NHS Isle of Wight Provider Services Quality Account 2010/2011
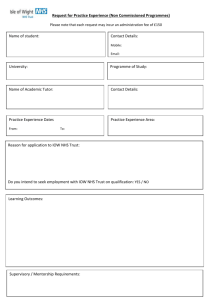
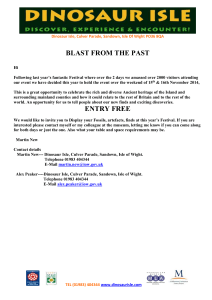
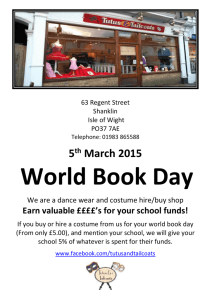
advertisement

NHS Isle of Wight Provider Services Quality Account 2010/2011 June 2011 Contents 1 2 2.1.1 2.1.2 2.1.3 2.1.4 2.1.5 2.1.6 2.1.7 2.1.8 2.2 2.2.1 2.2.2 2.2.3 2.2.4 2.2.5 2.2.6 2.2.7 2.2.8 3 3.1 3.1.1 3.1.2 3.1.3 3.1.4 3.1.5 3.1.6 3.1.7 3.1.8 3.1.9 3.1.10 3.1.11 3.2 3.3 3.4 Foreword Part 1: Chief Executive’s Statement on Quality Part 2: Priorities for Improvement for 2011/12 and Development of the Quality Account Priority 1: Identification and response to the deteriorating patient and hospital at night Priority 2: Prevention of Venous Thromboembolism Priority 3: Prevention of pressure ulceration Priority 4: Reduction in 28 day readmission rates in mental health Priority 5: Improving the pathway for clients with alcohol addiction Priority 6: Improving stroke care Priority 7: Community, outpatient and home antibiotic therapy Priority 8: Improving the experience of children and young people in psychiatric and emotional crisis Statements of assurance from the Board Review of services Dashboards and scorecards Patient safety walkrounds Participation in clinical audits Research Goals agreed with commissioners What others say about the provider Statements from the Care Quality Commission Safeguarding Children inspection and action plan HMP isle of Wight inspection Mortality Review Review of compliance - Sevenacres Review of compliance - White Lodge Data Quality Part 3: Review of Quality Performance 2010/11 Identification and response to the deteriorating patient Prevention and management of pressure ulceration Healthcare associated infections Ear Nose and Throat 24/7 on call service Health of the Nation Outcome Scales Patient Reported Outcome Measures Hospital mortality Getting it right in 2010/11 Reducing length of stay including enhanced recovery Complaints and compliments Workforce Statements provided by Commissioning PCT, LINks; OCS and patient Council Changes made to the final version of the Quality Account How to provide feedback on the account Appendix 1: Stakeholders engaged in the development of the NHS Isle of Wight Quality Account NHS Isle of Wight Quality Account 2 3 4 5 5 6 7 8 9 10 11 12 14 14 14 14 15 17 18 20 20 20 21 22 22 23 23 25 25 27 29 30 32 33 36 36 37 38 39 41 44 45 Foreword NHS Isle of Wight is an unusual Primary Care Trust in that it not only commissions but also provides most healthcare services for the people of the Isle of Wight. NHS Isle of Wight has a clear vision for what we should be like and this is set out below As an integrated organisation we: • Place great emphasis on integrated care delivery between physical and mental healthcare and between primary, community and acute care delivery • Focus on improving patient’s experiences of services as well as the outcome and safety of those services • Support people to take more responsibility for their health and healthcare and place greater emphasis on shared care • Increase availability of community based alternatives to hospital care, giving higher priority to keeping patients out of hospital • Increase the resources we deploy in community services relative to other sectors to enable an increasing focus in helping people to stay healthy • Deliver services as part of a strong clinical partnership with other provider organisations • Develop active case management • Focus on developing the role of clinicians as leaders – particularly by bringing improvements in quality, patient safety and delivering value as a means of improving all round performance • Use more technology, information and information systems to improve quality and productivity • Search harder for innovative solutions to deliver health care and seek to continuously improve • Mature further our capabilities to allow the greater creation of value driven partnerships with both public and commercial organisations The second Quality Account from NHS Isle of Wight includes details of the quality improvements made in 2010/11 and sets the direction for further improvements during the coming year. NHS Isle of Wight Quality Account 3 PART 1 1. Chief Executive’s Statement on Quality This is the second Quality Account published by NHS Isle of Wight and it outlines the successes and challenges of quality improvement within the services we provide at St Mary’s Hospital and across the services provided by an integrated healthcare service. NHS Isle of Wight is different from many other NHS organisations in that it is a PCT, that commissions and provides services for the residents of the Isle of Wight, and the provider services are unique in that they cover acute hospital services, mental health, ambulance, prison healthcare and community services. The Board of NHS Isle of Wight is committed to continuous quality improvement, the provision of high quality patient care, including high standards of patient safety, clinical effectiveness and patient experience. In developing this quality account we have taken account of what our patients have said to us, and we remain committed to driving up standards of patient safety, effectiveness and experience across all our services. During 2010/11 we have continued on our journey started in 2009/10 to strengthen clinical leadership across all sectors of the organisation. We have seen a number of significant achievements including a reduction in the number of patients having a cardiac arrest in the inpatient wards when compared to the previous year, a continued reduction in the number of patients developing clostridium difficile, reductions in the number of cancelled operations, with only 38 between October 2010 and March 2011 compared with 303 for the same period last year. The Chief Nurse has worked with Ward Sisters and Charge Nurses to enhance their understanding of accountability, responsibility and authority. The Chief Operating Officer, Medical Director and Chief Nurse are working with the Directorate leadership teams to ensure safe, high quality services are in place, providing strong clinical leadership to all areas. The last 12 months have been a time of significant change, with the new Coalition government creating a new direction for health services meaning that in the future NHS Isle of Wight can no longer commission and provide services and it has to plan to divest itself of its commissioning activities to GPs and a national board. With support from South Central Strategic Health Authority and the Department of Health, NHS Isle of Wight is undertaking an options appraisal process to determine a future organisational model for services on the Isle of Wight and to see if it can meet Foundation Trust criteria. The position will become clearer during 2011/12. This work has presented a significant opportunity to redesign services with clinicians and other stakeholders to drive up clinical standards even higher, whilst working hard to ensure that services are financially viable. The Quality Account has been developed in partnership with clinical staff from across NHS Isle of Wight, and has also included input from patient representatives; our Patients Council and Local Involvement Network members have contributed to the development of the priorities and provided feedback on our progress to date. I confirm that to the best of my knowledge the information contained within this 2010/11 Quality Account for NHS Isle of Wight is accurate. Kevin Flynn Chief Executive NHS Isle of Wight It is the policy of NHS Isle of Wight to take action to prevent fraud and this includes not including electronic signatures in documents. NHS Isle of Wight Quality Account 4 PART 2 2.1 Priorities for Improvement for 2011/12 and Development of the Quality Account The following priorities for improvement during 2011/12 have been set following discussion with a wide range of stakeholders. They include aspects from across the organisation to reflect the complexity of NHS Isle of Wight and include aspects of patient safety, patient experience and clinical effectiveness. Performance against all priorities will be reported to the Board within the monthly Quality Report. A wide range of stakeholder consultation has been undertaken prior to the development of the 2010/11 Quality Account, to support both the identification of priorities for 2011/12 and to ensure key elements of quality are included in the report. Service users have been invited to contribute to the decision-making process to agree the priority areas for improvement for 2011/12, which has included representatives from the Patient’s Council and LINks. Invitations to comment have also been posted on the organisation’s website. The priorities for the coming year were initially formulated into a long list of 21 areas; this was shared with the LINks, Patient Council, Directorate Forum and Service Delivery Executive Board, and published on the PCT website. Following consultation this list was revised and prioritised on the basis of the feedback to create the final eight priorities for 2011/12. Extensive staff consultation has taken place on the content of the quality account, both clinical and non clinical via the Directorate Forum; Service Delivery Executive Board and an invitation to contribute via the organisation’s staff e-bulletin. A dedicated group of staff have been involved in monthly Quality Account meetings, specifically designed to support the production process. This group consisted of the Chief Nurse; a senior representative from each of the Provider Directorates; a Business and Projects Manager; Provider Quality Manager and a Communications representative. A full list of those involved can be found in Appendix 1. PATIENT SAFETY 2.1.1 PRIORITY 1: IDENTIFICATION AND RESPONSE TO THE DETERIORATING PATIENT AND HOSPITAL AT NIGHT Identification and management of the deteriorating patient has been a priority for NHS Isle of Wight for a number of years, with a particular focus on the introduction of a Modified Early Warning System (MEWS) to identify early patients whose condition is starting to deteriorate to ensure appropriate action can be taken at the right time. However despite this action there is still in some instances a lack of compliance with the MEWS policy, which is demonstrated by avoidable admissions to the Intensive Care Unit and also inappropriate resuscitation attempts. This identified improvement priority is closely linked to the Hospital at Night programme and some areas of improvement will overlap, complement and support improvement in shared key performance indicators. The Hospital at Night / out of hours scheme came into being following implementation of the European Working Time Regulations (EWTR), and was initially piloted by four Trusts and supported by the NHS Modernisation Agency. It is a change programme that uses a multi-professional approach to delivering high quality standards of care. It typically involves changing the staff mix at night by developing a team of highly skilled advanced night nurse practitioners and reducing the reliance on Doctors in training. The scheme involves developing staff competencies to cover a wide range of interventions, but that has the capacity to call in specialist expertise when necessary. NHS Isle of Wight Quality Account 5 From a patient’s perspective, this means that the nearest available person with the appropriate skills will be diverted to treat the patient, rather than waiting for one specific person. In real terms, patients will be treated quicker. Hospital at Night will also apply to weekends / out of hours and can even apply to the emergency admissions side of the normal working day. It is essential that the system is properly followed. Hospital at Night advocates safer practice and supports safer training, whilst improving patient outcomes and quality of care. The effective and safe management of patients in hospitals during the out of hours period has emerged as a key challenge for NHS organisations in recent years. The Hospital at Night project sets out to improve response times to deteriorating patients by signposting the nearest appropriately skilled person to undertake any treatment needed. Monitoring and Measurement of Progress / Key Performance Indicators In order to measure performance, key performance indicators have been identified as follows: Measure Reduction of readmissions to the Intensive Care Unit Reduction of Inappropriate Admissions to Intensive Care Unit Reduction of unplanned admissions to Intensive Care Unit Reduction in cardiac arrests in adult acute wards Month on Month improvement in the compliance with the MEWS Policy No SIRIs relating to failure to rescue deteriorating patients Reduction in inappropriate bleeps to Junior Doctors Source of Data ICU admission data CCOS spread sheet data ICU admission data Frequency of Collection Data collected and Reported by Monthly Critical Care Outreach Lead Monthly Critical Care Outreach Lead Monthly Critical Care Outreach Lead Switchboard Monthly Productive Ward data set Risk Management PWG 1 Monthly Monthly Critical Care Outreach Lead Critical Care Outreach Lead Critical Care Outreach Lead 3 monthly PWG 1 Over the coming months, a bleep filtering system will be implemented to reduce the number of bleeps to junior Doctors. This will help signpost the nearest appropriately trained person to the patient by utilising the skills of Advanced Nurse Practitioners. 2.1.2 PRIORITY 2: PREVENTION OF VENOUS THROMBOEMBOLISM (VTE) Deep Vein Thrombosis and Pulmonary Embolism are the most common manifestations of venous thrombosis, collectively known as Venous Thromboembolism (VTE). VTE is known to be a significant cause of death in hospital patients and treatment of non-fatal symptomatic VTE and related long-term morbidities is associated with considerable cost to the health service. The House of Commons Health Committee reported in 2005 that an estimated 25,000 people die each year from preventable hospital-acquired VTE. Risks of thrombus formation increase with length of surgical procedures and increased periods of immobility. The first step in preventing death and disability in VTE is to identify those at risk so that appropriate treatments can be used. All providers of NHS funded acute hospital care must provide data on the use of the Department of Health recognised VTE Risk Assessment and the inclusion of appropriate treatment based on risk stratification. Since August 2010 we have undertaken a monthly audit of our compliance with the Department of Health goal of screening and treating 90% of appropriate NHS Isle of Wight Quality Account 6 patients. A number of mechanisms have been used to improve our compliance with this target which had to be met by the end of March 2011. This has included educational sessions for all hospital staff, direct approach, letter via email to consultants and junior doctors and ward managers and ongoing high level involvement in the programme by the Medical Director. During 2011/12 NHS Isle of Wight will continue to use the above mechanisms and any others we see fit to ensure that we consistently meet this target. It is anticipated that the roll out of e-prescribing will eventually provide feedback on the VTE status of every patient admitted. Whilst the 90% target was achieved by March 2011 it is recognised that it is still early days for the implementation of this requirement and the organisation needs to be confident that both assessment and treatment of patients is fully embedded within acute services for all appropriate patients, hence the decision to include this priority for 2011/12. Monitoring and Measurement of Progress / Key Performance Indicators Measure 90% of patients are assessed and treated in line with NICE guidance Source of Data Frequency of Collection Audit Monthly Data collected and Reported by Medical Director and Provider Quality Manager 2.1.3 PRIORITY 3: PREVENTION OF PRESSURE ULCERATION Pressure ulceration or bed sores are a significant cause of pain and distress to patients. NHS Isle of Wight has focussed on this priority for the last two years and this has been a focus of the Commissioning for Quality and Innovation Payment Framework (CQUIN) Indicators. The key indicators for the Provider that were adopted built on the previous years successes in this area. This included reducing the incidence of the most serious types of pressure ulcers. The Trust uses the European Pressure Ulcer Advisory Panel’s (EPUAP) grading system as required by the National Institute for Clinical Excellence, which grades pressure ulcers from 1 to 4. Whilst good progress has been achieved in approaching our targets for reducing pressure ulceration, there is still further work to do to reach a point where the organisation meets its commitment to a zero tolerance attitude for pressure ulcers. With the ratification and dissemination of the Pressure Ulcer Prevention and Management Policy, applicable to both hospital and community settings, it will become a key priority to audit the implementation of these standards against the NICE guidelines (CG29) for Pressure Ulcer Prevention and Management. These standards include: • • • Information on the timeliness of patient assessments, the quality of patient documentation. The provision of the appropriate pressure relieving equipment. Patients are receiving timely and appropriate interventions to ensure that the patient at risk of skin breakdown can expect to receive all the help that they need to avoid pressure ulceration, which may include help with nutrition, pain, continence, and mobility. Auditing of these key standards will demonstrate the impact that the policy is having on improving the quality of patient care in this area and will ensure that the organisation continues to aspire to avoiding these distressing and costly events. The audit findings will be fed back to ward sisters, district nursing team leaders, modern matrons and clinical leaders at all levels to further support the process of sustaining organisational change in this area. Intentional Rounding is one initiative which is starting to be adopted in the inpatient areas. This initiative is designed to ensure regular and timely checks and review of patients in ward areas to support patient safety and patient experience. In those areas in which Intentional rounding has already been implemented, there is already some evidence that these have improved patient experience and patient safety. It is a priority over the next year to support the roll out of this initiative to support effective and efficient delivery of safe, high quality clinical care. NHS Isle of Wight Quality Account 7 Monitoring and Measurement of Progress / Key Performance Indicators The key indicators for reduction in pressure ulceration that will continue to be adopted for 2011-12 will be: Measure A reduction in the number of hospitalacquired pressure ulcers of EPUAP grade 2 or above to below 2%. A reduction in the number of hospitalacquired pressure ulcers of EPUAP grade 3 or 4 to below 0.3%. Source of Data Frequency of Collection Data collected and Reported by Datix system Monthly Tissue Viability Nurse Datix system Monthly Tissue Viability Nurse CLINICAL EFFECTIVENESS 2.1.4 PRIORITY 4: REDUCTION IN 28 DAY READMISSION RATES IN MENTAL HEALTH Readmission rates within 28 days to in-patient services on the Isle of Wight are high in comparison to other Mental Health Trusts within the region and nationally. NHS Isle of Wight readmitted, within 28 days, 16.7% of Adults and 8.1% of Older Adults, discharged from hospital during the period April 2010 to March 2011. It is known that patients who have a higher number of previous admissions, who live alone or with family and who are discharged prematurely are at most risk of readmission. Readmission to hospital can have a huge negative impact on both the individual involved and their families/carers. Preventing readmission to hospital will lead to a more stable lifestyle for individuals. Key service based factors which can contribute to high readmission rates include high bed occupancy and high levels of patient turnover, shorter lengths of stay, lack of discharge planning and insufficient community follow up. During 2011/12 this priority will include a focus on whole systems bed management and discharge planning which will be centred on the needs of the service user. Strategies to prevent readmission will be a key part of care planning and will be considered throughout the admission. There are a number of work programmes that the Directorate is undertaking over this year which will have a direct impact on this priority. Implementation of the Productive Ward will release capacity of inpatient nursing staff to focus on direct patient care and the redesign of community services will improve the support available on discharge from hospital. Monitoring & Measuring of Progress / Key Performance Indicators Measure A reduction in the number of readmissions within 28 days during 2011/12, in comparison to 2010/11, baseline. Source of Data Frequency of Collection Data collected and Reported by PAS System Monthly Business and Performance Manager Admission & Discharge Records Quarterly Modern Matron Community Mental Health Service (2010/11 baseline = Adults16.7%, Older Adults 8.1%) Regular audit of readmissions reported to the Directorate Quality meeting and quarterly service review reporting to the Directorate Service Board. NHS Isle of Wight Quality Account 8 2.1.5 PRIORITY 5: IMPROVING THE PATHWAY FOR CLIENTS WITH ALCOHOL ADDICTION Whilst local Drug and Alcohol Services do provide a range of support and treatment services to people with alcohol addiction including supportive counselling and recovery based group work and community and home based detoxification including substitute prescribing services, a gap has been identified in the range of this service provision for the people with a severe alcohol addiction and associated mental health problems. Within NHS Isle of Wight there have never been any dedicated beds for people who require an admission to hospital for the safe provision of a detoxification programme. An audit of inpatient detoxification undertaken Sevenacres demonstrated that emergency detoxification provision had been ongoing, but this was not undertaken in a planned way and often resulted in unsuccessful detoxification. It also showed that only a small percentage of those receiving the service had been known to the Drug and Alcohol Services. Research shows that the chance of successful detoxification is significantly less if the individual being treated does not receive the appropriate preparatory and post detoxification support. Work has been undertaken between the Island Drug and Alcohol Services (IDAS) and Sevenacres in-patient services to identify a safe and reliable pathway for people requiring in-patient detoxification. It is now standard practice that individuals requiring in-patient detoxification at Sevenacres will be assessed and provided with motivationally based preparatory work prior to admission. The IDAS staff remain involved with the patient during their admission. When discharged IDAS and other partner service providers ensure the provision of follow-up to help maximise the chance for successful outcomes. To support this work a Dual Diagnosis Strategy and Pathway has been recently updated and ratified. Training plans are being developed to embed the principles of alcohol detoxification pathways into local practice. Monitoring and Measurement of Progress / Key Performance Indicators Measure Quarterly increase in the percentage of patients having undertaken preparatory counselling/therapy, completing detoxification and going on to start relapse prevention, as outlined below:- Quarter 1 – baseline Quarter 2 – 75% Quarter 3 – 80% Quarter 4 – 85% Audit of all patients on the pathway to show:1. % of individuals admitted for detoxification having undertaken preparatory work 2. % of individuals completing detoxification 3. % of individuals going on to start relapse therapy Source of Data Frequency of Collection Data collected and Reported by Admission & Discharge Records Quarterly Service Lead Inpatient Services Admission & Discharge Records Quarterly Service Lead Inpatient Services A CQUIN scheme has been created to support this development during 2011/12. NHS Isle of Wight Quality Account 9 2.1.6 PRIORITY 6: IMPROVING STROKE CARE In 2007, the Department of Health introduced the National Stroke Strategy, which includes 20 quality markers that are designed to provide excellent standards of care for stroke patients. In April 2010 a further 10 accelerated markers were introduced which needed to be fully implemented by April 2011. These markers are designed to improve the quality of services patients receive by addressing all aspects of the stroke care pathway; from emergency admission via Ambulance, prioritisation through CT scanning, direct admission to the Stroke Unit within 4 hours and provision of Thrombolysis (a drug that can be used in stroke patients that have suffered a clot). NHS Isle of Wight has recently been granted Hyper-Acute status, which means the necessary measures are in place to offer Thrombolysis to those patients that are eligible for the treatment. The Stroke Service is currently undertaking the necessary work to ensure high standards of clinical care are in place for this service through linking with a mainland hospital for additional support in the delivery of Thrombolysis to Island patients. Monitoring and Measurement of Progress / Key Performance Indicators The 10 accelerated stroke markers defined by the South Central Cardiovascular Network are: Source of Frequency of Data collected Measure Data Collection and Reported by Proportion of patients presenting with Stroke Data Stroke Services Atrial Fibrillation, presenting with Monthly Capture Form / stroke, that are anti-coagulated on Administrator Patient Notes discharge (60% by April 2011) Proportion of people with high risk TIA TIA Data Stroke Services Monthly that are fully investigated and treated Capture Form Administrator within 24 hours (60% by April 2011) Proportion of patients admitted directly Symphony / Stroke Services to an acute Stroke Unit within 4 hours Monthly Patient Notes Administrator of hospital arrival (90% by April 2011) Proportion of patients spending 90% of their inpatient stay on specialist Stroke Data Stroke Services Monthly Capture Form Administrator Stroke Unit (80% by April 2011 – vital sign) Proportion of stroke patients scanned Picture Stroke Services within one hour of hospital arrival Archiving Monthly Administrator (50% by April 2011) Communication System (PACS) Proportion of stroke patients scanned Picture Stroke Services within 24 hours of hospital arrival Archiving Monthly (100% by April 2011) Communication Administrator System (PACS) Proportion of patients supported by an Stroke Data Stroke Services Monthly Early Supported Discharge Team Capture Form Administrator (40% by April 2011) Proportion of patients and carers with joint care plans on discharge from Audit of Patient Stroke Services Monthly hospital to final place of residence Records Administrator (85% by April 2011) Proportion of patients that are Patient Stroke Services Monthly reviewed at 6 months after leaving Administration Administrator hospital (95% by April 2011) System (PAS) Proportion of patients who have received psychological support for Patient Stroke Services Administration mood, behaviour or cognitive Monthly Administrator disturbance by 6 months after stroke System (PAS) (40% by April 2011) NHS Isle of Wight Quality Account 10 These priorities are monitored and measured by the South Central Cardiovascular Network on a monthly basis. Progress within each of the markers is reported via the Stroke Steering Group, Chief Operating Officer’s meetings, Community Service Level Agreement and Trust Board. The Stroke Association have recently held a meeting with patients and members of staff to ensure patients are involved in planning stroke service care and priorities for the future. All in all, this is an exciting time for stroke services within NHS Isle of Wight where the key priorities are improving patient outcomes and quality of service. PATIENT EXPERIENCE 2.1.7 PRIORITY 7: COMMUNITY OUTPATIENT AND HOME ANTIBIOTIC THERAPY In June 2010, in response to key drivers such as the Trust’s Vision and Strategy document and the McKinsey Report (2009), which stated that up to 40% of patients may not need to be in hospital, it was agreed the need to explore the provision of an Out Patient and Hospital Parenteral Antibiotic Therapy (OHPAT) service for the Isle of Wight. This would provide patients with the therapy they required without having to be an in patient. So rather than having to be cared for in hospital for the duration of treatment, patients are visited daily by either the Community Nurses or the IV Nurse Specialist to administer the Intravenous (IV) antibiotics, or they attend an out-patients clinic daily. Patients remain under the care of the hospital Consultant and prior to their transfer into the community dates are established for weekly reviews (more frequent if needed). Community Nurses and/or the IV Nurse Specialist follow a set regimen that involves – administration of IV antibiotics; taking of blood samples; wound dressings if required and patient education, thus playing a part in maintaining patients in Primary care setting. Funding for a pilot scheme was agreed so that an OHPAT service could be set up and its potential evaluated. Patients that would normally be treated as in-patients with IV antibiotics and are suitable for the service are now able, under tight clinical governance, to be treated within their own homes or as out-patients. Thus promoting patient choice, and delivering care in an environment that provides: • • • • • • Ability to enjoy own food Ability to sleep in own bed Ability to be with family and friends Less feelings of confinement and loss of privacy Greater independence Ability to function more normally, even with the possibility of some work (or education) Extended length of stay in hospital alters the possibility of acquiring a healthcare acquired infection (HCAI). Through providing the OHPAT service we are able to reduce the number of days a patient would need to stay in hospital, therefore addressing the issue of increased bed pressures. OHPAT is establishing itself within NHS Isle of Wight as a service that provides: equivalent (or superior) care under a tight clinical governance framework at a fraction of the cost, whilst promoting patient choice and working in partnership with the District Nurses in primary care. NHS Isle of Wight Quality Account 11 By providing this service we plan to:• Reduce in number of days in hospital • Ease bed blockage pressures • Cost effective • Reduce waiting times • Enhancing multidisciplinary working across Primary and Secondary Care, providing seamless care • Reduce non-essential admissions • Reduction in risk of Hospital Acquired Infections Datasets have been established to record activity and the costs effectiveness of the service. Monitoring and Measurement of Progress / Key Performance Indicators Measure Improve Patient Experience Reduce the number of infections (Establish a baseline for the previous year. Monitor all line infections as part of the OHPAT Service during 2011/12) Training for further staff to insert midlines Source of Data Adapted Getting it Right Survey Reviewing the PVAD data Training records Frequency of Collection On discharge from OHPAT Service Data collected and Reported by IV Nurse Specialist Monthly IV Nurse Specialist Quarterly IV Nurse Specialist 2.1.8 PRIORITY 8: IMPROVING THE EXPERIENCE OF CHILDREN AND YOUNG PEOPLE PRESENTING IN PSYCHIATRIC AND EMOTIONAL CRISIS “Pushed into the Shadows” (Young Minds, 2007) was a disturbing way of describing the treatment of children and young people with mental health needs. Sir Albert Aynsley–Green the Commissioner for Children used this powerful analogy to recommend twenty changes to be made in the delivery of services for young people needing in–patient mental health services in his comprehensive review. Seven of these recommendations were direct to the Department of Health and sixteen were to Primary Care Trusts and Mental Health Trusts. Standard 9 of the National Service Framework for Children had an expectation that by 2006 all localities should have a clear plan in place that states how the range of users’ needs are to be met across the whole range of children’s mental health services. These changes required local policies to be developed and it is the way in which these directives have been interpreted and implemented that is relevant. Until April 2010 there was a working practice in place that enabled young people to be admitted onto the adult psychiatric ward for initial assessment and treatment. In certain cases, this admission could last for several weeks. This allowed for close family and social support but exposed young people to acute adult mental health patients in what could be considered a potentially abusive environment. The changes in the Mental Health Act 2007 section 31 ended this inappropriate admission of anyone under the age of 18 to an adult mental health ward, by ensuring that the rights of the individual to be accommodated, in hospital, in an age appropriate environment had to be considered and “appropriate” measures taken to address their needs in accordance with the Children Act (1989&2004), Human Rights Act (1998), the Mental Capacity Act (2005), Family Law Reform Act (1969) as well as the United Nations Convention on the Rights of the Child. The Act prescribes that young people should have appropriate physical facilities, staff with the right training, skills and knowledge to understand and address their specific needs, a routine that will allow for their personal, social and educational development to continue as normally as possible and equal access NHS Isle of Wight Quality Account 12 to educational opportunities as their peers, in so far as is consistent with their ability to make use of them, considering their mental state. Following these changes, a new policy regarding local admissions has been developed and arrangements for emergency admissions for young people have been commissioned with the Priory Hospital at Marchwood. Planned admissions to Leigh House (NHS Adolescent Hospital) at Winchester remain the primary placement choice if admission to the Children’s Ward at St Mary’s Hospital is not appropriate due to issues of risk and patient safety. By using these providers the inreach/outreach service in Specialist Child and Adolescent Mental Health Services, set up in January 2010, there is the opportunity to link closely with regular visits and intensive support to the young person and their family in order to prepare them for the admission if this is necessary and support them enabling a shorter admission and a closer working relationship on return home. The In-reach/Outreach Team are involved in all young people’s admissions to the Children’s Ward in cases where there are concerns about the emotional health and wellbeing of the child. This has enabled collaborative working practices to be developed in the management of complex issues for example in eating disorders and self harm, and has developed a programme for daily management in conjunction with Dieticians, Paediatricians and Nursing staff that follows national guidelines and enables family and friends to remain closely involved to support the young person. In partnership with the Paediatric Unit, a capital bid has been developed to improve the current adolescent inpatient area to facilitate an enhanced place of safety. Priorities to improve the monitoring and service developments that have been introduced are: • Regular reports to the quality meeting at the directorate service board and all exceptions to the admissions policy are subject to a case review. • A service review is being undertaken as part of the clinical doctorial psychology student’s placement that will provide a baseline for future service audits of the in-reach /outreach service. • Introducing CORC (Clinical Outcome Reporting Consortium) to monitor clinical effectiveness and outcomes in combination with Health of the National Outcome Scales Child and Adolescent (HONOSCA). • Involving service users in completing questionnaires recording their experience to improve service delivery. • Bi monthly paediatric meetings to develop closer working practices and pathways for patient care. • Following the workforce development programme completed in November closer liaison with key stakeholders in the development of Community Child and Adolescent Mental Health service by multidisciplinary co operative training and case management including the use of the Solihull Training Approach. • Patient safety was addressed by a comprehensive medication audit of young people on anti psychotic medication and a care pathway developed to improve patient care. • Development of the Care Programme Approach and Risk Assessments appropriate to the new service. Monitoring and Measurement of Progress / Key Performance Indicators Measure No children aged 16 or under will be admitted to an adult mental health ward Collection of baseline data for the number of children admitted to other places (including Mainland Specialist Mental Health Units/Children’s Ward) and data regarding the length of stay NHS Isle of Wight Quality Account Source of Data Exception Reporting Form / DATIX System CAMHS Patient Database 13 Frequency of Collection Data collected and Reported by Monthly Team Leader CAMHS Monthly Team Leader CAMHS 2.2 Statements of Assurance from the Board 2.2.1 Review of Services During 20010/11 NHS Isle of Wight provided and/or sub-contracted 81 NHS services. NHS Isle of Wight has reviewed all the data available to them on the quality of care in 61 of these NHS Services. The income generated by the NHS services reviewed in 2010/11 represents 65 per cent of the total income generated from the provision of NHS Services by NHS Isle of Wight for 2010/11. 2.2.2 Dashboards and Scorecards NHS Isle of Wight is currently in the process of developing its reporting capability and as part of this process a series of dashboards have been developed in order to report and assess various elements of performance. One of the early dashboards to be developed was the Clinical Quality Indicators dashboard. This has been made available to relevant staff throughout the organisation and reviews both current performance and trends in the following indicators of quality at directorate level: • • • • • • • Clinical Risk Audit Compliance Complaints / Good News Patient Claims Healthcare Acquired Infections Patient Falls Reported Incidents This, along with other dashboards, is used at the monthly directorate performance reviews as part of the overall performance management process. The aim is to highlight positive performance as well as areas for concern. This focus enables appropriate action to be taken to address performance issues with the aim of improving overall clinical quality. Going forward the Clinical Quality Dashboard can be developed to incorporate further indicators as appropriate one such example currently being developed is hospital mortality. 2.2.3 Patient Safety Walkrounds NHS Isle of Wight has undertaken a programme of Patient Safety Walkrounds throughout the year. Dr Allan Frankel, an Anaesthetist from Boston, USA, designed the idea of Patient Safety Walkrounds. The aim of the walk round process being to: 1. Increase the awareness of safety issues among all staff 2. Make safety a priority for senior leaders by spending a dedicated time promoting a safety culture 3. Educate staff about patient safety concepts such as incident reporting 4. Obtain and act on information gathered that identifies areas for improvement 5. Build communication and relationships with frontline staff. Over the course of 2010/11 a total of 54 walkrounds took place covering acute services including inpatient wards at St Mary’s Hospital, Mental Health and Learning Disabilities Services, Community Services, including District Nursing and Intermediate Care, the Ambulance Service and Prison Healthcare. These were attended by a team of two reviewers; an Executive Director and a Senior Medical Consultant or the Chief Nurse. NHS Isle of Wight Quality Account 14 The walkrounds focused on issues of patient safety, but were an opportunity for Senior Executives to visit front line areas to see services for themselves, and for staff to highlight both successes and challenges to the executives. Each walkround involved a tour of the area and a discussion with area staff and lasted around 60-90 minutes. The walkrounds were received well by areas and most reported that the walkrounds were useful. Actions were identified for most areas, these ranged from minor works that had been delayed (for example the fixing of large oxygen cylinder to the wall in respiratory department) to more substantial actions involving capital bids for building works (for example, the Physiotherapy Department). These actions were shared between area staff, and the executives themselves. A new programme of walkrounds that also covers areas previously not visited is in development. These will look at progress made against the actions of the previous year and identify any further issues that may require attention. 2.2.4 Participation in Clinical Audits During 2010/2011, 41 national clinical audits and 3 national confidential enquiries covered NHS services that NHS Isle of Wight provides. During that period NHS Isle of Wight participated in 95% national clinical audits and 100% national confidential enquiries of the national clinical audits and national confidential enquiries which it was eligible to participate in. The national clinical audits and national confidential enquiries that NHS Isle of Wight was eligible to participate in during 2010/11 are outlined in the table below: The national clinical audits and national confidential enquiries that NHS Isle of Wight participated in during 2010/11 are outlined in the table below: The national clinical audits and national confidential enquiries that NHS Isle of Wight participated in, and for which data collection was completed during 2010/11 are listed below alongside the number of cases submitted to each audit or enquiry as a percentage of the number of registered cases required by the terms of that audit or enquiry. Audit Participated Perinatal mortality (CEMACH) Neonatal intensive and special care (NNAP) Paediatric pneumonia (British Thoracic Society) Paediatric asthma (British Thoracic Society) Paediatric fever (College of Emergency Medicine) Childhood epilepsy (RCPH National Childhood Epilepsy Audit) Yes Yes Yes Yes Yes Yes Diabetes (RCPH National Paediatric Diabetes Audit) Emergency use of oxygen (British Thoracic Society) Adult community acquired pneumonia (British Thoracic Society) Yes Yes Yes Non invasive ventilation (NIV) - adults (British Thoracic Society) Yes Pleural procedures (British Thoracic Society) Cardiac arrest (National Cardiac Arrest Audit) Vital signs in majors (College of Emergency Medicine) Adult critical care (Case Mix Programme) (ICNARC) Potential donor audit (NHS Blood & Transplant) Yes Yes Yes Yes Yes Diabetes (National Adult Diabetes Audit) Heavy menstrual bleeding (RCOG National Audit of HMB) Yes Yes NHS Isle of Wight Quality Account 15 % cases submitted to Each audit All cases – ongoing All Cases – ongoing 100% 100% 100% Registration only during 2010/11 100% 100% All cases – data entry still open All cases- data entry still open 100% All cases ongoing 100% All Cases – ongoing 100% of deaths from ITU & A&E are recorded and submitted 100% 100% eligible cases Audit Participated Chronic pain (National Pain Audit) Ulcerative colitis & Crohn’s disease (National IBD Audit) Parkinson’s disease (National Parkinson’s Audit) COPD (British Thoracic Society/European Audit) Adult asthma (British Thoracic Society) Bronchiectasis (British Thoracic Society) Hip, knee and ankle replacements (National Joint Registry) Elective surgery (National PROMs Programme) Familial hypercholesterolaemia (National Clinical Audit of Mgt of FH) Acute Myocardial Infarction & other ACS (MINAP) Heart failure (Heart Failure Audit) Stroke care (National Sentinel Stroke Audit) Renal colic (College of Emergency Medicine) Lung cancer (National Lung Cancer Audit) Bowel cancer (National Bowel Cancer Audit Programme) Head & neck cancer (DAHNO) Hip fracture (National Hip Fracture Database) Severe trauma (Trauma Audit & Research Network) Falls and non-hip fractures (National Falls & Bone Health Audit) Prescribing in mental health services (POMH) National Audit of Schizophrenia (NAS) Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Depression & anxiety (National Audit of Psychological Therapies O neg blood use (National Comparative Audit of Blood Transfusion) Platelet use (National Comparative Audit of Blood Transfusion NCEPOD Study – Surgery in Children’s Study No Yes Yes Yes NCEPOD Study – Perioperative Care Study Yes NCEPOD Study – Cardiac Arrest Procedures Yes National confidential Inquiry into Suicide and Homicide (NCISH) Yes invited Ongoing data collection % cases submitted to Each audit Ongoing 100% 100% All cases 100% 100% 100% - All cases 90.10% 100% All cases - ongoing All cases ongoing 100% 100% All cases – ongoing All cases – ongoing All cases – ongoing 100% - All cases All cases ongoing All cases ongoing 100% - ongoing Data collection to start in 2011 *see note below 100% 100% Data collection underway – current estimated response 100% (1 case only applicable) Data collection underway – current estimated response rate 54% Data collection underway – current estimated response rate 100% 100% *The one national audit not participated in was National Audit of Psychological Therapies (Depression & Anxiety) The Mental Health & Learning Disabilities Directorate declined to participate in the National Audit of Psych Therapies after careful consideration. The Directorate Management Team felt that the audit was poorly designed, with ill-defined criteria for therapy which meant that meaningful benchmarking would be impossible. The Directorate Management Team met with the National Team leading this audit, and urged them adopt more appropriate clearer definitions NCEPOD have released finalised data following the studies undertaken during 2009/10 which were reported in last years Quality Account. Our response rate varied from what was previously published for the following two studies: • Parenteral Nutrition – published response rate 48% actual response rate 83% • Surgery in the Elderly – published response rate 70% actual response rate 64% The reports of 14 national clinical audits were reviewed by the provider in 2010/11 and NHS Isle of Wight intends to take the following actions to improve the quality of healthcare provided: • Risk assess every inpatient on admission for Venous Thromboembolism • Develop clear protocols for the post operative management of elderly patients • Ensure robust monitoring of patients prescribed lithium NHS Isle of Wight Quality Account 16 The reports of 27 local clinical audits were reviewed by the provider in 2010/11 and NHS Isle of Wight intends to take the following actions to improve the quality of healthcare provided: • Increase awareness of end of life care • Revision of hand held maternity notes • Ensure that all patients discharged from ICU to a general ward area have a fully documented Multidisciplinary discharge summary • Ensure that service users with substance misuse problems are given care plans that are focussed on psychosocial interventions in order to emphasise rehabilitation. Clinical Audit Prize The annual competition for the Clinical Audit Prize is open to all staff who have undertaken an audit within the NHS Isle of Wight during the previous financial year. The shortlisted finalists present their audit project to an invited audience, which includes senior staff from across the organisation who judge the projects based on the structure and outcome of the audit project. In June 2010, the second year of the competition, the winner was Dr Banu Rudran for her audit of Acute Kidney Injury, which was based on the recommendations from the National Confidential Enquiry into Patient Outcome and Death (NCEPOD) report - 'Adding Insult to Injury' published in 2009. 2.2.5 Research Participation in Clinical Research The number of patients receiving NHS services provided or sub-contracted by NHS Isle of Wight in 2010/11 that were recruited during that period to participate in portfolio research (e.g. studies within the NIHR Clinical Research Network Portfolio) approved by an NHS Research Ethics Committee was 1138, compared to 954 in the previous year. These studies were conducted in the following specialties: Cancer, Cardiovascular, Diabetes, Mental Health, Musculoskeletal, Neurology, Inflammatory and Immune, Injuries and Accidents, Primary Care and Reproductive Health, and Childbirth. The Trust approved 68 new studies (portfolio and non-portfolio) during the year, compared with 52 during 2009-10, which together with the 60 ongoing projects from 2009-10, continues to represent a healthy research portfolio for the Island. Research Management & Governance Performance Metrics and Measures Research Activity 2010/11 Number of externally funded studies NIHR portfolio 43* Number of externally funded studies Non portfolio 17 Number of commercial studies 1(*portfolio) Number of “Own Account” studies 8 Number and proportion of studies where Trust has acted as Sponsor 1 (1.5%) Number and proportion of types of studies: Clinical Trials of Investigational Medicinal Product 7 Clinical Trials of medical devices 0 Other Clinical trials 20 Human Tissue studies 5 Questionnaire studies 25 Qualitative studies 5 Service Evaluation 6 2009/10 35 6 7 4 3 (6%) 13 1 13 3 16 3 3 Resources Number of research support posts (employed by the Trust whose main purpose is research support and who help people do research at any stage of the R&D lifecycle): 2010/11: 2.2 WTE NHS Isle of Wight Quality Account 17 Number of Research Nurses/Allied Health Professionals/Clinical support posts: 2010/11: 3.65 WTE Number of staff involved in research in each band: 8.5 PAs Consultant 2.8 WTE Band 6 Research Nurse 0.25 WTE Band 7 Research Nurse 0.6 WTE Band 8 Research Nurse/Manager 0.6 WTE Band 6 Pharmacy Technician 0.2 WTE Band 7 Pharmacist 0.2 WTE Band 6 Biomedical Scientist (Pathology) 0.1 WTE Band 8 MLSO (Pathology) 0.2 WTE Band 5 Radiographer 0.92 WTE Band 3 non clinical delivery staff 1.0 WTE Band 4 non clinical delivery staff 0.3 WTE Band 5 non clinical delivery staff Funding Increase in NIHR support funding: 2010/11: £526,756 (72.9% increase) 2009/10: £304,612 Patient recruitment Number of patients recruited to participate in portfolio research approved by a NHS Research Ethics Committee: 2010/11: 1138 (19% increase) 2009/10: 954 2.2.6 Goals Agreed with Commissioners A proportion of NHS Isle of Wight’s income in 2010/11 was conditional on achieving quality improvement and innovation goals agreed between NHS Isle of Wight and any person or body they entered into a contract, agreement or arrangement with for the provision of NHS services, through the Commissioning for Quality and Innovation payment framework (CQUIN). Monthly Clinical Quality Review meetings are held with the Commissioners to monitor progress with both CQUINs and quality schedules within each contract as outlined below. Further details of the agreed goals for 2010/11and for the following 12 month period are outlined below and available electronically at:http://www.institute.nhs.uk/commissioning/pct_portal/cquin_schemes_11%1012.html Ambulance 2010/11 CQUIN Indicator Non conveyance where the ambulance service have actively been involved in giving advice only, or implementing an alternative pathway of care The service actively engages with service users to get feedback on performance and patient experience Prisons 2010/11 CQUIN Indicator All prison health performance and quality indicators will achieve AMBER or better on or before December 2010 20% = 7 prison health performance and quality indicators, which are Amber or red at April 2010, will achieve GREEN on or before December 2010 NHS Isle of Wight Quality Account 18 Achievement Achieved CQUIN Payment £46 797 Achieved £ 23 398 Achievement 97% achieved CQUIN Payment £27 498 97% achieved £13 749 Acute 2010/11 CQUIN Indicator Reduce avoidable death, disability and chronic ill health from Venous-thromboembolism (VTE) Improve responsiveness to personal needs of patients Improve the outcomes and experiences of patients in hospital with by implementing care bundles for Heart Failure, Acute Myocardial Infarction, Community Acquired Pneumonia, Hip and Knee surgery in line with the Advancing Quality methodology A demonstrable reduction in the number of patients with preventable pressure ulcers by 2012. A year on year reduction in newly acquired pressure ulcers of no less than 25% against the baseline. Staff training for end of life. Systems to identify patients requiring end of life care Raise awareness of dementia in acute hospital and primary care Fully completed discharge summaries as per Schedule 2 resulting in improved primary care clinical confidence and patient safety. Mental Health 2010/11 CQUIN Indicator Using patient experience to directly influence service provision All patients to have access to drug and alcohol assessment on admission to mental health unit as appropriate to Drugs and Alcohol National Occupational Standards (DANOS). All organisations providing services for CYP age 11 – 19 should demonstrate adherence to You’re Welcome quality standards and work towards achieving quality criteria. Community 2010/11 CQUIN Indicator The Provider to set up systems and processes for staff training/ development for End of Life care Provider to set up systems and processes for identifying patients who are dying and identifying the needs of patients that are dying Implementing training re: caring for people with dementia Implementing training re: caring for people with learning disabilities COPD patients with a personalised care plan Heart Failure patients with a personalised care plan Stroke patients with a personalised care plan Drawing up and implementing action plan following annual patient survey Achievement 50% achieved 50% achieved Not achieved due to factors beyond control of the Provider. Provider has participated in a pilot scheme to improve implementation across SC SHA CQUIN Payment £52 412 £52 411 £139 764 50% achieved £52 411 12.5% achieved £26 206 Achieved Not achieved £209 644 £0 Achievement CQUIN Payment £92 784 £92 784 Achieved Achieved Achieved £92 784 Achievement 50% achieved CQUIN Payment £11 219 50% achieved £11 219 50% achieved £11 219 Not achieved Achieved £89 757 50% achieved £22 439 An outline of the agreed goals for 2011/12 is detailed below:Ambulance CQUIN Scheme 2011/12 No. Description of goal 1. To achieve a defined set of national targets 2. Admission avoidance –See and Treat by Paramedics and ECPs 3. Patient experience – personal needs Prison CQUIN Scheme 2011/12 No. Description of goal 1. To achieve a defined national target 2. Prison Health Performance and Quality Indicators (PHPQIs) 3. Patient experience - Personal needs NHS Isle of Wight Quality Account 19 4. Improved outcomes against the Quality Outcomes Framework (QOF) Acute CQUIN Scheme 2011/12 No. Description of goal 1. Reduce avoidable death, disability and chronic ill health from Venous-thromboembolism (VTE) 2. Improve responsiveness to personal needs of patients 3. To achieve a defined set of national targets 4. Admission avoidance - Establish the Unscheduled Care Hub as a well used conduit for clinical/patient information to identify appropriate clinical interventions/services for patients as an alternative to hospital admission. 5. To improve end of life care for patients cared for in the acute setting 6. To improve health by ensuring that all in-patients over 16 years who smoke, are identified and provided with a brief intervention and support on quitting and to develop an action plan to extend to other lifestyle choices Mental Health & Learning Disability CQUIN Scheme 2011/12 No. Description of goal 1. Involving carers of service users and measuring carer satisfaction 2. Alcohol strategy: integrated alcohol pathway and inpatient detox 3. Review the use of Antipsychotic Drugs in Dementia 4. Transition from Specialist CAMHS Model to Community CAMHS Model of Service. Community CQUIN Scheme 2011/12 No. Description of goal 1. To achieve a defined set of national targets 2. Admission Avoidance through a reduction in falls 3. Improved rehabilitation outcomes through the configuration of rehabilitation services 4. Analysis of health needs of children, young people and their families 5. Improved Case Management of NHS Funded Care clients 2.2.7 What Others Say about the Provider Statements from the CQC NHS Isle of Wight is required to register with the Care Quality Commission (CQC) and its current registration status is registered with no compliance conditions. The Care Quality Commission has not taken enforcement action against NHS Isle of Wight as of 31 March 2011. NHS Isle of Wight has participated in special reviews or investigations by the Care Quality Commission relating to the following areas during 2010/11 - Safeguarding Children; Inspection of HMP Isle of Wight, the Stroke Mortality Review, Reviews of Compliance in Sevenacres and White Lodge. NHS Isle of Wight intends to take the following action to address the conclusions or requirements reported by the CQC, as outlined below. NHS Isle of Wight has made the following progress by 31st March 2011 in taking such action as outlined below. Safeguarding Children Inspection and Action Plan During Sept 2010 NHS IOW underwent a two week Care Quality Commission (CQC) inspection looking at the contribution of health services to safeguarding and the care of Looked after Children. This was in conjunction with our local authority colleagues who were inspected by Ofsted during the same two weeks in order to form a joint evaluation on the care of vulnerable children on the IOW. NHS Isle of Wight Quality Account 20 Several areas of good practice by health were identified by the inspector including our joint working with Children’s Centres and other partners, the effective use of the Common Assessment Framework (Caf) by Midwives and Health Visitors, the provision of safeguarding training to core staff as well as a sound system for tracking vulnerable children who attend the Accident and Emergency Department. All the statutory safeguarding professionals were in place and aware of their specific roles and responsibilities in relation to keeping children safe. The overall joint assessment by Ofsted and the CQC judged services on the IOW as “adequate” with NHS Isle of Wight meeting all its statutory responsibilities for safeguarding children. An action plan was developed to address the recommendations made. This included: • • • • Improvement to the Children & Adolescent Mental Health Services (CAMHS) which is being well progressed through the Community CAMHS implementation plan. More robust monitoring of the quality of health care provided to Looked after Children. This is now being overseen by the newly appointed Children in Care Nurse and reported to the Corporate Parenting Board. Commissioning monitoring to evidence the adherence with safeguarding procedures and training for all independent contractors. Wider consultation with children & young people to inform the planning and development of health services. This is being developed during 2011 /12. Progress against this action plan will continue to be monitored by the Chief Nurse and the CQC. HMP Isle of Wight Inspection Under an agreement with the Care Quality Commission, an inspection of HMP Isle of Wight was undertaken in October 2010 by Her Majesty's Inspectorate of Prisons also covered the healthcare services NHS Isle of Wight provides to prisoners. The inspection was welcomed, as it provided an opportunity to highlight the many improvements that have been made to our services since previous inspections. It also enabled us to share with the inspecting team those areas where we felt further work is still required to bring the care we provide to prisoners up to a standard equivalent to that provided to the wider Island community. There is still a way to go with developments in Primary Care Services for prisoners and, with the inspecting team's experiences from other prisons, they were able to provide some helpful guidance on how approaches may be implemented locally, that have been found to be successful elsewhere. In their report, the inspectors made a total of 34 recommendations and 16 “housekeeping points" relating to our services. Work was already underway on a number of these areas at the time of the inspection and has since been completed, with a further number against which significant progress has already been made. A total of 140 recommendations had been made following previous inspections that we have been actively working on since 2008. Acknowledging that improvement work needs to continue, we can be encouraged by the significantly smaller number of recommendations made on this occasion. In addition to identifying areas where further work is required, the inspectors also highlighted areas of development and good practice that included: • • • The new Prison Inpatient Healthcare Unit which was reported as being “light and clean and a considerable improvement on the previous facility on the Parkhurst site” A Nurse led support group for prisoners with cancer and other life threatening conditions The Nurse Prescriber role in specialist mental healthcare. A more detailed action plan is currently being developed that will underpin our work on the recommendations with our Prison Service partners over the coming months. NHS Isle of Wight Quality Account 21 Mortality Review The Acute Cerebrovascular Disease (stroke) Mortality review related to patients admitted during November and December 2009 and the report was sent to the CQC in July 2010. In September 2010 the CQC advised that they did not feel that they needed to undertake further action at the time. However, the regional CQC contacts would be in touch regarding the implementation of our Stroke Improvement action plan and with particular respect to the training of consultants in the delivery of thrombolysis. Since that time the following actions have been taken: • • • • • Relevant Consultants undertook a full day’s training in the delivery of thrombolysis on 1st October 2010, delivered by Professor Kwan from the Royal Bournemouth Hospital. Consultants and Nurses are currently undergoing National Institute of Health Stroke Scale (NIHSS) training. Consultants are currently undertaking Stroke Training and Awareness Resources (STARS) Training. Arrangements have been made for Consultants to spend time in the Hyper Acute Unit in Portsmouth, to gain first hand experience of Thrombolysing patients (between 3-5 days). Senior Staff Nurses on the Stroke Unit have spent a day in the Hyper Acute Unit in Portsmouth. Review of Compliance – Sevenacres During March 2011, Sevenacres, the Inpatient Mental Health Unit underwent an unannounced inspection from the Care Quality Commission. During this inspection they found that the unit was not meeting one or more of the essential standards and that improvement was needed. The report is due for publication by the Care Quality Commission during May 2011 and this Quality Account will be updated for final publication if there are any changes. There were three areas that the Care Quality Commission felt NHS Isle of Wight was not compliant with the essential standards and that compliance actions were required: 1. Outcome 4: care and welfare of people who use services – the CQC were concerned that the quality of care planning documentation varied, that not all physical health needs were fully assessed and that care plans did not include sufficient detail on how these needs should be met. They were concerned that there was no formal care file auditing programme in place. Finally they were concerned that it was not clear whether patients had been involved in decisions about their care treatment and support. 2. Outcome 11: safety, availability and suitability of equipment. They were concerned that cleaning products on a cleaner’s trolley were not kept secure at all times. 3. Outcome 16: assessing and monitoring the quality of service provision. Despite having a range of quality monitoring processes in place they felt that these did not necessarily capture the risks or improvements needed at Sevenacres. There were three further areas where NHS Isle of Wight was compliant with the essential standards, however actions for improvement were suggested: 1. Outcome 7: safeguarding people who use services from abuse. The CQC confirmed suitable arrangements are in place and most staff have received the necessary training, however some staff still needed training 2. Outcome 13: staffing. The CQC were concerned that there seemed to be an over-reliance on good will of staff to cover absences. 3. Outcome 14: Supporting workers. The CQC commented on the good induction and training processes in place but felt NHS Isle of Wight must ensure all staff complete the necessary training. The Management Team for Sevenacres has already put in place an action plan to address these issues. NHS Isle of Wight Quality Account 22 Review of Compliance – White Lodge During March 2011, White Lodge, who provide inpatient services for people with learning disabilities, underwent an unannounced inspection from the Care Quality Commission. During this inspection they found that the unit was meeting all the 16 essential standards, but to maintain this they suggested some minor improvements are made. The report is due for publication by the Care Quality Commission during May 2011, and this Quality Account will be updated for final publication if there are any changes. The three improvements the Care Quality Commission suggested are: 1. Outcome 9: management of medicines. They felt that some records did not clearly show that people had received all medication as prescribed. 2. Outcome 13: staffing. They felt there were some occasions when there not sufficient staff on duty to enable people to do every thing they wanted to do. 3. Outcome 17: complaints. Information on how to complain was not readily available for all visitors. The Management Team for White Lodge has already put in place an action plan to address these issues 2.2.8 Data Quality i) Statement on relevance of Data Quality and actions to improve data quality NHS Isle of Wight will be taking the following actions to improve data quality High quality information is a vital asset, both in terms of the clinical management of individual patients and the efficient management of services and resources. It plays a key part in clinical governance, service planning, performance and business management that all help to demonstrate the quality of the services we provide. Therefore the Trust views Data Quality as an essential element of delivering high quality health care service. Whilst some elements of our data quality are extremely high work to monitor and improve data quality is ongoing in order to drive continual improvement. Some of the actions that we have been working on include: The development of a Data Quality Dash Board - this is being developed to focus on specific elements of data quality that have been identified for improvement. This will be integrated within the Executive dashboard which will provide the necessary focus to deliver stepped improvement in these areas of concern. The Trust is subject to a series of Audits that cover elements of data quality (both internal and external undertaken to review various business processes - Payments by Results, Clinical Coding, Information Governance) where these have highlighted either poor data quality or risks to data quality recommended remedial actions will be implemented. Nationally poor data quality has been recognised as a risk to the commissioning process. Commissioners are therefore using the Service Level Agreements as leverage to influence providers to improve data quality with the introduction of a new Data Quality schedule. Within the Operating Framework 2011/12 it outlines an expectation that commissioners will use contract sanctions if they are not satisfied about the completeness and quality of a provider's data. ii) NHS Number and General Medical Practice Code Validity NHS Isle of Wight submitted records during 2010/11 to the Secondary Uses Service for inclusion in the Hospital Episode Statistics which are included in the latest published data. The percentage of records in the published data: NHS Isle of Wight Quality Account 23 - which included the patient’s valid NHS number was: 97.8% for admitted patient care; 99.3% for out patient care; and 97.1% for accident and emergency care.” - which included the patient’s valid General Medical Practice Code was: 100% for admitted patient care; 100% for out patient care; and 100% for accident and emergency care.” iii) Information Governance Toolkit Attainment Levels NHS Isle of Wight’s Information Governance Assessment Report overall score for 2010/11 was 66% and was graded Pink. An action plan is in place to address the shortfalls and includes improving written confirmation of systems and processes in place from Information Technology, establishing the role of the Information Asset Administrator and rolling out the national information governance e-learning programme to all staff. iv) Clinical Coding Error Rate NHS Isle of Wight was subject to a Payment by Results clinical coding audit during the reporting period by the Audit Commission and the error rates reported in the latest published audit for that period for diagnoses and treatment coding (clinical coding) are outlined below: • • The attendance error rate (that is the appointments with errors which had a financial impact) has reduced to 0.7 per cent which is a significant improvement over the 2009/10 results and the Trust should be commended for this. This equates to only one attendance error in the sample of 150 cases Data quality arrangements were found to be adequate in the four areas assessed, including policies and procedures, which were assesses as below minimum requirements in 2009/10. NHS Isle of Wight Quality Account 24 PART 3 3.1 Review of Quality Performance 2010/11 has been a year of significant achievements for the whole organisation including attaining NHS Litigation Authority level 1 accreditation and excellent results in the annual PEAT assessment process. NHS Isle of Wight was successful in achieving Level 1 accreditation against the NHS Litigation Authority risk management standards following the recent external assessment in February 2011. NHS Isle of Wight was set a target of achieving 56 of a possible 69 points in order to pass the assessment (80% pass rate) and actually achieved 67 of the 69 available points; this represents the best result NHS Isle of Wight has ever achieved for this important external review. The assessment included all of our acute, primary care, ambulance and mental health and learning disabilities services. The assessors were particularly complimentary about the quality of our policy documentation generally. The annual Patient Environment Action Team (PEAT) inspection results published in July 2010 at St Mary’s Hospital resulted in excellent scores for Food and Environment and good for Privacy and Dignity, with White Lodge achieving excellent in all three areas. An external assessor, a NonExecutive Director and patient representatives were part of the inspection team to support the independent approach to this process. The success from both of these assessments has been shared with the Board of NHS Isle of Wight within public board meetings. The successes and challenges of the 2010/11 quality account priorities are outlined below and demonstrate the ongoing commitment of NHS Isle of Wight to driving up quality of patient services. PATIENT SAFETY 3.1.1 IDENTIFICATION AND RESPONSE TO THE DETERIORATING PATIENT Identification and management of the deteriorating patient has been a priority for NHS Isle of Wight for a number of years. The main focus has been on the introduction of a Modified Early Warning System (MEWS) to identify patients whose condition is starting to deteriorate early to ensure appropriate action can be taken at the right time. However despite this action there is still, in some instances, a lack of compliance with the MEWS policy, demonstrated by avoidable admissions to the Intensive Care Unit. Actions taken in the Last Year: 1. A Critical Care Outreach Service (CCOS) was established in April 2010 as a nurse led service that has been developed from within the existing budget for the Intensive Care Unit. The service was initially provided between 08:30hrs and 16:30hrs Monday to Friday. It is an adjunct for the general ward based teams to support them in caring for patients who are critically ill or have potential to develop such an Illness and/or the potential for their condition to deteriorate. The Critical Care Outreach Service is there to support, educate and empower ward based teams and not to take over or take responsibility away from the ward based teams for their patients. After a service evaluation of the Outreach Service which was presented to the Service Delivery Executive Board in October 2010, it was agreed to support the full implementation of the service. The service is now provided 7 days a week, from 08:30 to 19:00hrs. 2. Introduced annual mandatory training sessions for acute staff on the track and trigger system called MEWS. 3. Monthly Ward based audits for the compliance against the MEWS policy. NHS Isle of Wight Quality Account 25 4. Introduction of a defined care pathway for all deteriorating adult patients in the hospital setting. 5. Introduction of a clear tracking tool of deteriorating and at risk patients which is shared with the out of hour’s team to ensure effective management of these patients, assign the correct resources and ensure the patient is placed in the correct care environment. 6. Introduction and use of a standard communication tool called SBAR to standardise the communication of deteriorating patient needs between healthcare professionals. 7. Continued delivery of multidisciplinary education to support the identification and response to the deteriorating patient. This includes the ALERT course and a full range of resuscitation training courses. 8. Reviewed and updated the Intensive Care Unit (ICU) discharge documentation to ensure safe and effective discharge of patients from ICU to the general wards. Performance against Key Performance Indicators: The chosen indicators to demonstrate improvement were decided upon from local decision making and based on recommended measurements from the National Patient Safety Agency work stream on deterioration. These included the following measures: 1. No Serious incidents requiring investigation (SIRI) relating to the non recognition and response to the sick patient -. In 2009/10 there were 6 Serious Incidents relating to failure to rescue deteriorating patient, since the introduction of CCOS there has been a reduction in the number with 4 Serious Incidents in 2010/11; one of these was in a non acute clinical area and since that time additional training has been provided to staff in that area. 2. Reduced Unplanned admissions – The number of unplanned admissions to ICU from inpatient ward areas has reduced and those patients that have experienced an unplanned admission have had lower MEWS scores compared to patients admitted prior to the introduction of the critical care outreach service. During 2010/11 there were 161 unplanned admissions to ICU compared with 172 in 2009/10 Reduce Unplanned Adm issions to Intensive care from Wards 25 20 15 Pre CCOS (2009/10) 10 Post CCOS (2010/11) 5 h M ar c Au gu st Se pt em be r O ct ob er N ov em be r D ec em be r Ja nu ar y Fe br ua ry Ju ly Ju ne M ay Ap ri l 0 3. Reduced readmissions to the Intensive Care Unit – Since the introduction of the Critical Care Outreach Service the number of readmissions to ICU has remained the same. When unplanned admissions did occur this was correlated to the Outreach Service not being available. There were 12 readmissions to ICU in 2010/11 compared to 12 readmissions in 2009/10 NHS Isle of Wight Quality Account 26 4. Reduction in the number of cardiac arrests – Since the introduction of the Critical Care Outreach Service there has been a 44% reduction in cardiac arrests in the in patient areas. The chart below shows a comparison of the total number of cardiac arrests prior to the introduction of CCOS (2009/10) and after the introduction of CCOS (2010/11). There has been a significant reduction in the number of cardiac arrests in the in-patient wards, 124 in 2009/10 compared to 70 in 2010/11, since the introduction of the Critical Care Outreach Service. In-patient Ward Cardiac Arrests 16 14 12 10 Pre CCOS (2009/10) 8 Post CCOS (2010/11) 6 4 2 Au gu st Se pt em be r O ct ob er N ov em be r D ec em be r Ja nu ar y Fe br ua ry M ar ch Ju ly Ju ne M ay Ap ril 0 Next Steps: The identification and response to the deteriorating patient remains as a key area for improvement for NHS Isle of Wight for 2011-2012, in order to build on the current success to ensure all the correct measures are in place to build on the success of 2010/11. Patient Story My husband was in Intensive Care for 3 months and almost died several times in that period. I was so scared when he left Intensive Care to go to a general ward; we were so used to one-one nursing and being closely monitored. When I heard about the outreach team, I was so reassured that my husband would be ok with their support on the ward and a close eye kept on him. I was also told that I could ask the ward nurse to bleep the outreach nurse if I was concerned about my husbands condition at all, that made me feel safe and in control of his next steps to recovery. Wife of a patient who was in ICU for 91 days and was followed up by the Critical Care Outreach Service 3.1.2 PREVENTION AND MANAGEMENT OF PRESSURE ULCERATION Over the last year, NHS Isle of Wight has continued with its commitment to reducing pressure ulcers, building on the progress made over the last two years. The key patient safety measures in this area have been: • Reducing pressure ulceration of European Pressure Ulcer Advisory Panel (EPUAP) grade 2 or above to below 2% • Reducing ulceration of EPUAP grades 3 and 4 to below 0.3%. These indicators were part of the CQUINs payment scheme for the trust, which promotes improvements in clinical quality by also providing financial incentives to the provider for achievement of the schemes highlighted. Figure 1 demonstrates the progress that has been made towards achieving the reduction of pressure ulcers of grade 2 or above to below 2%. NHS Isle of Wight Quality Account 27 Figure 1: Percentage of Newly Acquired Pressure Ulceration of EPUAP grades 2 to 4, month on month in the inpatient areas (target indicated in red) 4.00% 3.66% 3.50% 2.74% 3.00% 2.50% 2.98% 2.66% 2.21% 2.06% 2.00% 2.10% 1.50% 1.88% 1.55% 1.00% 1.41% 0.98% 0.50% 0.91% 0.00% Apr10 May- Jun- Jul-10 Aug- Sep10 10 10 10 Oct10 Nov10 Dec10 Jan11 Feb11 Mar11 As figure 1 shows the overall trend is downward towards achieving the target set at the start of 2010-11. It is only over the last month the incidence has dropped below the target, and this is not yet consistent; hence the importance of continuing to focus on this area as a key indicator of quality. Figure 2 demonstrates the progress that has been made to reducing the number of EPUAP grade 3 and 4 pressure ulcers to below 0.3%. Figure 1: Percentage of Newly Acquired Pressure Ulceration of EPUAP grades 2 to 4, month on month in the inpatient areas (target indicated in red) 4.00% 3.66% 3.50% 2.50% 2.98% 2.74% 3.00% 2.66% 2.21% 2.06% 2.00% 2.10% 1.50% 1.88% 1.55% 1.00% 1.41% 0.98% 0.50% 0.91% 0.00% Apr10 May- Jun- Jul-10 Aug- Sep10 10 10 10 Oct10 Nov10 Dec10 Jan11 Feb11 Mar11 Figure 2 similarly shows a downward trend in the development of the more serious types of pressure ulceration. This trend has not however approached the target set by the CQUINs scheme at the start of the year and so also remains as a priority for 2011/12. A number of initiatives have contributed to this reduction, including: • • • Ongoing work to ensure that patients are offered the most appropriate pressure relieving mattress and/or cushion in a timely manner Raising awareness of the key messages of the Pressure Ulcer Prevention and Management Policy recently ratified and adopted by the Trust. Introduction of Intentional Rounding, which is intended to be further embedded in practice over the next year. NHS Isle of Wight Quality Account 28 3.1.3 HEALTHCARE ASSOCIATED INFECTIONS (HCAI) During 2010/11 NHS Isle of Wight has continued to see improvements in the prevention and management of healthcare associated infections both in the acute hospital and in primary care settings, working with general practitioners to reduce the incidence of Clostridium difficile. Throughout the year performance has been reported to the PCT Board on a monthly basis via the performance report and this will continue via the new Provider Board during 2011/12. Meticillin Resistant Staphylococcus Aureus (MRSA) During 2010/11 NHS Isle of Wight has continued its focus on reducing the incidence of healthcare associated infections towards zero in line with the national direction. This has included the introduction of MRSA screening for all emergency patients, building on the work in 2009/10 to ensure all elective patients were screened. Now all patients meeting the national criteria for screening prior to or on admission to St Mary’s Hospital are appropriately screened. During 2010/11 NHS Isle of Wight saw a slight increase in the number of patients who developed MRSA bacteraemia whilst in hospital on the Island to 4, during 2009/10 there were 2 cases. Work is ongoing to drive these numbers as low as possible including enhanced blood culture collection training for doctors and nurses, as mentioned full MRSA screening for all patients meeting the national criteria, maintaining high standards of hand hygiene and ensuring best practice in peripheral venous access device management (a cannula or needle entering a vein to provide fluid or medication). There have been no cases of MRSA bacteraemia developing in a patient in the care of St Mary’s Hospital since October 2010. Cumulative Number of MRSA Bacteraemia Cases Developed in the care of St Mary's Hospital, NHS Isle of Wight (3 year comparison) 5 Number of cases 4 3 2008/09 2009/10 2010/11 2 1 March February January December November October September August July June May April 0 Clostridium difficile 2010/11 saw NHS Isle of Wight report 22 cases of Clostridium difficile infection, 2 less cases than in 2009/10. The number of cases saw a small jump on June/July when a localised outbreak of Clostridium difficile was connected to one of the medical wards, which was quickly brought under control. The numbers of Clostridium difficile infection occurring within inpatients remained low again during the winter months and ensuring the numbers of this significant healthcare associated infection continue to reduce further remains a key priority for NHS Isle of Wight. The following graph outlines progress made in tackling this infection over the last three years. NHS Isle of Wight Quality Account 29 Cummulative numbers of Clostridium difficile cases developed in the care of St Mary's Hospital, NHS Isle of Wight (3 year comparison) 50 45 40 35 30 2008/09 2009/10 2010/11 25 20 15 10 5 March February January December November October September August July June May April 0 Data Discrepancy in Performance Reporting – Clostridium difficile In preparing the information for the Quality Account it became apparent that there is a slight discrepancy in the data contained within the monthly NHS Isle of Wight performance report in terms of the number of Clostridium difficile cases attributed to Provider Services within NHS Isle of Wight. The final performance report indicates 24 cases attributed to Provider Services whereas the actual figure is 22. It is believed this discrepancy has occurred due to timing of the data extraction from the Health Protection Agency (HPA) website and the confirmation of allocation of cases based on whether these cases are hospital or community acquired. There is a slight delay from sign off by the organisation to when the data is verified by the HPA and if the performance report data is extracted too early, cases may not be correctly apportioned. This occurred during 2010/11 with one case in June and a further case in September. The records on the HPA website have been checked and confirmed that this is the case. To prevent this happening in future, data will be extracted from the HPA website as late as possible to ensure the correct information is available and a retrospective check of the previous month’s data will also be undertaken and updates made as necessary. CLINICAL EFFECTIVENESS 3.1.4 EAR NOSE AND THROAT 24/7 ON CALL SERVICE From 1st April 2010 the Ear Nose and Throat Department has provided a 24 hour 7 day a week on call service to Island patients. The previous emergency service had only been provided locally from 9.00 am Monday to 5.00 pm Friday, with transfer of telephone on call and emergency services to Portsmouth Hospitals outside these hours The current investment in ENT Services was as a result of an external review commissioned by NHS Isle of Wight Commissioners and carried out by a representative from the Royal College of ENT surgeons and a GP; this review took place in early 2009 and recommended that NHS Isle of Wight should provide a 24 hours a day, 7 days a week secondary care on call service and therefore to enable this to take place the review recommend the recruitment of three full time consultants. NHS Isle of Wight Quality Account 30 Three full time consultants with special interests in Head and Neck Cancer, Rhinology, Otology were appointed and commenced in post in April 2010. Measure of Quality The following quality measures for 2010/11 were identified: 1. To reduce the number of emergency admissions to Portsmouth Hospitals Trust for patients with ENT Conditions • Emergency admissions to Portsmouth Hospitals were 27 in 2008/09 and 30 in 2009/10. • The number of emergency admissions to Portsmouth Hospitals should fall by a minimum of 75% to a maximum of 7 patients. • Emergency admissions to St Mary’s Hospitals IoW were 47 2009/10. This number will increase to 57 due to repatriation from Portsmouth Hospitals. • The total number of emergency ENT admissions will reduce from 77 -64 a fall of 17%. 2. To reduce the number of emergency ENT patients travelling to the mainland for their treatment • Emergency admissions for complex head and neck cancer may continue to be referred to Portsmouth Hospitals, for intermediate/ urgent radiotherapy. This number should not exceed 7 patients per annum. • Emergency outpatients will no longer have to travel to Portsmouth for out of hours care, thus the number of such patients should reduce to zero. Performance against Key Performance Indicators: For the period April 2010 to February 2011, the number of Isle of Wight ENT emergency admissions to Portsmouth Hospitals Trust has reduced significantly to just three patients. This is in comparison to 27 and 30 admissions in the previous two years. The quality measure for NHS Isle of Wight emergency admissions to Portsmouth Hospital Trust was set at no more than 7 patients, therefore this quality measure has been achieved and exceeded the required performance. For the same period there have been 135 emergency admissions to St Mary’s Hospital and as expected the admissions St Mary’s Hospital have increased as a result of this investment in service provision. The 135 emergency admissions is greater than expected, however this is a positive as it has been discovered that the previous year’s data did not include those patients with an ENT condition who were admitted in an emergency under the management of other specialities for example General Surgery. The improved ENT service has therefore provided more specialist and focussed care to such patients from the time of admission. There were no emergency admissions to Portsmouth Hospitals Trust for patients with complex head and neck cancer; this was against a measure of no more than 7 patients. NHS Isle of Wight is not aware of any patients who have had to travel to Portsmouth Hospitals Trust for emergency outpatient treatment. This has not been required as the organisation offers a 24 hours a day, seven day a week ENT on call service. Conclusion The 24 hour a day 7 day a week ENT on call service has been a success. This is demonstrated by the achievement (and overachievement) of the quality measures set in last years Quality Account. As a result of this success NHS Isle of Wight does not intend to continue to monitor performance as it is satisfied that the current arrangements will continue to provide a quality service to the Island. NHS Isle of Wight Quality Account 31 3.1.5 HEALTH OF THE NATION OUTCOME SCALES (HoNOS) – MENTAL HEALTH The Royal College of Psychiatrists Research Unit developed the Health of the Nation Outcome Scales and these have been in use in Mental Health Teams for some years. The Royal College originally developed HoNOS as a means of recording progress towards the Health of the Nation target ‘to improve significantly the health and social functioning of mentally ill people’. HoNOS consists of 12 categories measuring behaviour, impairment, symptoms and social functioning. When a patient is referred to the service their HoNOS score is recorded and measured periodically afterwards. This can help with identifying the progress an individual is making towards recovery and help improve their treatment. The use of HoNOS is recommended by the National Service Framework for Mental Health and by the working group to the Department of Health on outcome indicators for severe mental illnesses. The Mental Health and Learning Disabilities Directorate planned a consistent and organised role out to implement HoNOS across most of its services. Completing assessments at the start of treatment, then at regular intervals, will help in ensuring that we measure the health and social functioning of mental health patients and any improvement in symptoms. It will then be used to identify the most appropriate care pathway for the individual service user, with further assessment and adjustment of care plans as required. Performance against Key Performance Indicators: Training staff to use the HoNOS tool began in November 2009 and by June 2010 all 14 of the identified teams were using the appropriate HoNOS tool for their patient group. The Directorate acknowledged that the HoNOS data should be held at individual patient level within an electronic record. This would enable easy comparison of scores to show progress towards recovery. Discussions with staff from the Systems Support Department within the organisation identified that the current Patient Administration System (PAS) could be developed to capture the required data. The PAS system was already in use across all in-patient services and plans were put in place to roll-out the system to the community services during September and October. However, to enable the collection and reporting of HoNOS data in the statutory Mental Health Minimum Data Set submission an interim system was put in place to collect all of the scores for each patient at each assessment. The data screens were developed within PAS but unfortunately during testing a problem was encountered. The Systems Support Manager worked with the software supplier to identify a solution and a software update is expected in April 2011 to resolve the issue. However, the planned rollout of PAS to the teams has continued and all community teams were live on the system from February 2011. This means that as soon as the new software has been customised and tested locally to capture the HoNOS data staff will be able to begin capturing and comparing scores at patient level. The data will be used to compare the effectiveness of treatment by individual, teams and clinicians. The data will also assist with acuity studies, support discharge from services and as a performance management tool, i.e. if a patient has no improvement then the clinician needs to review treatment plan. Work will be undertaken during 2011/12 to ensure the HoNOS assessment has embedded into practice across the teams. Senior clinical staff will participate in a working group to review the quality and outcomes of HoNOS assessments to ensure consistency and good practice. Further support and training will be offered to staff as necessary. NHS Isle of Wight Quality Account 32 Alongside this data quality and completeness will be continually monitored to fulfill our statutory reporting obligations. This will also provide good quality information to support individual clinicians and teams in ensuring appropriate interventions are in place for the patient. Monitoring of performance will continue via the Mental Health and Learning Disabilities Directorate Board meeting. HoNOS Assessments 2010 - 2011 800 600 400 200 0 Ap ril M ay Ju ne Ju Au ly Se gu pt st em b O er ct o No be ve r De mb ce e r m b Ja e r nu Fe a ry br ua ry M ar ch Total Number of HoNOS Assessments Completed 3.1.6 PATIENT REPORTED OUTCOME MEASURES (PROMS) In May 2009 patient related outcome measures (PROMS) were implemented within NHS Isle of Wight to measure the clinical effectiveness of specific operative procedures. This included hip surgery, knee surgery and groin hernia repairs. The Pre Assessment Unit is responsible for ensuring patients complete the questionnaires at their pre assessment attendance at the hospital. These are collected by courier to be processed at the National Administration Centre. Since last years quality report outlining the PROMs the post operative questionnaires have been collated from the 3rd and 6th month follow up returns sent direct by the National Administration Centre. Performance against Key Performance Indicators The national comparisons provided in this report are based on eligible episodes with an episode start date between 1st April 2009 and 30th April 2009 and submitted to the National Administration Centre by 23rd June 2009. With both pairs of questionnaires matched, the resulting comparative data can be used for analysis. The data analysed in this report is based on the EQ-5D descriptive system, which comprises of the following five dimensions describing the patient’s general health: • • • • • Mobility Self care (washing and dressing) Usual activities (work, study, housework, family or leisure) Pain/discomfort Anxiety/Depression Each level has three levels: No problems, some problems, or severe problems. The following graphs demonstrate a comparison with national benchmarking for hernias, hips and knees. NHS Isle of Wight Quality Account 33 Groin Hernia: Groin Hernia score comparison 100% 90% 80% 70% 60% 49% 50% 45% 40% 30% 26% 30% 27% 24% 20% 10% 0% Felt better following surgery Felt the same following surgery National Felt worse following surgery Isle of Wight NHS PCT NHS Isle of Wight, scores slightly better than the national average in relation to a positive response post surgery, indicating that 49% of NHS Isle of Wight patients are reporting good outcomes post surgery. Hip Replacement Surgery: Hip Replacement score comparison 100% 90% 80% 70% 60% 50% 40% 30% 20% 85% 82% 12% 6% 10% 0% Felt better following surgery 5% Felt the same following surgery 9% Felt worse following surgery National Isle of Wight NHS PCT NHS Isle of Wight, scores slightly better than the national average in relation to a positive response post surgery, indicating that 85% of NHS Isle of Wight patients are reporting good outcomes post surgery. NHS Isle of Wight Quality Account 34 Knee Replacement Surgery: Knee Replacement score comparison 100% 90% 80% 74% 76% 70% 60% 50% 40% 30% 17% 20% 8% 10% 16% 8% 0% Felt better follow ing surgery Felt the same follow ing surgery National Felt w orse follow ing surgery Isle of Wight NHS PCT NHS Isle of Wight is comparable to the national average in relation to a positive response post surgery, indicating that 76% of NHS Isle of Wight patients are reporting good outcomes post surgery. Overall across all surgical procedures 74% of NHS Isle of Wight patients have reported a better health score post procedure against the national averages. Overall health score comparison 100% 90% 80% 71% 74% 70% 60% 50% 40% 30% 18% 20% 11% 10% 16% 10% 0% Felt better following surgery Felt the same following surgery National Felt worse following surgery Isle of Wight NHS PCT PROMS will continue to be monitored by clinical staff working in the relevant speciality to ensure outcomes continue to be achieved; ongoing performance will also be monitored via the monthly performance report to the Provider Board, so it is felt this does not need to be included in the Quality Account priorities for 2011/12.. NHS Isle of Wight Quality Account 35 3.1.7 HOSPITAL MORTALITY Following a disappointing increase in our Hospital Standardised Mortality Ratio (HSMR) a number of initiatives have been undertaken to improve both our data capture and quality monitoring of in hospital death. With respect to data gathering this was felt to be important as the Trust received feedback to suggest that the change in the position of our HSMR was largely due to insufficient data being submitted by the Trust to adequately code co-morbidities. From the end of 2010 and continuing into 2011 all hospital cases of mortality are now coded from the notes. This has resulted in the number of coded co-morbidities increasing by approximately 50% consistently since this time. As annual HSMRs are published on a financial year end basis, we will not be able to detect a significant effect on mortality this year. However feedback from Dr Foster does suggest a reduced alert level in the last quarter of the year, due to improved coding. We have also undertaken two audits as part of a regional programme looking at 50 consecutive deaths every six months, these audits have shown that patients are not dying due to poor standards of care. Information from this has been used to improve a number of aspects of care including the use of the Liverpool Care Pathway, the use of the Do Not Attempt Cardio-Pulmonary Resuscitation (DNACPR) form and quality in note keeping. This is an ongoing process which allows us to benchmark the type of problems we have with those of other hospitals in our region. The results suggest that all hospitals have similar issues and through a series of regional meetings we hope to develop new strategies to address these. PATIENT EXPERIENCE 3.1.8 GETTING IT RIGHT IN 2010/11 NHS Isle of Wight has been undertaking the Getting it Right Survey in inpatient areas since April 2010. The Survey consisting of seven key questions has been given to all patients at the time of their discharge from inpatient areas. The surveys are collected on a weekly basis to ensure that the Organisation is collecting real time data. From November 2010 the Getting it Right survey was extended to Outpatient areas. These areas give out the survey to all outpatients one day a week on a rolling basis. Results are fed back to these areas on a regular basis. As with the inpatient survey, the key measure was to receive positive feedback from 95% of patients surveyed. Monitoring and Measurement of Progress: During 2010 / 2011 the Getting it Right survey had one key measure which was to receive positive feedback from 95% of patients surveyed on their experience of our services with at least 50% inpatients surveyed. Whilst the organisation achieved positive feedback from 96% of inpatients surveyed, the organisation only managed to survey 24% of discharged patients. Since November 2010, 1216 surveys have been returned from Outpatient Areas. This has shown that overall 97% of patients are either very satisfied (78%) or satisfied (19%). The data from the surveys has been presented to the board on a monthly basis as part of the quality report presented by the Chief Nurse and Director of Infection Prevention Control. The Getting it Right Survey is being revised for 2011/12, focusing on areas for improvement identified from National Patient Surveys and will continue to be reported on monthly to the Board via the Quality Report NHS Isle of Wight Quality Account 36 3.1.9 REDUCING LENGTH OF STAY INCLUDING ENHANCED RECOVERY Reducing hospital admissions and caring for people more appropriately outside of hospital remains a key priority to reduce the risks associated with hospital admissions. When hospital care is needed, the NHS needs to minimise the time spent in hospital whilst not undermining patient safety or quality of care. A protracted length of stay in hospital increases the risk of: • Infection • Loss of independence / confidence • Frustration • Depression • NHS resources being used inappropriately To address this over the past year, the organisation has implemented two quality improvement schemes: • Enhanced recovery • Reduction in overall length of stay Enhanced recovery Enhanced recovery involves developing a pathway of personal care that minimises stress for patients by harmonising the whole care pathway to ensure that patients are fully informed of what to expect. The patients are informed of their expected length of stay from the first point of contact with their GP, throughout the pathway that eventually leads to follow on care. The same message is continually reiterated throughout the pathway of care, and clinicians engage in a ‘contract of care’ with patients that empowers them to take control of their recovery. Over the past year, the general surgical wards have undertaken this and it is in the process of being implemented in Orthopaedics. Once these are fully established, the system will be rolled out across the emergency pathway. Early results indicate that there has been a reduced length of stay in colorectal patients from 10 days to 5 days, and gynaecology patients’ length of stay has reduced from 5 days to 2 days. Reduction in overall length of stay Patients are admitted to hospital 24 hours a day, 7 days a week, 365 days a year. It is therefore vital to keep patient flow moving in readiness for potential admissions. To help achieve this, acute wards over the past year have been tasked with discharging 5 patients per day; with the longer stay wards required to discharge one patient per day. To monitor performance against this, each ward has been flagged as red, amber or green; red meaning failing to achieve their target, amber is almost there and green is achieving or exceeding expectations. Currently there are 7 wards that are achieving or exceeding their targets and 5 are amber. There are now a significant number of discharges and these have particularly improved on Saturdays. Sunday remains the day where more work is needed. A recent pilot scheme was introduced for a 2 month trial period using Discharge Facilitators, to assist in speeding up discharges. During the two months that they were operational, the following improvements were noted: Average weekly discharge rate before team in place Average weekly discharge rate now Stroke Unit 3.375 6 Rehab Unit 2 5.4 17.125 23.6 8.5 16.2 CCU Newchurch NHS Isle of Wight Quality Account 37 A significant amount of work has been undertaken to improve discharge processes, including the introduction of Patient Status at a Glance boards on the wards. These help identify those patients that could potentially be discharged so that work can be focussed on getting them home in a timely manner. A new Community Stroke Rehabilitation Team has been introduced, that takes patients out into their own homes much earlier. The team then works with the patient and teaches them to adapt to their own surroundings rather than the false environment of a hospital ward, and they can visit patients up to 5 times a day in the early stages if necessary. The impact of winter pressures in relation to elective bed capacity has been proactively managed this year with 6 cancellations taking place during the month of December compared with 101 cancellations taking place during the same month in the previous year. Total aggregate performance for winter period (October - March) is 38 cancellations compared to previous YTD position of 303 cancellations. Also being monitored is the percentage of emergency readmissions within 14 days. This year to date, we are currently running at 3.27% emergency readmissions against a performance target of less than 4.66%. The percentage of emergency readmissions within 28 days is 5.10%, against a target of less than 6.41%. This clearly demonstrates that NHS Isle of Wight is performing well in these areas. Although this has not been included as a priority for 2011/12 due to the significant amount of work undertaken during 2010/11, ongoing monitoring of performance in relation to enhanced recovery and reducing length of stay will continue to be monitored via the relevant clinical directorate boards; Elective Services and Medicine, Emergency and Diagnostic Services 3.1.10 COMPLAINTS AND COMPLIMENTS During 2010/11 the reporting of complaints data has been part of the Chief Nurse’s Quality Report to Board, as well as reported at various other committees as part of performance reports. The main areas of concern raised in complaints include: • • • • Clinical care – concerns about diagnosis / treatment Nursing care – quality of basic nursing care provided Staff attitude – which relates to the attitude or conduct of staff from all areas of the organization Communication – failure to communicate/lack of information provided All complaints within NHS Isle of Wight are investigated and reviewed directly with staff involved, with lessons learnt developed and shared with the wider clinical area. The following positive outcomes and actions have been identified following the review of a selection of complaints in order to prevent similar situations happening again: • • • • • • • Use of electronic request forms in diagnostic imaging being reviewed, to improve communication to support diagnosis and treatment of patients. Importance of individualised patient care being led by Matrons and Ward Sisters. Two hourly comfort checks have been implemented on wards. Improvement of the information given to patients relating to catheter care. Systems developed to identify and reduce the number of bed moves for patients. Introduction of a discharge checklist to ensure efficient discharge of patients. Clearer emphasis included in patient information leaflet, to highlight the need for patients to take pain relief prior to attendance for outpatient procedures. The numbers of compliments about NHS Isle of Wight services continue to exceed complaints with on average 11 compliments for every one formal complaint received. One of the Non-Executive Directors provides an assurance process to the Board by regularly meeting with the Quality team to review complaints and monitor progress. NHS Isle of Wight Quality Account 38 3.1.11 WORKFORCE Health and Wellbeing NHS Isle of Wight has developed a Health and Wellbeing group with Multidisciplinary representation. The group has produced a Health and Wellbeing strategy and in year action plan supported by the Quality, Innovation, Productivity and Prevention (QIPP) and System Transformation Team. The group has carried out research into lifestyle and health attitudes in key departments within the organisation. The group has close links with Occupational Health and Public Health and has focussed on: • • • • • • Exercise Healthy Eating Alcohol Smoking Health MOT’s Psychological Wellbeing Reducing Sickness Absence NHS Isle of Wight has committed to a 1% reduction in overall sickness absence in 2010/11 with challenging targets for future years. Currently the organisation monitors long term sickness absence on a case by case basis in association with Occupational Health, Human Resources and Directorates. The focus is on rehabilitation back to work but where no progress is likely, ill health, retirement or the capability policy are also options. The organisation also closely monitors short-term sickness absence and has a six month triage project ongoing which focuses on a number of key areas of high absence within the Trust. The triage will offer supportive contact with individuals within 24 hours of an ill health episode commencing. The project will complete on 31 March 2011 and be reviewed based on outcomes for continuation. Most absence is monitored through the e-Rostering system to ensure accuracy and Key Performance Indicator data reported to the Board on a monthly basis. Through membership of ‘NHS Benchmarking’, the organisation also produces value for money data in this and a range of other corporate functions. NHS Isle of Wight is also reviewing “Fast-track” process for staff awaiting treatment. Staff Engagement Through its Communication Strategy the organisation regularly uses a variety of media to keep staff engaged. These range from group meetings with the Chief Executive, monthly ‘Executive Briefing’ meetings with Budget Managers and the Executive Team, regular E-Bulletins and co-ordinated ‘Team Briefing’ arrangements after each Board Meeting. Staff currently ‘at risk’ of change are also offered regular workshops and one to one meetings to supplement the above. NHS Isle of Wight is committed to working in partnership with representative organisations and has a monthly ‘Staff Partnership Forum’ and a bi-monthly ‘Joint Local Negotiating Committee’ to relate to non-medical and medical and dental organisations respectively. These forums consider the QIPP plan as a standing item. Workforce Planning Strategy NHS Isle of Wight has produced a 5 year workforce plan which is an integral part of the QIPP plan. Currently this shows the requirement for workforce reductions year on year. The proposals are based on cost improvements through skill mix, management cost reductions, vacancy and variable hours control and a recurrent Mutually Agreed Resignation Scheme (MARS). NHS Isle of Wight Quality Account 39 The reductions are slightly offset by cost pressure funding and a limited number of Commissioning Investment initiatives to support prioritised clinical outcomes in Health Visiting, End of Life, Stroke Care, Prescribing, Autism and Development Support for the GP Commissioning Consortium. In addition to the above, a variety of ‘Back Office Efficiency and Management Optimisation’ schemes are underway:• • • • A comprehensive review of corporate functions and the production of costed Service Level Agreements The 100% rollout of the E-Rostering system. The simplification and standardisation of policies and procedures (E-CRB, E-Expenses) The review of shared models with the Isle of Wight Council and Mainland NHS Trust partners. Workforce data is monitored through the workforce plan, weekly and monthly key performance indicator monitoring, the integration of data with the Performance Management structure and regular reports to the System Reform Board and the QIPP Programme Board. The alignment of Workforce data with activity and finance data is closely monitored at the QIPP Programme Board and a written Workforce Planning process and policy is currently in progress. A five year Medical Workforce Strategy is close to completion. Leadership, Education and Training In partnership with South Central Strategic Health Authority and local providers in the education sector NHS Isle of Wight maintains a comprehensive education and training strategy for all staff. Increasingly reliance is placed on effective and streamlined mandatory training, the use of elearning and a clearer link between development and productivity through Training Needs Analysis, cascaded and monitored through comprehensive Appraisal Policy. The organisation is trying to streamline the administration of training using E-Technology, effective partnerships with other organisations and clearer alignment with activity and organisational vision. It is also exploring the investment to achieve the Organisational Development to support its 5 year IT strategy. Medical Revalidation NHS Isle of Wight is a pilot site for Medical Revalidation and is making good progress with the framework, monitored by an Executive-led Revalidation Project Group. The Trust has invested in My-Job Plan software to enhance Job Planning and the review of Programmed and Special Programmed activities. All of the above is clearly aligned to the emerging Medical Workforce Strategy. Workforce and Productivity Through close alignment with Activity and Finance, the organisation monitors all productivity schemes through the QIPP Programme Board. A key project is the Option Appraisal of Provider Services. This project along with other key skill mix issues throughout the organisation will enhance the existing Workforce Plan, particularly in 2011/2012. Structural changes within Public Health, Commissioning and Back Office Functions will be both supported and maintained in close partnership with the emerging PCT Clusters, Commissioning Support Units, Local Authorities and the GP Commissioning Consortium. The existing Organisational Change Policy and support programme for staff will be adapted to the requirements of Local and National initiatives, as the details become known. The organisation will maintain its local networks, its networking with SHIP (Southampton, Hampshire, Isle of Wight and Portsmouth) partners and other NHS and Local Authority organisations in the South Central Area. NHS Isle of Wight will explore all forms of Pay and Terms and Conditions flexibility to support Transition and Sustainability in partnership with staff organisations. In association with Bevan Brittan, Zenon Consulting and Allocate, the organisation is currently considering a diagnostics and support proposal around existing and future QIPP schemes, for implementation in 2011/2012. NHS Isle of Wight Quality Account 40 3.2 Statements provided by Commissioning PCT, LINks and OSCs Statement from NHS Isle of Wight Commissioners Isle of Wight NHS PCT Commissioners welcomed the opportunity to participate in the governance ‘sign-off’ process and provide a statement in response to the presented Quality Account. The Quality Account was widely shared with Senior Commissioners and a representative of the GP Commissioning Consortia (GPCC) for their comments. ‘Commissioners acknowledge the provider’s unique position and the challenge it faces in representing the broad range of services provided - Acute, Mental Health and Learning Disability, Community and Ambulance Services - within a single Quality Account. In response, the provider has identified a range of quality improvement priorities, associated with Patient Safety, Clinical Effectiveness and Patient Experience, for the coming year that build upon previous priorities and address new areas for improvement, reflecting both local and national priorities and the interests of the Commissioners. To ensure future engagement with the emerging Clinical Commissioning Consortia, the Provider is asked to share its proposed priorities for 2012/13 with the Consortia for feedback, before they are signed off and written into the draft report next year. This is on the understanding that Commissioners can only influence and not dictate content. The Provider has demonstrated quality improvement in the priorities it set out in last year’s Quality Account and, as previously mentioned, has chosen to continue to drive up quality in some of these areas in the coming year. Also identified are CQUINS (Commissioning for Quality and Innovation Schemes); targets for quality improvement mutually agreed between the Provider and Commissioner. These, together with other quality outcomes in contracts, will be monitored in detail by Commissioners, as part of the performance management of the Provider through regular Clinical Quality Review Meetings. It was noted, with disappointment, the missed opportunity for quality improvement through many of the acute and community CQUIN schemes last year. Commissioners felt that where a CQUIN was not achieved, action to be taken to enable improvement could have been detailed. It is hoped that closer working between commissioning and provider quality leads will better support next year’s position on the achievement of CQUINS. Where appropriate, CQUIN schemes that were not achieved in 2010/11 have been included as Quality Requirements within the relevant 2011/12 contracts; including penalties for nonachievement. Commissioners would like to congratulate the Provider on the development and robustness of their clinical audit process and for the future would recommend the inclusion of examples of re-audit to evidence on-going and sustainable quality improvements. Given national interest in basic care for patients, Commissioners would like to see a focus on ‘Essence of Care’ and how it could be introduced into the audit programme by the Provider and reflected in the Quality Account next year. In next year’s Quality Account the Commissioner would also like to suggest the inclusion of the outcomes and learning from the review of incidents, which provide qualitative reflection on the quality of care and services received by patients. The Commissioner understands that the quality of patient care can be linked to the health and well being of staff. Whilst workforce is included in the Quality Account there is no reference to the key findings of the most recent staff survey. NHS Isle of Wight Quality Account 41 Overall, Commissioners, including representation from the GP Commissioning Consortia, would commend the Quality Report as a fair reflection of the Provider's positive achievement across the quality agenda and the high level of commitment and effort across a diverse organisation to constantly improve the quality of services provided. Statement from the Isle of Wight LINks The Isle of Wight LINk welcomes the opportunity to comment on the Isle of Wight NHS Quality Account and to provide the following statement in response to the completed document. The LINk membership feel that the Quality Account is a reasonable reflection of the healthcare services provided. We congratulate the IW NHS on its ability to respond to the challenges presented over this last year due to adverse weather and sincerely hope that any amalgamation of health services within the SHIP area will not affect the ability of the local NHS to respond to local needs. The LINk welcomes the patient-focused priorities for the next year though there remains concern that, due to the changes within the health and social scare sector, clinical time may be reduced to focus on infrastructure development. Patients must remain a priority. We are particularly keen to support the IW NHS in improving stroke care – over the last year the LINk, through its development of the Island Dignity Network, has worked tirelessly with local people and professionals, including NHS representatives, to improve dignity in all care settings with a specific focus on the Stroke Unit due to the number of concerns raised by LINk participants about this ward. It is also reassuring to note the IW NHS has prioritised the pathway for those with alcohol addiction. This clearly shows a commitment to consider the holistic health and well-being of a person and will no doubt reduce readmittance to St Mary’s though we would hope focus extends beyond Sevenacres to other wards. It is a concern that the IW NHS failed its target on completing discharge summaries, not only because of the payment then not received through CQUIN but because incomplete discharge summaries can have severe consequences for the patient. Similarly, insufficient detail has been noted by CQC on care plans for Sevenacres inpatients, again, an omission that can have very negative consequences for the patient. With regards to priority 8 the IW LINk is encouraged that following the changes in the Mental Health Act 2007 section 31, no child will be admitted on to an adult mental health ward. However, the LINk is concerned to note that when emergency admission to the children’s ward at St. Mary’s is inappropriate due to issues of patient risk and safety, that the children have to be admitted to services in Winchester or Marchwood. The IW LINk appreciates the steps taken by the reach/ outreach service in Specialist Child and Adolescent Mental Health services to enable regular visiting but feels that there is a need for Island-based service provision to children and young people presenting in psychiatric distress and emotional crisis. The IW LINk is pleased to note that, in benchmarking against national data, patients consistently feel better following surgery than patients elsewhere. The NHS Trust is to be congratulated on the development of its Enhanced Recovery programme that has reduced length of stay for specific patient groups. Based on current evidence, the rollout to other patient groups will ensure increased bed availability at peak times. The LINk is also encouraged to note the increase in weekly discharges across acute wards – we sincerely hope this increase is not due to patients being discharged too early as this will not only impact on patients but will have severe financial repercussions for the NHS Trust. In 2010/11 the NHS Trust managed to only survey 24% of discharged patients. Last year the IW LINk offered to conduct the Getting It Right survey as an independent group, to encourage openness and response. Once again, we would like to offer to assist in conducting surveys to establish patient and relative views, and to then assist the NHS Trust in any required improvement planning. In addition, the LINk has continued to gather feedback, as a result of significant national and local changes, from both its own participants and the wider public regarding health services on the Isle of Wight. As a result, the LINk has identified some specific areas of focus for the next year. These include: NHS Isle of Wight Quality Account 42 • • • • The effectiveness of public health programmes Developing GP knowledge of community-based services Ensuring the NHS Trust is meeting the social care needs of patients upon discharge Ensuring the Island population remains a priority within the NHS as the local NHS works in partnership with mainland NHS organisations. This next year will be a taxing year for the NHS Trust. Job losses have already been cited as inevitable. The relationship between the commissioning arm and provider arm will need to be disentangled. Sufficient support needs to be provided to the GP Commissioning Group. Restructuring will also continue within the Local Authority. Each of these areas is a significant concern in isolation – together they present a big concern but also a great opportunity to review what has been carried out historically and what can be done better. The LINk looks forward to working together with the Trust over the coming year to meet the challenges presented. Laura Spooner Chair, Isle of Wight LINk. Statement from the Health and Community Wellbeing Scrutiny Panel, Isle of Wight Council The Quality Accounts clearly demonstrates the work being undertaken to address areas where performance has been assessed as requiring improvement. The actions that are being taken show the commitment to continuous quality improvement with a patient focus. The contents illustrate that the views and experiences of patients and the public have been taken into account. The involvement of partners in key elements of service delivery is also shown. The document is a valuable reference tool that will assist the Scrutiny Panel in the formulation of its future work plan both in terms of health scrutiny and the wider scrutiny of services to develop effective and efficient community wellbeing. Councillor Margaret Webster Chairman of the Isle of Wight Council’s Health and Community Wellbeing Scrutiny Panel Statement from NHS Isle of Wight Patient Council The Patient Council has had a busy year supporting the development of quality services for Island residents and visitors. Our role includes reviewing plans, participating in service improvement groups and monitoring services which we undertake with presentations to the Council and visits to services. Our views and recommendations are made known directly to the Board and we are represented at Board meetings. We welcome the opportunity to comment on the Quality Account. NHS Isle of Wight is to be commended on the improvements demonstrated in this Quality Account, and we congratulate the Trust on the progress being made. We make specific comment as listed below: • The introduction of the Out Patient and Hospital Parenteral Antibiotic Therapy (OHPAT) service (priority 7, para 2.1.7) for the Island has reduced pressures on beds is welcome and the success of the NHS Isle of Wight in dealing with the winter pressures during late 2010 and early 2011 is to be commended. NHS Isle of Wight must continue to work closely with outside agencies to ensure that services outside the direct control of the NHS are resilient and meet set quality standards. • The developments and improvements in discharge planning and the low level of emergency readmissions are good news. NHS Isle of Wight must continue to work with partners to identify gaps in the patient pathway which might lead to unnecessary readmissions. • Nutrition is identified as a contributing to improving the care of patients with pressure ulcers and the Patient Council would urge NHS Isle of Wight to continue to ensure that issues affecting the nutrition of patients are addressed to enable patients to build up their strength and recover more NHS Isle of Wight Quality Account 43 quickly. • Information is a vital component of care for any group of patients including those with physical disabilities. We would encourage NHS Isle of Wight to ensure that patients are put in touch with appropriate support groups as this can be vital to a patients ongoing care, support and recovery. The Patient Council congratulates the NHS Isle of Wight on its many achievements during 2010/11 and, recognising the challenges ahead, looks forward to working with the NHS over the coming year. Mike Carr Chair, Patient Council 3.3 Changes to Final Version of the Quality Account During April and May 2011, this Quality Account was subject to consultation and feedback from a wide range of internal and external stakeholders, including PCT Commissioners; LINks; Health and Community Wellbeing Scrutiny Panel (OSC) and the Patient Council. Amendments to the final version include:Section 2.1.2 Priority 2, Prevention of Venous Thromboembolism (VTE) - updated to reflect why this is a priority for NHS Isle of Wight. Section 2.1.4 Priority 4, Reduction in 28 Day Readmission rates in Mental Health – updated in line with 2011/12 CQUIN scheme. Section 2.2.3 Patient Safety Walkrounds – updated to reflect the wide range of areas involved in the process. Section 2.2.4 Participation in Clinical Audit – section added on the annual Clinical Audit Prize. Section 2.2.6 Goals Agreed with Commissioners – CQUIN schemes 2011/12 updated in line with the latest versions from NHS Isle of Wight Commissioners. Section 3.1 Review of Quality Performance – Introduction added including NHS Litigation Authority (NHSLA) and Patient Environment Action Team (PEAT) results. Section 3.1.3 Healthcare Associated Infections (HCAI) – Introduction added including reporting mechanisms and data discrepancy in performance reporting for C.difficile. Section 3.1.5 Health of the Nation Outcome Scales (HoNOS) – Information added regarding ongoing reporting. Section 3.1.6 Patient Reported Outcome Measures (PROMS) – Information added regarding ongoing reporting. Section 3.1.7 Hospital Mortality – Comment added on audit. Section 3.1.9 Reducing Length of Stay including Enhanced Recovery – Information added regarding ongoing reporting. Section 3.1.10 Compliments and Compliments – information added on actions taken and NonExecutive Director involvement. NHS Isle of Wight Quality Account 44 3.4 How to Provide Feedback on the Account This important document sets out how we continue to improve the quality of the services we provide. Your Views on Quality We welcome your views and suggestions on our Quality Priorities for 2010/11 set out in Part 2 of this Quality Account. We welcome feedback at any time on our Quality Account. This can be sent to the Quality Team NHS Isle of Wight, St. Mary’s Hospital, Parkhurst Road, Newport, Isle of Wight, PO30 5TG or emailed to quality@iow.nhs.uk. You can read more about the national requirements for Quality Accounts on the NHS Choices or Department of Health websites. You can download a copy of this Quality Account from www.iow.nhs.uk/publications. NHS Isle of Wight Quality Account 45 Appendix 1 Stakeholders engaged in the development of the NHS Isle of Wight Quality Account Full List Chief Nurse and Director of Infection Prevention and Control NHS Isle of Wight Trust Board members Business and Projects Manager – Quality & Clinical Standards Directorate Provider Quality Manager Head of Communications Communications Assistant Patient’s Council Representatives Local Involvement Networks (LINks) Representatives Adult Social Care, Health & Housing Scrutiny Panel Representatives Chief Operating Officer Associate Director, QIPP & Reform Team Associate Director – Medical, Emergency & Diagnostics Directorate Associate Director – Elective Services / Mental Health & Learning Disabilities Directorates Head of Clinical Services - Elective Services Directorate Head of Clinical Services – Medical, Emergency & Diagnostics Directorate Head of Clinical Services - Community, Family and Therapy Services Directorate Senior Nurse Manager – Mental Health & Learning Disabilities Directorate Clinical Director / Consultant – Mental Health & Learning Disabilities Directorate Clinical Director / Consultant Paediatrician – Community, Family and Therapy Services Directorate Clinical Director / Consultant General Surgeon – Elective Services Directorate Clinical Director / Consultant in Emergency Medicine – Medical, Emergency & Diagnostics Directorate Head of Governance and Assurance Assistant Director of Finance Head of Public Health Strategy & Partnerships Medical Director Lead Cancer Manager Business Co-ordinator – Provider Services Deputy Director - Human Resources General Managers – Elective Services Directorate Tissue Viability Nurse Infection Prevention and Control Team IV Nurse Specialist Senior HR Manager Critical Care Outreach Service Deputy Chief Nurse / Head of Clinical Standards Research Management & Governance Manager Deputy Associate Director – Mental Health and Learning Disabilities Directorate Head of Prison Healthcare Designated Nurse Safeguarding Children Chief Pharmacist Deputy Director of Finance NHS Isle of Wight Quality Account 46