Quality Account 2012-13 Birmingham Community Healthcare NHS Trust Birmingham Community Healthcare
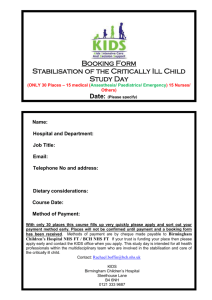
advertisement

Birmingham Community Healthcare NHS Trust Birmingham Community Healthcare NHS Trust Quality Account 2012-13 Contents Section 1................................................................................................................. 1 • • • • • • • • • Statement of quality from Chief Executive....................................................... 2 - 3 Statement from the Chairman................................................................................. 4 Directors’ declaration............................................................................................... 4 Putting quality first .................................................................................................. 5 About our services.................................................................................................... 9 Our values............................................................................................................... 10 Where our services are provided........................................................................... 11 Community Foundation Trust - application update............................................. 12 Accolades for our Trust and staff during 2012-13................................................ 13 Section 2.............................................................................................................. 14 • • • • Our priorities for clinical improvement in 2013-14 ............................................. 15 Review of performance - clinical priorities update 2012-13................................ 23 Commissioning for Quality and Innovation (CQUINs) 2012-13............................ 30 Quality performance data - statutory content .................................................... 50 Section 3............................................................................................................ 61 • • • • • • • Review of quality in clinical services - National quality indicators...................... 62 Snapshots of quality improvements during 2012-13..................................... 86 Investments in our Trust................................................................................ 106 Assurance process................................................................................................. 111 Statements received from external organisations ..................................... 111 -112 Acknowledgements.............................................................................................. 113 How to provide feedback .................................................................................... 113 Glossary................................................................................................................. 114 Membership form......................................................................................... 115 -116 Section 1 • Statement of quality from Chief Executive • Directors’ declaration • Statement from the Chairman • Putting quality first • About our services • Our values • Where our service are provided • Community Foundation Trust application update • Accolades for our Trust and staff during 2012-13 1 Statement of quality from Chief Executive Quality Accounts continue to represent an important part of the overall quality improvement landscape of the NHS. The Health Act 2009 creates the duty for all providers of NHS services to produce an annual Quality Account providing the public with clear information about the quality and safety of our organisation. The primary purpose of the NHS and everyone working within it is to provide a high quality service, free at the point of delivery to everyone who needs it. Care provision and the experience patients have of the care they receive is central to all that we do. This report summarises our progress against our priorities for the year; what we did and why; where we are now; and our on-going commitment to continue to improve the quality and responsiveness of our services. ‘Quality’ is much more than a word or a set of action plans, it is about the day-to-day excellent care which is delivered by our dedicated clinicians and their teams. As a newly developed organisation following the Transforming Community Services Programme during 2010/11, we as a Trust Board have been impressed throughout the year by the continuous commitment of staff to providing high quality care to patients on a daily basis and the pride they take in doing the very best for each and every person they meet. 2 This commitment will continue to be fundamental as we move forward to realise our aspiration of becoming an NHS Foundation Trust. This report provides examples from across our services which reflect the quality care that is being delivered and has been developed over the past year. Just as importantly, we have also recognised the areas where further focus is required to support and drive improvement over the coming years. We continually reflect on the recommendations from external reports such as the first Francis Report into the Mid Staffordshire NHS Foundation Trust Public Enquiry in 2009 where a series of actions were undertaken. We also have moved swiftly in responding to the Francis Report this year and reviewed the recommendations and key points with our Board and through our governance structures to take forward. Our organisation’s stated aim is to deliver quality improvements “with, for, and in the community” and I welcome the chance to share with you the achievements and challenges this year has brought. The organisation is very conscious of the financial restraints that the NHS will face over the coming years and the importance of safeguarding quality of care. The essence of how we will deal with this is through service transformation and service redesign. Meeting this challenge - the Quality Innovation Productivity and Prevention (QIPP) challenge - is about achieving the highest possible value from the resources allocated to the NHS. Our focus is on maintaining and improving quality whilst reducing cost by increasing productivity. We have focussed on a number of quality and safety priorities and we have developed an Integrated Business Plan (IBP) to ensure we are well placed to deliver those key initiatives. The actions taken and resulting outcomes are described in the Quality Account. We are keen to make it easy for patients and members of the public to see information about quality and safety. During 2012/13 the Trust has provided monthly information on quality and performance as part of the Board reports. These reports are available on the Birmingham Community Healthcare NHS Trust website www.bhamcommunity.nhs.uk These reports include information such as our response to complaints, patient satisfaction survey results and various other measures covering each of the three domains of quality - patient safety, clinical effectiveness and patient experience. Our Quality Account outlines our commitment to continual improvement in service provision and to be transparent and accountable to patients, the public, Commissioners, partners and other stakeholders. Our intention is to make this document as informative as possible, and we welcome receiving your feedback, which will assist us in improving the content and format of future Quality Accounts. On behalf of the Trust Board, I can confirm that to the best of my knowledge and belief the information contained in the Quality Accounts is accurate and represents our performance in 2012-13 and our commitment to quality improvement. Tracy Taylor, Chief Executive, Birmingham Community Healthcare NHS Trust 3 Statement from the Chairman I am proud to say that quality remains at the heart of what we do and remains a significant focus of the Board. The challenge for healthcare providers continues to be to build high quality service delivery systems and structures at a time of austerity. But, healthcare is a peopleoriented service, therefore we must strive to ensure that our systems and structures are robust and fair to all, yet with the flexibility to adapt and respond to individual need. This Quality Account is an opportunity to showcase the excellent work of BCHC staff as we continue to develop and improve our services across the city and to embed policies and practices that make patient experience the key driver of care. Understanding the healthcare needs of all the communities we serve will be the key to getting decisions right as we move forward. As we progress towards Foundation Trust status, I am encouraged by the on-going work around building a strong public membership which is truly representative of those communities and the recruitment of our governors. Making sure the views and needs of our members are reflected in the way we provide services will be a central part of our continuous improvement efforts. I hope you find the Quality Account interesting and informative. If you would like to comment on any part of it, details of how you can do that are included at the back of the document. We would be delighted to hear from you. Tom Storrow, Chair, Birmingham Community Healthcare NHS Trust Directors’ Statement of Responsibilities: Our Board is ultimately responsible for the delivery and quality of services delivered throughout the organisation. It is therefore also responsible for the accuracy of information that is presented within our Quality Account. Directors declaration: We can confirm that to the best of our knowledge and belief the information contained in the Quality Accounts is accurate and represents our performance in 2012-13 and our commitment to quality improvement. Shokat Akbar, Commercial and Marketing Director Rick Roberts, Medical Director (Has subsequently retired as of 31.03.2013) Peter Axon, Finance Director Tom Storrow, Chairman Andy Harrison, Chief Operating Officer Joanne Thurston, Director of Compliance and Assurance Beverly Ingram, Director of Nursing and Therapies 4 Tracy Taylor, Chief Executive Putting quality first BCHC provides a combination of specialist and local healthcare services, delivered on a locality basis, citywide and regionally in a wide variety of settings including community hospitals, intermediate care centres, outpatient facilities and in people’s homes. We strive to deliver high quality local services while recognising that patients travel from across the wider West Midlands region to receive highly specialised services. Our clinical strategy, approved by our Board, places the individual at the centre of service delivery, supporting our vision of accessible and responsive, patient-focussed healthcare for people in all the communities we serve, throughout their lifetimes. BCHC recognises its responsibility to ensure that all the services it provides are safe, of high quality and that the patient has a positive experience when receiving care in any setting. As part of our on-going commitment to quality, the Trust Board has in place a number of mechanisms by which they ensure quality is measured, monitored and improved. Examples of board level assurance • the Board monitors indicators of essential care, which demonstrates ‘ward to board’ quality of care provision • the Trust Board has agreed quality metrics in addition to the national targets that are in place. In the event of deviation, a full narrative is given in the Quality Report, and where necessary the Quality Governance and Risk Committee discusses issues/receives further information to assure the Trust Board that appropriate action is being taken or monitors any resultant action plans • the essential care indicators contained within the Board Quality Report are cascaded down to divisional and ward level and all staff are involved in the review of performance against the quality goals • the Trust Board receives a monthly Quality Report and Performance Report which contain both national and local quality metrics, whereby the Trust Board approves the key performance indicators (KPIs) and essential care indicators at the start of each year in order to monitor quality and achieve its annual objectives • there is an assessment of the impact on quality, innovation and productivity of all strategic intentions and cost improvement programmes • the Trust actively involves patients and service users in the formulation of strategy and service developments to identify quality implications • quarterly Care Quality Commission (CQC) assessments are undertaken to review and ensure on-going compliance and consider risks to compliance • all Board members engage in regular Patient Safety Walkabouts, at which they meet and engage with staff, patients and service users and are able to derive an understanding of issues that are affecting staff on the frontline. 5 The Board receives comprehensive and detailed information providing Directors with a clear picture of progress against our quality goals and demonstrates where we need to improve to ensure we can reach the high standards we set for our organisation. Clinical quality is the cornerstone of the Board’s strategic vision and I am delighted our Quality Account portrays that vision with such clarity. John Craggs, Non-Executive Director for Quality Patient safety visits The patient safety visits or patient safety walkabouts have been a feature of the organisation for a number of years. They are a proactive way of ensuring discussion between Trust Board Executive and Non Executive Directors and frontline staff. They provide a great opportunity to have a meaningful and structured dialogue and they enhance the specific focus on patient safety and patient experience. The key aims are to: • demonstrate top level commitment to patient safety and clinical engagement • provide a further line of communication about patient safety among our staff, executives, and managers • provide opportunities for senior executives to learn about patient safety and experiences of frontline teams • encourage a culture of reporting of clinical issues, errors and near misses • establish and support local solutions to minimise risk • share good practice and innovations. The patient safety visits take place twice per month and are based around The National Patient Safety First campaign methodology. Patient safety walkabouts ensure that executives are informed first hand regarding the safety concerns of frontline staff and that they visibly demonstrate this commitment in listening to and supporting staff when issues are raised. An annual programme is drawn up every year and a record of the visit takes place with any actions noted and followed up. Any areas of good practice or significant concerns are reflected in the Quality Report which is presented to quality governance and risk committee. 6 Board priorities During 2012-13 the Trust Board’s clinical priorities were: • implementation of Safety Express • nutrition and hydration • improving the quality of our health visiting services • improving the quality of referrals to our services at Birmingham Dental Hospital • Combined Community Dental Services - membership of Quality in Dental Services Scheme (a scheme which supports measuring quality). As an organisation, when reviewing and selecting the clinical priorities for 2013-14, the organisation has reflected on: Beverly Ingram, Director of Nursing and Therapies • the consultation undertaken with key stakeholders; • our past performance against quality indicators; and • local and national priorities. Though significant progress has been made across the clinical priorities selected for 2012-13, we have decided to carry forward these for 2013-14 and build on the work and initiatives implemented across the organisation. These are linked and support our quality goals detailed in our three year forward plan. In addition, we have also included a patient experience related clinical priority, this being a priority scored highly following the consultation with key stakeholders. Our clinical priorities for 2013-14 are as follows: Patient safety (supports NHS Outcome domain 5: Treating and caring for people in a safe environment; and protecting them from avoidable harm) 1. implementation of Safety Express Clinical effectiveness (supports NHS Outcome domain 2: Enhancing quality of life for people with long-term conditions and NHS Outcome domain 4: Ensuring that people have a positive experience of care) 2. Health Visitor Implementation Plan 3.dementia Patient experience (supports NHS Outcome domain 4: Ensuring that people have a positive experience of care) 4. family and friends test (net promoter) Further details around each of the clinical priorities can be found on pages 15 to 21. Progress against these priorities will be provided in next year’s Quality Account for 2013-14. 7 Response to the second Francis Inquiry report The second report prepared by Robert Francis QC into the failings at Mid Staffordshire NHS Foundation Trust between 2005 and 2008 following the Public Inquiry was published on 6 February, 2013. The second Francis report considers the operation of the commissioning, supervisory and regulatory organisations, and other agencies involved, to examine why the problems at the Trust were not identified sooner and appropriate action taken. The inquiry and subsequent report has identified numerous warning signs which could, and should have alerted the ‘system’ as a whole to the developing problems. The Francis report is a very lengthy document, and the Trust has put in place actions to consider its implications and determine how to effectively implement the recommendations. We have noted that the recommendations are both direct and indirect in that many relate to changes to the NHS commissioning and regulatory framework which are outside of the control of the Trust. The following actions were taken as immediate steps: 1. A full gap analysis of the 290 recommendations in the report was undertaken to establish the actions that the Trust is required to take and to identify lead officers and committees. This was presented to the Trust Board in March and will be monitored at Quality Governance and Risk Committee. 2. Development of an information and presentation pack on the findings and recommendations of the report for use across the Trust at team and divisional level 3. A Clinical Leads meeting was held to review the findings and recommendations, to outline the internal and external professional network, and to identify how best to ensure pace and rigour to implementation. 4. A programme of staff focus groups was held to discuss the findings and implications of the report, and to give a further opportunity for staff to raise any concerns or suggestions of ways to further improve care and safety for patients. 5. A review of the template for the Patient Safety Executive Visit Programme was carried out to align the key lines of enquiry with the findings and recommendations from the report. 6. A dedicated Board development session was held to review the findings and recommendations and align to our strategies. The NHS identifies three fundamental elements of quality care: Patient safety patients are safe and free from harm. PATIENTsafety CLINICAL effectiveness PATIENTexperience 8 Clinical effectiveness the treatment and care we deliver is the best available. Patient experience service users have a positive experience that meets or exceeds their expectations. About our services Birmingham Community Healthcare (BCHC) NHS Trust provides high quality accessible and responsive community and specialist NHS services across Birmingham and the West Midlands and employs 5,157 staff (as at March 2013). We deliver community-based healthcare to people of all ages across Birmingham, covering a population of approximately 1 million people and a geographical area of 103 square miles. These services are delivered in a variety of settings including people’s homes, primary care premises and community inpatient facilities. We also deliver a range of specialist services for a population of approximately 5 million people in the wider West Midlands region, including Warwickshire, Staffordshire, Worcestershire, Shropshire and Herefordshire. These services include Specialist Rehabilitation and a purposebuilt teaching Dental Hospital that provides undergraduate teaching and postgraduate dental training, secondary and tertiary specialist dental care. More than 100 different healthcare services are provided by the organisation. Each year the organisation’s staff engage in more than two million contacts with patients and other service users. BCHC comprises three clinical divisions providing services to patients: 1. The Children and Families Division brings together all the specialist community services for children and young people across Birmingham and offers a co-ordinated approach for child healthcare, as well as delivering the universal children’s services of health visiting, mainstream school nursing and the paediatric eye-screening service. 2. The Adults and Community Division provides a range of services for the local communities within Birmingham including community-based urgent care and hospital admission avoidance, district nursing, community podiatry and physiotherapy to specialist services for older people. The division also operates two community hospitals, enhanced recovery centres and a palliative care facility. 3. The Specialist Division comprises: • Birmingham Dental Hospital (BDH), in partnership with the University of Birmingham School of Dentistry, provides a range of dental services for people in the West Midlands, training and development of the dental workforce and an extensive research programme • Combined Community Dental Services provides a range of specialist dental services across Birmingham, Dudley, Sandwell and Walsall • Specialist Rehabilitation Services provides a range of services across the West Midlands for adults with long- term neurological conditions and children and adults with limb amputations • Learning Disability Services provides specialist health services for people with learning disabilities across the city of Birmingham. The clinical services are supported by a range of corporate functions, such as human resources, finance, performance, governance and risk management. A dedicated patient experience team liaises with service users and their representatives. 9 Our values 10 Accessible We will provide a range of services that reach out into the community and meet individual need where everyone counts; celebrating diversity and valuing difference. Responsive We will listen and work with our service users and partners to meet needs and improve health and well being. We will encourage innovation and excellence, celebrating success and learn from experiences. Quality We will provide safe effective personalised care to the highest standard, providing information to support service users and their carers to make informed choices. Caring We will deliver our services with respect, compassion and understanding where people are valued and we will act in their best interest. Ethical Promoting a culture of dignity and respect we will make morally sound, fair and honest decisions and be openly accountable. We will commit to investing wisely whilst being socially and environmentally responsible. Commitment Through our actions and commitment we will strive to make a positive difference to people’s lives. We will value our staff, the commitment and contributions they make. Where our services are provided Staffordshire Shropshire East and North Birmingham Worcestershire Warwickshire Herefordshire Central and West Birmingham South Birmingham Key Service Coverage Population Community Services for children and adults and Specialist Services for people with learning disabilities Birmingham 1.1 million Community Dental Services Specialist Rehabilitation Services and Birmingham Dental Hospital Birmingham, Sandwell, Dudley 2 million and Walsall West Midlands 5.5 million 11 Foundation Trust - application update The Trust continued to make significant progress in its journey towards becoming a Foundation Trust during 2012/13 across a number of work streams and is in the final phase of assessment at the time of writing. The Trust has successfully completed the first phase of assessment, an assessment of readiness undertaken by the Strategic Health Authority, early in 2012. This included a review of the arrangements we have in place to manage our patient and service quality and safety arrangements. An assessment of our financial management arrangements also took place at around that time and we commenced the second phase of assessment in May 2012. This phase of the assessment was undertaken by the Department of Health. Our application was reviewed by the Department of Health’s Applications and Technical Committees. A recommendation was then made by the Department of Health to the Secretary of State for Health to progress our Foundation Trust application to the third and final phase. We received Secretary of State approval in October 2012 when we made formal application to the health sector regulator, Monitor. Following submission of key strategic documents to Monitor, the third and final phase of our formal assessment commenced in earnest in December 2012. Our application is now undergoing a thorough and forensic review in order to satisfy the regulator of the following: • financial planning and management arrangements and forecasts are robust • quality governance arrangements, including patient safety and quality are sound and provided to the satisfaction of our service users, Commissioners and the public • capacity and capability of the Trust and its managers are sufficient to deliver against its plans • the Trust is legally constituted and will continue to be well governed into the future. An active programme has run alongside the assessment process to develop a representative membership of the Trust and a Council of Governors; ensuring that the patients, service users and key partners have a strong voice and that the Trust is held to account for the services that it delivers. We exceeded our target to recruit 10,000 public members and had achieved a membership of 11,000 by October 2012. We also have over 5,000 staff members. Level 2 and Level 3 members have already been involved in the Quality Account consultation process for year 2013/14 in order to provide feedback and help to establish the quality priorities for the forthcoming year. We conducted an independent and formal election process to elect our Council of Governors over the winter period 2012. This resulted in our Council of Governors being fully elected at the end of January 2013 and we look forward to working closely with them. The Trust expects to receive authorisation to become a licensed Foundation Trust early in the financial year 2013/14. 12 Accolades for our Trust and staff during 2012-13 Trust shortlisted for HSJ ‘provider of the year’ The Trust’s innovative work to transform access to urgent and non-urgent citywide community services for adults was highly commended in the ‘primary care and community service redesign’ category at the HSJ Awards. Chief Executive Tracy Taylor said: ‘Being shortlisted for ‘provider of the year’ is a great achievement and testimony to the dedication of our staff to deliver consistently high quality services.’ The recognition from the healthcare industry’s most prestigious annual prize-giving followed earlier endorsement in the HSJ Efficiency Awards of the biggest service redesign of its kind in the country. The Trust was among the six finalists who narrowly missed out on the coveted title ‘HSJ provider of the year’. A right Royal honour Mary Partridge, lead nurse for safeguarding adults, has received the prestigious title of Queen’s Nurse. Director of nursing and therapies Beverly Ingram said: “Mary is unstinting in her dedication to safeguarding vulnerable adults and improving patient care. “She is a well respected team leader, appreciated by all of her colleagues and certainly deserves the award.” The title of Queen’s Nurse is given to individuals in recognition of commitment to patient-centred values and practice improvement. Locally, they lead improvement projects while nationally, bodies including the Department of Health, the National Patient Safety Agency and the National Institute for Health and Clinical Excellence have drawn upon their expertise in community nursing. Proud partner BCHC was among the winning team at Birmingham City Council’s annual Chamberlain Awards. The multi-agency Birmingham Safeguarding Adults Board’s campaign to raise awareness of adult abuse received an award in recognition of outstanding partnership work between the local authority, NHS organisations, police and other public agencies. 13 Section 2 • Our priorities for clinical improvement in 2013-14 • Review of performance - clinical priorities update 2012- 13 • Commissioning for Quality and Innovation (CQUINs) 2012-13 • Quality performance data - statutory content 14 Our priorities for clinical improvement in 2013-14 Clinical priorities for 2013-14 The trust agreed to consult widely on our clinical priorities for 2013-14 with our stakeholders, including staff, commissioners, and the public. Consultation took place from December through to the end of January 2013. The consultation allowed feedback to be sent via a number of options, these being an online survey, by completing and returning the paper consultation form via freepost address, or where appropriate through discussion forums. Stakeholders were asked to select up to five priorities and given the opportunity to suggest priorities not appearing on the proposed list. The list covered priorities across the three domains of quality. Stakeholders were also given the opportunity to suggest any measures against their chosen list and leave any additional comments. We have had a great response this year where we had over 400 responses of which 60 per cent were from staff and 40 per cent were from the public or external to the organisation. Information was collated and analysed from the consultation and reflected upon as well as our past performance against quality indicators and reflecting on local and national priorities. Suggested proposals were then taken to and discussed through a number of our executive led committees and the Board for further discussion and agreement. Consideration was also given to carry forward any priorities from the previous year. Reflecting on the feedback received, the following five priorities scored highly: • patient experience • best practice in infection control • fundamentals of care • developing intelligent information technology / data systems to support the delivery of healthcare • effective pain management. The majority of these areas have been covered through the clinical priorities chosen for 2013-14 or have been included in our quality goals within the three year forward plan. Details around the priorities can be found in the following pages and the progress and achievements which support these priorities will be included in the Quality Account for 2013-14. 15 Patient safety 1. Implementation of Safety Express Rationale: We want to continue to strive towards our ambition of HarmFREE Care through continuing to use the NHS Safety Thermometer with other sources of patient safety information and Safety Express. This will include goals towards delivery of HarmFREE Care from pressure ulcers, falls, urinary catheter infections, and blood clots using the three primary drivers; leadership and safety culture, clinical care 95 per cent reliable and supporting infrastructure to influence the secondary drivers; nutrition and hydration, care rounds, risk assessments and management, equipment, medicines management and continence. Baseline, goals and measures: (see following tables) Criterion: baseline Using the NHS Safety Thermometer to measure harms at the point of care and use the information together with other patient safety metrics to measure and monitor improvement goals for the four harms: • pressure ulcers • falls • catheter associated urinary tract infections • blood clots • proportion of patients that are ‘harm free’ Specialist Complete the NHS Safety Thermometer for 100 per cent of patients on the neuro rehabilitation ward every month for the four harms and make Rehabilitation improvements against the baseline established during 2012-13 for the four harms and the composite measure for HarmFREE Care. Services Review the NHS Safety Thermometer results with incident reporting for falls and pressure ulcers, and serious incident root cause analysis findings to measure and monitor improvement goals. Use the trigger tool review of case notes adverse event rate as a measure for improvement with NHS Safety Thermometer data and incident data. Adults and Community Division Learning Disability Services 16 Complete the NHS Safety Thermometer for 100 per cent of patients every month for the four harms and make improvements against the baseline established during 2012-13 for the four harms and the composite measure for HarmFREE Care. This should apply equally for every person seen - as an inpatient, by a community nursing team, in the inpatient prison ward, by the rapid response team or as part of complex care delivery. Review the NHS Safety Thermometer results with incident reporting for falls and pressure ulcers, and serious incident root cause analysis findings to measure and monitor improvement goals. Start to use trigger tool to review case notes and establish an adverse event rate. Complete the ST on 100 per cent of patients on three new harms: violence and aggression, medication errors and self-harm as part of the pilot national tool to establish a baseline and complete the ST for the four harms every month for patients over 65 and monitor improvements against the baseline. Review the ST results and triangulate with incident reporting on self harm, violence and aggression and falls. Criterion: goal - where do we want to be? Continue with Safety Express plan to progress towards delivery of HarmFREE Care from pressure ulcers, falls, urinary catheter infections, and blood clots using the three primary drivers; leadership and safety culture, clinical care 95 per cent reliable and supporting infrastructure to influence the secondary drivers; nutrition and hydration, care rounds, risk assessments and management, equipment, medicines management and continence. The clinical teams will use patient safety information to track improvements over time and aim to eliminate ‘preventable harm’. Specialist • survey 100 per cent of relevant patients on the specified day • achieve the CQUIN and meet the agreed composite target for HarmFREE Rehabilitation Care and sustain it to 31 March 2014 • achieve the CQUIN for a reduction in avoidable community acquired pressure ulcers and zero avoidable hospital acquired pressure ulcers • from the baseline NHS Safety Thermometer data achieve a 50 per cent reduction in catheter acquired urinary tract infections • from the baseline data achieve a 50 per cent reduction in avoidable venous thromboembolism (VTE) events • 95 per cent of patients admitted to ward/unit have a documented VTE risk assessment • from the inpatient incident data and bed occupancy data achieve a 10 per cent reduction in falls • achieve 95 per cent in essential care indicators to ensure clinical care is reliable to deliver the outcomes for the four harms • use the patient safety dashboards, NHS Safety Thermometer outcome data and Gel Solutions to measure and monitor improvement. Adults and Community Division Learning Disability Services • survey 100 per cent of relevant patients on the specified day • achieve the CQUIN and meet the agreed composite target for HarmFREE Care and sustain it to 31 March 2014 • achieve the CQUIN for a reduction in avoidable community acquired pressure ulcers and zero avoidable hospital acquired pressure ulcers • from the baseline NHS Safety Thermometer data achieve a 50 per cent reduction in catheter acquired urinary tract infections • from the baseline data achieve a 50 per cent reduction in avoidable VTE events • 95 per cent of patients admitted to ward/unit have a documented VTE risk assessment • from the inpatient incident data and bed occupancy data achieve a 10 per cent reduction in falls • achieve 95 per cent in essential care indicators to ensure clinical care is reliable to deliver the outcomes for the four harms • use the patient safety dashboards, NHS Safety Thermometer outcome data and Gel Solutions to measure and monitor improvement. • survey 100 per cent of relevant patients on the specified day • achieve the CQUIN and meet the agreed composite target for HarmFREE Care and sustain it to 31 March 2014 • achieve the CQUIN for a reduction in avoidable community acquired pressure ulcers and zero avoidable hospital acquired pressure ulcers • undertake VTE risk assessment on all inpatient admissions • survey 100 per cent of relevant patients for three new harms using the national tool (pilot) • triangulate with incident data • use Gel Solutions • complete audit programme. 17 Criterion: monitoring and reporting Safety Express is a key objective in the patient safety plan and is monitored in the integrated quality report fro the Quality Governance and Risk Committee. The quality report includes progress against the safety objectives, the NHS Safety Thermometer outcomes report on the four harms and the patient safety dashboard. The clinical governance committee receives the patient safety report. In addition groups that monitor the Safety Express plan are: Safety Express, falls and pressure ulcer reference groups and fundamentals of care. Specialist Rehabilitation Progress to be included in the business units monthly reports and the Rehabilitation Governance Committee. Use the dashboards, the NHS Safety Thermometer outcomes report and Gel Solutions benchmarking tool to monitor and report progress. Clinical teams to use the data to help them introduce, track changes and make improvements. Adults and Community Division Progress to be included in the inpatient and community services clinical effectives committees. Use the internal quality/assurance reviews to monitor progress. Use the dashboards, the NHS Safety Thermometer outcomes report and Gel Solutions benchmarking tool to monitor and report progress. Clinical teams to use the data to help them introduce, track changes and make improvements. Learning Disability Services Progress to be reported at the two clinical business units and then at the • Learning Disability Clinical Effectiveness Group • Learning Disability Clinical Safety Group • Divisional Governance Committee Use the dashboards, the NHS Safety Thermometer outcomes report and Gel Solutions benchmarking tool to monitor and report progress. Clinical teams to use the data to help them introduce, track changes and make improvements. Criterion: responsible lead Director of Nursing Associate Director of Therapies Head of Clinical Governance Patient Safety Lead Clinical specialists Specialist Clinical Director and Director Associate Directors/Service Heads Rehabilitation Ward Manager Governance Lead Adults and Division Clinical Director and Director Associate Directors/Service Heads Matrons Governance Lead Learning Disability Services Clinical Director and Director Associate Directors/Service Heads Governance Lead Community 18 Criterion: how the goal will be achieved As part of the patient safety plan, Safety Express improvements will be tracked over time. The drivers are: leadership and safety culture, clinical care 95 per cent reliable and supporting infrastructure and will be achieved through the secondary interventions: nutrition and hydration, care rounds, risk assessments and management, equipment, medicines and continence management. The clinical teams, committed to delivering care free from harm, will continue building on the achievements of 2012-13 integrating Safety Express within existing workflows and routines. Rehabilitation Part of the Rehabilitation Services quality and patient safety plan to support Safety Express: Services • completion of NHS Safety Thermometer at point of care • trigger tool case note review • embed care rounds and care bundles used for pressure ulcer prevention and falls reduction, catheter care and venous thromboembolism (VTE) • nutrition and hydration, equipment and environment management • medication reviews • learning from incidents • essential steps for catheter care to audit compliance catheter care passport • training and competency • essential care indicators and use of dashboards to monitor improvements. Through the divisional clinical effectiveness workstream: Adults and • completion of safety thermometer at point of care Community • trigger tool case note review • embed care rounds and care bundles used for pressure ulcer prevention Division and falls reduction, catheter care and VTE • link dementia and falls pathways • nutrition and hydration • improved access to equipment • medication reviews • learning from incidents • essential steps for catheter care to audit compliance • catheter care passport • training and competency • safety crosses to monitor the harms and using electronic dashboard to benchmark data • partnership work with other care providers. The work will form part of the Learning Disabilities clinical effectiveness Learning and clinical safety work programme: Disability • completion of NHS Safety Thermometer • continue to work with the national team on the three new harms, Services pertinent to service needs • falls reduction and use of prevention plans • VTE risk assessments • nutrition and hydration • medicines management • learning from incidents • ligature points audit • suicide and self harm audit • triangulating incident data with NHS Safety Thermometer data • essential care indicators and use of dashboards to monitor improvements. 19 Clinical effectiveness 2. Health Visitor Implementation Plan Rationale: We will continue working towards achieving the health visitor implementation plan (DH, 2010) which sets out the ambitious vision of increasing health visitor numbers by 4,200 by April 2015 providing a significant opportunity to improve health visiting services in Birmingham for future generations. We also recognise that training in the use of the family common assessment framework underpins a multi-agency team around the family approach based on holistic assessment using paperwork that is consistent across agencies. Participation in the common assessment framework plan is a way to demonstrate implementation of learning from the training. Increasing the number of common assessment frameworks participated in or initiated demonstrates an improvement in multi agency working (CQUIN). Criterion: Children and Families Division Goal: a. ensuring that we deliver the required number of training places for the increased number of health visitor students b. common assessment framework training (CQUIN): • Identification of the per cent of Mainstream School Nurses, Community Staff Nurses and Qualified Health Visitors who have evidence of having completed training in the Common Assessment or Family Common Assessment Framework (CAFS) • 200 CAFS to be initiated between the HV, FNP the specialist services within the Children and Families Division. Measures: a. • continue to recruit to the numbers of health visiting students • proactively recruit student health visitors into permanent posts • continue work with the Higher Education Institution (HEI) to further develop and improve the training experience of the health visiting students b. 85 per cent (170) community staff nurses and qualified health visitors and FNP nurses have provided evidence of having undertaken training in the common Assessment or Family Common Assessment Framework, 200 CAFS to be initiated between the HV, FNP and the specialist services within the Children and Families Division. 20 3. Dementia (CQUIN) Rationale: a. to identify and investigate new patients with dementia, inform GP of the outcome of the screening process and support patient and carers by signposting to community services b. training of all identified relevant clinical staff both inpatient and community to improve management of patients and support for carers c. ensuring carers feel supported and have a positive experience. Criterion: Adults and Community Division and Specialist Services Division Goal: a. •patients age 75 and over who are screened using the agreed screening tool following admission to hospital •discharge summaries include results of screening test / full dementia blood test results, working diagnosis and signposting information for carers •discharge letter sent out within 48 hours. b. •training of all identified relevant clinical staff both inpatient and community to improve management of patients and support for carers •development of resources for patients and carers to improve signposting to community services c. ensuring carers feel supported and have a positive experience monthly audit of carers of people with dementia to test whether they feel supported and reported the results to the Board. Measures: a. quarterly audit identifying minimum of: •90 per cent patients age 75 and over screened for dementia using agreed screening tool •90 per cent of patients’ GPs informed of outcome of screening process with discharge summaries containing a minimum of screening and blood test results •results of additional question regarding the discharge letter being sent out within 48 hours of discharge b. •identify all relevant staff requiring access to relevant dementia training programme based on a training needs analysis •implementation of training programme and 90 per cent of relevant staff have completed •resources developed for patients and carers to improve signposting to relevant service. c. annual audit report detailing results and identifying areas for improvement and has been reported to the Trust Board. 21 Patient experience 4. Family and friends test (FFT) (CQUIN) Rationale: It is important that we listen and seek the views from service users to support continuous monitoring and to improve the quality of our services. The Mid Staffordshire Public Inquiry reviewed the poor standards of care patients and their families received. The FFT (also known as the net promoter score) was shortly introduced after the Mid Staffordshire Public Inquiry Report in 2013 was published. This method provides another communication channel to service users to express their opinion around the care and service they experienced from a healthcare organisation. This supports provider organisations and commissioners to obtain an insight to the service users experience and use this data to identify issues and help make the necessary improvements, supporting some of the recommendations within the Public Inquiry report. Criterion: Across all divisions within the Trust Goal: a. improved performance on the staff friends and family test where there is a larger sample size (2,000 staff) than the national staff survey and is therefore more statistically significant b. improvements are implemented in the identified areas across the organisation in line with findings from the FFT c. devise methodology by end of quarter 1 to implement FFT with the most vulnerable patients within their care and then demonstrate an improved response rate by end of quarter four d. devise alternative method for service areas where the FFT would not be appropriate to use. Measures: a. to produce a comprehensive action plan detailing the staff survey results during quarter one, broken down by directorate and milestones for actions to be completed - improved score in the annual staff survey b. report compiled outlining actions implemented in response to findings from the FFT data with action plan submitted in quarter two c. methodology developed for all patients to be asked FFT to include all patients who may have been previously excluded i.e. dementia, learning disability, frailty. Implement FFT for all patients and demonstrate an increase in the response rate for FFT across all inpatient units d. alternative methods developed and trialled where identified. 22 Review of performance - clinical priorities update 2012-13 Implementation of Safety Express Implementation of Safety Express through the work of the clinical teams, within the Adults and Community Division, Rehabilitation Services and Learning Disability Services has been a priority during 2012-13 for improving clinical quality. Progress towards achieving HarmFREE Care (absence of all four harms) for pressure ulcers (also known as pressure sores), falls, urinary tract infections in patients with catheters and blood clots (deep vein thrombosis and pulmonary embolism) has been as a result of three primary drivers; leadership and safety culture, clinical care 95 per cent reliable and supporting infrastructure. These have influenced the secondary drivers (interventions) of the Safety Express plan. Safety Express has enabled the Trust to work together effectively to review the four harms in one forum with the frontline clinicians, matrons, clinical specialists and executives offering practical solutions to delivering HarmFREE Care. The Safety Express Group is supported by reference groups, set up to steer the workstreams. There have been a number of examples of achievements this year. Trust achievements during 2012 -13 and continuing priorities for sustaining improvements during 2013-14 • Think SSKIN (pressure ulcer prevention care bundle) resources have been used by clinical teams to involve patients and carers in preventative care • in the inpatient areas, implementing care rounds provides staff with regular patient contact. Patients are kept better informed, have confidence that staff will be seeing them on a regular basis, making sure needs are met and preventing harms from occurring • tools for assessing patient risks, planning care using care bundles, investigating incidents with bespoke root cause analysis tools and improve learning, for falls, pressure ulcers (SSKIN),and venous thromboembolism have been standardised • Infection Prevention and Control are using Essential Steps for catheter care to audit compliance with standards and the continence team has developed a catheter care passport to minimise harm from catheter associated urinary tract infections • feedback to teams is often identified to be a concern and during this year a monthly patient safety bulletin has been established providing clinical teams with patient safety information on the four harms and medication topics. Safety Express notice boards include the latest information helping to keep staff and patients appraised on the latest bulletin • safety crosses are being used by staff in the inpatient and community teams to monitor the harms, aiming to keep track and make sure action is taken • an electronic dashboard has been developed and accessible via the intranet to enable teams to benchmark their data and to understand their patient safety profile, their hot spots and areas for improvement. When BCHC staff visit patients in their own homes, they link in with primary care and social care to ensure that patients receive HarmFREE Care. This has been evident when nursing staff are preventing pressure ulcers. A key priority for 2013-14 is to work more closely with partners in primary care and social care to make sure that patients are harm free whatever the care setting. 23 Trust achievements during 2012 -13 and continuing priorities for sustaining improvements during 2013-14 continued... • integrating processes, training and multidisciplinary work has been a real focus. Pharmacy is leading on developing a medication risk screening tool and the dietetic team promoting nutrition and hydration to prevent the four harms. All are working together with falls, tissue viability, continence, infection prevention and control and the education lead have been working together on a HarmFREE Care training pack • improvements made to the prompt access to equipment, with teams having equipment that meets their needs for pressure ulcer prevention and falls, e.g. heel protectors, mirrors to check heel redness, cushions, mattresses, hi-low beds, slippers • embedding the NHS Safety Thermometer has helped staff to review HarmFREE Care from the patient’s perspective and at the same time collect information on a dedicated day every month to understand their own safety achievements and areas needing action. At the same time it provides the Trust with information to measure and benchmark improvement. Measurement for improvement We measure harm using incident reporting, routine administrative data, case note reviews using trigger tools and point of care audits using the NHS Safety Thermometer. These different sources of information are used to help staff understand how we can make improvements to our systems. The NHS Safety Thermometer has been a national CQUIN for 2012-13 with organisations collecting baseline data on the four harms to incentivise the achievement of improvement goals. The Trust has used the NHS Safety Thermometer to collect a rich source of patient safety information across all healthcare settings, including those that are often hard to reach. The Trust has achieved the CQUIN during 2012/13 with 100 per cent of relevant patients surveyed every month since 1 April, 2012 which equates to a census of around 2,300 patients every month. Patients are surveyed as inpatients, in the community setting, in the prison setting, within the Learning Disability Services and the Children’s Service, providing a rich source of patient safety information. Measuring harm from the patients perspective helps staff to understand and implement solutions to improve clinical care. As well as keeping track on these four harms (for patients over 65), the Learning Disability Services measure an additional three; violence and aggression (patients) medication errors and self harm by their participation in a regional pilot. The Children and Families Division has also participated in a pilot with Birmingham Children’s Hospital to consider harms more pertinent to them, collecting data ‘at point of care’. They will use this information during 2013-14 to track harms. 24 The graph shows the proportion of patients that have received HarmFREE Care across the Trust using the NHS Safety Thermometer tool. There has been a steady improvement with a year end position of 94.85 per cent HarmFREE Care. The focus for 2013-14 is to continue to make improvements. Moving forwards for 2013-14 • partnership work with primary care and care agencies, GP practices and social care on the harm reduction programme to improve clinical care whatever the setting • making sure that staff training needs meet competency (especially relevant to link dementia pathway and falls pathway • building on ‘trust me to care’ and improving care rounds • front line staff and matrons to review the various risk assessments and to see whether a single risk assessment is practicable to streamline documentation • assist individual teams to ensure accuracy of NHS Safety Thermometer data and help teams to use it to support and evidence their improvement work • develop further the benchmark report to look at community hospitals and community nursing teams’ comparative data. Work with the services to facilitate local benchmarking • use the data analysis work of the national team to ensure that we are targeting the improvement work in the correct areas. Pareto charts can be used to target activity • work with the specialist leads to explain and explore what the patient safety information is telling us, especially in the areas where we have limited patient safety data, such as catheter care, urinary tract infections, blood clots • nutrition and dietetic leads to develop resource material for staff and patients to be clear about food and drink requirements • building on the work of medicines management on prescribing for the four harms, taking into account the complex needs of patients and engaging with doctors • progressing with Learning Disability Services and the Children and Families Division on tracking their harms. Julie Jones, Patient Safety Lead says: Treatment plans for patients are used to assess and manage patients care on a day to day basis to deliver HarmFREE Care. Patients ‘Trust us to care’ and want to be free from all harms, the pain of a pressure ulcer, harm from a fall, an unnecessary urinary tract infection and a blood clot. We will continue to use the NHS Safety Thermometer with other sources of patient safety information and Safety Express will continue to be a clinical priority for 2013-14 as we strive towards our ambition of HarmFREE Care. We will sustain the improvement made during 2012-13 and build on them for 2013-14. 25 Nutrition and hydration Achievement by March 2013 We have continued to roll out, implement and develop the essential care indicators (ECI) during 2012-13. This indicator is supported through work programme of Safety Express and through initiatives such as the Nutrition and Hydration week. Service area Performance District nursing teams 100% Inpatient bedded units 92.1% Learning Disability Services units 82.7% During 2013-14 we plan to: • develop integrated nutrition and hydration assessment and care planning documentation • pilot the use of mealtime volunteers to support the mealtime experience • continue with mealtime audits which examine the patient experience, food safety and nutritional content of the meals in our bedded units • review and standardise the special diets we provide for people with swallowing difficulties • undertake a formal review of nutrition support against the recent NICE quality standards published. 26 Children and Families Division - improving the quality of our health visiting services Rationale Birmingham is an area with an increasing birth rate and with high deprivation and generally worse health outcomes than for people in other parts of the country. The health visiting service has high caseloads with a significant focus on safeguarding. The Health Visitor Implementation Plan (DH, 2010) sets out the ambitious vision of increasing health visitor numbers by 4,200 by April 2015. This equates to an increase of 122 across Birmingham and represents a significant opportunity to improve health visiting services in the city for future generations. The programme also includes the roll-out of Family Nurse Partnership across the city. The result will be to ensure healthy lifestyle outcomes for all children and families, by providing access to advice, support and universal services that work in partnership to promote health, intervene early and protect and safeguard vulnerable children and families. Baseline We plan to deliver our CQUIN for new birth visits and new-to-area visits. We also plan to exceed our levels of patient satisfaction from the June to August 2011 annual survey. Our goal Our goal is that all children known to our service achieve their potential and those with an assessed need have an integrated care plan and all are protected and safeguarded by a competent and confident workforce. We want all users to have a high level of satisfaction with the service they access and our staff to be confident and competent in their roles, as measured by a completed personal development review. Achievement by March 2013 Appraisals: 54 per cent of health visitors’ personal development reviews (PDR) were up to date for the year 2011/12. During 2012/13 an improvement was demonstrated where 76 per cent of health visitors were up to date for the year 2012/13. Staff will continue to receive PDRs as part of their training and development review. Service user experience: the service has continually measured service user satisfaction and feedback over the past year has demonstrated that service satisfaction remains high and has continued to improve over the year - 96 per cent in quarter three. Service satisfaction and feedback will continue to be measured and reviewed within the service to support continuous improvement. Integrated care plan: the clinical records for health visitors and school nurses have been updated across the services so that the Common Assessment Framework processes that are integral to how families and children are supported in Birmingham are aligned with other agencies. This wellbeing record now forms part of the Universal Plus process whereby when additional needs are identified above the universal offer given to all children as part of the Healthy Child Programme, a record is opened and the child’s needs are identified. 27 Birmingham Dental Hospital - improving the quality of referrals to our services Rationale Commissioners and the emerging clinical networks wish to understand the quality of referrals being made into Birmingham Dental Hospital. This will enable the successful completion of managed clinical network objectives and the effective commissioning of primary care for the future. Baseline An audit will be carried out to understand the quality of referrals currently being received, with plans put in place to educate referring organisations on good referral practices. Our goal Poor referrals are a drain on NHS resources. Standardising and improving referrals will improve the pathway in which patients access services along with improving information available. How we will monitor and report our progress Information update and reports will be submitted to Commissioners on a quarterly basis, evidencing achievements against milestones and the action plan going forward to ensure completion of final indicators. How our goal will be achieved The Trust will work in partnership with service leads, Commissioners and the local dental committee to ensure achievement of the CQUIN. Achievements by March 2013 A full audit has been completed with summary analysis and interpretation of the data forming a final report which has been presented to Commissioners to take forward during 2013/14. Key areas for development include referring organisations increasing the provision of radiographic information. 28 Combined Community Dental Services (CCDS) - membership of Quality in Dental Services Scheme Rationale The government wishes to move towards an NHS dental service delivering high quality clinically appropriate preventative, routine and complex care for those who choose it. The Quality in Dental Services Scheme (QIDS) is a quality assurance tool which helps salaried dental services demonstrate how they meet current accepted standards of good practice. The scheme involves completing a self-assessment against the required standards and completing a portfolio of evidence in support of the application for membership. This documentation is independently assessed and verified by the British Dental Association assessors prior to awarding QIDS accreditation. Our goal CCDS aim to submit it’s application for membership of the QIDS in June 2012. How we will monitor and report our progress Achievement of this priority will be reported to and monitored by the specialist division governance committee which reports, through the corporate governance arrangements, to the Trust’s clinical governance committee. How our goal will be achieved Arrangements include: • provision of support by the clinical governance lead for CCDS • identification of a local lead for each clinic who is responsible for progressing the QIDS application process. Achievements by March 2013 The principles and standards of the 10 domains in The Quality Assurance Programme for Dental Services (QUIDS), continues to be additional benchmark standards for CCDS. The ability to produce the evidence to demonstrate the compliance necessary for the portfolio submission and subsequent assessment visit has been delayed by the need to demonstrate agreed joint documentation in practice following the merger of the four individual community dental services, and the subsequent auditing of that. The final part of this has been the bringing together of the four services into one electronic clinical system which was completed in November 2012. As one of the last pieces of evidence needed for the portfolio a service specific baseline records audit of this system has just been completed, with the results due to presented to clinicians in May 2013. It is now proposed to submit our portfolio for assessment in July 2013. 29 Commissioning for Quality and Innovation (CQUINs) 2012-13 What is CQUIN? CQUINs (Commissioning for Quality and Innovation) are projects agreed between the Commissioners (who buy our services) and the Trust. The projects are set up to improve quality standards in key areas. A proportion of Birmingham Community Healthcare’s income in 2012-13 was conditional on achieving quality improvement and innovation goals agreed between the Trust and any person or body it entered into a contract, agreement, or arrangement with for the provision of NHS services, through the Commissioning for Quality and Innovation payment framework. CQUINs for our Adults and Community Division and Children and Families Division (No. 1 - 12) Venous thromboembolism (VTE) risk assessment 1 Adults and Community Division 1. Why is this a priority?: Venous thromboembolism, also known as a bloodclot, is a significant patient safety issue. The process of measuring the risk of developing VTE will set an effective foundation for appropriate preventative treatment. This gives the potential to save thousands of lives each year. 2. Baseline: The requirement to audit patient notes for VTE risk assessment is new this year. 3. Our goal: From April 2012 to March 2013, at least 90 per cent of all adult inpatients have a VTE risk assessment upon admission using the national tool. 4. How we will monitor and report on progress: Monthly divisional performance reporting that feeds into our monthly board integrated performance report. 5. How we will achieve our goal: By assessing every patient for their risk of developing VTE when they are admitted to one of our inpatient units. 6. Achievement by March 2013: The practice of assessing for the risk of VTE is successfully embedded into the inpatient units. The target of 90 per cent compliance has been exceeded each month. VTE risk assessment 30 100% achieved Venous thromboembolism (VTE) prophylaxis – preventing VTE Adults and Community Division 2 1. Why is this a priority?: VTE - deep vein thrombosis (DVT) and pulmonary embolism (PE) - are potentially fatal complications of hospital admission. It is important that those people who need preventative medicines (prophylaxis) are offered them in accordance with NICE guidance. 2. Baseline: Data from quarter one (April-June) used as a baseline to set quarter four milestones. 3. Our goal: That by March 2013 we achieve 99 per cent compliance for community hospitals. 4. How we will monitor and report on progress: Monthly divisional performance reporting that feeds into our monthly board integrated performance report. 5. How we will achieve our goal: By prescribing appropriately for all patients at risk of VTE. 6. Achievement by March 2013: All of the required improvements were achieved by March 2013 which is the final indicator period for the CQUIN. VTE prophylaxis NHS Safety Thermometer Adults and Community Division 100% achieved 3 1. Why is this a priority?: Participation in data collection using the NHS Safety Thermometer is an important preparatory step for reducing harm from clinical care. The four harms we are focusing on are: pressure ulcers, falls, urinary tract infections (UTIs) (with catheters) and VTEs. This will allow the establishment of quality improvement aims for year two (further details to follow) and contribute to the provision of data required for the outcomes framework and government transparency agenda. 2. Our goal: A completed NHS Safety Thermometer survey for all relevant patients must be included for each month in the relevant quarter’s submission. 3. How we will monitor and report on progress: Monthly divisional performance reporting that feeds into our monthly board integrated performance report. 4. How we will achieve our goal: Data will be collated locally using the NHS Safety Thermometer tool on a single day per month (day to be determined locally in each provider). This monthly data will be uploaded by each provider to the NHS Information Centre on a quarterly basis. 5. Achievement by March 2013: Successful in collating and submitting data routinely on a monthly basis. NHS Safety Thermometer 100% achieved 31 Patient experience in community hospitals and patient experience in community services 4 Adults and Community Division and Children and Families Division 1. Why is this a priority?: Carrying out patient satisfaction surveys and monitoring results helps to ensure that all service activities and improvements are orientated towards improving the experience of patients. 2. Baseline - a measured starting point: By August 2012 the two initial surveys will have been carried out and the findings will be reported and used as a baseline to improve against in the second half of the year. 3. Our goal: That the second two surveys will show an increase in scores compared to the initial surveys, demonstrating that positive actions have been taken to improve patient experience. 4. How we will monitor and report on progress: Monthly divisional performance reporting that feeds into our monthly board integrated performance report. 5. How we will achieve our goal: Implement action plans based upon survey findings. 6. Achievement by March 2013: An overall improvement in patient satisfaction was achieved across the services surveyed. Scores increased by an average of 5 per cent for 10 of the 13 questions asked in quarter three compared to quarter one, the remaining scores fell by just 0.5 per cent on average. Patient experience Family and friends test (net promoter) Adults and Community Division 100% achieved 5 1. Why is this a priority?: NHS Midlands and East are developing a standardised approach with a single metric to obtain real-time monitoring of Patient Experience. The net promoter score captures perceptions of the local population about the health care they have received. The score is the difference between the proportion of people surveyed who said they would recommend the local service and the proportion who said they would not. 2. Our goal: Demonstration that the question is established and reported for at least 10 per cent of inpatient discharges, with patients surveyed at or within 48 hours of discharge. 3. How we will monitor and report on progress: Monthly divisional performance reporting that feeds into our monthly board integrated performance report. 4. How we will achieve our goal: Establish named persons in each inpatient unit to co-ordinate the completion of the questionnaires on day of discharge or within 48 hours of discharge. Set-up a reporting template to show weekly results per ward. Results will be analysed to identify service improvements and formulate action plans. 5. Achievement by March 2013: This first year of using the friends and family test on a weekly basis has enabled the organisation to embed the survey across all inpatient wards. The patient experience team have worked closely with ward teams to successfully learn lessons and implement changes as a result of responding to the experience and feedback of patients. Friends and family test 32 100% achieved 6 Avoidable pressure ulcer Adults and Community Division 1. Why is this a priority?: Eliminating avoidable pressure ulcers is a cluster top ten priority for quality improvement. This CQUIN will support the national ambition to eliminate avoidable pressure ulcers. Achievement of this CQUIN will have a positive impact on patient experience, safety and quality effectiveness. 2. Our goal: To have zero avoidable grade three or four pressure ulcers in our inpatient units and to have at least a 30 per cent reduction zero avoidable grade three or four pressure ulcers in our community in quarter four compared to quarter one. 3. How we will monitor and report on progress: Monthly divisional performance reporting that feeds into our monthly board integrated performance report. 4. How we will achieve our goal: The tissue viability team will establish a pressure ulcer prevention and management work programme. 5. Achievement by March 2013: The target for community avoidable grade three and four pressure ulcers was nine per month in quarter four. In January there was only one avoidable pressure ulcer in the community and the Trust is on track to achieve this CQUIN. This is largely due to the preventative work of community staff in identifying at risk patients and ensuring information on safer care was provided and equipment put in place. The target for inpatient avoidable grade three and four pressure ulcers for the quarter was zero, however there has been one recorded in March. While it is a disappointment that we have had any avoidable pressure ulcers the improvement represents a significant achievement for in-patient to have reduced the numbers to such a low level. Detailed root-cause analysis is undertaken for each grade three and four pressure ulcer which occurs in our care, to help prevent them happening again. Interventions to achieve improvements include the work of a director-led strategic group which meets weekly and has helped maintain the drive to reduce pressure ulcer incidents. The next step is to work in partnership with social care to spread the Think SSKIN preventative model for patients where BCHC does not provide regular care. The tissue viability team is working with the Birmingham City Council to support agency staff who provide care in patient’s homes. This will help them to identify signs of skin damage at an early stage and encourage them to contact community teams to visit and prevent pressure ulcers developing. Avoidable pressure ulcer elimination - inpatient Not achieved Avoidable pressure ulcer reduction - community Achieved 33 Healthy lifestyles - smoking Adults and Community Division and Children and Families Division 7 1. Why is this a priority?: Over 80,000 people a year in England die prematurely from smoking-related diseases. Stopping smoking amongst patients not only improves the overall health and wellbeing (reduces risk of heart disease, cancer and premature death) but reduces post-operative complications (decreases wound healing time, reduces length of stay, etc). If more pre-operative patients were to stop smoking prior to operation, more post-operative complications would be avoided each year which would reduce bed days and produce cost savings. The number of smokers identified and given advice or referral should reflect the smoking prevalence in that population. 2. Our goal: Patients in contact with services: a) 90 per cent of patients to have smoking status recorded b) 90 per cent of smokers to have received brief advice c) 90 per cent of smokers to have a record of referral to a local stop smoking service or . evidence of opt out from referral d) 90 per cent of patient facing staff that have completed approved training in delivering brief advice for smoking cessation. 3. How we will monitor and report on progress: Monthly divisional performance reporting that feeds into our monthly board integrated performance report. 4. How we will achieve our goal: Ensure staff are fully briefed on the requirements of the CQUIN, roll-out paperwork for staff to complete. Establish monthly auditing to collect results and ensure that targets are being achieved. 5. Achievement by March 2013: Each of the four targets have been achieved in quarter four. Healthy lifestyles - smoking 34 100% achieved Healthy lifestyles - alcohol Adults and Community Division and Children and Families Division 8 1. Why is this a priority?: There is strong evidence that frontline staff delivering brief opportunistic advice for both alcohol and smoking are both clinically and cost effective interventions. Consequently, smoking and alcohol have been identified in QIPP (Quality, Innovation, Productivity and Prevention), as target areas where improvements to interventions such as brief advice, are likely to have a significant impact upon patient health and where cost-savings can be demonstrated. The number of drinkers identified in each category and given advice/referral should reflect the prevalence in that population. 2. Our goal: Patients in contact with services: a) 80 per cent alcohol status recorded b) 70 per cent of patients whose score indicates hazardous drinking receiving brief advice to stop drinking c) 70 per cent of patients whose score indicates harmful or dependent drinking receiving referral to alcohol services via a single contact number d) 90 per cent of frontline staff have completed approved training in delivering brief advice for alcohol harm reduction. (Goals a - c apply to the Adults and Community Division, d applies to the Children and Families Division). 3. How we will monitor and report on progress: Monthly divisional performance reporting that feeds into our monthly board integrated performance report. 4. How we will achieve our goal: Ensure staff are fully briefed on the requirements of the CQUIN, roll-out paperwork for staff to complete. Establish monthly auditing to collect results and ensure that targets are being achieved. 5. Achievement by March 2013: Each of the four targets have been achieved in quarter four. Healthy lifestyles - alcohol 100% achieved 35 Making every contact count (MECC) Adults and Community Division and Children and Families Division 9 1. Why is this a priority?: MECC is one of the five Strategic Health Authority (SHA) cluster ambitions outlined in the regional commissioning framework 2012/13. Unhealthy lifestyle behaviours create a financial and resource burden on the NHS and society as a whole and generate inequalities in health outcomes. Across the region: • smoking 20 per cent of our population smoke • alcohol 25 per cent are drinking at increasing risk or high risk levels • obesity 22 to 26 per cent of men and 24 per cent to 28 per cent of women are obese • physical activity 61 per cent of men and 71 per cent women do not meet recommended levels • diet 75 per cent of men and 71 per cent of women do not eat five portions of fruit and vegetables a day • but people who follow all the healthy lifestyles live 14 years longer on average than those who follow none. 2. Our goal: By end of quarter four: a) evidence of board level commitment to implementation b) board level lead / champion in place c) evidence of organisational policies and procedures in place, for example organisational health and wellbeing development strategy, suitable data collection and reporting mechanisms, use of induction d) evidence of activity to support employees own health and wellbeing for example implementation with NICE public health Guidance for Tobacco in Workplaces. 3. How we will monitor and report on progress: Monthly divisional performance reporting that feeds into our monthly board integrated performance report. 4. How we will achieve our goal: Health and wellbeing lead to ensure that all targets are met by formulating implementation plan and monitoring progress throughout the year. 5. Achievement by March 2013: The make every contact count campaign has been successfully implemented throughout the Trust to help us improve the health and wellbeing of our patients, staff and public. Making every contact count 36 100% achieved 10 Safer transfer of medicines on discharge Adults and Community Division 1. Why is this a priority?: The Royal Pharmaceutical Society published guiding principles for the safer transfer of medicines at interfaces of care. These principles were endorsed by a number of national bodies. Definitions: Medications changes means changes to a patient’s pre-admission medication regimen which are intended to continue after discharge. These include: - initiation of a new medicine - change in the dose, form, route or frequency of a drug taken prior to admission - stopping of a medicine taken prior to admission. If there are no changes, this should also be explicitly communicated in the discharge documentation. Explanation for changes should include sufficient detail to inform future decisions about medicines. 2. Our goal: To improve the effectiveness of processes to ensure that medicines information is transferred with patients on discharge. 3. How we will monitor and report on progress: Monthly divisional performance reporting that feeds into our monthly board integrated performance report. 4. How we will achieve our goal: Medicines management to lead on project by designing audits and developing action plan to achieve agreed targets with the involvement of service leads, clinical director, GPs and acute trusts. 5. Achievement by March 2013: All of the required improvements were achieved by March 2013 which is the final indicator period for the CQUIN. Safer transfer of medicines on discharge 100% achieved 37 End of life care Adults and Community Division 11 1. Why is this a priority?: The BCHC contract for Integrated Multidisciplinary Teams service (IMTs) identifies district nurses/IMTs as coordinators of end of life care, working in partnership with all GPs and end of life providers. Improving the advanced planning of care has been found to be one of the most important and effective ways that we can ensure reliable patient-focused care. Improvement in end of life care can have a high impact on patient experience as well as the experience of family members and carers. A patient driven service will enable patients to have greater control at the end of their life. Greater coordination of care improves quality, communication and supportive working relationships between different providers should support patients effectively to die in a place of their choice. 2. Our goal: To develop an improvement plan, based on 2011/12 quarter four data, to ensure improvement on the number of patients identified as having a care plan based on recognised integrated care pathway for supportive care, including documented preferred place of death. 3. How we will monitor and report on progress: Monthly Divisional performance reporting that feeds into our monthly board integrated performance report. 4. How we will achieve our goal: Complete baseline audit and document improvement plan. Project lead to organise the collection of monthly audit data and evaluate against the plan ensuring milestones are met and service improvements put in place. 5. Achievement by March 2013: As part of the improvement plan, in quarter four 100 per cent of palliative care patients sampled had a care plan in place and 92 per cent of care plans identified the preferred place of death for the patient which exceeded the set target. End of life care Blood glucose shared care record Adults and Community Division 100% achieved 12 1. Why is this a priority?: Diabetes is a common lifelong health condition which can lead to serious complications and premature death, but people with diabetes, working together with their health care providers, can take steps to control the disease and lower the risk of complications. It is imperative that timely, accurate, shared care records exist. Different clinical disciplines should be able to record clinical details, update treatment delivered, indicate next stage of treatment required which can be acted on such as between GPs and community nursing teams. 2. Our goal: Increase early detection of undiagnosed diabetes within the local community and support the development of shared clinical records in the community integrated teams 3. How we will monitor and report on progress: Monthly divisional performance reporting that feeds into our monthly board integrated performance report. 4. How we will achieve our goal: Develop and agree an implementation plan covering the process of detecting undiagnosed diabetes within patients in the local community, their subsequent GP referral and the protocols to support the usage of shared care records. 5. Achievement by March 2013: In quarter four the number of eligible patients that had their fasting blood sugar recorded and shared was 87 per cent against a 90 per cent target. Blood glucose shared care record 38 90% achieved CQUINs for Birmingham Dental Hospital (BDH) and Combined Community Dental Services (CCDS) 2012-13 (No.13 - 24) Making every contact count (MECC) 13 Birmingham Dental Hospital 1. Why is this a priority?: MECC is one of the five Strategic Health Authority (SHA) cluster ambitions outlined in the Regional Commissioning Framework 2012/13. Unhealthy lifestyle behaviours create a financial and resource burden on the NHS and society as a whole and generate inequalities in health outcomes. Across the region: • smoking 20 per cent of our population smoke • alcohol 25 per cent are drinking at increasing risk or high risk levels • obesity 22 to 26 per cent of men and 24 per cent to 28 per cent of women are obese • physical activity 61 per cent of men and 71 per cent women do not meet recommended levels • diet 75 per cent of men and 71 per cent of women do not eat five portions of fruit and vegetables a day • but people who follow all the healthy lifestyles live 14 years longer on average than those who follow none. 2. Our goal: a) evidence of board level commitment to implementation b) board level lead / champion in place c) evidence of organisational policies and procedures in place, for example organisational health and wellbeing development strategy, suitable data collection and reporting mechanisms, use of induction d) evidence of activity to support employees own health and wellbeing e) system to routinely record the number of NHS staff completing locally agreed training in delivering lifestyle brief advice f) system to routinely record the number of referrals to local stop smoking services, (as a key indicator for brief opportunistic advice delivery). 3. How we will monitor and report on progress: Monthly Divisional performance reporting that feeds into our monthly board integrated performance report. 4. How we will achieve our goal: Health and wellbeing lead to ensure that all targets are met by formulating implementation plan and monitoring progress throughout the year. 5. Achievement by March 2013: The MECC campaign has been successfully implemented to help us improve the health and wellbeing of our patients, staff and public. Referrals and training figures are successfully being recorded and monitored. Every contact counts - BDH 100% achieved 39 Healthy lifestyles - smoking Birmingham Dental Hospital and Combined Community Dental Services 14 1. Why is this a priority?: There is strong evidence that delivering brief opportunistic advice by frontline staff for both alcohol and smoking are both clinically and cost effective interventions. Consequently, smoking and alcohol have been identified in QIPP (Quality, Innovation, Productivity and Prevention), as target areas where improvements to interventions such as brief advice, are likely to have a significant impact upon patient health and where cost-savings can be demonstrated. The number of smokers identified in each category and given advice/referral should reflect the prevalence in that population. 2. Our goal: Develop a detailed plan for providing brief advice with regard to smoking cessation, to patients on their clinic, in a manner appropriate for their patient group. This should include a review of current health promotion material with a view to updating material as necessary. Conduct meetings to review current health promotion material, in house stop-smoking services and to consider referrals to external stop-smoking services. Healthy lifestyles - alcohol Birmingham Dental Hospital and Combined Community Dental Services 15 1. Why is this a priority?: There is strong evidence that delivering brief opportunistic advice by frontline staff for both alcohol and smoking are both clinically and cost effective interventions. Consequently, smoking and alcohol have been identified in QIPP (Quality, Innovation, Productivity and Prevention), as target areas where improvements to interventions such as brief advice, are likely to have a significant impact upon patient health and where cost-savings can be demonstrated.The number of drinkers identified in each category and given advice/referral should reflect the prevalence in that population. 2. Our goal: Develop a detailed plan for providing brief advice with regard to alcohol consumption, to patients on their clinic, in a manner appropriate for their patient group. This should include a review of current health promotion material with a view to updating material as necessary. Conduct meetings to review current health promotion material, in house stop-smoking services and to consider referral to alcohol services. For both smoking and alcohol CQUINs (No. 14 and No. 15): 3. How we will monitor and report on progress: Monthly divisional performance reporting that feeds into our monthly board integrated performance report. 4. How we will achieve our goal: Appoint project lead to arrange meetings and develop a detailed plan for providing brief advice. Regular reports will be produced to update progress against plan throughout the year. 5. Achievement by March 2013: The Dental Hospital can refer patients to healthy lifestyle support services, and staff are using the leaflets and referral forms as appropriate for their patients. Brief intervention, referrals and health promotion literature will continue as part of each patient contact at Birmingham Dental Hospital going forward. 40 Healthy lifestyles - smoking 100% achieved Healthy lifestyles - alcohol 100% achieved Healthy lifestyles - diet Birmingham Dental Hospital and Combined Community Dental Services 16 1. Why is this a priority?: The identification of patients and parents / carers of patients where oral health would indicate that brief advice on diet would be beneficial and where appropriate provide referral to weight management programmes. 2. Our goal: Develop a detailed plan for providing brief advice with regard to diet, to patients on their clinic, in a manner appropriate for their patient group. This should include a review of current health promotion material with a view to updating material as necessary. Conduct meetings to review current health promotion material, dietary advice that promotes general health as well as oral health. 3. How we will monitor and report on progress: Monthly divisional performance reporting that feeds into our monthly board integrated performance report. 4. How we will achieve our goal: Appoint project lead to arrange meetings and develop a detailed plan for providing brief advice. Regular progress reports will be produced to update progress against plan throughout the year. 5. Achievement by March 2013: The Dental Hospital can refer patients to healthy lifestyle support services, and staff are using the leaflets and referral forms as appropriate for their patients. Brief intervention, referrals and health promotion literature will continue as part of each patient contact at Birmingham Dental Hospital going forward. Healthy lifestyles - diet Oral Medicine Managed Clinical Networks Birmingham Dental Hospital 100% achieved 17 1. Why is this a priority?: Managed Clinical Networks (MCNs) and Local Professional Networks (LPNs) for dentistry are being developed as a means for dental professionals to be involved in influencing local strategy and policy; they will enable clinicians to have a role in developing patient pathways, service planning and delivery, quality assurance and clinical governance. 2. Our goal: The clinical network will be accountable to the emerging Birmingham and Solihull Local Professional Network for dentistry being established during 2012-13 and its structure will need to be consistent with the model of other MCNs also accountable to the Local Professional Network. The MCN must also aim to encompass the West Midlands in its approach and feed into the work plans of other Local Professional Networks across the region. 3. How we will monitor and report on progress: Progress report to be produced at six and 12 months. This should include a summary of progress against the plan, any problems with implementing the plan and an action plan as appropriate. This will be submitted to the Local Professional Network, Commissioners and Dental Public Health for approval. 4. How we will achieve our goal: By appointing a project lead to organise the initial meeting and ensure that the membership and terms of reference are completed by the set deadlines. 5. Achievement by March 2013: The MCN for Oral Medicine has been successfully established and many of the agreed objectives have been met. Some objectives were not achieved due for a variety of reasons, including clinicians giving priority to clinical commitments, however they will be addressed as the clinical network continues on into next year. Oral Medicine MCN 70% achieved 41 Restorative Dentistry Managed Clinical Network 18 Birmingham Dental Hospital 1. Why is this a priority?: Managed Clinical Networks (MCNs) and Local Professional Networks (LPNs) for dentistry are being developed as a means for dental professionals to be involved in influencing local strategy and policy; they will enable clinicians to have a role in developing patient pathways, service planning and delivery, quality assurance and clinical governance. 2. Our goal: The clinical network will be accountable to the emerging Birmingham and Solihull Local Professional Network for dentistry being established during 2012-13 and its structure will need to be consistent with the model of other MCNs also accountable to the Local Professional Network. The MCN must also aim to encompass the West Midlands in its approach and feed into the work plans of other Local Professional Networks across the region. 3. How we will monitor and report on progress: Progress report to be produced at six and 12 months. This should include a summary of progress against the plan, any problems with implementing the plan and an action plan as appropriate. This will be submitted to the local professional network, Commissioners and Dental Public Health for approval. 4. How we will achieve our goal: By appointing a project lead to organise the initial meeting and ensure that the membership and terms of reference are completed by the set deadlines. 5. Achievement by March 2013: The Restorative Dentistry Managed Clinical Network has been successful in establishing its structure and attracting a sound and effective membership. Restorative Dentistry MCN 100% achieved Patient experience 19 Birmingham Dental Hospital 1. Why is this a priority?: To ensure weaknesses highlighted by 2011-12 Patient Experience survey are addressed and required improvements made. 2. Our goal: To continue to enhance patient experience at Birmingham Dental Hospital. 3. How we will monitor and report on progress: Monthly divisional performance reporting that feeds into our monthly board integrated performance report. 4. How we will achieve our goal: Establish a Picker Patient Experience Working Group to identify top four areas for improvement and put action plans in place in order to implement and monitor changes to boost patient experience. 5. Achievement by March 2013: Of the four priority areas for improvement; ‘information about who to contact when leaving hospital’ was shown to have improved significantly whilst ‘communication about students’ remained at the same satisfaction level when compared to 2011-12. The other two areas ‘delays and communication about waiting times’ and ‘privacy and dignity’ both showed a slight drop in satisfaction levels of around three per cent. The Dental Hospital requires continuing focus on all elements of the 2012 action plan with further targeted work required around the top four areas. It is disappointing that the work that has been achieved in efforts to improving patient experience has not been reflected in the autumn survey response. Patient experience - BDH 42 80% (TBC) Referrals 20 Birmingham Dental Hospital 1. Why is this a priority?: Managed Clinical Networks (MCNs), Commissioners and the emerging clinical networks will need to understand the quality of referral being made into secondary care to enable the successful completion of MCN objectives and the effective commissioning of primary care. Poor referrals are a drain on NHS resources and it is in the entire systems interests to improve and standard that improvement. 2. Our goal: The CQUIN scheme will require the Dental Hospital to audit referrals across all specialties made to the hospital over a four month period and produce a summary report. This will allow the Provider and Commissioners as well as emerging MCNs to make sense of the scale and quality of referrals being received. 3. How we will monitor and report on progress: Monthly divisional performance reporting that feeds into our monthly board integrated performance report. 4. How we will achieve our goal: Project lead to plan the methodology and scale of audit by the end of May for approval. Audit to be then carried out and results presented via a report to Commissioners. 5. Achievement by March 2013: The audit was carried out as planned with Commissioners and a detailed report of the findings produced and shared with the emerging Managed Clinical Networks. Referrals 100% achieved Patient experience 21 Combined Community Dental Services 1. Why is this a priority?: Carrying out patient satisfaction surveys and monitoring results helps to ensure that all service activities and improvements are oriented towards improving the experience of patients. 2. Our goal: The 2012-13 patient experience CQUIN for the Combined Community Dental Services is intended to establish a survey to enable the service to improve patient experience against the criteria being proposed for the Dental Quality Outcomes Framework (QOF).w The survey will be completed on a quarterly basis with results feeding through to the patient experience team, enabling results to be collated and analysed to form the basis for an action plan for any areas for improvement that are identified. The content of the survey should be approved by Commissioners and Dental Public Health. 3. How we will monitor and report on progress: Monthly divisional performance reporting that feeds into our monthly board integrated performance report. 4. How we will achieve our goal: Lead appointed to plan the design and roll-out of the patient survey. Ensure results are analysed to identify those areas requiring improvement in order to create an action plan to address priority areas for enhancement of patient experience. 5. Achievement by March 2013: The survey was rolled out and results used to formulate an action plan for improvement which was shared with commissioners. Patient experience CCDS 100% achieved 43 Making every contact count (MECC) 22 Combined Community Dental Services 1. Why is this a priority?: MECC is one of the five Strategic Health Authority (SHA) cluster ambitions outlined in the Regional Commissioning Framework 2012/13. Unhealthy lifestyle behaviours create a financial and resource burden on the NHS and society as a whole and generate inequalities in health outcomes. Across the region: • smoking 20 per cent of our population smoke • alcohol 25 per cent are drinking at increasing risk or high risk levels • obesity 22 to 26 per cent of men and 24 per cent to 28 per cent of women are obese • physical activity 61 per cent of men and 71 per cent women do not meet recommended levels • diet 75 per cent of men and 71 per cent of women do not eat five portions of fruit and vegetables a day • but people who follow all the healthy lifestyles live 14 years longer on average than those who follow none. 2. Our goal: By end of quarter four: a) evidence of board level commitment to implementation b) board level lead / champion in place c) evidence of organisational policies and procedures in place, for example organisational health and wellbeing development strategy, suitable data collection and reporting mechanisms, use of induction d) evidence of activity to support employees own health and wellbeing e) system to routinely record the number of NHS staff completing locally agreed training in delivering lifestyle brief advice f) system to routinely record the number of referrals to local stop smoking services, (as a key indicator for brief opportunistic advice delivery). 3. How we will monitor and report on progress: Monthly divisional performance reporting that feeds into our monthly board integrated performance report. 4. How we will achieve our goal: Health and wellbeing lead to ensure that all targets are met by formulating implementation plan and monitoring progress throughout the year. 5. Achievement by March 2013: The make every contact count campaign has been successfully implemented throughout the Trust to help us improve the health and wellbeing of our patients, staff and public. Every contact counts - CCDS 44 100% achieved Paediatric Dentistry Managed Clinical Network Combined Community Dental Services 23 1. Why is this a priority?: Managed Clinical Networks (MCNs) and Local Professional Networks (LPNs) for dentistry are being developed as a means for dental professionals to be involved in influencing local strategy and policy; they will enable clinicians to have a role in developing patient pathways, service planning and delivery, quality assurance and clinical governance. 2. Our goal: The clinical network will be accountable to the emerging Birmingham and Solihull Local Professional Network for dentistry being established during 2012-13 and its structure will need to be consistent with the model of other MCNs also accountable to the Local Professional Network. The MCN must also aim to encompass the West Midlands in its approach and feed into the work plans of other Local Professional Networks across the region. 3. How we will monitor and report on progress: Progress report to be produced at six and 12 months. This should include a summary of progress against the plan, any problems with implementing the plan and an action plan as appropriate. This will be submitted to the local professional network, Commissioners and Dental Public Health for approval. 4. How we will achieve our goal: By appointing a project lead to organise the initial meeting and ensure that the membership and terms of reference are completed by the set deadlines. 5. Achievement by March 2013: The Managed Clinical Network for Paediatric Dentistry has been successfully established as planned. Paediatric Dentistry MCN Special Care Dentistry Managed Clinical Network Combined Community Dental Services 100% achieved 24 1. Why is this a priority?: Managed Clinical Networks (MCNs) and Local Professional Networks (LPNs) for dentistry are being developed as a means for dental professionals to be involved in influencing local strategy and policy; they will enable clinicians to have a role in developing patient pathways, service planning and delivery, quality assurance and clinical governance. 2. Our goal: The clinical network will be accountable to the emerging Birmingham and Solihull Local Professional Network for dentistry being established during 2012-13 and its structure will need to be consistent with the model of other MCNs also accountable to the Local Professional Network. The MCN must also aim to encompass the West Midlands in its approach and feed into the work plans of other Local Professional Networks across the region. 3. How we will monitor and report on progress: Progress report to be produced at six and 12 months. This should include a summary of progress against the plan, any problems with implementing the plan and an action plan as appropriate. This will be submitted to the Local Professional Network, Commissioners and Dental Public Health for approval. 4. How we will achieve our goal: By appointing a project lead to organise the initial meeting and ensure that the membership and terms of reference are completed by the set deadlines. 5. Achievement by March 2013: The Managed Clinical Network for Special Care Dentistry has been successfully established as planned. Special Care Dentistry MCN 100% achieved 45 CQUINs for Rehabilitation Services 2012-13 (No.25 and 26) NHS Safety Thermometer 25 1. Why is this a priority?: Participation in data collection using the NHS Safety Thermometer is an important preparatory step for reducing harm from clinical care. The four harms we are focusing on are: pressure ulcers, falls, urinary tract infections (UTI’s) (with catheters) and venous thromboembolism (VTEs). This will allow the establishment of quality improvement aims for year two (further details to follow) and contribute to the provision of data required for the outcomes framework and government transparency agenda. 2. Our goal: A completed NHS Safety Thermometer survey for all relevant patients must be included for each month in the relevant quarter’s submission. 3. How we will monitor and report on progress: Monthly divisional performance reporting that feeds into our monthly board integrated performance report. 4. How we will achieve our goal: Data will be collated locally using the NHS Safety Thermometer tool on a single day per month. This monthly data will be uploaded by each provider to the NHS Information Centre on a quarterly basis. 5. Achievement by March 2013: Successful. Data collection and submission on a monthly basis. NHS Safety Thermometer Access to specialist neuro-rehabilitation (local CQUIN) 100% achieved 26 1. Why is this a priority?: There is a requirement for rehab providers to begin to work as a network and operate a ‘pull system’ from secondary/tertiary care. This needs to continue to be developed during 2012. This will allow for an early referral process to ensure faster access out of the tertiary centres to alternative community provision. Patients will receive the right care, at the right place, at the right time, improving rehabilitation outcomes. 2. Baseline: 2011/12 achievement of CQUIN. 3. Our goal: To improve the referral process and level of access to specialised rehabilitation; 100 per cent of referrals received will be recorded electronically via referral hub and tracked through the rehabilitation database. Where an outreach visit is requested by the referring hospital or in order to determine suitability for referral to the unit 100 per cent should have been undertaken by a member of the multidisciplinary team and 100 per cent of patients waiting to come into Inpatient Neuro Rehabilitation Unit (INRU) to have a pre-admission rehabilitation management plan. Average time to transfer patient to the unit should be an improvement on the 2011/12 position. 4. How we will monitor and report on progress: Monthly divisional performance reporting that feeds into our monthly board integrated performance report. Quarterly monitoring arrangements in place with Commissioners. 5. How we will achieve our goal: Continue providing this service, which was successfully piloted in 2011/12, using the same robust monitoring of delivery against CQUIN criteria at regular CQUIN Project Group meetings. 6. Achievement by March 2013: Service has successfully continued throughout 2012/13, building upon the work put into piloting the service last year. All of the requirements of the CQUIN have been met and reported. Access to specialist neuro-rehabilitation 46 100% achieved CQUINs for Learning Disability Services 2012-13 (No.27-30) NHS Safety Thermometer Learning Disability Services 1. Why is this a priority?: Participation in data collection using the NHS Safety Thermometer is an important preparatory step for reducing harm from clinical care. The four harms we are focusing on are: pressure ulcers, falls, UTIs (with catheters) and venous thromboembolism (VTEs). This will allow the establishment of quality improvement aims for year two (further details to follow) and contribute to the provision of data required for the outcomes framework and government transparency agenda. 2. Our goal: A completed NHS Safety Thermometer survey for all relevant patients must be included for each month in the relevant quarter’s submission. 27 3. How we will monitor and report on progress: Monthly divisional performance reporting that feeds into our monthly board integrated performance report. 4. How we will achieve our goal: Data will be collated locally using the NHS Safety Thermometer tool on a single day per month (day to be determined locally in each provider). This monthly data will be uploaded by each provider to the NHS Information Centre on a quarterly basis. 5. Achievement by March 2013: Monthly data has been successfully collated and uploaded onto the NHS Safety Thermometer every month throughout 2012/13. NHS Safety Thermometer 100% achieved Monthly performance report Learning Disability Services 1. Why is this a priority?: Providing robust data analysis on a monthly basis will enable the identification of any problems/blockages in service delivery so that remedial action can be put in place. Evidence can be gathered to demonstrate that services are outcome focused and that positive experiences are received by patients at the point of service delivery. Robust data will contribute to an informed decision-making process and the data set will contribute to the production of a monthly performance dashboard for the Integrated Commissioning Board. 28 2. Our goal: To provide robust and meaningful performance information to Commissioners and providers on a monthly basis. 3. How we will monitor and report on progress: Monthly divisional performance reporting that feeds into our monthly board integrated performance report. 4. How we will achieve our goal: Content and structure of data set to be mutually agreed, then collected and submitted monthly for analysis at the Performance, Quality and CQUIN group. 5. Achievement by March 2013: The required performance report has been submitted to Commissioners on a monthly basis throughout the year successfully meeting the CQUIN requirements. Performance report 100% achieved 47 Health facilitation Learning Disability Services 1. Why is this a priority?: People with learning disabilities experience worse healthcare and health outcomes than the rest of the population. Healthcare providers have a responsibility to ensure they make reasonable adjustments to services in order to address the imbalance. Better health outcomes for patients with learning disabilities benefit the individual by improving life expectancy and quality of life and benefit services by reducing the cost of healthcare (e.g. reducing length of stay, avoiding unnecessary re-admissions). 29 The Health Facilitation Service has been developed within Birmingham Community Healthcare NHS Trust to assist the rest of the healthcare system in this duty. It provides training in working with people with learning disabilities and advice / assistance on supporting individual patients to other healthcare providers, including acute hospitals and GP practices. This CQUIN focuses on service provided to acute hospitals in Birmingham. Some patient data is already collected by the service but there is a need to expand the data to include the specific types of support provided and outcomes for the patient. While the implementation of reasonable adjustments and health outcomes for individual patients are beyond the scope of control of the facilitation service, the ability to report on these is a valuable resource in planning and evaluating its impact. 2. Our goal: The goal will involve the quarterly reporting of the following data: • • • • • • • • number of referrals received in the quarter by acute hospital, broken down by those referred and those identified in service ‘sweeps’ a breakdown of how the Health Facilitation Service assisted/advised hospitals in fulfilling their obligation to make necessary adjustments a breakdown of how many patients required reasonable adjustments details of reasonable adjustments made by hospital trusts in cases where reasonable adjustments were not made, details of the reason why not number of training sessions provided by hospital number of staff trained in the quarter by grade number of staff trained in the quarter by admin/support and clinical. 3. How we will monitor and report on progress: Monthly divisional performance reporting that feeds into our monthly board integrated performance report. 4. How we will achieve our goal: Collation and submission of quarterly report to address all required indicators. 5. Achievement by March 2013: The required data and information across the required indicators has been submitted to the Commissioners every quarter. Health facilitation 48 100% achieved Making every contact count (MECC) Learning Disability Services 30 1. Why is this a priority?: MECC is one of the five Strategic Health Authority (SHA) cluster ambitions outlined in the Regional Commissioning Framework 2012/13. Unhealthy lifestyle behaviours create a financial and resource burden on the NHS and society as a whole and generate inequalities in health outcomes. Across the region: • smoking 20 per cent of our population smoke • alcohol 25 per cent are drinking at increasing risk or high risk levels • obesity One in three people with a learning disability are obese as compared with one in four of the general population • physical activity Over 80 per cent of adults with a learning disability engage in levels of physical activity below the DoH minimum recommended level as compared with 53 - 64 per cent within the general adult population • diet Less than 10 per cent of people with a learning disability living in supported accommodation eat a balanced diet with an insufficient intake of fruit and vegetables, compared with 75 per cent of men and 71 per cent of women do not eat five portions of fruit and vegetables a day within the general adult population • but people who follow all the healthy lifestyles live 14 years longer on average than those who follow none. 2. Our goal: By end of quarter four: a) evidence of board level commitment to implementation b) board level lead / champion in place c) evidence of organisational policies and procedures in place, for example organisational health and wellbeing development strategy, suitable data collection and reporting mechanisms, use of induction d) evidence of activity to support employees own health and wellbeing e) 50 per cent of patient facing staff trained in approved learning disabilities specific healthy lifestyles brief advice (every contact counts). 3. How we will monitor and report on progress: Monthly divisional performance reporting that feeds into our monthly board integrated performance report. 4. How we will achieve our goal: Health and wellbeing lead to ensure that all targets are met by formulating implementation plan and monitoring progress throughout the year. Service to arrange appropriate training in delivering healthy lifestyles brief advice for staff and monitor attendance. 5. Achievement by March 2013: The MECC campaign has been successfully implemented to help us improve the health and wellbeing of our patients, staff and public. The training element has also been achieved, with the overall compliance has exceeding the target. Every contact counts 100% achieved 49 Quality performance data - statutory content Review of services During 2012-13 Birmingham Community Healthcare NHS Trust provided and/or sub-contracted 137 NHS services. Birmingham Community Healthcare NHS Trust has reviewed all the data available on the quality of care in all of these services. The income generated by the services reviewed in 2012-13 represents 100 per cent of the total income generated from the provision of NHS services by Birmingham Community Healthcare NHS Trust for 2012-13. Data quality Birmingham Community Healthcare NHS Trust will be taking the following actions to improve data quality: Data Quality Programme Board is a sub-committee of the Information Steering Group. The overall objective of the Board is to oversee the overall data quality programme for the Trust. It is responsible for identifying and addressing the data quality issues and agree the actions to ensure that improvement are gained. It will address stakeholder concerns about the quality of the data. In this context, data quality means data that is accurate, complete, timely and fit for the purpose for which it is collected and used. To achieve this the Trust will: • identify the business critical information systems that it requires and agree required work programme to provide data quality assurances against each system • control, manage and monitor the data quality risk register • develop, approve and continually monitor the data quality work programme • identify milestones against each project and report each month against the milestones • facilitate a culture of continuous improvement in data quality amount stakeholders • act as the gatekeeper for the introduction of new information systems within the Trust, ensuring data quality standards following the data quality framework • baseline standard and trajectory for improvement against agreed milestones in each information system to be identified, in conjunction with ‘system owner’ • continually match the data quality risks against the Trust strategic objectives and the Assurance Framework to identify the rolling work programme. 50 Participation in clinical audits During 2012/13, four national clinical audits and zero national confidential enquiries covered NHS services that Birmingham Community Healthcare NHS Trust provides. During that period, Birmingham Community Healthcare NHS Trust participated in 100 per cent of national clinical audits and 100 per cent of national confidential enquiries of the national clinical audits and national confidential enquiries which it was eligible to participate in. The national clinical audits and national confidential enquiries that Birmingham Community Healthcare NHS Trust was eligible to participate in during 2012/13 are as follows: National audits • Sentinel Stroke National Audit Programme (SSNAP), includes Stroke Improvement National Audit Programme (SINAP) • Royal College of Paediatrics and Child Health (RCPCH) Epilepsy12 National Audit • Head and Neck Oncology • National Pain Audit (data collection took place 2011/12, report published Dec 2012). The national clinical audits and national confidential enquiries that Birmingham Community Healthcare NHS Trust participated in during 2012/13 are as follows: • SSNAP includes SINAP (BCHC contributes a small number of data items to this audit as a partner to University Hospital Birmingham Foundation Trust) • RCPCH Epilepsy12 National Audit (BCHC contributes to this audit as a partner to Birmingham acute trusts) • Head and Neck Oncology (BCHC contributes to this audit as a partner to University Hospital Birmingham Foundation Trust) • National Pain Audit (data collection took place 2011/12, report published Dec 2012). The national clinical audits and national confidential enquiries that Birmingham Community Healthcare NHS Trust was eligible to participate in, and for which data collection was completed during 2012/13, are listed below alongside the number of cases submitted to each audit or enquiry as a percentage of the number of registered cases required by the terms of that audit or enquiry. *P - Participation *% - Number of cases submitted by BCHC expressed as a % of the number of registered cases required by the terms of the audit or enquiry. Title Acute coronary syndrome or acute myocardial infarction Adult asthma Adult cardiac surgery Adult community acquired pneumonia Adult critical care Bowel cancer Bronchiectasis Cardiac arrest Cardiac arrythmia Cardithoracic transplant Cartoid interventions P* No No No No No No No No No No No %* N/A N/A N/A N/A N/A N/A N/A N/A N/A N/A N/A 51 Title Comparative audit of blood transfusion Congenital heart disease (paediatric cardiac surgery) Coronary angioplasty Diabetes (adult) Diabetes (paediatric) Emergency use of oxygen Epilepsy 12 (childhood epilepsy) (BCHC contributes a number of cases to this national audit as a partner to Birmingham Acute Trusts.) Fever in children Fractured neck of femur Head and neck oncology (BCHC contributes to this national audit as a partner to University Hospital Birmingham Foundation Frust.) 52 P* No No No No No No %* N/A N/A N/A N/A N/A N/A Yes 100% No No N/A N/A Yes 100% Heart failure Hip fracture database Inflammatory bowel disease Lung cancer National joint registry Neonatal intensive and special care Non-invasive ventilation Oesophago-gastric cancer Paediatric asthma Paediatric intensive care Paediatric pneumonia Pain database Parkinson’s disease Potential donor Prescribing observatory for mental health Psychological therapies Pulmonary hypertension Renal colic Renal registry Renal transplantation (NHSBT UK Transplant Registry) Stroke national audit programme (combined sentinel and sinap) Trauma Vascular surgery (VSGBI vascular surgery database) National audit of dementia Confidential enquiries No No No No No No No No No No No No No No No No No No No No Yes No No No No N/A N/A N/A N/A N/A N/A N/A N/A N/A N/A N/A N/A N/A N/A N/A N/A N/A N/A N/A N/A 100% N/A N/A N/A N/A Asthma deaths No N/A Child health No N/A Maternal infant and perinatal No N/A Patient outcome and death No N/A Suicide and homicide in mental health No N/A Elective surgery (National Proms Programme) No N/A The reports of five national clinical audits were reviewed by the provider in 2012/13 and Birmingham Community Healthcare NHS Trust intends to take the following actions to improve the quality of healthcare provided. Audit Royal College of Paediatrics and Child Health (RCPCH) National Childhood Epilepsy Audit Action Taken BCHC contributed a number of cases to this audit as a partner to a number of acute trusts, therefore results are reported at acute trust level. BCHC’s designated lead for this audit has reviewed the report and key findings in conjunction with leads from partner acute organisations. BCHC intends to take the following actions: • complete an audit to identify those paediatricians and nurses who have accredited expertise in epilepsies with a view to developing this resource within our services • support opportunities for integrated care pathway development and partnership working. Audit Action Taken National Parkinson’s Disease Audit The report has been shared with staff within BCHC’s Parkinson’s Disease Service and action has been taken to make information, including leaflets from Parkinson’s Disease UK and details of local support groups, available in clinic areas and to ensure patients continue to receive information about their medication. Audit Action Taken National Pain Audit The Phase 2 report has been reviewed and key findings presented to the Trust’s Clinical Effectiveness Committee by the head of service. Key recommendations met include, among others: • access to physiotherapy and psychology • recommended standards re staffing and structure and multidisciplinary team model • patient information and support • medical consultants underpinning service. Areas identified for further action include: • greater focus on promoting Return To Work • improved recording. 53 Audit Action Taken National Adult Diabetes Audit The report has been shared with the Trust’s Diabetes Service Leads and will also be shared with GPs and Practice Nurses in the Diabetes LES Journal Club meeting to provide an opportunity to reflect on the findings. The Trust’s Diabetes Service leads will be presenting this audit to the Trust’s Clinical Effectiveness Committee identifying key recommendations from the report and further action to be taken. Audit Sentinel Stroke National Audit Programme (SSNAP), includes Stroke Improvement National Audit Programme (SINAP) (BCHC contributes as a partner to University Hospital Birmingham) Action Taken SSNAP has now been superseded by the SINAP in acute hospital settings. The clinical component of SSNAP began in December 2012 and a minimum data set is being collected for every stroke patient. This core data set will initially cover acute care including rehabilitation and six-month follow-up, and will collect outcome measures. • actions have been taken to ensure the relevant data collection processes are in place, including feedback into clinical teams to drive service redesign where required • in addition, BCHC performance against the NHS Midlands and East Stroke Specification has been reviewed. The reports of 121 local clinical audits were reviewed by the provider in 2012/13 and Birmingham Community Healthcare NHS Trust intends to take the following actions to improve the quality of healthcare provided: Trustwide Clinical Record Keeping Audit • review of current record keeping training for staff • ensure all records record allergies and hypersensitivities. Serious Case Review Audits • caseload management days introduced for teams to review their active caseload and care plans associated with cases (good practice in terms of peer review and supervision • care plans reviewed a minimum of three monthly in keeping with record keeping standards • storage arrangements for out of area records reviewed • staff briefings held to highlight learning from case with the themes and key findings. 54 Documentation of Consent Audit (Birmingham Dental Hospital) • ensure all clinicians staff and students are aware of current Trust consent policy • raise awareness of requirements for written consent forms, and documentation of verbal consent. Vision Screening Referral Criteria (Children and Families Division) • the main recommendation from the audit is to increase the vision pass level from 0.2 to 0.1 and this has been implemented locally • we have shared this audit with The British Orthoptic Journal for publication 2013/2014. It will not be known how it effects their actions of practice until published and distributed. Tissue Viability Audit (Adult and Communities Division) • continued development of staff education and support around prevention and treatment of pressure ulcers. Orthodontic Patient’s Satisfaction Survey/Audit • give patients starting treatment leaflets on cleaning of teeth and appliances/foods to avoid • explore possibility of Nurse-Led clinics offering oral hygiene instructions and care of appliances to be made available at orthodontic clinics • review of instruction leaflet • produce handouts for various stages of treatment to be used throughout the service when needed. Moor Green ‘Did Not Attend’ Review (Specialist Rehabilitation Service) The service is reviewing the findings of the service evaluation, including the implications for: • • • introducing text message cancellation service considering strategies to minimise non-attendance at appointments displaying the information about the number of missed appointments in a visible place, e.g. in the reception area. Podiatry - percentage of improvement in pain, following Biomechanical intervention. • audit results used to inform care planning and treatment options provided by the service. Progress against the action plans for local audits will be monitored through the divisional governance arrangements or through corporate workstreams. (For a full report on action plans for local audits please refer to BCHC’s clinical audit annual report available by July 2013). Please note a number of local clinical audits for this reporting period had data collection periods which spanned quarter four (Jan-March 2013) and quarter one (April-June 2013-14). The Trust anticipates the reports associated with these audits will be completed during quarter one 2013/14 following data verification and analysis. 55 Research Participation in clinical research The number of patients receiving NHS services provided or sub-contracted by Birmingham Community Healthcare NHS Trust in 2012-13 that were recruited during that period to participate in research approved by a research ethics committee was 327. Research and Development listening event Research and Development contribution occurs at many levels more than only formal research projects. Initiatives address developing the possibilities of research studies happing in this new Trust whilst supporting existing and new definite research studies, especially those of two divisions who have lengthy historical international research track records. One initiative to increase the possibility has been three listening events that targeted thinking at the earliest gestation of approaches to research. The most recent attracted 32 people from our Specialist Services Division and six academics was held at Birmingham Medical Institute. Listening events mix our staff with local academics who are more familiar with asking research questions. Our research team has collaborated with academic partners at Aston University Health Research Innovations. Aston’s Facilitator Director Nichola Seare uses a large group dialogue technique called the ‘World Café’ where small groups of the event’s attendees talk together in a ‘café’ environment - sitting at tables within the one large conference hall. Talk happens, notes are made, groups mix with each other and the next round of talking begins from the notes made by the people sitting at the last table. Groups used words, doodles and key ideas on flip charts. Energy levels remained high throughout the workshop and there were clear synergies and commitment for the group to work collaboratively. Nichola asked the meeting: “What research could we undertake that would make a substantial impact on the provision of effective and appropriate services for our diverse population?” Answers included improving patient experience, reducing barriers to access services, carers who are invisible, personalised care pathways, media relations - educating all ‘positively’. Enablers were ‘funding’ and ‘leadership’. As a result of the listening events and a research education needs survey research and developments are running three ‘introductions to research’ courses for our Trust staff. The courses will be free and offer a proportion of trainees mentoring for a research project. Research and Development is also looking into follow-up workshops for interest groups identified in the listening events. 56 What others say about the provider NHS Number and General Medical Practice Code Validity Health records play an important role in modern healthcare. The primary function of healthcare records is to record important clinical information which may need to be accessed by the healthcare professionals involved in providing care. To improve access to healthcare records, the use of the NHS Number has been encouraged during the year. Everyone registered with the NHS in England has their own unique NHS Number. Using it to identify a patient correctly is an important step towards improving safety and efficiency of healthcare. To find out your NHS Number contact your GP surgery and ask them to look it up. To protect your privacy you may be asked to show a passport, driving licence or some other proof of identity. If you are registered with a GP you will already have an NHS Number. If you know your NHS number or have it on a document or letter you can help healthcare staff to find your records more easily and share them safely with other people who are caring for you. Birmingham Community Healthcare NHS Trust submitted records during 2012-13 to the Secondary Uses service for inclusion in the Hospital Episode Statistics which are included in the latest published data. The percentage of records in the published data which included the patient’s valid NHS number was: • 96.51 per cent for admitted patient care • 99.20 per cent for outpatient care The percentage of records in the published data which included patients’ valid General Medical Practice was: • 99.3 per cent for admitted patient care • 98.1 per cent for outpatient care Our Information Governance (IG) toolkit attainment level Information Governance is the way in which the NHS handles all organisational information, but particularly personal and sensitive information about patients and employees. It allows organisations and individuals to ensure that personal information is dealt with legally, ethically, confidentially, securely, efficiently and effectively, in order to deliver the best possible care. The IG governance toolkits measures our performance against 45 requirements and in 2012-13 the Trust’s Information Governance Assessment Report score overall was 69 per cent satisfactory and was graded ‘green’. Clinical coding error rate Clinical coding is ‘the translation of medical terminology as written by the clinician to describe a patient’s complaint, problem, diagnosis, treatment or reason for seeking medical attention, into a coded format’ which is nationally and internationally recognised. ‘BCHC was not subject to the payment by results clinical coding audit during 2012-13 by the audit commission’. 57 NHSLA The National Health Service Litigation Authority (NHSLA) handles negligence claims made against NHS organisations. The authority works with NHS providers to improve risk management practices in the NHS using a set of risk management standards. BCHC is compliant with Level One (of three levels) NHSLA standards. This means the process for managing risks has been described and documented in our policies, procedures and guidelines. Care Quality Commission (CQC) Inspections of the Essential Standards of Quality and Safety Birmingham Community Healthcare NHS Trust (BCHC) is required to register with the Care Quality Commission which is the responsible body for ensuring that the Trust meets the appropriate standards of care. The Trust is currently registered with the CQC and its current registration status is unconditional meaning that there are no restrictions placed on the Trust in the provision of its services. The Care Quality Commission has not taken enforcement action against BCHC during 2012-13. BCHC has not participated in any special reviews or investigations by the CQC during 2012-13. During 2012-13 the Care Quality Commission inspected the following Trust locations: Adults and Community Division: Norman Power Centre Moseley Hall Hospital Specialist Division - Learning Disability Services: Bristol Road South Elliott Lodge Handsworth Wood Road Hob Moor Road Kingswood Drive Nineveh House Sayer House Tessall Lane Specialist Division - Dental Services: Birmingham Dental Hospital Of the eleven locations inspected, nine were found to be fully compliant with the CQC standards that were assessed. However two locations, Birmingham Dental Hospital and Moseley Hall Hospital, were assessed as non-compliant with one of the standards inspected. In both cases the CQC judged that this had a minor impact on people using the service. A minor impact means people who use the service experienced care below the standard expected however the impact was not significant and the matter could be managed or resolved quickly. 58 Below are further details on the areas the CQC found to be non-compliant and the actions the Trust has taken. Areas of non-compliance: Birmingham Dental Hospital In September 2012, Birmingham Dental Hospital (BDH) was inspected and found to be compliant with four out of five of the standards inspected on that day. However the service was assessed as non-compliant with cleanliness and infection control which states that people should be cared for in a clean environment and protected from the risk of infection. The CQC said: “The provider was not meeting this standard. People were not being consistently cared for in a clean and hygienic environment. We judged that this had a minor impact on people using this service and action was needed for this essential standard.” Following this judgement an action plan was developed to address these concerns. In December 2012 the CQC reassessed and found the hospital to be compliant with this essential standard. Moseley Hall Hospital In January 2013 Moseley Hall Hospital was inspected and found to be compliant with four out of the five standards inspected on the day. However the service was assessed non-compliant with the requirements in relation to staffing, which state that there should be enough members of staff to keep people safe and meet their health and welfare needs. The CQC said: “The provider was not meeting this standard. There were not always enough qualified, skilled and experienced staff to meet people’s needs”. The CQC report had highlighted a concern that had already been recognised by the management team who have responsibility for wards at Moseley Hall Hospital, West Heath Hospital and the Sheldon Unit. A review of staffing had already been undertaken and a plan formulated to not only increase staff levels but also to ensure the right mixture of nursing staff to fully meet the needs of our patients. In addition our plans include displaying welcome posters and information signposting patients and families to whey they can find information about care and treatment plans. We have also put in place procedures for ensuring staff document that they have discussed the treatment plan with the patient and family. We have measures in place to ensure that these plans are being followed including audit and conversations with our patients to ensure they understand their care and treatment plans. The CQC will reassess sometime during 2013. 59 West Midlands Quality Review Service The West Midlands Quality Review Service (WMQRS) is a collaborative venture supported by PCTs and Trusts in the region. The service will help support organisations in ensuring they have a robust framework of quality assurance across their portfolios of services and will: • develop evidence-based Quality Requirements • carry out developmental and supportive quality reviews • produce comparative information on quality of services • provide development and learning for all involved. The aim of WMQRS is to support organisations in improving the quality of health services by undertaking clinical reviews of the quality of clinical services. In particular, WMQRS aims to: • ensure services/care pathways are as safe as possible • improve the quality and effectiveness of care • improve the patient and carer experience • undertake independent, fair reviews of services • provide development and learning for all involved • encourage dissemination of good practice • support and add value to organisations’ own clinical quality. During January 2013, the Adults and Community Division and Rehabilitation Services within the Specialist Services Division both participated in an external review carried out by the West Midlands Quality Review Service. The Trust is currently awaiting the publication of the report which will be received by the Board and published on our website. Details of the findings and actions taken will be included in next year’s Quality Account 2013-14. 60 Section 3 • • Review of quality in clinical services - National quality indicators - Snapshots of quality improvements during 2012-13 - Investments in our Trust Assurance process • Statements received from external organisations • Acknowledgements • How to provide feedback • Glossary • Membership form 61 Review of quality in clinical services - National quality indicators Indicator Meticillin-resistant staphylococcus aureus (MRSA) new bactereamia Annual target Month 12 position 1 1 Clostridium difficile new cases ≤24 ≤24 Methicillin-sensitive Staphylococcus aureus (MSSA) new cases ≤3 ≤3 Escherichia coli (E. Coli) new cases ≤14 ≤14 100% 100% ≤14 32 Elective meticillin-resistant staphylococcus aureus (MRSA) screening Falls resulting in severe injury or death Grade 3 or 4 avoidable pressure ulcers community (quarter total) ≤27 in quarter 4 ≤27 in quarter 4 (see page 32) Grade 3 or 4 avoidable pressure ulcers inpatients (quarter total) (see page 32) 0 in quarter 4 1 in quarter 4 100% compliance with WHO surgical checklist 100% 100% Number of Serious Incidents reported in 48 hours 100% 100% 0 2 % Serious Incidents Root Course Analysis completed in timescale 100% 100% NHS Safety Thermometer (HarmFREE Care) 95% 95% Attendance at mandatory training (recovery) 85% 88% Medical appraisals 95% 81% ≤9.48% 8% Essential care indicators (aggregated measure) (see page 67) 95% 93% % staff appraised (within 18 months) (recovery) 85% 85% Number of complaints acknowledged within 3 days 100% 100% % complaints responded to within ≤ 6 months or as agreed 100% 100% 18 week pathway (admitted patients) 90% 95% 18 week pathway (non-admitted patients) 95% 97% 18 week pathway (incomplete pathways) 92% 99% Cancer referrals (urgent 2WW) 93% 100% Customer experience - patient surveys completed in all areas in past 12 months 100% 100% 44 60 <30% <30% ≤3.39% ≤5.60% Number of Never Events (see page 77) Spend on temporary staffing Net promoter score Acute admission avoidance 1 month in arrears % sickness absence (1 month in arrears) (Recovery) Further details around the full range of indicators reported to the Board through the Trust Quality and Performance scorecard can be found on our Trust website via the following link http://www.bhamcommunity.nhs.uk/ 62 National quality indicators Indicator: The data made available to the National Health Service Trust or NHS Foundation Trust by the Health and Social Care Information Centre with regard to the percentage of patients on Care Programme Approach who were followed up within seven days after discharge from psychiatric in-patient care during the reporting period. Birmingham Community Healthcare NHS Trust considers that this data is as described for the following reasons: • 100 per cent compliance has been achieved throughout 2012/13. Birmingham Community Healthcare NHS Trust has taken the following actions to continuously maintain 100 per cent compliance, and so assure the quality of its services, by monitoring and reviewing compliance both internally and externally with Commissioners. % of patients followed up in seven days of discharge 2012-13 2011-12 100 Data was not required to be collected Indicator: The data made available to the National Health Service Trust or NHS Foundation Trust by the Health and Social Care Information Centre with regard to the percentage of staff employed by, or under contract to, the Trust during the reporting period who would recommend the Trust as a provider of care to their family or friends. Birmingham Community Healthcare NHS Trust considers that this data is as described for the following reasons: The national staff survey report published by the Department of Health shows scores against 28 key findings. Key finding 24 is known as the ‘friends and family test’; the wording being ‘staff recommendation of the Trust as a place to work or receive treatment’. For the national report, key finding 24 is calculated from three questions within the staff survey: • Q12a: care of patients is the Trust’s top priority • Q12c: I would recommend the Trust as a place to work, and • Q12d: if a friend or relative needed treatment, I would be happy with the standard of care provided by this organisation. 63 The national report is based on feedback from a random sample of 850 staff that completed the survey. For the 2012 survey BCHC chose to survey all staff. Therefore, we have two sets of data which is as follows: 1. The national score for Key Finding 24 (as a number where 1 is worse and 5 is good): 2011 score for Key Finding 24 2012 score for Key Finding 24 Comparison group (20 other community Trusts) 3.50 3.30 3.58 2. The breakdown of the results for each of the questions is as follows: Question 2011 score 2012 Sample score 2012 Census result 12a: care of patients is the Trust’s top priority 58 55 57 12c: I would recommend the Trust as a place to work 52 40 45 12d: if a friend or relative needed treatment I would be happy with the standard of care provided by this organisation 63 56 59 However, additional local questions included in the survey indicated that: • 82 per cent of patients/service users were involved in decisions about their care and treatment with 92 per cent being treated with respect and dignity and 70 per cent receiving enough emotional support • 82 per cent of patients/service users were given enough privacy when being examined or treated with 79 per cent having confidence and trust in clinicians working for the Trust • for 84 per cent of patients/service users, their safety is a priority for staff in the organisation, and • 78 per cent of patients/service users are given enough information about their condition/treatment with 66 per cent receiving consistent information about their treatment by different staff members, and 74 per cent receiving answers they could clearly understand when they ask a clinically important question. Birmingham Community Healthcare NHS Trust intends to take the following actions to improve the above scores, and so the quality of its services: • The organisation has devised a three point action plan to focus on short term actions which will impact on the outcomes of the survey. • In addition the Trust is revising its Organisational Development Strategy which will incorporate longer term goals. • We are looking at divisional variances for these indicators and developing local actions with each area for addressing this. Going forward this will include further staff engagement to fully understand the reasons behind these results. 64 Indicator: The data made available to the National Health Service Trust or NHS Foundation Trust by the Health and Social Care Information Centre with regard to the percentage of patients who were admitted to hospital and who were assessed for risk of venous thromboembolism (VTE) during the reporting period. Birmingham Community Healthcare NHS Trust considers that this data is as described for the following reasons: • Increased compliance of above 90 per cent of all inpatients who were admitted into our care receiving a VTE risk assessment. Birmingham Community Healthcare NHS Trust has taken the following actions to improve on the average rate of VTE risk assessment from 92 per cent in 2011-12 to 97.5 per cent in the reporting period 2012-13: The clinical staff, through doctors and the matron’s clinical leadership, have made and sustained improvement for this safety measure this year in the following way: By regular feedback to the medical and nursing teams they are able to quickly identify any gaps if they are not 100 per cent compliant with their assessment. Dr Martin Goodman Clinical Director for Adults and Community Division Doctors, nurses and pharmacists are included in the improvement programme and this has been a good example of multidisciplinary working that has made a difference. The Trust has a VTE Reference Group chaired by Dr Goodman that has steered the work programme and helped to bring together the work of all the health professionals. BCHC’s VTE prevention programme supports the implementation of the national guidance that that every adult patient undergoes an assessment of their risks of developing a blood clot and bleeding whilst in hospital. Patients are then prescribed prophylaxis if appropriate. The purpose of VTE prevention is to reduce the risk of venous thromboembolism - deep vein thrombosis (DVT) and pulmonary embolism (PE) and save lives and avoid long term ill health. We have developed a VTE root cause analysis tool used to identify any lessons that can be learned if a patient develops a DVT or PE whilst in any of our hospitals or intermediate care units. 65 Indicator: The data made available to the National Health Service Trust or NHS Foundation Trust by the Health and Social Care Information Centre with regard to the rate per 100,000 bed days of cases of clostridium difficile infection (CDI) reported within the Trust among patients aged two or over during the reporting period. Birmingham Community Healthcare NHS Trust considers that this data is as described for the following reasons: • Reduction of clostridium difficile cases on average for the reporting year 2012/13 being 1.22 in comparison to 1.62 in 2011/12. Birmingham Community Healthcare NHS Trust has either taken or will be taking the following actions to improve the 1.22 rate and so the quality of its services, by: • Clostridium difficile guidelines written in 2012 in line with DH Guidance • RCAs completed on all cases of CDI. Rolling out table top review process across the Trust 2013-14 • essential steps CDI Care Bundles are being rolled out across the inpatient facilities • all patients confirmed Clostridium difficile toxin positive receive a CDI passport • Hydrogen Peroxide Vapour (HPV) System used for terminal cleaning of Clostridium difficile patient rooms following outbreak in an inpatient area • two HPV machines now purchased by the Trust, staff are currently awaiting training on this equipment • customised training for areas on specific Infection Prevention and Control issues • cleaning review currently being undertaken by Adults and Community Division • audit programme revised to include one all-encompassing environmental infection prevention control audit tool, with essential steps observational audits • the audit tool flow chart now incorporates feedback to relevant leads detailing escalation process • Clinell universal sanitising wipes rolled out for decontamination of nursing equipment but not for use with CDI patients • implementation of Sporicidal wipes for use with patients who have CDI or suspected CDI • admission risk assessment of healthcare-associated infections (HCAIs) to be implemented in 2013-14 • Clostridium difficile e-learning training being developed in 2013-14. 66 Indicator: The data made available to the National Health Service Trust or NHS Foundation Trust by the Health and Social Care Information Centre with regard to the number and, where available, rate of patient safety incidents reported within the Trust during the reporting period, and the number and percentage of such patient safety incidents that resulted in severe harm or death. Birmingham Community Healthcare NHS Trust considers that this data is as described for the following reasons: • The percentage of patients related resulted in severe harm or death has remained consistent over the last two reporting periods (please see table below). Birmingham Community Healthcare NHS Trust intends to take the following actions to improve the 1.4 per cent rate of incidents and so the quality of its services, by improving on the 1.4 per cent rate of incidents which result in severe harm by continuing to develop a number of initiatives to reduce patient harm, including the work around the elimination of pressure ulcers, preventing falls, catheter acquired infections, medicines management and sharing lessons learnt. Year Total incidents Severe harm/death % 2011/12 4925 68 1.4 2012/13 5192 71 1.4 Essential care indicator 2012-13 performance: Environmental criteria 95% target 88% achieved Falls assessment indicator criteria 95% target 95.8% achieved Medicines management criteria 95% target 95.6% achieved Nutritional criteria 95% target 92.1% achieved Patient observations indicator criteria 95% target 93.4% achieved Tissue viability indicator criteria 95% target 93.7% achieved 67 Essential care indicators (ECIs) The ECIs are a set of metrics for assessing the quality of care plan and assessment tools used to manage fundamentals of care. They were initially developed as nursing metrics in Blackpool and Fylde NHS Trust and have been adapted by BCHC for use in adult inpatient units, district nursing and integrated multidisciplinary teams and bedded units for people with learning disabilities. The reports from these metrics form a key part of the monthly quality reporting for the Board and are also fed back to teams and operational managers for rapid improvement. The metrics are collected monthly and are used as one of the early warning signs to tell us where teams need more support or further assessment of standards. In 2012/13 we have reported on the following trends and initiatives for the ECIs: • adult bedded units showed a steady improvement in compliance throughout the first eight months of the year with good levels of compliance achieved for the majority of units across all the standards • following the introduction of care rounding in the adult bedded units, the metrics were changed to capture information about the quality and completeness of the care rounding documentation. This has resulted in a fall in the overall compliance for one of the sections of the indicators since January 2013 and is being addressed by a review of the process and documentation used for care rounding • there has been a fall in the overall compliance for the majority of adult bedded units in the last two months of the year. A series of measures have been put in place to improve the compliance, including further training, improvements to documentation and the use of additional local weekly checks on compliance carried out by clinical teams to check their progress • Learning Disability Services and integrated multidisciplinary teams have now moved to monthly checks of their compliance with these metrics • further refinement of the standards are being undertaken for the use of ECIs in Learning Disability Services and integrated multidisciplinary teams to ensure that the metrics are focused on the key elements of patient safety for these services. BCHC is the first organisation to expand the use of these metrics into learning disabilities and community-based teams • we have developed a dashboard tool for reporting the results of the ECIs and this is now in place on our internal website with access for all staff. Lisa Eden Associate Director of Therapies 68 Patient-led assessments of the care environment A new patient-led approach to assessing key care quality indicators in hospitals has been launched for 2013. Patient-led assessments of the care environment (PLACE) replace patient environment action team (PEAT) inspections, which have been carried out annually in inpatient healthcare sites with more than 10 beds since 2000. From April 2013, the new PLACE system will report publicly on standards of care in all hospitals, hospices and independent treatment centres providing NHS-funded care. The annual assessments will see members of the local community such as patients, relatives, carers and HealthWatch or patient involvement and action group members go into hospitals as part of teams to report on the overall care environment and assume lead responsibility for writing the reports of their findings. The Trust has already had more than 50 expressions of interest in taking on the role. Clinical care or the practice of members of staff are not subject to the assessments but the intention is that, by providing direct feedback from service users, the reports will represent a valuable driver of service improvement. PLACE teams will focus particularly on how well sites maintain and protect patients’ privacy and dignity; the quality of food provided; how helpful signage, access arrangements and transport facilities are; and the general standards of cleanliness and maintenance in inpatient sites such as Moseley Hall or West Heath Hospital and our intermediate care units. In the new PLACE process, Trusts are allocated dates to complete the assessment from April to June 2013 and the results of the PLACE programme were not available at the time of reporting for this Quality Account. The PLACE assessments which will be undertaken during 2013-14 will be therefore reported within the Quality Account 2013-14. Same sex accommodation: declaration of compliance 2012-13 BCHC is pleased to confirm that we are compliant with the government’s requirement to eliminate mixed-sex accommodation, except when it is in the patient’s overall best interest, or reflects their personal choice. Every patient has the right to receive high quality care that is safe, effective and respects their privacy and dignity. Birmingham Community Healthcare NHS Trust is committed to providing every patient with same sex accommodation, because it helps to safeguard their privacy and dignity when they are often at their most vulnerable. We have the necessary facilities, resources and culture to ensure that patients who are admitted to our hospitals will only share the room where they sleep with members of the same sex, and same-sex toilets and bathrooms will be close to their bed area. Sharing with members of the opposite sex will only happen when clinically necessary (for example where patients need specialist equipment such as in the provision of specialist bathrooms which cannot be designated as single sex), or when patients actively choose to share. This achievement is regularly monitored and if our care should fall short of the required standard, we will report it. We have also set up an audit mechanism to make sure that we do not misclassify any of our reports. The review of compliance forms part of our annual audit programme and each bedded unit has had an assessment following the template developed by the NHS Institute for Innovation and Improvement. This audit has both confirmed overall compliance and identified areas for further improvement in privacy and dignity with respect of delivering same sex accommodation. Developments in 2012/13 include the purchase of bed area curtains with embroidered privacy signs to remind staff not to enter the area without permission, and improve signage for toilet and bathroom facilities. 69 Engaging learning listening improving. A word from Brian Hanson, Chair of the Public Involvement Action Group (PIAG): Patients and the public now have the opportunity to contribute to how the Trust is being run by being included in committees where such topics as patient safety, quality, infection prevention and control and quality of food are discussed. The lay members are able to bring their experience and knowledge as well as a patient’s perspective in commenting upon the work done by the committee. One such particular public participation group is PIAG. This meets every month and frequently involves the CEO and the Chairman of the Trust who report on progress towards being a Foundation Trust. We always welcome new members and, I’m sure they are likely to find the discussions both interesting and lively. To get more information telephone 0121 465 7810 or email: adam.dandy@bhamcommunity.nhs.uk Peter Mayer, member of PIAG: Since I retired in 2007 from my post as a specialist in geriatrics and stroke medicine I have become involved in groups which represent patients and clients of health and social care. I joined PIAG as a representative from the advisory committee and have found it one of the best organised meetings. The NHS staff have ensured that timely and necessary information and changes to structures and services are presented in a clear and understandable way to the members who are active advocates of their areas and organisations. We all feel we not only learn about what is happening in the Trust and its services but further that we contribute to improving and developing those services for patients and those caring for them. I was delighted that a route to be involved in the board’s deliberations became available through standing as a public governor and even more delighted to be elected. It is a real privilege to return to oversee the unique and important services the Trust manages and to assist in maintaining the high quality we deliver and in developing new services in Birmingham and surrounding areas. We really care for and respect those we serve and already work closely with the primary care teams now integral to the new clinical commissioning groups. I will be a pathway for representing the views of the people of South Birmingham that inform the Trust’s services in continuing to meet the needs of its patients and their carers. 70 Compliments: some examples … Diabetes - East and North Locality: Excellent service. The diabetic nurse I saw was helpful, patient and informative and also went through the choices which were convenient for me taking into account my life styles, comfort, preference of treatment and more importantly, listened to me. Birmingham Dental Hospital (Oral Medicine and X-Ray Department): Thanks to all! Excellent healthcare provision. All staff are to be commended for their friendly, reassuring manner. Great to be cared for in a dignified way. Ward 14 Moseley Hall Hospital: Everything went well, all the staff are very helpful and caring at this hospital. I feel very safe when am here and the quality of the food is excellent. I have recommended this hospital to my friends. Norman Power: The environment and accommodation has been good and welcoming. Cleanliness of the room and bathroom. I would like to acknowledge the hard work of the domestic staff. Ann Marie Howes: On arrival I was unable to walk, had very poor upper body mobility and needed help in all aspects. Due to the excellent care that I received this has now changed and I am now able to do far more for myself and walk with a Zimmer frame. None of this would have been possible without the hard work and dedication of all here. Community Podiatry: I have already written several months ago to commend the exceptionally HIGH STANDARD of care I have received from all the staff. They are outstanding, highly trained professionals. Child Development Centre Castle Vale: We just want to say thank you for all the great work you all have done for our child and the team have always made us feel like you really care and not just doing your jobs. Every week my child is progressing brilliantly and that’s due to you helping by pointing us in the right direction. 71 Customer Service (formerly known as Patient Advice and Liaison Service - PALS) The Customer Service team supports BCHC in improving services for patients. It provides confidential impartial advice and support to patients and staff, helping to sort out concerns or queries people have about their care and treatment. The team also help enquirers navigate the services provided by the Trust and signpost them to appropriate points of contact within the Trust. The Customer Service team is part of the wider Patient Experience Team for the Trust. Contact Customer Service: Tel: 0800 917 2855 Email: contact.bchc@.nhs.net Text: 07540 702 477 Service Number of enquiries Number excluding (including compliments compliments logged by PE Team) None BCHC services 329 329 • Birmingham Dental Hospital 456 418 • Combined Community Dental 55 31 • Learning Disability Services 34 19 • Rehabilitation Services 177 139 Children and Families Division 312 249 Adults and Community Division 1039 966 Total 2402 2151 Specialist Division: 72 Call received Response Appointment systems and appointment correspondence. Amended wording in appointment letters; training for staff to improve verbal communication with patients; central booking service introduced in several community services. Cleanliness of corridors and general décor of Ward 9 (Moseley Hall Hospital). The feedback was discussed with the clinical team; repairs immediately made; environment was cleaned; arrangements made for further decorative / remedial building work. New bay created which would allow for patients with different needs to have more privacy and dignity and more space. Patient satisfaction We measure patient satisfaction a number of ways: • patient surveys - overall satisfaction and net promoter score • customer Service / PALS • compliments • complaints • other feedback (NHS choices / patient opinion, listening to you / help us to help you) • events / public engagement / focus groups / user groups. Below are some examples of the lessons learnt from the feedback we receive: • check relatives understanding of post-operative instructions and clarify if they have any further questions • parents to be advised in advance and prepared for the potential for their child to be upset and confused following anaesthetic • ensure letters sent out without delay and within 2 weeks of dictation - urgent work is picked up immediately by a colleague in the absence of the medical secretary • develop a hand-out for bank staff to detail general information regarding ward and systems in use and the vital importance of completing records of fluid intake • ensure waiting areas are checked to confirm patients are waiting in correct area • staff to clear away spillages and remove and dispose of used bed pans, continence products and tissues promptly; staff to wear gloves when administering intravenous (IV) injections • indicate the day of the week as well as the date when booking appointments to reduce risk of error in booking appointment • reminder to staff that ID badges should be visible at all times • clinician has undertaken a clinical assessment exercise as learning tool and constructive feedback given • staff reminded of importance of patient having opportunity to rinse mouth. 73 Complaints Division Number of complaints (12/13) Number of com- Number of complaints shown as plaints shown as rate per 10,000 rate per 10,000 contacts 2012-13 contacts 2011-12 Adults and Community Division 99 1 1 Children and Families Division 27 1 1 • Birmingham Dental Hospital 38 3 4 • Combined Community Dental Services 6 1 2 • Learning Disability Services 9 1 2 • Rehabilitation Services 19 3 3 Total 198 1 1 Specialist Division: Of over 2 million contacts per year we can see that less than one per cent of those result in dissatisfaction for our service users, carers or relatives. Overall, the figures show a minor improvement with a fewer number of complaints recorded. BCHC is committed to thorough and detailed investigation of each complaint and learning from such complaints, all of which are reviewed and signed personally by our Chief Executive. Our Associate Director of Patient Experience reviews complaints and shares lessons learnt across the organisation to minimise the likelihood of reoccurrence of the cause for complaint. Jo Thurston Director of Compliance and Assurance 74 Complaints and lessons learnt (top four complaint themes) 1. Attitude and behaviour of staff Specific actions for individual cases: Observation of (and feedback to) reception areas at Birmingham Dental Hospital (BDH); observations in Orthodontics at BDH; iCARE / customer care training - Birmingham Wheelchair Services, central booking (Children and Families Division), Perry Trees, health visiting teams, wards 10 and 12, inpatient neuro rehabilitation unit (INRU); BDH; 1:1 coaching and mentoring for specific staff following complaints; performance management of specific staff following complaints; Lazarus Consultancy programme for BDH staff and manager; increased staffing levels for inpatient units. Trust wide actions: iCARE training in induction; patient experience team members provide support at Being Open Meetings and ad hoc advice and support to service managers and leads around how to manage difficult situations; neuro linguistic programming (NLP) training for staff and managers across BCHC; coaching and mentoring programme. 2a. Poor / lack of communication: not responding to emails / letters / phone messages Specific actions for individual cases: as above plus additional temporary post funded in BDH to address backlog of calls and to review systems to identify and enable rectification plans; support by customer services team to facilitate communication as necessary; improved correspondence with parents and information about waiting times for speech and language therapy; inpatient information pack contains details of how relatives can contact consultant; dignity champions introduced to a unit where these were not in place, customer care standards discussed at team meeting for relevant team. Trust wide actions: as above. 2b. Poor / lack of communication: unable to contact services by telephone Specific actions for individual cases: patient experience team took details of patients contacting the customer services team and asked central booking staff to telephone patients in the afternoons when the booking line was not open to incoming calls; additional temporary post funded in BDH to address backlog of calls and to review systems to identify and enable rectification plans; support by customer services team to facilitate communication as necessary. Trust wide actions: redesign programmes need to impact assess at the outset how any changes will affect patients’ experience and how to mitigate against these. This process is in place for Cash Releasing Efficiency Savings (CRES) programmes which directly link to many redesign programmes but which tend to look at the overall patient experience rather than the more detailed stages of the patient journey at critical stages of the redesign. 3. Access to and waiting time for appointments: waiting time for assessment / treatment / appointments Specific actions for individual cases: parent telephone survey in speech and language therapy to seek further feedback about waiting times and evaluation of service received as part of a service review. On-going discussions with commissioners. 4a. Clinical care: insufficient staffing in inpatient areas Specific actions for individual cases: review of establishments with regard to patient need, with recommendations for revised staffing levels for inpatient areas. 4b. Clinical care: food served in inpatient areas Specific actions for individual cases: mealtime audits taking place as part of the fundamentals of care work stream. 75 Incident reports An incident is any event which has given rise to actual harm or injury or to damage/loss of property (Ref: NHS Executive). This definition includes patient or client injury, fire, theft, vandalism, assault and employee accident. It also includes incidents resulting from negligent acts, deliberate or unforeseen. Incident by type Total 2012-13 Total 2011-12 Confidentiality, data and information governance 233 244 Fire safety 31 42 Infrastructure 194 408 Medication, medical gas, medication delivery system 548 523 Patient incident 5192 4929 Security 258 305 Staff, visitor, contractor incident 1482 955 Total 7938 7404 Incident by type Patient Incident Staff, visitor, contractor incident Medication, medical gas, medication delivery system Serious incidents Top 3 Categories Total Care delivery (including pressure ulcers) 1918 Slips, trips and falls 1566 Admissions, transfer, discharge, access to services 418 Violence, abuse assault 482 Staffing levels 432 Needle stick (sharps) incident 125 Administration 218 Preparation/dispensing 116 Prescribing 71 338 A serious incident is • an accident or incident when a patient, member of staff (including those working in the community), or a member of the public (including contractors) suffers serious injury, major permanent harm or unexpected death (or the risk of death or serious injury) on either premises where healthcare is provided, or whilst in receipt of healthcare, or • any event where actions of health service staff are likely to cause significant public concern • any event that might seriously impact upon the delivery of services and / or which is likely to produce significant legal, media or other interest and which, if not properly managed, may result in loss of the Trust’s reputation or assets • damage or loss to property by fire, flood, theft or negligent, deliberate or unforeseen act. 76 Incident Type A&C* BDH* C&F* CCDS* Absconded patient LD* RS* 1 1 2 1 1 Accident whilst in hospital Allegation against HC professional (assault) Total 1 1 Assault by inpatient (in receipt) 1 1 Assault by inpatient (not in receipt) 1 1 C. Diff and health care acquired infections 2 1 Confidential information leak 3 2 Dentistry 1 Dentistry (‘never event’ - see page 77 for details) 1 2 1 1 2 Drug incident (general) 1 1 Drug incident (insulin) 1 1 MRSA bacteraemia 1 Pressure ulcer - grade three 172 Pressure ulcer - grade three/four 7 Pressure ulcer - grade four 91 Safeguarding/bogus health worker 1 Slips, trips and falls 29 172 7 1 92 1 2 Unexpected death 1 32 1 Ward closures 15 Grand total 322 1 1 2 4 16 1 5 4 338 * A&C - Adults and Community Division * CCDS - Combined Community Dental Services * LD - Learning Disability Services * BDH - Birmingham Dental Hospital * C&F - Children and Families Division * RS - Rehabilitation Services Across the Trust, 80 per cent of all serious incidents relate to the development of pressure sores either in a patient’s home or within an in-patient setting. The Trust Pressure Ulcer Prevention and Management work programme continues to be a high priority across the Trust and has focused on the delivery of the CQUIN and the ambition for the elimination of grade 3 and 4 pressure ulcers. Clinical staff have worked consistently hard across our inpatient services to ensure that these incidents are identified and appropriate care and treatment plans are in place. Effectiveness of these measures is monitored through the CQUIN scheme and essential care indicators. We have put in place a number of mechanisms to reduce the number of incidents, specifically we: • have established a Tissue Viability Reference Group to provide leadership and expert support for staff • have established common themes within root cause analysis that are developed, and have shared learning • use guidelines consistently and evaluate risk assessment tools and care plans. 77 Never events ‘Never events’ are serious, largely preventable patient safety incidents that should not occur if the available preventative measures have been implemented by healthcare providers. During the period 2012-2013, The Trust had two ‘never events’, both of which related to ‘wrong site surgery’ involving dental surgery. One of the incidents took place within the Combined Community Dental Services, whilst the other occurred at Birmingham Dental Hospital. The definition of ‘wrong site surgery’ is: a surgical intervention performed on the wrong site (for example wrong knee, wrong eye, wrong patient, wrong limb, or wrong organ); the incident is detected at any time after the start of the operation and the patient requires further surgery, on the correct site, and/or may have complications following the wrong surgery. In both cases, the wrong tooth was extracted. Both ‘never events’ have been subject to root cause analysis and have been examined by an Independent Inquiry Panel. Any learning has been shared to prevent reoccurrence. Understanding and learning from our incidents - patient incidents Slips, trips and falls are the highest number of recorded incidents, which is due to the relatively high proportion of elderly and rehabilitation patients cared for within our services. Significant work has been undertaken across all services to ensure that patients are appropriately assessed for their risk of falling on admission to hospital or on initial community services contact and that a suitable plan of care is implemented should patients be identified as being at risk. This work has been supported and monitored throughout the year through the CQUIN schemes and through essential care indicators. A falls reference group is now planning the initiatives to improve management of falls risk across the Trust. Incidents that occur at the point of care delivery. Further interrogation of these incidents shows that the majority of incident reported under this category are incidents of pressure sore development. The CQUIN scheme has significantly raised awareness of the need to report this type of incident and reporting figures have risen significantly throughout the year as a consequence. Further improvements have been made to the care plan documentation and to the patient information care bundles (Think SSKIN). In addition, there is now a collaborative project with the local authority to support pressure ulcer prevention for people receiving social care services but with no current health involvement. This work is aligned with the “Your Turn” programme. Medication incidents The majority of incidents in this category relate to issues at the point that medication is/should be administered. Many of the incidents recorded report that medication has not been administered at the time it is due. The medicines management committee maintains an oversight of medication-related incidents in order to identify any themes. The committee works closely with services to identify lessons that can be learned and to prevent reccurrence. 78 Staff, visitor, contractor incidents Violence and abuse incidents against staff remain the highest reported incidents affecting staff. The majority of these incidents occur within either Learning Disability Services or within elderly inpatient services and are often related to the nature of illness / disability affecting our patients. Staff receive training appropriate to their service areas and client groups to help them to effectively manage this type of incident and much work has taken place within Learning Disability Services to demonstrably reduce the number and frequency of this type of incident. Where malicious violence is targeted against our staff, BCHC takes a strong stance. Staff are supported in a number of ways including counselling and occupational health services and by the local security management specialist should more formal action be required. Working with the NHS Commissioning Board Special Health Authority. On 1 June 2012 the key functions and expertise for patient safety developed by the National Patient Safety Agency (NPSA) transferred to the NHS Commissioning Board Special Health Authority. The NHS Commissioning Board Special Health Authority utilizes the National Reporting and Learning System (NRLS), the world’s most comprehensive database of patient safety information, to identify and tackle important patient safety issues at their root cause. NHS Trusts use this information to improve patient safety and compare safety incident reporting trends with other organisations. NPSA data is indicative of a positive reporting culture. Experience in other industries has shown that staff are more likely to report incidents as the organisations reporting culture matures. This reflects a safer organisation where staff collectively have safety at the forefront of their minds and know they will be fairly treated if they report an incident. Learning from incidents is shared with staff throughout the Trust to improve safety and prevent harm. The most recent ‘organisation patient safety incident report’ from the NHS Commissioning Board Special Health Authority relating to the Trust for the period 1 April 2012 30 September 2012 is detailed to the right. This data shows that the Trust reporting rate is 51.1 incidents per 1,000 bed days, compared to 53.3 incidents per 100 bed days for the same period in 2011. 79 Staff survey feedback Each year NHS organisations across the country ask their staff to participate in a national survey. The results are used by organisations primarily to help them improve the working lives of staff and their experiences in the workplace in order to support them to provide safe and high quality care. The results of the survey are also used to: • • • • inform our patients, service users and the public of how we are regarded by our employees help the Trust monitor how national standards for quality and safety are achieved provide the Department of Health with benchmarking information make improvements to services and develop policies and procedures. Staff survey: turning feedback into action Thank you to all those who responded to the 2012 staff survey. For the first time, the survey was sent to all staff and the Trust achieved an overall response of 45 per cent which is a total of 2,077 responses (more than double previously received). The Trust looks forward to working with colleagues to turn feedback into action. Here are some of the things that have been improved during 2012 as a result of staff feedback from the previous survey: Staff said: I would like the quality of Performance Development Reviews (PDRs) to be improved We have: • Reviewed the PDR process and documentation to help make the process more meaningful • Continued to promote and monitor PDRs undertaken working towards compliance of 85 per cent Staff said: I want incident reporting procedures to be fair and transparent We have: • Made sure risk management reports produced include actions taken following incidents reported • Made sure the approval process encourages concerns to be raised with openness and transparency Staff said: The Trust should increase number of staff who have undertaken equality and diversity training 80 We have: • Provided a range of training available which has been undertaken • Ongoing communication of training available through e-newsletter Key findings for 2012 The NHS Constitution sets out a number of commitments and pledges to patients and the public, and also to its own staff. Those relevant to the Staff Survey and how well BCHC scored are set out below. We are looking at divisional variances for these indicators and developing local actions with each area for addressing this. Going forward this will include further staff engagement to fully understand the reasons behind these results. NHS constitution What staff said 2011 2012 Indicator results results Commitment 1: 64% 62% • Staff have a comfortable working space provide a good • Staff have a clean work space 73% 75% working environment. • Staff have the right equipment to do their job 67% 63% • Staff feel safe and secure in their working environment Commitment 2: 25% 25% • Staff working part time provide flexible • Staff saying their line manager was 74% 71% working opportunities. supportive in a personal crisis Commitment 3: * 89% Staff who have never: have healthy and safe • Experienced physical violence from the public 98% working conditions • Experienced physical violence from colleagues and in particular an • Experienced harassment, bullying or abuse 72% environment free from from the public harassment bullying and • Personally experienced harassment, bullying 74% violence. or abuse from colleagues Commitment 4: Staff who have: staff will be treated fairly, • Not experienced discrimination from the 94% 93% equally and free from public discrimination. • Not experienced discrimination from 91% 91% colleagues Pledge 1: 68% 67% • Staff have clear, planned goals and all staff will have clear objectives roles and responsibilities. • Staff have a set of shared objectives 73% 73% where they work in a team Pledge 2: 80% • Staff who were satisfied with the quality of 87% jobs will be rewarding care they give for teams and individuals • Staff who feel their role makes a difference 88% 88% that make a difference to to patients patients. • Staff who were satisfied with the 42% 44% recognition they received for good work Pledge 3: 80% • Staff who have had an appraisal / review in 75% all staff will be entitled the last 12 months to personal development • Staff who said this helped to agree clear 76% 81% and training and line objectives management support • Staff who said that their manager 83% * to succeed. supported them to receive the training, learning or development identified within their appraisal Pledge 4: there will be • Staff who said their immediate manager 74% 71% opportunities for staff was supportive in a personal crisis to maintain their health • Staff who said they had felt unwell due to 32% 50% well being and safety. work related stress in the last 12 months * Indicates comparison with 2011 staff survey not possible due to change in the questions Continued... 81 NHS constitution What staff said Indicator Pledge 5: staff will be • Staff who said that they were encouraged engaged in decisions to work as a team that affect them and the • Staff who said they had clear feedback services they provide. from their manager • Staff who said their opinion was asked for before decisions were made that affected their work Pledge 6: staff will • Staff who said their role makes a difference be empowered to put to patients/service users forward ways to deliver • Staff who said they had opportunity to better and safer services show initiative for patients. • Staff who said could make suggestions • Staff who agreed they were able to make improvements happen 2011 2012 results results 76% 66% 61% 47% 56% 46% 88% 88% 62% 65% 71% 72% Investors in People The Trust is pleased to announce that we have maintained our bronze award following the Investors in People (IiP) assessment. The Trust has yet to receive the full report, however areas of good practice that have been highlighted include: • • • • • • • • Trust values as driver for corporate planning and for patient care commitment, dedication and vocational drive of front-line clinical teams co-operative and supportive culture executive teamwork and strategic planning annual plans and objectives built around values and 6Ps focus on risk and compliance training and development - activity and central processes recruitment and Induction process. Some of the key priorities for the coming year include: • clearly define the leadership actions and behaviours expected of all people managers and ensure that they demonstrate them • senior divisional managers to be more visible at front-line and more supportive of junior managers and team leaders • clinical and admin teams to be better informed of reasons behind initiatives, decisions and directives, and more involved in discussions about them • more time to be devoted to people through team and 1:1 meetings • better recognition of the contribution people make. We will be also focusing on some key priorities around health and wellbeing (H&W) and these will include: • managers to include the H&W issues of their teams into their planning, to support and reflect the Trust’s H&W strategy • provide greater opportunities for people to discuss their individual and team H&W needs, not just when issues and problems have arisen, to bring about a more preventative culture. Progress against these will be reported on in the Quality Account 2013-14. 82 Equality and Diversity We are also committed to ensuring equality in all aspects of employment and service delivery. We continue to meet the milestones in the Equality, Diversity and Human Rights Strategy (EDHR) with updates against the implementation plan presented twice yearly. The Trust has also adopted the NHS Equality Delivery System (NHS EDS) and has completed the first self assessment, verified by local interest groups. The Trust scored achieving for all EDS outcomes. Feedback from the self assessment is used to inform the EDHR Strategy implementation plan. We expect our staff and service users to be treated with dignity and respect and we have an Equalities Policy and Anti Bullying and Harassment (Dignity at work) policy that have been developed within our overall Equality, Diversity and Human Rights framework. In the wider context we have an established Equality and Human Rights Analysis (E&HRA) framework which ensures that equality and human rights considerations are built into the development / design and delivery of Trust functions such as strategies, policies and services. This has been extended to include organisational change. We have seen a big increase in the percentage of staff that have completed their mandatory Equality and Diversity Training, with further equality training included within other training programmes including Recruitment and Selection and Management of Attendance. We are committed to providing support to employees with a disability and we have met our responsibilities under the Equality Act 2010 by ensuring that our Recruitment and Selection Guidelines, Management of Attendance Policy and Capability Policy reflect the legislation, and specific training has been provided for managers. We enjoy a positive working relationship with the Occupational Health Service and with our staff side colleagues, and have a well established Disability Initiative Group that comprises staff, service users and carers with a wide range of disabilities. Safeguarding adults The requirement to safeguard vulnerable adults has been highlighted in the national media over 2012/13 with the publication of a number of Department of Health reports into Winterbourne View Hospital. On 31 May, 2011 Winterbourne View Hospital was the subject of a BBC Panorama programme, “Undercover care: the abuse exposed”. The programme revealed shocking and disturbing scenes of the systematic abuse of vulnerable patients by the staff employed to care for them. During 2012/13 four key publications relating to Winterbourne View Hospital were published: • Department of Health Winterbourne View Hospital: Interim Report (June, 2012) • South Gloucestershire Safeguarding Adults Board Serious Case Review (August, 2012) • Report of the NHS Review of Commissioning of Care and Treatment at Winterbourne View (NHS South of England, August 2012) • Department of Health Transforming Care: a national response to Winterbourne View Hospital (December, 2012). Continued... 83 Safeguarding adults continued... As an Organisation, providing services to vulnerable adult, each of the reports and particularly the Serious Case Review has been examined in detail and key messages have been shared with the Trust Board, Trust Committees and sub Committees. Key messages have been incorporated into training packages and presentations have been delivered across the Organisation. The Specialist Division have base lined their Learning Disability Services against the recommendations and continue to actively monitor the quality of care provided to vulnerable adults. The Care Quality Commission unannounced inspection visits to Learning Disability Services have provided additional assurance that the organisation’s services to vulnerable adults meet regulatory and statutory requirements. During 2012/13 the safeguarding adult team have continued to implement the training strategy; e-learning programmes have been developed to improve clinical teams’ access to training and reduce their time away from delivering clinical care. The Birmingham Safeguarding Adult Board commissioned one Serious Case Review during the year which we contributed to. The Serious Case Review was published on the Safeguarding Adult Website on 25 April, 2013. The number of Dignity Champions across the organisation has increased to 60. Dignity Champions actively promote privacy dignity and respect in clinical areas, acting as role models and keeping privacy dignity and respect at the heart of patient services. Safeguarding children Compliance with the BCHC safeguarding supervision policy is monitored closely. Staff engaged with child protection cases receive mandatory one-to-one support and supervision and all Trust staff have access to safeguarding advice and practice support. A compliance baseline of 90 per cent and above has been achieved across the health visiting and school nurse and special school nurse workforce. The health visitor implementation programme has necessitated a programme of close safeguarding support for the newly qualified staff. Staff evaluation of the programme showed 100 per cent of the staff felt supervision had helped them focus on the needs of the child and 95 per cent better able to identify risk and concerns and move children forward more safely. Internal and multi agency evaluations of supervision are regularly undertaken to quality assure the process. Supervision constantly expands within the Trust. The named nurse team have supported staff in court attendances and in the preparation of over 300 reports for court or care proceedings this year, the volume reflecting the national increase in care proceedings. An expanded training menu of single and multi-agency opportunities is accessible for all staff. Workshops on sexual exploitation and the impact on children of parental alcohol use have been rolled out and BCHC named nurse team devised and leads new multi agency training for BSCB in respect of safeguarding children with disabilities. The serious case and domestic homicide review process is supported by the team. Daily integrated partnership working with the police and social care saw approximately 10,000 children identified at reported domestic abuse incidents assessed for risk and a joint pilot multi agency safeguarding hub (MASH) at Bournville Police Station has informed future joint working in the city. BCHC remains committed to working in partnership across the city to effect an improvement in the safety and wellbeing of children in Birmingham. 84 Who’s in charge? Raising awareness of the impact of everyday parental alcohol consumption on children BCHC Safeguarding Children team devised a project in September 2011 to raise awareness of the harmful impact of parental alcohol consumption in relation to the neglect children can suffer where parents consume alcohol above safe limits. Studies of findings from national and local Serious Case Reviews into the death or serious injury of a child show a worryingly increasing relationship between parental alcohol use and neglect, serious injury or the death of a child. Nationally, the identification of alcohol use as a risk factor has more than doubled from 10 per cent to 22 per cent (Brandon et al, 2010). A successful bid from the project team secured a £6,000 grant from the Birmingham Safeguarding Children Board (BSCB) to support the delivery of the proposed multidisciplinary project. School health nurses designed and delivered interactive awareness raising sessions to ‘young parents of tomorrow’, year nine and year ten pupils, in four pilot schools, which included the use of ‘beer goggles’ to perform tasks. The sessions were preceded by a new interactive drama workshop ‘One too many’ commissioned from Birmingham’s Loudmouth Theatre Group, depicting scenarios involving alcohol in which teens may find themselves. The evaluations to date are encouraging that such interventions are effective in enabling young people to say ‘no’ to alcohol. Signposting cards have been produced to support advice given to young people who attend school health ‘drop in clinics’, and posters for the foyers are planned. The health visiting service have been supported to initiate new parent routine screening and offer brief interventions where unsafe alcohol consumption is occurring. This has been supported by the delivery of workshops by the safeguarding team to enable all team members to screen for alcohol use and provide support to parents. To further aid awareness raising, toolkits have been developed for frontline health visiting teams to use with parents. With the use of ‘beer goggles’ parents can experience how alcohol affects their parenting ability through engaging in parenting tasks with a baby doll. In partnership with the BCHC Communications Team, a public campaign is developing. Asking ‘Who’s in Charge?’ through posters, the campaign aims to raise awareness of the dangers of drinking within the home whilst ‘in charge’ of children, to promote safer drinking practices. Posters and leaflets illustrate the ‘child’s voice’ in asking ‘Who’s in Charge’ when both parents are drinking within the home. Young people, parents, grandparents, professionals and voluntary sector partners have been involved in focus group work to inform the campaign message which will be launched in 2013. References: Brandon, M; Bailey, S; Belderson, P. (2010) ‘Building on the Learning from Serious Case Reviews: A 2-Year Analysis of Child Protection Database Notifications 2007-09. www.education.gov.uk/ publications, accessed 18 Jan 2013. 85 Snapshots of quality improvements during 2012-13 safetyeffectivenessexperience Safety Express Campaign PATIENTsafety Birmingham Community Healthcare’s plans for Patient Safety leads with the work of Safety Express, a part of ’The NHS Safe Care’ quality improvement workstream. Our aim is to work together and develop safer system in hospitals and in community settings with a shared aim of dramatically reducing harm from: • • • • hospital and community acquired pressure ulcers falls urinary tract infections in patients with catheters blood clots (DVT and pulmonary embolism) Harm from pressure ulcers, falls urinary catheters and venous thromboembolism is estimated to affect over 200,000 people each year and the estimated direct costs to the NHS is over £430 million per year. Our ambition is to eliminate harm from these conditions in 95 per cent of patients by December 2012. Early detection, action or treatment can eliminate preventable harm in these four key areas and improve patient care and comfort. All harms are interlinked. Safety Express is about working with the patient, family or carer to reduce harm and help patients to: • • • • eat well and drink the right amounts of fluid encourage regular movement and at the same time consider their environment and their risk of falling think about their medication, taking it at the right time consider their skin with particular regard to continence and moisture The Safety Express programme is simple and its key objective is to consider complications from a patient’s perspective. Staff are urged to stop dealing with safety issues in silos and aim for the absence of all four harms to each and every patient. 86 safetyeffectivenessexperience PATIENTsafety Safety Express Our driving force and our plan to reduce four harms Local clinical leadership Leadership and safety culture Walk rounds and rounding To deliver HarmFREE Care as defined by the absence of pressure ulcers, falls, catheter associated Executive support Active risk management Clinical care 95% reliable Continence, skin and moisture Nutrition/hydration UTI and venous thromboembolism. Medication reconciliation Supporting infrastructure Equipment Education and training We aim to deliver HarmFREE Care to our patients through the work of Safety Express with a plan that will be implemented locally and is part of existing work flow and routines. The above diagram gives us the key drivers bringing them together to achieve our aim. We are already making improvements in many of these safety areas. It is not about starting again...it is building on what we are already doing. 1. Use the safety information to identify where you need to make changes - have you had any new pressure ulcers this month? 2. Look at your essential care indicators to make sure your care is 95 per cent reliable. 3. Share the information with your team use their ideas for improvement and share top tips for success. 87 safetyeffectivenessexperience PATIENTsafety Care rounds - implementation at Birmingham Community Healthcare NHS Trust Birmingham Community Healthcare NHS Trust commenced care rounds In October 2011 as part of the launch of BCHC’s ‘trust me to care’ which formed a key part of the Safety Express programme and commitment to eliminating preventable harm. Care rounds aim to encourage frontline staff who undertake patient rounds (checking a patient’s medical status) to focus not only on health status, but also general care and comfort. The launch included all of the wards at Moseley Hall Hospital, West Heath Hospital and BCHC’s intermediate care units. The inpatient neuro rehabilitation ward commenced care rounds at the start of 2012 which meant that all of our inpatient units were involved in care rounds. Staff and patient questionnaires were used as part of the implementation to gain feedback as it was a new initiative and this feedback continues. Care rounds continues to take place on 100 per cent of BCHC’s wards/units. Implementation of care rounds is an intervention within the Trust’s Quality Strategy aiming to deliver our ambition and drive towards our aim of HarmFREE Care. BCHC is using the Safety Thermometer to measure the outcomes of the four harms, pressure ulcers, falls catheters and urinary tract infections and blood clots. Since implementing the Safety Thermometer as a measurement tool, the prevalence of HarmFREE Care has increased from 91.42 per cent in April to 94.43 per cent in November 2012. The Trust also uses incident reporting information, and the results of patient experience questionnaires to assess the effectiveness of care rounds. Within BCHC, we are routinely monitoring levels of patient falls, pressure ulcers, catheterassociated urinary tract infections and blood clots. The patient experience team has received positive feedback on care received. The metrics enables teams and the Trust to make changes where necessary. Recognising that sustainability is important and that there is a need to continuously focus staff on the usefulness of this structured approach to nursing interventions BCHC has set up an observational audit of care rounds using the Royal College of Nursing observational audit guidelines. Included in this is the opportunity for staff to make suggestions for improvements to care rounds and the care round tool. 88 safetyeffectivenessexperience Think...... S S K I N PATIENTsafety Stop the Pressure Birmingham Community Healthcare NHS Trust has been working alongside the Midlands and East Strategic Health Authority (SHA) looking at reducing harms occurring within healthcare. Pressure ulcers are one of the four harms identified through NHS Safety Thermometer and BCHC has signed up to a national initiative to eliminate all avoidable pressure ulcers. In April 2012, BCHC saw the launch of a pressure ulcer prevention campaign entitled ‘Think SSKIN’. This campaign concentrated on a bundle of care to prevent pressure ulcer development. The five elements of care are: Surface, Skin Inspection, Keep Moving, Incontinence and Nutrition/Hydration. The campaign consisted of patient guides for pressure ulcer prevention, leaflets encouraging communication between patients and community staff entitled ‘Tell Us’, SSKIN bundle charts to monitor the five elements of care and report back to community nurses if any problems arose and wallet size cards to alert other health care professionals that the patient had been identified at risk of developing a pressure ulcer. Over the last year there have been multiple initiatives and strategies put in place to achieve elimination of all avoidable pressure ulcers from BCHC care, examples overleaf. A launch of new care plan documentation and pressure ulcer prevention and treatment pathways linked into the Think SSKIN campaign has been very successful and rolled out across community patients and inpatients. The new tools were launched at a Stop the Pressure study event in September 2012. There was training on all of the new tools and opportunity to ask questions, there were clinical elements with training on pressure ulcer grading and assessment of moisture lesions, there were patient stories included throughout the day presented by DVD, and there was an accountability aspect with the presence of a coroner in the afternoon and a very realistic mock court scenario. In November 2012, BCHC launched a Pressure Ulcer Prevention Champion programme and asked for volunteers from each clinical area including the evening community nursing service, rapid response and complex care. The first of the monthly meetings was held in December 2012 and we introduced them to the ambition of achieving 100 days pressure ulcer free care from the 1 January, 2013. The monthly event is exciting and lively and brings up to 120 clinicians from both community and inpatient areas together to discuss strategies for eliminating all avoidable pressure ulcers within our care. The champions are a motivated and dedicated group of staff with the same passion to deliver high standards of care and eradicate harm. 89 safetyeffectivenessexperience Think...... S S K I N PATIENTsafety We are making excellent progress in our aim to eliminate avoidable pressure ulcers and the progress continues towards our aim to have 100 days pressure ulcer free across the organisation with 100 per cent of all attending clinical areas reporting on the day that they are up and running with their safety cross. Of the 42 areas represented at the February 2013 meeting, 86 per cent of those reported their safety cross had remained green since 1 January, meaning no avoidable pressure ulcers had developed in their care. The champion role is incredibly important to quality patient care and the drive in BCHC to always provide HarmFREE Care. The focus is on the key messages below and utilising support networks: • all clinical staff achieve a pressure ulcer prevention competency completed by the champion • all clinical areas have a visible board with a safety cross and relevant information to promote pressure ulcer prevention • all clinical areas have a pressure ulcer safety cross which is up to date and reflects the status of pressure ulcers in the team • champions are checking in handovers if the skin checks have been done • the events are an opportunity for champions to share good practice and overcome issues. At the February event 2013, all champions were given the opportunity to share ideas and innovative practice using a poster format and gallery walk with clinicians voting for the changes that inspired them or could be adapted into their area. Further examples of how teams have taken these initiatives forward in their local area have been included later in the Quality Account. Ward 4 Moseley Hall Hospital Love Your Skin theme display during the period near Valentine’s Day 90 safetyeffectivenessexperience Infection, prevention and control PATIENTsafety The Trust infection prevention and control team (IPCT) objectives are set to meet the patients’ needs and safety as a priority, thus underpinning the annual infection prevention and control (IPC) programme and reflects specific priorities and service objectives which will be monitored in-line with the audit calendar by the infection prevention and control committee. This programme supports: • compliance with the Health and Social Care Act (2008), National Health Service Litigation Authority (NHSLA) and the Care Quality Commission (CQC) • annual IPC training programme for community staff, patients and carers • working collaboratively within the divisions to roll out the Root Cause Analysis table-top review process as standard • an audit programme of antibiotic prescribing in-line with the Quality and Outcomes NHS Framework 2013-14 an environmental IPC audit tool which now incorporates feedback to relevant leads detailing the escalation process, covering preventing the spread of infection, urinary catheter management, enteral feeding and Clostridium difficile Infection (CDI) which will be rolled out across the Trust. Incorporating ‘My five moments of hand hygiene’ (Sax et al 2007; National Patient Safety Agency (NPSA) 2008) into our local hand hygiene policy; and using both the ‘Essential Steps to Safe Clean Care Observational Tool in Preventing the Spread of Infection’ and the ‘Lewisham Hand Hygiene Observational Tool’ in Combined Community Dental Services and the Birmingham Dental Hospital, has improved patient safety, patient experience, teamwork, communication and efficiency. The tools have enabled staff to discuss issues relating to hand hygiene objectively that previously were not expressed in the infection prevention and control link worker, team and audit meetings. The drivers for success to raise awareness of the importance of effective hand hygiene include: • the use of infection prevention and control link workers • engagement of clinicians at all levels within with the organisation, with support from executive leadership. Implementing the revised hand hygiene policy and observational tools has added value by embedding quality improvement into everyday clinical practice, compliance with national guidance, and assurance trust objectives around MRSA and Clostridium difficile remain within trajectory. Alert organism surveillance continues within the Trust and for 2012-13 the outturn figures were: • the total number of Clostridium difficile toxin positive cases for 2012-13 is 19 against a trajectory of 24 • the total number of MRSA bacteraemias for the year is one case of MRSA Bacteraemia against a trajectory of one • the total number of MSSA bacteraemia cases for 2012-13 is two • the total number of E.coli bacteraemia cases for 2012-13 is nine. 91 safetyeffectivenessexperience PATIENTsafety Ward 6 and the ‘Stop the Pressure’ collaborative. In August, Ward 6 at Moseley Hall Hospital were invited to participate in a collaborative programme facilitated by the Strategic Health Authority (SHA) called ‘Stop the Pressure’. The participants in the programme came from across the NHS Midlands and East and included acute trusts and community services. The aim was to eliminate avoidable pressure ulcers, a key quality indicator, by December by building on the heightened awareness of these painful and debilitating complications brought about by the Think SSKIN campaign. By meeting together the collaborative allowed the participants to learn from each other, and experts in the subject, how to embed into practice interventions which lead to improved results. The ward was represented by Sister Sinead Henson, Rehabilitation Assistant Sandra Josephs and physiotherapist Deb Skerrett, who brought back lots of ideas to the rest of the team. This led to an improved focus on and communication of patients risk factors at handovers, multidisciplinary meetings and via handover sheets and the patient status board. The ward learned the ‘See, Swarm, Solve’ approach where, if any member of staff spots skin damage, they get together with any available colleagues to devise a strategy for the individual patient to treat the problem and prevent worsening. Data collection showed that improved documentation of risk scoring and skin inspection and displaying the occurrence of any pressure damage on a safety cross enabled staff to see their progress. By being part of the collaborative staff saw their enthusiasm mirrored by colleagues and, as Sister Sinead Henson said: It really gave us a leg up to tackle the subject. 92 safetyeffectivenessexperience PATIENTsafety Patient Safety Award Perry Tree rehabilitation unit contacted the East and North Therapy Hub Team concerning a patient who was ready for discharge, but would need specialist support to go home. The patient had been treated to replace a hip joint, but had experienced problems and the joint had dislocated twice post-operatively. The hip joint was now stable, but this was being maintained by application of a special brace before getting out of bed, which also needed removal once in bed. The therapy hub manager and physiotherapist clinical lead visited the patient in Perry Tree, and together with the unit staff and the patient, worked out the key risks in going home and created a plan to address them. The main risk issue was found to be the safe application and removal of the hip brace to prevent further dislocations. The brace would need to be worn by the patient for a further six weeks and the patient was then going to see her consultant for a review. Because of the health need and particular risks involved for this brace application, the team agreed that it should be health staff to undertake the activity, and that individual training for the community health team providing the care would be required. The rehabilitation assistants in the East and North rapid response team were enlisted to provide the care to remove and apply the brace once the patient was home. The therapy hub lead worked with the Perry Tree therapy team to devise a training plan specific to the patient’s need and the manual handling risk advisor provided valuable assistance in providing the patient-specific training plan and worksheets for the team to use. The training for the rehabilitation assistants was provided by therapy staff in Perry Tree, and with the very kind tolerance of the patient, everyone was well prepared for the patient to come home. The occupational therapist at Perry Tree made sure all the necessary equipment was in place and the patient came home. The community rehabilitation assistants followed the care plan which was reviewed and monitored by her physiotherapist key worker from the therapy hub. The patient was safely discharged following review from her consultant as she had recovered well and no longer required her hip brace. This initiative won the BCHC Patient Safety Campaign award for 2012. Bev Ingram, Director of Nursing and Therapies said: Congratulations to the winning team, who embodied the philosophy of team-working while delivering a truly person-centred approach. 93 safetyeffectivenessexperience CLINICAL effectiveness Service improvements: Birmingham Dental Hospital, Primary Care Clinic and Healthcare Records Department: Walk-in Service In June 2012 the Primary Care Clinic and Healthcare Records Department reviewed and re-designed the service they provide for walk-in patients. This is part of our commitment to engage with service users and staff to identify and prioritise service improvements for enhanced patient experience. Prior to June 2012, Patients that used our walk-in service were presented with no first point of contact other than our main reception staff in the foyer where they receive their initial ticket for registering. These tickets are given out in numerical order from 7.30am onwards. The healthcare records staff and dental nursing staff for the primary care clinic did not start their day until 8.30am and the consultants start at approximately 9am. The problems identified from this process include: • the staff group at main reception are not qualified to give clinical information to patients • patients do not have anyone to speak to regarding their dental problems • no emergency triage for patients is available as no nurses are on clinic • patients could wait over one hour to speak to nurse/staff member. Staff were consulted and engaged in the redesign of the service at various stages following the suggestion of introducing a rotation system to rectify the above problems identified, whereby one member of the front desk healthcare records staff and one of the dental nurses would work together starting their shift at 8am and ending at 4pm. The new system was trialled for one week and reviewed with staff and it was acknowledged that patients were much happier knowing they had a member of staff on hand to speak to if they needed assistance prior to being seen on clinic. This includes access to clinical, general and appointment information and updating their personal details if required. Emergency patients e.g. swelling or trauma patients were getting triaged earlier as a dental nurse would be on standby for any clinical questions the healthcare records clerk could not answer. Staff also commented on how patients like to see a friendly face at the front desk rather than a darkened reception area as there was prior to these changes. It was also noted that when the additional Healthcare Records staff arrived on the front desk at 8.30am they were aware that the amount of patient queries had reduced due to the extra service provided from 8am to 8.30am. Following the positive feedback and great success from the trial of this new system, it was decided that this be rolled out as we see it working for the foreseeable future. With the new dental hospital building in focus we are looking at different ways of working and are now in the process of rolling out similar processes throughout the departments. 94 safetyeffectivenessexperience CLINICAL effectiveness Growing approval for adult care model The single point of access (SPA) for citywide adults and community services celebrated its first anniversary with evidence growing that, as GPs and other referrers become familiar with the system, patients are seeing real benefits to their care. That success has earned the Trust national recognition with Health Service Journal awards for efficiency and community service redesign. There are now 43 integrated multidisciplinary teams (IMTs) in Birmingham, each incorporating district nurses, case management, domiciliary physiotherapy, occupational therapy and community rehabilitation. Accessed by professionals through a single point of access telephone line for urgent- and non-urgent referrals, the model is designed to prevent avoidable hospital admissions by delivering high quality, flexible healthcare in the community. A bed bureau service for all Birmingham acute hospitals is also now provided through the SPA, with alternatives to admission being offered across the city where appropriate. And a team within the SPA now also co-ordinates alerts generated from the growing telemonitoring service for patients with long-term conditions. In a recent survey of 70 rapid response service patients, every respondent said they were treated in the most appropriate place to meet their needs and wishes. Nearly all felt the initial response had been sufficiently prompt and just over two thirds felt they would have needed hospital admission had it not been for the rapid response team. Over half rated their experience ‘excellent’, with the remainder judging it ‘good’ or ‘very good’. Intensive efforts have been made over the past year to engage with GP practices across the city and ensure the service is meeting their needs and that they understand its potential benefits. A recent survey of Birmingham GPs revealed high levels of satisfaction with the single point of access with the overwhelming majority judging it highly efficient and resulting in patients receiving the most appropriate care in the most appropriate place. Single point of access manager Emma Edgington said: We’ve come a very long way since the SPA was launched in October 2011. It’s been a very complex exercise - setting up the telephone service at Moseley Hall, engaging with our acute hospital partners, GPs and others to listen and explain why we believed in this model, and consulting with our own nursing and therapy teams to standardise a delivery model across the city based on the best practice from the three localities. A big ‘thank you’ goes to all those staff across the city who have helped to meet the challenges and make this service model - the first of its kind on this scale in the country - a success. 95 safetyeffectivenessexperience CLINICAL effectiveness The Libyan Conflict and the part played by the West Midlands Rehabilitation Centre in Birmingham. The conflict lasted months and cost thousands of lives, but ended the 42 year dictatorship of Colonel Gadaffi. The revolution made headline news across the world, but what was not so widely publicised was the devastation and suffering caused to the Libyan people. However David Cameron did recognize this suffering, when he made a public statement in Tripoli in December 2010, agreeing to offer humanitarian aid to the ravaged population of Libya. He agreed that the UK would provide care for 50 acutely ill people and 75 Amputees. The West Midlands Rehabilitation Centre was one of eight specialist centres across the UK selected by the Department of Health to provide amputee rehabilitation to 15 patients. We received the first tranche of these patients in January 2012. In order to be well prepared for this unique enterprise, a project team was set up in WMRC led by Dr Jeff Lindsay, a very experienced and highly acclaimed Consultant in Rehabilitation Medicine. Weekly conference calls were held with the Department of Health and the Libyan Embassy in London. A series of meetings were arranged with the local Libyan community in Birmingham, including many doctors and they provided us with extremely valuable insight into the physical, psychological and cultural needs of the severely injured men coming to us for help. This was a project that celebrated diversity, valued difference and reached out into the community to do so. We were able to demonstrate innovation in working with a wide range of partners across the NHS and with private enterprise - this was the first time since the Second World War that war-injured people from abroad had been treated in the UK. We were extremely careful to ensure that NHS patients were not disadvantaged in any way by this humanitarian intervention and the Libyan government paid in full for the extra staff and other resources required to deliver the project. Due to the dedication and commitment of our staff, we delivered safe effective care of the highest standard and made a positive difference to the victims of this horrific conflict, despite the cultural and language differences and the devastating nature of the injuries. Our staff said they felt they were really delivering our Trust values of accessible and responsive community healthcare, in a very special way. The nine patients who were successfully fitted with limbs and provided with intensive rehabilitation said they would never forget their wonderful experience with us here in Birmingham and would be eternally grateful to the NHS and the fantastic staff who work in it. Amputee rehabilitation is alive and thriving in Birmingham every day, but never more so than during this project. 96 safetyeffectivenessexperience CLINICAL effectiveness Clinical Measurements Laboratory (CML) The CML provides a specialist service for people who have movement disorders with a main focus on walking. A specialist team of healthcare professionals (led by Professor David Pratt) collect and analyse data on movements, muscle activity, pressure patterns, loading and energy expenditure. This information is combined with other sources of information (such as X-Rays) to produce a holistically viewed but targeted treatment programme for each individual. These treatments usually include a number of options such as surgery, physiotherapy, use of orthoses (splints) and medication (such as botulinum toxin injections). From mid-2011 until just prior to the London Paralympics in 2012, the team worked with six key athletes with the aim of improving their performance in partnership with senior medical and training staff at UK Athletics. Two athletes who benefited from the assessments in CML were Sophia Warner and Stephen Miller who both have cerebral palsy. Sophia is a runner and during the initial assessment process, she jogged on a treadmill with markers and electrodes attached to collect data on movement and muscle activity. Recommendations were made to improve her arm position, foot and leg placement and orthotic requirements. Following the adoption of these recommendations Sophia managed to run personal best times. During the Paralympics Sophia took fourth place in the Women’s 200m T35 event. She now has taken up a position as commercial director for UK Athletics. Stephen Miller is a seated athlete and throws a club in classification F32. In his assessment (see picture below), markers and electrodes were attached in a similar manner to that used for Sophia. Recommendations from his assessment focussed on the changes needed for his seating and strapping and the use of Lycra shorts to assist his stability Despite Stephen having problems on the day of his Paralympic event he is still more stable than before and was men’s team captain for Team GB. Because of the success of this venture UK Athletics plan to use the skills and facilities of CML leading up to the 2016 Paralympics in Rio de Janeiro. 97 safetyeffectivenessexperience CLINICAL effectiveness Family Nurse Partnership The Family Nurse Partnership is an early intervention and preventative programme for first time teenaged parents. It offers intensive and structured home visiting from early pregnancy until the child’s second birthday and is delivered by specially trained nurses and midwives. The programme sits at the intensive end of the prevention pathway for more vulnerable children and families and is embedded in the national Healthy Child Programme. Alongside the Health Visitor Implementation Plan (DH 2010) there has been a government commitment to double the number of places on the programme to 13,000 by 2015. In Birmingham this commitment has been matched by a recent expansion of the programme which means that since January 2013 we have provided a citywide service across three sites with three supervisors and 17 family nurses. Enrolment and participation in the programme is voluntary Jade Moore (left) with family and client involvement is highly valued and integral to the nurse supervisor Rachel Tuton programme methods and materials. In Birmingham specific client feedback has been encouraged and recorded in a variety of ways; through written comments and photographs for public events; by client attendance at the Trust Board; via contributions to the Customer Service Excellence standards and patient experience questionnaires; and through process evaluations of our service delivery. Our parents actively contribute to the quality assurance and improvement of the programme. They have been involved in our recruitment of new nurses and a supervisor, interviewing up to 40 candidates on three separate occasions. In the past year they have attended our Board meeting every quarter, presenting their own report with valuable comments and suggestions for service improvements. We are particularly proud of their most recent involvement in the national FNP Study Event in February 2013 with attendance by nearly 700 delegates. The event was opened by our clients who were also present at and supported the delivery of every workshop. At the end, two clients gave a performance of a song that they had written about their family nurse and the service they had received. The following comment was received from Dr Dulcie McBride, Service Development and Public Health Lead for the programme: I just wanted to write and thank you for your attendance and for your contribution to the FNP National Study Day on Wednesday. The feedback we have received already from senior civil servants in Department of Health, our new partners at the Tavistock and Dartington Social Research Unit, Connecting for Health and the delegates themselves has been fantastic. The event was an amazing showcase of the potential of Birmingham’s clients, the skill and talent of all the family nurses and supervisors in Birmingham and the organisational commitment to FNP. 98 safetyeffectivenessexperience CLINICAL effectiveness Child Development Centres A review of the role of the Child Development Centres (CDCs) was undertaken with the aim of standardising practice across the five CDCs and developing a clear pathway for children referred to the service. A project team was set up, and workshops took place, involving representatives from the CDCs and other children’s services including other agencies. Parental views were also gathered. The team collaboratively agreed a new process and new pathways were completed. There have been several benefits from this review. An equitable service is offered across the city; the same clear pathways are delivered at all five CDCs. There has been a significant improvement in the number of children seen within 18 weeks of referral. There is a sense of unity across the CDCs which has facilitated team-working and cross-cover between sites. Families have clearer guidance about what they can expect e.g. the number of sessions involved, report following assessment back to parents within two weeks. 99 safetyeffectivenessexperience CLINICAL effectiveness Clinical library - use of latest evidence for best practice The primary aims of the library in serving the clinical staff are: • help them use the best evidence to provide the best patient care, and improve patient safety • provide resources to keep all staff up to date in their practice • support their revalidation, where appropriate • help them with their personal development by supplying evidence and support with essays and dissertations when undertaking studies • help them with evidence to conduct research and development. We do this by: • having well-trained professional staff • providing a literature searching service • training in using health database to help them find the evidence themselves. This year we have been commissioned to provide information literacy skills training to staff at two other large NHS Trusts in the region-University Hospitals Birmingham NHS Foundation Trust and Walsall Healthcare Trust. This has been so successful that they have re-commissioned for 2013/14 • purchasing relevant resources; databases, e-journal and books in a cost effective way • working collaboratively with other NHS library services to save cost in purchasing these resources • developing a knowledge management strategy to maximise staff time with their patients, and using the knowledge within the organisation more effectively • innovating to improve the service: this year, the library team has developed a web-based online document ordering service that reduces paperwork, provides an audit trail for copyright purposes, allows 24/7 ordering of journal article, and allows users to monitor the progress of their orders. Two other Trusts-University Hospitals Birmingham NHS Foundation Trust and Heart of England Foundation Trust are also using this product, and we hope to sell this to other libraries. A community physiotherapist said: The literature search service enabled us to update our care pathway which will be distributed to physio/occupational therapist staff across the city. 100 safetyeffectivenessexperience PATIENTexperience Birmingham Dental Hospital A display was set up by the main hospital entrance, inviting service users to feed back through completing a short survey. The survey was administered using paper based questionnaires and also through directly interacting with service users using an iPad to record and collate the feedback received. This is the response we received from 45 service users: How satisfied are you with the methods of engagement and involvement that we currently use? Would you like to see more engagement and involvement in how services are developed? Very satisfied 42% Yes 58% No 7%11% 9% Satisfied Neither satisfied 9% or dissatisfied Dissatisfied Very dissatisfied 64% What could we undertake to increase your level of satisfaction with how we engage with our customers? Develop a patient group i.e. action group. Meet and greet person standing on the door upon arrival. I have had to ask what was going on with my late appointment, instead of being told. The comment card boxes need to be made more visible to customers. Sessions can prove to be a bit long! But well looked after. Consultations. The results and comments from this survey have helped to evidence that our current methods of engaging are acceptable and have helped to support the development in 2012 of the Dental Highlights report and information posters to signpost users to how they can engage with us and access further information. 101 safetyeffectivenessexperience PATIENTexperience Prison service A key recommendation of the National Institute for Mental Health study was to develop a regular structure of inmate feedback in the prison. However little capital was made of the recommendations identified in terms of service user development until November 2010. Birmingham and Solihull Mental Health NHS Foundation Trust (BSMHFT) and Birmingham Community Healthcare NHS Trust were awarded the contract for HM Prison Birmingham in late 2009. This allowed for a great opportunity to ensure that service user involvement was firmly back on the prison healthcare agenda. Six focus groups were facilitated with a range of inmates. The information that was generated from the groups influenced the service redesign of integrated drug treatment systems in the prison. Key developments for the progression of service user involvement have been built on the foundation of the focus groups. These are: • the HMP patient experience group • wing inmate healthcare representatives • healthcare representative council meetings Service user involvement in healthcare delivery at HMP Birmingham is now established. Service users are involved in planning and influencing positive changes in the way services are delivered to them. It is important that service user engagement and involvement opens up lines of communication that can engender a mutual respect from all parties as common areas of concern are highlighted and addressed. This process can lead to a sense of ownership from inmates (service users) as they seek to influence change and sustain momentum their involvement brings with it. My prison term has made me acutely aware of the impact my illicit drug use and subsequent contact with the criminal justice system has had on my wider family members. It has offered me insight into why I used and the impact using heroin has had on my mental health. Reflection and raised self-awareness of why I find myself in my current situation, also remorse has given me extra motivation to change my lifestyle choices and move on. 102 The ward nurses and healthcare staff are attentive and helpful. Healthcare complaints and any developments in relation to matters raised are dealt with in a timely fashion. safetyeffectivenessexperience PATIENTexperience Engagement and involvement in the learning and development service The learning and development service has a patient experience network (PEN) which includes patients, service users, family carers, paid carers, staff and stakeholders. Over the past two years PEN has expanded to become more than a meeting. We are reaching out to encourage people with a learning disability using our health services to join PEN and become involved in what we do. We identify ways to engage with our ‘hard to reach’ population. We are working to ensure measurable outcomes for patients, carers and staff. Below are some of our achievements over the past 12 months: • people have the opportunity to attend our current meetings and are encouraged to share information • the 2012 event invited people to tell us what it is like to live with a learning disability, or care for someone with a learning disability, what helps and what gets in the way. The wealth of information we received encouraged us to start to develop a film of people’s stories which we will complete during 2013. Involvement in PEN provides opportunities for people to: • receive minutes and agendas to comment on • attend our PEN events • tell us their stories which we can use to help other people with learning disabilities to overcome obstacles • help us to update our website • review our current surveys • comment on documents • help plan new initiatives to improve our service. We are planning to hold our next event in summer 2013 to improve ‘Health and Wellbeing.’ 103 safetyeffectivenessexperience PATIENTexperience Quality care right down the line The ability for patients to self-assess is an important element of BCHC’s plans to provide safe, responsive services closer to home. One Birmingham man is benefiting from a high-tech approach to healthcare. After a couple of collapses caused by heart and breathing problems, Gordon Taylor faced a future of increasing dependence on others. In one incident, Gordon had to be rushed to hospital by ambulance after collapsing in Birmingham city centre. Medical staff warned his family he may not recover. But just months later, Gordon has regained much of his lost confidence and independence after BCHC’s district nursing service provided him with state-of-the-art kit enabling him to self-monitor vital health indicators, which are automatically relayed, monitored and recorded instantly. If there are any causes for concern, Gordon may be asked to repeat the tests and, if necessary, might receive a visit from the district nursing team. Gordon, aged 65 said: I collapsed a couple of times - firstly on Christmas morning and then about six months later in the city centre. The second time, I ended up in hospital for 24 hours. When I got back home, a member of the district nursing team came to see me and asked me if I would like to try out this new ‘telemonitoring’ system. I said I’d be happy to try anything that meant I could stay out of hospital, monitor my condition myself and then make sensible decisions about how active I could be from day to day. The first day I had it, I was on my own and a bit nervous but I sailed through it. Some people might think it’s a bit ‘Big Brother’ but it’s nothing like that at all. If anything, it makes me feel more in control of my health and I really like that about it. I get up, make myself a cup of tea then settle down and switch the machine on. Firstly, I answer some questions about how I’ve been feeling then do my oxygen reading, blood pressure and weigh myself. All that information goes straight down a phone line to Moseley Hall Hospital. Sometimes they might ask me to do the readings again. For example, if my oxygen is low, I can go on the cylinder for a while and then take the reading again. And if necessary, I might get a visit from one of the nursing team - they’re never far away if I need them. 104 safetyeffectivenessexperience PATIENTexperience Continued... Gordon, who spent 45 years as a gardener and park ranger with Birmingham City Council, says the equipment gives him peace of mind so that he can get on with enjoying life without constantly worrying whether his health will let him down. He says: It’s a life-saver. In hospital, I’ve got used to going by what the doctor or nurse says; then, I’ve come home and felt vulnerable because I’ve had no way of monitoring myself. Now, I can make my own decisions - whether to have more oxygen; whether to rest or go out. And it’s completely portable. So recently, I took it all with me on a trip to Blackpool and carried on doing my readings as normal. Understanding my own health gives me a great base to work from and tremendous reassurance, not only for me but also for my sisters who phone every day and come in to help me. Twice the hospital have phoned them to say ‘I don’t think he’s going to make it’; I never want them to go through that again. Cats have nine lives, not humans. And I feel as though I’ve already used two up! District nurse Bev Marriott has been caring for Gordon for about two years and remains his lead contact within BCHC’s community services. Bev says: It’s been great for Gordon because the system is very portable so he should always be aware of signs and symptoms arising from changes in his condition and act accordingly. It can massively improve quality of life for patients with conditions like Gordon’s. He is more in control of his own health and daily routine, is very organised with his reading and we’re working with him to maintain important lifestyle changes - he’s already given up smoking and we’re looking at his diet. He’s really enjoying life again and it’s been really nice to share some of that journey with him! 105 Investments in our Trust Infrastructure New Birmingham Dental Hospital Detailed planning permission has been granted by Birmingham City Council to build a new Dental Hospital and the University of Birmingham’s School of Dentistry on the former BBC Pebble Mill site. The proposed development, led by Birmingham Community Healthcare NHS Trust, together with its partners the University of Birmingham, Birmingham and Solihull LIFT (BaS LIFT) and Calthorpe Estates, would deliver the same range of services currently provided at the St Chad’s Circus site from a modern fit-for-purpose building. Councillors gave the scheme unanimous backing when the application was heard in December 2012. Proposals and designs for the Dental Hospital and School of Dentistry were developed by One Creative Environments Ltd, and shared with local residents, staff and students at different stages of development, via a number of public exhibitions held throughout 2011/12, providing details of where the four-storey building would be located and how the site would be accessed. Work during 2013 will focus on concluding the final stage of the business case and completing the legal documentation. It is hoped this will be concluded during the early part of the year so that work can begin in summer 2013, with the facility being operational in summer/autumn 2015. Former Birmingham Community Healthcare Medical Director Rick Roberts (who retired in May 2013) explained: We are very pleased to have received detailed planning consent. This represents a very significant step forward and reflects great credit on the excellent work of all partners involved in the project. We will continue to listen to the views of our staff and others and to work with the Strategic Health Authority on the final stage of the business case as we progress towards making these exciting plans a reality. Professor Philip Lumley, Head of University of Birmingham School of Dentistry said: We are delighted with the decision which brings us one step closer to having a new, modern facility which reflects our international reputation as a leader in research, teaching and clinical service within dentistry. 106 Staff Values in Practice (VIP) Award The VIP awards programme runs all year round so at any point when an individual or a team has done something above and beyond the call of duty for the benefit of patients, or their colleagues, they can be nominated. Nominations are presented to a panel who choose one winner and two finalists for each category. The panel is made up of: • • • • an executive director a non-executive director a staff side representative someone from our public membership. Members of staff, patients and the public can nominate any of the following people for an award: • individual members of staff • teams • volunteers for the Trust. Everyone who is nominated, whether successfully shortlisted or not, will be contacted regarding the status of their nomination. Governors During 2012/13, the Trust successfully recruited over 10,000 public members and 5,000 staff members. From this membership, our newly elected Governors have emerged. Following an initial event for our members to find out about the Governor role, and subsequent communications and support to our members, a sizeable number of members came forward to stand in our inaugural elections in January 2013. At this time our members voted who they wished to represent them. The first Council of Governors has been formed. In addition to the elected Governors, the Trust has liaised with partner organisations resulting in a full complement partner Governors being nominated to the Council. The Council will remain in shadow form until the time that we are licensed as a Foundation Trust, at which point, it will become fully operational. The Council has been actively supported by the Trust through its induction and early development in shadow form to ensure they have the knowledge and skills to assist them in undertaking their new role. The organisation has also given Governors a profile with the membership through communications activity. More information about the shadow Governors of Birmingham Community Healthcare NHS Trust is available on the Trust website: www.bhamcommunity.nhs.uk/membership 107 Technology Agile working BCHC has an ambition to bring smarter and more effective ways of working to the Trust with by piloting an agile working policy. ‘Agile working’ is a term used to describe a more modern working environment which takes into account the most appropriate use of Trust accommodation, incorporates the best use of technology and promotes a more efficient and productive workforce. The Trust wants to support its staff to be able to work in a way that better suits their work patterns and their patients, rather than having to work from a specific base, simply because that is what has been done historically. Agile working empowers staff to choose the most appropriate time and place to carry out their work; allowing duties to be completed in the most appropriate place, at the best time and in the best way. Key benefits for staff: • enables them to chose the most appropriate workplace for the task in hand • can reduce travelling times to a specific base • promotes improved work/life balance • provides a solution to a temporary problem where travel to the office is not possible. Key benefits for service users: • more face-to-face time with Trust staff • overall improved service user experience • experience of a more professional and joined-up service • opportunity to benefit from advanced technology (see mobile working for details). For the Trust: • supports continuity of service and the efficient functioning of the Trust • aids the retention of skilled and experienced staff whose personal circumstances change and who may otherwise leave the Trust • helps disabled employees to keep their existing employment and support the recruitment of disabled applicants. • enables the Trust to respond to an individual’s need for flexibility in working arrangements, for example to support staff with responsibilities as carers. 108 Mobile working Mobile working is one part of the Trust’s wider commitment to agile working, a term which describes a modern working environment, incorporating the best use of technology to help create efficiency and productivity. An agile working strategy is being developed to support staff in all aspects agile working, including mobile working. (See previous page for agile working information). The Trust ran a pilot with community-based staff, who tested a variety of devices from laptops to tablets, along with mobile dongles and VPN tokens, enabling them to connect to the intranet, internet and systems to support them in their work without returning to an office base. Feedback from staff involved in the pilots has actively shaped the solution, helping identify the most effective and user-friendly devices. Following on from successful pilot schemes across the Trust, mobile working solutions are set to be rolled out across community-based clinical divisions from April 2013. All staff due to receive a mobile device will be booked onto a training session between April and August. At the end of the session staff will leave with their allocated device ready for use. Key benefits: • reducing unnecessary journeys • more contact time with patients • Patient information is more accessible whilst out on visits • Reduces the amount of paperwork staff need to carry around, which reduces IG risks. Delivering care NHS Change Day The Trust recently joined thousands of NHS colleagues across the country by celebrating NHS Change Day. The idea behind the day was to create a mass movement of NHS staff pledging to do something small that could make a big impact on patient care. Nearly 200,000 NHS staff put forward pledges. The Trust chose this day to launch its new customer care standard, by displaying these at a number of inpatient sites across the city. Janet Fox, head of equality and organisational development is behind the customer care standards. She said: These standards are in themselves a kind of pledge - a pledge to our patients that wherever and whenever they are treated by us, they receive the best quality care and service. The principles around this are that every patient will receive: I - individualised care C - with effective communication A - and a positive attitude R - showing respect for you E - in an environment to meet your care needs The leaflet and poster can also be found on our website: www.bhamcommunity.nhs.uk/about-us/our-values/customer-care-standards/ 109 Back to the floor - In addition to a Trust pledge, staff were encouraged to make their own pledges as teams and individuals around customer services. Associate directors in adults and community chose to spend the day going ‘back to their roots’. Gary Crellin, Sally Plant and Tracey Sheridan shadowed colleagues in frontline roles linked to where they started their career. Gary’s career started in hospitality and facilities. He said: It is about 20 years since I washed up an entire ward’s worth of crockery and assisted with a meal service. NHS Change Day gave me the opportunity of being a housekeeper for three hours on Ward 11 at West Heath working with ward housekeeper Madeline Calvert, on her shift. It was good to witness how housekeeping staff were integral to the operation of the ward. It was great also having time to speak to the staff about the ward and care. What I took from it was how good our patient catering is (and what appetites our patients have!), the need for more toilets and the how we handle multiple admissions and discharges in the afternoon. Yes - these issues reach me as an associate director but nothing beats seeing the issues played out in front of you to enforce the need for change. Sally’s career began in occupational therapy so she shadowed an occupational therapist on home visits, while Tracey Sheridan, a nurse by background, teamed up with Helene Woodley, community staff nurse and pressure ulcer champion, to focus her energy on the Trust’s challenge to eliminate all avoidable pressure ulcers. Team pledges - The Combined Community Dental Services pledged to meet up with service users directly through patient journey mapping. All services users that were in contact with the service on 13 March will be invited to participate in a 1-2-1 discussion focusing on their experience whilst being under our care. Beverly Kelly, dental nurse manager, said: We hope this movement works toward empowering our service users to give them a voice to let us know what has happened to them (good and bad) throughout their journey and potentially drive towards improving on our future customers experiences. In the Learning Disability Services, the NHS Change Day pledge formed part of an allied health professional’s away day. Attendees were asked to pledge a small change they could make which could have a big impact on patient care. 110 Assurance process In order to assure ourselves that the information presented is accurate, and that the services described and the priorities for improvement are representative, our Board designated the Director of Nursing and Therapies to lead the process of developing the Quality Account progress was reported to a number of executive-led committees before final approval from the Board. The Director of Nursing and Therapies also ensured through the Clinical Quality Assurance Manager (project lead for the Quality Account) that staff and patients had an opportunity to consult around the key clinical priorities for the Quality Account. The organisation’s executive committees were pivotal in setting the clinical priorities. In addition to this other stakeholders provided an objective view around the content of this Quality Account. A wide range of internal corporate and service level leads and staff have been consulted on this Quality Account with a through our committee structures, through the Trust’s Public Involvement Action Group, with Healthwatch (formally known as LINks), Health and Wellbeing Board, our Commissioners and our Quality Accounts Editorial Group. The Quality Governance and Risk Committee, Clinical Forum, Management Board and the Trust Board were provided with an opportunity to review the Quality Account before the final version was agreed, thus ensuring as far as possible that the information is accurate. Statements received from external organisations Overview and Scrutiny Committee We recognise that healthcare providers publishing Quality Accounts have a legal duty to send their Quality Account to the Overview and Scrutiny Committee (OSC) in the local authority area where the provider has its registered office, inviting comments from the OSC by May. However the role of the OSC in providing assurance over a provider’s Quality Account is a voluntary one. The OSC were very grateful for having an opportunity to gain a greater insight into your organisation, but on this occasion will not be supplying a statement around the Quality Accounts received for 2012-13. Healthwatch (formerly known as LINks) Birmingham Community Healthcare NHS Trust has fulfilled its duty in providing a copy of their 2012-13 Quality Account to Healthwatch Birmingham. There were no further comments or statement received from Healthwatch Birmingham for submission to the Quality Account this year. Continued... 111 Statement for Quality Account 2012/13 Birmingham Community Healthcare NHS Trust Birmingham South Central Clinical Commissioning Group (BSC CCG) as coordinating commissioner for Birmingham Community NHS Trust (BCHC) welcomes the opportunity to provide this statement for their 2012/13 Quality Account. A draft copy of the Quality Account was received by BSC CCG and the statement has been developed from the information presented to date. Feedback on the draft account has been received from Birmingham CrossCity CCG, Solihull CCG and NHS England Area Team as the lead for specialised commissioning. We have reviewed the content of the Quality Account and confirm that this complies with the prescribed information, form and content as set out by Monitor and the Department of Health. BCHC have provided an update on progress against the clinical quality priorities set out for 2012/13 in their Quality Account and set out the proposed priorities for 2013/14. In reviewing this information for 2012/13 we have taken account of the progress made to date and considered how this is informing the proposed clinical quality priorities for 2013/14. Patient safety has been a key priority for BCHC with the implementation of the Safety Express Plan and the Trust has made good progress towards the aim of achieving harm free care during 2012/13. As part of this plan the Trust has implemented a comprehensive pressure ulcer prevention and management work programme and through this has demonstrated significant progress towards the aim of eliminating all avoidable grade 3 and 4 pressure ulcers in both community and inpatient settings. The challenge for BCHC will be to continue to build on and sustain this level improvement across all identified harms in 2013/14. Unfortunately, over the past year the Trust has experienced two serious incidents classified as “never events”, both within Dental Services. Commissioners have been invited to root cause analysis meetings for each of these incidents to identify the lessons to be learned. Progress with actions to be taken to prevent them re-occurring are reported through the clinical quality review meetings. BCHC successfully recruited to Health Visitor and Health Visitor Trainee posts in 2012/13 and there continues to be improvement in Health Visitor Teams in relation to New to Area and Primary Visit reviews with families. The Quality Account reflects a number of the performance quality indicators which are monitored monthly along with areas for improvement at the Clinical Quality Review Group as mandated by the service contract. In addition we are given copies of papers and reports of the Trust’s internal clinical governance committee. We have made some specific comments to the Trust directly in relation to their plan. Namely, how the impact of the 2013/14 clinical priorities will be measured and further information on CQUINs regarding outcomes and the levels of improvement to be achieved. We have also requested improved patient experience data with supporting narrative and inclusion of additional workforce data with related actions being taken in response to the issues identified. We have suggested some changes to make the document easier to read and understand and proposed that the account is aligned with the five domains of the NHS Outcomes Framework. The Quality Account provides evidence of ongoing commitment by the Trust to continue to improve the services it provides. We look forward to continuing our partnership with the Trust and in supporting them to deliver this year’s quality targets. Dr Raj Ramachandram, Chair - Birmingham South Central Clinical Commissioning Group Quality and Safety Committee 112 Response to the statement: BCHC has reflected on the comments received from the Commissioners. A number of consequent actions have been included within the final Quality Account; other points raised will be subject to further reflection, the outcomes of which will be reported upon in future Quality Accounts Acknowledgements Thank you to all members of staff and public members who have contributed towards this Quality Account. Quality Accounts Editorial Group consisted of: Adam Dandy David Disley-Jones Lisa Eden Colin Graham Brian Hanson Narvinder Kaur Alison Last Anne Pemberton Angie Villers Public Engagement and Patient Information Lead Communications Manager Associate Director of Therapies Head of Clinical Governance Chair of PIAG and public representative Clinical Quality Assurance Manager Associate Director of Patient Experience Advice and Information Service Lead Head of Compliance and Assurance How to provide feedback If you would like to provide feedback on the Quality Accounts you can do this by: Tel: 0121 466 7069 Email: clinical.governance@bhamcommunity.nhs.uk Address: Quality Accounts Clinical Governance Department 3 Priestley Wharf 20 Holt Street Birmingham Science Park Aston Birmingham B7 4BN 113 Glossary C. Dif (CDI) Clostridium Difficile An infection causing vomiting and diarrhoea CQC Care Quality Commission The independent regulator of heath and social care in England CQUINs Commissioning for Quality and Innovation Projects agreed between Commissioners who buy our services and the Trust to improve quality standards ECIs Essential care indicators A set of care standards used within the Trust KPIs Key performance indicators Standards which are used to measure performance LINk (currently now known as Healthwatch) Local involvement network A network of local people and groups which work to improve health and social care services MRSA Meticillin resistant staphylococcus aureus An infection caused by the staph bacteria which is resistant to most penicillin based antibiotics Meticillin sensitive staphylococcus aureus An infection caused by the staph bacteria which is able to be treated with most penicillin based antibiotics Malnutrition universal screening tool A national tool used to identify if people are at risk of malnutrition MSSA MUST NCEPOD PLACE 114 National confidential enquiries of patient outcomes and death review Organisation which reviews the management of patients and makes recommendations for the improvement of clinical practice Patient-led assessments of the care environment ! Birmingham Community Healthcare NHS Trust Membership application page 1 Please fill in your details below to become a member of Birmingham Community Healthcare NHS Trust. We are collecting information to ensure we contact you in the best way for you. The information you provide will also help us to ensure our membership is representative of the communities we serve. The minimum age to become a member is 16 years. If you are younger than this and wish to be involved, please email ft@bhamcommunity.nhs.uk Contact details (please use CAPITAL LETTERS) Fields marked with * are mandatory. Title.......................................................................................................................................... First name*............................................................................................................................... Last name*............................................................................................................................... Date of birth*.................................................. Gender (please tick) Male Female Address*.................................................................................................................................. Postcode*................................................................................................................................. Telephone (home)..................................................................................................................... Telephone (mobile).................................................................................................................... Email........................................................................................................................................ How would you describe your ethnic origin? (please tick as appropriate) White/British Black or Black British/African White/Irish Black or Black British/Any other Black background............................... White/Other Mixed White/Black African Asian or Asian British/Pakistani Mixed White/Black Caribbean Asian or Asian British/Indian Mixed White and Asian Asian or Asian British/Bangladeshi Asian or Asian British/Any other Asian backgound.............................. Black or black British/Caribbean Mixed Any other mixed background Chinese Any other ethnic group (please specify) . .......................................................... How would you prefer to be contacted? (please tick as appropriate) ! Email Post Telephone [continued over the page] 115 Birmingham Community Healthcare NHS Trust Membership application page 2 Do you have a disability? (please tick as appropriate) No Yes (please give details of any special requirement below): How would you like to be involved at the current time? (please tick as appropriate) Level 1 membership (limited involvement) Level 2 membership (active involvement) Level 3 membership (full involvement) Did a staff member recommend that you become a member? Yes: (please give their name and job title in the space provided below): No: (please specify other in the space provided below): Please tick here if you do NOT want your name and constituency to be available to the public through the Foundation Trust Register of Members. The data you supply will be used only to contact you about the Trust, membership or other related issues and will be stored in accordance with the Data Protection Act. Please see our website at www.bhamcommunity.nhs.uk/ft for more details. I apply to become a member of Birmingham Community Healthcare NHS Trust and agree to the processing of my information: Signature............................................................ Date......................... Please return completed forms to: Freepost RSUJ-TESZ-BHSH Membership Birmingham Community Healthcare NHS Trust 3 Priestley Wharf, 20 Holt Street, Birmingham B7 4BN 116 If you would like to request a copy of this document in an alternative format, or have any other queries about its content, please contact the Birmingham Community Healthcare NHS Trust communications team at: Communications team: 3 Priestley Wharf 20 Holt Street Birmingham Science Park Aston Birmingham B7 4BN Email: info@bhamcommunity.nhs.uk Or follow us on Twitter @bhamcommunity The report is also available at www.bhamcommunity.nhs.uk Or you can speak to a patient experience officer in our Customer Services team on Tel: 0800 917 2855 Accessible, Responsive Community Healthcare Design and print enquiries: Clinical Photography and Graphic Design Tel: 0121 466 5107 Reference: 43045 26.06.2013 Tel: 0121 466 7281