Return to Play in National Football League Players After Operative Jones Article 603983
advertisement

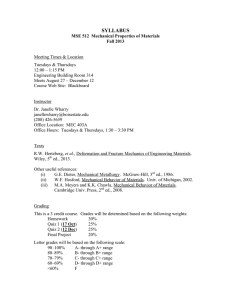
603983 research-article2015 FAIXXX10.1177/1071100715603983Foot & Ankle InternationalLareau et al. Article Return to Play in National Football League Players After Operative Jones Fracture Treatment Foot & Ankle International® 1­–9 © The Author(s) 2015 Reprints and permissions: sagepub.com/journalsPermissions.nav DOI: 10.1177/1071100715603983 fai.sagepub.com Craig R. Lareau, MD1, Andrew R. Hsu, MD1, and Robert B. Anderson, MD1 Abstract Background: Jones fractures commonly occur in professional athletes and operative treatment remains the standard of care in this patient population. In our clinical experience, an aggressive postoperative rehabilitation protocol for National Football League (NFL) players with an average return to play (RTP) between 8 and 10 weeks can have successful outcomes with few complications. The purpose of this study was to quantify RTP and rate of complications, including nonunion, refracture, and reoperation among a cohort of NFL players with operatively treated Jones fractures. Methods: Between 2004 and 2014, 25 consecutive NFL players who underwent acute Jones fracture fixation by a single surgeon were reviewed. Operative treatment for the majority of patients involved fixation with a Jones-specific intramedullary screw and iliac crest bone marrow aspirate with demineralized bone matrix injected at the fracture site. Additionally, our protocol involved the use of noninvasive bone stimulators, application of customized orthoses, and an aggressive patient-specific rehabilitation protocol. Patient demographics were recorded along with position played, seasons played after surgery, RTP, and complications. RTP was defined as the ability to play in a single regular-season NFL game after surgery. At the time of surgery, average age for all patients was 24.0 years and BMI 31.0. Results: Player positions included 8 wide receivers, 4 linebackers, 4 tight ends, 2 defensive tackles, 2 cornerbacks, 1 offensive tackle, 1 center, 1 tackle, 1 defensive end, and 1 quarterback. Seventy-six percent of players underwent operative fixation during their first 3 seasons. Forty-eight percent were diagnosed before or during their rookie (first) season. RTP was 100% for all players and 80% were still playing at time of publication. Three patients (12.0%) refractured and required revision surgery. Time until RTP was influenced by other variables and difficult to measure because many surgeries were performed early in the offseason. All 9 players who underwent surgery between July and October, and were therefore eligible to return to play in the same season, had an average RTP of 8.7 weeks (range 5.9-13.6). Conclusion: With an appropriately placed intramedullary screw and an aggressive rehabilitation protocol, early RTP was achievable with a low refracture rate in professional athletes. All NFL players in this series were able to return to play after surgery. We observed that these injuries were more likely to occur in the first 3 seasons of play and in wide receivers, linebackers, and tight ends. This at-risk subset of players may benefit from improved preventative measures. Level of Evidence: Level IV, retrospective case series. Keywords: Jones fracture, fifth metatarsal, athlete, return to play, NFL, football Introduction Proximal fifth metatarsal metaphyseal fractures are one of the most common foot injuries in the athletic population.26 These injuries are classified based on anatomic location as tuberosity avulsions (zone I), true Jones (zone II), or proximal diaphyseal stress fractures (zone III).14 True Jones fractures occur at the proximal fifth metatarsal metaphysis without extension distal to the fourth-fifth intermetatarsal articulation.14 Delayed healing is common in the case of zone II and III fractures because of the poor, retrograde blood supply of this region coupled with the mechanical forces it must withstand during activity.29,31 Athletes are especially predisposed to refracture and nonunion because of the repetitive stresses the bone must endure. Nonoperative treatment yields unfavorable results, particularly in high-demand athletes; therefore, primary fixation remains the standard treatment to expedite return to play and optimize outcomes.4-7,13,25 In the past, poor operative 1 OrthoCarolina Foot & Ankle Institute, Charlotte, NC, USA Corresponding Author: Craig R. Lareau, MD, OrthoCarolina Foot & Ankle Institute, 2001 Vail Avenue, Suite 200B, Charlotte, NC 28207, USA. Email: craig.lareau@gmail.com Downloaded from fai.sagepub.com at UNIV OF DELAWARE LIB on October 8, 2015 2 Foot & Ankle International outcomes have been attributed to premature return to play and inadequate screw size.26 Despite appropriate operative treatment along with advances in technique and implants, nonunion and refracture continue to occur in 4% to 12% of athletes.20,28 Our protocol for National Football League (NFL) players has been to perform limited incision intramedullary screw fixation for all proximal fifth metatarsal fractures, regardless of chronicity, displacement, and fracture completeness. We utilize an aggressive rehabilitation protocol with a goal of return to play (RTP) in professional competition at 8 to 10 weeks provided clinical and radiographic examinations are satisfactory. In this case series, we report the results of 25 consecutive NFL players who underwent percutaneous fixation of an acute proximal fifth metatarsal fracture with an indication-specific screw. Methods Prior to study initiation, this retrospective series was approved by an Institutional Review Board. Between 2004 and 2014, 25 NFL players who underwent screw fixation of an acute zone II or III proximal fifth metatarsal fracture by a single foot and ankle fellowship-trained orthopedic surgeon were identified. The average age for all patients was 24.0 years (range 20-31 years), and average BMI was 31.0 (range 25.8-38.8). For all players, fixation was achieved with a 5.5- or 6.5-mm Charlotte Carolina screw (Charlotte Carolina Jones Fracture System, Wright Medical Technology, Memphis, TN), ipsilateral iliac crest bone marrow aspirate (BMA), and demineralized bone matrix (DBM). Beginning in 2008, all players received BMA and DBM. The Charlotte Carolina screw is a partially threaded, solid stainless steel screw designed specifically for treatment of Jones fractures. All available clinic notes, operative reports, pre- and postoperative radiographs and computed tomographic scans, and physical therapy evaluations were reviewed. Patients with chronic injuries, those who had undergone previous operative treatment, had concomitant injuries, or had less than 6-month follow-up were excluded. Patient demographics were recorded as well as position played, fracture zone, fracture characteristics, time until surgery, ability to RTP, time until RTP, seasons played after surgery, complications, and reoperations (Table 1). RTP was defined as the ability to play in at least 1 regular-season NFL game after surgery, based on a previous study by Andrews et al.1 Number of games and seasons played postinjury was determined based on data available on the NFL website (http://www.nfl.com) and information obtained from the players’ athletic trainers. Differences between players who suffered refracture and those who did not were evaluated using Student t test and repeated-measures analysis of variance (SPSS, Chicago, IL), and differences in proportions between groups were evaluated using Fisher exact tests, with significance set at P < .05. Operative Technique Under ankle Esmarch tourniquet, a 1.5-cm longitudinal incision was made approximately 2-3 cm proximal to the base of the fifth metatarsal (Figure 1A) and a guide wire was inserted into the dorsal and medial aspect of the fifth metatarsal base adjacent to the cuboid articulation (“high and inside” starting point) (Figure 1B and C). The guide pin was carefully advanced across the fracture site under fluoroscopy taking care not to perforate the medial cortex. Next, a 3.2-mm cannulated drill was inserted over the guide wire and into the canal just across the fracture site. This was then removed and exchanged for a solid 3.2-mm drill, which was advanced on reverse to ream the canal and minimize the risk of cortical violation (Figure 2A and B). The canal was then sequentially tapped over a guide wire in 1-mm increments until adequate torque was achieved such that the surgeon felt the forefoot rotate slightly and screw length was measured radiographically (Figures 3A and 3B). Since 2008, our protocol for NFL players has been to harvest 30 to 40 mL of BMA from the ipsilateral iliac crest using a standard trochar and syringe system. The BMA was spun down over a period of 15 minutes into 4 mL of bone marrow concentrate using a separator system (MAGELLAN, Arteriocyte Medical Systems, Inc., Hopkinton, MA). This concentrate was then mixed with an injectable scaffold in DBM (Mini Ignite, Wright Medical Technology, Arlington, TN) which was injected through a separate small incision at the fracture site (Figures 4A and 4B) into the subperiosteal space within the periosteal envelope (particularly the plantar aspect) and within the medullary canal when possible. There is typically only space for 1-2 mL of graft. We utilized an aggressive rehabilitation protocol for professional athletes. Patients maintained non-weight-bearing precautions for 2 weeks following surgery then began weight bearing in a short controlled ankle motion (CAM) walker boot. Bone stimulators (Ultrasound Bone Healing System, Exogen, Durham, NC) were used (20 minutes/d) until radiographic healing. Once the fracture site was minimally tender, the patient used an accommodative shoe. When plain radiographs demonstrated bridging bone usually at 6 weeks (Figure 5A and B), the patient transitioned to a running shoe and began a run progression protocol followed by sport-specific integration. A clamshell orthosis (Figure 6) or turf toe plate was used during rehabilitation to minimize stress on the fifth metatarsal base. When the athlete returned to play, at an average of 8 to 10 weeks following surgery, a full-length orthosis with a lateral hindfoot post was utilized. Downloaded from fai.sagepub.com at UNIV OF DELAWARE LIB on October 8, 2015 3 Lareau et al Table 1. Patient Demographics and Operative Details for All Jones Fractures in NFL Players. Position Left / Days to played right surgery Age WR WR WR WR WR WR WR WR LB LB LB LB TE TE TE TE CB CB DT DT C DE OT QB T L R L L R R R L R L R L R L L R L R L L L L L R L 7 5 4 2 9 2 3 5 3 35 3 14 4 5 7 21 11 28 4 2 2 10 8 14 5 21 26 22 29 22 24 26 21 29 24 24 27 24 24 21 23 25 23 22 23 31 20 22 23 23 Height Weight (in.) (lb) 73 71 75 72 75 73 70 74 76 74 76 75 75 75 78 77 69 71 77 76 74 77 81 76 77 214 185 229 220 220 208 200 215 265 255 246 249 248 250 262 251 193 190 302 308 302 303 325 220 316 BMI 28.2 25.8 28.6 29.8 27.5 27.4 28.7 27.6 32.3 32.7 29.9 31.1 31.0 31.2 30.3 29.8 28.5 26.5 35.8 37.5 38.8 35.9 34.8 26.8 37.5 Screw Screw Season Fracture diameter length RTP of injury zone Typea (mm) (mm) Refracture (wk) 1st 3rd 1st 8th 1st 4th 4th 1st 7th 2nd 3rd 5th 2nd 1st 1st 2nd 3rd 2nd 1st 1st 8th 1st 1st 1st 1st 2 2 2 3 2 2 2 2 2 2 3 3 2 3 2 2 3 2 3 2 2 2 3 2 2 I CN C C I C CN C CN I C I I CN I I CN I CN I C I I CN CN 5.5 5.5 5.5 5.5 5.5 6.5 5.5 5.5 6.5 5.5 5.5 6.5 5.5 6.5 5.5 6.5 6.5 5.5 6.5 6.5 6.5 5.5 6.5 5.5 6.5 50 40 45 50 50 45 50 40 45 45 55 50 50 55 50 55 55 45 60 45 50 50 60 50 55 No No No No Yes No No No No Yes No No Yes No No No No No No Yes No No No No No 8 9.9 11.4 14.7 6 5.9 13.6 6 7 11.9 18.6 13.6 11.3 7 - No. of seasons since 6 2 5 2 1 3 2 1 5 3 1 1 6 1 1 8 2 1 4 4 2 1 1 3 1 Abbreviations: WR, wide receiver; LB, linebacker; TE, tight end; CB, cornerback; DT, defensive tackle; C, center; DE, defense end; OT, offensive tackle; QB, quarterback; T, tackle; respectively. a I, incomplete fracture; C, complete fracture; CN, complete, nondisplaced fracture. Results The most common positions played at the time of injury were wide receiver (32%), linebacker (16%), and tight end (16%). Player positions included 8 wide receivers, 4 linebackers, 4 tight ends, 2 defensive tackles, 2 cornerbacks, 1 center, 1 tackle, 1 quarterback, 1 defensive end, and 1 offensive tackle. Nineteen (76%) of the players underwent operative fixation during the time period between the pre-draft NFL Scouting Combine (a week-long showcase of college football players occurring every February) and their third season in the league. Twelve (48%) of the players were diagnosed before or during their rookie season. Forty-four percent of patients had incomplete injuries and 72% were true Jones zone 2 fractures. The average time between injury and surgery was 8.5 days (range 2 to 35 days). The average screw length was 50 mm (range 40-60 mm). Overall RTP was 100% for all players. Eighty percent (20 out of 25) were still playing at the end of the 2014-2015 season. Subgroup analysis of the relationships between position played, fracture zone, refracture, and union showed no significant differences, likely due to the small number of patients in each subgroup. Among players who underwent surgery between July and October and RTP during the same season was possible, the average RTP was 8.7 weeks (range 5.9-13.6 weeks). To date, the average number of seasons played postinjury was 2.7 (range 1-8). Two players were selected to participate in the Pro Bowl before injury and 2 different players achieved this status postoperatively. There were 3 players who had refractures (12%), two of which had CT confirmation of healing prior to reinjury. One occurred after more than 2 years and another after more than 6 months. All cases of refracture occurred in players with incomplete zone 2 fractures treated with 5.5-mm screws. All were able to return to play after screw exchange and iliac crest bone grafting. With regard to other complications, there were no instances of infection, delayed wound healing, sural nerve injury or neuritis, hardware failure, iatrogenic fracture, or symptomatic hardware necessitating screw removal. Downloaded from fai.sagepub.com at UNIV OF DELAWARE LIB on October 8, 2015 4 Foot & Ankle International Figure 1. (A) Incision marked 2 to 3 cm proximal to the base of the fifth metatarsal. (B) Ideal guide wire starting point “Inside” (medial) and (C) “High” (dorsal). Figure 2. (A) Intramedullary reaming with a solid 3.2-mm drill on oblique, and (B) lateral fluoroscopic views. Downloaded from fai.sagepub.com at UNIV OF DELAWARE LIB on October 8, 2015 5 Lareau et al Figure 3. (A) Ideal screw length is assessed both clinically and (B) radiographically. Figure 4. (A) Clinical and (B) oblique fluoroscopic views of BMA and DBM injection into and around fracture site. Discussion There has been ambiguity in the distinction between zone II and III fractures, dating back to the initial description by Sir Robert Jones in 1902 that included both fracture types.12 Because similar outcomes have been observed for these two zones, it has been proposed that they both be referred to as Jones fractures and treated in the same manner.3 Jones fractures are best managed in the athletic population with intramedullary screw fixation to expedite return to sport and minimize risk of refracture.5,13,18,19 Unfortunately, nonunion and refracture still occur in a small percentage of athletes as a result of the repetitive stresses endured by the proximal fifth metatarsal coupled with its tenuous blood supply. Currently, there is limited data regarding complication rates and RTP in professional athletes treated with modern techniques. Our series of 25 NFL players is the largest reported series of professional athletes with Jones fractures treated by a single surgeon with the same technique and an accelerated rehabilitation protocol. Our data demonstrate that 100% of players were able to return to play and 80% were most recently still in the league. We observed a similar playing experience pre and post-injury. This is consistent with the findings of Carreira et al who showed no significant difference in participation following Jones fracture based on the NFL Combine database for a single team over a 6-year period.2 Downloaded from fai.sagepub.com at UNIV OF DELAWARE LIB on October 8, 2015 6 Foot & Ankle International Figure 6. Clamshell orthosis used during rehabilitation to minimize stress on the metatarsal base. Figure 5. (A) Bridging bone across the fracture site visible on postoperative anteroposterior (AP) and (B) lateral radiographs. With an average return to play of less than 9 weeks, only three patients had refracture in our series, one occurring over 2 years postoperatively due to direct contact from another player. These players underwent revision procedures as described by Hunt et al.11 We did not observe any nonunions or other complications. Over half of the players in this series were wide receivers or linebackers, highlighting the frequency of occurrence of this injury in those playing these positions. Additionally, the majority of players had this injury during their first 3 seasons in the league and almost half occurred during the rookie season. This underscores the importance of educating this at-risk subset of players regarding pain that can represent impending fracture and considering preventative measures, such as clamshell orthoses and turf toe plates. Multiple factors have been attributed to poor outcomes after operative treatment of Jones fractures. Lee et al conducted two large series describing predictors of delayed healing and refracture in patients treated with tension-band wiring.15,16 In a series of 86 patients, it was demonstrated that stress fractures with a plantar gap greater than 1 mm take significantly longer to heal.16 Based on a series of 163 elite athletes, high BMI and radiographic protrusion of the fifth metatarsal head have a significant association with refracture after surgery.15 Therefore, the authors recommend that this subset of athletes should return to sport more slowly. There remains an ongoing debate regarding the time until RTP and the degree of healing that is necessary. Most believe that the fracture should be radiographically healed prior to RTP to minimize refracture. However, despite 100% clinical and radiographic healing, Wright et al observed 6 refractures on the day of return to full activity in athletes treated with 4.0- and 5.0-mm cannulated intramedullary screw fixation.32 This may have been due to undersized screws and the lack of functional bracing in this particular series. Similarly, Glasgow et al found that early return to play was associated with delayed union and refracture in patients treated with a 4.5-mm malleolar screw, indicating that this screw diameter did not provide sufficient support to allow healing.8 In our experience, some players who are pain-free and able to return to play have a persistent plantar and/or lateral gap with bridging trabeculation dorsally and medially. Breakage of 5.5- and 6.5-mm Downloaded from fai.sagepub.com at UNIV OF DELAWARE LIB on October 8, 2015 7 Lareau et al indication-specific screws has been exceedingly rare in patients treated at our institution because the bending rigidity of this intramedullary implant is proportional to its radius to the 4th power. Therefore, we rely on clinical examination and patient symptoms in addition to percentage of radiographic healing. There exists considerable variation in screw diameter, type, and material in different studies. We prefer stainless steel, solid, headed, partially threaded indication-specific large diameter (5.5 and 6.5-mm) screws for Jones fracture fixation in athletes. Only a handful of studies provide clinical outcomes in patients treated with these modern generation implants.11,17,20 Metzl et al reported greater than 95% union rates in patients treated with either traditional or indication-specific screws, with a higher number of adverse events in the traditional screw group.17 Nunley et al have performed two cadaveric studies demonstrating biomechanical superiority of an indication-specific screw over other implants.22,24 We do not recommend cannulated screws because of decreased fatigue strength and higher likelihood of refracture and nonunion.27,32 Headless screws are less likely to cause soft-tissue irritation21 but pose a challenge when screw removal is necessary. Variable pitch screws are inferior to partially threaded screws with respect to pull-out strength, fracture site compression and angulation.30 At our institution, we prefer to use the largest diameter screw that the fifth metatarsal can accommodate without fracture malreduction or distraction. A recent radiographic study demonstrated that the coronal diameter of the fifth metatarsal at its isthmus is greater than 4.5 mm in 81% of males and 74% of females.23 This confirms the need for a 5.5-mm or larger diameter screw for sufficient screw thread purchase. The shortest length screw with all threads just distal to the fracture site is optimal. This same study recommended that screw length remain less than the straight segment length, which is approximately 68% of the fifth metatarsal length and averaged 52 mm.23 A screw that is too long may abut the medial cortex as the metatarsal shaft bows laterally, resulting in distraction and varus angulation. Given the poor healing potential of the proximal fifth metatarsal, adjunct treatments including autogenous bone marrow aspirate and bone stimulation can be considered. Clinical studies have proven the efficacy of autogenous BMA for the treatment of nonunions.9,10 Although there is no high-quality data to justify this added expense in the general population, we believe that the benefits outweigh any risk in professional athletes under tremendous pressure to return to play as soon as possible. In our experience treating this injury, we have not observed any complications associated with these additional measures. Promising results have been achieved with the use of BMA and DBM in revision procedures for Jones fracture nonunion but future comparative studies are necessary to substantiate the benefits of these augments.11 The limitations of this study involve those inherent to a retrospective case series. Most studies pertaining to professional athletes are retrospective as a result of the small number of patients undergoing a specific procedure. In this transient population, it was not always possible to obtain radiographic images that demonstrated an exact date of fracture union because patients often followed up at other institutions. In addition, there was no control group consisting of patients undergoing a different procedure or nonoperative treatment. The benefit of each aspect of our treatment protocol (eg, screw type, BMA, functional bracing, and rehabilitation protocol) is not known. Lastly, no clinical outcome measure, such as SF-36, AOFAS, Foot Function Index, or visual analog scale, were recorded. These outcome measures are currently a standard part of our clinical intake forms but were not integrated during the data collection period for this study. Formal statistical analysis was not possible based on the small sample size and low complication rate. This study has several strengths. First, it is the largest study to date reporting outcomes of Jones fracture fixation in NFL players. Second, all 25 surgeries were performed by a single experienced surgeon based on the same treatment algorithm, operative technique, and postoperative protocol. Third, there were no cases of loss to follow-up. Although clinical outcome scores were not reported, the ability of professional athletes to return to play at their preinjury level is indicative of a high level of function. Although return to play data are commonly used to assess postoperative outcomes in professional athletes, there are a variety of factors that influence a football player’s ability to return to play. These include the occurrence of other injuries at a separate point in time (eg, knee injury when attempting to return to play after Jones fracture), position played, the point in a player’s career when the injury occurs (rookie vs 11th season), the amount of playing time received prior to injury, whether it occurred during free agency or a contract year, etc. Our time until return to play data is limited based on the fact that only a small subset of players underwent surgery immediately before or during the season. For the majority of players, surgery was performed early in the offseason. As a result, the time until return to play in a regular season NFL game was 5 to 8 months, far longer than when the player was cleared to return to full activity in practice and preseason games. Conclusion Professional American football players who undergo fixation of a Jones fracture using modern generation implants with BMA/DBM coupled with bone stimulators, an aggressive rehabilitation protocol and custom orthoses experienced a high rate of return to play and a low rate of refracture. This injury occurred more commonly in wide receivers, linebackers, and tight ends within their first 3 Downloaded from fai.sagepub.com at UNIV OF DELAWARE LIB on October 8, 2015 8 Foot & Ankle International seasons, particularly the rookie season, highlighting the potential need for injury prevention measures in this subset of players. Our experience suggests that physical examination and ability to return to play are as important as degree of radiographic healing. Future prospective studies including validated clinical outcome measures are necessary to draw more definitive conclusions. Authors’ Note No part of this study has been submitted or duplicated elsewhere prior. This study has been read and approved by all authors and each author believes that the manuscript is valid and represents honest work. Declaration of Conflicting Interests The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Robert B. Anderson, MD, reports Wright Medical Technology, Inc: paid consultant for a company or supplier, royalties from a company or supplier. Funding The author(s) received no financial support for the research, authorship, and/or publication of this article. References 1. Aune KT, Andrews JR, Dugas JR, Cain EL Jr. Return to play after partial lateral meniscectomy in national football league athletes. Am J Sports Med. 2014;42:1865-1872. http://dx.doi. org/10.1177/0363546514535069 2. Carreira DS, Sandilands SM. Radiographic factors and effect of fifth metatarsal Jones and diaphyseal stress fractures on participation in the NFL. Foot Ankle Int. 2013;34(4):518-522. http://dx.doi.org/10.1177/1071100713477616 3.Chuckpaiwong B, Queen RM, Easley ME, Nunley JA. Distinguishing Jones and proximal diaphyseal fractures of the fifth metatarsal. Clin Orthop Relat Res. 2008;466:1966-1970. http://dx.doi.org/10.1007/s11999-008-0222-7 4. Clapper MF, O’Brien TJ, Lyons PM. Fractures of the fifth metatarsal. Analysis of a fracture registry. Clin Orthop Relat Res. 1995;315:238-241. 5. DeLee JC, Evans JP, Julian J. Stress fracture of the fifth metatarsal. Am J Sports Med. 11(5):349-353, 1983. 6. Den Hartog BD. Fracture of the proximal fifth metatarsal. J Am Acad Orthop Surg. 2009;17:458-464. 7. Ekstrand J, van Dijk CN. Fifth metatarsal fractures among male professional footballers: a potential career-ending disease. Br J Sports Med. 2013;47:754-758. http://dx.doi. org/10.1136/bjsports-2012-092096. 8. Glasgow MT, Naranja RJ Jr, Glasgow SG, Torg JS. Analysis of failed surgical management of fractures of the base of the fifth metatarsal distal to the tuberosity: the Jones fracture. Foot Ankle Int. 1996;17(8):449-457. 9. Hernigou P, Poignard A, Beaujean F, Rouard H. Percutaneous autologous bone-marrow grafting for nonunions. Influence of the number and concentration of progenitor cells. J Bone Joint Surg Am. 2005;87:1430-1437. http://dx.doi.org/10.2106/ JBJS.D.02215. 10. Hernigou P, Poignard A, Manicom O, Mathieu G, Rouard H. The use of percutaneous autologous bone marrow transplantation in nonunion and avascular necrosis of bone. J Bone Joint Surg British. 2005;87(7):896-902. http://dx.doi. org/10.1302/0301-620X.87B7.16289. 11. Hunt KJ, Anderson RB: Treatment of Jones fracture nonunions and refractures in the elite athlete: outcomes of intramedullary screw fixation with bone grafting. Am J Sports Med. 2011;39:19481954. http://dx.doi.org/10.1177/0363546511408868. 12 Jones R. I. Fracture of the base of the fifth metatarsal bone by indirect violence. Ann Surg. 1902;35:697-700. 13. Kavanaugh JH, Brower TD, Mann RV. The Jones fracture revisited. J Bone Joint Surg Am. 1978;60:776-782. 14. Lawrence SJ, Botte MJ. Jones’ fractures and related fractures of the proximal fifth metatarsal. Foot Ankle. 1993;14(6):358-365. 15. Lee KT, Park YU, Jegal H, et al. Factors associated with recurrent fifth metatarsal stress fracture. Foot Ankle Int. 2013;34(12):16451653. http://dx.doi.org/10.1177/1071100713507903. 16.Lee KT, Park YU, Jegal H, et al. Prognostic classification of fifth metatarsal stress fracture using plantar gap. Foot Ankle Int. 2013;34(5):691-696. http://dx.doi.org/10.1177/1071100713475349. 17. Metzl J, Olson K, Davis WH, et al. A clinical and radiographic comparison of two hardware systems used to treat jones fracture of the fifth metatarsal. Foot Ankle Int. 2013;34(7): 956-961. http://dx.doi.org/10.1177/1071100713483100. 18.Mindrebo N, Shelbourne KD, Van Meter CD, Rettig AC. Outpatient percutaneous screw fixation of the acute Jones fracture. Am J Sports Med. 1993;21:720-723. 19. Mologne TS, Lundeen JM, Clapper MF, O’Brien TJ. Early screw fixation versus casting in the treatment of acute Jones fractures. Am J Sports Med. 2005;33:970-975. http://dx.doi. org/10.1177/0363546504272262. 20.Murawski CD, Kennedy JG. Percutaneous internal fixa tion of proximal fifth metatarsal jones fractures (Zones II and III) with Charlotte Carolina screw and bone marrow aspirate concentrate: an outcome study in athletes. Am J Sports Med. 2011;39:1295-1301. http://dx.doi.org/10.1177/ 0363546510393306. 21.Nagao M, Saita Y, Kameda S, et al. Headless compres sion screw fixation of jones fractures: an outcomes study in Japanese athletes. Am J Sports Med. 2012;40:2578-2582. http://dx.doi.org/10.1177/0363546512459460. 22. Nunley JA, Glisson RR. A new option for intramedullary fixation of Jones fractures: the Charlotte Carolina Jones Fracture System. Foot Ankle Int. 2008;29(12):1216-1221. http:// dx.doi.org/10.3113/FAI.2008.1216. 23. Ochenjele G, Ho B, Switaj PJ, et al. Radiographic study of the fifth metatarsal for optimal intramedullary screw fixation of jones fracture. Foot Ankle Int. 2015;36(3):293-301. http:// dx.doi.org/10.1177/1071100714553467. 24. Orr JD, Glisson RR, Nunley JA. Jones fracture fixation: a biomechanical comparison of partially threaded screws versus tapered variable pitch screws. Am J Sports Med. 2012;40:691698. http://dx.doi.org/10.1177/0363546511428870. 25. Porter DA, Duncan M, Meyer SJ. Fifth metatarsal Jones fracture fixation with a 4.5-mm cannulated stainless steel screw Downloaded from fai.sagepub.com at UNIV OF DELAWARE LIB on October 8, 2015 9 Lareau et al in the competitive and recreational athlete: a clinical and radiographic evaluation. Am J Sports Med. 2005;33:726-733. http://dx.doi.org/10.1177/0363546504271000. 26. Raikin SM, Slenker N, Ratigan B. The association of a varus hindfoot and fracture of the fifth metatarsal metaphyseal-diaphyseal junction: the Jones fracture. Am J Sports Med. 2008;36:13671372. http://dx.doi.org/10.1177/0363546508314401. 2 7. Reese K, Litsky A, Kaeding C, Pedroza A, Shah N. Cannulated screw fixation of Jones fractures: a clinical and biomechanical study. Am J Sports Med. 2004;32:1736-1742. 28. Roche AJ, Calder JD. Treatment and return to sport following a Jones fracture of the fifth metatarsal: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2013;21:1307-1315. http://dx.doi.org/10.1007/s00167-012-2138-8. 29.Shereff MJ, Yang QM, Kummer FJ, Frey CC, Greenidge N. Vascular anatomy of the fifth metatarsal. Foot Ankle. 1991;11(6):350-353. 30. Sides SD, Fetter NL, Glisson R, Nunley JA. Bending stiffness and pull-out strength of tapered, variable pitch screws, and 6.5-mm cancellous screws in acute Jones fractures. Foot Ankle Int. 2006;27(10):821-825. 31. Smith JW, Arnoczky SP, Hersh A. The intraosseous blood supply of the fifth metatarsal: implications for proximal fracture healing. Foot Ankle. 1992;13(3):143-152. 32. Wright RW, Fischer DA, Shively RA, Heidt RS Jr, Nuber GW. Refracture of proximal fifth metatarsal (Jones) fracture after intramedullary screw fixation in athletes. Am J Sports Med. 2000;28:732-736. Downloaded from fai.sagepub.com at UNIV OF DELAWARE LIB on October 8, 2015