Architecting the Healthcare System for Stakeholder Value Jorge Fradinho Oliveira
advertisement

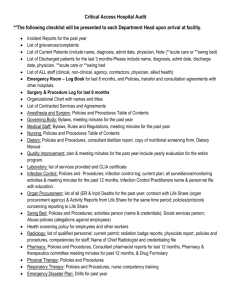
Architecting the Healthcare System for Stakeholder Value Jorge Fradinho Oliveira Massachusetts Institute of Technology 21st January 2009 US Health Care Issues “Simply stated, the US does not have a health care system.” William Brody, President of Johns Hopkins University, 2007 Access 15% of US population is uninsured 75% of care delivery is done by groups of five physicians or less Quality 44,000 to 98,000 patient deaths attributed to medical error 55% of recommended care is administered to adults Cost 16% of GDP spent on health care in 2005 30.8% of total health care expenditure is spent on hospitals “…the strategies [hospitals] develop and implement to compete have a significant effect on costs, quality, and access to care.” (Devers et al. 2003) http://lean.mit.edu © 2009 Massachusetts Institute of Technology Jorge Oliveira 01/ 21/09 -2 Health Care is a Complex Socio-Technical System Regulator Payer Patient Provider Nursing Home Hospital Labs Labs Operating Rooms Nurse Specialist Care Ancillary Services Inpatient Units Primary Care Radiology Psychologist Physician Supply Technician http://lean.mit.edu Interest Groups Pharmacy Pharmacy Emergency Department Cleaning Insurer Primary Care Flu Clinic Home Care Supplier Student resident Admin staff © 2009 Massachusetts Institute of Technology Jorge Oliveira 01/ 21/09 -3 Greater Boston Hospital Case • Leading multi specialty physician led group practice with national and international recognition (i.e. neuro, liver, heart & vascular, etc) 2006 Highlights • Emergency Visits: • Total Beds: • Total Staff: • Total Income: • Total Expenses: • Operating Income: Problem Statement 38,631 293 4263 $679,454,000 $628,525,000 $50,929,000 • Emergency Department (ED) struggling to keep up with demand • Long wait times in the ED and patient leaving without being seen • ED staff blame inpatient staff and vice versa • ED staff churn levels significant What can be done to speed patient flow in the ED? Where should a process improvement initiative focus? http://lean.mit.edu © 2009 Massachusetts Institute of Technology Jorge Oliveira 01/ 21/09 -4 Emergency Department VSM Patient Arrives Registration:: Patient orders (paper) 1 Not L1 L? T System:: Patient chief complaint MedTech Order Stack:: Patient orders (paper) T System:: Priority assignment (L1 :: L5) Blood lab: Blood vials T System:: Patient demographic, Insurance, etc details Follow-up if tests show an issue Patient leaves Radiology Lab Patient Tired of Waiting L1 Triage (room 1) Check in ED waiting area 1 ED waiting area 1 L? Not L1 Conduct tests (room 2) Complete Check in ED waiting area 1 ED waiting area Measure vital signs 1 Patient placed in ED bed ED waiting area Assessment/ treatment Patient in ED bed waiting diagnosis ? First EKG, blood draw, then external tests Patient leaves Yes No / “Tourist” L1 Patient ready? Discharge Note (1) Note (2) Patient Arrives as Transfer or EMS pick-up Patient Arrives as Transfer from ‘X’-Type Facility x Number of operators Information flow Patient flow Patient idle Patient healthy Re treat patient Phone: Admitting Physician requested Patient healthy Patient In ED bed No Note (3) Note: (1) if bed not available, creative process comes into play whereby a bed is found for the patient (i.e. hallway, other) Note (2): Check in initiated over phone and completed once patient arrives. Note (3): Some hospitals have an agreement with Lahey where patients just roll through the ER. ‘X’ is a fill-in until we know what to call these types of facilities. Note (1) Note (3) Pre Admit Tracking System: Bed request Note (1) No Patient direct Diagnosis? “Kick theto floor tires” Patient Observation Diagnosis? “Kick the tires” Admit patient Admit patient Initiate Patient Admit Process Check patient Ready? Patient In ED bed Waiting for admit physician Admit Physician arrives and checks patient (visual & paperwork) Yes Sign orders Note (2) Inpatient bed available? No Moving Yes Staff available? Transfer Patient Yes Patient In ED bed x Number of operators Information flow Note: (1) may involve additional tests, or lab work Note (2): Receiving floor requests ED to ‘hold onto’ patient for a period of time to complete shift change or catch up on work Note (3): After 11:00 p.m. Need to call Head Nurse shift supervisor for bed assignment. Patient flow Patient idle http://lean.mit.edu © 2009 Massachusetts Institute of Technology Jorge Oliveira 01/ 21/09 -5 Emergency Department Analysis Description of patient time spent in ED Description of patient arrivals and departures Simulation Modeling Average time for each step of the patient process http://lean.mit.edu © 2009 Massachusetts Institute of Technology Jorge Oliveira 01/ 21/09 -6 Preliminary Findings ED average length of stay considered problematic, but non-admitted patients took 4 hours, whereas admitted patients took over 8 hours Main Findings ED interacted well with some patient wards but not with others ED heroic employee efforts said to be common rather than sporadic ED metrics and strategic goals misaligned with overall hospital (X-Matrix) Questions For Further Study Why was the ED managed as a silo rather than end-to-end? Was the varying performance of ED interactions due to the payment model? Could it be that different observed EA configurations were directly related to the different observed performance levels? “The problem of redesign gets harder and the evidence weaker as one moves from the microsystem to the organization.” Donald Berwick, President of Institute for Healthcare Improvement, 2002 http://lean.mit.edu © 2009 Massachusetts Institute of Technology Jorge Oliveira 01/ 21/09 -7 “As Is” Enterprise Architecture Policy View Organizational View Knowledge View STRATEGY VIEW Knowledge View Knowledge View Knowledge View SURGERY SUPPORT (Labs, Pharm, Supplies) EMERGENCY DEPARTMENT Knowledge View FLOORS/ WARDS INTERNAL MED Process/Service View Process/Service View Process/Service View Process/Service View IT View T-System Knowledge View HEALTH WORKER Bed Tracking Medtech http://lean.mit.edu © 2009 Massachusetts Institute of Technology Jorge Oliveira 01/ 21/09 -8 “To Be” Enterprise Architecture Patient In the center of the architecture (Service-centered architecture) Hospital processes oriented around the patient (Process-centered architecture) Information Technology connects patient, knowledge, process, organization (IT/knowledge centered) http://lean.mit.edu © 2009 Massachusetts Institute of Technology Jorge Oliveira 01/ 21/09 -9