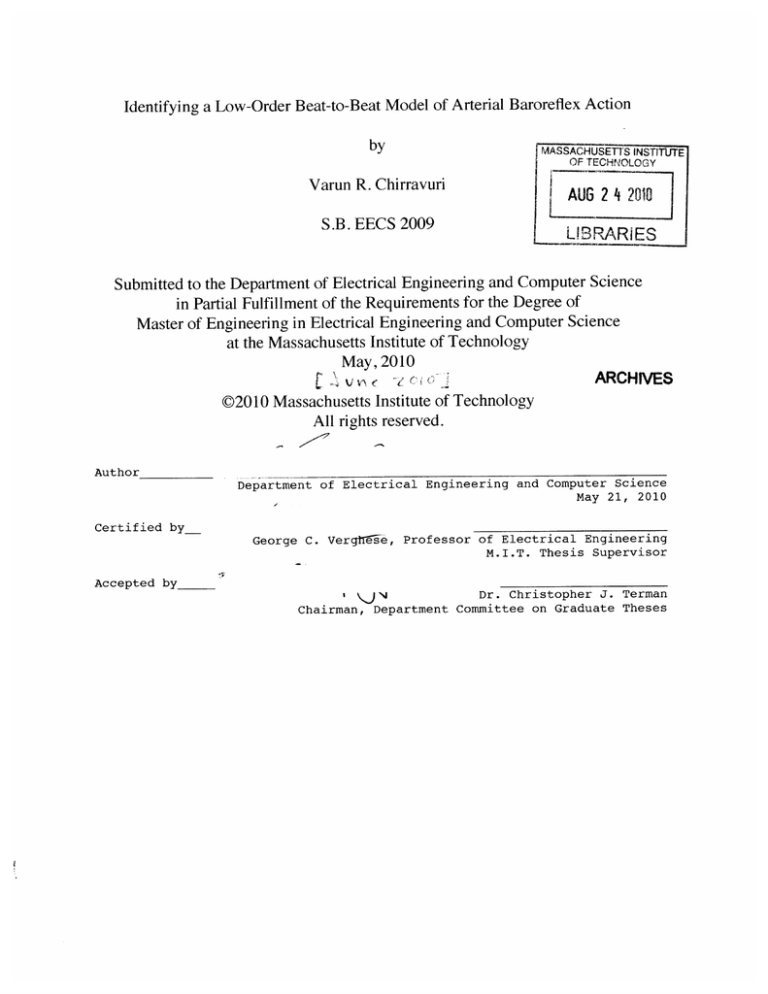
Identifying a Low-Order Beat-to-Beat Model of Arterial Baroreflex Action
by
Varun R. Chirravuri
S.B. EECS 2009
MASSACHUSETTS INSTITUTE
OF TECHNOLOGY
AUG 2 4 2010
L12RARiES
Submitted to the Department of Electrical Engineering and Computer Science
in Partial Fulfillment of the Requirements for the Degree of
Master of Engineering in Electrical Engineering and Computer Science
at the Massachusetts Institute of Technology
May, 2010
(
v\m- t
ARCHIVES
C2010 Massachusetts Institute of Technology
All rights reserved.
Author
Department of Electrical Engineering and Computer Science
May 21, 2010
Certified by
George C. Vergthse, Professor of Electrical Engineering
M.I.T. Thesis Supervisor
Accepted by_
Dr. Christopher J. Terman
\y
Chairman, Department Committee on Graduate Theses
Identifying a Low-Order Beat-to-Beat Model of Arterial Baroreflex Action
by
Varun Chirravuri
Submitted to the
Department of Electrical Engineering and Computer Science
May 21, 2010
In Partial Fulfillment of the Requirements for the Degree of
Master of Engineering in Electrical Engineering and Computer Science
ABSTRACT
The arterial baroreflex is a fast-acting control mechanism that the body relies
on to regulate blood pressure. Previous efforts to quantitatively model the
baroreflex have relied primarily on non-parametric characterization of the
transfer function from blood pressure to heart rate (Berger et al.,1989, Akselrod
et al., 1981,1985). Of the parametric models proposed, most focus on matching
empirical transfer functions with continuous-time models (Berger et al., 1991).
Use of these models is often restricted to simulation, and consequently not
focused on prediction. We develop a beat-to-beat, one-pole model for the
baroreflex that can parsimoniously capture both the empirical frequencydomain and time-domain characteristics of the baroreflex. Further, we develop
a robust identification method for on-line estimation of our model parameters
from clinical data. We conclude by presenting preliminary results of our model
and estimation method applied to patients undergoing drug-induced autonomic
blockade.
Thesis Supervisor: George Verghese
Title: Professor of Electrical Engineering
MIT Department of Electrical Engineering and Computer Science
Acknowledgements
I would like to acknowledge a few individuals who have been instrumental
in the success of this thesis. These individuals have made this M.Eng project
a formative, and eye-opening experience for me.
First, I must acknowledge (soon to be Dr.) Faisal Kashif for showing me
the ropes, so to speak. His willingness to meet and discuss the direction of
this research helped me overcome countless obstacles, and become a better
researcher and engineer. Thanks are also due to Dr. Thomas Heldt for continuously refocusing the project on its ultimate purpose, clinical monitoring,
no matter how hard I tried to ignore that fact. I am also deeply indebted to
Professor George Verghese, for his help in designing the core model for this
research, and providing timely and insightful guidance at every step of the
way-both in research and in life. And finally, I thank Jerry Wang for his
continued interest in my work, and for being willing to listen and lend his
brain power whenever I needed it.
I cannot conclude these acknowledgements without thanking my family.
Credit is due to my parents for encouraging me to pursue this degree, listening to my complaints along the way, and giving me hot meals and a bed to
sleep in when the need arose.
Support for this work has come from the National Institute of Biomedical
Imaging and Bioengineering of the National Institutes of Health, under grant
R01EB001659-6.
4
Contents
7
1 Introduction
1.1 Goals of this Research . . . . . . . . . . . . . . . . . . . . . .7
1.2 Prospective Look at this Thesis . . . . . . . . . . . . . . . . .9
13
..
...
1.3 Contributions of this Thesis..............
2 The Arterial Baroreflex
2.1 O verview . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
. . . . . . . . . . .
2.2 Cardiovascular Control Physiology
2.2.1 Anatomy and Function of the Cardiovascular System
2.2.2 Autonomic Nervous System Control of the Heart . .
. . . . . . . . ..
2.2.3 The Human Baroreflex . . . . .
2.2.4 Pharmacological Intervention and the Baroreflex . . .
2.3 Prior W ork . . . . . . . . . . . . . . . . . . . . .
2.3.1 Spectral Analysis of Heart Rate Variability
2.3.2 Modeling of Heart Rate Transfer Function
3
Modeling the Baroreflex
3.1 Modeling Considerations . . . . . . . . . . . . . . . . . .
3.2 Time Series Models . . . . . . . . . . . . . . . . . . . . .
3.2.1 Moving Average (MA) Models . . . . . . . . . . .
3.2.2 Autoregressive (AR) Models . . . . . . . . . . . .
3.2.3 ARX/ARMA Models . . . . . . . . . . . . . . . .
3.3 Derivation of Baroreflex Model . . . . . . . . . . . . . .
. . . . .
3.4 Time-Domain Behavior of our Baroreflex Model
. . . . .
.
.
.
3.4.1 Parasympathetic Impulse Response
3.4.2 Sympathetic Impulse Response . . . . . . . . . .
3.4.3 Total Model Impulse Response . . . . . . . . . .
3.5 Frequency Domain Behavior of the ARX Baroreflex Model
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
15
15
16
17
20
21
25
.
.
.
.
.
.
.
.
.
.
35
35
36
37
37
38
38
42
43
43
46
CONTENTS
3.5.1
3.5.2
3.5.3
Parasympathetic Transfer Function...
. . . . . ..
49
Sympathetic Transfer Function . . . . . . . . . . . . . 49
Total Model Transfer Function . . . . . . . . . . . . . . 51
4 Data and Their Analysis
4.1 Autonomic Blockade Data . . . . .
4.1.1 Acquisition . . . . . . . . .
4.1.2 Preprocessing . . . . . . . .
4.1.3 Storage . . . . . . . . . . .
4.2 Data Analysis . . . . . . . . . . . .
4.2.1 Frequency-Domain Analysis
5
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
Estimation of the One-Pole Model Coefficients
5.1 Optimality Criteria for Estimation..... . . . .
. . . . .
5.1.1 [2 cost function . . . . . . . . . . . . . . . . . . . . .
5.1.2 L1 cost function . . .... . . . . . . . . . . . . . . . .
5.1.3 E, cost function . . . . . . . . . . . . . . . . . . . .
5.2 The One-Pole Model of the Baroreflex as a Regression . . . .
5.3 Regression on Standing Control Patients . . . . . . . . . . .
5.4 Motivation for and Setup of the Windowed LMMSE . . . . .
5.5 Windowed Least Squares Regression . . . . . . . . . . . . .
5.5.1 Numerical Stability . . . . . . . . . . . . . . . . . . .
5.6 Regularization . . . . . . . . . . . . . . . . . . . . . . . . . .
5.6.1 Numerical Conditioning..
. . . . . . . . . . . . ..
5.6.2 Statistical Motivation for Regularization . . . . . . .
5.7 Further Consideration for On-line Estimation Algorithm . .
5.7.1 Sliding Window Regression for Improved Time-Domain
'Resolution'.. . . . . . . . . . . .
. . . . . . . . .
5.8 Spectral Estimation: A Brief Discussion...
. . . . . . . ..
5.9 Final Thoughts on Estimation....... . . .
. . . . . . ..
6 Preliminary Results
6.1 Effects of Regularization on Estimates
6.1.1
6.2
6.3
6.4
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
59
60
60
61
62
62
63
73
74
75
76
77
78
80
82
86
88
89
91
93
98
. 98
99
101
103
. . . . . . . . . . . . . 103
Regularization and PSR Across All Patient Classes
.
. 105
Estimate Time-Series....... . .
. . . . . . . . . . . . . . 107
Examination of Predicted Transfer Function . . . . . . . . . . 110
Concluding Remarks............
. . . . . . . . . .. 112
7
CONTENTS
7 Conclusion
7.1 A Retrospective on the Thesis
7.2 Topics for Future Work . . . .
7.2.1 M odeling . . . . . . .
7.2.2 Testing . . . . . . . . .
7.3 Concluding Remarks... . . . . .
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
A Convex Formulation of Optimization Problems
A.1 Norms, P-Norms, and Convexity . . . . . . . . . . . . . . . .
. . . . . . . . . . . . ..
A.1.1 Convexity....... . . . .
. . . . . . . . . . . ..
.
.
.
.
.
.
.
.
A.1.2 Vector Norms
A.1.3 Convexity of the Norm of an Affine Function . . . . .
A.2 Reformulation of Optimization Problems . . . . . . . . . . .
A.2.1 L -minimization as an LP . . . . . . . . . . . . . . .
A.2.2 C,,-minimization as an LP . . . . . . . . . . . . . . .
A.2.3 LE-regularized least squares problem as a QCQP . . .
A.2.4 Practical Solution of Convex Optimization Problems
B Various Model Criteria Applied to All Patients
.
.
.
.
.
115
115
119
119
121
122
133
. 133
133
134
. 135
. 136
. 136
. 137
. 137
. 139
141
8
CONTENTS
Chapter 1
Introduction
1.1
Goals of this Research
The arterial baroreflex is a fast-acting control mechanism that the body uses
to regulate blood pressure. Baroreflex action has been studied in depth by
physiologists, and its effects are qualitatively well documented in nearly all
physiology texts. The baroreflex is a complex system. Changes in blood
pressure are sensed by stretch-sensing receptors primarily lining the arterial
walls of the aortic arch and carotid sinus, and these changes are transmitted
by efferent nerves to the autonomic nervous system (ANS). There, they are
translated into signals that are sent down each of the two branches of the
autonomic nervous system, and ultimately regulate the heart-rate, vascular
resistance, and heart contractility accordingly' [25]. If either of these two
pathways is malfunctioning, or unresponsive, a number of pathologies may
1In
fact, these two pathways control much more than this, but as far as baroreflex
action, we restrict ourselves to this simplified model of the ANS's action.
CHAPTER 1. INTRODUCTION
present, such as acute hypotensive episodes and syncope. While much is
known about the role the baroreflex plays in regulating heart rate, because
there is no non-invasive way to actually measure the outputs of the ANS,
clinicians and physiologists cannot say with certainty how the baroreflex behaves during other, more serious cardiovascular pathologies. For these reasons, measuring baroreflex action through non-invasive methods is of clinical
significance.
The importance of the baroreflex has not been lost on the quantitative
physiology community at large. On the contrary, many works have come forward and tried to understand and model the baroreflex. These works can be
divided into two major classes -
non-parametric modeling, and parametric
modeling. The former focuses on examining the empirical power spectra and
transfer functions of the blood pressure to heart rate pathway, in the hopes
that the action of the baroreflex and subsequent identification of baroreflexrelated pathologies can be determined from a closer examination of the signals themselves. The second class of quantitative baroreflex research tries to
model the baroreflex using techniques from time-series analysis and controltheory. These works use the physiological signals to estimate the parameters
of their models, with the goal of deriving meaning from these parameters and
their changes.
This work is of the latter approach. We fit the baroreflex with a simple
model, one that allows for reliable estimation and interpretation of its parameters. Where we differ from previous research in modeling is that ours is
more focused on methodology. Instead of focusing on the physiological implications our particular model and estimated coefficients, we spend a great deal
1.2. PROSPECTIVE LOOK AT THIS THESIS
of time on defining an appropriate, robust estimation algorithm to identify
our model parameters on real, clinical data. Our belief is that, with care in
parameter estimation, we can rely on simpler and more easily interpretable
models to uncover the action of the baroreflex. The goals of this thesis are
then three-fold - to derive a simple model of the baroreflex based on careful
study of physiology; to understand the optimal parameter estimation method
given our model and data; and to test our model against clinical data to see
if our estimated parameters reflect known changes in physiology.
1.2
Prospective Look at this Thesis
We continue with a brief overview of the chapters of this thesis. The thesis
is structured in a way that logically reflects the evolution of this researchnamely, it sequentially addresses each of our three goals.
Chapter 2 -
The Arterial Baroreflex
In this chapter, we provide the
reader with an overview of the baroreflex and baroreflex-related research.
We begin with a comprehensive overview of the aspects of the cardiovascular
system relevant to the baroreflex and cardiovascular control. We then discuss the specifics of the baroreflex itself, both as a single 'reflex,' and then
addressing the action of the two pathways of the ANS independently. We
conclude by introducing two ANS blocking drugs that we will encounter later
in our data sets -
atropine and propranolol. Their action and effects are
summarized both generally, and specifically for the baroreflex.
We then switch gears and examine efforts to model the baroreflex. These
sections are subdivided into the two, major classes of research I introduced
CHAPTER 1. INTRODUCTION
earlier in this chapter. The goal in this section is to give the reader an
overview of the works that preceded this thesis, and in many ways, shaped
its course. It also serves as a good reference from which the reader can see,
in the subsequent sections, how our approach differs.
Chapter 3 -
Modeling the Baroreflex
Following our overview of the
baroreflex, we remind the reader of the salient features of baroreflex action
from which we hope to build our model. We then use these assumptions to
build up the subcomponents of our model, being careful to motivate each
modeling choice we make. We then introduce our complete model, both in
time-series and in transfer function form. Once our model has been motivated
and derived, we graphically present the various forms that it can take, both in
the time-domain and the frequency-domain, followed by a brief discussion of
these various shapes. We do this to demonstrate the rich behavior our simple
model is capable of producing, both to convince the reader of our choices,
and to allow him/her to compare ours against the prior works referenced in
Chapter 2.
Chapter 4 -
Data and Their Analysis
Since this thesis's second and
third goals require us to work with real data, we must formally introduce
and understand our data. Our data consist of blood pressure measurements,
ECG measurements, and respiratory traces from patients undergoing various
drug-induced ANS blockades
2.
We do this by first discussing the methods
in which the data were collected. Following this is a short discussion of the
steps we have taken to preprocess the data for our purposes, with an extra
2
We have borrowed these data from Saul et al. [46] with permission from the author.
1.2. PROSPECTIVE LOOK AT THIS THESIS
emphasis on describing the problems introduced by this preprocessing. We
conclude this chapter by examining the data themselves, using much of the
same non-parametric methods used by the studies mentioned in Chapter
2. We do this, once again, for comparison, and additionally, as motivation
for why non-parametric methods alone cannot sufficiently capture the entire
action of the baroreflex.
Chapter 5 -
Estimation of the One-Pole Model Coefficients
In
this chapter, we define and discuss the various schema that are available
to estimate our model parameters.
This is the largest, and by far, the
most methodological and systematic of the chapters. We begin with a general definition of an estimation problem, and narrow our focus to a class of
convex-optimization criteria called residual-error-normminimization criteria
While it would be tempting to default to using minimum-mean-squarederror (MMSE) criteria , we examine other possibilities, and systematically
[9].
show why the MMSE criteria is best suited for our needs. From here, we
examine the inadequacies of the standard MMSE formulation, and pose a
modification that lends to better estimation of our model parameters. Not
satisfied with this improvement, we demonstrate its failure modes, and pose
an additional concept, regularization,which overcomes many of the shortcomings of this already modified MMSE formulation. Finally, we account
for some of the artifacts introduced by regularization, and come to our final
estimation algorithm. The bulk of the research that went in to the thesis was
focused on estimation, and unfortunately, much of it is excluded from our
3
Which is a specific residual-error-norm minimizing solution.
CHAPTER 1. INTRODUCTION
discussion in this chapter. Not to completely disregard the other estimation
schema we have explored, we end the chapter with a brief introduction to
another, promising estimation algorithm that relies on the frequency-domain
representation of our signals to estimate our parameters.
Chapter 6 -
Preliminary Results
Because the work of this thesis is
ultimately focused on clinical, patient monitoring, we show preliminary results of our model and estimation setup applied to the data introduced in
Chapter 3. We show promising initial results, with our parameters demonstrating the expected changes when comparing data of patients before and
after autonomic blockade. Due to time constraints on the research, and the
nature of our data, we were unable to test our model's ability to predict
changes in physiology before they manifest. We then finish this chapter reflecting on the success of our model, and suggesting possible directions for
future experimentation.
Chapter 7 -
Conclusion
As any conclusion, ours begins with a reca-
pitulation of the goals we have laid out here in this introductory chapter,
followed by a sequential assessment of our performance against each of them.
We do so first at a high level, and then by revisiting each chapter, and detailing the specific implications and conclusions therein. We use this information
to discuss some of the many ways in which this work could be extended and
built-upon, with the hopes that another researcher will carry on this work.
1.3. CONTRIBUTIONS OF THIS THESIS
1.3
Contributions of this Thesis
The contributions of this thesis are clustered around the work in Chapter
5, in which we systematically probe the challenges of estimating parametric
models of the baroreflex. We began with what would have seemed like a
grossly underparameterized representation of the baroreflex, and showed that
it could yield meaningful results if care was taken in fitting it to real data. In
doing so, we have been forced to discuss the set of estimation issues, namely
numerical ill-posedness and unreliability of estimates, that we suspect has
long plagued quantitative modeling efforts in this field. We then expect that
the work we have done will alleviate the burden on future researchers, and
allow them to pursue the clinical monitoring aspects of this work in greater
detail.
16
CHAPTER 1. INTRODUCTION
Chapter 2
The Arterial Baroreflex
2.1
Overview
While the mechanics of the heart are that of a continuous pump, the salient
features of cardiovascular function, its periodicity and pumping pressure, are
best described by a beat-to-beat model. Beat-to-beat models of the heart
are not a new concept. The possibility of such a beat to beat model was
explored previously by DeBoer, Karemaker, and Strackee of the University
of Amsterdam, [16] who examined whether the baroreflex could be explained
as a finite impulse response discrete-time system. Their work utilized both
time-domain and spectral analyses to relate arterial blood pressure (ABP) to
R-R interval length (the time between successive heart beats). It is their work
that serves as a launching point for this thesis. Although a finite impulse
response filter does indeed do a good job of explaining the heart's beatto-beat fluctuations, we expect that an autoregressive model will provide a
more economical representation, and perhaps better physical intuition for the
CHAPTER 2. THE ARTERIAL BAROREFLEX
baroreflex. The purpose of this research then is to measure baroreflex from a
one-pole model. The coefficients in our model represent the different factors
that contribute to the function of the baroreflex, namely the sympathetic and
parasympathetic nervous system responses. Using R-R, interval and systolic
blood pressure waveforms, easily extractable from electrocardiogram (ECG)
and ABP waveforms, we can find good estimates of these coefficients. The
stability of these estimates under normal conditions, as well as their ability
to describe a patient's physiological state will be the criteria for the success
of our model.
2.2
Cardiovascular Control Physiology
When we speak of the cardiovascular system, we must be certain that we
understand its extent.
From the pumping heart and its massive efferent
arteries down to the myriad tiny capillary beds that perfuse blood to every
inch of the body, the cardiovascular system continuosly pumps approximately
5L of blood and fluids through over many miles of vascular tissue for nearly
a person's entire lifetime. At a high level, the human cardiovascular system
serves two main purposes - to bring nutrients and oxygen to, and to remove
waste and metabolic byproducts from the body's various tissues. Because the
rate at which different tissues need oxygen and nutrients, or waste removal,
varies significantly between tissues (e.g.
the brain versus the finger nail
beds), and changes with the state of the body (e.g. sleeping, exercising,
standing quickly from a hot bath), the cardiovascular system must employ
different mechanisms by which to increase, decrease, and direct the flow
2.2. CARDIOVASCULAR CONTROL PHYSIOLOGY
of blood throughout the body. Together, these mechanisms constitute the
body's cardiovascular control system. One such pathway, the baroreflex, is
the focus of this thesis.
2.2.1
Anatomy and Function of the Cardiovascular System
Before diving into the details of the baroreflex, a brief overview of the
anatomy of the cardiovascular system (CVS) is in order-tracing the path
of blood in systemic circulation, starting at with the plumbing: the vasculature.
The Vasculature
The human vascular system is vast, criss-crossing the entire body. Starting
with the aorta, the rigid, elastic arteries send oxygenated blood outwards
from the heart to the body. From the arteries, the arterial tree branches into
many smaller arterioles. Arterioles, surrounded by smooth muscle, are the
primary source of vascular resistance, and have the greatest influence on local
blood flow regulation. The final level of efferent vasculature subdivision are
the capillaries, which are no larger than a single cell in diameter, but extend
to every corner of the body. Their thin structure allows nutrients and oxygen
to easily diffuse into neighboring tissues.
Once blood passes through the capillary beds in systemic circulation, it is
de-oxygenated, and must be taken back to the heart to be re-oxygenated and
start the process again. The venous system serves this exact purpose. Veins
differ from arteries and arterioles in that while they do have smooth muscle
CHAPTER 2. THE ARTERIAL BAROREFLEX
lining their walls, they are generally thin and are not particularly contractile
in nature. Quite the contrary, veins are far more compliant than arteries and
can accomodate varying blood volumes. The venous tree then is similar in
structure to the arterial tree, but with blood flowing from the leaves to the
root. The root, the superior and inferior vena cava, serve as the last stop
for de-oxygenated blood before leaving the systemic circulation for the right
atrium of the heart.
The Heart and its Conduction Pathways
The human heart is subdivided into two halves, right and left. In each half,
blood enters the heart into the atrium, a small "filling-chamber". From there,
blood is pumped into the larger, more muscular ventricle, which pumps blood
into efferent arteries. The two halves of the heart serve different purposes
though: the right takes de-oxygenated blood returning from the venous system and pumps it into the lungs by way of the pulmonary artery; the left
takes freshly oxygenated blood from the pulmonary veins and pumps it back
into the aorta which subdivides into the rest of the body's vasculature.
When pumping, blood is pushed from both atria into their respective
ventricles by simultaneous contractions. After the ventricles have been filled
thusly, they too contract, forcing the blood outwards. Backflow of blood is
prevented in each of these contractions by a series of valves at the top and
bottom of both atria and both ventricles.
While this pumping action is purely mechanical, it is driven by the electric depolarizations and repolarizations of the myocardial (heart) tissue. All
myocardial tissue exhibits a phenomenon called automaticity-the ability to
2.2. CARDIOVASCULAR
CONTROL PHYSIOLOGY
generate an action potential impulse via rapid depolarization. In addition,
all myocardial tissue will itself depolarize if subjected to an action potential
impulse from neighboring tissue, and in doing so, propagate the depolarization throughout the entire myocardium. Obviously there are limitations to
this firing, as there is a set refractory period after a depolarization in which
the myocardial cells are non-reactive to these stimuli. Further, if a cell receives an action potential impulse before its own internal firing timer runs
down, it will immediately depolarize and its internal timer will reset. In this
way, the cells with the fastest internal timers continuously override the other
cells' timers, and act like a pacemaker, coordinating the beating of the heart.
In the normal heart, these pacemaker cells exist in the sinoatrial (SA) node
in the right atrium. A depolarization wave rapidly causes the right atrium to
contract. This wave immediately travels to the left atrium via Bachmann's
bundle, causing a nearly simultaneous contraction of both atria. In electrocardiogram (ECG) measurements of the heart, this is known as the P-wave.
The thick coronary sulci, that separate the atria from the ventricles, blocks
this depolarization from entering into the ventricles. As a result, the electrical
signal from the contracting atria is forced to travel through what is known as
the atrioventricular (AV) node, where conduction is much slower than in the
rest of the myocardium. This allows for the atria to fully contract and fill the
ventricles with blood before the ventricles begin contracting. Once through
the AV node, the contraction impulse is rapidly transmitted throughout both
ventricles via the bundle of His and the Purkinje fibers, propelling blood out
of the ventricles. This ventricular contraction manifests itself as the R-wave
in an ECG, and the total time between atrial and ventricular contractions is
CHAPTER 2. THE ARTERIAL BAROREFLEX
known as the P-R. interval.
Disruption of this conduction pathway or in the pacing of the heart manifest themselves in a number of pathologies. Though a discussion of these
pathologies is outside of the scope of this thesis, it is important to note that if
a portion of the myocardium does not receive a pacing signal for an extended
period of time, its own automaticity will cause it to generate its own pacing
signal. In some cases, these alternate pacing signals actually drive the heart
to beat spontaneously or in an abnormal way in what is known as an ectopic
heartbeat.
2.2.2
Autonomic Nervous System Control of the Heart
The autonomic nervous system (ANS) is the portion of the human nervous
system that governs involuntary behavior, such as metabolism, digestion,
and most important for this thesis, arterial blood pressure. Based on various
signals corresponding to blood pressure, blood gas levels, and blood metabolite levels, the autonomic nervous system both modulates cardiac output and
peripherally directs blood flow to maintain the body's health. The ANS can
be further subdivided into the parasympathetic and sympathetic nervous
systems, which can crudely be described as the "calming", and the "fightor-flight" pathways, respectively. The parasympathetic nervous system acts
on the CVS primarily through the vagus nerve and the neurotransmitter
acetylcholine (ACh), while the sympathetic system employs both nervous
and adrenergic chemical pathways. Of the many regulatory pathways the
ANS uses to modulate the human heart, this thesis hopes to explore the
pressure sensing pathway, the baroreflex. Because of the differing time-scales
2.2. CARDIOVASCULAR CONTROL PHYSIOLOGY
at which each of the different control pathways works, we can safely study
the baroreflex while ignoring the effects of these other pathways.
2.2.3
The Human Baroreflex
The human baroreflex is a wonderfully complex mechanism for maintaining
the requisite blood pressure the body needs for optimal perfusion of tissues.
While completely denervated patients, lacking a baroreflex alltogether, have
been shown to have perfectly functioning blood pressure regulation, the control an intact baroreflex exerts on the heart is both rapid and profound [25].
The baroreflex, administered by the ANS, relies on pressure sensors called
baroreceptors. Located in the aortic arch (near the heart) and the carotid
sinus (in the neck), the two most influential baroreceptors are highly innervated segments of the blood vessel walls that send electrical impulses to
the brain based on deformations in the diameter of the vessel walls-higher
stretch corresponds to a higher firing frequency. The carotid baroreceptor
are innervated by the glossopharyngeal nerve, while the aortic baroreptors
are innervated by the vagus nerve. Both pathways converge at the nucleus
of solitary tract (NTS) in the brain, which examines the firing frequency to
determine the state of the blood pressure, and then determines parasympathetic or sympathetic tone to maintain cardiovascular homeostasis. Because
vascular "stretches" are relative measures, firing frequencies are determined
by deviations in vascular stretch from a setpoint. As far back as the 1970's
Guyton et. al. demonstrated this concept by showing that baroreceptor activation is blunted in chronically hypertensive (high-blood pressure) patients,
and that this blunting occurs within hours of a sustained hypertensive episode
CHAPTER 2. THE ARTERIAL BAROREFLEX
[25]. While this is now a commonly accepted fact, determining how the body
determines this setpoint is a topic of continuing research.
On this topic, more modern research presented by Ganten and Pfaff has
demonstrated that due to the aortic baroreceptor's direct innervation of the
vagus nerve, it has a predominantly depressor effect on heartrate and pressure. To counteract this, their empirical examinations of the carotid baroreceptors have shown that its set point, instead of being centered at a "normal"
blood pressure, is centered higher up towards the receptors saturation limit
[15]. This could also be because the carotid baroreceptors need to be more
sensitive to drops in blood flow to the brain, and thus require increased
sensitivity to lower pressures.
Parasympathetic Control of Heart Rate
The baroreflex controls blood pressure primarily by increasing and decreasing
parasympathetic tone. When compared to the sympathetic nervous system,
equal changes in parasympathetic tone can elicit changes in heart rate and
blood pressure several times as great.This is because the SA node, the atria,
and to a lesser extent, the ventricles, are richly innervated by cholinergic
(parasympathetic) fibers, or in the case of the SA node, the vagus nerve
itself. Studies have shown that cutting the vagus nerve or administering a
parasympathetic blockade with drugs can elicit an increase in resting heart
rate of 35%, while a mechanical or electrical stimulation of the vagus never
can cause the atria to stop beating within 1 heart-beat [25]. In the latter case,
patients usually exhibit ventricular escape beats, a specific type of ectopic
beat triggered in the ventricle, within a matter of seconds, with beat strength
2.2. CARDIOVASCULAR CONTROL PHYSIOLOGY
reduced by 15-20% [25]. Further studies by Brown and Eccles (1934) found
that the strength and duration of vagal stimulation on the heart was directly
related to when during the heart-beat cycle the stimuli were administered,
and in all cases, cardiac function returned to normal within 10-15 seconds of
a stimulus [41]. They attributed this near immediate response and equally
short time constant to the short diffusion distance acetylcholine faces in the
SA node, and to the extremely high concentration of acetylcholinesterase
in the tissues surrounding the SA node. What is equally of importance to
note is that the parasympathetic nervous system exhibits what is known
as "accentuated antagonism" with its sympathetic counterpart: the negative
chronotropic effects of vagal stimulation increase when there is a simultaneous
stimulation of the sympathetic nervous system.
Sympathetic Control of Heart Rate
The sympathetic control of the heart rate is complex,especially when the
baroreflex is concerned. Unlike the parasympathetic nervous system which
acts mainly via the fast acting vagus nerve, the sympathetic nervous system
acts on the CVS via sympathetic nerves as well as by modulating adrenergic
chemicals in the body. Compared to stimulation of the vagus nerve, direct
stimulation of the sympathetic nerves causes a change in heart rate < 5%
[25]. This percentage jumps to nearly a 100% increase in heart rate when the
person is undergoing a parasympathetic blockade - further supporting the
notion that the sympathetic response of the baroreflex is as much because of
an inhibition of the parasympathetic system as it is because of stimulation
of sympathetic pathways. In fact, the sympathetic outflow of patients with
CHAPTER 2. THE ARTERIAL BAROREFLEX
increased intracranial pressure or ischemia (localized restriction of bloodflow)
is between 4 to 6 times as great as when baroreflex stimulates the sympathetic pathway. Unlike the parasympathetic nervous system, the sympathetic
nervous system tends to effect the heart's contractility, and therefore, the
beat strength of the heart. Maximal stimulation of the sympathetic nerves
increased beat strength by 60-70%, as compared to the 15-20% reduction
in strength caused by parasympathetic stimulation[25] .The time-constant of
the sympathetic control pathway is also markedly longer than that of the
parasympathetic system, ranging from 30 seconds to as long as 8 minutes
[25] .This in large part due to the greater role neurotransmitters play in the
sympathetic pathway. The main sympathetic adrenergic receptors can be
divided into a receptors, and 13 receptors (further subdivisions exist, but are
not relevant to this discussion). a receptors are most responsive to neurotransmitters norepinephrine and epinephrine, and primarily control smooth
muscle tone and act as neurotransmitter inhibitors.
/3 receptors
collectively
control changes in lipolysis, heart muscle contraction, and to a lesser extent,
smooth muscle contraction, and are most sensitive to the neurotransmitter
isoprenaline [41]. In addition to being vital for baroreflex, 0 receptors also
control the production of renin, a key component in the renin-angiotensinaldosterone (RAAS) system- a slower blood pressure regulatory pathway
mediated by the kidneys and lungs.
The sympathetic response is governed by adrenergic receptors in presynaptic and post-synaptic locations. Pre-synaptic sites can be stimulated
or inhibited by hormones and neurotransmitters, such as angiotensin, adenosine, catecholamines, prostoglandins, and ACh.In these presynaptic locations
2.2. CARDIOVASCULAR
CONTROL PHYSIOLOGY
(mainly comprised of a 2 receptors), receptors in axon-terminals react to exogenous agonists by releasing neurotransmitters, and are inhibited by endogenous neurotransmitters via negative feedback. In post-synaptic locations,
receptors stimulated by neurotransmitters release mediators that cause the
responses that constitute sympathetic cardiac control. Because this total
response can be modulated both pre and post synaptically, sympathetic response to different interventions can be complex.
2.2.4
Pharmacological Intervention and the Baroreflex
To better understand the baroreflex, part of this thesis involves analysis of
patients undergoing chemical blockade of parasympathetic and sympathetic
nervous pathways with atropine and propranolol, respectively. For this reason, it is important to briefly address the pharmacology and action of those
drugs, so we can better understand their effects.
Atropine
Atropine, 3-hydroxy-2-phenylpropanoate, is used as a parasympathetic nervous system blocking agent. Originally discovered in the nightshade plant,
atropine is a competetive antagonist of ACh with a half-life of ~2 hours [32].
Atropine is prized as an extremely selective blocker in cardiac and smooth
muscle cells, having a strong effect on all muscarinic acetylcholine receptors
(mAChR's: M 1 , M 2 , and M3 ) and having a negligible affect on nicotinic
acetylcholine receptors (nAChR's) [32]. At varying dosages, atropine has the
following effects on humans:
o 0.5 mg - Diminished salivary and sweating responses
CHAPTER 2. THE ARTERIAL BAROREFLEX
* 1-5 mg - Pupils dialate and heart rate increases
* > 5 mg - Motility and tone of the gut decreases, micturition inhibited
Because of the wide range of uncomfortable side-effects, more selective mAChR
blockers are preferred in a clinical setting.
Atropine in the Heart
Because parasympathetic control of the heart is
most notable in healthy adults atropine is not as effective when administered
to children or the elderly. In healthy adults, atropine blocks vagal stimulation
of the SA node by binding to A 2 mAChR's, causing an increase in heart rate.
Amongst other things, this may stop or decrease the occurrence of respiratory
sinus arrhythmia (RSA) in patients [22]. Atropine also increases heart rate
by reducing the AV node conduction time, effectively shrinking P-R interval
lengths. Further, atrial conduction times are also decreased. In extremely
high doses, atropine has been shown to cause atrial arrhythmia and possibly
atrioventricular dissociation [22].
Propranolol
Propranolol is a non-selective 73-blocking drug used most often to treat hypertension and related arrhythmias. Its effects are not as noticeable in normal
patients, but become more apparent in exercising patients or those undergoing tilt-tests. Propranolol acts to slow the release of norepinephrine from
nerve terminals, and also blocks the release of renin from the juxtaglomerular
apparatus [22].
2.3. PRIOR WORK
Propranolol in the Heart
In the atria, propranolol decreases the SA
node's firing rate, and thus, the heart rate. In addition, the heart's contractility is decreased, and the AV node conduction time is increased, causing
a slight decrease in blood pressure, and a more noticeable drop in cardiac
output (CO). Propranolol reduces the firing rate of all ectopic pacemakers
as well. Counterintuitively, the 3 blocking effects of propranolol appear to
increase a-receptor sensitivity to pressors, drugs that increase blood pressure
such as epinephrine, and increase the effects of the mAChR blocker, atropine
[32].
2.3
Prior Work
There exists a vast depth of literature pertaining to modelling the autonomic
nervous system regulation of the heart. Most of the significant works in the
area center around one of two topics: understanding the frequency dependence of the various control pathways, and determining models that explain
the action of these pathways.
2.3.1
Spectral Analysis of Heart Rate Variability
The majority of the work focusing on understanding the spectral dependence
of cardiac control aims to determine the dominant frequencies at which the
sympathetic nervous system, parasympathetic nervous system, and other
pathways such as the renin-angiotensin-aldosterone system (RAAS) regulate the heart. Using /-blockers and muscarinic receptor blockers, many of
these studies performed unilateral and bilateral autonomic nervous system
CHAPTER 2. THE ARTERIAL BAROREFLEX
blockades of subjects to identify the conditions under which different nervous
system pathways affect cardiac control. In all major cases surveyed, the frequencies relating to cardiac control are in the range of 0-0.5 Hz [2, 37, 39, 43].
Even more specifically, this frequency range can be partitioned into two subsets of interest - the low frequencies (LO-FR, approx. 0.05 < f < 0.12 Hz),
and high frequencies (HI-FR, approx. 0.2 < f < 0.28 Hz ). Pomeranz et. al
(1985) found that the power of the heart rate signal in the high frequency
band was correlated to the depth of breathing with the frequency of peak
power related to the breathing frequency. In addition, their research showed
that high-frequency cardiac control is almost entirely the responsibility of the
parasympathetic nervous system, while low frequency control is mediated by
both sympathetic and parasympathetic systems, as well as the RAAS [39].
In the low frequency band, they found that while both parasympathetic and
sympathetic nervous systems actively regulate heart rate, body tilt plays a
key role in determining the relative strength of each pathway. Specifically,
they found that in the standing position, both sympathetic and parasympathetic activity mediate heart rate variability, while in the supine position,
parasympathetic activity dominates.
The work of Akselrod et. al. (1985) corroborates each of these claims by
Pomeranz, and draws attention to two more spectral peaks in heart rate signals, namely a peak between 0.1 Hz and 0.15 Hz , and a very low frequency
peak between 0.04 Hz and 0.08 Hz. The former is often attributed to Mayer
waves, spontaneous unexplained 0.1 Hz oscillations in blood pressure, while
the latter is likely caused by changes in vascular tone caused by thermoregulation. They found that parasympathetic blockade reduces the variability of
2.3. PRIOR WORK
arterial blood pressure and heart rate at low, and especially at high frequencies. The reduction in HR variability was far more pronounced than that of
ABP variability, indicating that cardiac control might act on the former more
profoundly than the latter, a fact corroborated by Saul et. al. (1991) [46].
The work of Saul et al. studies the non-parametric transfer functions using
a broad-band respiratory drive previously discussed by Berger et al.' (1989)
[7], with both papers using this technique to try and tease apart the effect of
RSA on the baroreflex 2 . A byproduct of this work is that they demonstrate
that in sympathetic ) - blockade, the reduction in ABP and HR variability
is negligible at high frequencies, while noticeable at low frequencies.
Di Rienzo et. al. (2009) performed similar experimentation on cats, but
used surgical denervation to remove the sympathetic and parasympathetic
2
nervous pathways [43]. They analyzed the squared coherence modulus (Ik1
where S,,(w) is the power spectral density of x and Sx,(w) is
the cross spectral density of x and y) of the R-R interval length and systolic blood pressure of cats with intact nervous control and after autonomic
denervation. A high coherence modulus implies a more linear relationship
between the two signals at the given frequencies. They found that the noticeable peak in Ik12 value at 0.1 Hz in the control case was absent in the
denervated cats, which experienced an increase in |k12 at lower frequencies.
They concluded that at low frequencies, baroreflex mediation of heart rate
by autonomic nervous system is via nonlinear means and is relatively linear at higher frequencies. In addition, their work showed a marked drop
'The first authors of each paper being a named author on the other as well.
2
The RSA is thought to act only at the respiratory frequency. The authors have
patients breath according to a modified Poisson process, thereby attempting to whiten
the respiratory power across all frequencies
CHAPTER 2. THE ARTERIAL BAROREFLEX
in heart rate signal power when autonomic control was removed. DeBoer,
Karemaker, and Strackee examined the coherence of R-R interval length and
systolic blood pressure in humans with an intact baroreflex and found the
same peak located at around 0.1 Hz that Di Rienzo et. al. noted in cats
2.3.2
[16].
Modeling of Heart Rate Transfer Function
Research into modeling the heart rate transfer function focuses on determining the magnitude and the phase of the heart rate response to changes in
blood pressure and other physiological signals. The work of DeBoer, Karemaker, and Strackee (1987), which serves as the launching point of this thesis,
aims to model fast heart rate regulation by the autonomic nervous system,
at frequencies > 0.5 Hz [16]. They model the klh R-R interval length as a
moving average (See Ch 3.2.1) model, with blood pressure as the input. In
order for their model to agree with existing research that shows baroreceptor sensitivity (BRS =
RR)
as sigmoidal, the pressure values they input
into their model are what they define as, "effective systolic pressures," given
by S'
-
120 + 18 arctan
S 120
where S is the systolic blood pressure. In
their model, the coefficient of the k" effective systolic pressure represents
the vagal contribution to baroreflex, while the other coefficients represent
the sympathetic contribution. In order to perform simulations, DeBoer et.
al. restricted the number of taps of their model to k < 6, with the sum of
the systolic contribution equal to that of the vagal contribution. Their work
was limited to simulation, in which they simulate blood pressure by a priori
determining a respiratory frequency and fixing the mean blood pressure at
120 mmHg. In simulations of resting human blood pressure, their model
2.3. PRIOR WORK
implies that there is no phase lag between changes in ABP and changes in
R-R interval length. More specifically, their model claims that respiration
affects ABP which in turns affects R-R interval length via the baroreflex.
This directionality was partially demonstrated in clinical data by O'Leary et
al. (2003), who noticed that in the supine position, changes in MAP were
followed by a "directionally similar" change in TPR approximately 2 seconds
later [37].
Saul et. al. (1991) not only focused on modeling the ABP-HR transfer function, but also on the ABP-Respiration and HR-Respiration transfer functions
[46]. The authors are very careful to note that the ABP-HR transfer function
is closed loop and examining the transfer function phase does not truly capture causality. Theirs is an autoregressive, continuous-time model (See Ch
3.2.2) in which the sympathetic and parasympathetic pathways are modeled
as ideal low-pass filters, with an additional continuous-time-delay element
on the sympathetic pathway. In addition, they choose to model both the
vasculature and the baroreceptors themselves as independent, continuoustime delay elements. When the model is fitted to non-parametric transfer
functions from their data, the authors note a consistent phase lag between
instantaneous lung volume (ILV) and pulse pressure (PP) of -90', with a
significant increase in magnitude when standing than when supine.They also
posit that the sympathetic nervous system does not contribute to the effect
respiration has on ABP. Further, they claim that the mechanical coupling
between breathing and cardiac control is stronger in the standing than in
the supine position. This finding does in fact conflict with the research of
Pomerantz discussed earlier, as the mechanical breathing-heart rate coupling
CHAPTER 2. THE ARTERIAL BAROREFLEX
is often attributed to vagal stimulation.
Akselrod et. al. (1985) describe a novel closed loop model of baroreflex in
their work. They describe the forward path between HR and ABP as a linear, time-invariant (LTI)
system
HABPHR(f)
with an additive noise source
ny that represents the mechanical modulation of ABP due to intrathoracic
pressure and changes in localized autoregulation of vascular bed tone [2].
Similarly, the forward path between ABP and HR is modeled as an LTI system
HHR,ABP(f)
with another noise source n, that represents inputs from
receptors other than baroreceptors as well as centrally mediated variation
in autonomic tone. By modeling external factors in the HR-ABP pathway
as two separate noise sources, the model takes advantage of the frequency
dependence of the various external inputs noise sources. At low frequencies,
nx is nearly non-existant, and at high-frequencies, ny is nearly non-existant,
making a closed-form solution of the model possible if these approximations
are taken into account. The work by Barbieri, Parati, and Saul (2001) focused on characterizing closed-loop dynamics of the heart baroreflex using
discrete-time, bivariate modeling [4]. Their work centers around independently estimating the feedback loop (ABP to HR) baroreflex, and the closed
loop (feedback loop as well as their proposed HR to ABP feedforward loop)
heart baroreflex as separate, autoregressive elements. In doing this, they try
to show that examining the forward loop and feedback loop separately, as
many researchers are wont to do, provides inaccurate estimates of baroreflex gains and actions as compared to simultaneously modelling both directions.They performed estimation of their parameters using a recursive least
squares estimation method (RLS) with a forgetting factor tuned to between
2.3. PRIOR WORK
35
0.8 and 1 (corresponding to a per-beat blood pressure effect half-life of > 3
heartbeats).
To enhance the stationarity of their signals, the researchers
pre-filtered all of their signals with an IIR filter with a 0.03 Hz corner frequency.The authors conclude that independent open loop analysis of the
feedforward and feedback paths do produce different estimates of baroreflex
gains than closed loop analysis, with the open loop gains tending to be larger
than closed loop estimates. This, they claim, is due to the fact that unidirectional analysis attributes all changes in the output to changes in the input,
but in fact, these changes are bidirectional and simultaneous.
36
CHAPTER 2. THE ARTERIAL BAROREFLEX
Chapter 3
Modeling the Baroreflex
3.1
Modeling Considerations
In order to model the baroreflex, we must first decide on a class of models
that is rich enough to explain the baroreflex, yet simple enough to facilitate
easy estimation. We begin by examining the salient features of the ANS
baroreflex, namely:
"
High blood pressure elicits a baroreflex response that aims to lower
blood pressure and slow the heart, and vice versa.
" ParasympatheticPathways - The main affector of the baroreflex. Acts
within a heart-beat to control heart-rate via the vagus nerve, with a
relatively short time constant on its decay.
* Sympathetic Pathways - The lesser affector of the baroreflex.
Acts
within the span of a few beats via adrenergic neurotransmitters and
CHAPTER 3. MODELING THE BAROREFLEX
some direct innervation, with a long time constant (from ~ 15s to up
to ~ 5 minutes)
From this brief overview of the baroreflex, and considering the body of
research and work presented in Ch. 1, it is clear that many model classes
could serve as the proper platform to understand the baroreflex. Our goal in
modeling is to gain useful estimation about the state of the baroreflex. What
we do not hope to explain is the effects of other regulatory pathways such as
the RAAS and chemoreceptors, nor do we expect to be able to phenomena
such as RSA or Mayer waves. Understanding that these all play a role in
defining the function and regulation of the CVS, we expect that a carefully
chosen model and estimation scheme will demonstrate the baroreflex action,
without overfitting to the effects of other such mechanisms.
3.2
Time Series Models
Before discussing our chosen model of the baroreflex, a bit of modeling notation must be introduced. We will restrict our focus to four classes of
discrete-time models commonly used in physiological modelling: moving average (MA), autoregressive (AR), and autoregressive with exogenous inputs
(ARX) models. I will try and provide as succinct but complete description of
these time-series models, but for further reading, I direct the reader to other
resources, such as the books by Box and Jenkins [21], Porat [40], and Ljung
[33], among others.
3.2. TIME SERIES MODELS
3.2.1
Moving Average (MA) Models
A moving average model of time-series Yt relates Y to past and present values
of a (generally) white-noise input, and takes the form:
Yt
p
y±+5EWi -rt-i
i=0
where p, is a constant, wi are scalar weights, and p is the order of the
model. The noise values, ij, are independent draws from an zero mean, finite
variance white-noise process 1. The model then is a finite impulse response
(FIR) filter, with p impulse response coefficients. The primary assumption
of MA models is that the process Y is a stationary process [40]
2.
For this
reason, both inputs and outputs cannot exhibit seasonality or trends, and
should be de-trended before modeling is attempted.
3.2.2
Autoregressive (AR) Models
An autoregressive model of a time series Y recursively relates Yt to its past
values, by taking the form:
P
Y = yy +(
Oi -t-i
+ 77t
where the definitions for py, ir, and p are unchanged from the MA case, and
we replace weights wi with 6j. The same assumptions of stationarity apply to
'This white-noise assumption can be relaxed to allow for r to be another known timeseries.
2
In a broad sense, a signal is stationary if its statistical moments do not change based
on when the series is sampled.
CHAPTER 3. MODELING THE BAROREFLEX
the inputs and outputs of an AR model. AR coefficients are often discovered
from a time series of Y by solving the Yule-Walker equations, which are a set
of p equations that derive from the autocorrelation function of Y assumed
by the AR structure.
3.2.3
ARX/ARMA Models
An autoregressive model with exogenous inputs of time series Y recursively
relates Y to its past values, as well as past and present values of an exogenous
model input, Xt.
P
Yt=y+Z
i=1
q
1-Y- +(
-Xt-i + qt
i=0
where the model order is now described by two parameters, p and q, -yand
O are weight vectors, and 71 is again i.i.d. zero-mean white noise. Here, a
distinction must be made between ARX and autoregressive moving average
(ARMA) models, as in the ARMA case, Xt is replaced by it and the 7t term
in the ARX model can be subsumed by the -yo in the ARMA model.
3.3
Derivation of Baroreflex Model
We avoid modeling the entire closed-loop baroreflex as estimation of closedloop parameters is a challenging problem unto itself [21], and so we will stop
with trying to understand the forward ABP--HR pathway of the baroreflex.
Building on the success of DeBoer et al. at modeling the forward baroreflex using an MA model to model this forward loop, we seek to find an
3.3. DERIVATION OF BAROREFLEX MODEL
alternate, more parsimonious representation. From our examination of their
model, we believe that an ARX model can closely match the geometric constraints and impulse response DeBoer et al. simulated with their MA model.
More specifically, we believe that a one-pole, one-zero (1p1z) model can model
the baroreflex with more easily estimable coefficients than a MA model can.
While we expect higher order ARX models to be able to capture richer impulse responses, parameter estimation becomes much less reliable as model
order increases.
Our model represents the kth R-R interval (RRk) as the sum of components reflecting parasympathetic response (Pk) and the sympathetic response
(Wk),
(Sk),
both of which are assumed to be functions of systolic blood pressure
and an external noise source, Nk. We accordingly write:
RRk - Pk +Sk+
N
(3.1)
To better characterize the relationship among pressure, central nervous
system response, and R-R interval variability, we linearize our model by using
the signals' beat-to-beat deviations from their respective set-points instead of
from their nominal values, denoting these deviations with lowercase letters.
The estimation of an appropriate set-point parameter will be saved for future
work. Since the parasympathetic response is equated to the very fast acting
vagal response, we can describe the parasympathetic response as a function of
systolic blood pressure in the current heart-beat using the following equation:
Pk -- o
Sk
(3.2)
42
CHAPTER 3. MODELING THE BAROREFLEX
Figure 3.1: Block diagram of one-pole, one-zero model of baroreflex
where ao can be thought of as the gain for the parasympathetic tone. Because the sympathetic response relies more on adrenergic neurotransmitters
to control heart rate, we model the current sympathetic response at the kth
heart-beat as a function of the sympathetic response at the previous heartbeat, and the systolic blood pressure at the previous heart-beat:
Sk
a1
- Sk-1
+ 0
- Sk-1
A block diagram of our small-signal model is presented in Fig. 3.1
(3.3)
3.
This constitutes a single-pole autoregressive model for baroreflex, with a
pole at
0.
Putting the two components together, we arrive at our beat-to-
beat model of the baroreflex:
rk ~ cO - Sk
3
+ a1 - Sk-1 + 1
-rrk-1 -+-k
(3.4)
We describe our block elements as the z-transform of their discrete-time impulse responses, both of which are described in the following sections
3.3. DERIVATION OF BAROREFLEX MODEL
It is often assumed that the small-signal noise source, nk, is Gaussian, or
of some known distribution. Here we do not yet choose to do this. Instead
we further focus on our model parameters and their interpretation.
Model Parameters and Derived Parameters
To extract meaning from our model, it is important to understand what
each of our parameters means. It is easy to see that ao, being the only
parasympathetic parameter, should be the parasympathetic gain-its fluctuation should mirror the changes in parasympathetic tone. A naive approach
would then be to assume ai represents the sympathetic gain. This will, as
I will demonstrate later, validate the commonly accepted notion that the
parasympathetic gain is multiplicatively larger than the sympathetic gain.
Sympathetic activity continues far beyond the ai coefficient of our model, as
it includes a feedback loop with gain #. Therefore, I will say that sympathetic
c
[
a for 0 < < 1. Because
1i=
these gains are likely to be unique to each patient due to differences in heart
gain is defined as the infinite sum: a 1
rates and blood pressures, it is important that we normalize them somehow
for analysis. Define the parasympathetic-to-sympathetic ratio (PSR) as:
PSR
Gp
(3.5)
where G, and G, are respectively the parasympathetic and sympathetic
gains,as defined above, meaning:
PSR =
ao(1ao(1 - 0) + a1
CHAPTER 3. MODELING THE BAROREFLEX
We will use PSR extensively to compare patients undergoing various
interventions later in this thesis.
Because our model parameters reflect physiological gains, we impose certain restrictions on their ranges. First, we require all paramaters to take only
non-negative values, as the sign of the change in R-R interval length should
be the same as that of the change in blood pressure assuming the change
is due to baroreflex. Further, we force 0 to be strictly less than 1, as the
sympathetic impulse response should have finite-energy and be BIBO stable
oc
3.4
Time-Domain Behavior of our Baroreflex
Model
In order to properly interpret the results of future experimentation with our
1plz model, is necessary to understand its time-domain characteristics - both
as independent subcomponents, and then as a single model. For this analysis,
we will only consider the discrete-time impulse response of the constituent
sub-systems, where the input bpk = 6[k], where:
1 for k = 0
6[k] =
(3.6)
0
otherwise
Because we are discussing impulse responses of both Pk and sk, we will
use standard systems notation to denote these impulse responses, and refer
to them as p[k] and s[k], respectively. Further, we call the entire system's
3.4. TIME-DOMAIN BEHAVIOR OF OUR BAROREFLEX MODEL 45
impulse response h[k], with h[k] = p[k] + s[k] (this relationship holds by
linearity of the system). It is important to note that rrk is the convolution
(*) of bpk and h[k], as this is integral to understanding why we place so much
emphasis on the impulse responses of our system and subsystems:
O
(
rrk=h*bpk=
h[T- k] - bpk
(3.7)
T=-00
3.4.1
Parasympathetic Impulse Response
Because the parasympathetic contribution to R-R interval in our model is a
simple gain element, its impulse response is just a scaled impulse response,
shown for a different values of ao in Fig. 3.2, and given mathematically as:
p[k]
3.4.2
ao
for k = 0
0
otherwise
(3.8)
Sympathetic Impulse Response
The sympathetic pathway is modeled as a one-step delay applied to a onepole model, and consequently has more complex behavior when coefficients
ai and 0 change. Unlike the parasympathetic pathway, the sympathetic
pathway has an infinite impulse response, with initial "height" parameter,
ai, and "shape" parameter /. Mathemetically, we write the impulse response
as:
CHAPTER 3. MODELING THE BAROREFLEX
Parasympathetic Impulse Response
II
I
I
0
--
a O
.. .
-1
-0.8
-06
-84
0
-02
02
0.4
0.6
8a
0'8
k (beats)
Figure 3.2: Parasympathetic impulse responses for various values of ao
p[k] =
ai - Ok0
From Fig.
for k > 1
(3.9)
otherwise
3.3, we see that increasing ai can significantly change the
magnitude of the first few terms of s[k], but irrespective of the choice of
ai, the systems converge relatively quickly. On the other hand, if only
f
is changed, the long-term evolution of s[k] is changed dramatically. Specifically,the half life time of the system k changes goes as -
1 + 1 as seen
.........................
iiiiiii
3.4. TIME-DOMAIN BEHAVIOR OF OUR BAROREFLEX MODEL 47
in Fig. 3.4, with lim ki = oc, and lim ki = 1
/3-1
2
#02
It is interesting to note, however, that because the value of derived DC
gain parameter, G, depends on both a1 and 0, there are a series of curves,
of differing impulse response heights and durations, that corresponse to constant values of G, as shown in Fig. 3.5. For a given G, as /
and as 3 -+ 0, ai
-+
-
1, ai
--
0,
G,.
Sympathetic Impulse Response
.
E
<1
k (beats)
Figure 3.3: Sympathetic impulse responses for various values of 3
1.26c(
. ..............................
CHAPTER 3. MODELING THE BAROREFLEX
Sympathetic Impulse Response
k (beats)
Figure 3.4: Sympathetic impulse responses for various values of 3
3.4.3
Total Model Impulse Response
The total model impulse response is the additive sum of the sympathetic and
parasympathetic impulse responses, and so we write:
h[k]
a~o
for k
ai -0k-1
fork> 1
0
otherwise
0
(3.10)
Linearity dictates that the behavior of the total model impulse response
3.5. FREQUENCY DOMAIN BEHAVIOR OF THE ARX BAROREFLEX MODEL49
Iso-G. Impulse Responses
0
1
k (beats)
Figure 3.5: Sympathetic impulse responses for constant G, - various values
of ai, #
reacts in the same ways as its subcomponents to changes in ao, ai, and 0,
and so further discussion is not necessary.
3.5
Frequency Domain Behavior of the ARX
Baroreflex Model
Understanding the frequency-domain characteristics of our ARX model allows us to understand the filtering by which our system converts blood pres-
50
CHAPTER 3. MODELING THE BAROREFLEX
sure to R-R interval, as well as the limitations of our model has in capturing
R-R variability.
To understand the frequency-domain characteristics of the parasympathetic and sympathetic systems, we examine their transfer functions, where
the transfer function, H(e-jQ), of a discrete-time system with impulse response h[k], input
Xk,
and corresponding output Yk is given by:
Y(e-J0)
H(e-) = Y(-Q)(3.11)
X(e-inl)
where X(e
iQ) = F(Xk)
is the discrete-time Fourier transform of
Xk,
given
by the relationship:
00
F(Xk)
S
Xke-jk,
0 < Q < 27r
(3.12)
k=-co
We can think of the DTFT as the discrete-time equivalent of the standard
Fourier transform, and a special case of the Z-transform (replacing e-j9 in
the sum with z-'), itself the discrete-time analog of the Laplace transform.
Further, when considering the discrete-time case, we are limited to frequencies in the range 0 < Q < 27. Because ours is a beat-by-beat model, we are
in fact, not looking at a time-series, but a beat-series, and so our frequencies
will correspond to
beg
instead of Hz, but a more detailed discussion of that
topic will be presented in a later section.
3.5. FREQUENCY DOMAIN BEHAVIOR OF THE ARX BAROREFLEX MODEL51
3.5.1
Parasympathetic Transfer Function
The transfer function of the parasympathetic nervous system described by
our model takes the form:
H~i~~
__P(e-iuk)
(3.13)
.(Qk)a0
H(e-k
BP(e-30k)
Because we model the parasympathetic system as a gain element, it acts as
an all-pass filter, with a flat magnitude across all frequencies as shown in Fig.
3.6. Changing the value of a 0 then only serves to increase or decrease the
magnitude of the spectral response. Consequently, there is not much value
in discussing the parasympathetic system's frequency-domain characteristics
until we have understood the sympathetic pathway's more complex behavior.
3.5.2
Sympathetic Transfer Function
The transfer function of the sympathetic nervous system described by our
model takes the form:
H's(CQk)
-S(e-jQk)
BP(e-ijk)
aie-jQk
1 -
Be-iQk
The magnitude of the transfer function can be seen for varying a 1 and
rameters in Fig. 3.7 and 3.8. Because for all Q, Ie-jQ
# pa-
= 1, the ai term in the
sympathetic transfer function acts similarly to a gain element. On the other
hand, the
#
parameter once again acts as a "shape" parameter-either boost-
ing low frequencies and attenuating higher frequencies for large 3 near 1, or
having a small boosting effect on low frequencies but causing relatively small
..................................
......
.
...
...
CHAPTER 3. MODELING THE BAROREFLEX
Parasympathetic Frequency Responses
0
0.05
0.
0.15
0.2
025
0,3
0.35
0.4
0.45
0.5
Frequency (I/beats)
Figure 3.6: Parasympathetic frequency responses for various values of ao
attenuation of higher frequencies for small 0 near zero. Therefore sweeping
through the range of physiological 13 from 0 to 1 trades high frequencies gain
for low frequency gain.
As a quick sanity check, let us explicitly derive the magnitude |H,(e-j')|:
aie-jQk
1
1 - Oe-3k
1 - /3(cos(Q) + j'sin(Q))
1 + 32 - 20 cos(Q)
(3.15)
It is interesting to further explore the concept of iso-G, curves in the
context of the frequency-domain, and we do so in Fig.
3.9. As expected,
3.5. FREQUENCY DOMAIN BEHAVIOR OF THE ARX BAROREFLEX MODEL53
all iso-gain transfer functions have the same value at Q = 0, but the story
does not end there. From our previous analysis, we see that, for a given
gain, G8 , increasing ) increases high-frequency attenuation. Intuitively, this
means that as the sympathetic pathway's "memory" increases (i.e. increase
in k ), it is less sensitive to high-frequency changes in input signal bpk. When
the system has a very short memory, characterized by a small
#,
higher
frequency components of the signal are passed with nearly no attenuation to
the output R-R interval, increasing R-R variability. Because R-R variability
is an important metric physiologists use to understand various pathologies,
examining G, as the sole metric for the state of the sympathetic pathway
should be insufficient!
3.5.3
Total Model Transfer Function
The total model transfer function H(e-iQ) is given as the additive sum of its
two constituent subsystem transfer functions:
ao + (a 1 - aoj)e-i(316
H(6~~)
±
H(e-j") = H,(e-jo) + H,(e-j") = '0+(,-a~-"(3.16)
1-
-
with corresponding magnitude:
|H(e-
)|
=V/as + (a 1 - ao3) 2 + 2ao(ai - ao3) cos(Q)
21±+3 2 -20 cos(Q)
While the transfer functions themselves add due to linearity, the magnitude of the frequency of response of the system certainly is not the sum of
the magnitude responses of the subsystems! Fig. 3.10, 3.11, and 3.12 show
CHAPTER 3. MODELING THE BAROREFLEX
Sympathetic Frequency Responses
0
005
0.1
0.15
0.2
025
0.3
0.35
04
045
0.5
Frequency (I/beats)
Figure 3.7: Sympathetic frequency responses for various values of #
this dissimilarity quite clearly.
Effect of ao on the system transfer function
From
(3.17), we can see that increasing ao increases the leading term of
the denominator, but has an unclear effect on the sinusoidal term, by simultaneously decreasing the ai - ao/3 term. For sufficiently large ao such
that ai < ao,
increasing ao stops the attenuation of high frequencies, as
can be seen in Fig.
3.10. This is a unique consequence of our model, but
nonetheless, corroborates the work by Guyton that shows that parasympa-
3.5. FREQUENCY DOMAIN BEHAVIOR OF THE ARX BAROREFLEX MODEL55
Sympathetic Frequency Responses
0
005
0.1
0.15
0.2
025
03
0.35
04
0.45
05
Frequency (1/beats)
Figure 3.8: Sympathetic frequency responses for various values of #
thetic control is the primary determinant of baroreflex control, and has a
strong inhibitory affect on sympathetic action [25]. Thus, in the case where
parasympathetic tone dominates, we would expect to see higher heart-rate
variability by both our model's and physiologists' predictions.
Effect of a 1 on the system transfer function
The effects of ai are not as complicated as those of ao. In fact, from both
(3.17) and Fig. 3.11 we see that increasing a 1 has a uniquely one-sided effect
- increasingly low frequencies and attenuating high frequencies. This means
.: .1 11
...
..............................
,
..........
CHAPTER 3. MODELING THE BAROREFLEX
Iso-G3 Frequency Responses
0
005
0.1
0.15
025
0.2
0.3
0.35
0.4
0.45
0.5
Frequency (I/beats)
Figure 3.9: Sympathetic frequency responses for constant G, - various values
of ai, #
that when examining the frequency response of the sympathetic pathway
alone, we were mislead into believing that a 1 had a similar effect as ao. When
the two components are added, ai acts like another "memory" element in
the MA sense, we are quickly disabused of this notion.
Effect of 3 on the system transfer function
Varying the value of 0 has perhaps the most interesting effect on the system's
frequency response. This is because
/3 appears
in both numerator and de-
3.5. FREQUENCY DOMAIN BEHAVIOR OF THE ARX BAROREFLEX MODEL57
nominator of the transfer function, and is multiplicatively coupled with both
a 1 and ao. Thus, the particular choice of ao and a 1 have a significant impact
on the role
# plays in
shaping the frequency response of the system. A spe-
cific example of this "strange" effect is shown in Fig. 3.12, where increasing
magnifies frequencies less than 0.27r, attenuates middle frequencies from
0.27r to about 0.87, but magnifies frequencies between 0.87 and -r relative to
#
smaller values of 0!
From this cursory examination of the time and frequency-domain characteristics of our model, it has become clear that not only is examining more
than just the gain values computed from our model important, but also understanding the effects of different events on the coefficients themselves is
key to understanding the changes they induce in the baroreflex.
CHAPTER 3. MODELING THE BAROREFLEX
Baroreceptor Model Frequency Responses
0.1
0.15
0.2
025
0.3
0.35
0.4
0.45
Frequency (1/beats)
Figure 3.10: Total model frequency responses for various values of ao
0.5
.
.....
..........
..
-
a
3.5. FREQUENCY DOMAIN BEHAVIOR OF THE ARX BAROREFLEX MODEL59
Baroreceptor Model Frequency Responses
10
I
I
I
I
I
I
4al
-
0.25a
100 -
so
50
0
0.05
0.1
0.15
02
025
0.3
0.35
0.4
0.45
Frequency (1/beats)
Figure 3.11: Total model frequency responses for various values of ai
0.5
-
I
60
CHAPTER 3. MODELING THE BAROREFLEX
Baroreceptor Model Frequency Responses
.C:
025
Frequency (1/beats)
Figure 3.12: Total model frequency responses for various values of
#
Chapter 4
Data and Their Analysis
Data are an important part of model validation and tuning. Because validating our model requires us to understand, a priori, the state of the baroreflex
before applying our model to it, it is vital to find data from which this information is readily available. Unfortunately, this is easier said than done,
as there is no "gold-standard" model of the baroreflex against which we are
testing ours' performance. Instead, we require the next best thing - data sets
with patients undergoing interventions that alter the balance between sympathetic and parasympathetic pathways in the body in known ways. Once
acquired, these data must be preprocessed and converted to beat-by-beat
time series, and these series must be examined in both time-domain and
frequency-domain.
CHAPTER 4. DATA AND THEIR ANALYSIS
4.1
Autonomic Blockade Data
4.1.1
Acquisition
The data used to test our model come from the work of Saul et al. and is
used with consent from the authors [46]. The data relevant to our work consists of arterial blood pressure recordings from a radial artery catheter and
surface ECG measurements sampled at 360 Hz. Subjects consisted of 14 nonsmoking adult male volunteers, ages 19-38. All subjects were first screened
for having any history of cardiopulmonary disease. Subjects were instructed
to breathe with respiratory intervals governed by a modified Poisson process
with mean 12 breaths/min so as to whiten the spectrum of their breathing.
Data were recorded in six 13 minute segments. Subjects data were recorded
first in the supine position, and then in the standing position, with time
allowed between readings for the physiology to equilibrate. Subjects were
then administered either the parasympathetic blocking drug atropine (0.03
mg/kg, n=7) or the sympathetic blocking drug propranolol (0.2 mg/kg, n
-
7) [32], and after equilibration, signal measurements were again taken.
Finally, the patients were all given the "other" drug, either propranolol for
patients previously administered atropine, and atropine for patients previously administered propranolol. After time was again given for equilibration,
measurements were taken again in both standing and supine positions. For
the purpose of this thesis, we restrict ourselves to examining only those data
where patients are in a control state, or have been administered only one
drug.
4.1. AUTONOMIC BLOCKADE DATA
4.1.2
Preprocessing
The data were converted from integer to floating point format using the
rdsamp algorithm provided by PhysioNet [23], and beat detection was performed using an open source peak detection algorithm on the ECG signal
[13]. Data is then sampled beat-by-beat for the R-R interval length, systolic,
diastolic, and mean blood pressures of that beat.
A note on beat-to-beat data sampling
We chose to index our data by beat in a series of point events, as described
by DeBoer [45]. Authors Luczag and Laurig (1973), Kobayashi and Musha
(1982), and Pomeranz et. al (1985) opt for this type of analysis [26] [35] [39].
Doing so, we are not forced to make any assumption on inter-beat length as
we would if we used the interval spectrum method proposed by Mohn (1976),
in which each beat is considered to be spaced equidistantly at time intervals
equal to the average heart-rate [44]. The implicit downside of using a beatto-beat discrete-time model is that we are limited in our ability to analyze
the frequency spectrum, as all events that happens within a beat have the
same spectral contribution. Further, because our sampling rate is so low, we
have much more information clustered at higher frequencies than would be
seen by continuous-time analysis, and we suffer from low spectral resolution
at lower frequencies as well.
CHAPTER 4. DATA AND THEIR ANALYSIS
4.1.3
Storage
After beat-by-beat sampling, each patient's R-R interval, systolic blood pressure, mean arterial blood pressure, and pulse pressure were stored in MATLAB matrices, indexed by the onset time of each beat. The patient data are
named according to how they were originally stored by the previous author,
and take the form CRC-XX- YY-Z (the delimiter "-" is used for demonstration and not included in the patient names). In the naming schema, XX is
a numeric string, taking values between 01 and 14, corresponding to the patient number. Accordingly, YY is an alphabetical string, here either ST or
SU, corresponding to standing and supine positions, respectively. The final
character, Z, is reserved for the intervention associated with the recording,
either C - control, A - atropine administered, P - propranolol administered,
and for completeness, B - both atropine and propranolol administered. From
here onwards we will use this notation and related shorthand to discuss patients.
4.2
Data Analysis
In the time-domain, the interventions had the expected effect on the patients' signals - atropine drastically decreased R-R and its variability, and increased blood pressure slightly, and propranolol increased R-R interval length
and decreased blood pressure very slightly. For this reason, we look to the
frequency-domain for more interesting changes.
4.2. DATA ANALYSIS
4.2.1
Frequency-Domain Analysis
We further wish to analyze the frequency-domain properties of our signals.
For this, we introduce a new concept, the power spectral density (PSD). The
PSD of a random process z, SX(e-ja), is given as the Fourier transform of
the autocorrelation, R~x[ti, t2], defined as:
R2x[t 1 , t 2 ] = E[xtl -
Sxx(e-jQ) =F (R22)
(4.1)
J2]
where E[-] is the probabilistic expectation operator. Further, if we assume
the first and second moments of our process Xk do not change over time (or
the time window that we are considering), then we call the process wide sense
stationary (WSS) and can write the autocorrelation as follows:
Rxx[k] = E[xt -
S.(e-30) = Y(R~x)
(4.2)
Xt+k]
We further define the cross-correlation of a two random processes Yk and Xk,
Syx (e~
), as the Fourier transform of the cross correlation, Ry., which, for
a WSS process, is defined as:
Ryx[k]
=
(4.3)
E[yt - Xt+k]
Assuming that Yk is produced by some filter h[k] applied to the process
Xk,
when that same filtering is applied to the autocorrelation of
Xk,
we can
show by linearity that:
h * Rx[k]
=
Ryx[k]
(4.4)
CHAPTER 4. DATA AND THEIR ANALYSIS
Switching to the frequency-domain, we show this as a way to determine the
transfer function H(e-j') from
Xk
to Yk by relating the input power spectrum
Sx to the cross-power spectral density (CPSD), Syx:
Syx(e-ja) = H(e-iQ)Sxx(e-jQ)
<-+ H(e-0)=
S"
(4.5)
S. (e-i")
Because we are dealing with deterministic signals, we in practice compute
the cross-spectral and power-spectral densities using a modified periodogram
method [40], whereby the signal is divided into 8-10 overlapping segments,
each with a 50% overlap. For each window of length N, we compute the
N-1
N-point discrete Fourier transform (DFT(x)
-
e
Xk -S
k
k
n=O
0,..., N - 1) of the segment, and compute the autocorrelation of each segment, i, as $2 (e-'a) = Xi - (X,)* and the cross-correlation as Sy, (e-j) =
Yj - (Xi)* (where X* is the complex-conjugate of X). We come to our final,
averaged periodogram estimate of the cross-correlation and autocorrelation
of our signals by taking the average over all segments i of the respective signals. Only after computing these averaged spectral density estimates do we
compute the transfer function estimate, H(e-3 )
Parasympathetic Blockade
For the following section, we will focus on only 3 patients undergoing parasympathetic blockade, and point out the salient features of their various waveforms in both time-domain and frequency-domain. We have chosen patients
02,07, and 11 because they best span the characteristics of parasympathetic
blockade. Because our main interest is understanding the relationship be-
67
4.2. DATA ANALYSIS
(a) CRC02ST
(b) CRC07ST
(c) CRC11ST
Figure 4.1: Blood pressure power spectral density of standing atropine patients
tween blood pressure, R-R interval, and the governing transfer function estimate between the two, we will examine the PSD of blood pressure, the R-R
interval blood pressure CPSD, and the estimated transfer function between
blood pressure and R-R interval.
Blood Pressure Power Spectrum
In the standing case, we see in Fig.
4.1 that the low frequency (lo-f) component of the blood pressure power
spectrum is slightly decreased in height and lobe width after administration
of atropine, but not noticeably. What is noticeable is that patients experience
mid-f attenuation with the exception of patient 02, but all have diminished
hi-f components.
In the supine case, shown in Fig.
4.2, patient 02 now exhibits a strong
mid-f attenuation as compared to the standing case, as does patient 11, but
patient 07 seems to actually have an increase in mid-f magnitude.
important to notice that the hi-f attenuation visible in Fig.
It is
4.1 is all but
gone now in the supine case. Because we take bpk as the exogenous input to
our open loop model, we will not further analyzed the effects of atropine on
the blood pressure signal.
68
CHAPTER 4. DATA AND THEIR ANALYSIS
(a) CRC02SU
(c) CRC11SU
(b) CRC07SU
Figure 4.2: Blood pressure power spectral density of supine atropine patients
R-R interval-Blood Pressure Cross Power Spectrum
A clearer
pattern emerges when analyzing the R-R-BP CPSD of the parasympathetic
blockade patients. In the standing case, Fig.
4.3, there is a marked drop
in mid-f CPSD of all three patients after atropine is administered, but lo-
f
and hi-f are relatively unchanged. This mid-f divergence is even more
pronounced in the supine case, Fig. 4.4, except, once again, in patient 07.
Barring patient 07, we can attribute this more noticeable drop in Figs. 4.4a
and 4.4c as compared to Figs. 4.3a and 4.3c to the diminished sympathetic
control in the supine position compensating less for the loss of parasympathetic control. There is also a slight narrowing and shrinking of the lo-f peaks
in both cases as well, and that is noticed in the decrease in R-R intervals
shown in the time-domain.
Estimated BP-RR Transfer Function
As shown in Figs. 4.5 and 4.6,
the control transfer function estimate appears quite noisy, with a complicated
shape that seems unique to each patient, as expected. It is troublesome,
however, that the shapes are so complex, as they do not seem well suited for
fitting with the types of transfer functions our model can generate. However,
4.2. DATA ANALYSIS
(b) CRC07ST
(a) CRC02ST
(c) CRC11ST
Figure 4.3: R-R - Blood pressure cross power spectral density of standing
atropine patients
77
(a) CRC02SU
(b) CRC07SU
(c) CRC11SU
Figure 4.4: R-R - Blood pressure cross power spectral density of supine
atropine patients
70
CHAPTER 4. DATA AND THEIR ANALYSIS
(a) CRC02ST
(b) CRC07ST
(c) CRC11ST
Figure 4.5: Estimated transfer function of standing atropine patients
(a) CRC02SU
(b) CRC07SU
(c) CRC11SU
Figure 4.6: Estimated transfer function of supine atropine patients
the transfer function estimates after atropine is administered appear far more
well behaved. In all cases, there is a sharp attenuation at all values in the
mid-f range, with a slight ripple emerging again in the hi-f band. In the
standing case, Fig.
4.5, there is also a pronounced lo-f peak that is not
present in the supine case. In all cases, it appears as though the atropine
hi-f ripple seems correlated to the bigger hi-f ripples in the control case.
Sympathetic Blockade
For the following section, we will focus on only 3 patients undergoing sympathetic blockade, and point out the salient features of their various waveforms
in both time-domain and frequency-domain. We have chosen patients 01,05,
and 14 because they best span the characteristics of sympathetic blockade.
For the same reasons as the parasympathetic case, we will examine the PSD
4.2. DATA ANALYSIS
(a) CRCO1ST
1
(b) CRC05ST
(c) CRC14ST
Figure 4.7: Blood pressure power spectral density of standing propranolol
patients
of blood pressure, the R-R interval blood pressure CPSD, and the estimated
transfer function between blood pressure and R-R interval.
Blood Pressure Power Spectrum
The blood pressure PSD is relatively
unchanged after administration of propranolol.
In most cases, there is a
widening of the lo-f band, and this is most noticeable in Fig.
4.8b. In
addition, if we examine Figs. 4.8b, 4.7b, and 4.7a, we do see an increase in
mid-f and hi-f components, though this change is neither systematic across
all patients, nor attributable to only standing or supine patients. For this
reason, it is quite challenging to distinguish between patients undergoing
sympathetic blockade, and control patients from BP spectra alone.
R-R interval-Blood Pressure Cross Power Spectrum
Much like the
blood pressure PSD, the R-R interval - blood pressure CPSD lacks the clear
delineation between control and intervention cases! The lo-f peak is slightly
wider after propranolol is administered, as can be seen in Figs.
4.9, and
4.10, but again the shape of the intervention CPSD follow that of the control
CPSD closely, and there are no categorical changes in the mid-f and hi-f of
72
CHAPTER 4. DATA AND THEIR ANALYSIS
(a) CRC01SU
(b) CRC05SU
(c) CRC14SU
Figure 4.8: Blood pressure power spectral density of supine propranolol patients
the signals after propranolol is administered. In fact, only patient 05 shows
any real change in CPSD after propranolol is administered, with an increase
in mid-f and high-f components. To determine whether this was simply a
sampling error in choosing these three patients, we perform the same test
on the remaining candidates, and noticed some cases mirroring the changes
noted for patient 05, but with no clear trend across the majority of patients.
One possible explanation of this dichotomy between patients within the propranolol group is that there is a stronger coupling between BP and RR after
propranolol is administered (as shown by an increase in mid-f components
of the cross spectrum) in those patients who have higher sympathetic tone
under normal circumstances. The administration of propranolol in these patients should then "free" the mid-f components of parasympathetic control
to couple BP and RR more strongly, as seen in Figs. 4.9b and 4.10b.
Estimated BP-RR Transfer Function
To round out the confusing and
somewhat idiosyncratic spectral "story" of the propranolol patients, Figs.
4.11 and 4.12 again show that the BP-R-R transfer functions of patients do
not change systematically after propranolol is administered. In Fig. 4.11c,
.
. ...............................................
. A,
4.2. DATA ANALYSIS
(a) CRC01ST
(b) CRC05ST
(c) CRC14ST
Figure 4.9: R-R - Blood pressure cross power spectral density of standing
propranolol patients
(a) CRCO1SU
(b) CRC05SU
(c) CRC14SU
Figure 4.10: R-R Blood pressure cross power spectral density of supine
propranolol patients
CHAPTER 4. DATA AND THEIR ANALYSIS
(a) CRC01ST
( ) CRC05ST
(c) CRC14ST
Figure 4.11: Estimated transfer function of standing propranolol patients
Estimated
Tramfe,
F-Im
POprarz"
Frequenc~y(1eatsi)
(a) CRC01SU
Frequency
(keats)
(b) CRC05SU
(theelt)
Frequeny
(c) CRC14SU
Figure 4.12: Estimated transfer function of supine propranolol patients
we see a rise in lo-f components, but that is only partially matched by the
change demonstrated in one other patient of our three, in Fig. 4.12b. The
only possibly discernible pattern is seen in supine patients, Fig. 4.12, where
hi-f components tend to rise after propranolol is administered. Admittedly,
because of the noisiness of these transfer functions, none of these patterns are
verifiable when examined across all patients. We then leave our analysis of
propranolol with the hope that sympathetic blockade will still prove amenable
to interpretation by our model, despite its seemingly unrecognizable effect
on the frequency-domain characteristics of our signals.
Chapter 5
Estimation of the One-Pole
Model Coefficients
Recall that our one-pole model of the baroreflex describes the R-R interval
as a linear function of past R-R interval lengths, and blood pressure values
according to the following recursion relationship:
rrk = a0 - bpk + (a 1 - ao/)bp.1 - 0 - rrk_1
(5.1)
We are now charged with the task of learning our model coefficients, and
so we must understand the nature of the estimation problem we are facing.
Because we are modeling a highly non-linear system, we expect that our
model is not consistent, that is, there is no one choice of a 0 , ai, and 3 for
which the above equality will hold for all time steps k. We explain this
error in our model as coming from one of two sources: modeling error in our
system, and measurement error in our signals, the latter we expect to be
76CHAPTER 5. ESTIMATION OF THE ONE-POLE MODEL COEFFICIENTS
much smaller than the former.
r'rk
= O - bpk + (a1 - ao3)bpkl
+
/
rrk1 +
(5.2)
71k
where we introduce an additional term for our residual error, j1
While
we would like to limit the assumptions we make on ij, we expect that our
modeling efforts and data processing have been rigorous enough to produce
errors that are uncorrelated in time. Given this notion of residual error, we
then must find a choice of our three coefficients that best satisfy an a priori
optimality criteria that in some ways aims to explain this error, r/.
5.1
Optimality Criteria for Estimation
Given a data set Y and a set of n estimators of Y,
{Yi, Y2, ... , Yn},
how do we
decide which Yi is the "best" estimator of Y? While statistical literature is
rich in describing optimality constraints based on concepts such as maximum
likelihood (ML), maximum entropy (MaxEnt), and maximum a posteriori
probability (MAP) which hinge on the statistical properties of rj, I refer the
reader to other texts to understand the motivation and theory behind these
[17] [42].
Instead, we view our problem in terms of optimization of cost
functions, as that lends to easier interpretation and less exposition, and save
the formulation of these problems into 'standard' optimization problems for
Appendix A. We begin by defining a cost function, J, of an estimator Y of
'We do not yet assume a distribution on r for reasons that become clear later.
5.1.
OPTIMALITY CRITERIA FOR ESTIMATION
data Y as a function of both data and estimator:
J = f(Y, Yi)
Since we are after a choice of
Z' which
(5.3)
in some ways best describes Y, we
require our cost function, J, to reflect some "error" in describing Y with Yi.
Further, let us assume that our candidate estimators Yi are themselves functions of other, exogenous variables {X1
2,.
. . , Xk}
-
g(X 1 , X 2 ,..
. , Xk).
We also restrict our search space of cost function to convex functions of
estimators because they afford us sufficient richness in shaping our error, and
can guarantee that any optimal solution we discover is globally optimal.
5.1.1
L 2 cost function
We define the L2-norm of a vector x as
||x||2
o. This we define the
=
Xi EX
42 cost function of our predictor as:
J2 (Y, Yi)= Y - $z||2
(5.4)
The L 2 -norm optimality criterion is often referred to as the Sum of Squares
(S.O.S.) error-examining the expression for the squared J2 error should
show this-and the estimator which minimizes this cost function is referred
to as the minimum mean squared error (MMSE) solution, YMMSE (in the
case that Y is a linear estimator, it can be further specified as YLMMSE)Further, if we restrict ourselves to examining linear estimators of a data
vector y with input vectors x (not unlike our model), that is our candidate
78 CHAPTER 5. ESTIMATION OF THE ONE-POLE MODEL COEFFICIENTS
estimators take the form,
Qi
(5.5)
= Ax,
with known, full-rank mixing matrix A, then we in fact have a unique optimal
solution ,s. We show this in two steps, first expanding J2 as:
-Y
2
y
-
Ax
122y-FyyAx
= XTAAXT
2xTAy
+ yT
2l
-
(5.6)
Then, differentiating this expression w.r.t. xi and setting the resulting expression equal to zero finds the optimal -2:
dx
+x(xT AT Axi-2xAT y-YY) -- AT Axi-2 ATYy =
-
si
(ATA)--AT y
(5.7)
This estimator is of particular importance because it can be solved efficiently, in polynomial time, for full rank A.
5.1.2
L1 cost function
If we change the L 2 -norm penalty on our residual to an L1 -norm penalty,
where the L1 -norm of a vector x is 1x1
=
S
Xb
xil our Ji cost function
EX
becomes:
Ji(Y, Y) =||Y - Y>lli
(5.8)
where the optimal Yi is often called the minimizer of the sum of absolute
errors (SAE).
Again, restricting ourselves to linear estimators Q,of data vector y which
take the form Axi for a known, full-rank A, the solution can be efficiently
5.1.
OPTIMALITY CRITERIA FOR ESTIMATION
found by solving a linear program (LP). The solution,
zSAE,
differs from
iLAMSE in two major ways (which can be empirically verified): the residual
vector (y - A.'SAE) generally has more zero elements than (y - ALMMSE),
while the latter penalizes large residuals much more harshly and thus, has,
on average, smaller values.
5.1.3
Loc cost function
The third cost function we will explore when determining estimators is the
ECx-norm criteria, where the Ec norm of a vector x is defined as
| x.r
=
arg maxI xi with corresponding cost function:
Joe(Y, fi)
=|Y
- yi| c,
(5.9)
The optimal cost-minimizing solution for this problem is often known as the
minimax solution (zminimax in the linear case), and for convex functions of
Xi (which the affine expression Axi necessarily is), we can solve this problem
using efficient semidefinite program (SDP) solvers [9].
It can be empirically shown that the residual error of the minimax solution
of our matrix equation tends to be bimodal, with modes spaced symmetrically
around zero at 8minimax = ||y -
Azminimaxr||.
An intuitive explanation for
this is that our criteria is agnostic towards residual values that are less than
the minimax error, but place an infinite penalty on residuals that are greater
than this minimax error.
80CHAPTER 5. ESTIMATION OF THE ONE-POLE MODEL COEFFICIENTS
5.2
The One-Pole Model of the Baroreflex as
a Regression
We first explore our baroreflex model as a regression of the time-series rrk
with input variables bpk, bpk_1, and rrk-l. The problem is now reformulated
as finding the best linear mixture of the three regressors of rrk, as:
rr-k
=ao - bpk + a* - bPk-1+13
-rrk_1
a* - a 1 -00
(5.10)
We make the distinction to use a* because decoupling our regression coefficients makes the problem more interpretable. We will still interpret our
coefficients ao, a1, and 1 by post-computing ai from estimated regression
coefficients.
For the following section, we will examine the results of estimation on
standing control data. The same analysis was performed on all patients/interventions, and can be found in Appendix B.
We will begin by defining metrics by which we will judge our methods.
Measures of Cost Function Performance
We are hoping to decide
which of the three cost functions is most appropriate for our estimation
problem. Our goal is to understand how the minimizing solution of one-cost
function fares when measured against other cost functions. In a sense, we are
trying to find out which cost function satisfies all other cost functions best.
To do this, we define a new term, rp(Lq), the residual ratio of the Cp-norm
cost of the Cq-norm minimizer:
5.2. THE ONE-POLE MODEL OF THE BAROREFLEX AS A REGRESSION81
rp(,1q)
-
fly
-
A_~pl
Iq
for p,q E {1,2,oo}
(5.11)
where .4 represents the optimal Cp-norm solution.
Measures of Residual Error "Whiteness" Implicit in our discussion
of cost functions and estimators is the notion that an optimal estimate for
our model parameters produces a residual error signal that is "white". Here
I will intuitively explain our notion of the whiteness of a random process.
If we assume that a process follows a certain statistical distribution, we can
call it "white" if knowing the value that the process takes at any time tells
us nothing more than its assumed statistical properties. That is to say, the
process at a time step k is only correlated with itself, and not with the
process at any other time. Mathematically, for our residual error vectors ,
this means that Ree[k], the autocorrelation function defined in the previous
chapter, should take the form o-,2[k], where oe is the standard deviation of
the process. This noise is called "white" because its power spectral density
(recall, the PSD is the Fourier transform of the autocorrelation) is flat, and
contains equal power in all frequencies (akin to white light). This constrains
our residuals to being zero-mean. But why is "whiteness" so important in
our model noise and estimation residual? Assume that the unknown noise
in our model is not white. Unless we have some intuition as to the spectral
characteristics of our noise, we would then unable to distinguish its coloring
from our process's, and so our estimates would seek to explain both signal
and noise (we would overfit to the noise). For our residual, the explanation
is simpler - given that we believe our noise to be white, any coloring in our
82CHAPTER 5. ESTIMATION OF THE ONE-POLE MODEL COEFFICIENTS
residual spectra indicates components of our signal that our estimates do not
explain, implying that our estimates and perhaps our model cannot describe
our signal completely.
Because we need to test these properties on real data, we must put our
hats on, meaning that we must switch our notion of autocorrelation and PSD
to estimates of the autocorrelation and PSD (and add "hats" to our signals
to denote this!). We do this simply by changing our expectation operator
of random process Xk, E[Xk], into the sample-mean operator on time-series
N-1
Xk,
E[x]
Xk
(we do not bother with the 'bias' of this estimator).
k=-O
Because we are now dealing with empirical estimates of our autocorrelation,
we should relax our 'zero-mean' and 'single-impulse autocorrelation' characterizations of whiteness to 'near-zero mean' and 'rapidly decaying autocorrelation'. Further, due to the stationarity assumption on our residuals, we can
say that our sample autocorrelation Ree[k] is bounded above by a monotonically decreasing in
|kl.
Therefore, we view the ratio
R, [1]
as a measure of
the non-whiteness of our residual, and use it as a second metric to analyze
our regression model. We call this metric the one-step error correlation,as
it is theoretically (and almost numerically) equivalent to the often referenced
correlation coefficient of the two signals, and so for the C-norm minimizing
solution, we call this value p(L,).
5.3
Regression on Standing Control Patients
The mean residual ratios across all standing control patients (Table B.1),
shows the asymmetry of the various cost functions. It is clear that minimiz-
5.3. REGRESSION ON STANDING CONTROL PATIENTS
83
ers of both L 1-norm and L2-norm cost functions perform comparably well
against each other. This is due to both cost functions placing a penalty
on all non-zero errors. On the other hand, the L,-norm solution performs
abysmally by the other two criteria's standards. The interesting asymmetry
demonstrated by this is that the L1-norm and L2-norm minimizing solutions
perform much worse against the L4-norm criterion than the L4-norm solution does against the Li-norm and L2-norm criteria. This is because they
place varying emphasis on the maximal residual error - with the L2-norm
placing a quadratic penalty against large norms forcing a smaller maximal
residual than the L 1 -norm's linear penalty.
This is already interesting, as this makes L4-norm minimization seem
to be more versatile than the other two, but we must further examine the
coloring of the residual. We present the one-step error correlation in Table
B.2. In most patients, the L2-norm and L-norm solutions have "whiter"
residuals (as measured by smaller absolute-value one-step correlations) than
the LC-norm, with the L2-norm performing the best on the whole. This
pattern of residual ratio and one-step error correlations is repeated in all
other patient groups, and so it is at this point that we decide that all further
explorations will be done using the least squares error criteria (42-norm).
Table 5.1: Mean residual ratio for standing control patients
Cost Fcn/Res.Rat.
r(L 2)
r(L1)
r(Lc)
L2
1.00
1.02
1.77
4L
1.04
1.39
1.00
1.46
2.34
1.00
EC
84CHAPTER 5. ESTIMATION OF THE ONE-POLE MODEL COEFFICIENTS
Table 5.2: One-step error correlation for standing control patients
Pat. No.
CRCO1STC
CRC02STC
CRC03STC
CRC04STC
CRC05STC
CRC06STC
CRC07STC
CRC08STC
CRC09STC
CRC1OSTC
CRC11STC
CRC12STC
CRC13STC
CR.C14STC
5.4
p(12 2) P(L1)
-0.02
0.26
0.20
0.01
0.02
-0.02
-0.16
0.28
0.57
0.36
0.41
0.22
0.29
0.22
-0.06
0.23
0.20
-0.08
0.06
-0.08
-0.22
0.26
0.56
0.37
0.41
0.23
0.29
0.23
p(Lx)
-0.06
0.65
0.10
-0.12
0.13
0.40
0.51
0.27
0.68
0.34
0.42
0.45
0.29
0.45
Motivation for and Setup of the Windowed LMMSE
So far, we have discovered that the LMMSE solution is very well suited for
our problem: it is guaranteed to have a single, globally optimal solution;
its solution can be found analytically in polynomial time; and we have just
shown that it performs well when measured against a variety of error criteria.
The next logical step is then to look "under the hood" and examine the
estimates and residuals produced by this method a bit more closely. We begin
our examination again with standing control patients, as they seem most
amenable (in terms of estimation residual) . The results of this experiment
are presented in Table 5.3. At a glance, our parameters are, by our definition,
5.4. MOTIVATION FOR AND SETUP OF THE WINDOWED LMAISE85
physiologically reasonable, with only one instance of a negative estimate of
a 1 . In addition, we note that our estimates of a 1 are small compared to ao,
hovering around 1. We will return to this fact later.
Because of the promising results from the standing propranolol case, we
shift our focus to the supine control data. Based on the results of Saul, et
al.
[46], we expect that the patients' sympathetic action will be muted as
compared to the standing patients. Since our estimates of a 1 are already so
small, and our estimates of 3 are relatively large, we would expect that the
change from standing to supine position will cause either a further reduction
in ai, but likely a reduction in the feedback gain 3. The results of this
experiment are summarized in Table 5.4. It is immediately apparent that
our estimates of ai are physiologically unreasonable. This is disheartening,
as we would expect the control data to be better suited for estimation than
the corresponding intervention data, and so if we are having such serious
issues already, then we can assume to have very little hope at identifying our
parameters on the more physiologically interesting/important intervention
data.
We then look to the final column of our tables, to see if they can shed
some light on this problem. Luckily, a pattern emerges. In cases where the
mean of the estimated a 1 is negative, it appears as though the residual error
of the estimation is higher than in cases where a1 is "reasonable." Perhaps
the estimated coefficients are unreasonable when the problem does not lend
itself to estimation as shown by a high mean squared-residual.
Without
delving deeper into this line of analysis, we propose an intuitive solution to
our problem and first examine its performance.
86CHAPTER 5. ESTIMATION OF THE ONE-POLE MODEL COEFFICIENTS
Table 5.3: Estimated coefficients and RMS residual error for standing control
patients
Pat. No.
CRCO1STC
CRC02STC
CRC03STC
CRC04STC
CRC05STC
CRC06STC
CRC07STC
CRC08STC
CRC09STC
CRC1OSTC
CRC11STC
CRC12STC
CRC13STC
CRC14STC
do
(mrnmg)
di (mmmg)
3.24
0.81
2.88
0.92
16.09
0.89
2.10
8.31
1.99
2.26
1.13
2.44
3.35
2.44
0.44
1.03
0.55
1.86
-1.08
1.61
1.08
0.68
0.95
0.99
0.91
0.56
0.86
0.56
i3
0.87
0.74
0.87
0.63
0.84
0.70
0.79
0.90
0.84
0.84
0.81
0.89
0.76
0.89
RMS(8) (ms)
20.63
31.06
17.45
31.97
78.61
52.54
37.84
23.79
16.89
20.14
13.46
21.06
35.24
21.06
5.4. MOTIVATION FOR AND SETUP OF THE WINDOWED LMMSE87
Table 5.4: Estimated coefficients and RMS residual error for supine control
patients
Pat. No.
CRC01SUC
CRC02SUC
CRC03SUC
CRC04SUC
CRC05SUC
CRC06SUC
CRC07SUC
CRC08SUC
CRC09SUC
CRC1OSUC
CRC11SUC
CRC12SUC
CRC13SUC
CRC14SUC
do (m
8.78
8.34
11.44
10.06
22.07
10.73
12.22
11.09
8.74
11.50
5.39
10.17
10.55
10.17
)
di (ms)
-0.07
-0.38
-0.43
-0.72
-3.43
-1.27
-1.52
0.33
0.06
-0.26
-0.00
-0.30
-0.47
-0.30
0.83
0.79
0.81
0.72
0.73
0.62
0.62
0.85
0.87
0.87
0.91
0.86
0.85
0.86
RMS(8) (ms)
28.57
55.28
34.73
52.36
96.43
72.50
75.20
22.12
27.24
33.37
25.97
41.25
45.32
41.25
88CHAPTER 5. ESTIMATION OF THE ONE-POLE MODEL COEFFICIENTS
5.5
Windowed Least Squares Regression
If the issue with our estimation is that our noise is colored or non-stationary,
then we should look to ways to get around this. In order to do this, we
must examine why we assumed our noise was stationary and white. It is
obvious that blood pressure and heart rate are time-varying signals whose
mean and variance are complex functions of an individual's state and thus
non-stationary.
We assumed well-behavedness (stationarity, etc.)
of our
signals/noise because our signals were measured in a controlled setting, and
over a short enough time window that no other slow-acting blood pressure
control mechanisms (RAAS, chemoreceptors, etc.) are significantly affecting
our system. In stating this, we are shedding light on a major problem - if we
employ this method on progressively longer signals, then these assumptions
should get progressively weaker, and thus, estimation should get progressively
worse. So then even if our estimates had been well behaved, we still should
have been explicit in our formulation of the estimation problem.The natural
progression of this idea then, is that we should limit the number of beats
over which we estimate our coefficients. We will call this stretch of data our
"window", and so dividing our data into segments of this length is windowing.
Let us begin with the simplest form of windowing - divide our data into M
non-overlapping windows of length N, and our estimated model coefficients
will be a piecewise-constant function with at most M - 1 changes. We are
guaranteed to do no worse if we window our data sample than if we did not (if
choosing one estimate is the optimal choice, than each window is guaranteed
to produce estimates equal to this value, due to the global optimality of the
LMMSE), so then the question is, does windowing perform better? If so, by
M.
....
.........
M
5.5. WINDOWED LEAST SQUARES REGRESSION
RMS
Ri l Nb
tl
W
s CRC1T
RC085
RMReso v.NubrWfD Winoe-C
RMS
ReFdal NuneroDatWi
sT
- CR11l
Figure 5.1: RMS residual error for (Clockwise from Top Left) CRC01STC,
CRC07SUC, CRC08SUP, CRC11STA
how much?
RMS residual errors as a function of number of windows for 4 patients
are shown in Fig.
5.1 . Since the number of samples per window is in-
versely related to the number of windows a signal is divided into, a natural
interpretation of these results is that, there is consistently a downward linear
trend in the RMS residual estimation error as coefficients are estimated from
progressively shorter windows. The next step is to further examine whether
our coefficients are reasonable, but before we concern ourselves with this,
we should understand the "costs" associated with lowering our residual. As
most tradeoffs are, at best, zero-sum, we expect that we are doing worse in
some aspect of estimation due to windowing. As it happens, that area is
numerical stability.
90CHAPTER 5. ESTIMATION OF THE ONE-POLE MODEL COEFFICIENTS
5.5.1
Numerical Stability
When we say numerical stability, we are really interested in the effect errors
in both our input matrix Ak and output matrix bk have on our final estimates
.24 (because we window our signal, our matrices A and b are now time-variant
and thus, indexed on their final beat index). Given an equation Ax = b, with
b being the sum of its true value b and a measurement error e, we write the
ratio of the relative "stretch" induced by the error, IA ell2 to the contribution
Ilie
112
of the total vector b (measured in the same way). Thus, the ratio is given
by:
j A-1e||2
|b| 2
| C |2
||A- 1 b\\ 2
We define the condition number t(A) to be the maximum of this of this ratio,
which is ||A- 1 |2 - ||A\\2 . We can avoid dealing with matrix norms by going
through the algebra to show that K(A) is related to the singular values of A
in the following way:
K(A) = oma(A)
0-min
(A)
In our application, this measure of the maximal effect of errors in our measurement vector will serve as our metric for numerical stability, with large
condition numbers implying a poorly conditioned system. We present the
effect windowing has on condition number in Fig. 5.2. The downward linear
trend in RMS residual error is mirrored by an equally notably upward linear
trend in the condition number as the data is subdivided into more windows.
This is not too concerning for our current estimation setup and data, but it
is conceivable that with stationary signals and increasingly noisy data, our
solution is increasingly vulnerable to measurement errors. While we do not
. ..
..
.....
5.6. REG ULARIZATION
M
F'
AM
0DmW
CC
S
erD-t Wino -- CACOSSU
RMS
Conio v.Num-
Figure 5.2: RMS condition numbers v. window length for (Clockwise from
Top Left) CRC01STC, CRC07SUC, CRC08SUP, CRC11STA
expect for A to ever be singular given N > 15
2, it
is all too possible that A
is near singular, and this is worrisome. To counteract this, we introduce the
concept of regularization.
5.6
Regularization
Regularization is the process by which additional information is introduced
when solving an ill-posed or numerically unstable inverse problem (like ours)
in order to find a solution or prevent overfitting to noise. We then write the
2
We have experimentally determined this as a safe lower bound on window size.
92CHAPTER 5. ESTIMATION OF THE ONE-POLE MODEL COEFFICIENTS
regularized minimization problem of the matrix equation Ax = b as:
minimize : ||Ax - b p + |f(x)q
where f(x) is an arbitrary function called the regularizationterm. We restrict
our discussion to affine regularization terms of the form Fx + A, and for simplicity, we set p, q = 2. Now this problem can be formulated as an LMMSE
problems, and has all of the desirable efficiency and solvability properties
that we have discussed previously.
For our problem, we have a prior belief that our estimates should remain
relatively constant between estimation windows. Large changes in coefficients
indicate a significant change in the body's physiology, and since these generally evolve slowly (at fastest, on the order of minutes), we penalize changes
in estimates between successive windows, as hF(xk
-
Xkl-i)2,
meaning our
final estimation is the solution to the following equation:
F
A
[ k=
(5.12)
FXk._1
b
Numerical Motivation for Regularization
The numerical issues of our
original formulation can be viewed as an issue with the singularity of the
pseudo-inverse of A, specifically with the term: (ATA)-
1.
If A is near-
singular, we expect that this inversion is numerically unstable. In our regularized formulation, the analog for this term becomes (ATA + FF)-1. Since
we should choose a non-singular F with sufficiently large eigenvalues to have
a true regularizing effect on the final solution, we are guaranteed to have a
5.6. REG ULARIZATION
numerically well posed inverse problem (we must actually choose a positivesemidefinite F for reasons that will soon become clear). The natural question
that arises then is, what effect does this have on our residual errors, conditioning, and solution of our problem? We present results for these questions
for patient CRC05STC in Fig. 5.3. These patterns are reflected in a similar
manner across all patient classes.
5.6.1
Numerical Conditioning
We see that there is a drastic change in the condition number of the minimization problem when switching from normal LMMSE (/-.) to regularized
LMMSE solutions (r,). In both cases, the variance of the condition number increases as window size decreases as shown by the distance between the
+/- o bands, moreso in the normal LMMSE setup. What is equally interesting is that, while the K, is considerably smaller than , for all window lengths,
its magnitude increases with window length, while r, decreases. Further, this
increase in K, seems extremely smooth. To explain this, we look at the effect
that regularization has on our singular values. Assuming that F takes the
take
form (I where I is the 3x3 identity matrix, the SVD of the matrix
the form:
ai2 + (2
ofi
(5.13)
And so for small singular values, the regularized singular values tend
to (2, meaning that, in a poorly conditioned matrix with
Umin
<< (2, the condition number
smaller than
amran.
/, tends to ~ ",
max
>> (2
and
which is considerably
In our case, for small windows, omax becomes increas-
94CHAPTER 5. ESTIMATION OF THE ONE-POLE MODEL COEFFICIENTS
ingly small, and so Kr tends to unit magnitude, and for large window size,
the condition number rises towards the unregularized case, with the above
regularizing effect slowing this convergence to a sub-linear growth rate. For
sufficiently large windows, I expect
Kr
-+ K, though I have yet to perform
this experimentation on real data. Because we are not explicitly plotting singular values and how they change with window size, this is only a plausible
explanation that I am proposing for further examination.
Residual Error The RMS residual errors between regularized and normal
LMMSE seems to behave similarly. Before this experiment, our fear was that
regularization would have a significant, negative effect on the 'goodness' of
our model's estimation, but as shown in Fig. 5.3, this does not seem to be
the case at all. It is interesting to note that the residual error is not a linear
function as we had seen in Fig. 5.1. This discrepancy is due to what exactly
the images are depicting. We could construct Fig. 5.1 by sampling Fig. 5.3
at the ends of each interval denoted by the dotted black lines.
Coefficients
Our assumption is that regularization is primarily a numerical
safeguard, and to allow us to separate changes in our estimates caused by
real changes in the data from those cause by poor numerics. As a result,
we should expect that the coefficients reflect these intentions. At a glance,
both regularized and standard LMMSE seem to converge to the same RMS
solutions for windows greater than around 30 beats, with the regularized
solution having smaller estimate variances. For window sizes between 15 and
30 beats, there seems to be a difference in the solution that the LMMSE
finds and the one that the regularized estimator finds. Because the variance
5.6. REG ULARIZATION
bands around the solutions extend to physiologically unreasonable values, we
will not explore this difference further, and claim that neither method finds
adequate solutions for windows of length less than 30.
5.6.2
Statistical Motivation for Regularization
We have briefly explained the numerical reasoning for why to regularize, but
we have not properly motivated how to choose our regularization parameters.
In this section, I will try and provide a basic understanding of the statistics
that describe these types of problems (and briefly, of the LMMSE solution).
Let us return to our time-varying matrix equation AkX
~ bk. Assuming that
bk was generated from an equation of that form, then our LMMSE solution
would, in fact, converge to the true value of z4. Since it does not, we must
introduce noise to our system, which now takes the form Akxk = bk + rik.
Assuming q is from independent, identically distributed draws from a zeromean Gaussian process with unknown variance or. Then we view finding the
optimal estimate of x as finding the Xk for which the residual (bk - Akxk)
is most likely to be from i.i.d. draws from the
N(0, o
) distribution. For
simplicity, if we take the log of the distribution function of i,, substituting
(bk - AkXk) in for q, our log-likelihohod maximization takes the form:
maximize:
1
-2
I|bk - Akxk
2
Discarding the multiplicative constant introduced by the variance, we have
the canonical LMMSE solution for
fits in to this picture
z_.Now I will explain how regularization
0 ......
...........
....
..
..............................
.
....................................
..........
.. ....
96CHAPTER 5. ESTIMATION OF THE ONE-POLE MODEL COEFFICIENTS
Mm C-11tion
N-ba V,
Window
Leng1h
RMS
Rsi
v.
flMS
Reskluel
Errv
v.Winkow
Lenglh
Errr WiNdW
Lingd
Pr
7
o'v Window
Length
v.Window
Leng_
Wndow
Length
o'Window
Lengh
.,
Window
L
h
indow
L.n
OWindow
Length
ndoL
Window
L-ng0
Figure 5.3: (Top to Bottom) RMS condition number, residual error, and
estimated coefficients v. window length (beats) for CRC05STC using (Left)
LMMSE and (Right) regularized LMMSE methods. RMS values are shown in
blue, with +/- o bands in red. The dotted black lines represents the number
of windows used in estimation, starting at the far right with 1 window, and
increasing by 1 window per line
5.6. REG ULARIZATION
Bayesian Underpinnings
Assume that our estimates x are sequential samples from the following random process:
Xk = Xk-1 + yk
where Yk is a random variable that corresponds to a physiological 'event' e.g. standing from a supine position, exercise, valsalva maneuver, excitement.
We call -y a random variable and not a deterministic input because from our
perspective of looking only at the time-series bp and rr, we cannot know
what a subject is doing. Even if we know what the individual is doing, we
have no idea of how that should affect our coefficients. For this reason, we
introduce events as a random variable -y.
Further, we expect that a person is almost constantly experiencing these
events, but they are generally small in nature, such as eating food, or laughing at the television, so as to have minimal effect on the state of the baroreflex
gains. We do not, however, rule out the possibility that in very rare instances,
there could be events that trigger an extreme change in the physiology. For
this reason, we model our 'y as being i.i.d samples from a multivariate Gaussian distribution, AN(0, Z4). It is not altogether obvious that these samples
are i.i.d., but I make the weak argument that we have no better understanding of this mechanism, and are subsequently forced to assume this for
simplicity.
We now realize that, knowing our previous estimate Xk1, we have a prior
distribution on our current coefficient,
<r(Xk; Xk -
1), that allows us to switch
from ML estimation to MAP estimation, where the a posteriori probability
98CHAPTER 5. ESTIMATION OF THE ONE-POLE MODEL COEFFICIENTS
we are maximizing is:
;7xk-_1)
Pr (xxk
--
Pr('qkXk; Xk_1) .,w(xk; Xk_1)
r(7k
Pr(lk)
Again, taking the log-likelihood and disregarding the denominator, we
find that the maximizing the following quadratic form:
-
-1/
2
(bk - Akxk) |
-
which leads to solving the system in
- 1 / 2 (Xk - Xk_1)||1
(5.14)
(5.12). Note that if we are using a
statistical argument, we must explicitly state our assumptions on the form
of E, and E,, as opposed to in the standard LMMSE setup.
Regularization Parameter Choice
Through experimentation, it was found that a good structure for our regularization matrix F was diag(100, 100, 1000). This choice gave us a good
tradeoff between residual error and estimate smoothness. To better understand why these numbers work so well, a more obvious interpretation appeals
to the statistical arguments presented above.
Statistical Interpretation Because of our i.i.d assumptions on our noise,
we write their covariance matrices as:
Ell = diag(a , o , ... o12)
E2
diag(or, 1
27)
(5.15)
(5.15)
5.6. REGULARIZATION
From Tables 5.3 and 5.4, we see that the standard least squares solution has
an RMS residual error of around 20-30ms. Since we have already discussed
that the residual in the standard LS setup is, in fact, a direct ML estimate
of r/, we then have an idea of the upper bound of o.,
which we set at 50
ms. For our estimate variance values, we must make a few educated guesses.
Because ao and ai generally fall in the range (0, 15) and we would like to
think they have the same order of magnitude, we set their variances equal.
We guess that their standard deviation is around 3%-5%of their magnitude,
and so a safe guess is
, ,1 = o2 =0.5
. We make the same guess for
,3, but noting that its estimated value is usually one order of magnitude less
than those of the a's, we guess o,3= 0.05. We relate these values back to
the regularization matrix as:
F = oq -diag(
1
1
2
7,1
'7 ,2
1
2 )
'7y,3
= diag(100, 100, 1000)
Long-Tailed Distributions and the L1 penalty
If we return to the assumption we made on the distribution of -Y, we can
change -y to have a long tailed distribution. This will allow for larger onestep changes in our parameters.
If we specifically chose a Laplace prior
distribution, we would change the maximization problem to:
-||q
1
/
2
(bk - Akxk)
2 -|E--
1 2
/ (X
-
Xk-l)f
This would change our problem to the much talked about C1 norm regularized problem, which would be a hybridized cross between the LASSO
model selector and total variation signal reconstruction (TVR) [51] [10] [11].
100CHAPTER 5. ESTIMATION OF THE ONE-POLE MODEL COEFFICIENTS
The problem remains a convex optimization problem with the same globaloptimality of the LMMSE, but now becomes a quadratically constrained
quadratic program (QCQP). The main benefit to using this noise model is
that it expects that successive estimates will often remain constant, but that
large changes are penalized less strongly 3. In some sense, this may afford us
a more accurate description of our model, although the increased computational complexity seems excessive for whatever benefit we might hope to see.
Without any further discussion, I leave it to future work to assess the merits
of this method.
5.7
Further Consideration for On-line Estimation Algorithm
The first issue I have avoiding discussing is choosing an initial x0 . Because
we would like to start with the "best" possible x0 , we can perform standard
LMMSE on the first window, and then estimate forward using regularized
LMMSE.
5.7.1
Sliding Window Regression for Improved TimeDomain 'Resolution'
Originally when we introduce the idea of windowed regression, we allow for
no overlap between successive windows. We also assumed changes in the sympathetic and parasympathetic gains, and thus our model coefficients, occurs
3
They are penalized absolutely instead of quadratically.
5.8. SPECTRAL ESTIMATION: A BRIEF DISCUSSION
101
slowly and over the course of a few windows. In our no-overlap formulation,
this would be discovered as a series of step changes, and we would not have
the ability to watch the evolution of these changes. Further, if we introduce
a regularization term that penalizes changes in successive estimates, might
have other strange behavior in our estimates as they are now minimizing two
potentially opposing criteria.
Since we had no real reason in imposing the no-overlap condition, we
reverse it in favor of overlap. In fact, there is no reason why we should not
employ maximal overlap (N - 1 beat overlap for an N beat windows). This
is essentially a modified version of the popular on-line estimation scheme,
recursive least squares (RLS), which is itself a simple form of the Kalman
filter
[29].
Because these are such well studied topics, we will not discuss
the merits of switching to this formulation, save for the fact that it should
improve our ability to track changes that evolve over time. Further, our
regularization term seems more appropriate for this formulation, as we do
expect very small changes in successive estimates on a beat-to-beat time
scale.
5.8
Spectral Estimation: A Brief Discussion
As another method to overcome the difficulty posed by the poor numerics of
the input time-series rrk and bpk, we develop a frequency-domain identification scheme. We write the discrete-time transfer function of (3.17) as:
H(d Q)
Srrbp(e)
Sbp,b (ej")
-- ao + (ai - ao3)e
1 - f3e-i(516
(5.16)
102CHAPTER 5. ESTIMATION OF THE ONE-POLE MODEL COEFFICIENTS
where the power spectra Srr,jp(ej") and Sb,,b,(ej') are defined as in (4.1).
The method by which these spectra are computed for our data takes a bit
of care-as we should employ methods such as periodogram averaging and
Welch's method to tame the noisiness of that plague FFT spectral estimates
[38].
Assuming for the moment that the spectra are correctly estimated, using
our knowledge of the "peakedness" of the energy spectrum, we can sample
the transfer function at N specifically chosen frequencies, and construct the
following system of equations, which can be solved, again, by a standard
LMMSE approach.
1
e-j01
H(eiQl)e-ij
1
e6 P2
H(eij2)-jQ2
H(einN)e -jN
H(eiQl)
H(e2)
1
ai -
1 e-ijN
1
-
ao
=)(5.17)
_
H(e3 N)
This method is somewhat similar to a weighted principal component analysis method discussed by Xiao et al. [54], and while its derivation is quite
simple, the optimal frequency subsampling might be a much harder problem
to tackle. To truly examine the pros and cons of this method, we would have
to dedicate a great deal of time and analysis to understand how specific spectral estimation setups effect our coefficient estimates, and derive optimality
criteria to choose a suitable method. For this reason, I will not continue
with this estimation scheme. I will, however, mention that preliminary estimation trials with this method produced physiologically reasonable, stable
estimates without any regularization or complex power spectrum estimation
5.9. FINAL THOUGHTS ON ESTIMATION
103
techniques.
5.9
Final Thoughts on Estimation
The discussion presented in the above chapter is by no means the final word
on estimation parameters from physiological models. In truth, I intended it
to be demonstrative of the issues, both mathematical and numerical, that
plague system identification and model parameters identification.
In this
work, I had the benefit of being presented a model, and thus only facing an
estimation problem. Had I not been in such a fortunate position, I would
have first needed to attempt model order identification, another equally if
not more challenging issue to navigate. The upside of tackling the problem
first as a model order identification problem, and then an estimation problem
for the chosen model order, is that perhaps we would have found an equally
estimable but more accurate model of the forward loop of the baroreflex.
But given the circumstances, I have attempted to lay out an argument in
this chapter for the use of simple, intuitive modeling as a viable method to
approach modeling the baroreflex.
104 CHAPTER 5. ESTIMATION OF THE ONE-POLE MODEL COEFFICIENTS
Chapter 6
Preliminary Results
We have so far been very carefully developing a model and estimation scheme
to explain the arterial baroreflex. Now we are faced with testing our methods
against the patient data that we so painstakingly analyzed in Chapter 2.
As was mentioned in the previous chapter, we must make it clear that our
estimates are reasonable and worth analyzing.
6.1
Effects of Regularization on Estimates
Using a variant of the regularized estimation setup', we examine supine control patients again to see if our estimation produces physiologically reasonable estimates. Because we are using maximal overlap between successive
windows, our RMS error is in fact, the mean RMS error across all windows.
For comparison, we present the standard LMMSE coefficients and RMS error
again, this time using maximal overlap as well. The results for the regularas max(zk-1,0) to try and enforce- in a 'soft-constraint' sense -nonnegativity of our coefficients.
'We update Xk
105
106
CHAPTER 6. PRELIMINARY RESULTS
ized setup are shown in Table 6.1, and for comparison, the standard LMMSE
results are presented in Table 6.2. As expected, our regularized estimates
result in higher RMS errors, but the increase is at most 7 ms! On the other
hand, we see that the estimates from our regularized setup are all physiologically reasonable, as opposed to the standard LMMSE solution which results
in ai near or below zero. We also note a systematic decrease in the magnitude
of ao and 0 when regularizing our estimates. it is altogether possible that
without regularization, our estimation overvalues ao. Stated in another way,
if we try and estimate parasympathetic and sympathetic contributions independently at each window without examining their previous state, we consistently overestimate parasympathetic control. We demonstrate this principle
by examining the percentage sympathetic response (PSR). Recall that the
PSR is the ratio of the sympathetic DC gain to the total system DC gain,
PSR =
a1/(1 - 0)
a o + a1/(1 - 3)
Here, we are forced to use the absolute value of ai in defining the PSR, as
the PSR of the standard LMMSE estimates would have a nonsensical meaning otherwise (recall that this was the basis for us pursuing regularization
techniques). The results of this experiment are shown in Table 6.3. It is
then apparent that without regularization, ao subsumes a disproportionately
large amount of the baroreflex we are aiming to capture, and accounting for
the temporal continuity of our estimates via regularization increases the importance we place on the long-tailed sympathetic control mechanism. We
then see if this pattern is consistent across all patient classes.
6.1. EFFECTS OF REGULARIZATION ON ESTIMATES
107
Table 6.1: Regularized mean coefficients and RMS error for supine control
patients
Pat. No.
CRCO1SUC
CRC02SUC
CRC03SUC
CRC04SUC
CRC05SUC
CRC06SUC
CRC07SUC
CRC08SUC
CRC09SUC
CRC10SUC
CRC11SUC
CRC12SUC
CRC13SUC
CRC14SUC
6.1.1
6o
diZg
lg
2.83
3.57
4.12
3.85
6.73
4.04
4.59
6.58
4.42
4.24
1.53
3.17
3.08
3.17
1.83
1.48
2.14
1.64
1.84
1.61
1.83
3.23
2.19
2.28
1.02
1.81
1.75
1.81
#
RMS(a) (ms)
0.67
0.47
0.55
0.50
0.33
0.48
0.47
0.51
0.53
0.56
0.72
0.61
0.60
0.61
29.00
51.37
33.86
44.78
98.93
68.50
62.40
21.73
28.54
34.14
24.02
40.24
45.81
40.24
Regularization and PSR Across All Patient Classes
Because of the interesting results obtained by examining the PSR of supine
control patients, we wish to see if these types of changes occur in all patient
classes. Results for supine patients is presented in Table 6.4, and for standing
patients, in Table 6.5. It is clear that supine control patients were exceptional
in that the effect of regularization was so noticeable on their estimates. This
change is certainly not seen in the standing control case, or in either atropine
cases.
The only other class of patient where we do see such a dramatic
effect from regularization is in the patients administered propranolol. But in
these patients, the change we see is perhaps not the change we had hoped
for. Propranolol you will recall, is a sympathetic blocker, and so the fact
108
CHAPTER 6. PRELIMINARY RESULTS
Table 6.2: Standard LMMSE mean coefficients and RMS error for supine
control patients
Pat. No.
CRCO1SUC
CRC02SUC
CRC03SUC
CRC04SUC
CRC05SUC
CRC06SUC
CRC07SUC
CRC08SUC
CRC09SUC
CRC10SUC
CRCiSUC
CRC12SUC
CRC13SUC
CRC14SUC
do
8.38
7.70
9.70
9.26
21.33
11.13
10.65
12.25
8.26
10.63
5.94
10.05
9.25
10.05
g1
di,
0.09
0.30
-0.11
-0.35
-4.39
-1.71
-0.96
0.42
0.27
-0.11
0.03
-0.43
-0.01
-0.43
/3
RMS( ) (ms)
0.75
0.62
0.69
0.71
0.62
0.55
0.66
0.76
0.75
0.76
0.85
0.70
0.77
0.70
26.97
48.20
32.52
41.30
91.90
64.41
57.54
17.70
25.48
30.56
21.89
37.72
43.66
37.72
that regularization increases the PSR of patients given propranolol from the
standard LMMSE solution seems odd. If we only look down the regularized
column though, we do in fact see a drop in PSR from the control case, and so
we are still capturing the effect of the drug, albeit less noticeably. We again
see that the effect of the exponential decay of the sympathetic response has
a greater total effect than we would have found otherwise. It is also nice that
the PSR increases when atropine is administered, and the effects of both
propranolol and atropine are stronger in the standing position, in agreement
with what Saul et al. noted as increased sympathetic action in the standing
position. Thus, we can conclude that our model does in fact properly capture
the physiological changes of the various drug interventions.
109
6.2. ESTIMATE TIME-SERIES
Table 6.3: PSR for supine control patients
Pat. No.
CRCO1SUC
CRC02SUC
CRC03SUC
CRC04SUC
CRC05SUC
CRC06SUC
CRC07SUC
CRC08SUC
CRC09SUC
CRC1OSUC
CRC11SUC
CRC12SUC
CRC13SUC
CRC14SUC
Mean
6.2
Standard LMMSE PSR
0.21
0.28
0.16
0.22
0.34
0.22
0.19
0.20
0.15
0.16
0.12
0.26
0.27
0.26
0.22
Regularized LMMSE PSR
0.66
0.46
0.55
0.49
0.31
0.45
0.45
0.51
0.52
0.55
0.71
0.61
0.59
0.61
0.54
Estimate Time-Series
Now that we are comfortable that our estimation is producing meaningful
results, we can examine the estimates more carefully. While we could do
this by simulating BP and RR time series, we save that for future work
and instead focus on interpreting real data. An example of the estimated
coefficient time-series is presented in Fig. 6.1. We then ask whether or not
the smoothness we have imposed is artificial, or if coefficients indeed remain
stable over long stretches of time. To test this, we perform the following
experiment: estimate coefficients over the first 100 heart beats and compute
their mean values.
Freeze these mean values, and compute the one-step
prediction error using these frozen coefficients over the remaining time series.
110
CHAPTER 6. PRELIMINARY RESULTS
Table 6.4: PSR for supine patients
Pat. No.
CRCO1SUC
CRC02SUC
CRC03SUC
CRC04SUC
CRC05SUC
CRC06SUC
CRC07SUC
CRC08SUC
CRC09SUC
CRC1OSUC
CRC11SUC
CRC12SUC
CRC13SUC
CRC14SUC
Mean
CRC02SUA
CRC04SUA
CRC06SUA
CRC07SUA
CRC09SUA
CRC11SUA
CRC13SUA
Mean
CRCO1SUP
CRC03SUP
CRC05SUP
CRC08SUP
CRC10SUP
CRC12SUP
CRC14SUP
Mean
Standard LMMSE PSR
0.21
0.27
0.16
0.22
0.34
0.22
0.19
0.20
0.16
0.16
0.25
0.30
0.28
0.30
0.23
0.80
0.88
0.82
0.50
0.93
0.92
0.92
0.82
0.23
0.24
0.39
0.17
0.18
0.32
0.32
0.27
Regularized LMMSE PSR
0.66
0.46
0.55
0.49
0.31
0.45
0.45
0.51
0.52
0.55
0.71
0.61
0.59
0.61
0.53
0.55
0.90
0.97
0.61
0.90
0.92
0.93
0.83
0.37
0.54
0.17
0.42
0.48
0.49
0.48
0.42
111
6.2. ESTIMATE TIME-SERIES
Table 6.5: PSR for standing patients
Pat. No.
CRCO1STC
CRC02STC
CRC03STC
CRC04STC
CRC05STC
CRC06STC
CRC07STC
CRC08STC
CRC09STC
CRC1OSTC
CRC11STC
CRC12STC
CRC13STC
CRC14STC
Mean
CRC02STA
CRC04STA
CRC06STA
CRC07STA
CRC09STA
CRC11STA
CRC13STA
Mean
CRCO1STP
CRC03STP
CRC05STP
CRC08STP
CRC1OSTP
CRC12STP
CRC14STP
Mean
Standard LMMSE PSR
0.60
0.85
0.68
0.83
0.28
0.71
0.76
0.47
0.79
0.76
0.81
0.65
0.65
0.65
0.68
0.96
0.91
0.97
0.95
0.95
0.96
0.92
0.95
0.34
0.46
0.27
0.37
0.70
0.54
0.47
0.45
Regularized LMMSE PSR
0.75
0.74
0.71
0.61
0.50
0.69
0.71
0.68
0.76
0.76
0.75
0.80
0.63
0.80
0.71
0.97
0.97
0.99
0.99
0.98
0.98
0.98
0.98
0.59
0.67
0.36
0.59
0.74
0.73
0.73
0.63
.
..........
..
................
.
.....
..................................
CHAPTER 6. PRELIMINARY RESULTS
112
00
0
so
--
j
I
5
0
3200
300
30
400
450
Soo
250
300
350
400
450
S00
250
330
350
400
4150
500
0
1
0
so
100
150
1030
13
00
006
0
0
0
Figure 6.1: Estimated coefficient magnitude v. time (beats)
If the coefficients are indeed stable, then this error should remain small. On
the whole, we found that this was indeed the case. One particular example
of this can be seen in Fig. 6.2.
6.3
Examination of Predicted Transfer Function
We would like to return to the line of frequency domain analysis we introduced in Chapter 2. It is not of particular interest to compare our model's
implied transfer function to the empirical data transfer function as we have
already shown that ours will be insufficient at capturing the empirical form.
...
...........
.
....
.......
......
_-..... ....
..
................
....
.......
-
..
.......
...
I-..
- ..................
I'll,
..............................
...........................
..................
..
....
....
6.3. EXAMINATION OF PREDICTED TRANSFER FUNCTION
113
00
1500 -00
400'
0
100
200
300
400
600
Beats(ms)
Figure 6.2: Prediction error test. End of estimation/start of prediction denoted by dotted black line
Instead, we look to a way to compare changes in our transfer functions across
patient classes. We must then define a class transferfunction. Since we are
only interested in the shape of the transfer function, we can normalize our
coefficients such that we have unit parasympathetic gain (dividing a 1 and
ao by ao achieves this). Now that the gains are normalized, we can take the
mean of the coefficients for each patients in a particular class as the class
estimates, and estimate our transfer function from that. We present the class
transferfunctions for supine and standing patients in Fig. 6.3. The effects
of the various interventions are consistent between standing and supine positions. Administration of atropine consistently attenuates high frequencies
and amplifies low frequencies. Propranolol has a similar effect, but to a less
extent than atropine. In the standing case, the transfer function gains in-
114
CHAPTER 6. PRELIMINARY RESULTS
crease across all patient classes, with the DC gains being noticeably higher.
High frequencies are experience a much stronger attenuation in all standing
cases as well.
6.4
Concluding Remarks
While we have shown that our estimated coefficients do indeed track the
physiological changes induced by autonomic blockade drugs, we have carefully avoided asking the obvious question - so what? If we were to examine the heart-rate signal and its variability, we would see similar systematic
changes during the drug interventions. Over the course of experimentation,
I have performed many more tests on simulated and real data than I have
presented here, but none provide any more information and so are not worth
presenting. Unfortunately, because the R-R signal itself was such a good
measure of sympathetic and parasympathetic balance in these patients, we
can only use these signals for calibration and first-level testing of our model
- which we have shown here. I will address the need for different data sets
and testing methods in the following chapter.
115
6.4. CONCLUDING REMARKS
Frequency Response for Supine Patient
-
0
0F5
1
5
2
Control
Atropine
Propranolol
25
Frequency (2xubeats)
Frequency (2n/beats)
Figure 6.3: Class transferfunctions for (Top) supine and (Bottom) standing
patients
116
CHAPTER 6. PRELIMINARY RESULTS
Chapter 7
Conclusion
I hope that by now you have understood our motivation for pursuing this
research. I will begin this chapter with a few words on the content of this
thesis, followed by a discussion of the future of this research, and I will
conclude with some final thoughts on the process and value of writing this
document.
7.1
A Retrospective on the Thesis
We began this thesis with one, clear goal: to model the blood pressure
heart rate pathway of the arterial baroreflex in humans using a parsimonious
beat-to-beat model, with a clear physiological interpretation for our model
coefficients.
Ch. 1 In Chapter 1, we present an overview of the baroreflex, from both
physiological and quantitative modeling perspectives. The physiological re117
118
CHAPTER 7. CONCLUSION
search on baroreflex is rich and complex, with studies focusing on the. action
of the baroreflex, as well as the the neurological and neuroendocrinological
components of the baroreflex. From these, we conclude that the fast-acting
parasympathetic nervous system is the dominant effector in the baroreflex,
depressing the heart rate via direct innervation, as well as inhibiting the
longer-lasting sympathetic control. We then shift our focus to the modeling of the baroreflex. The bulk of the work done on modeling the baroreflex has been done in continuous time. Additionally, the focus has been on
non-parametric examination of the baroreflex, computing empirical transfer
functions, coherence moduli, etc. While the results of these studies have
diminished importance to us because we are not considering the baroreflex
with a continuous time model, we nonetheless take from them the idea of
examining the non-parametric frequency-domain components of our system
as a tool for understanding the baroreflex. We then discuss some attempts to
model the baroreflex, and particularly emphasize attempts to model it with
discrete time, beat-to-beat models.
Ch. 2
In Chapter 2, we begin with a statement physiological assumptions
drawn from Chapter 1 that we will use in deriving our model. Starting
with these assumptions, we derive both sympathetic and parasympathetic
subcomponents independently, and then merge the two pathways to come to
our final, one-pole model of the baroreflex. From here, we present some of
the time-domain and frequency-domain
1
characteristics that our model is
capable of exhibiting. This is done mainly to show that our simple model is
'frequency in the
bet
sense
7.1. A RETROSPECTIVE ON THE THESIS
119
still capable of producing a wide range of behaviors in the time and frequency
domain.
Ch. 3
In Chapter 3, we introduce the data set we are hoping to use for
testing and model verification. We use the autonomic blockade data from
Saul et al. [46], and so we recap the methods they employ for acquiring
and preprocessing the data. We then discuss how we convert our data from
"continuous" time (sampled at 360 Hz) to beat-to-beat time (sampled every
heart beat), and engage in a brief discussion of the pros and cons of our chosen
representation of time. Finally, we return to the non-parametric methods
introduced in Ch. 1, and analyze our data's blood pressure power spectrum,
heart rate - blood pressure cross spectrum, and the empirical blood pressure
- heart rate transfer function. We conclude Ch. 3 with a discussion of the
potential problems we may encounter using our model, given the empirical
spectra and the model's achievable spectra presented in Ch 2.
Ch. 4 In Chapter 4, we present a broad overview of estimation as it pertains to our model. We choose to approach the problem first by discussing
some of the various error minimization criteria we can use to serve our purposes without getting bogged down in the implied statistical properties of
each. Instead, we move straight to testing the performance of these various criteria, and decide on the standard least squares criteria (LMMSE) for
our minimization. We then introduce the concept of residual 'whiteness',
and use this as motivation for windowed least squares (WLS). Once the windowed algorithm is sufficiently motivated, described, and tested, we discuss
the numerical issues that it faces. As a solution, we introduce regularization.
120
CHAPTER 7. CONCLUSION
While regularization first appears as a numerical conditioning method, we
quickly move to its statistical interpretation in an effort to understand why it
works so well. Our focus is on C2-norm regularization, and so we reformulate
our problem as a regularizedwindowed least squares (RegWLS) problem, and
compare and contrast it to the LMMSE solution. We finish our discussion of
RegWLS with the concept of overlapping windows as a method to increase
time-domain resolution of our estimates, and arrive on our final estimation
algorithm. As a parting 'teaser', we discuss another class of least squares estimates - frequency domain parameter estimation - as a viable alternative
worth further study.
Ch. 5
In Chapter 5, we show more extensive tests on the RegWLS method,
demonstrating that it does, in fact, perform more reliably and produce more
meaningful results than the WLS method 2 . We also make note that the
changes in our model coefficients do indeed reflect the changes in the underlying physiology that we had hoped to see under the various autonomic
interventions. We also acknowledge that using the WLS method alone, we
were prone to overestimating the parasympathetic contribution to heart-rate,
and that regularizing our estimates attributed a larger portion of the heart
rate to the long-tailed sympathetic control. We then the examine the changes
to the model transfer function caused by the various drug interventions, for
completeness. Because of the nature of our data, we cannot draw many more
conclusions or results, and so we leave this section somewhat unfulfilled.
2
both now with overlapping windows
121
7.2. TOPICS FOR FUTURE WORK
7.2
Topics for Future Work
Because of the inconclusive nature of our study, I feel that there are many
opportunities to improve on this research. Specifically, I feel that these tasks
can be broken into two separate areas of focus -
7.2.1
modeling and testing.
Modeling
Model Order Selection
Our work began with an idea, which quickly
became a model, and then an estimation problem. Unfortunately, the estimation problem took the better part of a year to work through, but has
yielded many new techniques and methods to pursue. One important future
step would be to return to square one -
the model. Using the tools and
analysis metrics we have developed, we should examine various order MA,
AR, and ARMA models. Because we chose our model with the goal of parsimony , we should examine what the ultimate cost of that parsimony is.
Perhaps there is an optimal parsimony-performance tradeoff, and we owe it
to ourselves to see if this is the case.
Setpoint Determination and Linearization We had initially claimed
that we were 'linearizing' our model around setpoints BP and RR, but then
quickly mentioned that, for our work, we assumed we had zero-valued setpoints. This was as much to produce meaningful coefficients as it was because
proper setpoint determination was intractable given our time constraints.
We had not, and still have not, determined a proper method to linearize our
model, and so, as it stands, the strong performance of our estimation setup
and model are quite shocking. That said, a bit of time should be devoted to
122
CHAPTER 7. CONCLUSION
understanding why this is the case. One thought is that we are approaching
the task of 'linearization' foolishly. DeBoer et al. linearize their model by
passing BP and R-R through a non-linear filtering [16], and nearly all of
the non-parametric models relied on first low-pass filtering their data before
analysis.
Perhaps we, with our simple DC-component removal method, were naive
in our linearization approach. In much of the time-series modeling literature,
a great deal of emphasis is placed on the assumed spectral and time-domain
characteristics and correlation of the signals
[21] , [11].
While we briefly
examine the 'whiteness' of our residual error time-series and other related
details, we have not been as careful as we could have been in pre-filtering
our inputs for optimal estimation. There are many techniques to do this
-
pre-whitening filters, instrumental variable estimation - all of which are
presented in detail by Ljung
[33].
I would hope that future work, both
in model order selection, and in parameter estimation, draw heavily from
this source, as it provides sufficient mathematical and application specific
motivation for a variety of time-series and model analysis techniques.
Miscellaneous
While we have presented in this thesis one form of modified
least squares estimation, we have experimented with a few more promising
techniques. Of these, the frequency domain estimation method seems the
most exciting. I would then hope that future research engage in a broader
search through estimation literature to see if such a technique already exists,
and perhaps expand on the frameworks provided in Ch. 4. In some ways,
we might be able to circumvent the problems we face in the time domain by
123
7.2. TOPICS FOR FUTURE WORK
a careful understanding of the frequency domain nature of our signals.
7.2.2
Testing
While it is certain that we need a better way to understand and solve our
estimation problem, that is a problem that is unlikely to ever be fully solved.
On some level, we must be satisfied with the results produced by our estimation, and begin testing our model's ability to identify silent changes in the
baroreflex. What I mean here is that, in our autonomic blockade data, we
could determine the state of a patient by simply looking at his physiological
signals. While this is okay, it is not clinically significant to be able to use
a model that provides no more information that can be gleaned from the
signals themselves. By 'silent', I am referring to situations where either the
sympathetic or parasympathetic pathway is not properly functioning, but it
is not altogether obvious from the signals themselves (specifically, from the
heart rate signal). A hypothetical situation where this may occur is in a patient exercising after the sympathetic pathway of the baroreflex is removed
- ischemic and chemoreceptor drive should drive an increase in heart rate
but the action will not be through the baroreflex. We should then shift our
focus to how to generate these data.
It is highly unlikely that we can perform such invasive testing on humans,
but perhaps it is possible on rabbits.
For example, if we denervate the
sympathetic/parasympathetic connection (chemically or mechanically), we
can modulate the heart rate and blood pressure in the following ways:
. Injecting boluses of saline/exsanguination to modulate blood pressure
124
CHAPTER 7. CONCLUSION
" Administration of dopamine to increase heart rate and blood pressure
centrally (in the brain)
* Calcium channel blockers to decrease heart rate and blood pressure via
venous tone
* Administration of adenosine as a strong negative chronotrope and vasodilator with a short half life [32]
We could also test our model against known interventions and baroreflex
malfunctions, e.g. vasovagal syncope, and acute hypotensive episodes. If our
model does indeed track changes in patients that the waveforms themselves
do not, or if it has some predictive ability, we should then begin testing it on
larger classes of patients to try and learn. For example, it would be interesting
to see the effect of the baroreflex in pathologies like sleep apnea, valsalva
maneuver, various arrhythmias, and chronically hypertensive patients. As
the goal of this work is clinical monitoring and use, we should try and shift
our focus to that as soon as possible.
7.3
Concluding Remarks
Researching this topic and writing this thesis has taken a long time and
a lot of effort. During the process, we have uncovered the shortcomings
of existing modeling techniques, and found ourselves facing many new and
undocumented challenges both in estimation and in model validation. The
focus of this study was then much more mathematically focused than most
quantitative physiology theses, and yet less rigorous than most estimation
7.3. CONCLUDING REMARKS
125
and optimization focused theses. In trying to balance these two goals, perhaps we have left both somewhat unsatisfied. At the same time, pursuing
one and losing sight of the other would have likely led to conclusions that
made nebulous statements about the nature of the baroreflex, or worse still,
ones that were ignorant of the original purpose of the study! The ultimate
goal of research is not only to answer previously unanswered questions, but
also to help formulate more unanswered questions. As I write these, the last
sentences of this thesis, I am satisfied and hopeful. Whether or not it was
my original intent when I began this work, I leave satisfied that I have met
the latter goal, and hopeful that another person shall rise to the challenge of
fulfilling former.
126
CHAPTER 7. CONCLUSION
Bibliography
[1] Philip N. Ainslie, Leo Celi, Ken McGrattan, Karen Peebles, and Shigehiko Ogoh. Dynamic cerebral autoregulation and baroreflex sensitivity
during modest and severe step changes in arterial pco2. Brain Research,
1230:115-24, September 2008.
[2] Solange Akselrod, David Gordon, Jaffrey B. Madwed, Nancy C. Snidman, Daniel C. Shannon, and Richard Jonathan Cohen. Hemodynamic
regulation: investing by spectral analysis. American Journal of Physiology, 249(4), 1987.
[3] David M. Baekey, Thomas E. Dick, and Julian F. R. Paton. Pontomedullary transection attenuates central respiratory modulation of
sympathetic discharge, heart rate and the baroreceptor reflex in the in
situ rat preparation. Experimental Physiology, 93(7):803-16, July 2008.
[4] Ricardo Barbieri, Gianfranco Parati, and J. Philip Saul. Closed-versus
open-loop assessment of heart rate baroreflex. IEEE Engineering in
Medicine and Biology Magazine, 20 (2):33-42, 2001 (March-April).
[5] Jerry Batzel, Giuseppe Baselli, Ramakrishna Mukkamala, and Ki H.
Chon. Modelling and disentangling physiological mechanisms: linear
and nonlinear identification techniques for analysis of cardiovascular regulation. Philosophical Transactions. Series A, Mathematical, Physical,
and Engineering Sciences, 367(1892):1377-1391, April 2009.
[6] Jerry Batzell, Giuseppe Baselli, Ramakrishna Mukkamala, and Ki H
Chon. Modelling and disentangling physiological mechanisms: linear
and nonlinear identification techniques for analysis of cardiovascular regulation. Philosophical Transactions. Series A, Mathematical, Physical,
and Engineering Sciences, 367(1892):1377-1391, April 2009.
127
128
BIBLIOGRAPHY
[7] R.D. Berger, J.P. Saul, and R.J. Cohen. Assessment of autonomic response by broad-band respiration. IEEE Transactions on Biomedical
Engineering,36(11):1061 - 1065, 1989.
[8] R.M. Berne, M.N. Levy, B.M. Koeppen, and B.A. Stanton. Physiology.
Elsevier Inc, St. Louis, MO, 5th edition, 1989.
[9] Stephen Boyd and Lieven Vandenberghe. Convex Optimization. Cambridge University Press, 2004.
[10] E. Candes and J. Romberg. Li-magic. http://www.11-magic.org/,
2007.
[11] E. J. Candes, J. Romberg, and T. Tao. Robust uncertainty principles:
exact signal reconstruction from highly incomplete frequency information. IEEE Trans. Info. Theory, 52(2):489-509, February 2006.
[12] Alexandre Ceroni, Laiali J. Chaar, Rafael L. Bombein, and Lisete C.
Michelini. Chronic absence of baroreceptor inputs prevents traininginduced cardiovascular adjustments in normotensive and spontaneously
hypertensive rats. Experimental Physiology, 94(6):630-640, June 2009.
[13] Gari Clifford. Index of / gari/code/ecgtools.
-gari/CODE/ECGtools/, May 2009.
http: //www.mit . edu/
[14] Frangois Cottin, Claire Medigue, and Yves Papelier. Effect of heavy
exercise on spectral baroreflex sensitivity, heart rate, and blood pressure variability in well-trained humans. American Journal of Physiology. Heart and CirculatoryPhysiology, 295(3):H1150-H1155, September
2008.
[15] D. Pfaff D. Ganten, editor. Central CardiovascularControl Basic and
Clinical Aspects, volume 3. Springer-Verlag, Munich, Germany, 1983.
[16] R.W. DeBoer, J.M. Karemaker, and J. Strackee. Hemodynamic fluctuations and baroreflex sensitivity in humans: a beat-to-beat model.
American Journal of Physiology, 253(3), 1987.
[17] M.H. DeGroot and M.J. Schervish. Probabilityand Statistics. AddisonWesley, Boston, MA, 3 edition, 2002.
BIBLIOGRAPHY
129
[18] Dwain L. Eckberg. Point:counterpoint: respiratory sinus arrhythmia
is due to a central mechanism vs. respiratory sinus arrhythmia is due
to the baroreflex mechanism. Journal of Applied Physiology (Bethesda,
Md.: 1985), 106(5):1740-1742; discussion 1744, May 2009.
[19] J. L. Elghozi. [short-term variability of blood pressure: physiology
and pharmacology]. Annales PharmaceutiquesFrangaises, 66(3):15868, June 2008.
[20] Bertinieri G, Di Rienzo M, Cavallazzi A, Ferrari AU, Pedotti A, and
Mancia G. Evaluation of baroreflex by blood pressure monitoring in
unanesthetized cats. American Journal of Physiology, 254 (Heart Circ
Physiolog 23):H377-H383, 1988.
[21] Box G.E.P. and Jenkins G.M. Time series analysis: forecasting and
control. Holden-Day, San Francisco, CA, 1970.
[22] Alfred Goodman Gilman, Louis S. Goodman, and Alfred Gilman, editors. Goodman and Gilman's The PharmacologicalBasis of Therapeutics. Macmillan Publishing Co., Inc, New York, 6th edition, 1980.
[23] A. L. Goldberger, L. A. N. Amaral, L. Glass, J. M. Hausdorff, P. Ch.
Ivanov, R. G. Mark, J. E. Mietus, G. B. Moody, C.-K. Peng, and
H. E. Stanley. PhysioBank, PhysioToolkit, and PhysioNet: Components of a new research resource for complex physiologic signals. Circulation, 101(23):e215-e220, 2000 (June 13). Circulation Electronic Pages:
http://circ.ahajournals.org/cgi/content/full/101/ 2 3/e 2 15.
[24] Michael Grant, Stephen Boyd, and Yinyu Ye. CVX: Matlab Software
for Disciplined Convex Programming, 2008.
[25] Arthur C. Guyton, Carl E. Jones, and Thomas G. Coleman. Circulatory Physiology: Cardiac Output and its Regulation. W.B. Saunders
Company, Philadelpha, PA, 2nd edition, 1973.
[26] Luczag H and Laurig W. An analysis of heart rate varibility. Ergonomics,
16:85-97, 1973.
[27] Masashi Ichinose, Mitsuru Saito, Naoto Fujii, Takeshi Ogawa, Keiji
Hayashi, Narihiko Kondo, and Takeshi Nishiyasu. Modulation of the
130
BIBLIOGRAPHY
control of muscle sympathetic nerve activity during incremental leg cycling. The Journal of Physiology, 586(Pt 11):2753-66, June 2008.
[28] Claude Julien, Michael J. Parkes, Shieak Y. C. Tzeng, Peter Y. W. Sin,
Philip N. Ainslie, Philippe VAN DE Borne, Jacques-Olivier Fortrat,
Marc-Antoine Custaud, Claude Gharib, Alberto Porta, Frederic Vallais,
Giuseppe Baselli, Massimo Pagani, Daniela Lucini, Richard L. Hughson, J. Andrew Taylor, Can 0. Tan, David M. Baekey, Thomas E. Dick,
Julian F. R. Paton, and Basel Taha. Comments on point:counterpoint:
respiratory sinus arrhythmia is due to a central mechanism vs. respiratory sinus arrhythmia is due to the baroreflex mechanism. Journal
of Applied Physiology (Bethesda, Md.: 1985), 106(5):1745-1749, May
2009.
[29] R. E. Kalman. A new approach to linear filtering and prediction problems. Transactions of the ASME Journal of Basic Engineering, (82
(Series D)):35-45, 1960.
[30] John M. Karemaker. Last word on point:counterpoint: respiratory sinus
arrhythmia is due to a central mechanism vs. respiratory sinus arrhythmia is due to the baroreflex mechanism. Journal of Applied Physiology
(Bethesda, Md.: 1985), 106(5):1750, May 2009.
[31] Koji Kashihara, Toru Kawada, Masaru Sugimachi, and Kenji Sunagawa.
Wavelet-based system identification of short-term dynamic characteristics of arterial baroreflex. Annals of Biomedical Engineering, 37(1):11228, January 2009.
[32] Bertram G. Katzung, editor. Basic & Clinical Pharmacology. Lange
Medical Books/McGraw Hill, New York, 8th edition, 2001.
[33] Lennart Ljung. System Identification: Theory for the User (2nd Edition). Prentice Hall PTR, December 1998.
[34] J. Lfberg. Yalmip : A toolbox for modeling and optimization in MATLAB. In Proceedings of the CACSD Conference, Taipei, Taiwan, 2004.
[35] Kobayashi M and Musha T. 1/f fluctuation of heart beat period. IEEE
Trans. Biomed. Eng., 30:194-197, 1982.
BIBLIOGRAPHY
131
[36] Mark Mutsaers, Mostafa Bachar, Jerry Batzel, Franz Kappel, and Stefan Volkwein. Receding horizon controller for the baroreceptor loop
in a model for the cardiovascular system. CardiovascularEngineering
(Dordrecht, Netherlands), 8(1):14-22, March 2008.
[37] Deborah D. O'Leary, J. Kevin Shoemaker, Michael R. Edwards, and
Richard L. Hughson. Spontaneous beat-by-beat fluctuations of total
peripheral and cerebrovascular resistance in response to tilt. American
Journal of Physiology Regulatory Integrative ComputationalPhysiology,
287, 2003.
[38] Welch P.D. The use of fast fourier transform for the estimation of power
spectra: A method based on time averaging over short, modified periodograms. IEEE Transactions on Audio Electroacoustics,Volume AU15:70-73, 1967.
[39] Bruce Pomeranz, Robert J.B. Macaulay, Margarent A. Cadill, Ilan Kutz,
Dan Adam, David Gordon, Kenneth M. Kilborn, A. Clifford Barger,
Daniel C. Shannon, Richard J. Cohen, , and Herbert Benson. Assessment of autonomic function in humans by heart rate spectral analysis.
American Journalof Physiology: Heart CirculationPhysiology, 248:151153, 1985.
[40] Boaz Porat. Digital processing of Random Signals: Theory & Methods.
Prentice-Hall, Inc., Upper Saddle River, NJ, USA, 1994.
[41] Walter C. Randall. Nervous Control of CardiovascularFunction. Oxford
University Press, New York, 1984.
[42] J.A. Rice. Mathematical Statistics and Data Analysis. Duxbury-Press,
3 edition, 1994.
[43] M. Di Rienzo, A. Radaelli G. Parati, and P. Castiglioni. Baroreflex
contribution to blood pressure and heart rate oscillations: time scales,
time-variant characteristics and nonlinearities. Philosophical Transactions of the Royal Society, 367, 2009.
[44] Mohn R.K. Suggestions for the harmonic analysis of point process data.
Comp. & Biomed. Res., 9:512-530, 1976.
132
BIBLIOGRAPHY
[45] DeBoer RW, Karemaker JM, and Strackee J. Comparing spectra of a
series of point events particularly for heart rate variability data.. IEEE
Trans. Biomed. Eng., 31(4):384-387, 1984.
[46] J. Philip Saul, Ronald D. Berger, Paul Albrecht, Stephen P. Stein,
Ming Hui Chen, and Richard J. Cohen. Transfer function analysis of
the circulation: unique insights into cardiovascular regulation. American
Journal of Physiology, 261(4), 1991.
[47] Mauricio Scanavacca, Denise Hachul, Cristiano Pisani, and Eduardo
Sosa. Selective vagal denervation of the sinus and atrioventricular nodes,
guided by vagal reflexes induced by high frequency stimulation, to treat
refractory neurally mediated syncope. Journal of CardiovascularElectrophysiology, 20(5):558-563, May 2009.
[48] Stephen M. Smith, Nilesh J. Samani, Emily L. Sammons, Wendy E.
Rathbone, John F. Potter, Stephen Bentley, and Ronney B. Panerai.
Influence of non-invasive measurements of arterial blood pressure in
frequency and time-domain estimates of cardiac baroreflex sensitivity.
Journal of Hypertension, 26(1):76-82, January 2008.
[49] Hugo C. D. Souza, Geisa C. S. V. Terzini, Valdo J. D. da Silva, Marli C.
Martins-Pinge, Helio C. Salgado, and Maria-Cristina 0. Salgado. Increased cardiac sympathetic drive and reduced vagal modulation following endothelin receptor antagonism in healthy conscious rats. Clinical
and Experimental Pharmacology & Physiology, 35(7):751-6, July 2008.
[50] Jos F. Sturm, Oleksandr Romanko, Imre Polik, and Tamas Terlaky.
Sedumi, 2009. http: //mloss. org/software/view/202/.
[51] Robert Tibshirani. Regression shrinkage and selection via the lasso.
Journal of the Royal Statistical Society, Series B, 58:267-288, 1994.
[52] K. C. Toh, M.J. Todd, R.H. Ttnc, and R. H. Tutuncu. Sdpt3 - a matlab
software package for semidefinite programming. Optimization Methods
and Software, 11:545-581, 1998.
[53] B. W. Wilkins, C. Hesse, N. Charkoudian, W. T. Nicholson, H. P. Sviggum, T. P. Moyer, M. J. Joyner, and J. H. Eisenach. Autonomic cardiovascular control during a novel pharmacologic alternative to ganglionic
BIBLIOGRAPHY
133
blockade. Clinical Pharmacology and Therapeutics, 83(5):692-701, May
2008.
[54] Xiao X and Cohen RJ Mukkamala and. A weighted-principal component
regression method for the identification of physiologic systems. IEEE
Transactions on Biomedical Engineering, 53(8):1521-1530, 2006.
[55] Xiao X, Mullen TJ, and Mukkamala R. System identification: a multisignal approach for probing cardiovascular neural regulation. Physiological Measurement, 26:R41-R71, 2006.
134
BIBLIOGRAPHY
Appendix A
Convex Formulation of
Optimization Problems
A.1
A.1.1
Norms, P-Norms, and Convexity
Convexity
We call a set C convex if the line segment between any two points in C is
contained in C, or formally,
VX,y E C, 0 < 0 < 1, we have Ox + (1 - 0)y E C
We define a function,
f
: R" --
m,
to be convex if its domain and epigraph
are convex sets. Similarly, we say a function
f
is convex if domf is a convex
set, and
f(Ox + (1 - O)y) < Of(x) + (1 - 6)f(y)
135
V, y E domf, 0 < 0 < 1 (A.1)
136APPENDIX A. CONVEX FORMULATION OF OPTIMIZATION PROBLEMS
We then define a convex optimization problem to have the form:
minimize
f(x)
subject to gi(x) < bi, i
1,
.
,rn
n.
hj (x) = c, J=1,.,
where the objective
f
is a convex function, and the equality and inequality
constraints are convex as well (g's and h's are convex, and b's and c's are
constants).
We are placing so much emphasis on convex optimization because, by
definition, all convex optimization problems are guaranteed to have a global
minimum solution'. We can find these solutions using any number of available convex optimization solvers2 [9].
Now we must define a norm and show that all norms are convex functions
of their arguements.
A.1.2
Vector Norms
We define a norm as any function f : W" -+ R satisfying the three following
properties:
" Positive homogeneity - f(a - x) = |a - f(x) for any scalar a
" Triangle inequality - f (x + u) < f (x) + f (u)
lor no feasible solution
2
Linear Programs, Semidefinite Programs, Second Order Cone Programs, Geometric
Programs, Quadratic Programs, and a few more commonly discussed optimization problems are, in fact, convex optimization problems, and so reformulating a problem into one
of these forms will suffice for our purposes
A.1.
137
NORMS, P-NORMS, AND CONVEXITY
x = 0
e Positive definiteness - f (x) = 0
Furthermore, we define a p - norm to be a special norm satistifying the
For any norm, we know that by the
following property, Oxll, = (S1x:l)P.
triangle inequality,
f (Ox + (1 - O)y) < f (Ox) + f ((1 - O)y)
And from the positive homogeneity property,
f (Ox + (1 - O)y) < f (Ox) + f ((1 - O)y)
=
Of(x) + (1 - O)f (y)
Which shows that all norms as defined above are convex.
Because
I-||1and I -
are specific cases of p - norms, we know that they
are convex functions. We must now further show that the composition of a
p - norm and an affine function is also convex.
A.1.3
Convexity of the Norm of an Affine Function
It is easy to show that all affine and linear functions are convex by applying
the definition in (A.1). Without too much exposition, it is simple to visualize
that for any vector z E R", q(z)
-
Iz|
is a convex, nonnegative function.
Similarly, if we form y as an affine transformation of z, y
function q(y) =
|yl
Gz + h, the
remains convex and nonnegative.
n
with domp = , which is
i=1
convex and nondecreasing. Let g(x) = xll, and h(x) = Gx+h. We see that
We then consider the function p(x) =(5x)P
f (x) = p o q(x) = g o h(x). Invoking second-order conditions on convexity (if
f
is twice differentiable, f(x) convex
* f"(x) > 0 Vx E domf ):
138APPENDIX A. CONVEX FORMULATION OF OPTIMIZATION PROBLEMS
f"(x) > 0 m Vp(q(x))Tq"(x) + q'(x)TV 2 p(q(x))q'(x) > 0
Since the above holds for our choice of p and q, we know that
f
= p oq is
convex, and therefore, our composition of an affine function with a p - norm,
g o h is convex as well.
A.2
Reformulation of Optimization Problems
A.2.1
CI-minimization as an LP
We define a standard Linear Program (LP) as:
minimize
xERmt
cTX
subject to Gx < h
(A.2)
Fx = z,
Our i 1-norm minimization problem takes the form:
minimize
m
xElR
||Ax - b|1
(A.3)
If we introduce a dummy vector, t E R"', and add the constraints t <
Ax-b and -t > Ax-b, minimizing
ITt
will (with a little more matrix/vector
stacking) reduce to the standard form LP, ready to be solved by standard
LP solvers.
A.2. REFORMULATION OF OPTIMIZATION PROBLEMS
139
4C
0 -minimization as an LP
A.2.2
Our lioo-norm minimization problem takes the form:
minimize
m
xER
||Ax - bJ
(A.4)
If we introduce a dummy scalar, t E R, and add the constraints t < Ax - b
(</> in the elementwise sense) and -t > Ax - b, minimizing t will (with a
little more matrix/vector stacking) solve the minimax problem as a standard
form LP, ready to be solved by standard LP solvers.
L 1 -regularized least squares problem as a QCQP
A.2.3
We define a standard Quadratically Constrained Quadratic Program to take
the form:
minimize
xERmn
subject to
.xI'Hox + foTx
+ fTx + ci < 0 for i= {1, . . . m}
xT H
Fx
-
(A.5)
z,
where matrices Hi are positive semidefinite matrices to ensure convexity. We
can solve these problems efficiently using QCQP solvers, or more general
semidefinite program solvers [9].
Our L 1 -regularized least squares problem takes the form in (A.6) and we
wish to massage it into standard QCQP form (A.5):
140APPENDIX A. CONVEX FORMULATION OF OPTIMIZATION PROBLEMS
minimize
xERt t
\\Ax - b| \+||Gx + h||1
subject to
Xi < ci, i* =
(A.6)
1
7,m}
We begin by expanding the quadratic term in the objective function as:
minimize
xE R"-
X AT Ax + 2xT Ab+
subject to xi < ci, i = {1,
bTb + Gx + h|1
. , m}
We then introduce a new variable, t, and an additional constraint aimed
at removing the E1 -norm:
minimize
XERr"ntER
xT AT Ax + 2xT Ab + bTb + t
subject to xi < ci, i1=
{1,
. . .7,m}
Gx +h<t
Gx + h > -t
If we introduce yet another variable z where z = [xlt] (by [x~y] we mean
the vertical stacking of column vectors x and y), we arrive at our final QCQP
formulation:
141
A.2. REFORMULATION OF OPTIMIZATION PROBLEMS
[
T
-
zT
minimize
zERmt+10
T
A
A
0
-
-
-
-
z+ 2z T [-A
0
-
-
- -T'
--b + -b
0
0J
-
-
-b +
0 M1)
0
subject to
c
(1(1xm), 0)
(G, -1(mxi))
(-G,
A.2.4
-1(mxi))
z <
h
h
Practical Solution of Convex Optimization Problems
Because going through the mathematical gymnastics for every convex optimization problem you will come upon, there are a few modeling languages
that allow you to express convex optimization problems in their natural form,
and will go through the contortions for you. Most notable are YALMIP
[34]
and CVX [24], which interface with commonly available convex optimization
solvers as well as open source solvers, SeDuMi
a MATLAB interface.
[50]
and SDPT3 [52] using
142APPENDIX A. CONVEX FORMULATION OF OPTIMIZATION PROBLEMS
Appendix B
Various Model Criteria Applied
to All Patients
Table B.1: Mean Residual Ratio for Standing Control Patients
Cost Fcn/Res.Rat.
E2
L1
Ec
r(L2)
1.00
1.04
1.39
r(f1)
1.02
1.00
1.46
r(C.o)
1.77
2.34
1.00
Table B.2: One-Step Error Correlation for Standing Control Patients
Pat. No.
p(L2)
P(L1)
P(£oo)
CRCO1STC
CRC02STC
CRC03STC
CRC04STC
CRC05STC
CRC06STC
CRC07STC
CRCOSSTC
CRC09STC
CRC1OSTC
CRC1ISTC
CRC12STC
CRC13STC
CRC14STC
-0.02
0.26
0.20
0.01
0.02
-0.02
-0.16
0.28
0.57
0.36
0.41
0.22
0.29
0.22
-0.06
0.23
0.20
-0.08
0.06
-0.08
-0.22
0.26
0.56
0.37
0.41
0.23
0.29
0.23
-0.06
0.65
0.10
-0.12
0.13
0.40
0.51
0.27
0.68
0.34
0.42
0.45
0.29
0.45
143
144APPENDIX B. VARIOUS MODEL CRITERIA APPLIED TO ALL PATIENTS
Table B.3: Mean Residual Ratio for Supine Control Patients
Cost Fcn/Res.Rat..
I2
,12
Lo
r(L 2 )
1.00
1.03
1.46
r(C1)
1.02
1.00
1.55
r(Loo)
1.70
2.29
1.00
Table B.4: One-Step Error Correlation for Supine Control Patients
Pat. No.
P(C2)
p(L1)
p(Ioo)
CRCO1SUC
CRC02SUC
CRC03SUC
CRC04SUC
CRC05SUC
CRC06SUC
CRC07SUC
CRC08STC
CRC09SUC
CRC10SUC
CRC11SUC
CRC12SUC
CRC13SUC
CRC14SUC
0.01
-0.08
0.23
-0.17
-0.08
-0.09
-0.05
0.02
0.23
0.23
0.26
-0.10
0.23
-0.10
-0.02
-0.16
0.22
-0.31
-0.19
-0.12
-0.09
0.01
0.22
0.22
0.28
-0.12
0.23
-0.12
0.20
0.51
0.44
0.82
-0.11
0.30
0.18
0.89
0.29
0.06
0.36
0.27
0.28
0.27
Table B.5: Mean Residual Ratio for Standing Propranolol Patients
Cost Fcn/Res.Rat.
L2
Li
c
r(C
2
)
1.00
1.01
1.27
r(,12)
1.01
1.00
1.32
r(Lo,,o)
1.66
2.06
1.00
Table B.6: One-Step Error Correlation for Standing Propranolol Patients
Pat. No.
CRCO1STP
CRC03STP
CRC05STP
CRC08STP
CRCIOSTP
CRC12STP
CRC14STP
P(C2)
-0.16
-0.02
-0.05
-0.16
0.12
-0.14
-0.14
P(LI)
-0.23
-0.03
-0.06
-0.17
0.12
-0.19
-0.17
p(Lo)
0.28
0.11
0.15
-0.24
0.27
-0.11
-0.15
Table B.7: Mean Residual Ratio for Supine Propranolol Patients
Cost Fcn/Res.Rat.
£2
L1
r(I2)
1.00
1.02
1.29
r(L 1 )
1.01
1.00
1.31
r(Lo)
1.56
1.85
1.00
145
Table B.8: One-Step Error Correlation for Supine Propranolol Patients
Pat. No.
CRC01SUP
CRC03SUP
CRC05SUP
CRC08SUP
CRCIOSUP
CRC12SUP
CRC14SUP
P(£2)
-0.12
-0.04
-0.26
-0.09
0.22
-0.18
-0.17
P(C1)
-0.20
-0 18
-0.34
-0.17
0.23
-0.23
-0.26
p(£oo)
-0.04
0.10
-0.06
0.01
0.15
0.48
0.43
Table B.9: Mean Residual Ratio for Standing Atropine Patients
Cost Fcn/Res.Rat.
L2
L1
'co
r(L2)
1.00
1.02
1.27
r(L 1 )
1.02
1.00
1.27
r(Loo)
1.79
2.53
1.00
Table B.10: One-Step Error Correlation for Supine Propranolol Patients
Pat. No.
CRCO1SUP
CRC03SUP
CRC05SUP
CRC08SUP
CRC1OSUP
CRC12SUP
CRC14SUP
p(L2)
-0.12
-0.04
-0.26
-0.09
0.22
-0.18
-0.17
p(I1)
-0.20
0.18
-0.34
-0.17
0.23
-0.23
-0.26
p(Lo)
-0.04
0.10
-0.06
0.01
0.15
0.48
0.43
Table B.11: Mean Residual Ratio for Supine Atropine Patients
Cost Fcn/Res.Rat.
L2
l
-
oo
r(122)
1.00
1.06
1.21
r(£ 1 )
1.03
1.00
1.25
r(Co)
1.14
1.32
1.00
Table B.12: One-Step Error Correlation for Supine Atropine Patients
Pat. No.
CRC02SUA
CRC04SUA
CRC06SUA
CRC07SUA
CRC09SUA
CRC11SUA
CRC13SUA
p(£2)
-0.40
-0.37
-0.10
0.25
-0.49
-0.51
-0.58
p(L1)
-0.70
-0.32
-0.10
0.29
-0.50
-0.51
-0.59
p(Lo)
0.30
-0.18
-0.04
-0.01
-0.50
-0.46
-0.59
146APPENDIX B. VARIOUS MODEL CRITERIA APPLIED TO ALL PATIENTS
Table B.13: RMS Residual Error v. Number of Windows
Patient/Num.Win.
CRC01STC
CRCOISTP
CRC01SUC
CRC01SUP
CRC02STA
CRC02STC
CRC02SUA
CRC02SUC
CRC03STC
CRC03STP
CRC03SUC
CRC03SUP
CRC04STA
CRC04STC
CRC04SUA
CRC04SUC
CRC05STC
CRC05STP
CRC05SUC
CRC05SUP
CRC06STA
CRC06STC
CRC06SUA
CRC06SUC
CRC07STA
CRC07STC
CRC07SUA
CRC07SUC
CRC08STC
CRC08STP
CRC08SUC
CRC08SUP
CRC09STA
CRC09STC
CRC09SUA
CRC09SUC
CRC10STC
CRC1OSTP
CRClOSUC
CRC10SUP
CRC11STA
CRC11STC
CRC11SUA
CRCI1SUC
CRC12STC
CRC12STP
CRC12SUC
CRC12SUP
CRC13STA
CRC13STC
CRC13SUA
CRC13SUC
CRC14STC
CRC14STP
CRC14SUC
CRC14SUP
1
20.6
21.6
28.6
33.8
6.8
31.1
17.0
55.3
17.5
20.2
34.7
86.8
7.1
32.0
2.6
52.4
78.6
100.2
96.4
108.3
3.4
52.5
3.6
72.5
2.2
37.8
39.2
75.2
23.8
28.0
22.1
37.2
2.8
16.9
2.1
27.2
20.1
2
20.6
21.3
28.5
33.7
6.8
31.0
16.5
54.8
17.4
20.0
34.5
85.9
7.1
31.6
2.6
50.1
73.5
94.9
96.3
102.1
3.4
52.4
3.6
72.3
2.2
37.7
38.7
73.8
22.4
27.9
20.9
37.1
2.8
16.8
2.1
27.2
19.8
4
20.5
20.9
28.2
32.8
6.8
30.7
15.7
53.6
16.9
19.9
34.1
84.5
7.1
31.1
2.6
49.2
72.6
92.4
95.2
100.1
3.4
51.4
3.6
72.3
2.2
37.2
37.9
73.7
22.3
27.7
20.5
36.6
2.8
16.1
2.0
26.7
19.8
21.5
21.5
33.4
34.2
2.2
13.5
2.2
26.0
21.1
25.4
41.2
57.9
2.3
35.2
2.1
45.3
21.1
27.1
41.2
61.7
33.1
33.6
2.2
13.3
2.2
25.6
20.9
25.3
40.6
56.8
2.3
35.1
2.1
45.2
20.9
26.7
40.6
60.3
6
20.0
20.7
27.8
33.1
6.8
30.2
14.8
53.1
16.3
19.6
34.2
82.6
7.0
31.1
2.6
48.4
72.1
91.3
93.4
99.5
3.4
51.7
3.6
71.4
2.2
36.8
37.4
73.1
22.1
27.6
20.3
36.3
2.7
15.7
2.0
26.3
19.5
8
20.2
20.5
27.6
32.1
6.7
30.2
14.5
52.3
16.3
19.7
33.7
82.1
7.0
30.6
2.6
48.5
72.0
90.4
93.4
99.4
3.3
51.1
3.6
71.2
2.2
36.7
37.4
73.2
21.9
27.3
19.9
35.8
2.7
15.5
2.0
26.2
19.1
10
19.5
20.3
27.6
31.8
6.7
29.7
14.1
51.7
16.1
19.6
33.5
80.6
7.0
30.4
2.6
47.8
71.6
90.8
93.0
98.3
3.3
50.8
3.5
70.7
2.2
36.3
37.0
69.6
21.9
26.7
20.1
35.7
2.7
15.5
2.0
26.1
19.1
12
19.1
20.3
27.5
31.2
6.5
29.7
14.4
49.9
15.7
19.4
33.5
79.1
6.9
30.1
2.6
47.2
71.9
88.9
92.2
97.5
3.3
50.7
3.5
70.2
2.2
35.8
36.3
70.5
21.7
26.8
19.6
35.3
2.7
14.9
2.0
25.9
19.0
14
19.4
19.7
27.0
31.2
6.6
29.8
13.9
48.2
15.6
19.1
33.1
78.9
7.0
29.7
2.6
48.1
70.5
89.3
91.4
98.0
3.3
50.5
3.5
68.9
2.2
35.5
36.0
72.0
21.6
26.6
19.5
34.4
2.5
15.3
2.0
25.7
18.8
16
19.2
19.1
27.1
30.6
6.6
29.4
13.9
49.3
15.7
18.9
33.2
78.9
7.0
29.1
2.6
46.3
69.8
86.0
91.1
97.9
3.3
49.3
3.5
69.1
2.2
34.6
35.4
70.0
21.3
26.7
19.2
34.7
2.6
14.7
2.0
25.5
18.7
21.2
21.1
21.0
19.8
17.6
17.4
16.9
17.1
32.5
33.2
2.2
12.9
2.2
24.9
20.9
24.8
39.7
56.0
2.3
35.0
2.1
44.9
20.9
26.2
39.7
59.1
32.5
32.7
2.2
12.7
2.2
25.1
20.8
24.7
39.5
55.3
2.3
34.2
2.1
44.7
20.8
25.9
39.5
59.0
32.1
32.7
2.2
12.6
2.2
24.5
20.6
24.4
39.4
54.4
2.3
33.8
2.1
44.5
20.6
25.5
39.4
58.0
32.1
32.3
2.2
12.5
2.2
24.4
20.4
23.9
39.1
53.4
2.3
33.6
2.1
44.5
20.4
25.1
39.1
57.4
32.0
31.5
2.2
12.2
2.2
24.4
20.3
23.8
38.2
53.4
2.3
33.3
2.1
44.4
20.3
24.5
38.2
56.3
32.0
30.6
2.2
12.2
2.2
24.3
20.1
23.6
37.8
52.7
2.3
32.8
2.1
44.4
20.1
24.5
37.8
56.5
31.1
31.8
2.2
12.1
2.2
24.0
19.8
23.1
37.0
51.0
2.3
32.4
2.1
44.1
19.8
23.6
37.0
55.1
31.4
31.6
2.2
12.0
2.1
23.8
19.7
22.6
37.5
49.9
2.3
32.6
2.1
43.9
19.7
23.4
37.5
54.3
18
18.9
19.6
27.0
30.4
6.6
29.4
13.3
48.1
15.0
18.6
33.0
78.3
6.9
29.8
2.6
46.1
68.9
84.7
91.5
96.2
3.3
49.3
3.4
67.7
2.2
33.5
34.2
70.6
21.2
25.5
19.0
34.2
2.4
13.9
2.0
25.3
18.4
20
18.7
19.7
26.7
30.1
6.6
28.3
13.5
48.5
15.1
18.4
32.8
77.9
6.9
28.6
2.6
46.4
67.7
86.8
90.3
94.0
3.2
48.9
3.4
68.5
2.2
33.4
34.9
70.6
21.0
25.2
18.6
32.7
2.6
14.6
2.0
24.7
18.5
16.8
31.3
30.6
2.2
12.2
2.1
23.7
19.5
22.4
36.5
50.6
2.3
32.4
2.1
43.9
19.5
23.2
36.5
53.5
]
m
- 000
to
D o6
4o645
,qtx000m0
Cq
m0 N
I-
-,t
N t-
t- N
m 0
0
6 5
O00
00
O
66
"T x
0
m0
t
0
m
0 0 0 0
m0
00C,
0000t
0 0 0 0
00
0
6 o46
m0 t0-
0
txmO
m 0Cm
No 00l.
N0 Nm 00
00 m
CO M0 o-0
00o-
C
00 't
00000
()
CO t000z
t't0
01O 000000000m00000It 00
(0
)
N C O x
M 00 O 0CO
N- CO 0 -,t
t- c cS 6c"
- 0
00 4 tO0o0
00 N 0 0
0000C0
1616o oo
o
4
mO 10 00000
CO 0
00
't
t0
- CN -IT
o o
O 't
-IT
0 Ct-
I-
0o
tCO
zCr m
0T0O'
N*
CI 0
0
C
I0000 -
0
-
-Tt
CO.
.0
0
0-
6 r
t0t-
00
0
C N
00
C
0 ;t-0
m C- 00
I0
o tr-0
14
N
o
O) 1
x
6t
0
O
o'
0
CO
C
O
,,
00
1,1
)
t-
t
NOC
0
CO0)
C4
J
o
o m
C,4 1-00
m
C4 '0
0
m
000 N
0'0D
1
m
0-
00 0
00
m
000oom
t
00000
-C-4
q-~
O 0 60
ONt
N -
om
0
O 0
N 00
o-o
O 0000
00too
t00 Co
00 0
C0
to
N
C
0
zt
-S
0 CO
-0
C
C 00-0-M,00
60
C,6
CO 00 00 00 00 C4 00 00, DO 00 00t-00
COt 00 C O 0 CO
00 00 00 C4
00 C
NO CO0
CO 00 0
CN 0 N 0- 00 0
vO 00 0 0000 00
00 m O 00 N
C
00 C 00 - 00
0N tt-
co
CO
C,4C,4
I
6 166c
0ooeoo0C-ooo
00N00T
000-C00x0M00 o.ooo
M0 0-N0
x0-o
.0
O
CO C D0CO O0 00
-00
to O to
0- 0
(m r-O 0" 00
C
O
oo
o
0Coo-o-000-
.
00 -t-C
.
l)m 0
N
,
000 0
000
CO
N
m0Co
000
00 N0-
to 0
N t
CO00o
CO 00
It 00 000
CO 0I 00
-00-oo
m
0 -O
00 0
-N Cq
C
CO CO- coo
m-
o)
-
00io
o
e
r00
C) -o
0m
oo0-o00
0
GO 0
00 00 m O 00 " 0
0 0
O
0
t000
400 o C o
CO N Coo 000, 6 -,
CS 616 M CO D 00
000
0t
00
00 It
0)C
tI
1
oCt
00 N
0)0
Cn 1 a00
00 0 0Cq I C11 .
C 00 M C M 0
CO 10 t0
CO tIt
C
C N
00 "t
m
00 COt-0
oo
1-
to
;0St-.46 4
0 0-00O0~00000o0~0
-0~
100
00 "t
to
oo 0) NO t-0
0000 t0
O 00
-
10 00 Cq 0
C, I-
m
m0q
6
v m
N-
M00 N-.O
,4mo
0) )
t, CO 1 C
o
00
000
j
oo
0O 0 0 oo I
- 00
to0o
00
00 00 GO00 00
00- OD 0-0
00
00
tII
OOOOOOOGOoOoMooOoooooooo
o D
-t
00
)0
0
"
00000mm
0T lz
m 0F
m t-
CO
000
It
It00000
C
o 0O
)
to
0
00
t0
t- t-
e
00
o
0000t
M- to 0
1lzv'
C O 000
00
00
to
CO 000CO
~0
1O CO
u
0
0
u
0
-
0
D
u
ITI
000
-00
0
:
CO
0 0000
C 00
0C), 00
0-z
to
CO
00
t
-
- 000
00'C'otOO'
00 CNt
to
00 o6
1 1
llv1
0
C1
C
"
00 00
000-
0'
00
t
0
1
O 0
0
0
u
0 C
0
u
0 0
0
O
0-
CO
u
0
000 0-
0
Ox
u
0
00000
0
0-
00 to
-
-
No
c
-,"
mm
mOC
C O0
00t
t"t'
c
00
00 00
00
to
It
COm '
CO 00 0000O
00000000C0000
u
0
00 0-
- 000-0
00 600
00
C 00 00 00
00 00 00 00 00 00
00
0 00 00 00 00 00 00 00 00 00
O 00 0- 00 00 - 00
to t 'ITo
to
to
00
000 0 0
00 00 00 C O
0
00 00 :
O m O t-
00 00 00 0- CO 00 CO 00 CO 00 00 00CO0
00 - - CO 00 CO 00- 0 0
0
00
CO00000000
u
0
C IO
0
0
000-00000000000000
O 00 CO t-
-
0- 0- 00000-00000-x
CO 0m00000-0000CO 00000000000
0- 00 00 00 0- 00 00 00 00 00 00 00 00 00 00
C O 00
000 00 0 00 0
00 0 0 00 00
10
to
1
o
0
00 00 00 00
00 00 00 O
000
u
00
O 0 0
00 0
00 00
O
u
0 O -
CO 00 00 -00
-
o
CO00
00 CO 00 00
0000O00
00
C CO0 tO0 -7 0000
CO C C -000
000 CO 00 CO 00 0000
CO 00 0-00 00 00 CO0 0 C00 0 0 o
C 0CO M0 CO 00
o 0 00
00 00
O 00 00-0
-0 00 000000
0
00
C0 00 00 00 0
CO 000
to
ic
0 00
0 C
M 0- o 0 rO 0 00O
0to0
O CO
0 0 X 0 C O
00
tO - 00 00- CO 000 O
00 0
00 00 00 00 00
Io
000 00
00
00
00
00 0 0 00
00 00 00 000
00
tot
00 00i
Lo
0 I0
00 00 00 00
00CO r
00
2- 000C
00 00 00
65556o56
00: 00 00 00i 00 00 00 00 00 00 000
00
66
00 00005CO 0o 00
u
00 0-
0- CO 0 0 m
CO00
oo CO0
00 0- 00r 0- 00 00 00 00 0-x 0
0 0
0
0
O00000O0000-000
O
"O
0- 0000000-00000-0000000-00000-
0
000
00000 -
CO 00
00
00 -
0O CO
CO00
0CCO00
0 00 00
:0000
00
- o 0 M - 00 00 00C 00 oM CD 00 00 0
00 C4 00 00 00C
00 00 CO C 00
00 oo 0 00 C tCm
00 a)
0
CqO 00 00 4 00 C
)0 C 0
CO000
00 CO 00 00 00000000000
0
OC
" 0000-0t0
00 0o 00000)o0 0 0) 0 000 0 0 C00 04 0 0
to00000000000000000000000000
"
-uu