretation of a falling risk level in the FFS sector can therefore be ambiguous for the
direction of selection in HMOs, since beneficiaries who are healthy enough to be
lowering the average risk level in the FFS sector may still be high-risk in the HMO
sector. The correct interpretation will therefore depend on the magnitude of the effect that
changing benefits and premiums has on the average risk level in FFS. If the changes
cause a drop in the risk level larger than the average difference between the managed care
and FFS sectors, that implies that the HMOs are experiencing adverse selection. If,
however, the changes cause either an increase in the risk level or a drop in the risk level
62
smaller than the average difference between the managed care and FFS sectors, that
implies that the HMOs are experiencing favorable selection.
IV.
Data on Medicare HMOs and risk in the Medicare FFS sector
The data for this study consist of Medicare HMO premiums and prescription drug
benefits by plan-county and average demographic factors and market shares for the FFS
sector by county for the year 1999-2002. There are also average risk scores for the FFS
sector by county for the years 2000-2001. These data were all obtained from CMS. The
data for the premiums and benefits of Medicare HMOs came from the Medicare Compare
database, the online tool that allows Medicare beneficiaries to compare Medicare HMOs
available in their county. The FFS risk score data come from the FFS expenditure data on
CMS's website (http://www.cms.hhs.gov/healthplans/rates/default.asp).
The prescription drug benefit data consists of co-payments for brand-name and
generic drugs, and drug coverage limits and are measured in three ways. The first is a
simple indicator for whether or not the plan offered prescription drug benefits. About
one-third of HMOs do not offer prescription drug benefits at all. The second is the brandname coverage limit and the third is a measure of expenditure incurred by an average
prescription drug user that would be covered by the plan. (For details of how this variable
is calculated, see Chapter 1). To get a county-level measure of generosity in the HMO
sector, the premiums and benefits are averaged across HMOs within in the county.
As discussed in the introduction, the Balanced Budget Act caused both exit from
the Medicare HMO program and a reduction in benefits and increase in premiums for the
plans that stayed in. Table 1 reports summary statistics for each year, showing the
63
changes in the program. The average premium increased from about $13 to $38 and the
average expenditure of an average prescription drug user covered by the plan decreased
from $781 to $567.
Risk in the FFS sector is measured in two ways. First, it is measured by the
average demographic factor among FFS beneficiaries in the county. The demographic
factor is an adjustment made by CMS to the Medicare HMO county base reimbursement
rate for each Medicare HMO enrollee based on their observed demographic
characteristics. The adjustment is the ratio of the expected cost for that demographic
category to the expected cost of an average Medicare enrollee. The demographics used
are gender, age, institutionalization status, Medicaid status and employment status and
the factors range from .35 (for a 65- to 69-year-old female who is employed) to 2.6 (for
an 85+-year-old male who is on Medicaid and not working). In other words, if a 65- to
69-year-old female who is employed enrolled in a Medicare HMO, the HMO received
35% of the county base reimbursement rate (previous to the Balanced Budget Act, when
the formula was changed). Table 2 reports the demographic cost factors used by CMS
from 1997 to 2005.
As part of the base rate calculation process, CMS calculates the average
demographic factor for all FFS enrollees in the county and reports it in the FFS sector
expenditure data for the county. The demographic factors are for aged enrollees only and
are reported separately for Part A and Part B.
Risk is also measured using the average risk scores for FFS enrollees in the
county. In 2000, CMS began partially risk-adjusting reimbursements to Medicare HMOs
based on demographics and enrollees' inpatient diagnoses from the previous year (for
64
details, see Ingber 2000). The risk score is also reported as the ratio of the expected cost
for the enrollee to the average cost of an enrollee. Again, as part of the rate calculation
process, CMS reports average risk scores for the FFS sector for each county. Since risk
adjustment did not start until 2000 and the risk scores are missing in the 2002 expenditure
data for unknown reasons, the data are only available for 2000-2001. In 2000, the average
county risk scores ranged from .74 to 1.42 and in 2001, from .73 to 1.27.
V.
Empirical specification
The equation to be estimated is:
Average FFS riskmt= a*avg premiumm, + ,3*avgdrug benefitsmt+ mm + tt + £mt
(2)
where m is the county and t is the year. The county effects will be captured with county
fixed effects and the year effects will be captured with year dummy variables. Since
county fixed effects and year dummies demean the variables both cross-sectionally and
over time, (2) is equivalent to regressing the county-year specific change to average FFS
risk on the county-year specific changes to the HMO premiums and drug benefits. The
coefficients will therefore be estimates of the effect of variation in the HMO premiums
and benefits on variation in the average FFS risk that is not explained by the county or
the year.
Since the dependent variable is a county-level mean, the variance of the error term
is proportional to the population over which the mean is calculated. To correct for this
heteroskedasticity, the regressions are weighted by the square root of the relevant
population variable for the measure of risk being used: Part A enrollment for the Part A
demographic factor, Part B enrollment for the Part B demographic factor, and the aged
65
and disabled population together for the risk score. To correct for any remaining
heteroskedasticity
or serial correlation, robust standard errors are calculated by the
formula for fixed effects models given by Arellano (1987).
If we were considering this problem with conventional HMOs, a concern might
arise that HMO premiums and risk in the FFS sector are jointly determined because the
premiums are determined by the risk level of the HMO beneficiaries. The identifying
assumption will therefore be that the risk level of enrollees does not determine Medicare
HMO premiums and benefits in the plan. This assumption is plausible because Medicare
HMOs derive most of their revenue from the reimbursement they receive from the
government, not from the premium. In 1999 for example, the average base
reimbursement rate in counties that contained HMOs was $469.23, while the average
premium charged by HMOs was $10.87 and two-thirds of Medicare HMOs did not
charge a premium at all.
The size of the premium relative to the reimbursement is relevant because it
shows that the HMOs did not rely on the premium for very much of their revenue. They
were therefore free to adjust it and the benefits to influence selection. There is empirical
evidence that Medicare HMOs set their benefits and premiums to attract healthier
beneficiaries. Cao and McGuire (2003) show that average FFS costs for inpatient and
mental health services are higher when the HMO penetration rate is higher, suggesting
that the HMOs are under-providing those services, while the reverse is true for primary
care and general surgery. Gurol and Ellis (2004) show that there is little relation between
payment rates and the premiums Medicare HMOs charge. They also show that payment
rates have no effect on whether HMOs offer benefits that are attractive to healthy
66
enrollees (such as physicals) but payment rates combined with the level of competition
strongly affect whether or not HMOs offer benefits that attract sicker enrollees (such as
prescription drug benefits and foot care).
It is therefore plausible to assume that benefits and premiums are exogenous to
selection in the FFS sector since they are often deliberately set to influence selection in
the HMO sector. While the HMOs' power to affect selection might suggest that we
would only ever observe them experiencing favorable selection, it is still possible we
would observe adverse selection because the decisions of the HMOs remaining in the
program are not solely based on the potential effect on selection but on other factors as
well, including a desire to serve the community of Medicare beneficiaries as well as a
desire to maintain their reputation. As discussed above, some HMOs exited after the
Balanced Budget Act passed, and Lake and Brown (2002) show that the HMOs were
more likely to exit during this period if they were for-profit. These HMOs may have
therefore exited to avoid adverse selection because they were primarily motivated by
profit while the HMOs that remained may have undergone adverse selection rather than
exit because of their other motivations. The only requirement for exogeneity is that their
other motivations do not affect the risk level of who is enrolled in their plan.
In order to interpret the results, I will also have to make assumptions about the
direction of movement between FFS and HMOs that result from premium and benefit
changes. Both Chapter
and several other studies (Town and Liu 2003, Dowd et al.
2003, Atherly et al. 2004) have shown that HMO enrollees are sensitive to premiums and
benefits and that HMO market shares respond negatively to premium increases and
positively to benefit increases. I will assume therefore that, if HMOs raise their premiums
67
or decrease their benefits, these changes will cause movement from the HMO sector into
the FFS sector and conversely, if HMOs lower their premiums or increase their benefits,
these changes will cause movement from the FFS sector into the HMO sector. The
changes that HMOs made during this period were largely of the first type, however, and I
will focus on the effect of those.
VI.
Results
Table 3 shows results for the regressions with Part A and Part B demographic
factors as the dependent variable. As it shows, the coefficient on premium is positive and
significant across all specifications of the drug benefits, implying that raising the
premium in HMOs raises the average risk level in the FFS sector. Since I assume that an
increase in premiums causes a movement from the HMO sector into the FFS sector, a rise
in risk in the FFS sector implies that the beneficiaries switching into the FFS sector are
less healthy than the average beneficiary already enrolled in FFS Medicare. Since HMO
enrollees are, on average, healthier than FFS enrollees,
the beneficiaries
that are
switching must be much sicker than the average HMO enrollee and the positive
coefficient therefore indicates unambiguously that raising premiums increases the
HMOs' favorable selection.
The coefficient of .017 in column (1) implies that an increase of $10 in the
average premium in a county raises the average Part A demographic factor in the FFS
sector by .0017. (The demographic factors have been multiplied by 100 in the regressions
so that an average beneficiary has a demographic factor of 100.) This change appears to
be small but if the FFS share is large and the number of beneficiaries moving is relatively
68
small, a small change in average risk level can imply that the beneficiaries moving have
much higher risk.
It is impossible to know the risk level of beneficiaries moving without directly
observing those beneficiaries that move as a result of the change. It is possible to make an
estimate, however, using the regression coefficients and by making other assumptions
about the size of the market shares of FFS and the HMOs, about the number of people
moving in response to the change, and about the risk level in HMOs. To see this, consider
the following result from equation (2):
'IRiskFFS,+l = RiskFFS,+i- RiskFFSt =/ *
average premiumt+l
(3)
The change in risk that results from a change in premiums is equal to the coefficient
multiplied by that change. The change in risk occurs because there has been movement
from the HMC) sector to the FFS sector so we also know that the risk in FFS in period t+l
is a weighted average of the risk in FFS in period t and the risk of the beneficiaries that
moved into FFS:
RiskFFSt+l=
%FFS * RiskFFSt + %Movers* Riskmovers
(FFS+4)
%FFSt+i
(4
Note that:
%FFSt+
1 = %FFSt + %Movers
(5)
Combining (3) with (4) and solving for Riskmovers, we find that:
Riskmovers=
(6)
To solve this equation, we must make assumptions about %FFS, RiskFFSt, and
7%Movers.For %FFSt and RiskFFS, it seems natural to take the observed average of
these variables in the data in the first year of the period observed. The average FFS
69
market share in 1999 in counties that have an HMO is 84.9%, the average Part A
demographic
factor is .972, the average Part B demographic factor is .991 and the
average risk score in 2000 is .979.
It is less clear how to make assumptions about the number of people who move
since we do not directly observe the number of people who move because of the change,
but only observe the net movement of people in and out of the FFS sector. Other studies,
however, have made estimates of the effect on HMO market shares of changes in their
premiums and benefits, which can be used here. Both Chapter 1 and Town and Liu
(2003) estimate the effect of a $10 premium increase on that HMO's market share; Town
and Liu estimate that the increase lowers the market share by 9% and Chapter 1 estimates
that the increase lowers the market share by 5-8%.
Table 5 shows the calculation of the risk level of people moving in response to a
$10 premium increase in a market where the initial FFS market share is 84.9% and the
initial FFS risk levels are the averages, as described above. To test the sensitivity of the
calculation to assumptions about the number of people moving, the calculation was
performed for different values of the effect of the change on the HMO market share in the
neighborhood of Town and Liu's estimates and the estimates presented in Chapter 1.
The results show that, for a 5 percent drop in the HMO's market share, the
beneficiaries that move have an average risk level of 1.17, and for a 9 percent drop in the
HMO's market share, the beneficiaries that move have an average risk level of 1.08. The
results are very similar for the Part B demographic factor; for a 5 percent drop, the
beneficiaries that move have an average risk level of 1.16 and for a 9 percent drop, the
beneficiaries that move have an average risk level of 1.09. The beneficiaries that are
70
moving therefore belong to demographic categories that have a somewhat higher
predicted level of spending than average.
Table 4 reports the results for the regressions with the risk score as the dependent
variable. As it shows, changes in HMO premiums have no significant effect on the
average risk score in the FFS sector. In Table 5, we see that, for a 5 percent drop in the
HNMO'smarket share, the risk level of the beneficiaries moving is calculated to be .922
and, for a 9 percent drop, it is calculated to be .947. The difference in results between the
demographic factors and the risk score suggest that, while the people who leave HMOs
when premiums rise belong to demographic categories with higher predicted spending
(such as male, older, subsequently enrolling in Medicaid or being in a nursing home), in
fact, these people are no sicker than the average FFS beneficiary.
The results for the benefits have a similar interpretation. Columns (1) and (2) of
Table 3 show that dropping drug benefits increases the average FFS risk level by .014. In
Chapter 1, it was estimated that dropping a prescription drug benefit lowers an HMO's
market share by 10.8% so Table 6 shows the average risk level of beneficiaries moving
uLinder
the same assumptions as Table 5 and for values of the decrease in the HMO market
share in the neighborhood of 10.8%. The results show that dropping prescription drug
benefits triggers the movement of beneficiaries belonging to demographic categories that
are predicted to have very high spending; the average Part A demographic factor of these
movers is 1.73 and the average Part B demographic factor is 1.69. As Table 2 shows,
these averages are so high as to imply that the average beneficiary moving as a result of
prescription drug benefits dropping must be either institutionalized or on Medicaid. The
risk score results show, however, that the beneficiaries moving are not actually sicker
71
than the average FFS beneficiary since, as column (1) of Table 4 shows, dropping drug
benefits has no significant effect on the average risk score in the FFS sector. The
beneficiaries moving as a result of the change, while belonging to demographic
categories predicted to have high spending, are therefore not actually sicker than average,
as measured by their inpatient diagnoses of the previous year. (HMOs were required to
report the inpatient diagnoses of their enrollees to CMS so it is not the case that enrollees
moving into FFS had understated risk scores because of missing information.) Since FFS
enrollees are on average sicker than HMO enrollees, however, the risk score in the HMO
sector must have dropped as a result of losing these beneficiaries, so the change caused
favorable selection for the HMOs.
Columns (5) through (8) of Table 3 and columns (2) and (3) of Table 4 show
similar results when controlling for the level of drug benefits. Reducing the average level
of drug benefits in the HMO sector causes a significant rise in the FFS demographic
factors. Specifically, reducing the monthly brand-name coverage amount by $100 raises
the average Part A demographic factor by .0074 and the average Part B demographic
factor by .0081. Again, these estimates seem small but Table 7 shows the risk level of the
beneficiaries who move in response to reducing the monthly brand-name coverage
amount. In Chapter 1, it was found that halving brand-name coverage lowered the market
share of HMOs by 14.7% so the effect of the change is considered in the neighborhood of
this value. Since the average brand-name
coverage
amount in 1999 is $140, the
hypothesized change is a $70 drop in brand-name coverage. The results show that the
beneficiaries moving were above average in risk level as measured by their demographic
factor; beneficiaries moving had an average Part A demographic factor of 1.21 and an
72
average Part B demographic factor of 1.23. Changing the amount of brand-name
coverage has no significant effect, however, on the average risk score in the FFS sector
and the average risk score of beneficiaries changing sectors is .994. As in the case of
dropping drug benefits entirely, therefore, we find that the people who are moving in
response to the change fall into demographic categories predicted to have higher
spending but are not sicker than average as measured by their inpatient diagnoses in the
previous year.
The results are similar for the level of benefits as measured by the amount of
expenditure for an average prescription drug user covered by the plan. (For details on the
construction of this variable, see Chapter 1.) This measure differs from the amount of
brand-name coverage by including the generosity of the generic coverage and taking into
account the co-payments and which categories of drugs (generic or brand-name) the
coverage limit applies to.
The results in Table 3 show that lowering the monthly covered expenditure by $1
raises both the Part A and Part B demographic factors by .0003. Translating these
amounts into the implied risk level of the beneficiaries changing sectors, we find in Table
8 that a drop in the average monthly covered expenditure among HMOs of $27 causes
beneficiaries with an average Part A demographic factor of 1.25 and an average Part B
demographic factor of 1.29 to move to the FFS sector. This result assumes a 17.3% drop
in the initial HMO market share of 15.1%, following Chapter 1 where it was shown that
halving the monthly expenditure covered by the plan caused an HMO's share to drop by
17.3%. Again, the lowering of benefits has an insignificant effect on the risk score and
the beneficiaries moving are predicted to have an average risk score of 1.01.
73
VII.
Discussion
The results presented show that raising premiums and lowering benefits increases
HMOs' favorable selection. The beneficiaries predicted to move as a result of the
changes have average to above-average risk among FFS enrollees, so must be
considerably sicker than the average HMO enrollee. Greenwald et al. (2000) compare
risk scores of the FFS and HMO sectors on a county-by-county basis and find that in the
median county, the average risk score for HMO enrollees differs from the average risk
score for FFS enrollees by 13.6%. If FFS enrollees have an average risk score of .98, this
implies that HMO enrollees have an average risk score of .85 in the median county, so
enrollees with a risk factor equal to the FFS average are significantly less healthy than the
average HMO enrollee.
In the context of the model presented in Section III, therefore, the case presented
in Figure 2 holds. Either the sicker beneficiaries' valuation of the drug benefits is not that
great compared to the healthy's valuation or the sick have a great disutility of managed
care relative to the healthy.
As discussed in the previous section, there is a noticeable difference in the effect
of HMOs changing their premiums and benefits on the average demographic scores and
the average risk scores in the FFS sector. Increasing premiums and reducing benefits
significantly raised the average demographic factor in the FFS sector but had no
significant effect on the average risk score. There are two ways to interpret this
difference. First, it is possible that HMO enrollees are not just healthier unconditionally
but that, conditional on demographics, they are healthier, and so the enrollees leaving
74
HMOs are among the healthier in their demographic category. Even though enrollees
may belong tlo categories with above average predicted spending (that is, they are male,
older, institutionalized, or enroll in Medicaid), they may still be relatively healthy for
those categories and that is why they chose the HMO in the first place.
The other possibility
is that the risk score does not entirely capture the
beneficiaries' predicted spending. The risk adjustment model used by CMS during this
period reflected only inpatient diagnoses (see Ingber 2000). Since HMOs controlled
inpatient utilization more than FFS Medicare, HMO enrollees may therefore have
appeared healthier than they would have if they had been enrolled in the FFS sector.
There is evidence that the HMOs were successful in lowering inpatient utilization, even
after controlling for the favorable selection they had (Dhanani et al. 2004, Mello et al.
2002). The risk score would also have not reflected any chronic illnesses the beneficiary
had and Atherly et al. (2004) showed that having a chronic illness made a beneficiary
slightly more likely to enroll in an HMO offering a drug benefit. The beneficiaries
moving out of HMOs as a result of benefit cuts may therefore have been sicker than they
appear by the risk score. The risk score that is observed, however, is still a lower bound
on their true level of sickness and the results still point towards HMOs experiencing
increased favorable selection as a result of the changes.
VIII. Conclusion
This paper showed that the increases in premiums and cuts in prescription drug
benefits undertaken by Medicare HMOs during the period immediately following the
passage of the Balanced Budget Act caused significant rises in the average demographic
75
factors in the FFS sector but did not affect average risk scores in FFS Medicare. These
results imply that the risk levels of the beneficiaries that moved as a result of the changes
were at least as sick as the average beneficiary already enrolled in FFS and therefore
sicker than the average HMO beneficiary. Increasing premiums and lowering drug
benefits therefore increased favorable selection for the HMOs.
As discussed in the introduction, a motivation for exploring this question was to
see if raising premiums and lowering drug benefits caused adverse selection in the
HMOs, as some of the HMO executive claimed. The results presented here show that,
rather, these changes increased the HMOs' favorable selection. The results, however, are
necessarily limited by the endogeneity of exit; we can only observe those HMOs that
remained in the market and it is still possible that HMOs who, for idiosyncratic reasons,
would have experienced adverse selection as a consequence of raising premiums and
cutting benefits, chose to leave the market instead.
76
References
Arellano, M. (1987). "Computing Robust Standard Errors for Within-groups Estimators."
Oxford Bulletin of Economics and Statistics 49(4): 431-434.
Atherly, A., B. E. Dowd, et al. (2004). "The Effect of Benefits, Premiums, and Health
Risk on Health Plan Choice in the Medicare Program." Health Services Research
39(4, Part I): 847-864.
Cao, Z. and T. G. McGuire (2003). "Service-level selection by HMOs in Medicare."
Journal of Health Economics 22: 915-931.
Cutler, D. M. and S. J. Reber (1998). "Paying for Health Insurance: The Trade-off
Between Competition and Adverse Selection." Quarterly Journal of Economics
113(2): 433-467.
Cutler, D. M. and R. J. Zeckhauser (2000). The Anatomy of Health Insurance. Handbook
of Health Economics. A. J. Culyer and J. P. Newhouse, Elsevier Science B. V. 1:
563-643.
I)hanani, N., J. F. O'Leary, et al. (2004). "The Effect of HMOs on the Inpatient
Utilization of Medicare Beneficiaries." Health Services Research 39(5): 16071627.
I)owd, B. E., R. Feldman, et al. (2003). "The Effect of Health Plan Characteristics on
Medicare+Choice Enrollment." Health Services Research 38(1, Part I): 113-135.
D)raper, D., M. Gold, et al. (2002). The Role of National Firms in Medicare+Choice, The
Henry J. Kaiser Family Foundation: 58.
Ellis, R. P. and M. Garcia-Goni (2004). Selection in Medicare HMOs: Absence of
Evidence from Aged versus Disabled Payment Rates: 19.
Feldman, R., B. Dowd, et al. (2003). "Risk Selection and Benefits in the
Medicare+Choice Program." Health Care Financing Review 25(1): 23-36.
Greenwald, L. M., J. M. Levy, et al. (2000). "Favorable Selection in the
Medicare+Choice Program: New Evidence." Health Care Financing Review
21(3): 127-134.
Gurol, I. and R. P. Ellis (2004). Medicare Managed Care Choice of Benefits and
Premiums: Competition and Selection Incentives Really Matter: 27.
Hellinger, F. J. and H. S. Wong (2000). "Selection Bias in HMOs: A Review of the
Evidence." Medical Care Research and Review 57(4): 405-439.
Hurley, R. E., J. M. Grossman, et al. (2003). "Medicare Contracting Risk/Medicare Risk
Contracting: A Life-Cycle View from Twelve Markets." Health Services
77
Research 38(1): 395-417.
Ingber, M. J. (2000). "Implementation of Risk Adjustment for Medicare." Health Care
Financing Review 21(3): 119-126.
Lake, T. and R. Brown (2002). Medicare+Choice Withdrawals: Understanding Key
Factors, The Henry J. Kaiser Family Foundation: 41.
Mello, M. M., S. C. Stearns, et al. (2002). "Do Medicare HMOs still reduce health
services use after controlling for selection bias?" Health Economics 11: 323-340.
Mello, M. M., S. C. Stearns, et al. (2003). "Understanding Biased Selection in Medicare
HMOs." Health Services Research 38(3): 961-992.
Murgolo, M. S. (2002). "Comparison of Medicare Risk HMO and FFS Enrollees." Health
Care Financing Review 24(1): 177-185.
Rothschild, M. and J. Stiglitz (1976). "Equilibrium in Competitive Insurance Markets: An
Essay on the Economics of Imperfect Information." Quarterly Journal of
Economics 90(4): 629-649.
Town, R. and S. Liu (2003). "The welfare impact of Medicare HMOs." The RAND
Journal of Economics 34(4): 719-736.
78
U
0
A
Figure 1
79
Us(b,p)-os
-]
A B
Figure 2
[
"UHs(b,p)-oH
UH(b,p)-qOH
w
-$H
S
i
(
r
t
BA
Figure 3
80
b
E
0000
O C C)O
- - O
E
6116 6 6)
w--
._
-
--
(0
u CO
('tLO
(0
LOLO
00oCM 'COUO)
UD o Lo
-- wJ
co
1,y). - - - 6 6 6
6 6k6
I- U') C 0 0
C\l (.0
6021,69. 619-
f 6
C
6
69 69f 9 69 69l
Ot -
It
0 Co ) C co
-(D
b--CO
0
- (O
ci L6 oi r: 0) C\i
rC- c6S oo 6
C\ C
Ct)
CMCM
r'- ( L o 6 6 60 69 6 6 6. 4) 61) Sl)
O 00
a
z
00
CM
CO LO(
t CO
Ir
I'
C0 CO LO '
Ct)O- D
CO
CO
,t
t
CO
CO
C
060
C CO
CMl r,~
LO N-
60
600
CMj
-
LI
6 696--
O
) 0 0C0 0 'C)
0o C\J CM CM c0 C\j CM CM o00C\
C
C
'0t C)w
C]
Cj Cj C\j CO CM C\j CM O C~ CM
of
0d
O0O0 O0O
0 0
6
*ft
6
co r- CM r.
U- C) CMjC:
U' f.0 6
MC)OIt
co
OD T-
V
-N
C
C C
C Ci
C
_
C1l C
T
0
C
CM
,-ONNN
C)
CM CM CMj
CM co
- CM
0- C 0)0 000
0) 000
)0)0 000 0)00
0 0)
0o) 000
M
0)0 o 0 0 0 00 0) 000 0)000
O C -
o
CO
0o LO
w O CD
Lo (o
Q') c)
0000 0000 000
E
00 I
0) o
O0
ft
0) ft (n
NcO0N-rOJOLO
6969. 61;
69d
0
NC
CM CM
0
!
0)
o
0)
CM
CD
oDCM C14 04
0)
- 0
co
'a)=
c00
1-4-*
-
0
a)
e'
000
.Q
0
a)
U0
0
a
0)
O
Q~
.)
0)0
t
O0
O.
C
0a)
0
a.
0.
*0
a)
0)
a..
E
Q
0M.
Cu
0
'O
'C
0
0.
._M
0
C
M
M
0
.4.
.0d
0
C.)
0~
0
0)
M
.C.
E
I0E
I.
0a)
E
C
Q
O
a)
M
a-
M
IF
0
a
M
4-
C
CQ
E
.E
a)
0
a
6
0
._.
a..
'o
o
c.o
E
M
'6.
0)
M
a)
C
D
Cu
a)
0
0C.)
_00)
0.
a)
.Q
0
0
-
,..
C.
0
0
a)
E
M
9u
0.
L.)
0.
0
I..
a)
0.
0)
CL
I-
x
0
O)
0Q.
.
X
w
Table 2
Demographic Cost Factors for Aged 1997-2005
Part
A
B
Sex
Male
Ag e
Non-lnstitutionalized
Medicaid
Non-Medicaid
Institutionalized
Working
65-69
1.75
1.15
0.65
0.40
70-74
75-79
80-84
85+
2.25
2.25
2.25
2.25
1.50
1.95
2.35
2.60
0.85
1.05
1.20
1.35
0.45
0.70
0.80
0.90
Female 65-69
1.45
0.80
0.55
0.35
70-74
75-79
80-84
85+
1.80
2.10
2.10
2.10
1.05
1.45
1.70
2.10
0.70
0.85
1.05
1.20
0.45
0.55
0.70
0.80
65-69
1.60
1.10
0.80
0.45
70-74
1.80
1.35
0.95
0.65
75-79
80-84
85+
1.95
1.95
1.95
1.55
1.70
1.70
1.10
1.15
1.15
0.80
0.90
1.00
1.50
1.65
1.65
1.65
1.05
1.15
1.25
1.25
0.70
0.85
0.95
0.95
0.40
0.55
0.70
0.75
1.65
1.25
1.00
0.85
Male
Female 65-69
70-74
75-79
80-84
85+
Source: http://www.cms.hhs.gov/healthplans/rates/2005/demofac.asp
82
CD
cO(
.
(O 0
O.o. ¢
Io o
00
C-' O
a' C;
o
C
04
aC0
fU) CD
orv9o) t (0 00 -
a
00
9 66C
O
C co r- r-
c
C~-
fIQ
6
o"- o-
co
0~
E
.,
C/o
34
L)
00
t LOCo
U)
LO
oocs
o9r)o
0 0oo0c
OD.0
o0o
0
U)
o _o
1.
9o,
a4-C
C
._
.C
C
a
-n
.-
cc)
-
6
6C
6
ct)
O0
(0l
O0 v-
rp-
co
a-,
a
6
co 00
00
O0
o?
Io
7
o
LC
r-
CO 'O
0 0
._
G)
c C
)r
0 a7"t Lo
06
6ooOro odd
-
Ct
(U)
C
CM-
C
CD
0C _ C--cm
--
13.
r
)
CM CO
-
C
E
Co
0 L
0
CD-OdC .
gcn o.(D
W>
't,
C
v .4 NC)
C-n
')O a
M
IC
:
.0
>4
C
Co
0
o o
o
oi
.o
,3-0
c5
cw c, t :cul o &I
Ms W r_- ( (.0
r C:
CD00 C . -). C0cm C
6
00
a)
00
a
c)
L.
CM
-n.
o io
r- O (D
6 !2
rC
CZ
-D
-3
0O)
_CZ
_0
C
U)
CD
co
,O
(D
o0
a)
CCD0
::3
C
V.
4..
[L
0
C
cn
-Da D
,t
o 0
-
co
doo
-
C)
c0 - rr-
0
o o c6 0 C:0
.L
0cn
E
C.
.
. )
0
._C
a
a)
en CD0
@
Im
¢3.
L
0
00
Im
..
.0
C
0
0
ns
(D
n
(D
'O-_
a)
o3
C)
C
0)
~C
0
.)
)
a.C
O
(D0
)C
a) 'n
-COU
0)
6.
mQ
o0) E
_E
._ 0.
a)
Cu CD a)
E
:
CD
v
Cu~~~
E
2)
U
2)
0..
X
0
-E
o
o
D
0)
a
na
=
>
E > E >
a
<
n
=
a
(OaDOa
L..
<
n <
o
.2
II
11
>
Cssuv
,6
o
II
a-
C-)
a n
~~~~~~~~~~~~~~~~~~~~~(._
00
0co
X cDo
2)
6.
0.-
W
w
0
0
C
=O
0
0)
0
E
>
>
CZ
O
O
ao-
c
0
(0
'I-
00
0)
.0
if
co
II
11
S-
a)
>-
S-
a)
>.
L-
a
>.
O)
CT
Ocx
ns
a.-
.~=
0
o
o
C:
O
O
CZ
U)
(3
0
T_
cm
O
00o
0
n~
o~~~~~oo o
o oCo
9
~o
qn 0 C~
O~~9C;C
6
v 0
0
C;
0
c
E
0
U)
co
5
c
°,'
o
-)
&~
oC-C o
c
>
U)
s
oo -OU)
C)
cm
UCO
a)
1
.'-
LU.
0
C
0
000
'--0
0"Z
U)2c
cUC
o
._
-
I-
00
~~Odod
o-E Cia)C
E E
0Cl
0W
o
) 0 0
0.
0o 0
L.
a
0
0
2
EE
m c.o
x
0
0
E
o0nos
)
E~E
-
U)
0 4
()
C
c ~
C
c5
o
L;
U)
.0 0
I._.
U)
-
clc_ a)=
00
C)
U
'4-
he-
)
m
-- -~
E
0.
.0 'B
LU
<
04
oco
~.C
0 0e
EE
0.4
C
0E o
=
> 4> o0U)0
(
(
0C. 4
. 0.
>
Oc
0 -e0 D.
a)
0
>0.
OZUCZ
Z
00
Table 5
Average risk of beneficiaries moving in response to a change in
premium under different assumptions
Rt
%FFSt
Part A
demographic
factor
0.9723
Part B
demographic
factor
0.9909
Risk score
0.9785
0.017
0.015
-0.005
$10
$10
$10
84.9%
.Are..um
,&premium
Number of people
Percent drop in
HMO market
share
3%
4%
switching sectors in
percentage points
(%Movers)
0.45%
0.60%
1.29
1.21
5%
0.76%
1.17
1.16
0.92
6%
7%
8%
9%
10%
0.91%
1.06%
1.21%
1.36%
1.51%
1.13
1.11
1.09
1.08
1.07
1.13
1.11
1.10
1.09
1.08
0.93
0.94
0.94
0.95
0.95
85
Risk level of movers
1.27
1.20
0.88
0.91
Table 6
Average risk of beneficiaries moving in response to dropping
prescription drug benefits under different assumptions
Part A
Part B
demographic
factor
demographic
factor
Risk score
0.9723
0.9909
0.9785
-1.422
-1.316
0.021
-1
-1
Rt
%FFSt
84.9%
fiRx
ARx
-1
Number of people
Percent drop in
switching sectors in
HMO market
share
percentage points
(%Movers)
8.0%
8.5%
9.0%
9.5%
10.0%
10.8%
11.0%
11.5%
12.0%
12.5%
13.0%
13.5%
14.0%
14.5%
15.0%
1.21%
1.28%
1.36%
1.43%
1.51%
1.63%
1.66%
1.74%
1.81%
1.89%
1.96%
2.04%
2.11%
2.19%
2.27%
Risk level of movers
1.99
1.93
1.87
1.83
1.79
1.73
1.71
1.68
1.65
1.63
1.60
1.58
1.56
1.54
1.52
86
1.93
1.87
1.83
1.78
1.74
1.69
1.68
1.65
1.62
1.60
1.57
1.55
1.53
1.51
1.50
0.96
0.96
0.97
0.97
0.97
0.97
0.97
0.97
0.97
0.97
0.97
0.97
0.97
0.97
0.97
Table 7
Average risk of beneficiaries moving in response to lowering brand.
name coverage under different assumptions
Rt
%FFSt
Part A
Part B
demographic
factor
demographic
factor
Risk score
0.9723
0.9909
0.9785
-0.812
-0.883
-0.056
0.0002
-$70
84.9%
[coverageamount
Pcoverage
amount
squared
0.07
0.076
Acoverage amount
-$70
-$70
Number of
people
switching
Percent drop in
HMO market share
sectors in
percentage
points
(%Movers)
12.0%
12.5%
13.0%
13.5%
14.0%
14.7%
15.0%
15.5%
16.0%
16.5%
17.0%
1.81%
1.89%
1.96%
2.04%
2.11%
2.22%
2.27%
2.34%
2.42%
2.49%
2.57%
Risk level of movers
1.2607
1.2494
1.2390
1.2293
1.2204
1.2089
1.2042
1.1970
1.1901
1.1837
1.1777
87
1.3045
1.2922
1.2809
1.2704
1.2606
1.2481
1.2431
1.2352
1.2277
1.2208
1.2142
0.9973
0.9966
0.9959
0.9953
0.9947
0.9939
0.9936
0.9931
0.9927
0.9923
0.9919
Table 8
Average risk of beneficiaries moving in response to lowering
monthly covered expenditure under different assumptions
Part A
Part B
demographic
factor
demographic
factor
Risk score
0.9723
0.9909
0.9785
-0.031
-$27
-0.033
-0.003
-$27
-$27
Rt
%FFSt
84.9%
Pcoveredexpenditure
Acovered expenditure
Percent drop in
Number of people
switching sectors in
percentage points
HMO market share
(%Movers)
15.0%
15.5%
16.0%
16.5%
17.0%
17.3%
18.0%
18.5%
19.0%
19.5%
20.0%
20.5%
2.27%
2.34%
2.42%
2.49%
2.57%
2.61%
2.72%
2.79%
2.87%
2.94%
3.02%
3.10%
Risk level of movers
1.29
1.28
1.27
1.27
1.26
1.25
1.24
1.24
1.23
1.22
1.22
1.21
88
1.33
1.32
1.31
1.30
1.29
1.29
1.28
1.27
1.26
1.26
1.25
1.24
1.01
1.01
1.01
1.01
1.01
1.01
1.00
1.00
1.00
1.00
1.00
1.00
Chapter 3: The Welfare Loss from Medicare+Choice
I.
Introduction
The Balanced Budget Act of 1997 (BBA) made several changes to the Medicare
fHMN4O
program. It changed the formula for calculating the base reimbursement rate for the
HMOs, increased the administrative requirements for plans participating in the program,
and opened the program to other kinds of private health plans, including PPOs and
private fee-for-service plans. The goal of these changes was to expand the role of private
plans in the Medicare program and to provide more choice to Medicare beneficiaries.
The act had the opposite effect, however.
In the four years following the
implementation of the act in 1999, the Medicare+Choice
program (as the BBA renamed
the Medicare HMO program) saw the number of HMOs in the program drop from 290 to
147, or by just under 50%. Many of the plans that remained in the program made changes
that reduced their availability and desirability, such as reducing their service area,
increasing their premiums and lowering their benefits. The average premium charged by
Medicare HMOs rose from $12.68 to $37.62, nearly tripling, and the percent of plans
offering brand-name prescription drug coverage dropped from 68% to 39% between 1999
and 2002.
The effect of the withdrawals
and reductions
in service on availability and
enrollment was large. The number of counties that had Medicare HMOs available
dropped from 808 to 540 between 1999 and 2002, while total enrollment in the program,
89
which had been rising steadily throughout the 1990s, dropped from 6.1 million to 4.8
million.
The withdrawals
came
as a surprise
to legislators
and policy
analysts.
Immediately after the act passed, before the withdrawals started, an analyst from the
Congressional Budget Office reported that the CBO estimated that, as a result of the
BBA, enrollment in Medicare HMOs in 2005 would be 15% higher than it would
otherwise have been and would reach 34% of total Medicare enrollment (Christensen
1998). Instead, enrollment in the HMO program dropped from 17% of total Medicare
enrollment in 1999 to 13% in 2002, and dropped to 11% by the end of 2004 (Kaiser
Foundation 2004).
Several studies have been done on the factors that contributed to the HMOs'
decisions to withdraw or reduce their service area. A report by the General Accounting
Office in 1999 found that HMOs were more likely to withdraw from a county if they had
offered a plan in that county for a shorter time, had lower enrollment, faced larger
competitors or had not established a provider network in the county (GAO 1999). Lake
and Brown (2002) did a multivariate analysis of the first three years of withdrawals after
the BBA and found plans were more likely to withdraw if they were national or for-profit
plans, had lower enrollment, were in rural counties, had larger competition, or had been
in the county longer, or the county had a lower overall Medicare HMO penetration rate.
Ellis and Gurol (2002) do a more formal model of entry and exit in the commercial and
Medicare HMO markets and find that HMOs are more likely to offer a Medicare plan in a
county if the county has a larger Medicare population or already has a greater number of
Medicare HMO plans.
90
There has been relatively little attempt at quantifying the effect of the losses on
beneficiaries, however. Laschober et al. (1999) did a qualitative study of what happened
to Medicare HMO beneficiaries who were involuntarily disenrolled from their HMO.
They found that only two thirds of the beneficiaries enrolled in another Medicare HMO,
either because they chose not to or were unable to because there were no other HMOs in
their county. One third of involuntarily disenrolled beneficiaries had lower benefits, 39%
had higher premiums and one in six lost prescription drug coverage as a result of the
disenrollment. They found that the disabled, the oldest old, and the near poor were most
adversely affected.
In this paper, I take a more quantitative approach to understanding the effect of
the withdrawals and service reductions on beneficiaries. Using the parameter estimates
from the structural model of demand for HMOs and their prescription drug benefits
presented in Hall (2005), I calculate the welfare losses associated with the withdrawals of
the HMOs, their service area reductions, and the increases in premiums and reductions in
benefits during the period 1999-2002. Hall (2005) estimated a utility function of
Medicare HMOs and their prescription drug benefits for Medicare beneficiaries using a
nested-logit model of demand, and found that raising premiums by $10 lowered HMO
market share by 5-8% and doubling prescription drug benefits raised HMO market share
by 17%. It also estimated the welfare effects of changing prescription drug benefits and
found that raising annual brand-name coverage by $100 increased welfare by $25. As
discussed below, estimating welfare using a logit or nested-logit model of demand is
relatively straightforward.
91
I also calculate the change in costs resulting from the withdrawals. While the
withdrawals decreased consumer welfare by removing choices, they also reduced
spending on the Medicare program by the government. Spending would have been
reduced by a lower enrollment in the Medicare HMO program because of the favorable
selection Medicare HMOs experienced relative to traditional Medicare. Previous to the
BBA, the base reimbursement rate for Medicare HMOs was 95% of the projected per
capita spending by the traditional Medicare program in the county the HMO is servicing.
Studies have shown, however, that HMO enrollees probably would cost somewhere
between 80 and 90% of the reimbursement that is paid on their behalf, if they were
enrolled in traditional Medicare. As a result, Medicare HMO beneficiaries usually cost
less to treat in traditional Medicare than in an HMO, so the reduction in enrollment in the
Medicare HMO program would have resulted in savings for the Medicare program as a
whole. This cost savings can be calculated by multiplying the reduction in enrollment in
each county by the county reimbursement rate. These estimates of welfare loss and cost
saving will offer some evidence as to how great the damage caused by the plan
withdrawals was.
II.
Background: The Medicare HMO Program and the Balanced Budget Act
of 1997
While the Medicare managed care program has existed in one form or another
since the beginning of Medicare in 1965, the risk-based program, where HMOs contract
with Medicare for a flat reimbursement and bear all the risk themselves, did not start until
1982, with the passage of the Tax Equity and Fiscal Responsibility Act (TEFRA). The
program grew during the 1980s to peak in enrollment in 1987 and then shrank between
92
1987 and 1991. After that, enrollment began climbing again as enrollment in managed
care grew in the commercial
sector. Between the end of 1994 and the end of 1998,
enrollment in Medicare HMOs tripled from 2 million to 6 million and 74 percent of
beneficiaries had access to at least one Medicare HMO by 1998 (Zarabozo 2000).
Christensen (1998) discusses the motivation for reforming the Medicare HMO
program and the parts of the BBA that relate to it. By 1997, the Medicare HMO program
was widely viewed as needing reform for several reasons. First, researchers were calling
attention to the favorable selection in HMOs and therefore to the question of whether
HMOs were being paid more by the Medicare program than the TEFRA intended they
should. While some favorable selection comes from healthy beneficiaries having a
greater tolerance for managed care, the HMOs were also perceived as unfairly targeting
healthy beneficiaries and excluding sicker beneficiaries through their marketing
techniques (Neuman 1998). The reimbursement rates were also seen as having too much
variation, both across counties and over time and the cross-sectional variation was
blamed for the inequality in access to the program by beneficiaries. The change in the
formula for the reimbursement rate was therefore designed to reduce this variation.
As mentioned above, before the BBA passed, the base reimbursement rate was
95% of the projected per capita spending by the traditional Medicare program in the
county. The BBA changed the formula so that the reimbursement was the largest of three
numbers. The first was a fifty-fifty blend of the local and national per capita spending
rate by traditional Medicare. The second was a minimum floor for the rate (set at $379.80
in 1999) and the third was a minimum 2% raise from the reimbursement
rate for the
county the year before. These changes raised the reimbursement rates for rural counties,
93
which had relatively low reimbursement and few HMOs before, and reduced the rates for
urban counties, which were the counties that had the most HMOs offering plans.
The BBA also required that the Center for Medicare and Medicaid Services begin
risk-adjusting their payments to HMOs based on health status starting in 2000, to prevent
HMOs from being paid more than the expected value of taking care of the beneficiary
and also removed the government's payments for graduate medical education from the
calculation of local fee-for-service spending. Both of these changes would have the effect
of reducing the HMOs' revenue.
The act made other changes to the program
besides the formula
for the
reimbursement rate. It increased the administrative burden on the plans by requiring them
to implement quality-improvement programs and to submit encounter data, so that the
risk adjustment could be made. It also moved up the deadline for HMOs to submit
contract proposals for the following calendar year from September to May, which the
HMOs said was too early for them to predict costs and market conditions.
As mentioned above, the act also expanded the type of plan allowed in the
program to include PPOs and private fee-for-service
plans and it also removed the
requirement that plans in the program have no more than 50% of their enrollment from
Medicare and Medicaid.
As previously discussed, all these changes caused many HMOs to withdraw from
the program, either entirely or partially. The withdrawals came in several waves over the
next few years. The GAO report in 1999 found that 407,000 enrollees were involuntarily
disenrolled from their Medicare HMO as a result of the withdrawals that year and, of
these, 61,000 were unable to enroll in another HMO because there were no HMOs left in
94
their county. According to the GAO, the primary reasons for leaving cited by the plans
were that the reimbursement
rates did not keep up with medical inflation and that the
administrative requirements were too burdensome.
There were two legislative attempts during this period to encourage the HMOs to
stay in the Medicare program. The BBA did not allow HMOs who had left a county to
reenter it for five years; the Balanced Budget Refinement Act (BBRA) of 1999 lowered
this to two years and added a new-entry bonus for underserved areas (Berenson 2001).
The Benefits Improvement and Protection Act (BIPA) of 2000 raised the minimum floor
rates, added a new, higher floor rate for urban counties and raised the minimum update
rate for one year to 3%.
Neither of these acts had any discernible effect on the exits of the HMOs from the
program. Calculations from CMS's HMO enrollment data show that in 2000, 432,000
HMO enrollees (or 7% of the Medicare HMO population) were involuntarily disenrolled
from their HMO. In 2001, 1.3 million enrollees (or 21%) were disenrolled and in 2002,
900,000 (or 17%) were. In 2000, 85,000 of the disenrolled beneficiaries had no other
HMO in their county and in both 2001 and 2002, 100,000 enrollees had no other HMO
available.
Even larger numbers of enrollees were affected by premium increases and benefit
reductions. In 2000, 2.4 million HMO enrollees had their premium rise and 2.6 million
had their prescription drug benefits drop. In 2001, these numbers were 2.8 million and 1.9
million respectively and in 2002, 3.0 million and 1.2 million.
The effects of the BBA on the Medicare HMO program were therefore felt widely
and affected a large number of beneficiaries.
95
III.
My approach to estimating welfare
The challenge of estimating the welfare effect of the BBA is making assumptions
about what would have happened in the Medicare HMO program if it had not passed. The
Medicare HMO program was not in a steady state before 1997. While enrollment had
been rising since the early 1990s, it would not necessarily have continued rising even if
the act had not passed, since the managed care industry was in flux in the late 1990s. The
report from the GAO on the Medicare HMO withdrawals (GAO 1999) notes that many
HMOs were in financial trouble in 1999 and that there were several withdrawals from the
federal employees benefits program at around the same time, so it is possible HMOs
would have withdrawn from the program anyway. On the demand side, demand for
Medicare HMOs would probably peak at some point and enrollment would level off but
it is not clear when this would have happened without the BBA.
We also do not know what would have happened to premiums and benefits
without the BBA. Medicare HMO plans were rising in generosity up until the BBA (Gold
et al. 2004). Again, however, their generosity would have probably leveled off at some
point but we do not know when. The plans' generosity might have continued rising since
their reimbursement was so closely tied to spending in the fee-for-service sector which
would have continued rising, but, on the other hand, drug prices were also starting to rise
faster during this period and this increase might have caused the plans to pull back on
their generosity.
Since it is so difficult to know what would have happened if the BBA had not
passed, I will estimate welfare and costs under two different scenarios, one conservative
96
and one less so. Under the conservative scenario, I will merely calculate the welfare loss
from the withdrawals each year. That is, for each year I will calculate the welfare gain if
the plans that withdrew at the end of the previous year had stayed in just for that year.
This approach probably underestimates the overall welfare loss since plans that stayed in
the program for 1999 would probably have continued staying in for 2000 and after, but it
minimizes the uncertainty in predicting counterfactual benefits, premiums and service
areas.
Under this scenario, plans that stayed in will have the same benefit and premiums
that they offered in reality and plans that left will have benefits and premiums imputed to
them. To understand the method by which they are imputed, it is necessary to know that
the HMOs can offer multiple benefit packages within their service area. An HMO can
offer a different benefit package in each county of its service area, the same benefit
package in the whole service area, or group the counties into benefit packages. They can
also offer more than one benefit package in a county but the enrollment data is only
provided at a county level. As in Hall (2005), I assume all the enrollment is in the
cheapest plan the HMO offers. This approach understates the welfare from the HMO
program slightly.
The imputation was done as follows. Plans that partially withdrew and only
offered one benefit package will have the same benefits and premiums that were offered
in the county that they stayed in, assigned to the county that they left. If the plan offered
more than one benefit package, the county they left is grouped with the same counties
that it was grouped with the previous year. If it is ambiguous which county it should be
grouped with because the group it was in was split up into multiple packages, it is
97
grouped with a county it is geographically close to. If there is no county it is close to or
there were no counties it was grouped with (because the plan withdrew all the other
members of its group), it is assigned the average benefits and premiums of all the
counties the plan stayed in. If a plan withdrew entirely, it is assigned the average benefits
and premiums of the state it is in.
An example of imputing when a plan partially withdraws is given by the HMO
with contract number H 1406, which offered a Medicare HMO plan in the Chicago area in
2000 and 2001. Table 1 shows which benefit packages were offered in which counties by
the plan and Figure
shows a county-level map of the Chicago area. In 2000, the HMO
offered three different benefit packages in eight counties: one package in Cook County,
one in Kankakee County and one in the remaining six counties. In 2001, it also offered
three different packages, but the grouping of the counties changed and it withdrew from
three counties, including Kankakee County. Since Kankakee County was not grouped
with any counties in 2000, the HMO's plan in this county is assigned the average
premiums and benefits of the five counties it stayed in. Since Lake County, IL and Will
County were grouped with Du Page, Kane and Kendall counties in 2000, they are
assigned the same benefit package as the HMO's plan in those counties in 2001.
Another example is given by the HMO with contract number H3251, which
offered a Medicare HMO plan in New Mexico in 2000 and 2001. In 2000, the HMO
offered one benefit package in nine counties. In 2001, the HMO withdrew from four
counties, and split the other five counties into two benefit packages. Table 2 shows which
counties were assigned which benefit packages and Figure 2 shows a county map of New
Mexico. Since splitting the counties made it ambiguous which counties the counties with
98
imputed benefits should be grouped with, the counties were grouped geographically. Rio
Arriba and Socorro counties were assigned benefit package #2, since they are closer to
Sandoval and Valencia counties while San Miguel County was assigned benefit package
#18 since it is closer to Santa Fe and Torrance counties. In the case of ties, MSA
boundaries were used to break them; Los Alamos County was therefore assigned benefit
package #18, since it is in the Santa Fe MSA.
This method of imputing benefits and premiums is not perfect. HMOs' premium
and benefit decisions are joint with their service area decisions, so, if they had stayed in
the counties they withdrew from, they probably would have offered different premiums
and benefits. In order to make the welfare estimate however, benefits and premiums had
to be imputed to the counties that plans withdrew from, and this is a conservative method
for doing so.
In the more generous scenario, however, I will assume that all plans that withdrew
stayed in until 2002 and that their benefits and premiums remained constant at their 1999
levels (or the level of their year of entrance, if they entered after 1999). This is not the
most generous scenario that could be imagined; the most generous would probably
involve enrollment rising and benefits becoming more generous over time but it is a
minimally generous scenario.
In both scenarios, I will assume that plans that entered in reality after 1999 still
entered. While more plans exited than entered during the period 1999-2002, it is not the
case that there was no entrance at all.
I also calculate costs for both scenarios by multiplying the increased enrollment in
each county by the reimbursement rate in that county. The reimbursement rates used are
99
the actual reimbursement
rates set by the formula in the BBA. While it would be
preferable to use the counterfactual reimbursement rates, they are not available. Since
actual reimbursement rates are usually lower than the counterfactual reimbursement rates
would have been in counties with HMOs, this approach will understate the increased
costs that would have been incurred if the plans had not withdrawn.
IV.
Estimating welfare in nested-logit models
Small and Rosen (1981) discuss estimating welfare in discrete-choice models. As
they show, the change in the expenditure function from a quality change can be found by
integrating over the share function with respect to the utility function. In logit and nestedlogit models, this integral has a closed-form expression.
Share in the nested logit model are given by:
exp(Uj
/I -a)
Z exp(Uk/-
Iexp(Uk
/- a)j[
kEGC
g
()
- r)
kE g
Uj represents the mean utility, i.e., the portion of utility common across
consumers (and omitting the individual error term). The integral of this share formula
with respect to the utility function evaluates to:
JsjdUj = In
0
exp( Uk)
~g ~kEg
(2)
1
Logit and nested-logit models have the property that the matrix of the derivatives
of the shares with respect to the utilities is symmetric. That is,
si
auj
- sj for all
aui
plans i
and j. This property is useful because it allows the welfare effect of several simultaneous
100
quality changes to be evaluated with this one integral. When there are multiple quality
changes in multiple products, the difference in welfare can be measured by evaluating
each utility function with and without all of the quality changes. Since the integral is in
utils, to find the welfare effect in dollars, the integral is divided by the marginal utility of
income.
As mentioned above, Equation (2) gives the change in the expenditure function
from a quality change, also known as the compensating variation. More specifically, it
gives the compensating variation from a quality change for a representative person in the
market. To find the total welfare change in a market, it must be multiplied by the
number of consumers in the market.
V.
Applying welfare estimation to the Medicare HMO market
For the purposes of calculating welfare, I will be using the same mean utility
function for Medicare HMOs as in Hall (2005):
Umt
-tP
m- XjmtJ
jmt
t
(3)
+
where j represents the plan, m the county and t the year. pjmt is the plan premium, Xjmtis a
vector of prescription drug benefit characteristics, and
quality.
(jmt
represents unobserved plan
is a year-specific effect, to account for the change in demand for Medicare
HMO benefits over time.
The utility parameter estimates were made in Hall (2005). I use the estimates from
the IV nested log specification,
with the prescription drug benefits measured as the
amount of expenditure by an average prescription drug user that would be covered by the
101
plan. (Estimates using the actual features of the plan, such as the amount of brand-name
drug coverage, were qualitatively similar.)
To calculate the effect of the withdrawals, utilities were calculated for each plan
using the parameter estimates from Hall 2005 and inputted into the integral in equation
(2). For the endpoint without the withdrawals, the premiums and benefits given under the
two counterfactual scenarios discussed above were used and for the endpoint with the
withdrawals, the premiums and benefits that were offered in reality.
In Hall (2005),
was estimated with the residual from the demand regression. It
therefore had to be imputed to observations (plan-county-year combinations) that were
not in the sample. Since the demand regression included plan-county fixed effects, a plan
had to be in the county for at least two years in order for the observations to be in the
sample. If an observation was not in the sample because the plan was in the county for
only one year,
could be predicted easily using the actual share and plan characteristics.
For all other observations,
, was assumed to be zero, since, as the demand regression is
estimated with a constant, that is its expected value.
Since the mean utility of traditional Medicare was normalized to zero in Hall
2005, the endpoints each give the amount of welfare provided by the Medicare HMO
program above the welfare from traditional Medicare. This amount is always positive
since, in logit models, welfare is always increasing in the number of choices available.
Since the welfare measures give the welfare added by the Medicare HMO
program, in order to correctly compare the costs, the total costs must be adjusted to find
the cost added by the Medicare HMOs to the costs incurred by traditional Medicare. It is
difficult to know exactly which enrollees in traditional Medicare would have enrolled in
102
HMOs without the withdrawals so it is therefore difficult to estimate exactly the
difference in costs. Estimates of the expected cost of HMO enrollees if they had enrolled
in traditional Medicare in the literature range from 88% of their cost in the HMO
program (Riley et al. 1996) to 100% (Rogers and Smith 1995, Dowd et al. 1996). The
higher the cost of treating the enrollee in traditional Medicare, the more net welfare is
added by the Medicare HMO program. I present results calculated under several different
assumptions about the cost differential between traditional Medicare and the Medicare
HMO program.
The counterfactual enrollments were also calculated, to give an estimate of how
many people were affected by the change. They were calculated using the share formula
in equation ()
and the premiums and benefits from each counterfactual scenario, and
then multiplying these predicted shares by the number of Medicare eligibles in each
county.
VI.
Results of welfare and cost calculations
The results of the welfare and cost calculations are reported in Tables 3 and 4.
Table 3 reports the results for the first, more conservative scenario. As the middle
column shows, the Medicare HMO program generates net positive welfare in all four
years even with the most conservative assumption about how much HMO enrollees
would have cost in the traditional Medicare program. Over the period 1999-2002, the
Medicare HMO program generated gross welfare of $64.8 billion and incurred gross
expenditure of $156.2 billion. If we assume that HMO enrollees' costs would have been
80% of the total expenditure
of the HMO program if they had been enrolled in
103
traditional Medicare, then the HMO program only added $31.2 billion to overall
Medicare expenditure and thus generated net welfare of $33.5 billion. If, as is more
likely, their costs would have been 90% of the costs in the HMO program, the HMO
program only added $15.6 billion to overall Medicare expenditure and thus generated
net welfare of $49.1 billion.
The first column of Table 3 shows how much welfare and expenditure the HMO
program would generate under the conservative scenario, where plans are assumed to
only stay in the program for one more year and did not have more generous benefits.
Under this conservative assumption, it can be seen that the withdrawals caused a
significant reduction in both enrollment and welfare from the Medicare HMO program.
Total enrollment over the four years from 1999-2002 was 2.8 million less because of the
plan withdrawals, equivalent to an 11.1% reduction in enrollment. For welfare, under the
most conservative assumption that HMO enrollees would have cost 80% of what they
cost in the HMO program if they had been enrolled in traditional Medicare, the
withdrawals caused a $4.3 billion loss in welfare in the four years from 1999-2002,
equivalent to lowering net welfare by 11.5%. Under the more plausible 90% assumption,
the withdrawals caused a $6.2 billion loss in welfare, equivalent to lowering net welfare
by 11.2%.
The withdrawals also seemed to have lowered the HMO program's costeffectiveness slightly. The last four rows in each panel of Table 3 give the average cost of
$1 of welfare in the program with and without the withdrawals and of the plans that
withdrew. This number was calculated by simply dividing the estimated cost added by
the HMO program by the gross welfare generated by the program. As they show, the
104
plans that withdrew in 1999, 2000, and 2001 were providing more welfare at a lower cost
than the plans that remained, and the cost-effectiveness of the program was slightly
lowered by the withdrawals. This result offers evidence against the hypothesis suggested
by the GAO that HMOs were withdrawing
in 1999 because some of them had over-
entered and could not compete effectively, not because of the BBA. In 2002 however, the
plans that withdrew were less cost-effective, suggesting that the kinds of plans who were
leaving the program were changing over time.
Table 4 reports the results for the less generous scenario. In this scenario, since I
did not have detailed benefit data for 1998, I had to start the simulation at the 1999 levels
of benefits and entry. In this respect, the scenario is less generous than the previous one,
which assumed the plans that left in 1998 stayed in for one more year. The welfare
without the withdrawals and the enrollment are still considerably larger, as the last panel
with the totals shows. The withdrawals lowered enrollment by 5.3 million beneficiaries
from 28.0 million, equivalent to a reduction of 19.0%. Total gross welfare without the
withdrawals is estimated to be $81.4 million over the three years. Under the conservative
assumption that HMO enrollees would have cost 80% as much in traditional Medicare,
the HMO program added $37.2 billion to expenditure, implying a net welfare amount of
$44.2 billion. Under the more plausible assumption that they would have cost 90%, the
HMO program added only $18.6 billion to expenditure, generating a net welfare amount
of $62.3 billion. Under the 80% assumption, the withdrawals caused a loss of $12.3
billion in welfare (or 27.8%) and under the 90% assumption, they caused a loss of $16.6
billion in welfare (or 23.0%).
105
Under the scenario presented in Table 4, the loss of cost-effectiveness was even
greater than in Table 3. Under the 80% assumption, without the withdrawals, the average
cost of $1 of welfare would be $0.46, while, with the withdrawals, it was $0.48. The
plans that left had an implied cost of only $0.36 per $1 of welfare. Under the 90%
assumption, the plans that left had an implied cost of $0.18, raising the cost of $1 of
welfare from $0.23 to $0.24.
In summary therefore, the estimates of the gross welfare loss from the plan
withdrawals ranged from $8.1 billion to $16.6 billion and the gross expenditure decrease
from $18.7 billion to $29.6 billion. The estimates of the net welfare loss range from $4.3
billion to $16.6 billion, depending on the scenario and what we assume about how much
enrollees who would have enrolled in HMOs if the plans had not withdrawn, ended up
costing in traditional Medicare. The implied percentage decrease in welfare from the
withdrawals ranges from 11.5% in the first scenario to 21.5% in the second scenario, both
under the 90% assumption.
VII.
Conclusion
The intent of the TEFRA of 1982 in creating the risk-based Medicare HMO
program was that the federal government would take advantage of the presumed greater
efficiency of HMOs to create savings for the Medicare program. As many have noticed,
and as this paper shows, the program has not really worked out that way since Medicare
HMOs have increased overall spending by Medicare. The plan withdrawals in the
Medicare+Choice program were highly publicized, affected many people, and made a
deep impression on all parties concerned. As a result, in 2003, when the program was
106
renamed the Medicare Advantage program by the Medicare Modernization Act (MMA),
the reimbursement rates were raised to 100% of the expected per capita cost of traditional
Medicare in the county, to encourage plans to come back into the program.
This change obviously resulted in an increase in expenditure for the program; the
Medicare Payment Advisory Commission estimated that Medicare paid 7% more for
HMO enrollees in 2004 than it would have if they had been in traditional Medicare. The
welfare estimates presented here, however, show that the Medicare HMO program is not
a waste since it does generate a positive return on spending, even under the most
conservative assumptions. The estimates suggest that $1 spent on the Medicare HMO
program brings just over $2 in welfare for beneficiaries in the form of lower cost-sharing
and supplemental benefits.
The welfare results also show that total net welfare from the program would have
been higher by an amount that is estimated to be from $4.3 billion to $16.6 billion if
plans had stayed in after the passage of the BBA in 1997. They also show that cost-
effectiveness of the Medicare HMO program was slightly reduced by the withdrawals.
This leads to an optimistic conclusion for the Medicare Advantage program: that, as plans
reenter the program, cost-effectiveness will rise again.
107
References
Berenson, R. A. (2001). "Medicare+Choice: Doubling Or Disappearing?" Health
Affairs(Web Exclusive): W65-W82.
Christensen, S. (1998). "Medicare+Choice Provisions in the Balanced Budget Act of
1997." Health Affairs 17(4): 224-231.
Dowd, B., R. Feldman, et al. (1996). Competitive Pricing for Medicare. Washington, DC,
AEI Press.
Ellis, R. P. and I. Gurol (2002). Health Plan Entry and Exit in the Medicare Managed
Care Market. Boston University: 28.
General Accounting Office (1999). Medicare Managed Care Plans: Many Factors
Contribute to Recent Withdrawals; Plan Interest Continues.
Gold, M., L. Achman, et al. (2004). Monitoring Medicare+Choice: What Have We
Learned? Finding and Operational Lessons for Medicare Advantage,
Mathematica: 51.
Hall, A. E. (2005). Estimating the Demand for Prescription Drug Benefits by Medicare
Beneficiaries. Working paper, MIT.
Kaiser Family Foundation (2004). Medicare Advantage: Fact Sheet. Menlo Park, CA.
Lake, T. and R. Brown (2002). Medicare+Choice Withdrawals: Understanding Key
Factors, The Henry J. Kaiser Family Foundation: 41.
Laschober, M. A., P. Neuman, et al. (1999). "Medicare HMO Withdrawals: What
Happens To Beneficiaries?" Health Affairs 18(6): 150-157.
Neuman, P., E. Maibach, et al. (1998). "Marketing HMOs To Medicare Beneficiaries."
Health Affairs 17(4): 132-139.
Riley, G., C. Tudor, et al. (1996). "Health Status of Medicare Enrollees in HMOs and
Fee-For-Service in 1994." Health Care Financing Review 17: 65-76.
Rogers, J. and K. E. Smith (1995). Do Medicare HMOs Reduce Fee-for-Service Costs?
Washington, DC, Price Waterhouse.
Small, K. A. and H. S. Rosen (1981). "Applied Welfare Economics with Discrete Choice
Models." Econometrica 49(1): 105-130.
Zarabozo, C. (2000). "Milestones in Medicare Managed Care." Health Care Financing
Review 22(1): 61-67.
108
Table 1: Benefit packages and service areas for contract number
H1406 in 2000-2001
County
Benefit package number in Benefit package number in
Cook County, IL
Du Page County, IL
Kane County, IL
2000
8
6
6
2001
13
15
15
Kankakee County, IL
13
Withdrew
Kendall County, IL
Lake County, IL
6
6
15
Withdrew
Will County, IL
6
Withdrew
Lake County, IN
6
17
Table 2: Benefit packages and service areas for contract number
H3251 in 2000-2001
County
Benefit package number in Benefit package number in
Bernalillo County
2000
2
2001
2
Los Alamos County
Rio Arriba County
2
2
Withdrew
Withdrew
Sandoval County
2
2
San Miguel County
2
Withdrew
Santa Fe County
2
18
Socorro County
2
Withdrew
Torrance County
Valencia County
2
2
18
2
109
Table 3
Welfare effect of plan withdrawals from the Medicare HMO program
1999-2002
Scenario : Plans stay in program for one year longer than in actuality
In $ millions
Without
withdrawals
With
withdrawals
(estimated)
(actual)
Difference
7,012,938
$20,536
$45,237
6,133,876
$17,781
$39,757
879,062
$2,755
$5,480
$9,047
$7,951
$1,096
$4,524
$3,976
$548
$2,262
$1,988
$274
1999
Total annual HMO enrollment
Tot. ann. welfare from HMO program
Tot. exp. on the HMO program
Costs added by HMO if FFS enrollee
of HMO enrollee cost
Costs added by HMO if FFS enrollee
of HMO enrollee cost
Costs added by HMO if FFS enrollee
of HMO enrollee cost
Costs added by HMO if FFS enrollee
100% of HMO enrollee
costs 80%
costs 90%
costs 95%
costs
cost
Net welfare gain (80%)
Net welfare gain (90%)
Net welfare gain (95%)
Net welfare gain (100%)
Average cost of $1 of welfare
Average cost of $1 of welfare
Average cost of $1 of welfare
Average cost of $1 of welfare
(80%)
(90%)
(95%)
(100%)
$0
$0
$0
$11,489
$16,013
$18,275
$20,536
$0.441
$0.220
$0.110
$0.000
$9,830
$13,805
$15,793
$17,781
$0.447
$0.224
$0.112
$0.000
$1,659
$2,207
$2,481
$2,755
$0.398
$0.199
$0.099
$0.000
6,573,776
$19,118
$44,157
6,166,351
$17,957
$41,603
407,425
$1,161
$2,554
$8,831
$8,321
$511
$4,416
$4,160
$255
$2,208
$2,080
$128
2000
Total annual HMO enrollment
Tot. ann. welfare from HMO program
Tot. exp. on the HMO program
Costs added by HMO if FFS enrollee costs 80%
of HMO enrollee cost
Costs added by
of HMO enrollee
Costs added by
of HMO enrollee
Costs added by
HMO if FFS enrollee costs 90%
cost
HMO if FFS enrollee costs 95%
cost
HMO if FFS enrollee costs
100% of HMO enrollee cost
Net welfare gain (80%)
Net welfare gain (90%)
Net welfare gain (95%)
Net welfare gain (100%)
Average cost of $1 of welfare
Average cost of $1 of welfare
Average cost of $1 of welfare
Average cost of $1 of welfare
(80%)
(90%)
(95%)
(100%)
110
$0
$0
$0
$10,286
$14,702
$16,910
$19,118
$0.462
$0.231
$0.115
$0.000
$9,637
$13,797
$15,877
$17,957
$0.463
$0.232
$0.116
$0.000
$650
$905
$1,033
$1,161
$0.440
$0.220
$0.110
$0.000
Table 3 (con.)
Welfare effect of plan withdrawals from the Medicare HMO program
1999-2002
Scenario : Plans stay in program for one year longer than in actuality
In $ millions
2001
Total annual HMO enrollment
Tot. ann. welfare from HMO program
Tot. exp. on the HMO program
Costs added by HMO if FFS enrollee
of HMO enrollee cost
Costs added by HMO if FFS enrollee
of HMO enrollee cost
Costs added by HMO if FFS enrollee
of HMO enrollee cost
Costs added by HMO if FFS enrollee
5,496,639
$15,683
$39,163
1,022,546
$2,828
$6,971
$9,227
$7,833
$1,394
$4,613
$3,916
$697
$2,307
$1,958
$349
costs 80%
costs 90%
costs 95%
costs
100% of HMO enrollee cost
Net welfare gain (80%)
Net welfare gain (90%)
Net welfare gain (95%)
Net welfare gain (100%)
Average cost of $1 of welfare
Average cost of $1 of welfare
Average cost of $1 of welfare
Average cost of $1 of welfare
6,519,185
$18,511
$46,134
(80%)
(90%)
(95%)
(100%)
$0
$0
$0
$9,284
$13,898
$16,204
$18,511
$0.498
$0.249
$0.125
$0.000
$7,851
$11,767
$13,725
$15,683
$0.499
$0.250
$0.125
$0.000
$1,434
$2,131
$2,479
$2,828
$0.493
$0.247
$0.123
$0.000
5,371,742
$14,673
$39,405
4,852,681
$13,337
$35,715
519,060
$1,336
$3,691
$7,881
$7,143
$738
$3,941
$3,571
$369
$1,970
$1,786
$185
2002
Total annual HMO enrollment
Tot. ann. welfare from HMO program
Tot. exp. on the HMO program
Costs added by HMO if FFS enrollee
of HMO enrollee cost
Costs added by HMO if FFS enrollee
of HMO enrollee cost
Costs added by HMO if FFS enrollee
of HMO enrollee cost
Costs added by HMO if FFS enrollee
costs 80%
costs 90%
costs 95%
costs
100% of HMO enrollee cost
Net welfare gain (80%)
Net welfare gain (90%)
Net welfare gain (95%)
Net welfare gain (100%)
Average cost of $1 of welfare
Average cost of $1 of welfare
Average cost of $1 of welfare
Average cost of $1 of welfare
(80%)
(90%)
(95%)
(100%)
111
$0
$0
$0
$6,792
$10,733
$12,703
$14,673
$0.537
$0.269
$0.134
$0.000
$6,194
$9,766
$11,552
$13,337
$0.536
$0.268
$0.134
$0.000
$598
$967
$1,151
$1,336
$0.553
$0.276
$0.138
$0.000
Table 3 (con.)
Welfare effect of plan withdrawals from the Medicare HMO program
1999-2002
Scenario : Plans stay in program for one year longer than in actuality
In $ millions
Total
Total annual HMO enrollment
Tot. ann. welfare from HMO program
Tot. exp. on the HMO program
Costs added by HMO if FFS enrollee costs 80%
of HMO enrollee cost
Costs added by HMO if FFS enrollee costs 90%
of HMO enrollee cost
Costs added by HMO if FFS enrollee costs 95%
of HMO enrollee cost
25,477,641
$72,838
$174,933
22,649,549
$64,759
$156,238
2,828,093
$8,079
$18,695
$34,987
$31,248
$3,739
$17,493
$15,624
$1,869
$8,747
$7,812
$935
Costs added by HMOif FFSenrollee costs
100% of HMO enrollee
cost
$0
$0
$0
Net welfare gain (80%)
Net welfare gain (90%)
Net welfare gain (95%)
Net welfare gain (100%)
Average cost of $1 of welfare (80%)
Average cost of $1 of welfare (90%)
Average cost of $1 of welfare (95%)
$37,852
$55,345
$64,092
$72,838
$0.480
$0.240
$0.120
$33,511
$49,135
$56,947
$64,759
$0.483
$0.241
$0.121
$4,340
$6,210
$7,145
$8,079
$0.463
$0.231
$0.116
Average cost of $1 of welfare (100%)
$0.000
$0.000
$0.000
112
Table 4
Welfare effect of plan withdrawals from the Medicare HMO program
1999-2002
Scenario I: Plans stay in program through 2002
In $ millions
Without
withdrawals
With
withdrawals
(estimated)
(actual)
Difference
6,133,876
$17,781
$39,757
6,133,876
$17,781
$39,757
0
$0
$0
$7,951
$7,951
$0
$3,976
$3,976
$0
$1,988
$1,988
$0
1999
Total annual HMO enrollment
Tot. ann. welfare from HMO program
Tot. exp. on the HMO program
Costs added by HMO if FFS enrollee costs 80%
of HMO enrollee
cost
Costs added by
of HMO enrollee
Costs added by
of HMO enrollee
Costs added by
HMO if FFS enrollee costs 90%
cost
HMO if FFS enrollee costs 95%
cost
HMO if FFS enrollee costs 100%
of HMO enrollee
cost
$0
$0
$0
Net welfare gain (80%)
Net welfare gain (90%)
Net welfare gain (95%)
$9,830
$13,805
$15,793
$9,830
$13,805
$15,793
$0
$0
$0
Net welfare gain (100%)
$17,781
$17,781
$0
0.4472
0.2236
0.1118
0
0.4472
0.2236
0.1118
0
0
0
0
0
6,796,390
$20,062
$44,820
6,166,351
$17,957
$41,603
630,039
$2,105
$3,218
$8,964
$8,321
$644
$4,482
$4,160
$322
$2,241
$2,080
$161
Average
Average
Average
Average
cost
cost
cost
cost
of
of
of
of
$1 of
$1 of
$1 of
$1 of
welfare
welfare
welfare
welfare
(80%)
(90%)
(95%)
(100%)
2000
Total annual HMO enrollment
Tot. ann. welfare from HMO program
Tot. exp. on the HMO program
Costs added by HMO if FFS enrollee
of HMO enrollee cost
Costs added by HMO if FFS enrollee
of HMO enrollee cost
Costs added by HMO if FFS enrollee
of HMO enrollee cost
Costs added by HMO if FFS enrollee
of HMO enrollee
costs 80%
costs 90%
costs 95%
costs 100%
cost
Net welfare gain (80%)
Net welfare gain (90%)
Net welfare gain (95%)
Net welfare gain (100%)
Average cost of $1 of welfare
Average cost of $1 of welfare
Average cost of $1 of welfare
Average cost of $1 of welfare
(80%)
(90%)
(95%)
(100%)
113
$0
$0
$0
$11,098
$15,580
$17,821
$20,062
0.4468
0.2234
0.1117
0
$9,637
$13,797
$15,877
$17,957
0.4634
0.2317
0.1158
0
$1,461
$1,783
$1,944
$2,105
0.3058
0.1529
0.0764
0
Table 4 (con.)
Welfare effect of plan withdrawals from the Medicare HMO program
1999-2002
Scenario I: Plans stay in program through 2002
In $ millions
2001
Total annual HMO enrollment
Tot. ann. welfare from HMO program
Tot. exp. on the HMO program
Costs added by HMO if FFS enrollee costs
of HMO enrollee cost
Costs added by HMO if FFS enrollee costs
of HMO enrollee cost
Costs added by HMO if FFS enrollee costs
of HMO enrollee cost
Costs added by HMO if FFS enrollee costs
of HMO enrollee cost
Net welfare gain (80%)
Net welfare gain (90%)
Net welfare gain (95%)
Net welfare gain (100%)
Average cost of $1 of welfare (80%)
Average cost of $1 of welfare (90%)
Average cost of $1 of welfare (95%)
Average cost of $1 of welfare (100%)
7,454,451
$21,739
$50,352
5,496,639
$15,683
$39,163
1,957,811
$6,056
$11,189
$10,070
$8,321
$644
$5,035
$4,160
$322
$2,518
$2,080
$161
$0
$11,669
$16,704
$19,222
$21,739
0.4632
0.2316
0.1158
0
$0
$7,363
$11,523
$13,603
$15,683
0.5305
0.2653
0.1326
0
$0
$5,413
$5,734
$5,895
$6,056
0.1063
0.0531
0.0266
0
7,580,396
$21,774
$50,921
4,852,681
$13,337
$35,715
2,727,714
$8,437
$15,207
$10,184
$7,143
$3,041
$5,092
$3,571
$1,521
$2,546
$1,786
$760
$0
$11,590
$16,682
$19,228
$21,774
0.4677
0.2339
0.1169
0
$0
$6,194
$9,766
$11,552
$13,337
0.5356
0.2678
0.1339
0
$0
$5,396
$6,916
$7,677
$8,437
0.3605
0.1802
0.0901
0
80%
90%
95%
100%
2002
Total annual HMO enrollment
Tot. ann. welfare from HMO program
Tot. exp. on the HMO program
Costs added by HMO if FFSenrollee costs 80%
of HMO enrollee cost
Costs added by HMO if FFS enrollee costs 90%
of HMO enrollee cost
Costs added by HMO if FFS enrollee costs 95%
of HMO enrollee cost
Costs added by HMO if FFS enrollee costs 100%
of HMO enrollee cost
Net welfare gain (80%)
Net welfare gain (90%)
Net welfare gain (95%)
Net welfare gain (100%)
Average cost of $1 of welfare (80%)
Average cost of $1 of welfare (90%)
Average cost of $1 of welfare (95%)
Average cost of $1 of welfare (100%)
114
Table 4 (con.)
Welfare effect of plan withdrawals from the Medicare HMO program
1999-2002
Scenario I: Plans stay in program through 2002
In $ millions
Total
Total annual HMO enrollment
Tot. ann. welfare from HMO program
Tot. exp. on the HMO program
Costs added by HMO if FFS enrollee
of HMO enrollee cost
Costs added by HMO if FFS enrollee
of HMO enrollee cost
Costs added by HMO if FFS enrollee
of HMO enrollee cost
Costs added by HMO if FFS enrollee
22,649,549
$64,759
$156,238
5,315,564
$16,598
$29,613
$37,170
$31,248
$5,923
$18,585
$15,624
$2,961
$9,293
$7,812
$1,481
costs 80%
costs 90%
costs 95%
costs 100%
of HMO enrollee cost
Net welfare gain (80%)
Net welfare gain (90%)
Net welfare gain (95%)
Net welfare gain (100%)
Average cost of $1 of welfare
Average cost of $1 of welfare
Average cost of $1 of welfare
Average cost of $1 of welfare
27,965,113
$81,357
$185,851
(80%)
(90%)
(95%)
(100%)
115
$0
$0
$0
$44,186
$62,771
$72,064
$81,357
0.4569
0.2284
0.1142
0
$33,023
$48,891
$56,825
$64,759
0.4825
0.2413
0.1206
0
$12,269
$14,434
$15,516
$16,598
0.3568
0.1784
0.0892
0
116
Figure
1
Map of area around Chicago showing counties
lmm
--Rockford
I
·
~BOONE
wINNEBAGo
I
.
\
.
McHENRY LAKE
I
hli'~
,>.
orth Chic
cago
.
7
I
LAKE
!-
CHICAGO-.
GARYKENOSHA
(PART)
Source: U.S. Department of Commerce, Economics and Statistics Administration, Bureau
of the Census
117
Figure 2
Map of northern New Mexico showing counties
Source: U.S. Department of Commerce, Economics and Statistics Administration, Bureau
of the Census
118