CitiHealth NHS Nottingham QUALITY ACCOUNT 2010/11 30 June 2011
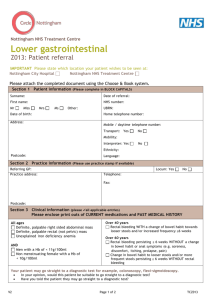
advertisement

CitiHealth NHS Nottingham QUALITY ACCOUNT 2010/11 30 June 2011 Health at the heart of the city Contents Page Part One Introduction from the Chief Executive and Statement on Quality 1 Part Two Review of Quality Performance 3 includes statements of assurance from the Board 2.1 Review of services 3 2.2 Patient Safety 3 2.3 Clinical Effectiveness 10 2.4 Patient Experience 20 2.5 Participation in Clinical Audit and National Confidential Enquiries 24 2.6 Research 29 2.7 Commissioning for Quality and Innovation (CQUIN) framework 29 2.8 What others say about us 31 Care Quality Commission Registration 2.9 Statement on Data Quality 32 Part Three Priorities for improvement 33 3.1 Patient Safety 33 3.2 Clinical Effectiveness 36 3.3 Patient Experience 39 Part Four Commentary from other organisations 40 4.1 NHS Nottingham City 40 4.2 Nottingham LINk 40 4.3 Local Authority Health and Adult Social Care Select Committee 41 Part Five Our commitment to you Health at the heart of the city 42 Part 1 – Board Statement on Quality Welcome to the first Annual Quality Account for Nottingham CityCare Partnership CIC. We will be looking back to our quality achievements during our final year as CitiHealth NHS Nottingham, as well as looking forward to our new quality aspirations as a social enterprise organisation. This has been an eventful time for us as we have transformed from an NHS organisation to a Social Enterprise company whilst still meeting all of our many quality challenges and maintaining and improving patient safety, patient experience and clinical effectiveness. Our commitment to quality is paramount. It is exemplified in our vision to provide “better health and complete care, owned and delivered locally” as well as in one of our six strategic objectives to “provide services that are equitable, accessible and of high quality.” The Board and the organisation continually assess and strive to improve the services so they are responsive to the needs of our local communities as well as to the commissioners of those services. We recognise that it is important to have the right approach but even more vital are the successful outcomes generated from the vision. Patient safety is a top priority in CityCare and in our Quality Account we are pleased to report that along with the health and social care workforce in Nottingham we achieved a “good” rating for providing children safeguarding services by Ofsted in October 2010. Safeguarding children is taken very seriously in CityCare and is everyone’s business, so we were especially satisfied that interagency and individual hard work had been recognised. Another notable success occurred when we were declared one of the highest reporters of low harm incidents in the region by the National Patient Safety Agency, who asked if we would provide support to other organisations to develop in this area. In our first Quality Account we have chosen to highlight clinical effectiveness by focusing on the high impact actions for nurses and midwives; though the actions are not exclusively owned by those groups and all our services have contributed to the actions set out in this Department of Health initiative. The high impact actions cover the issues of pressure ulcers, falls prevention, nutrition, promoting normal birth, end of life care, reducing sickness and absence among staff, improving discharge processes and reducing urinary tract infections in the patient population. There have been considerable achievements across the high impact actions initiative but some notable successes have been the contribution by the organisation to research and development with consistently high rates of staff involvement in many projects. For example one of our Health at the heart of the city 1 occupational therapist Dr Phillippa Logan had research published in the British Medical Journal on the work undertaken into falls prevention. This work has been instrumental in improving the falls prevention service as well as leading to the support of many other organisations in their efforts to reduce falls in the elderly population. The perceptions of patients/users and their carers as they experience our services is fundamental to enabling us to understand how to improve the quality of care provided. There has been significant progress in this area throughout the year. We now have patient surveys set up for every service undertaken on a regular basis. There is a system for taking the themes forward and translating them into change in services. There is however also much room for improvement and we recognise that we are at the beginning of a journey in getting to know all the voluntary and third sector organisations and many groups which work on behalf of different health service users in the community in Nottingham. There is also a need to ensure that we tackle individual complaints and issues actively and promptly in a transparent and equitable way. We are committed to acting on people’s concerns over the next year to ensure that there is meaningful engagement and participation in decision making at all levels and in the development of our services. To the best of my knowledge, the information in this document is accurate, and a true account of our quality of services. Lyn Bacon, Chief Executive Health at the heart of the city 2 Part 2 – Review of Quality Performance This section includes nationally mandated statements of assurance by the board in addition to locally decided sections, which were included following consultation internally and with other external organisations. 2.1 REVIEW OF SERVICES During 2010-2011 CitiHealth provided and/or sub-contracted 55 NHS services. CitiHealth has reviewed all the data available to it on the quality of care in 53 of these NHS services in line with the requirements of the commissioners of these services. The contract for the other two services has recently been split and performance data for them is currently being collated for reporting next year. The income generated by the NHS services reviewed in 2010-2011 had a contract value of £54.3m for 2010/11 and is 100 per cent of the total income, generated from the provision of NHS services by CitiHealth for 2010-2011. 2.2 PATIENT SAFETY CitiHealth NHS Nottingham recognises the importance of ensuring systems and processes are in place to record, monitor, report and analyse any concerns relating to patient safety. We propose we review how we have performed in the following areas including lessons learnt and improvements made. Safeguarding of Children and Vulnerable Adults The delivery of safe services is extremely important to the organisation. During 2009/10 we invested a significant amount of time training our staff in safeguarding vulnerable people. We work with partner organisations to make sure all people in our care are safe. We review all our incidents and complaints to ensure no safeguarding concerns go unreported and work closely with social care. Safeguarding adults 2010-11 was an important developmental year for CitiHealth Adult Safeguarding. The introduction of a professional lead has been instrumental in bringing about closer liaison with patient safety; improved access to expert professional advice and increased presence, participation and development of the multi-agency adult safeguarding policy and procedures. The constitution of the Adult Safeguarding Steering Group, (November 2010) has been key in delivering on an organisational action plan for adult safeguarding and has provided the basis for Health at the heart of the city 3 During the year we took part in a Department of Health pilot, developing a Standardised Framework for assessing Adult Safeguarding against a set of National Standards. The organisation scored ‘effective’ in the majority of areas; the self assessment highlighted where improvements would be welcome around developing training for staff, gaining service user satisfaction, and developing a system for ‘flagging’. These are being addressed as part of the ongoing safeguarding adults work programme. Safeguarding children A Quality Assurance Schedule was completed for NHS Nottingham City during February 2011. This was a self assessment to provide assurances to commissioners that our safeguarding children governance and structures met the required standards. During 2010-11 we completed our annual Markers of Good Practice assessment and Section 11 audit. This is a process led by NHS East Midlands whereby we rate our services against key standards. We received positive feedback on this assessment from NHS East Midlands. Good areas of practice were identified within the Common Assessment Framework (CAF), record keeping, safeguarding supervision and safeguarding training. The areas for development highlighted were embedding the evidence and learning from serious case reviews, providing training to staff on making a referral to social care, and the importance of completing family chronologies. Training was changed in response to these requirements. © NHS Photo Library developing improving quality services into the future. For the first time we have been able to collect data on the numbers of adult safeguarding referrals which will be important in monitoring CityCare’s recognition of and response to adult safeguarding from this point forward. We will be looking to increase on the 33 referrals that were made between September 2009 and September 2010. Safeguarding and Looked After Services Inspection Safeguarding and Looked After Services in Nottingham have been judged as “good” following an inspection undertaken in December 2010 by Ofsted and the Care Quality Commission. The report confirmed that the agencies of Nottingham Children’s Partnership, of which CityCare is a member, are well prepared to meet the challenge, with good training programmes in place for staff at all levels, focusing on early intervention. The city’s strategic plan explicitly highlights safeguarding as top priority suitably undertaken with joint resources. The contribution of health agencies to keep children and young people safe - GRADE 2 (GOOD) There is an effective round-the-clock on call safeguarding service, which ensures that health staff are able to speak to a health professional for advice and support or if they need to escalate a safeguarding referral with social care staff. The only domestic violence specialist nurse provides a highly valued service but is often stretched. Health at the heart of the city 4 Community based staff who co-locate with other agencies and those based and working in children centres have reported improved communication and information sharing and enhanced working with colleagues in all agencies leading to improved identification of vulnerable families and children. There has been good joint safeguarding referral training with Children’s Centres and Family Nurse Partnership staff which is enhancing the mutual understanding of roles and responsibilities. The referral form is now electronic which has helped to improve services access. Leadership and Management GRADE 2 (GOOD) This is reinforced by strong health leadership. Joint workforce development is good. All staff in contact with children and young people have been subject to Criminal Records Bureau clearance (CRB) and no new staff take up post until they are appropriately cleared. Partnership working GRADE 2 (GOOD) Good practice is identified in the level of safeguarding training provided across agencies with a key focus on early intervention and prevention through the use of Common Assessment Framework and other early intervention approaches. Robust MAPPA and MARAC are in place with good attendance by participating agencies. Serious Incidents investigated and reports There is no single definition of a serious untoward incident; they can broadly be described as: An accident or incident when a patient, member of staff, or member of the public suffers serious injury, major permanent harm or unexpected death, (or the risk of death or injury), on our premises or other premises where health care is provided Where actions of health service staff are likely to cause significant public concern Any event that might seriously impact upon the delivery of service plans and/or may attract media attention, and/or result in litigation, and/or may reflect a serious breach of standards or quality of service All NHS organisations are required to report serious untoward incidents and provide investigation reports to their coordinating commissioner. 33 serious incidents were reported from 1 April 2010 to 31 March 2011. This is an increase from the previous year. The increase is accounted for by the new requirement to report all grade three and four pressure ulcers as serious incidents. The table below highlights the category of incidents reported. It includes the infection prevention and control incidents which need to be investigated within four weeks rather than 12 week target for all other serious incidents. Serious Incident reporting Incident type Serious incidents can include death, prisoner death, fire, disruption to service, sexual assault, attempted suicide, serious self-harm, serious accident or injury, unexplained serious injury, security breach, confidentiality breach, serious allegation against staff, serious medication errors, pressure ulcers and loss of patient data. Number Pressure ulcer grade 3 or 4 21 Confidential information leak 2 MRSA bacteraemia 5 Unexpected death 1 Prisoner in receipt of care 2 Suicide 1 Communicable Disease and Infection Issue 1 Table 1: Number and category of incidents Health at the heart of the city 5 Of the incidents reported 19 were closed within the 12 week target. Eight incidents have investigations that are ongoing and are within target for closure. Three incidents remain open over the target but these relate to prison incidents which are subject to an independent investigation commissioned by NHS Nottingham City as part of the Prison Ombudsman investigation. Of the three remaining incidents, one was closed over the 4 week target and two are still under investigation. Due to the complexity of some investigations there are circumstances, for example, where care is provided over more than one organisation, which may delay the incident investigation so that it cannot be closed within the four week target. CitiHealth NHS Nottingham did not report any serious untoward incidents as never events in 2010/11, a never event is ‘defined as serious, largely preventable patient safety incidents that should not occur if the available preventative measures had been implemented by healthcare providers’ (NPSA Never Events Framework 2010-11, March 2010). Learning from investigations All serious incidents have a root cause analysis investigation and action plans are developed and monitored by the Governance Committee, only being signed off once all actions are complete. Learning from our patient safety incidents is shared with staff to improve patient safety. This is done in a variety of ways. Safety First – This is our newsletter to staff which is produced monthly and is cascaded to all staff by email. All incidents are anonymised. Our patient safety committee meets monthly and members represent all our clinical services. All incidents are reviewed and discussed and learning shared through team meetings. Individual feedback to staff following an incident report and incidents are discussed in team meetings. The organisation realises the importance of learning lessons. Whenever an incident is reported a thorough investigation is carried out and reports made outlining areas for improvement. In the cases of some of the more significant incidents this information is anonymised and shared with all grades of clinical staff through team meetings. The governance team supported the development of team managers in the organisation to enable them to better support all staff in the reporting and management of incidents for example by providing structured and impromptu training. We continually use staff feedback to update and improve processes. For example, as a result of feedback from our staff we revised and updated the incident report form to include sections detailing information needed on the investigation. We ran a number of drop in sessions for staff, covering 115 staff, where we discussed the new incident report form. Achievements in the last year We are one of the highest reporters of incidents to the National Patient Safety Agency. The vast majority of our patient safety incidents are classed as no harm or low harm incidents. We are committed to building a Safety Culture by encouraging reporting of incidents and supporting the recognition of lessons that can be learned from incidents and ensuring that lessons are shared and implemented to improve safety for all patients. The NHS Litigation Authority Risk Management Standards The NHS Litigation Authority Risk Management standards for NHS Trusts providing Acute, Community, or Mental Health & Learning Disability Services and Independent Sector Providers of NHS Care aim to reduce the risk to patients through the establishment and upholding of systems and processes to strengthen service delivery. We have achieved Level 1 compliance, (the first of three levels of achievement); which is about having the right policies and procedures in place, and these to be in line with best practice guidance. Health at the heart of the city 6 Infection Prevention and Control From April 2010 to March 2011 NHS Nottingham City Primary Care Organisation had two targets in relation to health care associated infections. The targets were as follows: To not exceed 115 cases of Clostridium difficile infection. To not exceed 10 MRSA bactera Patients are attributed to the Primary Care Organisation target if: Patients are attributed to the Primary Care Organisation target if: They reside in Nottingham and are registered with an NHS Nottingham City GP They reside in Nottingham and are registered with an NHS Nottingham City GP They are registered with an NHS Nottingham City GP but an in-patient for over 72 hours anywhere in the country. They are identified with Clostridium difficile in the first 72 hours of admission to hospital and are registered with an NHS Nottingham City GP. They are registered with an NHS Nottingham City GP but an in-patient for over 48 hours anywhere in the country. They are identified with MRSA within the first 48 hours of admission to hospital and are registered with an NHS Nottingham City GP.ia cases. Health at the heart of the city 7 Clostridium difficile (C difficile) and that the patient’s symptoms have resolved. It also allows data collection to occur about individual cases and ensure that isolation and the principles of infection prevention and control were adhered to in order to prevent further spread. The data collected has shown that awareness of C.difficile infections and surveillance has improved with a 44% increase in the number of samples being processed by the laboratory. The antibiotic guidelines produced in 2008 have had the desired effect of reducing Cephalosporin and Quinolone prescribing. During 2010-11 the NHS Nottingham City Primary Care Organisation target for C difficile infections has been exceeded, although the rates nationally and locally are much lower than when the targets were first set back in 2007. Since 2007 the Infection Prevention and Control Team have reviewed the serious incidents and cases and the findings from these incidents. The reviews of cases indicated the following: Elderly patients being prescribed a number of courses of antibiotics for non specific infections in quick succession. Anti-motility drugs such as Loperamide being prescribed for patients when an infectious cause for their diarrhoea had not been excluded. Samples not being sent for testing when patients developed diarrhoea. By analysing the data and trying to establish themes in relation to development of C.difficile infections the Infection Prevention and Control Team have developed C.difficile reduction strategies in line with the national guidance circulated in 2008 by the Department of Health, Clostridium difficile: How to Deal with the Problem. This work has continued and in primary care areas of work over 2010-11 have concentrated on the following: Antibiotic prescribing – reducing the prescribing of Quinolones and Cephalosporins. New antibiotic guidelines and script switch to alert clinicians to alternatives when they were prescribing have been utilised. Surveillance - timely samples to the laboratory to decrease the potential for C.difficile to go untreated and further complications to develop. New testing methodology for C.difficile to prevent false positive cases and a definition to apply to all cases to ensure only the true positive cases are captured. Monitoring and management of C. difficile – all cases that developed were reviewed to ensure the correct treatment has been given The ongoing monitoring of cases now seems to highlight that changes are occurring in relation to the causal factors for development of C.difficile. The number of serious incidents relating to C.difficile infections has reduced and ribotyping of strains would seem to suggest that less virulent strains are now causing infections rather than the 027 strain that was being isolated in 2007. MRSA The MRSA target was met and the total number for the Primary Care Organisation was nine. The number of pre-48 hour admission cases was five. All cases are reviewed and a root cause analysis investigation completed within 20 days of the case being reported. The investigation and lessons learnt were shared with the following: The clinician leading the care The Infection Prevention and Control Committee for dissemination to all clinical services The wider health economy at a monthly meeting to ensure common themes are discussed and actions put in place to address any themes. In an effort to effectively decolonize patients who have confirmed skin carriage / nasal carriage in the community the Infection Prevention and Control Team undertake the following; Review all cases from the laboratory that are registered with an NHS Nottingham City GP to ensure they are on the correct treatment and screening regime. Health at the heart of the city 8 © NHS Photo Library Review all patients on discharge from NUH that are registered with an NHS Nottingham City GP to ensure they are also on the correct treatment and that treatment and screening regimes are completed. The aim of this follow up is to try to prevent future more serious infections occurring. Medication The Organisation has been working hard over the last 12 months to reduce significant medication errors during the year and have utilised learning from the National Patient Safety Alerts to strengthen our systems and processes to ensure patients receive the right treatment at the right time. 16.2% of CitiHealth incidents reported to the National Reporting and Learning System (NRLS) were classed as medication related which was lower than the overall within our cluster in the latest National Reporting System report. There have been focused areas of work around medicines management notably with HMP Nottingham Prison where the Acting Head of Prison Healthcare, Prison Pharmacist and Head of Patient Safety reviewed the medication incidents to identify ways in which medication errors could be avoided. Furthermore, the Prison Pharmacist has developed a support package for nurses regarding medication. The work has resulted in a slight reduction in medication incidents and the majority remain no or low harm incidents. The organisation has a comprehensive system for co-ordinating all medical device alerts and other safety notices. This electronic system provides a clear audit trail of alerts issued and action taken across the organisation. During the year a total of 114 alerts were issued compared with 118 the previous year. This figure includes medical device alerts, National Patient Safety Alerts and Estates and Facilities specific alerts. The appropriate assessment and action has been taken in respect of each of the notifications and plans have been developed to ensure that where the organisation is not compliant with the recommendations this is rectified within the required timescale. Health at the heart of the city 9 Raising awareness of pressure ulcer prevention through the provision of continued training for registered nurses and health care assistants. Raising awareness of High Impact Actions and root cause analysis findings by the presentation of scenarios via the Tissue Viability Link Nurse System. Implementing and facilitating the recognition of the new pressure ulcer staging system (EUPUAP, 2009). Developing and facilitating the Skin Bundle documentation within Nottingham University Hospitals NHS Trust. Meeting CQUIN targets within primary care. 2.3 CLINICAL EFFECTIVENESS Our clinical effectiveness has been reviewed against the outcomes identified in the national NHS High Impact Actions for nurses and midwives. These not only have the potential for improving patient care, but also reducing cost. High impact action number 1: Your skin matters. No avoidable pressure ulcers in NHS provided care. Achievements The NHS Institute for Innovation and Improvement identifies a number of High Impact Actions as drivers to delivering enhanced quality care to patients (DH, 2009). One of those actions; Your Skin Matters aims to ensure there will be no avoidable pressure ulcers in NHS provided care. The structure of this initiative has been pioneered across Nottingham by Sarah Pankhurst, Service Head, Nottingham Tissue Viability Team. The team provides a service to both primary and secondary care. A number of key challenges led to the successful implementation of the Root, Cause, Analysis (RCA) process into the primary and secondary care settings. Sustaining an accurate pressure ulcer monitoring system. Implementing a reporting mechanism for all acquired stage 3 and stage 4 pressure ulcers. Developing a structured flow chart for the root cause analysis reporting process across the District. Implementing SystmOne and the incorporation of the Braden Risk Assessment tool and a core care plan for pressure ulcer prevention. Developing a root cause analysis investigation report template. Carrying out the root cause analysis, by identifying a timeline of the care provision; recognising critical issues and contributory factors; identifying main causal factors; making recommendations and assisting in the development of an action plan following the root cause analysis process. High impact action number 2: Staying safe – preventing falls. Demonstrate a year on year reduction in the number of falls sustained by older people in NHS provided care. Achievements In 2010 the British Medical Journal published research by Dr Philippa A Logan on the Nottingham Falls services: ‘Community falls prevention for people who call an emergency ambulance after a fall: Randomised controlled trial’ which showed that services to prevent falls in the community reduced the fall rate by 55% over the subsequent year and improved clinical outcome in the high risk group of older people who call an emergency ambulance after a fall but are not taken to hospital. Marie Ward, Falls Clinical Specialist with Nottingham CityCare and Nottinghamshire County falls services, developed a ‘falls tool’ for residents in care homes across Nottinghamshire which was presented at the Trent Falls Symposium 2010. Since September 2010, 96.4% (54 out of 56) of patients reviewed at 6 months have experienced 25% less falls following intervention by the team. The local target is 70%. The service is actively involved with the following audit and research projects: Health at the heart of the city 10 Pressure Ulcer Incidence - Nottingham City 2010-11 1.20% 1.00% 0.80% 0.60% 0.40% 0.20% 0.00% CQUIN Target Incidence Q1 Q2 Q3 Q4 1.05% 1.05% 1.04% 0.90% 1.03% 0.63% 1.02% 0.78% Figure 1: Demonstrates the successful achievement of CQUIN targets by the service each quarter. The target was set to reduce the incidence of pressure ulcers of grade 2 or higher. Audits Nottingham CityCare Falls Audit (measuring care delivered against national Guidelines NICE Falls and Osteoporosis guidelines). RCP Falls and Bone Health National Audit 2010. objective of this joint working project is to improve the quality and productivity of the management of patients at increased risk of falling or fracturing within the PBC group. It is designed to support: Research SAFER 2 national research project with East Midlands Ambulance Service - An evaluation of the clinical cost effectiveness of new protocols for emergency ambulance personnel to assess and refer older people who have fallen to appropriate community services. Nottingham CityCare Falls Services have been involved with Nottingham University/ Nottingham University Hospitals completing a Systematic review of chair based exercise to reduce falls risk. Other projects in 2010 - 11 Better Balance Better Bones Project Nottingham City Central Practice Based Commissioning group (PBC), GlaxoSmithKline, ProStrakan and Shire and Nottingham CityCare Falls Service are engaged in joint working to enhance the management of falls and osteoporosis to a standard of care defined by NICE (TA 160,161 & 204)), NOGG (2008). The The earlier and improved identification of patients at risk of falling and/or fracturing, and development of services and treatment protocols for management and support. The optimisation of osteoporosis management, including guideline review. Validation of existing risk registers with data quality improvements where appropriate. Active identification and management of patients identified as at risk with appropriate education and services in place to support healthcare professionals. Improvements in fracture patient management and community follow up. Equitable, cost effective service delivery across all practices within the PBC group. Improving the quality of referrals to secondary care and community services. The Falls Prevention Service provides a ‘rolling’ education and training programme for staff in Day Centres, Care Homes (ASH and Private) Health at the heart of the city 11 and staff in health and social care (including Homecare services) as well as staff in Warden Aided accommodation across the City of Nottingham, (893 trained over 2 year period). We provide Postural Stability evidence based exercise groups to clients across five sites across the city of Nottingham. Three times a year we provide a ‘chair based exercise’ trainers programme which is accessed by staff from Care Homes, Day Centres, Voluntary sector and others. We are working in partnership with Age UK, on a two year ‘Nottingham City Signposting Service’ project funded by Supporting People (Housing).The project provides a multi-agency approach to people over 60 years of age to access a range of preventative services through a single point of access. Partners include health, housing, ASH, fire, voluntary sector and others. Health at the heart of the city 12 High impact action number 3: Keeping nourished – getting better. Stop inappropriate weight loss and dehydration in NHS provided care. Improving sip feed guidance to impact on treatment and outcomes for service users. In 2007 the cost of malnutrition and associated disease to the NHS was estimated at in excess of £13.0 billion, about 80% of which was in England. The majority of those identified as being either malnourished or at risk of malnutrition were living in the community. There is evidence that malnourished patients: Visit their GP more often The 2011 guidelines incorporate NICE guidance for nutritional support in adults a review of current literature, particularly two systematic reviews suggesting positive benefits when oral nutritional supplements are used with patients who are underweight (BMI < 20). They have been developed to provide clear evidence-based guidance about how and when to use oral nutritional supplements effectively in adults. Nutritional screening, using a nationally recognised and validated tool, forms an intrinsic part of the guidelines, combined with a clear pathway detailing appropriate actions to be taken. Patient advice leaflets to help improve nutritional intake using everyday foods and information on the practical use of sip feeds are included. High impact action number 4: Need more prescriptions Have more hospital admissions and remain in hospital for longer Have increased morbidity and mortality Have reduced quality of life Promoting normal birth. Increase normal birth rate and eliminate unnecessary Caesarean Sections. During the year the community midwifery service provided a range of initiatives which aim to reduce Caesarian Section rates: Nottinghamshire Oral Nutritional Supplement (Sip Feed) Guidelines for Adults were originally written in 2000, and following their implementation there was a decrease in the prescription of sip feeds. However the level of spending on sip feeds has increased in recent years, and there is evidence that some patients continue to receive them when they are no longer required, whilst others are not prescribed them when they would be appropriate. Therefore a multidisciplinary review of the original guidelines took place, led by Nottingham Community Nutrition and Dietetic Service. The revised guidelines then underwent a large scale consultation exercise, involving GPs and other health professionals throughout Nottinghamshire. Subsequently additional changes were made, prior to submission to the Area Prescribing Committee for approval. Promoted normality as a philosophy of care, with Midwives acting as informed advocates offering a continuous and consistent message at each point of contact prior to labour Promoted normal birth workshops as part of preparation for labour with a focus on first time mothers as we know this is our greatest opportunity to reduce section rates Facilitated normal birth wherever possible at home, and with the maternity team in the hospital setting Supported Vaginal Birth After Caesarian (VBAC) and timely referral for specialist advice with regard to External Cephalic Version (ECV) for women with breech presentation Gave women accurate information following a Caesarian Section to support normal birth in subsequent pregnancies where appropriate Encouraged women to contribute to their birth plan Health at the heart of the city 13 To increase Home Birth rates we: Reported the local Caesarian Section rates to our staff to extend ownership of the shared goal Ensured women don’t get conflicting advice from different agencies through healthy pregnancy and normal birth information being available in Children’s Centres. In addition, to increase normal birth: We use the framework of the Optimum Care Pathway to optimise the potential for normal birth through the midwifery lead professional role and assessment of risk Support choice of place of birth with evidence-based information that is consistent and balances benefit and risk Manage expectations, addressing concerns and fears, to support appropriate choice of maternity team antenatal care Recommend medical intervention only when it is of benefit to the mother or baby through appropriate use of evidence-based intrapartum guidelines Ensure that where specialist care is needed, care is optimised to facilitate normal birth whenever possible Develop a shared philosophy in normality Offer home birth as a choice option in line with Maternity Matters Have an established home birth service that is delivered 24 hours a day by midwives on call Can demonstrate 1:1 midwifery care in the home setting Audit our care against NICE standards Support safe midwifery practice with an on call Supervisor of Midwives Can evidence working with a third sector provider to support women with hypno-birth techniques in labour Support women with identified risk factors who choose home birth against medical advice through managed care plans that minimise risk in collaboration with obstetricians Our home birth data below indicates how the initiatives are translated into positive outcomes. 250 200 200 150 148 2009-10 2010-11 100 50 0 Home birth rate April-March Figure 2: Highlights our figures for home births, demonstrating an increase this year in home birth rates since 2009-10. Health at the heart of the city 14 High impact action number 5: Important Choices; Where to die when the time comes. Avoid inappropriate admissions to hospital and increase the number of people who are able to die in the place of their choice. The key challenges of end of life care in Nottingham City are improving the skills of professionals to identify death and dying issues; for professionals to proactively approach the subject of end of life care with patients and their carers and the challenge to change perceptions of end of life care as a service primarily for patients with a cancer diagnosis to available care for all patients. The end of life care team work with specialist services including Chronic Obstructive Pulmonary Disease (COPD), Heart Failure and Neurology teams. Research has shown that identifying patients significantly increases a patient’s outcome of preventing unwanted admissions and achieving a preferred place of death. Between April 2010 and March 2011 the number of patients on the palliative care register has increased 215% from 250 patients on the palliative care registers to 789. Therefore 50% of all expected deaths in Nottingham City are identified on GP practice end of life care registers. 221 patients have been offered an Information Prescription to communicate their prognosis and allow patients to make choices about their future care; there were a further 64 patients who were not eligible for the Information Prescription because of issues relating to capacity to make decisions about their care. 267 information prescriptions have been offered to carers of patients with end of life care needs to support them during their care and into their bereavement. 317 patients have a completed end of life care index card which shows that 276 patients had their preferred place of care recorded and communicated with other health care professionals. 236 patients achieved their preferred place of care which is 75% of all patients referred to the District Nursing service for end of life/palliative care. High impact action number 6: Fit and well to care. Reduce sickness and absence in nursing and midwifery to no more than 3%. CitiHealth NHS Nottingham commenced the financial year with a challenging local Sickness Absence Target of 3.5% by October 2010 and 3.0% by April 2011. This was set against NHS East Midland’s Sickness Absence Target of 3.5% over the next two years. CitiHealth’s Board recognised that this is a point of concern for both staff and service users. A considerable amount of work has been undertaken to reduce the overall sickness absence rates and to identify the underlying causes of sickness absence. Human Resources have worked closely with senior managers to implement the 2009/2010 Sickness Absence Management Action Plan working alongside the Healthy Workforce Strategy. April 2010 saw the national introduction of the “fit note” which replaced the old “sick note” and aimed at focusing on what an employee may be able to do at work rather than what they could not do. This linked in with the Management of Absence Policy and with the agreed Phased Health at the heart of the city 15 Return to Work Programmes and an Early Interventions Strategy. The organisation implemented a robust training strategy with line managers booked onto sessions throughout the year. Sickness Absence is reported monthly to the Board. The rolling average for the ten month period up to December 2010 was 4.51% which was above the region’s PCT average of 4.38%. Whilst many of our reporting levels through 2010/2011 were within the NHS East Midlands average range, the organisation recognises that there is significant room for improvement. A number of systems and processes were put in place to manage and reduce sickness, including: Issuing services with a sickness absence reduction target/trend line for their area, against which they are performance managed on a monthly basis. Continuation of management absence training for managers. Referral to the Musculoskeletal (MSK) Team for staff with musculoskeletal injuries, as part of a return to work programme, or in some cases as a preventative programme. Managing health at work course – a six week programme looking at managing health and work for staff who have been off on long term sick or are experiencing signs of stress. Stress management workshops for staff and managers. Staff engagement events to follow up on the outcome of the healthy workforce survey and the national staff survey. Deploying social marketing techniques to encourage staff well-being, for example using flyers and holding health and well being workshops. Health4Health CitiHealth’s employees benefited from a new Healthy Workforce programme in 2010-11, called Health4Health, supporting both physical and mental well-being. The official launch of Health4Health took place on 18 March 2010. Dr Steve Boorman was the keynote speaker. Dr Boorman commended the organisation in leading the way for having an excellent healthy workforce strategy. Activities and programmes have run throughout the year. These have included staff offers, a ‘work survival course’ and health walks. We have also launched a new Healthy Workforce intranet section, a new musculoskeletal service for staff and stress busting massages. In July 2010 a six week ‘Work Survival’ pilot programme was conducted. Thirteen employees attended, with seven employees completing the programme. The pilot worked well and received positive feedback. The outcome of this was to launch the ‘Fit for Work Programme’ for the wider workforce. Workshops were free to all employees and provided three levels of support: Work Survival - Courses aimed specifically at helping employees to manage their health and work. Support into work – one to one help for employees from a health professional to tackle health issues and stay in work. Working for Health – Independent advice and support for organisations to help develop and retain a healthy workforce. Ongoing reviews of policy, procedure and guidance continues to support staff whilst absent from work. Health at the heart of the city 16 17 High impact action number 7: Ready to go – no delays. Increase the number of patients in NHS care who have their discharge managed and led by a nurse or midwife where appropriate. During the last year the following projects have been ongoing: We have joined the discharge operational group led by Nottingham University Hospitals. This is a cross City/County health and social care group set up to look at the discharge pathways from Nottingham University Hospitals. A pathway has been developed to ensure all incidents relating to discharge are fed back constructively to Nottingham University Hospitals who are ensuring that the feedback gets back to ward level to ensure processes are improved. The development of the in-reach worker within the Crisis Response pilot as part of the Intermediate Care service. This person is employed by Nottingham CityCare Partnership but is based within Nottingham University Hospitals. The Band 4 employee works across the GP admission wards and emergency department to actively find patients who can be discharged back to the community, avoiding a hospital admission or facilitating an early discharge. This constitutes 46% of the referrals to Crisis Response. There have been identified cost savings for both health and social care. Community Matrons will follow patients into Nottingham University Hospitals when admitted. Liaison with emergency department or ward staff enables the decision for discharge to be made in a more timely and appropriate manner. Current difficulties for Matrons are knowing when their patients have been admitted. Health at the heart of the city 18 High impact action number 8: Over 2010-11 the organisation has addressed this by developing: A standardised guide for the review of urinary catheters. Teams report on a monthly basis the number of patients with catheters on the caseload and the numbers who have had an assessment and as a result of the assessment have had a catheter removed. A discharge pathway for patients being transferred from hospital to home with a urinary catheter. A troubleshooting guide for carers and staff to alert carers and clinicians to review a patient’s care if they develop an infection, rather than just prescribe antibiotics to treat the infection. Leaflets for patients with supra pubic and urethral catheters to assist them with the day to day management and how they can prevent infections. Protection from infection – Demonstrate a dramatic reduction in the rate of Urinary Tract Infections (UTIs) for patients in NHS provided care. In response to the concerns raised nationally about the high level of urinary tract infections (UTIs) from which patients were suffering, the organisation has over 2010-11 begun to review the patient pathways associated with both urinary catheters and patients with a history of recurrent urinary tract infections. In conjunction with this NHS Nottingham City also developed a local commissioning for quality innovation (CQUIN) target relating to urinary urethral catheter care. Urinary Catheter Care Pathway Locally evidence from root cause analysis investigations had shown that there were issues with the care and management of urinary urethral catheters. The issues identified were as follows: No standardised review of the need for the urinary catheter. No discharge pathway identified for patients with urinary urethral catheters. Day to day management of catheters was by patients or by carers. Registered nurses were only involved at the time the catheter was due for change or if problems developed with the catheter such a blockage or leaking from the site. Recurrent Urinary Tract Infection Pathway Within CitiHealth, the Urology and Continence Advisory Services were seeing an increase in the number of patients being referred by clinicians due to recurrent urinary tract infections. Both departments have worked together to develop the following: The key challenges over 2010-11 were to ensure that if patients had urinary urethral catheters a definite need had been identified with a clear management plan and with roles and responsibilities of individual services clearly defined. A clear pathway for clinicians indicating what treatments should be tried and when patients should be referred. An in depth questionnaire to aid clinicians with the referral process Health at the heart of the city 19 2.4 PATIENT EXPERIENCE worked well and what could be better and these were themed under specific headings. Nottingham CityCare Partnership is committed to improving the experience of people using our services. We have worked hard this year to develop internal processes that are better co-ordinated, consistent, monitored and effective. We have established the following processes enabling patients/service users to tell us about their experience of our services, what we do well and how we can improve. To improve access, the survey is available in 42 community languages, large print and Braille. Patient/Service User Satisfaction Survey Involving people using our services and staff, we developed a standard satisfaction survey and a co-ordinated system to capture, collect, understand and act on patient experience. A standard survey and service improvement action plan were piloted and rolled out across all services from January 2011. People were invited to regularly rate our performance on issues important to them, like being well supported, informed, involved in decisions, treated with dignity and respect, confidentially, having particular needs met and overall satisfaction. People also told us what We know there are limitations to using surveys as a method of collating patient experience with some individuals and groups and we are exploring ways to address this. Establishing Systems to Capture and Report Patient Experience Survey results were collated using an ‘in house’ data system, enabling us to assess our performance on specific areas at both service and organisation level including actions to improve patient experience. In addition to surveys we have also developed monthly reporting via health centres capturing patient comments, concerns and compliments around our services. To date around 200 comments have been collated and are being analysed for trends and improvement actions. Data collated centrally and manually has proved to be labour intensive. We are therefore looking at options to improve efficiency, effectiveness and quality of patient experience data. Health at the heart of the city 20 Satisfaction Survey Results to Date 1465 people responded to our patient satisfaction survey between January and March 2011 and feedback exceeded our 85% satisfaction target (‘good’ or ‘excellent’). Overall Satisfaction Very Poor, 2, 0% Poor, 4, 0% Here is a summary of how service users rated our performance: OK, 71, 5% Good, 376, 26% No Comment 73.5% Excellent 939, 64% How well would you rate the support you received? Very Poor, 1, 0% Poor, 13, 1% Overall satisfaction of services was rated as good or excellent by 90% of people. No Comment, 35, 2% OK, 87, 6% Excellent 943, 65% Good, 386, 26% Figure 5: Charts Overall Satisfaction 91% said the support they received was good or excellent. Figure 3: Highlights service users rating of the support they received How well were you kept informed? Very Poor, 3, 0% Poor, 8, 1% OK, 99, 7% No Comment 35, 2% Excellent 865, 59% Good, 455, 31% Additional feedback: How well… Our Satisfaction Satisfaction Achieved Target Were you involved in decisions 85% Good or Excellent 88% Were you treated with dignity and respect 92% Was confidentiality respected 92% Were your particular needs met 88% Table 2: Additional feedback from service users 90% said their experience of being kept informed was good or excellent. Figure 4: Highlights how service users rated their experience of being informed. Service changes and improvements made as a result of patient and public feedback Services collate responses internally. Patient feedback from the surveys was collated and themed by teams who developed action plans in response to this. Health at the heart of the city 21 Results are forwarded to the Head of Patient and Public Engagement who centrally collates, coordinates, monitors and reviews patient satisfaction surveys, so that the organisation can monitor these results and actions and respond accordingly. The top five areas where patients told us we did well: Providing information Providing support/care Having friendly, knowledgeable, skilled, well presented staff Being treated with dignity and respect Being listened to, involved in decisions and able to have a say What works well? Other Information Provided Particular needs(eg. Disability, Language, Culture) Support/Care Provided Resources eg Products & Equipment Facilities - availability, quality and usefulness Cleanliness Ease of Access Location Ease of getting an Appointment Time of Appointment Wait for an Appointment Friendly, helpful, knowledgeable, skilled well presented Confidentiality respected Treated with Dignity and Respect Listened to involved in decisions, Able to have a say 0 50 100 150 200 250 300 350 Figure 6: Highlights service users perspective of what works well The top five areas where patients told us we could do better: Providing information Providing support/care Make it easier to get an appointment Improve access to services Reduce waiting times for appointments No adverse comments were made about cleanliness Individual services are progressing actions in response to their feedback and this is monitored quarterly by the Head of Patient and Public Engagement to ensure feedback is acted upon. What could be better? Other Information Provided Particular needs(eg. Disability, Language, Culture) Support/Care Provided Resources eg Products & Equipment Facilities - availability, quality and usefulness Cleanliness Ease of Access Location Ease of getting an Appointment Time of Appointment Wait for an Appointment Friendly, helpful, knowledgeable, skilled well presented Confidentiality respected Treated with Dignity and Respect Listened to involved in decisions, Able to have a say 0 10 20 30 40 50 60 Figure 7: Highlights service user suggestions for improvement Health at the heart of the city 22 Draft Patient Public Engagement Strategy and Action Plan As a result of Transforming Community Services and establishing Nottingham CityCare Partnership, we have drafted a Patient and Public Engagement Strategy and Action Plan and are consulting with patients, service users, carers and the public about this. PALS and Complaints reports The Complaints Team successfully handled 81 complaints about CitiHealth NHS Nottingham in 2010/2011 in accordance with the 2009 NHS complaints regulations. Complaints Officers have agreed the details of each complaint with the complainant, negotiated timescales and complaints handling, allocated them to Investigating Officers and drafted response letters for approval and sign off. Complaints about the Prison Healthcare Service presented challenges in terms of the numbers received (21 or 26%) and complainants moving from one establishment to another. The Complaints Team has worked in partnership with the Prison Healthcare Service to ensure that most complaints are handled in-house with only the most intractable complaints being handled by the Complaints team. Sometimes complaints are a result of problems with staffing levels which may be temporary or longstanding. During the year we saw an increase in complaints received about the Community Midwifery Service including complaints about continuity of care, and difficulties in arranging appointments; at that time the service was having difficulties recruiting midwives due to a shortage of qualified midwives. In response the service set up a programme to employ newly qualified midwives direct into the community; they were supported through a national preceptorship programme (a process to support newly qualified staff through the transition from student to accountable practitioner). The Complaints Team has also managed the Patient Advice and Liaison Service and 83 enquirers have been helped with information and advice about a number of services, including a significant number of enquiries about podiatry and physiotherapy appointments. Health at the heart of the city 23 2.5 PARTICIPATION IN CLINICAL AUDIT Clinical audit is a quality improvement process. It aims to improve patient care and outcomes through a review of care against clear criteria and making changes in light of this. During 2010-2011, no national confidential enquiries and two national clinical audits covered NHS services that CitiHealth provides. During that period CitiHealth participated in 50% national clinical audits and 100% national confidential enquiries of the national clinical audits and national confidential enquiries which it was eligible to participate in. The national clinical audits and national confidential enquiries that CitiHealth was eligible to participate in during 2010-2011 are as follows: National Audit of Psychological Therapies for Anxiety and Depression National Audit of Falls and Bone Health in Older People The national clinical audits and national confidential enquiries that CitiHealth participated in during 2010-2011 are as follows: National Audit of Psychological Therapies for Anxiety and Depression The national clinical audits and national confidential enquiries that CitiHealth participated in, and for which data collection was completed during 2010-2011, are listed below alongside the number of cases submitted to each audit or enquiry as a percentage of the number of registered cases required by the terms of that audit or enquiry. National Audit of Psychological Therapies for Anxiety and Depression 100% The reports of 1 national clinical audits were reviewed by the provider in 2010-2011 and CitiHealth intends to take the following actions to improve the quality of healthcare provided: Health at the heart of the city National Audit of Continence Care 2010 Promote documenting of duration of symptoms, nocturnal symptoms, and faecal incontinence frequency through training sessions Research potential standardised measures to record functional ability and cognition Promote increase in rectal examinations through training and through dissemination of new clinical guidelines for Manual Removal of Faeces and Digital Rectal Examinations Improve links to geriatric medicine though Geriatrician who now attends Multidisciplinary Team meetings and invite to Link Nurse Day Promote assessments of Quality of Life using a validated symptom score/ standardised assessment scale by discussing use of ICIQ (currently used by the Continence Advisory Service but not District Nurses) Promote documenting type and cause of incontinence through training sessions Practice Pharmacists to raise awareness with GPs (as part of prescribing audit of continence products) of minimising medicines which may exacerbate urinary incontinence Discuss ways of recording/ collating patient suggestions with District Nursing, potentially using PALS Explore re-establishing user group Discuss whether patient satisfaction survey used by Continence Advisory Service could be used within District Nursing Promote discussions with patients/ cares on type and cause of continence through training sessions. Promote provision of copies of treatment plans to patients and carers through training sessions. Obtain details from PALS of relevant support groups and psychological/ emotional support available as part of long-term faecal incontinence management Table 3: National Audit of Continence Care actions. 24 The reports of 15 local clinical audits were reviewed by the provider in 2010-2011 and CitiHealth intends to take the following actions to improve the quality of healthcare provided: Bilingual Co-Worker Client Access Report written and sent to Assistant Director of Adult Services, Human Resources, Service Head and Education & Development Manager. Meetings held and an action plan developed to put systems in place to improve access to the Bilingual Co-worker role for service users, and for the team to access the role appropriately. Contraceptive and Sexual Health (CASH) Blue Forms Chlamydia Screening Office to offer training to pharmacists to include collecting vital partner information. Altering the blue form to show if patients decline to give partner information. Amendments to the audit tool (to include questions about whether the patient has declined partner information and confirm whether treatment was given instead of what treatment given) in preparation for re-audit May 2011. Children’s Continence Circulating the Paediatric Continence Service Newsletter to GPs and Community Paediatricians via email. Considering shorter training packages or training on specific topics such as toilet training so staff are not away from their clinical workload. Looking at the option of developing e-learning packages. Looking at the way the Continence Advisory Service as a whole deliver training as they move into a social enterprise. Closer liaison with Community Paediatricians and GPs. Developing a pathway of care for children with continence problem in the community in conjunction with medical staff. Follow up letter for all referrals. Continuing Care Decision Support Tool (DST) Nurses to be reminded of the need to complete the ‘Lead co-ordinator name’ on the DST. Feedback the re-audit results to the whole Continuing Care Team. Alert nurses to change of form with regards Assessor’s details no longer on the front page of the DST tool. Take learning from the re-audit regarding different interpretation of questions by different people to Clinical Audit Team meeting and build into future practice by producing guidance notes for all data collectors. Remove legibility questions from the audit tool. Community Macmillan Bereavement Standards Only details of deceased patients whose deaths the team have been made aware of to be included in the Bereavement File. Health at the heart of the city 25 All staff to improve their documentation of bereavement follow-up once entries are made into the Bereavement File. Follow up telephone calls to bereaved relatives and carers to be made as soon as is reasonably possible to contact them following notification of the patient’s death. Subsequent calls to also be recorded by date in the Bereavement File. If a home visit or support in a clinic setting is deemed appropriate, the team will offer a one off appointment followed by signposting, referral on to other agencies or telephone follow up. Guidelines will be formulated to standardise the written contents of condolence cards and letters (in the form of letter templates). Documentation in Bereavement File to be developed to capture details of the support offered/provided as accurately as possible. Community Macmillan Referrals Not Seen Ensure all information relating to the referral is securely tagged together. Enter the date and relevant Referral Not Seen code on the front page of the notes. Document an agreed action plan in the patient’s records the reason not seen. Inform the referrer when the patient is not seen and the reason why if appropriate. Develop a standard “Referred Not Seen” letter. Ensure all team members are aware of service referral criteria. Include a copy of the service leaflet for professionals when writing back to referrers when referral was inappropriate or declined by the patient. Monitor the number of inappropriate referrals and those declined by patient. Essential Steps to Safe Clean Care Services to disseminate the findings from the audit across the clinical staff groups and to highlight the issues around single use items and the appropriate changing of gloves and aprons during procedures in accordance with the Aseptic non-touch technique policy. All new staff should have the process explained as part of their induction process. Infection Prevention and Control Team to standardise the tool to enable comparisons to be made across all services. Locality Leads to launch the new tool with services and to continue with the audits across clinical teams. Hand Hygiene Raise awareness of Uniform and Hand Hygiene Policies. Audit to be re-designed and re-launched in April 2011. Health at the heart of the city 26 Contraception Implant Retention Overall the service has successfully implemented implant removal into the drop in clinics but still have a long way to go to reduce and maintain the waiting list. It is probable that a waiting list initiative will be needed to reduce it but this is expensive and not a long term solution. Maintaining high standards of counselling, providing support to patients who do suffer problem side effects to encourage them to retain their device with emphasis placed on ‘six months’ as the time required for trying this method should enable continuing to provide a good service. The service are considering keeping a small stock of alternative medication for treatment of problem bleeding within clinic so these alternatives could be more easily offered. Musculoskeletal Physiotherapy Patient Results shared with MSK Physiotherapy team September 2010. Results shared with the service lead/s and Assistant Director of Adult Experience Audit Services. Results shared with commissioner responsible for MSK Clinics Record Keeping – Generic (33 services) Chase outstanding reports and outcomes forms through Assistant Directors Set up a time-limited group to discuss and action findings of the audit, including reviewing trends from action plans to identify any action required at organisational level, and identifying changes needed to the audit tool/ guidance to ensure clarity and consistency of results Sub-group to report to Governance Compliance Group Record Keeping – Infection Prevention & Control Access to SystmOne Patient documentation has been reviewed to include: Patients address, Patient postcode, Patient telephone number, Occupation, NHS number, Signature sheet Written guidance now in place for: Guidance on storage of filing cabinet keys, Documented named persons with permission to access patient notes, Tracking of records Corrections and use of abbreviations discussed at team meeting Team needs to review the records to include patient title and organisational address. Record Keeping – Safeguarding Children Improve documentation to incorporate demographic and diversity information Revise documentation to incorporate staff identification information Address changes at team meeting and at individual supervision sessions to increase awareness that information needs to be recorded Review organisation policy for transportation and transfer of records and adapt to fit service Health at the heart of the city 27 Safeguarding Children Health Visitors’ Supervision Safeguarding Children Nurse Specialists to ensure that database reviewed prior to supervision sessions in order that files are supervised within timescales Documentation revised to incorporate staff identification information Address at team meeting and at individual supervision sessions to increase awareness that information needs to be recorded Safeguarding Children Nurse Specialists to ensure that High Support Files taken to supervision sessions in order that all files reviewed within timescales Address at team meeting and at individual supervision sessions to ensure that photocopying completed and documentation attached to High Support Files for administration staff to file Design post-supervision action plan to be attached to each file for administrative purposes To investigate highlighting files which breach timescales, electronically, by contacting IT Department to discuss options and possibilities Transfer of Care Processes Following the audit, the Transfer of Care policy was revised and ratified in March 2011. A re-audit is planned for September 2011 Table 4: Local Audit Actions Health at the heart of the city 28 2.6 PARTICIPATION IN CLINICAL RESEARCH Clinical Research influences the safety and effectiveness of medications, devices/equipment, diagnostic products, treatments and interventions intended for patients. These may be used for prevention, treatment, diagnosis or for relief of symptoms in a disease. The number of patients receiving NHS services provided or sub-contracted by CitiHealth in 2010-11 that were recruited during that period to participate in research approved by a research ethics committee was 149. CitiHealth was involved in conducting 51 studies in 2010-11: 20 NIHR portfolio studies and 31 non portfolio studies. The studies involved a wide variety of community specialties including post stroke community rehabilitation, falls prevention, tissue viability, smoking cessation and community midwifery. 2.7 GOALS AGREED WITH COMMIS SIONERS Commissioning for Quality and Innovation (CQUIN) CQUIN is a payment framework which enables commissioners to reward excellence by linking a proportion of providers’ income to the achievement of local quality improvement goals. Use of the CQUIN payment framework During 2010/11 1.5% of CitiHealth NHS Nottingham’s income was conditional on achieving optional quality improvement and innovation goals agreed between CitiHealth and NHS Nottingham City, through the Commissioning for Quality and Innovation (CQUIN) payment framework. The table facing describes the detail of the targets set by our commissioners NHS Nottingham City Primary Care Trust (the local targets) and also those set by NHS East Midlands (the regional targets). In order to achieve the targets we set up a robust process with a task and finish team consisting of the CQUIN leads in each area, and staff from the Business Unit. Most importantly the frontline staff embraced the work involved and this resulted in an excellent outcome with most goals set achieved. Despite the hard work required to achieve the targets and the fact that they were optional for providers we have set a benchmark and will be keen to see further gains in the next year. Further details of the agreed goals for 2010/11and for the following 12 month period are available electronically at http://www.institute.nhs.uk/world_class_commiss KEY TO TABLE 5 OPPOSITE Target not met; 0% payment Target not met, but intermediate threshold applicable and met; 50% payment Target met or exceeded; 100% payment Quarterly target not applicable Result not yet known Health at the heart of the city 29 CitiHealth CQUIN 2010/2011 CQUIN Ref. Indicator Description Q1 Q2 Q3 Q4 Target Result Target Result Target Result Target Result Percentage of community provider drug delivery devices 25% 27% 50% 52% 75% 79% 100% that have been safety checked in the appropriate time period Incidence of grade 2 or higher CR3 - Pressure Sores pressure sore in older people Baseline Baseline 1.04% 0.90% 1.03% 0.63% 1.02% treated in a community setting CR4 - Dietetics City 19 days 18 days 17 days 16 days 16 days CR4 - Dietetics County Waiting times for treatment Baseline Baseline 60 days 32 days 55 days 27 days 50 days CR4 - Physiotherapy and therapy services 23 days 23 days 22 days 22 days 21 days CR4 - OT 23 days 10 days 22 days 14 days 21 days Percentage of Long Term CR5 - LTC Care Plan Condition (LTC) patients with Baseline Baseline 100% 100% 100% 100% 100% a personal health/care plan The percentage of people discharged from hospital and benefitting from intermediate CR6 - 91 days Status care/rehabilitation enablement Baseline Baseline 65% 78% 70% 81% 75% who have not been readmitted to hospital by day 90 Percentage of staff(with face to face patient contact, excluding CL1a - Brief Intervention administrative staff) from identified 10% 18% 30% 55% 60% 69% 75% teams trained to conduct stop smoking brief intervention Percentage of specialist nurses for identified conditions/disease CL1b - Cessation areas to be trained to conduct 10% 21% 30% 71% 60% 75% 75% smoking cessation intervention using New Leaf protocol and guidance Percentage of work days lost CL2 - Sickness Absence to long term sickness absence Annual Indicator- Result due May 2011 1.82% Percentage of adult patients with Indwelling urinary catheters CL3a- Assessment receiving an assessment of need 15% 22% 50% 64% 75% 75% 95% in relation to the catheter Percentage of adult patients whose Indwelling urinary catheters CL3b - Removal have been appropriately 15% 100% 50% 100% 75% 100% 95% removed following an assessment of need in relation to the catheter Percentage of patients using services have been involved in CL4a - PPI Surveys the agreed patient satisfaction Scoping Scoping Design Design Pilot Pilot Roll out surveys (asking additional questions beyond contract requirement) Percentage of services that have CL4b - PPI Services made service improvements on Format Format Identify Identify SummarySummary Final the basis of patient feedback Percentage of all eligible patients that have been offered an CL5a - EOL Patients Information Plan or there is 15% 27% 30% 35% 45% 64% 60% documentation that an Information Plan has been offered and declined Percentage of all eligible carers of EoL patients that have been offered CL5b - EOL Carers an Information Plan or there is 10% 40% 45% 56% 50% 64% 55% documentation that an Information Plan has been offered and declined Percentage of Chlamydia CL6 - Chlamydia contacts converted to screens 30% 26% 40% 29% 50% 25% 60% within identified services Increase the number of Common CL7 - CAFs Assessment Framework initiated 10 3 15 10 19 9 10 by midwives Percentage of all eligible women that have been asked about CL8a - MWsDV Domestic Violence at pregnancy 25% 32% 50% 100% 75% 100% 100% booking visit (Midwifery) Percentage of all eligible patients that have been asked about Domestic CLBb - HVsDV Violence at Health Visitor birth visit 25% 100% 100% 100% 100% 100% 100% Percentage of staff (with face to face patient contact, excluding CL9 - Alcohol Training administrative staff) from identified 10% 19% 30% 26% 60% 73% 75% teams trained to deliver brief advice (alcohol) Percentage of staff (with face to face patient contact, excluding CL10 - Warmth Training administrative staff) from identified 10% 0% 20% 20% 35% 49% 50% teams trained to identify and refer patients to the Healthy Housing CR1 - Drug Devices 100% 0.78% 14 days 25 days 20 days 11 days 100% 78% 81% 75% 0 91% 100% Roll out Final 63% 60% 28% 21 100% 100% 76% 88% 30 Table 5: CQUIN target achievements 2010-11 2.8 WHAT OTHERS SAY ABOUT US Statement on Care Quality Commission (CQC) registration The CQC is the independent inspector and regulator for health and social care organisations, ensuring we meet essential standards in quality and patient safety. CitiHealth NHS Nottingham is required to register with the Care Quality Commission and its registration status for the year 2010/11 was Registered. CitiHealth NHS Nottingham registered without condition to provide its regulated activities across its registered locations. CityCare Partnership is registered without condition to provide its regulated activities across its registered locations. The Care Quality Commission has not taken enforcement action against Nottingham CityCare Partnership to date. Full details of our registration can be found on the Care Quality Commission on line directory here www.cqc.org.uk CitiHealth NHS Nottingham participated in a Nottingham-wide review of Safeguarding and looked after Children by Ofsted and the Care Quality Commission during April 2010-March 2011: Nottingham was given a ‘good’ rating. The Care Quality Commission has not taken enforcement action against CitiHealth NHS Nottingham during April 2010 - March 2011. Since April 2011 Nottingham CityCare Partnership became newly registered with the Care Quality Commission and its current registration status is registered. Nottingham Health at the heart of the city 31 2.9 STATEMENT ON DATA QUALITY On going data quality improvement inline with Data Quality Improvement Plan (DQUIP) agreed with commissioners in line with section 5 and clause 32 of the NHS Community Contract. Priorities for data quality improvement for 2010/11 included collecting key information on first and follow appointments by GP practice for all applicable services. 31 tasks identified in the initial DQUIP had been completed by 31 March 2011. Information Governance Toolkit attainment levels The NHS Nottingham City (which includes CitiHealth NHS Nottingham) Information Governance Toolkit Assessment Report for 2010/2011 scored 72% overall and was graded Green ‘Satisfactory’. The Information Governance Toolkit Assessment was audited by East Midlands Internal Audit Service and received Significant Assurance. Clinical coding error rate CitiHealth NHS Nottingham was not subject to the Payment by Results clinical coding audit during April 2010-March 2011 by the Audit Commission. Monthly meetings are held with the lead commissioner to monitor progress against the DQUIP priorities. The initial focus was to ensure that all services had clear metrics relevant to their service specifications and could collect the basic data sets required. This provided evidence to support and under pin their clinical and cost effectiveness. The priority going forward is developing systems and processes for more proactive checking of data quality in a way that provides on going assurance to patients and evidence to commissioners of continuing data quality improvement. NHS Number and General Medical Practice Code Validity CitiHealth NHS Nottingham did not submit records during 2010/11 to the Secondary Uses Service for inclusion in the Hospital Episode Statistics which are included in the latest published data, as this is not applicable to us as a community service. Health at the heart of the city 32 Part 3 – Priorities for Quality Improvement 2011/2012 3.1 PATIENT SAFETY Review training strategy. Safeguarding Children and Vulnerable Adults Safeguarding Adults 2011-12 presents an opportunity for Nottingham CityCare to build on and develop the progress achieved last year under the supervision of the Adult Safeguarding Steering Group which directly reports to the Governance Committee and also via the work of the Adult Safeguarding Lead. Initiatives for 2011-12: We intend to carry out an evaluation of service user satisfaction. We will carry out an assessment against the Adult Safeguarding Assessment Framework which was developed by the Department of Health as part of the earlier pilot. We intend to deliver essential training to all relevant staff. As part of our CQUIN we intend to deliver basic dementia care training to all patient facing staff – this will comply with Quality Standard 1 in the Dementia Quality Standard (NICE June 2010). We will collaborate with the Walk in Centre and Nottingham Emergency Medical Services to further the work of the Adult Safeguarding Steering Group. Health at the heart of the city 33 Serious Incident Reporting Safeguarding children Nottingham CityCare will ensure the implementation and recommendations of the findings of the recent Safeguarding and Looked After Children Inspection. We will ensure that we implement the recommendations from the Markers of Good Practice Assessment and continue to take part in our annual assessments. Explore opportunities to work closer with Adults and Children’s social care. Nottingham CityCare continues to make a tangible shift to early intervention through use of the Common Assessment Framework, leading to improved identification of need and integrated delivery of health and social services. A review of the current model of Safeguarding Supervision is underway. Nottingham CityCare will increase its closer partnership working with Nottingham Emergency Medical Services (NEMS) and the Local Authority. To ensure the views of children and young people are recorded in a way that provides assurance that they have been heard and their wishes and feelings are being taken appropriately into account in planning. Ensure unconditional registration with CQC plan for the new organisation April 2011. HR department to establish a robust Electronic Staff Record (ESR) system for collection of safeguarding training records for staff and CRB checks. As one of the highest reporters of incidents to the National Patient Safety Agency, the Governance Team will continue to improve the way that information is made available to teams so that they are able to see trends that need to be addressed. The vast majority of our patient safety incidents are classed as no harm or low harm incidents. We are committed to continuing to build a Safety Culture by encouraging reporting of incidents and supporting the recognition of lessons that can be learned from incidents and ensuring that lessons are shared and implemented to improve safety for all patients. We are cascading web reporting so that staff can report incidents directly on line. The Head of Patient Safety will also be training staff and supporting the investigation of incidents and complaints using the Root Cause Analysis tools, to clearly identify system failures and support the development of the improvement of those systems. Four training sessions will be delivered to staff Team Leaders and clinical managers and the Head of Patient Safety will continue to support managers in more complex investigations. As part of Serious Incident investigation training several of our senior managers will also be provided with training in Being Open which involves specialist training in communicating with patients, their families and carers following a patient safety incident in which the patient was harmed. We will also be producing ‘spotlights’ to highlight areas of good practice and lessons learned to share across all services. Health at the heart of the city 34 Infection Prevention and Control Medicines Management MRSA The increased reporting of incidents, but with reducing seriousness, will remain a focus of our activity during 2011/12. Our Lead Pharmacist will be a member of the Patient Safety Committee and will review any significant medicine related incidents within 5 working days of their occurrence and agree if any immediate actions are required. Any incidents with actual harm greater than low harm will be investigated and a written action plan produced and approved by the Lead Pharmacist. To continue to review all cases and review the themes from root cause analysis investigations to ensure that change occurs. Change is monitored through the Health Economy County Wide Infection Prevention and Control Committee. C- Difficile During 2011-12 the antibiotic guidelines have been revised and will be launched to both non-medical and medical prescribers. We will review an electronic audit tool which has been developed by pharmacists locally, with a view to auditing the implementation of the guidelines within primary care. We will implement the definition of what constitutes a ‘positive case’ with the Infection Prevention and Control Team; individually reviewing all community and pre-72 hour admission cases. The Lead Pharmacist will also work with the Head of Patient Safety to support services in developing action plans in response to any patient safety alerts relating to medication. Other key priorities for medicines management for Nottingham CityCare for 2011-12 are to: Implement the new Non-Medical Prescribers (NMPs) policy, by ensuring full dissemination of the policy and monitoring the use of the policy Deliver a rolling programme of medicines management training to staff within care homes (includes refresher and new staff training on an 18 month rolling programme). Medicines management technicians will conduct compliance reviews of medication with patients/services users with Long Term conditions. Health at the heart of the city 35 3.2 CLINICAL EFFECTIVENESS These areas for improvement align with the NHS High Impact Actions identified from page 10. evidenced based and patient-centred primary/secondary care falls services. Referral for falls assessment will be included in the Fracture Liaison Service pathway. High impact action number 1: Your skin matters. No avoidable pressure ulcers in NHS provided care. Implementation of pressure ulcer incidence collection via SystmOne (a computerised health record). Restructuring of the feedback mechanism to the District Nursing Teams. Introduction of a two hour mandatory training programme for all registered nurses and health care assistants. This will incorporate all aspects of pressure ulcer prevention but also consider the themes of the RCA findings in relation to care provision. Review of the current documentation around risk assessment and core care plans currently accessible on system 1. Consider the introduction of Skin Bundles across District Nursing Services. High impact action number 2: Staying safe – preventing falls. Demonstrate a year on year reduction in the number of falls sustained by older people in NHS provided care. In partnership with Nottinghamshire county falls services/secondary and commissioners we will develop a single point of access for patients who reach the Emergency Department and need a falls assessment. (A high percentage of these patients do not get referred to services). Review the Falls Services, (linking with Nottingham University Hospitals rehabilitation unit) further streamlining processes to ensure effective, © NHS Photo Library This initiative will be taken forward by the achievement of the following objectives: High impact action number 3: Keeping nourished – getting better. Stop inappropriate weight loss and dehydration in NHS provided care. A multidisciplinary group has been set up to facilitate implementation of the sip feed guidelines across Nottinghamshire; the group will develop a full implementation plan. Prescribing costs of sip feeds will be monitored, as it is envisaged that they will be prescribed more appropriately and their usage better monitored due to the guidelines and this in turn should result in reducing costs over time. It is expected that the implementation of the guidelines should increase referral for patients with complex needs who require dietetic input. The service will monitor referral rates for this type of referral in order to assess if this occurs. Health at the heart of the city 36 High impact action number 4: Promoting normal birth. Increase normal birth rate and eliminate unnecessary caesarean sections. Midwifery services have now transferred and will be delivered by Nottingham University Hospitals; therefore this will not form such a significant part of our development planning for normal birth. The Family Nurse Partnership will however in its support for young teenage pregnant women continue to work to promote normal birth. High impact action number 5: Important Choices; Where to die when the time comes. Avoid inappropriate admissions to hospital and increase the number of people who are able to die in the place of their choice. The Nottingham End of Life Care Team offer teaching, advice and support to health and social care professionals to tackle these issues to empower staff to take end of life care forward with a positive supportive approach. The team has developed key documents to support professionals to face these challenges. The team are training professionals in the use of the Gold Standards Framework Prognostic Indicator guidance using a Read code search in GP practices to identify patients with organ failure, or frail/dementia to increase the number of patients on the palliative care register. The Information Prescription is a communication tool that incorporates preferred priorities of care for patients and their carer and provides patients and carers with the appropriate material they require when facing challenging care decisions at the end of their lives. The End of Life Care Team is introducing a new service to offer alternative choice for patients that is not hospital or their own home, but care in a hospice-like environment in a local care home where they can receive respite care and terminal care preventing an admission for the patient. High impact action number 6: Fit and well to care. Reduce sickness and absence in nursing and midwifery to no more than 3% Our aim for 2011/2012 remains to bring sickness absence down to the commissioner’s target of 3% across all services not just those within Nursing and Midwifery. It remains an important focus for us and is also important for our staff. Work has already commenced on reviewing our ESR data and a decision has been made to move from monthly to weekly reporting, to ensure more timely data is available to managers. Working alongside the revised Sickness Absence plan with new departmental trajectories, it is proposed that Organisational Development and Occupational Health work with managers to identify causal effects within targeted areas of high concern. There is a commitment to introducing “Management Self Service” within the Electronic Staff Record thus placing the management of absence with managers and ensuring managers are fully responsible for the management of absence levels within their area. We believe investing in our employees and improving the working environment is also an investment in patient care. The team are introducing the palliative card index which is a SystmOne template that records key points in the patient’s end of life care pathway. This enables professionals to plan and implement care to ensure that patients’ wishes and needs are met to facilitate their preferred priorities for care. Health at the heart of the city 37 High impact action number 7: High impact action number 8: Ready to go – no delays. Increase the number of patients in NHS care who have their discharge managed and led by a nurse or midwife where appropriate. Protection from infection – Demonstrate a dramatic reduction in the rate of Urinary Tract Infections (UTIs) for patients in NHS provided care. There should be an increase in the number of patients who have their discharge facilitated from community-led services due to the following initiatives: During 2011-12 the major priorities are as follows: The Community In-reach pilot aims to test the impact that a community in-reach team can have on reducing the numbers of patients with a 14 day length of stay or more and preventing the admission of people directly into long term care at the point of discharge from hospital. It is expected there will be a 50% reduction in the number of patients with a length of stay over 14 days. Initially the service will focus on one ortho-geriatric ward at the Queen’s Medical Centre but may expand during the pilot in light of available capacity and lessons learnt. This will be starting in June 2011 – March 2012. The pilot incorporates audit and qualitative service evaluation. The Crisis Response Team is to be mainstreamed from 1 June 2011. This will enable out of hours and weekend cover. Crisis response will be piloting clinicians working up to 10pm within Intermediate care to see if the number of out of hours discharges from Nottingham University Hospitals (NUH) can be increased. Development of a pilot to enable specialist information to be available at NUH to help decision making for discharge of COPD patients. Implement the pathway and troubleshooting guide for catheter care further to ensure it is embedded within care delivery. This will require an audit of practice to be undertaken and further work around implementation of findings. To implement and embed within practice the recurrent UTI management pathway. To start to review the hospital admissions as a result of UTIs particularly from care home environments to try and reduce the number to admissions and ensure the incidence of infections is reduced. Health at the heart of the city 38 3.3 PATIENT EXPERIENCE The Board is committed to continued improvements in the experience of people using Nottingham CityCare services. Based on our work last year, we wish to prioritise the following four areas within Patient Experience: Patient Satisfaction Survey and Service Improvement Action Plans We will build on the current process of seeking and acting upon patient satisfaction/ feedback by: Making electronic hand held devices and on line surveys available in addition to current paper surveys. Improving access for children and young people, people from black and minority ethnic groups, people with disability and learning disability, cognitive impairment and other seldom heard groups to feed back their experience. This fits with the organisation’s duty to meet the Equality Delivery System standards. Improving Processes for Collating and Reporting Patient Experience Patient Public Engagement Strategy and Action Plan Feedback from patients, staff, communities and the public will inform our final Patient Public Engagement Strategy and Action Plan. Meridian Patient Feedback System and Hand Held Devices. From 2011 the Meridian system will improve the access, quality and reporting of our patient experience data. Meridian will provide an integrated web-based system capturing patient feedback through the inputting of survey data and real time data collection for those who can complete surveys using hand held devices or via our website. In addition to formal complaints, we will continue to collate comments, concerns and compliments. Our intention is to triangulate patient surveys, incident reports, PALS data, complaints and comments, concerns and compliments data, to give us a fuller understanding of patient experience including actions for improving patient safety and experience. Patient Experience Group (PEG), Membership Panel and Strengthening Partnerships As a newly established Community Interest Company, we will facilitate a PEG and Membership Panel inclusive of diverse and seldom heard groups. We will strengthen our relationships with patient/ carer groups, LINks/HealthWatch and voluntary/ community groups. These forums will provide an invaluable insight into patient experience including suggestions for innovation and improvements. Mystery Shopper /Patient Safety and Experience Walkarounds To ensure the business of the organisation is informed by the experience and views of people using our services, we will develop a programme of activities supporting Board Members and the Senior Management Team to take part in ‘walk and talk’ events with staff, patients and service users. PALS and Complaints Following the setting up of a dedicated complaints/ PALS function in CityCare from April 2011, there will be a new programme to integrate the outcomes and learning from complaints and PALS issues into the services. There will be more focus on capturing the issues that are raised in the health centres at reception desks on a routine basis that have not in the past been logged. There will be increased scrutiny of all complaints to identify links with incidents and vice-versa. There will be improved reporting to the Governance Committee and the Board with trend analysis and tracking of learning from complaints and PALS issues and the changes made to services as a result of this activity. Health at the heart of the city 39 Part 4 – What other people think of our Quality Accounts 4.1 COMMIS SIONING PRIMARY CARE TRUST – NHS NOT TINGHAM CITY NHS Nottinghamshire City monitors quality and performance at CityCare Partnership CIC throughout the year. The information contained within this quality account is consistent with information about CitiHealth NHS Nottingham supplied to commissioners throughout the year. 4.2 LOCAL INVOLVEMENT NETWORK (LINK) NottinghamCity LINk – response to CitiHealth Quality Account There are monthly quality and contract review meetings to review and monitor performance, governance arrangements and quality standards and there is frequent ongoing dialogue as issues arise. Nottingham City LINk welcome the opportunity to comment on the Quality Account for CitiHealth NHS Nottingham at its meeting on Wednesday 16th March 2011. We appreciate the level of information along with face to face meetings of the two organisations during the year and welcome the oppportunity to extend and build on the relationship with the new CityCare Partnership. CityCare Partnership works constructively with commissioners and other partners to develop integrated care pathways that improve the health of the local community. Quality goals and indicators are jointly agreed in order to reduce health inequalities and improve the health of Nottingham and Nottinghamshire residents. We congratulate CitiHealth on the work it has undertaken to ensure that, in this initial year of Quality Account production, a clear commitment to quality service delivery for the local community has been established. We welcome the clarity and format of the Quality Account which is comprehensive and easy to read. When significant incidents or complaints occur, robust investigations are carried out so that lessons are learned and improvements can be made. These are shared in a systematic way with staff and monitored appropriately. Complaints are treated seriously and genuine efforts are made to improve services in the light of patient feedback. In conclusion, Nottingham City LINk believes, based on its knowledge of CitiHealth, that the report is a fair reflection of the services provided and looks forward to the continuation of the relationship that has developed between our two organisations. CityCare Partnership has demonstrated a high level of commitment to improving clinical effectiveness with significant achievements against the high impact actions initiative and a commitment to enable patients / service users to feedback their experiences of services so that good practice can be continued or improvements made. Health at the heart of the city 40 4.3 NOT TINGHAM CITY COUNCIL HEALTH AND ADULT SOCIAL CARE SELECT COMMIT TEE COMMENT The Health and Adult Social Care Select Committee believes that the Quality Account 2010-11 is a fair reflection of the services provided by CitiHealth NHS Nottingham / Nottingham CityCare Partnership, based on the knowledge the Committee has of CitiHealth NHS Nottingham / Nottingham CityCare Partnership. The information contained in the Quality Account is presented in clear and accessible language. We welcome the ‘good’ Ofsted / Care Quality Commission rating for safeguarding and looked after children services and the clear evidence of partnership working. As a committee we have had a particular interest in ensuring that adults are also properly safeguarded and appreciate the introduction of a professional lead in this area and the fact that it will be a priority in 2011-12. We recognise the challenge in achieving the target to reduce cases of Clostridium Difficile and the organisation’s commitment to take action to lower the number of cases. Falls prevention has been an area of interest for the Council’s scrutiny councillors for several years while reducing the rate of falls has remained a challenge. It is a relief to see the rate beginning to reduce and the continuing commitment to finding ways to prevent falls in NHS provided care. The Committee has been kept well informed throughout the process of Transforming Community Services and has appreciated the opportunity to comment on proposals and plans. Scrutiny councillors were consulted through the Nottingham City and Nottinghamshire County Joint Health Scrutiny Committee on changes to improve maternity and newborn services. The Joint Committee will continue its interest in promoting normal birth as Nottingham University Hospitals NHS Trust (NUH) delivers midwifery services. We welcome closer working with NUH on discharge pathways. The Joint Health Scrutiny Committee carried out a review on dementia care in hospital in 2010-11 - discharge planning and the need for a close relationship between hospital and community provision was raised as a concern. In relation to the need to improve services to dementia patients and their carers, we are also pleased to see that it will be a priority to deliver dementia care training to all patient-facing staff and that there are plans to reduce inappropriate admissions to hospital and increase the number of people who are able to die in the place of their choice. We recognise the organisation’s commitment to engaging patients and the public and in responding to their views and experiences, but would hope that next year’s Quality Account more explicitly demonstrates the involvement of patients and the public in determining priorities and reflecting what quality means to them for the year ahead. We would also suggest that the use of case studies and / or quotes from patients and carers could make the document more accessible to the public. We welcome the developing relationship with Nottingham Emergency Medical Services (NEMS) and the City Council to provide high quality integrated and efficient services and look forward to developing our relationship with Nottingham CityCare Partnership in the coming year. Health at the heart of the city 41 Part 5 – Our commitment to you This first Annual Quality Account has featured a review of 2010/11 and a look forward to 2011/12. There has been a transformational change for the organisation from CitiHealth NHS Nottingham to the inception on 1 April 2011 of Nottingham CityCare Partnership CIC (Community Interest Company). As a brand new social enterprise with a workforce of more than 1,200 we are determined and committed to continually improving the quality of the care we provide. We are proud of our achievements but not complacent, as there are many challenges and improvements to be made in the coming year. CityCare is accountable first and foremost to the people it serves and as a social enterprise is enthusiastic about the investment that we will make back into our community. There is important work to be done in building relationships with our many stakeholders, a requirement to be cost effective, productive, and innovative and to focus on the prevention agenda, but safe and quality services are paramount and what patients demand and deserve. Nottingham CityCare Partnership CIC will respond to people by listening and acting. We look forward to your participation on this journey. We would like to thank all the stakeholders, patient and community groups who gave their feedback and suggestions for the content of this report, particularly the Local Authority Health and Adult Social Care Select Committee, the NHS Nottingham City Patient Experience Group, Nottingham LINk, the BECONN Service, Friends of Clifton Cornerstone and the Pakistan Community Centre. Thanks also to all the staff involved in producing this document. Health at the heart of the city 42 If you have any comment, questions or want to be involved with our next Quality Account, please call our Head of Patient and Public Engagement on 0115 883 9324. Nottingham CityCare CIC is registered as a company limited by guarantee Company Registration Number: 07548602 www.nottinghamcitycare.nhs.uk Health at the heart of the city 43