Wakefield Hospice Quality Account 2013- 2014 “It’s perfect”
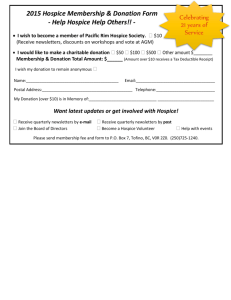
advertisement

Wakefield Hospice Quality Account 2013- 2014 “It’s perfect” Patient to CQC Inspector – Sept 2013 CHIEF EXECUTIVES STATEMENT Together with the Board of Trustees, Staff and Volunteers it gives me great pleasure to present Wakefield Hospice’s Quality Account for the period 2013 – 2014. This is the second year that we have produced a Quality Account and I hope that it will provide you with a summary of how the Hospice Team are continually striving to develop and improve the experience of Hospice care for those who use our services. We aspire to provide excellence in all that we offer to our patients and their families, however we appreciate that this cannot be achieved in isolation. It is essential that the Hospice Team communicates and works in collaboration with other health and social care providers to achieve the best possible outcomes for patients approaching the end of their life. To this end we are actively engaging with new commissioning practices, are involved with cross organisational working groups and are forging ahead with joint projects to ensure that local people can achieve independence and autonomy when making their end of life care decisions and be at all times supported by high quality palliative care services. This year we were very proud to unveil the complete refurbishment of the Hospice Day Therapy Unit. Our service users are delighted with the new and improved environment, whilst staff are enthusiastically considering the possibilities of developing new services to maximise the potential of the reconfigured unit. You will learn more of this as you read our Planning Priorities for the forthcoming year. My thanks as ever goes to not only our staff and volunteers who give tirelessly to ensure that we deliver on our promise to provide outstanding care for patients and their families, but also to our loyal local supporters who enable us to generate the 70% shortfall in our required income. This makes the people of Wakefield our major stakeholders and as such our major responsibility to deliver evidence based, high quality end of life care is directed at them. This Quality Account is a true reflection of the work that has been undertaken at Wakefield Hospice during the last twelve months. I am responsible for the production of this report and to the best of my knowledge the information contained in this Quality Account for 2013 - 14 is an accurate and a fair representation of the healthcare services provided by Wakefield Hospice. Karen Crawshaw Chief Executive Officer 8 May 2014 PART 1 2 1. PRIORITIES FOR IMPROVEMENT 2014 – 15 Wakefield Hospice is fully compliant with the National Minimum Standards (2002) and during a scheduled regulatory inspection held in September 2013 provided evidence to the Care Quality Commission that the regulatory standards had been met and as such, the Board do not have any areas of shortfall to include in the priorities for improvement for 2014 - 2015. However, we continually review and monitor our services and seek to improve and develop them. In addition the Hospice has a three year strategic plan which outlines our vision and plans for the future. The Quality Improvement Priorities identified for the purpose of this report are encompassed within our strategic plan and as such are subject to continual monitoring by the Hospice Senior Management Team and The Board of Trustees. FUTURE PLANNING PRIORITY 1 1.1 Clinical Effectiveness - 24/7 Out of Hours Hospice Admissions Project A twelve month extension of an existing project has been granted to both the Wakefield and Prince of Wales Hospices to increase the number of 24/7 admissions into their in-patient units. The original project outline has been revised by the Hospices’ Management Teams and NHS Wakefield CCG, as a result the project now has a wider scope of application. Crucially the project will go forward without the participation of the third member of the original project. Information will be collated to evidence the benefits to patients and their families of 24/7 access into both Hospices’ in-patient units, as well as to assist the CCG in determining if the project has an effect in reducing the number of inappropriate admissions into acute hospital beds by patients at the end of life. Wakefield Hospice’s aim continues to be to secure ongoing substantive funding for this element of the Hospice service. How was this identified as a priority? The 12 month extension to the project was given because despite a sound evidence base that had determined the demand for 24/7 access to hospice in-patient units, the two Hospices did not manage to achieve the target number of admissions during the initial pilot phase of the project. This was due to well documented circumstances and issues that arose with the third partner of the original project which were out of the control of both Hospices. How will this priority be achieved? The scope of the original project has been widened to enable access for more patients. This will now include patients from all Wakefield Hospice’s usual geographical areas of referral which had previously been limited. Further, patients may now be transferred from acute hospital settings over weekends and bank holidays, the initial project having precluded such hospital transfers. Significantly, the local Community Specialist Palliative Care Nurses are moving towards seven day working which will inevitably increase the demand for more hospice inpatient admissions outside normal weekday working hours. The third party member of the original project is no longer party to this extension of the project which has removed the issues and circumstances that had hampered the progress of the Hospices 24/7 element of the project. 3 How will this priority be measured? The project will continue to provide quantitative and qualitative evidence of the benefits and cost effectiveness of this service to secure mainstream funding. The two Hospices are managing the project in-house and have set key performance and quality indicators to ensure that targets are met, reports and audit of which will be made quarterly to the Hospices’ Boards of Trustees and monthly to NHS Wakefield CCG. The project will be reviewed in Quarter 3 to determine if the project has evidenced the need for ongoing future substantive funding. FUTURE PLANNING PRIORITY 2 1.2 Clinical Effectiveness - To Extend the Remit of In-patient and / or Day Services to Include Increased Provision of Intravenous Medications At the present time it is not possible to care for patients on the in-patient unit who require regular intravenous (IV) medications, or to administer these in the context of the Day Therapy Unit. This is because the Hospice’s qualified nurses are not competently trained to administer drugs intravenously and would therefore require the costly availability of a doctor over a 24 hour period to administer the injections. How was this identified as a priority? Because the Hospice’s qualified nurses do not have access to annual IV competency training, patients who are waiting for transfer into the Hospice from acute hospital services must complete their course of intravenous medications before they are transferred into the Hospice in-patient unit. Similarly patients in the community who require intermittent intravenous medications such as bisphosphonates could appropriately have these administered in the Day Therapy Unit which would free up clinic time in the acute Hospital Trust. Facilitating for patients to have intravenous medications whist an in-patient at the Hospice could reduce the number of inappropriate hospital admissions or the number of bed days for palliative care patients and provide a better experience of care. How will this priority be achieved? A Hospice IV Administration Project Team will be convened to establish and source the knowledge and skills training requirements for nursing staff. Essentially this must also include a means of assessing ongoing clinical competency in IV medication administration. We will liaise with Mid Yorkshire Hospitals Acute Trust to ascertain whether it is possible for Hospice nurses to link into the Hospital Trust IV competency training programme for nursing staff. A Hospice Intravenous Medications Policy will be produced which will be supported by the Hospice’s existing Medications Administration policy. How will this priority be measured? The Project Team will assess the feasibility of implementing this priority and will provide a report to the Hospital Clinical Governance Committee as well as to the Board of Trustees. If 4 it is possible, senior Hospice nurses will be trained and assessed to be competent to administer intravenous medications to patients. Ongoing competency training will be arranged for the nurses. Patients who require hospice care as well as intravenous medication will not have to wait until they have completed their course of intravenous medication before they can be admitted to the Hospice in-patient unit. Records of IV competency training will be retained and maintained. FUTURE PLANNING PRIORITY 3 1.3 Clinical Effectiveness / Patient Experience - To Review and Extend the Current Configuration of Day Therapy Services and Implement Changes Wakefield Hospice Day Therapy Services had an impressive 2732 attendances during the year. The Unit currently opens on four days of the week, Monday to Thursday. There is an excellent attendance record and uptake of therapies from Monday through to Wednesday, but Thursdays are not as well attended. This could be due to the reduced number of available therapies for service users to access on Thursdays. The Day Therapy Unit has just undergone an extensive refurbishment which has widened the scope for extending and reconfiguring services for patients, carers and the bereaved. How was this priority identified? The Hospice Team undertook a SWOT (Strengths, Weaknesses, Opportunities and Threats) and a PESTEL (Political, Environmental, Social, Technology, Environmental and Legal) analysis of the day service. This confirmed the current general trend in healthcare which is based upon the premise of care closer to home and avoiding unnecessary admissions into acute hospital services. The analyses also identified a gap in the statutory provision for timely access to physiotherapy services for palliative care patients. As a result, we are exploring the possibility of extending the remit of our current specialist physiotherapist provision to include an outpatient service which would operate out of the Day Therapy Unit. This service would provide patients with rapid access to palliative physiotherapy to meet rehabilitation needs, or re able people to continue with their activities of daily living. Access to specialist physiotherapy would enable patients to maintain maximum physical functioning and independence for as long as it is possible and to optimise their quality of life. This may provide the additional support that palliative care patients require to remain at home for their end of life care period, thus avoiding an unnecessary hospital admission. How will this priority be achieved? We will work with statutory physiotherapy services and local providers of community palliative care services to scope the need for a specialist physiotherapy service for palliative patients. We anticipate that the new service would include one to one appointments as well as group sessions. Dedicated time will be given to the Hospice physiotherapists to plan and commission the new service. The Hospice will provide specialist physiotherapist staff and a 5 dedicated rehabilitation unit to trial the project for 12 months. After which if the project is successful we will have hopefully collated a sound evidence base upon which to propose a case for the ongoing funding of this service to the CCG. Consideration could also be given to extend the service to provide a domiciliary specialist physiotherapy service in the future. How will this priority be measured? Evidence will be sought to base a case of need for this service. Further the 12 month project will demonstrate a better experience of care for patients and their carers. Demographic and clinical information will be collated in respect of patient characteristics, service activity and quality outcomes. Cost effectiveness of the service will be provided. The project will be overseen by the clinical members of the Hospice Senior Management Team and reports will be made available to the Board of Trustees and to the Hospice Clinical Governance Committee. FUTURE PLANNING PRIORITY 4 1.4 Patient Safety & Clinical Effectiveness - Reduction in the Level of Staff Sickness and Absence The Hospice requires £4.2 million to remain operational in the forthcoming financial year. We receive 30% of this sum (£1.2million – this includes restricted funding received for two projects in addition to the main grant) from statutory funds and must fundraise for the remaining 70%. The largest area of expense is attributable to staff salaries at a cost of £3.2 million (equating to 76% of total expenditure). Given that there is no flexibility within the budget, there is concern that unpredicted costs incurred through high staff sickness and absence is becoming financially unsustainable. How was this priority identified? Over the last few years we have experienced increasing costs associated with staff sickness and absence. We have benchmarked the Hospice figures for sickness and absence against those of NHS staff and were surprised to find that the percentage sick time is comparative. We had expected that as the Hospice generally offers better working conditions and available support than is available in the NHS, the Hospice staff sickness and absence costs percentage should be less. We are therefore committing to reduce the Hospice level of staff sickness and absence in the next 12 months. How will this priority be achieved? The Senior Management Team have utilised and explored different tools for managing sickness and absence over the years and have concluded that despite some criticism of its application, introducing the Bradford Factor of monitoring and dealing with staff sickness and absence would offer a workable solution to managing short term sickness and absence. An external company has been sought to deliver a training programme which will inform 6 managers and staff why this system is to be implemented and to instruct managers in its use. A staff group will be convened to cascade the implementation of the Bradford Factor into departmental use. The Hospice has also agreed to take part in a benchmarking exercise with other Yorkshire Hospices to establish whether or not Wakefield Hospice has a higher than average level of sickness and absence or not. How will this priority be monitored? Monthly monitoring and stringent management of sickness and absence in accordance with the current Hospice Sickness and Absence Policy will be introduced. Monthly costs and percentage sick time will be collated and shared with staff. Monthly statistics will be shared with the hospice that is collating the shared data for the Yorkshire Hospices Sickness and Absence benchmarking project. The training for staff to be able to competently use the Bradford Factor System will take place and the system will be introduced. Quarterly reports will be shared with the Board of Trustees. "The staff are very good. They treat me very well and always sort things out for me. "Service User Quote September 2013 PROGRESS MADE AGAINST THE PRIORITIES FOR IMPROVEMENT 2012 – 2013 1.5 Planning Priority 1 24/7 Rapid Response Team and Out of Hours Hospice Admissions Project To continue to develop 24/7 admissions to the in-patient unit, collating the information required within the scope of the project outline; to work collegiately to support the development of the Marie Curie Out of Hours Rapid Response Nurse Team within the district; 7 to meet the outcomes of the project with the aim of securing ongoing substantive funding for the service. This objective was achieved in part and remains ongoing with an amended project remit. (See 1. 1). It was unfortunate that due to some internal factors as well as external obstacles the Marie Curie Rapid Response Team element of the project failed to deliver its expected outcomes. This failure had a direct impact on the Hospices’ 24/7 element of the project which resulted in fewer out of hours admissions into both Hospices than was expected. Despite this, the project was able to demonstrate the value of out of hours admissions into the Hospices for patients, their families and carers. As a result the CCG and the Hospices have revised the remit and scope of the original project and funding has been provided for a further 12 month period of time in which to evidence the need for the service. 1.6 Planning Priority 2 Education Post To develop and recruit a dedicated Hospice Palliative Care Educator to provide end of life care education and training programmes for Hospice staff and volunteers and the wider health and social care community; to income generate from the programmes as is appropriate. Achieved and ongoing; This post was advertised twice during the year before a successful candidate was recruited. The post holder will take up the position in May 2014 and will undertake a training needs analysis of the Hospice staff and will develop in service education and training programmes as determined by the outcomes. The new post holder will also work with the Wakefield and Mid Yorkshire Palliative Care Education Forum and take forward initiatives to develop a Hospice programme of end of life care training and education for the benefit of the locality. “it’s the knowledge that she received such exemplary care that allows me to begin to cope with her passing” Patient’s Husband 2013 1.7 Planning Priority 3 Extend Mechanisms of Patient Feedback The Hospice will develop a more robust Patient / Carer Service User Group and widen the scope of available mechanisms of achieving patient feedback. Achieved. 8 The Hospice Service User Group has become much more established during the last year. During this time Group Members have been co-opted onto several of the Hospice’s operational committees and have assisted with patients and carer satisfaction audits including Wakefield Hospice Report on the Patient Led Assessment of the Care Environment (PLACE) 2013. The Group has reviewed patient literature including the Medicines Advice leaflet which is given to patients and carers upon discharge home from the in-patient unit. They have worked with the Hospice’s Web Site developer to include a page about the role of the Service User Group which invites feedback on the care and services that are provided by the Hospice and encourages new service users to join the Group. 1.8 Planning Priority 4 Infection Control Good infection control is an essential requirement in terms of providing good palliative care, maintaining registration with the Care Quality Commission and patient confidence. Achieved. Spot checks have been undertaken using the Kairos system. This is a device preloaded with hospice specific audits which has been in use during the year to assess, monitor progress and to benchmark against other Hospices. We have been able to demonstrate a continuing improvement in the consistency of infection control standards. Further to this the Bare Below the Elbows and Hand Washing audits are undertaken monthly and are regularly achieving 100% compliance. 1.9 Planning Priority 5 Refurbishment and small building extension for the Day Therapy Unit Funding from a non-recurrent capital grant has been made by the Department of Health to enable the existing facility to be completely reconfigured by removing dividing walls and building a small extension. This will provide a new relaxation room and create physiotherapy and complementary suites. The reconfiguration of the area will create a quiet communal space as well as a dedicated arts and craft area. Achieved; the Day Therapy Unit refurbishment and building project was completed on time and in budget, it was re-opened to service users in January 2014. Service Users are hugely enthusiastic and report positively about the new unit. The reconfigured unit has provided much more workable space and has already enabled the development of new services with the appointment of a Music Therapist, whilst a specialist physiotherapy outpatient service is currently under consideration. 9 “ It was a hard decision placing our dad in the Hospice but we now have the comfort that it was the right decision, a huge heartfelt thank you, not only for caring for him, but for supporting our family” Patient’s family 2014 PART 2 2. MANDATED STATEMENTS Statements of Assurance from the Board The following are a series of mandatory statements that all providers must include in their Quality Account. Many of these mandatory statements are not directly applicable to Hospices. Explanations (in italics) of what the mandatory statements mean are given as appropriate. 2.1 Review of Services During 1st April 2013 to 31st March 2014, Wakefield Hospice provided the following service: • • • • In–Patient Service Day Therapy Service Family Care Service Bereavement Services 10 • Education and Training Therapies; • Occupational Therapy • Physiotherapy • Complementary Therapies • Music Therapy The income generated by the NHS services reviewed in 2013 – 2014 represents 30% of the total income generated from the provision of NHS services by Wakefield Hospice for 2013 – 2014. (Mandatory Statement) Wakefield Hospice received an annual grant from NHS Wakefield Clinical Commissioning Group; this is a fixed sum regardless of the Hospice’s activity or the level of voluntary income. This means that 100% of the financial support that we receive from the NHS is spent directly on patient services. The remaining 70% of income required is generated through generous donations and support from our local community, legacies, fundraising initiatives, and our chain of charity shops. 2.2 Participation in Clinical Audits, National Confidential Enquiries During 2013 - 14 there were no national clinical audits and national confidential enquiries covered by the NHS services provided by Wakefield Hospice. (Mandatory Statement). This means that as a provider of specialist palliative care Wakefield Hospice was not eligible to participate in any of the national clinical audits or national confidential enquiries. This is because none of the 2013 – 2014 audits or enquiries related to specialist palliative care. However, Wakefield Hospice carries out a plan of internal clinical audits throughout the year as a means of measuring the quality of the services it provides. 2.3 Research The number of patients receiving NHS services provided by or subcontracted by Wakefield Hospice in 2013 – 2014 that were recruited during that period to participate in research approved by a research and ethics committee was 0. (Mandatory Statement). This means that In 2013 – 2014 there was not any local or national ethically approved research projects that patients at Wakefield Hospice were eligible to participate in. However, the Hospice has registrars on placement from the Leeds Deanery who are undertaking local research as part of their studies. 2.4 Goals Agreed with Commissioners Wakefield Hospice’s statutory income in 2013 – 2014 was not conditional on achieving quality improvement and innovation goals through the Commissioning for Quality and Innovation payment framework. This is because Wakefield Hospice as a third sector provider of services does not use any of the NHS National Standard Contracts and therefore is not eligible to negotiate a CQUIN Scheme. (Mandatory Statement). However, the high quality of services provided by Wakefield Hospice has always been central to the organisation’s intent and as a result the Hospice has always been open to scrutiny and readily shares the results of its own internal quality and improvement programme with CCG Commissioners. 11 2.5 What Others Say About the Hospice Statement from the Care Quality Commission: Wakefield Hospice is required to register with the Care Quality Commission and is registered as an Independent Hospital, Hospice for Adults. Wakefield Hospice’s current registration service is for the following activities: • • • Diagnostic and Screening Procedures Transport Services, triage and medical advice provided remotely Treatment of disease, disorder or injury Wakefield Hospice was subject to an unannounced inspection on 19 September 2013 and was found to be fully compliant with the standards by which it was measured. The Care Quality Commission has not taken any enforcement action against Wakefield Hospice during 2013 2014. (Mandatory Statement). 2.6 Data Quality Wakefield Hospice did not submit records during 2013 - 2014 to the Secondary Uses service for inclusion in the Hospital Episode Statistics which are included in the latest publication data. This is because Wakefield Hospice is not eligible to participate in the scheme. However, in the absence of this and with our patients consent, the Hospice utilises the electronic patient information system SystmOne to share information on patient records with our colleagues in primary and secondary care settings to support seamless patient care. The system uses the NHS number as the key identifier for patient records. In accordance with the Department of Health, additionally, Wakefield Hospice submits a National Minimum Data Set to the National Council for Palliative Care. (Mandatory Statement). 2.7 Information Governance The staff at Wakefield Hospice have undertaken a considerable amount of work over the last twelve months to improve the organisation’s information governance and to become compliant with NHS Information Governance Toolkit. The Hospice made its first submission as an NHS Business Partner in March 2014 and was assessed to be satisfactory at compliance level two with a score of 66%. 2.8 Clinical Coding Error Rate Wakefield Hospice was not subject to the Payment by Results clinical coding audit during 2012 - 2013 by the Audit Commission. (Mandatory Statement). 12 “I loved her (still do) very much, as do the kids and it broke my heart, but without you it would have been so much worse” Patient’s Husband 2014 PART 3 QUALITY OVERVIEW This section provides information about how many people use our services, how we monitor the quality of care that is provided and what our patients and families and regulators say about us. The Hospice is regulated by the Care Quality Commission and was last inspected on 19 September 2013 when no shortfalls were identified and the Hospice was found to be fully compliant in meeting all of the essential standards of quality and safety. The inspectors routinely talked to patients and relatives during the inspection process and were told that the Hospice staff communicated with them well and that they understood the care and treatment choices available to them. The Minimum Data Set (MDS) for Specialist Palliative Care Services is collected on an annual basis, with the aim of providing an accurate picture of hospice and specialist palliative care service activity. The Wakefield Hospice MDS shown here covers the period from 1 April 2013 to 31 March 2014 with comparative data from the previous year. 13 MDS In-Patient Unit 2013-2014 Wakefield Hospice In – patient Unit Wakefield 2013 - 2014 Hospice Wakefield 2012 -2013 Hospice National Median 2012 – 2013 Total No of Admissions 300 294 308 Total No of Completed Stays 306 294 304 Total No of Patients 241 263 274 New Patients 217 243 239 % Bed Occupancy 62% 73.7% 73% Average length of stay 11.6 days cancer 8.0 days non cancer 12.3 days cancer 13.6 days non cancer 12.8 days cancer 11.5 days non cancer 179 - 58.5% 181 – 61.2% 173 – 59.3% 11% 9.5% 11.1% Patient deaths % patients with a non-cancer diagnosis MDS Day Therapy Unit 2013- 2014 New Clients 163 Continuing Clients 267 Total Number of Attending Patients 110 Total Number of Attending Carers 101 Total number of patients with a cancer diagnosis 125 Total Number of patients with a non-cancer diagnosis 14 Total number of deaths / discharges 174 14 Number of day therapy sessions per year 300 Number of actual attendances in the year 2732 MDS Bereavement Services 2013 – 2014 New Service Users 66 Continuing Service Users 201 Re accessing service users 5 Total Service Users 272 Telephone contact lasting more then 10 minutes 1668 Face to face group work (facilitated) 16 Face to face individual counselling by professional accredited person 238 Other forms of contact 151 Number of discharged service users 125 Number of continuing service users at the end of the year 150 OUR PARTICIPATION IN CLINICAL AUDITS To ensure that the Hospice is providing a consistently high quality service we undertake our own clinical audits using national audit tools which have been developed specifically for hospices. This allows us to monitor the consistency and quality of the care that is provided to our patients and their families, as well as providing a cyclic quality framework upon which to base our judgements and seek improvement if necessary. The Hospice has an Audit and Policy Group which takes responsibility for undertaking and managing the audit cycle, preparing reports and highlighting any areas of shortfall or risk. Clinical audit reports feed into the Clinical Governance agenda which in return reports to the Hospice Board of Trustees. 15 During 2013 – 2014 the following audits were undertaken: AUDIT DATE ACTION PLAN ACTIONS REQUIRED TO IMPROVE PRACTICE Controlled Drugs Audit December 2013 None Repeated 3 monthly and is undertaken with Required Hospital Pharmacist. Medicines Chart Audit December 2013 Yes Minor documentation omissions by nursing and medical staff found. Reminders to all staff to ensure documentation is completed. Repeat in 6 months. In-Patient Satisfaction Survey June 2013 None required High level of satisfaction expressed. Repeat in 6 months. Accountable Officer Self-Assessment February 2014 None Required Syringe Driver Audit December 2013 Yes Wound & Pressure Area Audit March 2014 None Excellent audit report – all patients had Required pressure areas checked and swabbed if required within the recommended 6 hours of admission, appropriate well documented care plans initiated. Hand Washing Audit March 2014 None 100% compliance. Audit is undertaken Required monthly. Bare Below the Elbows Audit March 2014 None 100% compliance. Audit is undertaken Required monthly. Nutrition Audit January 2014 Yes Bowel Assessment Audit December 2013 None Excellent Audit report, 100% score for Required documentation, care planning and evidence that appropriate use of aperients had negated the need for rectal interventions in the sample of records audited. DTU Patient & Carer Satisfaction Audit March 2014 Yes High Satisfaction levels recorded. Conclusion suggests adapting the questionnaire to reflect changes to the new environment. Preferred Place of Care & ICP Audit April 2014 None required 100% of in-patients had the opportunity to discuss advance care planning including preferred place of death. 100% of patients had resuscitation status discussed with them and / or their family. Consider updating the Syringe driver prescription chart to allow more space to record completed checks. Excellent Audit report, but minor omissions in documentation were reported. 16 PLACE (Patient Led Assessment of the Care Environment) Audit August 2013 Yes The hospice building (24 years old) does not meet the standard for the visually impaired which is required for newer buildings. Plan to seek grant funding to bring the Hospice up to current requirement set for new buildings. QUALITY MARKERS THAT WE HAVE CHOSEN TO MEASURE INDICATOR 2013 -2014 COMPLAINTS Total Number of Complaints 0 Total Number of Complaints Upheld 0 Total Number of Complaints Upheld in Part 0 PATIENT SAFETY INCIDENTS Number of patient accidents excluding falls 14 Number of slips, trips and falls 26 Number of accidents reportable under RIDDOR 2 SAFEGUARDING Number of patients, clients, and families reported to Social Services because of safeguarding concerns 1 THE BOARD OF TRUSTEES COMMITMENT TO QUALITY The Board of Trustees is fully committed and supportive of the Hospice Quality Agenda. The Hospice has a well-established governance structure, with members of the Board having active roles in ensuring that the Hospice provides a high quality service in accordance with its Statement of Purpose. “The staff talk to us about my care and give us options. We can ask questions and the staff explain things” 17 18 19 20