Quality Account High quality care for all Reporting period: 1
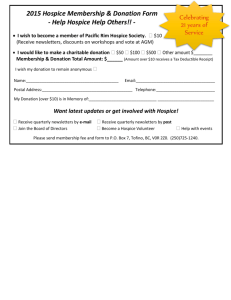
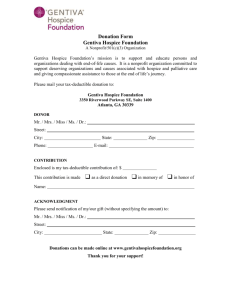
advertisement

. Quality Account High quality care for all Reporting period: 1st April 2010 to 31st March 2011 Coming to the hospice gives us reassurance and makes us feel safe. Everything seems to run smoothly and seems to work hand-in-hand with the NHS. All the information about us is at hand or can be obtained very quickly. It feels like a well-oiled machine and there is no urgency. There is time to treat us as individuals. We have a say in our treatment and care and are always asked for our opinion. Every patient is asked if there are any problems or issues and given all the time they need. If we need help when we are away from the hospice, we can telephone and ask for support. We have been given our dignity back and regained our self worth. The staff have helped us to accept our prognosis, to document our decisions about our future and to move on with the rest Patients’ Forum 30th March 2011 of our lives. 1 Chief Executive’s Statement Together with the Board of Trustees, I would like to thank all of our staff and volunteers for their achievements over the past year. Despite the current economic climate, the hospice has continued to provide a high quality service and remain financially sound. We have achieved this by providing high quality, cost-effective services to our patients and their families. For the reporting period 2010-2011, it has become clear that the Douglas Macmillan hospice is not required to produce a Quality Account. However, to demonstrate our commitment to quality, this hospice has chosen to produce a Quality Account. In this report, our aim is to show how the hospice measures quality, involves patients and strives for improvement. The Douglas Macmillan Hospice has been a leader and innovator in the hospice movement and now has a comprehensive clinical governance function. This has enabled the hospice to focus on the quality of the services provided. Once again this year, our regulators have assessed the treatment and care provided by the hospice as being of high quality. Following submission of our self-assessment in November 2009, the Care Quality Commission identified no shortfalls in the services provided by the hospice. This is a tribute to the hard work of every member of staff working for the Douglas Macmillan Hospice. The hospice has a culture of continuous quality monitoring, in which any shortfalls are identified and acted upon quickly. I am responsible for the preparation of this report and its contents. To the best of my knowledge, the information reported in this Quality Account is accurate and a fair representation of the quality of healthcare services provided by our hospice. The safety, experience and outcomes for all our patients and their loved ones are of paramount importance to us. We continue to actively seek the views of our service users. Michelle Roberts Chief Executive 20/06/2011 2 Section 1 Improvement priorities Priorities for improvement 2011-2012 Following our last self-assessment against the National Minimum Standards, the hospice was assessed as not needing an inspection. There were no areas for improvement identified. In October 2010, the hospice completed the re-registration process required under the Health and Social Care Act 2008. Following re-registration, the hospice received a Quality Risk Profile (QRP), which categorised the hospice as a low risk organisation. To maintain the QRP at this level, the hospice provides quarterly reports to the Care Quality Commission. The Board did not identify any specific areas of shortfall to include in the priorities for improvement for 2011-2012. In developing the strategic plan for the hospice, particular attention was paid to the national priority of developing community-based services, as outlined in the Demos report (Leadbeater and Garber, 2010). The Board looked at how the hospice could extend its services to better meet the needs of the local population, enabling people to receive care in the place of their choice, whilst taking account of the current national economic situation Following consultation with the staff and the Patients’ Forum, the DMH confirmed the top three quality improvement priorities for 2011 to 2012 to be as follows: Future planning Priority 1 Provision of home care in Community Lodges The Community Lodges were opened officially on March 22nd 2011 and will start to receive patients after April. These innovative Community Lodges reflect the vision for the future of palliative and end of life (EOL) care services set out in the recent Demos report entitled Dying for Change. As this is an innovation, the hospice will develop the model of care over the coming 12 months to meet the needs of the local population. This nurse-led facility will play a significant role in improving the quality, accessibility, flexibility and integration of palliative and end of life (EOL) care in North Staffordshire. The Community Lodges will be managed by the Douglas Macmillan Community Palliative Care team, and will improve integration and availability of palliative care services across primary and secondary care. The Community Lodges will provide an alternative place of death for patients, where they can be 3 with friends and family, have their personal care looked after and their pain relieved. In addition, the community lodges will provide support for carers by providing access to respite care for adults, including young adults who are too old to receive care from the local children’s hospice. As part of the integrated care provided by the hospice, the unit will assist in preventing inappropriate EOL admissions to hospital. . Future planning Priority 2 A new spiritual area, bereavement suite and reception area. On April 1st, the hospice will commence a major three-part building project. The hospice has obtained part of the costs in restricted grants. As this project is considered to be of such high priority the board has agreed to support the balance of the funding needed from reserves. The project includes the following elements: • A new multi-faith spiritual area, which is purpose built and is away from the hustle and bustle of the main building • A new bereavement suite close to reception will allow bereaved relatives to access the service without needing to enter any clinical areas which may hold difficult memories or associations for them. Also, it will enable visitors who are returning to the hospice to collect certificates and belongings to do so in a more private way which respects their privacy and dignity much more effectively than currently. • A new reception area to bring together the main functions of the hospice around one new user-friendly access and circulation area. All principal functions will be off the new reception area which will make the first visiting experience much less intimidating. This project brings together the main functions of the hospice around one new user-friendly access and circulation area. The Patients’ Forum continues to highlight the fear service users experience when coming to the hospice for the first time. 4 Future planning Priority 3 Enhancing the knowledge and skills of the Multi-disciplinary Team Over the last 12 months, the demand for psychological therapy at Level 4 (NICE Guidelines, 2004) has increased. In order to meet this increase in demand, the hospice will appoint a permanent, fulltime Clinical Psychological Therapist. This post will review current practice and take the service forward in line with current guidelines and best practice. The new role will enhance psychological services in the following areas: • Through the provision of a core member of the MDT • Provision of psychological therapy for patients • Provision of pre and post-bereavement support for carers • Input into the education and training of staff The hospice is placing an increasing focus on the rehabilitation of patients, enabling them to maintain independence and to maximise their quality of life. In addition, over recent years, the hospice has received an increase in the number of non-cancer referrals, particularly patients with COPD, who benefit from the input of a specialist physiotherapist. The hospice will appoint a permanent, full time physiotherapist, who will develop services to meet the needs of these patients. • Through the provision of a core member of the MDT • Provision of specialist physiotherapy • Provision of group sessions with a focus on breathing and fatigue. • Input into the education and training of staff Progress against the improvement priorities identified in 2010-2011 The Douglas Macmillan Hospice (DMH) was fully compliant with the National Minimum Standards (2002). As such, the Board did not have any areas of shortfall to include in the priorities for improvement for 2010-2011. The hospice had a series of ongoing initiatives to enable the hospice to offer a more comprehensive service to the local community, whilst remaining within the limitations of the financial constraints at that time. All plans for improvement were identified through needs assessments of the local community and direct patient involvement. As far as possible, we had discussed all initiatives with the hospice’s Patients’ Forum. 5 Inevitably, progress against the quality improvement priorities for 2010-2011 was influenced by financial constraints of the charity. Progress is discussed below. Progress made against Improvement Priority 1, 2010-2011 The Community Care Unit The hospice was successful in its application to the Department of Health to support this project, being awarded £500K against the £543K requested. The application specified that funding would be designed to provide an innovative new intermediate care unit. Building work was completed, on schedule, at the end of February 2011 and an Open Day was held on March 22nd 2011. The development of this innovative unit is a key priority for 2011-2012. Progress made against Improvement Priority 2: A new spiritual area, bereavement suite and reception area. This project is driven by the requirements of our patients and their families. The importance of this project is seen as a high priority for the development of hospice services for the local community. The hospice has obtained part of the costs in restricted grants. As this project is considered to be of such high priority the board has agreed to support the balance of the funding needed from reserves. This represents a significant commitment from the Board of Trustees. The building and development of this project is a key improvement priority for 2011-2012. Progress made against Improvement Priority 3, 2010-2011 Volunteer respite sitting service A volunteer respite sitting service was developed by the Hospice at Home Service to provide additional support to patients and respite for carers. The Patients’ Forum was asked for views on how this service should be developed. These views were incorporated into the service configuration. Following a successful pilot, the service commenced in January 2010, with tight referral and selection criteria. The service commenced with 4 volunteers and has since expanded to total 9. Support was 6 provided to 18 patients with a total number of 154 shifts of care (Respite shifts 103; patient companionship 51 shifts). Each shift had a duration of 2-3 hours. Training is now being offered by the Voluntary Services Department to develop the knowledge and skills of volunteers working in direct contact with patients. It is hoped that this will enable the hospice to expand the personal care we are able to offer from volunteer input in 2011. The hospice is committed to enabling patients to remain in their preferred place of care. This commitment is evidenced by the rating of the Hospice at Home service in terms of outcome (96%), satisfaction (97%) and experience (98%). 7 Section 2 Mandated Statements Statements of assurance from the board The following are a series of statements that all providers must include in their Quality Account. Many of these statements are not directly applicable to hospices. Review of services During 1st April 2010 to 31st March 2011, the DMH provided the following services: • In-Patient Unit • Day Hospice (renamed Day Therapy Unit) • Out Patients • Hospice at Home • Palliative Care Nurse specialist Service The DMH has reviewed all the data available to them on the quality of care in all of these services. The hospice provided 70% of the funding for these services. The PCTs provided 30% of the funding. Participation in clinical audits During 2010/11, the DMH was ineligible to participate in the national clinical audits and national confidential enquiries. The reports of five local clinical audits were reviewed by the DMH during 2010/11. The DMH intends to take the following actions to improve the quality of healthcare provided. • The nutrition and hydration audit highlighted some minor shortfalls, which were included in an action plan to be agreed by the Clinical Governance Operation Group. This action plan recommends the following: o Protective mealtimes o Ensure that all patients are screened in accordance with the NPSA guidelines. 8 Research The hospice is involved in a local, ethically approved, qualitative research study being undertaken by Susan Walker, whose PhD is entitled Preferred Place of Death: One UK Hospice Perspective. This study is ongoing but has led to one publication at this time (Walker S and Read S, 2011). Quality improvement and innovation goals agreed with our commissioners For Stoke-on-Trent PCT, 1.5% of DMH income in 2010/11 was conditional on achieving quality improvement and innovation goals through the Commissioning for Quality and Innovation payment framework. The goals and indicators for the hospice were as follows: Goal 1 Completion of an annual patient and carer survey to measure Patient and carer related Outcome Measures (PROMs and FROMs) and Patient and Carer Related Experience Measures (PREMs and FREMs). Indicator 1a Carry out a survey of patients and carers who have recently completed an episode of care with the hospice. Indicator 1b Demonstrate that the results have been reviewed and any learning points have been actioned and shared with hospice staff and patients/carers. Indicator 1c share the results and any subsequent action plan from the survey with NHS Stoke-on-Trent. The schedule of patient and carer surveys commenced in October 2010. These surveys have been designed to enable the hospice to quantitate the responses given for the following measures: • Patient Reported Experience Measures (PREMs) • Patient Reported Outcome Measures (PROMs) • Carer Reported Experience Measures (CROMs). • and Carer Reported Outcome Measures (CROMs) • Overall satisfaction. 9 In total, 474 surveys were sent to patients and carers with 206 completed surveys returned, giving an overall response rate of 45%. A summary of the results is given below. In-Patient Unit - Outcome Satisfaction Measure Measure Measure 94% 95% 88% 93% 91% 94% carer’s score 92% 94% 89% 91% 91% 93% patients’ score carer’s score 94% 98% 90% 93% 93% 95% carer’s score 98% 96% 97% patients’ score Day Therapy Unit - Experience carer’s score patients’ score Community Hospice at Home - The hospice will need to evaluate what these scores mean and what is an acceptable score for patients receiving specialist palliative care, where an outcome score may reflect high expectations which cannot be met. Unrealistic expectations would also influence the satisfaction measures. The differing expectations of the patient and family might explain why, in all areas, the carer gave more positive feedback than the patient. The high score achieved by the Hospice at Home Service demonstrated how important this service is to families at a time of great vulnerability. The hospice is committed to enabling patients to die in their preferred place of care and to help families through this difficult period. What others say about us The DMH is required to register with the Care Quality Commission and its current registration status is unconditional. The DMH has no conditions on registration. The Care Quality Commission has not taken any enforcement action against the DMH during 2010/11. The DMH is subject to periodic reviews by the Care Quality commission and its last review was November 2009. The last on-site inspection was on 5th February 2009. The hospice was assessed as being fully compliant and the Quality Risk Profile of the hospice categorises the hospice as low risk. 10 Data quality In accordance with agreement with the Department of Health, the DMH submits a National Minimum Dataset (MDS) to the National Council for Palliative Care. The DMH provides the MDS to the local commissioning PCTs. The DMH will be taking the following actions to improve data quality: • The IT manager will be required to undertake a series of actions in order to improve the quality of patient data reporting. Section 3 Quality overview Comparison with national minimum data sets The most recent National Minimum Dataset, which covers the period 1st April 2009 to 31st March 2010, compares the DMH with the national median values. The National Council For Palliative Care: Minimum Data Sets For Palliative Care 2009-2010 DMH National Median In-Patient Unit % New patients % Occupancy % Patients returning home Average length of stay- cancer Average length of stay- non-cancer (Data had been received from 44 large units) 84.7 88.3 73.0 75.5 45.7 48.1 11.6 14.1 10.9 12.5 Day Therapy Unit % New patients % Places used (Data had been received from 71 large units) 59.2 64.2 69.3 58.2 Outpatients % New patients % New patients with a non-cancer diagnosis Attendances per patient Attendances per clinic % attendances with a Medical Consultant (Data had been received from 50 large units) 83.9 60.0 12.5 8.1 1.3 1.5 70.2 11 1.5 2.8 58.3 DMH National Median Community: Palliative Care Nurse Specialist % New patients % New patients with a non-cancer diagnosis Face to face visits per completed series Telephone contacts per completed series (Data had been received from 42 large units) 64.2 68.1 13.1 9.6 7.0 4.4 7.8 4.2 Hospice at Home (Data had been received from 18 large units) 95.3 84.5 % New patients 12.3 13.4 % New patients with a non-cancer diagnosis 3.6 6.3 Face to face visits per completed series 0.2 3.6 Telephone contacts per completed series In-Patient Unit The hospice has a specialist community team, including a medical consultant, nurse specialists and Hospice at Home. As a result, patients are managed in their home environment, or alternative place of care, for as long as possible. Once the need arises for an in-patient admission, the hospice is committed to supporting patients to return to their home, or alternative place of care, as soon as their symptoms have been managed. Since 2006-7, the In-Patient Unit has reduced its average length of stay (LOS) from 13.6 day to 11.6 days for cancer patients and 10.9 days for noncancer patients, which is lower than the national median. The LOS and the effective use of the admission and discharge criteria enable the timely admission of patients needing specialist in-patient palliative care. This in turn has resulted in a percentage occupancy of 73.0%, which is lower than the national median value of 75.5%. Day Therapy Unit and Outpatients The percentage of new patients attending the Day Therapy Unit is 59.2%, which is lower than the national median value of 64.2%. However, the percentage of places used (69.2%) is relatively high when compared to the national median value of 12 58.2%. Throughout the reporting period, the hospice changed the emphasis of this unit to a day therapy unit, with an emphasis on clinical interventions. The percentage of out-patient attendances with a medical consultant is 70.2%, which is 20.4% higher than the national median of 58.3%. This is due to the appointment of a new Medical Consultant, whose main focus is community patients. The relatively high level of medical input, together with the comprehensive package of care offered in the Day Therapy Unit, is driven by the hospice’s commitment to enable patients to be treated in their preferred place of care and to enable them to remain at home, if this is their choice. Community: Palliative Care Nurse Specialist The hospice sees the community team as providing a significant role in improving the quality, accessibility, flexibility and integration of palliative and end of life (EOL) care in North Staffordshire. The percentage of non-cancer patients referred is 36% higher than the national median and is evidence of the hospice’s commitment to provide a service to all palliative patients. The commitment of the hospice to enable palliative patients to remain in their own home is evidenced by the number home visits patients receive per completed series, which at 7.0 is 59% higher than the national median value of 4.4 and the number telephone contacts per completed series, which at 7.8 is 86% higher than the national median value of 4.2 The relatively high level of input from the community PCNS service is indicative of the vision of the hospice for the future of palliative and end of life (EOL) care services set out in the recent Demos report entitled Dying for Change. Hospice at Home Many hospices provide a Hospice at Home Service. However the model provided by hospices is not identical and it is not easy to compare like with like. It is therefore difficult to understand the significance of the number of 3.6 face-to-face visits provided by the Douglas Macmillan Hospice per completed series, which is 57% of the national median and the number of telephone contacts per completed series of 0.2, which 5% of the nation median. The percentage of new patients seen 13 by the Hospice at Home Service is 95.3% as compared to the national median value of 84.3%. The percentage of non-cancer patients is 12.3, which is slightly lower than the median value of 13.4%. Local quality measures In addition to the limited number of suitable quality measures in the national dataset for palliative care, we have chosen to measure our performance against the following data which cover the period 1st April 2009 to 31st March 2010 and which are compared internally to the data obtained in previous years. Data for 2010-2011 are not available within the timeframe set for the completion of this Quality Account. Local quality measure Total number of new referrals to the DMH Total number of patients admitted to the In-Patient Unit (IPU) % of patients who went home Number of beds % Occupancy 2009- 2008- 2007- 2006- 2010 2009 2008 2007 1419 1439 1254 1323 649 633 591 618 46.0 47.5 49.7 52.1 28 28 28 28 73.3 74.6 72.4 Not recorded (NR) 250 213 143 129 3562 3326 3308 3447 31,811 32, 734 32,218 NR 2,163 2,254 2,063 NR Total number of complaints 7 6 4 4 The number of complaints which were upheld in full 0 0 0 0 The number of complaints which were upheld in part The number of serious patient safety incidents (excluding falls) Slips, trips and falls 4 1 0 3 0 0 0 0 105 116 79 105 1 1 3 1 Total number out-patient attendances Total number of attendances by patients at the Day Hospice Total number of contacts with patients by the community service Total number of Hospice at Home sessions provided The number of patients who experienced a fracture or other serious injury as a result of a fall. 14 Local quality measure The number of patients know to be infected with MRSA on admission to the IPU Patients infected with MRSA whilst on the In-Patient Unit Patients infected with MSSA whilst on the In-Patient Unit The number of patients know to be infected with Clostridium difficile, Pseudomonas, Salmonella, ESBL or Klebsiella pneumonia on admission Patients who contracted these infections whilst on the IPU Number of Patients admitted to the IPU with pressure sores Number of Patients who developed pressure sores whilst on the IPU Unplanned transfers from the IPU to another hospital Length of stay on the IPU (days) 2009- 2008- 2007- 2006- 2010 2009 2008 2007 6 9 8 7 0 0 0 0 0 NR NR NR 0 4 3 8 0 0 0 0 116 106 112 102 5 7 8 9 11 5 7 12 11.5 12.1 12.0 13.6 Referrals and admissions The hospice receives approximately 1400 referrals per year to its services. All of these referrals are assessed by the Palliative Care Nurse Specialist Service and the appropriate support put in place to suit the individual needs of the patient and their family. The hospice admits between 590-650 patients to the In-Patient Unit per year. Of these, up to 52% of patients are discharged home or to an alternative place of care. Prevention and management of falls Although many of our patients are vulnerable, they wish to retain their independence for as long as possible. The hospice philosophy is to support patients and to allow them the freedom to move around the unit. Every patient is risk-assessed on admission and provided with the appropriate level of support, such as a nurse call system and putting the more vulnerable patients in vision of the nursing station or in multiple-bedded rooms. The number of minor slips, trips and falls is fairly consistent at 5 falls per occupied bed per year. The literature provides figures of 5.7 – 6.2 falls per occupied bed per year in hospices and palliative care units (Goodridge, 2002; Pearse, 2004). In addition, eleven UK hospices have confirmed that 15 their figures are 4.5-5.1 falls per occupied bed per year (personal; communication). These figures have been assessed as acceptable for the patient group cared for in hospices. In the four reporting years, six patients experienced a fracture or other serious injury as a result of falling (0.2% of patients cared for). All of these patients had significant underlying health problems. All cases were reported to the regulator and RIDDOR and no concerns were raised about the level of care provided to patients. Prevention and management of infection Over the past four reporting years, 30 patients were known to have MRSA and 15 to have other infections when admitted to the In-Patient Unit. The nursing care and infection control measures in place ensured that no patient contracted MRSA or any other notifiable infection during a stay on the in-patient unit. Prevention and management of pressure sores Over the past four reporting years, twenty nine of 2491 patients (1.2% of the patients cared for) developed low grade pressure sores whilst an in-patient. In all cases the patients were particularly frail and their skin was very vulnerable. In all cases, appropriate treatment was given to minimise further deterioration of skin integrity. Unplanned transfer to hospital Patients were transferred to hospital where specific treatment of a non palliative nature was needed in the acute sector or the patient had experienced a fracture. Over the past four years, 35 patients (1.4% of the patients cared for) were transferred to the acute sector. Compliments, complaints and adverse comments. The existence of the hospice depends on the support of the local community, which funds over 70% of our costs. The hospice receives many letters of thanks and compliments from patients and the families we come into contact with. The number of compliments far outweighs the number of complaints. The quality of the service provided is of paramount importance to the hospice. All letters of complaint received are investigated thoroughly and note taken of any trends. Where shortfalls 16 are identified, immediate action is taken to minimise the risk of recurrence. An underlying theme to the complaints was that of communication. The hospice now requires clinical staff to undertake training in communication skills. Death location In the reporting year, 1205 of the patients being cared for by the hospice died. The death location of these patients is summarised in the following tables. Death location of patients receiving care from the Douglas Macmillan Hospice. Death Location Hospice All patients (n=1205) Death Location Local catchment area Figures from EOL strategy: based on ONS figures for 2004 Hospital Care home Hospice Other Patient's home (including home of relative or carer) 29.3% 5.2% 29% 0.6% 58% 17% 4% 3% 35% 18% The hospice is trying to obtain local comparator data regarding the place of death of patients in the local catchment area excluding acute deaths. At the time of finalising this report that data was not available but we would hope to include it in future reports. However, local data is available for the West Midlands with regard to deaths from cancer and is shown below. Death location for cancer patients receiving care from the Douglas Macmillan Hospice Death Location Acute Hospital Community Hospital Care home Hospice Other Patient's home (including home of relative or carer) * Hospice Cancer patients (n=1042) 28.8% 7.5% 3.9% 30.9% 0 35.4% Figures from WMCIU. Relates to 2005-2007.* 41% 4% 6% 15% 1% 32% Where do patients die? West Midlands Cancer Intelligence Unit, April 2011. The proportion of hospice deaths of 30.9% is clearly significantly higher than the regional figures. As these figures relate only to patients known to the hospice, it might 17 be expected that the figure would be relatively high. However, the WMCIU report 2011 notes that, although generally across the region there is an increase in hospice deaths in areas of increased affluence, both Stoke on Trent and North Staffordshire PCTs show a higher proportion of hospice deaths than the average despite not being “traditionally affluent PCTs”. Our participation in clinical audits Local quality measure 2009- 2008- 2007- 2006- 2010 2009 2008 2007 Percentage of audits completed on schedule 100% 100% 100% 100% Percentage of audits which resulted in an improvement in the quality of care. 100% 100% 100% 100% To make sure that the hospice is providing a consistently high quality service, we undertake our own clinical audits, using national audit tools developed specifically for hospices. This allows us to monitor the quality of care being provided in a systematic way and creates a framework by which we can review this information and make improvements where needed. Each year, the Board approves the audit schedule for the coming year. Priorities are selected in accordance with what is required by our regulators and any areas where a formal audit would inform the risk management processes within the hospice. Through the Clinical Governance report, the Board of Trustees is kept fully informed about the audit results and any identified shortfalls. Through this process, the Board has received an assurance of the quality of the services provided. The following audits were completed between 1st April 2010 and 31st March 2011. The hospice conducted the audits using national hospice-specific audit tools, which had been peer reviewed and quality assessed. 18 Self-assessment by the This audit has to be completed annually. Accountable Officer The hospice was fully complaint with the postShipman requirements. Management of controlled This audit has to be completed annually to provide drugs evidence to support the self assessment by the Accountable Officer. A few minor shortfalls were identified. The Board is assured that the hospice is now fully compliant. Infection control: Code of The hospice is fully compliant with the code of Practice Practice. Medical gases This was a re-audit of the strengthened procedures relating to the prescribing and administration of oxygen. A few minor shortfalls were identified. The Board has been given assurance that the hospice will fully comply with the action plan. Nutrition and hydration The Patients’ Forum assessed the hospice as 100% compliant from their perspective. The hospice found areas of shortfall with respect to documentation. An action plan has been formulated to be discussed and agreed by the Clinical Governance Operation Group. The hospice audit team has continued to develop. During 2010-2011, members of the community teams were introduced to audit and set their priorities for audit in the coming year. The hospice will present their audit results relating to nutrition and hydration at the first regional audit day on May 11th 2011, at which five hospices will share their audit results. 19 What our patients say about the organisation In 2010/11, patient and carer surveys were used to gather data to measure Patient Related Outcome Measures (PROM) and Carer Related Outcome Measures (CROM). The survey also asked questions concerning patient and carer experiences of their care episodes measured as Patient Related Experience Measures (PREM) and Carer Related Experience Measures (CREM). A response rate of 43% was achieved. Survey Type Service IPU Day Therapy Unit Community patient Hospice at Home PREM 94% 92% CREM 95% 94% PROM 88% 89% CROM 93% 91% Overall satisfaction Patient Carer 91% 94% 91% 93% 94% 98% 90% 93% 92% 95% N/A 98% N/a 96% N/A 97% This is the first time that the patient/family outcome surveys have been used by the DMH. In accordance with the requirements of our commissioners, surveys will carried out annually to monitor changes and improvements. In 2011/12, the hospice will extend the number of services included in the survey programme. During the period 1st March 2009 to 31st February 2011, 303 in-patients completed a 3-day post-admission questionnaire. This approach enables the staff to address any concerns immediately. All patients reported that they were very happy with the care provided. A patient pointed out that the sling was not suitable for bariatric patients. This concern was addressed by the Site Nurse Manager. Eight other patients highlighted that they would appreciate more information and this was given straight away by either the doctor or the nurse-in-charge. Our Patients’ Forum meets each month. At these meetings, the patients are given the opportunity to voice any concerns and make recommendations. The patients state that they enjoy the opportunity to be involved in such discussions and have input into important issues, which are reported directly to the Chief Executive. It is through the voice of the Patients’ Forum that future initiatives, such as the development of a new spiritual area, are being actively pursued. At the stage of their life at which patients receive hospice care, the patients state that it is the small things which become important to them. The patients want to be 20 involved and to have some input into the services they receive. In 2010/11, the Patients Forum influenced the following: • The hospice shop: The Patients’ Forum were passionate about the on-site shop. Having some input into this project made them feel as though they retained some control in their lives. • Spiritual area: The stained glass window in the hospice chapel provides much comfort to the majority of patients attending the Day Therapy Unit. The patients influenced the decision on how the window could be used in the new spiritual area being built at the hospice. • The Patients Forum asked if medical input could be provided on each weekday to patients attending the Day Therapy Unit. This was put in place. Each year a member of the Board of Trustees conducts an unannounced visit to provide assurance to the Board and to gain the views of service users at first hand. At the last visit, carried out on 15th July 2010, the patients and staff interviewed provided very positive feedback to the trustee. What our staff say about the organisation The Douglas Macmillan Hospice values the opinions of the staff regarding the quality of the service provided. The Hospice undertakes a staff survey every 2 years to ascertain engagement levels, celebrate success and to highlight areas for improvement. The hospice will participate in the next national DH supported staff survey when it becomes available. The hospice has a very low turnover of staff. 2010- 2009- 2008- 2007- 2011 2010 2009 2008 Staff leaving (other than retirement) 12 13 15 5 New staff 29 26 21 15 21 What our regulators say about the organisation The Douglas Macmillan hospice has to submit a self-assessment to the Care Quality Commission (CQC), formerly the Healthcare Commission, on request. In addition, to inform the CQC Quality Risk Profile, the hospice submits a quarterly quality report; a copy of this report is also provided to the commissioning PCTs. The hospice went though the re-registration between 1st April and 30th September 2010. The hospice became re-registered on October 1st 2010. As part of this re-registration the hospice received a rating of low risk. The Board of Trustees’ commitment to quality The Board of Trustees is fully committed to the quality agenda. The hospice has a well established governance structure, with members of the Board having an active role in ensuring that the hospice provides a high quality service in accordance with its statement of purpose. At regular intervals, a member of the Board undertakes an unannounced visit and produces a quality report for the Board. During this visit, the Trustee speaks to patients and staff on the In-Patient Unit and in the Day Therapy Unit. In this way, the Board has first hand knowledge of what the patients and staff think about the quality of the service provided. The Board is confident that the treatment and care provided by the Hospice is of high quality and is cost effective. 22 References DH 2008. End of Life Care Strategy: http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/documents/digital asset/dh_086345.pdf last accessed 13/05/11 Leadbeater, c. and Garber, J., 2010. Demos Report: Dying for Change. Demos, London. www.demos.co.uk/files/Dying_for_change_-_web_-_final_1_.pdf Last accessed 13/05/11 Walker, S and Read, S. 2011. International journal of palliative nursing, vol. 17, no. 1, pp 14-18. Goodridge, D. & Marr, H. 2002, "Factors associated with falls in an inpatient palliative care unit: an exploratory study", International journal of palliative nursing, vol. 8, no. 11, pp. 548556. Pearse, H., Nicholson, L. & Bennett, M. 2004, "Falls in hospices: a cancer network observational study of fall rates and risk factors", Palliative medicine, vol. 18, no. 5, pp. 478481. West Midlands Cancer Intelligence Unit. Report provide by Tim Evans (personal communication) http://www.wmciu.nhs.uk/documents/core_docs/info_pub/End_of_life_v2.0.pdf last accessed 13/05/11 23 Annex What Stoke PCT says about the organisation As a commissioner of services at the Douglas Macmillan Hospice, the PCT is pleased that the hospice, whilst not required to produce a Quality Account have chosen to do so. This demonstrates their openness and commitment to drive continuous quality improvement. In relation to CQUIN, the PCT was pleased that the hospice fully achieved its quality improvement and innovation goal. The hospice introduced patient and carer surveys to gather patient/carer reported outcomes. The results showed a high level of overall satisfaction ranging from 91% - 97%. It is pleasing to note the progress against 2010/11 priorities and also the involvement of staff and the Patients’ Forum in the identification of the quality improvement priorities for 2011/12. Having reviewed the information in the Quality Account against the information the PCT and its partners have on the areas covered, the PCT is happy to confirm that the information provided in the Quality Account is accurate. The PCT is also happy to confirm that the account provides a balanced reflection of the quality of services provided. 24