Ambulation in simulated fractional gravity using lower body positive
advertisement

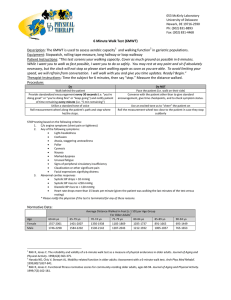
J Appl Physiol 101: 771–777, 2006. First published June 15, 2006; doi:10.1152/japplphysiol.00644.2005. Ambulation in simulated fractional gravity using lower body positive pressure: cardiovascular safety and gait analyses Adnan Cutuk,1 Eli R. Groppo,1 Edward J. Quigley,2 Klane W. White,1 Robert A. Pedowitz,1 and Alan R. Hargens1 1 University of California, San Diego, Department of Orthopaedic Surgery; and 2Children’s Hospital and Health Center, San Diego, Motion Analysis Laboratory, San Diego, California Submitted 31 May 2005; accepted in final form 18 May 2006 Cutuk, Adnan, Eli R. Groppo, Edward J. Quigley, Klane W. White, Robert A. Pedowitz, and Alan R. Hargens. Ambulation in simulated fractional gravity using lower body positive pressure: cardiovascular safety and gait analyses. J Appl Physiol 101: 771–777, 2006. First published June 15, 2006; doi:10.1152/japplphysiol.00644.2005.— The purpose of this study is to assess cardiovascular responses to lower body positive pressure (LBPP) and to examine the effects of LBPP unloading on gait mechanics during treadmill ambulation. We hypothesized that LBPP allows comfortable unloading of the body with minimal impact on the cardiovascular system and gait parameters. Fifteen healthy male and female subjects (22–55 yr) volunteered for the study. Nine underwent noninvasive cardiovascular studies while standing and ambulating upright in LBPP, and six completed a gait analysis protocol. During stance, heart rate decreased significantly from 83 ⫾ 3 beats/min in ambient pressure to 73 ⫾ 3 beats/min at 50 mmHg LBPP (P ⬍ 0.05). During ambulation in LBPP at 3 mph (1.34 m/s), heart rate decreased significantly from 99 ⫾ 4 beats/min in ambient pressure to 84 ⫾ 2 beats/min at 50 mmHg LBPP (P ⬍ 0.009). Blood pressure, brain oxygenation, blood flow velocity through the middle cerebral artery, and head skin microvascular blood flow did not change significantly with LBPP. As allowed by LBPP, ambulating at 60 and 20% body weight decreased ground reaction force (P ⬍ 0.05), whereas knee and ankle sagittal ranges of motion remained unaffected. In conclusion, ambulating in LBPP has no adverse impact on the systemic and head cardiovascular parameters while producing significant unweighting and minimal alterations in gait kinematics. Therefore, ambulating within LBPP is potentially a new and safe rehabilitation tool for patients to reduce loads on lower body musculoskeletal structures while preserving gait mechanics. exercise; cranial circulation; unloading; fractional body weight; ground reaction force; motion analysis; joint range of motion; stride length AFTER INJURY OR SURGERY to the lower extremities, patients are often unable to walk while supporting their entire body weight (BW). This may be due to pain, weakness, instability, or a requirement to protect surgically repaired tissues and implanted prostheses. However, immobilization causes muscle and bone loss, particularly in the lower limb (4). Furthermore, elderly patients are at heightened risk of injury or reinjury upon reambulation (8, 22). Because early mobilization and rehabilitation are highly desirable during the immediate postoperative period, elderly patients require the assistance of devices to decrease forces acting on the joints, bones, muscles, and ligaments of the lower extremities. Devices that are currently used for unloading of the lower extremities during rehabilita- Address for reprint requests and other correspondence: A. R. Hargens, Dept. of Orthopaedic Surgery, Univ. of California, San Diego, 350 Dickinson St. #121, MC 8894, San Diego, CA 92103-8894 (e-mail: ahargens@UCSD.edu). http://www. jap.org tion include walkers, parallel bars, therapist-assisted waist belts, overhead suspension harnesses, and swimming pools (1, 26). All of these have disadvantages associated with their use that interfere with patients’ rehabilitation and call for development of the novel rehabilitation techniques. Optimally, rehabilitation protocols should promote normal joint ranges of motion (ROMs) (30). However, many of the gait deviations observed in neurologically impaired patients result from their inability to bear weight adequately through their affected lower extremities during the loading phase of the gait cycle (5, 11, 34). A new device for loading and unloading lower extremities while walking and running has been developed by our laboratory (19). This device consists of a treadmill enclosed within a waist-high chamber. A seal is achieved between the patient and the chamber through the use of a neoprene kayak-type skirt that fastens over a lip in the aperture opening of the chamber. For unweighting, the pressure inside the chamber is increased above the external, ambient (atmospheric) pressure using an air compressor. This pressure differential causes an axial buoyant force that is proportional to the pressure differential multiplied by the cross-sectional area of the patient’s body at the waist seal (19), similar to a “piston effect.” The net ground reaction force (GRF) then becomes the difference between the patient’s weight and this axial force. In this way elderly and postsurgery patients can ambulate on the treadmill under simulated fractional gravity. Safety evaluation and studies of healthy individuals are necessary before the use of the LBPP rehabilitation concept by elderly patients with potential cardiovascular comorbidities. The purpose of this study is to 1) assess the impact of lower body positive pressure (LBPP) on the cardiovascular system, specifically on head perfusion, heart rate (HR), and blood pressure changes in healthy subjects standing and ambulating on a treadmill; and 2) examine the effects of LBPP unloading on gait mechanics during treadmill ambulation. We hypothesize that HR, blood pressure, brain blood flow velocity, head perfusion, and brain oxygenation do not change significantly during upright standing and treadmill ambulation in LBPP. We further hypothesize that GRF decreases linearly with LBPP, whereas gait mechanics remain unaffected. MATERIALS AND METHODS Our study was divided in two parts, first testing our hypothesis on cardiovascular safety of LBPP and, second, focusing on LBPP unweighting effects and its influence on walking and running gait. The The costs of publication of this article were defrayed in part by the payment of page charges. The article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact. 8750-7587/06 $8.00 Copyright © 2006 the American Physiological Society 771 772 LBPP AMBULATION subjects were healthy nonsmokers and none took any medication at the time of the study. All subjects came to the laboratory without any restrictions to their diet and fluid intake. Before testing, subjects were informed about all aspects of the experiment and familiarized with all measurement devices. All subjects provided informed, written consent. The protocol was approved by the University of California, San Diego Human Subjects Institutional Review Board. Subjects wore neoprene shorts with a kayak-type skirt attached at the level of the waist. Subjects then stepped into the LBPP chamber and a comfortable seal was achieved by securing the neoprene skirt over a lip in the top of the chamber. The compliance properties of the skirt were such that subjects were able to walk and run comfortably on an electronically controlled treadmill (model Q65, Quinten Instruments, Seattle, WA) without leaning on the seal for support. Seal height was adjusted level with each subject’s iliac crest, so that the seal itself exerted little or no vertical force in ambient pressure or LBPP. In cardiovascular part of the study, pressure in the chamber was applied in graded manner. In the gait analysis part of the study pressure was adjusted in graded manner until the desired level of unloading was achieved. The subject’s total net GRF was composed of BW reduced by the axial upward force produced by the pressure differential between inside and the outside of the chamber acting across the body cross-sectional area at the waist level (Fig. 1). In the cardiovascular safety component of our study, nine healthy subjects (6 men, 3 women; age 22–55 yr) underwent testing protocol on 2 separate days. The average weight of the subjects tested was 83.8 ⫾ 4.3 kg. On day 1, subjects stood on a spring weighing scale (Sunbeam Products, Boca Raton, FL), and their BW at ambient pressure was measured and recorded. LBPP was then applied in a graded manner at 10, 20, 30, 40, and 50 mmHg with the subjects in stationary standing position. On the basis of our pilot data, each level of LBPP was maintained for 1 min before data collection to allow subjects to acclimatize to the reduced gravity and achieve physiological steady state but with essentially no time interval between the different levels. We found that all recorded parameters reached steady state within this time frame. Data collected in stationary position included GRF and forehead skin microvascular blood flow, measured with laser (Doppler flow meter blood perfusion monitor 403A, Laserflo, Vasamedics, St. Paul, MN). Subjects then exited the chamber and returned later for additional testing. This allowed their cardiovascular parameters to normalize in ambient pressure before additional testing. On day 2 of testing, subjects first stood in the chamber while the LBPP was applied at graded levels of 10, 20, 30, 40, and 50 mmHg. Identical to day 1, each LBPP level was maintained for 1 min before data collection and with no delay between the different levels. Each subject’s HR, systolic blood pressure (SBP), diastolic blood pressure (DBP), brain blood flow velocity, and brain tissue oxygenation were recorded. HR was measured by use of a four-lead ECG monitor (model Q6500, Quinten Instruments), whereas SBP and DBP were measured utilizing a manual cuff applied to the left arm. Near-infrared spectroscopy continuously monitored brain tissue oxygenation under temporal bone (Run-Man CWS-2000, NIM). Brain blood flow velocity through the middle cerebral artery was measured with transcranial Doppler ultrasound (Transpect TCD, Medasonics, Mountain View, CA). To minimize data collection variability, one experimenter obtained all the blood pressure measurements for all the subjects, and another experimenter collected head perfusion, vascular flow velocity, and oxygenation data. After these measurements, the weighing scale was removed from the chamber. The treadmill was started and subjects were instructed to walk at constant speed of 3 mph (1.34 m/s). The LBPP was applied at 0, 25, and 50 mmHg (order randomized). One minute was allowed for acclimatization to LBPP before measurements of HR and blood pressure. Brain blood flow velocity, microvascular flow, and brain tissue oxygenation were not measured during the dynamic part of the test because of large motion artifacts created by an ambulating subject. Six healthy adult men participated in the unweighting and gait analysis part of the study. The mean age of the subjects was 30 yr (range ⫽ 22– 42), mean height was 1.86 m (range ⫽ 1.78 –1.98), and mean weight was 91.2 kg (range ⫽ 76.2–108.4). All subjects were relatively active and had no known gait abnormalities. A spring weighing scale was placed under each subject, and the chamber pressures needed to generate specific levels of unloading (100, 60, and 20% bodyweight) were determined. The scale was then removed and subjects walked at 3 mph (1.34 m/s) and ran at 6 mph (2.68 m/s) while the chamber pressure was adjusted to achieve each of the three BW conditions. Conditions were performed in randomized order for all subjects. It was previously demonstrated that walking kinematics rapidly adapt to simulated reductions in gravity (12); consequently, all data were acquired after 1 min of exercise to allow subjects time to acclimatize to the reduced gravity. Kinematic parameters included GRF; knee, and ankle sagittal ROM; and stride length. Along with walking exercise, running was explored from a comparison standpoint as well as to provide a baseline for future rehabilitation of competitive athletes. The vertical component of GRF was collected bilaterally at 2 kHz by using force-sensitive insoles (Electronic Quantification, 600 Galahad Road, Plymouth Meeting, PA) placed in each subject’s shoes. Force-sensitive insole systems have good correlation and small root mean square error compared with force plate systems (6). Force pads were calibrated using a standard spring scale and a two-point calibration at 0 and 100% static BW. GRF signals were smoothed with a 50-ms Fig. 1. Schematic diagram of the lower body positive pressure (LBPP) treadmill chamber. A buoyant force (F1) equal to the pressure differential (⌬P) between the pressure inside the chamber (P1) and outside the chamber (P2) multiplied by the cross-sectional area of the body and the flexible waist seal (Axy) counteracts the downward gravitational force (Mg), thus reducing the net vertical ground reaction force (GRF). During ambulation, an inertial force (Maz,CM) equal to the mass of the individual multiplied by the body’s acceleration also contributes to the net GRF. J Appl Physiol • VOL 101 • SEPTEMBER 2006 • www.jap.org 773 LBPP AMBULATION simple moving average filter. Peak GRF was defined as the maximum vertical force produced at the foot during the gait cycle. Heel strike and toe off were defined as the time at which the GRF signal exceeded three standard deviations above baseline noise, and temporal markers were placed at each heel strike and toe off. Stride length was calculated by multiplying the time between consecutive heel strikes by the treadmill speed. The positions of reflective markers attached to lateral thigh (midway between greater trochanter and the knee), lateral femoral condyle, lateral malleolus, calcaneus, and forefoot were sampled at 60 Hz using a video motion measurement system (Vicon Motion Systems, Spectrum Point, Lake Forrest, CA). Using these data, dynamic knee and ankle joint angular ROM in the sagittal plane was calculated. Because the pelvis and hip were obscured by the chamber frame, hip ROM data could not be obtained. Dynamic knee ROM was calculated by subtracting the angle of maximum extension from the angle of maximum flexion about the knee during the gait. Ankle ROM was calculated by subtracting the angle of maximum plantar flexion from the angle of maximum dorsiflexion about the ankle. All gait data were time normalized to a percentage progression through a gait cycle using the heel strike from the GRF signal as the beginning and end of each gait cycle. Data were averaged across all subjects to form a composite signal consisting of a mean and variance for each parameter collected. Data are presented as means ⫾ SE for all parameters. Statistical analyses were performed using one-way or two-way ANOVA for initial effects. When significance was detected (P ⬍ 0.05), post hoc individual comparisons were made using the Scheffé’s correction. RESULTS While standing inside the LBPP chamber, subjects’ HR decreased from 83 ⫾ 3 beats/min at ambient pressure to 73 ⫾ 3 beats/min at 50 mmHg LBPP with statistical significance (P ⬍ 0.05) between HR at ambient pressure and that measured at LBPP levels greater than 20 mmHg (Fig. 2A). With initiation of walking at 3.0 mph (1.34 m/s) in ambient pressure, HR increased significantly (P ⫽ 0.009) from 83 ⫾ 3 beats/min at rest to 99 ⫾ 4 beats/min while walking. With addition of the LBPP during walking, HR decreased from 99 ⫾ 4 beats/min at ambient pressure to 84 ⫾ 2 beats/min at 50 mmHg of LBPP with statistically significant decreases (P ⬍ 0.009) observed at both 25 and 50 mmHg of LBPP (Fig. 2B). During standing, SBP trended higher from a resting value of 130 ⫾ 6 mmHg in ambient pressure to 135 ⫾ 6 mmHg at 50 mmHg of LBPP (Fig. 3A). This increase of SBP, however, was not statistically different for the stationary upright subjects at all levels of LBPP (P ⫽ 0.464). Similarly, standing in various LBPP conditions tended to increase DBP from 75 ⫾ 6 mmHg in ambient pressure to 81 ⫾ 5 mmHg at 50 mmHg of LBPP (Fig. 3A), but again the increase was not statistically significant (P ⫽ 0.36). During walking, DBP increased from 73 ⫾ 3 mmHg at ambient pressure to 83 ⫾ 4 mmHg at 50 mmHg of LBPP (P ⫽ 0.053) (Fig. 3B). Blood flow velocity through the left middle cerebral artery, as measured with a transcranial Doppler, did not increase significantly between levels of LBPP ranging from 74.9 ⫾ 8.5 cm/s in ambient pressure to 78.4 ⫾ 10.1 cm/s at 50 mmHg of LBPP (Table 1). Forehead skin microvascular blood flow remained unchanged from 6.4 ⫾ 0.4 to 5.8 ⫾ 0.4 ml䡠min⫺1 䡠100 g⫺1 of tissue at various levels of LBPP. Finally, brain tissue oxygenation varied from 0.4 ⫾ 6.8 mV at ambient pressure to 15.0 ⫾ 10.9 mV at 50 mmHg LBPP without statistical significance associated with this trend (P ⫽ 0.875). J Appl Physiol • VOL Fig. 2. A: heart rate (HR) during standing in various levels of LBPP (mean ⫾ SE). *Statistically significant difference (P ⱕ 0.05) from HR during standing in ambient (0 mmHg LBPP) pressure. B: HR during standing and walking in various levels of LBPP (mean ⫾ SE). *Statistically significant difference (P ⬍ 0.05) from HR during standing in ambient (0 mmHg LBPP) pressure. **Statistically significant difference (P ⬍ 0.05) from HR measured during walking in ambient pressure. Standing subjects’ weight decreased linearly from 84 ⫾ 5 kg at ambient pressure to 13 ⫾ 3 kg at 50 mmHg LBPP. There were significant differences (P ⫽ 0.001) between the subjects’ weight at 0 mmHg and that measured at 10, 20, 30, 40, and 50 mmHg, indicating an inverse relationship between increasing LBPP and the net GRF (Fig. 4). For gait analysis all subjects were able to walk and run comfortably at each of the decreased BW conditions. Peak GRF decreased significantly as LBPP was increased during both walking and running (Fig. 5). Peak GRF during running was significantly higher than peak GRF during walking. Normalized to the peak GRF during walking at 100% BW, the peak GRF recorded during walking at 60% BW was 0.71 (⫾0.06) and walking at 20% BW was 0.30 (⫾0.09). Running at 100% BW was 1.52 (⫾0.10), running at 60% BW was 1.21 (⫾0.08), and running at 20% was 0.58 (⫾0.15) times the peak GRF during walking at 100% BW. LBPP exercise did not significantly change ankle ROM (Fig. 6). Ankle ROM at 100, 60, and 20% BW during walking was 30.6 (⫾9.3), 31.4 (⫾5.2), and 33.9° (⫾6.4), respectively. ROM at 20% BW during running was similar to the ROM at 101 • SEPTEMBER 2006 • www.jap.org 774 LBPP AMBULATION Fig. 4. Weight reduction during stance with increasing LBPP (mean ⫾ SE, n ⫽ 9). *Statistically significant difference (P ⬍ 0.05) compared with that for subjects standing in ambient pressure. Fig. 3. A: blood pressure (BP) in subjects standing in various LBPP levels (mean ⫾ SE). B: BP in subjects standing and walking in various LBPP levels (mean ⫾ SE). significant changes were observed with LBPP during running compared with the 100% BW condition (Fig. 7). Knee ROMs at 100, 60, and 20% BW during running were 57.5 (⫾8.5), 63.2 (⫾12.4), and 55.8 (⫾10.9), respectively. A significant increase in stride length was observed during running compared with walking at all BW conditions, but LBPP produced no significant changes compared with the 100% BW condition (Fig. 8). Stride lengths at 100, 60, and 20% BW during walking were 140.6 (⫾5.3), 148.8 (⫾8.5), and 159.4 cm (⫾9.5), respectively. Stride lengths at 100, 60, and 20% BW during running were 191.7 (⫾11.3), 211.9 (⫾10.8), and 244.7 cm (⫾6.7), respectively. In addition, five of the six subjects exhibited a float phase between steps while walking at 20% BW that is characteristic of a running gait. However, patterns of knee and ankle joint motion for this condition were more consistent with a walking than a running pattern. DISCUSSION 100% BW during walking. There was an expected significant increase in ankle ROM with running compared with walking. Ankle ROM at 100, 60, and 20% BW during running was 44.5 (⫾5.8), 44.8 (⫾1.4), and 36.3 (⫾6.4), respectively. There was a trend to lower dynamic knee ROM with increasing LBPP during walking, although this change was not significant (P ⫽ 0.09). Knee ROM at 100, 60, and 20% BW during walking were 50.2 (⫾7.3), 45.2 (⫾5.1), and 36.7 (⫾4.6), respectively. Knee ROM increased significantly during running compared with walking at 60 and 20% BW, but no Prevalence of conditions such as transient ischemic attack, stroke, cerebral vascular disease, hypertension, and coronary artery disease is high in adult and elderly populations undergoing rehabilitation (24a). Sudden systemic and head blood flow and pressure changes in patients with these medical conditions can produce serious and even catastrophic outcomes. For the LBPP chamber to be effective as a rehabilitation tool, it must safely reduce load in lower extremities, while not provoking brain hemorrhages or other potentially negative cardiovascular effects. Our study confirms our hypothesis that Table 1. Transcranial blood flow velocity, head microcirculatory blood flow, and brain tissue oxygenation in subjects standing in various LBPP levels Chamber Pressure, mmHg Head microcirculatory blood flow, ml䡠min⫺1䡠100 g of tissue⫺1 NIRS oxygenation, mV TCD blood flow velocity, cm/s⫺1 0 10 20 30 40 50 6.4⫾1.2 0.4⫾6.8 74.9⫾8.5 6.1⫾1.0 2.9⫾7.9 77.8⫾8.8 5.9⫾1.1 8.6⫾8.3 80.7⫾8.0 5.8⫾0.9 7.5⫾8.4 80.7⫾8.9 6.1⫾1.0 12.1⫾11.8 77.9⫾8.0 5.8⫾1.0 15.0⫾10.9 78.4⫾10.1 Values are means ⫾ SE. LBPP, lower body positive pressure; NIRS, near infrared spectroscopy; TCD, transcranial Doppler. J Appl Physiol • VOL 101 • SEPTEMBER 2006 • www.jap.org 775 LBPP AMBULATION Fig. 5. Peak vertical GRF during walking and running within LBPP (mean ⫾ SE). Data presented as amplitude normalized to the peak GRF observed during the 100% body weight (BW) walking condition. *Significant difference (P ⬍ 0.05) from the 100% BW condition during walking. †Significant difference (P ⬍ 0.05) from the 100% BW condition during running. ‡Significant difference (P ⬍ 0.05) between a running condition and the corresponding walking condition with the same level of LBPP. Fig. 7. Dynamic knee ROM during walking and running within LBPP (mean ⫾ SE). ‡Running ROM was significantly increased (P ⬍ 0.05) above ROM for walking at the same level of LBPP. mean arterial pressure (MAP), SBP, and DBP, although trending upward, do not significantly increase in standing and treadmill ambulating subjects exposed to 0 –50 mmHg of LBPP. To our knowledge, no one to date has determined whether blood pressure rises during upright, submaximal treadmill exercise in LBPP. Reneman and associates (27) document that changes in pressure around a limb are fully transmitted from the skin to the muscle. Elevation of tissue pressures in lower extremities generated by LBPP slightly increases central venous return and MAP in supine and seated subjects (2, 14, 23). Nishiyasu and coworkers (23, 24) demonstrate that systemic blood pressure response of subjects during seated and supine cycle ergometer exercise in LBPP is dependent on the intravascular fluid shift from lower extremities to torso and the subject’s body position. Similarly, Shi et al. (28) document that MAP increases 3– 6 mmHg at 20 –30 mmHg LBPP and by 4 –15 mmHg at 40 –50 mmHg LBPP in supine subjects. However, Nishiyasu and associates utilize a chamber that encloses subjects in seated or supine position, whereas we study subjects standing and ambulating fully upright on an exercise treadmill. This methodological difference could account for the slight difference in the LBPP effect on cardiovascular parameters observed in our study. Furthermore, we propose that upright treadmill exercise has greater application potential in patient rehabilitation than ergometric or supine exercise. To our knowledge, our study is also the first to assess whether LBPP causes any sudden shifts in microvascular perfusion, oxygenation, and blood flow velocity in the head. Our results confirm our hypothesis that head capillary perfusion, macrovascular circulation, and oxygenation are unchanged by the application of the LBPP. Although changes in these parameters are not detrimental per se, they may suggest that cerebral blood pressure and flow are adversely affected. As previously mentioned, this is especially important when this exercise device is utilized by adult and elderly patients. There- Fig. 6. Dynamic ankle range of motion (ROM) during walking and running within LBPP (mean ⫾ SE). LBPP produced no significant changes in ROM. ‡Running ROM was significantly increased (P ⬍ 0.05) above ROM for walking at the same level of LBPP. Fig. 8. Stride length during walking and running within LBPP (mean ⫾ SE). ‡Running stride length was significantly increased (P ⬍ 0.05) above the stride length for walking at the same level of LBPP. J Appl Physiol • VOL 101 • SEPTEMBER 2006 • www.jap.org 776 LBPP AMBULATION fore, this cerebrovascular safety assessment is a very important first step before the studies on an elderly patient cohort are carried out. Blood flow velocity through the middle cerebral artery does not change with application of different levels of LBPP. This is expected considering autoregulation of brain blood flow. Furthermore, head skin microvascular flow and frontal lobe oxygenation remain unaffected by various levels of LBPP. Independent of intravascular fluid shifts from lower extremities, the heart still must overcome the gravity gradient between the chest and the head, which remains unaffected by LBPP exposure. The small sample size limits us from extrapolating that the head blood pressure and flow are completely unaffected by the LBPP but allows us to conclude that this potential change is within clinically safe range. For this device to be effective as a rehabilitation tool, it should also provide adequate reduction of the forces acting on lower extremities while maintaining gait parameters. The total force imposed on the rehabilitating joint is equal to the sum of the internal or muscular forces and the external forces due to gravity or GRF. Our study shows that by altering the chamber pressure, we can precisely modulate the external load on subject’s lower extremities; hence, 50 mmHg of LBPP provides 85% reduction in static external lower extremity loading. Furthermore, LBPP produces significant reductions of GRF during both walking and running. The observed decrease in peak GRF with increasing LBPP indicates that external forces affecting the lower extremities are reduced. Devices that are currently used for unloading rehabilitation include walkers, parallel bars, therapist-assisted waist belts, overhead suspension harnesses, and water immersion therapy. However, each of these devices has practical limitations. Canes, crutches, walkers, and parallel bars require significant upper body strength to unload the lower extremities, limiting their usefulness in an elderly patient population. Additionally, the amount of weight relieved is neither constant nor quantifiable (17), and the energy expended by the patient using these appliances is higher than that of healthy subjects (10). Therapist-assisted waist belts require a therapist to be present during the patients’ entire rehabilitation. Currently, overhead suspension harness systems are widely used for rehabilitation (7, 15–17, 20, 25, 29, 33). A harness support system has been used effectively in total hip arthroplasty patients to reduce hip extension deficits, improve gait symmetry, and increase strength compared with a standard physical therapy protocol (20). However, there are some concerns about the ability of such systems to support large percentages of BW (⬎75%) comfortably (7, 17). Finally, water immersion therapy may increase the risk of infection and wound dehiscence during the immediate postoperative period, thus delaying the beginning of patient’s active rehabilitation. The viscous drag associated with water immersion therapy probably causes abnormal muscle activation patterns and joint ROMs (3, 9, 18). Although patients treated with water immersion therapy have less joint effusion, exercise in water may not be as effective as traditional land-based therapy in regaining maximum muscle performance (32). In contrast, our results during walking within LBPP suggest that decreased total force in the lower extremity protects healing tissues and musculoskeletal implants in the immediate postoperative period while maintaining normal gait and possibly reducing postoperative edema and joint effusion. J Appl Physiol • VOL Our results for running suggest that LBPP unloads lower body tissues similar to the effect of LBPP during walking exercise or standing. Thus running within LBPP may benefit athletes in their high-demand postoperative rehabilitation, allowing a running workout without the negative effects of increased lower extremity loading. Whether potential reduction in total joint force during rehabilitation is beneficial to protect healing tissues requires further investigation and is beyond the scope of the present study. Our gait analysis also demonstrates that LBPP does not significantly affect ankle or knee ROM. There is a trend to lower dynamic knee ROM with increasing LBPP during walking, but this trend is not statistically significant. Hip ROM and lumbar positions cannot be monitored with our methodological design, because the top of the LBPP chamber obscures the view of hips and waist. Hence, it is conceivable that these gait parameters could be affected by LBPP. Additionally, knee ROM measured during running is lower than previously reported values of 90.5° at 3.4 m/s and 103.1° at 5.0 m/s (21). Slow running speeds (2.68 m/s) in this study probably contribute to this difference. In addition, the waist seal used to maintain positive pressure in the LBPP chamber may limit upward displacement during ambulation, further decreasing knee ROM. However, knee ROM during walking at 100% BW is comparable to previously reported values (31). All variables are measured in healthy subjects without impairments for three reasons. The degree of unloading (reduction of GRF) that can safely and comfortably be achieved with LBPP must be determined before patients attempt to use this modality for rehabilitation. This is critical, as many of the prospective patients have weight-bearing restrictions. Moreover, data detailing the forces experienced by the lower extremities at various pressures are needed to prevent reinjury or exacerbation of existing injuries. From a scientific perspective, analysis of the effects of LBPP on gait is required on subjects without impairments so that future studies may determine which gait effects are due to patient’s injuries and which effects are due to the LBPP apparatus itself. Finally, cardiovascular safety must be established before any patients with preexisting medical conditions are subjected to LBPP exercise. Exercise in LBPP may help prevent muscle atrophy associated with bed rest or disuse, while at the same time decreasing joint forces, protecting healing tissues and prostheses, and decreasing pain associated with ambulation. Some patient groups who may benefit from this form of partial weight bearing during their postoperative recovery include those with ligament and meniscus repairs (13), joint replacements, and complicated fractures. Placing these patients in an LBPP chamber early during their postoperative period may allow them to ambulate earlier in their recovery. Future studies are planned to investigate the efficacy of exercise within LBPP for patients with hip and lower extremity injuries and disorders. In conclusion, our study is the first to examine LBPP effects on cephalic and systemic cardiovascular parameters and to quantify the antigravity and gait effects of LBPP during upright standing, walking, and running. This information provides insight into cardiovascular and cerebrovascular responses to LBPP in upright subjects and provides initial data about the safety of the LBPP chamber as an exercise modality before its use in rehabilitation by adult or elderly postoperative patients. Application of the LBPP to healthy subjects in stationary 101 • SEPTEMBER 2006 • www.jap.org 777 LBPP AMBULATION upright position and ambulating on a treadmill presents minimal risk in terms of head perfusion and vascular flow while offloading lower extremities and maintaining normal gait. ACKNOWLEDGMENTS We thank Brandon R. Macias for technical support. GRANTS This research was supported by the Toby Freedman Endowment Fund, University of California, San Diego Chancellor’s Associates, and by an Orthopaedic Research and Education Foundation Center of Excellence Grant. REFERENCES 1. Berman A and Studenski S. Musculoskeletal rehabilitation. Clin Geriatr Med 14: 641– 665, 1998. 2. Bevegard S, Castenfors J, and Lindblad LE. Effects of changes in blood volume distribution on circulatory variables and plasma rennin activity in men. Acta Physiol Scand 99: 237–245, 1977. 3. Biering-Sørensen F, Schröder AK, Wilhelmsen M, Lomberg B, Nielsen H, and Hoiby N. Bacterial contamination of bath-water from spinal cord lesioned patients with pressure ulcers exercising in the water. Spinal Cord 38: 100 –105, 2000. 4. Bloomfield SA. Changes in musculoskeletal structure and function with prolonged bed rest. Med Sci Sports Exerc 29: 197–206, 1997. 5. Carlsoo S, Dahlof AG, and Holm J. Kinetic analysis of the gait in patients with hemiparesis and in patients with intermittent claudication. Scand J Rehabil Med 6: 166 –179, 1974. 6. Chesnin KJ, Selby-Silverstein L, and Besser MP. Comparison of an in-shoe pressure measurement device to a force plate: concurrent validity of center of pressure measurements. Gait Posture 12: 128 –133, 2000. 7. Colby SM, Kirkendall DT, and Bruzga RF. Electromyographic analysis and energy expenditure of harness supported treadmill walking: implications for knee rehabilitation. Gait Posture 10: 200 –205, 1999. 8. Coventry MB, Beckenbaugh RD, Nolan DR, and Ilstrup DM. 2012 total hip arthroplasties: a study of post-operative course and early complications. J Bone Joint Surg 56A: 273–284, 1974. 9. Dadswell JV. Managing swimming, spa, and other pools to prevent infection. Commun Dis Rep CDR Rev 6: R37–R40, 1996. 10. Deathe AB. Canes, crutches, walkers and wheelchairs: a review of metabolic energy expenditure. Can J Rehab 5: 217–230, 1992. 11. Dickstein R, Nissan M, Pillar T, and Scheer D. Foot-ground pressure pattern of standing hemiplegic patients. Major characteristics and patterns of improvement. Phys Ther 64: 19 –23, 1984. 12. Donelan JM and Kram R. The effect of reduced gravity on the kinematics of human walking: a test of the dynamic similarity hypothesis for locomotion. J Exp Biol 200: 3193–3201, 1997. 13. Eastlack RK, Hargens AR, Groppo ER, Steinbach GC, White KK, and Pedowitz RA. Lower body positive-pressure exercise after knee surgery. Clin Orthop Relat Res 431: 213–219, 2005. 14. Eiken O and Bjurstedt H. Dynamic exercise in man as influenced by experimental restriction of blood flow in the working muscles. Acta Physiol Scand 131: 339 –345, 1987. 15. Finch L, Barbeau H, and Arsenault B. Influence of body weight support on normal human gait: development of a gait retraining strategy. Phys Ther 71: 842– 856, 1991. 16. Gardner MB, Holden MK, Leikauskas JM, and Richard RL. Partial body weight support with treadmill locomotion to improve gait after J Appl Physiol • VOL incomplete spinal cord injury: a single-subject experimental design. Phys Ther 78: 361–374, 1998. 17. Gazzani F, Fadda A, Torre M, and Macellari V. WARD: a pneumatic system for body weight relief in gait rehabilitation. IEEE Trans Rehabil Eng 8: 506 –513, 2000. 18. Gleim GW and Nicholas JA. Metabolic costs and heart rate responses to treadmill walking in water at different depths and temperatures. Am J Sports Med 17: 248 –252, 1989. 19. Hargens AR, Whalen RT, Watenpaugh DE, Schwandt DF, and Krock LP. Lower body negative pressure to provide load bearing in space. Aviat Space Environ Med 62: 934 –937, 1991. 20. Hesse S, Werner C, Seibel H, von Frankenberg S, Kappel EM, Kirker S, and Kading M. Treadmill training with partial body-weight support after total hip arthroplasty: a randomized controlled trial. Arch Phys Med Rehabil 84: 1767–1773, 2003. 21. Milliron MJ and Cavanagh PR. Sagittal plane kinematics of the lower extremity during distance running. In: Biomechanics of Distance Running, edited by Cavanagh PR. Champaign, IL: Human Kinetics, 1990. 22. Newington DP, Bannister GC, and Fordyce M. Primary total hip replacement in patients over 80 years of age. J Bone Joint Surg 72B: 450 – 452, 1990. 23. Nishiyasu T and Ikegami H. Effects of muscle pump on hemodynamics. J Phys Fitness Jpn 34: 167–175, 1987. 24. Nishiyasu T, Nagashima K, Nadel ER, and Mack GW. Effects of posture on cardiovascular responses to lower body positive pressure at rest and during dynamic exercise. J Appl Physiol 85: 160 –167, 1998. 24a.Older Americans, and Cardiovascular Disease-Statistics [Online]. American Heart Association. http://www.americanheart.org/presenter.jhtml? identifier⫽3000936 [2005]. 25. Pillar T, Dickstein R, and Smolinski Z. Walking re-education with partial relief of body weight in rehabilitation of patients with locomotor disabilities. J Rehabil Res Dev 28: 47–52, 1991. 26. Prins J and Cutner D. Aquatic therapy in the rehabilitation of athletic injuries. Clin Sports Med 18: 447– 461, 1999. 27. Reneman RS, Slaaf SW, Lindbom L, Tangelder J, and Arfors KE. Muscle blood flow disturbances produced by simultaneously elevated venous and total muscle tissue pressure. Microvasc Res 20: 307–318, 1980. 28. Shi X, Crandall CG, and Raven PB. Hemodynamic responses to graded lower body positive pressure. Am J Physiol Heart Circ Physiol 265: H69 –H73, 1993. 29. Schindl MR, Forstner C, Kern H, and Hesse S. Treadmill training with partial body weight support in nonambulatory patients with cerebral palsy. Arch Phys Med Rehabil 81: 301–306, 2000. 30. Siddiqi N, Gazzani F, Des Jardins J, and Chao EY. The use of a robotic device for gait training and rehabilitation. Stud Health Technol Inform 39: 440 – 449, 1997. 31. Sutherland DH. Gait Disorders in Childhood and Adolescence. Baltimore, MD: Williams & Wilkins, 1984. 32. Tovin BJ, Wolf SL, Greenfield BH, Crouse J, and Woodfin BA. Comparison of the effects of exercise in water and on land on the rehabilitation of patients with intra-articular anterior cruciate ligament reconstructions. Phys Ther 74: 710 –719, 1994. 33. Visintin M and Barbeau H. The effects of body weight support on the locomotor pattern of spastic paretic patients. Can J Neurol Sci 16: 315–325, 1989. 34. Wall JC and Turnbull GI. Gait asymmetries in residual hemiplegia. Arch Phys Med Rehabil 67: 550 –553, 1986. 101 • SEPTEMBER 2006 • www.jap.org