Annual Report 2013/14 F inancial and Quality Accounts www.hacw.nhs.uk
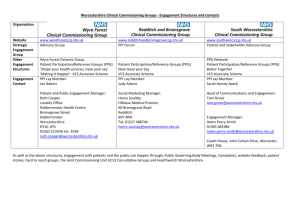
advertisement

Annual Report 2013/14 Financial and Quality Accounts www.hacw.nhs.uk 2 Annual Report 2014-15 Contents Message from the Chairman and Chief Executive About The Trust 04 06 Strategic Report 08 Plans for 2014/15 Sustainability report Performance against key performance indicators 10 11 16 Quality Accounts 22 Our Response to the Francis Enquiry Review of 2013/14 Other news …… 2013/14 Quality Account Priorities Review of 2013/14 - Patient Safety Our 2013/14 CQUIN Performance Looking Forward CQUINS for 2014/15 2013/14 Quality Account Technical Section – Mandatory Mandated Indicators 23 30 36 40 49 52 53 55 56 62 Financial statements 73 Operating and financial review (OFR) Annual Governance Statement Remuneration Report 92 103 115 Audit Committee Annual Report 2013/14 122 Details of Directors Glossary of terms used in Annual Report 125 128 3 Message from the Chairman and Chief Executive Arrow Valley, Redditch 2013/14 has been a good year for Worcestershire Health & Care NHS Trust with a number of high points and great achievements. Many of these are featured in our Look Back document which accompanies this Annual Report. The priority for providing high quality care has always been central to the Trust’s vision and values. The focus on being able to show how we are doing this, and measure whether we are getting it right, has never been greater than now. This year’s Quality Account summarises the progress we have made during the year, shows some of the measures we use to tell us how close we are to meeting our goals and puts forward the quality improvements we intend to make in 2014/15. The Quality Account provides an opportunity to evidence our commitment to sustaining services of the highest quality which make a real difference to the health and wellbeing of the people we serve. However, like all NHS providers, we face the challenge of maintaining and where possible improving quality at the same time as having to make unprecedented financial 4 savings. This really tests the ability of our staff to think and work differently, to be imaginative in solving the problems we face and to really question whether what we are doing is always the best thing for our patients. We have risen to the challenge and firmly believe that we will continue to do so. The approach taken is broadly three-fold:• Firstly, to transform our services so that they reflect patient expectations and the national policy directions to provide more care closer to home; • Secondly, to make sure that as an organisation we work in ways which maximise efficiency and deliver the best possible value for money; • Thirdly, to seek opportunities to strengthen our business in line with national policy and ensure we remain efficient and sustainable. In relation to transforming services we have already made changes, following extensive consultation, to our short breaks service for young people and have plans to re-configure some of our Child Development centres so Annual Report 2014-15 that they offer a better overall service for more people. Since our last report, we have opened a new ‘state of the art’ in-patient unit, New Haven in Bromsgrove, for older people with dementia and other forms of mental illness whilst at the same time investing in community mental health services so that fewer beds are required on our other wards. In 2014/15 we anticipate a strengthening of the role our community hospitals play so that patients with more complex conditions can be treated closer to home. Our transformation agenda will always involve extensive patient and public consultations so that noone’s voice is lost. In terms of efficiency and value for money, our SMART programme was launched during the year to focus on non-pay costs and to date we have achieved reductions in travel and energy costs, and have improved our procurement processes for the goods and services we need to buy. SMART working can deliver much more and contribute greatly to the sustainability of the Trust. Chris Burdon Chairman Opportunities for growth taken during the year enabled us to maintain our total income, offsetting tariff reductions and other changes made to our base contacts. In order to maintain progress towards achieving Foundation Trust status, thereby enabling our future direction to be determined locally through our members and governors, we need to continue to provide high quality services whilst maintaining financial sustainability. We anticipate a Chief Inspector of Hospitals visit shortly to assess quality, and sustainability will be dependent upon achieving further efficiency savings to build upon the £15m already delivered over the last two years. We have every confidence that with the on-going commitment and support of our staff our organisation is capable of meeting the ever increasing challenges ahead. We confirm that to the best of our knowledge the information in this report is accurate. Sarah Dugan Chief Executive 5 About The Trust Responsive: Focusing on the needs and expectations of people using our services Worcestershire Health and Care NHS Trust was established on 1 July 2011 in response to the Department of Health’s ‘Transforming Community Services’ initiative. The Trust manages the vast majority of the services which were previously managed by Worcestershire Primary Care NHS Trust’s Provider Arm, as well as the mental health services that were managed by Worcestershire Mental Health Partnership NHS Trust which sought dissolution as part of the process. Community and mental health services are provided to a population of approximately 560,000 across Worcestershire’s 500 square miles, covering the city of Worcester together with the towns of Bewdley, Bromsgrove, Droitwich, Evesham, Kidderminster, Malvern, Pershore, Redditch, Stourport, Tenbury Wells and Upton-Upon-Severn. The Trust works closely with the three local Clinical Commissioning Groups (Redditch & Bromsgrove, Wyre Forest and South Worcestershire), Worcestershire Acute Hospitals NHS Trust, Worcestershire County Council and a number of other statutory and non-statutory organisations. The Trust has defined a set of values that clarify what it believes in and how it will behave: Courageous: Displaying integrity, loyalty and the courage to always do what is right Ambitious: Striving to innovate and to improve through effective teamwork Empowering: Empowering people to take control of their own health and wellbeing Supportive: Enabling our staff to achieve their full potential and take pride in the services that they deliver The Trust Strategic Goals explain what the Trust aims to achieve, these goals are: • We will always provide an excellent patient experience • Our services will always be safe and effective • We will work in partnership to improve the integration of health and care • Our organisation will be efficient, inclusive and sustainable These four strategic goals have been translated into specific corporate objectives that relate to the strategic goals. Ten Corporate Objectives have been defined and these are: • To stimulate a revolution in the way we engage with patients • To redesign clinical pathways • To ensure patient safety • To ensure seamless care through integrating services • To strengthen leadership within our services • To develop our workforce • To improve our use of technology • To develop business opportunities • To deliver our efficiency programme • To make effective use of our estate CARE S Courageous 6 Ambitious Responsive EMpowering Supportive Annual Report 2014-15 Our Services: Bringing together the range of community and mental health services previously provided by Worcestershire Primary Care NHS Trust and Worcestershire Mental Health Partnership NHS Trust has offered opportunities to improve integration and partnership working which are central to the Trust’s objectives. The services provided by the Trust are divided into five service delivery units (SDUs): • Community Care Community Care provides in-patient, out-patient and community services on a locality basis to adults and older adults across Worcestershire. With five Community Hospitals, four older adult mental health in-patient wards, district nursing and podiatry, as well as numerous specialist services, this is the Trust’s largest service delivery unit. • Adult Mental Health The Adult Mental Health Service Delivery Unit provides mainly community and in-patient services to adults with mental health needs across Worcestershire, with community mental health services being delivered through integrated health and social care teams. • Children, Young People and Families The Children, Young People and Families Service Delivery Unit provides general child health and specialist mental health services to children, young people and their families across Worcestershire. • Specialist Primary Care The Specialist Primary Care Service Delivery Unit provides sexual, dental, and offender health services. • Learning Disabilities The Learning Disabilities Service Delivery Unit provides adult and children’s respite, out-patient and community contact activity for people with Learning Disabilities and their families, mainly for the population of Worcestershire The area we serve: The Trust provides a wide range of community and mental health services across the county. Services are focused on supporting patients to live independently at home, reducing the need for patients to be admitted into hospital. Where admission is appropriate the Trust makes use of Community Hospitals and mental health in-patient units across the county to provide care as close to home as possible. 7 Strategic Report Looking back This section summarises the Trust’s performance during 2013/14 and the key developments that took place during the year. During 2013/14, the Trust successfully delivered a range of national, regional and local performance targets. Highlights included: • 18-week referral to treatment waiting times targets achieved. • Minor Injuries Unit’s target of admitting, transferring or discharging patients within 4 hours of arrival achieved. • C.difficile trajectory achieved with only 5 cases against a target of 10. • Delay transfers of care target for Mental Health patients achieved. • Target achieved for patients on Care Programme Approach, discharged from a Mental Health inpatient unit and followed up within 7 days. In addition, the Trust delivered on all of the CQUINs agreed for 2013/14 and met all of its financial statutory duties. With regards to developments, 76 priority schemes were identified in 2013/14. Of these, 58 were delivered, 7 were longer term schemes and on plan at the end of the year, 3 were removed or revised, whilst 8 slipped and have been rolled forward to 2014/15. Looking ahead Our plans for the future seek to improve the patient experience by reducing the transfer of patients between services, teams and professions. Reducing unnecessary boundaries between services was one of the motivations for establishing the Trust with its broad portfolio and some of the early successes demonstrate the benefits that can be achieved. Examples include improved transition arrangements for CAMHs patients and more effective care for patients with dementia that are admitted to community hospitals and/or supported by our community teams. 8 Extending these principles of integration is a consistent theme across the range of improvements planned over the next 5 years. Ultimately some care may need to be provided in hospital. This may be through an urgent unplanned episode or through a planned care pathway. Regardless of the reason for admission the Trust will support transfer of care as close to home as possible as soon as it is clinically appropriate. The Trust has identified a series of work programmes that focus on achieving this aim through improvements in specific care pathways and the integration of services. The major programmes have been identified as ‘transformational programmes’ as they will contribute significantly to a change in the provision of care across the Trust and in some cases the broader health economy. In addition to the major transformational programmes the Trust is committed to continuous improvement across all services which are reflected in smaller scale service redesign in each Service Delivery Unit. The major transformational programmes are: • Sub acute care in the community - strengthening the role of community hospitals, increasing the acuity of patients that can be safely managed in community hospitals and establishing a more integrated model of care. • Care closer to home - the development of integrated community teams serving a neighbourhood, • Older Adult Mental Health, • Adult Mental Health, • Children and Family Services, • The development of integrated services including Health and Social Care integration. Annual Report 2014-15 Service capacity and developments: The Trust is working with commissioners to agree the extent to which its vision for the future can be supported through specific developments in out of hospital care. In the absence of specific agreements, the Trust has modelled a number of different future scenarios and ensured that the actions are defined that ensure the organisation remains sustainable under each scenario. These scenarios are illustrated in the graph below. Figure 1: Alternative growth projections Alternative Futures 400,000 350,000 300,000 250,000 200,000 150,000 100,000 50,000 2013/14 2014/15 2015/16 2016/17 2017/18 2018/19 Scenario 1 (limited investment) Scenario 2 (progressive development of the community) Scenario 3 (major strategic change) Scenario 4 (significant disinvestment) The development of a 5-year plan for the health and social care economy supports the Trust Board development plan. In particular, there is a commitment to developing stronger community based services. There are a number of strategic groups that are driving this broad strategic direction including the Health and Well Being Board, the Well Connected Programme Board and the Urgent Care Strategy Board. These groups and their programmes of work support the Trust’s strategic goals and will be used to shift the Trust’s overall position to one of growth. Strategic Report 9 Plans for 2014/15: This sets out the organisation’s priorities and plans for 2014/15 to 2015/16 and includes the key work programmes that have been agreed for the various corporate departments and the 5 service delivery units. Detailed action plans, with quarterly milestones, have also been developed and these will be monitored via the Trust’s performance review process. In addition to these priorities and work programmes, the Trust has to deliver against a range of statutory targets and standards including: • 18-week referral to treatment waiting time targets • Zero tolerance of waits over 52 weeks • MIU attenders admitted, transferred or discharged within 4 hours • Compliance with mixed sex accommodation • CPA follow up within 7 days • Psychological therapy access • MRSA zero tolerance • Delivery of agreed C. difficile trajectory Over the next two years the Trust anticipates income to be: Workforce Plan Over the next two years the Trust will implement a range of efficiency measures which will have a net impact of reducing the overall budgeted workforce from 3,414 WTE to 3,140 WTE. These changes are delivered through a series of projects; each of which has a detailed project plan and is assessed for potential impact on quality through the Trust Quality and Equality Impact process. Plans are developed working with staff and the Trust also has a formal process for engaging staff before changes are implemented. The range of projects also results in changes to roles and skill mix. Foundation Trust Application Since its establishment in July 2011, the Trust has had a programme in place to achieve Foundation Trust status. The programme has helped to strengthen governance arrangements and ensure the organisation has a capable Board. The Trust will continue its path towards FT status during 2014/15. It is anticipated that the Trust will be reviewed by the Chief Inspector of Hospitals in the second quarter of 2014/15 and is working towards being licenced as a Foundation Trust in Quarter 1 of 2015/16. 2014/15 income – £167.8m 2015/16 income – £165.4m The Trust plans to deliver an efficiency programme that will achieve an annual surplus in line with Monitor requirements, specifically: 2014/15 – £2.5m surplus, 1.5% of turnover CIP £7.7m 2015/16 – £2.6m surplus, 1.6% of turnover CIP £7.7m 10 Annual Report 2014-15 Sustainability report: The incentive to reduce the effect we have on our environment is stronger than ever; doing so not only helps to reduce the impact of climate change but also saves money and improves our efficiency. Our staff and patients benefit too: sustainable lifestyles, with more active travel and less energy intensive diets, are healthier lifestyles. The Trust emits 8,957 tonnes of CO2 equivalents a year (based on 2010/11 consumption figures), costing us £3.8 million. Our target for reduction figure is 7,466 tonnes CO2e by 2015. To date, the Trust has implemented the following projects supporting this ambitious target. • Hydrotherapy pool cover, pump replacement and control modifications at Osborne Court • Cavity Wall Insulation at the Robertson Centre and the Lucy Baldwin Unit, Kidderminster Hospital • Installation of renewable technology in large scale capital projects where feasible (Solar Panels at Newhaven) • Energy efficiency (lighting and sensors) infused in large scale capital projects (Hub project at Princess of Wales Community Hospital) • Installation of LED lighting throughout the Trust premises • Continuing sub metering programme (Steam meter at the Robertson Centre) • Rainwater Harvesting at Link Nurseries • Zone Control Heating at Evesham Community Hospital • Maintenance upgrades (Eco set points, control modifications etc.) • Continued estate rationalisation. Strategic Report Contracts The Trust currently procures its energy supply requirements through the Government Procurement Service (GPS). Its priority is to provide procurement savings for central government, health and the wider public sector. By procuring energy through the GPS we get the best value energy on the market (due to the large buying power of the GPS). The GPS ensure tariff charges are competitive, not least because of the overall buying power but also savings from wholesale procurement and procuring in advance. The Trust now has energy contracts in place with the following government preferred energy suppliers: • Corona (contract to 31/03/2016) • British Gas (contracting to 2017) • EDF (contract to 31/03/2016) Due to existing/rolling contracts and supplier transfer rejections the Trust has struggled to transfer several sites (Malvern Hospital, Pershore Hospital, Beacon Centre, 71 Ludlow Road, Tudor Lodge and Kidderminster Health Centre). The Trust has put these on new competitive energy contracts for a period to coincide with the expiry of the framework contracts so a complete re-tendering exercise can be undertaken at that point. 11 Travel Marketing and Communications have launched the Trust’s new SMART brand and logo. SMART is really about us working more efficiently to save money and a SMART Board has been established to identify specific initiatives to generate savings, including a focus on new ways of working which could potentially have a beneficial impact on our CO2 footprint. The focus on reducing staff travel during 2013/14 is expected to reduce our CO2 emissions. Whilst it is difficult to separate the impact of agenda for change re-imbursement rates, the estimated reduction from 2012/13 to 2013/14 is 42,810 miles (this equates to 14.4 tonnes of CO2). Figure 1: Carbon Dioxide Emissions resulting from Trust operations The green line in the graph illustrates that the Trust is reducing its emissions (Actual) against both the “Do Nothing” and “Target emissions” lines. At the end of the 2012/13 financial year we calculated that the CO2 emissions had reduced to 8597 tonnes against the trajectory target of 8296 tonnes. The graph also shows the estimated 2013/14 year end position. 12 Annual Report 2014-15 Resource 2011/12 2012/13 2013/14 15,587,000.00 17,665,000.13 18,545,803.24 3,185.20 3,609.84 3,934.31 29.09 0.00 0.00 tCO2e 0.01 0.00 0.00 Use (kWh) 0.00 0.00 0.00 tCO2e 0.00 0.00 0.00 6,315,871.49 6,875,111.12 6,637,322.65 3,434.43 3,682.93 2,853.05 6,619.64 7,292.77 6,787.36 £ 1.1m £ 1.5m £ 1.4m Use (kWh) Gas tCO2e Use (kWh) Oil Coal Use (kWh) Electricity tCO2e Total Energy CO2e Total Energy Spend Table 1: Carbon emissions from Energy The table above illustrates that our measured energy carbon emissions have decreased by 505.41 tonnes this year. However, this is primarily due to the increased proportion of renewable electricity we are receiving from one of our electricity suppliers and more accurate consumption data from buildings we occupy on the Acute Trust land. Water Mains m3 tCO2e Water & Sewage Spend 2011/12 2012/13 2013/14 101390 70760 61804 35 24 56 £235,704 £190,806 £166,655 Table 2: Water Consumption for the Trust Our water consumption has continued to reduce in comparison to previous financial years. This is due to improvements in billing, fault reporting and estate rationalisation. Strategic Report 13 Figure 4: Trust waste production Our waste production has continued to reduce in comparison to previous years. This is due to changes to classification of the Trust waste streams, treatment/disposal of waste and improved quantification. Some of the Trust’s 2013-14 figures are estimated based on ERIC data. The entity’s employees: The entity’s employees: including an account of the entity’s equal opportunities policy. Also required is an analysis of the gender distribution in the categories; Directors, Other senior managers and Employees. Category of Trust employees Sum of WTE Headcount at 31.3.2014 Directors 7.00 15 Female 3.00 4 Male 4.00 11 Employee 3,158.06 4,098 Female 2,693.16 3,533 Male 464.90 565 SMT 17.60 18 4.60 5 13.00 13 3,182.66 4,131 Female Male Grand Total 14 Annual Report 2014-15 Social and community issues: Up until July 2013 the Trust had a Community Engagement Committee, which was a sub-committee of the Trust Board. The Community Engagement Team developed a Community Engagement Strategy, which has successfully taken forward the work of the subcommittee. Over the last twelve months engagement and consultation work has been focused according to impact, interest and investment. To this end, the Trust has conducted full consultations with patients, carers and representatives of interested groups, who would be impacted by proposed service changes. The comments received were collated, reported on and fed into the creation of new care pathways and, where necessary, has been shared with the Health Overview and Scrutiny Committee and Children and Young People Overview and Scrutiny Panel. The Trust has also worked with interested groups and individuals and has offered those who want to be involved in the work of the Trust, lots of different opportunities from attendance at forums and events, to taking part in working groups, to sharing their patient stories and taking part in films for staff training. The level of interest shown has allowed the Trust to set up a Quality Account Working group, an Organisational Values Working group and led to regular and increased attendance at forum meetings. creation of a new Partnership Forum and a Youth Board whilst continuing to reach other ‘seldom heard groups’ such as the travelling community. Business Information and History: Worcestershire Health and Care NHS Trust was established on 1 July 2011 to manage the vast majority of the services which were previously managed by NHS Worcestershire’s Provider Arm, as well as the mental health services that were managed by Worcestershire Mental Health Partnership NHS Trust. Bringing together the range of services provided by the two organisations has offered opportunities to improve integration and partnership working which are central to the Trust’s objectives. The Trust is a community based provider of comprehensive health and social care services, expertise and choices for people with a range of health needs and/or disabilities. These services are provided in a wide range of community settings. These include people’s own homes, community clinics, outpatient departments, community inpatient beds, prisons, schools and GP practices. We also provide in-reach services into acute hospitals, nursing and residential homes and social care settings. One off quality events have considered such matters as the Francis Report, the Sub-Acute pathway and the Complaints process. The Trust has also sought to reach out to more patients and carers and in addition has sought the views and opinions of staff, through the Clever Together digital campaign. As a result of a survey of the Trust’s members over 200 more members indicated they were keen to get involved by attending forums, sitting on interview panels and taking part in patient led assessments of the clinical environment. The Trust has maintained its links with a variety of other groups and organisations. In total the Trust has engaged with 50 groups, non-statutory and statutory organisations during the last year. 2013/14 saw the Strategic Report 15 Performance against key performance indicators: Care Programme Approach (CPA) follow up contact within seven days of discharge from hospital The Trust’s performance in this area is measured on a quarterly basis as part of the Trust Development Authority’s Accountability Framework indicators. In order to achieve the highest level of compliance in this area (“Performing”) the Trust must achieve 95% of inpatients on CPA, followed up within seven days of discharge from hospital. The Trust is pleased to report that a level of ‘Performing’ was consistently achieved, with scores over 97%, for each quarter in 2013/14. The quarterly scores are shown in Table below. Percentage of people on CPA followed up within 7 days of discharge from hospital Performance Threshold 95% or over Actual Quarterly Performance 2013/14 Quarter 1 Quarter 2 Quarter 3 Quarter 4 98.9% 97.2% 99.0% 99.5% Minimising Delayed Transfers of Care Measuring delayed transfers of care forms part of the Trust Development Authority’s Accountability Framework, and helps the Trust to assess the impact of community-based care in facilitating timely discharge from hospitals. People should receive the right care in the right place at the right time and we must ensure that people move on from the hospital environment once they are safe to transfer. The indicator seeks to encourage organisations to work in partnership to minimise the number of patients remaining in hospital settings who are ready for discharge. The definition is as follows: “the number of patients (acute and non-acute, aged 18 and over) whose transfer of care was delayed, expressed as a percentage of the number of consultant and non-consultant led occupied beds.” In order to achieve the highest level of compliance in this area (“Performing”) the Trust must keep delayed transfers of care to 7.5% or less during each quarter. The Table below shows the Trust’s position for 2013/14. The Trust is pleased to report that a level of ‘Performing’ was consistently achieved, with scores under 5.1%, for each quarter in 2013/14. We routinely monitor our performance in this area across all services and where performance consistently falls below target we implement recovery plans that are monitored by the Trust Board. We actively work with our partner organisations to minimise any delays. 16 Annual Report 2014-15 Percentage delayed transfers of care Performance Threshold 7.5% or less Actual Quarterly Performance 2013/14 Quarter 1 Quarter 2 Quarter 3 Quarter 4 4.1% 4.5% 4.3% 5.1% The number of admissions to the Trust’s mental health acute wards that were gate kept by the Assessment and Home Treatment Teams When service user admissions are assessed (“gate kept”) by their local Assessment and Home Treatment Team, service users have the opportunity to be treated in their own home. Wherever possible we offer service users the choice to be supported in their own home as an alternative to hospital admission. This is recognised as best practice and monitored by the Trust Development Authority’s Accountability Framework. The method for calculating performance is as follows: “the number of admissions to the Trust’s acute wards (excluding internal transfers between wards, patients recalled from community treatment orders and patients on leave under Section 17 of the Mental Health Act) that were gate kept by the Assessment and Home Treatment team prior to admission. An admission has been ‘gate kept’ if the team assessed the service user before admission and involved them in the decision making process that resulted in the hospital admission. This is expressed as a percentage of total admissions to the Trust’s acute mental health wards.” In order to achieve the highest level of compliance (“Performing”) the Trust must ensure that 95% of admissions to acute mental health wards were gate kept by the Assessment and Home Treatment Teams. The 2013/14 performance is shown in the Table below. The Trust is pleased to report that a level of ‘Performing’ was consistently achieved, with scores over 97%, for each quarter in 2013/14. Percentage of admissions to mental health acute wards that were gate kept Performance Threshold 95% or over Strategic Report Actual Quarterly Performance 2013/14 Quarter 1 Quarter 2 Quarter 3 Quarter 4 98.8% 98.7% 97.4% 97.7% 17 Percentage of patients readmitted to hospital within 28 days of being discharged monitor success in avoiding (or reducing to a minimum) readmissions following discharge from hospital. Measuring the percentage of patients who were readmitted to hospital as an emergency within 28 days of being discharged provides information to help us The following table shows the quarterly percentage of all inpatient admissions that were readmitted in an emergency within 28 days of the previous discharge. Quarter 1 Quarter 2 Quarter 3 Quarter 4 Ages 0-14 0.0% 0.0% 0.0% 0.0% Ages 15+ 2.1% 2.5% 1.1% 2.9% Patient experience of community mental health services To improve the quality of services that the Trust delivers, it is important to understand what people think about their care and treatment. One way of doing this is by asking people who have recently used our services to tell us about their experiences. To assist with this, each year a survey of people aged 18 and over accessing community mental health services is conducted and collated by the Care Quality Commission. A questionnaire was sent to 850 people who accessed community mental health services between 1st July 2012 and 30th September 2012. A total of 269 people responded, giving a 32% response rate for the Trust. This compares to the national response rate of 29%. An excerpt of the survey results, specifically covering the patient’s experience of contact with a health or social care worker, is shown in the table below. The full report has been published by the CQC and is available on their website. Patient experience of contact with a health or social care worker Listening: for the health or social care worker seen most recently was listening carefully to them. Involvement: for the health or social care worker seen most recently taking their views into account Trust and confidence: for having trust and confidence in the health or social care worker seen most recently Respect and dignity: for being treated with respect and dignity by the health or social care worker seen most recently Time: for being given enough time to discuss their condition and treatment with the health or social care worker seen most recently Overall experience of contact with the health or social care worker seen most recently. Trust’s 2013 score. (score out of 10) Compared with the national response, we scored: 9.0 Better 8.6 2.5% 8.5 About the same 9.5 About the same 8.4 About the same 8.8 About the same Figures taken from the CQC website: http://www.cqc.org.uk/survey/mentalhealth/R1A 18 Annual Report 2014-15 The Trust’s performance against the 2013/14 key national targets Objective Perform Under Current Performance (March 2014) 95% 95% 94% 98.3% 18 18 20 14.3 Maximum time of 18 weeks from point of referral to treatment in aggregate patients on an incomplete pathway 92% 92% 91% 99.9% MIU Clinical Quality - Unplanned Reattendance Rate 5% 5% 6% 1.0% MIU Clinical Quality - Total time in MIU (95th Percentile) 235 235 240 97 MIU - Maximum waiting time of four hours from arrival to admission/transfer/ discharge 95% 95% 94% 100.0% MIU Clinical Quality - Left without being seen (LWBS) rate 5% 5% 6% 0.4% MIU Clinical Quality - Time to initial assessment (95th Percentile) 15 15 > 15 11.0 MIU Clinical Quality - Time to treatment (minutes - median) 60 60 80 11 Infection Control - Methicillin-Resistant Staphylococcus Aureus (MRSA) 0 0 1 1 YTD Avoidance of Mixed-Sex Accommodation (Community Hospitals) 100% 100% 90% 100% Venous Thromboembolism (VTE) Screening 100% 95% < 90% 97.4% Target/ Limit Measure Maximum time of 18 weeks from point of referral to treatment in aggregate non admitted 18 Week Referral To Treatment (RTT) - 95th Percentile (Weeks Waiting) To Ensure Patient Safety Statutory basis: This Order establishes a National Health Service trust called the Worcestershire Health and Care National Health Service Trust. The Order sets out the functions of the Trust, the number of executive and nonexecutive directors of the Trust, the operational date (the date on which the Trust assumes all its functions) and the accounting date of the Trust. It dissolves the Worcestershire Mental Health Partnership National Health Service Trust, which was established by the Worcestershire Community and Mental Health National Health Service Trust (Establishment) Order 1999. Further explanation: There are no items in the financial statements considered to have a strategic significance for 2013/14. In terms of Strategic Report Performance Threshold the Going Concern considerations the Trust auditors have accepted that the Trust has an excellent track record of delivering its key financial duties and has a robust Long Term Financial plan that includes a detailed cost improvement programme. Equality and Diversity and Human Rights We recognise that everyone is diverse and value all individuals for their contribution to the Trust through their experience, knowledge and skills. The Trust fully endorses the principles of Equality and Diversity in respect of Trust employees, service users (patients, carers, visitors and communities) and partners (health and social care economy, voluntary/third sector etc.). Our Equality and Inclusion Policy embraces the Equality Act 2010, setting the standards and expectations of the 19 Trust both internally and externally regarding the values and commitment of the Trust to deliver high quality healthcare that is fair and equitable. The Policy will be reviewed to ensure it is current and reflects changes in legislation, for example changes to marriage which now incorporates same sex couples. The Public Sector Equality Duty is a requirement on all public sector organisations to make society fairer by tackling discrimination, advancing equality of opportunity and fostering good relations regardless of age; disability, gender reassignment, marriage civil partnership, pregnancy and maternity, race, relation or belief, sex and sexual orientation, known as the 9 protected characteristics. We take every opportunity to strengthen our approach to equality and diversity through design, delivery and review of all of our functions, policies and practices. This is achieved by undertaking: • Equality Analysis (also known as Equality Impact Assessment), a way of identifying the impact the policy/ function may have on the protected characteristics and persons/groups who do not share these characteristics but could experience inequality e.g. carers, the homeless or travelling communities and record the evidence to demonstrate the consideration given and take action to eliminate or reduce any negative impact that may exist. • Equality Delivery System (EDS) - designed by the NHS for the NHS, to improve equality performance and deliver better outcomes for patients, communities and staff which are personal, fair and diverse. Central to the EDS, the Trust is required to analyse our equality performance against 18 outcomes grouped under four goals: • Better health outcomes for all • Improved patient access and experience • Empowered, engaged and inclusive staff • Inclusive leadership. The Trust engages with a wide range of stakeholders from across protected groups, patient groups, community organisations, the voluntary sector and statutory organisations and other interested groups to grade our performance, set equality objectives and develop an action plan. This is an on-going and continuous undertaking. 20 To ensure the best healthcare delivery possible our Interpreting and Translation services have been reviewed and developed to reflect the changing landscape of languages spoken in Worcestershire. Polish is the most common spoken language after English and is spoken in all 6 districts of Worcestershire. This is then followed by Urdu and closely by Panjabi (predominately in the Redditch and Worcester districts). There are a further 22 languages where 300 people or more speak that language in Worcestershire. A new booking system means that Trust staff have access to interpreters and translators which includes British Sign Language and Easy Read translation 24 hours a day, seven days a week providing (services) face-to-face or telephone services. The Trust is committed to ensuring employees work in an environment characterised by dignity and respect. Every person working for the Trust has a personal responsibility for implementing and promoting Equality, Diversity & Human Rights. It is expected that employees will treat each other, service users and partners in the same way with a view to creating a service that is fair and accessible to all. For further information please visit: http://www.hacw.nhs.uk/our-services/equality-anddiversity/ Emergency Preparedness: The Trust continues to work with local responders to ensure that it is able to provide the best possible response to a major emergency. There is a Major Incident Plan in place which is regularly tested and reviewed in line with the requirements of the NHS Commissioning Board EPRR Framework. The Trust also has a Business Continuity Plan which ensures that critical services can still be delivered in exceptional circumstances. The Trust has an established Emergency Planning, Resilience and Response (EPRR) sub-committee which provides assurance that we are able to meet our statutory and contractual requirements in relation to EPRR. Annual Report 2014-15 Principles for Remedy: Our Complaints Policy abides by the good practice ‘Principles for Remedy’ and aims to produce reasonable, fair and proportionate responses to complaints. The principles are: • Getting it right • Being customer focussed • Being open and accountable • Acting fairly and proportionately • Putting things right • Seeking continuous improvement Getting involved: We are committed to engaging patients, service users, their families and carers, members of the community and local organisations in the planning, development and monitoring of Trust services. The Trust wants to hear the views and concerns of the communities it serves. Involving the community is important because it assists us in making decisions and shaping services to meet the needs and preferences of those who use them. One way the Trust seeks to do this is by holding forums across the county. Forums consist of a presentation by Trust staff about service developments, and the members give opinions about changes, suggest ways to improve the experience of those people who use our services, and also advise on developments or changes occurring in each locality. Anyone who would like to come along to a forum, you would be warmly welcomed. You may be a patient, carer, member of the public or involved in a group or organisation. You may be interested in all our services or only one of them. Your voice and opinions matter. Strategic Report Looking after our staff: As services change, the roles for some of our staff may change too. Some may be required to learn new skills to meet the demands of a new or different role and in those instances the Trust will support the individual to help make sure they are equipped to do the job. Our commitment is, where possible, to re-deploy affected staff into alternative posts, and re-train people as required so our high standards are maintained. In short we want to support the staff we currently have. For those staff whose roles change we fully recognise the importance of supporting them and their managers throughout. Over the next five years our workforce numbers overall will reduce but we aim to manage this through redeployment and planned turnover, such as retirements. Whistleblowing: As a Trust we are committed to ensuring staff are encouraged to flag up anything which concerns them. In fact one of the key messages to staff following the Francis Report has been to take a step back and look critically at services to see if they are up to standard. We have also made a point of re-iterating our whistleblowing policy to staff so they are comfortable with the process and the options available should they feel something needs bringing to attention. We pride ourselves on being an open and transparent organisation. We are confident that we have a culture and an environment that does encourage staff to come forward but we know we need to keep on top of this. Our message to staff is clear: if it’s not right, speak up! This is in keeping with one of our key values which are about displaying integrity, loyalty and the courage to always do what is right. 21 Quality Accounts Statement on Quality from the Chief Executive Providing high quality care has always been central to the Trust’s vision and values and has always driven our decision making. Reviewing what we have achieved and whether we are getting it right for our patients is a key step towards ensuring we constantly improve. This Quality Account summarises the progress we have made in the last year, shows some of the measures we use to tell us whether we are making progress, and outlines our priorities for quality improvement for the next 12 months. It is our opportunity to share our commitment to sustaining the highest quality services that make a genuine and meaningful difference to the people who use our services. A key milestone in the last year was the publication of our outline response to the findings of the Francis Inquiry in June 2013. We held a special patient forum event to review the findings of the report, and held a series of staff workshops which helped us reflect on the learning in the report and develop an action plan that applied this learning and improvements to our own services. We recognise that there are areas for improvement, but our action plan will help to ensure that quality continues to be an absolute priority in the months ahead. We continue to review in detail all of the patient feedback that we receive locally and thank all of our patients for taking the time to share their thoughts with us. While it is vitally important that we learn from national reports and local feedback where care has not been of a high standard, we should also take time to be proud of our achievements. Some of these are set out in this Quality Account. Achieving high quality care is only possible through the activities of a highly skilled and committed workforce and I would like to thank all of our staff for their on-going commitment and dedication to providing the best possible service we can for our patients. 22 Chief Executive “I believe to the best of my knowledge and belief the information in this document is accurate.” Sarah Dugan Chief Executive Statement on Director’s Responsibilities There are proper internal controls over the collection and reporting of indicators and the data underpinning the indicators is robust and reliable. Introduction to the Quality Account This Quality Account is Worcestershire Health and Care NHS Trust’s report to the public about the quality of the services we provide. It summarises our challenges and achievements from the last year, setting out how well we did in achieving the five selected priorities from 2013/14 as well as other quality improvement measures. The quality of services we deliver is monitored closely throughout the year by the Trust Board using a raft of indicators, patient experience feedback, and staff involvement and by visiting and getting involved with clinical services. Further information on the way we track our services can be seen on our website and at a variety of public forums throughout the year. Looking ahead we have defined three Quality Account priorities for improvement over 2014/15 which are described further on in this document. Firstly though, we would like to take you through a review of some of the things the Trust has been doing over the last 12 months. Annual Report 2014-15 Our Response to the Francis Enquiry February 2013 saw the publication of Robert Francis QC’s final report of the Mid Staffordshire NHS Foundation Trust Public Inquiry. In November 2013 the Government responded in their report ‘Hard Truths’. Since then there have been a number of high profile reports about quality in the NHS, all of which shine a light on care failings. website and complaints are reported to every Trust Board. • We continue to work with the patient/carer groups and forums who provide important feedback on experience of using our services. At the Trust’s Quality and Safety Committee in March 2013, usual business was suspended to allow members of the committee to review the recommendations applicable to the Trust and consider the actions that we needed to take as an organisation. • We are piloting values based recruitment and appraisals and there is a new monthly staff award to recognise those staff that go beyond the call of duty. What have we done since the publication of the Francis Report? • We have undertaken a comprehensive review our staffing establishment and taken action to ensure the staffing levels are safe. • We reviewed ourselves against all of the 290 recommendations in the Francis Enquiry. • We have developed the Patient Safety Walkabout programme, which gives frontline staff an opportunity to raise patient safety issues with Board members. • We developed an action plan to monitor ourselves against agreed actions and reported on this at Quality and Safety Committee and Trust Board. The action plan is published on the Trust website. We reviewed ourselves against the recommendations in the subsequent Berwick, Keogh and Clywd reports and incorporated this into the plan. • We have held a number of focus groups, where we listened to the views of our staff, our patients and our members. • We have reviewed and re-launched our Raising Concerns at Work Policy (Whistle-blowing Policy). • We have improved our response times to complaints. A summary of all complaints are published on the Trust Quality accounts • We have improved our incident reporting culture. • Every Trust Board meeting includes a Patient Story. This provides patients with the opportunity to tell the Board directly about their experiences of using Trust services, both positive and negative. • We have launched a patient experience/feedback website and have undertaken the ‘Pause for Thought’ campaign with staff. Many staff also took part in ‘walking in their shoes’ initiative. • We are developing an ‘early warning system’, so that teams who may need support can be identified earlier. The following provides a high level update on progress with the Trust’s action plan as of March 2014. 23 Issues Identified Leads Outstanding Actions CULTURE The NHS and all who work for it must adopt and demonstrate a shared culture in which the patient is the priority in everything done (Francis) Healthcare employers recruiting nursing staff should assess candidates’ values, attitudes and behaviours towards the well-being of patients and their basic care needs (Francis) The development of the ‘cultural barometer’ should continue. This will determine if a workplace is suffering from a problem with staff attitudes or organisational approach. (Clywd/Hart) Associate Director of HR Ensure vision and values understood by staff through: • Recruitment of staff based on values • Recruitment of staff based on capacity for care and compassion • Appraisal process supports measuring staff against values • Set out clear expectations in job descriptions and contracts ‘Pledge to Care’ to incorporate ‘6 Cs’ – launch day to be held in June followed by inaugural nursing committee meeting. Development of in-house bank will to help ensure agency and bank staff have the same value ethos as permanent staff. Complete assessment of levels of achievement in Equality Delivery System in June. Head of Organisational Development STANDARDS OF CARE: Deputy Healthcare Director of professionals should be Nursing prepared to contribute to the development of, and comply with, standard procedures in the areas in which they work (Francis) Providers should invest in building capability within their organisations to enable staff to contribute to improvement of the quality and safety of services to patients (Berwick) 24 Trust Nursing Committee to be established, reporting to Quality and Safety Committee. Nursing metrics to be rolled out to more services. Competency framework in development to ensure staff have the right skills and knowledge for their role. Multi-disciplinary Mortality Group to be established to review clinical records for evidence of any omissions/ issues with care. Planned Review/ Completion Date September 2014 July 2014 Progress/Evidence – March 2014 Values based recruitment and appraisal testing underway. Staff Friends and Family Test and pulse surveys undertaken for ‘temperature checks’ with associated action plans. Extensive, well-evaluated training programmes for team leaders. Mentoring system in place. Whistleblowing policy relaunched and re-badged. Monthly staff award for ‘living the values’. In-house bank established with staff working to Trust policy/cultures. On line nursing metrics published by ward in spring 2014. Metrics now being rolled out to other services. Screens to be in place on all wards by summer 2014 displaying staffing levels and associated safety data for that clinical area. External reviews by CCGs positive. Successful nursing documentation launched in community hospitals January 2014 – now roll out to other services. Audit records of unexpected deaths reported quarterly. Clinical audit programme on track. Mandatory training levels now above 90% across Trust. Annual Report 2014-15 Issues Identified Leads STAFFING LEVELS: Boards and leaders of organisations should utilise evidence-based acuity tools and scientific principles to determine the staffing they require in order to safely meet their patients’ needs. They should make their conclusions public and easily accessible to patients and carers and accountable to regulators. Healthcare organisations should ensure that staff are present in appropriate numbers to provide safe care at all times and are wellsupported (Berwick). Director of Quality (Executive Nurse) DATA QUALITY: The first priority for any organisation charged with responsibility for performance management of a healthcare provider should be ensuring that fundamental patient safety and quality standards are being met. Such an organisation must require convincing evidence to be available before accepting that such standards are being complied with (Francis) Mortality data Keogh Improve data quality (p16) Head of Quality Governance Quality accounts Planned Review/ Outstanding Actions Completion Date Regular staffing levels reports July 2014 to Board. Staffing levels made available to public. Consideration of impact on community teams staffing levels. Progress/Evidence – March 2014 Establishment levels ascertained using acuity tools. Dashboards and processes introduced in readiness for full publication of staffing levels in June 2014. Staff using Ulysses to report staffing level incidents. These are directly reported to the Director of Quality, Deputy Director of Nursing and Medical Director. Screens on entrance to wards to be fitted. These will display staffing levels and patient safety data. Staffing levels to be published on Trust website. Quality Goals dashboard and Patient Safety Incident reports to be refined to include Statistical Process Controls and Pareto 80/20 principles. Data Quality Group to develop work plan to include data quality assurance measures for identified data sets. Data analysis to be fed back to clinical teams more clearly. Review of quality of data in line with Monitor’s Quality Governance Assurance Framework (QGAF) action. July 2014 Review of quality metrics dashboards underway with revised dashboard in draft ready for July Board meeting. Data quality improvement plan. Service Line Reports in development with assistance from clinical teams. Mortality Group established to review mortality across the Trust. Service Line Reporting in development. 25 Issues Identified Leads Outstanding Actions FINANCIAL PRESSURES: Impact and risk assessments should be made public, and debated publicly, before a proposal for any major structural change to the healthcare system is accepted (Francis) Placing the quality of patient care, especially patient safety, above all other aims. (Berwick) STAFF DEVELOPMENT, TRAINING AND LEADERSHIP: The NHS should continually and forever reduce patient harm by embracing wholeheartedly an ethic of learning. (Berwick) Staff need to be adequately trained, supervised and supported to deal with complaints effectively. (Clwyd/Hart) Director of Quality (Executive Nurse) Competency framework in development to ensure staff have the right skills and knowledge for their role. Medical Director Complaints workshops to continue to be delivered to staff in areas where high number of complaints/PALS issues received. Deputy Director of Nursing Trust Nursing Committee to be established, reporting to Quality and Safety Committee. 26 Nursing metrics to be rolled out to more services. Competency framework in development to ensure staff have the right skills and knowledge for their role. Multi-disciplinary Mortality Group to be established to review clinical records for evidence of any omissions/ issues with care. Planned Review/ Completion Date July 2014 July 2014 Progress/Evidence – March 2014 Supervisory ward managers now in place. Leadership training delivered – these courses receive excellent feedback from staff. Mandatory training compliance running at near 90% - benchmarking shows this is above average. On line nursing metrics published by ward in spring 2014. Metrics now being rolled out to other services. Screens to be in place on all wards by summer 2014 displaying staffing levels and associated safety data for that clinical area. External reviews by CCGs positive. Successful nursing documentation launched in community hospitals January 2014 – now roll out to other services. Audit records of unexpected deaths reported quarterly. Clinical audit programme on track. Mandatory training levels now above 90% across Trust. Annual Report 2014-15 Planned Review/ Issues Identified Leads Outstanding Actions Completion Date Increase use of the family and July 2014 Head of PATIENT EXPERIENCE/ Quality friends test (awaiting national INVOLVEMENT Governguidance). The patients must be Develop exit questionnaire as ance the first priority in all standard for patients who are of what the NHS does discharged from service. Head of (Francis) Communi- Quality Account priority in Patients and their carers ty Engage- relation to young people acshould be present, ment and cessing Sexual Health services to be undertaken. Patient powerful and involved Develop universal admisat all levels of healthcare Involvesion and discharge processes organisations from wards ment which includes good comto the boards of Trusts. munication with carers, (Berwick) family and other health care providers to ensure seamless Trusts should ensure that services. there is a range of basic information and support available on the ward for patients (Clwyd/ Hart) COMPLAINTS: Trusts must constantly promote to the public their desire to receive and learn from comments and complaints; constant encouragement should be given to patients and other service users, individually and collectively, to share their comments and criticisms with the organisation (Francis) Respond directly, openly, faithfully, and rapidly to safety alerts, early warning systems, and complaints from patients and staff (Berwick) Patients, carers and members of the public should be confident that their feedback is being listened to and see how this is impacting on their own care and the care of others (Keogh) Quality accounts Quality Governance Manager Improve assurance and evidence that learning from complaints is shared across the organisation. Revised Complaints Policy to be ratified and monitored for effective implementation. Duty of Candour Policy to be ratified and monitored for effective implementation. Survey of complainants who have received response to assess their experience of the Trust’s complaints system and approach. July 2014 Progress/Evidence – March 2014 Patient surveys evidenced high satisfaction with quality of care. Increased number of patient surveys. Webpage now live. Carers Policy in place. Patient representatives on many groups in the Trust. Patient representative volunteers assisting with patient suveys. ‘Walk in Their Shoes’ day. Pause for Thought campaign in March 2013. Focus groups Offender Healthcare services. Community Engagement – multiple initiatives and established Patient Forums. Patient Action Group established and helping collect patient surveys. Patient stories to board. Complaints training delivered to services who receive the highest number of complaints. Improved response times to complaints. Quality of complaints responses improved. Additional training provided to Investigating Officers. Safety Alert system in the Trust to be transferred to the Ulysses system. This will provide additional assurance that appropriate actions are taken. 27 Issues Identified Leads Outstanding Actions INCIDENTS AND SERIOUS INCIDENT REPORTING: Reporting of incidents of concern relevant to patient safety, compliance with fundamental standards or some higher requirement of the employer needs to be not only encouraged but insisted upon (Francis) Head of Quality Governance Adverse Incident Policy to be ratified and monitored for effective implementation. Promote understanding through clinical teams that line managers need to give constructive feedback to staff who report incidents. Shared learning from incidents reported through Team Brief. Evidence greater triangulation of incident data with complaints and claims and risk registers in quality reports. All leaders concerned with NHS healthcare – political, regulatory, governance, executive, clinical and advocacy – should place quality of care in general, and patient safety in particular, at the top of their priorities for investment, inquiry, improvement, regular reporting, encouragement and support (Berwick) Employers need to improve their support of staff around implementing guidance on reporting of serious incidents (Berwick) 28 Planned Review/ Completion Date Juy 2014 Progress/Evidence – March 2014 Incident reporting culture improved over year. Detailed incident reports provided to Trust committees and clinical teams. Safety Thermometer audits undertaken each month. Service line reporting in development to promote triangulation of data. Annual Report 2014-15 Issues Identified Leads WHISTLEBLOWING: A “duty of candour” should be imposed on NHS staff (Francis) Director of Quality (Executive Nurse) Every healthcare organisation and everyone working for them must be honest, open and truthful in all their dealings with patients and the public, and organisational and personal interests must never be allowed to outweigh the duty to be honest, open and truthful (Francis). Embracing transparency unequivocally and everywhere, in the service of accountability, trust, and the growth of knowledge (Berwick) Planned Review/ Outstanding Actions Completion Date Duty of Candour policy in de- July 2014 velopment based on national review. To be ratified. Staff to be supported to be open with patients and families in line with Duty of Candour – including explanations of why services might be constrained. The Trust web site will be used to make available to the public information regarding our care and performance. Nursing Staffing Levels in Inpatient Areas It is widely accepted that staffing levels are linked to the safety of care and that staffing shortfalls increases the risk of patient harm and poor quality care. Over the last year in the Trust we have developed a process for capturing staffing levels on a shift by shift basis on each of the 10 community hospital wards and the 6 wards across adult mental health and older adult mental health. The aim is to support and reinforce the ability and judgement of healthcare professionals and managers in decisions on staffing levels both on a daily basis and in the longer term. Quality accounts Progress/Evidence – March 2014 Whistleblowing Policy revised and rebadged into ‘Raising Concerns’ with aim of making it more accessible. Duty of Candour Policy in draft and out to consultation. This allows ward staff to use their professional judgement to determine if the ward activity levels are safely met by the skill mix and staffing levels on the ward. The tool we are using will be monitored daily by senior managers to ensure that appropriate decisions are being made and used as a mechanism for ensuring staffing issues are escalated appropriately. The Executive Nurse, Deputy Director of Nursing, relevant Senior Managers and Matrons will have access to a 7 day prospective summary view of a database to enable them to closely monitor staffing levels and to ensure appropriate mitigating actions are taken where required. Further detailed information regarding safe staffing levels in the Trust is available on the internet, and each ward is to have large television screens to display real time data at the entrance to each ward. 29 Review of 2013/14 April saw the formal introduction of the new NHS structure as outlined in the Health and Social Care Act 2012. It means that control for much of the NHS budget is in the hands of Clinical Commissioning Groups, or CCGs. The CCGs are responsible for commissioning, or buying, hospital, community and mental health services for the people of Worcestershire. They are overseen by a national organisation, NHS England. Other changes to the NHS structure saw Public Health fall under the remit of the local authority, Worcestershire County Council. A new health and social care ‘consumer champion’, HealthWatch has also been established. Locally, HealthWatch Worcestershire is chaired by Peter Pinfield and provides a channel for the public to comment and raise concerns about services across the health and social care system. Public Backing for our Vision The vast majority of those who attended our engagement events last spring said they were in support of our strategy to care for more people in or closer to home. We ran a round of hour-long events across the county which together attracted 100 people. A questionnaire handed out at the events shows support for the Trust’s direction of travel. It asked whether people supported the vision for more care in or closer to home, and whether they remained supportive if that had the potential for leading to fewer beds in our community hospitals. Just over 90% of those who completed the questionnaire said they were in favour of care in or closer to home, with 60% in support if that led to a bed reduction. Trust’s Secure Suite Improving Mental Health Care for County Figures released earlier in the year showed The Trust’s place of safety suite is helping to lower the number of patients being detained in police custody. The figures are collected when someone is detained under section 136 of the Mental Health Act 1983. This is for the person’s own protection and so they can be medically assessed. When a person is detained they have to be taken to a place of safety which could be a specialised secure suite, a hospital or a police cell. The Trust’s latest numbers show that 87% of people detained in a place of safety were taken to the specialised suite, with only 8 and 5 per cent going to police custody and hospitals respectively. The Trust’s secure suite was opened in 2007 at the Elgar Unit, Newtown Hospital in Worcester, catering for the entire county. Steve Goddard, Lead Acute Mental Health Practitioner for the Trust, said: “We feel we’ve made significant improvements around the detention of people under the police powers of section 136. This is reflected in the number of people taken to Newtown as opposed to police custody. This is a far more appropriate place to be when they are experiencing a crisis and prevent criminalisation of mental health.” New Haven – a New Kind of Facility The New Haven mental health unit opened in Bromsgrove on the site of the town’s community hospital. This unit has changed the way older people with mental health illnesses receive care and treatment in an impatient environment. New Haven is a true centre of excellence which serves the whole county. It has 30 beds which benefit those with varying degrees of dementia including Alzheimer’s, acute depression, acute anxiety and psychosis. Designed to inspire recovery and provide a stimulating environment, New Haven is unique in its design for a number of reasons: 30 Annual Report 2014-15 • Each patient has their own en-suite bedroom which will help create a ‘home from home’ environment and help ensure patients retain independence, privacy and personhood. Each room includes a memory box which is unique to each patient and provides added mental stimulus which will aid recovery. The rooms also provides a pleasant environment for families to visit and spend time with their loved one. • Large open courtyards and an allotment give patients the opportunity to go outdoors and enjoy spending time in pleasant surroundings. • People with dementia often purposefully walk (wander) and in their minds they are fulfilling a purposeful activity such as picking children up from school. Long corridors are not designed to support this and can often lead to agitation and frustration. New Haven has been specially designed with circulation loops, which allows the patient to walk freely around the building. Along the way special points of interest have been built in, including a 1960s themed launderette, which will provide an interactive and stimulating stop on their journey, reducing agitation, frustration and anxiety. • Art can be used to provoke thoughts and to stimulate memory and is a key part of the design of the building. An arts group was set-up to ensure the design of the building and the artwork included in and around it supports the ‘home from home’ and the ‘outdoors in’ theme. Projects include working with local artists on the creation of memory panels which feature words and objects which are important to them. In February Ruth May, lead nurse for NHS England for the Midlands and East Region visited New Haven. She was extremely impressed with the care that was provided to our patients and the environment we were operating in. She went as far to say it was “stunning” and could only recall one or two facilities nationwide that she thinks could match ours for team approach and physical environment. Quality accounts Trust’s Mental Health Employment Scheme Bucks Trend More people who have mental health issues are finding jobs through our employment programme, bucking the results of a national review released in July. Research carried out by the King’s College London suggested that the recession was having a profound impact on people with mental health problems. Between 2006 and 2010, the rate of unemployment for those with mental health problems rose twice as much as for other people - from 12.7% to 18.2%. Men and those with low levels of education were particularly affected, the study said. However our mental health employment team are reversing this trend and have reported major success in finding employment opportunities for its service users over the last 12 months. The number of paid jobs entered by service users has increased to 84, a 60% increase from 2011/12. This has contributed to the Trust’s Individual Placement and Support service, which is responsible for supporting service users to gain work experience and ultimately get paid jobs, being accredited as a national centre of excellence. Jobs that people have been found have ranged from catering and laundry work, to care work, teaching and engineering with aerospace. Pete Jordan, Worcestershire Health and Care NHS Trust’s Service Manager for the Mental Health Employment and Reablement Service, said: “Many of our people have previously held down good jobs before experiencing mental health difficulties. What we do now is to have an employment worker based in each of our mental health teams. They work alongside the clinical staff to help rebuild people’s confidence and target potential employers. The key issue is whether people want to work and if they do, it is our job to give them hope and make this happen”. 31 CAMHS Service Celebrates a Year of Achievement We reported how major improvements to Worcestershire’s Child and Adolescent Mental Health Service (CAMHS) have been made, a year after the service was re-designed. Worcestershire Health and Care NHS Trust’s CAMHS team celebrated a year since a re-design with reduced waiting times for service-users with the average wait for a first appointment down to five weeks compared to 18 eighteen weeks prior to the re-design, which is notable improvement. Fran Tummey, CAMHS Clinical Manager for Worcestershire Health and Care NHS Trust, said: “Staff across CAMHS have worked hard to make the much needed changes to the service and we now believe we offer a more focussed mental health service with the changes made based on user feedback. We will not rest on our laurels and will continue to improve the experience our children and young people and families receive when they are referred.” As well as reducing waiting times for the children and adolescents, results from a survey have shown that the majority of service users feel a positive impact on their mental health after seeing staff. The survey results showed that 78 per cent of Worcestershire children and young people who access CAMHS reported their difficulties were ‘much better’ or ‘a bit better’ after receiving a service. Staff Survey – What our Staff Told Us The Trust currently employs 4131 staff equating to 3182.66 Whole Time Equivalents. Nurses make up the largest professional group of staff followed by additional clinical services staff (clinical support staff ). Our workforce is generally representative of our community in terms of ethnicity diversity with 12.24% of staff classifying themselves as having an ethnic origin other than White-British. 32 We understand that our workforce has a direct impact on the quality of services provided and the experience of patients. To this end we place great emphasis on staff engagement, staff development and staff support. We monitor mandatory training and appraisal rates closely as we expect all of our staff to have the necessary skills and support to do their jobs well. We run Leadership Development Programmes which are very well evaluated, and promote a culture of strong clinical leadership. During the year we have progressed well with our service transformation to meet the needs of community services in the future. The results of the 2013 NHS National staff survey were formally released on Tuesday 25 February 2014. 422 responses were received from staff that took part in the sample survey (random sample of 850 were sent questionnaires) which resulted in a response rate of 50% which is average for mental health/learning disability trusts in England and compares with a response rate of 50% for the Trust in the 2012 survey. We have responded to the findings of the staff survey and produced an action plan that is being implemented. The top 5 ranking scores from Staff Survey were: • The number of staff receiving health and safety training in last 12 months. • The number of staff experiencing harassment, bullying or abuse from patients, relatives or the public in last 12 months. • Effective team working. • The number of staff believing the trust provides equal opportunities for career progression or promotion. • The number of staff reporting errors, near misses or incidents witnessed in the last month. The top 12 most improved areas from 2011 to 2012: • Percentage of staff having equality and diversity training in last 12 months • Percentage of staff having well-structured appraisals in last 12 months • Percentage of staff appraised in last 12 months • Percentage of staff having well-structured appraisals in last 12 months • Percentage of staff appraised in last 12 months Annual Report 2014-15 • Percentage of staff able to contribute towards improvements at work • Percentage of staff receiving job-relevant training, learning or development in last 12 months • Percentage of staff feeling satisfied with the quality of work and patient care they are able to deliver • Staff recommendation of the trust as a place to work or receive treatment • Effective team working • Percentage of staff reporting errors, near misses or incidents witnessed in the last month • Fairness and effectiveness of incident reporting procedures Going forward we are undertaking regular local staff surveys, and will be asking all staff whether they would recommend the Trust as a place to work and whether they would recommend the services to family and friends. More information about our staff is contained in the main Annual Report document. Seal of approval for County’s Mental Health Teams Services which support people across Worcestershire who have mental health problems were given a seal of approval by a national accreditation scheme. The services accredited were: • Holt Ward • Cromwell House • Hadley PICU • Harvington • Hill Crest • Keith Winter Close • Crisis Assessment Team • Home Treatment Teams covering Wychavon, Malvern and Worcester The programme provides quality assurance for service users, carers, commissioners, regulators and staff. It is only awarded to services that that have undergone a rigorous programme of assessments to ensure they are of high quality. Quality accounts Derek Hammond, Clinical Lead for Adult Mental Health, said: “This accreditation is the equivalent of a Kite Mark or a gold standard and is only awarded to those which deliver the highest quality services. It should provide service users, families, carers and the general public reassurance and confidence that people who need these services will get the very best care and support possible.” External Visits and Inspections The Care Quality Commission and our commissioners undertake visits to a variety of Trust services throughout the year to spend time with patients and staff and gather information to assure them that our services are safe and well managed. These visits and inspection can be announced (i.e. where the Trust is notified of them beforehand) or unannounced. The visits and inspections bring increased benefits to the Trust, and help to provide assurance on the continuous improvement in the quality and safety of our services. Following an external inspection the visiting body will produce a report and action plans are implemented in relation to any recommendations arising from the visit. CQC Visits The following locations were visited by the CQC during 2013/14 specifically to monitor our compliance with the Mental Health Act: • Witley Ward, Older Adult ward, Kidderminster • Keith Winter Close, Adult recovery ward, Bromsgrove • Holt Ward, Adult acute ward, Worcester • Harvington, Adult acute ward, Kidderminster • Hill Crest, Adult acute ward, Redditch • Athelon, Older adult ward, Worcester All of these visits have taken place on an unannounced basis, and there have been no common themes requiring addressing by the Trust noted by the CQC inspectors. Inspectors have been largely complimentary about the ward environment and staff attitudes to patients. As an 33 example, Holt was referred to as being “light, spacious and welcoming”, patients told inspectors that staff were “caring, friendly and helpful”. Hill Crest was “bright, spacious and clean” and patients felt safe. Patients on several of the wards told inspectors that they would recommend the wards to family and friends. The CQC are changing their approach to mental health regulation and inspection. Future inspections will be undertaken by teams rather than individuals and will consider services as a whole, rather than focussing on specific areas of care as they do currently. Offender Healthcare Inspections HMP Hewell In June 2013 the CQC undertook an unannounced follow up inspection of HMP Hewell, following on from an inspection in November 2012. The CQC looked at the personal care and treatment records of people who use the service, took advice from their pharmacist and reviewed the action plan, which explained how the staff have improved the areas they highlighted during their previous visit . The CQC didn’t identify any areas of concern and they recognise that some improvements are the subject of further work by HMP estates staff, and took this into account HMP Oakwood In June, the CQC and Her Majesty’s Inspector of Prisons (HMIP) undertook an unannounced inspection of the healthcare provision in HMP Oakwood. The CQC advised the Trust of a failure to comply with Regulation 13 (Management of Medicines) of the Health and Social Care Act (2008) Regulations 2010 (the Regulated Activities Regulations 2010). The Trust recognises the severity of the concerns found during the inspection, and we are extremely regretful that our services did not meet our own expected standards of care. We implemented swift and thorough improvement actions, and asked prisoners for their thoughts on how the services should be improved. 34 The CQC re-inspected HMP Oakwood in October 2013 and lifted the warning notice. We have since made further improvements and have sustained safe, good quality care for patients in HMP Oakwood. We are in close contact with the NHS England Local Area Team, The Trust Development Authority, the Pharmacy provider and the Prison Director to ensure there is a partnership approach to sustaining the improvement actions. We now undertake regular patient surveys and follow up with a ‘You Said, We Did’ leaflet to prisoners to maintain better communication and involvement. The South Staffordshire Area Team and NHS England undertook a visit to HMP Oakwood in November 2013 and noted many improvements. Our learning from the events at HMP Oakwood have been reviewed for relevance to HMP Hewell and HMP Long Lartin, and to services in the rest of the Trust. HMP Long Lartin The South Staffordshire Area Team and NHS England undertook a visit to HMP Long Lartin in November 2013 which produced largely positive findings, particularly in relation to multi-disciplinary working. Commissioner Visits The following locations were visited by the CCG during 2013/14 in order that the CCGs could gain assurance around the quality of care. The visits were a mixture of announced and unannounced: • The Princess of Wales Hospital, Bromsgrove • Community Enhanced Care Team, Pershore • Elgar Unit, Holt Ward, Athelon and Hadley, Newtown, Worcester • Malvern Community Hospital • Evesham Integrated Care Team • Evesham Community Hospital • Tenbury Minor Injuries Unit • Pershore Community Hospital • Tenbury Community Hospital The Joint Commissioning Unit undertook an announced visit to Churchview respite services in Bromgsrove. Annual Report 2014-15 The outcome from the vast majority of inspections has very positive and it could be said that this is the most common theme of the inspections. Where issues or concerns are raised, in most cases, actions to remedy them are very straightforward to implement and achieve. Action plans are implemented following all inspections to address any issues raised. The implementation of the Action Plans is monitored by the Quality and Safety committee. CQC Quality and Risk Profiles As part of their monitoring of providers’ compliance with the essential standards of quality and safety, the CQC produces a Quality and Risk Profile (QRP) which gathers together information about a provider’s possible risks. The profiles are produced 8 times a year. We have maintained a low overall risk score in the QRPs during the year. West Midlands Quality Review Service peer review programme for long term conditions 2013 was not intended as an inspection or performance management tool. The WMQRS programme confirmed several areas for improvement ,many of which had already been highlighted by the Trust .The programme also highlighted the unusual position in Worcestershire in that the majority of specialist teams are employed by the Acute Trust. At the time of the review programme several streams of work were planned or had commenced to address these areas for improvement; it was also a period when teams were integrating and not yet established. The report has assisted the health economy with prioritising areas for improvement. The greatest concern appeared to be around the model for specialist care for people with chronic neurological conditions, which was a common theme for the region in the WMQRS overview report. Representatives from across the health economy have developed plans and ideas for improving the care provision of people with long term conditions. As part of an on-going process, the representatives regularly review these plans together. The full reports are available on the WMQRS website: http://www.wmqrs.nhs.uk/publications The West Midlands Quality Review Service (WMQRS) visited Worcestershire in March 2013 to look at the quality of care for people with long-term conditions (LTC) across the local health economy, i.e. Worcestershire Health & Care Trust, Worcestershire Acute Trust, commissioners, primary care and linked services. They measured services against quality standards, which reflected national guidance. The LTC care pathways reviewed were chronic neurological conditions (such as Parkinson’s disease, multiple sclerosis, epilepsy), diabetes, COPD (Chronic Obstructive Pulmonary Disease), heart failure and multiple long term conditions. This peer review programme aimed to help organisations to improve the quality of clinical services in a developmental and supportive way, through acting as a `critical friend’ and Quality accounts 35 Other news …… Carole Shortlisted for HSJ Award Carole Clive, Nurse Consultant for Infection Prevention & Control, was announced as one of ten shortlisted nationally for the Clinical Leader of the Year Award, which is one of the categories in this year’s Health Service Journal (HSJ) Awards. Over 1000 entries were received for awards and Carole said she was “shocked and delighted” to have been initially nominated and then shortlisted. She also paid tribute to her team saying: “it is testament to the work that the team undertake across the Trust and county to ensure high standards of infection prevention and control and me being shortlisted is recognition of everyone’s efforts and achievements.” Sandra Brennan, Director of Quality & Director of Infection Prevention & Control at the Health and Care Trust, added: “It is typical of Carole to be modest about her achievements. She is highly regarded by staff across the Trust.” Admiral Nurses Celebrate 10-year Anniversary Local carers and health professionals helped celebrate the 10 year anniversary of Worcestershire’s dedicated army of Admiral Nurses. Worcestershire Admiral Nurses was launched in Wychavon in 2003 supporting family carers who look after people with dementia. The service has since spread and are now the only county-wide Admiral Nursing service in the UK. An event in the Guildhall, Worcester saw carers, professionals and representatives from local health organisations come together to pay tribute to the team and mark this milestone. A number of carers who have been supported by Admiral Nurses attended the event and one of them, Cheryl Hudson, whose father lived with dementia, was a key speaker at the event. She praised the local Admiral 36 Nurses for the wonderful support and guidance offered to her and her family and she paid special tribute to the team’s lead, Helen Springthorpe. Another carer, Anita Bailey from Evesham, attended the celebration. She looks after her husband who was diagnosed with Vascular Dementia at just 55 and she too was full of praise for the support she’s received from her local Admiral Nurses. She said: “They’re my life savers. I don’t know what I’d do without my Admiral Nurse.” Thank you to our Volunteers We hosted a number of events throughout October 2013 as a way of saying thank you to the 180 volunteers who dedicate their time to helping others. Volunteers from across the county attended events held in Tenbury Wells, Bromsgrove, Evesham and Worcester which offered them the opportunity to socialise with each other over a cup of tea and a scone. They undertake a wide and varied range of roles within the organisation from those who volunteer as porters to those who provide hair dressing and beautician services and everything in between. Some volunteers simply spend time with patients and provide them with a friendly face and someone to talk to. Rachel Kirkwood, Head of Organisational Development, said: “We are so grateful to all of our volunteers for the help they give us and just wanted to show them our appreciation and to let them know that they are extremely valued by the Trust”. High praise for our Language and Learning Course ‘Language for Learning’ is a self-funding project jointly owned by the Trust’s Speech and Language Team and Worcestershire County Council. The project provides training and resources to support all those working with children and young people with speech, language and communication needs. Annual Report 2014-15 We began selling our training packages out of county about 10 years ago and now we have a number of authorities licensed to deliver the training. A survey was conducted and the results, released in October, were really positive. Trainers clearly feel competent and supported in their role and value ‘Language for Learning’ training. Well Connected Named National Pioneer In November, Care Minister Norman Lamb announced that the county’s Well Connected programme had been named as one of just 14 ambitious initiatives the Government has selected to “blaze a trail for change” by pioneering new ways of delivering co-ordinated or more joined up care. Well Connected aims to ‘join up your health and care’ – helping the people of Worcestershire to ’be well and stay well’, be involved in planning their own care and improve the overall experience and coordination of the services they receive. The Well Connected programme brings together all the local NHS organisations (our Trust, Worcestershire Acute NHS Trust, and the Clinical Commissioning Groups), Worcestershire County Council and key representatives from the voluntary sector. Sexual Health Campaign Launched The trust launched a new campaign to raise awareness of the dangers of unprotected sex. The campaign was led by the Sexual Health team and aims to highlight the consequences of unprotected sex and coincides with the party season. It featured an advent calendar style countdown to Christmas which appeared on the Trust’s social networking sites throughout December alongside the hashtag #WrapUpThisChristmas. Each day in the calender provided facts and stats or provided advice for people Quality accounts concerned that they may have put themselves at risk of a Sexually Transmitted Infection (STI) or need emergency contraception. Launch of single point of access South Worcestershire Adult Mental Health Our Adult Mental Health team launched a new Single Point of Access (SPA) service within the South of the County. It is commissioned by South Worcestershire CCG to support health care professionals, predominantly GPs, by providing a simple, easy way to refer both urgent and routine adult mental health patients to the most appropriate service. The aim is that it will ensure one single point of contact for all adult mental health referrals within South Worcestershire, a seamless transition of care once the most appropriate service has been identified and extensive knowledge of the services available locally and what they can provide. EIDS Scoops National Innovation Prize Our Early Intervention in Dementia Service (EIDS) which provides early assessment, diagnosis and support for people with dementia won a national innovation award. The Early Intervention Dementia Service (EIDS) won a national NHS Innovation Challenge Prize for Dementia award. It’s run in collaboration with Janssen Healthcare Innovation (JHI) and is part of the NHS Innovation Challenge Prize Programme and the Prime Minister’s Dementia Challenge. EIDS was launched in 2010 to deliver a timely and person centred approach to the assessment and diagnosis of people with a suspected dementia, to help them to live their lives as they would wish and to support their families and carers. 2000 people have received an early and timely diagnosis in the first three years of EIDS being operational. 37 Mental Health Facility Passes Inspection With Flying Colours Tudor Lodge in Bromsgrove, a long-term residential unit for people with long standing mental health problems, passed an inspection by the Care Quality Commission (CQC) with flying colours. The CQC visited Tudor Lodge in January in an unannounced routine inspection. As part of this inspection, the CQC looked at the personal care or treatment records of people who use the service and observed how people were being cared for. Views of staff and those who use the service were also sought. In the report of the inspection, the CQC noted that people told the inspectors things like: “I am happy living here” and felt that their individual needs were being met by the staff. They also said that they felt safe and it was observed that the staff had a “kind and caring approach towards the people they supported”. The CQC also said that people were listened to and received a consistent level of care that met their individual needs. Mark Dickens, Adult Mental Health lead: “This also shows consistency within our mental health inpatient services as it comes off the back of five of our wards receiving Royal College of Psychiatrists accreditations, four of them accredited as “excellent”. International Recognition for Early Intervention On Tuesday 28th January 2014 the Early Intervention team were honoured to host a Nigerian delegation of mental health professionals: 3 psychiatrists and 1 matron. This delegation was funded through the Commonwealth Scholarship Commission, and they were staying in Birmingham for a few weeks to receive training in Behavioural Family Therapy (BFT) from the Meriden Team. They chose to visit our service as a model of how family interventions can be integrated within an Early 38 Intervention Service as this will be their goal on their return to Nigeria. Tony Gillam (EI clinical manager) started the day with an overview of Worcestershire EIS and our experience of implementing BFT within the service. Dr Alan Farmer, Matthew Lammas and Vicky Wormleighton followed with presentations on different aspects of the EI service and the day finished with Professor Jo Smith describing the development of Early Intervention services in the UK. Our visitors left full of enthusiasm and gratitude for what they had learnt and we were proud that they had chosen to visit Worcestershire EIS. More out of Hospital Support for People with Eating Disorders More people who have an eating disorder in Worcestershire are getting the support they need at home or out of hospital, with referrals into communitybased services on the up. The Worcestershire Eating Disorder Service revealed a rise in the number of people being referred, with figures increasing by 48% since 2005. The rise in referrals is attributed to a mix of increased awareness among the public and professionals both of eating disorders in general, but also of the out-of-hospital care and support provided locally by the Trust. The service works with people in the community and receives around 210 referrals per year. It offers wide ranging help and the team tailor each care plan to suit the needs of every individual. They can offer sufferers individual counselling, a course of cognitive behavioural therapy, food and nutrition guidance, group work and can also provide support with self-help manuals. Kay Lobo, Eating Disorder Service Clinical Manager, said the service was geared up to providing early communitybased support which reduced the risk of people getting so poorly they needed hospital treatment: “Early intervention and treatment can help a sufferer recover more quickly and either prevent hospital admission or shorten the length of their stay.” Annual Report 2014-15 Pilot Scheme Reaping Benefits for Mental Health Patients in Worcester It is said that one of the best ways to deal with your problems is to talk to those who have walked in your shoes and this philosophy is being embraced in our Trust through a new pilot scheme delivering real, tangible benefits for local people with serious mental ill health. Holt Ward is an 18 bedded mental health in-patient unit for adults whose illness cannot safely be treated at home or in the community. It is based on the Newtown Hospital site and in October last year the Trust launched a new Peer Support pilot scheme to help the ward’s patients on their road to recovery. Peer Support sees people with a lived experience of mental illness provide help to those struggling with similar problems. As part of the pilot four Peer Support workers were employed by the Trust to work alongside staff on the ward. Jodie, Joy, Mark and Paul have completed a rigorous Peer Support training programme and provide a different type of support which Quality accounts complements the professional nurses and doctors on the ward. Support may be social, emotional or practical and focuses on an individual’s strengths not weaknesses, and works towards the individual’s wellbeing and recovery. Marisa Manning, Holt Ward Manager, said: “Working with the Peer Supporters on the ward has been a fresh approach to working with patients.” Our staff walk in their shoes The Trust’s take on NHS Change Day was our “Walk in their Shoes” initiative which asked staff to spend some time experiencing what being a patient or service user in our services is really like. We know that patients generally experience excellent levels of care and treatment in our services but that doesn’t mean we are complacent and we recognise there is always more we can do. Walk in their Shoes Day is a chance for our staff to experience some of those things which might seem small, such as being fed or having your arm in a sling, but actually make a real difference to the whole patient experience. 39 2013/14 Quality Account Priorities For last year’s Quality Account we set five priorities for improvement. The progress of these is summarised ‘at a glance’ in the table below. Objective Achieved Continue to improve our response times and learning from complaints a a a Improved Use of Patient, Carer and Staff Feedback, including the ‘Friends and Family’ Test Improvement in the Capture of Real time feedback from Patients Almost Achieved Behind Schedule a We will have no incidents of avoidable pressure ulcers. Improve Evidence that We Learn from Patient Safety Incidents and Near Misses a Priority 1: Continue to Improve our Response Times and Learning from Complaints Result at end of March 2014 What did we measure? The percentage of complaints responded to within Policy timeframe (25 working days) The Clwyd-Hart review into the handling of complaints in the NHS was published in October 2013. The report stemmed from the Francis Inquiry and echoes many of the findings. We have added the recommendations from this review into our Trust Francis Action plan so that we can take forward the learning into our Trust. This work is a developing framework and will be taken forward in 2014/15. We carried ‘listening and learning from complaints’ forward as a priority from the previous year as Trust Board and the people who we consulted on our 2013/14 priorities thought that this should remain at the forefront of our quality measures. During the year 2013/2014 the Patient Relations Team 40 100% has received an increase overall in the contacts received compared to the previous year. This is largely due to the service being more visible to service users, carers and their families. The Team have ensured that there is a wide distribution of information about the Team that is easily accessible to all. An interactive, ‘contact us’ page is also available on the Trust’s website. The Patient Relations Team Lead has undertaken training sessions for healthcare staff within the Healthcare Teams at each of the three prisons and this has improved the quality of responses provided to prisoners from the Healthcare Team. Our Complaints Policy is in accordance with the ‘Principles for Remedy’ published by the Parliamentary Annual Report 2014-15 and Health Service Ombudsman and the Trust aims to produce reasonable, fair and proportionate responses to complaints. The principles are: • Getting it right • Being customer focused • Being open and accountable • Acting fairly and proportionately • Putting things right • Seeking continuous improvement During 2013/2014 the Trust has continued to focus on improving the responses to complainants, both in terms of timeliness and quality. The Trust is required to respond to written complaints within 25 working days. The average response time to complaints was 15 working days, with the exception of those complaints which required an extension to the 25 working day timescale. The Trust received 284 written complaints during the year compared to 302 in the previous year. We regard every complaint and concern as a positive opportunity to receive direct feedback on a patient’s perception of the care they receive from us, and more importantly, as an opportunity to learn how services can be improved. All complaints result in a learning plan whereby any changes or improvements are made and tracked as a result of a complaint. Services share learning in their own team meetings, and learning is shared more widely through governance meetings and trust-wide publications. A summary of all of our complaints is on the Trust website. We try to identify themes or trends from complaints, but as the complaints we receive cover diverse services, this can be a challenge. We do however find that communication, or the lack of it, is at the heart of some of the complaints. These are ‘one-offs’ in that there are no services who have a trend of complaints in this area. Examples of action taken and lessons learned during 2013/2014 include: • Concerns were raised that medication was changed abruptly – the team involved have reviewed their processes for prescribing medication and have taken Quality accounts action to ensure the reasons for the changes are recorded in the clinical records. Steps have also been taken to ensure there is improved communication with service users. • The attitude of the nurse was perceived as being detached – actions taken included improved communication with the patient and their family. In addition the nurse has reflected on how they may be perceived in order to prevent another family feeling this way. • Patient felt there was a lack of respect towards them The nurse reflected on their behaviour and agreed they had behaved in an unacceptable way. As a result of the patient’s experience the nurse attended a workshop on Delivering an Enhanced Patient Experience. • Delay in Healthcare Team responding to prisoner concerns – training has been provided by the Patient Relations Team Lead to staff within the Healthcare Team which has resulted in responses being provided in a much more timely way. • Medication had run out in one instance due to a shortfall in the system – the Pharmacist for Offender Health has undertaken a review into the system to ensure medication is received when needed. Compliments and Gifts Compliments are an important part of patient feedback and are seen as a means of learning how things have gone well. It is always gratifying when someone takes the time and trouble to voice their appreciation, particularly at what might be a very difficult time for them. During the year 2013/2014 2463 recorded compliments were received, compared to the previous year when 686 compliments were recorded. The Trust also received 1448 gifts, compared to 1100 in the previous year. Examples of compliments received include: • We cannot thank you enough for the care and attention you gave to our son. • I am pleasantly surprised by the efficiency of staff and how they put me at ease. Both nurses were excellent. • Just a small thank you for all your kindness and attention to mom in this last year of her life and also for the support you have given us. • Thank you so much for all the help and support given 41 to me during my time here. I am so grateful for all your patience, guidance and sharing your knowledge with me. • Staff attitude was positive, kind, easy going yet practical and professional, all at the same time. She made me feel nice/better and I admire you all. • Positive comments were made in respect to the Healthcare Team by a prisoner in a letter to the Head of Community Engagement at the prison. PALS/Professional Enquiries In 2013/2014 the Trust received 519 PALS enquiries, which is an increase on the 250 received during the previous year. The Patient Relations Team has been able to resolve PALS enquiries, the majority of cases within five working days. This has resulted in queries being resolved quickly. There were also 66 Professional Enquiries received during the year, compared to 46 received in the previous year. These include concerns from General Practitioners, Members of Parliament and Solicitors and have all been responded to within 10 working days. If a complainant remains dissatisfied with the response to their complaint they have the right to refer their complaint to the Parliamentary and Health Service Ombudsman (PHSO) and request an independent review. During 2013/2014, ten complainants referred their complaint to the PHSO. Of these, seven have been closed with no action required, one complaint has been closed requiring action regarding a communication plan and two are currently being considered by the PHSO. In addition, there is also a case open with the PHSO that was received in the previous financial year, which included recommendations and the Trust is taking action on these. Priority 2: Improved Use of Patient, Carer and Staff Feedback, including the ‘Friends and Family’ Test Measure Result at end of March 2014 Increase the number of people surveyed each quarter during the year. Achieved from 915 to 1,042 people surveyed. The aim of undertaking surveys is to improve the experience of patients who use our services in the Trust. The following Patient Experience data relates to: • Community Hospital Inpatient Wards • Minor Injury Units • Outpatient Physiotherapy Departments The Friends and Family Test Question (Would you recommend this service to your family and friends?) was asked in above services, together with ‘free text’ comments from patients on the quality of care received. We asked over 50% of patients who accessed the services. 42 Annual Report 2014-15 Period Three (1 Oct-31 Dec 2013) Sample Size Period Four (1 Jan-31 Mar 2014)) Net Promoter score Sample Size Net Promoter score % Patients Surveyed Worcestershire Health and Care NHS Trust 915 86 1,042 85 N/A Community Hospitals 81 75 111 74 63.6% Minor Injury Unit (MIU) 364 91 304 88 64.9% Physiotherapy 470 84 627 85 54.9% Recent examples of work undertaken, led by our Patient Experience Lead Naomi Seers, are: Prison Patient Experience Survey Following a CQC inspection undertaken in HMP Oakwood, Worcestershire Health and Care Trust undertook a patient experience survey. We received a large number of responses. The survey enabled prisoners who use healthcare services in the prison to give free text comments. Following feedback received a number of changes relating to healthcare were made. This feedback received was also shared both with patients and staff as part of the Prisoner Forums. The survey was undertaken again within HMP Oakwood and the feedback is currently being reviewed. Following the success of the prison patient experience work the survey has now been undertaken in HMP Long Lartin and plans are in place to undertake this in HMP Hewell. Learning Disability Forums Worcestershire Health and Care Trust currently receive a limited amount of the patient experience feedback from within the Integrated Learning Disability Service. To ensure that we have the appropriate feedback mechanism in place that meets the needs of the Quality accounts service we have held three learning disability forums to share experiences and discuss options of a feedback mechanism. The forums were held for patient and carers currently accessing the integrated service. The feedback is currently being reviewed and plans put in place to progress this work. National Staff Survey The results of the 2013 NHS National staff survey were formally released on Tuesday 25 February 2014. 422 responses were received from staff that took part in the sample survey (random sample of 850 were send questionnaires) which resulted in a response rate of 50% which is average for mental health/learning disability trusts in England and compares with a response rate of 50% for the Trust in the 2012 survey. The Trust’s score for overall staff engagement in the 2013 was average when compared with Trusts of a similar type. The staff ‘Friends and Family’ survey is now on the Trust intranet site until June 2014 and we are undertaking extra ‘Temperature Check’ surveys with staff to try and learn more about how we can engage more fully. 43 Priority 3 - Improvement in the Capture of Real time feedback from Patients Result at end of March 2014 Measure Register in place Register of current patient surveys and themes Patient feedback is important to us so we can understand how the services we deliver impact on the people receiving them. There is no single route to understanding patient experience. To give patients, service users, carers and family members a new and simple way of telling us about their experiences of the care they received, we launched a Patient Experience website. Patients or families can simply log on and tell us their story. This will provide us with an invaluable way of monitoring our performance so we can identify how we can continue to improve our services and develop our understanding of what matters most to the people we care for. We dedicated March 2014 as our Patient Experience month. We really wanted to gather more views from patients about what they think we do well and where we might do better; it’s about getting a better understanding of their experiences and perceptions of our services. There are comment cards on our wards for patients to complete but we realise this isn’t always appropriate, so we asked our staff to ‘Pause for Thought’ during March and ask patients/service users or families and carers to share their experiences of the care and treatment they are getting. By Pausing for Thought for just for a few minutes and taking that time to listen, we think we can make the kinds of changes which really do improve the whole 44 patient experience. Cyrus Baria, one of our patient/community representatives visited Tenbury hospital in March to gain some patient feedback for us. Cyrus gave the following feedback - “I visited Tenbury Wells Hospital for the Nutrition and Hydration Tea Party yesterday. I met up and talked to 9 people either whilst having tea in the common room or by their own beds/bedside, as some of them couldn’t come and join the party. Dianne Adams had laid on a very good spread of sandwiches, cakes, scones with cream and strawberry and cups of tea. This was very well received by the patients. This was my first visit to this hospital and I found it very clean, friendly and welcoming. All the patients and relatives I talked to, did not have one bad word to say. They all said, the food was good, staff very friendly and the staff really took care of them. One person said that she was greeted with a mug of tea, biscuits and a glass (real glass) of water. Sometimes its the small things which makes a big difference. One gentleman found his area of the ward, a bit noisy. When I questioned him what was the issue, his comments were, staff were laughing out loudly. I placated him by saying at least it was a happy ward and he agreed with me. I also spoke to a couple of admin staff and the way they look at the hospital was “this is my hospital”. Annual Report 2014-15 Patient Experience Feedback Poster Patient Experience Feedback posters have been designed to be displayed in clinical areas to show the results in a clear format from surveys. An example is given below – the actual posters are much bigger than the picture opposite! MIU: Patient Experience Survey LOCATION 364 patients from 4 sites (Bromsgrove, Malvern, Tenbury and Evesham) took part. WAS THIS SERVICE EASY TO ACCESS? 100% 364 out of 364 patients said this service was easy to access. HAVE STAFF COMMUNICATED WELL WITH YOU? Extremely Well 312 Very Well 52 Not Well 0 Not at all Well 0 Total 364 HOW SATISFIED WERE YOU WITH THE SERVICE YOU RECEIVED TODAY? 400 Fantastic that staff engaged with my daughter (the patient) – quick, easy, stress free service. Brilliant service – did not have to wait and was attended by very professional staff throughout my visit. My sincere thanks to the staff. Fast, efficient service much easier than A&E – sorted out within an hour including xray!! Staff very good. THE FRIENDS AND FAMILY TEST HOW LIKELY IS IT THAT YOU WOULD RECOMMEND OUR DEPARTMENT TO FRIENDS AND FAMILY IF THEY NEEDED SIMILAR CARE OR TREATMENT? 89 Worcestershire Health and Care Trust Patient Group The above group was set up during the year. It is made up of patient representative volunteers who are helping us to implement the patient experience agenda. This can be undertaking surveys, supporting ‘talking projects’ and the group is also a critical friend for discussing initiatives and ideas. We are grateful for the help of this proactive group of people in helping us to better understand the views of patients, service users and carers. FRIENDS AND FAMILY SCORE: 300 200 100 0 All the staff were polite and lovely to us and I felt very re-assured. Extremely Satisfied Satisfied Dissatisfied Quality accounts This means 89% of friends and family are extremely likely to recommend us! 45 Priority 4 - Pressure Ulcers Measure Result at end of March 2014 Harm free care thought the Safety Thermometer – pressure ulcers 93.9% harm free from pressure ulcers We want to reduce the incidence of avoidable pressure ulcers as we know pressure ulceration causes significant pain and distress for patients when they occur. The Trust has very few patients in our community hospitals who have acquired pressure ulcers. However there are a larger number of pressure ulcers in the community. This is challenging to manage because many people are looked after in the community by people that the Trust has no responsibility for. The Trust is committed to reducing pressure ulcers in the community setting and is taking this forward as a priority into 2014/15. Disappointingly, since June 2013, on the national Safety Thermometer audits, the Trust has reported a higher level of harm from pressure ulcers than the national and regional average. However it should be noted that the Safety Thermometer makes no distinction between those ulcers developed in our care or elsewhere. 46 We have implemented a wide reaching strategic plan to address this issue, and can evidence integrated working within the health and social care economy to address the causes of pressure ulcers. We now produce weekly team level reports to show where pressure ulcers are occurring. We draw detailed analysis from our incident reporting system, and thorough action plans from incidents are implemented. There are some signs at the end of 2013/14 that the aims of the plan are coming to fruition as there is evidence of a slight downward trend. The graph below sets out all pressure ulcers reported in the Trust over the last 12 months – both those that developed in our services and outside of them. Annual Report 2014-15 The graph below sets out reported pressure ulcer incidents in the community hospital wards per 1000 occupied bed days for the last 12 months. The graph sets out all grades of pressure ulcers, avoidable and unavoidable and includes those that have developed both in our care and outside of our care. The Department of Health definitions regarding avoidable/unavoidable pressure ulcers are as follows: Avoidable Pressure Ulcer: “Avoidable” means that the person receiving care developed a pressure ulcer and the provider of care did not do one of the following: evaluate the person’s clinical condition and pressure ulcer risk factors; plan and implement interventions that are consistent with the persons needs and goals, Although we often, rightly, concentrate on pressure ulcers developed in our care, we are committed to working together with our partners in the health economy so that we can learn from each other, and support each other in eradicating avoidable pressure ulcers wherever the patient is receiving care. On a more positive note, our Tissue Viability Consultant Nurse, Jackie Stephen-Haynes and Rosie Callaghan, Tissue Viability Nurse, won the British Journal of Nursing Quality accounts and recognised standards of practice; monitor and evaluate the impact of the interventions; or revise the interventions as appropriate.” Unavoidable Pressure Ulcer: “Unavoidable” means that the person receiving care developed a pressure ulcer even though the provider of the care had evaluated the person’s clinical condition and pressure ulcer risk factors; planned and implemented interventions that are consistent with the persons needs and goals; and recognised standards of practice; monitored and evaluated the impact of the interventions; and revised the approaches as appropriate; or the individual person refused to adhere to prevention strategies in spite of education of the consequences of non-adherence”. Pressure area care nurses of the year award for 2014 with their work on “The outcomes of a strategic plan for essential skin care and pressure ulcer prevention in the elderly in the care home setting across one primary care organisation”. We are committed to eradicating avoidable pressure ulcers and we are taking this priority forward into next year. 47 Priority 5 - Improve Evidence that We Learn from Patient Safety Incidents and Near Misses Measure Result at end of March 2014 Revised incidence reporting policy to further underpin the learning from incidents Due to be ratified in May 2014 Revised Route Cause Analysis training Achieved New patient safety reporting system which will give better reporting to teams so that trends can be identified Achieved Professor Don Berwick, renowned international expert in patient safety, was asked by the Prime Minister to carry out a review following the publication of the Francis Report. His report makes recommendations for the NHS, its regulators and the government to build a robust nationwide system for patient safety rooted in a culture of transparency, openness and continual learning with patients firmly at its heart. We have taken these recommendations and included them in our Francis Action Plan and will be publishing a ‘Duty of Candour’ Policy in the summer of 2014/15. Our quality measure of all ‘Incidents being reported within 48 hours of the incident occurring’ has improved during 2013/14 (86% in March 2014 compared to 71% in April 2013) ) as required by Trust policy and seen as best practice by the CQC. Systems of disseminating learning exist within Service Delivery Units via our Quality and Governance Leads, Clinical Leads and Team Managers. During 2013/14 there were some common themes arising from investigations and recommendations including: • The need for staff to receive training in clinical record keeping. As a result of this we have revised our training and plan to launch an on-line, easily accessible training 48 package in early 2014/15. • The need to ensure staff update care plans in a timely manner. This is being followed through by using the nursing metrics to track improvement initiatives. • The need to ensure patients and service users are involved in decision-making regarding their care, and that this can be evidenced in the notes. In the Trust we know we still have some way to go in improving our shared learning from incidents. We have however made some progress and have revised our training for undertaking Route Cause Analysis investigations. The feedback from the training has been excellent and we have seen a steady improvement in the quality of investigations which in turn has led to more focussed and effective learning outcomes. We introduced a new incident reporting system in August 2013. The system is much easier for staff to use and has led to an increase in the number of incidents being reported. It is widely accepted that Trusts who report more incidents have a more open safety culture. As more incidents are reported and lessons learned, the harm from incidents should reduce. Annual Report 2014-15 Review of 2013/14 - Patient Safety Falls Prevention Falls are a major cause for concern for us. Unfortunately people may be more likely to fall in-hospital than in their own homes, as a result of being in an unfamiliar environment. A full environment risk assessment is carried out at least once a year to identify any extrinsic factors that may influence fall rates across in-patient services. All patients who come into our hospitals are assessed for their risk of falling, so that appropriate care can To focus our falls prevention work efforts over the next year, we have established a Trust wide group; the Falls Improvement Group to lead the implementation of Royal College of Physicians ‘Falls Safe Care Bundle’. The group is chaired by the Deputy Director of Nursing and supported by the Falls Prevention Coordinator with representatives from training and development, quality governance, nursing, medical, therapists and senior clinical managers. The group will lead a strategy for the prevention and Quality accounts be planned to try and prevent a fall – for example by providing a specialist bed. We measure the overall rate of falls through our incident reporting system and use the data to identify whether falls occur on particular days or at particular times of the day. We review the root cause for all serious falls occurring in hospital and have developed nursing indicators to monitor improvement as a result of this work. management of falls across inpatient and community services and therefore bring together all the work that has already been achieved, and identify the gaps for further development. This will include progressing issues on the assessment of osteoporosis, identification of delirium, cognitive screening and immediate access to walking aids. 49 Infection Prevention and Control Actively minimising healthcare associated infections is a priority in the Trust. We are committed to ensuring that the risk of infections is kept to an absolute minimum. During 2013/14 we maintained an excellent performance on the prevention and control of infection across our services. For 2013/4, by year end the number of cases of Clostridium Difficile (C-diff ) was below the target threshold set by the commissioners. Unfortunately we have had one case of MRSA bacteraemia presenting in the year and as a result a full investigation into the cause was undertaken. Within the Trust it is widely acknowledged that infection prevention and control is everyone’s responsibility; this is in addition to the Infection Prevention and Control team who provide specific advice and guidance to staff. Across the Trust there have been a number of initiatives to reduce infection: • Ensuring staff attend appropriate training – the uptake of infection control training by year end is at nearly 90% • Promoting hand hygiene and undertaking audits • An infection control charter for both patient, service users, visitors and staff. The PLACE team carried out the formal inspections during 2013/14 and we are very pleased to have maintained good or excellent standards across our sites. Safeguarding Activity continues in the Trust to ensure that vulnerable children and adults are safeguarded since the last Quality Account. The Integrated Safeguarding Team along with the Safeguarding Working Groups have continued to embed learning from safeguarding audits and reviews in all aspects of the Trust’s work as the organisation continues to develop a learning culture 50 Key Activities have been the following: • Learning from multi agency Adult and Children’s Serious Case Reviews • Training and embedding a process for multi-agency information sharing and working to safeguarding children and young people form child sexual exploitation • Embedding a process for managing children and young people at risk of suicide. • Engaging in preparation with the Safeguarding Adult Board for the implementation of the Care Bill • Development and dissemination of guidance for Managing Self Neglect in Adults. • Preparation for single Agency Inspections of Safeguarding Children Services by Care Quality Commission • Supporting staff with training, supervision and reflection on safeguarding cases • Embedding robust responses to domestic abuse where children and adults at risk might be at risk of harm as a direct result of learning from a Serious Case Review in another County • Delivery of in house domestic Abuse Training in conjunction with the University of Worcester Mandatory Safeguarding Training levels that must be completed by all staff have now reached 96% for safeguarding children and 94% for safeguarding adults. The Trust maintains its approach of zero tolerance of the abuse of children and adults who are at risk of harm. Never Events Never Events are defined by the Department of Health as ‘serious, largely preventable safety incidents that should not occur if the available preventative measures have been implemented by healthcare providers’. Fifteen of the list of twenty five never events are relevant to the Trust. There have been no occurrences of Never Events in the Trust during 2013/14. Annual Report 2014-15 Central Alerting System The Central Alerting System is a means of alerting health and social care providers to the important safety information from a number of different sources. The actions required as a result of the alerts can be minor or involve significant change. During 2013/14 of all the alerts received, were responded to within the required timeframe. Training and Development and Development webpage which includes information regarding mandatory and essential training for certain staff groups, and also a weekly training bulletin advertising internal and external courses that are on offer to staff and information regarding completing e-learning. Same-sex Accommodation During 2013/14 we met the standards set by the Government to provide accommodation for patients that is not shared with the opposite sex. Our Training and Development team assist with staff development by working alongside them to develop skills, knowledge and required competencies. Some current work streams the team are actively involved with include Nursing Metrics, Safer Nursing Care Tool, High Impact Actions, Pledge to Care, the Skills Bus, Big Recovery and the development of the new nursing documentation for our community hospitals. Other areas that we cover include pre-registration nursing placements, preceptorship, specialist practitioner support, clinical policies, and other streams of work which support high quality care and professional practise. All mandatory courses are available through the team and support for e-learning is available from our dedicated administration team. Essential training for certain staff groups such as MAPA, Diligent and Resuscitation training are courses that many people think are the limit of the courses offered by TDU. However we offer a host of opportunities for development covering Leadership development courses, coaching, Dementia training, Mental Health first aid, Mentor updates, Intermediate Skills Programme as well as many more. Staff have access to the TDU webpage for up to date information regarding available training for both clinical and non-clinical staff. The Training and Development Team has actively supported trust staff throughout 2013/14 in achieving a huge increase in the completion of mandatory training for all staff groups. We have development a Training Quality accounts 51 Our 2013/14 CQUIN Performance Commissioning for Quality and Innovation (CQUIN) schemes require Trusts to improve quality and innovation by discussing, agreeing and monitoring quality indicators with its commissioners. When the quality improvement goals and indicators are achieved, the Trust earns a financial payment. The indicators set out in the table below were set for 2013/14 and present our performance. We were pleased to have achieved all of the quality improvement measures in our CQUINs and in some cases exceed them. CQUIN Goal description Achieved 1 Net Promoter ‘Friends and Family’ introduction and roll out a 2 Roll out of three further patient experience questions a 3 Triangulation of patient experience data a 4 Safety Thermometer data submissions a 5 Delivery of IV therapy training across community teams and community hospitals a 6 Improving patient flow a 7 Amber Care bundle a 8 Advanced Care Planning a 9 Improving the physical health care for people with severe and enduring mental health problems a 10 Engagement of family/friends and carers and advocates in the care planning process a 11 Patients on CPA to have on discharge from acute or secondary care services an agreed Crisis Support Plan a 12 Patients on all clusters to have a review in line with at the expected review intervals a 52 Annual Report 2014-15 Looking Forward Quality Account Priorities for 2014/15 The priorities for the coming year were shaped by: • the Trust’s own review of its quality performance, based on information for example from our incident data and complaints • the Quality Account Working Group • Staff survey • Members survey • Public website survey • Engagement with our commissioners • Engagement with the Trust Development Authority The three priorities for 2014/15, progress on which will be reported to our Quality and Safety Committee and Trust Board throughout the year, are: Priority 1 – Preventing Avoidable Pressure Ulcers (carried forward from 2013/14) A pressure ulcer is an area of damage to the skin and the underlying tissue, usually over a bony area of the body. Pressure ulcers range in severity from skin discolouration to severe open wounds. Why are we focussing on preventing pressure ulcers? • Pressure ulcers cause patients long term pain and distress • Pressure ulcers can mean longer stays in hospital • Avoidable pressure ulcers are widely seen as a key indicator of the quality of nursing care. • Giving clear information on what to look for helps patients and carers avoid pressure ulcers. How are we going to achieve this goal? We already have policies and procedures in place for preventing, assessing and treating pressure ulcers and we know that there are already many examples of excellent practice. We will build on this good work with a focussed plan: • The Quality Team will produce a weekly report from Quality accounts Ulysses, our incident reporting system, indicating all pressure ulcers by grade • All grade 2 pressure ulcers on the weekly report will be targeted by Team Leads to prevent escalation to grade 3. • All grade 2 pressure ulcers will have documentation and process of assessment and treatment checked by team leader/ ward manager. • Ward Managers/ team leaders will review patients within 24 hours of any pressure area damage being identified in order to accurately prescribe and /or ensure appropriate equipment is in place • All Grade 2 pressure ulcers will be discussed by Ward Manager/ team leader with nursing team as part of weekly meetings to ensure the plan of care is working and is appropriate • All Grade 3 and 4 pressure ulcers will undergo a rapid review, whereby a round table meeting is carried out within 2 weeks of the pressure ulcer being reported. This will determine the Route Cause of the pressure ulcer and will facilitate shared, effective learning and improvement. What measures will we use? We will track and report on the number of avoidable pressure ulcers. A baseline figure will be calculated from the 2013/14 data. This will be reported monthly to the Quality and Safety Committee. Priority 2 – Improving the care for people with Dementia and their carers Dementia is caused when the brain is damaged by diseases, such as Alzheimer’s disease or a series of strokes. Alzheimer’s is the most common cause of dementia but not all dementia is due to Alzheimer’s. The symptoms that someone with dementia experiences will depend on the parts of the brain that are damaged and the disease that is causing the dementia. Symptoms of Dementia may include memory loss and difficulties with thinking, problem-solving or language. These changes are often small to start with, but for someone with dementia they have become severe 53 enough to affect daily life. A person with dementia may also experience changes in their mood or behaviour. Why are we focussing on Dementia care? The numbers of people with dementia or signs of dementia admitted to Community Hospitals are increasing. A range of support can help a person and their family to live well with dementia. It is a challenge to obtain patient feedback on care from this group of people, so that we know whether the measures we are put in place really help.. How are we going to achieve this goal? • Dementia Care Mapping (DCM) has been recommended by the National Institute for Health and Clinical Excellence as a method for improving care practice for people with dementia. DCM is an observational method used to evaluate the experience of people with dementia. • Specially trained staff will observe and record care from the patient’s point of view over a 6 hour period. The data is then analysed and is fed back to staff as a means of changing and improving the patients’ • We will implement Dementia Care Mapping (DCM) in the Community Hospitals. All young people, including those aged under 16, are entitled to confidential sexual health and contraceptive advice and treatment. Access to confidential sexual health services, both in schools and in the community, is one of the ways in which young people can be supported to stay safe. Why are we focussing on young person’s experiences? We recognise that meeting the particular needs of young people is a key component in ensuring our services are effective. We wanted to include a priority in the accounts that would tell us more about the services we provide for young people. The Youth Board were asked for their views and the attitude of workers in sexual health services came out as one of the things young people think is important. How are we going to achieve this goal? This indicator will require asking the identified carer questions related to their experience of the Community Hospital in addition to that of their relative/friend The Department of Health has the ‘ You’re Welcome’ quality criteria which lays out principles to help health services become young people friendly. ‘You’re Welcome’ can increase health workers skills in working effectively, appropriately and sensitively with young people. Our Sexual Health services have been working with the ‘You’re Welcome’ criteria for some time so we want to know what young people think of our services. What measures will we use? What Measures will we Use? We will undertake two carer surveys, one at the beginning of the year and then one towards the end of the year when the Dementia Care Mapping actions will have been implemented. We will then compare the results to measure whether the actions have resulted in an improved experience for people with dementia and their carers. Priority 3 – Understanding and Improving Young People’s Experiences of Sexual Health Services 54 We will ask young people through a survey about their views. We will look at ways of how we can do this whilst ensuring confidentiality is not at risk. We will ask staff who work in the services for their own views about the quality of service provided. We will then implement any changes from the feedback and repeat the survey to assess whether any changes have led to improvements. Annual Report 2014-15 CQUINS for 2014/15 The following CQUINS have been agreed with our commissioners for 2014/15. We are committed to delivering these quality improvements and will be reporting on our progress with each of them to Trust Board and our commissioners during the year. Service Included in CQUIN CQUIN Theme/ Title Safety Thermometer- Tissue Viability Friends and Family Test (FFT) - staff FFT Patients (awaiting national guidance for community trusts) Older Adult Mental Health Tissue Viability – RCAs Hydration Physical health for patients with schizophrenia Communication with GPs a a a a a a a Patient Family and friends test. a a (PICU) Dementia Care Mapping. Carer experience. Staff confidence a a a a a a a Staff Family and Friends Test Repeat Point Prevalence Multiple indicators Clinical lead in wider strategy. 7 day reviews in RCAs Hydration bundles. Training. Peer audit Cardio metabolic assessment for patients with schizophrenia Focussing on patients on CPA, demonstrating an up-to-date care plan has been shared with the GP a Analysis of the health needs of population, and health related goals in Health Action Plan (HAP) a Offender health (still to be agreed) Quality accounts Learning Disability Reduction in incidents of Grade 2,3 & 4 pressure ulcers Health Action Plans for people with a Learning Disabilities Breast Feeding uptake Primary Care Offender Brief Description of indicators Health care a a a a a a a a a a a Patient Flow Dementia Community Care Children, Young MenPeotal ple Health and Families a a (HV) Well man clinics Promotion of breast feeding. 55 2013/14 Quality Account Technical Section – Mandatory Statements The following section contains the mandatory statements common to all Quality Accounts as required by the regulations set out by the Department of Health. Review of services During 2013/14 the Worcestershire Health and Care Trust provided and/or sub contracted 5 NHS services. • Community Care • Adult Mental Health • Children, Young People and Families • Specialist Primary Care • Learning Disabilities The Worcestershire Health and Care NHS Trust has reviewed all the data available to them on the quality of care in five of these NHS services. The income generated by the NHS services reviewed in 2013/14 represents 100 per cent of the total income generated from the provision of NHS services by the Worcestershire Health and Care NHS Trust for 2013/14. Participation in clinical audits During 2013/14 eight national clinical audits and one national confidential enquiry covered NHS services that Worcestershire Health and Care NHS Trust provides. During this period Worcestershire Health and Care NHS Trust participated in 100% national clinical audits and 100% national confidential enquiries of the national clinical audits and national confidential enquiries which it was eligible to participate in. The national clinical audits and national confidential enquiries that Worcestershire Health and Care NHS Trust was eligible to participate in during 2013/14 were: • National Audit of Schizophrenia • National Audit of Psychological Therapies for Anxiety and Depression (NAPT) • Prescribing Observatory for Mental Health (POMH-UK) Topic 13a: Prescribing for ADHD • POMH-UK Topic 7d: Monitoring of patients prescribed Lithium • POMH-UK Topic 4b: Prescribing Anti Dementia Drugs • National Confidential Inquiry into Suicide and Homicide by people with Mental Illness (NCISH) • BASHH Management of young people attending sexual health clinics • Profession specific stroke audit • English National Memory Clinics Audit The national clinical audits and national confidential enquiries that Worcestershire Health and Care NHS Trust participated in, and for which data collection was completed during Worcestershire Health and Care NHS Trust are listed below alongside the number of cases submitted to each audit or enquiry as a percentage of the number of registered cases required by the terms of that audit or enquiry. National clinical audits 2013/14 Participation % cases submitted POMH-UK Topic 13a: Prescribing for ADHD Yes n/a POMH-UK Topic 7d: Monitoring of patients prescribed Lithium Yes n/a POMH-UK Topic 4b: Prescribing Anti Dementia Drugs Yes n/a Other national audits Yes National Audit of Schizophrenia Yes 77% National Audit of Psychological Therapies for Anxiety and Depression (NAPT) Yes n/a Prescribing Observatory for Mental Health (POMH-UK) 56 Annual Report 2014-15 Continued... National clinical audits 2013/14 Participation % cases submitted British Association for Sexual Health and HIV (BASHH) Management of young people attending sexual health clinics Yes n/a Profession specific stroke audit Yes n/a English National Memory Clinics Audit Yes n/a Prescribing Observatory for Mental Health (POMH-UK) The reports of five national clinical audits were reviewed by the provider in 2013/14 and Worcestershire Health and Care NHS Trust intends to take the following actions to improve the quality of healthcare provided. Subject of audit Standard where audit identified need for improvement Actions that have been put in place since audit Outcome POMH-UK Topic 13a: Prescribing for ADHD Initiating drug treatment for ADHD: Before starting drug treatment, children, adolescents and adults with ADHD should have a full pretreatment assessment Checklist for doctors on medication form being used countywide Revised “Green Sheet” in use. Maintenance treatment: monitoring of BP, heart rate and growth Checklist for admin staff to ensure all necessary paperwork is included in notes (green sheet) All paperwork in single file easily accessible to doctors and admin staff in paediatrics and CAHMS. Symptom monitoring of medicated children Symptom monitoring questionnaire researched, agreed and easily available Symptom monitoring questionnaire in use. POMH-UK Topic 7d: Monitoring of patients prescribed Lithium Weaknesses were failure to measure Weight or BMI or waist circumference should be completed before initiating treatment. Commitment made to measure weights of people with LD receiving lithium and document in notes Easy-read information about lithium is available to give to patients. British Association for Sexual Health and HIV (BASHH) Management of young people attending sexual health clinics Young people’s proforma should be standardised across the service Young person’s proforma standardised with the imminent arrival of electronic notes in the service Awaiting electronic notes system National Audit of Psychological Evaluating the effectiveness of Therapies for Anxiety and interventions Depression (NAPT) CORE Outcome Measure currently being piloted as a way of evaluating both individual and group therapeutic interventions. Data collection underway. Report due end of May 14. Profession specific stroke audit No further action required N/a N/a English National Memory Clinics audit N/a N/a Quality accounts No further action required 57 The reports of 28 local clinical audits were reviewed by the provider in 2013/14 and Worcestershire Health and Care NHS Trust intends to take the following actions to improve the quality of healthcare provided. Please note this is a sample only to give an idea of the spread of audit work across the services. Subject of audit Standard where audit identified need for improvement Protected mealtimes Patient asked if they need the toilet prior to Staff prompted to start toileting meal procedure for all patients ½ hour prior to mealtime Amount eaten to be recorded Complete the food diary or food chart/ nutrition care plan. Training has been rolled out re documentation and competency documents have been introduced onto one of the wards. Ensure those patients requiring a red tray are given a red tray Venous Thrombo-embolism Follow national and local standards for VTE (VTE) Screening on Older screening. Adult Mental Health Inpatients wards Audit of WHO checklist for ECT Safer sleeping audit Ensure patient ID verification is being performed Ensure out of county babies are risk assessed, either by midwife or HV Audit of the standardised children’s’ equipment list Equipment to be requested from the standard list only 58 Actions that have been put in place since audit Introduce a visual prompt (red dot) next to patient’s name to indicate to catering staff that the patient requires a red tray. Document in handover sheet. Results presented to all consultants to take immediate action and maintain patient safety. To be specifically included in Junior Doctor induction programmes, and highlighted to ward managers. Guidelines to be developed for VTE screening in Older Adult mental health inpatients. Patient ID checks are completed in all 5 modalities Section added into the Worcestershire Safer Sleeping Guideline for out of county babies. All HV and Community midwife team leads informed of addition to policy so they are clear of their roles and responsibilities. Monitored via ICES equipment panel data. Annual Report 2014-15 Continued... Audit of opioid prescribing in palliative care All specialist and generalist palliative care providers to give consistent advice based on NICE & APC guidance Management of know side effects Management of Resuscitation & Medical Emergencies: Salaried Dental Service Knowledge of responsibilities, duties, training, risk assessment, equipment and drugs, emergencies outside the dental surgery Older Adult Mental Health and Driving audit Feedback and education sessions from specialist palliative care providers in the planning. Introduction of a patient information leaflet. Information shared with Trust Resuscitation training team in order to increase awareness of the specific areas that need to be stressed during training courses where dental team are in attendance. All patients undergoing a new referral Driving status has been added to the Risk assessment should have their driving status Assessment section on the template for discussed and recorded in correspondence. OA Wyre Forest Team. Participation in clinical research Statements for the CQC The number of patients receiving NHS services provided or sub-contracted by Worcestershire Health and Care NHS Trust in 2013/14 that were recruited during that period to participate in research approved by a research ethics committee was 20 (National Institute of Health research portfolio studies only). Worcestershire Health and Care NHS Trust is required to register with the Care Quality Commission and its current registration status is registered. Worcestershire Health and Care NHS Trust has no conditions imposed on its registration. Participation in clinical research demonstrates Worcestershire Health and Care NHS Trust’s commitment to improving the quality of care we offer and to making our contribution to wider health improvement. Goals agreed with Commissioners A proportion of Worcestershire Health and Care NHS Trust income in 2013/14 was conditional on achieving quality improvement and innovation goals agreed between Worcestershire Health and Care NHS Trust and any person or body they entered into a contract, agreement or arrangement with for the provision of NHS services, through the Commissioning for Quality and Innovation payment framework. Further details of the agreed goals for 2013/14 and for the following 12 month period are available electronically at www.hacw.nhs.uk Quality accounts The Care Quality Commission issued one warning notice against Worcestershire Health and Care NHS Trust during 2013/14. Following an inspection of the healthcare provision in HMP Oakwood in June 2013 the CQC advised the Trust of a failure to comply with Regulation 13 (Management of Medicines) of the Health and Social Care Act (2008) Regulations 2010 (the Regulated Activities Regulations 2010) at HMP Oakwood. The Trust recognises the severity of the concerns found during the inspection, and we are extremely regretful that our services did not meet our own expected standards of care. The CQC re-inspected HMP Oakwood in October 2013 and lifted the warning notice. We have since made further improvements and have sustained safe, good quality care for patients in HMP Oakwood. We are in close contact with the NHS England Local Area Team, The Trust Development Authority, the Pharmacy provider and the Prison Director to ensure there is a partnership approach to sustaining the improvement actions. 59 We are fully committed to continuing the effectiveness of actions we have put in place, both now and in the future. Worcestershire Health and Care NHS Trust has not participated in any special reviews or investigations under section 48 of the Health and Social Care Act 2008 by the CQC during 2013/14. Data Quality Worcestershire Health and Care NHS Trust will be taking the following actions to improve data quality. Improving Community Care Ethnic Origin Coding Since April 2013, monthly information has been shared with clinicians, and performance reported to the Trust’s Finance & Performance Committee. Throughout the year, there has been an upward trend in performance as shown in the following table: Month Jun 13 Sep 13 Dec 13 Mar 14 Completeness 57.9% 53.0% 82.5% 85.2% The Trust will continue to work with clinicians and report performance on a monthly basis, to ensure a score of 95% can be achieved and maintained. Other areas for development For the Financial Year 2014/15, Worcestershire Health and Care NHS Trust will be taking the following actions to improve data quality. Inpatient: Primary Diagnosis. Action By whom Timescale Monthly lists of episodes with a missing primary diagnosis to be produced and sent to Service Delivery Units. Information Dept On-going Diagnosis code identified and the relevant PAS updated. MH Clinicians / RWP Coders On-going Undertake an analysis of inpatient units to determine whether there are any specific wards where coding completeness is consistently low. Information Dept April 2014 onwards Share analysis with SDU Leads as part of monthly performance dashboard Information Dept April 2014 onwards 60 Annual Report 2014-15 Secondary Uses Service Worcestershire Health and Care NHS Trust submitted records during 2013/14 to the Secondary Uses Service for inclusion in the Hospital Episode Statistics which are included in the latest published data. The percentage of records in the published data which included the patient’s valid NHS Number was: • 99.8% for admitted patient care • 99.9% for outpatient care Worcestershire Health and Care NHS Trust was not subject to the payment by results clinical coding audit during 2013/14 by the Audit Commission. Information Governance The requirements of Information Governance are central to the way we operate to ensure all data we collect is held safely and securely. The percentage of records in the published data which included the patient’s valid general medical practice was: • 99.9% for admitted patient care • 99.8% for outpatient care Information Governance (IG) Toolkit Grading Clinical coding error rate Personal Data as Reported to the Information Commissioners Office: The Trust achieved a score of 77% and were graded ‘satisfactory’, which is the highest grade achievable. There is no longer a RAG rating on the IG Toolkit. SUMMARY OF SERIOUS INCIDENT REQURING INVESTIGATION INVOLVING PERSONAL DATA AS REPORTED TO THE INFORMATION COMMISSIONER’S OFFICE IN 2013-14 Date of Incident August 2013 Nature of Incident Loss of paperwork – a ward handover sheet was found at a railway station and was handed into the local Press Nature of Data Involved Name, age, GP name, diagnosis, past medical history, mobility, nursing interventions required, discharge information Number of data subjects affected Notification Steps Individuals contacted and offered support 18 Press statement released Full investigation undertaken Internal processes have been reviewed, improved and updated Further action on information risk Quality accounts The Trust will continue to monitor and assess its information risks, in light of the events noted above, in order to identify and address any weaknesses and ensure continuous improvement of our policies and procedures 61 Mandated Indicators Care Programme Approach (CPA) follow up contact within seven days of discharge from hospital. The Trust’s performance in this area is measured on a quarterly basis as part of the Trust Development Authority’s Accountability Framework indicators. In order to achieve the highest level of compliance in this area (“Performing”) the Trust must achieve 95% of inpatients on CPA followed up within seven days of discharge from hospital. The Trust is pleased to report that a level of ‘Performing’ was consistently achieved, with scores over 97%, for each quarter in 2013/14. The quarterly scores are shown in Table 1 below. Table below: Percentage of people on CPA followed up within 7 days of discharge from hospital. Performance Threshold 95% or over Actual Quarterly Performance 2013/14 Quarter 1 Quarter 2 Quarter 3 Quarter 4 98.9% 97.2% 99.0% 99.5% Minimising Delayed Transfers of Care Measuring delayed transfers of care forms part of the Trust Development Authority’s Accountability Framework, and helps the Trust to assess the impact of community-based care in facilitating timely discharge from hospitals. People should receive the right care in the right place at the right time and we must ensure that people move on from the hospital environment once they are safe to transfer. The indicator seeks to encourage organisations to work in partnership to minimise the number of patients remaining in hospital settings who are ready for discharge. The definition is as follows: “the number of patients (acute and non-acute, aged 18 and over) whose transfer of care was delayed, expressed as a percentage of the number of consultant and non-consultant led occupied beds.” In order to achieve the highest level of compliance in this area (“Performing”) the Trust must keep delayed transfers of care to 7.5% or less during each quarter. Table 2 shows the Trust’s position for 2013/14. The Trust is pleased to report that a level of ‘Performing’ was consistently achieved, with scores under 5.1%, for each quarter in 2013/14. We routinely monitor our performance in this area across all services and where performance consistently falls below target we implement recovery plans that are monitored by the Trust Board. We actively work with our partner organisations to minimise any delays. 62 Annual Report 2014-15 Table below: Percentage delayed transfers of care. Performance Threshold 7.5% or less Actual Quarterly Performance 2013/14 Quarter 1 Quarter 2 Quarter 3 Quarter 4 4.1% 4.5% 4.3% 5.1% The number of admissions to the Trust’s mental health acute wards that were gate kept by the Assessment and Home Treatment Teams When service user admissions are assessed (“gate kept”) by their local Assessment and Home Treatment Team, service users have the opportunity to be treated in their own home. Wherever possible we offer service users the choice to be supported in their own home as an alternative to hospital admission. This is recognised as best practice and monitored by the Trust Development Authority’s Accountability Framework. The method for calculating performance is as follows: “the number of admissions to the Trust’s acute wards (excluding internal transfers between wards, patients recalled from community treatment orders, and patients Performance Threshold 95% or over Quality accounts on leave under Section 17 of the Mental Health Act) that were gate kept by the Assessment and Home Treatment team prior to admission. An admission has been ‘gate kept’ if the team assessed the service user before admission and involved them in the decision making process that resulted in the hospital admission. This is expressed as a percentage of total admissions to the Trust’s acute mental health wards.” In order to achieve the highest level of compliance (“Performing”) the Trust must ensure that 95% of admissions to acute mental health wards were gate kept by the Assessment and Home Treatment Teams. The 2013/14 performance is shown in Table 3. The Trust is pleased to report that a level of ‘Performing’ was consistently achieved, with scores over 97%, for each quarter in 2013/14. Table below: Percentage of admissions to mental health acute wards that were gate kept. Actual Quarterly Performance 2013/14 Quarter 1 Quarter 2 Quarter 3 Quarter 4 98.8% 98.7% 97.4% 97.7% 63 Percentage of patients readmitted to hospital within 28 days of being discharged. Measuring the percentage of patients who were readmitted to hospital as an emergency within 28 days of being discharged provides information to help us monitor success in avoiding (or reducing to a minimum) readmissions following discharge from hospital. The following table shows the quarterly percentage of all inpatient admissions that were readmitted in an emergency within 28 days of the previous discharge. Quarter 1 Quarter 2 Quarter 3 Quarter 4 Ages 0-14 0.0% 0.0% 0.0% 0.0% Ages 15+ 2.1% 2.5% 1.1% 2.9% Patient experience of community mental health services. To improve the quality of services that the Trust delivers, it is important to understand what people think about their care and treatment. One way of doing this is by asking people who have recently used our services to tell us about their experiences. To assist with this, each year a survey of people aged 18 and over accessing community mental health services is conducted and collated by the Care Quality Commission. A questionnaire was sent to 850 people who accessed community mental health services between 1st July 2012 and 30th September 2012. A total of 269 people responded, giving a 32% response rate for the Trust. This compares to the national response rate of 29%. An excerpt of the survey results, specifically covering the patient’s experience of contact with a health or social care worker is shown in Table 6 below. The full report has been published by the CQC and is available on their website. Table below: Patient experience of contact with a health or social care worker: Trust’s 2013 score. (score out of 10) Compared with the national response, we scored: Listening: for the health or social care worker seen most recently was listening 9.0 carefully to them. Better Involvement: for the health or social care worker seen most recently taking their views into account 8.6 About the same Trust and confidence: for having trust and confidence in the health or social care worker seen most recently 8.5 About the same Respect and dignity: for being treated with respect and dignity by the health 9.5 or social care worker seen most recently About the same Time: for being given enough time to discuss their condition and treatment with the health or social care worker seen most recently 8.4 About the same Overall experience of contact with the health or social care worker seen most recently. 8.8 About the same Figures taken from the CQC website: http://www.cqc.org.uk/survey/mentalhealth/R1A 64 Annual Report 2014-15 Worcestershire Health Overview and Scrutiny Committee (HOSC) Comments 2014 Patient Safety Incidents The number of patient safety incidents reported in the Trust during 2013/14: 5,362 The number of patient safety incidents that resulted in severe harm or death: 72 (1.34%) Examples of Patient Safety Incidents that result in severe harm are grade 4 pressure ulcers (both avoidable and unavoidable) and falls where the patient sustains a fracture. All such incidents undergo a thorough investigation to establish the root cause of the incident, and in many instances nothing could have been done to prevent the incident. Where a death is recorded on the system, this is where a patient who is known to our services dies unexpectedly – this does not mean that the death was preventable. Large scale investigations are undertaken in such instances to establish if the care provided in our services was safe and appropriate, and whether there was anything that could have been done to prevent the death. Quality accounts In making its response, the HOSC considers information made available throughout the year which is supported by the Quality Account. The information received on a regular basis regarding Worcestershire Health and Care Trust (the Trust) includes regular bulletins, specific presentations about proposals for significant changes, and board meetings, which HOSC’s two lead members attend. Overall Comments 1. The Quality Account is very easy to read which makes it accessible and reassuring to the public. 2. The report is very positive about its performance this year, but also points out the areas where improvement is needed. 3. Whilst recognising that community hospitals are only a part of the Trust’s services, it is believed that the public would expect the role of community hospitals and medical care in prisons to be referred to. Review of 2013/14 1. The snapshot review is accessible to the reader and it is appreciated that inclusion of excessive performance criteria and data can be overwhelming to the public. However it is suggested that the report makes this clear and includes a link to the more detailed information and data available on the public website, for those who may be interested. 2. New Haven – a new kind of facility (for older people with mental health illnesses) – the appropriateness of the word ‘recovery’ is queried, although it is appreciated that it is a nationally recognised term within mental health. 3. Child and Adolescent Mental Health Service (CAMHS) – the Trust is congratulated on reducing average appointment waiting times from 18 to 5 weeks, and is encouraged to work towards reducing this further. (Children’s Scrutiny Panel Chair may have further comment) 4. West Midlands Quality Review Service peer review programme for long term conditions 2013 5. The Trust is encouraged to clarify the situation regarding the model for specialist care for people with chronic neurological conditions. 65 CCG Response to Worcestershire Health & Care Trust Quality Account 2013/14 Quality Account Priorities – progress review and looking forward 1. Continue to improve our response times and learning from complaints (Priority 2) – it would be helpful to include some background information in order to provide reassurance to the reader that learning has taken place. 2. Pressure ulcers (priority 4) are distressing for patients and the need to continue to focus on reducing pressure ulcers is recognised. It is appreciated that the Trust has been working hard to progress this and now has better reporting mechanisms in place to monitor documentation and assessment. The difficulty in inherited patient cases is appreciated. It would be helpful to clarify the term ‘avoidable pressure ulcer’. 3. Commissioning for Quality and Innovation (CQUIN) for 2014/15 – improving patient flow is also being looked at through a HOSC desktop exercise and the HOSC will liaise with the Trust on this. 4. Plans to understand and improve young people’s experiences of sexual health services are pleasing. 2013/14 Quality Account Technical Section – Mandatory Statements 1. Statements for the CQC (p36) - It would be helpful to clarify the background to the CQC’s warning notice issued against the Trust in respect of offender healthcare, and it is concerning that provision of medical care within the prison environment has become increasingly challenging. 2. Summary of serious incident (p38) – the commentary gives reassurance that this was a one-off incident. Worcestershire Health Overview and Scrutiny commentary In providing this response, the three Clinical Commissioning Groups (CCGs) for Worcestershire (NHS South Worcestershire CCG, NHS Redditch and Bromsgrove CCG and NHS Wyre Forest CCG), considers the regular information and assurance generated through the Clinical Quality Review and other associated on-going Quality Assurance processes. Based on the on-going assurance processes adopted within the Trust and the information available to us, commissioners believe this provides a broadly representative and balanced perspective of the quality of healthcare provided. However comments have been included to reflect areas where further information would have been helpful to more accurately describe the Trust outputs in relation to quality improvement over the last 12 months. Overall comments It is encouraging to continue to see the breadth of work and achievement against existing quality standards and initiatives across the three domains of patient safety, patient experience and clinical effectiveness. The account is written in plain English format and is very ‘readable’. Quality improvements are well detailed and are to be congratulated. The ‘Snapshot Review 2013/14’ provides a helpful and informative summary of achievements over this period. Improvement priorities for 2014/15 are detailed in a concise and ‘readable’ format, with purposeful explanations of what the Trust hopes to achieve; why it was identified as priority and how it is planned to achieve improvements. The achievement against the quality improvement measures within the CQUIN scheme for 2013/14 is indicative of a commitment to delivering high quality and safe care for patients, and the inclusion of 2014/15 CQUIN scheme detail is welcome. The Trust achievement in improving its complaints handlings processes and its focus on translating learning into sustained improvement is to be congratulated. There is provision of very detailed information regarding learning from individual clinical audits and what actions the Trust have taken to achieve improvement, which 66 Annual Report 2014-15 shows a commitment to understand and learn where improvement is needed. The improvements in the Trust’s systems and processes in identifying; investigating and learning from patient safety incidents are noted, and the Trust’s continued commitment to further improve is to be commended. There are number of areas detailed below where commissioners believe that more information would be helpful in highlighting where improvement activity has been focussed across all services. Inclusion of the following information would provide a more balanced account of how services have developed over the year: • The document focuses on the achievements made within Mental Health Services but does not, for example, reflect the areas of improvement made following additional investment in Community Services and Integrated Care Teams, or the impact of the role of the new Care Home Practitioner within South Worcestershire in enhancing the quality of care and experience for care home residents. • An update on developments within Children’s Services would have been helpful i.e. School Nursing Services; Health Visitors; Children’s Nursing Service. • Preventing Avoidable Pressure Ulcers (Priority 1 carried over from 2013/14). It would be helpful to understand what has been learned from investigations over the last year and how the Trust responded in translating learning into actions to achieve improvement. • Detail regarding the impact of patient falls and the work planned to reduce incidents of this nature would help provide assurance that the Trust continues to be focussed on this area of potential harm. • It would be helpful to see more detail regarding ‘Staff Survey’ results i.e. what was raised and how the Trust listened and responded to its staff. This would provide a more balanced view of how the organisation responds and acts upon feedback. It is also unclear what the ‘5 top ranking scores’ on page 5 means – again more explanation and context would be helpful. Commissioners will continue to hold the Trust to account for performance against the priorities and improvement targets detailed in this Quality Account during 2014/15, through the existing Quality Assurance processes Quality accounts established with the Trust. NB Offender Healthcare Services. Currently the Trust delivers Offender Healthcare Services for a number of West Midland’s Prisons. These services are currently commissioned through Staffordshire and Shropshire Area Team as lead commissioner for the West Midlands, who monitor performance of the Trust in this area. As such this response by the three Worcestershire CCGs has not commented on any areas relating to Offender Healthcare specifically. Changes Made as a Result of Feedback from HOSC and the CCGs We would like to thank HOSC and the CCGs for taking the time to read the draft Quality Account and for providing helpful feedback. The Trust provides a wide range of services, and we have to make difficult decisions regarding how much information can be included in the Quality Account whilst keeping the document within the recommended number of pages. Further information about Trust services is provided in the annual report and is available on the Trust’s website. The following changes were made to the Quality Account as a result of the feedback: • Clarification of the CQC’s warning notice issued against the Trust in respect of offender healthcare. • Further background information for learning from complaints • Addition of the definition of the term ‘avoidable’ and ‘unavoidable’ pressure ulcer included. • Additional information regarding falls prevention work in the Trust • Additional information regarding learning from investigations • More context around the staff survey and staff engagement is contained within the annual report. On behalf of NHS Redditch and Bromsgrove, South Worcestershire and Wyre Forest Clinical commissioning groups (CCGs). 67 Worcestershire Healthwatch comments on the Worcestershire Health and Care Trust Quality Account 2013/14 The response by Healthwatch Worcester does include other information provided by the Worcestershire Health and Care Trust (the Trust) on a regular basis throughout the year which underpins the information provided by the Quality Account. This includes reviewing and responding where appropriate, to written materials, attending Trust Board Meetings and Presentations explaining the work of the Trust, including proposals for significant changes to the service. General Comments. 1. One important objective of the Quality Account is to inform members of the public and service users what the Trust has been doing throughout the year, the achievements and the improvements it has made and to point out where the Trust needs to perform better. While it does that, it is hard to believe that the average member of the public is going to wade through a report this size. Notwithstanding the requirements on the Trust to meet a set standard for reporting, a pithier, user friendly document aimed at the general public would seem timely. 2. The report contains many examples of improvements to the Services provided by the trust and rightly recognises the hard work of staff at all levels this year, it does however, highlight areas where improvement need to be made 3. We appreciate that Community Hospitals are an important part of the trusts services to the general Worcestershire Community However; we would also expect the work of Community Hospitals and medical care in prisons to be reported. 4. Healthwatch would also like to see information on the provision of tier 3 & 4th beds for children. We would expect to have information on the number of children in those facilities and where those beds are and finally some information on outcomes. 5. WE were greatly heartened to see a significant reduction in waiting times for CAMHS. This Service faces great pressures and it would have been helpful to have reassurance that the improvements could be maintained. 6. While it is appreciated that the Trust has more beds for those with serious Mental Health conditions, it would be useful to know how many patients are successfully placed in the local hospital. Travel by families, 68 particularly, those without transport is becoming more problematical. 7. Significant changes are taking place in the Children’s Respite Services. Fewer days are being offered to parents and there is the prospect of variable days being introduced. Healthwatch would like reassurance that parents have been involved and meaningfully consulted on the proposed changes. 8. The Trust is to be congratulated in the successful efforts it has made in significantly improving employment for those with Mental Health conditions. All the more laudatory in a period of recession. 9. We note with interest the use of people who have experienced mental health conditions in hospital treatment teams and are impressed by the results. We appreciate this is a relatively new departure but are intrigued by the possibility of such a development in other areas of the service. 10. We would like to add our support to the trusts vision that whenever possible services should be provided in a person’s own home and we look forward to the vision being converted to a reality. However, we also recognise that some beds will be needed in Community Hospitals and that the balance requires fine judgements and delicate handling. Quality Account Priorities – progress review and looking forward. 1. We would find it useful to understand how learning from complaints manifests itself in improvements in the service. We would also be interested to learn if that process contained a module or section on Customer Care, since many complaints contain concerns about poor communication with carers. 2. We note that the Trusts objective to eradicate pressure ulcers, are behind schedule. While we appreciate the difficulties we would encourage the trust to continue to strive to eliminate those ulcers that are avoidable. It would be useful to understand when ulcers are unavoidable. 3. We support the Trust plans to improve Sexual Health Services for young people. Annual Report 2014-15 Statement of directors’ responsibilities in respect of the Quality Account Quality Account Technical SectionMandatory Statement We would find it helpful to understand the circumstances in which the warning was issued by the CQC, In view of reports that there are difficulties with Healthcare in Prisons and Worcestershire Health Trust have responsibilities her, more information would be welcome. Worcestershire Healthwatch. Statement of directors’ responsibilities in respect of the Quality Account The directors are required under the Health Act 2009 to prepare a Quality Account for each financial year. The Department of Health has issued guidance on the form and content of annual Quality Accounts (which incorporates the legal requirements in the Health Act 2009 and the National Health Service (Quality Accounts) Regulations 2010 (as amended by the National Health Service (Quality Accounts) Amendment Regulations 2011). In preparing the Quality Account, directors are required to take steps to satisfy themselves that: • The Quality Account presents a balanced picture of the Trust’s performance over the period covered; • The performance information reported in the Quality Account is reliable and accurate; • There are proper internal controls over the collection and reporting of the measures of performance included in the Quality Account, and these controls are subject to review to confirm that they are working effectively in practice; • The data underpinning the measures of performance reported in the Quality Account is robust and reliable, conforms to specified data quality standards and prescribed definitions, and is subject to appropriate scrutiny and review; and • The Quality Account has been prepared in accordance with Department of Health guidance. The directors confirm to the best of their knowledge and belief they have complied with the above requirements in preparing the Quality Account. By order of the Board 25 June 2014 ________________________________ Chair 25 June 2014 _________________________________ Chief Executive Quality accounts 69 70 Annual Report 2014-15 Quality accounts 71 72 Annual Report 2014-15 Financial statements The Financial Statements shown on the following pages are a summary of the information set out in the Trust’s statutory accounts for the year ended 31 March 2014. The Annual Report and Accounts (ARA) document is available on request from the Director of Finance at Isaac Maddox House, Shrub Hill Road, Worcester, WR4 9RW (Tel. 01905 760020). expenditure within its capital resource limit. The operating revenue surplus of £2.9m, includes an additional £0.6m on a non-recurrent basis, and was delivered on a turnover of £172m. The cash and capital out-turns were both satisfactorily managed, the latter to within a thousand pounds of the agreed limit. The 2014/15 budgets have been approved by the Trust Board and Service Delivery Unit managers can look forward to operating and managing services in the knowledge that their budgets have been adequately funded for inflation and that the Trust has a contingency reserve of 1%. The annual report itself comprises of: • Strategic report (replaces the business review), • Directors’ report, • Remuneration report • A statement of the Accountable Officer’s responsibilities • A Governance Statement • The primary financial statements and notes to the accounts. • The audit opinion and report. I am pleased to report that the Trust is well placed to deliver its healthcare responsibilities over the longer term with the Trust Board having approved a robust 5 year long term financial plan and integrated business plan. It is pleasing to report that for the third consecutive year the Trust has achieved each of its statutory financial duties by delivering overall financial balance, operating within its external financing limit and managing capital The Trust is proud of the achievements delivered over the last year and looks forward with confidence to 2014/15 and beyond. These plans are currently being updated and are being critically appraised and tested to ensure that there will be no diminution in the quality of our services. The external auditors have issued an unqualified opinion on the Trust’s 2013/14 annual report and accounts. That opinion confirmed that the information given in the 2013/14 annual report is consistent with the financial statements. Worcester Cathedral and the River Severn, Worcester Financial accounts 73 Statement of Comprehensive Income for year ended 31 March 2014 2013-14 £000 2012-13 £000 Employee benefits (129,458) (124,255) Other Operating costs (41,755) (43,224) Revenue from patient care activities 165,726 155,906 Other Operating revenue 6,588 14,929 Operating surplus/(deficit) 1,101 3,356 Investment revenue 39 35 Other gains and (losses) 0 (363) Finance costs (205) (204) Surplus/(deficit) for the financial year 935 2,824 Public dividend capital dividends payable (713) (986) Retained surplus/(deficit) for the year 222 1,838 Impairments and reversals 41 (272) Net gain/(loss) on revaluation of property, plant & equipment 3,527 0 Net gain/(loss) on revaluation of intangibles 0 0 Net gain/(loss) on revaluation of financial assets 0 0 Net gain/(loss) on other reserves 0 0 Net gain/(loss) on available for sale financial assets 0 0 Net actuarial gain/(loss) on pension schemes 0 0 Reclassification adjustment on disposal of available for sale financial assets 0 0 Other Comprehensive Income for the year 3,568 (272) Total Comprehensive Income for the year 3,790 1,566 Retained surplus/(deficit) for the year 222 1,838 Prior period adjustment to correct errors 0 0 IFRIC 12 adjustment 0 0 Impairments 2,672 667 Adjustments iro donated asset/gov’t grant reserve elimination 26 17 Adjustment re Absorption accounting 0 0 Adjusted retained surplus/(deficit) 2,920 2,522 Other Comprehensive Income Financial performance for the year The Trust’s Reported NHS financial performance position is derived from its retained surplus, but adjusted for the following: a) Impairments to Fixed Assets 2013/14 which were based upon the District Valuer’s report on the Trust’s land and buildings. b) Depreciation on donated assets. 74 Annual Report 2014-15 Statement of Financial Position as at 31 March 2014 31 March 2014 31 March 2013 £000 £000 Property, plant and equipment 89,762 43,241 Intangible assets 4 36 Investment property 0 0 Other financial assets 0 0 Trade and other receivables 0 0 Total non-current assets 89,766 43,277 Inventories 433 444 Trade and other receivables 4,020 7,707 Other financial assets 0 0 Other current assets 0 0 Cash and cash equivalents 12,520 9,105 Total current assets 16,973 17,256 Non-current assets held for sale 1,185 1,150 Total current assets 18,158 18,406 Total assets 107,924 61,683 Trade and other payables (15,354) (17,102) Other liabilities 0 0 Provisions (1,371) (910) Borrowings (38) (76) Other financial liabilities 0 0 Working capital loan from Department 0 0 Capital loan from Department (764) (764) Total current liabilities (17,527) (18,852) Non-current assets plus/less net current assets/liabilities 90,397 42,831 Non-current assets: Current assets: Current liabilities Financial accounts 75 Statement of Financial Position as at 31 March 2014 continued 31 March 2014 31 March 2013 £000 £000 Non-current liabilities Trade and other payables 0 0 Other Liabilities 0 0 Provisions (2,535) (1,889) Borrowings 0 (38) Other financial liabilities 0 0 Working capital loan from Department 0 0 Capital loan from Department (4,753) (5,517) Total non-current liabilities (7,288) (7,444) Total Assets Employed: 83,109 35,387 Public Dividend Capital 34,732 34,181 Retained earnings 35,074 (90) Revaluation reserve 13,277 1,270 Other reserves 26 26 Total Taxpayers’ Equity: 83,109 35,387 FINANCED BY: TAXPAYERS’ EQUITY The financial statements on pages 74 to 80 were approved by the Audit Committee under the delegated authority of the Trust Board on 5 June 2014 and signed on its behalf by: Sarah Dugan Chief Executive 76 Annual Report 2014-15 Statement of Changes in Taxpayers’ Equity For the year ended 31 March 2014 Public Dividend capital Retained earnings Revaluation Other reserve reserves Total reserves £000s £000s £000s £000s £000s 34,181 (90) 1,270 26 35,387 Retained surplus for the year 0 222 0 0 222 Net gain / (loss) on revaluation of property, plant, equipment 0 0 3,527 0 3,527 Balance at 1 April 2013 Changes in taxpayers equity for 2013-14 Net gain / (loss) on revaluation of intangible assets 0 0 0 0 0 Net gain / (loss) on revaluation of financial assets 0 0 0 0 0 Net gain / (loss) on revaluation of assets held for sale 0 0 0 0 0 Impairments and reversals 0 0 41 0 41 Other gains/(loss) 0 0 0 0 0 Transfers between reserves* 0 162 (162) 0 0 Transfers under Modified Absorption Accounting - PCTs & SHAs 0 43,381 0 0 43,381 Transfers to/(from) Other Bodies within the Resource Account Boundary 0 0 0 0 0 Transfers between Revaluation Reserve & Retained Earnings in respect of assets transferred under absorption 0 0 0 0 0 Reclassification Adjustments On Disposal of Available for Sale financial Assets 0 0 0 0 0 Reserves eliminated on dissolution 0 0 0 0 0 Originating capital for Trust established in year 0 0 0 0 0 New PDC Received** 551 0 0 0 551 PDC Repaid In Year** 0 0 0 0 0 PDC Written Off 0 0 0 0 0 Transferred to NHS Foundation Trust 0 0 0 0 0 Other Movements in PDC In Year 0 0 0 0 0 Net Actuarial Gain/(Loss) on Pension 0 0 0 0 0 Net recognised revenue/(expense) for the year 551 43,765 3,406 0 47,722 Transfers between reserves in respect of modified absorption PCTs & SHAs 0 (8,601) 8,601 0 0 Balance at 31 March 2014 34,732 35,074 13,277 26 83,109 Financial accounts 77 Statement of Changes in Taxpayers’ Equity For the year ended 31 March 2014 contined. Balance at 1 April 2012 Public Dividend capital Retained earnings Revaluation Other reserve reserves Total reserves £000s £000s £000s £000s £000s 32,412 (2,038) 1,652 26 32,052 Changes in taxpayers equity for 2012-13 Retained surplus/(deficit) for the year 0 1,838 0 0 1,838 Net gain / (loss) on revaluation of property, plant, equipment 0 0 0 0 0 Net gain / (loss) on revaluation of intangible assets 0 0 0 0 0 Net gain / (loss) on revaluation of financial assets 0 0 0 0 0 Net gain / (loss) on revaluation of assets held for sale 0 0 0 0 0 Impairments and reversals 0 0 (272) 0 (272) Movements in other reserves 0 0 0 0 0 Transfers between reserves* 0 110 (110) 0 0 Release of reserves to Statement of Comprehensive Income 0 0 0 0 0 0 0 0 0 0 Reclassification Adjustments Transfers to/(from) Other Bodies within the Resource Account Boundary On Disposal of Available for Sale financial Assets 0 0 0 0 0 Reserves eliminated on dissolution 0 0 0 0 0 Originating capital for Trust established in year 0 0 0 0 0 New PDC Received 2,718 0 0 0 2,718 PDC Repaid In Year (949) 0 0 0 (949) PDC Written Off 0 0 0 0 0 Transferred to NHS Foundation Trust 0 0 0 0 0 Other Movements in PDC In Year 0 0 0 0 0 Net Actuarial Gain/(Loss) on Pension 0 0 0 0 0 Net recognised revenue/(expense) for the year 1,769 1,948 (382) 0 3,335 Balance at 31 March 2013 34,181 (90) 1,270 26 35,387 Notes: * Transfers between reserves relates to backlog depreciation. ** The values for new PDC received in year and PDC repaid in year relate to the transfer of assets between this Trust and Worcestershire Acute Hospitals NHS Trust. 78 Annual Report 2014-15 Statement of Cash Flows for the year ended 31 March 2014 2013-14 2012-13 £000 £000 Operating Surplus/Deficit 1,101 3,356 Depreciation and Amortisation 2,881 2,288 Impairments and Reversals 2,672 667 Other Gains / (Losses) on foreign exchange 0 0 Donated Assets received credited to revenue but non-cash 0 0 Government Granted Assets received credited to revenue but non-cash 0 0 Interest Paid (157) (153) Dividend paid (649) (1,053) Release of PFI/deferred credit 0 0 (Increase)/Decrease in Inventories 11 (22) (Increase)/Decrease in Trade and Other Receivables 3,623 4,092 (Increase)/Decrease in Other Current Assets 0 0 Increase/(Decrease) in Trade and Other Payables (3,442) 1,829 (Increase)/Decrease in Other Current Liabilities 0 0 Provisions Utilised (434) (198) Increase/(Decrease) in Provisions 1,493 666 Net Cash Inflow/(Outflow) from Operating Activities 7,099 11,472 Interest Received 39 35 (Payments) for Property, Plant and Equipment (4,584) (8,748) (Payments) for Intangible Assets 0 0 (Payments) for Investments with DH 0 0 (Payments) for Other Financial Assets 0 0 (Payments) for Financial Assets (LIFT) 0 0 Proceeds of disposal of assets held for sale (PPE) 1,150 949 Proceeds of disposal of assets held for sale (Intangible) 0 0 Proceeds from Disposal of Investment with DH 0 0 Proceeds from Disposal of Other Financial Assets 0 0 Proceeds from the disposal of Financial Assets (LIFT) 0 0 Loans Made in Respect of LIFT 0 0 Loans Repaid in Respect of LIFT 0 0 Rental Revenue 0 0 Net Cash Inflow/(Outflow) from Investing Activities (3,395) (7,764) NET CASH INFLOW/(OUTFLOW) BEFORE FINANCING 3,704 3,708 Cash Flows from Operating Activities CASH FLOWS FROM INVESTING ACTIVITIES Financial accounts 79 Statement of Cash Flows for the year ended 31 March 2014 continued 2013-14 2012-13 £000 £000 CASH FLOWS FROM FINANCING ACTIVITIES 80 Public Dividend Capital Received 551 2,718 Public Dividend Capital Repaid 0 (949) Loans received from DH - New Capital Investment Loans 0 3,000 Loans received from DH - New Working Capital Loans 0 0 Other Loans Received 0 0 Loans repaid to DH - Capital Investment Loans Repayment of Principal (764) (464) Loans repaid to DH - Working Capital Loans Repayment of Principal 0 0 Other Loans Repaid (76) (76) Cash transferred to NHS Foundation Trusts 0 0 Capital Element of Payments in Respect of Finance Leases and On-SoFP PFI and LIFT 0 0 Capital grants and other capital receipts 0 0 Net Cash Inflow/(Outflow) from Financing Activities (289) 4,229 NET INCREASE/(DECREASE) IN CASH AND CASH EQUIVALENTS 3,415 7,937 Cash and Cash Equivalents ( and Bank Overdraft) at Beginning of the Period 9,105 1,168 Effect of Exchange Rate Changes in the Balance of Cash Held in Foreign Currencies 0 0 Cash and Cash Equivalents (and Bank Overdraft) at year end 12,520 9,105 Annual Report 2014-15 Pension Liabilities Past and present employees are covered by the provisions of the NHS Pensions Scheme. Details of the benefits payable under these provisions can be found on the NHS Pensions website at www.nhsbsa.nhs.uk/pensions. The scheme is an unfunded, defined benefit scheme that covers NHS employers, GP practices and other bodies, allowed under the direction of the Secretary of State, in England and Wales. The scheme is not designed to be run in a way that would enable NHS bodies to identify their share of the underlying scheme assets and liabilities. Therefore, the scheme is accounted for as if it were a defined contribution scheme: the cost to the NHS Body of participating in the scheme is taken as equal to the contributions payable to the scheme for the accounting period. Other Creditors include £1,730,000 pension costs at 31 March 2014 (£1,616,000 at 31 March 2013). The accounting policy for Pensions and outline of the scheme is set out on page 23 of the Trust’s Annual Accounts. The remuneration report on page 115 of the Annual Report provides the details of the pension entitlements of Senior Managers. Better Payment Practice Code Measure of compliance 2013-14 2013-14 2012-13 2012-13 Number £000 Number £000 Total Non-NHS trade invoices paid in the year 30,580 31,961 31,900 27,527 Total Non-NHS trade invoices paid within target 29,686 31,191 31,093 27,087 Percentage of NHS trade invoices paid within target 97.1% 97.6% 97.5% 98.4% Total NHS Trade Invoices Paid in the Year 669 16,727 987 19,193 Total NHS Trade Invoices Paid Within Target 651 16,679 977 19,135 97.3% 99.7% 99.0% 99.7% Non-NHS Payables NHS Payables Percentage of NHS Trade Invoices Paid Within Target The Better Payment Practice Code requires the Trust to aim to pay all valid invoices by the due date or within 30 days of receipt of a valid invoice, whichever is later. Prompt Payments Code: The Trust has applied to join the prompt payment code in accordance with David Nicholson’s letter of 18 May 2009. Financial accounts 81 Related party transactions Details of related party transactions with individuals are as follows: Age UK Herefordshire and Worcestershire (spouse of Trust Chairman is Head of Finance of this related party) Payments to Related Party Receipts from Related Party Amounts owed to Related Party Amounts due from Related Party £ £ £ £ 684 0 0 0 Worcestershire Health and Care NHS Trust is a corporate trustee of Worcestershire Health and Care NHS Trust Charitable Funds (Charity No. 1060335) The Trust has received revenue payments from this Charity, which are summarised below. The unaudited summary financial statements of this Charity are included in the Trust’s annual report. Payments to Related Party Receipts from Related Party Amounts owed to Related Party Amounts due from Related Party £ £ £ £ 0 17,983 0 0 The transactions between the Trust and the Charity are: Administration fee The Trust has not made any provisions for doubtful debts in respect of transactions with related parties. The Department of Health is regarded as a related party. During the year Worcestershire Health and Care NHS Trust has had a significant number of material transactions with the Department and with other entities for which the Department is regarded as the parent Department. The entities where these transactions were at least £500,000 in value for the year are: 82 Annual Report 2014-15 Related Party Birmingham Cross City CCG Birmingham South and Central CCG Health Education England Herefordshire CCG NHS England (Arden, Herefordshire & Worcestershire Area Team) Purpose of Transaction Supply of Healthcare Supply of Healthcare Funding for Training Supply of Healthcare Supply of Healthcare NHS England (Shropshire and Staffordshire Area Team) Redditch and Bromsgrove CCG South Worcestershire CCG Worcestershire Acute Hospitals NHS Trust Supply of Healthcare Supply of Healthcare Supply of Healthcare Purchase/Supply of Healthcare Supply of Healthcare Wyre Forest CCG In addition, the Trust has had a number of material transactions, a total of at least £100,000 in value in year, with other central and local government bodies. These transactions have been with: Related Party Bromsgrove District Council HM Revenue & Customs Malvern Hills District Council NHS Pensions Agency Redditch Borough Council Staffordshire County Council Worcestershire City Council Worcestershire County Council Wychavon District Council Wyre Forest Council Financial accounts Purpose of Transaction Payment of Rates Payment of Income Tax Payment of Rates Payment of Superannuation Payment of Rates/Supply of Healthcare Supply of Healthcare Payment of Rates Supply of Healthcare/ Staff Costs Payment of Rates/Rent Payment of Rates 83 NHS Trust Charitable Funds 2013-14 The unaudited summary financial statements for the Worcestershire Health and Care NHS Trust Charitable Funds (Charity No. 1060335) are shown below: Unaudited Statement of financial activities for the year ended 31 March 2014 Recommended categories by activity Unrestricted funds Restricted funds Endowment funds Total 2013/14 Total 2012/13 £000 £000 £000 £000 £000 Incoming resources Incoming resources from generated funds 0 0 0 0 0 37 150 0 187 184 0 0 0 0 0 Investment income 10 19 0 29 24 Total incoming resources 47 169 0 216 207 Costs of Generating Funds 0 0 0 0 0 Investment management costs 2 2 0 4 4 Charitable activities 7 52 0 59 92 Governance costs 7 13 0 20 19 Other resources expended 0 0 0 0 22 16 67 0 83 138 31 102 0 133 70 8 9 0 17 55 39 111 0 150 125 Total funds brought forward at 1 April 2013 251 633 0 884 759 Total funds carried forward at 31 March 2014 290 744 0 1,034 884 Voluntary income Activities for generating funds Resources expended Total resources expended Net incoming/(outgoing) resources before other recognised gains/(losses) Gains and losses on investment assets Net movement in funds 84 Annual Report 2014-15 NHS Trust Charitable Funds 2013-14 Unaudited Balance Sheet as at 31 March 2014 Unrestricted funds Restricted funds Endowment funds Total 2013/14 Total 2012/13 £000 £000 £000 £000 £000 Fixed assets Investments 253 696 0 949 784 253 696 0 949 784 Stock and work in progress 0 0 0 0 0 Debtors 1 3 0 4 4 36 48 0 84 107 37 51 0 88 111 0 3 0 3 11 Net current assets 37 48 0 85 100 Total net assets 290 744 0 1,034 884 Unrestricted funds 290 0 0 290 251 Restricted income funds 0 744 0 744 633 Endowment funds 0 0 0 0 0 290 744 0 1,034 884 Total fixed assets Current assets Cash at bank and in hand Total current assets Creditors: amounts falling due within one year Funds of the Charity Total funds Financial accounts 85 86 Annual Report 2014-15 Financial accounts 87 88 Annual Report 2014-15 Financial accounts 89 90 Annual Report 2014-15 Financial accounts 91 Operating and financial review (OFR) 1. Nature, objectives and strategies of the business. This provides an understanding of the NHS body, including a description of: The location and type of facilities provided and the structure of the business including its main services and users The Trust is one of two local National Health Service organisations that provide healthcare services commissioned by the three Clinical Commissioning Groups in Worcestershire and other neighbouring Commissioners, including Worcestershire County Council. 85% of the Trust’s £172m income will be secured through CCG commissioning arrangements, with 7% commissioned by NHS England and 8% through the Public Health service within the Local Authority. The Trust is the main provider of community, specialist primary care and mental health services to the population of Worcestershire and beyond. Many of our services, including learning disability services are integrated with Worcestershire County Council and we work in partnership across the county with voluntary organisations, our commissioners and communities to deliver high quality services. The Trust’s main responsibilities cover: 1. Working to deliver the best possible healthcare to the Trust’s patients in hospital, in the community and at home. For example the Trust provides these services from 150 properties across Worcestershire, including the community hospitals in Bromsgrove, Evesham, Pershore, Malvern and Tenbury along with various health centres and clinics. The Trust also delivers mental health in-patient care from four hospitals in Worcester, Redditch, Bromsgrove and Kidderminster. The Trust has a total of 402 inpatient beds. 2. Safeguarding the organisation’s assets and public funds. 3. Maintaining a sound system of internal control that supports the achievement of the organisation’s objectives. 4. Reporting upon its performance across the Targets and Performance indicators required by the Trust Development Authority; and to the Department of Health. 5. Delivering healthcare that is good value for money. The Trust is governed by a Board, which is supported by the following formal committees who meet on a regular basis throughout the year to review and assess and regulate the activities and responsibilities of the Trust: • Finance and Performance • Quality and Safety • Audit • Remuneration • Charitable funds • Community Engagement (up to July 2013) The Board has also established a Foundation Trust Programme Board to oversee the Trust’s application for NHS Foundation Trust status and a Partnership Forum is being developed to facilitate joint working and sharing of information across partner organisations. This forum is not a Board committee. The Trust currently measures performance against three performance regimes, which are the Trust Development Authority Provider Management Regime, the Mental Health Performance Framework and Monitor’s Compliance Framework. 92 Annual Report 2014-15 The 5 Service Delivery Units (SDUs) are responsible for the delivery of services, including all aspects of performance, quality, activity, assurance and financial matters, as well as significantly contributing to strategy and service development. The corporate services ‘wrap around’ SDUs to support overall strategic planning, implement and deliver against plans and provide assurance against all governance frameworks. The 5 Service Delivery Units are: • Community care • Adult Mental Health • Children, Young People and Families • Specialist Primary Care • Integrated Learning Disability The external Worcestershire Health and Care NHS Trust serves a population of approximately 569,000 environment in which it across an area of approximately 500 square miles, with a relatively high proportion of operates residents aged 65 and above, whereas in Worcester City there is a significant student population. A brief history of the NHS body and its statutory background Disclosure on legacy balance transfers Worcestershire Health and Care NHS Trust was established on 1 July 2011 to manage the vast majority of the services which were previously managed by Worcestershire PCT’s Provider Arm, as well as the mental health services that were managed by Worcestershire Mental Health Partnership NHS Trust. Bringing together the range of services provided by the two organisations has offered opportunities to improve integration and partnership working which are central to the Trust’s objectives. The Trust is a community based provider of comprehensive health and social care services, expertise and choices for people with a range of health needs and/or disabilities. These services are provided in a wide range of community settings. These include people’s own homes, community clinics, outpatient departments, community inpatient beds, prisons, schools and GP practices. We also provide in-reach services into acute hospitals, nursing and residential homes and social care settings. In accordance with the Health and Social Care Act 2012, Strategic Health Authorities and Primary Care Trusts were dissolved on 1 April 2013 and their assets and liabilities transferred to successor bodies in the NHS or to other entities. Under the terms of the Property Transfer Scheme: Schedule of properties and property related assets and liabilities, a number of assets and liabilities were transferred from Worcestershire Primary Care Trust to the Trust on that date. The most significant of these were: • Evesham Community Hospital • Malvern Community Hospital (Seaford Court) • Princess of Wales Community Hospital • Tenbury Community Hospital These assets and liabilities are associated with the Transforming Community Services (TCS) plan, under which the responsibility for providing many services previously provided by the Worcestershire Primary Care Trust passed to the Trust on 1 July 2011. The accounting arrangements in respect of these transfers are outlined in Note 1.3 to the Annual Accounts. Financial accounts 93 The objectives of the Trust over the long term, the time scale used being dependent on the type of objective. Objectives will be defined in terms of non-financial and financial performance The Trust has developed a five year integrated business plan that sets out the strategic direction for the organisation. The Trust’s vision is to be: ‘A leading organisation that works effectively in partnership with our stakeholders to deliver high quality integrated health and care services’ The Trust has defined a set of values that clarify what it believes in and how it will behave: • Courageous:Displaying integrity, loyalty and the courage to always do what is right • Ambitious: Striving to innovate and to improve through effective teamwork • Responsive:Focusing on the needs and expectations of people using our services • Empowering:Empowering people to take control of their own health and wellbeing • Supportive:Enabling our staff to achieve full potential and take pride in the services that they deliver. To achieve the Trust Vision four strategic goals have been set out, these are: • We will always provide an excellent patient experience • Our services will always be safe and effective • We will work in partnership to improve the integration of health and care • Our organisation will be efficient, inclusive and sustainable Following the formal establishment of the Trust further work has been undertaken to develop a clinical strategy. It sets out how the organisation will drive forward clinical care and improvements in quality over the next 5 years. The following statement summarises the Trust’s Clinical Strategy: ‘We deliver high quality expertise and choices for people with a range of health needs and/or disabilities that enable people to live independently or as close to home as possible’ The Trust’s strategic goals have been subdivided into corporate objectives that are more specific. The ten corporate objectives are listed below, the Trust defines specific projects to deliver each of the corporate objectives: • To stimulate a revolution in the way we engage with patients • To redesign clinical pathways • To ensure patient safety • To ensure seamless care through integrating services • To strengthen leadership within our services • To develop our workforce • To improve our use of technology • To develop business opportunities • To deliver our efficiency programme • To make effective use of our estate As part of the Trust’s planning process it has developed a clear plan for each of the services that it currently delivers and also considered market opportunities that could build on the strengths of the organisation. The Trust has ambitious plans to develop its services so that it is in a stronger position to work with partners across the health and social care community to support people to live independently at home or as close to home as possible through the provision of high quality, integrated health care. 94 Annual Report 2014-15 The directors’ strategies for achieving the objectives of the NHS body and the effect of past and current actions undertaken. This includes the Key Performance Indicators, both financial and non-financial, used by the directors to assess progress against their stated objectives At the start of the year the Board recognised, as it has in previous years, that it had a series of development needs and has throughout the year worked to ensure that the Directors continue to enhance and develop their skills and competencies to deliver the Trust’s vision. During 2013/14 the Chairman and Chief Executive have both been subject to 360 degree appraisal as part of their respective personal development. The afternoon of each of the six public Board meetings and an additional five days have been used to address specific Board development needs; or to dedicate time to consider a particular strategic issue e.g. the Francis report. The Trust’s aims and objectives are to establish mechanisms for monitoring and reviewing management performance and to ensure the Trust’s objectives are met, to oversee the delivery of planned services, to develop and maintain an annual business plan and to ensure that national policies and strategies are effectively addressed and implemented within the Trust. Key issues remain the quality and safety of services provided, identifying risks to strategic goals, identifying and delivering cost improvement programmes and achieving Foundation Trust status. The Executive Directors have all agreed personal objectives with the Chief Executive which delivers their contribution to the Trust’s strategies and key objectives. The Directors cascade their objectives to the Associate Directors, who in turn discuss and agree the objectives that they lead on. The Associate Directors then follow the same annual process with the Service Delivery Unit Leads and other Heads of Service. The formal committees to the Board meet on a regular basis throughout the year to review and assess progress with the delivery of the Trust’s strategies and objectives. The Committees are supported in their work by other key stakeholder meetings, such as the Contract Management Board, which is chaired by the one of the local Clinical Commissioning Groups. The Chairman of each Committee presents a report to the Board on the important matters considered by their respective Committees. The Trust Board also receives performance reports at every meeting. The organisation’s key priorities and plans for 2013/14 include the work programmes that have been agreed for the various corporate departments and the 5 service delivery units. Detailed action plans, with quarterly milestones, have also been developed and are monitored via the Trust’s performance review process. In addition to these priorities and work programmes, the Trust has to deliver against a range of statutory targets and standards including: • 18 week referral to treatment waiting time targets • Zero tolerance of waits over 52 weeks • Minor Injuries Unit attenders admitted, transferred or discharged within 4 hours • Compliance with mixed sex accommodation • Care Programme Approach follow up within 7 days • Psychological therapy access (subject to commissioner funding) • Zero tolerance of Meticillin-resistant staphylococcus Aureusis (MRSA) • Delivery of agreed Clostridium difficile (Cdiff ) Infection rate trajectory The Trust has also agreed a number of Commissioning for Quality and Innovation payments (CQUINS) for 2013/14, including the engagement of family/friends and carers/ advocates in the care planning process and improving the physical health care for people with severe and enduring mental health problems. The financial plan for 2013/14 builds on the financial position delivered in 2012/13 and the financial requirements of being a Foundation Trust. The financial plan looks to increase the overall surplus, create stronger contingency flexibility and deal with the legacy issues brought forward from both previous organisations. Financial accounts 95 2. Development and performance of the business for the period under review and in the future The significant features of the development and performance of the NHS body in the year The major service transformation programmes that the Trust will focus on over the next 5 years are: • Extended Primary Care Teams • Community Enhanced Care Teams • Community Treatment Hubs • Mental Health Inpatient and Community Care (including Personality Disorders) • Psychiatric Liaison • Learning Disability Crisis and Resolution Service • Health and Social Care Integration • Children’s Services Although these areas of work represent major transformation there are significant programmes of change and development across the organisation which have been phased over the 5 year timeframe of the integrated business plan. The Trust received additional recurrent funding of £1,142k in 2013/14 in respect of the following service developments: • Enhanced Care Development £500k, • Increase Administration support for the Admissions Prevention Service £17k, • Additional Weekly Blood Collection - HMP Long Lartin £3k, • LD Enhanced Community Service £333k, • Chlamydia Screening £37k, • Fall Specialist Physiotherapist £22k, • Health Visitor expansion £210k and, • £20k additional recurrent investment in Every Child a Talker (ECAT). The Trust’s performance against the 2013/14 key national targets are reported upon on page 19. Analysis of the main trends and factors that Directors consider likely to impact on the future, including the development of new services or the benefits expected from capital investment The main trends and factors that Directors consider likely to impact on the future include the requirement for delivering the Trust’s £7.7m cost improvement programme, in a recurrent manner; the development of service line reporting and the achievement of Foundation Trust status. The target date for Foundation Trust is currently uncertain due to the revised application process, which now involves the Chief Inspectors visit. This is a new form of Care Quality Commission (CQC) inspection, which reviews the quality of care and patient experience across a range of health facilities. If this is cleared it will be followed by a Board to Board meeting with the Trust Development Authority before an inspection by Monitor, the economic regulator. Currently, the Trust does face a degree of delivery risk, for planned CIP schemes, arising from Commissioner approval. The main Capital developments planned within the 2014/15 £6.4m programme concern the implementation of the Estates Strategy (£3.4m), Backlog Maintenance (£0.8m), Information Technology (£0.9m), Ward Refurbishment (£0.3m) and PLACE (Patient Led Assessments of the Care Environment) £0.4m.The balance of £0.6m will be invested in areas such as equipment replacement, anti-ligature works and invest to save schemes. 96 Annual Report 2014-15 The current level of investment expenditure; and planned future expenditure and how this will assist the NHS body to achieve its objectives In 2013/14 the Trust used internally generated funds from depreciation and brought forward revenue surpluses and an asset sale to cover a capital programme of £5.6m. The Trust’s main strategic scheme last year was the completion of the modernisation of New Haven, an Older Adult MH Inpatient facility, which cost £1.2m in year. The Trust also spent £1.3m on implementing its estates strategy, £1.2m on backlog maintenance, £0.5m on ward refurbishments and £0.4m was spent on PLACE. The other areas of substantial expenditure included the replacement of equipment £0.4m, anti-ligature works of £0.2m and information technology £0.4m. Overall there was an £1k under spend against the Trust’s 2013/14 Capital Resource Limit. 3. The resources, principal risks and uncertainties and relationships that may affect the entity’s long term value A description of the resources available to the NHS body and how they are managed For 2013/14, the total turnover for the Trust (mainly received via healthcare contracts with the three Worcestershire Clinical Commissioning Groups, Worcestershire County Council and other NHS Commissioners) was £172m (£171m last year). Budgets are set throughout the Trust up to this limit and it is the responsibility of Budget Holders to ensure that the Service Delivery Units are managed within the allocated budget. Progress during the year on this important area of responsibility is reported at Trust Board meetings and in detail at the Finance and Performance Committee. The business of the Trust is governed by the Trust’s Standing Orders and Standing Financial Instructions; and spending decisions regulated through an approved Scheme of Delegation. The Reported NHS Financial Performance for the year ended 31 March 2014 is an end of year surplus of £222k. This is adjusted for two technical items: • impairments of the Trust’s assets (due to professionally assessed building valuations) £2,672k and, • depreciation on the Trust’s donated assets £26k. The Adjusted Retained Surplus is therefore £2,920k, which is in accordance with the plan and target surplus agreed with the Trust Development Authority. The key strengths and resources, tangible and intangible, which assist it in the pursuit of its objectives and, in particular, those items that are not reflected in the balance sheet Financial accounts The Trust employs 3,200 whole time equivalent staff and has a skilled and committed workforce to meet the challenges of delivering high quality healthcare. The significant contribution made by the Trust’s staff at all levels across clinical and non-clinical activities continues to be a key factor in the Trust’s success. Another major strength of the Trust is its strong and positive partnerships with others which help the Trust to achieve its objectives. Our key partnerships include: • The Trust Development Authority, • Clinical Commissioning Groups, for the provision of healthcare, • Worcestershire County Council, for the pooled budget arrangements covered by section 75 of the NHS Health Act and Joint Commissioning Unit, • Worcestershire Acute Hospitals NHS Trust, in the sharing of support services such as Information Technology, • Staff Side Representatives. 97 Disclosure of strategic, commercial, operational and financial risks where these may significantly affect the NHS body’s strategies and development The Board Assurance Framework is a document in which the Trust Board sets out what it considers to be the most significant risks it sees in meeting its 2013/14 objectives. Annual workshops are arranged for the Board to review the framework by the Trust’s Internal Auditors. The Trust has identified a range of potential risks to achieving its strategic goals, across clinical, non-clinical and financial sectors. The risks have been identified from the Strengths, Weaknesses, Opportunities and Threats (SWOT) and other analyses and Service Delivery Unit risk logs and they have been mapped against the Assurance Framework, which the Board reviews at regular intervals. The Board have identified the following as its top risks to delivering its annual plan. These were identified at a Board Governance Assurance Framework workshop on 13 February 2013 and are as follows: • Lack of comprehensive patient and public feedback, • Local health and social care economy is not sustainable, • Serious failure in quality of care provided, • Inadequate IT systems including a lack of integrated electronic patient record, • Commissioning decisions and processes inhibit implementation of strategic plans, • Failure to identify and deliver cost improvement plans over a rolling 5-year period. Action plans are in place to manage these risks, which are subject to scrutiny by the relevant Board committee. The Trust has identified the following future risk(s): The directors’ policy for managing principal risks is to be disclosed Risk Mitigation Over the next 5 years the potential impact of cost improvement programmes (CIPs) on quality of services. Impact assessments undertaken on CIPs relating to the delivery of clinical services. Outcome In the period 1 April 201331 March 2014 there has been no adverse impact on the quality of clinical services. The Trust currently assesses and monitors risk by a variety of methods, not least via an assurance framework. This is the key document for the Trust Board to ensure all principal risks against strategic goals and associated corporate objectives are identified, managed, controlled and reported upon. The assurance framework is presented to, and discussed by, the Trust Board at each public meeting. The Risk Management processes are guided and provided for by the Risk Management Strategy. This sets out the organisation’s approach to risk and defines responsibilities and roles of the Chief Executive, Directors, senior managers and all other staff in relation to the effective delivery of the risk management agenda. It also highlights the links between Risk Management, the Assurance Framework and the business planning process. There is documented guidance for staff supported by comprehensive Policies and Procedures available via the Trust’s intranet. Whilst ultimate accountability rests with the Chief Executive, responsibility for risk management has been delegated to the executive leads for risk. The Director of Quality (Executive Nurse) and Medical Director have joint delegated responsibility for clinical risk management and clinical governance. The Director of Finance is responsible for financial risk management. The Company Secretary has delegated responsibility for managing the strategic development and implementation of corporate risk management and assurance, and is responsible for the development and maintenance of the Corporate Risk Register. The work of the Quality and Safety Committee is supported by a number of sub committees and working groups including the Clinical Risk Group. 98 Annual Report 2014-15 As part of the risk management strategy, training is delivered to managers and to other staff across the Trust, both at induction to the Trust and also as part of on-going development. Areas covered include: risk management, risk assessment, incident reporting, health and safety, infection control and the handling of complaints. The key elements of the Risk Management strategy focus on: • Individual and corporate responsibility, • A structured framework for the management of risk with a clear definition of the roles and responsibilities for directors, managers, clinicians and allied health professionals, • A purposeful approach to enabling the Trust to embed risk management within its structure and so support the Trust in meeting its new functions and objectives, • Compliance with all relevant statutory and non-statutory standards relating to the assessment and control of risk, • Identifying, and where possible eliminating, risk and controlling any remaining risk, • Monitoring the controls and procedures to ensure effective risk management within the Trust. Increasingly formal risk assessments are being undertaken locally. If advice and/or training is required on clinical risk assessment this will be provided by the Quality Governance Department. If advice and/or training is required on non-clinical/generic risk assessment this will be provided by the Risk and Security Manager and/or Health and Safety Manager. Risk assessment and incident reporting systems remain important to the on-going assessment of risk. Evaluation of any, or all, control measures are considered, not only by line management but also by the Quality Governance Department. This provides a robust double check within the system. All cost improvement plans are subject to a detailed quality and equality impact assessment involving the Director of Quality (Executive Nurse) and Medical Director and/ or their nominees. In respect of the publication of the report of the second Francis Inquiry into Mid Staffordshire NHS Foundation Trust the Trust Board is reviewing ward staffing levels. Implementation of the action plan relating to the Francis report and subsequent Berwick and Keogh reports is overseen by the Quality and Safety Committee. Information about significant relationships with stakeholders, which are likely, directly or indirectly, to influence the performance of the Trust Financial accounts The Trust has good working relationships with a wide range of partners ranging from local Clinical Commissioning Groups, Suppliers, Staff Side Representatives and employees to the Worcestershire County Council for the delivery of healthcare through the Section 75 pooled budgets. These strong and positive partnerships are a major strength helping the Trust to achieve its objectives. 99 4. Position of the business, including a description of the capital structure, treasury policies and objectives and liquidity of the entity both in the period under review and in the future. The events that have impacted on the financial position of the NHS body during the year, and factors that are likely to affect the financial position going forward The Trust commenced the financial year with a robust set of budgets and a 1% Contingency Reserve, which was created in order to help the Trust manage risks and cost pressures and unexpected service demands arising during the course of the year. The main cost pressures reported to the Finance and Performance Committee during 2013/14 were as follows: • Locum consultants • Continence Service • Bank and Agency costs • Increase in legal fees This is the Trust’s third Annual Report and this year’s surplus of £2.9m has been recorded on a turnover of £172m, which is 1.69% up from 1.48% last year and 0.8% in 2011/12. Looking forward the medium term financial position has a robust base with the Trust being able to confidently forecast a £2.5m (1.5%) surplus position for 2014/15, having created and maintained a Contingency Reserve (1%) for non-recurrent purposes. Accounting policies Standard NHS accounting policies have been adopted. The Trust has prepared its 2013/14 focusing on those draft Final Accounts in a form that complies with the International Financial Reporting which have required Standards (IFRS) and submitted them to the Department of Health and Auditors by the the particular exercise required date of 23 April 2014. of judgement and which have changed during the year Continuity of Service Risk Rating The Continuity of Service Risk Rating used by Monitor, the Economic Regulator of Foundation Trusts, focusses on the issues of liquidity and capital servicing. The Trust’s risk rating overall at the end of March 2014 was a satisfactory 4, out of maximum of 5, that is consistent with an aspirant Community Foundation Trust. Cash flow issues During the year the Trust took active measures to secure its working capital and cash which supplement liquidity. This initiative and move above the 10 days minimum operating cash required information provided by Monitor, resulted in an increase in cash for 2013/14 of £2.4m.This over-delivery is in the annual allowable by the Trust Development Authority and there is no adverse impact on the Trust’s accounts performance against its External Financial Limit (EFL). Carrying value versus market value of land The carrying value of the Trust’s land is £19.9m, which is based upon the District Valuation Office’s valuation as at 31 March 2014. 5. Policies adopted and the extent to which they have been successfully implemented regarding environmental, social and community issues:Sustainability report This is included on page 11 of this report under the heading ‘Sustainability report’. Emergency prepared- This is included on page 20 of this report under the heading ‘Emergency preparedness’. ness Complaints handling procedure and principles for remedy Better Payments Practice Code This is included on pages 40 and 41 of this report under the heading ‘Continue to Improve our Response Times and Learning from Complaints’. The Trust’s measure of compliance on the Better Payments Practice Code is shown on page 81 of this report. The Trust has for the second year running achieved full compliance on all 4 measures. 100 Annual Report 2014-15 Prompt Payments Code The Trust has applied to become a signatory to the Prompt Payments Code, and authorisation is awaited, pending receipt of references. The action taken to maintain or develop the provision of information to and consultation with the Trust’s employees The Trust has agreed over 80 Corporate policies and 35 Human Resource policies, which are all shown on the Trust’s website. While a majority of the policies are Health and Care Trust policies, some have been brought over from either Worcestershire Primary Care NHS Trust or Worcestershire Mental Health Partnership NHS Trust and will be replaced over the coming months by Trust Policies. Every week the Chief Executive issues an update to all staff to share the latest news regarding on-going developments. On a monthly basis a more detailed Team Brief is provided to Directors for dissemination to all staff. Health and safety The Trust employs two staff to provide competent and professional support, advice and guidance on all matters relating to health, safety and security: • Risk & Security Manager • Health & Safety Manager / Security Specialist Their role is to ensure the Trust complies with all health and safety legislation applicable to the Trust’s activities, its employees and non-employees; as well as compliance with NHS Protect Security Standards. The Polices on the Trust’s website are as follows: Health and Safety Display Screen Equipment First Aid Control of Substances Hazardous to Health Substance Misuse Stress Slip, Trip & Fall Medical Gases New & Expectant Mothers Young People at Work Safe Management of Contractors Safer Handling Latex Fire Safety Safe use of Mobile Phones Lone Working Personal Safety Security Lock Down Waste Management CCTV Water Hygiene, Air Conditioning & Legionella Asbestos Risk Assessment Policy in relation to disabled employees and on equal opportunities This is included on page 19 of this report under the heading ‘Equality and Diversity and Human Rights’. Information on policies and procedures relating to countering fraud and corruption The Trust’s Standards of Business Conduct and Anti-Bribery Policy were approved in December 2011 and a copy is available to staff on the Trust’s website. The Local Counter Fraud and Corruption Policy were added to the website after being approved in June 2012. The Trust also employs a full time local counter fraud specialist. The total days lost in 2013/14 were 32,631 (31,251 last year), which is 3,171 staff years (3,334 last year) with the average working days lost being 10 (9 last year). External audit disclosure The Trust’s auditor is Grant Thornton and the agreed statutory audit fees for 2013/14 were £69k (excluding VAT). In addition to these fees the Trust paid £10k (excluding VAT) for a review of the Trust’s Quality Account. The external auditors have issued an unqualified opinion on the Trust’s 2013/14 annual report and accounts. That opinion confirmed that the information given in the 2013/14 annual report is consistent with the financial statements. Other Auditor’s remu- Grant Thornton has, in addition to the statutory audit, also undertaken an Information neration Technology Strategy Review at a cost of £16k, which is within the limits allowed by the Audit Commission. Financial accounts 101 A statement that the entity has complied with HM Treasury’s guidance on setting charges for information is required. Serious untoward incidents Progress against agreed non-financial targets Social and community issues The Trust are fully compliant with HM Treasury’s guidance on setting charges for information in areas such as medical records and Freedom of Information requests. This is included on Page 61 of this report under the heading ‘Clinical coding error rate’ This is included on Page 19 of this report under the heading ‘The Trust’s performance against the 2013/14 key national targets’. Up until July 2013 the Trust had a Community Engagement Committee, which was a sub-committee of the Trust Board. The Community Engagement Team developed a Community Engagement Strategy, which has successfully taken forward the work of the sub-committee. Over the last twelve months engagement and consultation work has been focused according to impact, interest and investment. To this end, the Trust has conducted full consultations with patients, carers and representatives of interested groups, who would be impacted by proposed service changes. The comments received were collated, reported on and fed into the creation of new care pathways and, where necessary, has been shared with the Health Overview and Scrutiny Committee and Children and Young People Overview and Scrutiny Panel. The Trust has also worked with interested groups and individuals and has offered those who want to be involved in the work of the Trust, lots of different opportunities from attendance at forums and events, to taking part in working groups, to sharing their patient stories and taking part in films for staff training. The level of interest shown has allowed the Trust to set up a Quality Account Working group, an Organisational Values Working group and led to regular and increased attendance at forum meetings. Social and community issues One off quality events have considered such matters as the Francis Report, the Sub-Acute pathway and the Complaints process. The Trust has also sought to reach out to more patients and carers and in addition has sought the views and opinions of staff, through the Clever Together digital campaign. As a result of a survey of the Trust’s members over 200 more members indicated they were keen to get involved by attending forums, sitting on interview panels and taking part in patient led assessments of the clinical environment. The Trust has maintained its links with a variety of other groups and organisations. In total the Trust has engaged with 50 groups, non-statutory and statutory organisations during the last year. 2013/14 saw the creation of a new Partnership Forum and a Youth Board whilst continuing to reach other ‘seldom heard groups’ such as the travelling community. Persons with whom the The Trust works with a wide range of partners, from contracted and trade Suppliers, to entity has contractual those who jointly deliver services with us e.g. Worcestershire Clinical Commissioning or other arrangements Groups and Worcestershire County Council (for pooled budget arrangements and the which are essential to the Joint Commissioning Unit). The Trust is performance managed by the Trust Development business of the entity Authority. The entity’s employees: Category of Trust Employees Sum of WTE Sum of Headcount including an account of Directors 7.00 15 the entity’s equal opFemale 3.00 4 portunities policy. Also Male 4.00 11 required is an analysis Employees 3,158.06 4,098 of the gender distribuFemale 2,693.16 3,533 tion in the categories: Male 464.90 565 • directors Senior Management Team 17.60 18 • other senior managers Female 4.60 5 • employees Male 13.00 13 Grand Total 3,182.66 4,131 102 Annual Report 2014-15 Annual Governance Statement Annual Governance Statement covering the period 1 April 2013 – 31 March 2014 Scope of responsibility As Accountable Officer, and Chief Executive of this Board, I have responsibility for maintaining a sound system of internal control that supports the achievement of the organisation’s objectives. I also have responsibility for safeguarding the public funds and the organisation’s assets for which I am personally responsible as set out in the Accountable Officer Memorandum. Throughout the year the Trust has submitted monthly compliance monitoring and board statements selfcertification returns to the NHS Trust Development Authority (TDA). These inform the TDA about the Trust’s performance across the three domains of quality and governance, finance and delivering sustainability. The March 2014 compliance monitoring submission states that the Trust is not compliant against the standard relating to the appointment of Governors, which will happen later in the foundation trust application process. It also highlights the areas where action plans need time to bed in to resolve issues including those raised by the CQC visit to HMP Oakwood in June 2013 and the more recent performance issue that has been encountered regarding the CPA 12 monthly reviews. In both cases I am confident that the action taken has resolved these matters. Financial accounts As an employer with staff entitled to membership of the NHS Pension Scheme I confirm that control measures are in place to ensure all employer obligations contained within the Scheme regulations are complied with. This includes ensuring that deductions from salary, employer’s contributions and payments in to the Scheme are in accordance with the Scheme rules, and that member Pension Scheme records are accurately updated in accordance with the timescales detailed in the Regulations. The governance framework of the organisation The following framework of Board Committees provides, and comments upon, assurances to the Board and enables the Board to direct me to address areas requiring attention: • Audit Committee • Quality and Safety Committee • Finance and Performance Committee • Community Engagement Committee (up to July 2013) • Charitable Funds Committee • Remuneration Committee The Board has also established a Foundation Trust Programme Board to oversee the Trust’s application for NHS Foundation Trust status and a Partnership Forum is being developed to facilitate joint working and sharing of information across partner organisations.This forum is not a Board committee. 103 Jan Ditheridge n 1 1 1 1 8 8 8 6 4 1y 5 6 5 1 Extraordinary Trust Board 1 1 1 Informal Board Days/Sessions 8 7 8 1 8 Audit Committee 6 1y 1 Quality & Safety Committee 12 5n 12 2n Finance & Performance Committee 12 9n 1 9 Charitable Funds Committee 4 Community Engagement Committee 2 1n Remuneration Committee 6 6 FT Programme Board 9 7 11 3 6 6 6 1 1 1 7 7 7 3 5 10 10 Sue Harris Bill Creaney s 1 6 Robert Mackie Sarah Dugan 3 6 Sandra Brennan David Priestnall 5 Trust Board Meeting Stephen Collman v Martin Connor 6 Colin Phillips u 6 Peter Lachecki 6 Chris Burdon 5 Number held Jill Gramann Attendance by Board members at Trust Board and Board Committee Meetings 1 April 2013 to 31 March 2014 8 8 6 2 9 6 11 7 2 6 4 2 5 1 2 2 4 6 8 1 1 2 1 1 2 n Attended in observer capacity y Attended to cover absence of a member u Indisposed with effect from 10/05/2013 and stepped down on 31/03/2014 s Indisposed for a period during 2013/14 with phased return and reduced attendance at meetings n v In post until 22 September 2013 In post in acting capacity from 23 September 2013 and substantively from 3 March 2014 104 Annual Report 2014-15 Executive Director – voting rights a a a Executive Director – non-voting M Individual’s Appraisal undertaken by Trust Development Authority a M M F M M F a a a a a a Individuals’ Appraisals undertaken by Chief Executive Board and Board Committee Effectiveness Each Board member has a set of objectives that are agreed with their respective appraiser against which performance is measured and which are subject to formal appraisal at least annually. In terms of individuals’ performance on the Board, proformas are completed by each Board member on an anonymised basis. These invite Board members to comment on the contribution they make to the Board and provide an overview of how the Board as a whole is performing. This also informs areas for development. During 2013/14 the Chairman and Chief Executive have both been subject to 3600 appraisal as part of their respective personal development. Annually Board committee members (other than Audit Financial accounts a a a a Gender Individuals’ Appraisals undertaken by Chairman Sue Harris voting wef 12/09/2013 a Robert Mackie a Sandra Brennan David Priestnall a Stephen Collman from 23/09/2013 Martin Connor a Jan Ditheridge to 22/09/2013 Jill Gramann a Bill Creaney Colin Phillips a Sarah Dugan (Chief Executive) Peter Lachecki Non-Executive Director – voting rights Chris Burdon (Chairman) Balance, Completeness and Appropriateness of the Board membership 1 April 2013 to 31 March 2014 a M F M F M F a a a a a a Committee) are asked to complete a proforma selfassessment checklist designed to elicit comment on the effectiveness of the committee. The checklist is derived from the proforma checklist for audit committees published in the NHS Audit Committee Handbook. The Audit Committee completes the latter checklist. The five NEDs are determined by the Board to be independent on the basis that none: • has been an employee of the trust within the last five years; • has, or has had, within the last three years, a material business relationship with the trust either directly, or as a partner, shareholder, director or senior employee of a body that has such a relationship with the trust; • has received or receives additional remuneration from 105 the trust apart from a director’s fee, or is a member of the trust’s pension scheme; • has close family ties with any of the trust’s advisers, directors or senior employees; • holds cross-directorships or has significant links with other directors through involvement in other companies or bodies; • has served on the board of the trust for more than nine years from the date of their first appointment. Non-Executive Director membership of Board committees has subsequently been reviewed and changes implemented on 1 April 2014. In accordance with the Board’s succession plan 2 Non-Executive Directors (Designate) were appointed in November 2013. One of these, Rick Roberts, has been appointed to the vacancy created by Mr Phillips’ departure. Mr Roberts has a clinical background. In 2013/14 he has attended 3 Trust Board meetings, 1 Informal Board Day/Session, 4 Quality & Safety Committee meetings and has attended 1 Finance & Performance Committee meeting as an observer. The other Non-Executive Director (Designate), Steve Peak has attended 3 Trust Board meetings, 1 Informal Board Day/Session and 2 Finance & Performance Committee meetings in this period. At each formal Board meeting Board members are asked to declare any conflict of interest. There have been no departures from the requirements of the Standards of Business Conduct and Anti-Bribery policy and the overarching corporate governance framework. The Board of the Trust provides its leadership and is charged with securing the organisation’s long term success. The Board is collectively responsible for controlling the Trust. The Board sets strategic direction and supervises the work of the executive to ensure that corporate objectives and performance targets are achieved. The Board makes those decisions reserved unto itself, defines and sets the approach to risk and risk management and conducts itself in such a way that it takes the view of key stakeholders into account. The Trust has continued to review and update self-assessments against Monitor’s quality governance assurance framework and the Department of Health’s and Monitor’s board governance assurance framework. 106 The quality and safety of patient services has been maintained overall and where specific shortcomings have been identified such as at HMP Oakwood (see page 34) these have been addressed. There has been no loss of control of the Trust’s finances. Performance levels have been maintained against the key indicators contained within the NHS performance framework, the Monitor compliance targets, indicators and thresholds for 2013/14 and the mental health performance framework. Chairs of Board Committees present reports to the Board on the matters considered by their respective Committees. In the case of the Audit Committee the report informs the Board of the level of assurance that has been given by Internal Audit on the reviews that they have been commissioned to undertake in 2013/14. 23 reviews were undertaken during the year. 15 were given significant assurance, 4 were given moderate assurance and 4 were not assurance based reviews. The Audit Committee report also informs the Board of the programme of work that is undertaken by External Audit. This provided assurance that their initial testing of systems combined with a review of work undertaken by Internal Audit had not highlighted any significant system weaknesses or breakdowns in control. The Trust’s Local Counter Fraud Specialist attends the Audit Committee meetings as does the Trust’s Local Security Management Specialist. During 2013/14 the committee extended its remit to include oversight of the procurement function. At their meeting on 12 March 2014 the Trust Board agreed a proposal from the Audit Committee to establish a sub-committee to oversee data quality improvement with effect from 1 April 2014. Annual Report 2014-15 Summary of Quality Governance arrangements An integrated performance report provides Trust Board with assurance that the quality of services being delivered is being carefully monitored and that improvement measures are being implemented where required. Oversight of the quality governance arrangements rests with the Quality & Safety Committee. This Board committee is chaired by a Non-Executive Director and meets monthly. The Trust has a Quality Governance Strategy structured around the three domains of patient safety, clinical effectiveness and patient experience. It sets the direction for ensuring that people who use our services experience the highest quality, safest and most effective care. The strategy supports the delivery of nine, high level cross-organisational Quality Goals. The Goals each have sub-indicators to track progress towards achievement. Performance is reviewed at each Quality and Safety Committee and every meeting of the Board. Recovery plans are implemented for those goals that are not achieving their target performance. The quality governance framework supports the Quality and Safety Committee and promotes granulation of the reports and associated outcomes. Each Service Delivery Unit has a Quality Governance meeting to review their own performance and to facilitate shared learning. Unit Quality Leads provide narrative data to facilitate a broader understanding of context and risk. The best judges of the quality of care are the people who use our services and our staff. We undertake staff ‘Pulse surveys’ quarterly and have recently launched the staff Family and Friends test to gauge whether staff consider the services we provide are of a high quality. Regular communications are sent out to staff from the Chief Executive, with a clear email address and other routes for staff to directly contact the executive team. Our programme of patient experience work, patient safety walkabouts, patient and staff stories to board, together with analysis of complaints and compliments provides rich information about where we are getting it right, and where improvements are needed. Arrangements for assurance on the content and publication of the Quality Account The Trust Quality Account Working Group is responsible for producing the Quality Account, ensuring that the document complies with the Department of Health requirements, and that the information contained in the Account is balanced and accurate. All Cost Improvement Programmes or new service developments undergo a Quality and Equality Impact Assessment, signed off by the Director of Quality (Executive Nurse) and the Medical Director, and have measurements identified to monitor longer term effects on the quality of services. The draft Quality Account is reviewed by the local Health and Overview Scrutiny Committee, commissioners and the Quality and Safety Committee before it is signed off by Board and placed on the NHS Choices website. The Account is subject to external audit regarding the quality of the data included in the Account. This independent assurance confirmed that the 2012/13 Quality Account complied with national mandatory requirements and will apply to the 2013/14 Quality Account. Service Line Reporting has been developed for nine quality metrics. This provides summary quality performance data for each team and service in the Trust. This is reviewed by the teams themselves and at the Quality and Safety Committee to identify early warning signs or trends over time and allows for benchmarking between similar teams in the Trust. The Service Delivery The Trust Board approved the 2012/13 Quality Account in May 2013, including the adoption of the quality priorities for 2013/14 which were: • Improved use of patient, carer and staff feedback, including the Family and Friends test, • Improvement in the capture of real time feedback from patients, Financial accounts 107 • Continue to improve our response times and learning from complaints, • Improve evidence that we learn from patient safety incidents and near misses, • Continue the work to reduce avoidable pressure ulcers. Progress with each of the priorities is monitored through the Quality and Safety Committee. Arrangements for assurance on clinical audit, never events and serious incidents Clinical Audit There is a 3 year rolling audit programme in the Trust which is overseen by the Clinical Audit and Effectiveness Group. This group, which is chaired by the Deputy Medical Director, has good clinical representation, and reports through to the Quality and Safety Committee and Board both in terms of performance against the plan and clinical outcomes as a result of the audits. The Trust takes part in all national clinical audits that are relevant to the Trust and subscribes to the Prescribing Observatory for Mental Health audit programme. Further narrative regarding the clinical audit programme and the outcomes of audits is presented in the Quality Account. Never Events and Serious Incidents The Trust continues to support staff in the process of identifying, reporting and managing incidents. The Medical Director and Director of Quality (Executive Nurse) jointly lead the Serious Incident Forum. Each serious incident has a Root Cause Analysis undertaken by a trained Investigating Officer. A roundtable is held for each Serious Incident and action plans are overseen by the aforementioned Forum. Extensive, detailed reports on serious incidents are presented to clinical services, operational Quality Governance groups, Quality and Safety Committee and Board. Robust, sustainable systems are in place to maintain performance on serious incident closure times. Comprehensive information regarding incidents and Serious Incidents is included in the Trust Quality Account. 108 The risk of occurrence of Never Events is tracked through the incident reporting system and clinical audit. The Trust has had no incidents of Never Events reported to date. The Quality Forum which reports to the Quality & Safety Committee brings together the Quality Leads and the Quality and Safety Team to check for cross-organisational learning, and to identify trends from investigations. External Review of the quality of services provided During 2013/14 inspections of Trust services have been undertaken on: • 13 occasions by local Clinical Commissioning Groups • 1 occasion by the NHS Trust Development Authority • 2 occasions by Her Majesty’s Inspectorate of Prisons (HMIP) and the Care Quality Commission (CQC) • 1 occasion by an external consultancy commissioned by the Trust to review its self-assessment against Monitor’s quality governance assurance framework • 1 occasion by the Lead Nurse NHS Midlands and East • 2 occasions by South Staffordshire Area Team • 4 occasions by the CQC in relation to the Trust’s compliance with the Mental Health Act and essential standards of quality and safety • 1 occasion by the Joint Commissioning Unit, Worcestershire County Council Overall the CCGs’ inspection visits were positive. Each identified area for development has been incorporated into action plans. The Trust Development Authority’s inspection observed very positive practice and identified a number of areas for further consideration including continuing to promote Board visibility with staff and communicating the IT strategy to staff. The joint HMIP and CQC inspection of HMP Oakwood undertaken in June 2013 resulted in the issuing of a warning notice in relation to medicines management. Following representations from the Trust to the CQC the Trust was given until 30 September 2013 to implement an action plan to address the shortcomings identified. Annual Report 2014-15 This deadline was achieved. Subsequently the CQC revisited the prison on 7 & 8 October 2013 and reduced the warning notice to two minor compliance issues. The external consultancy’s review of the Trust’s selfassessment against Monitor’s Quality Governance Framework provided positive feedback about quality governance systems and suggested a number of areas for development including checking that communications were getting through to all areas and increasing the number of posters outlining the vision and values of the Trust. Commenting on her visit to the recently opened New Haven the Lead Nurse, NHS Midlands and East said she could only recall one or two units that matched this facility for team approach and physical environment. The South Staffordshire Area Team visited in their capacity as commissioners for offender health services. They visited the healthcare facilities at HMPs Long Lartin and Oakwood. Overall their feedback was positive. Areas for development have been incorporated into action plans. As well as assessing the Trust’s compliance with the Mental Health Act when visiting mental health facilities in the Trust the CQC inspectors also assured themselves that essential standards of quality and safety were being maintained. No concerns were identified and their feedback was very positive. The Joint Commissioning Unit visited a unit where a whistleblower had raised concerns with the CQC about the management of the unit. The purpose of their visit was to assure themselves that the remedial action plan was being implemented. The CQC’s Quality and Risk Profiles (QRP) are reviewed to take account of, and to address, any newly identified risks. There were no significant risks to report to the Board from the QRPs published during 2013/14. Financial accounts Community Engagement Over the last twelve months engagement and consultation work has been focused according to impact, interest and investment. To this end, the Trust has conducted full consultations with patients, carers and representatives of interested groups, who would be impacted by proposed service changes. The comments received were collated, reported on and fed into the creation of new care pathways and, where necessary, has been shared with the Health Overview and Scrutiny Committee and Children and Young People Overview and Scrutiny Panel. The Trust has also worked with interested groups and individuals and has offered those who want to be involved in the work of the Trust, lots of different opportunities from attendance at forums and events, to taking part in working groups, to sharing their patient stories and taking part in films for staff training. The level of interest shown has allowed the Trust to set up a Quality Account Working group, an Organisational Values Working group and led to regular and increased attendance at forum meetings. One off quality events have considered such matters as the Francis Report, the Sub-Acute pathway and the Complaints process. The Trust has also sought to reach out to more patients and carers and in addition has sought the views and opinions of staff, through the Clever Together digital campaign. As a result of a survey of the Trust’s members over 200 more members indicated they were keen to get involved by attending forums, sitting on interview panels and taking part in patient led assessments of the clinical environment. The Trust has maintained its links with a variety of other groups and organisations. In total the Trust has engaged with 50 groups, non-statutory and statutory organisations during the last year. 2013/14 saw the creation of a new Partnership Forum and a Youth Board whilst continuing to reach other ‘seldom heard groups’ such as the travelling community. 109 Risk assessment The Trust currently assesses and monitors risk by a variety of methods, not least via an assurance framework. This is the key document for the Trust Board to ensure all principal risks against strategic goals and associated corporate objectives are identified, managed, controlled and reported upon. The assurance framework is presented to, and discussed by, the Trust Board at each public meeting. The Risk Management processes are guided and provided for by the Risk Management Strategy. This sets out the organisation’s approach to risk and defines responsibilities and roles of the Chief Executive, Directors, senior managers and all other staff in relation to the effective delivery of the risk management agenda. It also highlights the links between Risk Management, the Assurance Framework and the business planning process. There is documented guidance for staff supported by comprehensive Policies and Procedures available via the Trust’s intranet. Whilst ultimate accountability rests with the Chief Executive, responsibility for risk management has been delegated to the executive leads for risk. The Director of Quality (Executive Nurse) and Medical Director have joint delegated responsibility for clinical risk management and clinical governance. The Director of Finance is responsible for financial risk management. The Company Secretary has delegated responsibility for managing the strategic development and implementation of corporate risk management and assurance, and is responsible for the development and maintenance of the Corporate Risk Register. The work of the Quality and Safety Committee is supported by a number of sub committees and working groups including the Clinical Risk Group. As part of the risk management strategy, training is delivered to managers and to other staff across the Trust, both at induction to the Trust and also as part of on-going development. Areas covered include: risk management, risk assessment, incident reporting, health and safety, infection control and the handling of complaints. The extent and level of training is dependent on a member of staff’s delegated responsibility. 110 Risk Management training in general can be evidenced in the Induction Programme, various ad-hoc incident reporting training sessions, risk refresher training and written guidance disseminated to all Clinical and Service leads. The legislative requirements of risk management and risk assessment within a safe system of work are actively promoted by the Trust. A new on line incident reporting system was implemented on 1 August 2013. The Trust utilises the incidents, PALS & Complaints, Risk and Litigation modules on the system. The Incident Reporting Module has an e-mail trigger facility, which alerts responsible managers to recent incidents. A trigger is also sent to key governance staff such as the Patient Safety Manager, Risk and Security Manager and Quality Leads for each Service Delivery Unit, who review recently submitted incidents and forward guidance on the information which is needed to complete the incident report to the responsible manager. The software contains data entry forms, which are used to record details of investigations, recommendations, actions and lessons learned. Monthly incident data reports are provided to the responsible managers and monthly reports are provided to the Quality and Safety Committee. These give all relevant details about the incidents and managers provide further contextual information to the Quality and Safety Committee to facilitate the organisational learning from incidents. Trend analysis reports are being developed to further inform managers and senior managers about any developing incident trends across the Service Delivery Units and the wider Trust. The need to engage each and every staff member and to provide the appropriate level of training to them remains a key objective and priority within the Trust. There are systems in place for staff to raise concerns/risks/near misses to allow action to be taken and for lessons to be learnt. Annual Report 2014-15 The risk and control framework Risk Management Strategy The key elements of the Risk Management strategy focus on: • Individual and corporate responsibility. • A structured framework for the management of risk with a clear definition of the roles and responsibilities for directors, managers, clinicians and allied health professionals. • A purposeful approach to enabling the Trust to embed risk management within its structure and so support the Trust in meeting its new functions and objectives. • Compliance with all relevant statutory and nonstatutory standards relating to the assessment and control of risk. • Identifying, and where possible eliminating, risk and controlling any remaining risk. • Monitoring the controls and procedures to ensure effective risk management within the Trust. Increasingly formal risk assessments are being undertaken locally. If advice and/or training is required on clinical risk assessment this will be provided by the Quality Governance Department. If advice and/ or training is required on non-clinical/generic risk assessment this will be provided by the Risk and Security Manager and/or Health and Safety Manager. Financial accounts Risk assessment and incident reporting systems remain key to the on-going assessment of risk. Evaluation of any, or all, control measures are considered, not only by line management but also by the Quality Governance Department. This provides a robust double check within the system. All cost improvement plans are subject to a detailed quality and equality impact assessment involving the Director of Quality (Executive Nurse) and Medical Director and/or their nominees. In respect of the publication of the report of the second Francis Inquiry into Mid Staffordshire NHS Foundation Trust the Trust Board is reviewing ward staffing levels. Implementation of the action plan relating to the Francis report and subsequent Berwick and Keogh reports is overseen by the Quality and Safety Committee. The Trust has inherited accreditation at level 1 of the NHS Litigation Authority (NHSLA) Clinical Negligence Scheme for Trusts (CNST) from its predecessor organisations. This entitles the Trust to a 10% discount on its premium for CNST and the Risk Pooling Scheme for Trusts (RPST). At level 1 assessors look for assurance that an organisation can demonstrate the process for managing risks has been described in approved documentation. Further information is awaited from the NHSLA regarding their intention to move away from assessing against the risk management standards from 2014/15. Risk management continues to be promoted and embedded throughout the Trust. 111 Major Risks 2013/14 The Trust has identified the following in year risks: Risk Mitigation Outcome Challenges in the local health economy such as the acute services review and changing and emerging commissioning arrangements. Active engagement in the acute services review. Focused attention on developing and maintaining relationships with commissioning organisations. Trust positioned to play a leading role in the future delivery of services as determined by the acute services review, e.g. Well Connected Programme. Contracts with commissioners have been signed off for 2014/15. Identification and delivery of a rolling 30 month programme of cost improvements. Focused attention to identify, on a prospective basis, opportunities to increase efficiency and cost effectiveness of delivery of services. A programme management office structure is in place with robust project management applied to each CIP scheme. Increased confidence about deliverability of recurrent CIPs. Achieving a reduction in the number of inherited patient administration systems (PAS). Option identified for rationalising the existing number of systems and timescale for doing so. The Trust has procured a single PAS but issues with the functionality and roll out of the system are being taken up with the contractor. Action plans are in place to manage the aforementioned risks. These are subject to scrutiny by the relevant Board committee. The Trust has identified the following future risk(s): Risk Mitigation Over the next 5 years the Impact assessments undertaken on CIPs potential impact of cost relating to the delivery of clinical services. improvement programmes (CIPs) on quality of services. 112 Outcome In the period 1 April 2013 – 31 March 2014 there has been no adverse impact on the quality of clinical services. Annual Report 2014-15 Risks to Data Security and Organisational Changes Data Security The Trust recognises the importance of the confidentiality of, and the security arrangements in place to safeguard, personal information about patients, staff, other persons and commercially sensitive information. Under the Data Protection Act 1998, the Trust is registered with the Information Commissioner’s Office for the purpose of processing personal information, Reference Number Z2745227. Information risk is managed and controlled by: • The Director of Finance is the Senior Information Risk Owner (SIRO) and takes overall ownership of the Trust’s Information Risk Management Programme. The SIRO undertakes annual training • The Medical Director is the Caldicott Guardian • All Information assets have been identified on the Trust’s information asset register, Information Asset Owners have been identified and information risk assessments have been undertaken or are planned • The information asset register is regularly reviewed by the SIRO • Defined authorised access to specific information systems as documented in specific System Level Security Policies • A robust Information Governance Management Framework is in place including: o the terms of reference for the Information Governance Steering Group and, o key IG policies such as, Information Governance, Safe Haven, Confidentiality, Data Protection, Information Risk, Records Management, Freedom of Information and IG Incident Reporting • The Information Governance Steering Group is chaired by the Company Secretary and the SIRO and Caldicott Guardian (Medical Director) are both members. All three are Board Members Financial accounts • Annual completion and submission of the latest version of the NHS Information Governance Toolkit (currently version 11) was to a ‘satisfactory’ minimum Level 2 performance score • The IG Toolkit return is subject to internal audit annually. ‘Significant’ assurance was given by internal audit for version 11 • Confidentiality Agreement for Contractors including authorised access for contractors who need or are required to access information systems • Mandatory annual IG training for all staff • Trust induction including information governance awareness raising and training • All IG related incidents are reported on the Trust’s incident reporting system and an automated email is sent to the Information Governance Team for investigation • All IG Serious Incidents Requiring Investigation (SIRIs) Level 2 (Reportable) are recorded on the IG Incident Reporting Tool, on STEIS and are published on the Trust’s website and in the Trust’s Annual Report • A Service level agreement is in place with Worcestershire Health ICT Services (WHICTS) which requires compliance with the relevant standards in the latest version of the DH Information Governance Toolkit • WHICTS provided network, policy and access control including: Network Security, Anti- Virus, Business Continuity and Disaster Recovery, Information Security, Internet and Email, Access Control and Mobile Device Encryption • The terms of reference of the Worcestershire Countywide Information Governance Steering Group whose members are drawn from: Worcestershire Acute Hospitals NHS Trust, Worcestershire Health and Care NHS Trust, 3 x NHS Clinical Commissioning Groups and Arden Commissioning Support Service. There has been one IG Serious Incident Requiring Investigation (SIRI) Level 2 (Reportable) in the period 1 April 2013 – 31 March 2014 which is outlined under the significant issues section on the final page of this document. 113 Significant Issue(s) Summary Of Serious Incident Requiring Investigations Involving Personal Data As Reported To The Information Commissioner’s Office In 2013-14 Number of data subjects affected Date of Incident Nature of Incident Nature of Data Involved August 2013 Loss of paperwork – a ward handover sheet was found at a railway station and was handed into the local press Name, age, GP name, diagnosis, past medical history, mobility, 18 nursing interventions required, discharge information Notification Steps Individuals contacted and offered support. Press statement released, full investigation undertaken Internal processes have been reviewed, improved and updated Further action on information risk The Trust will continue to monitor and assess its information risks, in light of the events noted above, in order to identify and address any weaknesses and ensure continuous improvement of our policies and procedures Accountable Officer : Sarah Dugan, Chief Executive Organisation: Worcestershire Health and Care NHS Trust Signature: Date: 31 March 2014 114 Annual Report 2014-15 Remuneration Report Details of the membership of the Remuneration Committee The Remuneration Committee of the Trust is a sub-committee of the Trust Board, which determines the remunerations, allowances and terms of service of the Chief Executive and those Executive Directors reporting directly to the Chief Executive. The membership of the Committee will comprise of the Chairman of the Trust and two Non-Executive Directors. The Committee shall undertake the following duties: a) To agree appropriate remuneration and terms of service for the Chief Executive and other executive directors including: • all aspects of salary (including any performance-related elements/bonuses), • provisions for other benefits, including pensions, • arrangements for terminations of employment and other contractual terms for all Trust employees. b) To monitor and evaluate the performance of individual Executive Directors c) To advise on, and oversee, appropriate contractual arrangements for Executive Directors, including the proper calculation and scrutiny of termination payments taking account of such national guidance as is appropriate. For 2013/14 the pay of the Directors and Senior Managers was increased by 1% from April 2013 in line with NHS National Pay inflation. The Trust Remuneration Committee approved a further pay increase for the Directors and Trust Chief Executive from 1 October 2013 following a benchmarking exercise with similar NHS Trust’s. Pay Multiples The remuneration and pension entitlements of Senior Managers are included in the tables on pages 119, 120a and 120b of this report along with the pay multiples section below. Reporting bodies, including the Trust are required to disclose the relationship between the remuneration of the highest paid Director in the Trust and the median remuneration of the organisation’s workforce. The banded remuneration of the highest paid Director in the Trust in 2013/14 was £145k – £150k (£145k – £150k in 2012/13). This was 5.5 (5.5 in 2012/13) times the median remuneration of the workforce which was £27k (£26k in 2012/13). In 2013/14 two Doctors received remuneration in excess of the highest paid Director at £166k and £162k respectively (in 2012/13 the two Doctors received sums of £165k and £153k). Total remuneration includes salary, non-consolidated performance related pay, benefits in kind as well as severance payments. It does not include employer pension contributions and the cash equivalent transfer value of pensions. Financial accounts 115 The policy on the remuneration of senior managers for current and future financial years Reporting related to the Review of Tax arrangements of Public Sector Appointees This is decided by the Remuneration Committee and for 2013/14 the agreement was in line with the national guidance. The Trust has reviewed in detail the extent to which it complies with the new Annual Report disclosure requirement in this area and considers that whilst the Trust doesn’t have any arrangements to declare for 2013/14 there are some clinician commitments associated with service level agreements that are under review and may transfer to the payroll of neighbouring NHS Trusts/Foundation Trusts. Negotiations are now underway, although the process may take some time to regularise in the manner required by Her Majesty’s Treasury. The two Disclosure tables required are shown below. Off-payroll engagements Table 1: For all off-payroll engagements as of 31 March 2014, for more than £220 per day and that last longer than six months: Number Number of existing engagements as of 31 March 2014 53 Of which, the number that have existed: for less than one year at the time of reporting 7 for between one and two years at the time of reporting 3 for between 2 and 3 years at the time of reporting None for between 3 and 4 years at the time of reporting 3 for 4 or more years at the time of reporting 36 are employed by another Trust & 4 by a Foundation Trust At this stage the Trust is not able to provide confirmation that all existing off-payroll engagements have at some point been subject to a risk based assessment as to whether assurance is required that the individual is paying the right amount of tax and, where necessary, that assurance has been sought. The majority of commitments the Trust has are ones that have been inherited and are currently under review. 116 Annual Report 2014-15 Off-payroll engagements Table 2: For all new off-payroll engagements between 1 April 2013 and 31 March 2014, for more than £220 per day and that last longer than six months: Number Number of new engagements, or those that reached six 7 months in duration, between 1 April 2013 and 31 March 2014 Number of new engagements which include contractual As above clauses giving the Trust the right to request assurance in relation to income tax and National Insurance obligations Number for whom assurance has been requested 6 as 1 is covered by the Construction Industry Scheme. Of which: assurance has been received 3 and 4 have been requested assurance has not been received 4, but these have been requested engagements terminated as a result of assurance not None being received None Number of off-payroll engagements of board members, and/or senior officers with significant financial responsibility, during the year Number of individuals that have been deemed “board 16 members, and/or senior officers with significant financial responsibility” during the financial year. This figure includes both off-payroll and on-payroll engagements. The methods used to assess whether performance conditions were met and why those methods were chosen. If relevant, why the methods involved comparison with outside organisations The objectives of the Directors are set in line with the Trust’s statement of overall objectives. The relative importance of the relevant proportions of remuneration which are, and which are not, subject to performance conditions The Remuneration Committee uses baseline Director salaries, which are then benchmarked against similar NHS Trusts across the West Midlands. A summary and explanation of policy on duration of contracts, and notice periods and termination payments The policy on contracts is that they are all substantive and the contract follows the national template. The majority of Director contracts include three months’ notice period from the individual and six months from the Trust. Any termination payments are contractual, in line with national guidance and the Trust Development Authority process. Financial accounts The overall corporate objectives are monitored and disclosed to the Board on a regular basis as well as there being an individual assessment by the Chief Executive with each Director. This is in line with NHS practice. 117 Details of the service In 2013/14, 14 staff (5 last year) left the Trust under the NHS Redundancy Scheme. The contract for each senior payments involved the sum of £428k (£151k last year). The staff leaving during the year manager who has included no (1 last year) senior managers at level 8a and above. served during the year: • date of the contract, the unexpired term, and details of the notice period; • provision for compensation for early termination; and • other details sufficient to determine the entity’s liability in the event of early termination. Pension Scheme and liabilities of the Trust NHS Creditors include £1.7m pension costs at 31 March 2014 (£1.6m at 31 March 2013). The accounting policy for Pensions and outline of the scheme is set out on page 23 of the Trust’s Annual Accounts. Explanation of any None were made in 2013/14. significant awards made to past senior managers 118 Annual Report 2014-15 Board of Directors Salaries and Allowances for Annual Report and Accounts 2013/14 Expense payments (taxable) total to nearest £100 Performance pay and bonuses (bands of £5,000) Long term performance pay and bonuses (bands of £5,000) All pension-related benefits (bands of £2,500) TOTAL (bands of £5,000) Salary (bands of £5,000) Expense payments (taxable) total to nearest £100 Performance pay and bonuses (bands of £5,000) Long term performance pay and bonuses (bands of £5,000) All pension-related benefits (bands of £2,500) TOTAL (bands of £5,000) 2012/13 Salary (bands of £5,000) Date Left Date Started Name and Title 2013/14 £’000’s £’00’s £’000’s £’000’s £’000’s £’000’s £’000’s £’00’s £’000’s £’000’s £’000’s £’000’s Chris Burdon, Chairman 20 - 25 Nil Nil Nil N/A 20 - 25 20 - 25 Nil Nil Nil N/A 20 - 25 Jill Gramann, Non-executive Director 5 - 10 Nil Nil Nil N/A 5 - 10 5 - 10 Nil Nil Nil N/A 5 - 10 Martin Connor, Nonexecutive Director 5 - 10 Nil Nil Nil N/A 5 - 10 5 - 10 Nil Nil Nil N/A 5 - 10 Peter Lachecki, Non-executive Director 5 - 10 Nil Nil Nil N/A 5 - 10 5 - 10 Nil Nil Nil N/A 5 - 10 David Priestnal, Non-executive Director 5 - 10 Nil Nil Nil N/A 5 - 10 5 - 10 Nil Nil Nil N/A 5 - 10 Colin Phillips, Non-executive Director 5 - 10 Nil Nil Nil N/A 5 - 10 5 - 10 Nil Nil Nil N/A 5 - 10 Sarah Dugan, Chief Executive 135 140 4 Nil Nil 60 62.5 195 200 135 140 15 Nil Nil (17.5 20) 115 120 Dr William Creaney, Medical Director 115 120 Nil Nil Nil 17.5 20 135 140 115 120 Nil Nil Nil 20 22.5 135 140 Robert Mackie, Director of Finance 110 115 Nil Nil Nil 55 57.5 170 175 100 105 Nil Nil Nil 7.5 - 10 110 115 Janet Ditheridge, Director of Operations Sep13 45 - 50 Nil Nil Nil 30 32.5 75 - 80 95 100 Nil Nil Nil 2.5 - 5 100 105 Financial accounts 119 Board of Directors Salaries and Allowances For Annual Report and Accounts 2013/14 continued Stephen Collman, Director of Operations Expense payments (taxable) total to nearest £100 Performance pay and bonuses (bands of £5,000) Long term performance pay and bonuses (bands of £5,000) All pension-related benefits (bands of £2,500) TOTAL (bands of £5,000) Salary (bands of £5,000) Expense payments (taxable) total to nearest £100 Performance pay and bonuses (bands of £5,000) Long term performance pay and bonuses (bands of £5,000) All pension-related benefits (bands of £2,500) TOTAL (bands of £5,000) 2012/13 Salary (bands of £5,000) Date Left Date Started Name and Title 2013/14 £’000’s £’00’s £’000’s £’000’s £’000’s £’000’s £’000’s £’00’s £’000’s £’000’s £’000’s £’000’s Oct13 40 - 45 Nil Nil Nil 27.5 30 70 - 75 N/A N/A N/A N/A N/A N/A Sandra Brennan, Director of Quality 90 - 95 Nil Nil Nil 32.5 35 125 130 90 - 95 Nil Nil Nil (20 22.5) 65 - 70 Susan Harris, Director of Strategy and Business Development 90 - 95 Nil Nil Nil 20 22.5 110 115 75 - 80 Nil Nil Nil 17.5 20 90 - 95 Robert Hipwell, Board Secretary 80 - 85 Nil Nil Nil 12.5 15 95 100 80 - 85 Nil Nil Nil (25 27.5) 55 - 60 Notes: 1) The expense payment made to Sarah Dugan in both years relates to a leased vehicle used under the terms of the Trust’s lease car policy. 2) The format required for reporting senior managers’ remuneration within the NHS has changed for the financial year ending 31 March 2014 as prescribed by the Companies Act 2006 and The Large and Medium-sized Companies and Groups (Accounts and Reports) Regulations 2008 (SI 2008 No 410). 3) The new salaries and allowances table requires disclosure of the value of future pension benefits that have accrued to senior managers during the year, as well as additional disclosures relating to performance-related pay and bonuses and these are totalled together with senior managers’ salary and expense payments to provide a total value of salaries and allowances earned. Comparative figures for the year 2012-13 have been re-stated in this year’s revised table. 120 A Annual Report 2014-15 Total accrued pension at age 60 at 31 March 2014 (bands of £5,000) Lump sum at age 60 related to accrued pension at 31 March 2014 (bands of £5,000) Cash Equivalent Transfer Value at 1 April 2013 Cash Equivalent Transfer Value at 31 March 2014 Real increase in Cash Equivalent Transfer Value Employer’s contribution to stakeholder pension Date Left Real increase in pension lump sum at aged 60 (bands of £2,500) Real increase in pension at age 60 (bands of £2,500) Date Started Name and Title Pension Benefits £’000’s £’000’s £’000’s £’000’s £’000’s £’000’s £’000’s £’000’s Sarah Dugan, Chief Executive 2.5 - 5 10 - 12.5 45 - 50 140 - 145 727 825 83 0 Dr William Creaney, Medical Director 0 - 2.5 5 - 7.5 10 - 15 40 - 45 222 267 40 0 Robert Mackie, Director of Finance 2.5 - 5 7.5 - 10 20 - 25 70 - 75 313 376 57 0 Janet Ditheridge, Director of Operations Sep-13 0 - 2.5 2.5 - 5 30 - 35 100 - 105 557 628 29 0 Sandra Brennan, Director of Quality 0 - 2.5 5 - 7.5 35 - 40 105 - 110 619 860 228 0 Susan Harris, Director of Strategy and Business Development 20 - 22.5 Nil 20 - 25 Nil 11 208 197 0 Robert Hipwell, Board Secretary 0 - 2.5 2.5 - 5 40 - 45 125 - 130 901 974 54 0 Oct-13 0 - 2.5 2.5 - 5 20-25 60 - 65 247 302 25 0 Stephen Collman, Director of Operations Financial accounts 120 B Reporting of other compensation schemes - exit packages Exit package cost band (including any special payment element) Number of compulsory redundancies Number of other departures agreed Cost of compulsory redundancies Total Cost of other number departures of exit agreed packages Number of departures where special payments have been made Total cost of exit packages Cost of special payment element included in exit packages Number £s Number £s Number £s Number £s Less than £10,000 3 18,971 0 0 3 18,971 0 0 £10,000£25,000 5 93,747 0 0 5 93,747 0 0 £25,001£50,000 3 81,675 0 0 3 81,675 0 0 £50,001£100,000 2 122,996 0 0 2 122,996 0 0 £100,001 £150,000 1 110,832 0 0 1 110,832 0 0 £150,001 £200,000 0 0 0 0 0 0 0 0 >£200,000 0 0 0 0 0 0 0 0 14 428,221 0 0 14 428,221 0 0 Totals Notes: All of the exit packages in year relate to compulsory redundancies. 121 Annual Report 2014-15 Audit Committee Annual Report 2013/14 1. Introduction The Audit Committee is established under Board delegation with approved terms of reference that are aligned with the Audit Committee Handbook 2011, published by the HFMA and Department of Health. The Committee consists of three Non-Executive directors and has met on six occasions throughout the financial year. It has discharged its responsibilities for scrutinizing the risks and controls which affect all aspects of the organisation’s business. 2. Principal review areas This annual report is divided into nine sections reflecting the key duties of the Committee as set out of the revised terms of reference, which were approved by the Trust Board in March 2014. 2.1 Governance, risk management and internal control • The Committee has reviewed relevant disclosure statements, in particular the Annual Governance Statement together with the Head of Internal Audit Opinion, external audit opinion and other appropriate independent assurances and considers that the Governance Statement is consistent with the Committee’s view on the Trust’s system of internal control. Accordingly the Committee supports the Board’s approval of the Governance Statement. • The Committee has reviewed the Assurance Framework. It believes that the Framework used during the year was fit for purpose and has reviewed evidence to support this. The Framework is in line with Department of Health expectations and has been reviewed by internal audit and external audit to give additional assurance that this opinion is soundly based. • The Committee has reviewed the completeness of the risk management system and the extent to which it is embedded in the organisation. The Committee believes that adequate systems for risk management are in place, and that these systems are now embedded throughout the whole organisation. At the February 2014 Committee meeting the external auditor introduced a report entitled “Communication with the Audit Committee“, which provided independent confirmation that the systems are in place and operating as intended. 2.2 Internal audit: throughout the year the Committee has worked effectively with internal audit to strengthen the Trust’s internal control processes. The Committee has also in year: • Received and considered the effectiveness of internal audit, taking into account self-assessment review alongside that of the Committee’s own review. • Reviewed and approved the internal audit strategy, operational plan and more detailed programme of work at its February meeting. • Considered the major findings of internal audit and are assured that management have responded in an appropriate manner and that the Head of Internal Audit Opinion and Governance Statement reflect any major control weaknesses. • Discussed and agreed the actions required in 23 reviews which were undertaken during the year. 15 were given significant assurance, 4 were given moderate assurance and 4 were not assurance based reviews. The exceptions concerned: • Procurement (Moderate Assurance). • Data Quality (Moderate Assurance). • Inpatient Core Clinical Documentation Compliance – Mental Health (Moderate Assurance) • Medical Devices (Moderate Assurance) • For Procurement the auditor identified that the Trust had yet to develop a procurement savings plan and a set of KPIs. It is acknowledged that these issues have since been addressed. • In the area of Data Quality audit testing identified concerns with data capture. • For Core Clinical Documentation Compliance (Mental Health) discrepancies were identified with the recording of some clinical assessments and indicators. • For the Medical Devices review issues were identified with the disposal of medical devices. 122 2.3 External Audit • The Committee reviewed and agreed external audit’s annual plan. • The Committee reviews and comments on all the reports prepared by external audit; including the External Audit Annual Governance Report. • The Committee will, on behalf of the Trust Board, review and sign off the 2013/14 annual accounts, alongside the External Audit Annual Governance Report on the 5 June. No issues have been raised to date, which give rise to any concerns or issues of note. • The Committee’s working assumption is that an unqualified audit opinion on the Annual Accounts and on the Trust’s Value for Money will be issued in early June 2014. • Received and considered the effectiveness of external audit, taking into account a self-assessment review alongside that of the Committee’s own review. 2.4 Management • The Committee has continually challenged the assurance process when appropriate and has requested and received assurance reports from Trust management and various other sources; both internally, and externally throughout the year. This process has also included calling managers to account when considered necessary to obtain relevant assurance. The Committee also works closely with the Trust’s Contracting, Information and Performance Manager to ensure that the assurance mechanism within the Trust is fully effective and that a robust process is in place to ensure that actions falling out of external reviews are implemented and monitored by the Committee. • The Committee receives a regular report on the business of the other Board Committees and works particularly closely with the Quality and Safety Committee, ensuring that reports requiring their scrutiny do so before these reports come to the Audit Committee. 2.5 Financial Reporting • During the course of the year the Committee received regular briefings from the Head of Finance (Systems and Reporting) on emerging accounting and reporting issues which were considered pertinent to the annual accounts or the Committee in its wider Governance role. • The Committee has reviewed and approved the Trust’s 123 accounting policies for inclusion within the 2013/14 annual accounts. • The Committee has reviewed the annual financial statements before submission to the Board and considers them to be accurate. • On 8th May 2014 the Committee received a detailed briefing on the Trust’s final accounts for 2013/14, which covered all the significant accounting issues for the year. 2.6 Counter Fraud Service • The Committee has reviewed and approved the annual Counter Fraud plan, terms of reference and its progress reports. A separate annual report is produced to cover the work of the Local Counter Fraud Service. 2.7 Local Security Management Specialist Service • The Committee has reviewed and approved the annual Local Security Management Specialist Service plan, terms of reference and its progress reports. A separate annual report is produced to cover the work of the Service which is considered by the Committee prior to submission to the Area Security Management Specialist and NHS Protect. 2.8 Procurement • At its February 2014 meeting the Committee took on responsibility for oversight of the Procurement strategy, including review and approval of the work plan alongside in-year monitoring of delivery. • The Committee reviewed and approved the 2014/15 work plan and noted the first progress report. 2.9 Data Quality Improvement Plan • At its February 2014 meeting the Committee took on responsibility for oversight of the Trust data quality improvement plan, including review and approval of the work plan alongside in-year monitoring of delivery and therefore work in this area will not fully commence until 2014/15. • From 2014/15 the Committee will also have a new sub-committee reporting to it covering the business conducted on the Trust’s data quality improvement plan. Annual Report 2014-15 3. Other matters worthy of note 5. Conclusion The Committee has reviewed the process and controls the Trust has put in place to achieve its financial obligations throughout the year. It further notes that the Trust has achieved these financial obligations. The Committee is of the opinion that this third annual report is consistent with the draft Annual Governance Statement, Head of Internal Audit Opinion and the external audit review and there are no matters that the Committee is aware of at this time that have not been disclosed appropriately. The Committee recognises the hard work that delivered the financial outcome for the year ending 31 March 2014. Both the financial surplus and proximity of the actual outcome to forecast are a reflection of sound management. Martin Connor Chairman of Audit Committee 9 May 2014 4. Review of the effectiveness and impact of the Audit Committee The Committee has been active during the year in carrying out its duty to provide the Trust Board with assurance that effective internal control arrangements are in place. Specifically the Committee has:• Reviewed the Assurance Framework and Risk Register and has influenced the drafting and on-going development of these tools. • Reviewed its compliance with the Audit Committee Handbook and has undertaken a self-assessment. Actions arising from this self-assessment will be included in the Audit Committee action plan. • Secured the delivery of a 99.2% implementation rate on internal audit recommendations with 362 actions being implemented promptly against a plan of 365. • Ensured that satisfactory progress is made with the implementation of external Audit recommendations, which by their nature are of a more strategic nature. • Worked closely with the two audit service providers and received annual confidential briefings from them. • Reviewed and approved the Trust’s key financial policies and procedures including salary sacrifice schemes for cars and Information technology products and a new lease car policy and ensured that they are fit for purpose. 124 Details of Directors Directors’ interests: The Trust has a Directors’ Register of Interests which is open to the public and may be accessed via the Trust’s internet Our Board of Directors: Chris Burdon, Chairman Chris took up his appointment on 1 July 2011 having been Chairman designate since February 2011. He is the Chair of the Remuneration Committee. Chris was appointed as NED with NHS Worcestershire in December 2008 and chaired their provider services Board. Chris held a series of senior executive positions in the metal processing sector. His last post was with Bradken, an Australian PLC, where he had responsibility for worldwide activity in the power generation and cement production markets and the management of three sites in the UK. Sarah Dugan, Chief Executive Sarah took up post on 1 July 2011 having been Chief Executive designate since March 2011. She is a member of the Quality & Safety and Finance & Performance Committees. Sarah previously worked for NHS Dudley as Chief Executive. Sarah is a trained nurse. She has held a wide range of senior positions with community and mental health service providers and in commissioning organisations. Sandra Brennan, Director of Quality (Executive Lead Nurse) Sandra took up post with the Trust in July 2011 as Director of Quality (Executive Nurse). She is a member of the Quality & Safety Committee. She previously worked for NHS Worcestershire from December 2006 as Director of Clinical Development and Lead Executive Nurse. Prior to this she was Director of Community Services and Nursing at North Birmingham Primary Care Trust. Sandra has a background in nursing management. Dr Bill Creaney, Medical Director Bill took up post with the Trust in July 2011 as Medical Director. He is a member of the Quality & Safety Committee. Previously he worked for Worcestershire Mental Health Partnership NHS Trust as Director of Medical Development from October 2009 and prior to this, as Consultant Old Age Psychiatrist from October 2006. Bill’s main responsibilities include Clinical Governance, engagement of medical staff with Trust’s strategic goals and the Mental Health Act. Bill’s previous experience includes working as a Consultant Old Age Psychiatrist and Associate Medical Director at NHS Ayrshire & Arran. 125 Annual Report 2014-15 Stephen Collman, Director of Operations Stephen was the Deputy Director of Service Delivery with the Trust from August 2011. He is responsible for the day to day running of the Service Delivery Units operations and management teams. Stephen qualified as a Nurse in 1990. He has held a number of management posts in mental health and community services. Robert Hipwell, Company Secretary Robert was previously the Company Secretary with Worcestershire Mental Health Partnership NHS Trust. His responsibilities include Board support, corporate governance / assurance, risk management, health and safety, and claims handling. Robert has over 30 years general management experience in the NHS. He has held director appointments in community & mental health NHS trusts between 1993 and 2001. From 2001 to 2005 he set up and led a Support Services Agency which provided a broad range of services to five NHS organisations. Robert Mackie, Director of Finance Robert took up post with the Trust on 1 July 2011 as Director of Finance. He is a Member of the Finance & Performance Committee. He previously worked for NHS Walsall, initially as Director of Resources from October 2008 and then from November 2010 as Interim Chief Executive. Robert is a qualified accountant and joined the NHS with the 1998 cohort of the national financial management training scheme, having previously worked in general management within the private sector. Sue Harris, Director of Strategy and Business Development Sue was appointed in May 2012. Sue is a member of the Finance & Performance Committee and her Directorate responsibilities include strategy and business development, marketing and communication, the Foundation Trust Programme, the Programme Management Office and procurement. Prior to a secondment to the Strategic Health Authority in 2011 Sue was, from 2009, Lead Commissioner for mental health services in Worcestershire. In this role she led on strategic planning, performance management, resource allocation and market reform. Previously a national director for Turning Point, Sue has 15 years business development experience in the health and social care field. Jill Gramman, Non-Executive Director Jill has been a Non-Executive Director with the Trust since 1 July 2011. She Chairs the FT Programme Board and is a member of the Finance & Performance and Audit Committees. She has a special interest role in patient experience. In a previous role she heard appeals by patients on section under the Mental Health Act. Jill is a former Director and Trustee of SCOPE and BILD. She ran her own marketing research company for over 30 years. Jill is a Magistrate and recently completed three years as Chair of the Kidderminster Bench. She is actively involved in a charity supporting disadvantaged and disabled people in the shanty areas of Lima, Peru. 126 Peter Lachecki, Non-Executive Director Peter has been a NED with the Trust since 1 July 2011. He is the Chair of the Quality & Safety Committee and one of its sub-committees – the Mental Health Act Monitoring Group. He has his own marketing and management consultancy and has held previous senior marketing and general management roles at Kraft Foods, both in the UK and Internationally. Peter is also a NED for Gloucester Cathedral Enterprises and is a member of the governing body of King’s School in Gloucester. David Priestnall, Non-Executive Director David has been a NED with the Trust since 1 August 2011. He is a member of the Audit Committee and Chair of the Finance & Performance Committee. He is also Vice Chairman and Senior Independent Director. David was previously a NED and Vice Chairman of NHS Worcestershire. Prior to this he was Chairman of Wyre Forest Primary Care Trust and Assistant Director of Housing for Birmingham City Council. Martin Connor, Non-Executive Director Martin has been a NED with the Trust since 1 July 2011. He is the Chair of the Audit and Charitable Funds Committees and a member of the Quality & Safety Committee. He is also a NED for the RAC Pension Scheme and Chair of their Audit and Governance Committee as well as Treasurer of both DIAL, a disability charity as well as Sampad, a South Asian Arts organisation. Martin previously worked for the Department of Work and Pensions and spent 20 years working for the RAC in a variety of senior management roles. Steve Peak, Non-Executive Director (Designate) Steve has been a NED (Designate) since 1 November 2013. He is a member of the Finance and Performance Committee. He has his own management consultancy company, lectures for Keele University and is Business Development Director for Vanguard Healthcare Solutions. Over the past 25 years he has held previous senior leadership roles in acute hospitals including a period of time as CEO of Birmingham Women’s NHS Foundation Trust. Rick Roberts, Non-Executive Director Rick has been a Non-Executive Director with the Trust since 1 April 2014, having previously served as a NED (Designate) from 1 November 2013. He is a member of both the Quality & Safety Committee and the FT Programme Board. Rick retired as Medical Director of the Birmingham Community Healthcare NHS Trust in April 2013, having served as an Executive Director in successive NHS Trusts for some 20 years. Previous appointments include Clinical Director of the Birmingham Dental Hospital and Consultant in Oral Surgery. 127 Annual Report 2014-15 Glossary of terms used in Annual Report A&E (Accident & Emergency) The emergency departments of hospitals that deal with people who need emergency treatment because of sudden illness or injury. Sometimes these services are referred to as casualty departments, or minor injury units. Acute services Medical and surgical interventions usually provided in hospital. The Trust only provided these services up to 30th June 2011, after which date these services were transferred to the local acute Trust. Capital CQUIN This is the term used for Commissioning for Quality and Innovation. This is a system introduced in 2009 to make a proportion of healthcare providers’ income conditional on demonstrating improvements in quality and innovation in specified areas of care. In-patient A person admitted on to a hospital ward for treatment. International Financial Reporting Standard (I.F.R.S.) Expenditure on the acquisition of land and premises, individual works for the provision, adaptation, renewal, replacement and demolition of buildings, items or groups of equipment and vehicles, etc. In the NHS, expenditure on an item is classified as capital if it is in excess of £5,000. Issued by the International Accounting Standards Board, financial reporting standards govern the accounting treatment and accounting policies adopted by organisations. Generally these standards apply to NHS organisations. Capital charges Capital charges are a way of recognising the costs of ownership and use of capital assets and comprise depreciation and interest/target return on capital. The Trust is required to put in place a major incident plan that is fully compliant with the requirements of the NHS Emergency Planning Guidance 2005 and all associated guidance. Care Quality Commission Monitor The Care Quality Commission use expert assessors to determine annual ratings for NHS Bodies on the quality of the services they operate. Clinical Commissioning Groups (CCGs) Major Incident plan Monitor is a non-departmental public body established in 2004. It is the public sector economic regulator of NHS-funded health care services and its main duty is to protect and promote the interests of patients. Clinical Commissioning Groups (CCGs) will from 1.4.2013 commission the majority of health services, including emergency care, elective hospital care, maternity services, and community and mental health services. All of the 8,000 GP practices in England are now part of a CCG. There are 211 CCGs altogether, commissioning care for an average of 226,000 people each. There are three CCGs in Worcestershire. NHS England Corporate Governance NHS Trusts The system and rules of delegation by which organisations are directed and controlled. Formally established as the NHS Commissioning Board on 1 October 2012, NHS England is an independent body at arm’s length to the Government. NHS Foundation Trusts NHS hospitals that are run as independent, public benefit corporations, which are both controlled and run locally. NHS trusts are hospitals, community health services, mental health services and ambulance services which are managed by their own boards of directors. NHS trusts are part of the NHS and provide services based on the requirements of patients as represented by Clinical Commissioning Groups (CCGs) and GPs. 128 Outpatient A person treated in a hospital but not admitted on to a ward. Payment by Results (PbR) better planning of patient care and management of long term conditions. Reference costs Transparent rules based system that sets fixed prices (a tariff ) for clinical procedures and activity in the NHS, enabling all trusts to be paid the same for equivalent work. Reference costs are the average cost to the NHS of providing a defined service in a given financial year. Reference cost data allows NHS trusts to compare their costs to the NHS average and therefore benchmark their relative efficiency. P.E.A.T. (replaced by P.L.A.C.E.) Revenue The PEAT (Patient Environment Action) inspections take place every year and comprise a team of health professionals along with an independent patient representative. The team assess each hospital they visit in terms of cleanliness, hygiene, privacy, dignity, patient information, food quality and service. Performance indicator Measures of achievement in particular areas used to assess the performance of an organisation. P.L.A.C.E. Patient led assessments of the care environment (formerly P.E.A.T.) Primary Care Trust (PCT) Primary Care Trusts ceased to operate from 31 March 2013 and were replaced by Clinical Commissioning Groups. Provisions Provisions are made when an expense is probable but there is uncertainty about how much or when payment will be required, e.g. estimates for clinical negligence liabilities. An estimate of the likely expense is charged to the Trust’s Operating Cost Statement as soon as the issue comes to light, although actual cash payment may not be made for many years, or in some cases never. The expense is matched by a balance sheet provision entry showing the potential liability of the organisation. Revenue is expenditure other than capital, for example, staff salaries and drug budgets. Also known as current expenditure. Secondary care Specialised medical services and hospital care, including outpatient and in-patient services. Access is often via referral from primary care services. Strategic Health Authority (SHA) Strategic Health Authorities ceased to operate from 31 March 2013 and were replaced by the Trust Development Authority. Trust Development Authority The focus of the Trust Development Authority from 1 April 2013 is to provide leadership and support to all non-Foundation Trust Hospitals and its goal is first and foremost to help each and every Trust to improve the services they provide for their communities. Virement The agreed transfer of money from one budget head, income or expenditure, to another, within a financial year. Virement is a measure of flexibility that allows budget-holding managers to receive either increases or decreases in their budgets in response to budget variances which cannot be managed within the year. For example activity levels are higher than those anticipated when the budget was originally set. Q.I.P.P. Quality, Innovation, Productivity and Prevention schemes which include Medicines use and procurement, staff productivity, clinical support rationalisation and the 129 Annual Report 2014-15 www.hacw.nhs.uk Annual Report 2014-15 131 If you would like this document in any other format, please contact the Communications Team by emailing communications@hacw.nhs.uk www.hacw.nhs.uk Annual Report 2014-15