NHS Isle of Wight Provider Services Quality Account 2009/2010
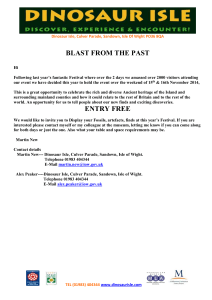
advertisement

NHS Isle of Wight Provider Services Quality Account 2009/2010 VERSION CONTROL Summary of meetings at which the Quality Account will be reviewed 12th April 2010 20th April 2010 10th May 2010 11th May 2010 13th May 2010 18th May 2010 18th May 2010 24th May 2010 2nd June 2010 Patients Council LINks Patients Council Commissioning Executive Board Overview Scrutiny Committee LINks Service Delivery Executive Board Executive Board Trust Board Version Control History: Version: 1.0 Date: 5th May 2010 2.0 21st May Carol Alstrom 2010 3rd June 2010 Carol Alstrom 3.0 Author: Carol Alstrom 2 Status Draft for Approval Final draft for approval Approved Comment: CONTENTS Part 1 Part 2 2.1 2.1.1 2.1.2 2.1.3 2.1.4 2.1.5 2.1.6 2.1.7 2.2 2.2.1 2.2.2 2.2.3 2.2.4 2.2.5 2.2.6 Part 3 3.1 3.1.1 3.1.2 3.1.3 3.1.4 3.1.5 3.1.6 3.1.7 3.1.8 3.2 3.3 3.4 Executive Summary Statement on Quality from the Chief Executive of NHS Isle of Wight Priorities for Improvement and Statements of Assurance Priorities for Improvement Patient Safety Priority 1: Identification & Management of the Deteriorating Patient Priority 2: Prevention and Management of Pressure Ulceration Clinical Effectiveness Priority 3: Patient Reported Outcome Measures Priority 4: 24/7 Ear Nose and Throat on Call Service Priority 5: Health of the Nation Outcome Scales – Mental Health Patient Experience Priority 6: Reducing Length of Stay Priority 7: Getting it Right in 2010/11 Statements of Assurance from the Board relating to the Quality of NHS Services Provided Review of Services Participation in Clinical Audit Participation in Clinical Research Goals Agreed with Commissioners What Others Say about NHS Isle of Wight Statements from the Care Quality Commission Data Quality i) NHS Number and General Medical Practice Code Validity ii) Information Governance Toolkit Attainment Levels iii) Clinical Coding Error Rate Page 4 5 6 6 6 7 9 9 10 12 14 15 15 15 19 19 20 22 22 22 Other Information Review of Quality Performance Patient Safety Infection Prevention and Control including cleanliness Falls Clinical Effectiveness Human Papilloma Virus Delivery Programme Quality in Endoscopy Mortality Patient Experience Relocation of the Neo-natal Intensive Care Unit Patient Experience in Mental Health Complaints and Compliments 33 34 34 Explanation of who has been involved Statement provided by Commissioning PCT, LINks or OSCs How to provide feedback on the Quality Account 36 37 39 Appendix 1 - CQUINs 2009/10 Appendix 2 – Care Quality Commission Annual Healthcheck 2008/09 40 42 3 23 23 25 28 29 32 EXECUTIVE SUMMARY NHS Isle of Wight is an unusual Primary Care Trust in that it not only commissions but also provides most health care services for the people of the Isle of Wight. Provider Services include an acute district general hospital, mental health services, community services, prison healthcare and the ambulance service. We have a clear vision for what we should be like and this is set out below As an Integrated Care Organisation we will: • • • • • • • • • • • Place greater emphasis on integrated service delivery- including social care, between physical and mental health care, and between primary, community and acute care delivery. Focus on improving patients experiences of services, as well as the outcome and safety of those services Support people to take more responsibility for their health and healthcare, and place greater emphasis on shared care Increase availability of community based alternatives to hospital care, giving higher priority to keeping patients out of hospital Increase the resources we deploy in community services relative to other sectors to enable an increasing focus in helping people stay healthy Deliver more services as part of strong clinical partnerships with other provider organisations Develop more active case management Focus more on developing the role of clinicians as leaders – particularly by bringing improvements in quality, patient safety and delivering value as a means of improving all round performance Use more technology, information and information systems to improve quality and productivity Search harder for innovative solutions to deliver health care and seek to continuously improve Mature our capabilities to allow the greater creation of value driven partnerships with both public and commercial organisations. During 2009/10 NHS Isle of Wight started on a journey to develop this vision, during 2010/11 we will see the building block put in place to deliver this vision for the people of the Isle of Wight. Quality in terms of patient safety, clinical effectiveness and patient experience are a fundamental part of that vision. This first Quality Account for NHS Isle of Wight Provider Services includes details of the quality improvements made during 2009/10 and sets the direction for further improvements during the coming year. It also outlines performance in national clinical audit and provides information on the views of others such as the CQC and Commissioners on the quality of services provided. The Patients Council. LINks and Overview and Scrutiny Committee have also reviewed the account and provided positive feedback. The information set out within this Quality Account has been endorsed by the Service Delivery Executive Board of NHS Isle of Wight as the Executive Committee for the Provider Services within the organisation. This account will be submitted to the NHS Isle of Wight Public Board Meeting for final approval in June 2010 prior to publication as part of the Annual Report and separately on the NHS Choices Website. The Isle of Wight NHS Primary Care Trust is a unique organisation, known as NHS Isle of Wight and referred to as such in this Quality Account 4 PART 1: STATEMENT ON QUALITY FROM THE CHIEF EXECUTIVE OF NHS ISLE OF WIGHT This is the first Quality Account to be published by NHS Isle of Wight and sets the baseline for the future measure of quality improvement within the services we provide at St Mary’s Hospital and across the services provided in our unique organisation. The Board of NHS Isle of Wight is committed to continuous quality improvement, the provision of high quality patient care, including high standards of patient safety, clinical effectiveness and patient experience. In developing this quality account we have taken account of what our patients have said to us, and we are committed to monitoring and improving patient safety, effectiveness and experience across the full breadth of our service During 2009/10 we have started on a journey to strengthen clinical leadership throughout the organisation, recognising at times that staff are not always clear about their accountability and responsibility and therefore their authority to act. The year has not been without its challenges including three unannounced visits from the Care Quality Commission to review services in relation to Healthcare Associated Infection, whilst those were difficult at the time, staff within the Provider Services have risen to the challenges and put in place mechanisms to ensure our services can clearly demonstrate that they are reducing further the risks associated with infection. The Chief Operating Officer, Chief Nurse and Medical Director provide the leadership team for the Provider Services and during 2010/11 it is envisaged that this team in conjunction with the newly configured directorate teams will provide the clinical leadership and direction for NHS Isle of Wight Provider Services. Despite the challenges through the year we have again delivered on almost all key targets relating to quality. We have continued to demonstrate strong performance in reducing healthcare associated infections, performed as one of the best organisations in NHS South Central in the delivery of the national the HPV vaccine delivery campaign, and significantly enhanced the environment in our Neonatal intensive care unit improving the experience for parents and staff. The first priority for NHS Isle of Wight during 2009/10 was to provide excellence in patient safety, clinical standards and patient experience. During the year we have developed a range of metrics that are monitored at Board level to provide an indication of how we were achieving this priority. We now have a much clearer understanding of the clinical incidents that occur in our services and the number of times these result in significant harm to our patients, and in the final 2 months of 2009/10 no patients suffered this level of harm, we anticipate this will continue into 2010/11. During the first 7 months of the year 5 patients suffered serious harm as a result of a fall but with the proactive work undertaken across NHS Isle of Wight there have been no falls in this category since October 2009, a significant improvement. During 2010/11 we intend to develop monitoring quality of services further, and have agreed a scorecard which includes mortality data, quality of services assessment, NHS litigation authority assessment standards, and patient experience measures. This will be set alongside measures already in place about clinical incidents, complaints and strengthened by the addition of ward to board performance indicators and assurance, allowing us to demonstrate our key priority of excellence in patient safety, quality and patient experience I confirm that to the best of my knowledge the information contained within this 2009/10 Quality Account for NHS Isle of Wight is accurate Kevin Flynn Chief Executive NHS Isle of Wight 5 PART 2: PRIORITIES FOR IMPROVEMENT AND STATEMENTS OF ASSURANCE FROM THE BOARD 2.1 Priorities for Improvement The next section provides the outline of the identified areas for improvement during 2010/11, and within each section there is a box highlighting the measures that will be monitored throughout the year. PATIENT SAFETY 2.1.1 Priority 1: Identification & Management of the Deteriorating Patient Identification and management of the deteriorating patient has been a priority for NHS Isle of Wight for a number of years, with a particular focus on the introduction of a Modified Early Warning System (MEWS) to identify early patients whose condition is starting to deteriorate to ensure appropriate action can be taken at the right time. However despite this action there is still in some instances a lack of compliance with the MEWS policy, which is demonstrated by avoidable admissions to the Intensive Care Unit. Over the last 10 years there have been a number of reports identifying the need for Critical Care Outreach Services to identify and manage deteriorating patients on general wards including in July 2007 the publication of ‘Acutely ill Patients in Hospital’ (2007) by the National Institute for Health and Clinical Excellence which recommended the implementation of MEWS scoring and the development of critical care outreach services. The Critical Care Outreach Service is a nurse led service that has been developed within the existing budget for the Intensive Care Unit, and is currently provided between 08:30hrs and 16:30hrs Monday to Friday. The service is an adjunct for the general ward based teams to support them in caring for patients who are critically ill or have potential to develop such an Illness and/or the potential for their condition to deteriorate. The Critical Care Outreach Service is there to support, educate and empower ward based teams and not to take over or take responsibility away from the ward based teams for their patients. If appropriate the Critical Care Outreach Nurse will undertake interventions for “at risk” patients if this is indicated and will refer directly to the Intensive Care Unit if the patient is not safe and needs immediate intervention in order to prevent further deterioration or death. Patient safety, providing high quality clinical services and improving patient experience are all key strategic priorities for NHS Isle of Wight. The identification and management of deteriorating patients supports this key objective for NHS Isle of Wight and fits with a number of national priorities including: • Lord Darzi’s Report, High Quality of Care for All - Next Stage Review, by providing high quality care that is safe and effective and patients are treated with compassion, dignity and respect (DoH 2008). The CCOS will ensure the basics are right every time for all patients in NHS IOW that are at risk of deteriorating. The CCOS will be able to measure its impact and success on patient experience, promoting safety and quality of care through data collection. • Due to an increasing ageing population and patients with long-term conditions, those needing to be admitted to NHS IOW acute beds are presenting with more complex acute on chronic health needs and higher morbidity. • Support staff with other developments in the organisation such as thrombolysis for stroke, noninvasive ventilation beds on Newchurch ward, hyper acute beds for stroke patients and cohorting wards for level 1 patients. • Support the implementation of the patient strategy for the NHS IOW. • Support the implementation of the End of Life Strategy within the hospital by identifying patients who are appropriate for the end of life pathway rather then admission to a critical care bed. • Support and contribute to the delivery of the Hospital at Night Agenda. The Critical Care Outreach Service was developed following audit of practice, se4rious untoward incidents and national recommendations. This priority has been identified by the Elective Services 6 Directorate and Service Delivery Board as a key area of improvement during 2010/11 with the establishment of a foundation Critical Care Outreach Service as a precursor to the development of a full service once the initial benefits and risks have been identified. The service is being provided across all clinical directorates within NHS Isle of Wight. Monitoring and Measurement of Progress: Specific key performance indicators that will be measures include: • No serious untoward incidents (SUI) relating to the non recognition and response to the sick patient • Reduced unplanned admissions/readmissions to the Intensive Care Unit Additional information will be collected on the progress and impact of service will be measured monthly via the deteriorating patient balance score card. Other measurement of improvements will be collected from the Critical Care Outreach Service data base which is linked to the Intensive Care Units audit database. Patient and staff satisfaction surveys will also be used to gain perception of the service as well as perceived benefits. Case studies will also be collected to demonstrate impact on the key dimensions of quality as well as providing a cost effective and efficient service within NHS Isle of Wight. Progress Reports: The progress and impact of the Critical Care Outreach Service will formally be reported back to Service Delivery Board in October 2010, with the aim of developing a permanent service to support the identification and management of deteriorating patients. We plan to expand the CCOS from November 2010 after a formal review and gaining agreement of the Service Delivery Board. It is anticipated that the fully approved Critical Care Outreach Service will then cover 7 days a week from 07:30hrs to 21:15hrs and deliver an on-call service for all out of hours critical care transfers. The development of this service cannot be considered in isolation and is being linked with the Hospital at Night project. 2.1.2 Priority 2: Prevention and Management of Pressure Ulceration Pressure ulceration or bed sores cause significant pain and distress for patients when they develop and place an added burden of financial cost on to the NHS. NHS Isle of Wight focused on Pressure Ulcers during 2009/10 as part of the Commissioning for Quality and Innovation Payment Framework CQUIN indicators demonstrating a reduction in the number of pressure ulcers grade 2-4 developing in patients who were admitted to hospital. During 2010/11 it is intended to drive this improvement further to improve patient safety and patient experience of NHS Isle of Wight services. Pressure ulcers are a key priority of the Patient Safety Federation within NHS South Central with a dedicated work stream for No Needless Skin Breakdown and in the 2010/11 CQUIN scheme with a further focus on these avoidable wounds. These priorities have been chosen as key indicators that support the process of avoiding pressure ulceration in patients at risk of skin breakdown, and managing ulceration when it occurs to support rapid healing. These contribute to meeting the National Audit Standards for Pressure Ulcer care, and their implementation has potential for reducing the impact of skin breakdown for patients in the care of NHS Isle of Wight both in acute hospital settings and within community services. Monitoring and Measurement of Progress: The specific patient safety measures that will be monitored are: • Reduction of reportable pressure ulcer incidence to NPSA (grade 2 or above) to 2% or less of total incidence. • Reduction of grade 3 and 4 pressure ulcer incidence to 0.3% or less of total incidence quarter on quarter. Additionally work will be undertaken to improve the quality of documentation for pressure ulcer incidence monitoring forms, documented repositioning regimes for patients who require these are in place, Patients with a Waterlow score of 10 or above have a pressure ulcer care plan in place and 7 that patients are reassessed at intervals as indicated by pressure ulcer care algorithm, as attached to Pressure Ulcer Prevention and Management Policy. When pressure ulcers develop those which are grade 2 or above there will be evidence of wound measurement, tracing and/or photography in the patient record. These measures will be monitored by: • Pressure ulcer incidence monitoring reported monthly and quarterly via Pressure Ulcer Reports and Tissue Viability Summary Reports. • Quarterly audit sample of patient notes quarterly for all standards related to documentation of care process. • Quarterly audit of a random sample of pressure ulcer incidence forms received by Tissue viability nurse. 8 CLINICAL EFFECTIVENESS 2.1.3 Priority 3: Patient Reported Outcome Measures (PROMs) From May 2009 the NHS introduced a national requirement to ensure that patient related outcome measure quality assessment forms (PROMs) have been implemented within all hospitals for a small number of operative procedures and this forms part of the Standard NHS Contract for Acute Services Patient related outcome measures are questionnaires given to patients undergoing certain procedures, to demonstrate their self reported health status before and after the procedure. At NHS Isle of Wight there is a requirement to collect the information for hip and knee replacements, and groin (inguinal) hernia procedures undertaken within St Mary’s Hospital on patients aged 16 or over. The Pre Assessment and Admissions Unit are responsible for ensuring that patients are given the PROMs questionnaire at pre assessment. The PROMs used to collect data from patients comprise of a condition specific questions, sociodemographic questions and questions about the patients general health, previous surgery, comorbidities and length of time with the condition. These questionnaires are confidential and consent from the patient for participation in this process is always obtained. The questionnaires are collected by courier and taken to the National Administration Centre, where the information is processed. At either three or six months after the procedure the National Administration Centre arrange for a second questionnaire to be sent to the patient at their home address to measure how the patient is post operatively. This is dealt with by the administration centre and NHS Isle of Wight is not involved in this aspect of the data collection. Monitoring and Measurement of Progress: The Department of Health released the first set of pre-operative outcomes as a benchmark for all hospitals on 8th April 2010. This information provides clinical outcomes of NHS services from the patients’ perspective and is currently being analysed to determine the measures NHS Isle of Wight will use in the 2010/11 Quality Account to demonstrate quality improvement. Improvement will be monitored by: • Increase the percentage of patients that have an improved outcome following a surgical procedure. • Monitor results and undertake benchmark analysis in order to compare against similar size organisations. The potential benefits from the collection of PROMs data are envisaged to be the following: • Supporting patients and GPs to make choices over treatment • Supporting clinicians and manager to benchmark their own performance • Supporting commissioners to judge the quality of care offered by their providers • Supporting reduction in inequalities • Strengthening audit and research 2.1.4 Priority 4: 24/7 Ear Nose and Throat (ENT) on Call Service Prior to 1st April 2010 the Isle of Wight PCT’s Ear Nose and Throat Service (ENT) provided a 5 day a week on call service based on the Isle of Wight, with Portsmouth Hospitals Trust responsible for the delivery of on call services from 5.00pm Friday until 9am the following Monday morning. The Department employed 1.40 full time equivalent Consultant ENT Surgeons and a full time Associate Specialist. In early 2009 it became apparent that all three clinicians would be retiring no later than March 2010. The retirement of all three clinicians provided an opportunity to review the future service configuration of the Islands Ear Nose and Throat Department and the secondary care provision of services. An external review of ENT services on the Island was undertaken early in 2009; this review was commissioned by NHS Isle of Wight Commissioners and carried out by a representative from the Royal College of ENT surgeons and a GP 9 The review recommended that NHS Isle of Wight should provide a 24 hours a day, 7 days week secondary care on call service and to ensure that this was possible the review recommended the appointment of three full time consultants. Three consultants were required to ensure that NHS Isle of Wight could provide the optimum level of on call cover. A lengthy consultation process then followed to ensure that all views were taken into consideration about the future of ENT services on the Isle of Wight. A series of meetings were held with patients, commissioners, GP’s and Secondary Care colleagues. Discussions also took place with both Southampton and Portsmouth Hospitals Trusts, along with representatives from the Cancer Network. A decision was then taken in the autumn of 2009 to recruit three full time ENT consultants each with a specialist interest. These new posts were recruited in partnership with Portsmouth Hospitals Trust with each consultant undertaking sessions in Portsmouth. Consultants were recruited with specialist interests in Head and Neck Cancer, Otology and Rhinology. The consultants will undertake the complex specialist surgery in Portsmouth. The new service configuration for ENT and in particular the new on call arrangements will help to ensure that both patient experience and, more significantly, patient safety are improved for Islanders. This change will also ensure that patients do not have to travel to the mainland for treatment at weekends, as has been the case in the past and those emergency patients are treated by local ENT Consultants. Monitoring and Measurement of Progress: The measure of quality that will be applied to this service during 2010/11 will be: To reduce the number of emergency admissions for patients with ENT conditions • Emergency admissions to Portsmouth Hospitals were 27 in 2008/09 and 30 in 2009/10. The number of emergency admissions to Portsmouth Hospitals should fall by a minimum of 75% to a maximum of 7 patients. • Emergency admissions to St Mary’s Hospital IoW were 47 in 2009.10. This number will increase to 57, due to repatriation from Portsmouth Hospitals. • The total number of emergency ENT admissions will reduce from 77 to 64 ~ a fall of 17%. To reduce the number of emergency ENT patients travelling to the mainland for their care to a minimum • Emergency admissions for complex head and neck cancer may continue to be referred to Portsmouth Hospitals, for example for immediate/urgent radiotherapy. This number should not exceed 7 patients per annum • Emergency outpatients will no longer have to travel to Portsmouth for out of hours care, thus the number of such patients will reduce to zero. These are patients who attend A & E department with ENT problems, at weekends. 2.1.5 Priority 5: Health of the Nation Outcome Scales (HoNOS) – Mental Health The Royal College of Psychiatrists Research Unit developed the Health of the Nation Outcome Scales and these have been in use in Mental Health Teams for some years. The Royal College originally developed HoNOS as a means of recording progress towards the Health of the Nation target ‘to improve significantly the health and social functioning of mentally ill people’. HoNOS consists of 12 categories measuring behaviour, impairment, symptoms and social functioning. When a patient is referred to the service their HoNOS score is recorded and measured periodically afterwards. This can help with identifying the progress an individual is making towards recovery and help improve their treatment. The use of HoNOS is recommended by the National Service Framework for Mental Health and by the working group to the Department of Health on outcome indicators for severe mental illnesses. It is recognised as an integral part of the Mental Health Minimum data set. The service is planning to role out the use of HoNOS across most of its services in a consistent and planned way. Completing assessments at the start of treatment, then at regular intervals, will help in 10 ensuring that we measure the health and social functioning of mental health patients and any improvement in symptoms. It will then be used to inform part of the Care Programme Approach for individual service user, potentially leading to further assessment and intervention if appropriate. Monitoring and Measurement of Progress: • • • • A total of 14 teams using HoNOS 95% of new patients in participating teams who have received a HoNOS Score 95% of Adult Inpatients who have received a HoNOS Score (both new and existing patients) Total number of patients who have received at least an Initial HoNOS Score (both new and existing patients) On a Directorate basis, the collected data will be used to compare the effectiveness of treatment by individual teams and clinicians. The data will also be collected to assist with acuity studies, support discharge from services and as a performance management tool, i.e. if a patient has no improvement then the clinician needs to review treatment plan. These measures will be developed and refined during 2010/11 to allow the publication of results in the next annual Quality Account. 11 PATIENT EXPERIENCE 2.1.6 Priority 6: Reducing Length of Stay NHS reforms have for the first time given real incentives for NHS hospitals to reduce the length of time their patients spend in hospital. Reducing hospital admissions and caring for people more appropriately outside of hospital remains a key priority to reduce the risks associated with hospital admissions. However when hospital care is needed the NHS needs to minimise that time, whilst not undermining patient safety or quality of care. Alongside changes to administrative systems and processes, a major factor in reducing length of stay is improving levels of care so that patients recover more quickly. Most people spend a very short period of their lives in hospital; their discharge follows a fairly predictable pattern and they usually return home. The development of high-level clinical care and intermediate care in the community now enables more people with disabilities and long-term illnesses to remain in their own homes. For those people already in the care system, or for those who will need ongoing support when they leave hospital, admission and discharge processes are now more characteristic of a ‘transfer of care’ process. It is continuity of the right care in the right place that is important for these people. A protracted length of stay in hospital increases the risk of: • infection; • depression/low mood; • boredom; • frustration; • loss of independence and confidence; and • NHS resources being used inappropriately. In the current challenging economic climate and likely reduced NHS growth, productivity and efficiency are paramount. Cash in the NHS will need to be spent more wisely. Considering the average cost for a patient to stay in an NHS surgical ward is up to £400 per day, the financial benefits of reducing length of stay are huge. Technology has a significant role to play in this. The average length of hospital stay ranges from 10.9 days in the top ten NHS trusts to 44.5 days in the lowest performing trusts for patients with a fractured neck of femur (broken hip); between 7.4 days in the top ten trusts to 29 days in the lowest performing trusts for hip replacement; 13 days in the top ten trusts to 55 days in the lowest performing trusts for patients following an acute stroke; and 6.4 days in the top ten trusts to 20 days in the lowest performing trusts for knee replacement. NHS Isle of Wight has two quality improvement schemes in place for 2010/11 to support the reduction in length of stay in hospital. These are Enhanced Recovery and reducing adult inpatient length of stay. Enhanced Recovery/Reducing Length of Stay to Improve Patient Experience and Outcomes Enhanced Recovery focuses on improving patient outcomes and speeding up a patient's recovery after surgery and results in benefits to both patients and staff. The programme focuses on making sure that patients are active participants in their own recovery process and it also aims to ensure that patients always receive evidence based care at the right time. It is a model of care that has the potential to have a significant impact in delivering the Shaping the Future or QIPP (quality, innovation, productivity and prevention) programme and in reaching the 18 week referral to treatment targets. It supports reducing patients return to normal from weeks to days and has the potential to save 200,000 bed days nationally whilst improving the patient experience. The overarching aim of enhanced recovery is to improve quality and reduce the length of stay for elective care pathways. Patients on enhanced recovery pathways recover more quickly following surgery, and so can leave hospital and get back to normal activities sooner; examples already show reductions in length of stay by as much as 10 days for colorectal patients. 12 Benefits of enhanced recovery Quality Improved clinical outcome Early detection of complications Earlier additional treatments i.e. radiotherapy Meeting quality standards Meeting operational standards Harmonisation of care across the NHS Productivity Reduce length of stay Reduced use of ITU Potential to treat more patients with same resources Increased capacity Longer term tariff benefits Local health community Closer working partnerships with acute, primary and prison care Improved reputation Staff Improved multi-disciplinary experience Team building Educational opportunities Improved focus Recognition for achieving improvements in quality and patient experience ↓ Patients Improved patient experience Empowering patients Planned early rehabilitation Early return to normal daily activities Reduced exposure to hospital infection Fewer complications During 2010/11 NHS Isle of Wight will introduce Enhanced Recovery into the following services – Colorectal starting July 2010 , Gynaecology and Orthopaedics starting September 2010 Reduction in Adult Patients’ Length of Stay in Hospital There is usually more variation between hospitals in the pattern of discharge than in the pattern of admission. For all hospitals, discharge rates generally peak on Fridays and drop steeply during the weekend. While patients are admitted seven days a week as emergency admissions, most are discharged on five. For patients admitted as an emergency, the reduction in discharges over the weekend compared to weekdays varies from over 75% to less than 15% The day of admission also affects the length of time patients with similar clinical requirements stay in hospital. A patient who is admitted on a Friday may have a length of stay 25% longer than a patient admitted on a Tuesday. NHS Isle of Wight Inpatient specialties current average length of stay is:Area Average LOS Average LOS emergency planned admissions admissions Surgical 6.08 days 2.52 days Trauma & Orthopaedics 14.46 days 5.62 days Medical 13.24 days 5.76 days Mental Health 41.68 days 55.20 days Monitoring and Measurement of Progress: During 2010/11 NHS Isle of Wight plans to achieve: • An overall reduction in our patients’ length of stay. NHS Isle of Wight is aiming to reduce length of stay in line with national top quartile performance, this will be finalised in year prior to reporting in the 2010/11 Quality Account. • No increase in readmission rate for medicine, surgery and trauma and orthopaedics Supporting this measure will be the delivery of the Community Rehabilitation Service for stroke patients in order to improve their outcomes, reduce mortality and long-term disability, ensuring that patients are cared for in the right setting to achieve the best possible outcome and the introduction of 13 enhanced recovery for a range of surgical patients to enable early recovery quicker discharge from hospital, and more rapid return to normal activities. 2.1.7 Priority 7: Getting it Right in 2010/11 Whilst the NHS Isle of Wight participates in all national, and undertakes a number of local patient experience surveys, feedback from both national and local surveys have highlighted that the views of our service users is often sought some time after discharge, which can often mean that the data is less meaningful. The National Surveys specifically ask the question of patients whether they have been asked about their care during their inpatient episode, the PCT’s results show NHS Isle of Wight is not asking patients to comment on their experiences whilst they are in hospital. Patient feedback is extremely valuable for improving and redesigning services in addition to providing benchmarking between services and organisations. Further benefits include provision of data to allow professionals to reflect on their own practices, to inform commissioners about the quality of services and to help patients choose high quality providers. From the 1 April 2010, all inpatients cared for by NHS Isle of Wight in St Mary’s Hospital or its outlying units, will be asked to complete a patient experience survey titled ‘Getting it Right’ at the time of their discharge from their episode of inpatient care. The surveys will be collected on a weekly basis to ensure we are capturing real time data. A written report will be available to each clinical area at the beginning of the following month showing the previous months feedback, wards will be asked to review their individual data and also display the results in a public area of the ward. Any key concerns will be raised with the ward immediately and will not wait for the next formal reporting period. Using real time data will mean that the ward areas will be able to have greater confidence and connection with the feedback, thus leading to more effective action to address any concerns in a timelier manner. The pilot of the ‘Getting it Right’ survey during January to March 2010 involving over 300 patients has indicated that almost 90% patients are either very satisfied or satisfied with the care they received. Outpatient areas will also be asked to participate in the survey on a monthly basis, with all outpatients being asked to complete a survey on a designated day each month during clinics, with results being provided back to the area within a week of undertaking the survey. Monitoring and Measurement of Progress: The Getting it Right survey has one key measure: • During 2010 / 2011 the PCT aim to receive positive feedback from 95% of patients surveyed on their experience of our services, with at least 50% inpatients surveyed The data from the survey will be presented to the board on a monthly basis as part of the quality report presented by the Chief Nurse / Director of Infection Prevention Control. 14 2.2 Statements of Assurance from the Board Relating to the Quality of NHS Services Provided 2.2.1 Review of Services During 2009/10 NHS Isle of Wight provided and/or sub-contracted 81 NHS services. The NHS Isle of Wight has reviewed all the data available to them on the quality of care in 66 of these NHS Services. The income generated by the NHS services reviewed in 2009/10 represents 45% of the total income generated from the provision of NHS Services by the NHS Isle of Wight for 2009/10. All departments were asked to verify and submit data supporting the quality of care within their services during 2009/10 to support the application for registration with the Care Quality Commission. This assessment took into account the 16 quality and safety standards set out by the Care Quality Commission. During 2010/11 this assessment tool will be developed further to provide the Board of NHS Isle of Wight that all Provider Services, at all locations, are monitoring their levels of compliance with the essential standards of quality and safety and taking appropriate action to address issues where necessary. The Service Delivery Executive Board and the four Clinical Directorate Boards are responsible for overseeing these assessments and acting on the results. 2.2.2 Participation in Clinical Audits During 2009/10, 22 national clinical audits and 6 national confidential enquiries covered NHS services that Isle of Wight NHS Primary Care Trust provides. During that period Isle of Wight NHS Primary Care Trust participated in 77% national clinical audits and 100% of national confidential enquiries of the national clinical audits and national confidential enquiries which it was eligible to participate in. The national clinical audits and national confidential enquiries that Isle of Wight NHS Primary Care Trust was eligible to participate in during 2009/10 are as follows: National Neonatal audit programme (NNAP) National Diabetes Audit Intensive Care National Audit and Research Centre (ICNARC) Case Mix Programme adult critical care units National Elective Surgery Patient Reported Outcome Measures (PROMS): four operations – hip replacement, knee replacement, hernia, and varicose veins Centre for Maternal and Child Enquiries (CEMACH): Perinatal Mortality National Joint Registry(NJR): hip and knee replacements National Lung Cancer Audit (NLCA). National Bowel Cancer Audit Programme (NBOCAP) Myocardial Infarction Audit Project (MINAP)(inc ambulance care): AMI & other ACS Heart Failure Audit Pulmonary Hypertension Audit National Hip Fracture Database: hip fracture National Audit of Psychological Therapies for Anxiety and Depression (NAPTAD) Trauma Audit and Research Network (TARN): severe trauma National Kidney Care Audit National Falls and Bone Health Audit National Prescribing Observatory for Mental Health (POMH): prescribing topics in mental health services National Comparative Audit of Blood Transfusion: Blood Issue British Thoracic Society: respiratory disease College of Emergency Medicine: Pain in children, asthma and fractured neck of femur 15 National Mastectomy and Breast Reconstruction Audit National Oesophago-gastric Cancer Audit Royal College of Physicians Continence Care Audit National Confidential Enquiry into Patient Outcome and Death (NCEPOD): Parenteral Nutrition NCEPOD: Acute Kidney Injury (AKI) Study NCEPOD: Surgery in the elderly study Centre for Maternal and Child Enquiries (CMACE): Head Injury in Children National Confidential Inquiry (NCI) into Suicide and Homicide by People with Mental Illness (NCI/NCISH) (Not directly – request via coroner to consultant if applicable) The national clinical audits and national confidential enquiries that Isle of Wight NHS Primary Care Trust participated in during 2009/10 are as follows:• • • • • • • • • • • • • • • • • • • • • • • National Neonatal audit programme (NNAP) National Diabetes Audit Intensive Care National Audit and Research Centre (ICNARC) Case Mix Programme adult critical care units National Elective Surgery Patient Reported Outcome Measures (PROMS): four operations:– o hip replacement o knee replacement o hernia o varicose veins (not applicable as not done locally) Centre for Maternal and Child Enquiries (CEMACH): Perinatal Mortality National Joint Registry(NJR): hip and knee replacements National Lung Cancer Audit (NLCA). National Bowel Cancer Audit Programme (NBOCAP) Myocardial Infarction Audit Project (MINAP)(inc ambulance care): AMI & other ACS National Hip Fracture Database: hip fracture Trauma Audit and Research Network (TARN): severe trauma Heart Failure National Comparative Audit of Blood Transfusion: Blood Issue British Thoracic Society: respiratory disease College of Emergency Medicine: Pain in children, Asthma and fractured neck of femur National Mastectomy and Breast Reconstruction Audit National Oesophago-gastric Cancer Audit Royal College of Physicians Continence Care Audit National Confidential Enquiry into Patient Outcome and Death (NCEPOD): Parenteral Nutrition NCEPOD: Acute Kidney Injury (AKI) Study NCEPOD: Surgery in the elderly study Centre for Maternal and Child Enquiries (CMACE): Head Injury in Children National Confidential Inquiry (NCI) into Suicide and Homicide by People with Mental Illness (NCI/NCISH) The national clinical audits and national confidential enquiries that Isle of Wight NHS Primary Care Trust participated in, and for which data collection was completed during 2009/10 are listed below alongside the number of cases submitted to each audit or enquiry as a percentage of the number of registered cases required by the terms of that audit or enquiry. 16 Audit Percentage of cases submitted to each audit 100% National Neo-natal audit programme (NNAP) National Diabetes Audit Intensive Care National Audit and Research Centre (ICNARC) Case Mix Programme adult critical care units National Elective Surgery Patient Reported Outcome Measures (PROMS): four operations* • hip replacement • knee replacement • hernia • varicose veins Centre for Maternal and Child Enquiries (CMACE): Peri-natal Mortality National Joint Registry(NJR): hip and knee replacements Data collection for 2009/10 not due until June 2010 100% Cumulative and for the period April to November 98.8% 107.1% 72.5% Not applicable 100% 100% National Lung Cancer Audit (NLCA) 80% National Bowel Cancer Audit Programme (NBOCAP) 70% Myocardial Infarction Audit Project (MINAP)(inc ambulance care): AMI & other ACS National Hip Fracture Database: hip fracture 100% Trauma Audit and Research Network (TARN): severe trauma 98% (from Oct 2009) 90% Heart Failure 70% National Comparative Audit of Blood Transfusion: Blood Issue 100% British Thoracic Society: respiratory disease 73% College of Emergency Medicine: • Pain in children • Asthma • Fractured neck of femur National Mastectomy and Breast Reconstruction Audit 100% 0% 0% 100% National Oesophago-gastric Cancer Audit 100% Royal College of Physicians Continence Care Audit 100% National Confidential Enquiry into Patient Outcome and Death (NCEPOD): Parenteral Nutrition NCEPOD: Acute Kidney Injury (AKI) Study 48% NCEPOD: Surgery in the elderly study 70% Centre for Maternal and Child Enquiries (CMACE): Head Injury in Children National Confidential Inquiry (NCI) into Suicide and Homicide by People with Mental Illness (NCI/NCISH) 100% 50% 100%. NHS Isle of Wight expects a minimum of 90% of eligible cases to be submitted to each audit, though it is recognised that this may not always be possible. During 2009/10 NHS Isle of Wight achieved 61% compliance with this requirement. Small numbers can mean compliance rates are artificially low for NHS Isle of Wight, for example the NCEPOD Acute Kidney Injury study had only 2 cases fitting the entry criteria in 2009/10. 17 The reports of 5 national clinical audits were reviewed by the Provider Services in 2009 / 10 and Isle of Wight NHS Primary Care Trust intends to take the following actions to improve the quality of healthcare provided • • • • Develop a single point of access for stroke patients Review of the documentation and care delivery to support ‘End of Life’ Care Review the delivery of thrombolysis in A & E following review of MINAP data. Introduction of multidisciplinary therapy in community for stroke patients. The reports of 19 local clinical audits were reviewed by the Provider Services in 2009/10 and Isle of Wight NHS Primary Care Trust intends to take the following actions to improve the quality of healthcare provided. • • • • • Improve the quality of patient information leaflets and increase subjects to cover lack in identified areas Update policies to ensure that a robust consent process is place for patients undergoing invasive procedures as part of breast screening process Introduction of monthly joint diabetes/maternity clinic to support patient care Review of the documentation within Mental Health Services to ensure Physical assessments are undertaken on all inpatients Review the clinical audit process within the PCT and improve local training by updating the audit policy, reviewing the training available to staff, and ensuring that results of audits are reported at appropriate trust committees. In order to reinvigorate audit the Primary Care Trust has been challenged by the Audit Committee to ensure that a robust annual audit programme is in place for each clinical directorate that focuses primarily on the national audit programme and that the findings and recommendations from audit are reviewed and appropriate actions taken to improve the quality of healthcare provided. The Medical Director and Chief Nurse have taken a key role in this process. Copies of audit results can be accessed by contacting the Quality Team, c/o Communications Team, NHS Isle of Wight, St Marys Hospital, Parkhurst Road, Newport, Isle of Wight PO30 5TG or via email from comms@iow.nhs.uk 18 2.2.3 Participation in Clinical Research The number of patients receiving NHS services provided or sub-contracted by NHS Isle of Wight in 2009/10 that were recruited during that period to participate in research approved by a research ethics committee was 1031. The Research & Development Committee continues to receive research proposals for approval from both primary and secondary care professionals. A further 52 studies have been granted research governance approval since April 2009, an increase of 44% from the previous year, which have included a mix of mainly multi-centre non-commercial externally funded projects and projects associated with postgraduate education studies. A central annual allocation of £304,612 was made available to the PCT by the Hampshire & Isle of Wight Comprehensive Local Research Network to provide NHS infrastructure support to studies within the National Institute for Health Research Clinical Research Network (NIHR CRN) Portfolio, which covers clinician sessions, research nurses and associated staff, NHS service support (pathology, radiology & pharmacy) and research management and governance. The Central South Coast Cancer Research Network formally monitored 15 cancer research studies currently open to recruitment at St Mary's Hospital, in accordance with the Research Governance Framework for Health & Social Care. The Research Passport Scheme was fully implemented from 31 August 2009. This national scheme streamlines procedures associated with issuing honorary research contracts or letters of access to researchers who have no contractual arrangements with NHS organisations who host research, and who carry out research in the NHS that affects patient care, or requires access to NHS facilities. 2.2.4 Goals Agreed with Commissioners A proportion of NHS Isle of Wight’s Provider Services income in 2009/10 was conditional on achieving quality improvement and innovation goals agreed between NHS Isle of Wight and any person or body they entered into a contract, agreement or arrangement with for the provision of NHS services, through Commissioning for Quality and Innovation payment framework. Further details of the agreed goals for 2009/10 and for the following 12 month period are available on request from the Quality Team, c/o Communications Team, NHS Isle of Wight, St. Mary’s Hospital, Parkhurst Road, Newport, Isle of Wight PO30 5TG or via email from comms@iow.nhs.uk A summary of CQUINs for 2009/10 can be found in appendix 1 19 2.2.5 What Others Say about the Provider Services Statements from the Care Quality Commission The NHS Isle of Wight is required to register with the Care Quality Commission (CQC) and its current registration status is registered without compliance conditions. The Care Quality Commission has not taken enforcement action against NHS Isle of Wight during 2009/10. NHS Isle of Wight is not subject to periodic reviews by the CQC. NHS Isle of Wight has participated in special reviews or investigations by the Care Quality Commission relating to the following areas during 2009/10. There were three unannounced visits relating to healthcare associated infection and compliance with the Health and Social Care Act by the CQC, two relating to the Ambulance Service and one relating to acute hospital services. The condition relating to the ambulance service was that the registered service provider must demonstrate that plans for ambulance cleaning, based on national guidance, are adequately resourced and implemented by 31 October 2009. The condition relating to acute services was the trust must ensure it uses effective arrangements for the decontamination of instruments and other equipment and these should be detailed in appropriate policies. The trust must take immediate action to address the issues raised. The trust must have addressed the area for improvement by 30 January 2010. NHS Isle of Wight took the following action to address the conclusions or requirements reported by the CQC. Ambulance Service The cleanliness team for the ambulance service has been in place since July 2009 and during the unannounced inspection by the Care Quality Commission on 10th September they identified weaknesses in the robustness of the new system. Issues identified included • There was no evidence that there was a system in place to ensure that ambulances would be deep cleaned each month • There was no evidence that there was a system in place to ensure that daily cleaning of ambulances had been completed • Despite all vehicles having undergone at least one deep clean and a protocol for daily cleaning, four vehicles were found to be insufficiently clean. • Clinical waste was stored inappropriately on 2 vehicles Following the inspection work was undertaken to strengthen these areas. A system to allow identification of when each ambulance has been deep cleaned has been put in place and that system also identifies the next date the vehicle is due to be deep cleaned. The cleanliness team and ambulance service have access to the system and if for any reason the vehicle is not deep cleaned e.g. it is being serviced, then it is rescheduled as a priority for deep cleaning A new directive has been issued to all ambulance crews advising that clinical waste must not be stored in the vehicles and disposed of either when attending A&E or when arriving back at the ambulance station. Acute Services The store cupboard on the Medical Assessment unit has been adapted and a separate store for food has been created so it can be kept separate from clinical items All mattresses found to be affected on the day of the inspection were replaced and a requirement that all mattresses are checked daily when the bed is made was put in place. A record of the check is recorded and held at ward level. 20 Since the unannounced visit the Chief Nurse/DIPC and Infection Prevention and Control Clinical Nurse Specialist have been undertaking checks of mattresses and, on only one occasion shortly after the introduction of the new scheme was a mattress found to have staining on the underside cover and this was due to staff not being clear on what to check for. Additional training was provided to staff on that ward to support checking. The NPSA alert and the colour poster has been issued to all wards so they are clear about what to check for A bed space checklist has been introduced on all wards and at the head of the bed a patient being admitted can see that a named nurse (the nurse is required to sign the checklist) has prepared and checked that the bed space is clean and meeting the required cleanliness standards. During the visits by the DIPC and Infection Control Clinical Nurse Specialist work has been ongoing to help ward staff refine the use of the checklist, a standard operating procedure has been developed for preparing a bed space and enhanced training is being delivered to ensure staff are able to meet the required standard. On the unannounced visits carried out on 28th January 2010 by the Chief Nurse/DIPC and Infection Prevention and Control Clinical Specialist no brown stains or blood splashes were seen on 6 beds that were inspected. (MAAU 3 beds, Whippingham 2 beds and Stroke Unit 1 bed) An audit was carried out to determine how many drip stands required replacement and an order for 75 was placed on 23rd December 2009, the delivery is expected imminently. As many drip stands that were in poor condition as possible have already been condemned and removed from the wards. This will be reviewed again to ensure all old ones are removed when the delivery of new stands arrives. 10 of the new drip stands have now arrived and are in use, a further 65 were delivered in the week commencing 22nd February 2010 A shower chair has been removed and condemned and a replacement has been obtained. NHS Isle of Wight has made the following progress by 31st March 2010 in taking such action. The CQC have now confirmed that there are no conditions of registration relating firstly to Healthcare Associated Infection for the Ambulance Service from 14th December 2009 and secondly for Acute Services from 17th February 2010 Annual Healthcheck The results of the 2008/09 Annual Healthcheck relating to NHS Isle of Wight can be found in appendix 2 21 2.2.6 Data Quality i) NHS Number and General Medical Practice Code Validity The NHS Isle of Wight submitted records during 2009/10 to the Secondary Uses service for inclusion in the Hospital Episode Statistics which are included in the latest published data. The percentage of records in the published data: - which included the patient’s valid NHS Number was: 98.1% for admitted patient care; 99.3% for out patient care; and 96.8% for accident and emergency care. - which included the patient’s valid General Practitioner Registration Code was: 100% for admitted patient care; 100% for out patient care; and 99.9% for accident and emergency care. ii) Information Governance Toolkit Attainment Levels The NHS Isle of Wight’s score for 2009/10 for Information Quality and Records Management, assessed using the Information Governance Toolkit was 85%. iii) Clinical Coding Error Rate The NHS Isle of Wight was subject to the Payment by Results clinical coding audit during the reporting period by the Audit Commission and the error rates reported in the latest published audit for that period for diagnoses and treatment coding (clinical coding) were:Primary diagnosis incorrect – 9.3% Secondary diagnosis incorrect – 6.8% Primary procedures incorrect – 3.3% Secondary procedures incorrect – 3.2% 22 PART 3: OTHER INFORMATION 3.1 Review of Quality Performance PATIENT SAFETY 3.1.1 Infection Control and Cleanliness During 2009/10 NHS Isle of Wight has continued its focus on reducing the incidence of healthcare associated infections towards zero in line with the national direction. This has included the introduction of MRSA screening for all elective admissions and developing the plans to roll this out to all emergency admissions during 2010. Numbers of MRSA bacteraemia (blood stream) infections have remained low, with only two patients developing this blood stream infection after admission, compared with four in 2008/09. The work in this area has focused on improving blood culture collection technique, MRSA screening, maintaining high standards of hand hygiene and improving the care of peripheral venous access devices (a cannula or needle entering a vein to provide fluid or medication) MRSA rates A similar picture is presented with the number of Clostridium difficile cases occurring whilst the person was an inpatient at St Mary’s Hospital, initially numbers during 2009/10 were higher than in 2008/09 but this situation reversed in September/October 2009 and the numbers of cases remained low even over the more challenging winter months of 2009/10. 23 PCT Prison Healthcare Inpatient Healthcare Unit, Albany site HMP Isle of Wight The Unit opened at the end of October 2009 and replaced very poor and outdated facilities at the Parkhurst site of HMP Isle of Wight. Although owned by the Prison Service and located within a prison environment, NHS Isle of Wight manages the Unit and provides a developing inpatient service to prisoners under a recently signed Partnership Agreement. Agreement was reached at an early stage that the new purpose built facility would be subject to the same PEAT standards as mainstream NHS facilities and additionally, the cleaning of the Unit is fully the responsibility of the PCT. This is undertaken by PCT employed Cleanliness Assistants. The Unit is subject to inspections by the PCT’s Infection Control Specialist Nurses, with day to day responsibility for cleanliness standards and audits within the remits of the Prison Healthcare Modern Matron and the Unit Team Leader. Further work is planned with HMP Isle of Wight partners during 2010/1 to bring the three Prison Primary Healthcare Centres on the three HMP Isle of Wight sites within the same arrangements for cleaning by the PCT. Hand Hygiene Hand hygiene is one of the most important factors in preventing the transmission of infection. There is clear evidence that consistent and rigorous application of good hand hygiene practice will prevent healthcare associated infection. It is essential that hand hygiene practice standards are consistently high and complied with by all healthcare staff (Hand Hygiene Policy 2008). Hand Hygiene Audits that have not achieved the required 90% compliance rating have been scrutinised by the Modern Matrons and Ward Sister for the area to ascertain causes of non compliance. This has resulted in the production of action plans by Ward Sisters and their teams which are reviewed on a daily basis by the Modern Matrons. Ward based Mandatory Hand Hygiene Training via Trainer Tracker is now Trust Wide with further training days identified. 24 Care Quality Commission Unannounced Visits Ambulance Service The Ambulance Service was subject to two unannounced visits during 2009/10 by the Care Quality Commission as outlined in section 2.2.5 of this report. The staff working in the Ambulance Service and the Cleanliness Team were extremely proactive in responding to the concerns raised by the Care Quality Commission, so much that on the second unannounced visit, the assessors could find no problems with the cleanliness of the vehicles and complemented the team on the efficiency of the cleaning service that had been implemented. Acute Services This took place in December 2009 and highlighted areas of concern as outlined in section 2.2.5 of this report. The areas of concern identified by the Care Quality Commission visit resulted in the development of an action plan by the Chief Nurse and Director of Infection Prevention and Control. The Modern Matrons led on implementation at ward level with ward sisters and teams. The following actions having successfully been implemented: • • • • • Mattress condition audits undertaken daily by ward staff and overseen by Matrons Introduction of disposable curtains across all critical inpatient areas, main theatre and day surgery. Bed space check lists have been introduced to all inpatient areas. These are located at every bed space to address cleanliness of bed space furnishings and associated equipment and are available for inspection by the patient on arrival in the ward Ensuring compliance with Peripheral Venous Access Device Policy by all nursing and medical staff. Care plans have been made more visible with the utilisation of coloured care plans/assessment charts to support clear decision making and documentation. Priorities for Improvement 2010/11 Providing a clean, safe environment remains an important priority. Modern Matrons, the Hotel Services Manager and associated teams are working collaboratively to drive up and maintain high cleanliness standards across all the inpatient wards. Further work is planned with community and ambulance services during 2010/11 to ensure the high standards we have come to expect on inpatient wards are fully implemented in these other settings. We aim to continue to audit our performance, actively manage any concerns identified and further improve standards of cleanliness and patient safety on the wards. 3.1.2 Falls Falls are one of the main causes of incidents within NHS Isle of Wight and are monitored at a range of committee across the organisation including at public board meetings via the quality section of the Performance Report. The National Service Framework (NSF) for Older People (DOH 2001) dedicated standard six to the prevention and management of older people who are at risk of falling or who have experienced falls in their every day environment. In 2009/10 the Trust developed a number of strategies to prevent falls, improve reporting mechanisms and reduce the number of injuries that arise from falls. During 2009/10 the number of patient suffering serious harm as a result of a fall has seen a significant improvement, with no patients experiencing this type of injury in the last 5 months of the year 25 Numbers of patients by month who sustained a serious injury as a result of a fall in 2009/10 Number of Patients 3 2 1 March February January December November October September August July June May April 0 Identified Areas of Improvement during 2009/10 • Introduction of a combined falls and manual handling risk assessment tool. Training of clinical staff delivered through annual manual handling training • Improving monitoring of patients identified as being at high risk of falling using Sensorcare Falls Prevention Systems1 and CCTV in areas of low visibility. • Environmental audits reviewing and improving the accessibility of toilets / commodes. • De-cluttering the ward environment with particular focus on the patient’s bedside utilising the concept of the Productive Ward Initiative. • Ensuring patients and carers provided appropriate footwear for patients, particularly in areas of high risk, i.e. rehabilitation wards. • Improving care delivered after a fall to prevent further recurrence, sharing learning across the Trust. • Attention to medication ensuring that appropriate medication at the right time. • Improving reporting mechanisms through a central DATIX system; and development of the Productive Ward key performance indicator. • Auditing using the Global Trigger Tool2 methodology. • All harm resulting from a fall resulted in a Serious Untoward Incident Investigation and subsequent recommendations were taken forward. • Improving working with allied health professionals, particularly physiotherapists, in carrying out risk assessments and the subsequent management of falls. 1. The SensorCare Falls Prevention System. Mobility is an important part of everyone’s quality of life. However for the vulnerable, vacating a bed or chair unassisted can mean that unnecessary risks and dangers exist. Using the latest technology the SensorCare System provides an early warning that alerts the carer that mobilisation is being initiated, thus enabling appropriate attention to be given. The SensorCare Falls Prevention System was interfaced to the existing nurse call systems on the wards. 2. Global Trigger Tool In 2008/09 the Trust began to introduce the Global Trigger Tool (GTT). This is an internationallyrecognised method of audit of patients’ notes in order systematically to identify sources of harm. A number of staff have now been trained in the method and monthly audits are undertaken routinely. The initial results have been compiled and will provide the basis for tracking our progress. The first 26 end of year report has demonstrated that falls are the second highest event in the Trust; 20 events (13%) were recorded patient falls. Further Improvements Identified Participation in a national research project called ‘Hip Hop Flooring’ this is study looking at a type of flooring that could result in reduced harm from falling. 27 CLINICAL EFFECTIVENESS 3.1.3 Human Papilloma Virus (HPV) Delivery Programme The Human Papilloma Virus (HPV) is the name of a family of viruses that affect the skin and the moist membranes that line your body, such as those in your cervix, anus, mouth and throat. These membranes are called the mucosa. There are more than 100 different types of HPV viruses, with about 40 types affecting the genital area. Infection with some types of HPV can cause abnormal tissue growth and other changes to cells, which can lead to cervical cancer and infection with other forms of HPV can also cause genital warts. Other types of HPV infection can cause minor problems, such as common skin warts and verrucas. The infection is also linked to vaginal cancer and vulval cancer, although both are rare conditions. In the UK, cervical cancer is the twelfth most common women's cancer. Worldwide, it is the second most common. In the UK, a woman's lifetime risk of developing cervical cancer is about one in 116 (0.86%). Cancer of the cervix usually takes 10-20 years to develop. In the UK, more than 1,000 women die from cervical cancer each year. In October 2007, the Department of Health announced the introduction of a funded HPV immunisation programme from September 2008. The routine programme includes girls in school year 8, typically aged 12 years, this immunisation programme will be undertaken year in year out and is undertaken by the School Nurses, a national target of 90% coverage for the routine programme by 2010/11 has been set. In addition to the routine programme there were three catch up programmes running through 2009/10 and 2010/11 for girls/and young women between the ages of 15-18 (in academic year . On the Isle of Wight School Nurses immunised the girls aged 14-16 i.e. years 10 and 11 (typically referred to as the 'Accelerated Catch Up' campaign) and the GPs immunised the young women aged 16-18 age range. (Typically referred to as the 'Catch Up' Campaign) The routine programme consists of 3 separate doses of the HPV vaccine which is administered to girls in school (16 middle schools) approximately cohort 805 which equates to having to provide 2415 vaccinations over 16 sites in addition to this are the girls in Private and Special Schools. The accelerated programme undertaken by the School Nursing Team also consisted of three separate doses across 5 High schools, the private and special schools; the cohort for this was 1607 girls which equates to 4821 vaccinations across the different sites. Prior to the implementation of the HPV programme a sound knowledge base was developed by the School Nursing Team and the Team leader attended the implementation meetings together with Public Health. A specific written instruction for the supply and administration of named medicines known as a Patient Group Directive (PGD) was developed. Specific training was developed and provided to the team who would be involved in service. Numbers of girls eligible for the vaccine was obtained from the Local Authority and a data base was developed for recording and monitoring purposes. A timetable was planned to run over one calendar month per dose visiting each Middle School between 08.30hrs to 11.00hrs to deliver the vaccine allowing five minutes per injection and allocating the number of Nurses and Support staff according to the number of girls. The time also included setting up and administration work and time to allow for any girls who may have had immediate reaction to the vaccine. Each School was visited the following week to catch any girls who may have been absent therefore enabling them to access the second dose alongside their peers. The timetables were sent out to all schools for approval which fortunately highlighted an issue for the one of doses being administered when SATS tests were due therefore the Team Leader was able to reschedule all schools a week later so timetables were revised and sent again, this meant there was no impact on either the academic or the vaccination timetable. 28 Letters were delivered to the schools for the girls with consent cards. These were then collected by school and a simple alphabetical system was put in place, the School keeps the cards until all 3 doses have been administered. A national media campaign was launched by the DOH and coverage for the first year 8 eligible cohort of 805 was 92% 1st dose, 91% 2nd dose and 90% 3rd dose. The catch up programme has run similarly for the year 10 and 11 girls attending high school and for the first dose we achieved 82.5% for year 10 and 80.1% for year 11. The media campaign was not continued into the second year. The Data for 2009/10 is currently being verified, early indicators suggest that there has been a slight dip in ‘take up’ of the vaccine however the Isle of Wight compares very favourably with other Trusts within the SHA., see the graph below outlining vaccination rates HPV Immunisation among Girls aged 12-13: Coverage in 2008-09 and 2009-10 (up to end Nov 2009) % of girls immunised England South Central SHA Isle of Wight Target 100% 80% 60% 40% 20% 0% Dose 1 Doses 1 & 2 Doses 1,2,3 2008-09 Dose 1 Doses 1 & 2 Doses 1,2,3 2009-10 To Date 3.1.4 Quality in Endoscopy Joint Advisory Group (JAG) accreditation is a national initiative that is designed to ensure that the safety of patients undergoing endoscopy is of primary importance. The five yearly assessment is undertaken to back up the six monthly returns that are made via the Global Rating Scale assessment. The Endoscopy Unit at St Mary’s was awarded unconditional accreditation in July 2009. This reflects the work undertaken by clinical, managerial and administrative teams to become compliant to nationally recognised standards. The Global Rating Scale is a tool that enables units to assess how well they provide a patient-centred service. It is a web-based assessment tool that makes a series of statements requiring a yes or no answer. From the answers it automatically calculates the Global Rating Scale scores, which provides a summary view of your service. These self assessments are completed in April and October of each year. To ensure compliance and to check that data entry can be verified a small number of trusts are required to submit written evidence. The Global Rating Scale results are shown below for the last 3 years and show continual improvement in patient safety over that time. The graphs following outline the performance of the Endoscopy Unit. The descriptors begin to create a more complete picture of what is going on by describing in words different levels of achievement for an item. These levels vary from basic (D) to excellent (A). 29 30 Other initiatives within the Endoscopy Unit include: • An ongoing quarterly audit that looks at safety issues, such as sedation rates, completion rates, and morbidity and mortality rates. These are then fed back and discussed with action plans formulated to address areas of concern. • An ongoing patient survey of patients who have had an endoscopy. One patient in four is sent an anonymous questionnaire by the clinical governance unit. The results are collated and any themes or obvious problems are discussed with in the unit along with a method of solving them. These surveys are available on request from the JAG/Global Rating Scale Coordinator for the unit. 31 • Nurse led consent is gradually being rolled out across the department. This streamlines the admission process and ensures consistency in the consent process. The ward manager is personally training and assessing the staff. • The Scorpio system in endoscopy allows for patient data and clinician activity to be recorded. This electronic system is also useful for capturing photographs of pathology which can then be accessed at the twice weekly Multi-disciplinary Team meetings. It also allows for comparison of disease progress or healing. It also allows patients to be booked onto the system for surveillance and follow up – this ensures no patients are missed from the system. 3.1.5 Mortality During 2009/10 NHS Isle of Wight has started to develop mechanisms to monitor mortality ratios across the inpatient services provided at St Mary’s Hospital. The most recently published mortality ratio for St Mary’s Hospital is 102.09 a reduction on the figures published in December 2009 indicating a rate of 103.76. Both of these ratios published by Dr Foster Intelligence are within the nationally expected performance for this type of NHS organisation and will be reported each month in the NHS Isle of Wight performance report during 2010/11. 32 PATIENT EXPERIENCE 3.1.6 Relocation of the Neo-natal Intensive care Unit The Neonatal Unit was relocated on the 23rd September 2009 from the lower ground level to be on the same level as the Maternity and the Labour Ward, following an extensive refurbishment plan costing £1,104,803. Prior to this relocation the unit was in a cramped space on the ground floor and created an unnecessary distance between mother and newborn baby. The unit was often required to exceed its capacity due to pressures of wanting to keep neonates in the local unit rather than transferring them to the mainland and possibly adding further separation from the parents and siblings. The new unit is light and airy and painted in calming relaxing colours that provide a welcoming feel to the unit. For the baby the new unit has provided larger bed spaces where their Parents can work alongside the staff to provide all aspects of care that they need. Curtained Cot spaces mean that the baby can have privacy and special time with their parents. For the parents, in particular the mothers that are in-patients on the Maternity unit, the move has meant that their baby is only a few steps along the corridor (sometimes only next door if the mother is in the last room on maternity). Previous to the relocation this would have been a long walk along the corridor and down in a lift that was not always reliable. At night this was often a bit frightening as the offices outside the old unit were closed overnight. The mother confined to her bed or in a wheelchair could not easily get to see her baby, especially if the lift was out of action. If in a bed, even if she could get to the unit, the mother could only look through the nursery window as the bed could not go into the nursery. The new unit has easy access for beds and wheelchairs and mothers can be wheeled right next to their baby. Talking to parents who have had a previous premature baby in the old unit and are now experiencing having a second premature baby in the new unit are amazed at the difference. The main comments are: “There is so much space”. “It is so light and airy”. “I don’t feel so separated from my baby” A letter received from a set of parents stated that “Our baby was fortunate enough to be one of the first babies to be moved into the impressive new unit during her stay. However, despite the state-ofthe-art clinical surroundings and fabulous new equipment, it has to be said that the new unit has lost none of the warm, caring atmosphere of the old one”. Today the neonatal staff can move easily between NICU and the Maternity floor to provide some aspects of Special Care to the baby at their mothers’ bedside. This has enabled some of these vulnerable babies and mothers to stay together on Maternity strengthening parent/infant attachment. After leaving the unit most babies need to be seen for follow up care. In the old unit patients waited in an overcrowded corridor. They were then examined in the unit dayroom (which was then not available for anyone else on the unit). The new unit has a designated waiting area with access to play facilities for siblings and a proper outpatient room with everything required. The whole experience from admission to discharge for these little patients and their parents has been greatly improved with the relocation to this new Neonatal Unit. 33 3.1.7 Patient Experience in Mental Health 2009/2010 was a productive year for the Mental Health and Learning Disability Directorate. The service has benefited from a range of quality initiatives across the directorate and picked up a number of prizes at the Island’s annual NHS awards scheme and Wight Mind Awards for the quality of its services. Adult mental health services have made steady progress in addressing recommendations from an external review commissioned in the previous year. Improvements include improving the ease of access to services to patients presenting in crisis, implementing tools to measure people’s recovery, making the ward and community team environments more pleasant and therapeutic and introducing more robust systems and procedures. Acute and Community Services We have carried out a range of welcome improvements to our inpatient and community-based facilities including improving privacy and dignity for patients, providing new equipment and improving the environment for patients and staff alike. The way we assess and support new adult patients has been redesigned and improved and we have carried out a review of adult rehabilitation services. This was focussed particularly on inpatient care and identified ways to enhance the service and reduce the number of people who have to travel to the mainland for care. In 2009/10 we have also trained significant numbers of staff to use the Health of the Nation Outcome Scores (HoNOS) system which helps us to measure whether or not people are getting better, this will be fully implemented in 2010/2011 because by measuring outcomes we can be clear on whether our interventions work. The active involvement of service users and carers in what we do is a high priority for us and we have established a user group for adults. We regularly involve service users in recruitment including young people and frequently undertake a number of service user satisfaction surveys. Service user satisfaction surveys will be expanded across key inpatient and community teams. This feedback will be used to change the service to make it better. We have invested heavily in our staff, improving communication, appraisal, training and professional development and have strengthened supervision for staff including those delivering psychological therapies to ensure the highest clinical standards and best treatment models are used. During the year we made progress on improving the care of people with personality disorders which will be further embedded this year. The Future Looking ahead, the coming year will see considerable efforts to improve quality and efficiency even further. This will include improving the way we care for people with dementia, help more people to be cared for at home and supporting the main acute hospital to care for people who have a mental health as well as physical health problem. We will also be establishing a new primary mental health care service for prisoners on the island and further enhance out-of-hours crisis support for adults. 3.1.8 Complaints and Compliments During 2009/10 reporting complaints data has become part of the NHS Isle of Wight Performance Report, focusing on the types of complaints received. The main areas of concern raised in complaints include • Clinical care – medical care, or concerns about diagnosis / treatment • Staff attitude – attitude or conduct of staff • Nursing care – quality of nursing care provided 34 • Concern over admission, discharge or transfer arrangements • Delays in appointments – both inpatient and outpatient. All complaints within NHS Isle of Wight are subject to investigation and review directly with the staff involved, with lessons learnt developed and shared within the relevant clinical area, During 2010/11 mechanisms will be established to ensure wider learning of lessons emerging from complaints The numbers of compliments about NHS Isle of Wight services continue to exceed complaints with on average 10 compliments for every formal complaint received 35 3.2 Explanation of who has been involved A diverse range of key stakeholders have been involved in the production of this Quality Account and have influenced content. Service users have been involved via the Patient’s Council, where 19 representatives were involved at an early stage. This patient group was also asked for comment at a later stage in the process. Staff involved in the production of the Quality Account are at all levels and from all Directorates within the organisation, both clinical and non clinical, via discussion at Departmental meetings. The staff group has included:• Chief Operating Officer • Chief Nurse • Chief Executive • Medical Director • Associate Directors (Medical, Elective, Child Family and Therapies, Access and Assessment and Mental Health and Learning Disabilities clinical directorates) • Clinical Directors • Heads of Clinical Services • Head of Ambulance Service • Consultants • Head of Governance and Assurance • Clinical Team Leaders / Heads of Service • General Managers • Ward Sisters/Leaders • Administrative and Clerical staff • Facilities Associate Director • Finance representatives • Governance Advisors • Modern Matrons • Human Resources representatives • Allied Health Professionals (Physiotherapy, Occupational Therapy, Dental, Speech and Language Therapy, Dietetics, Orthotics and Prosthetics, Radiology, Podiatry) • Midwives • School Nurses • Nursing staff at all levels (adult, mental health and paediatric, including hospital based and community based nurses) • Non Clinical Managers / Senior Managers • Specialist Nurses • Information Management representatives • Clinic Co-ordinator • Pharmacy representatives A dedicated group of staff have been involved in weekly Quality Account meetings, specifically designed to support the production process, the group has consisted of Chief Nurse, a senior representative from each clinical directorate (either Associate Director or Head of Clinical Services), a business and projects manager, provider quality manager, communications manager and an information analyst 36 3.3 Statement provided by Commissioning PCT, LINks or OSCs Commissioner Statement in response to the Provider Quality Account Isle of Wight NHS PCT Commissioners welcomed the opportunity to participate in the governance ‘sign-off’ process and provide a statement in response to the presented Quality Account. ‘The provider has developed a Quality Account which presents a broad overview of a wide range of quality improvement work being undertaken; the diversity of the organisation is reflected in the priorities chosen. The Commissioners acknowledge the challenges faced by the Provider when developing a Quality Account that would encompass Acute, Mental Health and Learning Disability, Community and Ambulance Services. Commissioners ensure that Provider contracts detail clear, quality outcomes that are expected from the Provider; the Quality Account appears to cover key areas of Commissioner interest. However, Commissioners wish to assure the Board that more detailed quality reporting is undertaken on a regular basis as part of the performance management of the Provider. We have recommended minor amendments and or refinements to some Monitoring Measurements; the Provider has agreed to make the suggested changes. Performance against CQUINS (Commissioning for Quality and Innovation Scheme) has been developed more so in 2010 -11 to incentivise the Provider to go further in achieving high quality services, rewarding additional effort and innovation. There is an expectation that subsequent Quality Reports would reflect such achievements associated with the CQUIN scheme. In addition we would expect to see the use of clinical audit data and outcomes more robustly demonstrated in the next Quality Account, together with a summary of progress under Clinical Effectiveness against National Service Frameworks (NSFs), National Institute for Clinical Effectiveness (NICE) guidance implementation, and Improving Outcomes Guidance. Commissioners, including representation from Practice Based Commissioning, would commend the Quality Report as a fair reflection of the Provider's achievement across the quality agenda and the high level of commitment and effort across a diverse organisation to constantly improve the quality of services provided. Statement by the Isle of Wight LINk The Isle of Wight LINk welcomes the opportunity to comment on the Isle of Wight NHS Quality Account and to provide the following statement in response to the completed document. Unfortunately, time constraints made it difficult to gain feedback from the wider LINk membership and the statement has been compiled with comments from the Stewardship group and a small focus group of LINk members. The Quality Account is a comprehensive and detailed document which accurately and effectively highlights the recorded achievements and improvements in the wide range of services provided over the past twelve months. The use of the three main areas of the report: Patient Safety; Clinical Effectiveness and Patient Experience has enabled the document to reflect the diversity of healthcare services and to identify the Trust’s main priorities for the coming year. The LINk is greatly encouraged by the successful consultation undertaken by the Trust which has resulted in expansion of the current ENT service to cover 24/7 day on call and a joint provision of this service with Portsmouth PCT. The LINk would welcome the opportunity to work with the Trust on future consultations. The Trust is to be congratulated for its continuing and successful work in the management and control of healthcare acquired infection rates, including the provision of a safe clean environment for patients. In addition, the LINk has continued to gather feedback from both its own participants and the wider public regarding health services on the Isle of Wight. The LINk has identified some specific themes or trends of concern expressed by Isle of Wight residents, some of which have been resolved, and 37 others which will be taken forward as part of the LINk future work plan, working with the Trust and other organisations to resolve. These are: • Discharge from Care • Dignity in Care • Transport access to health services • Communication The LINk welcomes the chosen priorities for 2010-2011, and in particular those for improvements in mental health services, and those where the patient experience (PROMS and Patient Surveys) is seen as a vital part of the monitoring and measurement process The LINk looks forward to working together with the Trust over the coming year utilising effective wider public consultation to ensure any service development meets identified need; effective service delivery is maintained, developing opportunities for public involvement in commissioning and that the high standard of services already provided by the Isle of Wight NHS continues to the benefit of the island population. The LINk membership feel that the Quality Account is an accurate reflection of the healthcare services provided and wish to congratulate the Trust on the achievements and improvements to services outlined in this document. Nancy Ellacott MBE, Chair, Isle of Wight LINk. Statement for inclusion in the NHS Isle of Wight Quality Account 2009/2011 The Isle of Wight Council’s Adult Social Care, Health & Housing Scrutiny Panel (acting in its capacity as the Health Overview & Scrutiny Committee) is of the view, based on the knowledge it has of the NHS Isle of Wight, that the Quality Account is a fair reflection of the healthcare services provided by NHS Isle of Wight. Cllr Margaret Webster, Chairman, 20 May 2010 Statement from the Patients Council The Patients Council welcomes the opportunity to comment on the Quality Account. We welcome the improvements demonstrated in NHS Isle of Wight’s 2009/10 Quality Account, and congratulate the Trust on the progress being made. We make specific comment as listed below: It is gratifying to note that following consultation on the reorganisation of the ENT service (para 2.1.4) our concerns on behalf of patients have been reflected in an improved service including 24/7 on-call. We have minor reservations regarding existing patients, but with the prospect of improved cross Solent travel arrangements for patients, it would seem that future patients will receive a far more ‘seamless’ service than has sometimes been the case in the past. • The Patients Council welcome the expansion of the ‘Getting it Right’ survey (para 2.1.7), especially the inclusion of outpatients. • We are concerned that two Island schools have chosen to opt out of the initiative to vaccinate Island Girls against HPV (para 3.1.3). We would urge the Public Health Department., working with the School Nursing Team, to revisit the outstanding schools and explore alternative ways of making this important programme available. We think it fatuous to include Choose and Book (para 3.1.4) as a measure of Quality Performance. Even with the reduced targets, we feel that undue effort is being wasted trying to achieve the unachievable. Island residents have an additional hurdle of crossing the Solent to get to alternative healthcare and the PCT receives no extra funding to acknowledge this. This target is distorting the otherwise admirable performance of NHS Isle of Wight. The Patients Council congratulates the NHS Isle of Wight on its achievement of ‘Excellent’ for quality of services and looks forward to working with it over the coming year. Mike Carr, Chair, Patients Council 38 3.4 How to Provide Feedback on the Account This important document sets out how we continue to improve the quality of the services we provide. Your Views on Quality We welcome your views and suggestions on our Quality Priorities for 2010/11 (LINK) We welcome feedback at any time on our Quality Account. This can be sent to Quality Account, c/o Communications Team, NHS Isle of Wight, St. Mary’s Hospital, Parkhurst Road, Newport, Isle of Wight PO30 5TG or emailed to comms@iow.nhs.uk You can read more about the national requirements for Quality Accounts on the Department of Health website. 39 Appendix 1 The Commissioning for Quality and Innovation Payment Framework for NHS Isle of Wight 2009/10 2009/10 was the first year of the NHS Commissioning for Quality and Innovation (CQUIN) Payment framework and was very much a learning process for both commissioners and providers. Some of the measures set were unachievable as they were not easily measurable and resulted in a small number not being achieved despite significant improvements being made in year. This included several with 100% targets which did not allow flexibility for situations where staff were absent for example due to long term sickness Although some indicators were not achieved in terms of reaching the required levels to secure the CQUIN payment, significant progress has been made in most areas to ensure these are delivered. Ambulance CQUIN indicator Production of Quality Improvement Plan to develop systems for monitoring and improving quality (working towards being in the top 10% of any national ambulance quality benchmarking; and 100% compliance with plan). Achievement Achieved Ambulance service to have plans in place and be fully compliant with the requirements of NPSA guidance on ambulance cleaning Achieved Acute CQUIN indicator Reduce the reported incidence of pressure ulcers developed in hospital from Q1 to Q4. Annual average achievement of 2% maximum Reduced morbidity and mortality from stroke - 90% of patients spending 100% of their admission on the stroke unit. 100% patients presenting with TIA are risk assessed and high risk patients treated within 24 hours. 100% pts admitted to hospital with a primary diagnosis of fractured proximal femur who are medically fit for surgery are operated on within 48 hrs of admission. Fully completed discharge - A sample of 100 discharges across medicine and surgical NEL show 100% completion compliance. Improved data collection and reporting of quality indicators and completion of Quality Account. Achievement Achieved Not achieved Achieved Partially achieved Partially achieved Achieved Community CQUIN indicator Personalised Care Planning - All relevant staff to have undertaken training by March 2010 to ensure that people with a long-term condition are offered a care plan by 2011 Child and Adult Safeguarding Awareness - All staff to have undertaken this training by 2010 Reduction in admissions of note of very high intensive users (VH IU) Community matrons and other community/specialist nurses to improve management of long-term conditions and hospital admissions by 30% this year. Delivery of minimum dataset - Timetable and agreed plan in place to ensure Provider can deliver the minimum dataset in line with National requirements Improved data collection and reporting - Improvement of all quality and performance indicators by 50% by March 2010. Training of Continuing Healthcare Case Managers - All case managers trained and undertaking reviews within agreed time frames 40 Achievement Not achieved Not achieved Not achieved Not achieved Not achieved Not achieved Mental Health CQUIN indicator Part A: Comparison of pre and post treatment HoNOS - "Successful completion of an effective intervention may be used as a proxy for a good outcome" Health and Social Care Information Centre. Part B: Comparison of pre and post treatment HoNOS65+ - "Successful completion of an effective intervention may be used as a proxy for a good outcome" Health and Social Care Information Centre Improvement in patient experience (10%+ year on year) - Patient satisfaction good proxy for outcome measurement in MH (80% alignment) Improve involvement of service users in decisions by 10%+ year on year Evidence that this is related to better outcomes Use a balanced scorecard - Many providers are already using these but not necessarily sharing data with commissioners Improve on staff survey by 10%+ year on year 41 Achievement Not achieved Achieved Achieved Not achieved Partially achieved Appendix 2 Care Quality Commission – Annual Healthcheck 2008/09 Performance Ratings for I.W. NHS Primary Care Trust 1. Top Line Results: (National picture for PCTs: Quality of Commissioning Weak/ Fair/ Good/ Excellent Quality of Financial Management Weak/ Fair/ Good/ 1.3% 46.1% 52.6% Excellent 0.0%) CQC comment on Quality of Finance result: “The NHS Isle of Wight has been given a score of fair for its quality of financial management as it has met the basic requirements in all areas of this assessment. Its arrangements are consistent with established guidance and are operating effectively” 2. Quality of Commissioning Results Meeting Core Standards Existing Targets National Priorities - Fully met Fully met Excellent Number of target indicators under-achieved = Number of target indicators failed (Compliant with all 44 standards) (All 14 indicators met) (19 of 23 indicators achieved) 4* = 0 * Reduction in cancer mortality rate in people aged under 75 Status/action plan for 2009/10: Cancer LIT. Implementing the bowel cancer screening programme * Chlamydia screening Status/action plan for 2009/10: Plans in place to increase uptake and return of tests (involving college, GP practices, pharmacy and others) * Commissioning a comprehensive CAMHS Status/action plan for 2009/10: Identified PCT priority area. Covered in strategy for TCS to be completed by end October 2009 * Proportion of individuals who complete immunisation by recommended ages Status/action plan for 2009/10: Improving accuracy of computer systems and increasing options e.g. GP led health centres and possible use of community pharmacies 3. Quality of Provider Services Results Meeting Core Standards Partly met Existing Targets Fully met National Priorities Good Number of target indicators under-achieved = Number of target indicators failed * (Compliant with 41 of 44 standards) (11 of 13 indicators met) (17 of 23 indicators achieved) 7* = 1** Management of patients with cardiac arrest (ambulance service) Status/action plan for 2009/10: Requires participation in data collection audits in 2009/10 and may still be a resource issue as we need to establish clinical supervision in order to improve overall clinical performance of paramedics to the CPI targets 42 * Stroke Care target Status/action plan for 2009/10: Working on taking direct admissions from A&E. Improvement of stroke services is PCT priority. Two year project plan in place to include development of community stroke rehab team. * Cancelled operation and patients not admitted within 28 days Cancellation protocol in place and regular weekly Status/action plan for 2009/10: monitoring. 28 day rebook performance is good. * Time to reperfusion for patients who have had a heart attack (Thrombolysis) Status/action plan for 2009/10: Marginal underachievement for 2008/09 as achieved 67.7% against target of 68%. All breaches are reviewed by project team. * Completeness of Mental Health minimum data set Work to ensure robust and complete data for the Status/action plan for 2009/10: MHMDS is ongoing and regularly monitored. * Child and adolescent mental health services Status/action plan for 2009/10: Performance against KPIs being closely monitored. Improvement over last year’s scores is already evident. * Learning Disability (Green light toolkit) Status/action plan for 2009/10: Plans agreed between commissioner and provider to address the ‘amber’ requirements and to ensure full implementation. ** Care Programme Approach (CPA) 7 day follow up Status/action plan for 2009/10: Protocols now in place to address this and there is evidence of improved performance so far this year. 4. SUMMARY Meeting Core Standards As a commissioner As a provider * Note - Compliant with all 44 standards Compliant with 41 of 44 standards (Exceptions * - C4a/ C4c/ C21) - C4c Decontamination – compliant as of January 2009 - C4a/C21 Infection control/cleanliness – compliant as of October 2009 Meeting National Targets As a commissioner As a provider - Achieved Underachieved Failed Achieved Underachieved Failed 33 of 37 indicators 4 of 37 indicators 0 of 37 indicators 28 of 36 indicators 7 of 36 indicators 1 of 36 indicators In total 61 of 73 target indicators were achieved and only 1 failed for IW NHS PCT = “Excellent” – Best ever results for quality of services on Isle of Wight. NHS Isle of Wight one of only three PCTs in the country to achieve an ‘ excellent ‘ rating for quality of services in the 2008/9 annual healthcheck, and the only PCT to achieve this rating in NHS South Central. 43