Martlets Quality Account 2013-2014
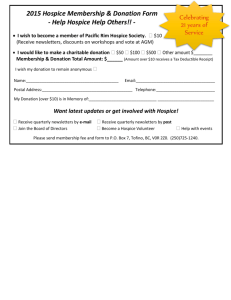
advertisement

Martlets Quality Account 2013-2014 “I have nothing but admiration and praise for the palliative and emotional support provided. It made one of the most traumatic experiences in our lives tolerable and has helped in the healing process.” Patient’s relative, 2013 1 Part 1: Statement from the Chief Executive __________________________________________________________________________________ continues to provide high quality Palliative and End of life Care for the people of Brighton and Hove. We pride ourselves in delivering the right care, at the right time, in the place that is right for patient and their families. This is made possible through the collaboration of all of the services provided by the Martlets. At the Martlets we have a range of professional teams delivering services. These include our 18 bedded in patient Unit, our Hospice at Home service which also has a respite arm, our Day Services with a range of services such as rehabilitation, complementary therapies, acupuncture and we are developing further services. We are committed to providing services which will support and enhance patients and carers quality of life. Responding to the changes within health and social care and the need to work collaboratively with the right partners to provide wider access to our services is very much one of our drivers. Our response to this has been to generate a more open and flexible approach to Day services for more people. In 2013 the Hospice at Home service formally collaborated with our NHS colleagues, the Community Palliative Care team, who are the Clinical Nurse Specialists team with Medical Consultant cover, to become the Palliative Care Partnership. This remodelled service provides 24hour access for patients, carers and professionals to support and advise from Palliative and End of Life Care services. It operates through a central hub function which means one number for all and so reducing duplication and increasing greater access. The report outlines the quality of the services we continue to provide and also identifies where innovation and growth has been identified and how we have responded to need such as investment in supporting people at home through setting up a range of Day services which have both a social and health value. This new model very much incorporates the needs of the carer as well as the patient. 2 Hospices are evolving and we have a duty of care to our local community in Brighton and Hove to continually show our skills, expertise and responsibility in adapting and responding to these changes. I hope this report demonstrates that we are delivering the quality and scope of service needed. Imelda Glackin Interim Chief Executive Officer Our Vision We believe a good and dignified death is everyone’s entitlement. To those dying in our community, we will provide the best possible care. We will raise as much money as possible to help as many people as we can. Through our work and reputation we will remain attractive to our stakeholders and deserving of their support 3 4 What we do well… Performance in 2013-2014 IPU Our 18 bed inpatient unit is staffed by 32 nurses and 20 nursing auxiliaries. Our bed occupancy rate remains consistently high at 88.8% (compared with the national average of 80%). In the year 2013-2014, 273 patients were admitted to our ward. These patients stayed on average for 16.7 days. 90% (246) of patients had a diagnosis of cancer. The remaining 10% of patients had conditions such as Motor Neurone Disease, heart failure and chronic respiratory disease. "The food is good and I can ask if I want a small, medium or large portion which is really good." Patient, CQC Report 2013 “My sisters and I all feel that we couldn't have managed without the Hospice@Home team. Mum's wish was to die at home and we achieved that with their help. We are eternally grateful.” Patient feedback, 2013 H@H Our Hospice at Home service provides community support for people in their own homes at the end of life. The team consists of 7 nurses and 4 nursing auxiliaries who do visits 7 days a week. The Hospice at Home service is part of the wider Palliative Care Partnership, which along with the Sussex Community NHS Trust Community Palliative Care Team, provides 24 hour telephone support and advice to patients, families and professionals. In the year 2013-2014, the team saw a total of 377 patients, and supported 197 people to die in their preferred place at home. 5 Bereavement Service Our bereavement service forms part of the Patient and Family Support Team, and consists of 3 part time qualified counsellors available for one to one counselling and trained bereavement volunteers who visit people in the community. In the year 2013-2014, a total of 157 clients were seen by the bereavement service, including 112 females and 45 males. The average length of support these individuals received was just over 4 months. "I cannot speak highly enough of the staff, they are always so helpful and kind and nothing is ever too much trouble." Patient, CQC Report 2013 Rehabilitation Our Specialist Physiotherapist and Specialist Occupational Therapist, along with a therapy assistant, provide rehabilitation input to patients on the ward and in the community. A new multidisciplinary rehabilitation clinic runs weekly for patients requiring specialist advice, therapy and support with such symptoms as breathlessness or fatigue. The clinic has just started and a total of 24 patients have been seen so far in the rehabilitation clinic. “The staff we observed understood the support needs of patients, their carers and family members.” CQC report 2013 Patient and Family Support Team The Patient and Family support team consists of Counsellors, a Chaplain, Social Workers and a Discharge Coordinator. The team support patients and families on the ward and also visit people in the community. The community Social Worker coordinates the community visiting volunteers who provide support to patients and families. During the year 2013-2014, the team saw a total of 619 clients, including 333 on the inpatient unit, 129 in the community and 157 outpatients. 6 Complementary Therapies Our complementary therapy service began during the year 2013-2014 and consists of a team of 20 volunteer therapists, which continues to expand. Massage and acupuncture are offered to patients on the inpatient unit and since the start of the service in January 2014, 100 therapy sessions were delivered to patients on the inpatient unit. Education The Hospice Learning and Development team provided 1037 training days in the year 2013-2014. A total of 1940 people attended these study days, which includes hospice staff and people from external organisations. The education events have covered a range of topics, including advance care planning, first aid, psychological assessment skills, dementia awareness and infection control. Online learning has been launched for staff and includes modules in information governance and anaphylaxis. "The staff are a first class act and you couldn't wish for anything better." Patient, CQC Report 2013 7 What we have improved in 2013-2014… The following priorities were identified for the past year and achievements against these priorities are outlined below. Priority 1: Achieve access to the NHS electronic network (N3/COIN) In order to gain access to the NHS electronic network, the hospice needed to demonstrate compliance with Information Governance standards applied to the NHS. This involved completing the Information Governance Toolkit, which the hospice has done and achieved 100% compliance with Level 2. Partial read-only access to the NHS electronic network has been achieved in the past year and expanding this access will continue to remain a target for the organisation. Priority 2: Improve access to hospice services by setting up the Palliative Care Partnership The establishment of the Palliative Care Partnership and the creation of a 24 hour single point of access to specialist community palliative care services, the ‘hub’, was achieved at the start of the year 2013-2014. This has led to an average of 90% of patients dying where they wanted to be during the year and the prevention of an average of 17 hospital admissions per month. Around 20% of patients accessing care from the Palliative Care Partnership have a non-cancer diagnosis. Priority 3: Increased engagement with service users by forming a service user group Setting up a service user group has not been achieved in the past year, however, a research and scoping exercise for engaging with service users has been carried out. This involved the inpatient social worker visiting other local hospices and learning about the different ways in which service users views are sought and acted on. Forming a service user group within Martlets Day Services remains an aim for the hospice. 8 Part 2: Priorities for Improvement __________________________________________________________________________________ What we want to achieve in 2014-2015… Below we have outlined the priorities for patient safety, clinical effectiveness and patient experience we want to achieve in the coming year. Priority 1: Patient Safety We will scope the need for and provision of a two week Step-down service for patients discharged from the inpatient unit and run a pilot step-down service to assess impact and sustainability. How was this identified as a priority? This was identified as a priority by the hospice discharge coordinator as there can sometimes be a lack of support in the community for patients discharged home from the inpatient unit. This is exacerbated if the patient has no family living nearby and is socially isolated. A step-down service provided by the hospice would help to provide continuity of care, prevent hospital admissions and assist in identifying further hospice services that may be of benefit to the patient. How will this be achieved? A scoping project will be completed, examining statistics of the numbers of patients discharged from the inpatient unit, the level of need of these patients, feedback from patients and families and a review of external services currently available in the community. A pilot project will be completed by the end of the year. How will progress be monitored/recorded? A timeline of delivery of the scoping project and pilot will be identified at the start of the year. The scoping project and pilot are to be completed by the end of the year. Priority 2: Clinical Effectiveness We will broaden access to hospice services through the new Martlets Day Services. How was this identified as a priority? It was identified that many patients and their families were not able to access services offering therapy, support and advice since the closure of the day hospice in 2012. How will this be achieved? The Martlets Day Services will offer the opportunity for patients and carers to access rehabilitation clinics or groups, support groups, complementary therapy sessions and specialist advice and support from our social workers, chaplain and benefits advisors. The Martlets Day Services will open in May 2014, with services commencing throughout the year. The complementary therapy service will be offered in Day Services from June 2014. The Martlets Day Services will expand to include a whole range of interventions and support for people living with life limiting conditions. How will progress be monitored/recorded? Each of the different services will record client activity and also gain feedback from patients and carers. The data collected along with the qualitative feedback, will inform future service developments. 9 Priority 3: Patient Experience We will standardise across each of the hospice services, the way in which feedback is sought from carers using a validated tool and explore benchmarking opportunities with other hospices. How was this identified as a priority? The creation of the Palliative Care Partnership, consisting of the Community Palliative Care Team and the Hospice at Home Team prompted the need for a single feedback survey to be developed for these teams. The existing feedback surveys did not account for patients who may have experienced services from both the inpatient unit and the community teams. The value of being able to benchmark with other hospices was identified and so a hospice wide feedback survey was sought. How will this be achieved? The VOICES-HOSPICE-SCH tool, developed by St Christopher’s Hospice and the University of Southampton, will be implemented. The survey covers both the inpatient and community setting. The survey is used by a number of other hospices and so we will seek to identify these organisations and work together with them to benchmark results. How will progress be monitored/recorded? Feedback obtained from the completed VOICES surveys will be analysed and presented as a report on a six monthly basis at the hospice Clinical Governance Meetings. Part 3: Statement of Assurance __________________________________________________________________________________ The following are statements that all providers must include in their quality account. Many of these statements are not directly applicable to specialist palliative care providers. Review of Services During 2013-2014, the Martlets Hospice supported the NHS commissioning priorities with regard to the provision of local specialist palliative care by providing: o IPU o H@H In addition the Hospice has provided the following services through charitable funding: o Bereavement Support Service, including professional counsellors and trained bereavement volunteers o Rehab Clinic delivering specialist Occupational Therapy and Physiotherapy o Volunteer Visiting Service o Complementary Therapy Service o Education and Training Income Generated The income generated by the NHS services reviewed in 2013-2014 represents less than one third of the total income generated by Martlets Hospice for 2013-2014. Through contracts with the local Clinical Commissioning Group, funding was also provided for two NHS continuing healthcare beds, allowing patients to continue to be cared for at the Hospice until the end of their life if their nursing needs and specialist palliative care needs are high. The remaining income is through charitable donations and through fundraising events such as our annual Midnight Walk, our 9 shops and the hospice lottery. 10 Participation in Clinical Audit During the 2013-2014 period, the Martlets Hospice was not eligible to participate in any national clinical audits or confidential enquiries. This is because none of the national clinical audits or confidential enquiries related to specialist palliative care. Hospice Clinical Audits The Martlets Hospice has completed a number of clinical audits in the 2013-2014 period, which form part of the annual audit programme. The monitoring and reporting of the results of these audits, as well as the implementation of recommended actions following the audits ensures that care delivery is safe and effective. The clinical audit programme can be viewed in the table below. Month April July August September October November February March Audit Review of all accidents, incidents and near misses, repeated every quarter Review of all drug errors, repeated every quarter Review of all informal and formal complaints received, repeated every quarter Standards of record keeping Patient Identification on inpatient unit Spiritual Care on inpatient unit Patient falls on inpatient unit Dignity in care on inpatient unit Use of antibiotics on inpatient unit Completion of manual handling risk assessment forms Discharge planning on inpatient unit Use of TTO/POD books Recording of informed consent Management of diabetes at end of life Compliance with Infection control standards Review of correct use, ordering, delivery, receipt and stock of controlled drugs Compliance with law and regulations of accountable officer for controlled drugs Qualitative evaluation of bereavement service Occurrence of pressure ulcers Use of pain assessment charts Compliance with psychological assessment Research The number of patients receiving NHS services provided or subcontracted by the Martlets Hospice in 2013-2014 that were recruited during that period to participate in research approved by a research ethics committee was: None. There were no appropriate, national, ethically approved research studies in palliative care in which we could participate. Use of CQUIN payment framework The Martlets Hospice income in 2013-2014 was not conditional on achieving quality improvement and innovation goals through the Commissioning for Quality and Innovation payment framework because it is a third sector organisation and as such was not eligible to participate in this scheme during the reporting period. 11 Care Quality Commission The Martlets Hospice is required to register with the Care Quality Commission. The Martlets Hospice is required to undertake only regulated activities at the following location: Martlets Hospice, Wayfield Avenue, Hove, East Sussex, BN3 7LW. The Martlets Hospice is subject to periodic reviews by the Care Quality Commission and the last on-site inspection was in September 2013. The Martlets Hospice has not participated in any special reviews or investigations by the Care Quality Commission during 2013-2014. Data Quality The Martlets Hospice did not submit records during 2013-2014 to the Secondary Users service for inclusion in the Hospital Episode Statistics which are included in the latest published data. This is because the Martlets Hospice is not eligible to participate in this scheme. However, the Martlets Hospice does submit data to the Minimum Data Set (MDS) for the Specialist Palliative Care Services collected by National Council of Palliative Care on an annual basis, with the aim of providing an accurate picture of hospice and specialist palliative care service activity. Information Governance Toolkit Attainment Levels The Martlets Hospice is not required to use the Information Governance Toolkit, however, as a standard for good practice we have completed the toolkit to 100% Level 2 compliance for the past three years. 12 Part 4: Quality Overview __________________________________________________________________________________ We have chosen to present an overview of the hospice inpatient unit for the year 2013-2014. Total number of patients seen Age of patients 273 25-64 years 32% 65-74 years 30% 75-84 years 24% 85+ years 14% Average bed occupancy rate 89% Patients seen with a diagnosis of cancer 90% Patients seen with other diagnoses 10% Average percentage of patients achieving their preferred place of death 79% The hospice asks for feedback from patients and carers who receive care and support from the inpatient unit. Below are just some of the positive comments we received in the last year from people who had experienced this service. “I could not fault the Martlets Hospice and received wonderful nursing for my husband. He couldn’t have died in a better place.” “Your excellent service eased the last weeks immensely. I was able to go back to being a friend rather than a stressed and worried carer. That time was precious. Thank you.” “My father only spent 36 hours with you before he died. But you gave the ending he deserved, peaceful, pain free and surrounded by his family in a supportive environment.” “Although my wife was only with you about two and a half days the service and treatment was amazing. It made her passing a little more bearable for us and for her hopefully. “ “I cannot fault the care, support and advice we received. Although my father deteriorated very quickly, the staff were wonderful in supporting us in our time of need. I cannot thank you all enough.” “I cannot find fault with anything to do with Martlets. My husband’s end of life could not have been in a better place. Thank you.” 13 A feedback survey is sent out to carers eight weeks following the death of the patient. Results from the feedback surveys are compiled every six months. The results from the surveys completed during 2013 and 2014 are presented below. Where people first hear about the Martlets Community Palliative Care Team (22.4%) Hospital Palliative Care Team (19.6%) District Nurse (9.4%) GP (8.4%) Other (40.2%) In comparison with previous surveys, there had been greater satisfaction reported in – Number 4b 4c 4d 4e 4f Question Was the hospice able to help your relative/friend when an inpatient with reducing nausea and vomiting? Was the hospice able to help your relative/friend when an inpatient with easing breathlessness? Was the hospice able to help your relative/friend when an inpatient with lessening restlessness? Was the hospice able to help your relative/friend when an inpatient with alleviating anxiety and fear? Was the hospice able to help your relative/friend when an inpatient with looking after mouthcare? Result (rated 4 or 5) 95.1% (from 88.1% and 93.3%) 96.9% (from 93.1% and 98.1%) 97.6% (from 89% and 95.5%) 94.7% (from 88.5% and 94.2%) 98.8% (from 91.9% and 94.1%) On one question, a lesser degree of satisfaction was reported than previous surveys however. This was – Number 4a Question Was the hospice able to help your relative/friend when an inpatient with relieving pain? Result (rated 4 or 5) 94.8% (from 98.9% and 96.4%) 14 Many of the questions identified no significant changes with previous surveys. These were – Number 2 Question Result (rated 4 or 5) 84.1% 7 Did you get a full explanation about what to expect from the hospice? Do you think the hospice was able to admit your relative/friend quickly enough? Was the hospice able to help your relative/friend when an inpatient with attending to washing and dressing? In general, were the staff able to make your relative/friend feel more comfortable? Did you feel involved in the decisions about the care of your relative/friend? Did you feel that staff listened to you? 8 Were you treated politely? 97% YES 9 Did you feel that staff supported you? 97% YES 10 98% YES 11a Did you feel able to discuss your worries or anxieties with the nursing team? Please rate the cleanliness of the premises 11b Please rate the quality of the catering 84% 11c Please rate the general environment / surroundings 98% 12 Did the service you receive match your expectations? 96% 3 4g 5 6 81.1% 98.8% 96% 86.3% 97% YES 97% These are largely positive results and help to identify specific areas for the hospice inpatient team to develop and/or improve. The results of the feedback surveys are always presented to the Clinical Governance Group within the hospice and to the Board of Trustees, reflecting our honesty and transparency and contributing to our culture of striving to achieve the best possible care. Supporting Statements As required by the regulations, this document has been sent to the following organisations for comment: Brighton and Hove Clinical Commissioning Group Brighton and Hove City Council Health and Wellbeing Overview and Scrutiny Committee Brighton and Hove Healthwatch Board 15 Comments received are included below. Brighton & Hove City Council’s Health and Wellbeing Overview and Scrutiny Committee has not had the opportunity to review the work that the Martlets Hospice carries out so we are not in a position to fully comment on the 2013-14 Quality Account. However we would like to record our appreciation for the valuable work that the Martlets Hospice does in the city, it is clear from some of the personal statements included in the Quality Account that they are able to help patients, their families and friends at a very difficult time, and we would like to thank them for all of the good work that they do in Brighton & Hove. Councillor Sven Rufus, Chair, HWOSC 16